Abstract
Objectives:
Mental stress-induced myocardial ischemia (MSIMI), a transient myocardial ischemic response to mental stress, is associated with poorer outcomes among patients with coronary heart disease (CHD) and is more likely to occur among women. Yet, predictors of MSIMI are not well explored. The current study investigated the association between experiences of everyday discrimination and MSIMI among patients with recent MI and contrasted the results with conventional stress-induced myocardial ischemia (CSIMI). We examined sex differences in associations.
Methods:
We studied 295 post-MI patients (145 women, 150 men). Provocation of myocardial ischemia with mental stress (speech task) and conventional stress (exercise or pharmacologic) was assessed by myocardial perfusion imaging. Frequency of exposure to everyday discrimination was assessed via questionnaire using the Everyday Discrimination Scale (EDS).
Results:
The mean age was 51 years in both women and men, and the EDS score ranged from 10 to 38 (mean 17; SD 6). After multivariable analysis, each standard deviation increase in EDS score (more frequent exposure) was associated with an increased odds of MSIMI (OR=1.57 [1.10 – 2.23]). EDS score was not associated with CSIMI (OR=0.86 [0.64 – 1.17]). Women demonstrated a two-fold increase (OR=1.96 [1.13 – 3.38], p=0.02) in the adjusted odds of MSIMI with each standard deviation increase in EDS score compared to a 1.4-fold increase (OR=1.40 [0.80 – 2.44], p=0.24) among men; however, interaction was not statistically significant.
Conclusions:
Among post-MI patients, everyday discrimination was positively associated with occurrence of MSIMI, but not with CSIMI; associations were more pronounced among women.
Keywords: Coronary artery disease, Mental-stress induced myocardial ischemia (MSIMI), myocardial infarction (MI), Social Determinants of Health, Social Discrimination, Women’s Health
Introduction
Mental stress-induced myocardial ischemia (MSIMI) is a transient myocardial ischemic response to mental stress. MSIMI has been observed in anywhere from 15% to 70% of patients with pre-existing coronary artery disease (CAD) (1). Similar to ischemia induced by conventional (exercise) stress tests, MSIMI is associated with a doubling of recurrent events and mortality among patients with CAD; however, unlike conventional (exercise) stress-induced myocardial ischemia (CSIMI), MSIMI occurs at a lower workload (i.e., lower heart rate, lower stroke volume), is largely independent of underlying CAD severity, and is usually silent (1–4).
Previous studies among patients with recent myocardial infarction (MI) and stable coronary heart disease (CHD) have shown that women are more likely to develop MSIMI compared to men, with only a modestly higher risk of CSIMI among women (5, 6). In fact, it has been suggested that MSIMI may be a potential mechanism explaining worse morbidity and mortality after MI among women, particularly young women (2, 7). There is growing evidence that the dominant mechanism driving MSIMI among women is not underlying CAD severity but microvascular dysfunction and peripheral vasoconstriction, for which women are particularly vulnerable, however other factors likely play a role (2, 8, 9). Yet, there has been limited research on the predictors of MSIMI overall and among young women in particular.
A number of psychosocial factors related to stress – including depression and state and trait-anger – have been associated with higher risk for MSIMI (10–12). Not only are women more likely to experience psychosocial risk factors, they are potentially at higher risk of adverse cardiovascular consequences as a result of these factors (13). One psychosocial factor that may have particular relevance for women with MI is discrimination. Discrimination – unfair treatment based on group identity – is disproportionately experienced by members of groups that have historically been oppressed, marginalized, and disenfranchised, and young women with MI are more likely to be low income and Black than their male counterparts (14–16). There is an increasing body of evidence linking exposure to discrimination, conceptualized as a form of psychosocial stress, with physical health outcomes (17, 18). Several studies have identified associations between self-reported discrimination and cardiovascular disease (CVD) risk factors (i.e., hypertension, visceral fat, and atherosclerosis), inflammatory markers (i.e., C-reactive protein, interleukin-6), and incident CVD (19–23). However, most of these studies have focused on healthy populations, and, to our knowledge, no studies have examined the association between discrimination and MSIMI. Investigating discrimination in patients with recent MI is particularly important as this is a high-risk group that may be subject to discrimination not just in everyday settings, but in their more frequent interactions with the healthcare system.
The current study seeks to investigate the association between self-reported discrimination and MSIMI in a population of young and middle-aged survivors of MI. This is an important group to study as previous studies have found that young and middle-aged, but not older, women have higher mortality and complication rates after an MI compared with men of similar age (24, 25). Additionally, disparities in MSIMI between women and men with CHD were only found in younger patients (26). We used CSIMI as a control condition. We also examined differences in these associations by sex. Our hypothesis was that there would be an association between discrimination and MSIMI but not with CSIMI due to the hypothesized mechanisms through which emotional stressors trigger ischemia. Additionally, we hypothesized that discrimination will be more strongly associated with MSIMI among women compared to men, independent of sociodemographic and clinical risk factors.
Methods
Study Design
Study participants were patients with a previous MI who participated in the Myocardial Infarction and Mental Stress 2 (MIMS2) study. The protocol has been described before in detail (2). Participants with a documented history of MI in the previous eight months were recruited from the pool of patients admitted at Emory-affiliated hospitals in Atlanta, Georgia. MI case diagnosis was verified with medical record review based on standard criteria of troponin level increase, symptoms of ischemia, and changes in the electrocardiogram (ECG) or other evidence of myocardial necrosis. Inclusion criteria included being 18 to 60 years of age at the time of recruitment; presence of obstructive CAD was not required for inclusion. Each participant underwent a two-day protocol that included a blood draw, measured height and weight, and clinic tests of myocardial perfusion imaging following rest and mental and conventional stress procedures. A research nurse obtained sociodemographic, medical history and medication information, and participants completed questionnaires on behavioral, social, and health status information. Data for this study were collected between June 2011 and March 2015. The Emory University Institutional Review Board approved the protocol and all participants provided written informed consent.
Study Participants
Of the 313 MI cases, 14 were missing information on everyday discrimination and seven were missing information on MSIMI due to technical difficulties with testing. Thus, 295 participants were included in the analytic dataset. Those excluded from analyses had a mean single-photon emission computed tomography (SPECT) summed rest score of 7.8 (SD=7.6) compared to 3.7 (SD=6.3) among those included in analyses, indicating more resting perfusion defects among those excluded (p=0.0301). Also, those excluded were more likely to be in a higher income category compared to those included in analyses (p=0.0195). Otherwise, those excluded from analyses were not substantially different from those included in analyses (see Table S1, Supplemental Digital Content).
Study Procedures
Mental Stress Procedure
Participants underwent a standardized mental stress test (7). After 30 minutes of resting in a quiet, dimly lit, temperature-controlled room, participants were given two minutes to make up a realistic story in which a close relative had been mistreated in a nursing home and three minutes to tell the story in front of a video camera and audience wearing white coats. Participants were told laboratory staff would be evaluating this presentation for content, quality, and duration. Blood pressure and heart rate were taken every five minutes during the 30-minute resting phase and every minute during the five-minute mental stress phase. The radioisotope for nuclear imaging, Technetium-99 (99mTc ) sestamibi, was injected one minute after the start of the public speaking task.
Conventional Stress Procedure
Conventional stress testing took place on a separate day up to one week apart from the mental stress testing. This consisted of a standard Bruce protocol in which participants underwent treadmill exercise testing. The ECG, blood pressure and heart rate were continuously monitored. Once the participant attained 85% of their target heart rate, they were injected with a dose of 99mTc-sestamibi intravenously. Pharmacological stress testing with regadenoson was conducted among participants who were unable to exercise and 99mTc sestamibi was injected immediately after regadenoson injection. In our sample, 76% of men (N=112) and 66% of women (N=95) underwent exercise testing, and the remainder pharmacological stress testing. A physician was present during the study and the ECG and vital signs were continuously monitored.
Myocardial Perfusion Imaging
Three SPECT myocardial perfusion imaging scans were obtained: one at rest, one after mental stress, and one after conventional (primarily exercise) stress. Participants were scanned following injection of 99mTc sestamibi as described above, with a dose of 10 to 14 mCi for rest imaging and 30 to 40 mCi for stress imaging based on weight. Forty to 60 minutes after isotope injection, stress SPECT imaging was performed. Following standard nuclear cardiology protocols, antiischemic medications were withheld 24 hours before testing.
An experienced nuclear cardiologist performed visual interpretation of the imaging scans blinded to stress test type and other patient information. Each myocardial segment was scored from zero to four (zero = normal, one = possibly normal, two = definitely abnormal, three = severely abnormal, and four = no perfusion) which was used to create a summed stress score, summed rest score, and summed difference score (27). Presence of ischemia was defined as a summed difference score ≥3 for mental stress and ≥4 for exercise and pharmacological stress.
Measurement of Discrimination
The 10-item version of the Everyday Discrimination Scale (EDS) was used to assess exposure to everyday discrimination, or everyday occurrences of unfair treatment (28, 29). Sample items include being treated with less courtesy than other people, receiving poorer service than other people at restaurants or stores, etc… without reference to race, gender or any other characteristic. For each item participants expressed frequency of occurrence using a 4-point Likert scale (one = “often”, two = “sometimes”, three = “rarely”, four = “never”). Responses were summed and reverse coded for higher scores to represent more exposure to experiences of everyday discrimination, the resulting scores ranging from 10 to 40. The EDS has been widely used with good reliability and validity across racial/ethnic groups (30).
Other Study Measures
Demographic information included self-reported sex, race/ethnicity, age, educational attainment, and income. Educational attainment was assessed as years of education (continuous) and dichotomized by <12 years or ≥12 years. Household income was categorized (<$35K, $35-<$75K, ≥$75K). Body mass index (BMI) was calculated as measured weight divided by the square of measured height (kg/m2). Previous medical history information included history of clinical cardiovascular risk factors (smoking, diabetes, hypertension, high blood cholesterol), type of previous MI (ST-Elevation Myocardial Infarction [STEMI] v. Non-ST-Elevation Myocardial Infarction [NSTEMI]), and left ventricular ejection fraction.
Depression was also measured using a validated self-report instrument. The Beck Depression Inventory-II (BDI-II), a 21-item inventory widely used in cardiac and non-cardiac populations, was used to measure severity of depression symptoms.
Statistical Analysis
We calculated descriptive statistics for the sample by sex. We tested differences in these statistics by sex using chi-squared tests for categorical variables and t-tests for continuous variables. In order to examine the relationship between everyday discrimination and MSIMI (defined as the difference between summed rest and mental stress scores ≥3), and everyday discrimination and CSIMI (defined as the difference between summed rest and conventional stress scores ≥4), we ran generalized linear models with a logit link to derive odds ratios (OR) and 95% confidence intervals (CI) for MSIMI for each standard deviation increase in the EDS score. Covariates to be included in the models were considered a priori. Model 1 was adjusted for sociodemographic factors (race, sex, age, education, and income). Model 2 was further adjusted for cardiovascular risk factors (history of smoking, diabetes, hypertension, high blood cholesterol, and BMI) and indicators of previous MI severity (type of MI, ejection fraction, and SPECT imaging perfusion defects at rest). Model 3 further adjusted for depression symptom severity as this is a psychosocial factor often linked to discrimination and found to be a risk factor for MSIMI (12, 23, 31). While we considered a range of other potential mediators along with depression – including perceived stress, posttraumatic stress, and state and trait anger – depressive symptom severity was the most highly correlated with reports of everyday discrimination in a prior analysis from the MIMS2 cohort (32). Furthermore, we assessed sex differences with two methods: 1) we ran models 1–3 separately for men and women, and 2) examined interactions on the multiplicative scale by adding a product term to models with a logit link and on the additive scale by adding a product term to models with an identity link (33). All statistical analyses were conducted using SAS version 9.4.
Results
Table 1 shows descriptive characteristics of the analytic sample by sex. A greater proportion of women were Black (74.5%) compared to men (57.3%); the cohort primarily self-identified as either Black or White, with only 17 identifying as other (7% of men (N=11) and 4% of women (N=6)). Women also had lower income than men. Additionally, women had a higher prevalence of diabetes, a higher BMI, and a higher left ventricular ejection fraction. Women and men were comparable on reports of everyday discrimination (women: mean 16.6 (SD 6.1); men: mean 17.2 (SD 6.0)), but women had higher scores on depression symptom severity. During rest, women had lower summed perfusion defect scores than men (women: mean 2.9 (range 0–32); men: mean 4.4 (range 0–30)), denoting fewer perfusion defects at rest compared with men. However, women had similar though slightly lower summed perfusion defect scores during mental stress (women: mean 4.1 (range 0–38); men: mean 4.9 (range 0–32)) and conventional stress (women: mean 4.9 (range 0–38); men: mean 5.3 (range 0–30)) compared to men. Therefore, women had higher summed difference scores for both MSIMI (mean 1.2 (range 0–13)) and CSIMI (mean 2.1 (range 0–16)) compared to men (mean 0.59 (range 0–10), mean 1.2 (range 0–14), respectively), indicating that women experience a more severe change in perfusion defects resulting from mental and conventional stress compared to at rest than men.
Table 1.
Descriptive characteristics of participants stratified by gender among post-MI participants (N = 295) in the Myocardial Infarction and Mental Stress 2 Study (MIMS2).
| Women (n=145) | Men (n=150) | p-value | |
|---|---|---|---|
| Sociodemographic Factors | |||
| Black race, n (%) | 108 (74.5%) | 86 (57.3%) | 0.002 |
| Age, years, mean (SD) | 50.6 (7.3) | 51.1 (6.0) | 0.56 |
| Education ≥12 Years, n (%) | 85 (58.6%) | 89 (59.3%) | 0.90 |
| Income | |||
| <$35K | 78 (53.8%) | 61 (40.7%) | |
| $35 – <$75K | 35 (24.1%) | 38 (25.3%) | |
| ≥$75K | 23 (15.9%) | 37 (24.7%) | 0.02 |
| Clinical Risk Factors & MI Severity | |||
| History of Smoking, n (%) | 81 (55.9%) | 81 (54.0%) | 0.75 |
| History of Diabetes, n (%) | 55 (37.9%) | 40 (26.7%) | 0.04 |
| History of Hypertension, n (%) | 120 (82.8%) | 119 (79.3%) | 0.45 |
| History of High Blood Cholesterol, n (%) | 114 (78.6%) | 112 (81.3%) | 0.56 |
| BMI, kg/m2, mean (SD) | 32.3 (8.0) | 30.0 (5.8) | 0.004 |
| STEMI, N (%) | 38 (26.2%) | 48 (32.0%) | 0.27 |
| Ejection Fraction, %, mean (SD) | 53.0 (11.1) | 48.6 (12.5) | 0.002 |
| SPECT Summed Rest Score, mean (SD) | 2.9 (5.7) | 4.4 (6.8) | 0.04 |
| SPECT Summed Mental Stress Score, mean (SD) | 4.1 (6.7) | 4.9 (7.0) | 0.33 |
| SPECT Summed Physical Stress Score, mean (SD) | 4.9 (6.7) | 5.3 (7.2) | 0.57 |
| Psychosocial Factors | |||
| BDI Score, mean (SD) | 14.1 (11.1) | 10.6 (9.7) | 0.005 |
| Everyday Discrimination Score, mean (SD) | 16.6 (6.1) | 17.2 (6.0) | 0.88 |
| Myocardial Ischemia Severity Score | |||
| Summed Difference Score for Mental Stress, mean (SD) | 1.2 (2.4) | 0.59 (1.5) | 0.01 |
| Summed Difference Score for Exercise or Pharmacological Stress, mean (SD) | 2.1 (3.3) | 1.2 (2.6) | 0.006 |
Abbreviations: SD: Standard deviation; BMI: Body mass index; BDI: Beck Depression Inventory.
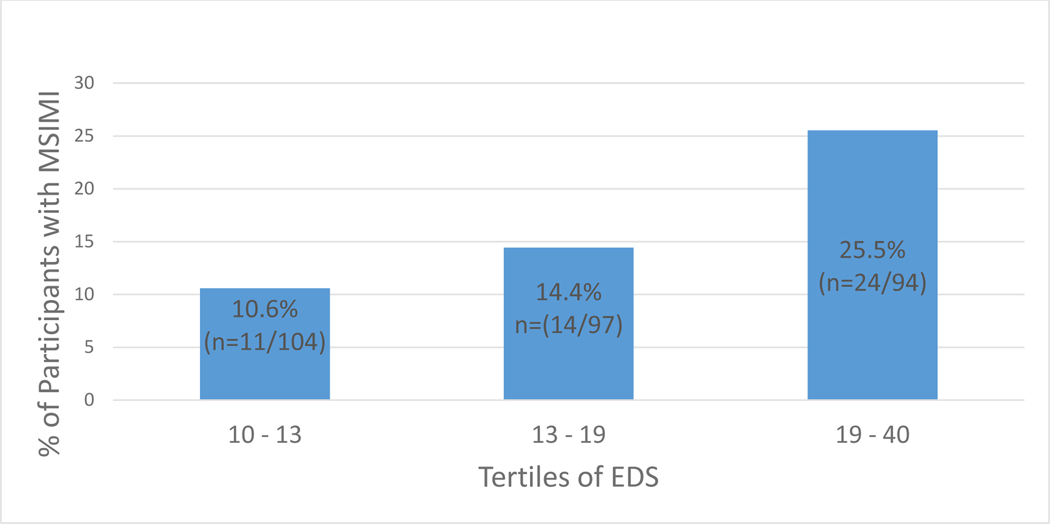
Of the 295 participants, 16.6% experienced MSIMI (N=49), with 18.2% of women (N=27) experiencing MSIMI and 14.7% of men (N=22). Although modeled continuously in all analyses, for descriptive purposes only we present the association between reports of everyday discrimination and the prevalence of MSIMI using approximate tertiles in Figure 1. From Figure 1 we see that as the everyday discrimination score increased, there was an increase in the proportion of participants experiencing MSIMI, showing a graded response. While approximately 11% of those in the lowest tertile of discrimination scores experienced MSIMI (N=11/104), 25% in the highest tertile experienced MSIMI (N=23/92).
Figure 1.
Percent of Participants with Mental Stress-Induced Myocardial Ischemia (MSIMI) by Tertiles of EDS with outliers removed (n=2); Abbreviations: MSIMI: Mental Stress-Induced Ischemia, EDS: Everyday Discrimination Score
Table 2 presents the results of the overall and sex-stratified models assessing the relationship between everyday discrimination and MSIMI, as well as results of interaction testing by gender. In the model adjusting for sociodemographic factors, the odds of MSIMI increased 1.4-fold (OR: 1.40, 95% CI: 1.07 – 1.83) for each standard deviation increase in the EDS score. This result was not fundamentally changed, after adjusting for cardiovascular risk factors and MI severity indicators, as well as depression symptom severity. Therefore, neither cardiovascular risk variables nor depression explained the association between discrimination and MSIMI.
Table 2.
Adjusted Association between Experiences of Everyday Discrimination (per 1-Standard Deviation in Total Score Increment) and Mental Stress Induced Myocardial Ischemia (N=295) in the Myocardial Infarction and Mental Stress 2 Study (MIMS2) Overall and By Sex.
| Interaction Assessment | |||||
|---|---|---|---|---|---|
| Model | Overall OR (95% CI) | Women OR (95% CI) | Men OR (95% CI) | Multiplicative p-value | Additive p-value |
| Adjusted for sociodemographic factors* | 1.40 (1.07 – 1.83) | 1.43 (1.00 – 2.04) | 1.36 (0.89 – 2.08) | 0.82 | 0.92 |
| Adjusted for the above plus cardiovascular risk factors and MI severity indicators** | 1.46 (1.08 – 1.98) | 1.70 (1.08 – 2.66) | 1.38 (0.85 – 2.25) | 0.56 | 0.62 |
| Adjusted for the above plus depression symptom severity*** | 1.57 (1.10 – 2.23) | 1.96 (1.13 – 3.38) | 1.40 (0.80 – 2.44) | 0.51 | 0.60 |
Race, age, educational attainment, income
History of smoking, diabetes, hypertension, and high blood cholesterol, BMI, type of MI, ejection fraction, SPECT summed rest score
Beck Depression Inventory score
In sex-stratified models, the association was more robust in women compared to men. In fully adjusted models, the OR of MSIMI in women was 1.96 (95% CI: 1.13 – 3.38) for each standard deviation increase in the EDS score; for men, the corresponding OR was 1.40 (95% CI: 0.80 – 2.44). However, formal testing for multiplicative and additive interactions indicated that the joint effect of everyday discrimination and sex was not greater than either the product or the sum of the individual effects, respectively.
Table 3 presents the results of the overall and sex-stratified models assessing the relationship between everyday discrimination and CSIMI, as well as results of interaction assessments. Both overall and sex-specific models did not provide evidence of a relationship between everyday discrimination and CSIMI.
Table 3.
Adjusted Association between Experiences of Everyday Discrimination (per 1-Standard Deviation in Total Score Increment) and Exercise or Pharmacologically-Induced Myocardial Ischemia (N=295) in the Myocardial Infarction and Mental Stress 2 Study (MIMS2) Overall and By Sex.
| Interaction Assessment | |||||
|---|---|---|---|---|---|
| Model | Overall OR (95% CI) | Women OR (95% CI) | Men OR (95% CI) | Multiplicative p-value | Additive p-value |
| Adjusted for sociodemographic factors* | 1.01 (0.79 – 1.28) | 1.03 (0.76 – 1.41) | 0.99 (0.66 – 1.48) | 0.62 | 0.51 |
| Adjusted for the above plus cardiovascular risk factors and MI severity indicators** | 0.95 (0.74 – 1.22) | 1.01 (0.72 – 1.42) | 0.91 (0.59 – 1.40) | 0.37 | |
| Adjusted for the above plus depression symptom severity*** | 0.86 (0.64 – 1.17) | 0.76 (0.49 – 1.20) | 1.02 (0.62 – 1.66) | 0.45 | 0.64 |
Race, age, educational attainment, income
History of smoking, diabetes, hypertension, and high blood cholesterol, BMI, type of MI, ejection fraction, SPECT summed rest score
Beck Depression Inventory score
Exploratory Analyses
Because the associations between everyday discrimination and MSIMI appear more robust in fully adjusted models with women relative to men, and the majority of women in our cohort were Black, we ran exploratory models examining the relationship between everyday discrimination and MSIMI among Black women in order to describe this association for this subgroup. Black women are the largest sub-group in this study and experience the most outcomes, and therefore we are able to appropriately examine the association of interest in this sub-group (unlike for non-Black women of which there were 37 in this sample, four of which experienced MSIMI). Of the 108 Black women included in analyses, 21.3% experienced MSIMI (N=23). After adjustment for sociodemographic and clinical risk factors, as well as depression symptom severity, the odds of MSIMI increased 2.5-fold (OR: 2.45, 95% CI: 1.27 – 4.71) for each standard deviation increase in the discrimination score among Black women.
Discussion
In this sample of men and women with recent MI, we found more frequent experiences of everyday discrimination were associated with an elevated risk for MSIMI after controlling for sociodemographic and clinical risk factors along with indicators of MI severity. Associations were especially robust among women. Even after adjustment for depression symptom severity, one standard deviation increase in the EDS score was associated with an OR for MSIMI of 1.96 (95% CI: 1.13 – 3.38) among women, nearly a two-fold increase, and 1.40 (95% CI: 0.80 – 2.44) among men. However, the interaction between everyday discrimination and sex was not statistically significant.
We found that experiences of discrimination were related to MSIMI and not to CSIMI. Findings from laboratory and human cohorts suggest that different mechanisms are involved in myocardial ischemia induced by mental stress compared to other forms of stress like exercise. Both mental stress and physical stress trigger an increase in myocardial workload (increased heart rate and blood pressure) and an increase in oxygen demand [1, 3]. However, while with mental stress there is also an increase in systemic vascular resistance and microvascular constriction, with exercise and pharmacological stress there is systemic vasodilation [1, 3, 31-33]. By these mechanisms, mental stress can impair coronary perfusion, potentially inducing myocardial ischemia even in the absence of coronary stenoses. In previous studies we have shown that these pathways for MSIMI are especially relevant for women (8, 34).
Previous studies have noted that reports of discrimination are related to mechanistic pathways that could explain vulnerability to MSIMI, including attenuated recovery of endothelial function in response to acute stress, increased visceral fat and increased inflammatory markers [18, 22, 23]. These studies also identified sex differences, with associations generally stronger among women than among men. Men in our study reported a similar exposure to everyday discrimination compared to women. However, women could be more vulnerable to the physiological effects of psychosocial stressors, as suggested by previous literature (13, 35, 36). Rodent and human studies have shown greater and prolonged hypothalamic-pituitary-adrenal (HPA) axis activation as well as greater potential for hyperarousal in response to emotional stimuli in females, which may reflect sex-related differences in signaling, structure, and function related to stress response (37). There is also evidence that women sustain higher levels of interleukin-6 before and after mental stress tests, potentially putting women at higher risk for abnormal vascular responses after stress (38). Such dysregulation of neuroendocrine and immune responses to stress can facilitate microvascular dysfunction and peripheral vasoconstriction, which are emerging mechanisms of MSIMI, and more prevalent in women (2, 8, 39). Moreover, rumination over stressful events, to which women have a greater tendency, can result in prolonged duration of cortisol activation, hyperarousal and greater HPA axis response to stress (37, 40, 41). Women may cope in ways that make them especially sensitive to interpersonal stressors (42).
It should also be noted that women in this study were more likely to be Black compared to men, and therefore potentially exposed to social disadvantage and discrimination both for sex and for race (43). In exploratory models, adjusted associations between discrimination and MSIMI were very pronounced among Black women. We found it important to examine CVD risk among Black women in particular since recent research shows the prevalence of CVD among black women aged 35–44 years exceeded that of White women and Black and White men of the same age (44). Future research with larger subgroups of women and men identifying as White and other races are needed to further explore race-sex differences in MSIMI prevalence and associations between discrimination and MSIMI within these sub-groups.
There are limitations to this study worth noting. The prevalence of MSIMI in this study is lower than that observed in others, such as the REMIT study, which used echocardiography with ischemia defined as left ventricular wall motion abnormalities, which can give a MSIMI prevalence upwards of 60% (6). Conversely, myocardial perfusion imaging was used in the current study as this is the gold standard for ischemia assessment, and yields a consistently lower prevalence of MSIMI (45–47). It is also possible that the older age of participants in the REMIT study (mean=63.81), or the lower proportion of women in the REMIT study (17%) may somewhat account for the MSIMI prevalence differences between studies. Another potential limitation worth discussing is the specific mental stress laboratory task used in the MIMS2 study, which while related to mistreatment, is fairly generic and designed to evoke a response from a wide range of sociodemographic groups. It is possible that a stressor focused more explicitly on discrimination or oppression on the basis of sociodemographic factors (i.e., sex, race/ethnicity, social class), might have evoked a stronger physiological stress response among those with more experiences of discrimination. Previous studies have shown that the prevalence of MSIMI varies depending on the type and duration of mental tasks being performed (48). Therefore, we may have seen stronger associations between discrimination and MSIMI with a more discrimination or oppression-based stressor task, the more generic stressor used in MIMS2 potentially biasing our results toward the null.
Additionally, the cross-sectional nature of these data do not allow us to make assumptions on temporality or causality in the association between everyday discrimination and MSIMI. However, participants were not aware of their MSIMI status when answering questions about discrimination. Furthermore, due to small samples of non-Black female participants, we were unable to examine interaction effects with everyday discrimination by both race and sex. Considering the potential for differential exposures and effects of discrimination by race and sex, this may be an important area of exploration for future studies.
Further, although consistent with those reported in other studies, everyday discrimination scores in our cohort are fairly low (29, 49–51). This provides evidence in support of arguments that self-reported measures of interpersonal discrimination alone may not capture the full extent to which discrimination can affect health outcomes. For instance, institutional discrimination – systemic policies, practices, and norms that promote unequal access to opportunities such as employment, education, housing, and health care – may sustain persistent disparities in exposure to many stressors which may affect health (including work stress, violence, financial instability, and relationship stress) (31). Moreover, vigilance or anticipating discrimination is an everyday stressor that may better capture the worry and rumination related to discrimination. The latter can in turn lend to hyperarousal or dysregulation of physiological systems (52). Future studies should consider multiple domains of discrimination to more fully capture the effect of everyday discrimination on MSIMI and to inform future interventions that address the burden of MSIMI.
There are also important strengths to this study. To our knowledge, this is the first study to examine the relationship between discrimination and MSIMI. We used well-validated questionnaires and the gold-standard assessment of MSIMI, and controlled for a range of relevant psychological, behavioral and clinical confounders. By additionally exploring sex differences and focusing on a population with recent MI, this study offers important exploration of potential mechanisms explaining worse morbidity and mortality after MI among women (53). Also, the large number of Black patients and the nearly equal numbers of men and women makes this study well-suited to explore these questions.
In sum, in a sample of young and middle-aged men and women with a recent MI, experiences of everyday discrimination were associated with risk of MSIMI. There were no observed associations with conventional stress ischemia. The risk of MSIMI tended to be greater among women, suggesting that this emotional stressor may trigger a response to which women are particularly vulnerable, however we did not find a statistically significant interaction between everyday discrimination and sex. These findings further implicate the role of psychosocial exposures explaining worse morbidity and mortality after MI. This study adds important new data to a growing field pointing to discrimination as a key chronic stressor linked to CVD risk. Our results highlight the importance of assessing discrimination in post-MI patients, potentially for women in particular, and support the incorporation of this measure in future intervention efforts to ameliorate risk in this population.
Supplementary Material
Acknowledgments
Sources of Funding
Grant Number: R01 HL109413; R01 HL109413–02S1; P01 HL101398; K23 HL127251; T32 HL130025; HL130471; AR070898
Abbreviations
- BDI-II
Beck Depression Inventory-II
- BMI
Body mass index
- CAD
Coronary artery disease
- CHD
Coronary heart disease
- CI
Confidence interval
- CSIMI
Conventional stress-induced myocardial ischemia
- CVD
Cardiovascular disease
- ECG
Electrocardiogram
- EDS
Everyday Discrimination Scale
- MI
Myocardial infarction
- MIMS2
Myocardial Infarction and Mental Stress 2
- MSIMI
Mental stress-induced myocardial ischemia
- NSTEMI
Non-ST-Elevation Myocardial Infarction
- OR
Odds ratio
- SPECT
Single-photon emission computed tomography
- STEMI
ST-Elevation Myocardial Infarction
- 99mTc
Technetium-99
Footnotes
Conflicts of Interest
None declared.
References
- 1.Arri S, Ryan M, Redwood S, and Marber M. Mental stress-induced myocardial ischaemia. Heart 2016: 102: 472–480. [DOI] [PubMed] [Google Scholar]
- 2.Vaccarino V, Sullivan S, Hammadah M, Wilmot K, Al Mheid I, Ramadan R, Elon L, Pimple PM, Garcia EV, and Nye J. Mental Stress–Induced-Myocardial Ischemia in Young Patients With Recent Myocardial Infarction: Sex Differences and Mechanisms. Circulation 2018: 137: 794–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hammadah M, Alkhoder A, Al Mheid I, Wilmot K, Isakadze N, Abdulhadi N, Chou D, Obideen M, O’Neal WT, and Sullivan S. Hemodynamic, catecholamine, vasomotor and vascular responses: determinants of myocardial ischemia during mental stress. International journal of cardiology 2017: 243: 47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wei J, Rooks C, Ramadan R, Shah AJ, Bremner JD, Quyyumi AA, Kutner M, and Vaccarino V. Meta-analysis of mental stress–induced myocardial ischemia and subsequent cardiac events in patients with coronary artery disease. The American journal of cardiology 2014: 114: 187–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Samad Z, Boyle S, Ersboll M, Vora AN, Zhang Y, Becker RC, Williams R, Kuhn C, Ortel TL, and Rogers JG. Sex differences in platelet reactivity and cardiovascular and psychological response to mental stress in patients with stable ischemic heart disease: insights from the REMIT study. Journal of the American College of Cardiology 2014: 64: 1669–1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jiang W, Samad Z, Boyle S, Becker RC, Williams R, Kuhn C, Ortel TL, Rogers J, Kuchibhatla M, and O’Connor C. Prevalence and clinical characteristics of mental stress–induced myocardial ischemia in patients with coronary heart disease. Journal of the American College of Cardiology 2013: 61: 714–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaccarino V, Shah AJ, Rooks C, Ibeanu I, Nye JA, Pimple P, Salerno A, D’Marco L, Karohl C, and Bremner JD. Sex differences in mental stress-induced myocardial ischemia in young survivors of an acute myocardial infarction. Psychosomatic medicine 2014: 76: 171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sullivan S, Hammadah M, Al Mheid I, Wilmot K, Ramadan R, Alkhoder A, Isakadze N, Shah A, Levantsevych O, and Pimple PM. Sex differences in hemodynamic and microvascular mechanisms of myocardial ischemia induced by mental stress. Arteriosclerosis, thrombosis, and vascular biology 2018: 38: 473–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ma H, Guo L, Huang D, Wang L, Guo L, Geng Q, and Zhang M. The role of the myocardial microvasculature in mental stress–induced myocardial ischemia. Clinical cardiology 2016: 39: 234–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pimple P, Shah A, Rooks C, Bremner JD, Nye J, Ibeanu I, Murrah N, Shallenberger L, Kelley M, and Raggi P. Association between anger and mental stress–induced myocardial ischemia. American heart journal 2015: 169: 115–121. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wei J, Pimple P, Shah AJ, Rooks C, Bremner JD, Nye JA, Ibeanu I, Murrah N, Shallenberger L, and Raggi P. Depressive symptoms are associated with mental stress-induced myocardial ischemia after acute myocardial infarction. PloS one 2014: 9: e102986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boyle S, Samad Z, Becker RC, Williams R, Kuhn C, Ortel TL, Kuchibhatla M, Prybol K, Rogers J, and O’Connor C. Depressive symptoms and mental stress induced myocardial ischemia in patients with coronary heart disease. Psychosomatic medicine 2013: 75: 822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vaccarino V. and Bremner JD. Behavioral, emotional and neurobiological determinants of coronary heart disease risk in women. Neuroscience & Biobehavioral Reviews 2017: 74: 297–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lockwood KG, Marsland AL, Matthews KA, and Gianaros PJ. Perceived discrimination and cardiovascular health disparities: a multisystem review and health neuroscience perspective. Annals of the New York Academy of Sciences 2018: 1428: 170–207. [DOI] [PubMed] [Google Scholar]
- 15.Association, A.P. Stress and health disparities: Contexts, mechanisms, and interventions among racial/ethnic minority and low-socioeconomic status populations. 2017: [Google Scholar]
- 16.Chandrasekhar J, Gill A, and Mehran R. Acute myocardial infarction in young women: current perspectives. International journal of women’s health 2018: 10: 267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pascoe EA and Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychological bulletin 2009: 135: 531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moody DLB, Chang Y, Brown C, Bromberger JT, and Matthews KA. Everyday discrimination and metabolic syndrome incidence in a racially/ethnically diverse sample: study of Women’s Health Across the Nation (SWAN). Psychosomatic medicine 2018: 80: 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lewis TT, Kravitz HM, Janssen I, and Powell LH. Self-reported experiences of discrimination and visceral fat in middle-aged African-American and Caucasian women. American journal of epidemiology 2011: 173: 1223–1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kershaw KN, Lewis TT, Roux AVD, Jenny NS, Liu K, Penedo FJ, and Carnethon MR. Self-reported experiences of discrimination and inflammation among men and women: The multi-ethnic study of atherosclerosis. Health Psychology 2016: 35: 343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Everson-Rose SA, Lutsey PL, Roetker NS, Lewis TT, Kershaw KN, Alonso A, and Diez Roux AV. Perceived Discrimination and Incident Cardiovascular Events: The Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol 2015: 182: 225–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lewis TT, Williams DR, Tamene M, and Clark CR. Self-Reported Experiences of Discrimination and Cardiovascular Disease. Curr Cardiovasc Risk Rep 2014: 8: 365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moody DLB, Leibel DK, Pantesco EJ, Wendell CR, Waldstein SR, Evans MK, and Zonderman AB. Interactive Relations Across Dimensions of Interpersonal-Level Discrimination and Depressive Symptoms to Carotid Intimal-Medial Thickening in African Americans. Psychosomatic Medicine 2020: 82: 234–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vaccarino V, Horwitz RI, Meehan TP, Petrillo MK, Radford MJ, and Krumholz HM. Sex differences in mortality after myocardial infarction: evidence for a sex-age interaction. Archives of internal medicine 1998: 158: 2054–2062. [DOI] [PubMed] [Google Scholar]
- 25.Vaccarino V, Krumholz HM, Yarzebski J, Gore JM, and Goldberg RJ. Sex differences in 2-year mortality after hospital discharge for myocardial infarction. Annals of internal medicine 2001: 134: 173–181. [DOI] [PubMed] [Google Scholar]
- 26.Vaccarino V, Shah AJ, Rooks C, Ibeanu I, Nye JA, Pimple P, Salerno A, D’Marco L, Karohl C, and Bremner JD. Sex differences in mental stress-induced myocardial ischemia in young survivors of an acute myocardial infarction. Psychosomatic medicine 2014: 76: 171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holly TA, Abbott BG, Al-Mallah M, Calnon DA, Cohen MC, DiFilippo FP, Ficaro EP, Freeman MR, Hendel RC, and Jain D. Single photon-emission computed tomography. Journal of nuclear cardiology 2010: 17: 941–973. [DOI] [PubMed] [Google Scholar]
- 28.Williams DR, Yu Y, Jackson JS, and Anderson NB. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of health psychology 1997: 2: 335–351. [DOI] [PubMed] [Google Scholar]
- 29.Lewis TT, Yang FM, Jacobs EA, and Fitchett G. Racial/ethnic differences in responses to the everyday discrimination scale: a differential item functioning analysis. American journal of epidemiology 2012: 175: 391–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taylor TR, Kamarck TW, and Shiffman S. Validation of the Detroit Area Study Discrimination Scale in a community sample of older African American adults: the Pittsburgh healthy heart project. International Journal of Behavioral Medicine 2004: 11: 88–94. [DOI] [PubMed] [Google Scholar]
- 31.Lewis TT, Cogburn CD, and Williams DR. Self-reported experiences of discrimination and health: scientific advances, ongoing controversies, and emerging issues. Annual review of clinical psychology 2015: 11: 407–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saelee R, Vaccarino V, Sullivan S, Hammadah M, Shah A, Wilmot K, Abdelhadi N, Elon L, Pimple P, and Kaseer B. Longitudinal associations between self-reported experiences of discrimination and depressive symptoms in young women and men post-myocardial infarction. Journal of psychosomatic research 2019: 124: 109782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Richards JL and Kramer MR, Analytic Methods for Assessing Joint Exposure Effects of Preterm Birth and Neighborhood Deprivation on First Grade Academic Outcomes Among Georgia Public School Children. 2017: SAGE Publications Ltd. [Google Scholar]
- 34.Almuwaqqat Z, Sullivan S, Hammadah M, Lima BB, Shah AJ, Abdelhadi N, Fang S, Wilmot K, Al Mheid I, and Bremner JD. Sex-specific association between coronary artery disease severity and myocardial ischemia induced by mental stress. Psychosomatic medicine 2019: 81: 57–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hallman T, Burell G, Setterlind S, Odén A, and Lisspers J. Psychosocial risk factors for coronary heart disease, their importance compared with other risk factors and gender differences in sensitivity. Journal of Cardiovascular Risk 2001: 8: 39–49. [DOI] [PubMed] [Google Scholar]
- 36.Di Pilla M, Bruno RM, Taddei S, and Virdis A. Gender differences in the relationships between psychosocial factors and hypertension. Maturitas 2016: 93: 58–64. [DOI] [PubMed] [Google Scholar]
- 37.Bangasser DA and Valentino RJ. Sex differences in molecular and cellular substrates of stress. Cellular and molecular neurobiology 2012: 32: 709–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sullivan S, Hammadah M, Wilmot K, Ramadan R, Pearce BD, Shah A, Kaseer B, Gafeer MM, Lima BB, and Kim JH. Young Women With Coronary Artery Disease Exhibit Higher Concentrations of Interleukin-6 at Baseline and in Response to Mental Stress. Journal of the American Heart Association 2018: 7: e010329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.EUGenMed, C.C.S. Group, Regitz-Zagrosek V, Oertelt-Prigione S, Prescott E, Franconi F, Gerdts E, Foryst-Ludwig A, Maas AH, and Kautzky-Willer A. Gender in cardiovascular diseases: impact on clinical manifestations, management, and outcomes. European heart journal 2015: 37: 24–34. [DOI] [PubMed] [Google Scholar]
- 40.Nolen-Hoeksema S. Emotion regulation and psychopathology: The role of gender. Annual review of clinical psychology 2012: 8: 161–187. [DOI] [PubMed] [Google Scholar]
- 41.Shull A, Mayer SE, McGinnis E, Geiss E, Vargas I, and Lopez-Duran NL. Trait and state rumination interact to prolong cortisol activation to psychosocial stress in females. Psychoneuroendocrinology 2016: 74: 324–332. [DOI] [PubMed] [Google Scholar]
- 42.Cunningham TJ, Seeman TE, Kawachi I, Gortmaker SL, Jacobs DR, Kiefe CI, and Berkman LF. Racial/ethnic and gender differences in the association between self-reported experiences of racial/ethnic discrimination and inflammation in the CARDIA cohort of 4 US communities. Social science & medicine 2012: 75: 922–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lewis TT and Van Dyke ME. Discrimination and the health of African Americans: The potential importance of intersectionalities. Current directions in psychological science 2018: 27: 176–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jolly S, Vittinghoff E, Chattopadhyay A, and Bibbins-Domingo K. Higher cardiovascular disease prevalence and mortality among younger blacks compared to whites. The American journal of medicine 2010: 123: 811–818. [DOI] [PubMed] [Google Scholar]
- 45.Hassan M, York KM, Li H, Li Q, Lucey DG, Fillingim RB, and Sheps DS. Usefulness of peripheral arterial tonometry in the detection of mental stress-induced myocardial ischemia. Clinical Cardiology: An International Indexed and Peer-Reviewed Journal for Advances in the Treatment of Cardiovascular Disease 2009: 32: E1–E6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ramadan R, Sheps D, Esteves F, Maziar Zafari A, Douglas Bremner J, Vaccarino V, and Quyyumi AA. Myocardial ischemia during mental stress: role of coronary artery disease burden and vasomotion. Journal of the American Heart Association 2013: 2: e000321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dorbala S, Ananthasubramaniam K, Armstrong IS, Chareonthaitawee P, DePuey EG, Einstein AJ, Gropler RJ, Holly TA, Mahmarian JJ, and Park M-A. Single photon emission computed tomography (SPECT) myocardial perfusion imaging guidelines: instrumentation, acquisition, processing, and interpretation. Journal of Nuclear Cardiology 2018: 25: 1784–1846. [DOI] [PubMed] [Google Scholar]
- 48.Strike P. and Steptoe A. Systematic review of mental stress-induced myocardial ischaemia. European heart journal 2003: 24: 690–703. [DOI] [PubMed] [Google Scholar]
- 49.Hunte HE and Williams DR. The association between perceived discrimination and obesity in a population-based multiracial and multiethnic adult sample. American journal of public health 2009: 99: 1285–1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Beatty DL, Hall MH, Kamarck TA, Buysse DJ, Owens JF, Reis SE, Mezick EJ, Strollo PJ, and Matthews KA. Unfair treatment is associated with poor sleep in African American and Caucasian adults: Pittsburgh SleepSCORE project. Health Psychology 2011: 30: 351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lewis TT, Aiello AE, Leurgans S, Kelly J, and Barnes LL. Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain, behavior, and immunity 2010: 24: 438–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lewis TT, Lampert R, Charles D, and Katz S. Expectations of Racism and Carotid Intima Media Thickness in African-American Women. Psychosomatic medicine 2019: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vaccarino V, Badimon L, Corti R, De Wit C, Dorobantu M, Manfrini O, Koller A, Pries A, Cenko E, and Bugiardini R. Presentation, management, and outcomes of ischaemic heart disease in women. Nature Reviews Cardiology 2013: 10: 508. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.