Abstract
Background
Older adults are the most sedentary segment of society, often spending in excess of 8.5 hours a day sitting. Large amounts of time spent sedentary, defined as time spend sitting or in a reclining posture without spending energy, has been linked to an increased risk of chronic diseases, frailty, loss of function, disablement, social isolation, and premature death.
Objectives
To evaluate the effectiveness of interventions aimed at reducing sedentary behaviour amongst older adults living independently in the community compared to control conditions involving either no intervention or interventions that do not target sedentary behaviour.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, Embase, CINAHL, PsycINFO, PEDro, EPPI‐Centre databases (Trials Register of Promoting Health Interventions (TRoPHI) and the Obesity and Sedentary behaviour Database), WHO ICTRP, and ClinicalTrials.gov up to 18 January 2021. We also screened the reference lists of included articles and contacted authors to identify additional studies.
Selection criteria
We included randomised controlled trials (RCTs) and cluster‐RCTs. We included interventions purposefully designed to reduce sedentary time in older adults (aged 60 or over) living independently in the community. We included studies if some of the participants had multiple comorbidities, but excluded interventions that recruited clinical populations specifically (e.g. stroke survivors).
Data collection and analysis
Two review authors independently screened titles and abstracts and full‐text articles to determine study eligibility. Two review authors independently extracted data and assessed risk of bias. We contacted authors for additional data where required. Any disagreements in study screening or data extraction were settled by a third review author.
Main results
We included seven studies in the review, six RCTs and one cluster‐RCT, with a total of 397 participants. The majority of participants were female (n = 284), white, and highly educated. All trials were conducted in high‐income countries. All studies evaluated individually based behaviour change interventions using a combination of behaviour change techniques such as goal setting, education, and behaviour monitoring or feedback. Four of the seven studies also measured secondary outcomes. The main sources of bias were related to selection bias (N = 2), performance bias (N = 6), blinding of outcome assessment (N = 2), and incomplete outcome data (N = 2) and selective reporting (N=1). The overall risk of bias was judged as unclear.
Primary outcomes
The evidence suggests that interventions to change sedentary behaviour in community‐dwelling older adults may reduce sedentary time (mean difference (MD) −44.91 min/day, 95% confidence interval (CI) −93.13 to 3.32; 397 participants; 7 studies; I2 = 73%; low‐certainty evidence). We could not pool evidence on the effect of interventions on breaks in sedentary behaviour or time spent in specific domains such as TV time, as data from only one study were available for these outcomes.
Secondary outcomes
We are uncertain whether interventions to reduce sedentary behaviour have any impact on the physical or mental health outcomes of community‐dwelling older adults. We were able to pool change data for the following outcomes.
• Physical function (MD 0.14 Short Physical Performance Battery (SPPB) score, 95% CI −0.38 to 0.66; higher score is favourable; 98 participants; 2 studies; I2 = 26%; low‐certainty evidence).
• Waist circumference (MD 1.14 cm, 95% CI −1.64 to 3.93; 100 participants; 2 studies; I2 = 0%; low‐certainty evidence).
• Fitness (MD ‐5.16 m in the 6‐minute walk test, 95% CI −36.49 to 26.17; higher score is favourable; 80 participants; 2 studies; I2 = 29%; low‐certainty evidence).
• Blood pressure: systolic (MD −3.91 mmHg, 95% CI ‐10.95 to 3.13; 138 participants; 3 studies; I2 = 73%; very low‐certainty evidence) and diastolic (MD −0.06 mmHg, 95% CI −5.72 to 5.60; 138 participants; 3 studies; I2 = 97%; very low‐certainty evidence).
• Glucose blood levels (MD 2.20 mg/dL, 95% CI −6.46 to 10.86; 100 participants; 2 studies; I2 = 0%; low‐certainty evidence).
No data were available on cognitive function, cost‐effectiveness or adverse effects.
Authors' conclusions
It is not clear whether interventions to reduce sedentary behaviour are effective at reducing sedentary time in community‐dwelling older adults. We are uncertain if these interventions have any impact on the physical or mental health of community‐dwelling older adults. There were few studies, and the certainty of the evidence is very low to low, mainly due to inconsistency in findings and imprecision. Future studies should consider interventions aimed at modifying the environment, policy, and social and cultural norms. Future studies should also use device‐based measures of sedentary time, recruit larger samples, and gather information about quality of life, cost‐effectiveness, and adverse event data.
Keywords: Aged, Female, Humans, Male, Middle Aged, Behavior, Bias, Blood Glucose, Blood Glucose/analysis, Blood Pressure, Goals, Independent Living, Randomized Controlled Trials as Topic, Sedentary Behavior, Selection Bias, Sitting Position, Time Factors, Waist Circumference, Walk Test
Plain language summary
What works for reducing sedentary behaviour in older adults living in the community?
Key messages
There is not enough evidence to allow for any clear conclusions about whether programmes or policies are effective in reducing sedentary time in older adults. It is also uncertain whether these programmes or policies improve the physical or mental health of older adults.
Why did we do this review?
Older adults spend about 80% of their time being sedentary. Sedentary time is the amount of time spent sitting or lying down whilst awake. For example, sitting down watching TV is considered a sedentary behaviour. Long periods of sedentary time have been linked with an increased risk of several long‐term diseases, becoming frailer, developing disabilities, needing help with everyday activities, and early death. We wanted to know if programmes or policies intended to help older adults reduce their sedentary time are effective. We also wanted to know if these programmes or policies also provide physical or mental health benefits.
What did we do?
We searched electronic databases and relevant journals to find studies. We included any randomised study (in which people have the same chance of being given the intervention or not) that looked at policies or programmes that were designed to reduce sedentary time in older adults (aged 60 or over) living independently in the community. We compared and summarised the results of the studies and rated our confidence in the evidence, based on factors such as study methods and sizes.
What did we find out?
We found seven studies including a total of 397 older adults. All of the studies looked at ways to help individual older adults to change their sedentary behaviour. The support included a range of strategies like counselling, goal setting, and information sessions. Some of the studies used technology that records behaviour, such as activity monitors. We did not find any studies that looked at changes to the natural environment, the built environment, a person's social environment, or home environment where older adults live. We did not find any studies that looked at the effect of changing policies and laws that affect the sedentary behaviour of older adults. We did not find any studies that looked at whether the benefits and use of the programme were at least worth what was paid for them. None of the studies reported on unwanted effects.
What are the limitations of the evidence?
We have only low confidence in these findings, due to low sample sizes and because some studies were conducted in ways that may have introduced errors into their results. The findings also combined results from studies using self‐reported measures of sedentary time together with device‐based measures.
How up‐to‐date is the evidence?
The evidence is current to January 2021.
Summary of findings
Summary of findings 1. Intervention for reducing sedentary behaviour in community‐dwelling older adults.
| Patient or population: Older adults living independently in the community Setting: Community Intervention: Intervention to reduce sedentary behaviour Comparison: No intervention, or intervention not targeting sedentary behaviour | ||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | |
| Risk with control | Risk with intervention to reduce sedentary behaviour | |||
| Primary outcomes | ||||
| Sedentary time Follow‐up: range 1 week to 12 months | The mean sedentary time ranged from 541 to 1240 minutes/day. | MD 44.91 minutes/day lower
(93.13 lower to 3.32 higher) |
397 (7 RCTs) | ⊕⊕⊝⊝ LOW 1 2 |
| Secondary outcomes | ||||
| Physical function Assessed with: Short Physical Performance Battery (higher score is better) Scale from: 0 to 12 Follow‐up: mean 12 weeks | The mean physical function ranged from 11.3 to 11.4. | MD 0.14 higher (0.38 lower to 0.66 higher) | 98 (2 RCTs) | ⊕⊕⊝⊝ LOW 3 |
| Waist circumference Follow‐up: range 8 weeks to 12 weeks | The mean waist circumference ranged from 103 to 114 cm. | MD 1.14 cm higher (1.64 lower to 3.93 higher) | 100 (2 RCTs) | ⊕⊕⊝⊝ LOW 3 |
| Systolic blood pressure Follow‐up: range 8 weeks to 12 weeks | The mean systolic blood pressure ranged from 123 to 141 mmHg. | MD 3.91 mmHg lower (10.95 lower to 3.13 higher) | 138 (3 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 3 |
| Diastolic blood pressure Follow‐up: range 8 weeks to 12 weeks | The mean diastolic blood pressure ranged from 67 to 77 mmHg. | MD 0.06 mmHg lower (5.72 lower to 5.60 higher) | 138 (3 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 3 |
|
Level of glucose in blood Follow‐up: range 8 weeks to 12 weeks |
The mean level of glucose in blood ranged from 105 to 114 mg/dL. | MD 2.20 mg/dL higher (6.46 lower to 10.86 higher) | 100 (2 RCTs) | ⊕⊕⊝⊝ LOW 3 |
| Adverse effects | ‐ | ‐ | ‐ | No studies measured adverse effects. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI: confidence interval; MD: mean difference; RCT: randomised controlled trial | ||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
1Downgraded one level for inconsistency due to wide variance of point estimates across studies (high heterogeneity). 2Downgraded one level for imprecision due to wide confidence intervals. 3Downgraded two levels for imprecision due to very small sample sizes.
Background
Description of the condition
Older adults (age ≥ 60 years) are one of the most sedentary groups in society, spending on average 80% of their time in a seated posture and with 67% being sedentary for more than 8.5 hours per day (Harvey 2013). Sedentary behaviour has been defined as an activity where the predominant posture is sitting or lying and energy expenditure is low (Chastin 2013; SBRN 2012). Sedentary behaviour is distinctly different from inactivity. Inactivity is often regarded as not meeting physical activity guidelines for health, or too little exercise, whilst sedentary behaviour is too much sitting (Owen 2010). Standing for long periods would therefore be considered inactivity, and sitting or lying down (except sleep) for long periods would be sedentary behaviour. Going for a slow walk would not be considered being sedentary (as the person is not sitting), and if the person never or rarely sweat or was out of breath (moderate activity), they would be categorised as being inactive. Older people can reduce their sedentary behaviour if they get up on their feet (if able) as often as possible during their waking hours. Although it may be desirable, it is not necessary that older people should spend this time on their feet engaged in an activity for which the level of intensity is moderate or vigorous.
There is increasing evidence to suggest that sedentary behaviour, especially when accumulated in prolonged and continuous bouts, is detrimental to physical health (de Rezende 2014; Dunstan 2012; Henson 2013), mental health (Lauder 2006), quality of life (Laforge 1999), and bone health (Chastin 2014), in addition to being associated with all‐cause mortality, disease incidence, and hospitalisation (Biswas 2015). Prolonged screen‐based sedentary activities, such as watching television, have been shown to be associated with depressive symptoms (Teychenne 2010), whilst metabolic syndrome has a significant correlation with lengthy sedentary periods (Bankoski 2011). Sedentary behaviour is also associated with lower odds of successful ageing (Dogra 2012). These deleterious health effects of sedentary behaviour are different to those of physical inactivity, and are partially independent of an individual’s physical activity levels (Bankoski 2011). Indeed, even individuals who meet the recommended daily moderate to vigorous physical activity guidelines might experience the adverse effect of sedentary behaviour (Katzmarzyk 2009). In fact, a meta‐analysis reveals that over one hour of daily moderate‐intensity activity is required to attenuate the association between sedentary time and mortality (Ekelund 2016).
The World Health Organization, the UK, the USA, and other countries have now issued recommendations to reduce sedentary time as part of their older adult physical activity guidelines (Bull 2020; DoH 2019; Piercy 2018). These guidelines recommend reducing sedentary time in addition to increasing time spent in both light‐ and moderate‐intensity physical activity. This pragmatic stance reflects the findings that solely promoting physical activity does not necessarily reduce sitting time, as one may achieve the recommended physical activity guidelines, yet still sit for large periods of the day (Dogra 2012; Katzmarzyk 2010). Indeed, reviews indicate that interventions aimed at promoting physical activity are ineffective at reducing sedentary time (Martin 2015; Prince 2014). Experimental work indicates that time spent in moderate‐intensity activity tends to displace time that individuals usually spend in light activity and activities incidental to daily living, but not sitting time (Gomersall 2015). Interventions devised specifically to reduce sedentary behaviour are needed (Owen 2011).
The aim of this review was to synthesise and compare the current evidence on the effectiveness of interventions to reduce sedentary time amongst community‐dwelling older adults.
Description of the intervention
This review assessed the effectiveness of interventions aimed specifically at reducing sedentary behaviour in community‐dwelling older adults. Sedentary behaviour is ubiquitous and occurs throughout the day during leisure time activities, eating, and transport. In order to reduce sedentary time, interventions must specifically encourage people to spend more time on their feet throughout the day. Interventions can specifically focus on sedentary behaviour or be part of physical activity programmes which include a component specifically addressing sedentary behaviour (Martin 2015; Prince 2014).
Reviews of the effects of sedentary behaviour reduction interventions in adults have found that interventions that target sedentary behaviour specifically were more successful in reducing sedentary time, and those using only physical activity intervention were ineffective (Martin 2015; Prince 2014).
Interventions may be delivered at the individual, environmental, or policy levels. Interventions at individuals level might be delivered on a one‐to‐one basis, or they may look at a wider reach through communities. These interventions provide education and behaviour change counselling sessions designed to help people implement a behaviour change plan using different behaviour change techniques (de Greef 2010). These behaviour change techniques might include setting goals and self‐monitoring, encouraging participants to track their sedentary time to raise awareness. With advances in body‐worn sensors and self‐tracking technology, the use body‐worn devices and activity monitors in interventions is starting to appear in the literature. Some of these interventions have been delivered via online media, for example using email messages (Adams 2013), whilst face‐to‐face consultations have also been shown to provide fruitful outcomes in decreasing sedentary periods (Gardiner 2011). At the environmental level, interventions might include change in the physical layout of the domestic environment, but also changes to the built environment. Finally, there might be policy developed to encourage standing and promote the reduction in sedentary behaviour.
There are some potential limitations in interventions attempting to reduce overall sedentary time in older adults. Primarily, some sedentary activities in which older adults participate, such as reading and socialising (Leask 2015), provide a mental health benefit (Alpass 2003), and facilitate cognitive function in ageing (Hertzog 2008). Although prolonged sedentary time may have a detrimental effect on physical health, some instances of sedentary time therefore provide a positive mental health benefit and should not be decreased. Further activities, for example eating and resting, are essential for daily living and should not be altered. Older adults value some sedentary activities to such an extent that they would be unwilling to alter them, and there might be notable cultural differences in this (Leask 2016; Palmer 2019).
The majority of interventions have focused on the individual, but others are attempting to modify more distal determinants of sedentary behaviour, or even target a different level of determinants (Owen 2011). For example, environmental restructuring interventions modifying home and workplace layout, standing desks, or implementing outdoor spaces and facilities have all been acknowledged as potentially potent ways of reducing sedentary time (Gardner 2016; Shrestha 2019; Tandon 2012). A systematic review identified that interventions based on environmental restructuring, persuasion, or education were more successful in reducing sitting time and that self‐monitoring, problem solving, and restructuring the social or physical environment were particularly useful behaviour change techniques (Gardner 2016).
To date, there are no widely accepted guidelines quantifying a daily limit for sedentary time. The Canadian 24‐hour movement guidelines recommend older adults limit sedentary time to a maximum of 8 hours per day (Ross 2020). One study suggests that substantial cardiovascular health benefits can be gained if adults reduce their sedentary time by two hours per day (Healy 2011). However, these guidelines remain too controversial to be used as behavioural targets that interventions could set (Stamatakis 2019).
How the intervention might work
There are different frameworks for understanding the determinants of sedentary behaviour and that inform interventions. The ecological model, proposed by Owen and colleagues (Owen 2011), places individuals' behaviour within different contexts: leisure time, transport, household, and occupation. The System of Sedentary (SOS) behaviour framework takes a systems approach to understand sedentary behaviour, as the interaction between groups of factors: physical health, social and cultural context, built and natural environment, psychology and behaviour, politics and economy, and institutional and home settings (Chastin 2016). Interventions to reduce sedentary time in adults have been either interventions with a specific goal of increasing physical activity levels alongside reducing sedentary time, or interventions aimed at reducing sedentary time only (Martin 2015; Prince 2014). Those interventions focused on reducing sedentary behaviour have resulted in a greater reduction of sedentary time (Martin 2015; Prince 2014). Indeed, the determinants of sedentary behaviour are distinct from those of physical activity (Chastin 2015b), and the intervention must specifically address these determinants.
There are a number of different ways that sedentary behaviour interventions could decrease total sedentary time or break up prolonged sitting time (bouts) in older adults. Based on the SOS framework, these could be as follows.
Changing the psychology and behaviour
Providing information: interventions could be used to educate individuals on the benefits of decreasing their overall sedentary time and breaking up prolonged sedentary periods, by using consultations/interviews, reviewing their own behaviour (self‐monitoring by diary), or employing a feedback system. An example of such a feedback system would be the use of objective monitors to detect sedentary behaviour and print out or provide digital feedback to identify times when prolonged sitting could be reduced (i.e. by avoiding valued seated activities such as social events, reading, and knitting).
Prompting: real‐time behaviour prompts using wearable sensor and mobile technology that detect prolonged sedentary periods and prompt the individual to rise and move. Less frequent reminders by email and phone messages may act as a less regular prompt system.
Altering the home settings and built environment
Environmental restructuring: interventions may alter indoor or outdoor spaces to attempt to decrease individuals’ sedentary time. More specifically, home or care setting layout changes might be considered in order to encourage individuals to sit less. Standing desks and perching stools rather than comfortable seats are some other potential examples of this.
Changing the social and cultural context
Challenge to cultural and social norms: it is culturally and socially acceptable in many places to expect older adults to sit. It is considered important to offer seats to older adults, such as on public transport. Friends and family often start doing household chores and tasks for older people rather than them being encouraged to be active and continue doing these activities. There is also a tendency for a risk‐averse culture around older adults, with a perception that sitting is safe and that standing might lead to a fall. Some interventions might challenge these cultural norms by education of older adults, family members, or carers or changing the perception of the place of older adults and active ageing in society.
Policy changes
Policy change: organisations which provide services and care for older adults might change working practices to encourage individuals to sit less.
Why it is important to do this review
There are well‐established benefits of older adults being physically active (Kerr 2012; King 2001). Evidence describing the effectiveness of different intervention types to increase physical activity has been summarised in several review articles (Sansano 2019; Stockwell 2019; Zubala 2017). Despite these findings, older adults spend large periods of the day sedentary, regardless of whether they are physically active at some time points (Harvey 2013; Harvey 2015). Increased sedentary time is associated with poorer health outcomes in older adults (Copeland 2017; de Rezende 2014), including physical function (Rosenberg 2015), onset of frailty (Song 2015), and less successful ageing (Dogra 2012). There is now robust epidemiological evidence showing that the effect on health of prolonged sedentary time cannot be compensated for by adherence to physical activity or any exercise protocol (Biswas 2015). Consequently, interventions that specifically target sedentary behaviour have been advocated in this population in addition to promoting physical activity (Manns 2012; Sparling 2015). Older adults are potentially the population that might benefit the most from a reduction of sedentary time, because they are the most sedentary group and have the highest chronic disease burden (Harvey 2013; Harvey 2015). In addition, qualitative research reveals that overweight or obese older adults consider interventions to reduce sedentary behaviour more acceptable and desirable for them to adhere to than exercise programmes (Greenwood‐Hickman 2016). Early feasibility studies have shown that changing sedentary behaviour amongst older adults is feasible (Gardiner 2011; Harvey 2015; Rosenberg 2015). Little is known about what older people feel are important outcome measures to report on within these interventions (Dogra 2012).
To date, there is a single narrative review available (Aunger 2019), but no systematic review and meta‐analysis that has summarised study findings which aim to reduce or change sedentary patterns in older adults. Three reviews summarised the evidence in adults, including older adults (Elavsky 2019; Martin 2015; Prince 2014), and two looked at digital interventions (Stockwell 2019; Yerrakalva 2019). They included studies with a control or comparison group and identified four studies in older adults, but none with a sole focus on sedentary time. An international consensus highlighted the need to understand the effectiveness of intervention to change sedentary behaviour in older adults as a main research priority (Dogra 2017). Compiling this information may help inform future interventions regarding the most successful and efficient methods to decrease sedentary time in older adults.
Objectives
Primary
To assess the effect on total sedentary time and the pattern of accumulation of sedentary time of interventions aimed at modifying sedentary behaviour in older adults who are 60 years and over compared to control conditions involving either no intervention or interventions that do not target sedentary behaviour.
Secondary
To summarise the effects of interventions to reduce sedentary behaviour on quality of life, depression, and health status in older adults.
To summarise any evidence on the cost‐effectiveness and unintended consequences of interventions that reduce sedentary behaviour in older adults.
Methods
Criteria for considering studies for this review
Types of studies
We wanted our conclusions to be based on the best available evidence, so we chose to include only randomised controlled trials (RCTs) and cluster‐RCTs in the review.
Types of participants
Studies had to report data on participants with the following characteristics.
Inclusion of a sample of adults of mean age of 60 years and over with no participants younger than 55 years old.
Older adults living independently in the community, either at home or in sheltered housing or a residential complex that does not provide daily nursing or social care. We excluded older adults living in care home or nursing homes.
Participants not recruited for belonging to specific clinical populations (e.g. stroke survivors) or having a specific condition or pathology. Participants may have comorbidities, but may not be recruited as a result of these.
Types of interventions
Studies had to report population‐, community‐, or individual‐based interventions specifically designed to reduce sedentary time, shorten lengths of prolonged sitting, and/or reduce particular sedentary behaviours, for example sitting time or watching television.
Interventions targeting the raising of awareness and provision of information. This might include interventions which use technology (e.g. digital, mHealth) and social networks in addition to peer support networks.
Interventions which use prompting on multiple occasions (vibration monitors, phones, emails) to raise awareness and provide feedback on sedentary behaviour.
Interventions which attempt to alter the environment, e.g. modifying the layout of indoor and outdoor spaces and furniture.
Interventions that aim to change culture, policy, and practice in people's work with older people, e.g. motivating staff to encourage older people to move more frequently.
We excluded studies reporting interventions aimed solely at increasing physical activity, but included interventions targeting both an increase in physical activity and a reduction in sedentary behaviour. The intervention could be delivered in community settings and within primary care. The interventions described above were compared with no intervention or with standard care or with interventions without sedentary behaviour change components.
Types of outcome measures
We included studies that reported sedentary behaviour as a primary or secondary outcome.
Primary outcomes
The primary outcome is sedentary behaviour, assessed at baseline and postintervention.
Time spent sedentary (measured by self‐reported measures or objective measures).
Time spent in specific sedentary behaviours (e.g. time spent watching TV) as defined by the Sedentary Behaviours International Taxonomy (SIT) (Chastin 2013).
Pattern of accumulation of sedentary time (e.g. number of breaks in sedentary time) (Chastin 2015a; Healy 2008), distribution of bouts of sedentary time (Chastin 2010).
Secondary outcomes
Little is currently known about patient‐valued outcomes. We considered the following outcomes to be of interest.
Health status (improvement in physical function, cardiovascular and metabolic outcomes, and cognition).
Quality of life.
Depression.
Cost‐effectiveness.
Adverse events.
Search methods for identification of studies
Electronic searches
We created a comprehensive search strategy derived from terms related to sedentary behaviour, study design type, and population of study participants. The search criteria were informed by previous reviews (e.g. Martin 2015; Prince 2014). We searched the following electronic databases up to 18 January 2021.
Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane Library. (Appendix 1)
MEDLINE (PubMed). (Appendix 2)
Embase (Embase.com). (Appendix 3)
CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature). (Appendix 4)
PsycINFO (ProQuest). (Appendix 5)
PEDro (Physiotherapy Evidence Database; www.pedro.org.au). (Appendix 6)
EPPI‐Centre databases (eppi.ioe.ac.uk/cms/Default.aspx?tabid=185): Trials Register of Promoting Health Interventions (TRoPHI) and The database on obesity and sedentary behaviour studies. (Appendix 7)
World Health Organisation (WHO) International Clinical Trials Registry Platform (ICTRP) (apps.who.int/trialsearch). (Appendix 8)
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov). (Appendix 9)
We also screened the reference lists of included articles and contacted authors to identify additional studies.
Searching other resources
We screened the reference lists of included articles and identified systematic reviews for additional studies. We also contacted experts in the field through the International Physical and Environment Network (www.ipenproject.org/index.html), International Society for Physical Activity and Health (www.ispah.org), Sedentary Behaviour Research Network (www.sedentarybehaviour.org), and other leading international research networks to identify any additional work which is unpublished.
Data collection and analysis
Selection of studies
We downloaded the references retrieved by the electronic and handsearches into Covidence (Covidence). Two review authors (out of a pool of nine) independently screened studies identified by the searches through two stages: 1) title and abstract screening and 2) full‐text screening using Covidence. Review authors coded the studies at each stage of the review process as 'included' or 'excluded'. The two review authors resolved any discrepancies regarding inclusion or exclusion by discussion or by consulting a third review author who acted as arbitrator. Review authors were not allowed to screen any studies on which they were co‐author. Duplicates of identified studies were excluded. We recorded the study selection process in a PRISMA flow diagram (Moher 2009). We did not find any potentially relevant papers in a language other than English, so we did not require translation services.
Data extraction and management
We extracted the following data from the included studies using Covidence extraction templates.
Methodological information: study design, randomisation, intervention duration, follow‐up duration, study date, context.
Participant information: inclusion and exclusion criteria, sample size, age range, pre‐intervention and postintervention sitting time, health status, socioeconomic status.
Sedentary behaviour monitoring method.
Intervention information: intervention description, length, and comparison condition. We categorised interventions using the SOS framework as individual psychology and behaviour, socio‐cultural settings, environmental, home settings, policy change intervention (Chastin 2016).
Outcome information: reporting both primary and secondary outcomes.
Additional information: missing data; conflicts of interest; intervention fidelity (whether the intervention was delivered as planned); information on the nature and extent of any additional actions given as part of the intervention (co‐interventions); intervention costs; source of study funding; adverse events.
Two review authors (from a pool of nine) independently extracted data from each study. Any disagreements regarding data extraction were resolved by discussion or by consulting a third review author if necessary. Review authors were not allowed to extract data from studies on which they were a co‐author.
Assessment of risk of bias in included studies
Two review authors (from a pool of nine) independently assessed risk of bias of the included studies using the Cochrane risk of bias tool (Higgins 2021). Any disagreements in risk of bias assessment were resolved by discussion or through consensus with a third review author. Review authors were not allowed to assess the risk of bias of any studies on which they were a co‐author. The risk of bias tool assesses the following five domains:
selection bias (sequence generation and allocation concealment);
performance and detection bias (blinding);
attrition bias (incomplete outcome data, withdrawals, dropouts, protocol deviations);
reporting bias;
and an open 'other bias' category (e.g. baseline comparability for age, gender, and occupation).
We graded each domain as being at 'low', 'high', or 'unclear' risk of bias and provided a justification for our judgement in the risk of bias tables. We considered blinding of outcome assessment differently when sedentary time was assessed objectively or by self‐report, as participants cannot be blinded to self‐reported measures (Shrestha 2014). For cluster‐RCTs, we considered:
recruitment bias;
baseline imbalance;
loss of clusters;
incorrect analysis; and
comparability with individually randomised trials.
We summarised risk of bias for each outcome as being as 'low' if none of studies contributing to the outcome had any domains assessed as at high risk of bias; unclear if fewer than the majority studies contributing to the outcome had more than three domains at high risk of bias, or 'high' (CPHG 2011).
Measures of treatment effect
To calculate treatment effects, we entered outcome data from all included studies into Review Manager 5 (Review Manager 2020). For studies with continuous outcome measures, we reported mean scores and standard deviations. We used the mean difference (MD) between intervention and control groups postintervention for each continuous outcome to analyse the size of the effects of interventions. We used the adjusted MD between groups for cluster‐RCTs.
Unit of analysis issues
We did not identify any studies with multiple intervention arms. For cluster‐RCTs, we assessed whether the reported results were properly adjusted to account for clustering effects.
We adjusted outcomes for cluster‐RCTs for clustering effect using the effective sample sizes method (Higgins 2021). We used an intraclass correlation coefficient of 0.07 based on previous research in activity behaviour research (Kerr 2018).
Dealing with missing data
We noted missing data on the data extraction form and reported this in the risk of bias table. Where we encountered missing numerical outcome data, we contacted study authors to obtain this information. Where outcome data such as standard deviations were missing and were not obtainable from the study authors, we derived them from other available statistics following the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2021).
Assessment of heterogeneity
We visually inspected the forest plots to assess statistical heterogeneity. In addition, we analysed heterogeneity using the I2 and Chi2 statistics and corresponding P value. We reported heterogeneity as follows:
low degree of heterogeneity (25% to 50%);
moderate degree of heterogeneity (50% to 75%);
high degree of heterogeneity (75% or higher).
We considered heterogeneity in design, intervention, participants, and outcomes, as recorded in the Characteristics of included studies table.
Assessment of reporting biases
As fewer than 10 studies were included per outcome, funnel plots could not be formally used to assess reporting bias, as the power of these tests would be too low to distinguish chance from real asymmetry (Sterne 2011).
Data synthesis
The findings of the studies were systematically examined and integrated across studies. The included studies were tabulated and grouped by study design, population, outcomes, and setting, to explore relationships within and between included studies in a narrative summary. We conducted meta‐analyses using Review Manager 5 (Review Manager 2020) employing a random‐effects model, which allows for a greater level of natural heterogeneity between studies (Deeks 2011). We included data from cluster‐RCTs in meta‐analyses, as clustering was already taken into account in the analysis reported in included studies. We compared the effect of interventions aimed at reducing sedentary behaviour against control. When the control condition was a physical activity condition, we treated it the same as usual care or any intervention not aimed at changing sedentary behaviour that was used as control. Our rationale for this was that evidence shows that physical activity interventions do not change sedentary behaviour in older adults (Gomersall 2015; Martin 2015). For some outcomes (primary outcome of breaks in sedentary time, secondary outcomes of depression, health status, and quality of life), it was not possible to conduct a meta‐analysis because insufficient data were available. We reported results for these outcomes narratively grouped by outcome.
Subgroup analysis and investigation of heterogeneity
We conducted a subgroup analysis based on the method of measurement of sedentary time as either objectively measured using body‐worn devices or measured using self‐report tools. We also conducted subgroup analysis according to the intervention duration, classified as interventions delivered during a single point of contact or interventions delivered longitudinally. This classification differs from that in our protocol, as the classification in our protocol did not fit the type of interventions we found. We planned further subgroup analysis based on sex, geographical location, intervention setting or 'deliverer', socioeconomic status, and health status, but due to the small number of included studies this was not possible.
Sensitivity analysis
We planned to conduct a sensitivity analysis to understand the impact of risk of bias on the findings by excluding from the analysis studies rated as at high risk of bias. However, overall risk of bias was uniform across studies, and we did not rank any studies as at high risk of bias.
Summary of findings and assessment of the certainty of the evidence
We summarised our findings according to the guidelines in Chapter 14 of the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2021). Two review authors (from a pool of nine) independently assessed the certainty of evidence for each of the primary outcome measures using the GRADE methodology (Guyatt 2011). Results were tabulated using a template adapted from GRADEpro GDT (GRADEpro GDT). The certainty of a body of evidence as assessed by GRADE is the extent to which one can be confident in the estimate of effect. We assessed the certainty of the evidence for each outcome as high, moderate, low, or very low. In the GRADE approach, RCTs are assessed as high certainty at the start. Five criteria are considered for possible downgrading of the certainty of evidence: study quality (risk of bias); consistency (consistency between studies); directness (the same study participants, intervention, and outcome measures in included studies is for the people, measures, and outcomes we wanted to study); precision of results; and reporting biases. Three criteria are considered for possible upgrading of results: strong or very strong associations between intervention and outcome; large or very large dose‐response effects; and where all plausible confounders would have reduced the effect. We reported the certainty of evidence in Table 1 alongside the synthesis of outcomes.
Results
Description of studies
See Characteristics of included studies, Characteristics of excluded studies, Characteristics of studies awaiting classification, Characteristics of ongoing studies.
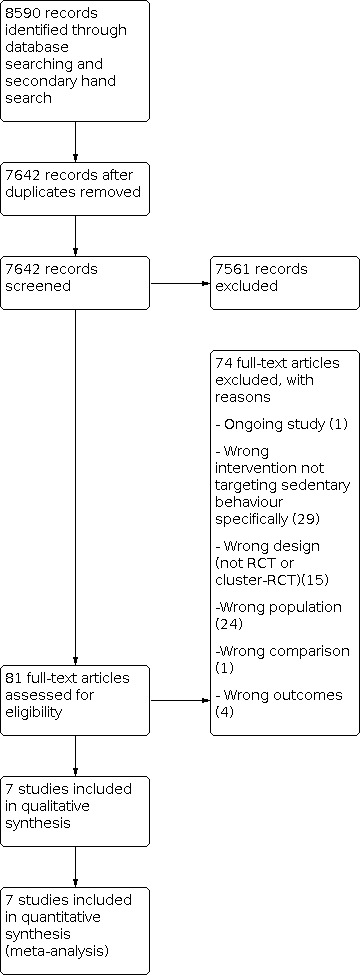
Results of the search
Our search identified 7642 unique articles. After title and abstract screening, 81 articles were assessed for inclusion as full text, of which 7 met the inclusion criteria for the review. The flow of information and the breakdown of included and excluded studies is shown in Figure 1.
1.
The full search strategies and the number of hits for the electronic databases and the clinical trials registries can be found in the Appendices. We contacted authors for Barone 2017 and Rosenberg 2020 to obtain detailed results, and received responses from both.
Included studies
Design
We included six RCTs, Barone 2017; Lyons 2017; Owari 2019; Roberts 2019; Rosenberg 2020; White 2017, and one cluster‐RCT (Maher 2017). Comparison conditions were not uniform across all studies, and included waiting list or usual care (Lyons 2017; Rosenberg 2020), physical activity intervention (Barone 2017; Roberts 2019), intervention to reduce social isolation (Maher 2017), and a simple information leaflet about physical activity (Owari 2019; White 2017).
Setting
Settings for all studies were in the community and used research facilities (Barone 2017; Lyons 2017; Roberts 2019; Rosenberg 2020), senior centres (Maher 2017), health clubs (Owari 2019), or primary care facilities (White 2017). Four studies were undertaken in the USA (Barone 2017; Lyons 2017; Maher 2017; Roberts 2019; Rosenberg 2020), one in the UK (White 2017), and one in Japan (Owari 2019).
Participants
The included studies involved a total of 397 participants (n = 284 females). Sample size varied from 38 participants, Barone 2017, to 96, White 2017. Participants were recruited through senior centres and older adults community groups (Maher 2017; Owari 2019; Roberts 2019), database of volunteers affiliated with universities (Barone 2017; Lyons 2017), advertisements in media (Lyons 2017; Roberts 2019), and primary care (Rosenberg 2020; White 2017). Participants were majority female, ranging from 58%, Rosenberg 2020, to 85%, Lyons 2017. In all of the included studies but Owari 2019, participants were predominantly from a white ethnic background, ranging from 65%, Lyons 2017, to 86%, Rosenberg 2020. Education level ranged across the study groups, with those having reached degree/bachelor level between 35%, Rosenberg 2020, and 81%, Barone 2017. Body mass index (BMI) ranged from 28 kg/m2, Owari 2019, to 35.5 kg/m2, Rosenberg 2020. Overall, the study groups consisted of relatively young older adults, with mean age between 61 years, Lyons 2017, and 72 years, Roberts 2019. One study had a slightly older participant population, with an average age of 77 years old (Maher 2017).
Intervention content, duration, and delivery
Interventions in the included studies were behavioural interventions targeting individual behaviour. We found no studies attempting to alter or restructure the environment of participants, challenge social or cultural norms, or change policy. All but two studies, Barone 2017; Owari 2019, were reported to be designed based on behaviour change theories including social cognitive theory (Bandura 1986), transtheoretical model (Prochaska 1992), or habit formation (Schwarzer 2007). All of the included studies employed a range of behaviour change techniques such as goal setting, education, and behaviour monitoring or feedback. Self‐monitoring was used in all studies except Owari 2019 and Maher 2017, but varied considerably in the methods of self‐monitoring. Most studies provided participants with feedback on their behaviour, using activity monitors (Barone 2017; Lyons 2017; Roberts 2019; Rosenberg 2020). White 2017 provided only paper‐based means of self‐recording behaviour. Additionally, two studies provided haptic prompts triggered when participants were inactive for longer than a self‐selected period of time (Lyons 2017; Rosenberg 2020). Five studies provided individualised interventions with some element of continuous tailoring through regular revision of goal settings and one‐to‐one interaction with the intervention provider (Barone 2017; Lyons 2017; Maher 2017; Roberts 2019; Rosenberg 2020), whilst two studies provided one‐size‐fits‐all messages through a leaflet (Owari 2019; White 2017).
Intervention duration ranged from 12 weeks, Barone 2017; Lyons 2017; Rosenberg 2020, to 20 weeks, Roberts 2019. However, in some studies the intervention was via a single point of contact (Owari 2019; White 2017), or a couple of group workshops over two weeks (Maher 2017). Follow‐up measures postintervention ranged from one week, Maher 2017, to one year, Owari 2019.
Measurement of sedentary behaviour
The majority of studies used objective measures of sedentary behaviour. However, there was some heterogeneity regarding how these devices defined and classified sedentary behaviour. This included the use of accelerometers such as ActiGraph worn on the hip (Roberts 2019), with a cut point of 100 count per minutes to identify sedentary time; SenseWear worn as an arm band (Barone 2017); and Active Style Pro (Owari 2019), with sedentary time obtained from periods of time with energy expenditure ≤ 1.5 metabolic equivalents (METs). Other studies used inclinometer instruments such as activPAL, which are worn on the thigh to identify periods of sitting (Lyons 2017; Rosenberg 2020). The remaining studies used self‐report methods with single‐item instruments such as the International Physical Activity Questionnaire (IPAQ) and Measure of Older Adults' Sedentary Time (MOST) questionnaire (White 2017), or multiple items assessing time in specific sedentary behaviours such as reading or watching TV (Maher 2017). Only one study reported on breaks in sedentary behaviour (Rosenberg 2020).
Secondary outcomes
Four studies also measured secondary outcomes. Two studies measured change in physical function and balance using clinically validated methods such as the Short Physical Performance Battery (SPPB), repeated chair stand tests, and gait speed (Barone 2017; Rosenberg 2020). Two studies considered measures of physical fitness using the 6‐minute walk test (Lyons 2017; Roberts 2019). Three studies measured change in obesity markers: fat mass (Lyons 2017), waist circumference (Roberts 2019; Rosenberg 2020), and BMI (Rosenberg 2020). Three studies reported on blood pressure (Barone 2017; Roberts 2019; Rosenberg 2020). Finally, two studies also reported on blood markers of cardio‐metabolic health including levels of blood cholesterol, high‐density lipoprotein (HDL), low‐density lipoprotein (LDL), triglycerides, glucose, and glycated haemoglobin (Roberts 2019; Rosenberg 2020). Only one study investigated changes in quality of life and depression (Barone 2017). We found no studies investigating cost‐effectiveness or adverse events.
Excluded studies
We excluded 74 articles at the full‐text stage (Characteristics of excluded studies). The main reasons for exclusion were that the intervention delivered did not target sedentary behaviour (n = 29); the study sample did not meet our inclusion criteria (n = 24); study design was not RCT or cluster‐RCT (n = 15); sedentary time was not measured (n = 4); and finally one study compared two sedentary behaviour change interventions (Harvey 2018).
Risk of bias in included studies
Risk of bias varied across studies (Figure 2). No study was assessed as at low risk of bias for all domains (Figure 3), but three studies were assessed as at low risk of bias for six of the seven domains considered (Lyons 2017; Roberts 2019; Rosenberg 2020).
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
All of the included studies but Barone 2017 described using computer‐generated random sequences, therefore we assessed these studies as having a low risk of bias for this domain. Four studies described an adequate method of concealing the allocation to control or intervention group (Lyons 2017; Maher 2017; Rosenberg 2020; White 2017); the allocation in these studies was performed by an independent research administrator or researcher. The allocation procedure was unclear for Roberts 2019, and was performed by an unblinded researcher in Owari 2019. Barone 2017 did not describe randomisation and allocation procedures and was therefore judged as at high risk of bias for both sequence generation and allocation concealment domains.
Blinding
Performance bias was the most common source of bias across the included studies. Only one study blinded participants to allocation to the control of the sedentary behaviour intervention group (White 2017).
There were issues with blinding of outcome assessors. Three studies reported procedures to make the researcher responsible for data entry and analysis blind to group allocation (Owari 2019; Roberts 2019; Rosenberg 2020). In two studies the blinding of the assessor was not clearly described (Barone 2017; Maher 2017). Finally, two studies clearly stated that no blinding of the assessor was performed (Lyons 2017; White 2017).
Regarding outcome assessment (detection bias), five studies used an objective measurement of sedentary time and were therefore judged as at low risk of detection bias (Barone 2017; Lyons 2017; Owari 2019; Roberts 2019; Rosenberg 2020). We assessed both Maher 2017 and White 2017 as at high risk of detection bias because both studies used self‐reported methods of assessing sedentary time, with well know large bias issues (Chastin 2018).
Incomplete outcome data
Attrition rates were generally very low in all studies and were well documented and reported. All of the included studies but Rosenberg 2020 employed intention‐to‐treat analysis with adequate methods for handling missing data. Owari 2019 declared having analysed only data from participants with high adherence to the programme. We therefore judged all of the included studies as at low risk of attrition bias except Rosenberg 2020 and Owari 2019, which we classified as at high risk.
Selective reporting
Four studies fully reported on all the outcomes described in their protocols and methods and were therefore judged as at low risk of reporting bias (Maher 2017; Owari 2019; Roberts 2019; Rosenberg 2020). We judged White 2017 as high risk for this domain as outcomes declared in the methods section of the paper were not reported on in the results section. We judged Barone 2017 and Lyons 2017 as at unclear risk of reporting bias, as in the former some of the prespecified outcomes were only partially reported, and in the latter there was no protocol to compare original outcome measure choice.
Other potential sources of bias
We identified no other sources of bias in the seven included studies, which were therefore all judged as low risk for this domain.
Additional risk of bias domain for cluster‐RCTs
We assessed the single cluster‐RCT by Maher 2017 as low risk of bias for all domains except the baseline imbalance domain, which was judged as unclear because no information about baseline characteristics per clusters or condition was reported.
Effects of interventions
See: Table 1
The main comparison is reported in Table 1. Below we present results per outcome only for outcomes for which data were available. As explained in the Included studies section, we did not find data for all secondary outcomes we intended to review.
Primary outcomes
Sedentary time
We pooled results from all seven included studies for the effect of intervention versus control on sedentary time. Overall the evidence suggests that interventions to change sedentary behaviour may reduce sedentary time (mean difference (MD) −44.91 min/day, 95% confidence interval (CI) −93.13 to 3.32; 397 participants; 7 studies; I2 = 73%; Analysis 1.1; Figure 4). Subgroup analysis showed no significant difference in outcome between studies that measured sedentary time subjectively or objectively. However, precision was higher for studies that used objective measures of sedentary time with narrower confidence intervals but lower mean difference estimates. The subgroup analysis according to intervention duration showed no significant difference between interventions delivered as a single point of contact (MD ‐79.34 min/day, 95% CI ‐179.31 to 20.62) and those involving longitudinal contact with participants up to 20 weeks (MD −20.34 min/day, 95% CI −67.25 to 26.56).
1.1. Analysis.

Comparison 1: Intervention for reducing sedentary behaviour versus control: main outcomes, Outcome 1: Sedentary time [min/day]
4.

Forest plot of comparison between intervention to reduce sedentary behaviour and control. Plot also shows subgroup analysis per measurement method for sedentary time.
Overall the certainty of evidence was low due to inconsistencies and heterogeneity in results and imprecision with wide confidence intervals and small sample sizes (Table 1). It is likely that further research, particularly studies using objective measures of sedentary time, might change both effect estimates and our confidence in the evidence.
Time spent in specific sedentary behaviour
Only one study reported the effect of the intervention on time spent in specific sedentary behaviours such as TV time (Maher 2017). The difference between the intervention and control group for sedentary time in these domains is presented in Figure 5.
5.
Forest plot of comparison between intervention to reduce sedentary behaviour and control for time spent in specific sedentary behaviour [min/day].
Pattern of sedentary behaviour
Only one study reported the effect of intervention on breaks in sedentary behaviour (Rosenberg 2020). No statistically difference between groups in number of breaks in sedentary behaviour was observed in this study (MD −8.00 number of breaks (nbr)/day, 95% CI −16.8 to 0.8). No study investigated the distribution of sedentary bouts.
Secondary outcomes
The effects of sedentary behaviour interventions on secondary outcomes are summarised in Analysis 2.1; Analysis 2.2; Analysis 2.3; Analysis 3.1; Analysis 3.2; Analysis 3.3; Analysis 4.1; Analysis 5.1; Analysis 5.2; Analysis 6.1; Analysis 6.2; Analysis 6.3; Analysis 6.4; Analysis 6.5; Analysis 6.6; Analysis 7.1; Analysis 7.2; Analysis 7.3; Analysis 7.4; Analysis 7.5; Analysis 8.1.
2.1. Analysis.

Comparison 2: Intervention for reducing sedentary behaviour versus control: physical function outcomes, Outcome 1: SPPB
2.2. Analysis.

Comparison 2: Intervention for reducing sedentary behaviour versus control: physical function outcomes, Outcome 2: Gait speed
2.3. Analysis.

Comparison 2: Intervention for reducing sedentary behaviour versus control: physical function outcomes, Outcome 3: Chair stands (seconds)
3.1. Analysis.

Comparison 3: Intervention for reducing sedentary behaviour versus control: obesity outcomes, Outcome 1: BMI
3.2. Analysis.

Comparison 3: Intervention for reducing sedentary behaviour versus control: obesity outcomes, Outcome 2: Waist circumference (cm)
3.3. Analysis.

Comparison 3: Intervention for reducing sedentary behaviour versus control: obesity outcomes, Outcome 3: Body fat (%)
4.1. Analysis.

Comparison 4: Intervention for reducing sedentary behaviour versus control: fitness outcomes, Outcome 1: 6‐minute walk (metres)
5.1. Analysis.

Comparison 5: Intervention for reducing sedentary behaviour versus control: blood pressure outcomes, Outcome 1: Systolic [mmHg]
5.2. Analysis.

Comparison 5: Intervention for reducing sedentary behaviour versus control: blood pressure outcomes, Outcome 2: Diastolic [mmHg]
6.1. Analysis.

Comparison 6: Intervention for reducing sedentary behaviour versus control: cardiometabolic markers outcomes, Outcome 1: Cholesterol [mg/dL]
6.2. Analysis.

Comparison 6: Intervention for reducing sedentary behaviour versus control: cardiometabolic markers outcomes, Outcome 2: HDL [mg/dL]
6.3. Analysis.

Comparison 6: Intervention for reducing sedentary behaviour versus control: cardiometabolic markers outcomes, Outcome 3: LDL [mg/dL]
6.4. Analysis.

Comparison 6: Intervention for reducing sedentary behaviour versus control: cardiometabolic markers outcomes, Outcome 4: Triglycerides [mg/dL]
6.5. Analysis.

Comparison 6: Intervention for reducing sedentary behaviour versus control: cardiometabolic markers outcomes, Outcome 5: Glucose [mg/dL]
6.6. Analysis.

Comparison 6: Intervention for reducing sedentary behaviour versus control: cardiometabolic markers outcomes, Outcome 6: Glycated haemoglobin
7.1. Analysis.

Comparison 7: Intervention for reducing sedentary behaviour versus control: quality of life, Outcome 1: SF‐36 Physical function
7.2. Analysis.

Comparison 7: Intervention for reducing sedentary behaviour versus control: quality of life, Outcome 2: SF‐36 Energy
7.3. Analysis.

Comparison 7: Intervention for reducing sedentary behaviour versus control: quality of life, Outcome 3: SF‐36 Emotional well‐being
7.4. Analysis.

Comparison 7: Intervention for reducing sedentary behaviour versus control: quality of life, Outcome 4: SF‐36 Pain
7.5. Analysis.

Comparison 7: Intervention for reducing sedentary behaviour versus control: quality of life, Outcome 5: SF‐36 General health
8.1. Analysis.

Comparison 8: Intervention for reducing sedentary behaviour versus control: depression, Outcome 1: Depression (Center for Epidemiological Studies‐Depression (CES‐D))
Physical function
We pooled two studies that reported on physical function using the Short Physical Performance Battery (SPPB) (MD 0.14, 95% CI −0.38 to 0.66; 98 participants; 2 studies; I2 = 26%) (Barone 2017; Rosenberg 2020). We also pooled two studies that reported gait speed at follow‐up, which is an important marker of physical function (MD 0.02 m/s, 95% CI −0.04 to 0.09; 98 participants; 2 studies; I2 = 0%) (Barone 2017; Rosenberg 2020). It is uncertain if interventions to reduce sedentary time impact physical function of older adults, as the certainty of evidence was low due to very small sample sizes.
Physical fitness
We pooled the results of the two studies that measured fitness using the 6‐minute walk test at follow‐up (MD −5.16 m, 95% CI −36.49 to 26.17; 80 participants; 2 studies; I2 = 29%) (Lyons 2017; Roberts 2019). It is uncertain if interventions to reduce sedentary time impact the physical fitness of older adults, as the certainty of evidence was low due to very small sample sizes.
Body composition
We pooled the results of the two studies that measured waist circumference at follow‐up (MD 1.14 cm, 95% CI −1.64 to 3.93; 100 participants; 2 studies; I2 = 0%) (Barone 2017; Rosenberg 2020). It is uncertain if interventions to reduce sedentary time impact the body composition of older adults, as the certainty of evidence was low due to very small sample sizes.
Blood pressure
We pooled the results of the three studies that measured blood pressure at follow‐up (Barone 2017; Roberts 2019; Rosenberg 2020). Pooled estimates were as follows: systolic blood pressure (MD −3.91 mmHg, 95% CI −10.95 to 3.13; 138 participants; 3 studies; I2 = 73%) and diastolic blood pressure (MD −0.06 mmHg, 95% CI −5.72 to 5.60; 138 participants; 3 studies; I2 = 97%). The certainty of evidence for this outcome was very low due inconsistency and imprecision, therefore it is uncertain if interventions to reduce sedentary time impact the blood pressure of older adults.
Blood markers of cardiometabolic health
We pooled the results of the two studies (100 participants) that examined blood markers of cardiometabolic health at follow‐up (Roberts 2019; Rosenberg 2020). There was no difference between groups in total cholesterol (MD 3.25 mg/dL, 95% CI −9.52 to 16.03), HDL cholesterol (MD −2.47 mg/dL, 95% CI −7.40 to 2.45), LDL cholesterol (MD 4.17 mg/dL, 95% CI −6.89 to 15.22), triglycerides (MD 2.13 mg/dL, 95% CI −18.95 to 23.21), and glucose (MD 2.20 mg/dL, 95% CI −6.46 to 10.86). We rated the certainty of evidence for all these outcomes as low due to very small sample sizes.
Quality of life
Barone 2017 reported no difference between groups in quality of life at follow‐up as measured by any of the domains of the 36‐item Short Form Health Survey (SF‐36) (Physical function, Energy/Fatigue, Pain, Emotional well‐being, General health).
Cognitive function
No data were reported for this outcome.
Depression
Barone 2017 reported no difference between groups in depressive symptoms at follow‐up.
Cost‐effectiveness
No data were reported for this outcome.
Adverse events
No data were reported for this outcome.
Discussion
Summary of main results
We included seven studies in this review. A summary of findings for the primary outcome of sedentary time is provided in Table 1. It is not clear whether interventions targeting sedentary behaviour in community‐dwelling older adults reduce sedentary time, as the certainty of evidence is low. We only found one study reporting on breaks in sedentary behaviour and one reporting on sedentary time in different domains such as TV time.
It is also unclear if interventions to reduce sedentary time in community‐dwelling older adults impact their physical function, body composition, fitness, blood pressure, and blood markers of lipidaemia and glycaemia. We only found one study reporting on quality of life and depression. We found no data on cost‐effectiveness or adverse effects.
All of the interventions evaluated were delivered at the individual level, and none considered changing the environment, policies, or social and cultural norms surrounding older adults. The majority of interventions used a combination of behaviour change techniques and included information, education, counselling, goal setting, feedback (including from wearable technology and apps), prompts including just‐in‐time haptic prompts, workshops, short message service (SMS) texts, and phone calls. These were delivered in the community setting. Data on adherence, fidelity, intensity, and frequency of the intervention were not available.
Overall completeness and applicability of evidence
The majority of recruited participants were female, white, overweight, and highly educated, and were overall relatively younger older adults. In addition, all studies were conducted in high‐income countries. It is therefore unclear if these types of interventions could be effective in other groups of community‐dwelling older adults. The currently available literature is insufficient to address all of our objectives for this review. We could not investigate two of the primary outcomes: breaks in sedentary behaviour and sedentary time in specific domains, as these were reported in only one study. There were very few data for our secondary outcomes. Functional capacity, blood markers of cardiometabolic health, and fitness were reported in only two studies, and only three studies reported on blood pressure. We could not meta‐analyse and investigate depression and quality of life, as these were reported in only one study, and no data were reported for cost‐effectiveness or adverse events.
Quality of the evidence
The currently available body of evidence does not permit a robust answer to the research questions of this review. We assessed the certainty of evidence for sedentary time as low according to GRADE considering all seven studies and 397 participants included. This result combined evidence from studies using self‐reported measures of sedentary time as well as those using device‐based measures. None of the studies was considered to be at overall low risk of bias, and sample sizes were small and confidence intervals large for sedentary time.
Potential biases in the review process
The main limitation of this review is the potential for publication bias. We were not able to assess the risk of publication bias using funnel plots or other methods due to there being an insufficient number of studies. Studies with negative results may not have been published. It is therefore possible that the current evidence base identified might overrepresent studies with positive results. We attempted to minimise this by contacting experts in the field and by searching trial registries to identify potential studies that might not have been published. Together with handsearching reference lists, this increased the likelihood of identifying all relevant studies.
There is also the potential for bias in review processes such as assessing risk of bias and certainty of evidence using GRADE. These include the potential for subjectivity, as they involve personal judgements. We tried to keep this to a minimum by having two review authors conduct these assessments independently and by putting in place a system to mitigate disagreement. We furthermore excluded review authors from taking part in this process for any included studies on which they were an author, and we have declared this openly below.
Agreements and disagreements with other studies or reviews
This is the first review and meta‐analysis of interventions specifically targeting sedentary behaviour in community‐dwelling older adults. This review is important, as older adults are the most sedentary segment of the population, spending around 80% of their waking day sedentary.
There is only one narrative review focusing on community‐dwelling older adults to date (Aunger 2019). This review included six studies consisting of a single RCT and five feasibility studies. It concluded that changing sedentary behaviour in older adults up to one hour per day appeared to be feasible in the very short term (less than eight weeks), but that the evidence base was very limited and lacked experimental evidence on clinical outcomes, such as physical function and cardiometabolic health. Conducting RCTs to reduce sedentary behaviour in older adults is feasible but does not substantiate claims about potential effect size. The experimental evidence is still too uncertain to provide robust conclusions about the impact of reduction in sedentary time on clinical outcomes.
Authors' conclusions
Implications for practice.
It is currently unclear whether interventions are effective in changing sedentary behaviour in community‐dwelling older adults. The evidence suggests that these interventions may reduce sedentary time. We were not able to draw any conclusions about the effectiveness of specific components of these interventions, or about the balance of benefits or harms and cost‐effectiveness. It is also unclear whether interventions to reduce sedentary time have an impact on the physical and mental health of community‐dwelling older adults. In summary, there is currently insufficient evidence to support decisions by policymakers and practitioners to recommend or implement interventions to reduce sedentary behaviour in community‐dwelling older adults.
Implications for research.
There is a clear need for higher‐quality randomised controlled trials assessing the impact of intervention to reduce sedentary behaviour in community‐dwelling older adults to improve the evidence base. To improve the certainty of the evidence, several factors need to be considered. Future studies should use device‐based measures, particularly devices that recognise posture (Chastin 2010), as they improve precision but also allow for outcome assessment blinding. In addition, future studies should measure and assess the change in patterns of sedentary behaviour, including breaks in prolonged sedentary behaviour, as well as total volume (Chastin 2015c). Larger trials are also required to improve upon precision.
In order to broaden the applicability of the evidence, future studies should recruit more varied samples in terms of age, gender, ethnicity, and socioeconomic background. More importantly, future research should examine the impact of modifying the environment, policy, and cultural social norms. None of the interventions included in this review attempted to modify these more distal determinants of sedentary behaviour. Future research should investigate the effect of intervention modifying factors included in the six clusters of the Determinants of Diet and Physical Activity (DEDIPAC) systems of sedentary behaviour (Chastin 2016). Research on the potential effects of modifying the built environment and home settings should be prioritised, as recent research suggests that this might be the most promising avenue for lasting change in sedentary behaviour amongst older adults (Buck 2019).
Whilst feasibility studies have shown that it is feasible to change sedentary behaviour in older adults, this review suggests that there is little to no effect compared to control. It is therefore possible that better implementation is needed. It has recently been suggested that co‐creation and participatory design might lead to more effective interventions (Leask 2017), therefore future research should investigate co‐created intervention to reduce sedentary behaviour in older adults. Patient‐valued outcomes are important, and more research is needed to understand what outcomes are important to older people (Dogra 2012).
In addition, studies should record key information such as quality of life, cost‐effectiveness, and adverse event data to permit a benefit‐to‐harm analysis. Finally, there should be a more systematic recording of intervention component frequency and intensity, using systematic methodology such as Perera 2007.
History
Protocol first published: Issue 9, 2017
Acknowledgements
The authors wish to acknowledge the editorial team of the Cochrane Public Health Group, in particular Jodie Doyle for her help and patience, and the librarians at Glasgow Caledonian University and University of Queensland; Lars Eriksson and Julie Hansen who will create and execute the search strategies for the electronic databases. No funding was used to prepare this protocol and review. We also would like to thank members of the original team who have left since the development of the protocol.
Appendices
Appendix 1. Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
The following search was conducted in the Cochrane Central Register of Controlled Trials on 8 April 2019.
1. (Elderly OR Senior OR seniors OR "older adult" OR "older adults" OR geriatric OR geriatrics OR “old people” OR older‐age OR “old age” OR adult OR adults OR “older people”):ti
2. (Elderly OR Senior OR seniors OR "older adult" OR "older adults" OR geriatric OR geriatrics OR “old people” OR older‐age OR “old age” OR adult OR adults OR “older people”):ab
3. #1 OR #2
4. MeSH descriptor: [Aged] explode all trees
5. MeSH descriptor: [Aged, 80 and over]
6. #3 OR #4 OR #5
7. MeSH descriptor: [Automobile Driving] explode all trees
8. MeSH descriptor: [Television] explode all trees
9. MeSH descriptor: [Sedentary Behavior] explode all trees
10. MeSH descriptor: [Computers] explode all trees
11. MeSH descriptor: [Video Games] explode all trees
12. (“screen behavior” OR “screen behaviour” OR “screen entertainment” OR “screen time” OR “screen watching” OR “screen‐based entertainment” OR “sedentary behavior*” OR “sedentary behaviour*” OR “sedentary lifestyle*” OR “sitting time” OR “television time” OR “television viewing” OR “television watching” OR “TV time” OR “TV viewing” OR “TV watching” OR “video game time” OR “video game” OR “video gaming” OR “view television” OR “watch television” OR “watch TV”):ti
13. (“screen behavior” OR “screen behaviour” OR “screen entertainment” OR “screen time” OR “screen watching” OR “screen‐based entertainment” OR “sedentary behavior*” OR “sedentary behaviour*” OR “sedentary lifestyle*” OR “sitting time” OR “television time” OR “television viewing” OR “television watching” OR “TV time” OR “TV viewing” OR “TV watching” OR “video game time” OR “video game” OR “video gaming” OR “view television” OR “watch television” OR “watch TV”):ab
14. #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13
15. #6 AND #14
The above search was repeated in the Cochrane Central Register of Controlled Trials on 18 January 2021 with limits on Publication Year from 2019 to 2021, with Cochrane Library publication date Between Apr 2019 and Jan 2021, in Trials
Appendix 2. MEDLINE search strategy
The following search was conducted in MEDLINE through PubMed on 8 April 2019.
((randomized controlled trial[pt] OR controlled clinical trial[pt] OR randomized[tiab] OR placebo[tiab] OR clinical trials as topic[mesh:noexp] OR randomly[tiab] OR trial[ti] OR "program evaluation"[Mesh] OR intervention*[ti] OR evaluation[ti] OR controlled trial[tiab] OR quasi‐experiment[tiab] OR feasibility[ti] OR health promotion[tiab] OR Health education[tiab] OR environmental design[tiab] OR environmental restructuring[tiab] OR evaluation studies[pt] OR "evaluation studies as topic"[mesh:noexp] OR (pre‐test[tiab] AND post‐test[tiab]) OR (pretest[tiab] AND posttest[tiab]) OR (program evaluation[tiab] OR effectiveness[ti])) AND (Elderly[tiab] OR Senior[tiab] OR seniors[tiab] OR older adult[tiab] OR older adults[tiab] OR elderly[tiab] OR geriatric[tiab] OR geriatrics[tiab] OR old people[tiab] OR older‐age[tiab] OR "aged"[Mesh] OR "aged, 80 and over"[Mesh] OR old age[tiab] OR adult[tiab] OR adults[tiab] OR older people[tiab]) AND ("Automobile Driving"[Mesh:noexp] OR "Television"[Mesh] OR video gaming[tiab] OR video game[tiab] OR computer gaming[tiab] OR video game time[tiab] OR computer game[tiab] OR "computers"[Mesh] OR "Video Games"[Mesh] OR screen time[tiab] OR screen entertainment[tiab] OR screen behaviour[tiab] OR screen behavior[tiab] OR screen‐based entertainment[tiab] OR television viewing[tiab] OR television watching[tiab] OR television time[tiab] OR TV viewing[tiab] OR TV watching[tiab] OR TV time[tiab] OR watch television[tiab] OR view television[tiab] OR watch TV[tiab] OR screen watching[tiab] OR screen time[tiab] OR screen entertainment[tiab] OR screen behaviour[tiab] OR screen behavior[tiab] OR screen‐based entertainment[tiab] OR sedentary behavior[tiab] OR sedentary behaviour[tiab] OR sedentary lifestyle[tiab] OR prolonged sitting[tiab] OR sitting time[tiab] OR lying time[tiab] OR "sedentary lifestyle"[MeSH]))
This search was re‐run on 18 January 2021 to include "Sedentary Behavior"[Mesh] with the publication date range of "1946/01/01"[Date ‐ Publication]: "2019/04/01"[Date ‐ Publication]"
The following search was conducted in MEDLINE through PubMed on 18 January 2021.
(((("randomized controlled trials as topic "[MeSH Terms] OR "Random Allocation"[MeSH Terms] OR "clinical trial, phase i"[Publication Type] AND "clinical trial, phase ii"[Publication Type] OR "clinical trial, phase iii"[Publication Type] OR "clinical trial, phase iv"[Publication Type] OR "controlled clinical trial"[Publication Type] OR "randomized controlled trial"[Publication Type] OR "multicenter study"[Publication Type] OR "clinical trial"[Publication Type] OR "Clinical Trials as topic"[MeSH Terms] OR randomized[tiab] OR randomised[tiab] OR placebo[tiab] OR randomly[tiab] OR trial[ti])) AND (Elderly[tiab] OR Senior[tiab] OR seniors[tiab] OR older adult[tiab] OR older adults[tiab] OR geriatric[tiab] OR geriatrics[tiab] OR old people[tiab] OR older‐age[tiab] OR "aged"[Mesh] OR "aged, 80 and over"[Mesh] OR old age[tiab] OR adult[tiab] OR adults[tiab] OR older people[tiab])) AND ("Automobile Driving"[Mesh:noexp] OR "computers"[Mesh] OR "Sedentary Behavior"[Mesh] OR "Television"[Mesh] OR "Video Games"[Mesh] OR “computer game*”[tiab] OR “computer gaming”[tiab] OR “lying time”[tiab] OR “prolonged sitting”[tiab] OR “physical inactivity”[tiab] OR “physically inactive”[tiab] OR Inactive[ti] OR “screen behavior”[tiab] OR “screen behaviour”[tiab] OR “screen entertainment”[tiab] OR “screen time”[tiab] OR “screen watching”[tiab] OR “screen‐based entertainment”[tiab] OR sedentary[ti] OR “sedentary behavior*”[tiab] OR “sedentary behaviour*”[tiab] OR “sedentary lifestyle*”[tiab] OR “sitting time”[tiab] OR “television time”[tiab] OR “television viewing”[tiab] OR “television watching”[tiab] OR “TV time”[tiab] OR “TV viewing”[tiab] OR “TV watching”[tiab] OR “video game time”[tiab] OR “video game”[tiab] OR “video gaming”[tiab] OR “view television”[tiab] OR “watch television”[tiab] OR “watch TV”[tiab])) AND (("2019/04/01"[Date ‐ Publication]: "2021/01/18"[Date ‐ Publication]))
PubMed was searched from 01/01/1946 ‐ 18/01/2021
Appendix 3. CINAHL search strategy
The following search was conducted in CINAHL via Ebscohost on 8 April 2019.
1. “randomized controlled trial” OR “controlled clinical trial” OR randomized OR placebo OR MH "Clinical Trials+" OR randomly OR TI trial OR MH "Program Evaluation" OR TI intervention* OR TI evaluation OR controlled trial OR quasi‐experiment* OR TI feasibility OR “health promotion” OR “Health education” OR “environmental design” OR “environmental restructuring” OR “evaluation studies” OR (TI “pre‐test” AND TI “post‐test”) OR (TI pretest AND TI posttest) OR (AB “pre‐test” AND AB “post‐test”) OR (AB pretest AND AB posttest) OR “program evaluation” OR TI effectiveness OR MH "Evaluation Research"
2. Elderly OR TI Senior OR seniors OR “older adult” OR “older adults” OR elderly OR geriatric OR geriatrics OR “old people” OR “older‐age” OR MH "Aged+" OR MH "Aged, 80 and Over" OR MH "Aging+" OR “old age” OR TI adult OR TI adults OR AB adult OR AB adults OR “older people”
3. MH "Automobile Driving" OR MH "Television" OR “video gaming” OR “video game” OR “computer gaming” OR “video game time” OR “computer game” OR MH "Computers and Computerization Utilization" OR MH "Video Games" OR “screen time” OR “screen entertainment” OR “screen behavior” OR “screen behavior” OR “screen‐based entertainment” OR “television viewing” OR “television watching” OR “television time” OR “TV viewing” OR “TV watching” OR “TV time” OR “watch television” OR “view television” OR “watch TV” OR “screen watching” OR “screen time” OR “screen entertainment” OR “screen behavior” OR “screen behavior” OR “screen‐based entertainment” OR “sedentary behavior” OR “sedentary behavior” OR “sedentary lifestyle” OR “prolonged sitting” OR “sitting time” OR “lying time” OR MH "Life Style, Sedentary+"
4. #1 AND #2 AND #3
The following search was conducted in CINAHL via Ebscohost on 4 June 2020.
1. MH "Random Assignment” OR MH "Clinical Trials+" OR "randomized controlled trials as topic "[MeSH Terms] OR MH "Multicenter Studies" OR “randomized controlled trial” OR “controlled clinical trial” OR randomized OR placebo OR MH "Clinical Trials+" OR randomly OR TI trial
2. Elderly OR TI Senior OR seniors OR “older adult” OR “older adults” geriatric OR geriatrics OR “old people” OR “older‐age” OR MH "Aged+" OR MH "Aged, 80 and Over" OR MH "Aging+" OR “old age” OR TI adult OR TI adults OR AB adult OR AB adults OR “older people”
3. “computer game” OR “computer gaming” OR “lying time” OR “physical inactivity” OR “physically inactive” OR “prolonged sitting” OR “screen behavior” OR “screen behaviour” OR “screen entertainment” OR “screen time” OR “screen watching” OR “screen‐based entertainment” OR “sedentary behavior*” OR “sedentary behaviour*” OR “sedentary lifestyle*” OR “sitting time” OR “television time” OR “television viewing” OR “television watching” OR “TV time” OR “TV viewing” OR “TV watching” OR “video game time” OR “video game” OR “video gaming” OR “view television” OR “watch television” OR “watch TV” OR MH "Automobile Driving" OR MH "Computers and Computerization Utilization" OR MH "Life Style, Sedentary+" OR MH "Television" OR MH "Video Games" OR TI Inactive OR TI sedentary
4. #1 AND #2 AND #3 Limiters ‐ Published Date: 20190401‐20200631; Language: English Database ‐ CINAHL
The following search was conducted in CINAHL via Ebscohost on 3 August 2020.
1. MH "Random Assignment” OR MH "Clinical Trials+" OR "randomized controlled trials as topic "[MeSH Terms] OR MH "Multicenter Studies" OR “randomized controlled trial” OR “controlled clinical trial” OR randomized OR placebo OR MH "Clinical Trials+" OR randomly OR TI trial
2. Elderly OR TI Senior OR seniors OR “older adult” OR “older adults” geriatric OR geriatrics OR “old people” OR “older‐age” OR MH "Aged+" OR MH "Aged, 80 and Over" OR MH "Aging+" OR “old age” OR TI adult OR TI adults OR AB adult OR AB adults OR “older people”
3. “computer game” OR “computer gaming” OR “lying time” OR “physical inactivity” OR “physically inactive” OR “prolonged sitting” OR “screen behavior” OR “screen behaviour” OR “screen entertainment” OR “screen time” OR “screen watching” OR “screen‐based entertainment” OR “sedentary behavior*” OR “sedentary behaviour*” OR “sedentary lifestyle*” OR “sitting time” OR “television time” OR “television viewing” OR “television watching” OR “TV time” OR “TV viewing” OR “TV watching” OR “video game time” OR “video game” OR “video gaming” OR “view television” OR “watch television” OR “watch TV” OR MH "Automobile Driving" OR MH "Computers and Computerization Utilization" OR MH "Life Style, Sedentary+" OR MH "Television" OR MH "Video Games" OR TI Inactive OR TI sedentary
4. #1 AND #2 AND #3 Limiters ‐ Published Date: 19660101‐20190431; Language: English
Searches 2 and 3 were re‐run on January 18 2021 without the English limit.
CINAHL was searched from 01/01/1966 ‐ 18/01/2021.
Appendix 4. Embase search strategy
The following search was conducted in EMBASE on 8 April 2019.
1. 'randomized controlled trial'/exp OR 'randomized controlled trial (topic)'/exp OR 'randomization'/exp OR 'phase 1 clinical trial'/exp OR 'phase 2 clinical trial'/exp OR 'phase 3 clinical trial'/exp OR 'phase 4 clinical trial'/exp OR 'controlled clinical trial'/exp OR 'multicenter study'/exp OR 'clinical trial'/exp OR randomized;ti,ab OR randomised;ti,ab OR placebo;ti,ab OR randomly;ti,ab OR trial:ti
2. elderly:ti,ab OR senior:ti,ab OR seniors:ti,ab OR 'older adult':ti,ab OR 'older adults':ti,ab OR geriatric:ti,ab OR geriatrics:ti,ab OR 'old people':ti,ab OR 'older‐age':ti,ab OR 'aged'/exp OR 'very elderly'/exp OR 'old age':ti,ab OR adult:ti,ab OR adults:ti,ab OR 'older people':ti,ab
3. 'computer game':ti,ab OR 'computer gaming':ti,ab OR 'lying time':ti,ab OR 'physical inactivity':ti,ab OR 'physically inactive':ti,ab OR inactive:ti,ab OR 'prolonged sitting':ti,ab OR 'screen behavior':ti,ab OR 'screen behaviour':ti,ab OR 'screen entertainment':ti,ab OR 'screen time':ti,ab OR 'screen watching':ti,ab OR 'screen‐based entertainment':ti,ab OR 'sedentary behavior':ti,ab OR 'sedentary behaviour':ti,ab OR 'sedentary lifestyle':ti,ab OR 'sitting time':ti,ab OR 'television time':ti,ab OR 'television viewing':ti,ab OR 'television watching':ti,ab OR 'tv time':ti,ab OR 'tv viewing':ti,ab OR 'tv watching':ti,ab OR 'video game time':ti,ab OR 'video game':ti,ab OR 'video gaming':ti,ab OR 'view television':ti,ab OR 'watch television':ti,ab OR 'watch tv':ti,ab OR 'car driving'/exp OR 'computer'/exp OR 'sedentary lifestyle'/exp OR 'television'/exp OR 'video game'/exp
4. #1 AND #2 AND #3
The following search was conducted in EMBASE on 4 June 2020.
1. 'randomized controlled trial'/exp OR 'randomized controlled trial (topic)'/exp OR 'randomization'/exp OR 'phase 1 clinical trial'/exp OR 'phase 2 clinical trial'/exp OR 'phase 3 clinical trial'/exp OR 'phase 4 clinical trial'/exp OR 'controlled clinical trial'/exp OR 'multicenter study'/exp OR 'clinical trial'/exp OR randomized;ti,ab OR randomised;ti,ab OR placebo;ti,ab OR randomly;ti,ab OR trial:ti
2. elderly:ti,ab OR senior:ti,ab OR seniors:ti,ab OR 'older adult':ti,ab OR 'older adults':ti,ab OR geriatric:ti,ab OR geriatrics:ti,ab OR 'old people':ti,ab OR 'older‐age':ti,ab OR 'aged'/exp OR 'very elderly'/exp OR 'old age':ti,ab OR adult:ti,ab OR adults:ti,ab OR 'older people':ti,ab
3. 'computer game':ti,ab OR 'computer gaming':ti,ab OR 'lying time':ti,ab OR 'physical inactivity':ti,ab OR 'physically inactive':ti,ab OR inactive:ti,ab OR 'prolonged sitting':ti,ab OR 'screen behavior':ti,ab OR 'screen behaviour':ti,ab OR 'screen entertainment':ti,ab OR 'screen time':ti,ab OR 'screen watching':ti,ab OR 'screen‐based entertainment':ti,ab OR 'sedentary behavior':ti,ab OR 'sedentary behaviour':ti,ab OR 'sedentary lifestyle':ti,ab OR 'sitting time':ti,ab OR 'television time':ti,ab OR 'television viewing':ti,ab OR 'television watching':ti,ab OR 'tv time':ti,ab OR 'tv viewing':ti,ab OR 'tv watching':ti,ab OR 'video game time':ti,ab OR 'video game':ti,ab OR 'video gaming':ti,ab OR 'view television':ti,ab OR 'watch television':ti,ab OR 'watch tv':ti,ab OR 'car driving'/exp OR 'computer'/exp OR 'sedentary lifestyle'/exp OR 'television'/exp OR 'video game'/exp
4. #1 AND #2 AND #3 AND [english]/lim AND [embase]/lim AND [1‐4‐2019]/sd NOT [5‐6‐2020]/sd AND ([article]/lim OR [article in press]/lim OR [review]/lim)
The second search was re‐run on 18 January 2021 without the English language limit.
EMBASE was searched from 01/01/1980 ‐ 18/01/2021
Appendix 5. PsycINFO search strategy
The following search was conducted in PsycINFO on 8 April 2019.
(((((title: ("randomized controlled trial"))) OR ((title: ("controlled clinical trial"))) OR ((title: (randomized))) OR ((title: (placebo))) OR ((title: (randomly))) OR ((title: (trial))) OR ((title: (intervention*))) OR ((title: (evaluation))) OR ((title: (controlled trial))) OR ((title: (quasi‐experiment*))) OR ((title: (feasibility))) OR ((title: ("health promotion"))) OR ((title: ("Health education"))) OR ((title: ("environmental design"))) OR ((title: ("environmental restructuring"))) OR ((title: ("evaluation studies"))) OR (((title: ("pre‐test"))) AND ((title: ("post‐test")))) OR (((title: (pretest))) AND ((title: (posttest)))) OR (((title: ("pre‐test"))) AND ((title: ("post‐test")))) OR (((title: (pretest))) AND ((title: (posttest)))) OR ((title: ("program evaluation"))) OR ((title: (effectiveness)))) OR ((((abstract: ("randomized controlled trial"))) OR ((abstract: ("controlled clinical trial"))) OR ((abstract: (randomized))) OR ((abstract: (placebo))) OR ((abstract: (randomly))) OR ((title: (trial))) OR ((title: (intervention*))) OR ((title: (evaluation))) OR ((abstract: (controlled trial))) OR ((abstract: (quasi‐experiment*))) OR ((title: (feasibility))) OR ((abstract: ("health promotion"))) OR ((abstract: ("Health education"))) OR ((abstract: ("environmental design"))) OR ((abstract: ("environmental restructuring"))) OR ((abstract: ("evaluation studies"))) OR (((abstract: ("pre‐test"))) AND ((abstract: ("post‐test")))) OR (((abstract: (pretest))) AND ((abstract: (posttest)))) OR (((abstract: ("pre‐test"))) AND ((abstract: ("post‐test")))) OR (((abstract: (pretest))) AND ((abstract: (posttest)))) OR ((abstract: ("program evaluation"))) OR ((title: (effectiveness)))) OR ((((IndexTermsFilt: ("Clinical Trials"))))) OR ((((IndexTermsFilt: ("Program Evaluation"))))))) AND ((((title: (Elderly)) OR (title: (Senior)) OR (title: (seniors)) OR (title: (older adult)) OR (title: (older adults)) OR (title: (elderly)) OR (title: (geriatric)) OR (title: (geriatrics)) OR (title: ("old people")) OR (title: (older‐age)) OR (title: ("old age")) OR (title: (adult)) OR (title: (adults)) OR (title: ("older people")))) OR (((abstract: (Elderly)) OR (abstract: (Senior)) OR (abstract: (seniors)) OR (abstract: (older adult)) OR (abstract: (older adults)) OR (abstract: (elderly)) OR (abstract: (geriatric)) OR (abstract: (geriatrics)) OR (abstract: ("old people")) OR (abstract: (older‐age)) OR (abstract: ("old age")) OR (abstract: (adult)) OR (abstract: (adults)) OR (abstract: ("older people"))))) AND ((((((IndexTermsFilt: ("Computer Games"))))) OR ((((IndexTermsFilt: ("Computers"))))) OR ((((IndexTermsFilt: ("Drivers"))))) OR ((((IndexTermsFilt: ("Sedentary Behavior"))))) OR ((((IndexTermsFilt: ("Television Viewing"))))) OR ((((title: ("video gaming"))) OR ((title: ("video game"))) OR ((title: ("computer gaming"))) OR ((title: ("video game time"))) OR ((title: ("computer game"))) OR ((title: ("screen time"))) OR ((title: ("screen entertainment"))) OR ((title: ("screen behavior"))) OR ((title: ("screen behavior"))) OR ((title: ("screen‐based entertainment"))) OR ((title: ("television viewing"))) OR ((title: ("television watching"))) OR ((title: ("television time"))) OR ((title: ("TV viewing"))) OR ((title: ("TV watching"))) OR ((title: ("TV time"))) OR ((title: ("watch television"))) OR ((title: ("view television"))) OR ((title: ("watch TV"))) OR ((title: ("screen watching"))) OR ((title: ("screen time"))) OR ((title: ("screen entertainment"))) OR ((title: ("screen behavior"))) OR ((title: ("screen behavior"))) OR ((title: ("screen‐based entertainment"))) OR ((title: ("sedentary behavior"))) OR ((title: ("sedentary behavior"))) OR ((title: ("sedentary lifestyle"))) OR ((title: ("prolonged sitting"))) OR ((title: ("sitting time"))) OR ((title: ("lying time")))))) OR ((((abstract: ("video gaming"))) OR ((abstract: ("video game"))) OR ((abstract: ("computer gaming"))) OR ((abstract: ("video game time"))) OR ((abstract: ("computer game"))) OR ((abstract: ("screen time"))) OR ((abstract: ("screen entertainment"))) OR ((abstract: ("screen behavior"))) OR ((abstract: ("screen behavior"))) OR ((abstract: ("screen‐based entertainment"))) OR ((abstract: ("television viewing"))) OR ((abstract: ("television watching"))) OR ((abstract: ("television time"))) OR ((abstract: ("TV viewing"))) OR ((abstract: ("TV watching"))) OR ((abstract: ("TV time"))) OR ((abstract: ("watch television"))) OR ((abstract: ("view television"))) OR ((abstract: ("watch TV"))) OR ((abstract: ("screen watching"))) OR ((abstract: ("screen time"))) OR ((abstract: ("screen entertainment"))) OR ((abstract: ("screen behavior"))) OR ((abstract: ("screen behavior"))) OR ((abstract: ("screen‐based entertainment"))) OR ((abstract: ("sedentary behavior"))) OR ((abstract: ("sedentary behavior"))) OR ((abstract: ("sedentary lifestyle"))) OR ((abstract: ("prolonged sitting"))) OR ((abstract: ("sitting time"))) OR ((abstract: ("lying time")))))))
The following search was conducted in PsycINFO on 5 June 2020. The search was limited to publication year 2019 to 2020.
((Index Terms: ("video gaming") OR Index Terms: ("Computer Games") OR Index Terms: ("Computers") OR Index Terms: ("drivers") OR Index Terms: ("Sedentary Behavior") OR Index Terms: ("Television Viewing")) OR (title: ("video game") OR title: ("computer gaming") OR title: ("video game time") OR title: ("computer game") OR title: ("screen time") OR title: ("screen entertainment") OR title: ("screen behavior") OR title: ("screen behavior") OR title: ("screen‐based entertainment") OR title: ("television viewing") OR title: ("television watching") OR title: ("television time") OR title: ("TV viewing") OR title: ("TV watching") OR title: ("TV time") OR title: ("watch television") OR title: ("view television") OR title: ("watch TV") OR title: ("screen watching") OR title: ("screen time") OR title: ("screen entertainment") OR title: ("screen behavior") OR title: ("screen behaviour") OR title: ("screen‐based entertainment") OR title: ("sedentary behavior*") OR title: ("sedentary behaviour*") OR title: ("sedentary lifestyle*") OR title: ("prolonged sitting") OR title: ("sitting time") OR title: ("lying time") OR title: ("physical inactivity") OR title: ("physically inactive")) OR (abstract: ("video game") OR abstract: ("computer gaming") OR abstract: ("video game time") OR abstract: ("computer game") OR abstract: ("screen time") OR abstract: ("screen entertainment") OR abstract: ("screen behavior") OR abstract: ("screen behavior") OR abstract: ("screen‐based entertainment") OR abstract: ("television viewing") OR abstract: ("television watching") OR abstract: ("television time") OR abstract: ("TV viewing") OR abstract: ("TV watching") OR abstract: ("TV time") OR abstract: ("watch television") OR abstract: ("view television") OR abstract: ("watch TV") OR abstract: ("screen watching") OR abstract: ("screen time") OR abstract: ("screen entertainment") OR abstract: ("screen behavior") OR abstract: ("screen behaviour") OR abstract: ("screen‐based entertainment") OR abstract: ("sedentary behavior*") OR abstract: ("sedentary behaviour*") OR abstract: ("sedentary lifestyle*") OR abstract: ("prolonged sitting") OR abstract: ("sitting time") OR abstract: ("lying time") OR abstract: ("physical inactivity") OR abstract: ("physically inactive"))) AND ((title: (Elderly) OR title: (Senior) OR title: (seniors) OR title: (older adult) OR title: (older adults) OR title: (elderly) OR title: (geriatric) OR title: (geriatrics) OR title: ("old people") OR title: ("older‐age") OR title: ("old age") OR title: ("older people") OR title: (adult) OR title: (adults)) OR (abstract: (Elderly) OR abstract: (Senior) OR abstract: (seniors) OR abstract: (older adult) OR abstract: (older adults) OR abstract: (elderly) OR abstract: (geriatric) OR abstract: (geriatrics) OR abstract: ("old people") OR abstract: ("older‐age") OR abstract: ("old age") OR abstract: ("older people") OR abstract: (adult) OR abstract: (adults))) AND ((Index Terms: ("Clinical Trials")) OR (title: ("randomized controlled trial") OR title: ("controlled clinical trial") OR title: (randomized) OR title: (placebo) OR title: (randomly) OR title: (trial) OR title: (intervention*) OR title: ("randomized controlled trial") OR title: ("controlled clinical trial") OR title: (randomized) OR title: (placebo) OR title: (randomly) OR title: (trial)) OR (abstract: ("randomized controlled trial") OR abstract: ("controlled clinical trial") OR abstract: (randomized) OR abstract: (placebo) OR abstract: (randomly) OR abstract: (trial) OR abstract: (intervention*) OR abstract: ("randomized controlled trial") OR abstract: ("controlled clinical trial") OR abstract: (randomized) OR abstract: (placebo) OR abstract: (randomly) OR abstract: (trial))) AND Year: 2019 To 2020
The following search was conducted in PsycINFO on 18 January 2021.
for ((IndexTermsFilt: ("video gaming") OR IndexTermsFilt: ("Computer Games") OR IndexTermsFilt: ("Computers") OR IndexTermsFilt: ("drivers") OR IndexTermsFilt: ("Sedentary Behavior") OR IndexTermsFilt: ("Television Viewing")) OR (title: ("video game") OR title: ("computer gaming") OR title: ("video game time") OR title: ("computer game") OR title: ("screen time") OR title: ("screen entertainment") OR title: ("screen behavior") OR title: ("screen behavior") OR title: ("screen‐based entertainment") OR title: ("television viewing") OR title: ("television watching") OR title: ("television time") OR title: ("TV viewing") OR title: ("TV watching") OR title: ("TV time") OR title: ("watch television") OR title: ("view television") OR title: ("watch TV") OR title: ("screen watching") OR title: ("screen time") OR title: ("screen entertainment") OR title: ("screen behavior") OR title: ("screen behaviour") OR title: ("screen‐based entertainment") OR title: ("sedentary behavior*") OR title: ("sedentary behaviour*") OR title: ("sedentary lifestyle*") OR title: ("prolonged sitting") OR title: ("sitting time") OR title: ("lying time") OR title: ("physical inactivity") OR title: ("physically inactive")) OR (abstract: ("video game") OR abstract: ("computer gaming") OR abstract: ("video game time") OR abstract: ("computer game") OR abstract: ("screen time") OR abstract: ("screen entertainment") OR abstract: ("screen behavior") OR abstract: ("screen behavior") OR abstract: ("screen‐based entertainment") OR abstract: ("television viewing") OR abstract: ("television watching") OR abstract: ("television time") OR abstract: ("TV viewing") OR abstract: ("TV watching") OR abstract: ("TV time") OR abstract: ("watch television") OR abstract: ("view television") OR abstract: ("watch TV") OR abstract: ("screen watching") OR abstract: ("screen time") OR abstract: ("screen entertainment") OR abstract: ("screen behavior") OR abstract: ("screen behaviour") OR abstract: ("screen‐based entertainment") OR abstract: ("sedentary behavior*") OR abstract: ("sedentary behaviour*") OR abstract: ("sedentary lifestyle*") OR abstract: ("prolonged sitting") OR abstract: ("sitting time") OR abstract: ("lying time") OR abstract: ("physical inactivity") OR abstract: ("physically inactive"))) AND ((IndexTermsFilt: ("Older Adulthood")) OR (title: (Elderly) OR title: (Senior) OR title: (seniors) OR title: (older adult) OR title: (older adults) OR title: (elderly) OR title: (geriatric) OR title: (geriatrics) OR title: ("old people") OR title: ("older‐age") OR title: ("old age") OR title: ("older people") OR title: (adult) OR title: (adults)) OR (abstract: (Elderly) OR abstract: (Senior) OR abstract: (seniors) OR abstract: (older adult) OR abstract: (older adults) OR abstract: (elderly) OR abstract: (geriatric) OR abstract: (geriatrics) OR abstract: ("old people") OR abstract: ("older‐age") OR abstract: ("old age") OR abstract: ("older people") OR abstract: (adult) OR abstract: (adults))) AND ((IndexTermsFilt: ("Clinical Trials")) OR (title: ("randomized controlled trial") OR title: ("controlled clinical trial") OR title: (randomized) OR title: (placebo) OR title: (randomly) OR title: (trial) OR title: (intervention*) OR title: ("randomized controlled trial") OR title: ("controlled clinical trial") OR title: (randomized) OR title: (placebo) OR title: (randomly) OR title: (trial)) OR (abstract: ("randomized controlled trial") OR abstract: ("controlled clinical trial") OR abstract: (randomized) OR abstract: (placebo) OR abstract: (randomly) OR abstract: (trial) OR abstract: (intervention*) OR abstract: ("randomized controlled trial") OR abstract: ("controlled clinical trial") OR abstract: (randomized) OR abstract: (placebo) OR abstract: (randomly) OR abstract: (trial))) AND Year: 1966 To 2021
PsycINFO was searched from 01/01/1860 ‐ 18/01/2021
Appendix 6. PEDro search strategy
The following search was conducted in PEDro on 18 January 2021.
Abstract & Title: Sedentary
Therapy: Behaviour Modification
Subdiscipline: Gerontology
Appendix 7. EPPI‐Centre search strategy
The following search was conducted on EPPI‐Centre on 18 January 2021.
1. What type of study does this report describe?: RCT
2. Focus of the report: physical activity OR Freetext (All but Authors): sedentary
3. Characteristics of the study population: older people (+55 yrs) OR adults (22‐54 yrs)
Appendix 8. WHO ICTRP search strategy
A search was conducted in the WHO ICTRP on 18 January 2021 using the search term sedentary.
Appendix 9. ClinicalTrials.gov search strategy
The following search was conducted on clinicaltrials.gov on 18 June 2021.
Elderly OR Senior OR seniors OR older adult OR older adults OR elderly OR geriatric OR geriatrics OR old people OR older‐age OR old age OR adult OR adults OR older people | Completed Studies | Interventional Studies | Sedentary Behavior | Older Adult
Data and analyses
Comparison 1. Intervention for reducing sedentary behaviour versus control: main outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Sedentary time [min/day] | 7 | 397 | Mean Difference (IV, Random, 95% CI) | ‐44.91 [‐93.13, 3.32] |
| 1.1.1 Self‐reported | 2 | 139 | Mean Difference (IV, Random, 95% CI) | ‐84.29 [‐270.14, 101.56] |
| 1.1.2 Objectively measured | 5 | 258 | Mean Difference (IV, Random, 95% CI) | ‐30.45 [‐72.68, 11.77] |
| 1.2 Sedentary time [min/day] per intervention duration | 7 | 397 | Mean Difference (IV, Random, 95% CI) | ‐44.91 [‐93.13, 3.32] |
| 1.2.1 Single point of contact | 3 | 219 | Mean Difference (IV, Random, 95% CI) | ‐79.34 [‐179.31, 20.62] |
| 1.2.2 Longitudinal interventions | 4 | 178 | Mean Difference (IV, Random, 95% CI) | ‐20.34 [‐67.25, 26.56] |
| 1.12 Sedentary time in specific domains [min/day] | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.12.1 TV time | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.12.2 Computer time | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.12.3 Reading | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.12.4 Socialising | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.12.5 Transportation | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.12.6 Hobbies | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.12.7 Paperwork | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.12.8 Eating | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.12.9 Other | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.13 Breaks in sedentary behaviour | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐8.00 [‐16.78, 0.78] |
1.2. Analysis.

Comparison 1: Intervention for reducing sedentary behaviour versus control: main outcomes, Outcome 2: Sedentary time [min/day] per intervention duration
1.12. Analysis.
Comparison 1: Intervention for reducing sedentary behaviour versus control: main outcomes, Outcome 12: Sedentary time in specific domains [min/day]
1.13. Analysis.

Comparison 1: Intervention for reducing sedentary behaviour versus control: main outcomes, Outcome 13: Breaks in sedentary behaviour
Comparison 2. Intervention for reducing sedentary behaviour versus control: physical function outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 SPPB | 2 | 98 | Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.38, 0.66] |
| 2.2 Gait speed | 2 | 98 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.04, 0.09] |
| 2.3 Chair stands (seconds) | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐1.49, 1.49] |
Comparison 3. Intervention for reducing sedentary behaviour versus control: obesity outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 BMI | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 0.50 [‐2.05, 3.05] |
| 3.2 Waist circumference (cm) | 2 | 100 | Mean Difference (IV, Random, 95% CI) | 1.14 [‐1.64, 3.93] |
| 3.3 Body fat (%) | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐0.65 [‐4.31, 3.01] |
Comparison 4. Intervention for reducing sedentary behaviour versus control: fitness outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 6‐minute walk (metres) | 2 | 80 | Mean Difference (IV, Random, 95% CI) | ‐5.16 [‐36.49, 26.17] |
Comparison 5. Intervention for reducing sedentary behaviour versus control: blood pressure outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Systolic [mmHg] | 3 | 138 | Mean Difference (IV, Random, 95% CI) | ‐3.91 [‐10.95, 3.13] |
| 5.2 Diastolic [mmHg] | 3 | 138 | Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐5.72, 5.60] |
Comparison 6. Intervention for reducing sedentary behaviour versus control: cardiometabolic markers outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Cholesterol [mg/dL] | 2 | 100 | Mean Difference (IV, Random, 95% CI) | 3.25 [‐9.52, 16.03] |
| 6.2 HDL [mg/dL] | 2 | 100 | Mean Difference (IV, Random, 95% CI) | ‐2.47 [‐7.40, 2.45] |
| 6.3 LDL [mg/dL] | 2 | 100 | Mean Difference (IV, Random, 95% CI) | 4.17 [‐6.89, 15.22] |
| 6.4 Triglycerides [mg/dL] | 2 | 100 | Mean Difference (IV, Random, 95% CI) | 2.13 [‐18.95, 23.21] |
| 6.5 Glucose [mg/dL] | 2 | 100 | Mean Difference (IV, Random, 95% CI) | 2.20 [‐6.46, 10.86] |
| 6.6 Glycated haemoglobin | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.11, 0.33] |
Comparison 7. Intervention for reducing sedentary behaviour versus control: quality of life.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 SF‐36 Physical function | 1 | 38 | Mean Difference (IV, Random, 95% CI) | ‐5.00 [‐19.12, 9.12] |
| 7.2 SF‐36 Energy | 1 | 38 | Mean Difference (IV, Random, 95% CI) | ‐5.00 [‐16.16, 6.16] |
| 7.3 SF‐36 Emotional well‐being | 1 | 38 | Mean Difference (IV, Random, 95% CI) | 4.00 [‐7.32, 15.32] |
| 7.4 SF‐36 Pain | 1 | 38 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐22.32, 22.32] |
| 7.5 SF‐36 General health | 1 | 38 | Mean Difference (IV, Random, 95% CI) | ‐5.00 [‐12.06, 2.06] |
Comparison 8. Intervention for reducing sedentary behaviour versus control: depression.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Depression (Center for Epidemiological Studies‐Depression (CES‐D)) | 1 | 38 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐3.57, 3.57] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Barone 2017.
| Study characteristics | ||
| Methods |
Study design: Randomised controlled trial Study grouping: Sit Less (sedentary behaviour intervention), Get Active (control physical activity intervention) Randomisation method: Participants were randomly assigned to 1 of the 2 intervention groups with a 1:1 ratio. Randomisation was stratified by sex and cohabitation. Cohabiting (e.g. married) participants were randomised at the level of the couple. Assessment: Assessments were performed at baseline and 12 weeks. Objective activity was measured by a blinded, SenseWearPro armband (SWA) that did not provide feedback. Sedentary behaviour was assessed by a 6‐item questionnaire in addition to SWA. The questionnaire assessed usual time spent in 6 sedentary activities (e.g. watching TV, using a computer for work or recreation, riding in a car) separately for weekdays and weekends. Physical function was assessed with a 400‐metre walk test and Short Physical Performance Battery (SPPB). Quality of life was assessed with the 36‐item Short Form Health Survey (SF‐36; Walters, Munro, & Brazier 2001). Depressive symptoms were evaluated using the Center for Epidemiological Studies Depression Scale (CES‐D). Blood pressure was averaged over 2 consistent measures (differences of < 10 mmHg in systolic blood pressure and < 6 mmHg diastolic blood pressure) using a Dinamap automated blood pressure system after a 5‐minute rest period. Operational definition of sedentary time: Total sedentary time was calculated as the sum of “awake” minutes for which energy expenditure was ≤ 1.5 METs and converted to hours/day. |
|
| Participants |
Baseline characteristics Sit Less
Get Active
Inclusion criteria: Eligibility criteria included age ≥ 60 years old, < 60 min per week of self‐reported moderate to vigorous physical activity (MVPA), ability to complete a 400‐metre walk test without an assistive device, ability to provide medical clearance from a physician to participate in the study, and access to a smartphone with Bluetooth. Exclusion criteria: A recent cardiovascular event (< 6 months), recent use of psychotropic medications or other treatment for psychological issues (< 6 months), any comorbid condition that limited participation in exercise (e.g. severe arthritis, current treatment for cancer), or self‐report of > 3 alcoholic beverages per day |
|
| Interventions |
Intervention characteristics 12‐week intervention in which both groups received a combination of individual, in‐person, and phone consultations with an exercise physiologist coupled with the use of the BodyMedia SWA and interface on their personal smartphone. In‐person visits (30 to 60 min) occurred weekly during weeks 1 to 4. During weeks 5 to 12, in‐person visits were biweekly and alternated with biweekly scripted phone calls lasting approximately 10 min with the interventionist. The Sit Less group had a goal to reduce sedentary time by 1 h each day. The Get Active group had a goal to reach 150 min of MVPA each week, accumulated in bouts of ≥ 10 min. Participants were able to see feedback from the activity tracker for time spent in the target behaviour. |
|
| Outcomes |
Primary outcomes Sedentary time (objectively measured)
Secondary outcomes Systolic blood pressure
Diastolic blood pressure
400‐metre walk
Gait speed
Short Physical Performance Battery (SPPB)
|
|
| Identification |
Sponsorship source: This research was funded by the University of Pittsburgh Claude D. Pepper Center Program (P30 AG024827). Country: USA Setting: Community Comments: This study compares intervening to reduce sedentary behaviour versus intervening to increase MVPA. Sitting reduction intervention did not change physical activity, and physical activity intervention did not change sitting. However, sitting intervention significantly increased physical function 0.5 on the SPPB (only the chair stand subscale changed 0.42 chair stands). The physical activity intervention did not change physical function. Author's name: Bethany Barone Gibbs Institution: Pittsburgh University Email: bbarone@pitt.edu Address: Department of Health and Physical Activity, Physical Activity and Weight Management Research Center, University of Pittsburgh, 32 Oak Hill Court, Room 205, Pittsburgh, PA 15261, USA |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | No information describing the sequence generation despite clear description of the stratification of the randomisation |
| Allocation concealment (selection bias) | High risk | Allocation was 1:1 between groups, but no information is provided regarding how this was achieved. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were assigned to a Sit Less or Get Active arm, and interventionists were assigned exclusively to 1 arm of the study. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Use of device‐based measure, but no information about blinding of assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reports that there were no missing data with clear description |
| Selective reporting (reporting bias) | Unclear risk | Not all outcomes listed in the methods section are presented clearly in the results section. |
| Other bias | Low risk | None |
Lyons 2017.
| Study characteristics | ||
| Methods |
Study design: Randomised controlled trial Study grouping: Sedentary behaviour intervention and 1 control group (waiting list) Assessment: Sedentary behaviour was measured using an activPAL device; fitness using the 6‐minute walk test; and body fat using dual‐energy x‐ray absorptiometry (DEXA). Operational definition of sedentary time: Postural, as per activPAL Randomisation method: Opaque envelopes randomly sorted by an independent individual then numbered sequentially. Randomisation stratified by the 2 cohorts for adequate numbers within each group. |
|
| Participants |
Baseline characteristics Intervention
Control (waitlist)
Inclusion criteria: Aged between 55 and 79 years, BMI between 25 and 35. Ability to read and understand English. Ability to read words on a tablet‐sized device Exclusion criteria: Self‐reported habitual physical activity more than 60 min per week. Health issues that might preclude safe walking. Psychological issues that might interfere with full participation. Current use of a wearable electronic activity monitoring system. Cardiovascular disease risk questions positive on the Physical activity readiness questionnaire ‐ PAR‐Q (doctor's consent if only about medications) |
|
| Interventions | 12‐week e‐health intervention involving a wearable activity monitor (Up24, Jawbone Inc, San Francisco, CA) coupled with a tablet (Apple iPad Mini, Apple Inc, Cupertino, CA). Participants set goals for physical activity and sedentary behaviour with the help of the interventionist, monitored by the activity monitor. Participant could monitor progress through a simple interface on the tablet. Intervention was delivered through an initial consultation and weekly phone calls discussing goals and targets and other behaviour change strategies. In addition, the monitor delivered haptic prompts when the participant was inactive for extended periods (duration set by the participant). Interventionists provided training for self‐monitoring, viewing feedback, and using sedentary behaviour prompts in the app. | |
| Outcomes |
Primary outcomes Sedentary time (objective)
Secondary outcomes Body fat
Fitness
|
|
| Identification |
Sponsorship source: This study was internally funded by the Claude D Pepper Older Americans Independence Center (P30AG024832) and Sealy Center on Aging. Additional salary support was provided by a Mentored Research Scholar Grant in Applied and Clinical Research (MRSG‐14‐165‐01‐CPPB) from the American Cancer Society, the American Heart Association (13BGIA17110021), and the Cancer Prevention Research Institute of Texas (RP140020). Country: USA Setting: Community Comments: This is a feasibility study based on an RCT design (intervention/control) with N = 40 in 2 groups. Intervention based on wearable feedback over 12 weeks and telephone counselling. Shows low effect size on sedentary time (decrease) Cohen's d ~ −0.21 and slight increase in stepping activity (d ~ 0.26) and loss of body fat (−0.17), no effect on fitness Author's name: Elizabeth J Lyons Institution: Department of Nutrition and Metabolism, The University of Texas Medical Branch, Galveston, TX, USA Email: ellyons@utmb.edu Address: Elizabeth J Lyons, MPH, PhD, Department of Nutrition and Metabolism, The University of Texas Medical Branch, 301 University Blvd, Galveston, TX, 77555, USA |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was conducted using standard opaque envelopes with foil (to prevent seeing the group assignment inside the envelope) and carbon paper (to provide an audit trail). The envelopes were randomly sorted by an individual not involved in the randomisation visit process, then numbered sequentially. Randomisation was carried out using sequentially numbered, opaque, sealed envelopes according to standard protocols, with randomisation stratified by the 2 cohorts to promote adequate numbers of participants able to talk to one another through the app. |
| Allocation concealment (selection bias) | Low risk | Envelopes were randomly sorted by an individual not involved in the randomisation visit process, then numbered sequentially. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Intensive intervention with weekly telephone counselling, and participants encouraged to view their data at least twice per day. Control was a waitlist condition. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Use of device‐based measure, but resource limitations precluded using blinded assessors for all participants |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Detailed description of missing data, and intention‐to‐treat analysis fully described |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | None |
Maher 2017.
| Study characteristics | ||
| Methods |
Study design: Cluster‐randomised controlled trial Study grouping: Intervention to reduce sedentary behaviour and control group (intervention to reduce social isolation) Assessment: Weekday and weekend day sedentary behaviour was assessed using a 9‐item domain‐specific measure of behaviour. Sedentary behaviour was measured on day 7 (prior to the delivery of the sedentary behaviour content in the intervention group or after the delivery of the social isolation content in the comparison group) and on day 14 in both groups. Operational definition of sedentary time: Self‐reported sitting time in different behaviour Randomisation method: Cluster randomisation was used to reduce the threat of contamination within sites. Randomisation was stratified based on senior centre size (large centres had ≥ 30 regular attendees, small centres had < 30) using data from the county’s Office of Aging. A computer‐generated allocation sequence yielded 1 large and 2 small senior centres in the intervention group and 1 large and 1 small senior centre in the comparison group. |
|
| Participants |
Baseline characteristics Overall
Inclusion criteria: Participants at senior centres Exclusion criteria: Diagnosed by a physician as having dementia or Alzheimer's disease. Injuries or illnesses that precluded standing or walking |
|
| Interventions | 2‐week intervention involving 3, 1.5‐hour meetings for each group. Content in both groups involved watching video segments and participating in group discussions. In the intervention group, the content of the video and discussion focused on creating awareness about sedentary behaviour and associated risks, developing an action plan for reduction of sedentary behaviour and personal goals, tasks involving the participants comparing their sedentary time to peer and normative values, and tasks to enhance self‐efficacy. In addition, participants were educated on the benefits associated with displacing sedentary time with light‐intensity physical activity (e.g. standing, slow walking), such as decreased risk of premature death and cardiovascular disease and maintenance of physical and cognitive functioning. Participants were engaged in discussing their progress or barriers in achieving these goals; however, participants’ goal completion was not formally tracked. 2 target behavioural goals were identified: (1) stand or move for at last 10 min each waking hour or (2) limit sedentary behaviour to less than 8 waking hours/day over the course of the next week. Video segments and discussions in the comparison group focused on (1) defining social isolation, (2) assessing individuals’ social isolation via self‐report measure, (3) reviewing normative levels of social connectivity, (4) reviewing evidence of the consequences associated with social isolation as well as benefits associated with social engagement, (5) developing action plans to increase or improve social connectivity, and (6) establishing target goals. |
|
| Outcomes |
Primary outcomes Sedentary time (subjective)
TV time (subjective)
Computer sedentary time (subjective)
Reading sedentary time (subjective)
Socialising sedentary time (subjective)
Hobbies sedentary time (subjective)
Paperwork sedentary time (subjective)
Eating sedentary time (subjective)
Other sedentary time (subjective)
|
|
| Identification |
Sponsorship source: Penn State CTSI Grant from the National Center for Advancing Translational Sciences, National Institutes of Health Country: USA Setting: Senior centres Comments: This is an RCT (with cluster randomisation) N = 42 of an intervention based on 3 workshops over 2 weeks. Assessment via subjective measure. Reports a decrease of SB of 837.8 min/week Author's name: Jaclyn P Maher Institution: The Pennsylvania State University Email: jmaher@usc.edu Address: The Pennsylvania University Park, PA, USA |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated allocation sequence |
| Allocation concealment (selection bias) | Low risk | Computer‐generated allocation sequence and cluster randomisation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The same interventionist delivered the programme in the intervention (reducing sedentary behaviour) and the control group (reducing social isolation). |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Self‐reported measures, and nothing specifically reported about blinding of assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data fully reported, little attrition, and all participants were included in the analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes listed in the methods section were presented in the results section. |
| Other bias | Low risk | None |
| Recruitment bias (cluster RCT only) | Low risk | Computer‐generated allocation sequence |
| Baseline imbalance (ClusterRCT only) | Unclear risk | No information reported about baseline characteristics per clusters or condition. |
| Loss of clusters (ClusterRCT only) | Low risk | No loss of clusters |
| Incorrect analysis (ClusterRCT only) | Low risk | Analysis adjusted for clustering. |
| Comparability with individually randomized trials(Cluster RCT only) | Low risk | Cluster randomisation was used to reduce the threat of contamination within sites. |
Owari 2019.
| Study characteristics | ||
| Methods |
Study design: Randomised controlled trial Study grouping: Intervention to reduce sedentary behaviour and control group (no intervention) Assessment: Sedentary time was assessed for 14 consecutive days using a traxial accelerometer (Active Style Pro HJA‐750 CC, Omron Healthcare, Japan). Operational definition of sedentary time: Sedentary time was defined as sum of minutes with energy expenditure ≤ 15 METs. Randomisation method: Computer‐generated sequence by a blinded research administrator not part of the research team |
|
| Participants |
Baseline characteristics Intervention group
Control group
Inclusion criteria: None reported. Participants were recruited from the college health club in Utazu‐cho, Kagawa, Japan, which provides health education. Exclusion criteria: None reported. |
|
| Interventions | The intervention group received a brochure called 'Active Guide', published by the Japanese Ministry of Health, Labour and Welfare (www.nibiohn.go.jp/eiken/info/pdf/active2013-e.pdf, www.nibiohn.go.jp/eiken/info/pdf/active2013.pdf), and additional documents explaining the benefits of reducing sedentary behaviour (“Let’s pay attention to time spent sitting”). Participants in both groups received a note of their baseline sedentary time. | |
| Outcomes |
Primary outcomes Sedentary time (objective)
|
|
| Identification |
Sponsorship source: No funding declared. Country: Japan Setting: Community dwelling Comments: Reports a decrease of SB of 2.2% in sedentary time in the intervention group, and an increase of 2.5% sedentary time in the control group after 1 year Author's name: Yutaka Owari Institution: Shikoku Medical College and Department of Hygiene, Faculty of Medicine, Kagawa University Email: owari@med.kagawa‐u.ac.jp Address: Kagawa University, Miki, Kagawa 761‐0793, Japan |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence performed by a blinded administrator |
| Allocation concealment (selection bias) | High risk | Allocation was done by an unblinded researcher. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were informed of which group they were in, and the intervention group received printed materials and the results of their baseline examination, and the control group received results from baseline examination. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Device‐based measure and use of blinded assessors |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Analysis was conducted only on participants attending 75% of the sessions. Dropout is described. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | None |
Roberts 2019.
| Study characteristics | ||
| Methods |
Study design: Randomised controlled trial Study grouping: Intervention to increase physical activity and reduce sedentary behaviour and control group (increase physical activity only) Assessment: Sedentary time was assessed for 7 consecutive days using a traxial accelerometer (Actigraph GT3X). Operational definition of sedentary time: Sedentary time was defined as sum of minutes with less than 100 counts/min accelerometer data. Randomisation method: Computer‐generated sequence by a blinded research administrator not part of the research team |
|
| Participants |
Baseline characteristics Intervention group
Control group
Inclusion criteria: Adults aged over 60 years, inactive lifestyle defined as less than 150 minutes per week of moderate to vigorous physical activity, moderate to high risk of cardiovascular diseases Exclusion criteria: Adults with absolute contraindications for exercise according to the American College of Sports Medicine (ACSM) guidelines. High blood pressure defined as systolic blood pressure > 180 mmHg and diastolic blood pressure > 110 mmHg, and any condition that impairs participation in exercise |
|
| Interventions | Participants in both groups underwent exercise training for 8 weeks designed to meet exercise and physical activity guidelines for older adults from ACSM and the American Heart Association. The intervention group received cognitive behavioural counselling to develop strategies to reduce sedentary behaviour and activity tracker (Fitbit Zip). Intervention group received weekly feedback, motivation, and goal setting by phone based on tracker data. | |
| Outcomes |
Primary outcomes Sedentary time (objective)
Secondary outcomes Systolic blood pressure
Diastolic blood pressure
6‐minute walk distance
Waist circumference
Total cholesterol
LDL cholesterol
HDL cholesterol
Triglycerides
Blood glucose
Glycated haemoglobin
|
|
| Identification |
Sponsorship source: Research was supported by the American Heart Association (16IRG27250237), National Institute on Aging (2P30AG028740), the National Center for Medical Rehabilitation Research (1P2CHD086851), and the University of Alabama at Birmingham Center for Exercise Medicine. Country: USA Setting: Community‐dwelling older adults Comments: Reports no significant difference in sedentary time, but a small improvement of 9.9 mmHg in systolic blood pressure Author's name: Lisa M Roberts Institution: Department of Medicine, Division of Gerontology/Geriatrics/Palliative Care, University of Alabama Email: twbuford@uabmc.edu Address: Department of Medicine, Division of Gerontology/Geriatrics/Palliative Care, University of Alabama at Birmingham, 1313 13th Street S, Birmingham, AL 35205, USA |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a random number generator |
| Allocation concealment (selection bias) | Unclear risk | No information about how the allocation was performed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants in both conditions received the same exercise programme and cognitive‐behavioural counselling. The study team monitored participants’ daily activity and communicated weekly with intervention participants to provide additional motivation and individual goal‐based strategies. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Device‐based measure, and study staff conducting assessment were blinded to randomisation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low dropout, fully reported, and data analysed following intention‐to‐treat |
| Selective reporting (reporting bias) | Low risk | Protocol published, and all outcomes are reported in the results. |
| Other bias | Low risk | None |
Rosenberg 2020.
| Study characteristics | ||
| Methods |
Study design: Randomised controlled trial Study grouping: Intervention to reduce sedentary behaviour and control group (usual care) Assessment: Sedentary time was assessed objectively using an activPAL activity monitor. Operational definition of sedentary time: Sedentary time was defined by posture allocation as time spent sitting. Randomisation method: Computer‐generated sequence based on a 1:1 allocation and stratified according to baseline sedentary time |
|
| Participants |
Baseline characteristics Intervention group
Control group
Inclusion criteria: Adults aged between 60 and 89 years with BMI ≥ 30 kg/m2 Exclusion criteria: Individuals living in long‐term care or with a diagnosis of cancer, heart failure, dementia, or a serious mental health disorder |
|
| Interventions | 12‐week intervention based on relevant behavioural theories, including social‐cognitive theory, the ecological model, and habit formation theory. Participants received 2 in‐person health coaching sessions of 30 to 60 minutes, 4 follow‐up health coaching phone calls of 15 to 30 minutes, and written materials. Participants were taught how to develop strategies to remind them to take breaks from sitting regularly throughout the day and received a wrist‐worn, commercially available fitness tracker (a Jawbone UP band), which provided gentle vibrations every 15 minutes to cue breaks from sitting throughout the day. Participants were not given the Jawbone smartphone application nor any other feedback from the device. Participants were provided with a chart of their progress as measured by activPAL at weeks 1, 6, and 12. | |
| Outcomes |
Primary outcomes Sedentary time (objective)
Sedentary breaks (objective)
Secondary outcomes Systolic blood pressure
Diastolic blood pressure
Waist circumference
BMI
Gait speed
Chair stand
Short Physical Performance Battery (SPPB)
|
|
| Identification |
Sponsorship source: Research was supported by the National Institute on Aging and the National Heart, Lung, and Blood Institute, K23HL119352, R21AG043853. Country: USA Setting: Community‐dwelling older adults Comments: Reports significant reduction in sedentary time, but no associated change in health outcomes over 12 weeks Author's name: Dori E Rosenberg Institution: Kaiser Permanente Washington Health Research Institute Email: Dori.E.Rosenberg@kp.org Address: 1730 Minor Ave, Suite 1600, Seattle, WA 98101‐1466, USA |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation used an autogenerated computer sequence. |
| Allocation concealment (selection bias) | Low risk | Randomisation was stratified according to baseline sedentary time and only revealed after baseline assessment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The intervention group had a greater number of contacts with the interventionists, and interventionists delivered both the intervention and control (healthy living) programmes. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Device‐based measurement, and assessors were blinded to randomisation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Analysis performed on complete‐case only. A sensitivity analysis was conducted with replacement of missing data with baseline value. |
| Selective reporting (reporting bias) | Low risk | Protocol published, and all outcomes reported. |
| Other bias | Low risk | None |
White 2017.
| Study characteristics | ||
| Methods |
Study design: Randomised controlled trial Study grouping: Intervention to reduce sedentary behaviour and control (fact sheet about physical activity) Assessment: Measure of sedentary time using the self‐reported MOST and IPAQ questionnaires Operational definition of sedentary time: Sum of time spent sitting as assessed by MOST and IPAQ Randomisation method: After consent, participants were randomised by an independent trial administrator using a computer‐generated 1:1 block randomisation schedule. |
|
| Participants |
Baseline characteristics Intervention
Control
Inclusion criteria: Aged >= 65 years. Self‐reported retired and sedentary (>= 6 hours sitting (leisure) per day). Self‐reported <= 30 consecutive minutes of leisure time physical activity of >= 3 METs Exclusion criteria: People with physical impairments precluding light‐intensity physical activity, lacking capacity to provide informed consent, living in the same household as another study participant, or unable to speak or read English fluently |
|
| Interventions | The intervention consisted of a printed A5‐sized information booklet outlining the health impact of sedentary behaviour and physical activity and 15 tips on reducing sedentary behaviour and forming physical activity habits, with 8 printed "tick‐sheets" for participants to record daily adherence to tips for both intervention and data collection purposes. | |
| Outcomes |
Primary outcomes Sedentary time (self‐reported; MOST)
|
|
| Identification |
Sponsorship source: The project is supported by a grant from the National Prevention Research Initiative. Country: UK Setting: Community Comments: Pilot RCT to look at the effect of habit formation on SB intervention. Show change in SB in both intervention and control group (albeit control group still gets education about SB), but no group effect Authors name: Isabelle White Institution: King's College London Email: benjamin.gardner@kcl.ac.uk Address: Department of Psychology, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, De Crespigny Park, London SE5 8AF, UK |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation performed by independent administrator using a computer‐generated sequence on 1:1 schedule. |
| Allocation concealment (selection bias) | Low risk | Computer‐generated randomisation, and independent staff performing the randomisation |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Both groups received printed materials and were recruited in 4 geographic clusters; participants were blinded to allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Self‐reported measures, and assessors not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition well described, intention‐to‐treat analysis with baseline data replacement for missing data. |
| Selective reporting (reporting bias) | High risk | Indicates that other measures were collected but not reported |
| Other bias | Low risk | None |
BMI: body mass index
HDL: high‐density lipoprotein
IPAQ: International Physical Activity Questionnaire
LDL: low‐density lipoprotein
METs: metabolic equivalents
MOST: Measure of Older Adults Sedentary Time
MVPA: moderate‐ to vigorous‐intensity physical activity
RCT: randomised controlled trial
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Annesi 2004 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Arrogi 2017 | Sample includes participants below the age of 60 years. |
| Ashe 2019 | Not an RCT or cluster‐RCT |
| Aunger 2020 | Sample recruited on the basis of a clinical condition. |
| Awick 2017 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Azizan 2016 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Britten 2017 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Buman 2011 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Burke 2013 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Burton 1995 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Chang 2013 | Sample recruited on the basis of a clinical condition. |
| Chiang 2019 | Sample includes participants below the age of 60 years. |
| Darvall 2016 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| De Greef 2010 | Sample recruited on the basis of a clinical condition. |
| De Greef 2011 | Sample recruited on the basis of a clinical condition. |
| Edwards 2018 | Sample includes participants below the age of 60 years. |
| Engelen 2019 | Sample includes participants below the age of 60 years. |
| Fanning 2016 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Fennell 2016 | Sample includes participants below the age of 60 years. |
| Fitzsimons 2013 | Not an RCT or cluster‐RCT |
| Gardiner 2011 | Not an RCT or cluster‐RCT |
| Goldstein 1999 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Greenwood‐Hickman 2016 | Not an RCT or cluster‐RCT |
| Hansen 2012 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Harvey 2018 | Wrong comparison, no control group with no sedentary behaviour intervention |
| Hetherington 2015 | Sample includes participants below the age of 60 years. |
| Kegler 2012 | Sample includes participants below the age of 60 years. |
| Kendzor 2016 | Sample includes participants below the age of 60 years. |
| Kerse 2005 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| King 2016 | Sample includes participants below the age of 60 years. |
| Koltyn 2019 | Not an RCT or cluster‐RCT |
| Kuck 2014 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Lakerveld 2013 | Sample includes participants below the age of 60 years. |
| Lerma 2017 | Not an RCT or cluster‐RCT |
| Lerma 2020 | Not an RCT or cluster‐RCT |
| Lewis 2016 | Not an RCT or cluster‐RCT |
| Lubans 2013 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Lyons 2014 | Sample includes participants below the age of 60 years. |
| Matei 2015 | Not an RCT or cluster‐RCT |
| Matson 2018 | Wrong outcome; does not measure sedentary behaviour |
| Matson 2019 | Not an RCT or cluster‐RCT |
| Muller 2016 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Nicklas 2014 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Overgaard 2018 | Sample includes participants below the age of 60 years. |
| Paing 2019 | Sample recruited on the basis of a clinical condition. |
| Paschoa 2016 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Pomeroy 2011 | Wrong setting, not community‐dwelling sample |
| Poppe 2019 | Sample recruited on the basis of a clinical condition. |
| Rasinaho 2012 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Rockette‐Wagner 2017 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Rosenberg 2015 | Not an RCT or cluster‐RCT |
| Ruscello 2014 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Sakurai 2012 | Sample recruited on the basis of a clinical condition. |
| Siddique 2017 | Sample includes participants below the age of 60 years. |
| Sparker‐Griffin 2013 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Spring 2018 | Sample includes participants below the age of 60 years. |
| Suboc 2016 | Not an RCT or cluster‐RCT |
| Takemoto 2020 | Wrong outcome; does not measure sedentary behaviour |
| Taylor 2016 | Not an RCT or cluster‐RCT |
| Tennstedt 2013 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Toto 2012 | Wrong outcome; does not measure sedentary behaviour |
| Turunen 2020 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Valerio 2012 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Van Hoecke 2014 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| von Berens 2018 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| von Bonsdorff 2009 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Walters 2017 | Wrong outcome; does not measure sedentary behaviour |
| Wheeler 2019a | Not an RCT or cluster‐RCT |
| Wheeler 2019b | Not an RCT or cluster‐RCT |
| Yan 2009 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
| Yeom 2010 | Not an RCT or cluster‐RCT |
| Yeom 2014 | Does not specifically target sedentary behaviour; reports a physical activity intervention |
RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
Kleinke 2018.
| Study name | MOVING: Motivation‐Orientation interVention study for the elderly IN Greifswald |
| Methods |
Study design: 2‐arm randomised controlled trial Study grouping: Parallel group Recruitment: Re‐contacting participants from a prior study, general medical practices, general recruitment Study SB/PA aim: The primary objective of the MOVING study is to examine the effects of an increase of PA and a reduction of ST after 6 months in the intervention group compared to the control group as assessed by accelerometer. Country: Germany Setting: Western Pomerania, rural area in Northeast Germany |
| Participants |
Inclusion criteria:
Exclusion criteria:
|
| Interventions | At baseline, all participants receive general information and recommendations about the positive effects of regular PA and less ST on the improvement of cardiovascular risk factors. The intervention comprises 2 individualised feedback letters using the variables number of steps per day, time in minutes of MVPA, and sedentary time in minutes per day. Participants in the intervention group will receive a feedback letter by mail shortly after wearing the accelerometer following the baseline examination and the 3‐month follow‐up. The feedback letters will contain personalised feedback based on accelerometry as well as ST behaviour. PA and ST data will be depicted in 3 comprehensive graphs. Additionally, participants receive leaflets with age‐appropriate recommendations for PA and ST at baseline. The leaflets are from the Federal Centre for Health Education. Control: (no other details provided) |
| Outcomes | Physical activity and sedentary time are measured with the ActiGraph wGT3X‐BT at 3, 6, and 12 months. Sedentary behaviour is captured by the Measure of Older Adults’ Sedentary Time (MOST) questionnaire in the German version at 3, 6, and 12 months. |
| Starting date | November 2016 |
| Contact information | Fabian Kleinke, fabian.kleinke@uni‐greifswald.de |
| Notes |
MVPA: moderate to vigorous physical activity PA: physical activity SB: sedentary behaviour ST: sedentary time WHO: World Health Organization
Differences between protocol and review
There are some differences between our published protocol, Chastin 2017, and this review.
We restricted the review to randomised controlled trials (RCTs) and cluster‐RCTs because of the growing amount of research since the publication of the protocol and our desire to focus solely on the best available evidence.
We did not limit our search strategy to articles written English only.
We did not search the AMED (Allied and Complementary Medicine) database.
We had planned to conduct a sensitivity analysis to determine the impact of risk of bias on the findings by excluding from the analysis studies rated as at high risk of bias. However, the small number of included studies precluded this analysis.
Planned subgroup analysis was not possible (see Subgroup analysis and investigation of heterogeneity).
We widened the age inclusion for study participants to studies with a sample with mean age of 60 years and over, and no participants below 55 years of age.
We categorised the type of interventions using the System of Sedentary (SOS) framework as individual behaviour, socio‐cultural settings, environmental, home settings, and policy change intervention (Chastin 2016).
We modified the classification for the length of intervention, as the classification in our protocol did not fit the type of interventions identified.
We searched for data on adverse events.
We did not consider performance bias in our protocol (Chastin 2017), as we believed it to be difficult to blind participants to allocation in this type of research. In our protocol, we considered outcome assessment and outcome assessors separately for the blinding risk of bias domain. We were advised to change this, and in the review we considered outcome assessors as part of performance bias, and also assessed risk of bias due to the lack of blinding of participants.
We adjusted outcomes for cluster‐RCTs for clustering effect using the effective sample sizes method (Higgins 2021). We used an intraclass correlation coefficient of 0.07 based on previous research in activity behaviour research (Kerr 2018).
Contributions of authors
Chastin, Skelton, Ashe, Helbostad, Gardiner, and Leask conceived and developed the protocol. Harvey commented on drafts of the protocol and the search strategies. Gardiner performed the searches with the help of a librarian. Chastin, Skelton, Harvey, Jerez‐Roig, Rosenberg, Gardiner, and Leask reviewed studies for eligibility, extracted data, and assessed risk of bias of the included studies. Chastin wrote the first draft of the review and performed the statistical analysis. Skelton, Ashe, Helbostad, Harvey, Leask, Gardiner, Jerez‐Roig, and Rosenberg commented on drafts and the final version of the review.
Sources of support
Internal sources
-
Source of support, UK
This review was not supported by any sources of support.
External sources
-
Source of support, UK
This review was not supported by any external sources of support.
Declarations of interest
Authors of this review were not allowed to screen, extract data from, or assess the risk of bias of studies on which they were a co‐author. Authors of this review were also authors of one of the studies included in this review (Rosenberg 2020).
Sebastien Chastin: no other conflicts of interest
Paul A Gardiner: no other conflicts of interest
Juliet A Harvey: no other conflicts of interest
Calum F Leask: no other conflicts of interest
Javier Jerez‐Roig: no other conflicts of interest
Dori Rosenberg: no other conflicts of interest
Maureen C Ashe: no other conflicts of interest
Jorunn L Helbostad is a professor at the Norwegian University of Science and Technology, Trondheim, Norway. She is a board member for the Norwegian Research Council. She has no competing interest related to this project.
Dawn A Skelton: no other conflicts of interest
All authors have worked on this review during the course of their employment and were therefore supported by their employing institutions as per their affiliation.
New
References
References to studies included in this review
Barone 2017 {published data only}
- Barone Gibbs B, Brach JS, Byard T, Creasy S, Davis KK, McCoy S, et al. Reducing sedentary behavior versus increasing moderate-to-vigorous intensity physical activity in older adults. Journal of Aging and Health 2017;29(2):247-67. [DOI: 10.1177/0898264316635564] [DOI] [PubMed] [Google Scholar]
Lyons 2017 {published data only}
- Lyons EJ, Swartz MC, Lewis ZH, Martinez E, Jennings K. Feasibility and acceptability of a wearable technology physical activity intervention with telephone counselling for mid-aged and older adults: a randomized controlled pilot trial. Journal of Medical Internet Research 2017;5(3):e28. [DOI: 10.2196/mhealth.6967] [DOI] [PMC free article] [PubMed] [Google Scholar]
Maher 2017 {published data only}
- Maher JP, Sliwinski MJ, Conroy DE. Feasibility and preliminary efficacy of an intervention to reduce older adults' sedentary behavior. Translational Behavioral Medicine 2017;7(1):52-61. [DOI: 10.1007/s13142-016-0394-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
Owari 2019 {published data only}
- Owari Y, Suzuki H, Miyatake N. "Active Guide" brochure reduces sedentary behavior of elderly people: a randomized controlled trial. Acta Medica Okayama 2019;73(5):427-32. [DOI] [PubMed] [Google Scholar]
Roberts 2019 {published data only}
- Roberts LM, Jaeger BC, Baptista LC, Harper SA, Gardner AK, Jackson EA, et al. Wearable technology to reduce sedentary behavior and CVD risk in older adults: a pilot randomized clinical trial. Clinical Interventions in Aging 2019;14:1817-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosenberg 2020 {published data only}
- Rosenberg DE, Anderson ML, Renz A, Matson TE, Lee AK, Greenwood-Hickman M, et al. Reducing sitting time in obese older adults: the I-STAND randomized controlled trial. Journal of Aging and Physical Activity 2020;28(6):864-74. [DOI: 10.1123/japa.2019-0470] [DOI] [PMC free article] [PubMed] [Google Scholar]
White 2017 {published data only}
- White I, Smith L, Aggio D, Shankar S, Begum S, Matei R, et al. On your feet to earn your seat: pilot RCT of a theory-based sedentary behaviour reduction intervention for older adults. Pilot Feasibility Studies 2017;3:23. [DOI: 10.1186/s40814-017-0139-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Annesi 2004 {published data only}
- Annesi JJ, Westcott WW, Gann S. Preliminary evaluation of a 10-wk. resistance and cardiovascular exercise protocol on physiological and psychological measures for a sample of older women. Perceptual and Motor Skills 2004;98(1):163-70. [DOI: 10.2466/pms.98.1.163-170] [DOI] [PubMed] [Google Scholar]
Arrogi 2017 {published data only}
- Arrogi A, Bogaerts A, Seghers J, Devloo K, Vanden Abeele V, Geurts L, et al. Evaluation of stAPP: a smartphone-based intervention to reduce prolonged sitting among Belgian adults. Health Promotion International 2017;34(1):16-27. [DOI: 10.1093/heapro/dax046] [DOI] [PubMed] [Google Scholar]
Ashe 2019 {published data only}
- Ashe MC, Edwards NY, Taylor A, Burnett L, Giangregorio L, Milne K, et al. Return to everyday activity in the community and home: a feasibility study for a lifestyle intervention to sit less, move more, and be strong. Pilot and Feasibility Studies 2019;5:84-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aunger 2020 {published data only}
- Aunger JA, Greaves CJ, Davis ET, Asamane EA, Whittaker AC, Greig CA. A novel behavioural INTErvention to REduce Sitting Time in older adults undergoing orthopaedic surgery (INTEREST): results of a randomised-controlled feasibility study. Aging Clinical and Experimental Research 2020;32(12):2565-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Awick 2017 {published data only}
- Awick EA, Ehlers D, Fanning J, Phillips SM, Wojcicki T, Mackenzie MJ, et al. Effects of a home-based DVD-delivered physical activity program on self-esteem in older adults: results from a randomized controlled trial. Psychosomatic Medicine 2017;79(1):71-80. [DOI: 10.1097/psy.0000000000000358] [DOI] [PMC free article] [PubMed] [Google Scholar]
Azizan 2016 {published data only}
- Azizan A, Justine M. Effects of a behavioral and exercise program on depression and quality of life in community-dwelling older adults: a controlled, quasi-experimental study. Journal of Gerontological Nursing 2016;42(2):45-54. [DOI: 10.3928/00989134-20151124-01] [DOI] [PubMed] [Google Scholar]
Britten 2017 {published data only}
- Britten L, Addington C, Astill S. Dancing in time: feasibility and acceptability of a contemporary dance programme to modify risk factors for falling in community dwelling older adults. BMC Geriatrics 2017;17(1):83. [DOI: 10.1186/s12877-017-0476-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Buman 2011 {published data only}
- Buman MP, Giacobbi PR, Dzierzewski JM, Morgan AA, McCrae CS, Roberts BL, et al. Peer volunteers improve long-term maintenance of physical activity with older adults: a randomized controlled trial. Journal of Physical Activity & Health 2011;8 Suppl 2:S257-66. [PMC free article] [PubMed] [Google Scholar]
Burke 2013 {published data only}
- Burke L, Jancey J, Howat P, Lee A, Kerr D, Shilton T, et al. Physical activity results of a home-based physical activity and nutrition program for seniors (PANS). Journal of Science and Medicine in Sport 2012;15:S47-8. [DOI: 10.1016/j.jsams.2012.11.115] [DOI] [Google Scholar]
- Burke L, Lee AH, Jancey J, Xiang L, Kerr DA, Howat PA, et al. Physical activity and nutrition behavioural outcomes of a home-based intervention program for seniors: a randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2013;10:14. [DOI: 10.1186/1479-5868-10-14] [DOI] [PMC free article] [PubMed] [Google Scholar]
Burton 1995 {published data only}
- Burton LC, Paglia MJ, German PS, Shapiro S, Damiano AM. The effect among older persons of a general preventive visit on three health behaviors: smoking, excessive alcohol drinking, and sedentary lifestyle. The Medicare Preventive Services Research Team. Preventive Medicine 1995;24(5):492-7. [DOI: 10.1006/pmed.1995.1078] [DOI] [PubMed] [Google Scholar]
Chang 2013 {published data only}
- Chang AK, Fritschi C, Kim MJ. Sedentary behavior, physical activity, and psychological health of Korean older adults with hypertension: effect of an empowerment intervention. Research in Gerontological Nursing 2013;6(2):81-8. [DOI: 10.3928/19404921-20121219-01] [DOI] [PubMed] [Google Scholar]
Chiang 2019 {published data only}
- Chiang L, Heitkemper MM, Chiang SL, Tzeng WC, Lee MS, Hung YJ, et al. Motivational counseling to reduce sedentary behaviors and depressive symptoms and improve health-related quality of life among women with metabolic syndrome. Journal of Cardiovascular Nursing 2019;34(4):327-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Darvall 2016 {published data only}
- Darvall JN, Parker A, Story DA. Feasibility and acceptability of remotely monitored pedometer-guided physical activity. Anaesthesia and Intensive Care 2016;44(4):501-6. [DOI: 10.1177/0310057X1604400415] [DOI] [PubMed] [Google Scholar]
De Greef 2010 {published data only}
- De Greef K, Deforche B, Tudor-Locke C, De Bourdeaudhuij I. A cognitive-behavioural pedometer-based group intervention on physical activity and sedentary behaviour in individuals with type 2 diabetes. Health Education Research 2010;25(5):724-36. [DOI: 10.1093/her/cyq017] [DOI] [PMC free article] [PubMed] [Google Scholar]
De Greef 2011 {published data only}
- De Greef KP, Deforche BI, Ruige JB, Bouckaert JJ, Tudor-Locke CE, Kaufman et al. The effects of a pedometer-based behavioral modification program with telephone support on physical activity and sedentary behavior in type 2 diabetes patients. Patient Education and Counseling 2011;84(2):275-9. [DOI: 10.1016/j.pec.2010.07.010] [DOI] [PubMed] [Google Scholar]
Edwards 2018 {published data only}
- Edwards MK, Loprinzi PD. Effects of a sedentary intervention on cognitive function. American Journal of Health Promotion 2018;32(3):595‐605. [DOI: 10.1177/0890117116688692] [DOI] [PubMed] [Google Scholar]
Engelen 2019 {published data only}
- Engelen L, Drayton BA, Young S, Daley M, Milton K, Bauman A, et al. Impact and process evaluation of a co-designed 'Move More, Sit Less' intervention in a public sector workplace. Work 2019;64(3):587-99. [DOI] [PubMed] [Google Scholar]
Fanning 2016 {published data only}
- Fanning J, Porter G, Awick EA, Wojcicki TR, Gothe NP, Roberts SA, et al. Effects of a DVD-delivered exercise program on patterns of sedentary behavior in older adults: a randomized controlled trial. Preventive Medicine Reports 2016;3:238-43. [DOI: 10.1016/j.pmedr.2016.03.005] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fennell 2016 {published data only}
- Fennell C. The Effects of a 16-Week Exercise Program and Cell Phone Use on Physical Activity, Sedentary Behavior, and Health-Related Outcomes [PhD thesis]. Kent State University, 2016. [Google Scholar]
Fitzsimons 2013 {published data only}
- Fitzsimons CF, Kirk A, Baker G, Michie F, Kane C, Mutrie N. Using an individualised consultation and activPAL feedback to reduce sedentary time in older Scottish adults: results of a feasibility and pilot study. Preventive Medicine 2013;57(5):718-20. [DOI: 10.1016/j.ypmed.2013.07.017] [DOI] [PubMed] [Google Scholar]
Gardiner 2011 {published data only}
- Gardiner PA, Eakin EG, Healy GN, Owen N. Feasibility of reducing older adults' sedentary time. American Journal of Preventive Medicine 2011;41(2):174-7. [DOI: 10.1016/j.amepre.2011.03.020] [DOI] [PubMed] [Google Scholar]
Goldstein 1999 {published data only}
- Goldstein MG, Pinto BM, Marcus BH, Lynn H, Jette AM, Rakowski W, et al. Physician-based physical activity counseling for middle-aged and older adults: a randomized trial. Annals of Behavioral Medicine 1999;21(1):40-7. [DOI: 10.1007/bf02895032] [DOI] [PubMed] [Google Scholar]
Greenwood‐Hickman 2016 {published data only}
- Greenwood-Hickman MA, Renz A, Rosenberg DE. Motivators and barriers to reducing sedentary behavior among overweight and obese older adults. Gerontologist 2016;56(4):660-8. [DOI: 10.1093/geront/gnu163] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hansen 2012 {published data only}
- Hansen AW, Gronbaek M, Helge JW, Severin M, Curtis T, Tolstrup JS. Effect of a Web-based intervention to promote physical activity and improve health among physically inactive adults: a population-based randomized controlled trial. Journal of Medical Internet Research 2012;14(5):e145. [DOI: 10.2196/jmir.2109] [DOI] [PMC free article] [PubMed] [Google Scholar]
Harvey 2018 {published data only}
- Harvey JA, Chastin SFM, Skelton DA. Breaking sedentary behaviour has the potential to increase/maintain function in frail older adults. Journal of Frailty, Sarcopenia and Falls 2018;3:26-34. [DOI: 10.22540/JFSF-03-026] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hetherington 2015 {published data only}
- Hetherington SA, Borodzicz JA, Shing CM. Assessing the real world effectiveness of the Healthy Eating Activity and Lifestyle (HEAL) program. Health Promotion Journal of Australia 2015;26(2):93-8. [DOI: 10.1071/he14031] [DOI] [PubMed] [Google Scholar]
Kegler 2012 {published data only}
- Kegler MC, Alcantara I, Veluswamy JK, Haardorfer R, Hotz JA, Glanz K. Results from an intervention to improve rural home food and physical activity environments. Progress in Community Health Partnerships: Research, Education, and Action 2012;6(3):265-77. [DOI: 10.1353/cpr.2012.0042] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kendzor 2016 {published data only}
- Kendzor DE, Shuval K, Gabriel KP, Businelle MS, Ma P, High RR, et al. Impact of a mobile phone intervention to reduce sedentary behavior in a community sample of adults: a quasi-experimental evaluation. Journal of Medical Internet Research 2016;18(1):e19. [DOI: 10.2196/jmir.5137] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kerse 2005 {published data only}
- Kerse N, Elley CR, Robinson E, Arroll B. Is physical activity counseling effective for older people? A cluster randomized, controlled trial in primary care. Journal of the American Geriatrics Society 2005;53(11):1951-6. [DOI] [PubMed] [Google Scholar]
King 2016 {published data only}
- King AC, Hekler EB, Grieco LA, Winter SJ, Sheats JL, Buman MP, et al. Effects of three motivationally targeted mobile device applications on initial physical activity and sedentary behavior change in midlife and older adults: a randomized trial. PLOS ONE 2016;11(6):e0156370. [DOI: 10.1371/journal.pone.0156370] [DOI] [PMC free article] [PubMed] [Google Scholar]
Koltyn 2019 {published and unpublished data}
- Koltyn KF, Crombie KM, Brellenthin AG, Leitzelar B, Ellingson LD, Renken J, et al. Intervening to reduce sedentary behavior in older adults - pilot results. Health Promotion Perspective 2019;9(1):71-6. [DOI: 10.15171/hpp.2019.09] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kuck 2014 {published data only}
- Kuck J, Pantke M, Flick U. Effects of social activation and physical mobilization on sleep in nursing home residents. Geriatric Nursing 2014;35(6):455-61. [DOI: 10.1016/j.gerinurse.2014.08.009] [DOI] [PubMed] [Google Scholar]
Lakerveld 2013 {published data only}
- Lakerveld J, Bot SDM, Ploeg HP, Nijpels G. The effects of a lifestyle intervention on leisure-time sedentary behaviors in adults at risk: the Hoorn Prevention Study, a randomized controlled trial. Preventive Medicine 2013;57(4):351-6. [DOI: 10.1016/j.ypmed.2013.06.011] [DOI] [PubMed] [Google Scholar]
Lerma 2017 {published data only}
- Lerma NL, Swartz AM, Rowley TW, Maeda H, Strath SJ. Increasing the energy expenditure of seated activities in older adults with a portable elliptical device. Journal of Aging and Physical Activity 2017;25(1):99-104. [DOI: 10.1123/japa.2015-0277] [DOI] [PubMed] [Google Scholar]
Lerma 2020 {published data only}
- Lerma NL, Cho CC, Swartz AM, Maeda H, Cho Y, Strath SJ. Acceptance and feasibility of seated elliptical pedaling to replace sedentary behavior in older adults. Journal of Aging and Physical Activity 2020;28:844–53. [DOI] [PubMed] [Google Scholar]
Lewis 2016 {published data only}
- Lewis LK, Rowlands AV, Gardiner PA, Standage M, English C, Olds T. Small Steps: preliminary effectiveness and feasibility of an incremental goal-setting intervention to reduce sitting time in older adults. Maturitas 2016;85:64-70. [DOI: 10.1016/j.maturitas.2015.12.014] [DOI] [PubMed] [Google Scholar]
Lubans 2013 {published data only}
- Lubans DR, Mundey CM, Lubans NJ, Lonsdale CC. Pilot randomized controlled trial: elastic-resistance-training and lifestyle-activity intervention for sedentary older adults. Journal of Aging and Physical Activity 2013;21(1):20-32. [DOI] [PubMed] [Google Scholar]
Lyons 2014 {published data only}
- Lyons EJ, Lewis ZH. An activity monitor and mobile device intervention is feasible among older adults. Clinical and Translational Science 2014;7(3):254-5. [DOI: 10.1111/cts.12171] [DOI] [Google Scholar]
Matei 2015 {published data only}
- Matei R, Thune-Boyle I, Hamer M, Iliffe S, Fox KR, Jefferis BJ, et al. Acceptability of a theory-based sedentary behaviour reduction intervention for older adults ('On Your Feet to Earn Your Seat'). BMC Public Health 2015;15:606. [DOI: 10.1186/s12889-015-1921-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Matson 2018 {published data only}
- Matson TE, Renz AD, Takemoto ML, McClure JB, Rosenberg DE. Acceptability of a sitting reduction intervention for older adults with obesity. BMC Public Health 2018;18(1):706. [DOI: 10.1186/s12889-018-5616-1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Matson 2019 {published data only}
- Matson TE, Anderson ML, Renz AD, Greenwood-Hickman MA, McClure JB, Rosenberg DE. Changes in self-reported health and psychosocial outcomes in older adults enrolled in sedentary behavior intervention study. American Journal of Health Promotion 2019;33(7):1053-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Muller 2016 {published data only}
- Muller AM, Khoo S, Morris T. Text messaging for exercise promotion in older adults from an upper-middle-income country: randomized controlled trial. Journal of Medical Internet Research 2016;18(1):e5. [DOI: 10.2196/jmir.5235] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nicklas 2014 {published data only}
- Nicklas BJ, Gaukstern JE, Beavers KM, Newman JC, Leng X, Rejeski WJ. Self‐monitoring of spontaneous physical activity and sedentary behavior to prevent weight regain in older adults. Obesity 2014;22(6):1406-12. [DOI: 10.1002/oby.20732] [DOI] [PMC free article] [PubMed] [Google Scholar]
Overgaard 2018 {published data only}
- Overgaard K, Nannerup K, Lunen MKB, Maindal HT, Larsen RG. Exercise more or sit less? A randomized trial assessing the feasibility of two advice-based interventions in obese inactive adults. Journal of Science and Medicine in Sport 2018;21(7):708-13. [DOI: 10.1016/j.jsams.2017.10.037] [DOI] [PubMed] [Google Scholar]
Paing 2019 {published data only}
- Paing AC, McMillan KA, Kirk AF, Collier A, Hewitt A, Chastin SFM. Dose-response between frequency of breaks in sedentary time and glucose control in type 2 diabetes: a proof of concept study. Journal of Science and Medicine in Sport 2019;22(7):808-13. [DOI: 10.1016/j.jsams.2019.01.017] [DOI] [PubMed] [Google Scholar]
Paschoa 2016 {published data only}
- Paschoa L, Ashton C. The evaluation of an exercise program for older rural adults. Activities, Adaptation and Aging 2016;40(1):67-77. [DOI: 10.1080/01924788.2016.1127075] [DOI] [Google Scholar]
Pomeroy 2011 {published data only}
- Pomeroy SH, Scherer Y, Runkawatt V, Iamsumang W, Lindemann J, Resnick B. Person-environment fit and functioning among older adults in a long-term care setting. Geriatric Nursing 2011;32(5):368-78. [DOI: 10.1016/j.gerinurse.2011.07.002] [DOI] [PubMed] [Google Scholar]
Poppe 2019 {published data only}
- Poppe L, De Bourdeaudhuij I, Verloigne M, Shadid S, Cauwenberg JV, Compernolle S, et al. Efficacy of a self-regulation-based electronic and mobile health intervention targeting an active lifestyle in adults having type 2 diabetes and in adults aged 50 years or older: two randomized controlled trials. Journal of Medical Internet Research 2019;21(8):e13363. [DOI: 10.2196/13363] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rasinaho 2012 {published data only}
- Rasinaho M, Hirvensalo M, Tormakangas T, Leinonen R, Lintunen T, Rantanen T. Effect of physical activity counseling on physical activity of older people in Finland. Health Promotion International 2012;27(4):463-74. [DOI] [PubMed] [Google Scholar]
Rockette‐Wagner 2017 {published data only}
- Rockette-Wagner B, Storti KL, Dabelea D, Edelstein S, Florez H, Franks PW, et al. Activity and sedentary time 10 years after a successful lifestyle intervention: The Diabetes Prevention Program. American Journal of Preventive Medicine 2017;52(3):292-9. [DOI: 10.1016/j.amepre.2016.10.007] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosenberg 2015 {published data only}
- Rosenberg DE, Gell NM, Jones SMW, Renz A, Kerr J, Gardiner PA, et al. The feasibility of reducing sitting time in overweight and obese older adults. Health Education & Behavior 2015;42(5):669-76. [DOI: 10.1177/1090198115577378] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ruscello 2014 {published data only}
- Ruscello B, D’Ottavio S, Padua E, Tonelli C, Pantanella L. The influence of music on exercise in a group of sedentary elderly women: an important tool to help the elderly to stay active. Journal of Sports Medicine & Physical Fitness 2014;54(4):536-44. [PubMed] [Google Scholar]
Sakurai 2012 {published data only}
- Sakurai T, Iimuro S, Sakamaki K, Umegaki H, Araki A, Ohashi Y, et al. Risk factors for a 6-year decline in physical disability and functional limitations among elderly people with type 2 diabetes in the Japanese elderly diabetes intervention trial. Geriatrics & Gerontology International 2012;12:117-26. [DOI: 10.1111/j.1447-0594.2011.00819.x] [DOI] [PubMed] [Google Scholar]
Siddique 2017 {published data only}
- Siddique J, Chavez PJ, Craft LL, Freedson P, Spring B. The effect of changes in physical activity on sedentary behavior: results from a randomized lifestyle intervention trial. American Journal of Health Promotion 2017;31(4):287-95. [DOI: 10.4278/ajhp.150129-QUAN-693] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sparker‐Griffin 2013 {published data only}
- Sparker-Griffin C. Wii-habilitation: using Wii as an effective intervention tool for seniors. OT Practice 2013;18(3):18-9. [Google Scholar]
Spring 2018 {published data only}
- Spring B, Pellegrini C, McFadden HG, Pfammatter AF, Stump TK, Siddique J, et al. Multicomponent mHealth intervention for large, sustained change in multiple diet and activity risk behaviors: The Make Better Choices 2 randomized controlled trial. Journal of Medical Internet Research 2018;20(6):e10528. [DOI: 10.2196/10528] [DOI] [PMC free article] [PubMed] [Google Scholar]
Suboc 2016 {published data only}
- Suboc TB, Knabel D, Strath SJ, Dharmashankar K, Coulliard A, Malik M, et al. Associations of reducing sedentary time with vascular function and insulin sensitivity in older sedentary adults. American Journal of Hypertension 2016;29(1):46-53. [DOI: 10.1093/ajh/hpv063] [DOI] [PMC free article] [PubMed] [Google Scholar]
Takemoto 2020 {published data only}
- Takemoto M, Godbole S, Rosenberg DE, Nebeker C, Natarajan L, Madanat H, et al. The search for the ejecting chair: a mixed-methods analysis of tool use in a sedentary behavior intervention. Translational Behavioral Medicine 2020;10(1):186-94. [DOI: 10.1093/tbm/iby106] [DOI] [PMC free article] [PubMed] [Google Scholar]
Taylor 2016 {published data only}
- Taylor N. A 2-year physical activity program for sedentary older adults does not improve cognitive functioning more than a health education program. Journal of Physiotherapy 2016;62(2):115. [DOI: 10.1016/j.jphys.2015.12.008] [DOI] [PubMed] [Google Scholar]
Tennstedt 2013 {published data only}
- Tennstedt SL, Unverzagt FW. The ACTIVE study: study overview and major findings. Journal of Aging & Health 2013;25(8):3S-20S. [DOI: 10.1177/0898264313518133] [DOI] [PMC free article] [PubMed] [Google Scholar]
Toto 2012 {published data only}
- Toto PE, Raina KD, Holm MB, Schlenk EA, Rubinstein EN, Rogers JC. Outcomes of a multicomponent physical activity program for sedentary, community-dwelling older adults. Journal of Aging and Physical Activity 2012;20(3):363-78. [DOI: 10.1123/japa.20.3.363] [DOI] [PubMed] [Google Scholar]
Turunen 2020 {published data only}
- Turunen KM, Aaltonen-Määttä L, Törmäkangas T, Rantalainen T, Portegijs E, Keikkala S, et al. Effects of an individually targeted multicomponent counseling and home-based rehabilitation program on physical activity and mobility in community-dwelling older people after discharge from hospital: a randomized controlled trial. Clinical Rehabilitation 2020;34(4):491-503. [DOI: 10.1177/0269215519901155] [DOI] [PubMed] [Google Scholar]
Valerio 2012 {published data only}
- Valerio M, Vilela F, Da Silva L, Ramos L. Intervention to increase older adults' physical activity: results of the Epidoso project, Brazil. Journal of Science and Medicine in Sport 2012;15:S47. [DOI: 10.1016/j.jsams.2012.11.114] [DOI] [Google Scholar]
Van Hoecke 2014 {published data only}
- Van Hoecke AS, Delecluse C, Bogaerts A, Boen F. The long-term effectiveness of need-supportive physical activity counseling compared with a standard referral in sedentary older adults. Journal of Aging and Physical Activity 2014;22(2):186-98. [DOI: 10.1123/japa.2012-0261] [DOI] [PubMed] [Google Scholar]
von Berens 2018 {published data only}
- von Berens Å, Koochek A, Nydahl M, Fielding RA, Gustafsson T, Kirn DR, et al. “Feeling more self-confident, cheerful and safe”. Experiences from a health-promoting intervention in community dwelling older adults - a qualitative study. Journal of Nutrition, Health and Aging 2018;22(4):541-8. [DOI: 10.1007/s12603-017-0981-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
von Bonsdorff 2009 {published data only}
- Bonsdorff MB, Leinonen R, Kujala UM, Heikkinen E, Törmäkangas T, Hirvensalo M, et al. Effect of physical activity counseling on home care use in older people. Journal of the American Geriatrics Society 2009;57(3):571-3. [DOI: 10.1111/j.1532-5415.2009.02163.x] [DOI] [PubMed] [Google Scholar]
Walters 2017 {published data only}
- Walters K, Kharicha K, Goodman C, Handley M, Manthorpe J, Cattan M, et al. Promoting independence, health and well-being for older people: a feasibility study of computer-aided health and social risk appraisal system in primary care. BMC Family Practice 2017;18(1):47. [DOI: 10.1186/s12875-017-0620-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wheeler 2019a {published data only}
- Wheeler MJ, Dunstan DW, Smith B, Smith KJ, Scheer A, Lewis J, et al. Morning exercise mitigates the impact of prolonged sitting on cerebral blood flow in older adults. Journal of Applied Physiology 2019;126(4):1049-55. [DOI: 10.1152/japplphysiol.00001.2019] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wheeler 2019b {published data only}
- Wheeler MJ, Dunstan DW, Ellis KA, Cerin E, Phillips S, Lambert G, et al. Effect of morning exercise with or without breaks in prolonged sitting on blood pressure in older overweight/obese adults: evidence for sex differences. Hypertension 2019;73(4):859-67. [DOI: 10.1161/HYPERTENSIONAHA.118.12373] [DOI] [PubMed] [Google Scholar]
Yan 2009 {published data only}
- Yan T, Wilber KH, Aguirre R, Trejo L. Do sedentary older adults benefit from community-based exercise? Results from the Active Start program. Gerontologist 2009;49(6):847-55. [DOI: 10.1093/geront/gnp113] [DOI] [PubMed] [Google Scholar]
Yeom 2010 {published data only}
- Yeom H, Keller C, Fleury J, Belyea M. Culturally tailored motivational strategies for increasing regular physical activity in older Korean Americans: challenges and recommendations. Communicating Nursing Research 2010;43:248. [Google Scholar]
Yeom 2014 {published data only}
- Yeom HA, Fleury J. A motivational physical activity intervention for improving mobility in older Korean Americans. Western Journal of Nursing Research 2014;36(6):713-31. [DOI: 10.1177/0193945913511546] [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Kleinke 2018 {published data only}
- Kleinke F, Schwaneberg T, Weymar F, Penndorf P, Ulbricht S, Lehnert K, et al. MOVING: Motivation-oriented intervention study for the elderly in Greifswald: study protocol for a randomized controlled trial. Trials 2018;19(1):57. [DOI: 10.1186/s13063-017-2425-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Adams 2013
- Adams MM, Davis PG, Gill DL. A hybrid online intervention for reducing sedentary behavior in obese women. Frontiers in Public Health 2013;1:45. [DOI: 10.3389/fpubh.2013.00045] [DOI] [PMC free article] [PubMed] [Google Scholar]
Alpass 2003
- Alpass FM, Neville S. Loneliness, health and depression in older males. Aging & Mental Health 2003;7(3):212-6. [DOI: 10.1080/1360786031000101193] [DOI] [PubMed] [Google Scholar]
Aunger 2019
- Aunger JA, Doody P, Greig CA. Interventions targeting sedentary behavior in non-working older adults: a systematic review. Maturitas 2018;116:89–99. [DOI: 10.1016/j.maturitas.2018.08.002] [DOI] [PubMed] [Google Scholar]
Bandura 1986
- Bandura A. Englewood Cliffs NJ: Prentice Hall,. Prentice-Hall Inc, 1986. [Google Scholar]
Bankoski 2011
- Bankoski A, Harris TB, McClain JJ, Brychta RJ, Caserotti P, Chen KY, et al. Sedentary activity associated with metabolic syndrome independent of physical activity. Diabetes Care 2011;34(2):497-503. [DOI: 10.2337/dc10-0987] [DOI] [PMC free article] [PubMed] [Google Scholar]
Biswas 2015
- Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Annals of Internal Medicine 2015;162(2):123-32. [DOI: 10.7326/M14-1651] [DOI] [PubMed] [Google Scholar]
Buck 2019
- Buck C, Loyen A, Foraita R, Van Cauwenberg J, De Craemer M, Mac Donncha C, et al. Factors influencing sedentary behaviour: a system based analysis using Bayesian networks within DEDIPAC. PLOS ONE 2019;14(1):e0211546. [DOI: 10.1371/journal.pone.0211546] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bull 2020
- Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. British Journal of Sports Medicine 2020;54:1451-62. [DOI: 10.1136/bjsports-2020-102955] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chastin 2010
- Chastin SFM, Granat M. Methods for objective measure, quantification and analysis of sedentary behaviour and inactivity. Gait & Posture 2010;31(1):82-6. [DOI: 10.1016/j.gaitpost.2009.09.002] [DOI] [PubMed] [Google Scholar]
Chastin 2013
- Chastin S, Scwartz U, Skelton D. Development of a consensus taxonomy of sedentary behaviors (SIT): report of Delphi Round 1. PLOS ONE 2013;8(12):e82313. [DOI: 10.1371/journal.pone.0082313] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chastin 2014
- Chastin SFM, Mandrichenko O, Helbostadt JL, Skelton DA. Associations between objectively-measured sedentary behaviour and physical activity with bone mineral density in adults and older adults, the NHANES study. Bone 2014;64:254-62. [DOI: 10.1016/j.bone.2014.04.009] [DOI] [PubMed] [Google Scholar]
Chastin 2015a
- Chastin SFM, Egerton T, Leask C, Stamatakis E. Meta-analysis of the relationship between breaks in sedentary behavior and cardiometabolic health. Obesity 2015;23(9):1800-10. [DOI: 10.1002/oby.21180] [DOI] [PubMed] [Google Scholar]
Chastin 2015b
- Chastin SFM, Buck C, Freiberger E, Murphy M, Brug J, Cardon G, et al. Systematic literature review of determinants of sedentary behaviour in older adults: a DEDIPAC study. International Journal of Behavioral Nutrition and Physical Activity 2015;12(1):127. [DOI: 10.1186/s12966-015-0292-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chastin 2015c
- Chastin SFM, Winkler EAH, Eakin EG, Gardiner PA, Dunstan DW, Owen N, et al. Sensitivity to change of objectively-derived measures of sedentary behavior. Measurement in Physical Education and Exercise Science 2015;19(3):138-47. [DOI: 10.1080/1091367X.2015.1050592] [DOI] [Google Scholar]
Chastin 2016
- Chastin S, De Craemer M, Lien N, Bernaards C, Buck C, Oppert JM, et al. The SOS-Framework (Systems of Sedentary Behaviours): an international transdisciplinary consensus framework for the study of determinants, research priorities and policy on sedentary behaviour across the life course: a DEDIPAC-study. International Journal of Behavioral Nutrition and Physical Activity 2016;13(1):83. [DOI: 10.1186/s12966-016-0409-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chastin 2017
- Chastin S, Gardiner PA, Ashe MC, Harvey JA, Leask CD, Balogun S, et al. Interventions for reducing sedentary behaviour in community-dwelling older adults. Cochrane Database of Systematic Reviews 2017, Issue 9. Art. No: CD012784. [DOI: 10.1002/14651858.CD012784] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chastin 2018
- Chastin SFM, Dontje ML, Skelton DA, Čukić I, Shaw RJ, Gill JMR, et al. Systematic comparative validation of self-report measures of sedentary time against an objective measure of postural sitting (activPAL). International Journal of Behavioral Nutrition and Physical Activity 2018;15(1):21. [DOI: 10.1186/s12966-018-0652-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Copeland 2017
- Copeland JL, Ashe MC, Biddle SJH, Brown WJ, Buman MP, Chastin S, et al. Sedentary time in older adults: a critical review of measurement, associations with health, and interventions. British Journal of Sports Medicine 2017;51:1539-47. [DOI: 10.1136/bjsports-2016-097210] [DOI] [PubMed] [Google Scholar]
Covidence [Computer program]
- Covidence. Version accessed 26 January 2021. Melbourne, Australia: Veritas Health Innovation. Available at covidence.org.
CPHG 2011
- Cochrane Public Health Group. Guide for developing a Cochrane protocol. ph.cochrane.org/review-authors (accessed prior to 21 June 2021).
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG. Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins JPT, Green S, editors(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
de Greef 2010
- Greef K, Deforche B, Tudor-Locke C, Bourdeaudhuij I. A cognitive-behavioural pedometer-based group intervention on physical activity and sedentary behaviour in individuals with type 2 diabetes. Health Education Research 2010;25(5):724-36. [DOI: 10.1093/her/cyq017] [DOI] [PMC free article] [PubMed] [Google Scholar]
de Rezende 2014
- Rezende LFM, Rey-López JP, Matsudo VKR, Luiz OC. Sedentary behavior and health outcomes among older adults: a systematic review. BMC Public Health 2014;14(1):333. [DOI: 10.1186/1471-2458-14-333] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dogra 2012
- Dogra S, Stathokostas L. Sedentary behavior and physical activity are independent predictors of successful aging in middle-aged and older adults. Journal of Aging Research 2012;2012:Article ID 190654. [DOI: 10.1155/2012/190654] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dogra 2017
- Dogra S, Ashe MC, Biddle SJH, Brown WJ, Buman MP, Chastin S, et al. Sedentary time in older men and women: an international consensus statement and research priorities. British Journal of Sports Medicine 2017;51:1526-32. [DOI: 10.1136/bjsports-2016-097209] [DOI] [PMC free article] [PubMed] [Google Scholar]
DoH 2019
- Department of Health and Social Care. UK Chief Medical Officers' Physical Activity Guidelines. assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/832868/uk-chief-medical-officers-physical-activity-guidelines.pdf (accessed prior to 21 June 2021).
Dunstan 2012
- Dunstan DW, Kingwell BA, Larsen R, Healy GN, Cerin E, Hamilton MT, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care 2012;35(5):976-83. [DOI: 10.2337/dc11-1931] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ekelund 2016
- Ekelund U, Steene-Johannessen J, Brown JW, Fagerland MW, Owen N, Powell KE, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016;388(10051):1302-10. [DOI: 10.1016/S0140-6736(16)30370-1] [DOI] [PubMed] [Google Scholar]
Elavsky 2019
- Elavsky S, Knapova L, Klocek A, Smahel D. Mobile health interventions for physical activity, sedentary behavior, and sleep in adults aged 50 years and older: a systematic literature review. Journal of Aging and Physical Activity 2019;27(4):565-93. [DOI: 10.1123/japa.2017-0410] [DOI] [PubMed] [Google Scholar]
Gardiner 2011
- Gardiner PA, Eakin EG, Healy GN, Owen N. Feasibility of reducing older adults’ sedentary time. American Journal of Preventive Medicine 2011;41(2):174-7. [DOI: 10.1016/j.amepre.2011.03.020] [DOI] [PubMed] [Google Scholar]
Gardner 2016
- Gardner B, Smith L, Lorencatto F, Hamer M, Biddle SJ. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychology Review 2016;10(1):89-112. [DOI: 10.1080/17437199.2015.1082146] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gomersall 2015
- Gomersall SR, Maher C, English CK, Rowland A, Olds T. Time regained: when people stop a physical activity program, how does their time use change? A randomised controlled trial. PLOS ONE 2015;10(5):e0126665. [DOI: 10.1371/journal.pone.0126665] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Version accessed 20 May 2021. Hamilton (ON): McMaster University (developed by Evidence Prime). Available at gradepro.org.
Greenwood‐Hickman 2016
- Greenwood-Hickman MA, Renz A, Rosenberg DE. Motivators and barriers to reducing sedentary behavior among overweight and obese older adults. Gerontologist 2016;56(4):660-8. [DOI: 10.1093/geront/gnu163] [DOI] [PMC free article] [PubMed]
Guyatt 2011
- Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. Journal of Clinical Epidemiology 2011;64(4):380-2. [DOI: 10.1016/j.jclinepi.2010.09.011] [DOI] [PubMed] [Google Scholar]
Harvey 2013
- Harvey JA, Chastin SFM, Skelton DA. Prevalence of sedentary behavior in older adults: a systematic review. International Journal of Environmental Research and Public Health 2013;10(12):6645-61. [DOI: 10.3390/ijerph10126645] [DOI] [PMC free article] [PubMed] [Google Scholar]
Harvey 2015
- Harvey JA, Chastin SF, Skelton DA. How sedentary are older people? A systematic review of the amount of sedentary behavior. Journal of Aging and Physical Activity 2015;23(3):471-87. [DOI: 10.1123/japa.2014-0164] [DOI] [PubMed] [Google Scholar]
Healy 2008
- Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Zimmet PZ, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care 2008;31(4):661-6. [DOI: 10.2337/dc07-2046] [DOI] [PubMed] [Google Scholar]
Healy 2011
- Healy GN, Matthews CE, Dunstan DW, Winkler EAH, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. European Heart Journal 2011;32(5):590-7. [DOI: 10.1093/eurheartj/ehq451] [DOI] [PMC free article] [PubMed] [Google Scholar]
Henson 2013
- Henson J, Yates T, Biddle SJH, Edwardson CL, Khunti K, Wilmot EG, et al. Associations of objectively measured sedentary behaviour and physical activity with markers of cardiometabolic health. Diabetologia 2013;56(5):1012-20. [DOI: 10.1007/s00125-013-2845-9] [DOI] [PubMed] [Google Scholar]
Hertzog 2008
- Hertzog C, Kramer AF, Wilson RS, Lindenberger U. Enrichment effects on adult cognitive development. Psychological Science in the Public Interest 2008;9:1-65. [DOI: 10.1111/j.1539-6053.2009.01034.x] [DOI] [PubMed] [Google Scholar]
Higgins 2021
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook. [DOI] [PMC free article] [PubMed]
Katzmarzyk 2009
- Katzmarzyk T, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Medicine & Science in Sports & Exercise 2009;41(5):998-1005. [DOI: 10.1249/MSS.0b013e3181930355] [DOI] [PubMed] [Google Scholar]
Katzmarzyk 2010
- Katzmarzyk PT. Physical activity, sedentary behavior, and health: paradigm paralysis or paradigm shift? Diabetes 2010;59(11):2717-25. [DOI: 10.2337/db10-0822] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kerr 2012
- Kerr J, Rosenberg DE, Nathan A, Millstein R, Carlson J, Crist K, et al. Applying the ecological model of behavior change to a physical activity trial in retirement communities: description of the study protocol. Contemporary Clinical Trials 2012;33(6):1180-8. [DOI: 10.1016/j.cct.2012.08.005] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kerr 2018
- Kerr J, Rosenberg D, Millstein RA, Bolling K, Crist K, Takemoto M, et al. Cluster randomized controlled trial of a multilevel physical activity intervention for older adults. International Journal of Behavioral Nutrition and Physical Activity 2018;15(1):32. [DOI: 10.1186/s12966-018-0658-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
King 2001
- King AC. Interventions to promote physical activity by older adults. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 2001;56:36-46. [DOI: 10.1093/gerona/56.suppl_2.36] [DOI] [PubMed] [Google Scholar]
Laforge 1999
- Laforge RG, Rossi JS, Prochaska JO, Velicer WF, Levesque D, McHorney C. Stage of regular exercise and health-related quality of life. Preventive Medicine 1999;28(4):349-60. [DOI: 10.1006/pmed.1998.0429] [DOI] [PubMed] [Google Scholar]
Lauder 2006
- Lauder W, Mummery K, Jones M, Caperchione C. A comparison of health behaviours in lonely and non-lonely populations. Psychology, Health & Medicine 2006;11(2):233-45. [DOI: 10.1080/13548500500266607] [DOI] [PubMed] [Google Scholar]
Leask 2015
- Leask C, Harvey JA, Skelton DA, Chastin SFM. The context of sedentary behaviour in older adults (what, where, why, when and with whom). European Review of Aging and Physical Activity 2015;12:4-8. [DOI: 10.1186/s11556-015-0146-7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Leask 2016
- Leask CF, Sandlund M, Skelton DA, Tulle E, Chastin SFM. Modifying older adults’ daily sedentary behaviour using an asset-based solution: views from older adults. AIMS Public Health 2016;3(3):542-54. [DOI: 10.3934/publichealth.2016.3.542] [DOI] [PMC free article] [PubMed] [Google Scholar]
Leask 2017
- Leask CF, Sandlund M, Skelton DA, Chastin SFM on behalf of the GrandStand Research Group. Co-creating a tailored public health intervention to reduce older adults’ sedentary behaviour. Health Education Journal 2017;5:595–608. [DOI: 10.1177/0017896917707785] [DOI] [Google Scholar]
Manns 2012
- Manns PJ, Dunstan DW, Owen N, Healy GN. Addressing the nonexercise part of the activity continuum: a more realistic and achievable approach to activity programming for adults with mobility disability? Physical Therapy 2012;92(4):614-25. [DOI: 10.2522/ptj.20110284] [DOI] [PubMed] [Google Scholar]
Martin 2015
- Martin A, Fitzsimons C, Jepson R, Saunders DH, Ploeg HP, Teixeira PJ, et al. Interventions with potential to reduce sedentary time in adults: systematic review and meta-analysis. British Journal of Sports Medicine 2015;49(16):1056-63. [DOI: 10.1136/bjsports-2014-094524] [DOI] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Medicine 2009;6(7):b2535. [DOI: 10.1371/journal.pmed.1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
Owen 2010
- Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population-health science of sedentary behavior. Exercise and Sport Sciences Reviews 2010;38(3):105–13. [DOI: 10.1097/JES.0b013e3181e373a2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Owen 2011
- Owen N, Sugiyama T, Eakin EE, Gardiner PA, Tremblay MS, Sallis JF. Adults’ sedentary behavior determinants and interventions. American Journal of Preventive Medicine 2011;41(2):189-96. [DOI: 10.1016/j.amepre.2011.05.013] [DOI] [PubMed] [Google Scholar]
Palmer 2019
- Palmer VJ, Gray CM, Fitzsimons CF, Mutrie N, Wyke S, Deary IJ, et al. What do older people do when sitting and why? Implications for decreasing sedentary behavior. Gerontologist 2019;59(4):686–97. [DOI: 10.1093/geront/gny020] [DOI] [PMC free article] [PubMed] [Google Scholar]
Perera 2007
- Perera R, Heneghan C, Yudkin P. Graphical method for depicting randomised trials of complex interventions. BMJ 2007;334(7585):127-9. [DOI: 10.1136/bmj.39045.396817.68] [DOI] [PMC free article] [PubMed] [Google Scholar]
Piercy 2018
- Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA 2018;320(19):2020-8. [DOI: 10.1001/jama.2018.14854] [DOI] [PMC free article] [PubMed] [Google Scholar]
Prince 2014
- Prince SA, Saunders TJ, Gresty K, Reid RD. A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: a systematic review and meta-analysis of controlled trials. Obesity Reviews 2014;15(11):905-19. [DOI: 10.1111/obr.12215] [DOI] [PMC free article] [PubMed] [Google Scholar]
Prochaska 1992
- Prochaska JO, DiClemente CC, Norcross JC. In search of the structure of change. In: Klar Y, Fisher J, Chinsky JM, Nadler, editors(s). Self Change. New York: Springer, 1992:87-114. [Google Scholar]
Review Manager 2020 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.4. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2020.
Rosenberg 2015
- Rosenberg DE, Bellettiere J, Gardiner PA, Villarreal VN, Crist K, Kerr J. Independent associations between sedentary behaviors and mental, cognitive, physical, and functional health among older adults in retirement communities. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 2016;71(1):78-83. [DOI: 10.1093/gerona/glv103] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ross 2020
- Ross R, Chaput JP, Giangregorio LM, Janssen I, Saunders TJ, Kho ME, et al. Canadian 24-hour movement guidelines for adults aged 18-64 years and adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Applied Physiology, Nutrition, and Metabolism 2020;45(10):S57-102. [DOI: 10.1139/apnm-2020-0467] [DOI] [PubMed] [Google Scholar]
Sansano 2019
- Sansano-Nadal O, Giné-Garriga M, Brach JS, Wert DM, Jerez-Roig J, Guerra-Balic M, et al. Exercise-based interventions to enhance long-term sustainability of physical activity in older adults: a systematic review and meta-analysis of randomized clinical trials. International Journal of Environmental Research and Public Health 2019;16(14):E2527. [DOI: 10.3390/ijerph16142527] [DOI] [PMC free article] [PubMed] [Google Scholar]
SBRN 2012
- Sedentary Behaviour Research Network. Standardized use of the terms "sedentary" and "sedentary behaviours" Letter to the Editor. Applied Physiology, Nutrition, and Metabolism 2012;37:540-2. [DOI] [PubMed] [Google Scholar]
Schünemann 2021
- Schünemann HJ, Higgins JPT, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook.
Schwarzer 2007
- Schwarzer R, Schüz B, Ziegelmann JP, Lippke S, Luszczynska A, Scholz U. Adoption and maintenance of four health behaviors: theory-guided longitudinal studies on dental flossing, seat belt use, dietary behavior, and physical activity. Annals of Behavioral Medicine 2007;33(2):156-66. [DOI: 10.1007/BF02879897] [DOI] [PubMed] [Google Scholar]
Shrestha 2014
- Shrestha N, Ijaz S, Kukkonen-Harjula KT, Kumar S, Nwankwo CP. Workplace interventions for reducing sitting at work. Cochrane Database of Systematic Reviews 2014, Issue 1. Art. No: CD010912. [DOI: 10.1002/14651858.CD010912] [DOI] [PubMed] [Google Scholar]
Shrestha 2019
- Shrestha G, Grgic J, Wiesner G, Parker A, Podnar H, Bennie JA, et al. Effectiveness of interventions for reducing nonoccupational sedentary behaviour in adults and older adults: a systematic review and meta-analysis. British Journal of Sports Medicine 2019;53:1206-13. [DOI: 10.1136/bjsports-2017-098270] [DOI] [PubMed] [Google Scholar]
Song 2015
- Song J, Lindquist LA, Chang RW, Semanik PA, Ehrlich-Jones LS, Lee J, et al. Sedentary behavior as a risk factor for physical frailty independent of moderate activity: results from the Osteoarthritis Initiative. American Journal of Public Health 2015;105(7):1439-45. [DOI: 10.2105/AJPH.2014.302540] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sparling 2015
- Sparling PB, Howard BJ, Dunstan DW, Owen N. Recommendations for physical activity in older adults. BMJ 2015;350:h100. [DOI: 10.1136/bmj.h100] [DOI] [PubMed] [Google Scholar]
Stamatakis 2019
- Stamatakis E, Ekelund U, Ding D, Hamer M, Bauman AE, Lee IM. Is the time right for quantitative public health guidelines on sitting? A narrative review of sedentary behaviour research paradigms and findings. British Journal of Sports Medicine 2019;53:377-82. [DOI: 10.1136/bjsports-2018-099131] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D. Chapter 10: Addressing reporting biases. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Stockwell 2019
- Stockwell S, Schofield P, Fisher A, Firth J, Jackson SE, Stubbs B, et al. Digital behavior change interventions to promote physical activity and/or reduce sedentary behavior in older adults: a systematic review and meta-analysis. Experimental Gerontology 2019;120:68-87. [DOI: 10.1016/j.exger.2019.02.020] [DOI] [PubMed] [Google Scholar]
Tandon 2012
- Tandon PS, Zhou C, Sallis JF, Cain KL, Frank LD, Saelens BE. Home environment relationships with children’s physical activity, sedentary time, and screen time by socioeconomic status. International Journal of Behavioral Nutrition and Physical Activity 2012;9(1):88. [DOI: 10.1186/1479-5868-9-8810.1186/1479-5868-9-88] [DOI] [PMC free article] [PubMed] [Google Scholar]
Teychenne 2010
- Teychenne M, Ball K, Salmon J. Sedentary behavior and depression among adults: a review. International Journal of Behavioral Medicine 2010;17(4):246-54. [DOI: 10.1007/s12529-010-9075-z] [DOI] [PubMed] [Google Scholar]
Yerrakalva 2019
- Yerrakalva D, Yerrakalva D, Hajna S, Griffin S. Effects of mobile health app interventions on sedentary time, physical activity, and fitness in older adults: systematic review and meta-analysis. Journal of Medical Internet Research 2019;21(11):e14343. [DOI: 10.2196/14343] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zubala 2017
- Zubala A, MacGillivray S, Frost H, Kroll T, Skelton DA, Gavine A, et al. Promotion of physical activity interventions for community dwelling older adults: a systematic review of reviews. PLOS ONE 2017;12(7):e0180902. [DOI: 10.1371/journal.pone.0180902] [DOI] [PMC free article] [PubMed] [Google Scholar]


