Abstract
Objective/Hypothesis
Investigate potential problems in the daily life communication of cochlear implant (CI) patients due to the widespread use of face masks in public places during the COVID‐19 pandemic.
Study design
Prospective survey study.
Methods
This study used an online questionnaire about the effects of face masks on daily life communication of adult CI users. The questionnaire consists of three parts: (a) A face mask questionnaire, (b) loneliness question (c) three subdomains of the Nijmegen Cochlear Implant Questionnaire to assess quality of life. The questionnaires were send out on October 20, 2020. Four hundred and seven adult CI users were invited to participate in the study. The survey inclusion was closed on November 5, 2020. The study setting was the Rotterdam Cochlear Implant Center, Erasmus MC, a tertiary referral center in The Netherlands. The loneliness question and Nijmegen Cochlear Implant Questionnaire were analyzed for possible differences between the current situation with masks and the situation before, when masks were not commonly used.
Results
Two hundred and twenty one adult CI users (54% female, mean age 62 years) participated in the study. The face mask questionnaire showed that face masks cause considerable problems in daily life communication of 80% of the participants. Also, CI users tend to feel more lonely and all used subdomains of the Nijmegen Cochlear Implant Questionnaire worsened due to the use of face masks.
Conclusion
The widespread use of face masks greatly complicates the daily life communication of CI users and reduces quality of life.
Level of Evidence
3.
Keywords: cochlear implants, Covid19, facemasks, hearing loss, quality of life

During the COVID‐19 pandemic, the use of face masks is generally mandatory. The effects of the face masks on the daily communication of patients have not yet been studied.Our study shows that face masks have a major influence on the daily communication of cochlear implant users. Patients feel more lonely and the quality of life deteriorates.
1. INTRODUCTION
During the COVID‐19 pandemic, more and more countries recommended or mandated the use of face masks for the general public. The World Health Organization (WHO) also advised governments to encourage the general public to wear masks in specific situations and environments as part of a comprehensive approach to suppress SARS‐CoV‐2 transmission. 1 In the Netherlands, face masks were strongly advised for by the government since the end of September 2020 for (indoor) public spaces.
With masks covering people's faces in these public spaces, speech sounds are attenuated and people cannot see the facial expressions and lip movements essential for everyday communication. Wearing masks is a challenge for everyone, but for people with hearing difficulties, the introduction of face masks in public spaces can be a real problem for their day‐to‐day communication and interactions. This can potentially lead to social withdrawal and, possibly, an increase in social isolation, loneliness, and depression. As some studies already show an increase of loneliness, also because of the other safety measures taken by governments, this is something to seriously consider during this pandemic. 2 , 3
The potential negative impact of face masks on communication in general has recently been appointed in the popular press and in scientific literature. 4 , 5 , 6 , 7 , 8 , 9 Most of these papers address the problem from the perspective of the patient—health worker relationship. Trecca et al (2020) showed preliminary results on the impact of the use of face masks by medical personnel on the perceived difficulties of 59 adults with hearing loss during their hospital visit. Mild to severe problems were experienced by 86.4% of these patients. The main problem with the face masks was the impossibility of lip reading (for 33 people) and sound attenuation was the main problem for 26 people. The survey study of Naylor et al (2020) on the effect of social distance restrictions and safety measures for people with hearing loss who use hearing aids, included some survey questions about face masks. Their results showed that speech understanding problems with the use of face masks are widespread. However, they did not find an association with the degree of hearing loss and the severity of the experienced communication problems due to face masks.
Two studies 10 , 11 investigated the effect of face masks on speech understanding in normal hearing people. Both found decreased speech perception scores in background noises when face masks were worn. Atcherson et al (2017) investigated the effect of conventional and transparent masks on speech perception for persons with and without hearing loss. For normal hearing subjects, no differences between the masks was found, but subjects with hearing loss showed improved speech perception in noise scores when visual input was provided through the use of a transparent surgical mask compared with a conventional mask. 12
In our Cochlear Implant Center Rotterdam, many cochlear implant (CI) users complained about the face masks during their visits to our outpatient clinic because of the negative impact of the face masks on their communication. The impact of the introduction of face masks in public spaces has not yet been studied for patients with CIs. Even for people with normal hearing and for people with hearing aids, speech understanding is impaired by the use of masks. Therefore, we hypothesize that for people with severe to profound hearing loss, the use of masks in public spaces can be devastating. Although cochlear implantation (CI) has caused a major shift in the treatment of severe to profound sensorineural hearing loss, CI users experience poorer sound quality compared to people with normal hearing. Despite the adequate speech intelligibility in quiet that is often achieved, speech understanding in acoustically complex, realistic environments often remains challenging due to reverberation and distracting background noise. 13 , 14 Therefore, many CI users will rely on facial expressions and lip reading in these more complex listening situations in everyday life.
In our research, we aimed to investigate the effect of face masks in public spaces in the Netherlands on adults with severe to profound hearing loss with a CI. The communication and participation problems due to face masks were investigated by means of an online questionnaires. We used a specific face masks questionnaire to examine general problems with the use of face masks, a question to investigate loneliness, and three subdomains of the Nijmegen Cochlear Implant questionnaire 15 to assess quality of life.
2. MATERIALS AND METHODS
2.1. Subjects
A total of 407 adult CI users from the Rotterdam Cochlear Implant Centre were invited to participate in this study via electronic mail. All invited patients had severe to profound hearing loss and were implanted with a CI at the Erasmus University Medical Center, Rotterdam. Participants needed to be fluent in Dutch language and be implanted before July 1, 2020. No other inclusion or exclusion criteria were applied.
Two hundred and twenty one CI users participated in the study, see Table 1 for demographics. Age ranged from 18 to 92 years (group mean age = 62 years; SD = 18 years), 54% was female. All were implanted with either an AB, Medel, Cochlear, or Oticon implant. The participants had used their CI on average 6.9 years (SD = 5.1 years). Forty‐eight (22%) CI users were prelingual deaf, half of whom used sign language in daily life. The participants and non‐participants were comparable in age, age at implantation, and sex but differed significantly in CI experience (P < .001), average CI experience for participants was 7 years and for non‐participants 9 years.
TABLE 1.
Demographics of participants and non‐participants of the study
| Participants | Not participated | P | |
|---|---|---|---|
| Male/Female (n) | 102/119 | 98/88 | .7 |
| Age (y) | 62 (range 18‐92) | 59 (range 18‐100) | .2 |
| Implanted at age (y) | 55 (range 2‐87) | 50 (range 1–90) | .2 |
| CI experience (y) | 7 (range 0.3‐23) | 9 (range 0.3‐28) | <.001 |
2.2. Statement approval of all human procedures
The Medical Ethics Committee of the Erasmus MC has reviewed the research protocol and has judged that the rules laid down in the Medical Research Involving Human Subjects Act do not apply to this research proposal. The study was conducted according to the principles of the Declaration of Helsinki (64th WMA, 2013) and the general Data Protection Regulation.
2.3. Study design and procedures
A prospective observational design was used for the study. After development of the questionnaire the questions were evaluated by a panel of CI specialists of our CI center. Besides, the questionnaires were evaluated by a representative of the Dutch CI patient association. After alterations were made, the online secured questionnaire was built in an online open source survey tool, LimeSurvey© (LimeSurvey GmbH, Hamburg, Germany). The questionnaires were sent to the participants digitally by electronic mail. Participants indicated that they had read the consent text and were willing to participate by clicking a consent button. After informed consent was given, participants were able to complete the questionnaire on an online web page. A few participants asked for the questionnaire on paper which we sent out to them (n = 4). The data collection started on October 20, 2020, the period when face masks were strictly advised by the Dutch government for indoor public spaces and were therefore widely used by the general public. See Table 2 for an overview of the safety measures in the period of this research project. Data collection stopped on November 5, 2020, the day all public spaces were closed by the Dutch government due to stricter security measures.
TABLE 2.
Overview of safety measuring during data collection of this study
| Safety measure | |
|---|---|
| Restaurants and cafes | Closed |
| Visit at home | Maximum of three persons per day |
| Sport | With a maximum of four persons with 1.5 m distance |
| Events | Forbidden |
| Shops | Open (closed from 20:00u) |
| Traveling | As least as possible |
| Face masks | Strongly advised |
2.4. Questionnaires
2.4.1. Face masks questionnaire
We developed a short specific questionnaire on the effect of face masks in public spaces. We asked the participants (a) does the use of face masks hinder your communication? (5‐point scale; never to always) (b) How many communication problems do you experience caused by the use of face masks? (5‐point scale; no problems to very severe problems) (c) If the use of a face mask affects your communication, is it because of poor(er) sound quality/impossibility of lip reading/other (more answers possible)? (d) Are you more insecure in communication because people have to wear face masks? (5‐point scale; never to always). Question two and three are comparable to the questions Trecca et al (2020) used in their questionnaire about face masks in the hospital.
2.4.2. Loneliness
A recent systematic review concluded that there is a link between hearing loss and increased loneliness and social isolation. 16 We hypothesized that the feeling of loneliness may increase if daily life communication deteriorates. Therefore, in the second part of the questionnaire we asked the participants how lonely they felt. Loneliness was assessed by the single question “Do you feel lonely” from the Center for Epidemiological Studies of Depression Scale (CES‐D). 17 Participants answered the question for the current situation and for the situation before the recommendation of the face masks. The responses were one of the following: never / rarely (less than 1 day a week), sometimes (1‐2 days a week), often (3‐4 days a week), or mostly (5‐7 days a week). The “single question” has the advantage of asking directly about the feeling of loneliness and has been used in many previous studies. 18 , 19 , 20
2.4.3. NCIQ
In the third part of the questionnaire, participants completed three subdomains of the Nijmegen Cochlear Implant Questionnaire. 15 The NCIQ is a health‐related quality of life tool for use with CI users. We used the subdomains: “Advanced Sound Perception,” “Activity” and “Social Interaction.” These subdomains were chosen because we expected that face masks in public spaces would affect these subdomains. Each subdomain contains 10 items, formulated as statements with five responses on a Likert‐type scale ranging from “never” to “always.” The subjects had to answer which statement best suited their experiences with regard to the question.
Participants were asked to complete the questions twice in a row. First for the current situation with face masks that are strictly advised in public spaces and second for the situation a few months earlier, when face masks were almost non‐existent in public spaces. Not all questions from the subdomains were expected to be related to the use of face masks, such as the questions about music and phone calls. However, we decided to use all questions from the three domains to be able to compare our results with previous NCIQ data in the literature.
2.5. Data analysis
Before computation of the three subdomains of the NCIQ, the scores for 19 items of the questionnaire that were phrased in opposite form were recoded and the response categories for all items were transformed: 1 = 0, 2 = 25, 3 = 50, 4 = 75, and 5 = 100, both as in the original paper by Hinderink et al (2000). The scores for the subdomains were calculated by adding the scores of at least seven completed items from each subdomain and dividing by the number of items completed. For easy representation of our results, we numbered the NCIQ questions used in our study from 1 to 30, Table S1 displays the questions and the original question numbers from the study of Hinderink et al 2000.
Data interpretation and analysis were performed with SPSS (v25). The data appeared to be non‐normally distributed, therefore non‐parametric statistical methods were used to analyze the differences between current and previous situation with the Wilcoxon Signed Rank test. A Spearman's rank‐order correlation was used to determine the relationship between age, gender, pre‐ or postlingual deafness and the impact of face masks. The Benjamini‐Hochberg method was used to control the false discovery rate for multiple comparisons. 21 The displayed P‐values are corrected for multiple comparisons. A P‐value of <.05 was considered statistically significant.
3. RESULTS
A total of 221 (100%) participants filled in the first part of the questionnaire about the face masks and loneliness in the current situation. The NCIQ subdomains for the current situation was filled in by 220 participants (99.5%). Two hundred and one participants (91%) answered also the loneliness question and the NCIQ for the situation when face masks were not advised and generally used in the public domain. Unfortunately, due to technical issues during the first period of the study, question 20 of the NCIQ was not asked for the situation before face masks were used, resulting in only 48 answers to this question in total.
3.1. Face masks questionnaire
Figure 1 shows the results for the face mask questionnaire. Eighty percent of the participants experienced “regularly” to “almost always” problems with face masks in their communication. The seriousness of the problems was rated as moderate to severe for 83% of the participants. Face masks made 59% of the participants often to almost always feel more insecure about their communication. Forty‐four percent of the participants having problems thought that losing their lip‐reading ability had the most impact on their communication, 14% thought it was the disturbance in sound quality, and for 40% of the participants it was equally important. We also asked if other things were interfering with their communication, three participants replied that the lack of facial expressions bothered them the most, for one person the mandatory distance of 1.5 m had a major impact on the daily communication.
FIGURE 1.
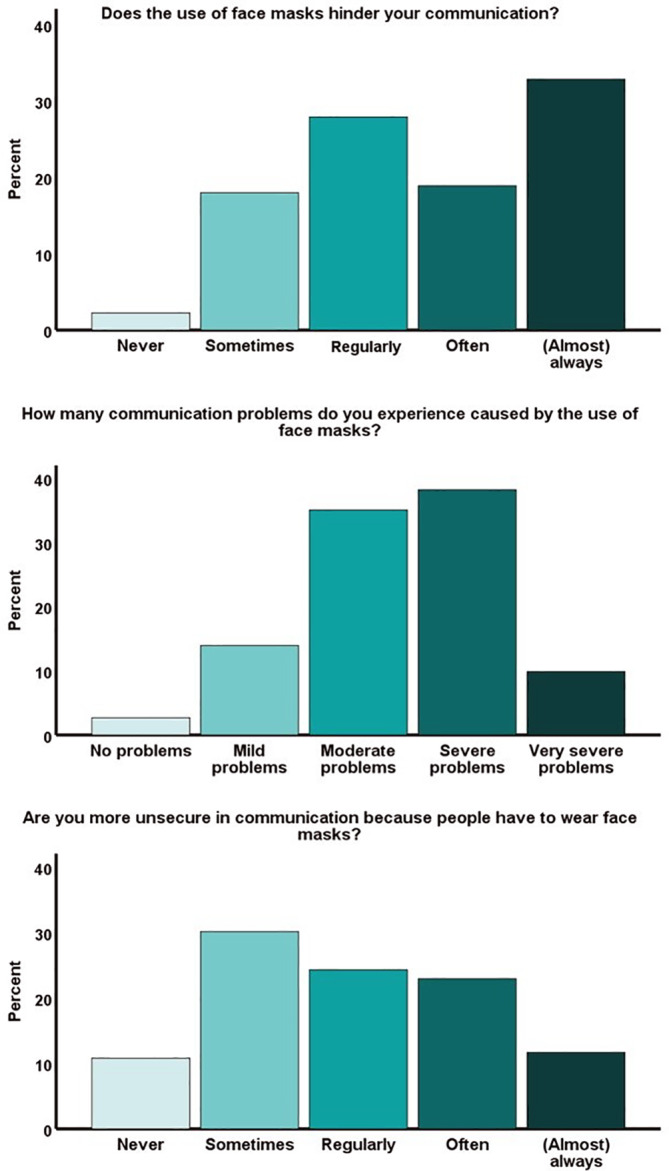
Results for the face mask questionnaire
3.2. Loneliness
Participants scored significantly higher on the loneliness question for the current situation compared with the situation when face masks were not generally worn (Z = −4.892, P < .001), see Table 3. The increase in loneliness was, weakly but significantly, correlated with age and gender (rs = −.205; P = .012 and rs = .151; P = .034, respectively), which means the elderly are less affected during this pandemic and the increase in loneliness is slightly greater among men than women. Prelingually deaf participants also experienced a greater increase in loneliness (rs = −.149; P = .034).
TABLE 3.
Answers on the loneliness question
| Loneliness | Mostly (%) | Often (%) | Sometimes (%) | Never/rarely (%) | P |
|---|---|---|---|---|---|
| Before | 5 (2.5) | 8 (4.0) | 29 (14.4) | 159 (79.1) | <.001 |
| Current situation | 11 (5.0) | 15 (6.8) | 54 (24.4) | 141 (63 |
Note: Before is the situation before face masks were generally used and current situation is the situation with face masks regularly worn in public spaces.
3.3. NCIQ
The scores of the NCIQ subdomains and questions are presented in Table 4 and Figure 2. The NCIQ scores showed significant deterioration in all three subdomains (advanced sound perception: difference in NCIQ score 10 [Z = −8.795; P < .001]; activity: difference 5 [Z = −6.443, P < .001]; social interactions: difference 2 [Z = −4.866; P < .001]). Figure 2 shows that the greatest deterioration is found in questions 1 to 3, the three questions about speech perception (conversation with one person, with two or more people and in a busy shop). The decrease in NICQ scores for the sub domain of advanced sound perception is weakly correlated with age (rs = .290, P < .001), meaning less impact of face masks on NCIQ scores for elderly persons compared with younger participants. No correlation for gender was found, but prelingually deaf participants experienced more impact on the Advanced Sound perception scale (rs = .171, P = .023). For the other NICQ sub domains, no significant correlations were found.
TABLE 4.
The scores of the NCIQ subdomains and separate used questions of the NCIQ
| Current facemask situation | Former situation without facemask | ||||||
|---|---|---|---|---|---|---|---|
| Mean | Median | SD | Mean | Median | SD | P | |
| Sound perception advanced | 40 | 38 | 19 | 50 | 50 | 22 | <.001 |
| Activity | 63 | 66 | 19 | 68 | 72 | 20 | <.001 |
| Social interaction | 66 | 69 | 17 | 68 | 70 | 17 | <.001 |
| Question 1 | 57 | 50 | 32 | 82 | 100 | 24 | <.001 |
| Question 2 | 26 | 25 | 27 | 48 | 50 | 31 | <.001 |
| Question 3 | 25 | 25 | 24 | 46 | 50 | 28 | <.001 |
| Question 4 | 33 | 25 | 32 | 39 | 25 | 36 | .002 |
| Question 5 | 36 | 25 | 30 | 42 | 50 | 34 | <.001 |
| Question 6 | 45 | 50 | 30 | 48 | 50 | 34 | .8 |
| Question 7 | 30 | 25 | 25 | 41 | 50 | 29 | <.001 |
| Question 8 | 57 | 50 | 31 | 63 | 75 | 30 | <.001 |
| Question 9 | 52 | 50 | 30 | 55 | 75 | 32 | .3 |
| Question 10 | 36 | 25 | 33 | 39 | 25 | 36 | .5 |
| Question 11 | 64 | 75 | 30 | 69 | 75 | 30 | <.001 |
| Question 12 | 74 | 75 | 24 | 75 | 75 | 24 | .6 |
| Question 13 | 71 | 75 | 26 | 75 | 75 | 25 | .2 |
| Question 14 | 78 | 75 | 23 | 83 | 75 | 20 | <.001 |
| Question 15 | 66 | 75 | 28 | 74 | 75 | 24 | <.001 |
| Question 16 | 66 | 75 | 29 | 67 | 75 | 28 | .5 |
| Question 17 | 38 | 50 | 33 | 45 | 50 | 33 | <.001 |
| Question 18 | 54 | 50 | 32 | 61 | 75 | 31 | <.001 |
| Question 19 | 56 | 75 | 30 | 64 | 75 | 30 | <.001 |
| Question 20 | 67 | 75 | 30 | 71 | 75 | 24 | .6 |
| Question 21 | 64 | 75 | 27 | 68 | 75 | 25 | .04 |
| Question 22 | 73 | 75 | 30 | 74 | 75 | 30 | .2 |
| Question 23 | 51 | 50 | 32 | 58 | 75 | 30 | <.001 |
| Question 24 | 77 | 75 | 23 | 81 | 75 | 21 | <.001 |
| Question 25 | 70 | 75 | 31 | 75 | 75 | 27 | .003 |
| Question 26 | 23 | 25 | 25 | 23 | 25 | 28 | .9 |
| Question 27 | 74 | 75 | 21 | 75 | 75 | 22 | .8 |
| Question 28 | 75 | 75 | 24 | 75 | 75 | 24 | .8 |
| Question 29 | 75 | 75 | 25 | 78 | 75 | 23 | .2 |
| Question 30 | 77 | 75 | 27 | 78 | 75 | 28 | .8 |
FIGURE 2.
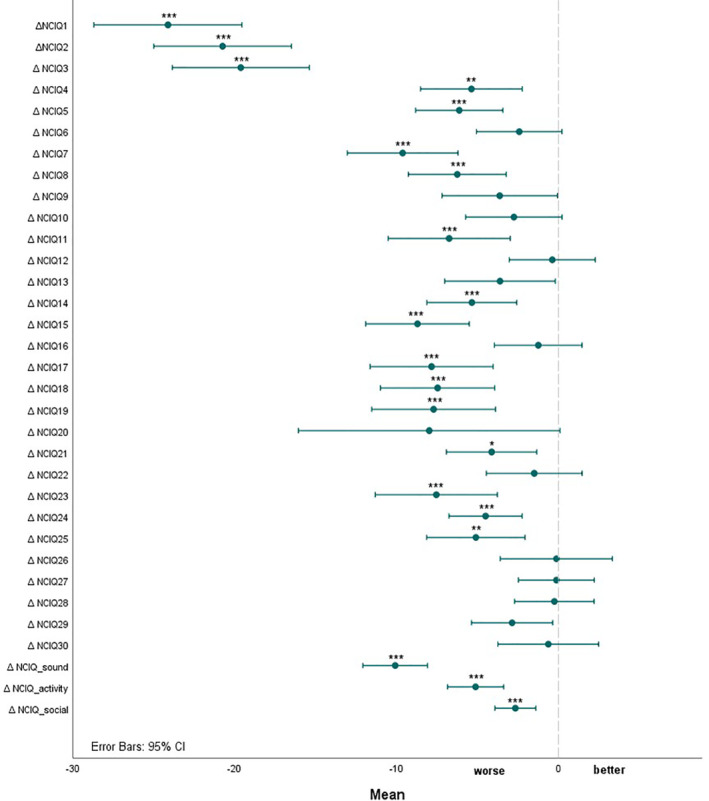
Results for the NCIQ subdomains and separate questions. * P < .05, ** P < .01, ***P < .001. Δ is the difference between the current situation with face masks and the former situation
4. DISCUSSION
In our study, we investigated the effect of face masks in public (indoor) spaces in the Netherlands on adults with severe to profound hearing loss who wear a CI. The results of our study show that the use of face masks in public spaces greatly affects communication for CI users. The specific face mask questionnaire, the loneliness question, and the validated NCIQ questions all point in this direction.
4.1. Face mask questions
As 80% of the participants experience “regularly” to “almost always” problems with daily life communication when people use face masks, this problem is widespread for CI users. Eighty three percent of the CI users experience these problems as moderate to severe. Ninety seven percent does experience some kind of problems, which is comparable with the data of Trecca et al 2020 and Naylor et al (2020). In the study of Naylor et al (2020), 93% of the participants agreed that understanding people wearing face masks is harder because the speech is muffled and 81% agreed with that it is harder because they cannot see their mouth moving. The distortion of speech seems to be the largest cause in their study, which differs from our study. This is possibly because our participants had more severe hearing loss as they wear CIs instead of hearing aids and therefore rely more on lip reading in daily life communication. Sound attenuation due to masks was demonstrated in a study by Corey et al (2020) 22 who tested the acoustic effects of 12 different masks, including face shields and transparent masks. All masks attenuated frequencies above 1 kHz, transparent masks had the worst acoustic performance, and future research is needed to the effect of transparent masks on speech perception for people with hearing loss.
Besides the fact that understanding a speaker who is wearing a face mask poses additional problems, it is also difficult for the CI wearer to wear a face mask because the chance of damage or loss when putting on and taking off the face mask, is quite high. These concerns were also highlighted by the participants in the free text of the questionnaire. This is, therefore, also something to take into account when working with people with CIs or hearing aids.
4.2. Loneliness
The participants in our study tend to feel more lonely with the use of face masks in public spaces, probably due to the deterioration of their daily life communication. Some studies 2 , 3 specific to loneliness during COVID‐19 pandemic found an increase of loneliness due to the security measures taken by the governments, however other studies found stable loneliness prevalence values. 23 , 24 , 25 Our study is a first indication that general use of face masks is possibly one of the factors contributing to loneliness for patients with severe hearing loss during this pandemic. However, other safety measures may also have influenced the feeling of loneliness, as the safety measures when face masks were not commonly worn (during last summer) were different during the situation when face masks were generally worn.
When it comes to loneliness, older people seem a little bit less affected by the safety measures and facemasks than the younger CI users. We hypothesize that these elderly people may already spend less time in large groups and public places, which means that the impact might be a little smaller. In addition, a great deal of national attention was devoted to the loneliness of the elderly during the pandemic, as a result of which some of the elderly may even have received more visits or attention than in the period before the pandemic.
Prelingually deaf participants also experienced an increase in loneliness. These participants often have to rely (entirely) on lip reading and may be very disaffected by the input of the face masks. Also the use of the telephone, to keep in touch with friends and family, is less self‐evident for these participants.
4.3. NCIQ
All three subdomains of the NCIQ showed worse scores for the current situation when compared with the situation before face masks were often used. Especially, the questions about speech understanding deteriorated a lot. When comparing our NCIQ scores with the literature, we found equal or lower scores on the different subdomains compared with norm data in the literature. 15 , 26 , 27 The small differences might be explained by the fact that 22% of our participants were prelingually deafened, which might lower the NCIQ score, especially the “advanced sound perception” subdomain. 28 Besides, more than 50 % of the participants in our study is older than 65 years old, and for the elderly also lower NCIQ values are reported in the literature. 29 The NCIQ is asking about daily activities, for example, group activities. This might have been influenced by other safety measures as well. During the time of the questionnaire, public places and shops were open, but (private) parties or big (work) meetings were forbidden, and sports was only allowed in small groups.
4.4. Strength and limitations
A strength of the study is the relatively high number of participants and the opportunity it offers to give a platform to the seriousness of the communication problems for CI users in the COVID19 pandemic.
Due to the sudden closure of all public spaces by the government on November 5, we decided to end the inclusion of the survey as we thought it could affect our results. However, a longer admission period might have allowed us to achieve a higher response rate.
Because of its urgency, the face mask questionnaire was developed quickly and not validated first as would normally have been done. Due to this quickly development of the questionnaire, test‐retest reliability was not assessed for the new developed questions; however, for the NCIQ, test‐retest reliability was already assessed in the original study of Hinderink et al (2000) and rated as satisfactory.
As we used an online questionnaire only patients were invited who had an electronic mail address and we can imagine that people with more digital skills would be more likely to participate in the survey. However, we provided an option to send it by general mail and only four participants used this possibility.
Due to the rapid development of security measures around COVID‐19, data before face masks were used by the general public was obtained through recall, introducing the possibility of recall bias (ie, the tendency to overestimate and/or overestimate positive or negative past experiences). Recall bias has been extensively researched 30 , 31 and this form of research with current and pre‐pandemic data is widely used during COVID‐19 crisis. 32 , 33 In addition, the NCIQ itself is also used in studies where participants had to fill it in the questionnaire for the current situation (post‐implantation) and the past situation (pre‐implantation) through recall. 15 , 26 , 27 The studies found a strong agreement between the retrospective responses of the CI users regarding their preimplantation NCIQ scores and the NCIQ observed by a control group. The strong resemblance between the CI users and the controls in those studies supports the validity of interpreting retrospective data with the NCIQ.
More research is needed to investigate the effect of face masks on speech perception and sound attenuation. Another point to address in future studies will be the possible solutions for the face masks for patients with hearing loss, like possibly face shields or transparent masks. Also the use of assistive listening devices to overcome the problems for face masks needs to be addressed in future research projects.
5. CONCLUSION
This study shows that the general use of face masks complicates the daily life communication of CI users. It is important that governments and the general public are aware of this problem for people with severe to profound hearing loss. More research is needed to investigate possible solutions like (safe) transparent masks.
CONFLICT OF INTEREST
The authors whose names are listed above report no financial interests or potential conflicts of interest.
Supporting information
Appendix S1: Supporting information
ACKNOWLEDGMENT
The authors gratefully acknowledge all participants of the research project. They also thank Anouk Heine for her help in putting the survey online.
Homans NC, Vroegop JL. Impact of face masks in public spaces during COVID‐19 pandemic on daily life communication of cochlear implant users. Laryngoscope Investigative Otolaryngology. 2021;6:531–539. 10.1002/lio2.578
Funding information Erasmus Universitair Medisch Centrum Rotterdam
BIBLIOGRAPHY
- 1. WHO . Advice on the use of masks in the context of COVID‐19. Available at: file:///C:/Users/919846/AppData/Local/Temp/WHO-2019-nCov-IPC_Masks-2020.4-eng.pdf. Accessed November 16, 2020; 2020.
- 2. van Tilburg TG, Steinmetz S, Stolte E, van der Roest H, de Vries DH. Loneliness and mental health during the COVID‐19 pandemic: a study among Dutch older adults. J Gerontol B Psychol Sci Soc Sci. 2020:1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lee CM, Cadigan JM, Rhew IC. Increases in loneliness among young adults during the COVID‐19 pandemic and association with increases in mental health problems. J Adolescent Health. 2020;67:714‐717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chodosh J, Weinstein BE, Blustein J. Face masks can be devastating for people with hearing loss innovation is urgently needed to ensure clear communication in medical settings. BMJ Brit Med J. 2020;370(8255). [DOI] [PubMed] [Google Scholar]
- 5. McKee M, Moran C, Zazove P. Overcoming additional barriers to care for deaf and hard of hearing patients during COVID‐19. Jama Otolaryngol. 2020;146:781‐782. [DOI] [PubMed] [Google Scholar]
- 6. Park J. Unraveling the invisible but harmful impact of COVID‐19 on deaf older adults and older adults with hearing loss. J Gerontol Soc Work. 2020;63:598‐601. [DOI] [PubMed] [Google Scholar]
- 7. Trecca EMC, Gelardi M, Cassano M. COVID‐19 and hearing difficulties. Am J Otolaryngol. 2020;41:102496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. West JS, Franck KH, Welling DB. Providing health care to patients with hearing loss duringCOVID‐19 and physical distancing. Larynscope Investig. 2020;5:396‐398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Naylor G, Burke LA, Holman JA. Covid‐19 lockdown affects hearing disability and handicap in diverse ways: a rapid online survey study. Ear Hear. 2020;41:1442‐1449. [DOI] [PubMed] [Google Scholar]
- 10. Hampton T, Crunkhorn R, Lowe N, et al. The negative impact of wearing personal protective equipment on communication during coronavirus disease 2019. J Laryngol Otol. 2020;134:577‐581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bandaru SV, Augustine AM, Lepcha A, et al. The effects of N95 mask and face shield on speech perception among healthcare workers in the coronavirus disease 2019 pandemic scenario. J Laryngol Otol. 2020;134:1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Atcherson SR, Mendel LL, Baltimore WJ, et al. The effect of conventional and transparent surgical masks on speech understanding in individuals with and without hearing loss. J Am Acad Audiol. 2017;28:58‐67. [DOI] [PubMed] [Google Scholar]
- 13. Srinivasan AG, Padilla M, Shannon RV, Landsberger DM. Improving speech perception in noise with current focusing in cochlear implant users. Hearing Res. 2013;299:29‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lenarz M, Sonmez H, Joseph G, Buchner A, Lenarz T. Long‐term performance of Cochlear implants in Postlingually deafened adults. Otolaryng Head Neck. 2012;147:112‐118. [DOI] [PubMed] [Google Scholar]
- 15. Hinderink JB, Krabbe PFM, Van den Broek P. Development and application of a health‐related quality‐of‐life instrument for adults with cochlear implants: the Nijmegen Cochlear implant questionnaire. Otolaryngol Head Neck. 2000;123:756‐765. [DOI] [PubMed] [Google Scholar]
- 16. Shukla A, Harper M, Pedersen E, et al. Hearing loss, loneliness, and social isolation: a systematic review. Otolaryngol Head Neck. 2020;162:622‐633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Radloff L. The CES‐D scale: a self‐report depression scale for research in the general population. Appl Psychol Measur. 1977;1:385‐401. [Google Scholar]
- 18. Holmen K, Ericsson K, Winblad B. Loneliness and living‐conditions of the oldest‐old. Scand J Soc Med. 1994;22:15‐19. [DOI] [PubMed] [Google Scholar]
- 19. Jylha M. Old age and loneliness: cross‐sectional and longitudinal analyses in the Tampere longitudinal study on aging. Can J Aging. 2004;23:157‐168. [DOI] [PubMed] [Google Scholar]
- 20. O'Luanaigh C, O'Connell H, Chin AV, et al. Loneliness and cognition in older people: the Dublin healthy ageing study. Aging Ment Health. 2012;16:347‐352. [DOI] [PubMed] [Google Scholar]
- 21. Benjamini Y, Hochberg Y. Controlling the false discovery rate—a practical and powerful approach to multiple testing. J R Stat Soc B. 1995;57:289‐300. [Google Scholar]
- 22. Corey RM, Jones U, Singer AC. Acoustic effects of medical, cloth, and transparent face masks on speech signals. J Acoust Soc Am. 2020;148:2371‐2375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Groarke JM, Berry E, Graham‐Wisener L, McKenna‐Plumley PE, McGlinchey E, Armour C. Loneliness in the UKduring the COVID‐19 pandemic: cross‐sectional results from the COVID‐19 psychological wellbeing study. PLoS One. 2020;15:e0239698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Luchetti M, Lee JH, Aschwanden D, et al. The trajectory of loneliness in response to COVID‐19. Am Psychol. 2020;75:897‐908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020;324:93‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sanchez‐Cuadrado I, Gavilan J, Perez‐Mora R, Munoz E, Lassaletta L. Reliability and validity of the Nijmegen cochlear implant questionnaire in Spanish. Eur Arch Otorhinolaryngol. 2015;272:1621‐1625. [DOI] [PubMed] [Google Scholar]
- 27. Ottaviani F, Iacona E, Sykopetrites V, Schindler A, Mozzanica F. Cross‐cultural adaptation and validation of the Nijmegen cochlear implant questionnaire into Italian. Eur Arch Otorhinolaryngol. 2016;273:2001‐2007. [DOI] [PubMed] [Google Scholar]
- 28. Straatman LV, Huinck WJ, Langereis MC, Snik AFM, Mulder JJ. Cochlear implantation in late‐implanted prelingually deafened adults: changes in quality of life. Otol Neurotol. 2014;35:253‐259. [DOI] [PubMed] [Google Scholar]
- 29. Mosnier I, Bebear JP, Marx M, et al. Improvement of cognitive function after cochlear implantation in elderly patients. JAMA Otolaryngol. 2015;141:442‐450. [DOI] [PubMed] [Google Scholar]
- 30. Neugebauer R, Ng S. Differential recall as a source of bias in epidemiologic research. J Clin Epidemiol. 1990;43:1337‐1341. [DOI] [PubMed] [Google Scholar]
- 31. Bhandari A, Wagner T. Self‐reported utilization of health care services: improving measurement and accuracy. Med Care Res Rev. 2006;63:217‐235. [DOI] [PubMed] [Google Scholar]
- 32. Hong N, Yu W, Xia J, Shen Y, Yap M, Han W. Evaluation of ocular symptoms and tropism of SARS‐CoV‐2 in patients confirmed with COVID‐19. Acta Ophthalmol. 2020;98(5):e649‐e655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Speth MM, Singer‐Cornelius T, Oberle M, Gengler I, Brockmeier SJ, Sedaghat AR. Mood, anxiety and olfactory dysfunction in COVID‐19: evidence of central nervous system involvement? Laryngoscope. 2020;130(11):2520‐2525. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1: Supporting information


