Abstract
Objective
This article aimed to investigate older adults visiting a geriatric institution for a bone density measurement who reported dizziness on a daily or weekly basis (but who are not seeking care for dizziness), according to BPPV, vestibular function, walking abilities, and frequency of falls.
Methods
Patients coming for a bone density measurement answered questions regarding occurrence of dizziness. Patients having dizziness on a daily or weekly basis were considered eligible for the study and invited for investigation at the Ear, Nose, and Throat clinic at Södra Älvsborg Hospital, Sweden. The patients answered questions about history of dizziness, medications, and comorbidities. They were also investigated for BPPV, vestibular deficits using the video head impulse test (vHIT), walking speed, Timed Up and Go test (TUG), and for perception of verticality and horizontality and Romberg test.
Results
A total of 55 patients with dizziness were included. Fifteen (27%) were diagnosed with BPPV. Forty (73%) patients reported falling during the previous year, including 11 with BPPV. Dizziness when turning in bed was more common among patients with BPPV and increased the risk of BPPV 8‐fold.
Conclusion
BPPV is common among older adults with dizziness, including among those not seeking medical care. It is important to identify older adults with BPPV and treat the condition since BPPV may contribute to falls. Asking about dizziness when turning in bed can help to distinguish patients with increased risk for BPPV and older adults with dizziness should be investigated for BPPV even when typical history is lacking.
Level of evidence: 4
Keywords: aged, BPPV, dizziness, vestibular function, walking
1. INTRODUCTION
Dizziness, vertigo, and balance disturbances are a common yet striking problem among older adults. Dizziness is reported to occur in about 30% to 40% of persons older than 70 years 1 , 2 with frequency rising with increasing age. 3 Having dizziness as well as disturbed balance is one of the most important factors contributing to falls among older adults 4 , 5 and loss of balance and stumbling is one of the most common cause of falling. 4 Despite the high prevalence of dizziness in older individuals, the condition is complex to diagnose and manage for many clinicians as dizziness, especially for this age group, can have multiple etiologies. Proprioceptive functions may be affected as well as other sensory inputs related to aging. Dizziness is more common among women than among men, at least in younger age groups, and most vestibular conditions show female predominance. 6
Benign paroxysmal positional vertigo (BPPV) is the single most common cause of dizziness originating from the vestibular system 7 and is characterized by repeated episodes of dizziness triggered by positional changes like lying down or turning in bed. 8 The symptoms of BPPV are caused by displaced otoconia, which are normally attached to the otolithic membrane but may detach and enter the semi‐circular canals where they can send false signals of movement to the brain. 7 The majority of BPPV cases are idiopathic. The condition gets more common with increasing age and is more frequently seen among women, especially after menopause. 6 Association between BPPV and impaired calcium metabolism and low vitamin D levels exists, but current evidence recommends supplementation with vitamin D only for recurrent BPPV. 9 , 10
In contrast to younger individuals with BPPV, older adults suffering from the same condition complain of less rotatory vertigo and more often of nonspecific unsteadiness or dizziness. Older adults with BPPV report fewer spinning sensations, less positional dizziness and more unsteadiness by gait, than younger adults with the same condition. 11 , 12 Because of milder symptoms, BPPV in older adults may go unrecognized, 13 , 14 however, the condition may result in a feeling of unsteadiness and tendency to fall wherefore treatment is recommended to decrease symptoms. 15 , 16 , 17 Diagnosis of BPPV is made through tests, specifically the Dix‐Hallpike test for posterior BPPV (pBPPV) and supine roll‐test for horizontal BPPV (hBPPV), and diagnostic criteria include dizziness and canal‐specific nystagmus during testing. 18
Dizziness is sometimes considered part of the geriatric syndrome and aging. Degeneration of all balance‐enhancing systems and postural control components occurs throughout life, including both sensorial (vestibular, visual, proprioceptal) and muscle strength, flexibility as well as central processing in the brain. 19 Vestibular degeneration and disfunction are more common in older populations than in younger although more poorly examined than cochlear degeneration. 19 The vestibular‐ocular reflex (VOR) enables examination of the vestibular system through the head impulse test or video head impulse test (vHIT). 20 Despite the high frequency of dizziness among older individuals, investigations with vHIT in this population remains relatively unexplored and the procedure can be difficult to perform due to stiffness of the neck. Walking speed can be a valuable indicator of health, overall wellbeing and function, 21 where a walking speed of >1 m/s reflects good health and a good functional status. 22 , 23 Older persons with dizziness or impaired balance tend to walk more slowly and limit their walking speed. 1 , 24 The Timed Up and Go test (TUG) was originally used to predict the probability to fall, and a time of <13.3 seconds is often uses as a cut of to identify fallers. 25
Due to the current state of knowledge, we know that dizziness and impaired balance are frequent issues in older individuals, however, how often these experiences are due to a manageable condition like BPPV is largely unknown. This article aims to investigate occurrence and characteristics of BPPV, vestibular function, walking ability, frequency of falls, medications, and comorbidities in older adults visiting a geriatric institution in Sweden who report at least weekly dizziness but are not seeking care for dizziness.
2. MATERIALS AND METHODS
2.1. Study population
Patients aged 70 to 85 years referred to the geriatric clinic for bone density measurements were provided with a screening questionnaire including questions about occurrence of dizziness, imbalance and previous falls. Patients reporting problems with dizziness or imbalance on a daily or weekly basis were considered eligible for the study and contacted by telephone. If they wanted to participate, they were invited to the Ear, Nose and Throat (ENT) clinic at Södra Älvsborg Hospital, Sweden, a secondary referral center, for a dizziness examination. All patients were examined by the same ENT doctor and asked about symptoms of dizziness and previous falls within the last 12 months, medication use, conditions, and diseases and were then investigated for vestibular function and assessed for walking speed, and the Timed Up and Go (TUG) test. Comorbidities were quantified using the Charlson comorbidity index. 26
2.2. Vestibular function testing
2.2.1. Head shake test and smooth pursuits
All patients underwent a standardized otoneurological examination including evaluation for spontaneous nystagmus with and without video Frenzel goggles, gaze deviation and smooth pursuits, and the head shake test. In the head shake test, the patient was positioned upright with video Frenzel goggles and their head was moved briskly back and forth in the yaw plane for 20 cycles and then abruptly stopped. More than three nystagmus beats to one side was considered a pathological test.
2.2.2. Video head impulse test (vHIT)
The vHIT was performed for lateral semi‐circular canals (SCC) using the EyeSeeCamHIT (Interacoustic) vHIT system. The horizontal canals were evaluated. Patients were instructed to gaze at a target on the wall 1.5 m ahead. Calibration was performed, then the examiner stood behind the patient and quickly moved the patient's head in horizontal (lateral) head impulses within a small angle. 20 Ten correct impulses in each direction were performed. The mean horizontal vHIT gains were recorded. Abnormal criteria were set for horizontal gain values <0.7, corrective saccades peak >100°/s.
2.2.3. Benign paroxysmal positional vertigo (BPPV)
Tests for BPPV included the Dix‐Hallpike test for pBPPV and the supine roll test for hBPPV. 27 The posterior canal was first tested with the patient seated on a bed with the head rotated at 45°. The patient was then quickly lowered into supine position with their neck extended below the level of the bed. With the patient's head extended, the examiner observed the patient for nystagmus. In the supine roll test, the patient's head was turned about 90° to each side while the patient was supine. Video Frenzel goggles with infrared cameras were used during both tests. Tests were considered positive when dizziness and canal specific nystagmus were observed as per the Barany criteria. 18
2.2.4. Subjective visual vertical (SVV) and subjective visual horizontal (SVH) tests
SVV and SVH tests were performed using a bucket with a straight line inside and no visual cues. A plumb line and a protractor on the back of the bucket showed the degree of tilt. The patient was told to look into the bucket to avoid visual cues and to set the straight line to be horizontal as well as vertical. Deviations of 3° or above were considered pathological.
2.3. Walking speed and TUG test
Walking speed was calculated using time consumed for walking a distance of 20 m at a self‐selected walking speed. The TUG test was performed as per. 28 Briefly, the patient was seated in an armchair and the time for the patient to stand up, walk 3 m to a marked line, turn, and then walk back to the chair and sit down again was measured for the entire maneuver. The maneuver was performed twice and the best outcome (shortest time) was used. The Romberg test was performed where the patient stood with the feet together, eyes closed and the arms along the side and the time was registered, maximum time 30 seconds.
2.4. Ethical considerations
The study was conducted according to the Declaration of Helsinki and approved by the Regional Ethical Review Board in Gothenburg, Sweden. Written informed consent for participation in the study was obtained from all participants.
2.5. Statistics
Mean, median, and 95% confidence intervals (CI) of the mean or SD (SD) were calculated for descriptive purposes. Mean and CI or SD were determined for continuous variables while number and percent were calculated for categorical variables. Fisher's exact test was used for comparison between groups for dichotomous variables, Mantel‐Haenszel chi square for ordered categorical variables, and the Mann‐Whitney U‐test for continuous variables. To identify variables indicative of having a BPPV diagnosis, logistic regression analyses were performed. Results were presented as odds ratios with 95% CI, P value and area under the receiver operating characteristic (ROC) curve. All significance tests were two‐sided and conducted at 5% significance level. SAS 9.4 was used for analyses.
3. RESULTS
Of the 380 patients who received the screening questionnaire, a total of 241 answered and returned the questionnaire at their bone density measurement appointment. Of those, 170 initially reported interest to participate in the study and 71 declined participation. Of the 170 patients who expressed interest, 113 reported problems with dizziness and 57 had no problems with dizziness. In total, 74 patients met the inclusion criteria, that is, having dizziness as often as daily or weekly, and 55 patients (74.3%) agreed to come for investigation regarding dizziness and were thus included in the study (Figure 1). Nine patients could not be reached due to invalid phone number (n = 7) or incomplete personal identity number (n = 2), while a further 10 patients were too sick to participate (n = 7) or otherwise declined due to too far to travel (n = 2) or not able to communicate in Swedish (n = 1).
FIGURE 1.
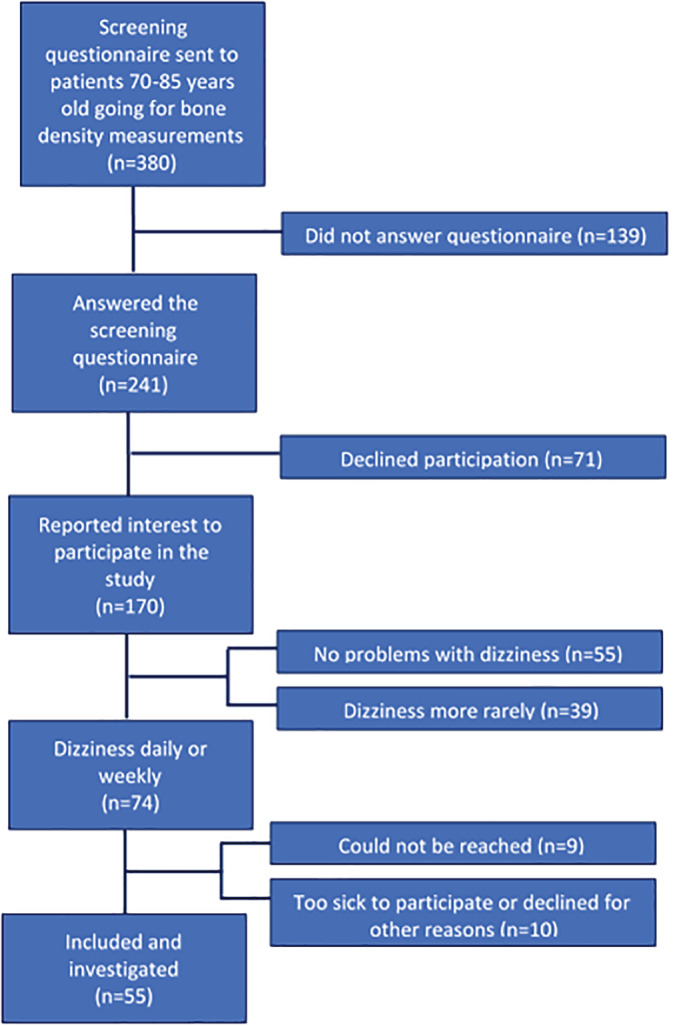
Population flow chart over study inclusion
3.1. BPPV
BPPV was identified among 15 (27%) patients during testing (Table 1). Two‐thirds of these patients (n = 10) had pBPPV and five had hBPPV. Two‐thirds of the patients (n = 10) with confirmed BPPV reported dizziness when lying down and/or turning in bed. Of the questions and tests performed, univariable analysis revealed a significant relationship between a positive BPPV diagnosis and experiencing dizziness when lying down and/or turning in bed. The odds ratio of having BPPV if reporting dizziness when turning in bed was 8.23 (95% CI 2.1‐32.2) and 3.94 (95% CI 1.1‐13.8) if having dizziness when lying down in bed (Table 2). Eleven (73%) patients with BPPV reported feeling unsteadiness when walking and 53% reported dizziness problems on a daily basis.
TABLE 1.
Descriptive characteristics of the study cohort
| Characteristics of the study cohort | Total n = 55 | Dizziness no BPPV n = 40 | Dizziness BPPV n = 15 | P value |
|---|---|---|---|---|
| Women | 52 (95) | 38 (95) | 14 (93) | 1.0 |
| Men | 3 (5) | 2 (5) | 1 (7) | |
| Age (years) | ||||
| Mean (SD) | 78 (4) | 78 (4.5) | 79 (3.8) | .2 |
| Median | 77 | 77 | 80 | |
| Dizziness how often | ||||
| Every day, n (%) | 34 (62) | 26 (65) | 8 (53) | .4 |
| Every week, n (%) | 21 (38) | 14 (35) | 7 (47) | |
| Dizziness symptoms since how long ago: | ||||
| <6 months | 30 (63) | 24 (72) | 6 (40) | .5 |
| 6‐12 months | 11 (23) | 5 (15) | 6 (40) | |
| 1‐2 years | 3 (6) | 2 (6) | 1 (7) | |
| >2 years | 4 (8) | 2 (6) | 2 (13) | |
| Dizziness when lying down in bed, n (%) | 13 (24) | 9 (23) | 8 (53) | .07 |
| Dizziness when turning in bed, n (%) | 16 (29) | 7 (18) | 9 (64) | .002 |
| Dizziness when lying down and/or turning in bed, n (%) | 22 (40) | 12 (30) | 10 (67) | .03 |
| Duration of dizziness | ||||
| Seconds | 31 (61) | 24 (65) | 7 (50) | .7 |
| Minutes | 13 (26) | 8 (22) | 5 (36) | |
| Hours | 2 (4) | 1 (3) | 1(7) | |
| Continuously | 5 (10) | 4 (11) | 1(7) | |
| Unsteadiness when walking | 44 (80) | 33 (83) | 11 (73) | .5 |
| Dizziness resulting in stopping activities, n (%) | 34 (60) | 24 (60) | 10 (67) | .8 |
| Fallen last year, mean (SD) | 2.0 (2.1) | 2.0 (2.1) | 2.1 (2.3) | .8 |
| Number of falls in previous year, n (%) | ||||
| 0 | 15 (27) | 11 (28) | 4 (27) | .9 |
| 1 | 12 (22) | 7 (18) | 5 (33) | |
| 2 | 10 (18) | 9 (23) | 1 (7) | |
| 3 | 10 (18) | 8 (20) | 2 (13) | |
| >3 | 8 (15) | 5 (13) | 3 (20) | |
| Spontaneous nystagmus, n (%) | 4 (9) | 3 (8) | 1 (7) | 1.0 |
| Pathological head shake test (>3 nystagmus beats), n (%) | 5 (9) | 3 (8) | 2 (13) | .6 |
| Saccadic smooth pursuits, n (%) | 28 (51) | 20 (50) | 8 (53) | 1.0 |
| Walking 20 m, mean time seconds (SD) | 20.5 (5.2) | 1.05 (0.22) | 0.95 (0.20) | |
| Median (min; max) | 1.08 (0.53; 1.67) | 1 (0.49; 1.18) | .2 | |
|
Timed up and go, mean time seconds (SD) Median (min; max) |
12 (3.9) 12 (6; 26) |
12 (4) 12 (6; 26) |
13 (5) 12 (7; 25) |
.6 |
| Romberg, n (%) | ||||
| 0‐10 seconds | 3 (6) | 2 (6) | 1 (8) | .5 |
| 11‐20 seconds | 2 (4) | 1 (3) | 1 (8) | |
| 21‐30 seconds | 43 (90) | 39 (92) | 10 (83) | |
| Subjective visual vertical, n (%) | ||||
| < ±3 normal | 46 (87) | 35 (88) | 11 (85) | 1.0 |
| ≥ ±3 | 7 (13) | 5 (13) | 2 (15) | |
| Subjective visual horizontal, n (%) | ||||
| < ±3 normal | 45(85) | 34 (85) | 11 (85) | 1.0 |
| ≥ ±3 | 8 (15) | 6 (15) | 2 (15) | |
| vHIT, n (%) | 1.0 | |||
| ≥0.7 normal | 30 (79) | 6 (21) | 11 (20) | |
| <0.7 | 8 (21) | 22 (79) | 2 (80) | |
| Number of medications, n (%) | ||||
| 0 | 11 (20) | 5 (13) | 6 (40) | .09 |
| 1‐4 | 20 (36) | 16 (40) | 4 (27) | |
| 5‐8 | 16 (29) | 13 (33) | 3 (20) | |
| >8 | 8 (15) | 6 (15) | 2 (13) | |
| Charlson comorbidity index, mean (SD) | 0.58 (0.70) | 0.54 (0.68) | 0.73 (0.8) | |
| Median (highest; lowest) | 0.5 (0; 2) | 0 (0; 2) | 1 (0; 2) | .4 |
Note: P values based on Fisher's exact test for dichotomous variables and Mantel‐Haenszel chi square‐test for continuous variables. P values representing differences between patients with and without BPPV.
Abbreviation: BPPV, Benign paroxysmal positional vertigo.
TABLE 2.
Univariable analysis of questions, tests, and diagnosis of BPPV (n = 15) in a cohort of older adults with dizziness (total n = 55)
| Variable | Value | n (%) of events | OR (95% CI) BPPV | P value | Area under ROC‐curve (95% CI) |
|---|---|---|---|---|---|
| Dizziness when lying down in bed |
No Yes |
7 (18) 8 (47) |
3.94 (1.1‐13.8) |
0.033 |
0.65 (0.5‐0‐8) |
| Dizziness when turning in bed |
No Yes |
9 (56) 5 (15) |
8.23 (2.1‐32.2) |
0.0025 |
0.73 (0.6‐0.9) |
| Dizziness how often |
Every day Every week |
8 (23) 7 (33) |
1.63 (0.49‐5.2) |
0.43 |
0.56 (0.4‐0.7) |
| Duration of dizziness |
Seconds Minutes Hours Continuously |
2 (22) 5 (38) 1 (50) 1 (50) |
1.14 (0.6‐2.1) |
0.69 |
0.56 (0.4‐0.7) |
| Romberg test |
0‐10 seconds 11‐20 seconds 21‐30 seconds |
1 (33) 1 (50) 10 (23) |
0.69 (0.2‐2.2) |
0.52 |
0.54 (0.4‐0.7) |
| SVV/SVH |
< ±3 norm ≥ ±3 |
12 (28) 3 (25) |
0.86 (0.2‐3.7) |
0.84 |
0.51 (0.4‐0.6) |
| vHIT |
≥0.7 normal <0.7 |
13 (28) 2 (25) |
0.87 (0.16‐4.9) |
0.88 |
0.51 (0.4‐0.6) |
| Walking speed |
<1 m/second ≥1 m/second |
7 (32) 5 (18) |
0.47 (0.1‐1.7) |
0.26 |
0.59 (0.4‐0.7) |
| Timed Up and Go test |
<10 second 11‐20 second >20 second |
4 (20) 7 (25) 1 (25) |
1.25 (0.4‐3.6) |
0.68 |
0.54 (0.4‐0.7) |
| Charlson comorbidity index |
0 1 2 |
7 (24) 5 (28) 3 (43) |
1.46 (0.6‐3.3) |
0.37 |
0.56 (0.4‐0.7) |
| Number of medications |
0 1‐5 > 5 |
6 (54) 5 (21) 4 (20) |
0.46 (0.2‐1.08) |
0.073 |
0.64 (0.5‐0.8) |
Abbreviations: BPPV, benign paroxysmal positional vertigo; CI, confidence interval; OR, odds ratio; ROC, receiver operating characteristic.
3.2. Vestibular tests and BPPV
Eight patients (22%) demonstrated pathological gain on horizontal testing of the vHIT. There was no significant difference observed between patients with BPPV and no BPPV in vestibular tests (vHIT, SVV/SVH) (Tables 1 and 2), nor regarding vestibular disfunction defined as pathological vHIT (horizontal gain <0.7) or reported duration of symptoms of dizziness. Two patients with BPPV had pathological vHIT (Table 1).
3.3. Walking tests and falls
The mean time for walking 20 m was 20.5 seconds (Table 1), or a mean walking speed of 1 m/s. Twenty (39%) patients managed the TUG test under 10 seconds. No significant difference regarding walking speed and TUG was observed between the group of patients with BPPV compared to patients without BPPV (Table 2). Twenty‐two (44%) patients had a walking speed of less than 1 m/s. No significant differences were seen between patients with low (<1 m/s) or normal (>1 m/s) walking speed regarding results on vestibular tests, including vHIT, SVV/SVH or having BPPV (Table 2). A total of 40 (73%) patients reported experiencing at least one fall during the previous year and 18 (33%) had fallen three times or more (Table 1). There was no significant difference regarding the number of falls among those with or without BPPV.
3.4. Characteristics of conditions and diseases
The diseases and conditions of the patients are listed in Table 3, where several showed multimorbidity and were diagnosed with more than one condition.
TABLE 3.
Characteristics of conditions and diseases of the study cohort
| Diagnosis potentially affecting balance | |
| BPPV, n (%) | 15 (27) |
| Central neurological disorder, n (%) | |
| Parkinson | 2 (4) |
| Dementia | 3 (5) |
| Prior stroke or multiple TIA | 4 (7) |
| Meniere's disease, n (%) | 1 (2) |
| Otosclerosis, n (%) | 2 (4) |
| Bilateral vestibulopathies, n (%) | 3 (5) |
| Unilateral vestibulopathies, n (%) | 2 (4) |
| Normal otoneurological examination, n (%) | 19 (35) |
| Comorbidity | |
| Rheumatoid arthritis, n (%) | 7 (13) |
| Diabetes, n (%) | 5 (9) |
| Polymyalgia rheumatic, n (%) | 10 (18) |
| Joint problems/back pain, n (%) | 29 (53) |
| Hypertonia, n (%) | 29 (53) |
| Osteoporosis, n (%) | 25 (45) |
| Atrial fibrillation, n (%) | 9 (16) |
| Hypothyroidism, n (%) | 5 (9) |
| Vision impairment, n (%) | 15 (27) |
| Glaucoma | 5 (9) |
| Cataract | 9 (16) |
| Other | 5 (9) |
| Daily use of walking aids, n (%) | 20 (36) |
| walker | 13 (24) |
| walking stick | 7 (13) |
| Use of wheelchair | 2 (4) |
Abbreviations: BPPV, benign paroxysmal positional vertigo; TIA, transient ischemic attack.
4. DISCUSSION
This study investigated a group of older adults coming to the geriatric clinic for bone density measurements, who reported dizziness on a daily or weekly basis, but who did not seek medical care for their symptoms. Following testing, as many as 27% of these older adults with dizziness were diagnosed with BPPV. We also found that vestibular impairment, measured with vHIT, as well as impairment in perception of verticality and horizontality, are common among seniors with dizziness and unsteadiness.
Meeting patients with dizziness and unsteadiness can be frustrating for clinicians since these conditions can have several etiologies in older patients, while serving as major contributors to falls and potential injuries. Finding persons with extended risk for falls for preventive interventions can be cost effective and reduce suffering. Accidental falls generate around 300 000 health care visits annually in Sweden of which 1700 (2%) patients die in fall‐related injuries 29 ; the majority of these patients are over 75 years of age.
BPPV is a common cause of dizziness, especially among older women, 6 , 30 and is a condition that in most cases can easily be treated and managed through canalith reposition maneuvers (CRM), such as Epley's or Semont's manuevers. 17 Treatment is highly recommended to reduce symptoms. 17 The most effective question to distinguish patients with BPPV from those not having other causes of dizziness, was asking about dizziness when turning in bed. Reporting dizziness when turning in bed enhanced the risk of BPPV diagnosis by eight times, and thus this question can assist the examiner when investigating older adults for dizziness.
As many as 73% of patients included in this study had fallen due to dizziness during the past year and half of them had fallen twice or more. This is a considerably higher frequency of falls in dizzy patients compared to other similar age groups, where an estimate of 30% to 40% of adults over 70 years of age fall annually is reported. 2 , 31 Our findings highlight the importance of identifying older adults with dizziness and engaging them in fall prevention programs to help them avoid fall‐related accidents and injuries.
Dizziness of all causes often results in a feeling of unsteadiness and a tendency to fall, and being dizzy is connected to a reduction in health‐related quality of life. 30 Huebner et al showed significant improvement of symptoms measured with the Dizziness Handicap Inventory scale after treatment with canalith repositioning maneuvers. 32 Some older adults, as well as clinicians, consider dizziness a part of aging and therefore not treatable. As a result, older adults tend to adapt to their condition by avoiding situations that may cause dizziness. In this study, 27% of patients had previous undetected BPPV and had not been seeking medical care for their symptoms, even though the dizziness symptoms made them stop doing activities. As BPPV is curable in most people, it is of great importance for every clinician meeting older people with dizziness and balance problems to have knowledge of BPPV testing and treatment options and to test for the condition in every patient after cardiac and vascular or neurological causes have been eliminated.
Vestibular decline measured with vHIT was found among one‐fifth of the patients herein. Patients with vestibular impairment may benefit from vestibular rehabilitation, also in older ages. 33 For example, Jung et al showed that vestibular rehabilitation therapy for older adults can reduce symptoms of dizziness also of unspecific origin, which is why this form of exercise should be widely considered. 34 As vestibular impairment is so frequent, vestibular training together with balance and weight training may be a way to reduce dizziness symptoms, enhance balance, and prevent falls in older populations. 35 , 36
There were no statistically significant differences between patients with or without BPPV in terms of number of falls, walking tests (TUG, 20 m), or vestibular tests (vHIT, SVV/SVH). However, the investigated patients were similar in that they all reported dizziness on a daily or weekly basis. The groups compared in this study are small and it is possible that a larger study population would have yielded statistically significant results.
Older adults with dizziness reported on a daily or weekly basis can have multiple causes of dizziness as well as vestibular impairment. It is of importance to widely test all older adults with dizziness using positioning tests to identify BPPV when present. Reported dizziness when turning in bed may enhance the examination findings for the condition.
4.1. Strengths and limitations
This is one of few studies investigating older adults not actively seeking medical care for dizziness, by using otoneurological examinations including testing for BPPV with video Frenzel goggles and vHIT. One limitation is the small population included in the study and the skewed gender distribution with more women than men. The reason for more women included in the study is due to patient selection; more women require bone measurements (original population for selection) and more women than men reported dizziness on a daily or weekly basis. Not all patients completed all investigations as some had too poor function to complete walking tests and some patients did not give their consent for vHIT or had too fragile or stiff of a neck to perform this test.
5. CONCLUSION
BPPV is a common cause of dizziness among older adults not seeking medical care for dizziness. As BPPV is often treatable, it is important to identify older adults with BPPV and treat the condition since BPPV may contribute to falls. Asking about dizziness when turning in bed can help to distinguish patients with increased risk for BPPV, but older adults with dizziness should be investigated for BPPV even if no typical medical history exists.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ACKNOWLEDGMENTS
The authors thank Mattias Molin for statistical support. The study was financed by grants from the Swedbank Sjuhärad foundation as well as Local Research and Development Council, Södra Älvsborg, the Amlöv's foundation.
Lindell E, Karlsson T, Kollén L, Johansson M, Finizia C. Benign paroxysmal positional vertigo and vestibular impairment among older adults with dizziness. Laryngoscope Investigative Otolaryngology. 2021;6:488–495. 10.1002/lio2.566
Funding information Rune och Ulla Amlövs Stiftelse för Neurologisk och Reumatologisk Forskning; Södra Älvsborgs Sjukhus; Västra Götalandsregionen
REFERENCES
- 1. Kollen L, Horder H, Moller C, Frandin K. Physical functioning in older persons with dizziness: a population‐based study. Aging Clin Exp Res. 2017;29:197‐205. [DOI] [PubMed] [Google Scholar]
- 2. Lindell E, Kollen L, Johansson M, et al. Dizziness and its association with walking speed and falls efficacy among older men and women in an urban population. Aging Clin Exp Res. 2020;32:1049‐1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jonsson R, Sixt E, Landahl S, Rosenhall U. Prevalence of dizziness and vertigo in an urban elderly population. J Vestib Res: Equilib Orient. 2004;14:47‐52. [PubMed] [Google Scholar]
- 4. Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(Suppl 2):ii37‐ii41. [DOI] [PubMed] [Google Scholar]
- 5. Boelens C, Hekman EE, Verkerke GJ. Risk factors for falls of older citizens. Technol Health Care: Off J Eur Soc Eng Med. 2013;21:521‐533. [DOI] [PubMed] [Google Scholar]
- 6. Hülse R, Biesdorf A, Hörmann K, et al. Peripheral vestibular disorders: an epidemiologic survey in 70 million individuals. Otol Neurotol. 2019;40:88‐95. [DOI] [PubMed] [Google Scholar]
- 7. Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999;341:1590‐1596. [DOI] [PubMed] [Google Scholar]
- 8. Lindell E, Finizia C, Johansson M, Karlsson T, Nilson J, Magnusson M. Asking about dizziness when turning in bed predicts examination findings for benign paroxysmal positional vertigo. J Vestib Res: Equilib Orient. 2018;28:339‐347. [DOI] [PubMed] [Google Scholar]
- 9. Rhim GI. Serum vitamin D and recurrent benign paroxysmal positional vertigo. Laryngosc Investig Otolaryngol. 2016;1:150‐153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. AlGarni MA, Mirza AA, Althobaiti AA, Al‐Nemari HH, Bakhsh LS. Association of benign paroxysmal positional vertigo with vitamin D deficiency: a systematic review and meta‐analysis. Eur Arch Oto‐rhino‐laryngol. 2018;275:2705‐2711. [DOI] [PubMed] [Google Scholar]
- 11. Piker EG, Jacobson GP. Self‐report symptoms differ between younger and older dizzy patients. Otology Neurotol. 2014;35:873‐879. [DOI] [PubMed] [Google Scholar]
- 12. Batuecas‐Caletrio A, Trinidad‐Ruiz G, Zschaeck C, et al. Benign paroxysmal positional vertigo in the elderly. Gerontology. 2013;59:408‐412. [DOI] [PubMed] [Google Scholar]
- 13. Kollen L, Frandin K, Moller M, Fagevik Olsen M, Moller C. Benign paroxysmal positional vertigo is a common cause of dizziness and unsteadiness in a large population of 75‐year‐olds. Aging Clin Exp Res. 2012;24:317‐323. [DOI] [PubMed] [Google Scholar]
- 14. van der Zaag‐Loonen HJ, van Leeuwen RB, Bruintjes TD, van Munster BC. Prevalence of unrecognized benign paroxysmal positional vertigo in older patients. Eur Arch Oto‐rhino‐laryngol. 2015;272:1521‐1524. [DOI] [PubMed] [Google Scholar]
- 15. Gananca FF, Gazzola JM, Gananca CF, Caovilla HH, Gananca MM, Cruz OL. Elderly falls associated with benign paroxysmal positional vertigo. Braz J Otorhinolaryngol. 2010;76:113‐120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jumani K, Powell J. Benign paroxysmal positional vertigo: management and its impact on falls. Ann Otol Rhinol Laryngol. 2017;126:602‐605. [DOI] [PubMed] [Google Scholar]
- 17. Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014;Cd003162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. von Brevern M, Bertholon P, Brandt T, et al. Benign paroxysmal positional vertigo: diagnostic criteria. J Vestib Res: Equilib Orient. 2015;25:105‐117. [DOI] [PubMed] [Google Scholar]
- 19. Ji L, Zhai S. Aging and the peripheral vestibular system. J Otol. 2018;13:138‐140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Halmagyi GM, Chen L, MacDougall HG, Weber KP, McGarvie LA, Curthoys IS. The video head impulse test. Front Neurol. 2017;8:258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rydwik E, Bergland A, Forsen L, Frandin K. Investigation into the reliability and validity of the measurement of elderly people's clinical walking speed: a systematic review. Physiother Theory Pract. 2012;28:238‐256. [DOI] [PubMed] [Google Scholar]
- 22. Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Abellan van Kan G, Rolland Y, Andrieu S, et al. Gait speed at usual pace as a predictor of adverse outcomes in community‐dwelling older people an international academy on nutrition and aging (IANA) task force. J Nutr Health Aging. 2009;13:881‐889. [DOI] [PubMed] [Google Scholar]
- 24. Lindell E, Kollén L, Johansson M, et al. Dizziness and its association with walking speed and falls efficacy among older men and women in an urban population. Aging Clin Exp Res. 2020;32:1049‐1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shumway‐Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community‐dwelling older adults using the timed up & go test. Phys Ther. 2000;80:896‐903. [PubMed] [Google Scholar]
- 26. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373‐383. [DOI] [PubMed] [Google Scholar]
- 27. Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003;169:681‐693. [PMC free article] [PubMed] [Google Scholar]
- 28. Browne W, Nair BKR. The timed up and go test. The Medical Journal of Australia. 2019;210:13‐14.e11. [DOI] [PubMed] [Google Scholar]
- 29. Shylander J. Fallolyckor. Myndigheten för samhällsskydd och beredskap; 2014.
- 30. Lindell E, Kollén L, Johansson M, et al. Benign paroxysmal positional vertigo, dizziness, and health‐related quality of life among older adults in a population‐based setting. Eur Arch Oto‐rhino‐laryngol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. WH Organization . WHO Global Report on Falls Prevention in Older Age. WHO Library Cataloguing‐in‐Publication Data; 2007. [Google Scholar]
- 32. Huebner AC, Lytle SR, Doettl SM, Plyler PN, Thelin JT. Treatment of objective and subjective benign paroxysmal positional vertigo. J Am Acad Audiol. 2013;24:600‐606. [DOI] [PubMed] [Google Scholar]
- 33. MN MD, Hillier SL. Vestibular rehabilitation for unilateral peripheral vestibular dysfunction. Cochrane Database Syst Rev. 2015;1:Cd005397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jung JY, Kim J‐S, Chung PS, Woo SH, Rhee CK. Effect of vestibular rehabilitation on dizziness in the elderly. Am J Otolaryngol. 2009;30:295‐299. [DOI] [PubMed] [Google Scholar]
- 35. Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;1:Cd012424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Moncada LVV, Mire LG. Preventing falls in older persons. Am Fam Phys. 2017;96:240‐247. [PubMed] [Google Scholar]


