Abstract
Despite efforts to address HIV-infection, adolescents and young peoples’ (AYP) engagement in interventions remains suboptimal. Guided by a risk protection framework we describe factors that support positive and negative experiences of HIV and SRH interventions among AYP in rural KwaZulu-Natal, South Africa, using data from: community mapping; repeat semi-structured individual interviews (n= 58 in 2017, n=50 in 2018, n=37 in 2019–2020); and group discussions (n=13). AYP who had appropriate and accurate HIV-and SRH-related information were reported to use health care services. Responsive health care workers, good family and peer relationships were seen to be protective through building close connections and improving self-efficacy to access care. In contrast to cross-generational relationships with men, alcohol and drug use and early pregnancy were seen to put AYP at risk. Policies and interventions are needed that promote stable and supportive relationships with caregivers and peers, positive social norms and non-judgemental behaviour within clinical services.
Keywords: HIV, Protective Factors, Prevention Interventions, Adolescents, Risk, South Africa
Introduction
The greatest burden of HIV remains among adolescents and young people (AYP) aged 15–24 years in East and southern Africa, with an estimated 300,000 new infections and 36,000 AIDS-related deaths in 2017 (UNICEF, 2017). A 2019 systematic review and meta-analysis showed that in the decade following anti-retroviral treatment scale-up (2006–2015), HIV incidence rates among young women declined in many East and southern African settings, but remained high in KwaZulu-Natal, South Africa: 7.79 per 100 person-years among females aged 15–19 years, and 8.63 in those aged 20–24 years (Birdthistle et al., 2019). Heterosexual transmission is the dominant mode of HIV transmission among adolescent girls and young women (AGYW) who, on average, acquire HIV five to seven years earlier than adolescent boys and young men (ABYM) (Baxter and Karim, 2016). This gender difference persists despite highly effective, affordable biomedical and socio-behavioural tools to reduce HIV acquisition, transmission, mortality; and improved access and uptake to sexual and reproductive health (SRH) services.
Adolescence presents a time of rapid biological, psychological and behavioural development that can lead to health-related vulnerability (Patton et al., 2016). For adolescents, decisions about health are more reactionary than preventive, influencing the ability to make reasonable choices in daily life situations (Leshem, 2016). Satisfaction of immediate needs and mitigation of short-term dangers can result in overwhelming HIV-related consequences for AYP limiting: life chances, access to services, education, health outcomes, and access to social networks and processes (Strauss, Rhodes, & George, 2015; Tomita et al., 2019). Studies from South Africa and other low-income settings have consistently shown that extreme poverty, poor access to services, family conflict, early pregnancy and other adversities put AYP at increased risk of HIV infection and poorer educational and economic outcomes (Meinck, Cluver, Boyes, & Loening-Voysey, 2016; Ward, Makusha, & Bray, 2015). Understanding the factors that enhance protection is important in developing interventions which support AYP adapt to stressful and risky life situations (Lee, Cheung, & Kwong, 2012).
In 2016, a population-based study conducted in uMkhanyakude district in rural KwaZulu-Natal showed that in addition to the high burden of sexually acquired HIV (40% antenatal prevalence) there was a high burden of wider sexual health morbidity amongst AGYW (Francis et al., 2018). About 20% of women and 10% of 15–24-year olds had a curable STI and 40% of the women had bacterial vaginosis (Francis, et al., 2018). Factors associated with having an STI included being an older adolescent, being female, not being in school and not working. Another study found that the incidence of teenage pregnancy is 6.4% (5.7–8.6) and the majority of AGYW (15–24) start contraception after their first pregnancy (Chimbindi et al., 2018).
We explore young people’s conceptualisations of protective processes and risk factors contributing to this high burden of HIV and sexual health morbidity to inform interventions to improve resilience in AYP.
Conceptual framework
We used the protection-risk framework by Jessor (1991) in our analysis to situate a young person in the context where specific HIV prevention interventions are being delivered. The framework allows for the examination of contextual, social and individual factors that promote experiences of HIV interventions among AYP (Jessor et al., 2003), see (Table 1). The table outlines characteristics of protective factors (which enhance positive health behaviour) and risk factors (which increase the probability of engaging in risk behaviours) (Jessor, et al., 2003). The framework provides a structure for explaining why some adolescents effectively engage with HIV and/or sexual health interventions for treatment or for prevention, while others do not and as a result are exposed to or remain at risk of contracting HIV and other STIs. The framework highlights factors that are associated with resilience which can improve activities for promoting well-being.
Table 1:
Characteristics of the protection-risk framework
| Conventional behaviour involvement: Protective factors | Description |
|---|---|
| Models | Factors which include peer models who promote and encourage prosocial behaviour |
| Controls | Include individual-level or social- environment level factors promoting social values |
| Support | Refers to contextual support or other social environments that promote prosocial or health enhancing behaviour |
| Problem behaviour involvement: Risk Factors | |
| Models | Include models who induce health-compromising behaviour |
| Opportunity | Refers to exposure to or access to situations that increase the likelihood of engaging in risk behaviours |
| Vulnerability | Refers to individual characteristics that increase the likelihood of engaging in risk behaviour |
Source: Jessor, R. et.al, (2003). Adolescent problem behaviour in China and the United States: A cross-national study of psychosocial protective factors. Journal of Research on adolescence, 13(3), 329–360.
Methods
A qualitative inquiry was undertaken to solicit views of positive and negative experiences of HIV interventions among AYP in four rural communities in KwaZulu-Natal, South Africa.
Setting
The Hlabisa sub-district of uMkhanyakude district is largely rural, made up of scattered settlements (Tanser, Hosegood, Benzler, & Solarsh, 2001) with a population of about 27,000 AYP (10–24 years old); 85% of those aged 22–24 are unemployed (Tanser et al., 2007). Within the district, there is one hospital, 13 fixed primary health care clinics and 30 mobile clinic points which are visited twice every month (Tanser, et al., 2001). Free HIV testing, treatment and care is available from these public health care facilities, in accordance with South African department of health (DoH) guidelines (Department of Health). In this setting, about 19% of AGYW and 5.6% of ABYM are living with HIV (Francis, et al., 2018). Within this context, a multisectoral HIV prevention programme – the DREAMS Partnership (Determined, Resilient, Empowered, AIDS-Free, Mentored, and Safe lives) - was implemented between April 2016−September 2018 to reduce HIV infection in AGYW (and their male sexual partners) through a combination of evidence-based health, educational and social interventions (Chimbindi, et al., 2018; Saul et al., 2018) including among others, condom promotion and provision, PrEP, post-violence care, VMMC, HIV testing and treatment. We use data collected in the community as part of a wider evaluation of DREAMS between May 2017−January 2020 to understand factors that support positive and negative experiences of HIV interventions among AYP at high risk of HIV.
Target population and sampling
Stratified purposive sampling was used to recruit individual in-depth interview (IDI) participants and group discussion (GD) participants. Participants were recruited if they were within the age targeted by DREAMS (10–24 years AGYW,15–35 years ABYM), and if they were willing to provide written informed consent to participate in audio-recorded IDIs or GDs. Signed consent was provided by participants and was sought from parents or guardians with assent for participants under 18 years of age. The study and research procedures were explained to participants, parents or guardians during recruitment. IDI participants were approached and recruited from their households, schools, and from locations where AYP gathered. GD participants were recruited within the community from areas such as local trading stores and community water collection points. Separate gender and age GDs were organised for younger and older participants to maximize participants ability to voice opinions, particularly on gender-related matters and interventions targeted specifically to males or females of different ages, offered through the DREAMS programme. We included community leaders in the identification of venues to conduct GDs to allow participants to feel comfortable and we also piloted all data collection tools with younger and older participants in two rural communities for a period of 2 months to gauge the appropriateness of instruments.
Data collection and management
Data were collected by a team of eight research assistants (4 men and 4 women) who speak fluent isiZulu, the local language used in the area. Oversight of data collection was provided by the first author, an experienced isiZulu speaking social science researcher who had worked in the same community for ten years. IDIs took between 30–60 minutes and were conducted in participant’s homes and venues where participants felt comfortable such as schools. Group discussions were conducted once off, in 2017, in places where AYP came together naturally during daily social activities i.e. ‘natural’ group discussions, not pre-arranged, and also with groups that were organised and conducted in venues arranged by the researcher with the support of community leaders (‘focus’ group discussion) (Kielmann, Cataldo, & Seeley, 2012), taking between 60–120 minutes. During GDs, one research assistant was responsible for leading the discussion and a second research assistant observed proceedings and took field notes. Rapid community mapping was undertaken to gain a broad understanding of the social context for AYP and took between three to five days in each community. An open-ended topic guide was used in IDIs and GDs and an observation checklist supported community mapping (Bond et al., 2019). IDIs were repeated with the same participants at three time points between August 2017−January 2020 to enable validation of findings and to tease out participants’ explanations around differences and similarities of perceptions and experiences and to provide understanding about issues suggested by participants in previous interviews. Repeat interviews provided an opportunity for interviewers and participants to engage in a process of elaboration and collective understanding of the perspectives and experiences shared by participants in interviews. Participants had an opportunity to share the meaning and events shaping their lives, without being interpreted only by the interviewer.. Subsequent interviews were arranged with participants through phone calls or once a participant was visited at home and agreed to a follow-up interview. This extended contact with participants provided an opportunity to obtain rich descriptions of individual views of what facilitates or hinders engagement with HIV prevention interventions. Discussions from IDIs and GDs were audio recorded, transcribed verbatim and translated from isiZulu to English by the same research team members who collected the data. Quality checks were conducted by the first author.
Data analysis and interpretation
Guided by the protection-risk conceptual framework, TZ and SM read field notes to guide decisions and thoughts through the research process and read transcripts to generate an initial coding framework using NVIVO version 11. Findings from IDIs, GDs and community mapping were triangulated throughout data collection. Narratives clarifying factors that enhance risk or support wellbeing were extracted and categorised into themes and were discussed by TZ and MS with the research team during the analysis process. TZ, JS and MS iteratively reviewed the initial themes, reconciled differences and discrepancies and refined themes throughout the analysis process. Further description and interpretation were undertaken by all authors during analysis and write up.
Ethics
Full ethical approval was granted by the University of KwaZulu-Natal’s Biomedical Research Ethics Committee (BREC) (Ref: BFC339/16) and the London School of Hygiene & Tropical Medicine’s Research Ethics Committee (Ref: 11835) as well as the Hlabisa District Hospital, and the AHRI Somkhele Community Advisory Board.
Findings
Participants characteristics
A total of 137 participants were included in the study (Table 2). GD participants included 79 (n= 31 females and n= 48 males) and IDI participants included 58 (n= 35 females and n= 23 males). Most participants in individual interviews had secondary level education and (n= 20 male/n= 3 female) were unemployed. In 2018, eight (n= 3 females and n=5 males) and in 2019–2020, 21 participants (n=12 females and n=9 males) were lost to follow up. The main reason for loss to follow up was relocation out of the area and in 2019–2020, four participants refused to be interviewed for the third time, stating that they did not have time.
Table 2:
Description of study participants
| Interviews | Group discussions | |
|---|---|---|
| Number of participants | n= 58 in year one n= 50 repeated with the same individuals in year two n=37 repeated with the same individuals in year three |
FGD= 11 FGDs with n=61 participants Natural groups = 2 NGs with n=18 participants Total of 13 GDs n=79 participants Conducted in year one |
| Age range (years) | Female (10–24) Male (12–35) |
Female (11–21) Male (11–27) |
| Gender | Female: n=35 Male: n=23 |
n=31 n=48 |
We draw on six cases to provide an in-depth explanation of participants who took part in the longitudinal qualitative interviews and we use their lived experiences to illustrate each of the main themes. All the cases included life stories of participants from the first to the third year that participants engaged with researchers. Cases were selected to illustrate changes and adjustments made by young people over time and to represent diversity in events narrated in IDIs. Selected cases provide examples of how risks such as unemployment, lack of information, being moved from safe environments and having friends who endorse risk exposes AYP to HIV risk behaviours. Additionally, examples demonstrate how high levels of protective factors are likely to promote resilience to AYP exposed to similar risks. To maintain anonymity, these six people have been assigned pseudonyms. We use direct quotes from IDIs and GD transcripts to illustrate factors that support resilience and protection amongst young people and to validate themes. Unique identifying codes (age, gender, IDI or GD) are used for all participants in IDIs and GD. Different risk and protective factors related to contextual (peer models), social (support), and individual characteristics (controls), for example, heath care competence, reduced self-efficacy, social context, and family and peer networks emerged as shown in (diagram 1).
Diagram 1:
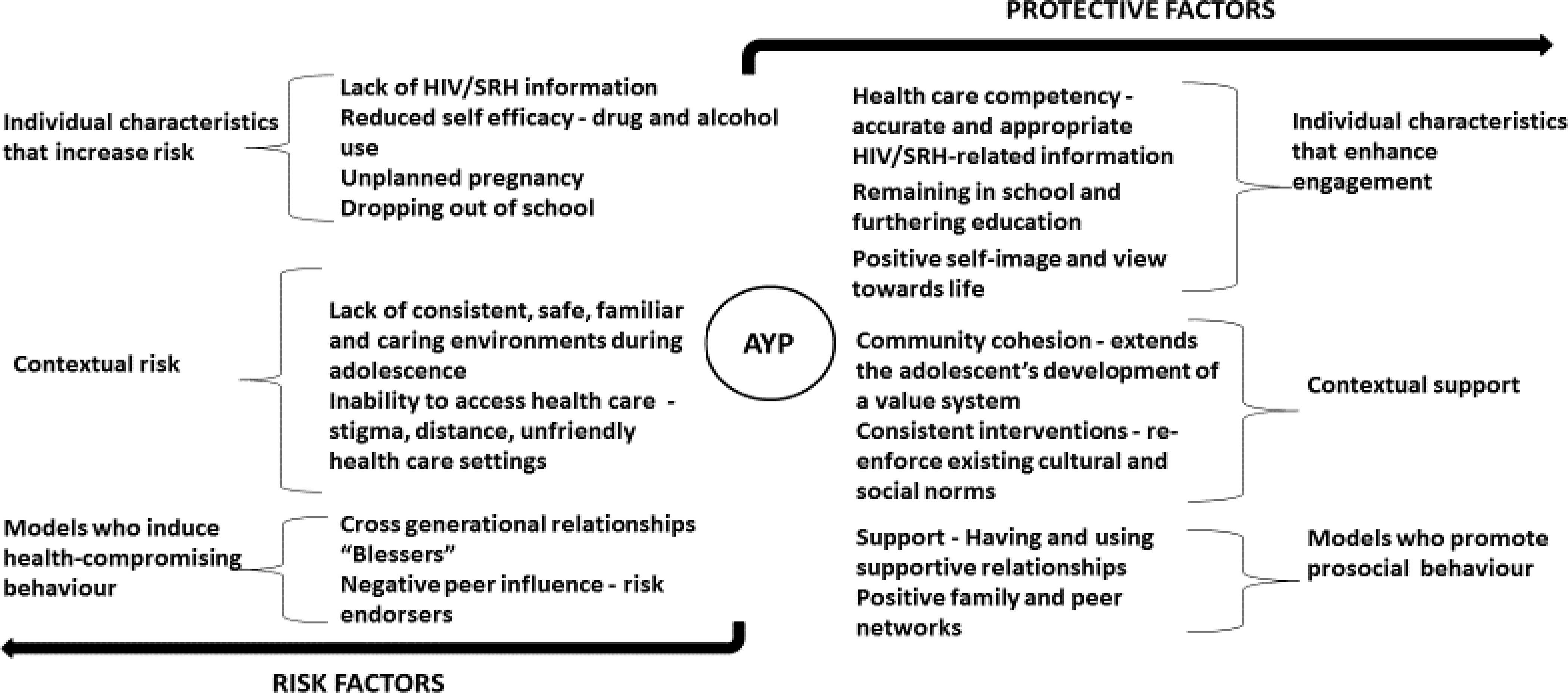
Risk and Protective factors
Risk Factors
Individual characteristics that increase risk
Mandla is a 21-year-old male who dropped out of school before completing secondary level education and had no plans to go back to school as ‘he had grown in age’. When we first met Mandla he had been looking for employment in a local mine for over a year. He told us that he hoped to be a security guard or a public transport driver but did not have financial support from his family to have his plans realised. He regarded his home as a place ‘to sleep and eat’. He said, ‘I wish God could help me find a job because I do not have any more strength’. To cope, Mandla started using drugs, including alcohol and marijuana. One Friday night when Mandla was drinking with his friends, he was arrested for four days when he was implicated in a shooting.
To protect himself from HIV-infection Mandla said he used 2 condoms at a time, did not sleep with a girl he knew ‘was sleeping around’ and when he thought that a girl was not HIV-infected (judged, he said, by the way she talked), he did not use a condom. He said that at school there were people who came to teach them about HIV and SRH. Since he left school, a year after our first interview, there was no one he talked to and it was difficult for him to go to the clinic because it was always full, and he feared being judged. Mandla’s understanding of risks and prevention was echoed in the narratives of other AYP in the study:
Lack of HIV/SRH Information:
Individual HIV and SRH knowledge had an impact on access and utilisation of interventions. One 17-year-old-female said that without this information ‘young people will grow up without knowing what they should do, so we need the information’; another 16-year-old female observed that ‘as young people we do not have platforms where we can meet and we do not have much information’. Participants said that acquiring relevant information allowed them to make informed sexual health decisions and take necessary precautions once they were sexually active. This they contrasted to views held by their parents and caregivers, that sexual health information was going to make it easy for them to have sex. One 23-year-old male said, ‘there are few parents who are able to explain to their teenagers about pregnancy, HIV/AIDS, and sex; it isn’t all parents who have that courage and time’. Most participants said there was a lack of guidance for AYP from their immediate family or households. AYP felt that their parents were opposed to them accessing SRH treatment and care as it was seen to be an indication that they were sexually active.
Reduced self-efficacy as a result of substance use:
In both IDIs and GDs, participants mentioned a high rate of drug and alcohol use among AYP, particularly among those aged 13–24 years (secondary school and post-secondary school).
For ABYM, risks included having unprotected sex as they said intoxication interfered with condom use and increased sexual risk behaviour. AGYW mentioned being forcefully grabbed by men, unwelcome sexual advances, having unprotected sex with someone they did not know, unplanned pregnancy, dropping out of school and challenges related to returning to school as they had to care for the child and study at the same time. Unplanned pregnancy affected the mother more than the father because the child would belong to the maternal side of the family after birth if the pregnancy was out of wedlock and if compensation or “damages” (In Zulu tradition, this is paid to the family of a woman who becomes pregnant out of wedlock by the father of the future child) were not paid to the girl’s family.
For both AGYW and ABYM, the use of whoonga was reported, a drug cocktail rumoured to contain illicit drugs and HIV antiretroviral medication (notably efavirenz). Participants said that the use of drugs and alcohol led to increased crime, rape and “ukulahla” (unplanned sex) which often did not involve condom use, other contraceptives or PrEP, as it was normally not premeditated. In a GD with males, one participant said, ‘using drugs and alcohol is like a style’, meaning that drug and alcohol are seen as a normative part of youth and the transition into adulthood.
Unplanned pregnancy:
Unplanned and teenage pregnancy were common themes in the interviews. Similarly, lack of knowledge of contraception methods and fear were recurrent themes. A 17-year-old female mentioned that:
I will just be confused as to which injection to go for, as they say there are injections for 3 months, 2 months and one month. I will not be sure which injection to choose and besides it gets full there [at the clinic].
Some AGYW believed that contraceptives did not work or caused death; and others were concerned about side effects including weight loss, weight gain, fear of becoming infertile when they used contraceptives before having a first child and bleeding disorders. Additional barriers which resulted in unplanned pregnancy was fearing disapproval of contraceptive use by parents or older adults at home, not having regular sexual partners and lacking skills to negotiate condom use with sexual partners.
Both AGYW and ABYM said that the high rate of teenage pregnancy in their communities showed that young people were not using condoms or other methods of contraceptives. AGYW further reported that some sexual partners did not like to use condoms but were in multiple relationships. Multiple sexual conquests seemed to be celebrated among ABYM. Narratives of multiple sexual partners were associated with the practice of polygamy which allows men to have multiple partners, and the expectation that women should remain monogamous.
Dropping out of school:
A secondary risk linked to alcohol use and unplanned pregnancy, was dropping out of school and taking a break from school. For AGYW, dropping out of school was mostly related to pregnancy as they needed to attend antenatal care, which was often delayed due to fear of being judged for engaging in premarital sex and for not wanting to be behind with schoolwork. Out of 35 AGYW in interviews, 3 who were still in school disclosed that they were pregnant. Those who became pregnant did not live with their parents or family members.
ABYM were likely to drop out of school if they constantly performed poorly in secondary school, as suggested above started using drugs and/or alcohol, and if they thought they were older and needed to work. One 18 year old male said ‘I had failed a lot, and I lost the love for school, I realized I had to leave and make some other [find a job] effort like others [other men]’.
Even if they finished secondary, most of the young people in our interviews couldn’t enrol for tertiary education because their families lacked financial resources: about 23, of 137, AYP in this study were not in education or employment. For older adolescents, not being in school and being unemployed resulted in despair, as it was expressed in an IDI with an 18-year-old female, ‘you see that this person’s life is a pity since he has nothing in life. He does have grade 12 [finished secondary school] but he is just staying [not doing anything] like a nobody’.
Participants said that being away from school often triggered a cycle of events which exposed AYP to more risks and less access to health care interventions and services than those who were in school. Accounts from younger participants who were in school in contrast were filled with ambition and hope for a prosperous future.
Opportunity Risk Factors
The following case provides an example of inconsistent and safe environments for young people. Zodwa, a 17-year-old female was in secondary school during our first interview in 2017. She had relocated from where she was born and was staying with her aunt and cousins. On weekends, she visited her grandmother who resided 55 kilometres away from where she stayed with her aunt. Her father had passed away and her mother was staying 350 kilometres away from her where she worked. On our second encounter with Zodwa, she was in the final year of senior school and her mother had passed away due to reasons unknown to her. She told us that after her mother died, life was difficult. She had difficulties at school, and she started drinking alcohol. As a result of excessive drinking, Zodwa was hospitalised and was told she had a liver problem. In our last interview she told us that on her return from hospital, she was moved to live with her uncle and her uncle’s wife in a nearby town. Staying in a new place made Zodwa anxious and she said she was never told why she was moved from her aunt. She started feeling like she was a burden to her family with no one she could talk to and confide in. She said even going to a health care facility was difficult because young people were judged by community members and health care workers. She talked to her peers about sexual health and received such information from school.
Other respondents also lacked a consistent, safe and familiar environment during adolescence exacerbated by high mobility, poverty, high rates of crime, unemployment and barriers to access healthcare.
Lack of consistent, safe, familiar and caring environments:
Participants indicated that when there was no one and ‘no platforms where we can meet as young people’, they tended to be drawn into risk situations and lacking guidance and care from older adults intensified the risks. As was the case with Zodwa, older (aged above 15) participants did not generally stay with their biological parents, as a result of furthering education, finding employment or losing parents through death. The distance from parents ranged from 25 kilometres, within the study location, and 600 kilometres, outside of the study location. Participants lived with their grandparents, aunts or uncles when parents were absent because of employment or a change in relationship or marriage status. An 18-year-old female whose mother left for employment and who was staying with her grandmother said, ‘I go to school in an empty stomach and come back, I go to bed without food, I live in that routine’. Fragmented family units posed a risk for AYP.
A dominant risk factor was living in an unsettled community. Participants reported community conditions including high rates of poverty and unemployment. One male participant (IDI, aged 23) shared:
when you grow up, […] it’s better when you have something to do as a youth, so that you can build your brighter future, keeping yourself busy. When you stay back home you end up doing all wrong things done by your peers without progress.
Other factors which affected AYP safety were lack of recreational facilities, lack of utilities such as water and electricity, and widespread violence and crime. Violence within the community was observed during community mapping, including in schools. Prevalent violence, lack of employment and recreational facilities seemed to leave no sense of belonging, particularly for ABYM. In addition, ABYM reported that they lacked opportunities for advancement in their communities with those who could, often leaving their communities in pursuit of financial stability.
Inability to access health care:
Health care facilities were reported as places which could compromise the health and wellbeing of AYP. Participants said that accessing health facilities, particularly for services such as SRH, HIV testing and treatment was a challenge as a result of judgemental behaviour by health care providers and by members of the community, as AYP were not expected to be engaging in sexual relations. This was expressed by a young female (IDI, aged 14) who said, ‘some young people who are pregnant don’t attend the clinic because they fear being seen by old people’. To deal with being stigmatised in health care facilities, participants preferred interventions and health care services that were community-based. They said that there were organisations offering home-based HIV testing and they also had community care givers who linked individuals to different services. Participants said that home-based interventions and health care services provided more privacy and confidentiality. Lack of confidentiality in health facilities was a prominent barrier that AYP encountered. A 15-year-old female participant said, ‘we are afraid because it seems our nurses cannot keep our information confidential’. Being treated differently because of their youth seemed to be an additional challenge for AYP.
The fear of moralistic and judgemental attitudes limited AYP opportunities to utilise HIV-related interventions, including those delivered through the DREAMS partnership. Generally, participants feared an HIV positive diagnosis, being known by others to be living with HIV and taking treatment for life, but they acknowledged the effectiveness of ART. Participants expressed difficulties normalising love and relationships in the time of HIV. Elements of stigma (internal and external), directed to people living with HIV coexisted with information and knowledge that once infected, they could use lifesaving ART and live “normal” lives:
I fear being HIV positive because it sometimes makes it hard to live life, because other people end up not even getting married, some do not get the partners they want, and some don’t reach their goals in life because they will say their lives are a mess (18-year old male).
In addition to having unsafe and inconsistent environments some AYP were surrounded by people who hindered effective functioning such as friends who endorsed risky behaviour as described below.
Factors which induce health-compromising behaviour
Zanele was 18 years of age and doing final school examinations when we first met her in 2017. She lived with her aunt, her uncle and her siblings. Her father and stepmother lived 56 kilometres away. She spoke to her father over the phone and sometimes visited over holidays. She said that in her community, there were high rates of teenage pregnancy, that most young people who had finished school were unemployed and that there was a high rate of crime. In 2018, Zanele did not pass her secondary level examination, she said because she was mixed with wrong friends who did not listen. In 2019, Zanele had a boyfriend who was in University. She told us that she had started having sex with her boyfriend, but she had not wanted to have sex. She said she did it because ‘girls are overpowered by boys in relationships.’ Her boyfriend was not working but he supported her financially when he had money and he had promised that he will ‘make things right’ and marry her when he had completed studying.
Social contacts which affected functioning of AYP also comprised cross generational relationships and negative peer influences.
Cross generational relationships:
Being involved with “blessers” (cross-generational partnerships in exchange for money and/or material goods) or “boys in cars” was perceived to increase HIV-related risk and non-use of health services due to fear of being found out. According to participants, being involved with blessers was common in their communities, particularly among AGYW who were looking for money to buy drugs and alcohol, those whose families were unable to provide necessities such as toiletries and food, and those who wanted money for other things, including clothes. Even though involvement with blessers was reported as common in both IDIs and GDs, none of the female participants reported having been in a cross-generational relationship themselves. Participants distanced themselves from this contextually based marginalized identity of a “blessee”:
even here [in this community] around they do date, there is no need to go faraway but even here around. You would find him [a blesser] parking a car and waiting for a young person, they would stay chatting in the car and the young person [blessee] will come out with nice things, (a female participant in a GD).
Whilst it was mentioned as something common in the community, it was also forbidden behaviour and therefore difficult for AYP to discuss or seek support.
Negative peer influence:
Additionally, some participants mentioned being exposed to friends who endorsed risk, could not provide support, advice and peer counselling. Young men said some friends encouraged experimenting with drugs and alcohol and having unprotected sex. An 18-year old female said:
I made the wrong decisions, I met with my friends, wrong people. They said let us involve ourselves in drugs. It got too much for me and I stopped. I was drinking alcohol […].
AGYW reported that peer pressure resulted in early sexual debut, as expressed by a 19-year-old male, ‘Yes, I can say there are risks, you hang up with the wrong people and you end up doing the same thing as they are’. Participants also reported that negative influence and distractions, like in Zanele’s case influenced not doing well at school.
Intergenerational transmission of adolescent sexual norms:
Participants descriptions illustrated the dominance of gendered sexual norms in their communities. Norms in which men should take full control of relationships and sexual activity and women should hold off having sex until they were old or had “reached age 21”, finished secondary or tertiary education, were working or if they had met a right partner to get married to. While ABYM narrated stories of sexual encounters and freedom, AGYW expressed wanting to protect themselves from pregnancy and STIs. Young men often communicated narratives related to sexual pleasure and young women, expressed self-judgement in relation to sexual engagement, ‘a young girl must take care of herself until the age of 21, it is then that she can be free to get a child’ (10-year-old female, interview), driving shame, fear of censure and poor engagement with SRH care, particularly for AGYW. Younger participants who were in primary school said they were not involved in sexual activities and did not contribute their experiences on such discussions.
Most AGYW discussed sexual-related matters with their peers and some said they discussed with older female siblings, grandmothers and their mothers. For AGYW, discussing sexual matters with peers was easier. In an interview, one 18-year-old female said, ‘you speak to your peers only. You can’t just ask such things (sexual matters) from an elder, you see’. ABYM discussed sexual matters with peers and uncles in their families as shown in this quote from a 19-year-old male ‘I normally talk with my friends and my older brothers who are of course not my age’. A few ABYM said they discussed with their parents.
Protective Factors
Individual characteristics that enhance engagement
Protective factors associated with individual characteristics included personal attributes which supported engagement with HIV prevention interventions and SRH care. During our first encounter with Vusi, a 21-year-old male who had finished secondary school, we learned that his parents did not have money to send him to a tertiary institution where he could pursue his studies, but they supported him to get employment and make something out of his life. He spent a lot of his time in his home, read a lot around issues that affect young people from books he got from his local library and was interested to talk to the research team about his experiences in his community as a young person. He told us that he was aware of HIV prevention interventions in his community and aware of health care services offered at the clinic. Even though he told us that ‘I am scared to discuss sexual health with old people, I will never even talk to my mother’, he did get a lot of information at his local clinic and he used to get information from school when he was still in school. Vusi had a positive outlook in life. In our third interview in 2019, he told us that he was going to leave his home to look for employment in Mpumalanga province, 517 kilometres away from his home. He said in Mpumalanga there were several prospects in mining which he could pursue even though he did not have any formal training.
Accurate and appropriate HIV/SRH-related information:
An ability to link to care was seen as important and participants said that being taught about different treatment and prevention approaches, including approaches for HIV testing, circumcision, contraceptives and STI treatment allowed them to appreciate sexual encounters and make better and informed decisions.
Participants who were still in school (age 10–20), were more likely to receive information and be engaged in interventions through DREAMS. Commonly received information was related to the ABC-Àbstain, condomise, be faithful strategy’, HIV testing and treatment, circumcision and curriculum-based interventions which focused on AGYWs’ behaviour modification. ABYM said that they mostly engaged in medical male circumcision, one male participant in discussion shared that ‘there are a lot of boys who circumcise, even those at the young age of 13 years get circumcised’. They reported that circumcision protected them from HIV and other STIs and that circumcision was offered together with HIV testing. AGYW mostly engaged in curriculum-based interventions offered through DREAMS said that they were taught to “behave well” and some were linked to primary health care settings where they were offered HIV testing, contraceptives and were also taught to “become responsible and stay in school”. Even though condoms were widely available, distributed in local food trading shops and in primary health care settings, both young women and men said condom use had decreased among young people because of the high rate of teenage pregnancy they witnessed in their communities. Young men said they could not enjoy sex when using condoms and young women feared to collect condoms due to social disapproval of young unmarried women accessing condoms.
Remaining in school and furthering education:
Participants praised AYP who stayed in school. Perceived benefits of staying in school included being protected from risky behaviour such as drinking alcohol. Other benefits included having a better future with financial stability. One of the examples was captured in an interview with a primary school learner, ‘education is your future and your life, because if you are not educated you will not get employment, you will not become what you want to become and you may end up getting HIV’. Most participants aspired to finish school and enrol in tertiary institutions to become “doctors, pilots, nurses, lawyers or engineers”. However, many of their aspirations were unrealistic and not concrete plans. Participants lacked knowledge of chosen careers and the institutions where they could enrol. Greater emphasis was placed on combating poverty in their families in the form of “finishing school”, “working” and “being able to take care of their families”. Many felt that financial stability was important to improve lives of young people in the community. Having a good and secure life where they were able to pursue a good livelihood was viewed as important. Even though adversity was acknowledged, AYP were motivated to change their unfavourable circumstances.
Support Factors
Community solidarity and consistent interventions supported AYP around health-related resources as narrated by Mzwandile. He told us that there were no conflicts in his community, and he felt safe. He was 22 years of age and was out of school. Even though some young people in his community drank alcohol and used other drugs, he did not drink and did not smoke. He said he found solid support within his family. His brother was the first person he went to when he encountered problems. If his brother could not assist him, the problem will be reported to his father who will come up with solutions. He lived with both his parents and his siblings. He said, ‘because I am a male, I report my health problems to my father and brother’. He did this because he thought they would understand better than his mother would because they were also males and probably had gone through the same things that he was going through as a young man. His brother and father provided him with sexual health education and he also visited the clinic to test for HIV. He told us that he knew he should use condoms when having sex and he did that all the time.
Community cohesion and consistent interventions:
Networks which included institutions (such as police and health services as well as schools) and broader community solidarity and consistent interventions were regarded as important protective factors as they encouraged AYP to access and use HIV and SRH services. In addition to family members, teachers also played a role in disciplining children who were “hanging out with boys in cars”. Values such as hope, religion and rituals were mentioned by participants as playing a role in reducing risk factors. Participants who lacked hope, felt that they would not have community and health facility support and those who expressed that they would not have “normal” sexual relationships were scared to test and were also scared of being diagnosed with HIV. This suggested that if they managed to test, they would have challenges linking to care and receiving appropriate support because of perceived absence of support and perceived stigma. Generally, AGYW reported having support from schoolteachers and most had been to a health facility over the past year for primary health care, however services mentioned did not include SRH.
Few ABYM had visited a health facility, generally they said, ‘I don’t get sick’ or ‘when one is sick, he fears that people will think that he is sick’. A few who had been to the health facility had been encouraged by their mothers or other family member, ‘it was my mother who took me to clinic, so now it’s the first thing in mind when I’m sick to do’ (19-year-old male, interview). This reflected caring and modelling care-seeking behaviour from parents and carers at home.
Consistent community-based interventions, including HIV testing, condom distribution, and VMMC were received positively by AYP. Participants reported that these interventions were acceptable and to some extent accessible as they did not have to go to health facilities to access them.
Models who promote prosocial behaviour
Social capital included networks or relationships which enabled effective functioning of AYP. Nobuhle (aged 15 years) lived with her uncle and siblings, her mother got married and moved to a nearby community where she lived with her husband. She had never visited her mother, she said ‘I do not have courage to visit her there because she is married now’. When we first met her she had said that she was not sexually active and she said she did not know whether having unprotected sex was good or bad as ‘young girls have sex to prove to their partners that they loved them’. She told us that when she had questions around relationships and sex, she asked her friend’s mother who was very open and was able to tell them about what they should and should not do to stay protected from STIs and not fall pregnant. Nobuhle became pregnant and when we visited her for the third time, her baby was 10 months old. She said that her family was supportive, she had someone who looked after her baby when she was at school. Even though her mother was married and did not live with her, she supported her financially and emotionally as they talked on the phone regularly. Nobuhle was happy to have support from her family and she felt she was able to access health care for herself and her baby from a local clinic and nurses treated her well.
Family:
Relationships that facilitate the ability to cope and engage with interventions included supportive relations with family. The family unit played an important role in making AYP feel safe and protected and provided a place of belonging and support for health access and care. A family unit might be made up of different combinations: parents, grandparents, aunts, uncles, siblings and cousins. Participants said that young people who had meaningful relationships with older adults, who felt safe and cared for, had someone who they trusted and shared common norms and values with, were less likely to contract HIV because they had close connections which helped them to get by, ‘I have realised that this is a good place because I have my aunt and we are Christians here, everything is good, the clinic and the school is closer, there is nothing that will worry me’ (15-year-old-female, interview).
Positive peer networks:
According to participants, support from peers led to the rise of VMMC uptake, particularly for ABYM who were still in school and had easy access to this service. In an interview, a 25-year-old male said:
it was due to my friends that I got to circumcise, and they said that if you’re not circumcised you are not a man. There was also that saying which was going around about how better one becomes in bed when they are circumcised… we wanted to experience all that.
In addition to the positive influence from peers, the narrative also provides a nuanced picture of adolescents’ desires and their dilemmas through which sexuality is experienced. It reveals sex as something pleasurable that adolescents want to enjoy as opposed to the common silence, risk and shame surrounding adolescent sexuality. When they were with their peers, they were able to express their sexual desires, something they said was not easy to do at home and with other older people, often leading to secrecy around sex, SRH and HIV which potentially led to non-use of services. Younger participants reported more support from family and peers, while older participants reported support from peers and siblings.
Discussion
Contextual, social and individual level factors increasing the probability of engaging in risk behaviours for AYP in this context included: difficulties of navigating their relationships with interventions and health services in a setting where they face a rise in youth unemployment; mobility; a decline of stable family structure; and gender inequalities that drive risk. Opportunity risk factors presented by AYP’s context such as stigmatised and moralised HIV and SRH are not just health-related issues, but also social and cultural ones. Together these have huge consequences around how AYP safely and confidently navigate love, social relationships, and pleasure as part of growing up. Our in-depth study shows that under similar adverse conditions and vulnerability, AYP with high levels of protective factors, including peer models for prosocial behaviour and an intolerant attitude towards deviance are more likely to be resilient and engage with health and social interventions provided, in this case through the DREAMS partnership.
Narratives of AYP suggested that important protective factors moderating the impact of exposure to risk include accurate HIV and sexual health-related information. Moreover, supportive families and carers, strong and positive peer networks and access to safe and supportive adults enables AYP to navigate environments and institutions such as health care settings. However, these protective factors are juxtaposed by multiple and intersecting forms of discrimination and gender inequality which affects the lives of AYP and increases their vulnerability to HIV and other STIs. These manifest in a multitude of risk that adolescents face as they transition into adulthood. Such findings illustrate the influence on young people’s engagement with SRH services and interventions, not only from their individual characteristics, such as health-information, but also the broader social environment which includes significant others as well as broader societal influences within which different interventions, individuals and social environments are embedded.
During the implementation of DREAMS, AYP demonstrated a high individual awareness of biomedical interventions. The delivery of interventions within the community strengthened convenience and access as most of these interventions afforded AYP the privacy they required, away from public facilities where they felt judged and stigmatised (Zuma et al., 2019). Nevertheless, alcohol and transactional sex, as well as deep rooted negative social attitudes to female sexuality (and to a lesser degree young male sexuality) continued to be a barrier to SRH. The DREAMS intervention excluded mechanisms to respond to gender-related norms and the experience of sexuality for young women (Chimbindi et al., 2020). For young men, openness for male sexuality is acknowledged, and there is also pressure to have multiple partners and enjoy sex, also putting young men at risk. DREAMS enhanced information and knowledge of SRH services, however, young women remained constrained by power relations between men and women and DREAMS reduced its impact by leaving out young men in curriculum based education which also focused on dispelling gender-norms (Zuma et al., 2019). Although DREAMS implemented a cash transfers intervention to respond to some of the gender dynamics, by limiting engagement of young men, this intervention did not directly respond to the gendered nature of risks that drive HIV infection among AYP (Chimbindi et al., 2020).
A report by (Jessor, 1991) suggests that under similar conditions of high risk, AYP with high levels of protective factors, including peer models for prosocial behaviour and an intolerant attitude towards deviance are more likely to be resilient. Special attention is therefore needed to assess the development of socially responsible behaviour in AYP. For example, it is important to establish what influences sexual identity and who influences AYP’s values and beliefs. Interventions that address HIV risk behaviours in the context of adolescent transition to adulthood may have a great impact in preventing the spread of HIV and other STIs in this community.
Sexual behaviour remains strongly gendered, and sexual activity has different meanings for gendered identities. For example, uptake of HIV and SRH services have been shown to be influenced by different constructions of masculine identities based on ‘reputation’ and ‘sexual potency’ (Siu, Seeley, & Wight, 2013). It will be important to further explore how to deliver sex and sexuality messaging and interventions in a context where there is tension between perceived and actual sexual norms, and where sexual encounters for AYP are often unplanned.
Our findings suggest different levels of protective factors that could help AYP overcome some of the barriers. At the level of positive peer models these include peer support, supporting families and caregivers in provision of continuous care. At the individual- or social-environment level these include positive social norms, accurate health information and safe environments. At the contextual or other social environment level these include strengthened institutional support, such as schools and non-judgemental accessible health care. Protecting factors mentioned above could be in the form of improved provisioning of healthcare facilities, safe environments, including schools, psychological and social support, and access to medical treatment and HIV-related information, supported by participatory intervention design involving AYP.
Social protection has been reported to have the potential to interrupt risk pathways to HIV infection and offer protection to AYP (Toska et al., 2016). Literature indicates that social protection might reduce the social and economic drivers of HIV risk, improve utilization of prevention technologies and improve adherence to ART for AYP (Cluver et al., 2015). Further examples of protective factors include gendered HIV testing and treatment strategies, provision of HIV-related education and changing patterns of HIV-related stigma (Delany‐Moretlwe et al., 2015; Dovel, Yeatman, Watkins, & Poulin, 2015). These strategies could be used in combination with each other to offset risk, foster accurate and consistent SRH use for both male and female AYP and build youth capacity, involvement and leadership (Cluver et al., 2018; Denison et al., 2017). Findings from this study did not affect how DREAMS interventions were rolled out, however, they highlight how individual, structural and contextual factors may influence engagement with interventions and they provide lessons for how similar interventions may be implemented in the future.
Strengths and limitations
IDIs were repeated with the same participants, strengthening the quality of the relationship that developed with participants over time and fostered understanding of shifting realities. Moreover, the process provided the researcher an ability to seek clarification or additional information about issues raised in earlier interviews in order to capture experiences and perceptions over time. Issues raised in IDIs and group norms were clarified in GDs.
Using both IDIs and GDs, we could not determine how protective factors support AYP from surviving risk and adapting successfully to instabilities that threaten their daily functioning. Future studies should look at the processes for understanding the interplay between protective factors and AYP’s successful adaptation to instabilities in their communities. The HIV status and prevalence of STIs among participants was unknown, and none of the participants disclosed their status. Therefore, we could not show how AYP are directly affected by HIV/STI-related consequences, more research is needed to understand these direct links. More research is also needed to understand how different protective factors, including those in the community (families, peers, community-based interventions) in organisations and institutions such as schools, health care facilities and police services, can partner to develop systems of support and address changes needed in the social context for AYPs wellbeing.
Conclusions
Findings from this study support the need to recognise the many ways in which adolescents and youth harness social protection and resilience through their engagement with their peers, caregivers and institutions, and the dynamic nature of their lives during adolescence and young adulthood as well as the multiple challenges they face. We need combination interventions that harness and strengthen peer support to engage with the social norms and rewrite the narrative of love and relationships in the time of HIV.
Acknowledgements
The authors are grateful, to the communities of the Hlabisa sub-district who contributed their data to this study, to AHRI staff who collected the data in this study – Sakhile Mdluli, Lindiwe Sibiya, Mxolisi Nhlenyama, Penrose Mthethwa, Mpilonhle Nzuza, Khayelihle Mngomezulu, Nqobile Ntombela, and Nondumiso Mpanza, the DREAMS P & P group who reviewed the abstract and the DREAMS project management group who reviewed the paper.
Funding
AHRI is supported by a grant from the Wellcome Trust (082384/Z/07/Z). The research leading to these results has received funding from National Institutes of Health grant (5R01MH114560–03) and the Bill and Melinda Gates Foundation (OPP1136774). NMcG is a recipient of an NIHR Global Health Research Professorship award (Ref: RP-2017–08-ST2–008).
Biography
Thembelihle Zuma* PhD (Public Health) masters (Research Psychology), is a Research Scientist at the Africa Health Research Institute’s Social Science and Research Ethics Department. She is involved in developing and supporting peer led interventions focusing on sexual health promotion and peer-mentorship to navigate resources and improve retention in HIV care among adolescents and young people. Her research interests combine public health, health promotion and health literacy, with a focus on how community-based participation in health promotion and health literacy can function as a progressive force on the road towards enabling community members to make informed health choices to manage their wellbeing. She has managed multiple social science studies in the field of HIV and sexual and reproductive health in rural communities.
Janet Seeley is a social anthropologist by training with 35 years of research and development experience working on the social aspects of health. She is Professor of Anthropology and Health at the London School of Hygiene and Tropical Medicine, and faculty lead for Social Science and Research Ethics at the Africa Health Research Institute, KwaZulu-Natal, South Africa.
Sakhile Mdluli has an Honors Degree in Development Studies. At the time of the study, he worked as a Senior Social Science Research Assistant under the Department of Social Science and Research Ethics at the Africa Health Research Institute. He is interested in working with young people.
Dr Natsayi Chimbindi is an early-career post-doctoral researcher working with adolescents and young people in HIV-prevention, in a high HIV-burden rural area in KwaZulu-Natal South Africa. She is currently working as a research programme manager for the HIV prevention programme at the Africa Health Research Institute (AHRI) in South Africa, leading on major mixed-method evaluation and development of complex HIV prevention interventions among young people at AHRI including: the impact evaluation of MTV Shuga and the PEPFAR-funded Determined Resilient Empowered AIDS-free Mentored and Safe (DREAMS) HIV prevention interventions targeted at adolescent girls and young women (AGYW) rolled-out in the district in KwaZulu-Natal, South Africa, and development of interventions to improve uptake and retention in a multilevel HIV-prevention programme. Her research interests are in developing a theoretically derived intervention to deliver sexual health and HIV prevention interventions in schools.
Nuala McGrath is Professor of Epidemiology and Sexual Health and NIHR Global Health Professor at the University of Southampton. Evaluating HIV treatment and prevention strategies including the promotion of HIV testing to reduce the onward transmission of HIV in sub-Saharan Africa is a critically important and long-standing theme of her work. Her work also explores the value of couples-focused behaviour change strategies for health intervention research and practice in sub-Saharan Africa. https://www.southampton.ac.uk/medicine/about/staff/nmm1c12.page
Sian Floyd is an Associate Professor in Medical Statistics and Epidemiology, in the Department of Infectious Diseases Epidemiology at the London School of Hygiene & Tropical Medicine. Her research focuses on HIV and tuberculosis in sub-Saharan Africa
Isolde Birdthistle, MSc PhD, is Associate Professor of Epidemiology and Adolescent Health at the London School of Hygiene & Tropical Medicine. She leads a portfolio of studies to generate evidence of ‘what works’ to prevent HIV and promote the health of young women. This includes impact evaluations of complex interventions, like DREAMS in multiple settings, and mass media campaigns to boost demand for HIV technologies like self-testing and PrEP. She previously worked in adolescent health promotion programmes with the World Health Organisation, UNICEF, Harvard School of Public Health, and the MIT Media Lab.
Guy Harling is a Wellcome Trust/Royal Society Sir Henry Dale Senior Research Fellow in the Institute for Global Health at University College London. His research focuses on the social determinants of health in sub-Saharan-Africa. Much of this work focuses on how social networks affect sexual behaviour and risk of HIV/STI acquisition in adolescents and young adults. Guy also investigates how social interaction and support is related to cognitive health in older adults and conducts methodological research on how to improve data collection and account for imperfect data collection during analysis. He holds undergraduate and masters degrees in Economics, a masters in public health and a doctorate in health-related social and behavioural sciences.
Professor Lorraine Sherr is a Prof of Clinical and Health Psychology at University College London. She is the editor of three international journals (AIDSCare, Psychology Health and Medicine and Vulnerable Children and Youth Studies). She is co-director of the GCRF Hub on Accelerating achievements for Africa’s adolescents
Maryam Shahmanesh is an Associate Professor at the University College London Institute for Global Health, (Hon) Consultant in HIV and Faculty of the Africa Health Research Institute. She was appointed as a consultant physician in sexual health and HIV medicine in October 2012. She has a PhD in clinical epidemiology, who brings expertise in working in the interdisciplinary space between social science, clinical research and epidemiology. Following a promising early academic career, supported by a Wellcome Trust Clinical Fellowship, a NIHR (Walport) clinical lectureship, and a US National Institute of Health early investigator R01 award, she has gone on to lead a large interdisciplinary programme to develop and evaluate complex interventions to reduce HIV and improve the sexual health of adolescents and young adults living in rural KwaZulu-Natal, South Africa. She also leads a large postgraduate teaching portfolio at UCL.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors
Data availability statement
The datasets generated for this study are available on request to the Africa Health research Institute through the corresponding author.
References
- Baxter C, & Abdool Karim S (2016). Combination HIV prevention options for young women in Africa. African Journal of AIDS Research, 15(2), 109–121. [DOI] [PubMed] [Google Scholar]
- Birdthistle I, Tanton C, Tomita A, de Graaf K, Schaffnit SB, Tanser F, & Slaymaker E (2019). Recent levels and trends in HIV incidence rates among adolescent girls and young women in ten high-prevalence African countries: a systematic review and meta-analysis. The Lancet Global Health, 7(11), e1521–e1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond V, Ngwenya F, Murray E, Ngwenya N, Viljoen L, Gumede D, . . . Dodd PJ (2019). Value and limitations of broad brush surveys used in community-randomized trials in Southern Africa. Qualitative Health Research, 29(5), 700–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chimbindi N, Birdthistle I, Floyd S, Harling G, Mthiyane N, Zuma T, . . . Shahmanesh M (2020). Directed and target focused multi-sectoral adolescent HIV prevention: Insights from implementation of the ‘DREAMS Partnership’ in rural South Africa. Journal of the International AIDS Society, 23(S5), e25575. doi: 10.1002/jia2.25575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chimbindi N, Mthiyane N, Birdthistle I, Floyd S, McGrath N, Pillay D, . . . Gareta D (2018). Persistently high incidence of HIV and poor service uptake in adolescent girls and young women in rural KwaZulu-Natal, South Africa prior to DREAMS. PloS one, 13(10), e0203193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cluver L, Hodes RJ, Sherr L, Mark Orkin F, Meinck F, Lim Ah Ken P, . . . Vicari M (2015). Social protection: potential for improving HIV outcomes among adolescents. Journal of the International AIDS Society, 18, 20260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cluver L, Orkin M, Campeau L, Toska E, Webb D, Carlqvist A, & Sherr L (2018). Improving Lives by Accelerating the Sustainable Development Goals for Adolescents Living with HIV. Available at SSRN 3258671. [DOI] [PMC free article] [PubMed]
- Delany‐Moretlwe S, Cowan FM, Busza J, Bolton‐Moore C, Kelley K, & Fairlie L (2015). Providing comprehensive health services for young key populations: needs, barriers and gaps. Journal of the International AIDS Society, 18, 19833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denison JA, Pettifor A, Mofenson LM, Kasedde S, Marcus R, Konayuma KJ, . . . Pulerwitz J (2017). Youth engagement in developing an implementation science research agenda on adolescent HIV testing and care linkages in sub-Saharan Africa. AIDS, 31(Suppl 3), S195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health. KZN HEALTH 2017/18 BUDGET SPEECH. Retrieved from www.kznhealth.gov.za/speeches/2017/Budget-Speech-Booklet2017-2018
- Dovel K, Yeatman S, Watkins S, & Poulin M (2015). Men’s heightened risk of AIDS-related death: the legacy of gendered HIV testing and treatment strategies. AIDS, 29(10), 1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis SC, Mthiyane TN, Baisley K, Mchunu SL, Ferguson JB, Smit T, . . . Mutevedzi T (2018). Prevalence of sexually transmitted infections among young people in South Africa: A nested survey in a health and demographic surveillance site. PLoS Medicine, 15(2), e1002512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jessor R (1991). Risk behavior in adolescence: a psychosocial framework for understanding and action. Journal of Adolescent Health. [DOI] [PubMed] [Google Scholar]
- Jessor R, Turbin MS, Costa FM, Dong Q, Zhang H, & Wang C (2003). Adolescent problem behavior in China and the United States: A cross‐national study of psychosocial protective factors. Journal of Research on Adolescence, 13(3), 329–360. [Google Scholar]
- Kielmann K, Cataldo F, & Seeley J (2012). Introduction to qualitative research methodology: a training manual. Retrieved from Bangalore, India: [Google Scholar]
- Lee TY, Cheung CK, & Kwong WM (2012). Resilience as a positive youth development construct: a conceptual review. The Scientific World Journal, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leshem R (2016). Brain development, impulsivity, risky decision making, and cognitive control: Integrating cognitive and socioemotional processes during adolescence—An introduction to the special Issue: Taylor & Francis. [DOI] [PubMed] [Google Scholar]
- Meinck F, Cluver LD, Boyes ME, & Loening-Voysey H (2016). Physical, emotional and sexual adolescent abuse victimisation in South Africa: prevalence, incidence, perpetrators and locations. Journal of Epidemiology and Community Health, 70(9), 910–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, . . . Bonell C (2016). Our future: a Lancet commission on adolescent health and wellbeing. The Lancet, 387(10036), 2423–2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saul J, Bachman G, Allen S, Toiv NF, Cooney C, & Beamon TA (2018). The DREAMS core package of interventions: a comprehensive approach to preventing HIV among adolescent girls and young women. PloS one, 13(12), e0208167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siu GE, Seeley J, & Wight D (2013). Dividuality, masculine respectability and reputation: How masculinity affects men’s uptake of HIV treatment in rural eastern Uganda. Social Science and Medicine, 89, 45–52. [DOI] [PubMed] [Google Scholar]
- Strauss M, Rhodes B, & George G (2015). A qualitative analysis of the barriers and facilitators of HIV counselling and testing perceived by adolescents in South Africa. BMC Health Services Research, 15(1), 250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanser F, Hosegood V, Bärnighausen T, Herbst K, Nyirenda M, Muhwava W, . . . Newell M-L (2007). Cohort Profile: Africa centre demographic information system (ACDIS) and population-based HIV survey. International Journal of Epidemiology, 37(5), 956–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanser F, Hosegood V, Benzler J, & Solarsh G (2001). New approaches to spatially analyse primary health care usage patterns in rural South Africa. Tropical Medicine and International Health, 6(10), 826–838. [DOI] [PubMed] [Google Scholar]
- Tomita A, Vandormael A, Bärnighausen T, Phillips A, Pillay D, De Oliveira T, & Tanser F (2019). Sociobehavioral and community predictors of unsuppressed HIV viral load: multilevel results from a hyperendemic rural South African population. AIDS, 33(3), 559–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toska E, Gittings L, Hodes R, Cluver LD, Govender K, Chademana KE, & Gutiérrez VE (2016). Resourcing resilience: social protection for HIV prevention amongst children and adolescents in Eastern and Southern Africa. African Journal of AIDS Research, 15(2), 123–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF. (2017). Children and AIDS: Statistical Update URL: https://data.unicef.org/wp-content/uploads/2017/11. HIVAIDS-Statistical-Update-2017. pdf [accessed 2019–02-19][WebCite Cache].
- Ward C, Makusha T, & Bray R (2015). Parenting, poverty and young people in South Africa: What are the connections. South African Child Gauge, 69–74. [Google Scholar]
- Zuma T, Seeley J, Sibiya LO, Chimbindi N, Birdthistle I, Sherr L, & Shahmanesh M (2019). The changing landscape of diverse HIV treatment and prevention interventions: experiences and perceptions of adolescents and young adults in rural KwaZulu-Natal, South Africa. Frontiers in Public Health, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated for this study are available on request to the Africa Health research Institute through the corresponding author.


