Abstract
COVID-19 is the most severe pandemic globally since the 1918 influenza pandemic. Effectively responding to this once-in-a-century global pandemic is a worldwide challenge that the international community needs to jointly face and solve. This study reviews and discusses the key measures taken by major countries in 2020 to fight against COVID-19, such as lockdowns, social distancing, wearing masks, hand hygiene, using Fangcang shelter hospitals, large-scale nucleic acid testing, close-contacts tracking, and pandemic information monitoring, as well as their prevention and control effects. We hope it can help improve the efficiency and effectiveness of pandemic prevention and control in future.
Keywords: COVID-19, Control strategies, Effect comparison
1. Introduction
COVID-19, the most severe infectious pandemic globally in the past century, has not only caused significant loss of life and health worldwide, but also created a general and systematic impact on the economic development and social stability of almost all countries. It also has a great and far-reaching influence on the global development pattern and the governance of security. Practice shows that the comprehensive use of multiple prevention and control measures from the perspectives of three principles, i.e., controlling the infection sources, cutting off infection routes, and protecting susceptible groups, can effectively postpone and control the spread of infectious diseases. Universal online access and social media makes information about the pandemic more transparent and promptly available, greatly facilitating the public’s full participation in the response to the pandemic, and thus playing an important role in prevention and control.
However, due to differences in economic, social cultural, climatic and other conditions, countries adopt varied prevention and control strategies against COVID-19, resulting in wide regional variations in the spread, duration, and intensity of COVID-19. East Asian countries, represented by China, that first reported the pandemic outbreak, have taken active and strict prevention and control measures, and have quickly and effectively controlled domestic virus spread, leaving only sporadic cases or low-intensity re-occurrence. After a period of strict control, the pandemic in European countries such as Italy, Spain, and Germany, which was severe in the early stages, had entered a stable/declining period. However, after gradual relaxation of social restrictions because of economic recovery targets and public resistance, the pandemic has inevitably rebounded. A severe pandemic situation exists in some countries and regions such as the United States and Brazil, South Asia dominated by India, as well as some European countries due to their generally loose prevention and control measures1. The COVID-19 pandemic in India, which has a poor economic base and poor sanitary conditions, has been seriously out of control since April 20212.
The COVID-19 pandemic, with a worldwide spread, has killed over 3 million people until May 2021. With large-scale vaccination, many countries have achieved remarkable results in fighting the pandemic after more than a year of hard work. However, consolidating the anti-pandemic achievements has become a worldwide challenge. Because of emerging variants of the novel coronavirus and the differences in national realities and anti-pandemic strategies, there are still many countries on the verge of or in the state of an uncontrollable large-scale outbreak. Before a vaccine is widely used to form an immune barrier, it is difficult to bring the global pandemic situation under control.
2. Main prevention and control measures by representative countries
2.1. Remarkable effects of lockdown or social distancing
Lockdown and social distancing are measures adopted by many countries in the early stage. Unique national realities and pandemic situations in each country make it difficult to strictly distinguish between lockdown and social distancing during the implementation process. For the convenience of analysis, the following content will distinguish them slightly based on the priority of the measures of lockdown or social distancing.
2.1.1. Lockdown and its effect
Lockdown is a major measure for countries to fight against the novel coronavirus in the early stage. The unique national realities and pandemic intensity in each country lead to the differences in timing and degree of lockdown, as well as different effects.
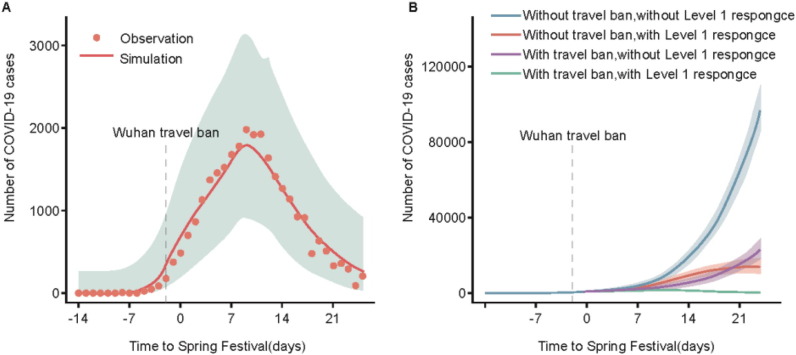
On December 31, 2019, the respiratory disease due to novel coronavirus was first detected in Wuhan, Hubei province, China. On January 23, 2020, Wuhan implemented a strict citywide lockdown to prevent the spread of COVID-19 pandemic from Wuhan to other regions. Subsequently, a nationwide Level-1 response was initiated, and travel restrictions were imposed in the Hubei province and all the other provinces in the mainland. However, 4.3 million people had already left Wuhan before travel bans had been enforced. Consequently, 262 cities reported cases in the following 28 days. The timing of the COVID-19 outbreak was closely related to the urban population and travelers from Wuhan. It was fortunate that Wuhan’s travel ban postponed the outbreak of COVID-19 in other cities by an average of 2.91 days. More than 130 cities in China, covering over half of China’s geographical area and population, have benefited from the implementation of the lockdown and suffered a delayed pandemic. Studies have shown that only the comprehensive use of multiple measures such as lockdown, urban traffic ban, and Level-1 response can effectively reverse the rising trend of cases3(Fig. 1).
Fig. 1.
Effect of interventions on control of the COVID-19 outbreak in China.3 (Reproduced with permission from reference 3).
America did not enforce a lockdown, but took measures such as closing public places and issuing a stay-at-home order to prevent and control the pandemic. On March 16, 2020, the White House issued a 15-day stay-at-home order recommendation. In large cities where the stay-at-home order was enforced earlier, the daily growth rate of cases decreased by 12.8%, while in other large cities where the stay-at-home order was enforced at a later period, the daily growth rate reduced by 7.89%. In the states that did not enforce this order, the decline was 4.32%. Charles Courtemanche et al. found that banning large social activities did not reduce the daily growth rate4 .
In early March 2020, the pandemic began to spread in European countries. On March 2, Switzerland became the first country among them to enforce mandatory quarantine measures for COVID-19 patients. On March 5, Italy announced a nationwide school closure. Soon afterwards, European countries started to issue various prevention and control measures, such as social distancing, a ban on social gatherings, and citywide lockdowns. Seth Flaxman et al.5 reported that interventions enforced in Europe could effectively reduce the novel coronavirus infection coefficient Rt to below 1, thus controlling the virus spread. Interestingly, although Sweden did not ban social gatherings or enforce a lockdown, the infection coefficient dropped below 1 on May 4.
Restricted by social mobilization capacity and other factors, most countries did not enforce a very strict lockdown, but took measures to close specific places and venues. As many countries enforced multiple measures simultaneously, it is difficult to quantify the impact of each control measure on the virus spread.
In general, the lockdown by most countries reduced the infection coefficient R to below 1, demonstrating that it is a very effective prevention and control measure. Although India also enforced a strict lockdown, the coefficient R did not fall below 1, which may be related to its high population density and limited implementation in practice.
2.1.2. Social distancing and its effect
Before the completion of large-scale vaccination to form a protective immune barrier, social distancing is a key measure to constrain the spread of the COVID-19. Almost all countries have suppressed a regional outbreak of the pandemic in various degrees by requiring people to maintain social distancing6. Measures to maintain social distancing include closure of schools and workplaces and ban on social gatherings. Such measures aim to counter the virus spread by delaying the pandemic peak time and shortening the peak period, thereby gaining the initiative for healthcare systems and buying time for vaccine development and drug production4.
The Level-1 response measures adopted in the Chinese mainland for public health events have produced very remarkable results. Tian Huaiyu and his partners summarized the pandemic prevention and control measures adopted in 342 cities across China. All cities suspended school classes, isolated the suspected and confirmed cases, and disclosed related information. The analysis results of the mathematical model show that different interventions and the timing of implementation also have a certain impact on the pandemic development in a city. Compared with cities that enforced delayed control measures, laboratory-confirmed cases reported in the first week of the outbreak by the cities that had taken the initiative in implementing a Level-1 response prior to the COVID-19 outbreak were reduced by 33.3%. The most effective interventions were suspension of urban public transport, closure of recreational venues, and a ban on public gatherings3, 7.
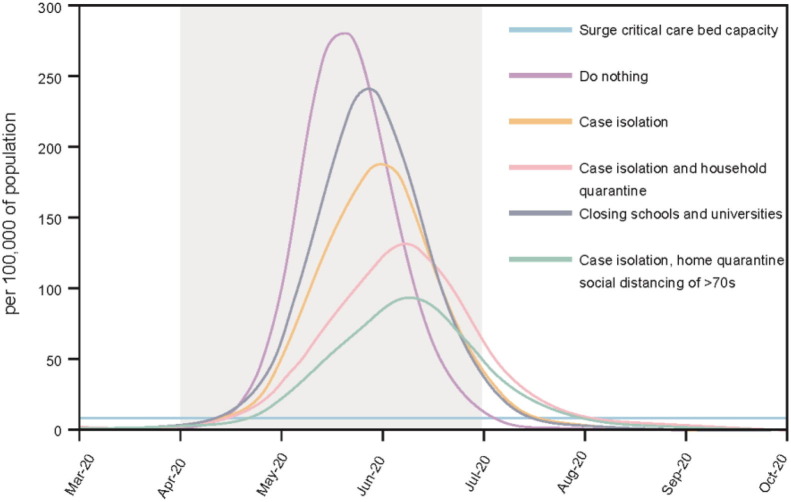
The underlying effect of many public health measures was to reduce the rate of exposure among the people, thereby controlling the virus spread. Ferguson et al.8 applied the micro-simulation model to Britain and America, and studied the effects of different combinations of prevention measures on relieving the pressure on medical systems (Fig. 2 ). This study found that the optimal mitigation strategy (a combination of home isolation of suspected cases, home isolation of co-residents of suspected cases, and social distancing with the elderly and others susceptible to serious diseases) could reduce peak medical demands by two-thirds and decrease deaths by half.
Fig. 2.
Mitigation strategy scenarios in Britain relative to the ICU bed demand8 (Reproduced with permission from reference 8).
Compared with other European countries, Sweden adopted relatively lax prevention measures. Sweden did not enforce a lockdown, require people to wear masks or close restaurants or schools, leading to a relatively high death rate of 15% in April. This situation attracted much attention. Shina C. L. Kamerlin and Peter M. Kasson used an individual-based model to explain the pandemic situation in Sweden9. They pointed out that despite the lax prevention strategy adopted in Sweden, voluntary self-isolation by its people could have contributed towards controlling the pandemic.
The above study reveals that social distancing is also a very effective prevention and control measure. If the public voluntarily cooperates with the government, moderate prevention and control measures can be adopted. For example, Japan and Sweden did not enforce a lockdown, but their citizens cooperated very well and isolated themselves voluntarily, thus benefiting the pandemic control. As for a stay-at-home order, its effect on controlling the spread of the novel coronavirus is varied in various places. In densely populated areas, this order is more effective. A study based on Twitter data found that New Zealanders paid the highest attention to prevention and control measures, while Americans paid the lowest attention10, which to some extent indicates whether social distancing can control the pandemic effectively. To achieve better prevention and control, governments need to increase awareness, and make the public understand the danger of the novel coronavirus and the necessity of social distancing.
2.2. The important role of wearing masks and hand hygiene
The strict implementation of personal prevention measures, headlined by wearing masks and hand hygiene, helps control the source of infection and protect susceptible groups, and plays a key role in the COVID-19 response. On one hand, these measures can protect susceptible groups from any possible source of infection and prevent healthcare providers from being infected when attending to patients. On the other hand, such measures can also relieve the situation where virus carriers release the virus and pollute the surrounding environment. A meta-analysis of 21 previous research papers concludes that wearing masks has a significant inhibitory effect on the spread of respiratory viruses. The risk of respiratory virus infection for healthcare providers and non-healthcare workers can reduce by 80% and 47%, respectively. It also has a remarkable effect on the spread of the influenza virus, SARS-CoV and SARS-CoV-211.
2.3. Construction of Fangcang shelter hospitals is a pioneering action
COVID-19 is a once-in-a-century severe public health event and has posed a huge challenge to medical resources. The Huoshenshan Hospital and Leishenshan Hospital, built following the model of the Beijing Xiaotangshan Hospital used to fight SARS in 2003, cannot completely satisfy the demands for treatment, prevention, and control of COVID-19.
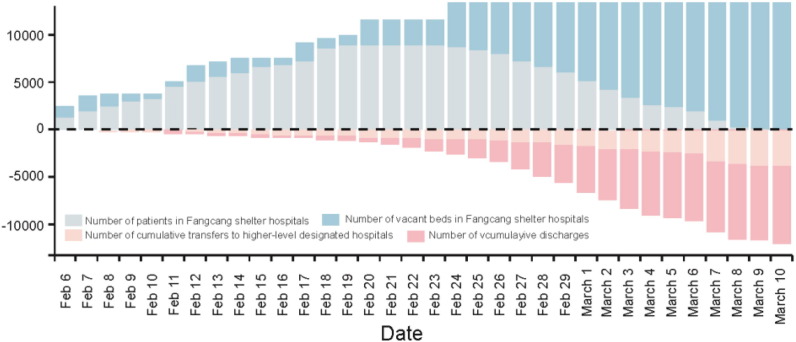
At the suggestion of Wang Chen, who is an academician of the Chinese Academy of Engineering, large venues were requisitioned and transformed into Fangcang shelter hospitals capable of admitting, treating, and isolating a large number of patients. By the end of February 2020, 16 Fangcang shelter hospitals had been built in Wuhan, with over 13,000 beds available, and 12,000 patients admitted and treated. One out of every four COVID-19 case in Wuhan was admitted and treated in such hospitals12 (Fig. 3).
Fig. 3.
Bed capacity and occupancy rate of Fangcang shelter hospitals over time12 (Reproduced with permission from reference 12).
The Fangcang shelter hospitals in Wuhan used to fight COVID-19 have the following major functions: isolation, distribution, provision of basic medical services, close monitoring and rapid referral, and satisfying the needs in life and social interaction12. Based on the five major functions, the experience is summarized as follows:
(1) Centralized isolation is more conducive to pandemic control than home isolation; (2) Classification and distribution of patients at different disease stages and degrees helps allocate medical resources properly; (3) It can ensure the sufficient provision of basic medical services for all patients, especially those who suffer from hypertension and diabetes; (4) Changes in patients’ conditions can be identified timely and rapidly, and the period of referral for critical care can be shortened; (5) The hospitals provide a living community for patients with mild and moderate symptoms, where patients can support each other and participate in recreational activities to maintain mental health.
2.4. The key effect of large-scale testing and close-contacts tracking
Large-scale nucleic acid testing is an effective method to monitor COVID-19 cases actively, confirm infection with the SARS-CoV-2 virus, and implement the measures of early confirmation, isolation, and treatment. Hence, it becomes one of the important means for countries to prevent further infection and spread of the SARS-CoV-2 virus in the population.
China took strict lockdown and closure measures, but did not introduce large-scale nucleic acid testing in the early prevention and control stage. Later, large-scale nucleic acid testing was carried out in local areas in Beijing and Dalian, where the outbreak reoccurred, and effective isolation measures were taken. Without an overall lockdown, testing and isolation also effectively controlled the wide spread of the pandemic13.
Singapore took proactive border-control measures and tracked close contacts extensively. Based on the experience and lessons from the SARS prevention in 2003, Singapore made a rapid and proactive response. It tracked close contacts in detail within 2 h after infected cases were identified. Close-contact trackers surveyed and recorded details of patients’ activities and interactions during the 14 days prior to infection. Therefore, close contacts could be identified rapidly and isolated, and contacts of these close contacts could be also tracked13.
South Korea carried out extensive testing and tracked contacts. Based on the experience and expanded capabilities since the MERS outbreak in 2015, it rapidly developed the COVID-19 diagnostic toolkit and started large-scale testing to help public health officials identify and isolate infected cases and potentially infected ones13.
America started nucleic acid testing among the public on March 14, 2020, but failed to make the testing compulsory among all key groups. There were still problems such as the late reporting of testing results. The case tracing was very inadequate, and there were no mandatory isolation requirements for confirmed or positive cases. Consequently, America had become one of the greatly affected countries. Similarly, for countries like Britain, Spain, and France, despite the great increase of their nucleic acid testing capacity and quantity, a second outbreak occurred to varying degrees due to the absence of strict isolation measures (Table 1).
Table 1.
Comparison of nucleic acid testing strategies against COVID-19 in several representative countries and regions as of September 15, 2020.14
| Country | Nucleic Acid Testing Strategies | Case Tracing, Quarantine, and Isolation Measures | Effect |
|---|---|---|---|
| China | Tested all the people with symptoms possibly in an early stage; Wuhan conducted two waves of large-scale testing from April 8 to June 3, 2020; Beijing and Dalian adopted a strategy of “compulsory testing for all required groups” and “testing on a voluntary basis” in June and July, respectively. |
Strict case tracing, quarantine, isolation and city lockdown | Full control |
| South Korea | Tested all the people with symptoms possibly in an early stage, and started to test the public quickly on February 7. | Strict case tracing, quarantine, and isolation | Basic control |
| Japan | Tested only the people with symptoms or meeting specific criteria before June 15, and tested anyone with symptoms thereafter. | Tracing, quarantine and isolation for clustered cases only; relying on the highly disciplined behavior of the public. | The pandemic was contained and only occurred at a low level. |
| Singapore | Tested specific groups before January 23, and tested anyone with symptoms thereafter. | Strict case tracing, quarantine and isolation | Full control |
| Germany | Tested only specific groups in an early stage, and then started to test the public from April 29. | Relatively strict case tracing, quarantine and isolation | The pandemic was contained and only occurred at a low level. |
| France | Tested anyone with symptoms from February 25 to March 16; tested specific groups from March 17 to May 10; started to test the public from May 11. | Limited tracking of close contacts before May 10; strict case tracing, quarantine and isolation after May 11. | A second outbreak occurred as of September 15, 2020. |
| Britain | Tested groups who met certain conditions before May 17; then tested anyone with symptoms after May 18. | Strict case tracing from January 31 to March 11; case tracing was suspended from March 12 to May 26; strict case tracing was gradually resumed after May 27. | A second outbreak occurs as of September 15, 2020. |
| America | No testing policy before February 27; Tested specific groups or those with symptoms from February 28 to March 13. Public-oriented testing service was available after March 14. |
Failed to provide testing on a voluntary basis, and the feedback was late. Case tracing was conducted at a limited level. No strict isolation measures. |
One of the severely affected countries |
2.5. Significance of pandemic surveillance
When fighting against COVID-19, apart from traditional surveillance methods and information systems, various countries generally apply big data and internet information technology for acquisition, analysis, and application of COVID-19 information.
From the perspectives of pandemic surveillance and information utilization in various countries, experience and lessons from COVID-19 prevention and control are summarized as follows:
-
(1)
In terms of COVID-19 surveillance channels, various countries mainly rely on the existing infection- and disease-surveillance systems, despite improvement or expansion of the existing surveillance systems for COVID-19 in some countries or regions.
-
(2)
From the perspective of prevention and control, if countries or regions develop proactive surveillance of COVID-19 cases, especially by undertaking great efforts in nucleic acid testing for key groups or close contacts in an early stage, and strictly implement quarantine-related measures such as isolation, their pandemic control would be better and remarkable.
-
(3)
Big data plays a vital role in the COVID-19 prevention and control. Multi-source data like traffic and location information greatly help to discover confirmed cases, look for close contacts, identify high-risk groups, and resume work, production, and normal life.
-
(4)
As for China’s response to COVID-19 in early January 2020; there are obvious deficiencies in monitoring pneumonia of unknown causes, identifying the etiology and nature of emerging infectious diseases, and predicting the pandemic situation. Specifically, monitoring pneumonia of unknown causes is confronted with both technological challenges and administrative imperfections. It needs to be studied carefully and further improved.
2.6. Precise prevention and control based on big data
A successful pandemic response consists of scientific prevention and control as well as precise measures. Methods like big data should be used to monitor the pandemic and trace its source at a higher level. Big data can integrate interconnected and interactive individual and group data, thus improving the decision-making and management abilities of governments and experts, and enhancing cities’ “immunity” effectively15. In addition to its important role in COVID-19 prevention and control, and resumption of work and production, big data is also greatly beneficial for regular pandemic prevention and control.
In the context of globalization, cross-regional human mobility is a major reason for the pandemic spread. Therefore, after an outbreak occurs, dynamic spatiotemporal data related to human mobility focusing on airways, railways, and highways can help track potentially infected cases quickly, predict the dynamic evolution trend, trace suspected close contacts, and check potential high-risk groups who resume work and production. Specifically, big data concerning spatiotemporal mobility of humans plays a key role in COVID-19 responses such as pandemic situation study and judgment16, close-contacts tracing17, pandemic risk rating18, etc. Telecom big data provides strong support in population flow statistics based on mobile phone terminal position, pandemic situation study and judgment as well as local prevention and control, greatly helping governments make precise policies19. Network big data has a critical function in the pandemic trend analysis and medical resource distribution, helping joint efforts in advance prevention and precise policy-making by various departments involved in prevention and control, directing enterprises to resume work and production, and can be used for platforms sharing information about the production and distribution of pandemic prevention material20, and for the integration and dissemination of dynamic pandemic data17.
3. Conclusion
Considering the different practices against the COVID-19 and the current pandemic situation in various countries, it is hard to develop a set of common control measures applicable to all countries. Various countries should implement appropriate control measures based on the three principles of infectious disease control, as well as their national conditions including epidemic stage, economic development, and social culture. China needs to continue the following measures in future to consolidate the anti-pandemic achievements and guarantee smooth production and healthy life: regular and unremitting pandemic prevention and control; systematic construction of the public health surveillance system; establishment of a multi-point trigger mechanism for intelligent early warning of infectious diseases; timely and effective control of infection sources based on large-scale testing capacity; optimization of vaccine studies and vaccination strategies, and proactive surveillance; upgrading of prevention and control measures by using big data and AI; creation of a pandemic information sharing mechanism to improve data utilization efficiency; improving pandemic prevention awareness and health education among the public, etc. Meanwhile, other countries could also learn from China on how to make effective control strategies against the COVID-19 pandemic based on their own national conditions. However, real control effects depend not only on knowing the right control strategies, but also effectively implementing these strategies.
4. Financial disclosure
This work was funded by the Advisory Research Project of the Chinese Academy of Engineering (No. 2020-XZ-37), the National Natural Science Foundation of China (No. 81871738), and the Mega-projects of Science and Technology Research (No. 2018ZX10711001).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Johns Hopkins University & Medicine Coronavirus Resource Center. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. Johns Hopkins University, 2020-09-25. https://coronavirus.jhu.edu/map.html.
- 2.Weekly epidemiological update on COVID-19 - 20 April 2021. 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---20-april-2021.
- 3.Tian H., Liu Y., Li Y., et al. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368(6491):638–642. doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Courtemanche C., Garuccio J., Le A., Pinkston J., Yelowitz A. Strong Social Distancing Measures In The United States Reduced The COVID-19 Growth Rate. Health Aff. 2020;39(7):1237–1246. doi: 10.1377/hlthaff.2020.00608. [DOI] [PubMed] [Google Scholar]
- 5.Flaxman S., Mishra S., Gandy A., et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- 6.Courtemanche C. Strong Social Distancing Measures In The United States Reduced The COVID-19 Growth Rate. Health Affairs NLM (Medline) 2020;39(7):1237–1246. doi: 10.1377/hlthaff.2020.00608. [DOI] [PubMed] [Google Scholar]
- 7.Lai S., Ruktanonchai N.W., Zhou L., et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020;585(7825):410–413. doi: 10.1038/s41586-020-2293-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferguson NM, Laydon D, Nedjati-Gilani G, Imai N, Ghani AC. Imperial College COVID-19 Response Team Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. London. 2020 [Google Scholar]
- 9.Kamerlin S.C.L., Kasson P.M. Managing Coronavirus Disease 2019 Spread With Voluntary Public Health Measures: Sweden as a Case Study for Pandemic Control. Clin Infect Dis. 2020;71(12):3174–3181. doi: 10.1093/cid/ciaa864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Doogan C., Buntine W., Linger H., Brunt S. Public Perceptions and Attitudes Toward COVID-19 Nonpharmaceutical Interventions Across Six Countries: A Topic Modeling Analysis of Twitter Data. Journal of medical Internet research. 2020;22(9):e21419. doi: 10.2196/21419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liang M., Gao L., Cheng C., et al. Efficacy of face mask in preventing respiratory virus transmission: A systematic review and meta-analysis. Travel Med Infect Dis. 2020;36 doi: 10.1016/j.tmaid.2020.101751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen S., et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. The Lancet. 2020;395(10232):1305–1314. doi: 10.1016/S0140-6736(20)30744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu N., Cheng K.-W., Qamar N., Huang K.-C., Johnson J.A. Weathering COVID-19 storm: Successful control measures of five Asian countries. Am J Infect Control. 2020;48(7):851–852. doi: 10.1016/j.ajic.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oxford BSoGUo. Coronavirus government response tracker. 2021. https://www.bsg.ox.ac.uk/research/research-projects/coronavirus-government-response-tracker.
- 15.Zhu Y., Zhang Y. Relying on big data to actively fight against the epidemic. China's national conditions and strength. 2020;04:4–5. [Google Scholar]
- 16.Gilbert M, Pullano G, Pinotti F, et al. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. 2020;395(10227):871–877. doi: 10.1016/S0140-6736(20)30411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tang C., Li R. Analysis and Discussion on the Application of Information Technology in the Prevention and Treatment of New Epidemics of COVID-19 (in Chinese) World Science and Technology Research and Development. 2020;42(04):426–438. [Google Scholar]
- 18.Cui C., Zeng S. Ditigal Technology Fighting Epidemic: China's Big Data Security Is in Action(in Chinese) Journal of Information Securyity Research. 2020;6(03):194–201. [Google Scholar]
- 19.Huang Y., Feng M., Ding S. Big Data Development Strategy for Telecom Operators(in Chinese) Telecommunications Science. 2013;29(03):7–11. [Google Scholar]
- 20.Ye Y., Yu J., Sheng X., Zhou M. Analysis on the application of big data in the prevention and control of COVID-19(in Chinses) Technology Vision. 2020;22:16–18. [Google Scholar]