Abstract
Dermatofibrosarcoma protuberans is a rare tumor that arises in the dermis, with a strong tendency to recur locally. It is slow growing and often presents as a skin-colored plaque on the trunk, although it may arise anywhere on the body. Dermatofibrosarcoma protuberans has a distinctive histologic appearance, and immunohistochemical studies can help make the diagnosis. This case report describes a young man who presented with complaints of an enlarging right scrotal mass and was diagnosed with dermatofibrosarcoma protuberans.
Keywords: Dermatofibrosarcoma protuberance, excision, neoplasia, scrotum, skin tumor
Dermatofibrosarcoma protuberans (DFSP) is an uncommon and locally aggressive cutaneous soft tissue sarcoma. Even though they rarely metastasize, these tumors tend to recur locally. DFSP manifests most commonly in middle-aged adults, between the ages of 25 and 45. Here, we present the case of a young man who presented with complaints of an enlarging right scrotal mass and was later diagnosed with the rare entity of DFSP.
CASE DESCRIPTION
A 24-year-old black man presented to the hospital for evaluation of a gradually enlarging right scrotal mass, which he first noticed 2 years earlier. The scrotal mass was painful to touch and was occasionally associated with some clear discharge. He denied any scrotal trauma, dysuria, gross hematuria, or family history of genitourinary cancer.
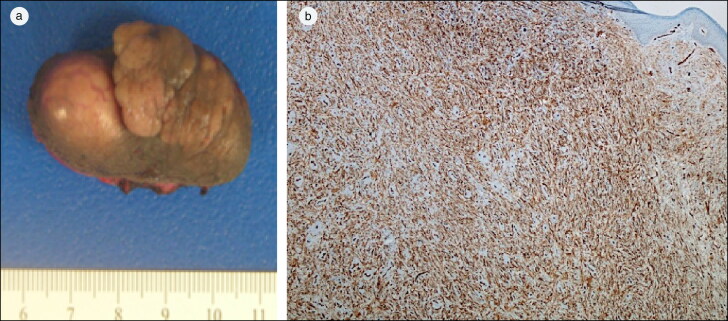
On exam, the right hemiscrotum had two adjacent growths (felt to be separate from the testes), with a total size of approximately 4 cm (Figure 1a) and was tender to touch. There was no appreciable drainage, surrounding erythema, induration, or fluctuance. Testicular ultrasound showed a 4.2 cm heterogeneous and hypervascular right scrotal extratesticular mass. The right scrotal mass was excised, and histopathological evaluation was suggestive of DFSP with fibrosarcoma component. The immunohistochemical stain of the specimen was diffusely positive for CD34 (Figure 1b). The more hypercellular area resembling fibrosarcoma was focally and weakly positive for CD34. Staining was negative for desmin, SMA, and S100. He moved out of state and was lost to follow-up.
Figure 1.
(a) Gross image of excised lesion. (b) Diffuse positive CD34 staining of spindle cells.
DISCUSSION
DFSPs constitute <0.1% of all malignant tumor cases and <1% of all soft tissue sarcomas, with a higher incidence among African Americans than Caucasians.1–3 DFSP commonly presents as an asymptomatic indurated plaque that slowly grows over months to years. As it enlarges, it becomes raised, firm, and nodular, and surrounding skin may be telangiectatic. DFSP most commonly manifests on the trunk or proximal extremities; only 1% of cases have been reported to occur in the genital area, most of which have been vulvar DFSPs.4 DFSPs follow an indolent growth pattern, often go undiagnosed for years, rarely metastasize to regional lymph nodes, and spread hematogenously even less commonly. DFSP–fibrosarcomatous differentiation variants have increased mitotic activity and are considered intermediate-grade sarcoma with higher predilection for metastasis.4
Most DFSPs are marked by a unique translocation, t(17;22) (q22;q13), which results in the fusion of the gene for platelet-derived growth factor (PDGF) with the highly expressed type 1A1 collagen (COL1A1) gene.5 The COL1A1-PDGFB fusion places the expression of the normally inhibited PDGF gene under the activating control of COL1A1 promoter, producing a fully functional PDGF gene and continuous activation of the PDGF receptor β, a tyrosine kinase.4
Core needle or excisional biopsy is required for definitive diagnosis. Histologically, DFSPs are made up of uniform spindle cell fascicles growing in a storiform pattern in the subcutaneous and dermal layers. Immunohistochemically, the spindle cells of DFSP reveal strong and diffuse cytoplasmic expressions of CD34. Standard therapy for resectable DFSPs is complete surgical excision with either wide local excision with at least 2-cm tumor-free margins or Mohs micrographic surgery.2 Unresectable, recurrent, or metastatic DFSPs are treated with radiation therapy and/or targeted therapy (i.e., imatinib mesylate, a tyrosine kinase inhibitor).5–7
References
- 1.Allen A, Ahn C, Sangüeza OP.. Dermatofibrosarcoma protuberans. Dermatol Clin. 2019;37(4):483–488. doi: 10.1016/j.det.2019.05.006. [DOI] [PubMed] [Google Scholar]
- 2.Bogucki B, Neuhaus I, Hurst EA.. Dermatofibrosarcoma protuberans: a review of the literature. Dermatol Surg. 2012;38(4):537–551. doi:10.1111/j.1524-4725.2011.02292 [DOI] [PubMed] [Google Scholar]
- 3.Kreicher KL, Kurlander DE, Gittleman HR, Barnholtz-Sloan JS, Bordeaux JS.. Incidence and survival of primary dermatofibrosarcoma protuberans in the United States. Dermatol Surg. 2016;42(Supplement 1):S24–S31. doi: 10.1097/DSS.0000000000000300. [DOI] [PubMed] [Google Scholar]
- 4.Hao X, Billings SD, Wu F, et al. Dermatofibrosarcoma protuberans: update on the diagnosis and treatment. JCM. 2020;9(6):1752. doi: 10.3390/jcm9061752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thway K, Noujaim J, Jones RL, Fisher C.. Dermatofibrosarcoma protuberans: pathology, genetics, and potential therapeutic strategies. Ann Diagn Pathol. 2016; 25:64–71. doi: 10.1016/j.anndiagpath.2016.09.013. [DOI] [PubMed] [Google Scholar]
- 6.Han A, Chen EH, Niedt G, Sherman W, Ratner D.. Neoadjuvant imatinib therapy for dermatofibrosarcoma protuberans. Arch Dermatol. 2009;145(7):792–796. doi: 10.1001/archdermatol.2009.140. [DOI] [PubMed] [Google Scholar]
- 7.Al Tarakji M, Toro A, Di Carlo I, Junejo K.. Unusual presentation of dermatofibrosarcoma protuberans in a male patient’s breast: a case report and review of the literature. World J Surg Onc. 2015;13(1):158. doi: 10.1186/s12957-015-0562-1. [DOI] [PMC free article] [PubMed] [Google Scholar]