Abstract
Objective
To evaluate the evidence regarding the association between lateral ankle sprain (LAS) history and the subsequent LAS risk, as well as sex differences in the observed associations.
Data Sources
PubMed, CINAHL, and SPORTDiscus were searched through July 2020 for articles on LAS history and incidence during the study period.
Study Selection
Studies were included if they were prospective in nature and the authors reported the number of participants with and those without a history of LAS at study initiation as well as the number of participants in each group who sustained an LAS during the investigation.
Data Extraction
Data were study design parameters as well as the number of participants with and those without an LAS history and the number of subsequent LASs that occurred in both groups. Risk ratios (RRs) with 95% CIs compared the risk of LAS during the study period between those with and those without an LAS history for each investigation.
Data Synthesis
A total of 19 studies involving 6567 patients were included. The follow-up periods ranged from 14 weeks to 2 years. Assessment scores indicated the studies were of moderate to high quality. A significantly higher risk of LAS during the study period was observed among those with a history of LAS in 10 of 15 studies (RR range = 1.29–6.06). Similar associations were seen in 4 of 6 studies of all-male samples (RR range = 1.38–8.65) and 1 of 4 studies with an all-female sample (RR = 4.28).
Conclusions
Strong evidence indicates that a previous LAS increased the risk of a subsequent LAS injury. Men with a history of LAS appeared to be at a higher risk of sustaining a subsequent LAS, but women were not. However, further data are needed to draw definitive conclusions from the limited number of sex-specific studies.
Keywords: risk ratios, risk factor, epidemiology, sex
Key Points
Overall, an individual with a lateral ankle sprain had a greater risk of a subsequent lateral ankle sprain than an uninjured person.
After a lateral ankle sprain, the risk of a subsequent lateral ankle sprain was increased for men but not for women.
Lateral ankle sprain (LAS) is the most common lower extremity musculoskeletal injury1,2 and affects individuals of all ages participating in organized sports or unstructured play.3 The LAS is often erroneously considered a 1-time injury, but researchers4 have estimated that up to 74% of individuals who sustain an LAS will develop persistent adverse outcomes (eg, pain, swelling, weakness, and instability), often referred to as chronic ankle instability. An LAS has also been linked with ankle-joint degeneration and posttraumatic osteoarthritis.5 In addition to the long-term health-related consequences, LASs and their sequelae represent a significant financial burden on injured individuals and the health care system.3
Due to the extensive cost and burden of LASs, numerous authors have focused on identifying both the intrinsic (eg, balance) and extrinsic (eg, LAS history) risk factors for initial and recurrent LASs.2,6–9 Whereas multiple factors likely contribute to the risk of recurrent LAS, an LAS history has been accepted as a major risk factor for 2 main reasons: (1) selective referencing in the existing literature (ie, only citing work supporting the case being made) and (2) an LAS causes many of the other investigated risk factors (eg, poor balance, ligamentous laxity).10–12 This belief may be erroneous given that (1) a body of evidence13–17 indicates that an LAS history does not increase the risk of a subsequent LAS, and (2) no systematic examination of the cumulative literature has been completed. Due to the conflicting results across the literature, a systematic examination is necessary to gain a comprehensive understanding of how an LAS history may influence the subsequent LAS risk and thus appropriately inform primary and secondary prevention strategies (ie, prevention of index injuries and subsequent rehabilitation protocols).
Epidemiologic studies6,7,18–20 have suggested that women may be at higher risk of sustaining an initial LAS. However, fewer data exist regarding the risk of subsequent LASs among women. Only 1 study7 of collegiate athletes showed that recurrent LASs did not differ between men and women in sex-comparable sports. These varying results indicate the need for further examination of both sexes in comparable situations.
Therefore, the purpose of our investigation was to conduct a systematic review to evaluate evidence surrounding the association between LAS history and subsequent LAS risk, as well as sex differences in any observed associations. A secondary purpose was to evaluate whether a meta-analysis of the available literature was feasible. Based on the existing literature, we hypothesized that the risk of subsequent LAS would be higher in those with versus those without an LAS history. We also hypothesized that this association would not vary by sex, given data7 suggesting that the risk of recurrent LAS did not differ between men and women.
METHODS
Search Strategy
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to perform this systematic review of the available English literature. Two researchers (M.S.C. and T.R.) conducted a systematic literature search to identify studies that addressed how an LAS history might be associated with the risk of a subsequent LAS during a follow-up study period. Three databases (PubMed, CINAHL, and SPORTDiscus) were used to search for articles from the earliest available date to July 2020. The key words used were (ankle sprain* or lateral ankle sprain* or inversion sprain* OR history of ankle sprain*) and (risk or recurrence or reinjur* or re-injur* or incidence or prevalence or injury sequence or injury order or etiolog* or aetiolog*). Additional tools, such as the reference lists of screened full-text articles and Google Scholar, were also reviewed.
Selection Criteria
Studies included in this systematic review were required to meet the following criteria: (1) a prospective study, either experimental or observational in nature, involving human participants, with a sufficient study period (ie, follow-up duration) for the population of interest; (2) original research published as an article in a peer-reviewed journal; (3) publication in English and available in full text; (4) provided the number of participants who had or did not have a history of LAS at the start of the study; and (5) provided the number of participants in each group who sustained an LAS during the study period. Criteria related to the age of the study (ie, date published) were not imposed because the LAS incidence did not seem to change over time. A sufficient study period was operationally defined as at least 1 unit of time pertinent to the study population (eg, 1 season for a sporting population, 1 training block for a military population, or 1 year for a general population cohort).
Evaluation of Study Quality
A modified Newcastle-Ottawa Quality Assessment Scale for cohort studies (NOS)21 was used to evaluate the methodologic quality of each article's study design. Our inclusion criteria required all studies to involve individuals with a history of LAS. Because LAS history was the outcome of interest, our inclusion criteria therefore invalidated the fourth NOS item (“Demonstration that outcome of interest was not present at start of study”). As a result, this item was removed from the modified NOS. The modified NOS assessed nonrandomized study quality based on 8 items in 3 domains: (1) selection of the study groups, (2) comparability of the groups, and (3) ascertainment of the outcome of interest. The total score of the modified version ranged from 0 to 8 (2 points could be obtained from 1 item on comparability). A higher score indicated better methodologic quality. Each study was independently evaluated and scored by 2 authors (K.S. and K.M.). If any disagreement in scoring occurred, the 2 authors met to discuss their independent assessments and reach consensus.
Data Extraction and Analysis
Two authors (M.S.C. and T.R.) independently extracted all pertinent data from the included studies. Data were study design, study duration, study location, population of interest, number of participants with and those without an LAS history, and number of subsequent LASs sustained by both groups. When available, data stratified by sex were also extracted.
We calculated study-specific estimates of LAS risk, computed as the number of participants who incurred at least 1 LAS during the study period divided by the total number of participants. We then computed study-specific risk ratios (RRs) with 95% CIs to compare the risk of a subsequent LAS during the observation period in the LAS history group with that of the no-LAS history group, which served as the referent. The following is an example of such an RR:
 |
When possible, data for male and female participants were analyzed separately to calculate sex-stratified RRs. All RRs not including 1.00 in the 95% CI were considered statistically significant.
Assessment of Heterogeneity
Data from all studies were then consolidated to determine the magnitude of heterogeneity across studies and whether it was appropriate to conduct a meta-analysis (ie, moderate or lower heterogeneity). Statistical heterogeneity was examined using the I2 statistic. An I2 value of ≥ 70% represented a high level of heterogeneity22 and was used as the threshold for not performing a meta-analysis.
RESULTS
Articles Included
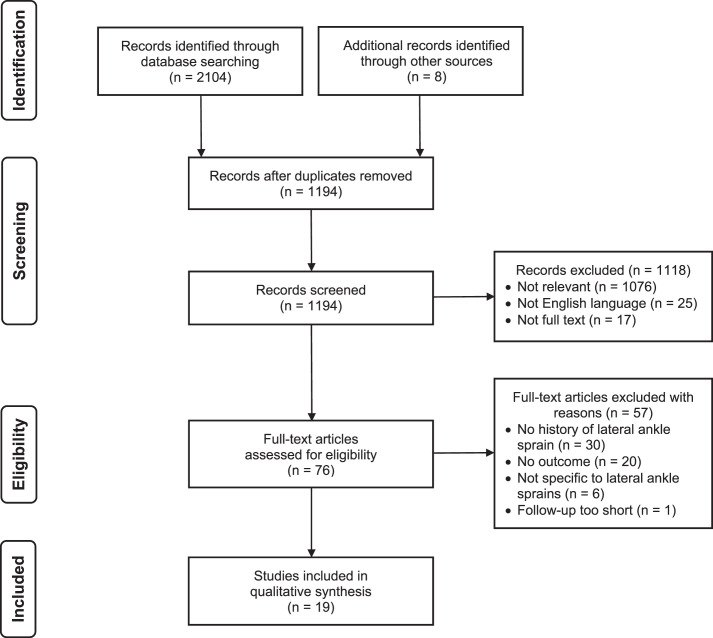
The Figure summarizes the results of the systematic search that identified a total of 2104 potential articles and 8 additional articles (eg, reference lists, Google Scholar). Overall, after we screened the potential articles by title and abstract, removed duplicates, and performed a full-text review, 19 studies were included. The studies included in the systematic review are detailed in Table 1.
Figure.
Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA): 2009 flow diagram of study-selection process.
Table 1.
Characteristics of Included Studies
| Study (Year) |
Study Duration |
Population (Age, y) |
Study Location |
Total No. of Participants |
| Arnason et al12 (2004) | 1 season (∼4 mo) | Elite soccer (16–38 y) | Iceland | 517 |
| Attenborough et al13 (2016) | 1 season (∼4 mo) | Club netball (15–29 y) | Australia | 94 |
| Bahr and Bahr27 (1997) | 1 season (TNS) | Amateur volleyball (17–28 y) | Norway | 466 |
| Barrett et al14 (1993) | 1 season (∼2 mo) | Intramural basketball (18–35 y) | United States | 569 |
| Baumhauer et al15 (1995) | 1 season (TNS) | Collegiate lacrosse, soccer, field hockey (18–23 y) | United States | 145 |
| Cumps et al34 (2007) | 22 wk | Elite youth and senior (division, not age) basketball (13–28 y) | Finland | 100 |
| de Noronha et al11 (2013) | 52 wk | Active university students (18–24 y) | Brazil | 121 |
| Ekstrand and Gillquist28 (1983) | 1 y | Elite soccer (12 teams; 17–38 y) | Sweden | 324 |
| Faude et al29 (2006) | 1 season (TNS) | Professional soccer (17–28 y) | Germany | 143 |
| Frey et al23 (2010) | 1 season (TNS) | Secondary school volleyball (15–18 y) | United States | 999 |
| Hartley et al24 (2018) | 2 y | NCAA all sports (17–22 y) | United States | 551 |
| Henry et al33 (2016) | 2 seasons (TNS) | Amateur soccer (15–23 y) | Australia | 210 |
| Hiller et al16 (2008) | 13 mo | Secondary school dance and ballet (12–16 y) | Australia | 115 |
| Kofotolis and Kellis30 (2007) | 2 y | Professional basketball (20–30 y) | Greece | 202 |
| Kofotolis et al31 (2007) | 2 y | Amateur soccer (20–30 y) | Greece | 312 |
| McGuine and Keene25 (2006) | 5 wk + Season | Secondary school soccer and basketball (15–18 y) | United States | 765 |
| Meeuwisse et al26 (2003) | 2 y | Collegiate basketball (NA) | Canada | 448 |
| Milgrom et al32 (1991) | Basic training: 14 wk | Military infantry recruits (NA) | Israel | 390 |
| Pourkazemi et al8 (2018) | 1 y | Generally active (14–40 y) | Australia | 96 |
Abbreviations: NA, not available; NCAA, National Collegiate Athletic Association; TNS, time not specified.
Assessment of Study Quality
All studies scored 5 points or more (of 8) on the modified NOS (mean = 6.58 ± 0.61) as seen in Table 2. From a comparability perspective, no study controlled for additional factors and, subsequently, each lost 1 quality-assessment point. Four studies (21%) involved a subgroup (ie, volunteers) rather than the average member of the population of interest for the question, which resulted in the loss of 1 quality-assessment point. In the outcome domain, 4 studies (21%) did not explicitly address the percentage of participants lost at follow-up or whether that percentage was small enough to draw meaningful conclusions, and they subsequently lost 1 quality-assessment point.
Table 2.
Modified Newcastle Ottawa Quality Assessment Scale21 Items and Total Scores for Included Articles
| Study (Year) |
Item, Score (Point) |
Total |
|||||||
| Selectiona |
Comparabilityb | Outcomec |
|||||||
| Q1 |
Q2 |
Q3 |
Q4 |
Q1 |
Q1 |
Q2 |
Q3 |
||
| Arnason et al12 (2004) | c (0) | a (1) | a (1) | NA | a (1) | a (1) | a (1) | a (1) | 6 |
| Attenborough et al13 (2016) | b (1) | a (1) | a (1) | NA | a (1) | a (1) | a (1) | b (1) | 7 |
| Bahr and Bahr27 (1997) | b (1) | a (1) | b (1) | NA | a (1) | b (1) | a (1) | b (1) | 7 |
| Barrett et al14 (1993) | b (1) | a (1) | b (1) | NA | a (1) | b (1) | a (1) | b (1) | 7 |
| Baumhauer et al15 (1995) | b (1) | a (1) | b (1) | NA | a (1) | a (1) | a (1) | b (1) | 7 |
| Cumps et al34 (2007) | c (0) | a (1) | b (1) | NA | a (1) | a (1) | a (1) | b (1) | 6 |
| de Noronha et al11 (2013) | c (0) | a (1) | b (1) | NA | a (1) | a (1) | a (1) | b (1) | 6 |
| Ekstrand and Gillquist28 (1983) | b (1) | a (1) | a (1) | NA | a (1) | b (1) | a (1) | a (1) | 7 |
| Faude et al29 (2006) | b (1) | a (1) | a (1) | NA | a (1) | b (1) | a (1) | a (1) | 7 |
| Frey et al23 (2010) | b (1) | a (1) | a (1) | NA | a (1) | b (1) | a (1) | d (0) | 6 |
| Hartley et al24 (2018) | c (0) | a (1) | a (1) | NA | a (1) | a (1) | a (1) | d (0) | 5 |
| Henry et al33 (2016) | b (1) | a (1) | a (1) | NA | a (1) | a (1) | a (1) | d (0) | 6 |
| Hiller et al16 (2008) | b (1) | a (1) | b (1) | NA | a (1) | a (1) | a (1) | b (1) | 7 |
| Kofotolis and Kellis30 (2007) | b (1) | a (1) | a (1) | NA | a (1) | b (1) | a (1) | b (1) | 7 |
| Kofotolis et al31 (2007) | b (1) | a (1) | a (1) | NA | a (1) | b (1) | a (1) | a (1) | 7 |
| McGuine and Keene25 (2006) | b (1) | a (1) | a (1) | NA | a (1) | b (1) | a (1) | b (1) | 7 |
| Meeuwisse et al26 (2003) | b (1) | a (1) | a (1) | NA | a (1) | b (1) | a (1) | b (1) | 7 |
| Milgrom et al32 (1991) | b (1) | a (1) | a (1) | NA | a (1) | b (1) | a (1) | d (0) | 6 |
| Pourkazemi et al8 (2018) | a (1) | a (1) | b (1) | NA | a (1) | b (1) | a (1) | a (1) | 7 |
Abbreviations: NA, not applicable; Q, question.
Q1, Representativeness of the exposed cohort; Q2, Selection of the nonexposed cohort; Q3, Ascertainment of exposure; Q4, Demonstration that outcome of interest was not present at the start of the study.
Q1, Comparability of cohorts on the basis of the design or analysis.
Q1, Assessment of outcome; Q2, Was follow-up long enough for outcomes to occur?; Q3, Adequacy of follow-up of cohorts.
Sample Characteristics
The 19 included studies8,11–16,23–34 contained a pooled total of 6567 participants. Of these, 4341 (66%) participants reported no LAS history, and 2226 (34%) participants reported an LAS history. Reporting of a history of LAS was not consistent across investigations.
Most studies were from Europe (42%, n = 8) and North America (32%, n = 6). Sixteen (84%) examined athletes; 2 (11%), the general or active population; and 1 (5%), military personnel. The sport-related research most commonly evaluated soccer athletes or players12,15,24,25,28,29,31,33 (42%, n = 8) or basketball athletes or players14,24–26,30,34 (32%, n = 6). Twelve studies8,11–16,23,25,27–29 (63%) had a 1-season or 1-year follow-up period, whereas 5 studies24,26,30,31,33 (26%) had follow-up periods of 2 seasons or 2 years.
Analysis of RRs
Across individual investigations, 15 (79%) had elevated RR point estimates, suggesting that those with a history of LAS had a higher risk of sustaining a subsequent LAS (RR range = 1.29–6.06; Table 3). Of these, 10 had RRs that were statistically significant (ie, 95% CI did not include 1.00), whereas the remaining 5 demonstrated elevated RR point estimates but had a 95% CI that included 1.00. The remaining 4 (21%) without statistically significant results had point estimates < 1.00.
Table 3.
Risk Ratios and 95% CIs Examining the Risk of Subsequent Lateral Ankle Sprain Among Those With Versus Those Without a History of Lateral Ankle Sprain
| Study (Year) |
Group, No. |
Group, Subsequent Lateral Ankle Sprain, No. (%) |
Risk Ratio (95% CI)a |
||
| No Lateral Ankle Sprain History |
Lateral Ankle Sprain History |
No Lateral Ankle Sprain History |
Lateral Ankle Sprain History |
||
| Arnason et al12 (2004) | 305 | 212 | 3 (1.0) | 11 (5.2) | 5.28 (1.49, 18.68)b |
| Attenborough et al13 (2016) | 40 | 54 | 6 (15.0) | 5 (9.3) | 0.62 (0.20, 1.88) |
| Bahr and Bahr27 (1997) | 234 | 232 | 10 (4.3) | 38 (16.4) | 3.83 (1.96, 7.51)b |
| Barrett et al14 (1993) | 328 | 241 | 10 (3.0) | 5 (2.1) | 0.68 (0.24, 1.97) |
| Baumhauer et al15 (1995) | 96 | 49 | 11 (11.5) | 4 (8.2) | 0.71 (0.24, 2.12) |
| Cumps et al34 (2007) | 58 | 42 | 7 (12.1) | 7 (16.7) | 1.38 (0.52, 3.64) |
| de Noronha et al11 (2013) | 69 | 52 | 10 (14.5) | 21 (40.4) | 2.79 (1.44, 5.40)b |
| Ekstrand and Gillquist28 (1983) | 243 | 81 | 19 (7.8) | 17 (21.0) | 2.68 (1.47, 4.91)b |
| Faude et al29 (2006) | 56 | 87 | 11 (19.6) | 22 (25.3) | 1.29 (0.68, 2.44) |
| Frey et al23 (2010) | 683 | 316 | 49 (7.2) | 44 (13.9) | 1.94 (1.32, 2.85)b |
| Hartley et al24 (2018) | 492 | 59 | 33 (6.7) | 24 (40.7) | 6.06 (3.86, 9.52)b |
| Henry et al33 (2016) | 162 | 48 | 9 (5.6) | 5 (10.4) | 1.88 (0.66, 5.33) |
| Hiller et al16 (2008) | 60 | 55 | 20 (33.3) | 16 (29.1) | 0.87 (0.51, 1.51) |
| Kofotolis and Kellis30 (2007) | 64 | 138 | 8 (12.5) | 24 (17.4) | 1.39 (0.66, 2.93) |
| Kofotolis et al31 (2007) | 180 | 132 | 55 (30.6) | 84 (63.6) | 2.08 (1.61, 2.69)b |
| McGuine and Keene25 (2006) | 583 | 182 | 35 (6.0) | 27 (14.8) | 2.47 (1.54, 3.97)b |
| Meeuwisse et al26 (2003) | 281 | 167 | 33 (11.7) | 27 (16.2) | 1.38 (0.86, 2.21) |
| Milgrom et al32 (1991) | 339 | 51 | 51 (15.0) | 16 (31.4) | 2.09 (1.29, 3.36)b |
| Pourkazemi et al8 (2018) | 68 | 28 | 3 (4.4) | 7 (25.0) | 5.67 (1.58, 20.36)b |
Risk ratios compared the risk of subsequent lateral ankle sprain in the lateral ankle sprain history group versus the no lateral ankle sprain history group, which served as the referent.
Indicates risk ratio was different (ie, 95% CI excluded 1.00).
Notably, only 1 study presented data stratified by sex, whereas 8 presented data on a specific sex (Table 4). Across individual studies, a higher risk of LAS was suggested in those with a history of LAS in 6 studies that included data specific to male athletes (RR range = 1.38–8.65); 4 of these studies had RRs that were statistically significant (ie, 95% CI did not cross 1.00). Similarly, a higher risk of LAS in the follow-up study period was observed among those with a history of LAS (versus the referent) in 4 studies that provided data specific to female athletes (RR range = 0.62–4.28); however, only 1 of these had an RR that was statistically significant (ie, 95% CI did not cross 1.00).
Table 4.
Risk Ratios and 95% CIs Examining the Risk of Subsequent Lateral Ankle Sprain Among Those With Versus Those Without a History of Lateral Ankle Sprain by Sex
| Sex |
Study (Year) |
Group, No. |
Group, Subsequent Lateral Ankle Sprain, No. (%) |
Risk Ratio (95% CI)a |
||
| No Lateral Ankle Sprain History |
Lateral Ankle Sprain History |
No Lateral Ankle Sprain History |
Lateral Ankle Sprain History |
|||
| Male | Arnason et al12 (2004) | 305 | 212 | 3 (1.0) | 11 (5.2) | 5.28 (1.49, 18.68)b |
| Hartley et al24 (2018) | 346 | 38 | 20 (5.8) | 19 (50.0) | 8.65 (5.09, 14.71)b | |
| Henry et al33 (2016) | 162 | 48 | 9 (5.6) | 5 (10.4) | 1.88 (0.66, 5.33) | |
| Kofotolis et al31 (2007) | 180 | 132 | 55 (30.6) | 84 (63.6) | 2.08 (1.61, 2.69)b | |
| Meeuwisse et al26 (2003) | 281 | 167 | 33 (11.7) | 27 (16.2) | 1.38 (0.86, 2.21) | |
| Milgrom et al32 (1991) | 339 | 51 | 51 (15.0) | 16 (31.4) | 2.09 (1.29, 3.36)b | |
| Female | Attenborough et al13 (2016) | 40 | 54 | 6 (15.0) | 5 (9.3) | 0.62 (0.20, 1.88) |
| Faude et al29 (2006) | 56 | 87 | 11 (19.6) | 22 (25.3) | 1.29 (0.68, 2.44) | |
| Hartley et al24 (2018) | 146 | 21 | 13 (8.9) | 8 (38.1) | 4.28 (2.02, 9.08)b | |
| Kofotolis and Kellis30 (2007) | 64 | 138 | 8 (12.5) | 24 (17.4) | 1.39 (0.66, 2.93) | |
Risk ratios compared the risk of subsequent lateral ankle sprain in the lateral ankle sprain history group versus the no lateral ankle sprain history group, which served as the referent.
Indicates risk ratio was different (ie, 95% CI excluded 1.00).
Heterogeneity of Studies
The observed I2 value was 71% (95% CI = 50%, 89%), indicating substantial variability among the included studies. As a result, we did not pursue a meta-analysis.
DISCUSSION
We aimed to evaluate the evidence regarding the association between LAS history and subsequent LAS risk, as well as sex differences in any observed associations. The studies were generally of high quality and involved diverse populations. Results from the systematic review supported our primary hypothesis that an LAS history is associated with a subsequent LAS risk. The results are also consistent with published findings10,35–40 that were not included in this systematic review. However, the substantial variability among the included studies prevented us from conducting a meta-analysis. Nevertheless, these findings highlight the need to develop, implement, and evaluate prophylactic interventions that prevent index injury and provide rehabilitative strategies that prevent reinjury among individuals with an LAS history.
The exact mechanism by which an LAS history increases the subsequent LAS risk remains unclear because current theoretical models suggest that a risk of recurrent LAS and the development of chronic ankle instability are influenced by multiple factors. Yet many of these possible factors are a consequence of both an index LAS and a history of multiple LASs.41,42 For example, a history of LAS is known to disrupt the structural integrity of the ligaments and sensorimotor function,3 likely impairing an individual's ability to avoid injurious situations. Evidence also suggests that individuals with chronic ankle instability (ie, those with a history of multiple LASs) alter how they weight sensory information43 and respond to fatigue,44 which would further limit an individual's ability to mitigate risk. However, it is unclear whether these adaptations appear before chronic ankle instability develops (ie, after a history of a single LAS). Based on the known consequences of an LAS, primary prevention programs that focus on sensorimotor function (eg, balance training) are effective45–47 in preventing first-time LAS. Similarly, comprehensive strategies that aim to restore sensorimotor function are recommended after an LAS48,49 because of their efficacy in treating individuals with a first-time or recurrent LAS.45–47
Despite evidence that a history of LAS and the subsequent risk of LAS were associated in both men and women, we found more robust evidence of this association in men than in women. This is contrary to our a priori hypothesis and inconsistent with data7 that demonstrated no sex differences in the proportion of recurrent LASs reported in National Collegiate Athletic Association athletes over a 5-year period. It is important to note that although the finding from the systematic review for women was not statistically significant, the effect estimate of 1.56 still reflected a moderate association that is worth additional research.50 Furthermore, given the scarcity of sex-stratified data, we advocate for continued research to better determine how this association may vary by sex. This can include increasing efforts to recruit larger samples of female participants and stratifying findings by sex.
Also, the RRs in the individual studies originated from tabular methods that did not permit control of factors such as age, playing position in sport, comorbidities, and other LAS risk factors. This was primarily due to our reliance on the demographics and statistics described in the articles to calculate risk and RRs. However, from these analyses, several trends emerged. For example, the majority of studies indicating higher subsequent LAS risk in those with an LAS history involved larger samples (total sample size ≥ 100).11,12,23–33,51 Cumulatively, these findings reinforce the importance of adequate power to capture effects and obtain precise effect estimates related to associations between LAS risk factors and recurrent LAS risk. Significant results were also noted across 3 populations (general or active adults, military, sporting): all 3 studies8,11,32 in nonsporting populations demonstrated a higher risk of subsequent LAS among those with an LAS history versus those without. Despite the consistent results among nonathletes, the generalizability of these results could be enhanced with additional samples from the general population, as well as heterogeneous samples from sporting populations (ie, samples including athletes from different sports and various levels of competition). Furthermore, significant findings were noted across studies with various follow-up durations (from 14 weeks in a military population to 2 years in a sporting population). Thus, future researchers should consider time-to-event analyses to better determine how the subsequent LAS risk changes over time. Additional exploration is also needed to confirm our initial sex-specific results and to better detect whether the injury risk varies among subgroups (eg, initial injury severity, sport).
Clinical Implications
Clinically, these results highlight the importance of (1) preventing the index LAS (ie, primary injury prevention) and (2) emphasizing the need for rehabilitative strategies (ie, secondary prevention programs) to prevent negative long-term health outcomes after an LAS. Primary52 and secondary prevention programs are effective at reducing the LAS and recurrent LAS risks, respectively,45–47 but strong barriers hinder consistent implementation of both. For example, a lack of coach education and perceived time constraints by coaches limit the deployment of programs designed to prevent an index LAS.53,54 Rehabilitative programs intended to prevent recurrent LAS are hampered by an erroneous public perception that LASs are inconsequential injuries that do not need rehabilitation. Indeed, fewer than 7% of patients with LASs complete any physical therapy within 30 days of their injury.55 Also, patients who did not seek medical care for their LASs described a greater number of recurrent LASs and worse patient-reported outcomes than those who participated in formal medical care.56 Elucidating mechanisms to overcome these barriers should be the focus of future research.
Limitations
This investigation, like all research, is not without limitations. First, we cannot determine whether our sample (ie, 34% with a history of LAS) represented the overall population of those with a history of LAS because this population has yet to be defined. Second, the existing literature did not document details related to prior or subsequent LASs (eg, number of previous LASs, severity of sprains, concurrent injuries) or the presence and severity of other potential LAS risk factors; such data might have helped to explain differences among the study findings. An example of these concerns is that most but not all of the included investigations relied on participant self-reports for the LAS history. Similarly, operational definitions of LAS were not consistent across studies, and not all authors provided complete operational definitions. As noted previously, the effect estimates computed in our study were crude and therefore did not account for possible confounding factors (eg, sensorimotor function, ligamentous laxity) that could also influence the subsequent LAS risk because those data were not included in the original research reports. Our results also did not account for exposure, a common confounding variable in injury risk, and a wide variety of follow-up periods were included in this systematic review. The body of evidence was also not robust enough to permit us to assess the associations of interest within small subgroups (eg, specific sports, positions within a sport) or at different follow-up time points (eg, 1 year, 2 years), thus limiting further subgroup analyses. Finally, we could not pursue meta-analytic techniques because of a high degree of heterogeneity among studies, which was a direct result of the small body of evidence available across various subpopulations to examine the various subgroups discussed.
CONCLUSIONS
The literature base regarding the association between an LAS history and subsequent LAS is of high quality, provides strong evidence, and supports the clinical consensus that an LAS history increases the subsequent LAS risk. Unlike female athletes, male athletes with a history of LAS appeared to be at a higher risk of sustaining a subsequent LAS. Also, substantial variability exists in the literature, which prevented us from conducting a meta-analysis.
REFERENCES
- 1.Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 2.Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92(13):2279–2284. doi: 10.2106/JBJS.I.01537. [DOI] [PubMed] [Google Scholar]
- 3.Gribble PA, Bleakley CM, Caulfield BM, et al. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact, and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50(24):1496–1505. doi: 10.1136/bjsports-2016-096189. [DOI] [PubMed] [Google Scholar]
- 4.Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39(3) doi: 10.1136/bjsm.2004.011676. e14. discussion e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Song K, Wikstrom EA. Plausible mechanisms of and techniques to assess ankle joint degeneration following lateral ankle sprains: a narrative review. Phys Sportsmed. 2019;47(3):275–283. doi: 10.1080/00913847.2019.1581511. [DOI] [PubMed] [Google Scholar]
- 6.Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44(1):123–140. doi: 10.1177/0363546516660980. [DOI] [PubMed] [Google Scholar]
- 7.Roos KG, Kerr ZY, Mauntel TC, Djoko A, Dompier TP, Wikstrom EA. The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association sports. Am J Sports Med. 2017;45(1):201–209. doi: 10.1177/0363546516660980. [DOI] [PubMed] [Google Scholar]
- 8.Pourkazemi F, Hiller CE, Raymond J, Black D, Nightingale EJ, Refshauge KM. Predictors of recurrent sprains after an index lateral ankle sprain: a longitudinal study. Physiotherapy. 2018;104(4):430–437. doi: 10.1016/j.physio.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Fousekis K, Tsepis E, Vagenas G. Intrinsic risk factors of noncontact ankle sprains in soccer: a prospective study on 100 professional players. Am J Sports Med. 2012;40(8):1842–1850. doi: 10.1177/0363546512449602. [DOI] [PubMed] [Google Scholar]
- 10.Tyler TF, McHugh MP, Mirabella MR, Mullaney MJ, Nicholas SJ. Risk factors for noncontact ankle sprains in high school football players: the role of previous ankle sprains and body mass index. Am J Sports Med. 2006;34(3):471–475. doi: 10.1177/0363546505280429. [DOI] [PubMed] [Google Scholar]
- 11.de Noronha M, Franca LC, Haupenthal A, Nunes GS. Intrinsic predictive factors for ankle sprain in active university students: a prospective study. Scand J Med Sci Sports. 2013;23(5):541–547. doi: 10.1111/j.1600-0838.2011.01434.x. [DOI] [PubMed] [Google Scholar]
- 12.Arnason A, Sigurdsson SB, Gudmundsson A, Holme I, Engebretsen L, Bahr R. Risk factors for injuries in football. Am J Sports Med. 2004;32(suppl 1):5S–16S. doi: 10.1177/0363546503258912. [DOI] [PubMed] [Google Scholar]
- 13.Attenborough AS, Sinclair PJ, Sharp T, et al. The identification of risk factors for ankle sprains sustained during netball participation. Phys Ther Sport. 2016;23:31–36. doi: 10.1016/j.ptsp.2016.06.009. [DOI] [PubMed] [Google Scholar]
- 14.Barrett JR, Tanji JL, Drake C, Fuller D, Kawasaki RI, Fenton RM. High- versus low-top shoes for the prevention of ankle sprains in basketball players. A prospective randomized study. Am J Sports Med. 1993;21(4):582–585. doi: 10.1177/036354659302100416. [DOI] [PubMed] [Google Scholar]
- 15.Baumhauer JF, Alosa DM, Renstrom AF, Trenino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;23(5):564–570. doi: 10.1177/036354659502300508. [DOI] [PubMed] [Google Scholar]
- 16.Hiller CE, Refshauge KM, Herbert RD, Kilbreath SL. Intrinsic predictors of lateral ankle sprain in adolescent dancers: a prospective cohort study. Clin J Sports Med. 2008;18(1):44–48. doi: 10.1097/JSM.0b013e31815f2b35. [DOI] [PubMed] [Google Scholar]
- 17.Fousekis K, Tsepis T, Vagenas G. Intrinsic risk factors of noncontact ankle sprains in soccer: a prospective study on 100 professional players. Am J Sports Med. 2012;40(8):1842–1850. doi: 10.1177/0363546512449602. [DOI] [PubMed] [Google Scholar]
- 18.Beynnon BD, Vacek PM, Murphy D, Alosa D. First-time inversion ankle ligament trauma: the effects of sex, level of competition, and sport on the incidence of injury. Am J Sports Med. 2005;33(10):1485–1491. doi: 10.1177/0363546505275490. [DOI] [PubMed] [Google Scholar]
- 19.Hosea TM, Carey CC, Harrer MF. The gender issue: epidemiology of ankle injuries in athletes who participate in basketball. Clin Orthop. 2000;(372):45–49. doi: 10.1097/00003086-200003000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Shah S, Thomas AC, Noone JM, Blanchette CM, Wikstrom EA. Incidence and cost of ankle sprains in United States emergency departments. Sports Health. 2016;8(6):547–552. doi: 10.1177/1941738116659639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wells GA, Shea B, O'Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute Web site. 2020 http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp Accessed November 22.
- 22.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analysis. BMJ. 2003;327(6):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frey C, Feder KS, Sleight J. Prophylactic ankle brace use in high school volleyball players: a prospective study. Foot Ankle Int. 2010;31(4):296–300. doi: 10.3113/FAI.2010.0296. [DOI] [PubMed] [Google Scholar]
- 24.Hartley EM, Hoch MC, Boling MC. Y-balance test performance and BMI are associated with ankle sprain injury in collegiate male athletes. J Sci Med Sport. 2018;21(7):676–680. doi: 10.1016/j.jsams.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 25.McGuine TA, Keene JS. The effect of a balance training program on the risk of ankle sprains in high school athletes. Am J Sports Med. 2006;34(7):1103–1111. doi: 10.1177/0363546505284191. [DOI] [PubMed] [Google Scholar]
- 26.Meeuwisse WH, Sellmer R, Hagel BE. Rates and risks of injury during intercollegiate basketball. Am J Sports Med. 2003;31(3):379–385. doi: 10.1177/03635465030310030901. [DOI] [PubMed] [Google Scholar]
- 27.Bahr R, Bahr IA. Incidence of acute volleyball injuries: a prospective cohort study of injury mechanisms and risk factors. Scand J Med Sci Sports. 1997;7(3):166–171. doi: 10.1111/j.1600-0838.1997.tb00134.x. [DOI] [PubMed] [Google Scholar]
- 28.Ekstrand J, Gillquist J. Soccer injuries and their mechanisms: a prospective study. Med Sci Sports Exerc. 1983;15(3):267–270. doi: 10.1249/00005768-198315030-00014. [DOI] [PubMed] [Google Scholar]
- 29.Faude O, Junge A, Kindermann W, Dvorak J. Risk factors for injuries in elite female soccer players. Br J Sports Med. 2006;40(9):785–790. doi: 10.1136/bjsm.2006.027540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kofotolis N, Kellis E. Ankle sprain injuries: a 2-year prospective cohort study in female Greek professional basketball players. J Athl Train. 2007;42(3):388–394. [PMC free article] [PubMed] [Google Scholar]
- 31.Kofotolis ND, Kellis E, Vlachopoulos SP. Ankle sprain injuries and risk factors in amateur soccer players during a 2-year period. Am J Sports Med. 2007;35(3):458–466. doi: 10.1177/0363546506294857. [DOI] [PubMed] [Google Scholar]
- 32.Milgrom C, Shlamkovitch N, Finestone A, et al. Risk factors for lateral ankle sprain: a prospective study among military recruits. Foot Ankle. 1991;12(1):26–30. doi: 10.1177/107110079101200105. [DOI] [PubMed] [Google Scholar]
- 33.Henry T, Evans K, Snodgrass SJ, Miller A, Callister R. Risk factors for noncontact ankle injuries in amateur male soccer players: a prospective cohort study. Clin J Sport Med. 2016;26(3):251–258. doi: 10.1097/JSM.0000000000000240. [DOI] [PubMed] [Google Scholar]
- 34.Cumps E, Verhagen E, Meeusen R. Efficacy of a sports specific balance training programme on the incidence of ankle sprains in basketball. J Sports Sci Med. 2007;6(2):212–219. [PMC free article] [PubMed] [Google Scholar]
- 35.Herzog MM, Mack CD, Dreyer NA, et al. Ankle sprains in the National Basketball Association, 2013–2014 through 2016–2017. Am J Sports Med. 2019;47(11):2651–2658. doi: 10.1177/0363546519864678. [DOI] [PubMed] [Google Scholar]
- 36.Kofotolis N. Ankle sprain injuries in soccer players aged 7–15 years during a one-year season. Biol Exerc. 2014;10(2):37–55. doi: 10.4127/jbe.2014.0077. [DOI] [Google Scholar]
- 37.Ekstrand J, Tropp H. The incidence of ankle sprains in soccer. Foot Ankle. 1990;11(1):41–44. doi: 10.1177/107110079001100108. [DOI] [PubMed] [Google Scholar]
- 38.Verhagen EA, Van der Beek AJ, Bouter LM, Bahr RM, Van Mechelen W. A one season prospective cohort study of volleyball injuries. Br J Sports Med. 2004;38(4):477–481. doi: 10.1136/bjsm.2003.005785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McHugh MP, Tyler TF, Tetro DT, Mullaney MJ, Nicholas SJ. Risk factors for noncontact ankle sprains in high school athletes: the role of hip strength and balance ability. Am J Sports Med. 2006;34(3):464–470. doi: 10.1177/0363546505280427. [DOI] [PubMed] [Google Scholar]
- 40.Kucera KL, Marshall SW, Wolf SH, Padua DA, Cameron KL, Beutler AI. Association of injury history and incident injury in cadet basic military training. Med Sci Sports Exerc. 2016;48(6):1053–1061. doi: 10.1249/MSS.0000000000000872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hertel J, Corbett RO. An updated model of chronic ankle instability. J Athl Train. 2019;54(6):572–588. doi: 10.4085/1062-6050-344-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wikstrom EA, Hubbard-Turner T, McKeon PO. Understanding and treating lateral ankle sprains and their consequences. Sports Med. 2013;43(6):385–393. doi: 10.1007/s40279-013-0043-z. [DOI] [PubMed] [Google Scholar]
- 43.Song K, Burcal CJ, Hertel J, Wikstrom EA. Increased visual use in chronic ankle instability: a meta-analysis. Med Sci Sports Exerc. 2016;48(10):2046–2056. doi: 10.1249/MSS.0000000000000992. [DOI] [PubMed] [Google Scholar]
- 44.Webster KA, Pietrosimone BG, Gribble PA. Muscle activation during landing before and after fatigue in individuals with or without chronic ankle instability. J Athl Train. 2016;51(8):629–636. doi: 10.4085/1062-6050-51.10.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Doherty C, Bleakley C, Delahunt E, Holden S. Treatment and prevention of acute and recurrent ankle sprain: an overview of systematic reviews with meta-analysis. Br J Sports Med. 2017;51(2):113–125. doi: 10.1136/bjsports-2016-096178. [DOI] [PubMed] [Google Scholar]
- 46.Rivera MJ, Winkelmann ZK, Powden CJ, Games KE. Proprioceptive training for the prevention of ankle sprains: an evidence-based review. J Athl Train. 2017;52(11):1065–1067. doi: 10.4085/1062-6050-52.11.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schiftan GS, Ross LA, Hahne AJ. The effectiveness of proprioceptive training in preventing ankle sprains in sporting populations: a systematic review and meta-analysis. J Sci Med Sport. 2015;18(3):238–244. doi: 10.1016/j.jsams.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 48.Delahunt E, Bleakley CM, Bossard DS, et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the International Ankle Consortium. Br J Sports Med. 2018;52(20):1304–1310. doi: 10.1136/bjsports-2017-098885. [DOI] [PubMed] [Google Scholar]
- 49.Kerkhoffs GM, van den Bekerom M, Elders LA, et al. Diagnosis, treatment, and prevention of ankle sprains: an evidence-based clinical guideline. Br J Sports Med. 2012;46(12):854–860. doi: 10.1136/bjsports-2011-090490. [DOI] [PubMed] [Google Scholar]
- 50.Wilkerson GB, Denegar CR. A growing consensus for change in interpretation of clinical research evidence. J Athl Train. 2018;53(3):320–326. doi: 10.4085/1062-6050-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McKay GD, Goldie PA, Payne WR, Oakes BW. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35(2):103–108. doi: 10.1136/bjsm.35.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Grimm NL, Jacobs JC, Kim J, Amendola A, Shea KG. Ankle injury prevention programs for soccer athletes are protective. J Bone Joint Surg Am. 2016;98(17):1436–1443. doi: 10.2106/JBJS.15.00933. [DOI] [PubMed] [Google Scholar]
- 53.Donaldson A, Callaghan A, Bizzini M, Jowett A, Keyzer P, Nicholson M. A concept mapping approach to identifying the barriers to implementing an evidence-based sports injury prevention programme. Inj Prev. 2019;25(4):244–251. doi: 10.1136/injuryprev-2017-042639. [DOI] [PubMed] [Google Scholar]
- 54.Mawson R, Creech MJ, Peterson DC, Farrokhayar F, Ayeni OR. Lower limb injury prevention programs in youth soccer: a survey of coach knowledge, usage, and barriers. J Exp Orthop. 2018;5(1):43. doi: 10.1186/s40634-018-0160-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Feger MA, Glaviano NR, Donovan L, et al. Current trends in the management of lateral ankle sprain in the United States. Clin J Sport Med. 2017;27(2):145–152. doi: 10.1097/JSM.0000000000000321. [DOI] [PubMed] [Google Scholar]
- 56.Hubbard-Turner T. Lack of medical treatment from a medical professional after an ankle sprain. J Athl Train. 2019;54(6):671–675. doi: 10.4085/1062-6050-428-17. [DOI] [PMC free article] [PubMed] [Google Scholar]