Abstract
Population aging has increased the need for long-term care of older persons who suffer from multi-morbidity and chronic conditions. Today, the majority of older people are living alone in their home in which they try to cope with highly risky conditions such as sensory impairment, diminished mobility, and medication management. Recent developments in information technologies could improve the access to care for older people as well as reducing the need for full-time caregivers both in homes and institutions such as nursery homes and hospitals. This study aimed to review the economic evaluation of such technological advancements in the care of older people. Through a systematic approach, electronic databases were searched and of 2732 records retrieved, three papers were included in the final review. Three different models of economic evaluation including cost analysis, cost–benefit analysis and cost-effectiveness analysis were applied in these studies in the context of telemedicine and older persons' care. Since the methodological approaches were quite different and the outcomes reported were not consistent between studies, no meta-analysis was applicable and we qualitatively reviewed the papers. All studies have reported cost savings associated with the use of telemedicine technologies such as video visits and smart homes in the care of older persons.
Keywords: Aging, cost-effectiveness, telemedicine
Introduction
Based on the demographic estimations, the increased life expectancy has resulted in population aging around the world. The great majority of older people are living alone in their home in which they try to cope with highly risky conditions such as falls, sensory impairment, diminished mobility, isolation, and medication management. Aiming to a society with healthy citizens, we seek solutions that will improve the quality of their lives and allow them to stay safe at home. Recent developments in information and communication technologies related to computer networks and artificial intelligence have made the vision of building a smart home environment technologically feasible.[1] Through advances in sensor and telecommunication technology, monitoring technology may become one of the key solutions for achieving a more efficient health-care system and allowing older people to live longer independently.[2]
The population aging will be followed by an increase in the number of disabled persons, therefore, the need for care and assistance to these people is highly important from both economic and social perspective. Considering the fact of aging society in connection with the existence of new care models, the home care demand is imperative.[3]
Telemedicine is an extended term in health information technology that comprises procedures for transmitting medical information electronically to improve patients' health status. Telemedicine can be beneficial to patients living in isolated communities and remote regions, who can receive care from doctors or specialists far away without the patient having to travel to visit them. There is increasing interest in the use of telemedicine as a means of health-care delivery. This is partly because technological advances have made the equipment less expensive and simpler to use and partly because increasing health-care costs and patient expectations have increased the need to find alternative modes of health-care delivery.[4]
Telehealth, the provision of care at a distance, is also a key component in future information and communication technology infrastructure for integrated care. An increasingly solid evidence base is emerging, indicating that telehealth can be used effectively to help support better integrated care, in particular for those with long-term chronic conditions.[5]
With the increase in the number of older adults, the home health-care industry has also expanded. Telemedicine programs expand the range of services that can be provided to older patients as part of home health care, and many home health-care agencies include technology-based services or serve clients who receive treatment from telemedicine programs.[6]
Telemedicine-based care provides remote health and social care to maintain people's autonomy and increase their quality of life. The rapidly aging population has come with a significant increase in the prevalence of chronic diseases and their effects, and thus the need for increased care and welfare.[7]
A significant percentage of the older adult population experience at least one chronic illness that requires regular monitoring and some degree of self-management through symptom monitoring, treatment seeking, and evaluating the effects of treatment.[8] The rising prevalence of chronic diseases combined with population aging now represents a very real problem for public health. The cost of these chronic diseases has rocketed and is estimated at several billion dollars in developed countries. What's more, these patients are often older people and have one or more chronic diseases, and their management is a challenge for health-care professionals. Their needs eat up large amounts of medical resources, just as a shortage in the time careers can provide beginning to be felt, with medical deserts and a lack of access to health-care professionals, among other problems. In this setting, telemedicine is a promising solution.[9]
Therefore, older persons have become one of the main target groups for telecare technologies. Smart home systems allow older adults to live in the environment of their choice and protect them against institutionalization or placement in a nursing home. It gives the older person a feeling of reassurance and safety and appears to be one of the most promising approaches to facilitate independent living in a community-dwelling situation. Telecare solutions provide new opportunities for diagnosis, treatment, education, and rehabilitation and make it possible to monitor patients with a number of chronic diseases. It also reduces socioeconomic disparity with regard to access to care and gives equal chances to patients from urban and rural areas.[7]
In many cases, the informal care by family members is being replaced by these technologies. Nevertheless, despite all speculations over economic benefits of telehealth interventions in older persons' care, there have not been a comprehensive review to assess the economic evaluation of such interventions so far. Therefore, in this study, we planned to systematically review these technologies when applied to the care of older persons to evaluate their economic benefits. The purpose of this study was to evaluate the economic impact of eHealth interventions in older persons' care to provide the evidence needed to decide on the financial support for these effective strategies and their inclusion in long-term care plans.
Materials and Methods
This study was a systematic review of literature and the protocol of this study had been submitted in Prospero with following ID: CRD42018117405.
Searches
We searched the following electronic databases: MEDLINE, OVID, EMBASE, Global Health, the Cochrane, Health Technology Assessment Database, and Web of Science (science and social science citation index) during February 1–15, 2019. References of related papers were also searched. We applied no language or date restrictions. The search strategy is as follows, with no filter on the title and abstract.
(effectiveness or economic evaluation or cost effectiveness)) and (eHealth or mobile care or smart health or computer care or telemedicine)) and (fall prevention) and (elderly or aging).
Participants/population
Inclusion
older people (aged 65 years or older) with a need to long-term care in a nursing home, hospital, or their own home were included in the study.
Exclusion
older persons who are receiving social care in residential centers as well as older people with neuropsychiatric disorders like Alzheimer or dementia were excluded from the study.
Intervention
electronic health interventions for older persons' care are those interventions to help caregivers and older people for better care such as chronic disease management, medication management/adherence, managing cognitive impairment in older adults, loss of independence in older patients, mobility impairment, and fall preventions. These interventions mainly rely on computer programs and smart phones such as mobile phones, web-based technologies and services, sensor based-telemedicine, virtual reality and robotics, and wearable and portable monitoring.
Comparator(s)/control
Alternative treatment could be direct observation of patient by a nurse or caregiver.
Types of study to be included initially
We included all cohort and randomized clinical trial studies regarding the economic evaluation of these interventions including cost-effectiveness analysis, cost–benefit studies, and cost–utility ones. Original researches as well as systematic reviews were considered. Other types of papers like editorials and commentaries were not reviewed.
Primary outcome(s)
Primary outcomes include changes in the rate of falls in intervention and comparison groups in the period of the study including baseline and follow-up rates.
Data extraction
Two researchers (HJ, BA) screened title and abstracts of paper and then critically reviewed all the papers included in the study. Each paper was reviewed independently and information was extracted into a table using a preestablished data entry format. We followed the preferred reporting items for systematic reviews and meta-analyses checklist in gathering the relevant information. The consolidated health economic evaluation reporting standards (CHEERS) checklist was also used to assess the economic evaluation method of each included study. Basic information describing each of the studies such as names of authors, title, year of publication, country of focus, method, interventions, population, main outcome, and costing was extracted. Any disagreement between the two reviewers in terms of data extracted was resolved by consensus among all authors. Each member of the review team critically examined the evidence extracted into the table to ensure that it addressed the objective of the review.
Strategy for data synthesis
A narrative synthesis of the findings including type of intervention, target population characteristics, and type of outcomes is provided.
Results
A total of 2732 records were retrieved by searching the databases PUBMED, OVID, EMBASE, Global Health, the Cochrane, Health Technology Assessment Database, and Web of Science (science and social science citation index). There were 740 duplicate records which were excluded from the study. The study retrieval is presented in Figure 1.
Figure 1.
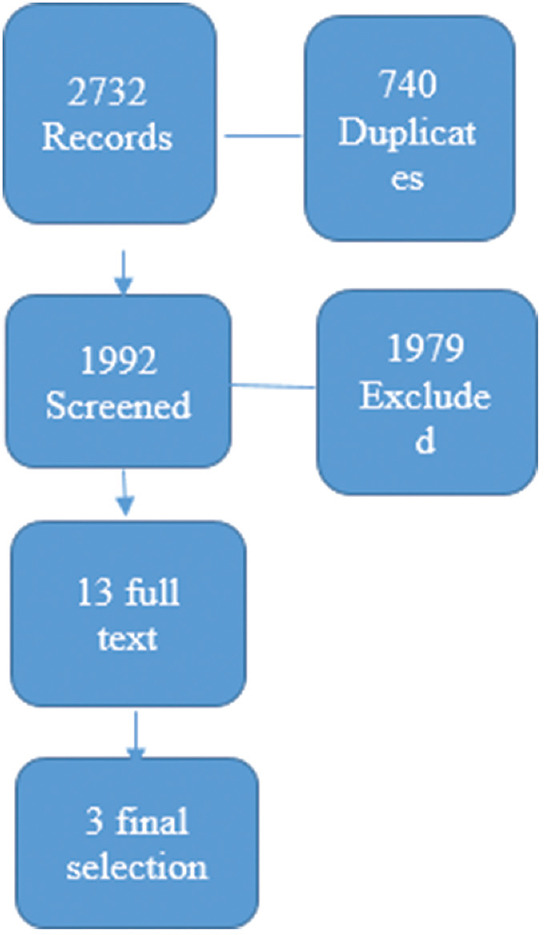
Study retrieval : Preferred reporting items for systematic reviews and meta-analyses
After reviewing the titles and abstracts of the papers, 13 articles were selected for full-text review. Of these 13 articles, three articles were selected for final review along with an appraisal by CHEERS checklist, a summary of their information is presented in Table 1.
Table 1.
Economic evaluation assessment (Cheers checklist)
| Reference number/criteria | 11 | 12 | 10 |
|---|---|---|---|
| 1 Title | Yes | Yes | Yes |
| 2 Abstract | Yes | Yes | Yes |
| 3 Background and objectives | Yes | Yes | Yes |
| 4 Target population and subgroups | Yes | Yes | Yes |
| 5 Setting and location | Yes | Yes | Yes |
| 6 Study perspective | Yes | Yes | Yes |
| 7 Comparators | Yes | Yes | Yes |
| 8 Time horizon | No | Yes | Yes |
| 9 Discount rate | No | No | Yes |
| 10 Choice of health outcomes | Yes | No | Yes |
| 11a Measurement of effectiveness | Yes | Yes | Yes |
| 11b Measurement of effectiveness | NA | NA | NA |
| 12 Measurement and valuation of preference based outcomes | No | NA | NA |
| 13a Estimating resources and costs | Yes | Yes | Yes |
| 13b Estimating resources and costs | NA | NA | NA |
| 14 Currency, price date, and conversion | No | No | Yes |
| 15 Choice of model | No | No | Yes |
| 16 Assumptions | No | No | Yes |
| 17 Analytical methods | No | No | Yes |
| 18 Study parameters | Yes | Yes | Yes |
| 19 Incremental costs and outcomes | Yes | No | No |
| 20a Characterizing uncertainty | No | Yes | Yes |
| 20b Characterizing uncertainty | No | No | No |
| 21 Characterizing heterogeneity | No | No | NA |
| 22 Study findings, limitations, generalizability, and current knowledge | Yes | Yes | Yes |
| 23 Source of funding | No | Yes | Yes |
| 24 Conflicts of interest | No | Yes | Yes |
NA=Not available
The classification of telemedicine intervention, type of economic evaluation, study design, population, and time span was conducted through reviewing the summary and the full text of the papers. A summary of the findings of these studies is provided in Table 2.
Table 2.
Data extraction
| Author year | Service setting | Study design | Economic evaluation | Assessment quality | perspective | Time horizon | Sample size | Cost measure ment | Conse quence measurement | Key findings |
|---|---|---|---|---|---|---|---|---|---|---|
| Versleijen et al., 2015[10] | Hospital geriatric visit | Case study | Cost analysis | One way sensitivity analysis of all parameters | Health service | Per annum | 20 patients | Cost per patient per round | 131AUD$ saving by using tele geriatric model | |
| Aanesen et al., 2011[11] | Home care | Review of case studies | CEA | Home care providers, relatives, hospital | Cost per visit | Percentage annual average wage costs per patient | The annual cost of nursing per patient 5296€ , twice as using SHT | |||
| Akiyama et al., [12] | Home care | Implementation study | CBA | Mont carlo simulation | Societal | 5 years | Capital +operation cost | Annual WTP | Base case BCR of model 1 and 2 was 1.63 and1.03 respec tively | |
| Giordano et al., 2016[13] | Home care | RCT | Societal | 6 months | 290 patients | Healthcare and patient cost cost diary | Fall reduction |
RCT=Randomized controlled trial, WTP=Willingness to pay, CEA=Cost Effectiveness Analysis , CBA=Cost Benefit Analysis, BCR=Benefit Cost Ratio, SHT=Smart Home Technology
As shown in Table 2, of the selected articles, only one paper is fully consistent with the primary outcome considered in the study protocol (fall reduction among older people), which is a study protocol itself and no results have been released so far.[13]
In the remaining three studies, the amount of decrease in the cost of physicians' visits to the patients site was considered as a benchmark for comparison between the studies.[10,11,12]
Discussion
To the best of our knowledge and based on searches conducted through electronic databases, this study is the first systematic review of the economic evaluations of electronic technologies in the care of the older persons, conducted during February 1–15, 2019. So far, studies have been conducted on the economic evaluation of telemedicine technologies in general[14,15] and not specifically in the care of the older people. Studies we have found in the literature do not address the primary outcome (falls rate) of predefined protocol; instead, they report cost savings happened by employing electronic health interventions. Although there are significant methodological differences between these papers, all of them report cost savings when using electronic health technologies in the care of the older persons.
In the study of “cost analysis of Tele geriatric services in a rural hospital,” the cost of visiting a long-distance geriatric specialist was compared to a video conference model in a rural hospital. In a basic model (assuming four patients per round on a 312 km round trip), an Australian Dollar (AUD) $ 131 fee per patient visit can be saved using the telegeriatric model. The most important cost drivers include the number of patients in each round and the distance and time in the model. With a workload of four patients per round and assuming a round trip time of more than 76 min, the cost of using telegeriatric service is lower.[10]
In the study of “Cost-benefit analysis of Tele-homecare for older people living independently in Japan,” the two models of governmental and nongovernmental support were compared. Using the decision tree model, two telehomecare operating models were analyzed using parameters derived from the literature review. In model 1 (nongovernment model), a monthly fee was paid by the clients to cover operating costs, and in model 2, which was a government-sponsored model, only programs' start-up costs were charged and there was no monthly charge. The cost–benefit ratio was calculated from the perspective of the community over a 5-year period by applying a 3% discount rate for costs and benefits. The benefits were calculated in terms of willingness to pay of consumers and preventive medical costs. The basic benefits of model 1 and model 2 were $ 417 and $ 97.30, respectively. The benefit–cost ratio for model 1 was 1.63 and model 2 was 1.03. The breakeven analysis also showed that the cost of the model 2 should be <$ 187,500. According to the results, the government model, which requires 5 years of start-up costs to pay, is less profitable than the second model, which has no government support and benefits from a consumer franchise on a monthly basis.[12]
The study of “Cost-effectiveness analysis of technology implementation in aging care” examined smart home technology and video home care services considering the cost of service providers, hospitals, and relatives and the savings happened in terms of time and cost incurred by these groups of caregivers and facilities. The study showed that smart home technology is cost-effective even if we consider only cost of care offered by relatives. Video visits have a higher start-up cost and need to be considered from both relatives and service providers to make it cost effective.[11]
As presented here, three different models of economic evaluation including cost analysis, cost–benefit analysis, and cost-effectiveness analysis are applied in these studies in the context of telemedicine and older persons' care. Since the methodological approaches were quite different and the outcomes reported were not consistent between studies, no meta-analysis was applicable and we qualitatively reviewed the papers.
Conclusion
Findings show that in all studies included in this review, there is cost saving in favor of using electronic health intervention as an alternative care approach. In the study of Versleijen (2015), investigating the use of telegeriatric services for remote rural areas, an AUD $ 131 fee per patient visit can be saved. The study of Aanesen (2011) assessed the cost-effectiveness of two technologies of smart homes and video visits in aging care considering cost of service providers, hospitals, and relatives. The smart home technology has shown to be cost-effective even when we only consider the cost of care offered by relatives. The video visit has more start-up cost but is still cost-effective when including costs of both relatives and service providers. In the study of Akiyama (2017), the technology itself was not analyzed; instead, two financing models of telehomecare for older people were analyzed in terms of cost and benefits and the government model, which requires 5 years of start-up costs to pay, found to be less profitable than the second model benefits from a consumer co-payment.
Overall, the studies included in this review have shown significant economic benefits in favor of these interventions, which could be a valuable evidence for policymakers to consider the use of these technologies in the older persons' care. Since older people often suffer from chronic illnesses and require frequent visits, providing such services through information technology for distance visits can provide them with invaluable assistance to receive long-term care while reducing the costs.
Since studies on the economic evaluation of electronic interventions are limited when applied in aging care, it is suggested that economic analysis should be added to the clinical trials or case studies regarding the use of telemedicine in aging care. Moreover, another systematic review could be conducted considering all economic evaluations reporting different clinical and nonclinical outcomes of using such technologies.
Limitations
The main limitation of this systematic review was the lack of enough economic evaluation studies on the use of electronic and telemedicine interventions in the context of older people's care. The existing studies also have employed different methodological approaches which made the comparison difficult. Studies screened for this systematic review have shown that the use of telemedicine technologies in the care of the older people has received less attention than in the areas of chronic conditions such as cardiovascular diseases and psychiatric disorders. In these areas, clinical trials on the use of telemedicine technologies and electronic interventions have been designed and economic evaluation studies have been conducted around them. In the field of older peoples' care, however, the present study has shown that limited evidence is available for the economic evaluation of these technologies.
Financial support and sponsorship
Health Management and Economics Research Centre, Iran University of Medical Sciences, Grant number (: 9605-163-32769).
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This study has received funding from Health Management and Economics Research Centre, Iran University of Medical Sciences (Grant number: 9605-163-32769). We would like to express our warmest gratitude to the colleagues in this centre who supported our research both financially and administratively.
References
- 1.Moraitou M, Pateli A, Fotiou S. Smart health caring home: A systematic review of smart home care for elders and chronic disease patients. Adv Exp Med Biol. 2017;989:255–64. doi: 10.1007/978-3-319-57348-9_22. [DOI] [PubMed] [Google Scholar]
- 2.Peetoom KK, Lexis MA, Joore M, Dirksen CD, De Witte LP. Literature review on monitoring technologies and their outcomes in independently living elderly people. Disabil Rehabil Assist Technol. 2015;10:271–94. doi: 10.3109/17483107.2014.961179. [DOI] [PubMed] [Google Scholar]
- 3.Arif MJ, El Emary IM, Koutsouris DD. A review on the technologies and services used in the self-management of health and independent living of elderly. Technol Health Care. 2014;22:677–87. doi: 10.3233/THC-140851. [DOI] [PubMed] [Google Scholar]
- 4.Delgoshaei B, Mobinizadeh M, Mojdekar R, Afzal E, Arabloo J, Mohamadi E. Telemedicine: A systematic review of economic evaluations. Med J Islam Repub Iran. 2017;31:113. doi: 10.14196/mjiri.31.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stroetmann KA, Kubitschke L, Robinson S, Stroetmann V, Cullen K, McDaid D. Copenhagen: World Health Organization; 2010. [Last accessed on 2020 Oct 07]. How Can Telehealth Help in the Provision of Integrated Care. Available from: https://apps.who.int/iris/handle/10665/332044 . [Google Scholar]
- 6.Kropf NP, Grigsby RK. Telemedicine for older adults. Home Health Care Serv Q. 1999;17:1. doi: 10.1300/J027v17n04_01. [DOI] [PubMed] [Google Scholar]
- 7.Bujnowska-Fedak MM, Grata-Borkowska U. Use of telemedicine-based care for the aging and elderly: Promises and pitfalls. Smart Homecare Technol Telehealth. 2015;3:91–105. [Google Scholar]
- 8.Foster MV, Sethares KA. Facilitators and barriers to the adoption of telehealth in older adults: an integrative review. Comput Inform Nurs. 2014;32:523–33. doi: 10.1097/CIN.0000000000000105. [DOI] [PubMed] [Google Scholar]
- 9.Andrès E, Talha S, Hajjam M, Hajjam A. Telemedicine in elderly patients: The time of maturity with telemedicine 2.0! A short review with a focus on the E-care project. Am J Gerentol Geriatr. 2018;1:1011. [Google Scholar]
- 10.Versleijen M, Martin-Khan MG, Whitty JA, Smith AC, Gray LC. A telegeriatric service in a small rural hospital: A case study and cost analysis. J Telemed Telecare. 2015;21:459–68. doi: 10.1177/1357633X15611327. [DOI] [PubMed] [Google Scholar]
- 11.Aanesen M, Lotherington AT, Olsen F. Smarter elder care? A cost-effectiveness analysis of implementing technology in elder care. Health Informatics J. 2011;17:161–72. doi: 10.1177/1460458211409716. [DOI] [PubMed] [Google Scholar]
- 12.Akiyama M, Abraham C. Comparative cost-benefit analysis of tele-homecare for community-dwelling elderly in Japan: Non-Government versus Government Supported Funding Models. Int J Med Inform. 2017;104:1–9. doi: 10.1016/j.ijmedinf.2017.04.017. [DOI] [PubMed] [Google Scholar]
- 13.Giordano A, Bonometti GP, Vanoglio F, Paneroni M, Bernocchi P, Comini L, et al. Feasibility and cost-effectiveness of a multidisciplinary home-telehealth intervention programme to reduce falls among elderly discharged from hospital: Study protocol for a randomized controlled trial. BMC Geriatr. 2016;16:209. doi: 10.1186/s12877-016-0378-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wade VA, Karnon J, Elshaug AG, Hiller JE. A systematic review of economic analyses of telehealth services using real time video communication. BMC Health Serv Res. 2010;10:233. doi: 10.1186/1472-6963-10-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akiyama M, Yoo BK. A systematic review of the economic evaluation of telemedicine in Japan. J Prev Med Public Health. 2016;49:183–96. doi: 10.3961/jpmph.16.043. [DOI] [PMC free article] [PubMed] [Google Scholar]


