Abstract
Context
As sports are reinitiated around the United States, the incidence of COVID-19 among youth soccer athletes remains unknown.
Objective
To determine the incidence of COVID-19 among youth soccer athletes and the risk-mitigation practices used by youth soccer organizations.
Design
Cohort study.
Setting
Survey distributed to Elite Clubs National League member clubs.
Patients or Other Participants
Youth soccer club directors throughout the United States.
Main Outcome Measure(s)
Surveys were completed in late August 2020 regarding the club's current phase of return to soccer (individual only, group noncontact, group contact), date of reinitiation, number of players, cases of COVID-19, and risk-reduction procedures being implemented. Case and incidence rates were compared with national pediatric data and county data from the prior 10 weeks. A negative binomial regression model was developed to predict club COVID-19 cases using the local incidence rate and phase of return as covariates and the log of club player-days as an offset.
Results
A total of 124 respondents had reinitiated soccer, representing 91 007 players with a median duration of 73 days (interquartile range = 53–83 days) since restarting. Of the 119 clubs that had progressed to group activities, 218 cases of COVID-19 were reported among 85 861 players. Youth soccer players had a lower case rate and incidence rate than children in the United States (254 versus 477 cases per 100 000; incidence rate ratio = 0.511, 95% CI = 0.40, 0.57; P < .001) and the general population in the counties where data were available (268 versus 864 cases per 100 000; incidence rate ratio = 0.202, 95% CI = 0.19, 0.21; P < .001). After adjusting for the local COVID-19 incidence, we found no relationship between the club COVID-19 incidence and the phase of return (noncontact: b = 0.35 ± 0.67, P = .61; contact: b = 0.18 ± 0.67, P = .79). Soccer clubs reported using a median of 8 (interquartile range = 6–10) risk-reduction procedures.
Conclusions
The incidence of COVID-19 among youth soccer athletes was relatively low when compared with the background incidence among children in the United States during the summer of 2020. No relationship was identified between the club COVID-19 incidence and the phase of return to soccer.
Keywords: adolescents, infectious disease, pediatrics, SARS-CoV-2, sports
Key Points
These findings suggested that participation in youth soccer activities did not result in an increased risk of COVID-19 among US participants during the summer of 2020.
No difference in COVID-19 incidence was identified between those groups participating in socially distanced, noncontact play and those that had returned to contact participation, even after adjusting for the local background disease incidence.
All respondents reported having a formal COVID-19 plan in place, and the majority described using a broad range of risk-mitigation procedures.
COVID-19 has had an unprecedented influence on virtually every aspect of our lives, and youth sports are no exception. As groups across the country look to reinitiate youth sports, the risks of competing should be considered in all settings. Physical activity and sport participation have tremendous physical and mental health benefits for children, but these must be balanced against the possibility of viral transmission during activity. Early researchers1–3 suggested that school and sport cancellations during the initial months of the COVID-19 pandemic were associated with significant decreases in physical activity and worsening of depressive symptoms in children and athletes. Prolonged restriction has been projected to contribute significantly to long-term increases in obesity and mental health disorders.4–6 Together, these results suggested that isolation and physical inactivity during COVID-19 restrictions may represent significant threats to physical and mental health in children.
Nonetheless, COVID-19 continues to spread throughout the country, and more than 530 000 deaths in the United States have been attributed to the virus.7 In general, children and young athletes appear to experience milder symptoms than adults,8 but there is concern that sport participation could contribute to community transmission and expose individuals who may be more likely to experience severe consequences of the disease.9 Multiple groups10–14 have developed protocols and recommendations for sport participation to reduce this risk, but whether youth sport participation with risk-mitigation procedures in place increases the incidence of COVID-19 among youth sport participants remains unclear.
Soccer remains the most popular sport in the United States, and as local guidelines began to ease during the summer of 2020, many youth soccer organizations began to reinitiate participation. Recommendations have been published15,16 regarding procedures to mitigate the COVID-19 risk in soccer specifically, but it is unknown whether this has resulted in an increased risk of COVID-19 among youth soccer participants that could potentially contribute to a greater degree of community spread. Consequently, this uncertainty limits discussions about whether the risks of participation outweigh the physical and mental health risks of restriction from participation. Therefore, the purpose of our study was to identify the incidence of COVID-19 among a nationwide sample of youth soccer players, as well as the current mitigation procedures being implemented to reduce the risk of disease spread.
METHODS
Through a collaboration with the Elite Clubs National League, a leading nationwide youth soccer competition and development platform, we distributed surveys to the directors of all member clubs between August 26 and 31, 2020. Soccer club directors were asked to provide information for their entire organization. In addition to facility location, clubs were asked whether they had reinitiated participation in soccer since the initial COVID-19 restrictions in the spring of 2020. Those directors who reported reinitiating soccer were asked which stage of participation they had returned to (individual training only; noncontact, physically distanced; contact, not physically distanced; or other), the date of their reinitiation, the total number of players and staff members participating, the number of trainings and games that their players had participated in, and the number of players and staff members who had been diagnosed with COVID-19 since restarting soccer participation. Clubs that reported a positive case of COVID-19 were asked to provide the number of cases among players or staff that were traced back to soccer participation or that resulted in hospitalization or death. Finally, each club was asked whether they had a formal plan for COVID-19 risk reduction and which of 12 procedures they used. We conducted follow up of outlying values.
Data were initially evaluated using descriptive statistics: estimates of central tendency (mean, median) and variability (SD, interquartile range [IQR], range) for continuous variables and counts and percentages for categorical variables. The overall case rate was expressed as the number of cases per 100 000 players (reported cases/total number of players · 100 000). The duration since restarting was identified for each club as the difference in days between the date of reinitiation and the date the survey was completed. The overall incidence rate was determined as the number of reported cases divided by the total player-days (calculated as the sum of the product of players and duration for each club). Given a median duration of 73 days of soccer participation for the respondent clubs, we calculated the national pediatric case rate and incidence over the 10 weeks before survey administration using data provided by the American Academy of Pediatrics on August 27, 2020. Case rates from the total club data and national data were compared descriptively, and incidence rates were compared using median unbiased estimation.
Based on publicly available online information from the Centers for Disease Control and Prevention and local health authorities,17 we determined the number of cases, case rate, and incidence rate during the previous 10 weeks for each county in which a respondent club was located. For those clubs with available county information, case rates and incidence rates were compared between the aggregate club and county data. For those counties with more than 500 players, the relationship between COVID-19 case rates among club soccer athletes and the general population in their respective counties was evaluated using a linear regression model, weighted for the number of players in each county. Incidence rates were also compared between those clubs that had returned to individual training only (individual); noncontact, physically distanced (noncontact) play; or contact, not physically distanced (contact) play. Finally, to assess the independent relationships between COVID-19 cases and phase of play, we developed a negative binomial regression model to predict the number of club cases, including the incidence rate within each county in the prior 10 weeks, the phase of current soccer play for each club (contact, noncontact), and the log of player-days as an offset in the model. Many clubs reported 0 cases, but a separate 0-inflated negative binomial model with the same predictor and outcome variables yielded virtually identical results and model fit parameters. All statistical analyses were performed in R statistical software (The R Foundation for Statistical Computing). The study protocol was reviewed by the Institutional Review Board at the University of Wisconsin. Because we did not solicit individual-level health information from the respondents, our investigation was determined to not constitute human subjects research and was exempted from formal review.
RESULTS
Surveys were completed by 129 respondents, of whom 124 had restarted playing soccer since local restrictions were put in place at the beginning of the COVID-19 pandemic. These 124 respondents represented 91 007 players from 34 states who had participated in 45 574 trainings and 6208 games since restarting. The time since restarting varied across clubs, with a median duration of 73 days (IQR = 53–83 days). With respect to phase of return, 5 clubs (4%) remained in individual training and 49 clubs (39%) had progressed to noncontact or physically distanced group play, while 70 clubs (57%) had progressed to soccer participation that involved contact or unrestricted group play and the remainder had not.
A total of 282 cases of COVID-19 were reported, consisting of 239 players and 43 staff members from 78 clubs (63%). (One club initially reported many cases in players, which on follow up was determined to have been misinterpreted as the number of players who had been quarantined due to exposure and subsequently clarified to include only players diagnosed with COVID-19.) Among youth soccer players specifically, this represents 263 cases of COVID-19 per 100 000 children and an incidence rate of 4.3 × 10−5 cases per person-day.
Among the 119 clubs that had progressed to noncontact or contact group play, 218 cases were reported among players. The comparison of COVID-19 in youth soccer clubs versus national pediatric data is shown in Table 1. Youth soccer players had a lower incidence rate than the general population of children in the United States (incidence rate ratio [IRR] = 0.511, 95% CI = 0.40, 0.57; P < .001). Population-level COVID-19 data were publicly available for 55 of the 76 counties in which respondent clubs were located. The comparisons of COVID-19 between these clubs and their respective counties is shown in Table 2. Youth soccer participants had a lower incidence rate than the general population in the respondent counties (IRR = 0.202, 95% CI = 0.19, 0.21; P < .001). County and club case rates were significantly related (β = 0.20 ± 0.071, P = .0081; Figure).
Table 1.
Comparison of COVID-19 Cases, Case Rate, and Incidence Between Youth Soccer Players From Clubs That Had Reinitiated Group Soccer Participation and US Children Nationwide
| Variable |
Youth Soccer Players |
US Childrena |
| Total population | 85 861 | 75 471 700 |
| Total cases | 218 | 360 263 |
| Total person-days | 6 317 004 | 5 283 019 000 |
| Cases per 100 000 people | 254 | 477 |
| Incidence rate (cases/person-day)b | 0.0000345 | 0.0000682 |
Data for June 18 to August 27, 2020, were extracted from the American Academy of Pediatrics “Children and COVID-19: State Data Report” on August 27, 2020.8
Incidence rate ratio (exposure to soccer) = 0.511, 95% CI = 0.40, 0.57; P < .001.
Table 2.
Comparison of COVID-19 Cases, Case Rate, and Incidence Between Youth Soccer Players and Population Data From Each Respondent's County (Where Available)
| Variable |
Youth Soccer Clubs (n = 94) |
Respondent Counties (n = 56)a |
| Total population | 58 588 | 72 654 438 |
| Total cases | 157 | 665 980 |
| Total person-days | 4 296 925 | 5 810 646 |
| Cases per 100 000 people | 268 | 917 |
| Incidence rate (cases/person-day)b | 0.0000365 | 0.000131 |
Data extracted from available public information on local health authority websites.
Incidence rate ratio (exposure to soccer) = 0.202, 95% CI = 0.19, 0.21; P < .001.
Figure.
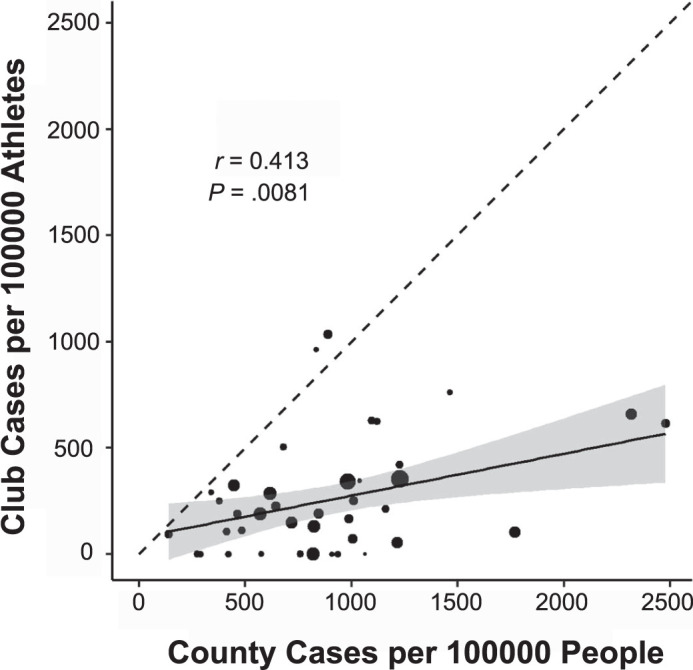
Reported COVID-19 case rates for club soccer athletes and the general population of their respective counties during the summer of 2020. The size of points was scaled to the number of players from each county, and the dashed line represents a line of equality. The solid line and shaded area represent the regression line and 95% CI, respectively, from the linear model, weighted for the number of players from each county. r = correlation coefficient.
The comparison of COVID-19 cases by phase of return to soccer is shown in Table 3. In the unadjusted analysis, players in noncontact group play had a lower incidence rate than those who remained in individual training (IRR = 0.47, 95% CI = 0.29, 0.80; P = .003), as did those in contact group play (IRR = 0.54, 95% CI = 0.35, 0.88; P = .008). No difference in incidence rate was identified between those in contact and noncontact group play (IRR = 1.10, 95% CI = 0.85, 1.50; P = .40). In the multivariable negative binomial model adjusted for local COVID-19 incidence, the number of club cases was positively associated with the local incidence rate but not the phase of return (Table 4). Of the 282 cases reported, 1 case in a player was reportedly attributed to transmission during soccer. No cases were reported to have resulted in hospitalization or death. Of the clubs that had restarted playing soccer, 124 (100%) responded that they had a formal plan in place regarding COVID-19 risk-reduction procedures. The median number of risk-mitigation procedures used was 8 (IQR = 6–10), and most clubs reported incorporating a number of COVID-19 risk-reduction procedures (Table 5).
Table 3.
Comparison of COVID-19 Cases, Case Rate, and Incidence Rate in Youth Soccer Players Between Clubs at Each Phase of Progression to Return to Soccer
| Variable |
Individual Training Only (n = 5) |
Noncontact, Distanced (n = 49) |
Contact, Not Distanced (n = 70) |
| Total population | 5146 | 28 905 | 56 956 |
| Total cases | 21 | 58 | 160 |
| Total person-days | 318 591 | 1 844 041 | 4 472 963 |
| Cases per 100 000 people | 408 | 201 | 281 |
| Incidence rate (cases/person-day)a | 0.0000785 | 0.0000369b | 0.0000423c,d |
Incidence rate ratios calculated using unbiased median estimation and mid-P CIs.
P = .003 versus individual.
P = .008 versus individual.
P = .40 versus noncontact.
Table 4.
Association of Local COVID-19 Incidence and Phase of Soccer Play With COVID-19 Incidence Among Youth Soccer Clubsa
| Variable |
Estimate |
SD |
P |
| Local (county) incidence | 5900 | 770 | <.001 |
| Phase of play–noncontact | 0.73 | 0.84 | .38 |
| Phase of play–contact | 0.57 | 0.82 | .49 |
Estimates, SD, and significance level for each variable were derived from a negative binomial regression model to predict COVID-19 cases within each club, including the local COVID-19 incidence and the phase of play (referent = individual training) as covariates as well as log (player-days) as an offset.
Table 5.
Proportion of Youth Soccer Clubs That Reported Implementation of COVID-19 Risk-Reduction Procedures
| Risk-Mitigation Procedure |
% of Clubs |
| Player or staff symptom monitoring | 93 |
| Player or staff temperature checks at home | 85 |
| Player or staff temperature checks on site | 32 |
| Face-mask use by players off the field | 80 |
| Face-mask use by staff | 85 |
| Social distancing for players while playing | 54 |
| Social distancing for players off the field | 92 |
| Social distancing for staff | 85 |
| Increased facility disinfection | 74 |
| Staggered arrival and departure times for events | 84 |
DISCUSSION
These findings suggest that the incidence of COVID-19 among youth soccer athletes after reinitiating participation during the summer of 2020 was relatively low. The number of cases per 100 000 players and the incidence rates since returning to play that were reported by the participant clubs were both lower than those reported by the American Academy of Pediatrics for children in the United States during the same period.8 The disease burden and risk of COVID-19 varied considerably in different parts of the country, so we also sought to compare the COVID-19 risk of the respondents' clubs with data from the county in which the club was located. We again found that this population of youth soccer athletes had lower case and incidence rates than the populations of the counties in which their clubs are located. Despite the limitations in comparing the overall case and incidence rates in this study with the case and incidence rates of the general populations in each county, county-level data for children over the 10-week timeframe before the study were not publicly available. Nonetheless, we observed that reported club case rates were significantly related to the background case rates for their county population. Similarly, in the negative binomial models used to evaluate the influence of phase of play, county COVID-19 incidence was a highly significant predictor of reported COVID-19 incidence among clubs. Therefore, it seems reasonable to suggest that, although related to the background local COVID-19 incidence, participation in youth soccer activities was not associated with an increased risk of reported COVID-19 among participants.
In addition, these findings agree with the existing literature regarding COVID-19 severity in children,8 as none of the cases were reported to result in hospitalization or death. Finally, of the 282 reported cases among players, only 1 was attributed to transmission during soccer activities. We recognize that whether this information was obtained through formal contact tracing by the respondent clubs or another informal process to identify sources of infection is unknown. We did not solicit information regarding other known sources of reported COVID-19 infections, so the proportion of the reported cases that had any identified source outside of soccer activities cannot be assessed.
As a secondary analysis, we sought to determine whether the phase of return to soccer was associated with the risk of COVID-19 among youth players. Soccer is an outdoor sport with relatively widely distributed players who do not appear to spend significant amounts of time in proximity to one another during normal game play. Nonetheless, it has been generally accepted that contact participation would result in an increased risk of viral transmission. Initially, we found that those clubs that remained in a phase of individual training only had higher incidence rates than clubs that had progressed to noncontact or contact group play, but no difference existed between the noncontact and contact groups. Because the phase of return to youth sports was at least partly a function of the local COVID-19 disease burden, this may simply reflect a higher background incidence among those clubs that had not progressed to group play. In fact, when we adjusted for the local county COVID-19 incidence, the differences in reported COVID-19 incidence among the clubs in different phases were no longer significant.
After adjusting for the local incidence rate in the multivariable model, we did not find a significant relationship between the phase of return and the number of COVID-19 cases within each club, whereas local COVID-19 incidence remained a significant predictor. It is difficult to fully interpret these results, as most of the clubs that had advanced to contact play likely progressed through a period of noncontact play initially, and we do not know whether the reported cases among these clubs occurred during the initial noncontact phase or later during the contact phase. Nonetheless, incidence rates were similar between clubs participating in noncontact and contact group play, and neither noncontact nor contact group play was associated with an increased incidence of COVID-19 after adjusting for the local COVID-19 incidence. This may indicate that the COVID-19 risk among these youth soccer clubs was primarily a function of the background disease burden rather than participation in soccer. Given the risk-mitigation procedures in place and the outdoor, physically distributed nature of soccer, it may be that participation in soccer activities did not result in a large enough increase in COVID-19 incidence to be statistically detectable in our sample.
Multiple sports organizations, academic organizations, research groups, and federal and local health authorities11–16 have developed and recommended risk-mitigation procedures to be incorporated by sports organizations when participation restarts. Within youth sports, these may vary by activity but generally include recommendations regarding social distancing, mask use, symptom monitoring, hygiene and disinfection practices, staggered arrival and departure times, and return-to-play procedures after diagnosis or exposure. Among the respondent clubs in our study, all reported having a formal COVID-19 plan in place, and the majority described a broad range of risk-mitigation procedures. For example, more than 80% stated they had adopted symptom monitoring and temperature checks among players and staff, social distancing and face-mask use by staff and by players off the field, and staggered arrival and departure times. This suggests that youth soccer organizations were motivated to maintain an environment that would reduce the risk of COVID-19 transmission during reinitiation. However, we cannot comment on the incidence or transmission risk of COVID-19 among attendees other than players at soccer events. Although this risk remains undefined, it represents an important potential contribution to COVID-19 community spread, and several implemented risk-mitigation procedures were also intended to help reduce the risk of infection among attendees. Consequently, these measures should remain a priority for youth sports organizations.
This survey-based study had several limitations. The information self-reported by the club directors could not be verified through medical records or another independent source. It is unlikely that clubs were using serial testing of asymptomatic players, so the true COVID-19 incidence among these athletes cannot be defined. Nonetheless, the testing of symptomatic or exposed youth soccer athletes is likely comparable with the testing of children in general in the United States. Still, children from families of low socioeconomic status may be disproportionately affected by COVID-19 and yet underrepresented among the respondent clubs in our data, and we cannot account for the influence of this potential source of bias. Similarly, we were only able to obtain local-level data for respondent counties during the 10 weeks before the study and could not compare our data with local pediatric cases or incidence rates. Whether formal contact tracing was performed by the clubs involved is unknown, and we cannot directly account for the possibility of transmission between players that went unidentified. Furthermore, we do not know how many cases were attributed to sources outside of soccer as opposed to having no identified source; therefore, we cannot address the true transmission rate in youth soccer activities. Finally, although these data represent information regarding many male and female youth athletes in a nationwide sample, they should not be generalized to other sports.
In conclusion, these results suggest that the incidence of COVID-19 among youth soccer athletes was relatively low when compared with either the background incidence among children across the country or the incidence in the local general population. In addition, no difference in COVID-19 risk was identified between those clubs that had returned to contact participation and those that had not, even after adjusting for the local background disease burden and the number of risk-reduction procedures in place. These youth soccer club directors universally reported having a formal plan in place to reduce the risk of COVID-19 spread, and the overwhelming majority described using a variety of risk-mitigation procedures. Even as we hope that this information will help contribute to the ongoing discussions about the relative risks and benefits of youth sport participation, we recognize that the COVID-19 risk will surely vary among sports and different areas of the country. Also, we cannot address the potential risk of transmission among attendees at youth sporting events, which remains a vital area of future research. Therefore, these data should represent an initial step toward developing a more complete picture of the relative risk of COVID-19 transmission during sport participation for youth soccer athletes during the summer of 2020. Expansion of these efforts to make informed decisions about specific contexts is urgently needed.
REFERENCES
- 1.Bates LC, Zieff G, Stanford K, et al. COVID-19 impact on behaviors across the 24-hour day in children and adolescents: physical activity, sedentary behavior, and sleep. Children (Basel) 2020;7(9):138. doi: 10.3390/children7090138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health. 2020;20(1):1351. doi: 10.1186/s12889-020-09429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gouttebarge V, Ahmad I, Mountjoy M, Rice S, Kerkhoffs G. Anxiety and depressive symptoms during the COVID-19 emergency period: a comparative cross-sectional study in professional football. Clin J Sport Med. 2020 doi: 10.1097/JSM.0000000000000886. [DOI] [PubMed]
- 4.An R. Projecting the impact of the coronavirus disease-2019 pandemic on childhood obesity in the United States: a microsimulation model. J Sport Health Sci. 2020;9(4):302–312. doi: 10.1016/j.jshs.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174(9):819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- 6.Singh S, Roy D, Sinha K, Parveen S, Sharma G, Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. 2020;293:113429. doi: 10.1016/j.psychres.2020.113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Provisional death counts for coronavirus disease 2019 (COVID-19) Centers for Disease Control and Prevention. 2021 https://cdc.gov/nchs/nvss/vsrr/covid19/index.htm Updated April 1, 2021. Accessed April 1.
- 8.Children and COVID-19: state-level data report. American Academy of Pediatrics. 2020 https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/ Updated February 22, 2021. Accessed September 1.
- 9.Toresdahl BG, Asif IM. Coronavirus disease 2019 (COVID-19): considerations for the competitive athlete. Sports Health. 2020;12(3):221–224. doi: 10.1177/1941738120918876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asif IM, Chang CJ, Diamond AB, Raukar N, Zaremski JL. Returning athletes back to high school sports in the COVID-19 era: preparing for the fall. Sports Health. 2020;12(6):518–520. doi: 10.1177/1941738120953851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hughes D, Saw R, Perera NKP, et al. The Australian Institute of Sport framework for rebooting sport in a COVID-19 environment. J Sci Med Sport. 2020;23(7):639–663. doi: 10.1016/j.jsams.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.COVID-19 interim guidance: return to sports. American Academy of Pediatrics. 2020 https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/covid-19-interim-guidance-return-to-sports/ Updated December 17, 2020. Accessed December 21.
- 13.Considerations for youth sports. Centers for Disease Control and Prevention. https://cdc.gov/coronavirus/2019-ncov/community/schools-childcare/youth-sports.html Updated December 31, 2020. Accessed February 24, 2021.
- 14.COVID-19 return-to-sport considerations for secondary school athletic trainers. National Athletic Trainers' Association. 2020 https://nata.org/sites/default/files/covid_19_return-to-sport_considerations_for_secondary_school_ats_1.pdf Published May 2020. Accessed September 22.
- 15.Recommendations for returning to play in a training environment. Elite Clubs National League. 2020 https://theecnl.com/wp-content/uploads/2020/09/ECNL_x_Return_to_Play_Recs_V5.pdf Updated May 26, 2020. Accessed September 22.
- 16.Play on recommendations guides. United States Soccer Federation. 2020 https://ussoccer.com/playon/guides Accessed September 22.
- 17.US coronavirus cases & deaths by state. USAFacts. 2021 https://usafacts.org/visualizations/coronavirus-covid-19-spread-map Updated February 24, 2021. Accessed January 7.


