Abstract
International literature has shown that adolescents represent the population most at risk of fatal and nonfatal motor vehicle collisions (MVCs). Adolescents’ alexithymic traits and significant use of immature defense strategies have been seen to play a key role. This study aimed to investigate the possible mediation role played by defense strategies use in the relationship between alexithymia and MVCs. Our sample consisted of 297 adolescents divided into four subgroups, based on the number of visits to the emergency department due to an MVC. We assessed adolescents’ alexithymic traits and defense strategies use through self-report instruments. Results showed that males reported a higher rate of MVCs than females. Higher rates of MVCs are associated with more alexithymic traits and maladaptive defense strategies use. Adolescents’ Acting Out and Omnipotence use significantly mediated the relationship between alexithymia and MVCs. Our findings suggest the recidivism of MVCs as an attempt to cope with emotional difficulties, with important clinical implications.
Keywords: motor vehicle collision, alexithymia, defense strategies use, adolescence
1. Introduction
Injuries among adolescents represent a research issue that has increasingly involved the scientific community [1,2,3]. In this field, motor vehicle collisions (MVCs) represent one of the main causes of death among 14- to 19-year-olds worldwide [4,5,6], who constitute the population most at risk even of nonfatal MVCs. Epidemiological studies on adolescents’ road collisions have reported a rate of prevalence of approximately of 50% [7,8,9], with important consequences for their psychological and physical well-being [10,11,12]. Most studies have shown a higher prevalence of injuries and road accidents among males [13,14,15,16,17], and results concerning females in relation to road accidents are few and inconsistent [18,19].
From a developmental point of view, adolescence represents a crucial phase of the human life cycle [20,21], due to irreversible changes in affective, cognitive, behavioral and social functioning [22,23,24], as well as the redefinition of relationships with family and peer groups [25,26]. Evidence from neuroscience studies has also shown the presence of important brain transformations during adolescence, such as a decrease in synapses and modifications in the limbic system [27,28,29]. These characteristics seem to be crucial in terms of adolescents’ emotional regulation and behavioral conducts [30,31,32], predisposing youths to greater susceptibility to different risky behaviors [33,34,35], including MVCs [36,37,38,39].
1.1. Literature Review
Adolescents’ MVCs represents a major public policy and health concern due to their severe psychological and physical consequences. Given the clinical relevance of the phenomenon, a better understanding of the underpinning mechanisms associated with multiple MVCs in adolescence is needed. In this context, some authors have considered MVCs as a consequence of adolescents’ practical inexperience and related errors (including loss of control, inadequate surveillance, speeding, and slippery roads) [40,41], distractions [42], deliberate violations of driving rules, or other factors commonly related to substance use [43,44]. However, a growing body of research has shown that MVCs during adolescence tend to occur many times over a few years [45,46], suggesting a more complex underlying etiology [47,48,49]. Interestingly, it has been recently suggested that personal factors (e.g., low education level and income, impulsivity, sensation-seeking, and low levels of altruism) [50,51], as well as their interaction with environmental/situational features (e.g., time delay, volume and traffic conditions) may lead to a higher risk of road collisions [52,53]. Nevertheless, to date, most of studies have focused on the possible consequences of adolescents’ MVCs (such as psychological and physical acute, chronic, fatal outcomes) [54,55,56]. Only a few studies have explored the possible individual vulnerabilities that may predispose the adolescent to a higher risk of MVCs [57,58,59,60]. In this field, clinicians and researchers rooted in the Developmental Psychopathology framework [61,62] have suggested that the presence of adolescents’ emotional difficulties preceding the accidents may lead to a higher risk of a MVC [63,64,65], as a form of acting out to cope with underlying psychological sufferance [66,67,68]. Some studies have focused on clinical samples of adolescents, evidencing significant associations between MVCs and ADHD [69], depression [70], personality disorders [71], and binge eating disorder [64]. However, the key role played by adolescents’ emotional difficulties has also been highlighted in non-clinical samples. Specifically, adolescents’ alexithymic traits and massive use of immature defense strategies have been widely prospectively associated with a broad range of externalizing problems [72], including behavioral addiction [73], substance use [74], and risk taking [75].
Interestingly, international literature has shown that the relationship between alexithymia and immature defense strategies is dynamic [76,77], evidencing a strong association between these variables [78,79], both in clinical [80,81] and non-clinical samples [82]. However, to date, research in the field of adolescents’ high-risk behaviors (such as MVCs) and externalizing difficulties has reported conflicting findings regarding the possible interplay between alexithymia and defense strategies use. Indeed, whereas some studies have suggested the mediation role of alexithymia in the relationship between dysfunctional defense mechanisms and adolescents’ high-risk activities [83], other studies have suggested that the relationship between alexithymic traits and maladaptive psychological functioning could be mediated by immature defense strategies use [76,79]. Research specifically focusing on MVCs in adolescence is scarce [45,46,84], but it has also shown significant associations both with alexithymia and immature defense strategies [63,64,85]. However, to date, no study has explored this complex relationship in relation to adolescents’ MVCs.
1.2. Current Study
A growing body of research in the field of high-risk behaviors during adolescence has underlined the key role played by adolescents’ emotional difficulties (i.e., alexithymia and massive use of maladaptive defense strategies) in increasing the risk of MVCs [45,46,75,84,85]. Consequently, it is important to implement knowledge of the complex relationship between these risk factors associated with adolescents’ MVCs to guide the planning of more effective prevention programs and reduce recidivism. Indeed, psycho-educational prevention programs aimed primarily at the promotion of adolescents’ copying skills related to safe driving, have produced mixed results for their effectiveness [86,87]. Based on these premises, we aimed to explore whether maladaptive defense strategies use may be a mechanism through which alexithymia affects the incidence of MVCs among adolescents.
Specifically, this study aimed to verify in a sample of male and female adolescents: (1) the possible differences between male and female youths in the recidivism of MVCs. Based on previous literature [13,14,15,16,17], we hypothesized a higher rate of MVCs among adolescent males. (2) The possible associations between MVCs, alexithymic traits, and maladaptive defense strategies use. We hypothesized that a higher rate of MVCs is associated with higher emotional difficulties in terms of alexithymia and significant use of immature defense strategies, in line with previous studies in the field [63,64,85]. (3) Possible mediation role played by adolescents’ maladaptive defense strategies use in the relationship between alexithymia and frequencies of MVCs. In accordance with recent studies that have shown that immature defense strategies use mediated the relationship between alexithymia and a wide range of psychopathological problems [76,79], we hypothesized that adolescents’ massive use of immature defense strategies may be a mechanism through which alexithymia leads to a higher incidence of MVCs.
2. Materials and Methods
2.1. Subjects, Recruitment and Procedure
Over a period of one year, we recruited n = 516 adolescents aged from 14 to 19 years through the collaboration of an Italian emergency department (ED) and private and public high schools in central Italy. To recruit adolescents who had experience with one or more MVCs, we used consecutive sampling, selecting all adolescents who accessed an ED over a period of one year. Given that it is a nonprobability sampling method, our sample should not be representative of the population due to inherent biases in the sampling process. Within the total sample, n = 285 of adolescents visited an ED for an MVC. From these subjects, as suggested by previous studies in this field [63,64,85], we excluded adolescents who were passengers at the moment of the collision (n = 29), adolescents with serious injuries (n = 20), adolescents who were positive for alcohol or drug use (n = 15), adolescents with a mental and/or physical disability (n = 21), adolescents who were following a psychological and/or psychiatric treatment (n = 17), adolescents who did not complete the assessment procedure (n = 13), and adolescents who did not consent to participate to the study (or whose parents denied consent to participate in the study) (n = 20). The final sample of adolescents, who had experienced one or more MVCs, consisted of n = 180 adolescents (73.3% males), with an average age of 16.62 (SD = 1.79). We also recruited a control group of n = 231 adolescents from which we excluded adolescents who had physical or mental disorders (n = 19), who were following psychological and/or psychiatric treatment (n = 21), who did not complete the assessment procedure (n = 35), and who refused to participate in the study (n = 29). The final normative sample (control group) consisted of n = 117 adolescents (50.4% males) aged from 14 to 19 years (M = 16.30, SD = 1.77).
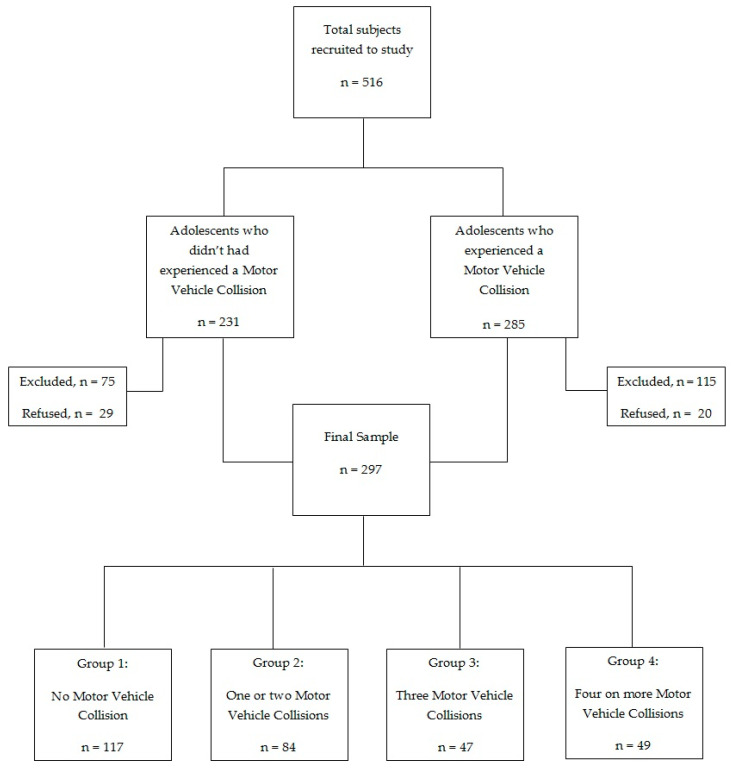
As suggested by Marcelli and colleagues [88], the sample (n = 297) was divided into the following four groups, based on the number of visits to the emergency department: Group 1 (n = 117): adolescents who had not experienced a MVC; Group 2 (n = 84): adolescents who had experienced one or two MVCs; Group 3 (n = 47): adolescents who had experienced three MVCs; Group 4 (n = 49): adolescents who had experienced four or more MVCs. The flowchart of the recruitment process is presented in Figure 1.
Figure 1.
Recruitment process flowchart.
Most of the adolescents’ families were Caucasian (93.9%), and 66% had a household income between 28,001 and 55,000 euros per year. Of the adolescents, 78.11% were in intact family groups and 63% were firstborns. Before the start of the study, in line with the Declaration of Helsinki, La Sapienza University of Rome Ethical Committee approved the research plan. All the participants fill out an informed consent document. Finally, the privacy of the personal data was guaranteed. The complete description of the sample demographic characteristics is reported in Table 1.
Table 1.
Sample Demographic Characteristics.
| Group 1 (n = 117) |
Group 2 (n = 84) |
Group 3 (n = 47) |
Group 4 (n = 49) |
|
|---|---|---|---|---|
| Age in years, M(SD) | 16.30(1.77) | 16.01(1.63) | 17.28(1.75) | 17.02(1.80) |
| Sex, n(%) | ||||
| Male | 59(50.4) | 55(65.5) | 39(83.8) | 38(77.6) |
| Female | 58(49.6) | 29(34.5) | 8(17) | 11(22.4) |
| Race, n(%) | ||||
| Caucasian | 115(98.3) | 76(90.5) | 44(93.6) | 44(89.8) |
| Other | 2(1.7) | 8(9.5) | 3(6.4) | 5(10.2) |
| Household income (EUR/year) | ||||
| 0–15,000 | 12(10.2) | 14(16.6) | 5(10.6) | 4(8) |
| 15,001–28,000 | 8(6.8) | 6(7.1) | 4(8.6) | 28(4) |
| 28,001–55,000 | 75(64.1) | 47(55.9) | 35(74.4) | 39(79.6) |
| 55,001–75,000 | 19(16.2) | 15(17.8) | 3(6.4) | 4(8) |
| >75,000 | 3(2.5) | 2(2.3) | 0 | 0 |
| Family structure, n(%) | ||||
| Intact | 84(71.8) | 63(75) | 41(87.2) | 44(89.8) |
| Broken | 33(28.2) | 21(25) | 6(12.8) | 5(10.2) |
| Number of siblings, n(%) | ||||
| 0 | 23(19.5) | 31(37) | 16(3) | 21(42.8) |
| 1–2 | 68(58.1) | 37(44) | 19(40.4) | 15(30.6) |
| 3–5 | 21(17.9) | 15(17.8) | 12(24.3) | 13(26.6) |
| >5 | 5(4.2) | 1(1.2) | 0 | 0 |
| Birth order, n(%) | ||||
| First position | 102(87.1) | 39(46.4) | 27(57.4) | 19(38.8) |
| Other positions | 15(12.8) | 45(53.6) | 20(42.6) | 30(61.2) |
Group 1 = Adolescents who had not experienced a motor vehicle collision; Group 2 = Adolescents who have experienced one or two motor vehicle collisions; Group 3 = Adolescents who have experienced three motor vehicle collisions; Group 4 = Adolescents who have experienced four or more motor vehicle collisions.
All participants were administered an ad-hoc anamnestic questionnaire, evaluating different aspects (psychological, relational and social characteristics). The administration of questionnaires was made by expert psychologists inside a room made available, respectively, by an ED and private and public high schools. The following questionnaires were distributed to all study participants in a randomized order.
2.2. Measures
The Toronto Alexithymia Scale (TAS-20) is a self-report instrument for the assessment of alexithymia, composed of 20 items [89,90]. All items to be answered are scored on a 5-point Likert scale (from 1 = strongly disagree, to 5 = strongly agree). The scale is composed of three factors that reflect the more relevant elements of the construct of alexithymia. The first factor (Factor 1) assesses the ability to recognize emotions, differentiating them from physical sensations. Factor 2 refers to the ability to describe verbally one’s own emotions. Factor 3 assesses externally oriented thinking. The three-factor structure of the scale has been reported to be theoretically congruent with the alexithymia construct. Higher scores on the scales indicate difficulty in identifying and describing emotion and limited emotional functioning. Specifically, scores ≤50 indicate no alexithymia, scores between 51 and 60 are indicative of borderline alexithymia, and scores ≥61 indicate alexithymia. The TAS-20 showed good internal consistency and test–retest reliability (the total score’s internal reliability coefficient is 0.86). In the present study, Cronbach’s alpha for Factor 1 was 0.77, for Factor 2 was 0.79, and for Factor 3 was 0.87.
Adolescents’ use of defense strategies was measured by the Response Evaluation Measure (REM-71) [91,92]. The REM-71 is a self-report questionnaire composed of 71 items that assess various defense strategies, reporting the following: Acting out, Splitting, Displacement, Dissociation, Fantasy, Passive aggression, Projection, Repression, Omnipotence, Undoing, Conversion, Somatization, Withdrawal, Suppression, Denial, Humor, Intellectualization, Reaction Formation, Idealization, Altruism, and Sublimation. All items are scored on a 9-point scale from ‘‘strongly disagree” (scored as 1) to ‘‘strongly agree” (scored as 9). Higher scores on the scales indicate a massive and problematic use of the defense strategies. Research has shown good validity, reliability, and internal consistency for the scales of REM-71 [91]. In the present study, reliability of the REM-71 was also adequate (α = 0.74–0.88).
2.3. Statistical Analyses
Preliminary statistical analyses were conducted using descriptive statistics (frequencies, reliability of the measures, and mean scores). Chi-Square analysis was used to verify possible association between adolescents’ sex and MVCs. The number of cases in a cell can be considered significantly larger than those expected if the value of the relative adjusted residual is higher than 1.96 in absolute value. We reported information about the frequency distribution of the variables within a contingency table. Differences between the four groups in adolescents’ alexithymic traits and defense strategies use, considering the possible role played by adolescents’ sex, were examined using two-way multivariate analyses of variance (MANOVA). The differences between the sample means were identified used Bonferroni’s post hoc test. Finally, parallel mediation analyses were conducted to verify whether defense strategies use mediated the effect of alexithymia on the frequency of MVCs. We used Hayes’s PROCESS macro [93], considering adolescents’ sex and age as covariates. Before performing the mediation analyses, the scores of the independent variable and of the mediators were standardized. Indirect effects were evaluated with 95% bias-corrected confidence intervals (CI) based on 10.000 bootstrap samples. When CI do not include zero, it indicates that the effect is significant at α = 0.05. All analyses were performed using IBM SPSS software 25.0.
3. Results
3.1. Association between Adolescent’s Sex and Motor Vehicle Collisions
To verify the possible significant association between MVCs and adolescents’ sex, Chi-Square analysis was carried out. Results showed the presence of a significant association between adolescent sex and MVCs frequencies, χ2 (3, n = 297) = 20.75, p < 0.001. Specifically, as shown in Table 2, a detailed inspection of the contingency table showed that there was a significant association between female sex and the absence of MVCs, whereas male sex was associated with having had three or more MVCs in the past two years.
Table 2.
Association between adolescents’ sex and motor vehicle collisions (MVCs).
| Adolescent’s Group | Total | |||||
|---|---|---|---|---|---|---|
| Sex | Group 1 | Group 2 | Group 3 | Group 4 | ||
| Male | n | 59 | 55 | 39 | 38 | 191 |
| Exp. Val. | 75.2 | 54.0 | 30.2 | 31.5 | ||
| % within sex | 30.9% | 28.8% | 20.4% | 19.9% | ||
| % within group | 50.4% | 65.5% | 83.0% | 77.6% | ||
| St. R | −4.0 | 0.30 | 2.9 | 2.1 | ||
| Female | n | 58 | 29 | 8 | 11 | 106 |
| Exp. Val. | 41.8 | 30.0 | 16.8 | 17.5 | ||
| % within sex | 54.7% | 27.4% | 7.5% | 10.4% | ||
| % within group | 49.6% | 34.5% | 17.0% | 22.4% | ||
| St. R | 4.0 | −0.30 | −2.9 | −2.1 | ||
| Total | n | 117 | 84 | 47 | 49 | 297 |
Exp. Val = Expected Values; % within sex = percentage within sex group; % within group = percentage within adolescent’s motor vehicle collision group; St. R = Standardized Adjusted Residuals. Group 1 = Adolescents who have not experienced a motor vehicle collision; Group 2 = Adolescents who have experienced one or two motor vehicle collisions; Group 3 = Adolescents who have experienced three motor vehicle collisions; Group 4 = Adolescents who have experienced four or more motor vehicle collisions.
3.2. Alexithymic Traits and Defense Strategies Use in the Four Groups
To verify the possible differences between the four groups in alexithymic traits and defense strategies use, two-way MANOVA analyses were conducted. Results showed a non-significant interaction effect between sex and group, but there was a main significant effect of group [λ = 0.10, F = 11.66, p = <0.000, ηp2 = 0.53]. As shown in Table 3, analysis of the univariate effects showed the presence of significant differences between the four groups in the scores of Factor 1, Factor 3, and the Total score of TAS-20. Specifically, the Bonferroni post-hoc test showed that adolescents in Group 1 reported significantly lower scores of Factors 1 and 2 than other groups, whereas adolescents in Group 4 had the highest scores in the same dimensions of TAS-20. Moreover, they exceeded the clinical range cut-off in the Total score of TAS-20. At the same time, adolescents in Group 3 reported higher scores than adolescents in Group 2. However, both adolescents in Group 2 and Group 3 reported Total scores of TAS-20 in the borderline range. Moreover, there were significant group differences in the scores of Acting out, Omnipotence, Passive Aggression, Denial, Conversion, and Withdrawal. In particular, adolescents in Group 4 reported significantly higher scores of Acting Out, Omnipotence, and Passive Aggression than all other groups, and higher scores of Denial, Conversion, and Withdrawal with respect to adolescents in Groups 1 and 2. Adolescents in the control group (Group 1) reported significantly lower scores for all these defense strategies with respect to other groups, except for Conversion.
Table 3.
Univariate results of the differences between the three groups in youth’s family functioning, impulsivity, depression and anxiety problems between youth’s sex and IA.
| Adolescent’s Group | |||||||
|---|---|---|---|---|---|---|---|
| Group 1 M(SD) |
Group 2 M(SD) |
Group 3 M(SD) |
Group 4 M(SD) |
F3293 | p-Value | ||
| TAS-20 | Factor 1 | 7.12(1.72) a | 14.60(3.96) b | 17.44(4.37) c | 19.44(4.18) d | 208.94 | <0.001 |
| Factor 2 | 15.81(5.37) a | 17.58(6.13) a | 16.31(4.98) a | 16.79(6.94) a | 1.56 | 0.19 | |
| Factor 3 | 11.36(3.51) a | 20.86(4.57) b | 21.51(4.99) c | 25.46(5.65) d | 152.86 | <0.001 | |
| Total | 34.30(7.27) a | 53.05(9.02) b | 55.27(7.78) b | 61.71(10.85) c | 163.35 | <0.001 | |
| REM-71 | Acting out | 2.93(1.36) a | 4.28(1.41) b | 5.20(1.69) c | 6.28(1.92) d | 62.93 | <0.001 |
| Splitting | 6.08(1.70) a | 6.11(1.56) a | 5.79(1.86) a | 5.72(1.89) a | 0.83 | 0.47 | |
| Displacement | 4.31(2.02) a | 4.10(1.80) a | 4.34(1.86) a | 4.95(4.81) a | 1.10 | 0.34 | |
| Dissociation | 4.16(1.83) a | 4.42(1.77) a | 4.21(1.54) a | 3.90(1.88) a | 0.91 | 0.43 | |
| Fantasy | 4.05(2.06) a | 4.96(4.03) a | 4.55(2.11) a | 4.25(2.05) a | 1.84 | 0.14 | |
| Omnipotence | 3.45(1.26) a | 5.36(1.09) b | 5.56(1.64) c | 7.27(1.75) d | 97.86 | <0.001 | |
| PassiveAggression | 4.20(1.74) a | 5.13(1.88) b | 5.08(1.73) c | 6.46(1.71) d | 18.96 | <0.001 | |
| Projection | 3.08(1.80) a | 3.17(1.74) a | 3.16(1.91) a | 3.29(2.13) a | 0.15 | 0.92 | |
| Suppression | 4.18(1.85) a | 4.32(1.78) a | 4.35(1.89) a | 4.66(1.89) a | 0.79 | 0.49 | |
| Undoing | 5.13(1.85) a | 5.30(1.63) a | 4.84(1.92) a | 4.76(1.75) a | 1.29 | 0.27 | |
| Sublimation | 5.19(1.61) a | 5.20(1.55) a | 5.15(1.56) a | 5.34(1.68) a | 0.12 | 0.94 | |
| Altruism | 7.13(1.41) a | 7.13(1.44) a | 7.38(1.64) a | 6.75(1.83) a | 1.41 | 0.23 | |
| Denial | 4.39(1.94) a | 4.21(1.73) b | 5.43(1.46) b | 5.85(1.90) c | 12.19 | <0.001 | |
| Humor | 5.07(1.71) a | 5.57(1.82) a | 5.35(1.56) a | 5.66(1.76) a | 1.97 | 0.11 | |
| Idealization | 6.11(1.74) a | 6.40(1.93) a | 6.35(1.96) a | 6.42(1.68) a | 0.54 | 0.65 | |
| Intellectualization | 5.42(1.55) a | 5.30(1.91) a | 4.89(1.56) a | 5.15(1.71) a | 1.19 | 0.31 | |
| Reactive Formation | 4.44(2.57) a | 4.48(1.84) a | 3.78(1.75) a | 4.14(1.64) a | 1.38 | 0.24 | |
| Repression | 4.92(1.60) a | 4.75(1.53) a | 4.83(1.48) a | 4.95(1.79) a | 0.24 | 0.86 | |
| Conversion | 1.33(.79) a | 1.61(1.11) a | 1.86(1.61) a | 2.25(2.06) b | 6.18 | <0.001 | |
| Somatization | 3.42(1.85) a | 3.58(1.93) a | 3.63(1.80) a | 3.92(2.05) a | 0.80 | 0.49 | |
| Withdrawal | 3.76(2.24) a | 5.21(2.18) b | 5.86(1.85) b | 6.55(1.60) c | 26.05 | <0.001 | |
Different letters indicate significant differences. TAS-20 = Toronto Alexithymia Scale; Factor 1 = Difficulties identifying feelings; Factor 2 = Difficulties describing feelings; Factor 3 = Externally oriented thinking; REM-71 = Response Evaluation Measure-71; Group 1 = Adolescents who have not experienced a motor vehicle collision; Group 2 = Adolescents who have experienced one or two motor vehicle collisions; Group 3 = Adolescents who have experienced three motor vehicle collisions; Group 4 = Adolescents who have experienced four or more motor vehicle collisions. All bold values are statistically significant.
3.3. Adolescents’ Defense Strategies Use as Mediators of the Relationship between Alexithymia and MVCs
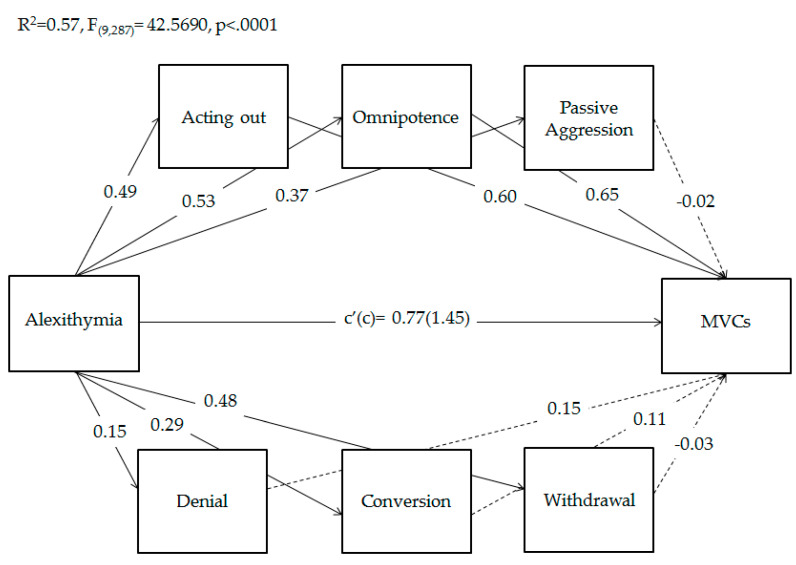
Finally, based on previous results, to verify whether adolescents’ specific defense strategies use (i.e., Acting out, Omnipotence, Passive Aggression, Denial, Conversion, and Withdrawal) mediated the relationship between adolescents’ alexithymia and the frequency of MVCs, parallel mediation analyses were conducted using PROCESS macro [85]. As shown in Figure 2, results of mediation analyses showed that both the total and direct effects of alexithymia on MVCs were significant. Moreover, the direct effects of alexithymia on all considered defense strategies use were significant. In addition, adolescents’ use of Acting Out and Omnipotence significantly predicted MVCs, while the other defenses did not. Overall, this model explained 57% of the variance in adolescents’ MVCs.
Figure 2.
Parallel mediation of adolescents’ defense strategies use on the relationship between alexithymia and the frequency of motor vehicle collisions (MVCs). Coefficients shown are standardized path coefficients. Dotted lines represent non-significant parameters. c’ = direct effect; c = total effect.
Regarding indirect effects, Table 4 shows that the indirect paths via Acting out and Omnipotence were significant. Conversely, the single mediations of Passive Aggression, Denial, Conversion, and Withdrawal were not significant. Notably, the coefficient of direct effect was greater than that of indirect effects, indicating a partial mediation.
Table 4.
Indirect effects of adolescents’ alexithymia on motor vehicle collisions through defense.
| Indirect Effect | Effect(BootSE) | LLCI | ULCI |
|---|---|---|---|
| Alexithymia→Acting out→MVCs | 0.29(0.05) | 0.16 | 0.46 |
| Alexithymia→Omnipotence→MVCs | 0.34(0.08) | 0.19 | 0.52 |
| Alexithymia→Passive Aggression→MVCs | −0.01(0.05) | −0.12 | 0.09 |
| Alexithymia→Denial→MVCs | 0.02(0.01) | −0.01 | 0.06 |
| Alexithymia→Conversion→MVCs | 0.03(0.04) | −0.04 | 0.12 |
| Alexithymia→ Withdrawal→MVCs | −0.01(0.06) | −0.15 | 0.09 |
MVCs = Motor Vehicle Collisions; BootSE = Boot-strapped standard error; LLCI = Lower level confidence interval; ULCI = Upper level confidence interval; all bold values are statistically significant.
4. Discussion
The present study aimed to explore the complex relationship between adolescent’s MVCs, alexithymia, and the defense strategies use. We chose to explore the possible role played by adolescent psychological and emotional functioning because international literature has extensively highlighted that difficulties in recognizing and defining emotions and the significant use of immature defense strategies represent key risk factors in risk-taking behaviors among adolescence [75,94]. The same associations have also been found for adolescents who recurrently visited emergency departments due MVCs [63,64,85], but to our best knowledge, no study has considered the possible mediation role played by defense strategies use in the relationship between adolescents’ alexithymic traits and MVCs.
4.1. Main Findings
The first aim of this study was to verify sex-related differences in adolescents’ frequency of MVCs. Previous studies have reported conflicting results, with some studies finding a higher prevalence among adolescent males [4,14,15,16], but research reports few and inconsistent results concerning females and road accidents [95]. However, our study is in line with recent studies by Breen and colleagues [4] and by Le and colleagues [5], which evidence a greater risk of recurrent MVCs for adolescent males than females. Specifically, our findings showed that female sex is associated with the absence of MVCs, whereas there were significant associations between male sex and adolescent groups with a major number of MVCs (i.e., Groups 3 and 4). This could be due to the fact that adolescent males are more impulsive and tend to perceive behavior as less risky than females [96,97], with an overall greater tendency towards risk-taking [98,99,100]. In contrast, females tend to be more sensitive to the uncertainty and punishment potentially associated with risky behavior [101,102] and show a general aversion to risk compared with males [103]. Interestingly, a recent study by Cordellieri and colleagues [95] found the same level of risk perception during driving for males and females but significant sex differences in the level of concern about the risk of road accidents, with males being less concerned about risks and dangers. As suggested by some authors, this could be due the fact that adolescent males tend to overestimate their risky competence [104,105] and feel more invulnerable to driving risks compared with their female peers [106,107].
Then, we verified the possible differences in alexithymia and defense use between the four study groups. As expected, we found that adolescents’ maladaptive functioning, in terms of alexithymia and defense strategies used, was associated with a higher recurrence of MVCs. Specifically, adolescents with higher rates of MVCs reported greater difficulties in the ability to identify feelings and higher externally oriented thinking compared with adolescents of all other groups. Moreover, they exceeded the clinical range cut-off in the Total score of TAS-20. At the same time, they reported the highest use of immature defense strategies, including Acting Out, Omnipotence, Passive Aggression, Denial, Conversion, and Withdrawal. Our results are in accordance with previous studies that evidenced significant associations between adolescents’ tendencies to incur multiple MVCs, difficulties in identifying their feelings and emotions [64], and significant use of maladaptive defense strategies [63,108], suggesting that the accident could be placed in the area of non-integration between the adolescent’s affective life and cognitive abilities [67]. The relationship between alexithymia, immature defense strategies use, and unhealthy conduct has been widely investigated in the adolescent literature. In fact, adolescents with limited access to their emotions due to difficulties in identifying and coping with emotions are at higher risk of involvement in a wide range of negative risky behaviors, including substance use and abuse [109] and behavioral addiction [110,111]. In this field, clinicians and researchers from a psychodynamic perspective have considered risky behaviors (including nonfatal injuries) as an adolescent’s real attempt to cope with psychological discomfort [67,112]. Our findings provide further support to this evidence, suggesting that the recurrence of accidents may be considered a result of adolescents’ difficulties in managing their emotions and psychological sufferance [113,114,115]. At the same time, as suggested by Carbone [112], subsequent recurrent ED visits due to MVCs may be interpreted as an unconscious attempt to receive both psychical and psychological help from health operators.
4.2. The Mediation Role of Defense Strategies Use on the Relationship between Alexithymia and MVCs
Finally, our last aim was to verify whether the relationship between adolescents’ alexithymia and the frequency of MVCs could be mediated by maladaptive defense strategies use. Indeed, recent studies have evidenced that defense use mediated the effect of alexithymia and negative outcomes (such as psychological distress and psychopathological problems) [76,79], but this is the first study to explore this relationship in adolescents’ MVCs. Our results showed that both total and direct effects of alexithymia on MVCs were significant. Moreover, adolescents’ alexithymia significantly predicted all considered defense strategies use (i.e., Acting Out, Omnipotence, Passive Aggression, Denial, Conversion, and Withdrawal), in accordance with the study by Chung and colleagues [80] that found a predictive effect of alexithymia on maladaptive defense use. Moreover, adolescents’ use of Acting Out and Omnipotence significantly predicted MVCs. The same defense strategies partially mediated the relationship between alexithymia and MVCs. These findings supported the evidence that adolescents’ alexithymic traits represent an important risk factor for the recurrence of MVCs [64]. This influence seems to be exerted both directly and through the effects of adolescent massive use of Acting Out and Omnipotence. In this context, some authors posited that alexithymia may be considered as an individual primitive mental defense resulting as a strategy to reduce emotional involvement in a distressing situation [116,117]. A high presence of alexithymic traits has also been shown to further increase the use of other immature strategies [80,118], which transform individual emotional experiences [119]. Moreover, the incidence of high-risk behaviors during adolescence has been found to be associated with both alexithymia [120,121] and immature defense strategies use [83,122], which are in turn associated with each other [123]. Our study further supported this evidence, showing a specific role played by Acting Out and Omnipotence. In this field, according to Manciaux [124], self-punitive action is not deliberate in road accidents, but it would be considered as a distinct form of the dynamics of Acting Out: a dramatization in the external world of internal conflicts where psychic pain is replaced by a concrete and recognizable physical pain [109,110,111]. Other authors [125,126] have also highlighted the link between the incident and the need to increase the feeling of omnipotence; thus, in many cases, the recurrence of MVCs would express the adolescent’s attempt to deny their mortality and feel a sense of their invulnerability [66]. This dynamic has been suggested to be at the basis of a particular type of risk-taking behavior, defined by Marcelli [126] as ‘hordalic’, in which the escaped danger and the adrenalin rush would reinforce the feeling of omnipotence, even if fleetingly. However, the state of euphoria produced is only ephemeral and, like a drug, tends to induce addiction and trigger escalation towards increasingly extreme and risky behavior.
4.3. Limitations and Strengths
This study has some limitations. First, the cross-sectional nature of the design implies that the hypothesized causal links between alexithymia, defense strategies use, and MVCs must be treated with caution and should be verified by further longitudinal study. Moreover, the homogeneity of the sample limits the generalizability of the results to other races and geographical origins. Finally, we did not consider the possible role played by families and peer influence [127,128,129,130,131], which the literature has shown to play a key role in adolescents’ tendency to be involved in MVCs and other high-risk behaviors. Despite the above limitations, our study has several strengths. To our best knowledge, this is the first study to explore the possible interplay between adolescents’ MVCs, alexithymic traits, and immature defense strategies use. Our findings evidenced a key role played by alexithymia, which exerted its risk influence on adolescents’ MVCs both directly and indirectly via Acting Out and Omnipotence use, which may be informative for the planning of more targeted and effective intervention treatments.
4.4. Implications for Practice and Clinic Applications
Overall, our findings supported the importance of an early assessment of adolescents’ alexithymia and defense strategies use to prevent adolescents’ risk of MVCs. Generally, preventive programs on adolescents’ risk of MVCs are usually conducted in schools with the primary aim of incrementing teens’ copying skills related to safe driving. However, our results suggested that the planning of intervention strategies focused on the promotion of the ability to recognize and discriminate one’s own and others’ emotions is needed and may be more effective. Moreover, this study further supports the emerging evidence that adolescents who recurrently visited ED due to MVCs are seeking psychological help for their emotional difficulties. This could suggest the importance of an early assessment and the planning of secondary prevention programs directly in the ED, where adolescents could be psychologically supported in the identification of their psychological sufferance related to the MVC, to reduce recidivism, with important clinical, health and economic implications.
5. Conclusions
The recent literature in the field of adolescents’ risk taking has underlined that alexithymic traits and the significant use of maladaptive defense strategies represent crucial risk factors for the incidence of adolescents’ MVCs. Previous studies on the complex relationship between these two variables have reported mixed results. To date, no study has yet explored this relationship among adolescents who recurrently access an ED due to MVCs, suggesting the importance of implementing knowledge of these mechanisms to make the planning of preventive programs more targeted. This study has shown that adolescents’ alexithymia represents a key risk factor for MVCs, which leads to a higher risk of a MVC both directly that indirectly through adolescents’ Acting Out and Omnipotence use. Overall, these findings further supported the emerging evidence considering immature defense strategies use as a mechanism through which alexithymia affects the incidence of high-risk behaviors among adolescents, including MVCs, with important clinical implications.
Author Contributions
Conceptualization, S.C., L.C., P.C. and E.C.; methodology, E.M.; data curation, M.E.; writing—original draft preparation, E.M., M.E.; writing—review and editing, S.C., L.C.; supervision, P.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethical Committee of the Psychology Faculty at Sapienza, University of Rome (protocol code: 4/2015_2).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are openly available in FigShare at doi:10.6084/m9.figshare.14402444.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Beck N.I., Arif I., Paumier M.F., Jacobsen K.H. Adolescent injuries in Argentina, Bolivia, Chile, and Uruguay: Results from the 2012–2013 Global School-based Student Health Survey (GSHS) Injury. 2016;47:2642–2649. doi: 10.1016/j.injury.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Gorios C., Souza R.M.D., Gerolla V., Maso B., Rodrigues C.L., Armond J.D.E. Transport accidents among children and adolescents at the emergency service of a teaching hospital in the southern zone of the city of São Paulo. Rev. Bras. Ortop. 2014;49:391–395. doi: 10.1016/j.rbo.2013.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kwan K., Wiebe D., Cerdá M., Goldman-Mellor S. Repeat assault injury among adolescents utilizing emergency care: A statewide longitudinal study. J. Emerg. Med. 2019;57:254–262. doi: 10.1016/j.jemermed.2019.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Breen J.M., Naess P.A., Gjerde H., Gaarder C., Stray-Pedersen A. The significance of preexisting medical conditions, alcohol/drug use and suicidal behavior for drivers in fatal motor vehicle crashes: A retrospective autopsy study. Forensic Sci. Med. Pathol. 2018;14:4–17. doi: 10.1007/s12024-017-9934-x. [DOI] [PubMed] [Google Scholar]
- 5.Le T.M.T., Oleck N.C., Liu F.C., Halsey J.N., Hoppe I.C., Lee E.S., Granick M.S. Motor vehicle collision injuries: An analysis of facial fractures in the urban pediatric population. J. Craniofac. Surg. 2020;31:1910–1913. doi: 10.1097/SCS.0000000000006671. [DOI] [PubMed] [Google Scholar]
- 6.Rothman L., Macarthur C., Wilton A., Howard A.W., Macpherson A.K. Recent trends in child and youth emergency department visits because of pedestrian motor vehicle collisions by socioeconomic status in Ontario, Canada. Inj. Prev. 2019;25:570–573. doi: 10.1136/injuryprev-2018-043090. [DOI] [PubMed] [Google Scholar]
- 7.McGarvey C., Hamilton K., Donnelly J., Nicholson A.J. Trends in road transport collision deaths in the Irish paediatric population: A retrospective review of mortality data, 1991–2015. BMJ Paediatr. Open. 2019;3:e000361. doi: 10.1136/bmjpo-2018-000361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peden M., Kayede O., Ozanne-Smith J., Hyder A.A. World Report on Child Injury Prevention: World Health Organization. [(accessed on 2 March 2021)];2008 :79–93. Available online: http://www.who.int/violence_injury_prevention/child/injury/world_report/en/ [PubMed]
- 9.Roberts Z., Collins J.A., James D., Bouamra O., Young M., Lyttle M.D., Roland D., Mullen S., PERUKI Epidemiology of adolescent trauma in England: A review of TARN data 2008–2017. Emerg. Med. J. 2020;37:25–30. doi: 10.1136/emermed-2018-208329. [DOI] [PubMed] [Google Scholar]
- 10.Wu X., Kaminga A.C., Dai W., Deng J., Wang Z., Pan X., Liu A. The prevalence of moderate-to-high posttraumatic growth: A systematic review and meta-analysis. J. Affect disord. 2019;243:408–415. doi: 10.1016/j.jad.2018.09.023. [DOI] [PubMed] [Google Scholar]
- 11.Moreira M.R., Ribeiro J.M., Motta C.T., Motta J.I.J. Mortality by road traffic accidents in adolescents and young people, Brazil, 1996–2015: Will we achieve SDG 3.6? Cien. Saude Colet. 2018;23:2785–2796. doi: 10.1590/1413-81232018239.17082018. [DOI] [PubMed] [Google Scholar]
- 12.Wang H., Zhou Y., Liu J., Ou L., Zhao Y., Han J., Xiang L. Traumatic fractures as a result of motor vehicle collisions in children and adolescents. Int. Orthop. 2018;42:625–630. doi: 10.1007/s00264-018-3777-2. [DOI] [PubMed] [Google Scholar]
- 13.Breen J.M., Næss P.A., Hansen T.B., Gaarder C., Stray-Pedersen A. Serious motor vehicle collisions involving young drivers on Norwegian roads 2013–2016: Speeding and driver-related errors are the main challenge. Traffic Inj. Prev. 2020;21:382–388. doi: 10.1080/15389588.2020.1770237. [DOI] [PubMed] [Google Scholar]
- 14.Kar I.N., Guillaume C., Sita K.R., Gershon P., Simons-Morton B.G. US adolescent street racing and other risky driving behaviors. J. Adolesc. Health. 2018;62:626–629. doi: 10.1016/j.jadohealth.2018.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shults R.A., Bergen G., Smith T.J., Cook L., Kindelberger J., West B. Characteristics of single vehicle crashes with a teen driver in South Carolina, 2005–2008. Accid. Anal. Prev. 2019;122:325–331. doi: 10.1016/j.aap.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang H., Wu M., Cheng X., Schwebel D.C. The road user behaviors of Chinese adolescents: Data from China and a comparison with adolescents in other countries. Ann. Glob. Health. 2019;85:76. doi: 10.5334/aogh.2452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO U., Mathers C. Global strategy for women’s, children’s and adolescents’ health (2016–2030) Organization. 2016;201:4–103. [Google Scholar]
- 18.Roberts S.E., Vingilis E., Wilk P., Seeley J. A comparison of self-reported motor vehicle collision injuries compared with official collision data: An analysis of age and sex trends using the Canadian National Population Health Survey and Transport Canada data. Accid. Anal. Prev. 2008;40:559–566. doi: 10.1016/j.aap.2007.08.017. [DOI] [PubMed] [Google Scholar]
- 19.Kahane C.J. Injury Vulnerability and Effectiveness of Occupant Protection Technologies for Older Occupants and Women (No. DOT HS 811 766) [(accessed on 3 March 2021)];2013 Available online: https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/811766.
- 20.Raphael D. Adolescence as a gateway to adult health outcomes. Maturitas. 2013;752:137–141. doi: 10.1016/j.maturitas.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 21.Sawyer S.M., Afifi R.A., Bearinger L.H., Blakemore S.J., Dick B., Ezeh A.C., Patton G.C. Adolescence: A foundation for future health. Lancet. 2012;379:1630–1640. doi: 10.1016/S0140-6736(12)60072-5. [DOI] [PubMed] [Google Scholar]
- 22.Crone E.A., Dahl R.E. Understanding adolescence as a period of social–affective engagement and goal flexibility. Nat. Rev. Neurosci. 2012;13:636–650. doi: 10.1038/nrn3313. [DOI] [PubMed] [Google Scholar]
- 23.Patton G.C., Sawyer S.M., Santelli J.S., Ross D.A., Afifi R., Allen N.B., Arora M., Azzopardi P., Baldwin W., Bonell C., et al. Our future: A Lancet commission on adolescent health and wellbeing. Lancet. 2016;387:2423–2478. doi: 10.1016/S0140-6736(16)00579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Duijvenvoorde A.C., Peters S., Braams B.R., Crone E.A. What motivates adolescents? Neural responses to rewards and their influence on adolescents’ risk taking, learning, and cognitive control. Neurosci. Biobehav. Rev. 2016;70:135–147. doi: 10.1016/j.neubiorev.2016.06.037. [DOI] [PubMed] [Google Scholar]
- 25.Lampropoulou A. The role of the family in adolescents’ subjective well-being. Psychiatriki. 2018;29:172–182. doi: 10.22365/jpsych.2018.292.172. [DOI] [PubMed] [Google Scholar]
- 26.Roach A. Supportive peer relationships and mental health in adolescence: An integrative review. Issues Ment. Health Nurs. 2018;39:723–737. doi: 10.1080/01612840.2018.1496498. [DOI] [PubMed] [Google Scholar]
- 27.Casey B.J., Jones R.M., Hare T.A. The adolescent brain. Ann. N. Y. Acad. Sci. 2008;1124:111–126. doi: 10.1196/annals.1440.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Petanjek Z., Kostović I. Epigenetic regulation of fetal brain development and neurocognitive outcome. Proc. Natl. Acad. Sci. USA. 2012;109:11062–11063. doi: 10.1073/pnas.1208085109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vijayakumar N., Op de Macks Z., Shirtcliff E.A., Pfeifer J.H. Puberty and the human brain: Insights into adolescent development. Neurosci Biobehav Rev. 2018;92:417–436. doi: 10.1016/j.neubiorev.2018.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Blakemore S.J., Robbins T.W. Decision-making in the adolescent brain. Nat. Neurosci. 2012;15:1184–1191. doi: 10.1038/nn.3177. [DOI] [PubMed] [Google Scholar]
- 31.Bludau A., Royer M., Meister G., Neumann I.D., Menon R. Regulation of the Social Brain. Trends Neurosci. 2019;42:471–484. doi: 10.1016/j.tins.2019.04.001. [DOI] [PubMed] [Google Scholar]
- 32.Casey B.J., Heller A.S., Gee D.G., Cohen A.O. Development of the emotional brain. Neurosci Lett. 2019;693:29–34. doi: 10.1016/j.neulet.2017.11.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bos M., Wierenga L.M., Blankenstein N.E., Schreuders E., Tamnes C.K., Crone E.A. Longitudinal structural brain development and externalizing behavior in adolescence. J. Child. Psychol. Psychiatry. 2018;59:1061–1072. doi: 10.1111/jcpp.12972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dow-Edwards D., MacMaster F.P., Peterson B.S., Niesink R., Andersen S., Braams B.R. Experience during adolescence shapes brain development: From synapses and networks to normal and pathological behavior. Neurotoxicol. Teratol. 2019;76:106834. doi: 10.1016/j.ntt.2019.106834. [DOI] [PubMed] [Google Scholar]
- 35.van Hoorn J., McCormick E.M., Telzer E.H. Moderate social sensitivity in a risky context supports adaptive decision making in adolescence: Evidence from brain and behavior. Soc. Cogn. Affect. Neurosci. 2018;13:546–556. doi: 10.1093/scan/nsy016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chong S.L., Tyebally A., Chew S.Y., Lim Y.C., Feng X.Y., Chin S.T., Lee L.K. Road traffic injuries among children and adolescents in Singapore—Who is at greatest risk? Accid. Anal. Prev. 2017;100:59–64. doi: 10.1016/j.aap.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 37.Mokdad A.H., Forouzanfar M.H., Daoud F., Mokdad A.A., El Bcheraoui C., Moradi-Lakeh M., Kyu H.H., Barber R.M., Wagner J., Cercy K., et al. Global burden of diseases, injuries, and risk factors for young people’s health during 1990-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387:2383–2401. doi: 10.1016/S0140-6736(16)00648-6. [DOI] [PubMed] [Google Scholar]
- 38.Ramisetty-Mikler S., Almakadma A. Attitudes and behaviors towards risky driving among adolescents in Saudi Arabia. Int. J. Pediatr. Adolesc. Med. 2016;3:55–63. doi: 10.1016/j.ijpam.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Varnaccia G., Saß A.C., Rommel A. Unintentional injuries among children and adolescents in Germany. Data sources and results] Bundesgesundheitsblatt Gesundh. Gesundh. 2014;57:613–620. doi: 10.1007/s00103-014-1962-z. [DOI] [PubMed] [Google Scholar]
- 40.Braitman K.A., Kirley B.B., McCartt A.T., Chaudhary N.K. Crashes of novice teenage drivers: Characteristics and contributing factors. J. Saf. Res. 2008;39:47–54. doi: 10.1016/j.jsr.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 41.Curry A.E., Hafetz J., Kallan M.J., Winston F.K., Durbin D.R. Prevalence of teen driver errors leading to serious motor vehicle crashes. Accid. Anal. Prev. 2011;43:1285–1290. doi: 10.1016/j.aap.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 42.Bingham C.R., Shope J.T. Adolescent developmental antecedents of risky driving among young adults. J. Stud. Alcohol. 2004;65:84–94. doi: 10.15288/jsa.2004.65.84. [DOI] [PubMed] [Google Scholar]
- 43.Behnood A., Mannering F.L. The effects of drug and alcohol consumption on driver injury severities in single-vehicle crashes. Traffic Inj. Prev. 2017;18:456–462. doi: 10.1080/15389588.2016.1262540. [DOI] [PubMed] [Google Scholar]
- 44.Hingson R., Zha W., Simons-Morton B., White A. Alcohol-Induced Blackouts as Predictors of Other Drinking Related Harms Among Emerging Young Adults. Alcohol. Clin. Exp. Res. 2016;40:776–784. doi: 10.1111/acer.13010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Awaluddin S.M., Ahmad F.H., Jeevananthan C., Ganapathy S.S., Sooryanarayana R., Mohamad Anuar M.F., Alias N., Saminathan T.A., Mohd Yusoff M.F., Rosman A. Prevalence of Nonfatal Serious Injury Due to Motor Vehicle Accidents Among Malaysian School-Going Adolescents: Findings from the Adolescent Health Survey 2017. Asia Pac. J. Public Health. 2019;31:65S–72S. doi: 10.1177/1010539519872662. [DOI] [PubMed] [Google Scholar]
- 46.Mirman J.H. Agency, Adolescence, and Motor Vehicle Crash Risk. J. Adolesc. Health. 2018;62:509–510. doi: 10.1016/j.jadohealth.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 47.Banz B.C., Fell J.C., Vaca F.E. Complexities of Young Driver Injury and Fatal Motor Vehicle Crashes. Yale J. Biol. Med. 2019;92:725–731. [PMC free article] [PubMed] [Google Scholar]
- 48.Hayashi Y., Rivera E.A., Modico J.G., Foreman A.M., Wirth O. Texting while driving, executive function, and impulsivity in college students. Accid. Anal. Prev. 2017;102:72–80. doi: 10.1016/j.aap.2017.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.MacArthur G., Caldwell D.M., Redmore J., Watkins S.H., Kipping R., White J., Chittleborough C., Langford R., Er V., Lingam R., et al. Individual-, family-, and school-level interventions targeting multiple risk behaviours in young people. Cochrane Database Syst. Rev. 2018;2012:10. doi: 10.1002/14651858.CD009927.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ehsani J.P., Gershon P., Grant B., Zhu C., Klauer S.G., Dingus T.A., Simons-Morton B.G. Learner Driver Experience and Teenagers’ Crash Risk During the First Year of Independent Driving. JAMA Pediatr. 2020;174:573–580. doi: 10.1001/jamapediatrics.2020.0208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Marengo D., Settanni M., Vidotto G. Drivers’ subtypes in a sample of Italian adolescents: Relationship between personality measures and driving behaviors. Transp. Res. Part F Traffic Psychol. Behav. 2012;15:480–490. doi: 10.1016/j.trf.2012.04.001. [DOI] [Google Scholar]
- 52.Zhu D., Sze N.N., Bai L. Roles of personal and environmental factors in the red light running propensity of pedestrian: Case study at the urban crosswalks. Transp. Res. Part F Traffic Psychol. Behav. 2021;76:47–58. doi: 10.1016/j.trf.2020.11.001. [DOI] [Google Scholar]
- 53.Zhu D., Sze N.N. Propensities of red light running of pedestrians at the two-stage crossings with split pedestrian signal phases. Accid. Anal. Prev. 2021;151:105958. doi: 10.1016/j.aap.2020.105958. [DOI] [PubMed] [Google Scholar]
- 54.Cavalcanti A.L., Lino T.H., de Oliveira T.B., de Oliveira T.S., Cardoso A.M., de Macedo R.F., Padilha W.W., Xavier A.F. Head and maxillofacial injuries in child and adolescent victims of automotive accidents. Sci. World J. 2014:632720. doi: 10.1155/2014/632720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Papadatou D., Bellali T., Tselepi K., Giannopoulou I. Adolescents’ trajectory through peer loss after a road traffic accident. Death Stud. 2018;42:383–391. doi: 10.1080/07481187.2017.1355341. [DOI] [PubMed] [Google Scholar]
- 56.Horvath C., Lewis I., Watson B. The beliefs which motivate young male and female drivers to speed: A comparison of low and high intenders. Accid. Anal. Prev. 2012;45:334–341. doi: 10.1016/j.aap.2011.07.023. [DOI] [PubMed] [Google Scholar]
- 57.McDonald C.C., Sommers M.S., Fargo J.D. Risky driving, mental health, and health-compromising behaviours: Risk clustering in late adolescents and adults. Inj. Prev. 2014;20:365–372. doi: 10.1136/injuryprev-2014-041150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Steinberger F., Moeller A., Schroeter R. The antecedents, experience, and coping strategies of driver boredom in young adult males. J. Saf. Res. 2016;59:69–82. doi: 10.1016/j.jsr.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 59.Kumar S., Mahima, Srivastava D.K., Kharya P., Sachan N., Kiran K. Analysis of risk factors contributing to road traffic accidents in a tertiary care hospital. A hospital based cross-sectional study. Chin. J. Traumatol. 2020;23:159–162. doi: 10.1016/j.cjtee.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cicchetti D.A.N.T.E., Beauchaine T.P., Hinshaw S.P. A multiple-levels-of-analysis perspective on research in development and psychopathology. Child. Adolesc. Psychol. 2008;1:27–57. [Google Scholar]
- 61.Sroufe L.A., Rutter M. The domain of developmental psychopathology. Child. Dev. 1984;55:17–29. doi: 10.2307/1129832. [DOI] [PubMed] [Google Scholar]
- 62.Cerniglia L., Cimino S., Ballarotto G., Casini E., Ferrari A., Carbone P., Cersosimo M. Motor vehicle accidents and adolescents: An empirical study on their emotional and behavioral profiles, defense strategies and parental support. Transp. Res. Part. F Traffic Psychol. Behav. 2015;35:28–36. doi: 10.1016/j.trf.2015.09.002. [DOI] [Google Scholar]
- 63.Cimino S., Simonelli A., Parolin M., Ballarotto G., Carbone P., Cerniglia L. Theoretical and Empirical Linkage between Road Accidents and Binge Eating Behaviors in Adolescence. Int. J. Environ. Res. Public Health. 2018;15:355. doi: 10.3390/ijerph15020355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.M’bailara K., Atzeni T., Contrand B., Derguy C., Bouvard M.P., Lagarde E., Galéra C. Emotional reactivity: Beware its involvement in traffic accidents. Psychiatry Res. 2018;262:290–294. doi: 10.1016/j.psychres.2017.12.019. [DOI] [PubMed] [Google Scholar]
- 65.Carbone P. Le Ali di Lcaro; Capire e Prevenire Gli Incidenti dei Giovani. Bollati Boringhieri; Torino, Italy: 2009. [Google Scholar]
- 66.Carbone P., Casini E., Ferrari A. Pronto Soccorso. In: Carbone P., Cimino S., editors. Adolescenze Itinerari Psicoanalitici. Edizione Magi; Roma, Italy: 2017. [Google Scholar]
- 67.Scott-Parker B., Watson B., King M.J., Hyde M.K. The psychological distress of the young driver: A brief report. Inj. Prev. 2011;17:275–277. doi: 10.1136/ip.2010.031328. [DOI] [PubMed] [Google Scholar]
- 68.Aduen P.A., Day T.N., Kofler M.J., Harmon S.L., Wells E.L., Sarver D.E. Social Problems in ADHD: Is it a Skills Acquisition or Performance Problem? J. Psychopathol. Behav. Assess. 2018;40:440–451. doi: 10.1007/s10862-018-9649-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Aduen P.A., Kofler M.J., Cox D.J., Sarver D.E., Lunsford E. Motor vehicle driving in high incidence psychiatric disability: Comparison of drivers with ADHD, depression, and no known psychopathology. J. Psychiatr. Res. 2015;64:59–66. doi: 10.1016/j.jpsychires.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 70.Räisänen T., Hakko H., Riipinen P., Räty E., Kantojärvi L. Personality disorders of drivers killed in fatal motor vehicle accidents in Finland during 1990-2011. Acta Psychiatr. Scand. 2019;140:39–49. doi: 10.1111/acps.13039. [DOI] [PubMed] [Google Scholar]
- 71.Wachs S., Vazsonyi A.T., Wright M.F., Ksinan Jiskrova G. Cross-National Associations Among Cyberbullying Victimization, Self-Esteem, and Internet Addiction: Direct and Indirect Effects of Alexithymia. Front. Psychol. 2020;11:1368. doi: 10.3389/fpsyg.2020.01368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cerniglia L., Guicciardi M., Sinatra M., Monacis L., Simonelli A., Cimino S. The Use of Digital Technologies, Impulsivity and Psychopathological Symptoms in Adolescence. Behav. Sci. 2019;9:82. doi: 10.3390/bs9080082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Parolin M., Miscioscia M., De Carli P., Cristofalo P., Gatta M., Simonelli A. Alexithymia in Young Adults With Substance Use Disorders: Critical Issues About Specificity and Treatment Predictivity. Front. Psychol. 2018;9:645. doi: 10.3389/fpsyg.2018.00645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gonzales N.A., Liu Y., Jensen M., Tein J.Y., White R., Deardorff J. Externalizing and internalizing pathways to Mexican American adolescents’ risk taking. Dev. Psychopathol. 2017;29:1371–1390. doi: 10.1017/S0954579417000323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fang S., Chung M.C., Wang Y. The impact of past trauma on psychological distress: The roles of defense mechanisms and alexithymia. Front. Psychol. 2020;11:992. doi: 10.3389/fpsyg.2020.00992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ziadni M.S., Jasinski M.J., Labouvie-Vief G., Lumley M.A. Alexithymia, Defenses, and Ego Strength: Cross-sectional and Longitudinal Relationships with Psychological Well-Being and Depression. J. Happiness Stud. 2017;18:1799–1813. doi: 10.1007/s10902-016-9800-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Helmes E., McNeill P.D., Holden R.R., Jackson C. The construct of alexithymia: Associations with defense mechanisms. J. Clin. Psychol. 2008;64:318–331. doi: 10.1002/jclp.20461. [DOI] [PubMed] [Google Scholar]
- 78.Lenzo V., Barberis N., Cannavò M., Filastro A., Verrastro V., Quattropani M.C. The relationship between alexithymia, defense strategies, eating disorders, anxiety and depression. Riv. Psichiatr. 2020;55:24–30. doi: 10.1708/3301.32715. [DOI] [PubMed] [Google Scholar]
- 79.Chung M.C., Di X., Wan K.H. Exploring the interrelationship between alexithymia, defense style, emotional suppression, homicide-related posttraumatic stress disorder and psychiatric co-morbidity. Psychiatry Res. 2016;243:373–381. doi: 10.1016/j.psychres.2016.05.057. [DOI] [PubMed] [Google Scholar]
- 80.Khademi M., Hajiahmadi M., Faramarzi M. The role of long-term psychodynamic psychotherapy in improving attachment patterns, defense styles, and alexithymia in patients with depressive/anxiety disorders. Trends Psychiatry Psychother. 2019;41:43–50. doi: 10.1590/2237-6089-2017-0144. [DOI] [PubMed] [Google Scholar]
- 81.Besharat M.A., Shahidi S. What is the relationship between alexithymia and ego defense styles? A correlational study with Iranian students. Asian J. Psychiatr. 2011;4:145–149. doi: 10.1016/j.ajp.2011.05.011. [DOI] [PubMed] [Google Scholar]
- 82.Nikmanesh Z., Darvish Molla M., Mehranfard M. The Mediating Role of Alexithymia in the Relationship Between Defense Mechanisms and Tendency to High-risk Behaviors Among Adolescents. J. Res. Health. 2021;11:29–36. doi: 10.32598/JRH.11.1.363.6. [DOI] [Google Scholar]
- 83.Desapriya E.B., Iwase N., Shimizu S. Adolescents alcohol related traffic accidents and mortality in 1999–2000—Problem and solutions. Nihon Arukoru Yakubutsu Igakkai Zasshi. 2002;37:168–178. [PubMed] [Google Scholar]
- 84.Marzilli E., Ballarotto G., Cimino S., Cerniglia L. Motor vehicle collisions in adolescence: The role of family support. [Incidenti stradali in adolescenza: Il ruolo del supporto genitoriale] Rass. Psicol. 2018;34:17–28. [Google Scholar]
- 85.Lund J., Aarø L.E. Accident prevention. Presentation of a model placing emphasis on human, structural and cultural factors. Saf. Sci. 2004;42:271–324. doi: 10.1016/S0925-7535(03)00045-6. [DOI] [Google Scholar]
- 86.Hole G. Motor Vehicle Collisions. Academic Press; Cambridge, MA, USA: 2008. Predictors of motor vehicle collisions; pp. 13–43. [Google Scholar]
- 87.Marcelli D., Ingrand P., Ingrand I., Delamour M. Scale for the Evaluation of Circumstances Surrounding an Accident and the Risk of Recurrence (ECARR): A Prospective Validation Study of Accident Repetition. Psychiatr. Enfant. 2011;54:253–299. doi: 10.3917/psye.541.0253. [DOI] [Google Scholar]
- 88.Bagby R.M., Parker J.D., Taylor G.J. The twenty-item Toronto Alexithymia Scale--I. Item selection and cross-validation of the factor structure. J. Psychosom. Res. 1994;38:23–32. doi: 10.1016/0022-3999(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 89.La Ferlita V., Bonadies M., Solano L., De Gennaro L., Gonini P. Alessitimia e adolescenza: Studio preliminare di validazione della TAS-20 su un campione di 360 adolescenti italiani. Infanz. E Adolesc. 2007;6:131–144. [Google Scholar]
- 90.Steiner H., Araujo K.B., Koopman C. The response evaluation measure (REM-71): A new instrument for the measurement of defenses in adults and adolescents. Am. J. Psychiatry. 2001;158:467–473. doi: 10.1176/appi.ajp.158.3.467. [DOI] [PubMed] [Google Scholar]
- 91.Prunas A., Madeddu F., Pozzoli S., Gatti C., Shaw R.J., Steiner H. The Italian version of the response evaluation measure-71. Compr. Psychiatry. 2009;50:369–377. doi: 10.1016/j.comppsych.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 92.Hayes A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Publications; London, UK: 2017. [Google Scholar]
- 93.Lee C.W., Lee J., Jun J.Y., Lee S.H., Yu S.Y., Park J., Kim S.J. Associations between defense mechanisms and life satisfaction among North Korean refugees. Ann. Gen. Psychiatry. 2021;20:18. doi: 10.1186/s12991-021-00339-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cordellieri P., Baralla F., Ferlazzo F., Sgalla R., Piccardi L., Giannini A.M. Gender effects in young road users on road safety attitudes, behaviors and risk perception. Front. Psychol. 2016;7:1412. doi: 10.3389/fpsyg.2016.01412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gardner M., Steinberg L. Peer influence on risk taking, risk preference, and risky decision making in adolescence and adulthood: An experimental study. Dev. Psychol. 2005;41:625–635. doi: 10.1037/0012-1649.41.4.625. [DOI] [PubMed] [Google Scholar]
- 96.Reniers R.L., Murphy L., Lin A., Bartolomé S.P., Wood S.J. Risk Perception and Risk-Taking Behaviour during Adolescence: The Influence of Personality and Gender. PLoS ONE. 2016;11:e0153842. doi: 10.1371/journal.pone.0153842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kim Y., Park I., Kang S. Age and gender differences in health risk perception. Cent. Eur. J. Public Health. 2018;26:54–59. doi: 10.21101/cejph.a4920. [DOI] [PubMed] [Google Scholar]
- 98.Walshe E.A., Ward McIntosh C., Romer D., Winston F.K. Executive Function Capacities, Negative Driving Behavior and Crashes in Young Drivers. Int. J. Environ. Res. Public Health. 2017;14:1314. doi: 10.3390/ijerph14111314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Oviedo-Trespalacios O., Scott-Parker B. The sex disparity in risky driving: A survey of Colombian young drivers. Traffic Inj. Prev. 2018;19:9–17. doi: 10.1080/15389588.2017.1333606. [DOI] [PubMed] [Google Scholar]
- 100.Lee T.M., Chan C.C., Leung A.W., Fox P.T., Gao J.H. Sex-related differences in neural activity during risk taking: An fMRI study. Cereb. Cortex. 2009;19:1303–1312. doi: 10.1093/cercor/bhn172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.van den Bos R., Homberg J., de Visser L. A critical review of sex differences in decision-making tasks: Focus on the Iowa Gambling Task. Behav. Brain Res. 2013;238:95–108. doi: 10.1016/j.bbr.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 102.Van Leijenhorst L., Westenberg P.M., Crone E.A. A developmental study of risky decisions on the cake gambling task: Age and gender analyses of probability estimation and reward evaluation. Dev. Neuropsychol. 2008;33:179–196. doi: 10.1080/87565640701884287. [DOI] [PubMed] [Google Scholar]
- 103.Glendon A.I., Dorn L., Davies R., Matthews G., Taylor R.G. Age and gender differences in perceived accident likelihood and driver competences. Risk Anal. 1996;16:755–762. doi: 10.1111/j.1539-6924.1996.tb00826.x. [DOI] [PubMed] [Google Scholar]
- 104.Gonzales J., Field T., Yando R., Gonzales K. Adolescents’ perception of their risk-taking behavior. Adolescence. 1994;29:701–709. [PubMed] [Google Scholar]
- 105.Quadrel M.J., Fischhoff B., Davis W. Adolescent (in)vulnerability. Am. Psychol. 1993;48:102–116. doi: 10.1037/0003-066X.48.2.102. [DOI] [PubMed] [Google Scholar]
- 106.Harré N., Field J., Kirkwood B. Gender differences and areas of common concern in the driving behaviors and attitudes of adolescents. J. Saf. Res. 1996;27:163–173. doi: 10.1016/0022-4375(96)00013-8. [DOI] [Google Scholar]
- 107.Erriu M. Emotional–Behavioral Profiles and Parental Support in Adolescents with Motor Vehicle Accidents. Eur. Proc. Soc. Behav. Sci. EpSBS. 2016;13:303–312. [Google Scholar]
- 108.Craparo G., Ardino V., Gori A., Caretti V. The Relationships between Early Trauma, Dissociation, and Alexithymia in Alcohol Addiction. Psychiatry Investig. 2014;11:330–335. doi: 10.4306/pi.2014.11.3.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Gori A., Craparo G., Caretti V., Giannini M., Iraci-Sareri G., Bruschi A., Janiri L., Ponti L., Tani F. Impulsivity, alexithymia and dissociation among pathological gamblers in different therapeutic settings: A multisample comparison study. Psychiatry Res. 2016;246:789–795. doi: 10.1016/j.psychres.2016.10.046. [DOI] [PubMed] [Google Scholar]
- 110.Schimmenti A., Passanisi A., Caretti V., La Marca L., Granieri A., Iacolino C., Gervasi A.M., Maganuco N.R., Billieux J. Traumatic experiences, alexithymia, and Internet addiction symptoms among late adolescents: A moderated mediation analysis. Addict. Behav. 2017;64:314–320. doi: 10.1016/j.addbeh.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 111.Carbone P. L’Adolescente Prende Corpo. II Pensiero Scientifico Editore; Roma, Italy: 2010. [Google Scholar]
- 112.Berger S.S., Elliott C., Ranzenhofer L.M., Shomaker L.B., Hannallah L., Field S.E., Young J.F., Sbrocco T., Wilfley D.E., Yanovski J.A., et al. Interpersonal problem areas and alexithymia in adolescent girls with loss of control eating. Compr. Psychiatry. 2014;55:170–178. doi: 10.1016/j.comppsych.2013.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Raffagnato A., Angelico C., Valentini P., Miscioscia M., Gatta M. Using the Body When There Are No Words for Feelings: Alexithymia and Somatization in Self-Harming Adolescents. Front. Psychiatry. 2020;11:262. doi: 10.3389/fpsyt.2020.00262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Shank L.M., Tanofsky-Kraff M., Kelly N.R., Jaramillo M., Rubin S.G., Altman D.R., Byrne M.E., LeMay-Russell S., Schvey N.A., Broadney M.M., et al. The association between alexithymia and eating behavior in children and adolescents. Appetite. 2019;142:104381. doi: 10.1016/j.appet.2019.104381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Fukunishi I., Maeda K., Kubota M., Tomino Y. Association of alexithymia with low utilization and perception on a measure of social support in patients on peritoneal dialysis. Psychol. Rep. 1997;80:127–130. doi: 10.2466/pr0.1997.80.1.127. [DOI] [PubMed] [Google Scholar]
- 116.Thome A. Alexithymia and acquired immune deficiency syndrome. Psychother. Psychosom. 1990;54:40–43. doi: 10.1159/000288375. [DOI] [PubMed] [Google Scholar]
- 117.Boogar I., Moazedian A. Improvement of borderline personality disorder at different time frames of transference focused psychotherapy: A case report. J. Med. Sci. 2020;31:255–266. [Google Scholar]
- 118.Gross J.J. Emotion regulation. Handb. Emot. 2008;3:497–513. [Google Scholar]
- 119.Greene D., Boyes M., Hasking P. he associations between alexithymia and both non-suicidal self-injury and risky drinking: A systematic review and meta-analysis. J. Affect. Disord. 2020;260:140–166. doi: 10.1016/j.jad.2019.08.088. [DOI] [PubMed] [Google Scholar]
- 120.Lyvers M., Jamieson R., Thorberg F.A. Risky cannabis use is associated with alexithymia, frontal lobe dysfunction, and impulsivity in young adult cannabis users. J. Psychoact. Drugs. 2013;45:394–403. doi: 10.1080/02791072.2013.844525. [DOI] [PubMed] [Google Scholar]
- 121.Rachão I., Campos R.C. Personality styles and defense mechanisms in a community sample of adolescents: An exploratory study. Bull. Menn. Clin. 2015;79:14–40. doi: 10.1521/bumc.2015.79.1.14. [DOI] [PubMed] [Google Scholar]
- 122.Tozzi E., Andrisani G., Maiorani D., Pezzi L., Leopardi R., Fiorentini N., Sechi E. Alexithymia in headache sufferers: A psychosomatic symptom or comorbidity in adolescents? Educ. Res. 2013;4:289–293. [Google Scholar]
- 123.Manciaux M.R.G. Accidents in childhood: From epidemiology to prevention. Acta Paediatr. 1985;74:163–171. doi: 10.1111/j.1651-2227.1985.tb10944.x. [DOI] [PubMed] [Google Scholar]
- 124.Turz A. Adolescence et Risque. Syros; Paris, France: 1993. [Google Scholar]
- 125.Marcelli D. La position autistique: Hypotheses psychopathologiques et ontoge-nethiques [The autistic position: Psychopathological and ontogenetic hypothesis] Psychiatr. Enfant. 1983;24:5–55. [PubMed] [Google Scholar]
- 126.Cerniglia L., Cimino S., Marzilli E., Pascale E., Tambelli R. Associations Among Internet Addiction, Genetic Polymorphisms, Family Functioning, and Psychopathological Risk: Cross-Sectional Exploratory Study. JMIR Ment. Health. 2020;7:e17341. doi: 10.2196/17341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Van Hoorn J., McCormick E.M., Rogers C.R., Ivory S.L., Telzer E.H. Differential effects of parent and peer presence on neural correlates of risk taking in adolescence. Soc. Cogn. Affect. Neurosci. 2018;13:945–955. doi: 10.1093/scan/nsy071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Marzilli E., Cerniglia L., Ballarotto G., Cimino S. Internet Addiction among Young Adult University Students: The Complex Interplay between Family Functioning, Impulsivity, Depression, and Anxiety. Int. J. Environ. Res. Public Health. 2020;17:8231. doi: 10.3390/ijerph17218231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sherman L.E., Greenfield P.M., Hernandez L.M., Dapretto M. Peer Influence Via Instagram: Effects on Brain and Behavior in Adolescence and Young Adulthood. Child. Dev. 2018;89:37–47. doi: 10.1111/cdev.12838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Tafà M., Marzilli E., Cimino S., Cerniglia L., Bracaglia F. Anorexic families and bulimic families: Psychopathological risk and family functioning [Famiglie anoressiche e bulimiche: Rischio psicopatologico e funzionamento familiare] Rass. Psicol. 2017;34:5–23. [Google Scholar]
- 131.Weston L., Hellier E. Designing road safety interventions for young drivers–The power of peer influence. Transp. Res. Part F Traffic Psychol. Behav. 2018;55:262–271. doi: 10.1016/j.trf.2018.03.003. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are openly available in FigShare at doi:10.6084/m9.figshare.14402444.