Abstract
Background:
In this study, the basic criteria, models, and indicators of intersectoral collaboration in health promotion were investigated to facilitate the implementation of collaboration.
Methods:
This scoping review was conducted using datasets of Embase, Web of Science, Scopus, and PubMed, and search engines of Google, Google Scholar, and ProQuest.
Results:
52 studies were included, and 32 codes in Micro, Meso, and Macro level, were obtained. Micro-level criteria had the highest frequency. Among the models used in the reviewed studies, social network analysis, Diagnosis of Sustainable Collaboration, Bergen, and logic models had the highest frequency. Among the indicators studied, the number of participants and the level of collaboration as well as its sustainability were the most frequent indicators.
Conclusion:
The findings identified the most important and widely used criteria, models, and indicators of intersectoral collaboration in health promotion which can be useful for decision-makers and planners in the domain of health promotion, in designing, implementing, and evaluating collaborative programs.
Keywords: Intersectoral collaboration, Health promotion, Scoping review, Model, Indicator, Criteria
Introduction
Various population health approaches are available, including health promotion, disease prevention, and disease treatment. The health promotion approach is applied without patient identification, encompasses the entire population, makes individuals resilient, and creates environments that support the community health (1). Health promotion as action requires cooperation and investment for achieving a common goal, and as a process prepares health prerequisites such as peace, shelter, education, food, income, sustainable ecosystems, sustainable resources, and social justice and equity through public policy-making (2). Therefore, it should be considered as a collective action that focuses on empowering people to have control over their social health determinants (3).
Intersectoral collaboration has entered the domain of health through the Alma Ata Declaration in Kazakhstan in 1978. This declaration referred to the provision of comprehensive health services while considering economic and social issues (4). In 1980, Ottawa Declaration explained further need for more intersectoral actions to achieve better health outcomes. After the introduction of the concept of social determinants of health in 1990, efforts to develop intersectoral collaboration were expanded. Moreover, by holding a conference on intersectoral actions by WHO in 1997 and Bangkok’s declaration in 2000, the need for collaboration between various sectors for health promotion was further emphasized. For this purpose, a number of European countries attempting to implement intersectoral collaboration faced some problems. As a result, in 2006, the European Union (EU) proposed “Health in All Policies” (HiAP) as a guide for developing, implementing, and evaluating intersectoral policies (5). For example, The Public Health Act (2000) in Quebec obliged all organizations to consult with the Minister of Health and Social Services before setting the rules or regulations, which had a significant effect on health (6).
Proponents of the cross-sectoral approach argue that successful public health measures to control infectious, emerging, cardiovascular, and cancer diseases can be learned (7). In developing countries, the intersectoral collaboration strategy is not well implemented (8). There is a scatter in the criteria, models and indicators used in different studies that may to make policy makers and planners slow in understanding its flow. A scoping review aimed to investigate the scope and subject area of a field, summarize the findings of studies, and determine the gap in the existing literature on a subject (9).
Methods
This scoping review was conducted using Arksey and O’Malley framework (2005) (definition of research questions, identification of the related studies, and selection of the studies, tabulating the selected studies, and the summarization, and reporting of results). According to the main research question, three category keywords, including intersectoral collaboration and its different spectra, health promotion and its related dimensions, and model, index, and criteria (and their equivalents) were explored in Web of Science, PubMed, Scopus, and Embase databases. In addition, Google Scholar, Google, and ProQuest databases were also explored for up to the first 200 cases. In order to keep the article short, the search method in Scopus database was given as an example. The complete search of the database is attached in the additional files.
(TITLE-ABS-KEY (health) AND ((TITLE-ABS-KEY (intersectoral AND collaboration)) OR (TITLE-ABS-KEY (intersectoral AND coordination)) OR (TITLE-ABS-KEY (intersectoral AND cooperation)) OR (TITLE-ABS-KEY (intersectoral AND interaction)) OR (TITLE-ABS-KEY (intersectoral AND linkage)) OR (TITLE-ABS-KEY (joint AND activity)) OR (TITLE-ABS-KEY (networking)) OR (TITLE-ABS-KEY (intersectoral AND partnership))) AND ((TITLE-ABS-KEY (sensitization)) OR (TITLE-ABS-KEY (campaign)) OR (TITLE-ABS-KEY (negotiation)) OR (TITLE-ABS-KEY (“health promotion”)) OR (TITLE-ABS-KEY (advocacy))) AND ((TITLE-ABS-KEY (model)) OR (TITLE-ABS-KEY (measures)) OR (TITLE-ABS-KEY (indicators)) OR (TITLE-ABS-KEY (indices)) OR (TITLE-ABS-KEY (index)) OR (TITLE-ABS-KEY (metrics)) OR (TITLE-ABS-KEY (scales)))).
Inclusion/Exclusion Criteria
Original articles, review articles, and reports on health promotion published by the WHO written in English and reviewed regardless of time constraints were included. In terms of subject, articles examining the basic criteria, models, or indicators of intersectoral collaboration in health promotion were included (date of search: May 7, 2019).
Studies on the challenges and opportunities for intersectoral collaboration in the domain of health and those on services other than promotion services (disease prevention, treatment, and rehabilitation) as well as editorials, commentaries, and letters were excluded.
To ensure that the related studies were not lost from the beginning of the study until the time of writing the article, an alert was defined for each database to inform the researcher if a new article was published in this scope. The alert for the main databases was controlled until the preparation of the final version of the article.
Extraction of Results
At first, the results of the search in databases were entered into Endnote X7 software. In the second step, the first screening was performed independently by two authors. After reading the title and abstract of the articles, the related studies that met the inclusion criteria were identified, and their full text was downloaded. In the second screening, the articles selected from the previous stage were marked with five stars (much-related articles) in Endnote. Papers whose inclusion was not decided upon were marked with four stars, and other suspicious items with three stars. The third author reviewed the three- and four-star articles and determined their status.
The intersectoral collaboration criteria were manually and thematically extracted.by this steps: Studying the full text of all articles, initial encoding of the data, Identifying themes for codes that had a common field, Reviewing and modifying the themes, naming the themes, providing the extracted themes (10).
In the final step, studies were deeply restudied, and the title and year of the study, study area, type of study, and the criteria, indicators and models mentioned in the study were summarized (Additional file 1: Summary of included studies). In order to ensure that all articles retrieved from the study databases were analyzed, the selected studies were manually reference-checked, and related articles were added. After entering the details of the studies into Excel, descriptive characteristics of the studies were reported.
Results
Search results
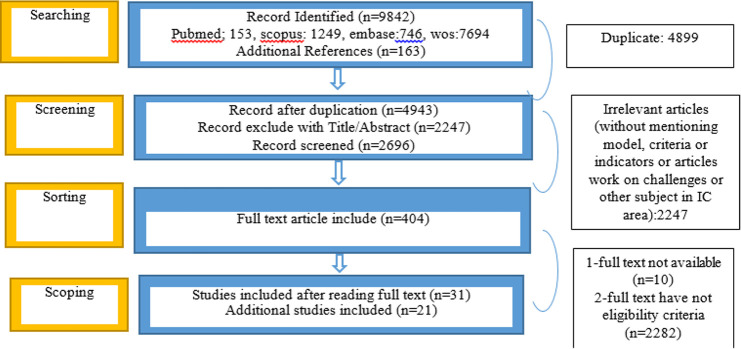
9842 articles were obtained. After the removal of duplicates, 4943 articles remained, and the abstract of 404 articles met the inclusion criteria. After obtaining the full text of the articles from the first screening, 52 articles met the inclusion criteria (Fig. 1).
Fig. 1:
Levels of search and selection of articles
Descriptive characteristics of studies
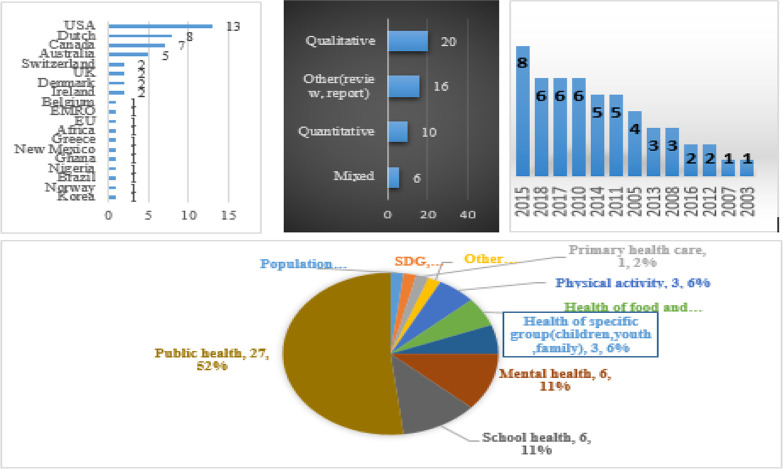
The studies were mostly qualitative that conducted in 2015 in countries such as the USA, the Netherlands, and Canada. The main scope of the studies was public health (27 articles), mental health (6 articles), school health (6 articles), water and food health (3 articles), and physical activity (3 articles) (Fig. 2).
Fig. 2:
Characteristics of the included studies
Results of the extraction of criteria, models, and indicators
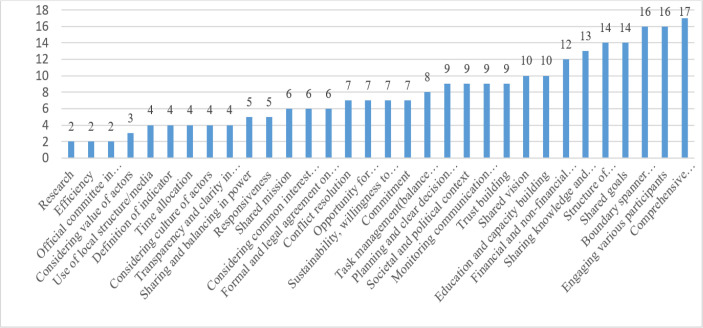
Analysis of the criteria showed the main criteria (Table 1, Fig. 3) included comprehensive support (political, organizational, and motivational) (n=17), engaging various participants, boundary spanner leadership (n=16), shared goals and structure of communication (formal and informal, quality of communication, the proximity of communication, etc.) (n=14), sharing knowledge and information (n=13), financial and non-financial resources (n=12), education and capacity building and having a shared vision (n=10).
Table 1:
Extracted criteria of studies
| Criteria | Reference | |
|---|---|---|
| 1 | Societal and political context | (42), (43), (44), (38), (15), (27), (11), (10), (45) |
| 2 | Commitment | (17), (46), (11), (47),(27),(48),(49),(16), |
| 3 | Boundary spanner leadership/direction | (11), (10), (45), (50), (51), (37),(27),(52), |
| (44),(4),(53),(42),(48),(49),(54) | ||
| 4 | Task management(balance between rols and activities) | (11), (10), (50), (37),(55),(15),(42),(49) |
| 5 | Structure of communication(formal and informal,…) | (11), (56), (45), (50), (47), (23),(27),(52),(44),(35),(48),(49),(57) |
| 6 | Education and capacity building | (11), (58), (50), (59), (47),(60), (61),(4),(7), (55) |
| 7 | Shared mission | (10), (37),(27),(44),(35),(15),(18) |
| 8 | Engaging various participants | (10), (62), (47), (20),(63), (64), (61), (37), (27),(65),(36),(44),(4),(42),(49),(66),(67) |
| 9 | Monitoring communication and result of participation | (68), (59), (52), (37), (10), (11), (27), (53), (4), |
| 10 | Trust building | (10), (11),(45), (62), (50),(63), (51), (27),(36),(57), |
| 11 | Shared vision | (50), (47), (69), (37), (27),(12),(44),(43),(35),(57) |
| 12 | Shared goals | (10), (45), (50), (37),(52),(36),(12),(44),(4),(26),(42),(49),(18),(70) |
| 13 | Considering common interest for contributor | (45), (62),(23), (37), (27),(4) |
| 14 | Considering value of actors | (20), (37),(67) |
| 15 | Responsiveness | (45), (47), (37), (27),(57) |
| 16 | Comprehensive support (political, organisational, motivational) | (11), (50), (59), (47), (24),(20), (64), (14),(27),(65),(71),(4),(32),(70),(66),(57),,(35) |
| 17 | Formal and legal agreement on collaboration | (50),(14), (60), (37),(71),(12) |
| 18 | Defenition of indicator | (45), (61), (37),(35) |
| 19 | Power | (10), (44),(43),(54) |
| 20 | Transparency and clarity in collaboration | (72), (37),(38),(54) |
| 21 | Time allocation | (59), (46),(52),(21) |
| 22 | Conflict resolution | (62), (50),(23), (37),(52),(21) |
| 23 | Planning and clear dicision making mechanism | (62), (50), (60), (37),(44),(53),(15),(67),(21) |
| 24 | Considering culture of actors | (20),(65),(38),(44),(48) |
| 25 | Efficiency | (69), (51),(54) |
| 26 | Apportunity for dialouge/create common language | (56),(61), (27),(36),(7), (70),(66) |
| 27 | Official committee in collaboration | (50),(60) |
| 28 | Financial and non-financial resources | (25), (24), (64),(46), (37), (27),(36),(4),(73),(7),(15),(49),(66),(65) |
| 29 | Use of local structure/media | (64), (27),(65),(4) |
| 30 | Sustainability, willngness to continue/positive experience | (50), (14), (23), (27),(44),(55),(49) |
| 31 | Sharing knowledge and information | (10), (62), (16), (24),(19), (61), (37), (27),(36),(44),(49),(59),(60) |
| 32 | Research | (64),(71) |
Fig. 3:
The frequency of criteria
Based on the analysis, 32 criteria were categorized into three main categories of micro, meso, and macro (Tables 2). Seventeen studies in this review explain models. Assessment of the applied models revealed that there was a fairly good variation in studies. The applied models were: DISC (11–14), Bergen (10, 15), Himelman (16), social network analysis (17–19), act for life collaboration continuum (20), Tukman (21), collective impact approach (22), system analysis (23), and logic (24, 25). Five studies of 52, in this review declare indicators for intersectoral collaboration assessment (Table 3).
Table 2:
Intersectoral collaboration criteria in the area of health promotion
| Level | Basic Criteria | Frequency | Percentage (%) |
|---|---|---|---|
| ➢ Boundary spanner leadership | 16 | ||
| ➢ Task management(balance between roles and activities) | 8 | ||
| ➢ Education and capacity building | 10 | ||
| Micro | ➢ Conflict resolution | 7 | |
| ➢ Trust building | 9 | ||
| ➢ Transparency in collaboration | 4 | ||
| ➢ Structure of communication(formal and informal) | 14 | ||
| ➢ willingness to continue/positive experience | 7 | ||
| ➢ Sharing knowledge and information | 13 | ||
| ➢ Opportunity for dialogue/create common language | 7 | ||
| ➢ Considering culture of actors | |||
| Total | 100 | 39.37% | |
| ➢ Engaging various participants | 17 | ||
| Meso | ➢ Monitoring communication and result of participation | 9 | |
| ➢ Considering common interest for contributor | 6 | ||
| ➢ Responsiveness | 5 | ||
| ➢ Financial and non-financial resources | 12 | ||
| ➢ Efficiency | 2 | ||
| ➢ Research | 2 | ||
| ➢ Definition of indicator | 4 | ||
| ➢ Time allocation | 4 | ||
| ➢ Official committee | 2 | ||
| Total | 63 | 24.80% | |
| ➢ Societal and political context | 9 | ||
| Macro | ➢ Commitment | 8 | |
| ➢ Shared mission | 6 | ||
| ➢ Shared vision | 10 | ||
| ➢ Shared goals | 14 | ||
| ➢ Considering value of actors | 17 | ||
| ➢ Comprehensive support (political, organizational, motivational) | 6 | ||
| ➢ Formal and legal agreement | 5 | ||
| ➢ Power(sharing / balancing) | |||
| ➢ Planning and clear decision making mechanism | 9 | ||
| ➢ Use of local structure/media | 4 | ||
| Total | 91 | 35.82% |
Table 3:
Expressed indicators and models
| Indicators | Model | Author/year |
|---|---|---|
| Context | Wagemaker et al (27) (2010) | |
| -Number and quality of collaboration structures | ||
| -Amount of funding | ||
| -Availability of resources | ||
| Participants/stakeholders | ||
| -Experience(number of years worked on issue) | ||
| -Number of partners recruited and dropped out | ||
| -Partners work together in a constructive manner | ||
| Partnership/coalition | ||
| -Level of agreement on roles | ||
| -Number of tasks of participants | ||
| -Number of participants attending meetings or attendance rate | ||
| -Quality of communication | ||
| -Comprehensiveness of evaluation | ||
| Processes | ||
| -Satisfaction with contribution of partners | ||
| -Scores on quality of action plan | ||
| -Opinion about participation | ||
| -Level of participation | ||
| Outcomes | ||
| -Number of organized activities | ||
| -Number of participants per activity | ||
| -The intensity of use of facilities | ||
| -The number/percentage of resolved problems or the to which they are solved | ||
| - | DISC(Diagnostic of Sustainable Collaboration | Hermens et al (11) (2018) |
| - | Bergen | Corbin et al (10) (2018) |
| - | Himelman | Quinn et al (16)) 2016) |
| - | DISC | Pucher et al (13)) 2015) |
| - | DISC | Pucher et al (14) (2015) |
| Frequency of contacts, Level of collaboration | System analysis method | Schoen et al (19)) 2014) |
| -Frequency of contacts; | Social Network Analysis (SNA) | Kothari et al (17) (2014) |
| - Continuity of involvement; | ||
| - Level of contribution of members to their network; | ||
| - Level of influence and decision-making power; | ||
| -Combination of professional and personal relationship. | ||
| Network membership measures: Number and names of organizations in network, Include in their type, sector/mission, size | Social Network Analysis | Leppin et al (18) (2018) |
| Network interaction measures: Location of organizations over geography and the ties that connect them, including presence and types of subnetworks) | ||
| Role and reach of the bridging hub measures: | ||
| Measures of in-degree and betweeness centrality,… | ||
| Network collaboration measures: | ||
| Measures of collaboration or frequency of interactions, trust and reciprocity of communication | ||
| - | DISC | Leurs et al (12 )) 2008) |
| - | Bergen | Haugstad (15)) 2011) |
| - | Tuckman | McMorris et al (21)) 2005) |
| - | Act for Life Collaboration Continuum Framework | Burgess et al (20)) 2015) |
| - | Multisectoral collaboration | Kuruvilla (2018) |
| - | Collective Impact | Roblin (2018) |
| - | Systems Analysis | Spitters (2017) |
| - | Logic | Sánchez (2015) |
| - | Logic | Miro (2015) |
Discussion
In terms of collective actions in health promotion, several studies have been published as original articles or review studies, the discrepancies between the results of that and the present study can be due to their focus on determining effective factors in the collaboration, study period (2001–2015), the studied databases (MEDLINE, CINAHL, Science Direct, and Psych INFO), and the research questions (26).
Another review analyzed the results of studies which investigated supportive and inhibitive factors for collaboration in the promotion of health through the Bergen model. However, there are some differences between this study and the present study in terms of the study period (2007–2015), some of the studied databases (CINAHL, ERIC, MEDLINE, and Psych INFO), and the research questions (10). Scoping review was conducted using datasets of Embase, Web of Science, Scopus, and PubMed, and search engines of Google, Google Scholar, and ProQuest.
Developed countries such as the US, the Netherlands, and Canada conducted more studies on intersectoral collaboration in the domain of health, which may be due to the greater attention of the central government of these countries to the role of health and its impact on the rules governing various organizations. From the last decade (2010 onwards), attention has been paid to studies on intersectoral collaboration in the domain of health, which may have been due to a paradigm shift towards different approaches to health (biomedicine viewpoint to health towards more comprehensive approaches such as health in all policies).
Among common indicators used in this area, some indicators such as the number of participants, the level of collaboration, and sustainability in the collaboration were the most frequent indicators (11, 17, 19, and 27). Because of the application of these indicators at different studies, they can be useful for whom they want to evaluate their collaboration in health fields. Examining the models employed in the studies showed that there were some general similarities between the models, but there were also some differences in the segmentation of the components of the models. As a result, in the DISC model, which was one of the most commonly used models, five components of external factors, context, change management, project management, and sustainability/support were considered. In another study, this model was implemented with two institutional components (sociopolitical context and organizational commitment) and organizational dimension (leadership, task management, capacity building, communication structure, and visible results) (11).
The Tukman model (21), had many similarities with the stages of team development (forming, storming, norming, and performing). The Bergen model (10, 15), examined the structure of intersectoral collaboration at three levels of input, process, and outcome. In the Himmelman model, the defined criteria referred to a variety of collaborations (cooperation, collaborating, networking, and coordinating) (16). The collective impact approach, examined five criteria: putting the subject on the agenda, a common measurement system, synergistic activities, communication, and structural support for the success of collective actions. The criteria used in the act for life model (20) had a high degree of similarity with those extracted from the present study, (continuous engagement of participants, clear intersectoral communication channels, and understanding of the culture of other sectors, etc.). In the social network analysis model, criteria of network membership, collaboration in the network, and the role of centrality in collaborative sub-networks were taken into consideration (28). This model is employed to understand communication networks using variables such as density measurement, closeness centrality, betweenness centrality, and Eigenvector centrality.
The multisectoral collaboration model is composed of six consecutive stages. A strong motivation to convince the stakeholders for cross-sectoral action, A clear definition of the situation and the assessment method, innovations related to the area under consideration, the implementation of designed mechanisms, monitoring and evaluation of process, synergy and strengthening the dialogue between stakeholders, and ultimately learn from the successes and failures resulting from collective actions (29).
The system analysis model has four consecutive stages: The first stage is the identification of stakeholders’ network through exploring political documents, government sites, and interviewing key actors. In the second stage, the schematic plan of the relative status of stakeholders identified in the stakeholders’ network is prepared. The third stage involves the description of relationships between stakeholders. Finally, the fourth stage encompasses the review and finalization of the schematic model of the relationships among stakeholders (23).
The logic model was used in two studies (24, 25). In this model first, the facilitators or barriers are listed, and then the processes, techniques, tools, and measures of the program under study are determined. The output is the result of the direct implementation of the program, which forms the third part of the model. Outcomes modifying the behavior, attitude, knowledge, skill, or expected level of performance of the program are the fourth part of the program. The final impact of the last part of this model can be organizational or community changes, presented as increased capacity, change in policy, etc.
Comparative evaluation of the models used in intersectoral actions in health promotion revealed that the social network analysis, DISC, Bergen, and logic models were the most commonly used models in health promotion, which may be due to the comprehensiveness of the criteria mentioned in them. For brevity, from each level, three criteria that had the highest frequency in the studies were discussed.
In this study, to ease the understanding of the criteria and their implementation, all the criteria repeated in the studies were categorized into three levels of micro, meso, and macro (30). This model applied based on a research that conducted on Intersectoral Action for Health and Many of the criteria used in this study were consistent with that (31). These three levels complement each other, and failure at one level leads to failure at other levels, therefore, by considering these criteria, planners and policymakers can prevent incorrect actions to implement collaborative actions. Micro-level is a level in which involving actors are important. In this stage, social interaction among stakeholders, capacity building for framing relationships are stated (31). 39.4% of the criteria were at the micro-level, and dimensions of the boundary spanner leadership, communication structure, and knowledge and information sharing were the most frequently used criteria in this area.
The features of a boundary spanner leader include the ability to manage boundaries (knowledge sharing and understanding of different perspectives), the creation of a shared context (the resources integration and mobilization by defining shared vision and values), and the discovery of new boundaries (the creation of creative ideas (32). Open and face-to-face communication can be used to build trust-based relationships with other sectors (33, 34). Effective communication will only be achieved by building trust between various governmental and nongovernmental organizations, holding regular meetings, and allocating sufficient time to it (35). Sharing information and effective communication have been reported effective in reducing disagreement and other forms of conflict between different sectors (36).
At the meso-level, issues such as strengthening management and leadership, trust-building, and a shared understanding of problems are considered. It refer to structure and process inside and between actors. At this level, some criteria can be defined at organizational culture levels and refers to the government’s actions and structures. 24.8% of the criteria were at this level. The engagement of different stakeholders, provision of resources, and monitoring the relationship between collaborators had respectively the highest frequency at this level. A clear definition of contributors, the inclusion/exclusion criteria, and acceptance criteria is important for stakeholder’s engagement (37). Resource provision include money, materials, and equipment (10). and methods used for making decisions on financial, mechanisms, and tools that are used to ensure financial integrity, should be determined (37). Monitoring contributors’ perceptions of the collaboration can provide valuable information on how to adjust relationships. Moreover, assessment of the quality of collaboration at different levels, is essential for predicting future problems and responding to existing problems (10).
The third level is the macro level that implies to ideologies and dominant values, this level refers to governmental and national layers. Some criteria such as structure, organization, market, and government measures are taken into account. The main motivator at this level is politics, defined as a legal issue or a statement of values and principles related to goals, by individuals, communities, or societies (31). Macro level contains 35.82% of the criteria. Comprehensive supports, sharing goals, and shared vision, had respectively the highest frequency in the studies.
Since the process of intersectoral collaboration often requires a new structure, and accordingly, new resources, therefore adequate financial support for these efforts must be considered (38). In Sweden, Quebec, and South Australia, financial incentives could act as a facilitator for the implementation of health program in all policies (28). The goals of collaboration should not be opposed to the contributors’ authorities (39), but it must be predetermined, accessible, measurable, and understandable for all actors through a common language (40). Creating a long-term perspective from the beginning of and during the collaboration process is necessary to create a shared perception (41).
Overall, the results of this study were consistent with those of other studies, with the difference that, in this study, the basic criteria for intersectoral collaboration in the area of health promotion were categorized, and related models and indicators were identified.
Limitations
only studies with basic criteria for intersectoral collaboration in the domain of health or those with a specific model or index were included, so studies that investigated challenges, barriers, strategies might have been missed, justified according to the main objectives of this study. Furthermore, some criteria that were not repeated in other studies might have been excluded from this study.
Conclusion
There is a lack of comprehensive research that tell us what should we do when we want to start Intersectoral collaboration in the health promotion field. In this study, the basic criteria, models, and indicators for intersectoral collaboration in the domain of health promotion were identified and categorized, that can help planners and decision-makers to use of them at shared actions and models and indicators can also be applied to assess achievements.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
This work was supported by the Iran National Science Foundation (INSF).
Footnotes
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.Population and Public Health Division MoHaLTC, Ontario (2018). Mental Health Promotion Guideline. https://health.gov.on.ca/en/pro/programs/publichealth/oph_standards/docs/protocols_guidelines/Mental_Health_Promotion_Guideline_2018.pdf
- 2.Raphael D. (2013). The political economy of health promotion: part 1, national commitments to provision of the prerequisites of health. Health Promot Int, 28(1):95–111. [DOI] [PubMed] [Google Scholar]
- 3.Marshall M, Leatherman S, Mattke S. (2004). Selecting indicators for the quality of health promotion, prevention and primary care at the health systems level in OECD countries. https://www.oecd.org/els/health-systems/33865865.pdf
- 4.Public Health Agency of Canada Ottawa (PHAo) (2007). Crossing sectors: experiences in intersectoral action, public policy and health. https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/publicat/2007/cro-sec/pdf/cro-sec_e.pdf
- 5.Evans T. (In press 2006). Making the Case for Financing the Social Determinants of Health (presentation deck) [Presentation].
- 6.Bernier NF. (2006). Quebec’s approach to population health: an overview of policy content and organization. J Public Health Policy, 27(1):22–37. [DOI] [PubMed] [Google Scholar]
- 7.Hermann H, Saxena S, Moodie R. (2005). Promoting Mental Health: Concepts, emerging evidence, practice. A report of the World Health Organisation, Department of Mental Health and Substance Abuse in collaboration with the Victorian Health Promotion Foundation and the University of Melbourne. World Health Organization. http://apps.who.int/iris/bitstream/handle/10665/43286/9241562943_eng.pdf?sequence=1 [Google Scholar]
- 8.Friedli L. (2009). Mental health, resilience and inequalities. Copenhagen: WHO Regional Office for Europe. https://www.euro.who.int/__data/assets/pdf_file/0012/100821/E92227.pdf
- 9.Arksey H, O’Malley L. (2005). Scoping studies: towards a methodological framework. Int J Soc Res Methodol, 8(1):19–32. [Google Scholar]
- 10.Corbin JH, Jones J, Barry MM. (2018). What makes intersectoral partnerships for health promotion work? A review of the international literature. Health Promot Int, 33(1):4–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hermens N, Verkooijen KT, Koelen MA. (2019). Associations between partnership characteristics and perceived success in Dutch sport-for-health partnerships. Sport Manage Rev, 22(1):142–52. [Google Scholar]
- 12.Leurs MT, Mur-Veeman IM, van der Sar R, Schaalma HP, de Vries NK. (2008). Diagnosis of sustainable collaboration in health promotion - a case study. BMC Public Health, 8:382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pucher KK, Candel MJJM, Boot NMWM, et al. (2015). A multiple-case study of intersectoral collaboration in comprehensive school health promotion using the DIagnosis of Sustainable Collaboration (DISC) model. Health Educ, 115(3/4):301–21. [Google Scholar]
- 14.Pucher KK, Candel MJJM, Krumeich A, et al. (2015). Effectiveness of a systematic approach to promote intersectoral collaboration in comprehensive school health promotion-a multiple-case study using quantitative and qualitative data. BMC Public Health, 15: 613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haugstad A. Promoting public health in Norway: A case study of NGO-public sector partnership using The Bergen Model of Collaborative Functioning [Master thesis]. School of Psychology, The University of Bergen, Norway; 2011. [Google Scholar]
- 16.Quinn MA, Southerland JL, Richards K, et al. (2016). Quantifying collaboration using Himmelman’s strategies for working together: Findings from the Tennessee coordinated school health program. Health Educ, 116(1):34–49. [Google Scholar]
- 17.Kothari A, Hamel N, MacDonald JA, et al. (2014). Exploring Community Collaborations: Social Network Analysis as a Reflective Tool for Public Health. Syst Pract Action Res, 27(2):123–37. [Google Scholar]
- 18.Leppin AL, Okamoto JM, Organick PW, et al. (2018). Applying Social Network Analysis to Evaluate Implementation of a Multisector Population Health Collaborative That Uses a Bridging Hub Organization. Front Public Health, 6:315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schoen MW, Moreland-Russell S, Prewitt K, Carothers BJ. (2014). Social network analysis of public health programs to measure partnership. Soc Sci Med, 123:90–5. [DOI] [PubMed] [Google Scholar]
- 20.Burgess T, Braunack-Mayer A, Tooher R, et al. (2016). Optimizing intersectoral collaboration between health and education: the Health Bridges study. J Public Health (Oxf), 38(4):e430–e437. [DOI] [PubMed] [Google Scholar]
- 21.McMorris LE, Gottlieb NH, Sneden GG. (2005). Developmental stages in public health partnerships: A practical perspective. Health Promot Pract, 6(2):219–26. [DOI] [PubMed] [Google Scholar]
- 22.Butler J, Fryer CS, Reed EA, Thomas SB. (2011). Utilizing the school health index to build collaboration between a university and an urban school district. J Sch Health, 81(12):774–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Henderson S, Kendall E, Forday P, Cowan D. (2013). Partnership functioning: A case in point between government, nongovernment, and a University in Australia. Prog Community Health Partnersh, 7(4):385–93. [DOI] [PubMed] [Google Scholar]
- 24.Miro A, Kishchuk NA, Perrotta K, Swinkels HM. (2014). Healthy canada by design CLASP: Lessons learned from the first phase of an intersectoral, cross-provincial, built environment initiative. Can J Public Health, 106(1 Suppl 1):eS50–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sanchez V, Andrews ML, Carrillo C, Hale R. (2015). New Mexico Community Health Councils: Documenting Contributions to Systems Changes. Prog Community Health Partnersh, 9(4):471–81. [DOI] [PubMed] [Google Scholar]
- 26.Seaton CL, Holm N, Bottorff JL, et al. (2018). Factors that impact the success of interorganizational health promotion collaborations: a scoping review. Am J Health Promot, 32(4):1095–109. [DOI] [PubMed] [Google Scholar]
- 27.Wagemakers A, Vaandrager L, Koelen MA, et al. (2010). Community health promotion: A framework to facilitate and evaluate supportive social environments for health. Eval Program Plann, 33(4):428–35. [DOI] [PubMed] [Google Scholar]
- 28.Molnar A, Renahy E, Patricia OC, et al. (2016). Using Win-Win Strategies to Implement Health in All Policies: A Cross-Case Analysis. PLoS One, 11(2):e0147003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van den Broucke S, Jooste H, et al. (2010). Strengthening the capacity for health promotion in South Africa through international collaboration. Glob Health Promot, 17(2 Suppl):6–16. [DOI] [PubMed] [Google Scholar]
- 30.Lucy G. (2012). Health Policy and Systems Research. World Health Organization. https://www.who.int/alliance-hpsr/alliancehpsr_abridgedversionreaderonline.pdf [Google Scholar]
- 31.Mikkonen JP. (2018). Intersectoral Action for Health: Challenges, Opportunities, and Future Directions in the WHO European Region. http://mikkonen.kapsi.fi/archive/Mikkonen-2018-PhD-Intersectoral_action_for_health.pdf
- 32.Fick-Cooper L, Williams A, Moffatt S, Baker EL. (2019). Boundary Spanning Leadership: Promising Practices for Public Health. J Public Health Manag Pract, 25(3):288–90. [DOI] [PubMed] [Google Scholar]
- 33.Misener K, Doherty A. (2013). Understanding capacity through the processes and outcomes of interorganizational relationships in nonprofit community sport organizations. Sport Manage Rev, 16(2):135–47. [Google Scholar]
- 34.Corbin JH, Mittelmark MB. (2008). Partnership lessons from the Global Programme for Health Promotion Effectiveness: a case study. Health Promot Int, 23(4):365–71. [DOI] [PubMed] [Google Scholar]
- 35.Kania J, Kramer M. (2011). Collective impact. Stanford social innovation review New York. https://www.glc.org/wp-content/uploads/2016/10/Collective-Impact-Stanford.pdf
- 36.Agbanu SK. The impact of stakeholder collaboration on effectiveness of health program implementation in Ghana [Ph.D. thesis]. Ann Arbor: Walden University, United States; 2010. [Google Scholar]
- 37.Hospedales CJ, Jané-Llopis E. (2011). A multistakeholder platform to promote health and prevent noncommunicable diseases in the region of the Americas: the Pan American Health Organization partners forum for action. J Health Commun, 16 Suppl 2:191–200. [DOI] [PubMed] [Google Scholar]
- 38.Andersen PT, El Ansari W, Rasmussen HB, Stock C. (2010). Municipalities Collaborating in Public Health: The Danish Smoking Prevention and Cessation Partnership. Int J Environ Res Public Health, 7(11):3954–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Panel-Ramond J. (1992). Partnership: Myth or reality? Community Dev J, 27(2):156–65. [Google Scholar]
- 40.Raišienė AG, Baranauskaitė L. (2018). Investigating complexity of intersectoral collaboration: contextual framework for research. CROMA Journal, 6 (1):79–89. [Google Scholar]
- 41.El Ansari CJP, Walid (2001). Partnerships, community participation and intersectoral collaboration in South Africa. J Interprof Care, 15(2):119–32. [DOI] [PubMed] [Google Scholar]
- 42.Koelen MA, Vaandrager L, Wagemakers A. (2008). What is needed for coordinated action for health?. Fam Pract, 25(Suppl_1):i25–i31. [DOI] [PubMed] [Google Scholar]
- 43.World Health Organization (2005). Child and adolescent mental health policies and plans. https://www.who.int/mental_health/policy/services/9_child%20ado_WEB_07.pdf?ua=1
- 44.Dempster B, Tucs E. (2008). best and promising practices of multi-sectoral collaboratives: indicators for reflection and assessment. Civics Research Cooperative on behalf of the Ontario Healthy Communities Coalition. https://www.canada.ca/content/dam/canada/employment-social-development/migration/documents/docs/hcbe_indicators.pdf
- 45.Rasanathan K, Bennett S, Atkins V, et al. (2017). Governing multisectoral action for health in low- and middle-income countries. PLoS Med, 14(4):e1002285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McCormack DRNP, Buck DMBM, McGraw BRNBN. (2013). Learning to use tension to create sustainable partnerships for responsive policy and practice in the health sector. Int Public Health J, 5(1):17–29. [Google Scholar]
- 47.Queiroz AC, Cardoso LS, Heller L, Cairncross S. (2015). Integrating surveillance data on water-related diseases and drinking-water quality; action-research in a Brazilian municipality. J Water Health, 13(4):1048–54. [DOI] [PubMed] [Google Scholar]
- 48.Johnson LJ, Zorn D, Tam BKY, et al. (2003). Stakeholders’ views of factors that impact successful interagency collaboration. Except Child, 69(2):195–209. [Google Scholar]
- 49.Atkinson M, Doherty P, Kinder K. (2005). Multi-agency working: models, challenges and key factors for success. J Early Child Res, 3(1):7–17. [Google Scholar]
- 50.Kang E. (2016). Intersectoral collaboration for physical activity in Korean Healthy Cities. Health Promot Int, 31(3):551–61. [DOI] [PubMed] [Google Scholar]
- 51.Jones J, Barry MM. (2011). Exploring the relationship between synergy and partnership functioning factors in health promotion partnerships. Health Promot Int, 26(4):408–20. [DOI] [PubMed] [Google Scholar]
- 52.Tzenalis A, Sotiriadou C. (2010). Health promotion as multi-professional and multi-disciplinary work. Int J Caring Sci, 3(2):49–55. [Google Scholar]
- 53.Kendall E, Muenchberger H, Sunderland N, et al. (2012). Collaborative capacity building in complex community-based health partnerships: a model for translating knowledge into action. J Public Health Manag Pract, 18(5):E1–13. [DOI] [PubMed] [Google Scholar]
- 54.Jones J, Barry MM. (2018). Factors influencing trust and mistrust in health promotion partnerships. Glob Health Promot, 25(2):16–24. [DOI] [PubMed] [Google Scholar]
- 55.Nelson JD, Moore MJB, Blake Christine, et al. (2013). Characteristics of successful community partnerships to promote physical activity among young people, North Carolina. Prev Chronic Dis, 10:E208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tooher R, Collins J, Braunack-Mayer A, et al. (2017). Intersectoral collaboration to implement school-based health programmes: Australian perspectives. Health Promot Int, 32(2):312–21. [DOI] [PubMed] [Google Scholar]
- 57.Dunlop JM, Holosko MJ. (2004). The story behind the story of collaborative networks-relationships do matter! J Health Soc Policy, 19(3):1–18. [DOI] [PubMed] [Google Scholar]
- 58.Botezat I, Campion J, Garcia-Cubillana P, et al. (2017). Mental Health in All Policies. Situation Analysis and Recommendations for Action. https://ec.europa.eu/health/sites/health/files/mental_health/docs/2017_mh_allpolicies_en.pdf
- 59.Van der Kleij R, Coster N, Verbiest M, et al. (2015). Implementation of intersectoral community approaches targeting childhood obesity: a systematic review. Obes Rev, 16(6):454–72. [DOI] [PubMed] [Google Scholar]
- 60.Whiteford H, McKeon G, Harris M, et al. (2014). System-level intersectoral linkages between the mental health and non-clinical support sectors: a qualitative systematic review. Aust N Z J Psychiatry, 48(10):895–906. [DOI] [PubMed] [Google Scholar]
- 61.World Health Organization (2012). Regional strategy on mental health and substance abuse. https://apps.who.int/iris/bitstream/handle/10665/116830/EMROPUB_2012_EN_1067.pdf?sequence=1&isAllowed=y
- 62.European Union (2017). Joint Action on Mental Health and Well-being, MENTAL HEALTH IN ALL POLICIES Situation analysis and recommendations for action. https://ec.europa.eu/health/sites/health/files/mental_health/docs/2017_mh_allpolicies_en.pdf.
- 63.Andres B. (2014). Collaboration for addiction and mental health care: Best advice: Canadian Centre on Substance Abuse. https://www.ccsa.ca/sites/default/files/2019-05/CCSA-Collaboration-Addiction-Mental-Health-Best-Advice-Report-2015-en.pdf
- 64.Larsen M, Koudenburg OA, Gulis G, Rantala R. (2014). Intersectoral action for health: The experience of a Danish municipality. Scand J Public Health, 42(7):649–57. [DOI] [PubMed] [Google Scholar]
- 65.Skeen S, Kleintjes S, Lund C, et al. (2010). ‘Mental health is everybody’s business’: roles for an intersectoral approach in South Africa. Int Rev Psychiatry, 22(6):611–23. [DOI] [PubMed] [Google Scholar]
- 66.Gray S, Jones M, Means R, et al. (2018). Intersectoral Transfer of the Food for Life Settings Framework in England. Health Promot Int, 33(5):781–90. [DOI] [PubMed] [Google Scholar]
- 67.Barile JP, Darnell AJ, Erickson SW, Weaver SR. (2012). Multilevel Measurement of Dimensions of Collaborative Functioning in a Network of Collaboratives that Promote Child and Family Well-Being. Am J Community Psychol, 49(1–2):270–82. [DOI] [PubMed] [Google Scholar]
- 68.Caldas de Almeida J, Mateus P, Tomé G. (2015). Towards community-based and socially inclusive mental health care: Situation analysis and recommendations for action (Joint action on mental health and well-being).
- 69.Cooper TV, Cabriales JA, Taylor T, et al. (2015). Internal Structure Analysis of a Tobacco Control Network on the U.S.-Mexico Border. Health Promot Pract, 16(5):707–14. [DOI] [PubMed] [Google Scholar]
- 70.Pan American Health Organization(PAHO) (2015). Advancing the Health in All Policies Approach in the Americas: What Is the Health Sector’s Role?. https://www.paho.org/hq/dmdocuments/2015/hiap-Brief-Guide-and-Recomendations-ENG.pdf
- 71.Adeleye OA, Ofili AN. (2010). Strengthening Intersectoral Collaboration for Primary Health Care in Developing Countries: Can the Health Sector Play Broader Roles? J Environ Public Health, 2010:272896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rosas SR. (2017). Systems thinking and complexity: considerations for health promoting schools. Health Promot Int, 32(2):301–311. [DOI] [PubMed] [Google Scholar]
- 73.Diminic S, Carstensen G, Harris M, et al. (2015). Intersectoral policy for severe and persistent mental illness: review of approaches in a sample of high-income countries. Glob Ment Health (Camb), 2:e18. [DOI] [PMC free article] [PubMed] [Google Scholar]