The COVID-19 pandemic disrupted the 2020 to 2021 integrated plastic surgery residency application cycle. The American Council of Academic Plastic Surgeons wisely recommended that residency interviews should be conducted virtually for the safety of students, faculty, and the general public. However, the pandemic has both exacerbated and highlighted a longstanding problem.
In an open letter, the Association of American Medical Colleges suggested that above-average applicants accepted more interview offers in the 2020 to 2021 cycle compared with previous years.1 Historically, time and money have been the predominant factors limiting interview hoarding. Virtual interviews removed these limitations, consequently eliminating the principal reason for declining an invitation. Declined interviews are normally extended to the next tier of applicants. This phenomenon, well-known among applicants as the trickle, was almost nonexistent this cycle. We suspect that the paucity of away rotations and uncertainty in how programs would evaluate students in virtual interviews was responsible for this trend. By stockpiling invitations, applicants hoped to increase their probability of matching into an integrated plastic surgery residency. Unfortunately, this left other students with fewer interviews than anticipated.
During the 2020 to 2021 match cycle, plastic surgery applicants applied to 18% more programs than the previous 5 years. This comes after programs in the 2019 to 2020 cycle were bombarded with 21% more applications than the year before (Fig. 1). Hyperinflation of applications has introduced congestion in the interview process.2 Proposed solutions to hyperinflation in the plastic surgery match include implementing secondary applications and capping both the maximum number of programs to which applicants can apply and to where they can interview.3,4 However, there was little urgency to adapt proposed changes as plastic surgery has had an efficient match rate of >99% over the past 5 years. The consequence of interview hoarding will likely result in a disparity between above- and below-average applicants in the match if immediate action is not taken. Although these strategies can no longer be implemented to create a more equitable interview process for this cycle, we propose a new solution—one which applicants still have the ability to enact and can enact in future years.
FIGURE 1.
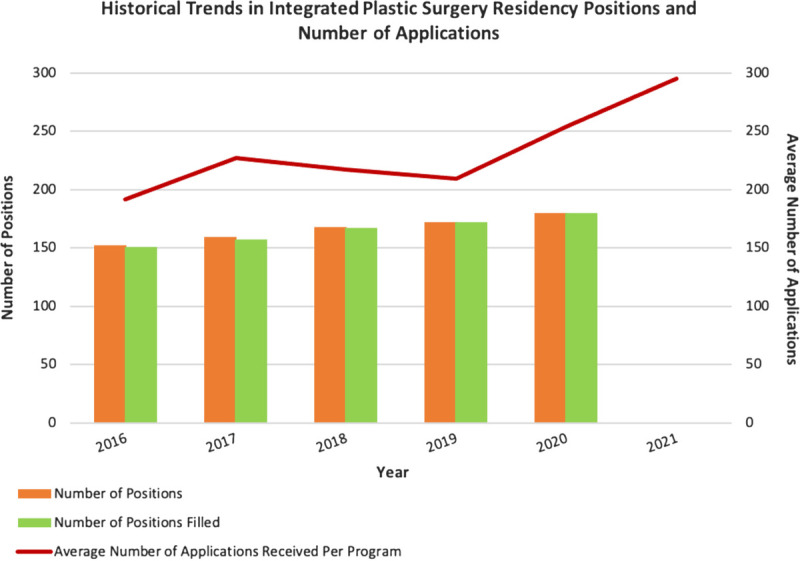
Total number of available and filled positions and average number of residency applications received per program. Data obtained from ERAS reports and NRMP Charting Outcomes in the Match publications. Data for the 2021 cycle are not yet publicly available. NRMP, National Resident Matching Program.
In the midst of this unique application cycle, we are calling to applicants to consider their role in making this year another successful match. For applicants, 15 contiguous rankings provide a greater than 95% probability of matching in integrated plastic surgery residency.5 Those with a sufficient number of interviews should consider releasing some invitations to extend the opportunity to their colleagues. All students should refer to historical match data and guidance from advisors to maximize their chance of a successful match. However, a truly equitable process can only be achieved when these concerns are addressed by programs and organizations overseeing the residency process at the national level. One mechanism for achieving this would include offering extending more interviews during times of uncertainty as travel restrictions may still be in place next year. Despite these difficulties, we wish all applicants the best of luck during this challenging time.
Footnotes
Author Contributions: C.B. was directly involved in the collection of resources, formulation of ideas, writing the article, and approving the final version for submission. S.A. was directly involved in the collection of resources, formulation of ideas, writing the article, and approving the final version for submission. R.V. was directly involved in the collection of resources, formulation of ideas, writing the article, and approving the final version for submission. T.K. was directly involved in the, formulation of ideas, writing the article, and approving the final version for submission. P.S. was directly involved in the, formulation of ideas, writing the article, and approving the final version for submission.
Conflicts of interest and sources of funding: none declared.
Contributor Information
Shivani Ananthasekar, Email: ashivani@uab.edu.
Rebecca Vernon, Email: Rebecca.Vernon@nyulangone.org.
Timothy W. King, Email: twking@uabmc.edu.
Pierre B. Saadeh, Email: Pierre.Saadeh@nyulangone.org.
REFERENCES
- 1.Whelan A. Open letter on residency interviews. Association of American Medical Colleges December. 2020;18. Available at: https://www.aamc.org/media/50291/download. [Google Scholar]
- 2.ERAS Statistics. Washington, DC: Association of American Medical Colleges; 2020. Available at: https://www.aamc.org/data-reports/interactive-data/eras-statistics-data. [Google Scholar]
- 3.Boyd CJ. BS implementation of a secondary application to increase efficiency in the plastic surgery match. Ann Plast Surg. 2020;84:475. [DOI] [PubMed] [Google Scholar]
- 4.Asaad M, Rajesh A, Kambhampati PV, et al . Virtual interviews during COVID-19. Ann Plast Surg. 2021;86:367–370. [DOI] [PubMed] [Google Scholar]
- 5.National Resident Matching Program . Charting Outcomes in the Match: Senior Students of U.S. Medical Schools, 2020. Washington, DC: National Resident Matching Program; 2020. [Google Scholar]


