Abstract
South Asian countries have been struggling to control the COVID-19 pandemic despite imposing months of lockdown and other public health measures. This review aims to describe the epidemiological features and shortcomings in public health preparedness to tackle COVID-19 as well as derive lessons from these events in the context of Bangladesh. We have shown that an increase in human mobility was evident throughout the lockdown period. Over 20,000 frontline health workers were affected, and more than 2100 unofficial deaths possibly linked with COVID-19 diagnosis were reported. Males were disproportionately affected in terms of infection (71%) and death (77%) than females. Over 50% of infected cases were reported among young adults (20-40-year age group). After seven months into the pandemic, a downward trend in laboratory test positive percentage was seen, although the number of new deaths per day remained largely unchanged. We believe our findings, observations and recommendations will remain as a valuable resource to facilitate better public health practice and policy for managing current and future infectious disease like COVID-19 in resource-poor developing countries.
Keywords: COVID-19, Pandemic, Bangladesh, Dhaka, Epidemiology, SARS-CoV2
COVID-19, Pandemic, Bangladesh, Dhaka, Epidemiology, SARS-CoV2.
1. Introduction
The novel coronavirus disease 2019 (COVID-19) has triggered a public health emergency of international concern. Within a period of six months, the Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) has spread to more than 200 countries/territories, infected more than 30 million people worldwide, and claimed over 900,000 lives. The COVID-19 causes a plethora of clinical manifestations; the severity and outcomes of the disease may vary depending on the underlying comorbidities (diabetes, heart diseases, hypertension, COPD), age, sex, and geographic locations [1]. In South Asia, despite implementing various public health measures, the overall response to containing the viral spread remains questionable as there is no indication of the anticipated growth curve for the pandemic to flatten. As of 10 September 2020, over 5 million cases and 94,000 deaths have been reported in the South Asia, and hence created an alarming situation as one-third of the world's population (~1.7 billion) with similar socio-economic characteristics live in these densely populated and resource-limited regions. In this regard, Bangladesh could be an interesting setting to understand the characteristic of the COVID-19 pandemic from the South Asian perspective.
With a population of over 160 million, Bangladesh is one of the most densely populated (1265 per square km) countries in the world. About 60% of its population is between 15 to 64 years old and only 4.7% is above 65 years of age [2]. The care-home facility is virtually non-existent and the extended family structure combines the aged with the young in the same household. Because of economic growth, the country has undergone a rising trend of unplanned urbanization, and more than 32 per cent of people are currently living in urban areas. Bangladesh is also experiencing nutrition and epidemiologic transition with a higher burden of noncommunicable diseases (NCDs). A recent meta-analysis has shown that overall prevalence for metabolic syndrome (a cluster of health problems including high blood pressure, abdominal fat, high triglycerides, high blood sugar, and low HDL cholesterol) is higher in Bangladesh compared to the estimated world prevalence (30% versus 20–25%) [3]. Besides, approximately 34% of adults are overweight and NCDs account for 67% of deaths in Bangladesh [4, 5].
The capital of Bangladesh, the Dhaka city, has a population of nearly 20 million, and is currently the epicenter of COVID-19 infection in the country. The first three official COVID-19 cases were reported on March 8, 2020, which included two men returning from Italy. The first official death was confirmed on 18 March 2020 amidst the upsurges of unofficial deaths of people with COVID-19 like symptoms. With more than one million slum dwellers and marginal communities who live in close proximity, the capital Dhaka city remains at high risk since these people are deprived of adequate facilities for maintaining personal hygiene as bathroom/toilets and water reservoirs are shared between several families [6, 7].
Since adequate information on in-depth epidemiological features of the COVID-19 pandemic is lacking from the setting of developing countries, particularly from South Asia; in this context, we aimed to describe the gaps in public health preparedness, epidemiological characteristics including incidence, mortality, and geospatial distribution of the COVID-19 pandemic in Bangladesh. Moreover, comparative epidemiological trends were shown between Bangladesh and other countries with significant incidences of the disease.
2. Publicly available data used in this review article
2.1. Mobility data
Country-level mobility data for Bangladesh were obtained from Google COVID-19 Community Mobility Reports (www.google.com/covid19/mobility) based on the google maps/location usage from smartphones, over a period of 3 January 2020 to 19 September 2020. The data was normalized and the baseline was used as the median value of 5 weeks (3 January 2020 to 6 February 2020). Five different categories of mobility data were plotted: (i) mobility at grocery and pharmacy, (ii) mobility at parks, (iii) mobility at retail & recreation, (iv) mobility at transit stations and (v) mobility at workplaces. Mobility of grocery and pharmacy data was constructed on user-visits to grocery markets, drugstore, food warehouse, etc. In parks, mobility involves public gardens, national forests, castles, etc. Retail and recreation mobility include restaurants, cafes, shopping centers, theatres. At transit stations, mobility includes bus stations, airports, railway stations, public transport hubs, etc. Workplace mobility covers offices, factories, etc.
2.2. Incidence and mortality
Data were obtained from the Directorate General of Health Services (DGHS), the Government of Bangladesh [8]. Information on COVID-19 infected frontline professionals (medical doctor, health workers, police, and journalists) were extracted from the websites of Bangladesh Medical Association, major newspapers and online portals, professional societies and then verified with the government press releases whenever possible [9, 10, 11, 12, 13]. Data regarding disease severity and pre-existing comorbidity of the patients were obtained from COVID-19 TelehealthCenter Daily Report at https://corona.gov.bd/website. Unofficial death counts with COVID-like symptoms were collected from weekly bulletins published by Bangladesh Peace Observatory, Centre for Genocide Studies (CGS) at the University of Dhaka along with the official death counts [14].
2.3. Geospatial distribution of reported COVID-19 cases
District-wise case reports data was collected from the Institute of Epidemiology, Disease Control and Research (IEDCR), a sister organization of DGHS and COVID-19 Bangladesh situation reports by World Health Organization (WHO) [15, 16]. The population data were retrieved from the Bangladesh Population Census 2011 dataset. The spatial map was created using layers downloaded from the Bangladesh Geospatial Data Sharing Platform (GeoDASH) on ArcGIS Desktop (Esri Inc., Redlands, California, United States) [17]. District-wise data for active COVID-19 cases were plotted on a map.
2.4. Epidemiological trends
Descriptive statistics were used to report incidence, mortality, age, and gender-specific attributes. Data from the Johns Hopkins University Coronavirus Resource Centre was used to illustrate the current trend of Bangladesh compared to South Asian countries (India, Pakistan, and Nepal) and other countries with higher incidence (Saudi Arabia, Brazil, UK, USA, and Italy) [18].
3. Key events and epidemiological features of COVID-19 pandemic in Bangladesh based on analyzed data
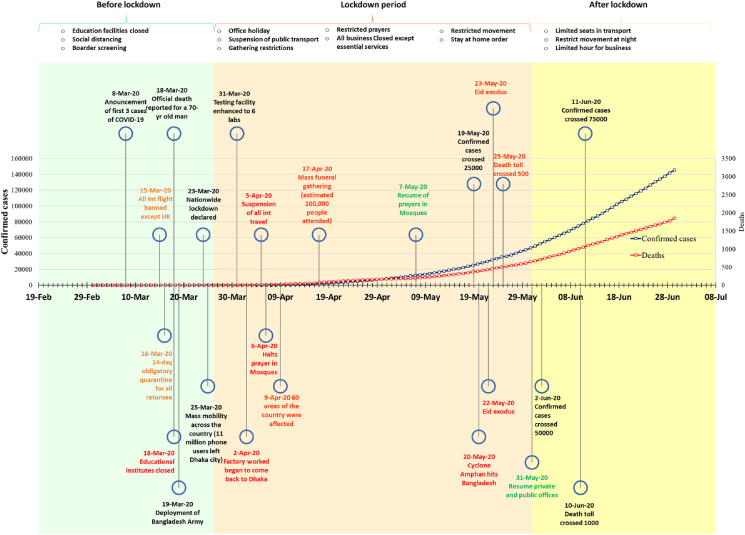
Following the detection of the first case on March 8, 2020, the government limited flights, closed educational institutions, and imposed mandatory health screening in the airport. A nation-wide lockdown was also in-effect from 23 March to 30 May 2020. During this period, all offices, public transportation, and large gatherings were shut, prayers in places of worship were suspended, and mandatory stay-at-home order was imposed. Figure 1 represents an overall timeline of COVID-19 related major events before and after lockdown in Bangladesh.
Figure 1.
Major events and public health measures in COVID-19 in Bangladesh before and after lockdown periods. Deaths over time are represented in the secondary axis.
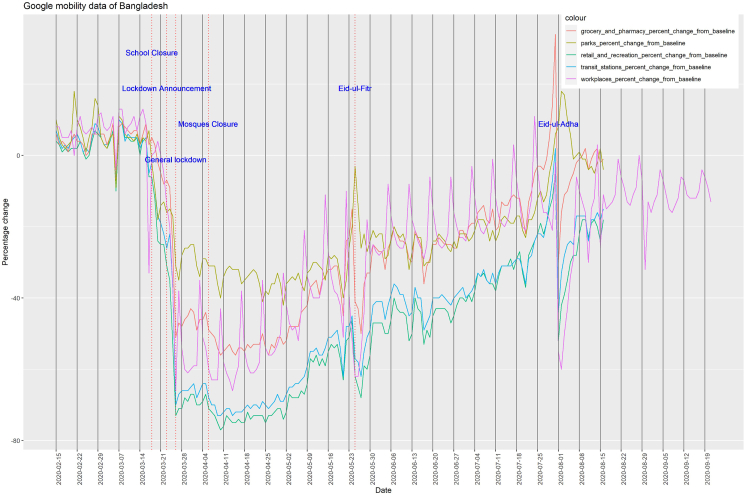
The human mobility during the COVID-19 pandemic was severely impacted as at the onset of non-pharmaceutical interventions, all five classes of mobility were close to zero (baseline) (Figure 2). There was a steady decrease of 67, 68, 56, 29, and 66 percentage in retail and recreation, transit station, grocery and pharmacy, parks and workplaces, respectively, from the introduction of first intervention measures to the implementation of general lockdown (Table 1). This state of reduced mobility was found to maintain until the first week of April. An increase in human mobility was also documented linked to public events such as the Eid festivals (the biggest Muslim festival). By early August 2020, all but one class of mobility showed a positive percentage increase from the baseline. This demonstrated a declining trend in the effectiveness of general lockdown over time.
Figure 2.
Human mobility in Bangladesh during COVID-19 pandemic (8 March 2020 to 19 September 2020). The baseline is the median value, for the corresponding day of the week, during the 5-week period Jan 3–Feb 6, 2020.
Table 1.
A summary of percentage change of human mobility from baseline using Google mobility data for Bangladesh.
| Date (event) | Retail and recreation |
Transit stations |
Grocery and pharmacy |
Parks |
Workplaces |
|---|---|---|---|---|---|
| percent change from baseline | |||||
| 08/3/20 (First case detected) | +9 | +9 | +9 | +10 | +13 |
| 18/3/2020 (School closure) | -6 | -2 | 5 | -2 | 0 |
| 23/3/2020 (Lockdown Announcement) | -31 | -26 | -7 | -16 | -14 |
| 26/3/2020 (General lockdown) | -73 | -70 | -51 | -31 | -66 |
| 6/4/2020 (Mosques Closure) | -71 | -68 | -49 | -31 | -60 |
| 25/5/2020 (Eid-ul-Fitr) | -62 | -57 | -41 | -3 | -62 |
| 1/8/2020 (Eid-ul-Adha) | -52 | -44 | -30 | 8 | -55 |
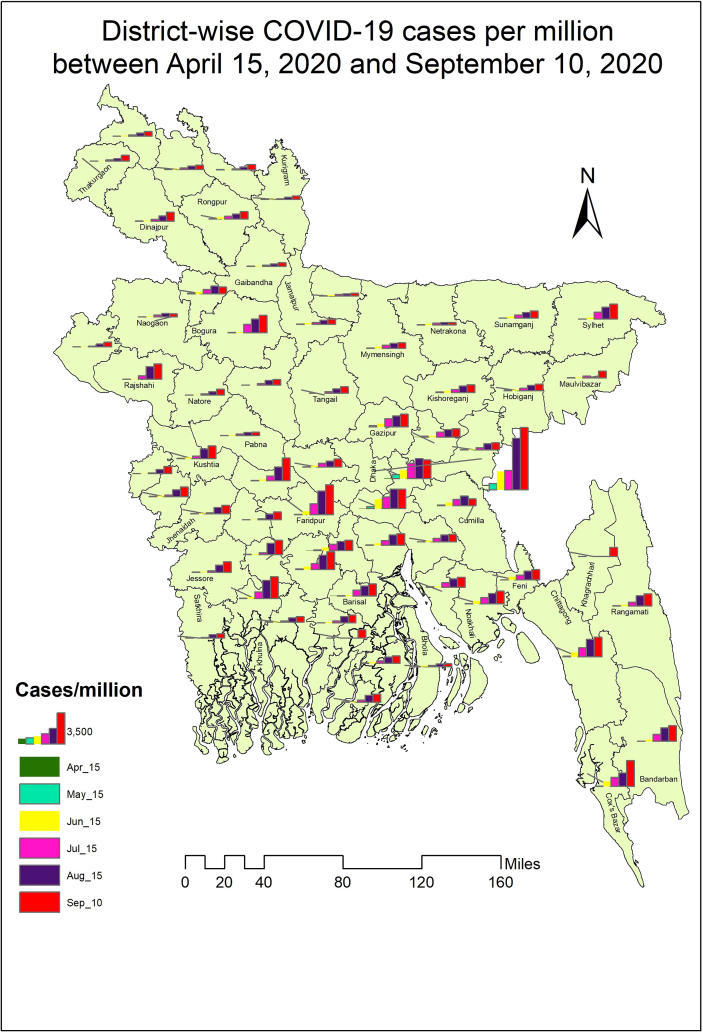
Geospatial distribution of reported COVID-19 cases showed that the infection rate was very low during mid-April as 27 districts out of 64 did not report any COVID-19 positive cases. Among others, none of the districts had more than a total of 30 cases except for Chittagong (n = 31), Gazipur (n = 53), Narayanganj (n = 214), and Dhaka (n = 546). The district-wise analysis of cases per million between April 15, 2020 to September 10, 2020 revealed that the number of positive cases in Dhaka, Munshiganj, Cox's Bazar, Narayanganj, and Chittagong rose rapidly in June (Figure 3). As lockdown ended, the infection rate increased from 275 cases per million on June 07 to 521 cases per million on June 30 – nearly a 90% increase over three weeks. Interestingly, the incidence rate in Dhaka had a 13% reduction as the number of cases decreased from 1735 to 1507 cases per million. This could suggest that, following the cessation of lockdown measures, the disease was spreading out from the epicenter Dhaka towards the peripheral districts. The rapid spread of the disease was observed in Tangail (from 15 cases per million to 168 cases) and Khulna (from 66 cases to 742 cases per million). By September 2020, the districts at the peripheral parts of Bangladesh have seen a sharp increase in the number of COVID-19 positive cases. The Bandarban district had only 12 cases per million in May, whereas the number escalated to 1752 cases per million population in September. So far, the Dhaka division has the highest number of COVID-19 cases of which nearly 70% were in the capital Dhaka city. The rest of the divisions in order of a total of case numbers include Chittagong, Khulna, Rajshahi, Sylhet, Rangpur, Barishal, and Mymensingh.
Figure 3.
District-wise geospatial distribution of COVID-19 cases per million between April 15, 2020 and September 10, 2020 in Bangladesh.
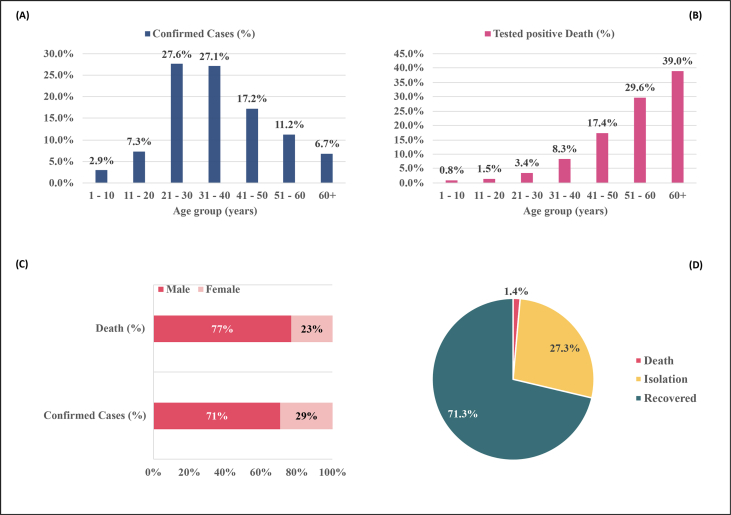
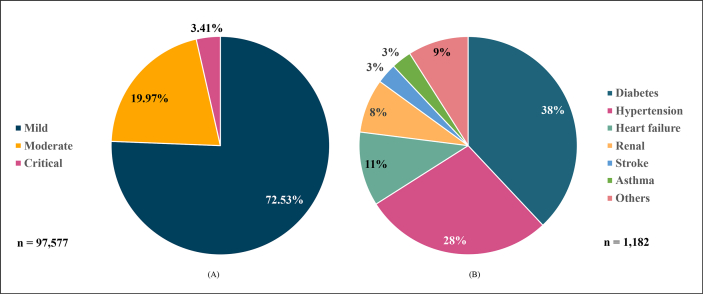
More than 50% of patients infected with SARS-CoV-2 were aged between 21 and 40 years (Figure 4A). Children and elderly people belonged to the least infected group. Deaths due to COVID-19 in Bangladesh increased with the age of patients (Figure 4B). Males were infected (71%) and died (77%) in a higher proportion than females (Figure 4C), and the overall case fatality rate (CFR) in Bangladesh was estimated to be 1.4% (Figure 4D). The proportion of deaths in male patients was higher than females (1.52% vs 1.11%). Most of the patients had mild to moderate complications as compared to only 3.41% of patients requiring critical care (Figure 5A). Among the patients who died, the most common pre-existing comorbidity was diabetes (38%) followed by hypertension (28%) and heart failure (11%) (Figure 5B).
Figure 4.
Demography of reported COVID-19 cases and deaths in Bangladesh (8 March 2020–9 September 2020). (A) Age group specific cases, (B) Age group specific deaths, (C) Sex specific cases and deaths, (D) Percentage of recovered, isolation and deaths.
Figure 5.
Proportion of COVID-19 patients' analysis by- (A) Disease Severity, and (B) Deceased Patients by Co-Morbidity Status based on the COVID-19 TelehealthCenter Daily Report.
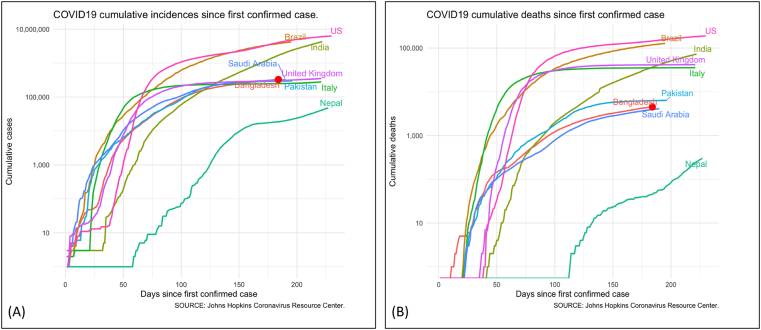
The incidence and mortality of COVID-19 in Bangladesh were compared with some South Asian and other countries. In Figure 6A, Bangladesh had a similar trend of incidence during the initial phase of the pandemic (first 30 days or so). After that, the incidence in Bangladesh and other South Asian countries slowed down compared to Brazil, the USA, and European countries. As for mortality, the South Asian countries had significantly fewer reported deaths over time compared to the other countries in the EU and the USA (Figure 6B). Interestingly, both incidence and deaths in Nepal started to pick up after more than one and a half months since the first confirmed case. The testing capability was minimal in Bangladesh in the first month of the outbreak (March 2020) and was increased to 99 laboratories nationwide. As of September 2020, the overall testing rate of Bangladesh was only 10,560 tests per 1 million people, whereas other south Asian countries such as India, Nepal, and Pakistan, conducted 39,915 tests, 28,086 tests and 13,117 tests per 1 million people, respectively.
Figure 6.
Progression COVID-19 pandemic in South Asia and other countries. A) Trends of COVID-19 cumulative incidences B) Trends of cumulative deaths.
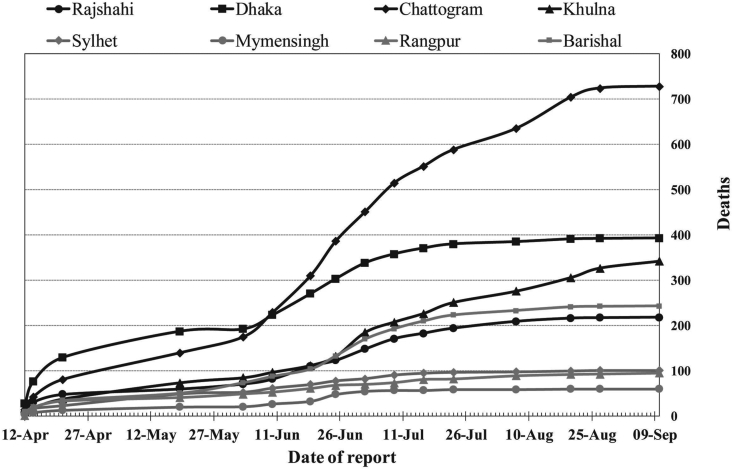
Over 20,000 frontline health workers (5483), law enforcement officers, and journalists were infected (Table 2). A high CFR (3.16%) was recorded for frontline physicians. A total of 2100 unofficial deaths with COVID-19 like symptoms were also reported (Figure 7). In the first three weeks of April, the unofficial death of COVID-19 suspects increased rapidly in the Dhaka division while the number of deaths increased alarmingly in Chittagong in post-lockdown period. The trend of an increase in the number of deaths was slow in other division including Barishal, Rangpur, Mymensingh, Sylhet, Khulna, and Rajshahi as compared to Dhaka and Chittagong.
Table 2.
Infections and deaths among frontline COVID-19 fighters (Police, health workers, Army, Journalists).
| Frontliners | Infected (n) | Death n (%) |
|---|---|---|
| Physicians | 2753 | 87 (3.16%) |
| Nurse | 1949 | NA |
| Medical Staff | 3243 | NA |
| Police | 11302 | 44 (0.38%) |
| Army∗∗ | 3477 | NA |
| Journalists | 378 | 06 (1.58%) |
Both in service and retired
Figure 7.
Trends of unofficial deaths with COVID-19 like symptoms in different divisions across Bangladesh.
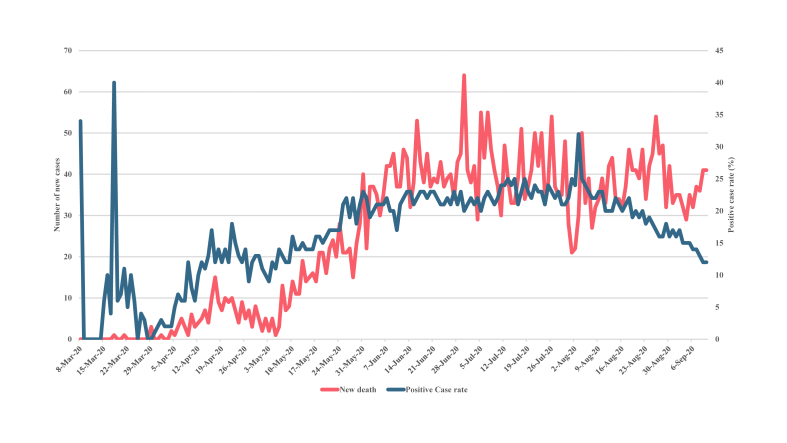
After six months into the pandemic, Bangladesh witnessed a drop in case rates below 15% which was as high as 40% in March. Based on the test positive case-rate data, a steady increase was observed throughout March to July and a probable peak of infection occurred in late July 2020. However, the number of new deaths per day due to COVID-19 has not declined, rather the numbers have increased over time to some extent (Figure 8). While the case-rate indicates a downward trend, the death rate has remained largely unchanged since the first week of June. Notably, the number of total RT-PCT tests performed has also decreased. On April 15, the number of RT-PCR test was 1740, and by June 26, the numbers increased to 18,498; however, the test numbers were reduced to 10,723 by September 12.
Figure 8.
Trends of the number of daily new deaths and the percentage (%) of test positive rate.
4. Discussion
The COVID-19 pandemic has appeared as a daunting disaster for Bangladesh. With constrained resources and a gigantic population, the experience of Bangladesh illustrated some of the common challenges faced by the developing countries concerning the public health response to an infectious disease such as COVID-19.
4.1. Ineffective public health crisis communication and countermeasures
After the official announcement of COVID-19 cases in Dhaka, the Government took a number of initiatives to revamp the testing facility, medical equipment supply, and nationwide surveillance. However, the public health countermeasures were not up to the mark to flatten the curve as the country was witnessing a steep rise in the number of confirmed cases. The human mobility data also confirmed the gradual increase in mobility during the lockdown periods. A series of events such as the mobilization of 11 million mobile users from city to rural areas, local violence, massive gathering for Janaza prayer (funeral), and purposive rule-breaking indicated that people, by and large, failed to take into account the importance of maintaining social distancing. While strict lockdown policy has shown some success in China, New Zealand, Italy, and largely in the developed countries, a similar approach did not achieve the desired outcome in Bangladesh, for which the possible underlying socioeconomic and demographic factors were at fault, for instance, poverty, low wages, and comparatively younger population. At the beginning of April during the lockdown period, Bangladesh had only 54 cases, but it increased to about 50,000 cases by the end of May as the lockdown ended. A similar trend was also observed in India and Pakistan where the early lockdown measures might have helped in the preparation of medical logistics but ultimately failed to contain the viral spread.
One recent study in Bangladesh has shown that people were confused about the English language terms such as “stay at home,” “social distancing,” “quarantine,” and “lockdown” [19]. The upward trajectory of positive cases despite an extended period of nationwide lockdown and restrictions indicated the inefficiency of public health risk communication. The gap in the public health preparedness in battling COVID-19 could be minimized by considering the nuances of geographical & cultural contexts and devising specific strategies. Significant investment and support are required to generate sufficient data for improving the efficiency of public health decisions.
4.2. Gender disparity and spatial distribution of infection
In Bangladesh, men were disproportionately affected with COVID-19 in higher number than women, although studies around the world suggested that both men and women were equally susceptible to the virus [15, 20]. A similar observation was noted in India and Pakistan where men comprised about 65% and 70% of confirmed cases, respectively [21, 22]. Also, the percentage of susceptibility might vary since COVID-19 is more fatal for men, causing them to seek medical care and subject to testing [23]. Thus, the health seeking behaviour and the health access issues among men and women might play a critical role. Interestingly, men were also found to be affected more by dengue, typhoid, and malaria in Bangladesh [24, 25, 26]. This disparity in susceptibility could be explained in light of the cultural aspects since men dominate the outdoor activities and are less careful towards keeping up with personal hygiene [27]. The death rate among males was found higher in Bangladesh. Studies showed that men over 60 years of age were twice as likely to die of COVID-19 than women [23, 28]. This could partly be explained by the presence of higher comorbidity and the smoking habit in men, although the exact reason remains to be elucidated [29].
In Bangladesh, the existing data suggested that the infection rate in people from urban areas was higher than in rural villages. This is unsurprising because urban settings offer a higher chance of catching the virus. For instance, the Dhaka or Chittagong city relies heavily on congested infrastructures where the population density is the highest, and the citizens receive reduced sunlight exposure. Vitamin D deficiency in city areas is well documented, and some early studies indicated that vitamin D deficiency could be a risk factor for COVID-19 adversity [30, 31]. However, the rural remote regions of the country suffer from a lack of proper medical support. The unavailability of the testing facilities in the rural regions could be a reason for low infection rate. Out of 64 districts, almost half of the districts have over 100,000 people who are aged above 65 years, and data show that the proportion of the elderly is higher in rural areas [32, 33]. As hospital facilities and medical assistance are more centered towards urban residents, about 3 million people from 50 tribal and ethnic minor communities living in remote areas in Bangladesh remain vulnerable to COVID-19 [32]. In Brazil, around 9.1% of indigenous people infected with the disease died, and the rate of infection was soaring in distant communities [34].
4.3. Low fatality rate as compared to other countries
Interestingly, despite the official numbers jumping above 339,332 (as of 15 September 2020) cases, the death rate remained fairly low (1.4%) in Bangladesh and close to the other South Asian countries such as India (1.64%), and Pakistan (2.11%). The lower mortality rate in the developing countries may be due to the fact that the overall life expectancy is within 64–72 years, leaving out the overly elder population; and there is a higher proportion of young populations in Pakistan, India, and Bangladesh. By comparison, the proportion of people aged over 70 years is much higher in the western settings [35].
Speculations regarding the low death rate in developing countries questioned the under-reporting of actual death cases as testing facilities were very limited. The unofficial sources indicated that a slightly higher number of deaths (n = 2100) occurred in Bangladesh during the initial phase of the outbreak. The combined overall mortality rate, however, remained surprisingly lower than what has been observed in the western world. The western countries offer care home facilities that are practically non-existent in South Asian culture where the extended family structure incorporates the elderly with the young in the same household. As opposed, the rapid spread of the infection among the elderly in care homes contributed to half of the total deaths in the western world. In France, the deaths linked to care homes were 51%, and in Canada, as many as 82% of COVID-19 deaths occurred among care home residents [36].
4.4. Slow progression of COVID-19 pandemic
Despite higher population density and low awareness of personal hygiene, Bangladesh has witnessed a rather noticeable slow progression. Moreover, Pakistan's curve has flattened, India continued to see a sharp increase in the number of new infections. It is speculative that COVID-19 was already circulating in this region since South Asian countries are closer to and have strong economic relations with China. Of note, the first COVID-19 positive case was identified on January 30 in India, February 26 in Pakistan, and March 8 in Bangladesh. Despite such early detection, the subsequent numbers of infection and mortality continued to rise slowly. One study reported that community level transmission had occurred in Bangladesh in March 2020, and only four districts had high-risk clusters before May. In the Dhaka city, the space-time clusters of COVID-19 exhibited lower risk in the early phase, presumably due to lockdown effects, whereas the clusters emerging between 30 May to 15 June showed a relative higher risk of spread [37]. Our mobility data also highlighted the similar pattern of high human mobility during these periods. Interestingly, despite the violation of social distancing, the cumulative cases increased at a slower pace when compared to other countries. Several factors might influence the disease progression such as the wide-scale adaptation of facemask, tropical climate, or cross-immunity from other viruses as the region is under the high burden of disease [38, 39]. The lack of quality testing facility, however, might also be a crucial factor to determine the actual infection rate. Further studies are needed to investigate the factors contributing to apparent slow progression of COVID-19 in the South Asian countries.
One probable reason for slow progression was that unlike China that locked down Wuhan city, the South Asian countries including Bangladesh went for a nationwide total lockdown and imposed mandatory face-mask at public places which might have slowed down the disease progression. As the countries eased down on lockdown measures, the numbers began to soar up. In Bangladesh, a dramatic shift in the percent-change of disease transmission was observed as the post-lockdown COVID-19 infection was dispersing quickly from the cities towards the peripheral districts. This underpins the fact that relaxing social distancing measures might bring about similar infection rates for developing countries.
4.5. Overburden of healthcare system
A significant number of medical personnel and law enforcement workers were infected during the first wave of the COVID-19 epidemic. In particular, the fatality rate among the doctors in Bangladesh was 3.16% as opposed to the reported data for the healthcare workers in Pakistan (1.01%), India (3.30%) and Afghanistan (3.75%) [40]. The higher proportion of frontliners contracting the virus implied the lack of personal safety and inconsistency in management. The quality of personal protective equipment (PPE) and its training of proper handling remained in doubt. Moreover, hospitals suffered from the scarcity of intensive care units. With only 733 intensive care unit (ICU) beds in government hospitals, the healthcare has crumbled as the COVID-19 infection rate continued to increase in torrent [41]. It is surmised that the number of deaths in the age range of 60–70 could be subverted if proper ICU and medical support were provided. This underscores the need for urgent investment and remodeling of the healthcare sector.
Undoubtedly, the biggest problem with social distancing in Bangladesh lies in the population density and city-based centralized facilities. Besides, the healthcare system is also largely centralized in metropolitan settings especially the capital Dhaka and divisional cities. The disaster of the COVID-19 pandemic thus points out the fragility of the existing system and urges to prioritize the decentralization of healthcare facilities. There is a greater need to ensure the minimization of the urban-rural disparity in the healthcare facilities. The establishment of universal health care should also be directed as a long-term goal.
4.6. Limited testing facility
The abrupt onset of critical patients at the hospitals has strained medical resources; and expensive PCR (polymerase chain reaction) based testing facilities and related workforce remained in pestilence to meet the demand. As of September 2020, the RT-PCR test based positive case-rate has started to decline while the number of new deaths per day has remained largely unchanged, which could indicate that the positive case rate was subject to the number of RT-PCR test performed. Since the laboratory test numbers have decreased, the incidence rate and the case rate may not be representative of the current situation of the COVID-19 pandemic. With regard to laboratory tests per million of population, India (161,413), Sri Lanka (103,639), Nepal (74,703), Pakistan (41,818) have performed more tests than Bangladesh (25,425) [42]. Interestingly, Vietnam has performed 26,534 test per 1 million of population and recorded 1060 cases in total and 35 deaths. It indicated that proper contact tracing and quarantining were equally important than simply performing massive tests.
Since public health measures in the developing countries are constrained by resources both in terms of financial support and trained workforce, it is essential to devise a strategy that is most suitable for such settings. It is recommended that instead of depending on RT-PCR based tests that are costly and time-consuming, the low-middle income countries could focus on syndromic diagnosis based on the constellation of symptoms and signs of COVID-19 in a disease afflicted area [43]. This way, the burden of expensive testing could be largely reduced, the suspected patients identified earlier, and the investment channeled out into rebuilding healthcare facilities. Moreover, patients who were denied hospital admittance because of the absence of a COVID-19 test report will also receive early medical support. While the pandemic situation will not be under control very soon, the COVID-19 testing laboratories should be turned into regional surveillance centers instead of dissolving them by the time COVID-19 ends. Because only a national framework of proactive monitoring can assist in prompt action in the event of future outbreaks.
5. Conclusion
We found that despite imposing several public health measures to ‘flatten the curve’, the outbreak continued to spread steadily across Bangladesh. Large scale public gatherings and festivals increased the overall human mobility during the lockdown period. Males were disproportionately tested COVID-19 positive and died at a higher percentage. The mortality rates were relatively higher among frontline medical workers and law enforcement officials. The lack of medical support for patient care in hospitals and COVID-19 testing facilities remains a challenge to overcome. The overall death rate has also remained relatively unchanged after seven months of the pandemic. Our findings thus recommend continuing to limit public gatherings, increase medical support, revamp testing facilities as well as opt for syndrome-based diagnosis for patient admittance in hospitals. The conversion of COVID-19 testing centers into the regional surveillance hubs will also safeguard against future pandemics.
Declarations
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
The authors would like to thank Mahbubul H. Siddiquee for his thoughtful suggestion during the manuscript preparation.
References
- 1.Assessing Risk Factors for Severe COVID-19 Illness | CDC. 2020. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/assessing-risk-factors.html [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 2.National Report Volume-04: Socio Economic and Demographic Report. 2011. http://www.bbs.gov.bd/site/page/47856ad0-7e1c-4aab-bd78-892733bc06eb/Population-&-Housing [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 3.Chowdhury M.Z.I., Anik A.M., Farhana Z., Bristi P.D., Abu Al Mamun B.M., Uddin M.J. Prevalence of metabolic syndrome in Bangladesh: a systematic review and meta-analysis of the studies. BMC Publ. Health. 2018 Mar 2;18(1):308. doi: 10.1186/s12889-018-5209-z. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-018-5209-z [Internet] [cited 2020 Jul 14]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization - Noncommunicable Diseases (NCD) Country Profiles | Bangladesh. 2018. https://www.who.int/nmh/countries/bgd_en.pdf?ua=1 [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 5.Mitra D.K., Mistry S.K., Afsana K., Rahman M. Demographic, socio-economic and lifestyle determinants of under- and over-nutrition among Bangladeshi adult population: results from a large cross-sectional study. J. Epidemiol. Glob. Health. 2018;8(3–4):134–142. doi: 10.2991/j.jegh.2018.03.002. https://pubmed.ncbi.nlm.nih.gov/30864754/ [Internet] [cited 2020 Jul 14]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anwar S., Nasrullah M., Hosen M.J. COVID-19 and Bangladesh: challenges and how to address them. Front. Public. Heal. 2020 Apr 30;8:154. doi: 10.3389/fpubh.2020.00154. https://www.frontiersin.org/article/10.3389/fpubh.2020.00154/full [Internet] [cited 2020 Jul 14];Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed N., Jahangir Rony R., Tuz Zaman K. Social distancing challenges for marginal communities during COVID-19 pandemic in Bangladesh. J. Biomed Anal. 2020 May 21;3(2):5–14. www.jBiomedAnalytics.org [Internet] [cited 2020 Jul 14];Available from: [Google Scholar]
- 8.Coronavirus Disease 2019 (COVID-19) Information Bangladesh | corona.gov.Bd. 2020. https://corona.gov.bd/ [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 9.BMA | District Wise Total Number of Affected Doctor. Nurse & Staff (COVID-19); 2020. https://bma.org.bd/covid-19/Total Affected Doctor, Nurse & Staff.pdf [Internet] [cited 2020 Jul 12]. Available from: [Google Scholar]
- 10.BMA | List of Death Doctors Due to COVID-19. 2020. https://bma.org.bd/covid-19/List of Death Doctors Due to COVID-19_Detail.pdf [Internet] [cited 2020 Jul 12]. Available from: [Google Scholar]
- 11.The Number of Police Personnel Affected by Corona Exceeded 11,000 | Ittefaq. 2020. [Internet] [cited 2020 Jul 14]. Available from: https://www.ittefaq.com.bd/capital/163701/করোনায়-আক্রান্ত-পুলিশ-সদস্%E0. [Google Scholar]
- 12.Covid-19: 3,477 from Armed Forces Infected So Far in Bangladesh | Dhaka Tribune. 2020. https://www.dhakatribune.com/health/coronavirus/2020/06/13/covid-19-3-477-from-armed-forces-infected-so-far-in-bangladesh [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 13.378 media Workers of 99 Organizations Affected by Corona. 2020. https://www.jagonews24.com/mass-media/news/591082 [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 14.Bangladesh Peace Observatory | COVID-19 Graphics. 2020. http://www.peaceobservatory-cgs.org/#/highlights [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 15.IEDCR | Bangladesh Covid-19 Update. 2020. https://iedcr.gov.bd/ [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 16.Coronavirus Disease (COVID-2019) Bangladesh Situation Reports. 2020. https://www.who.int/bangladesh/emergencies/coronavirus-disease-(covid-19)-update/coronavirus-disease-(covid-2019)-bangladesh-situation-reports [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 17.GeoDASH. 2020. https://geodash.gov.bd/ [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 18.GitHub - CSSEGISandData/COVID-19: Novel Coronavirus (COVID-19) Cases, provided by JHU CSSE. 2020. https://github.com/CSSEGISandData/COVID-19 [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 19.Crisis of Communication during COVID-19: A Rapid Research - Brac Institute of Governance and Development. 2020. https://bigd.bracu.ac.bd/study/crisis-of-communication-during-covid-19-a-rapid-research/ [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 20.COVID-19 Sex-Disaggregated Data Tracker – Global Health 50/50. 2020. https://globalhealth5050.org/covid19/sex-disaggregated-data-tracker/ [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 21.Joe W., Kumar A., Rajpal S., Mishra U.S., Subramanian S.V. Equal risk, unequal burden? Gender differentials in COVID-19 mortality in India. J Glob Heal Sci. 2020 May 14;2(1) [Internet] [cited 2020 Jul 14]; Available from: [Google Scholar]
- 22.COVID-19 Health Advisory Platform by Ministry of National Health Services Regulations and Coordination | Pakistan. 2020. http://covid.gov.pk/ [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 23.Sex, Gender and COVID-19 - Coronavirus: the Science Explained - UKRI. 2020. https://coronavirusexplained.ukri.org/en/article/cad0007/ [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 24.Salje H., Paul K.K., Paul R., Rodriguez-Barraquer I., Rahman Z., Alam M.S. Nationally-representative serostudy of dengue in Bangladesh allows generalizable disease burden estimates. Elife. 2019;8 doi: 10.7554/eLife.42869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sattar A.A., Chowdhury M.S.J.H., Yusuf M.A., Jesmin S., Ara S., Islam M.B. Age and gender difference of typhoid fever among paediatric patients attended at a tertiary care hospital in Bangladesh. Bangladesh J Infect. Dis. 2017 Aug 31;3(2):36–39. http://www.banglajol.info/index.php/BJID/index [Internet] [cited 2020 Dec 20]. Available from: [Google Scholar]
- 26.Haque U., Overgaard H.J., Clements A.C.A., Norris D.E., Islam N., Karim J. Malaria burden and control in Bangladesh and prospects for elimination: an epidemiological and economic assessment. Lancet Glob. Heal. 2014 Feb 1;2(2):e98–e105. doi: 10.1016/S2214-109X(13)70176-1. www.thelancet.com/lancetgh [Internet] [cited 2020 Dec 20]; Available from: [DOI] [PubMed] [Google Scholar]
- 27.Muurlink O.T., Taylor-Robinson A.W. COVID-19: cultural predictors of gender differences in global prevalence patterns. Front. Public Heal. 2020 Apr 30;8:174. doi: 10.3389/fpubh.2020.00174. https://www.frontiersin.org/article/10.3389/fpubh.2020.00174/full [Internet] [cited 2020 Dec 20]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guan W.J., Liang W.H., Zhao Y., Liang H.R., Chen Z.S., Li Y.M. Comorbidity and its impact on 1,590 patients with Covid-19 in China: a nationwide analysis. Eur. Respir. J. 2020 May 1;55(5) doi: 10.1183/13993003.00547-2020. [Internet] [cited 2020 Jul 14]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vardavas C.I., Nikitara K. COVID-19 and smoking: a systematic review of the evidence. Tob. Induc. Dis. 2020 Mar 20;18(March) doi: 10.18332/tid/119324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ning Z., Song S., Miao L., Zhang P., Wang X., Liu J. High prevalence of vitamin D deficiency in urban health checkup population. Clin. Nutr. 2016 Aug 1;35(4):859–863. doi: 10.1016/j.clnu.2015.05.019. https://pubmed.ncbi.nlm.nih.gov/26093537/ [Internet] [cited 2020 Jul 14]; Available from: [DOI] [PubMed] [Google Scholar]
- 31.Mitchell F. Vitamin-D and COVID-19: do deficient risk a poorer outcome? Lancet Diabetes Endocrinol. 2020 Jul 1;8(7):570. doi: 10.1016/S2213-8587(20)30183-2. www.thelancet.com/diabetes-endocrinology [Internet] [cited 2020 Jul 14]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Needs Assessment Working Group Bangladesh | ReliefWeb. COVID-19: Bangladesh Multi-Sectoral Anticipatory Impact and Needs Analysis. 2020 Apr. https://reliefweb.int/sites/reliefweb.int/files/resources/COVID_NAWG Anticipatory Impacts and Needs Analysis.pdf?fbclid=IwAR1J73_wT0Ycfhh8tKUuwZJCgf884_MpcnuNqXrC75y46IXzcnNJVQ0Q7vU [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 33.Bangladesh Bureau of Statistics . 2015. Elderly Population in Bangladesh: Current Features and Future Perspective — Population Monograph.http://203.112.218.65/WebTestApplication/userfiles/Image/PopMonographs/Volume-12_UM.pdf [Internet] Available from: [Google Scholar]
- 34.Disaster Looms for Indigenous Communities as COVID-19 Cases Multiply in Amazon. National Geographic; 2020. https://www.nationalgeographic.com/history/2020/06/disaster-looms-indigenous-amazon-tribes-covid-19-cases-multiply/ [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 35.Life Expectancy by Country and in the World (2020) - Worldometer. 2020. https://www.worldometers.info/demographics/life-expectancy/ [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 36.Number of Deaths of Care home Residents and the COVID-19 Pandemic: Growing International Evidence | International Long-Term Care Policy Network. 2020. https://ltccovid.org/2020/05/22/number-of-deaths-of-care-home-residents-and-the-covid-19-pandemic-growing-international-evidence/ [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 37.Masrur A., Yu M., Luo W., Dewan A. Space-time patterns, change, and propagation of COVID-19 risk relative to the intervention scenarios in Bangladesh. Int. J. Environ. Res. Publ. Health. 2020 Aug 14;17(16):5911. doi: 10.3390/ijerph17165911. https://www.mdpi.com/1660-4601/17/16/5911 [Internet] [cited 2020 Dec 22]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Javid B., Weekes M.P., Matheson N.J. Covid-19: should the public wear face masks? BMJ. 2020 Apr 9:369. doi: 10.1136/bmj.m1442. https://www.bmj.com/sites/default/files/attachments/resources/ [Internet] [cited 2020 Jul 14]. Available from: [DOI] [PubMed] [Google Scholar]
- 39.Sette A., Crotty S. Pre-existing immunity to SARS-CoV-2: the knowns and unknowns. Nat. Rev. Immunol. 2020 Jul 7:1–2. doi: 10.1038/s41577-020-0389-z. http://www.ncbi.nlm.nih.gov/pubmed/32636479 [Internet] [cited 2020 Jul 14]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Doctors Hold Highest Mortality Rate from Covid-19 | the Business Standard. 2020. https://tbsnews.net/coronavirus-chronicle/covid-19-bangladesh/doctors-hold-highest-mortality-rate-covid-19-92857?fbclid=IwAR281wVf23WLBhzUnS_CMEJppzKSzlK4qfd6BKDvUN99-SLmGARRW-kxjZY [Internet] [cited 2020 Jun 14]. Available from: [Google Scholar]
- 41.733 ICU Beds in Govt Hospitals in Bangladesh. 2020. https://www.newagebd.net/article/108076/733-icu-beds-in-govt-hospitals-in-bangladesh [Internet] [cited 2020 Jul 14]. Available from: [Google Scholar]
- 42.Coronavirus Update (Live): 118,923,047 Cases and 2,636,612 Deaths from COVID-19 Virus Pandemic - Worldometer. 2021. https://www.worldometers.info/coronavirus/ [Internet] [cited 2021 Mar 12]. Available from: [Google Scholar]
- 43.Cash R., Patel V. Has COVID-19 subverted global health? Lancet. 2020 May 30;395(10238):1687–1688. doi: 10.1016/S0140-6736(20)31089-8. https://www [Internet] [cited 2020 Jul 14]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.