Abstract
Background
Evidence from disease epidemics shows that healthcare workers are at risk of developing short‐ and long‐term mental health problems. The World Health Organization (WHO) has warned about the potential negative impact of the COVID‐19 crisis on the mental well‐being of health and social care professionals. Symptoms of mental health problems commonly include depression, anxiety, stress, and additional cognitive and social problems; these can impact on function in the workplace. The mental health and resilience (ability to cope with the negative effects of stress) of frontline health and social care professionals ('frontline workers' in this review) could be supported during disease epidemics by workplace interventions, interventions to support basic daily needs, psychological support interventions, pharmacological interventions, or a combination of any or all of these.
Objectives
Objective 1: to assess the effects of interventions aimed at supporting the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic.
Objective 2: to identify barriers and facilitators that may impact on the implementation of interventions aimed at supporting the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic.
Search methods
On 28 May 2020 we searched the Cochrane Database of Systematic Reviews, CENTRAL, MEDLINE, Embase, Web of Science, PsycINFO, CINAHL, Global Index Medicus databases and WHO Institutional Repository for Information Sharing. We also searched ongoing trials registers and Google Scholar. We ran all searches from the year 2002 onwards, with no language restrictions.
Selection criteria
We included studies in which participants were health and social care professionals working at the front line during infectious disease outbreaks, categorised as epidemics or pandemics by WHO, from 2002 onwards. For objective 1 we included quantitative evidence from randomised trials, non‐randomised trials, controlled before‐after studies and interrupted time series studies, which investigated the effect of any intervention to support mental health or resilience, compared to no intervention, standard care, placebo or attention control intervention, or other active interventions. For objective 2 we included qualitative evidence from studies that described barriers and facilitators to the implementation of interventions. Outcomes critical to this review were general mental health and resilience. Additional outcomes included psychological symptoms of anxiety, depression or stress; burnout; other mental health disorders; workplace staffing; and adverse events arising from interventions.
Data collection and analysis
Pairs of review authors independently applied selection criteria to abstracts and full papers, with disagreements resolved through discussion. One review author systematically extracted data, cross‐checked by a second review author. For objective 1, we assessed risk of bias of studies of effectiveness using the Cochrane 'Risk of bias' tool. For objective 2, we assessed methodological limitations using either the CASP (Critical Appraisal Skills Programme) qualitative study tool, for qualitative studies, or WEIRD (Ways of Evaluating Important and Relevant Data) tool, for descriptive studies. We planned meta‐analyses of pairwise comparisons for outcomes if direct evidence were available. Two review authors extracted evidence relating to barriers and facilitators to implementation, organised these around the domains of the Consolidated Framework of Implementation Research, and used the GRADE‐CERQual approach to assess confidence in each finding. We planned to produce an overarching synthesis, bringing quantitative and qualitative findings together.
Main results
We included 16 studies that reported implementation of an intervention aimed at supporting the resilience or mental health of frontline workers during disease outbreaks (severe acute respiratory syndrome (SARS): 2; Ebola: 9; Middle East respiratory syndrome (MERS): 1; COVID‐19: 4). Interventions studied included workplace interventions, such as training, structure and communication (6 studies); psychological support interventions, such as counselling and psychology services (8 studies); and multifaceted interventions (2 studies).
Objective 1: a mixed‐methods study that incorporated a cluster‐randomised trial, investigating the effect of a work‐based intervention, provided very low‐certainty evidence about the effect of training frontline healthcare workers to deliver psychological first aid on a measure of burnout.
Objective 2: we included all 16 studies in our qualitative evidence synthesis; we classified seven as qualitative and nine as descriptive studies. We identified 17 key findings from multiple barriers and facilitators reported in studies. We did not have high confidence in any of the findings; we had moderate confidence in six findings and low to very low confidence in 11 findings. We are moderately confident that the following two factors were barriers to intervention implementation: frontline workers, or the organisations in which they worked, not being fully aware of what they needed to support their mental well‐being; and a lack of equipment, staff time or skills needed for an intervention. We are moderately confident that the following three factors were facilitators of intervention implementation: interventions that could be adapted for local needs; having effective communication, both formally and socially; and having positive, safe and supportive learning environments for frontline workers. We are moderately confident that the knowledge or beliefs, or both, that people have about an intervention can act as either barriers or facilitators to implementation of the intervention.
Authors' conclusions
There is a lack of both quantitative and qualitative evidence from studies carried out during or after disease epidemics and pandemics that can inform the selection of interventions that are beneficial to the resilience and mental health of frontline workers. Alternative sources of evidence (e.g. from other healthcare crises, and general evidence about interventions that support mental well‐being) could therefore be used to inform decision making. When selecting interventions aimed at supporting frontline workers' mental health, organisational, social, personal, and psychological factors may all be important. Research to determine the effectiveness of interventions is a high priority. The COVID‐19 pandemic provides unique opportunities for robust evaluation of interventions. Future studies must be developed with appropriately rigorous planning, including development, peer review and transparent reporting of research protocols, following guidance and standards for best practice, and with appropriate length of follow‐up. Factors that may act as barriers and facilitators to implementation of interventions should be considered during the planning of future research and when selecting interventions to deliver within local settings.
Plain language summary
What is the best way to support resilience and mental well‐being in frontline healthcare professionals during and after a pandemic?
What is ‘resilience’?
Working as a 'frontline' health or social care professional during a global disease pandemic, like COVID‐19, can be very stressful. Over time, the negative effects of stress can lead to mental health problems such as depression and anxiety, which, in turn, may affect work, family and other social relationships. ‘Resilience’ is the ability to cope with the negative effects of stress and so avoid mental health problems and their wider effects.
Healthcare providers can use various strategies (interventions) to support resilience and mental well‐being in their frontline healthcare professionals. These could include work‐based interventions, such as changing routines or improving equipment; or psychological support interventions, such as counselling.
What did we want to find out?
First (objective 1), we wanted to know how successfully any interventions improved frontline health professionals’ resilience or mental well‐being.
Second (objective 2), we wanted to know what made it easier (facilitators) or harder (barriers) to deliver these interventions.
What did we do?
We searched medical databases for any kind of study that investigated interventions designed to support resilience and mental well‐being in healthcare professionals working at the front line during infectious disease outbreaks. The disease outbreaks had to be classified by the World Health Organization (WHO) as epidemics or pandemics, and take place from 2002 onwards (the year before the severe acute respiratory syndrome (SARS) outbreak).
What did we find?
We found 16 relevant studies. These studies came from different disease outbreaks ‐ two were from SARS; nine from Ebola; one from Middle East respiratory syndrome (MERS); and four from COVID‐19. The studies mainly looked at workplace interventions that involved either psychological support (for example, counselling or seeing a psychologist) or work‐based interventions (for example, giving training, or changing routines).
Objective 1: one study investigated how well an intervention worked. This study was carried out immediately after the Ebola outbreak, and investigated whether staff who were training to give other people (such as patients and their family members) 'psychological first aid' felt less ‘burnt out’. We had some concerns about the results that this study reported and about some of its methods. This means that our certainty of the evidence is very low and we cannot say whether the intervention helped or not.
Objective 2: all 16 studies provided some evidence about barriers and facilitators to implement interventions. We found 17 main findings from these studies. We do not have high confidence in any of the findings; we had moderate confidence in six findings and low to very low confidence in 11 findings.
We are moderately confident that the following two factors were barriers to implementation of an intervention: frontline workers, or the organisations in which they worked, not being fully aware of what they needed to support their mental well‐being; and a lack of equipment, staff time or skills needed for an intervention.
We are moderately confident that the following three factors were facilitators to implementation of an intervention: interventions that could be adapted for a local area; having effective communication, both formally within an organisation and informal or social networks; and having positive, safe and supportive learning environments for frontline healthcare professionals.
We are moderately confident that the knowledge and beliefs that frontline healthcare professionals have about an intervention can either help or hinder implementation of the intervention.
Key messages
We did not find any evidence that tells us about how well different strategies work at supporting the resilience and mental well‐being of frontline workers. We found some limited evidence about things that might help successful delivery of interventions. Properly planned research studies to find out the best ways to support the resilience and mental well‐being of health and social care workers are urgently required.
How up‐to‐date is this review?
This review includes studies published up to 28 May 2020.
Summary of findings
Background
Description of the condition
Evidence from infectious disease epidemics has shown that healthcare workers are at risk of developing both short‐ and long‐term mental health problems (Maunder 2006), with up to one‐third of frontline healthcare workers experiencing high levels of distress (Lynch 2020). Health and social care professionals may develop a lack of resilience or mental health problems, or both, as a result of working in a variety of stressful situations. However, working during or immediately after an outbreak of an infectious disease which has, or has the potential to, overwhelm the health and social care system, may have a particularly negative impact on the health and well‐being of individual health and social care staff and on the maintenance of a functional workforce and healthcare system. The common work‐related factors affecting mental health and well‐being during a pandemic include: concern about exposure to the virus; personal and family needs and responsibilities; managing a different workload; lack of access to necessary tools and equipment (including personal protection equipment, PPE); feelings of guilt relating to the lack of contribution; uncertainty about the future of the workplace or employment; learning new technical skills; and adapting to a different workplace or schedule (CDC 2020a; Houghton 2020; Shanafelt 2020).
The mental health of frontline health and social care professionals may also be negatively affected by witnessing death, and feeling powerless over the levels of patient death. During epidemics of contagious diseases, frontline health and social care professionals may experience particular concerns around the risk of infection and re‐infection. These can have adverse effects on individual health and social care professionals, the delivery of patient care, and the capacity of healthcare systems to respond to the increased demands during a disease epidemic or pandemic (Kang 2020).
The World Health Organization (WHO) defines mental health as "a state of well‐being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community" (WHO 2004). The term 'mental health' describes someone's psychological and emotional well‐being, and good mental health can be considered to be "a positive state of mind and body, feeling safe and able to cope, with a sense of connection with people, communities and the wider environment" (Strathdee 2015). Symptoms associated with mental health problems commonly include depression, anxiety, or stress. Mental health problems can result in additional cognitive and social problems, and can lead to long‐term issues, including post‐traumatic stress disorder (PTSD). These problems can impact on function in the workplace, while a negative working environment can lead to mental health problems (WHO 2019a).
Possible symptoms that frontline health and social care professionals may experience include: feelings of irritation, anger, uncertainty, stress, nervousness or anxiety; lack of motivation; tiredness; feeling sad, depressed or overwhelmed; difficulty in sleeping or concentrating (CDC 2020a). Negative effects of mental health may result in unhealthy behaviours, such as alcohol, tobacco or drug abuse, which may contribute to reduced ability to function at work (CDC 2020b). Moreover, these unhealthy behaviours could also potentially be linked to family breakdown and domestic abuse, further increasing feelings of depression, anxiety and stress and impacting negatively on ability to function. Health and social care professionals experiencing mental health problems may have high levels of absenteeism or presenteeism (turning up for work when unable to function in an optimal way).
Definitions of resilience vary, but often refer to the ability to cope with negative effects of stress or adversity. For the purposes of this review, we define resilience as a dynamic, multifactorial process in which an individual can “adjust to adversity, maintain equilibrium, retain some sense of control over their environment, and continue to move on in a positive manner” (Jackson 2007). Often resilience is contrasted with the concept of burnout, which is characterised by distress and exhaustion, and dysfunction at work (WHO 2019b).
A pandemic is defined as a global outbreak of a disease (WHO 2020a), while an epidemic is a greater than normal expected number of cases of a disease in a population, often with a sudden increase in cases (CDC 2011). Pandemics are generally classified as epidemics prior to reclassification as a pandemic if there is global spread of a disease. While declarations of diseases as epidemics or pandemics are not always clear, and local outbreaks of a disease may or may not be categorised as an epidemic by local government or health service organisations, the WHO plays a key role in international detection and classification of epidemics and pandemics. Within this review we focus on infectious diseases that have been categorised by WHO 2020a as "pandemic or epidemic diseases", as these diseases arguably have the greatest potential to affect adversely the mental well‐being and resilience of health and social care professionals and, consequently, the function of health and social care systems and the delivery of patient care.
Description of the intervention
A number of strategies have been recommended to support the mental health and well‐being of frontline health and social care professionals during disease outbreaks. These include accurate work‐related information, regular breaks, adequate rest and sleep, a healthy diet, physical activity, peer support, family support, avoidance of unhelpful coping strategies (e.g. alcohol and drugs), limitation of social media use, and professional counselling or psychological services. During the COVID‐19 pandemic, healthcare managers have been urged to consider the long‐term impact on their workers, and to ensure clear communication with staff (WHO 2020b). Several strategies that healthcare providers could implement have been proposed, such as rotating workers from higher‐ to lower‐stress roles, partnering experienced and less experienced workers (buddy systems), initiation and monitoring of work breaks, flexible schedules, and provision of social support (WHO 2020b). Training key staff members in 'psychological first aid' has been proposed to provide basic emotional and practical support to people affected by their stressful work environment. Interventions aim to strengthen and maintain personal resilience, enabling a worker to manage their experiences and increased work‐related demands and continue to perform well in the workplace (Robertson 2016).
How the intervention might work
Interventions aimed at supporting the mental health and well‐being of frontline health and social care professionals, or helping them cope with highly stressful or anxiety‐provoking situations, may work in a variety of different ways. The WHO highlights that the promotion of positive mental health and the prevention of negative mental health consequences are overlapping and complementary activities (WHO 2002). Interventions might work in the following ways.
Changing the workplace or organisation of work. These interventions may work by adjusting work practices or providing opportunities for rest and relaxation during the workday,or both (e.g. regular breaks, shorter working hours, regular team meetings, relaxation/recreation areas in workplaces), or by enabling workers to cope better (e.g. through provision of information, guidance, mentorship, or training). These strategies might work by reducing stress to a manageable level, by providing time for health and social care professionals to develop or optimise their own coping mechanisms or support systems, or by placing a worker away from frontline work for a period of time.
Supporting the basic daily needs of frontline health and social care professionals. These interventions may promote or support a healthy lifestyle and self‐care, such as eating, sleeping, exercising, following a routine, avoiding excess social media, staying in touch with family and friends, doing things that are enjoyable; or may comprise the use of techniques such as progressive muscle relaxation or meditation, which aim to help stop ‐ or distract from ‐ negative thoughts. While there are a number of studies that report a link between lifestyle changes and mental health benefits, the underlying mechanisms have not been fully established. The benefits of physical activity are proposed to be associated with a range of neurobiological, psychosocial and behavioural mechanisms (Lubans 2016).
Providing psychological support. These interventions may use cognitive‐behavioural techniques to help people find ways to stop negative cycles of thoughts and to change the way they respond to things that make them feel anxious or distressed. Interventions may include: self‐help management techniques (e.g. online cognitive behavioural therapy (CBT), mindfulness, writing down worries) including the use of well‐being and sleep apps; and professional psychological or counselling support (e.g. talking therapies, support groups or psychotherapy, which can include CBT). These psychological support mechanisms can also teach people how to avoid unhelpful coping strategies.
Medication (e.g. prescribed medication for depression, anxiety, sleep problems and/or other mental disorders). Antidepressant drugs can act on neurochemicals in the brain, but may also mediate complex neuroplastic and neuropsychological mechanisms (Harmer 2017).
It is thought that workplace stress can negatively impact resilience, but that processes of adaptation and personal development can potentially build resilience and influence the ability to cope with stressful situations (Robertson 2016). Strategies to strengthen and maintain personal resilience within a workplace may incorporate the development of positive relationships and networks (e.g. through mentorship), as well as personal skills, such as emotional insight and maintaining a healthy work‐life balance (Jackson 2007). Evidence suggests that recovery‐enhancing interventions, such as relaxation, physical activity, stress management and workplace changes, may prevent the development of ill health amongst workers (Verbeek 2018).
Why it is important to do this review
In March 2020, the WHO declared the COVID‐19 coronavirus outbreak a pandemic (WHO 2020c), and warned about the potential negative impact of the crisis on the psychological and mental well‐being throughout the population, including and, in particular, health and social care professionals (WHO 2020b).
The negative impact on health and social care professions may result in effects at multiple levels, from the individual worker to the entire health and social care system at the macro level. This topic was identified as a high priority for a rapid review by the Cochrane COVID‐19 rapid reviews initiative (Priority Question 78).
This review is important in order to inform recommendations to support the mental health of frontline personnel during the COVID‐19 crisis and during the subsequent (‘de‐escalation’) phase, and during other disease epidemics and pandemics. This is important for the health and well‐being of individual health and social care staff and for the maintenance of a functional workforce and healthcare system.
There are currently a number of systematic reviews that synthesise evidence relating to workplace health and well‐being, including several that focus on issues relevant to mental health, or resilience, or both. Key Cochrane Reviews and protocols that are potentially relevant to this topic are summarised in Table 3. These include two reviews and one protocol specifically focused on the population of healthcare workers, addressing issues relating to prevention (Ruotsalainen 2015), and reduction (Giga 2018, protocol) of workplace stress and fostering of workplace resilience (Kunzler 2020). Ruotsalainen 2015 reports moderate‐certainty evidence that physical relaxation may reduce stress levels of healthcare workers, as compared to no intervention, low‐certainty evidence that stress levels of healthcare workers may reduce following cognitive‐behavioural intervention (with or without relaxation) as compared to no intervention, and low‐certainty evidence that changing work schedules of healthcare workers may reduce stress levels. Kunzler 2020 reports that there is very low‐certainty evidence that resilience training for healthcare professionals may result in higher levels of resilience, lower levels of depression, stress or stress perception, and higher levels of some resilience factors, as compared to control. Furthermore, there are reviews summarising evidence relating to general well‐being of workers, including issues such as stress and sleep; workers with diagnosed mental health problems; and issues associated with sick leave and return to work (see Table 3).
1. Summary of Cochrane Reviews and protocols potentially relevant to workplace mental health, resilience, or both.
| Review | Review title | Population | Interventions | Outcomes |
| Reviews focused specifically on healthcare workers/professionals | ||||
| Giga 2018 | Organisational‐level interventions for reducing occupational stress in healthcare workers (protocol) | "adult workers, aged 18 years or above, employed in a healthcare setting, who have not actively sought help for conditions such as stress and burnout. This includes workers, such as nurses and physicians, who are in training and undertaking clinical work" | "organisational level interventions aimed at reducing stress. Eligible interventions include the following.
|
|
| Kunzler 2020 | Psychological interventions to foster resilience in healthcare professionals | "Adults aged 18 years and older, who are employed as healthcare professionals, i.e. healthcare staff delivering direct medical care such as physicians, nurses, hospital personnel, and allied healthcare staff working in health professions, as distinct from medical care (e.g. psychologists, social workers, counsellors, physical therapists, occupational therapists, speech therapists, medical assistants, medical technicians)" | "Any psychological resilience intervention, irrespective of content, duration, setting or delivery mode." |
|
| Ruotsalainen 2015 | Preventing occupational stress in healthcare workers | "healthcare workers officially employed in any healthcare setting or at student nurses or physicians otherwise in training to become a professional who were also doing clinical work" "workers who had not actively sought help for conditions such as burnout, depression or anxiety disorder" |
"any kind of intervention aimed at preventing or reducing stress arising from work." Including:
|
|
| Reviews focused on participants with diagnosed mental health problems | ||||
| Nieuwenhuijsen 2014 | Interventions to improve return to work in depressed people | "adult (that is over 17 years old) workers (employees or self‐employed)" | "all interventions aimed at reducing work disability, thereby differentiating work‐directed interventions from clinical interventions." |
|
| Suijkerbuijk 2017 | Interventions for obtaining and maintaining employment in adults with severe mental illness, a network meta‐analysis | "adults aged between 18 and 70 years who had been diagnosed with severe mental illness. We defined severe mental illness as schizophrenia or other psychotic disorders, bipolar disorder, depression with psychotic features or other long‐lasting psychiatric disorders, with a disability in social functioning or participating in society, such as personality disorder, severe anxiety disorder, post‐traumatic stress disorder, major depression or autism with a duration of at least two years. Study participants had to be unemployed due to severe mental illness." | "We included trials of all types of vocational rehabilitation compared to each other or to no intervention or psychiatric care only." These included:
|
|
| Reviews focused on sick leave, absenteeism, job loss and/or return to work | ||||
| Kausto 2019 | Self‐certification versus physician certification of sick leave for reducing sickness absence and associated costs | "individual employees or insured workers" | "We included studies evaluating the effects of introducing, abolishing, or changing the period of self‐certification of sickness absence. We included any sickness certification practice in which the employee could report sick for a certain number of days without physician certification or certification by any other healthcare professional. Self‐certification could be accepted for any disease or restricted to certain types of diseases. We also included studies that combined self‐certification with an intervention related to supervisor role or practices, working conditions (e.g. flexible working conditions), or terms of sickness benefit (e.g. number of waiting days), etc. (i.e. multicomponent interventions)." |
|
| Liira 2016 | Workplace interventions for preventing job loss and other work‐related outcomes in workers with alcohol misuse (protocol) | "workers with alcohol misuse aged 18 years or above.......participants who fulfil the criteria for hazardous drinking, that is, weekly drinking an amount that regularly exceeds 190 grams of pure alcohol for men or 100 grams for women, as defined by the National Institute on Alcohol Abuse and Alcoholism" | "interventions that target either the workplace, work team or the individual worker" |
|
| Vogel 2017 | Return‐to‐work co‐ordination programmes for improving return to work in workers on sick leave | "adults of working age (16 to 65 years) who:
|
Return‐to‐work co‐ordination programmes, defined as:
|
|
| Reviews focused on well‐being of employees (not specifically healthcare workers) | ||||
| Erren 2013 | Adaptation of shift work schedules for preventing and treating sleepiness and sleep disturbances caused by shift work (protocol) | "any adult workers (age > 18) in shift work schedules that include night shift work, irrespective of industry, country, age or comorbidities" | "any intervention that deals with a shift work schedule" |
|
| Kuehnl 2019 | Human resource management training of supervisors for improving health and well‐being of employees | "any type of supervisors, of any gender and their dependently employed subordinates of any gender. For the purpose of this review a supervisor was defined as a person who has the authority to give instructions to at least one subordinate and is held responsible for their work and actions. We included studies that had been conducted in profit, non‐profit or governmental organisations, that is, in a real working environment." | Human resource management training of supervisors, including:
|
|
| Kuster 2017 | Computer‐based versus in‐person interventions for preventing and reducing stress in workers | "full‐time, part‐time, or self‐employed working individuals over 18 years of age" | "any type of worker‐focused web‐based stress management intervention, aimed at preventing or reducing work‐related stress with techniques such as CBT, relaxation, time management, or problem‐solving skills training. These interventions had to be delivered via email, a website, or a stand‐alone computer programme" |
|
| Liira 2014 | Pharmacological interventions for sleepiness and sleep disturbances caused by shift work | "workers who undertake shift work (including night shifts) in their present jobs and who may or may not have sleep problems." | "any pharmacological intervention aimed at preventing or reducing sleepiness at work or sleep disturbances caused by shift work" |
|
| Naghieh 2015 | Organisational interventions for improving well‐being and reducing work‐related stress in teachers | "teachers working at primary and secondary schools, serving children aged between 4 and 18 years." | "Organisational interventions for employee wellbeing target the stressors in the work environment, rather than the stress response of the individual employee. They aim to alter the psychosocial work environment by changing some aspect of the organisation, such as structures, policies, processes, climate, programmes, roles, tasks, etc." |
|
| Pachito 2018 | Workplace lighting for improving alertness and mood in daytime workers | "adults aged 18 years and above performing work exclusively indoors, in the period restricted to 7:00 am to 10:00 pm, irrespective of type of work, industry and comorbidities" | "different types of light interventions" |
|
| Slanger 2016 | Person‐directed, non‐pharmacological interventions for sleepiness at work and sleep disturbances caused by shift work | "adult workers engaged in shift work schedules that include night‐shift work, irrespective of industry, country, age or comorbidities." | "any person‐directed, non‐pharmacological intervention" |
|
| CBT: cognitive behavioural therapy; WHO: World Health Organization | ||||
While these Cochrane Reviews provide evidence that there are interventions that can benefit the mental well‐being of healthcare workers, this evidence is not specific to health and social care workers in frontline positions during disease outbreaks. As described above, the work of frontline health and social care professionals during a disease outbreak, epidemic or pandemic places a unique burden on the mental health and resilience of these workers and – as such – a separate review with this specific focus is merited. Furthermore, the current body of Cochrane Reviews focuses on the synthesis of quantitative evidence of effectiveness of interventions, and these do not incorporate qualitative evidence relating to the barriers and facilitators to implementation of these interventions. During disease epidemics and pandemics there may be particular challenges to implementation of workplace, or worker‐focused, interventions, and it is therefore important to bring both quantitative and qualitative evidence together. This review is therefore important as it will bring unique evidence, which is relevant and useful to decision making relating to interventions to support mental health and resilience of frontline health and social care professionals during disease outbreaks. This will create accessible evidence, highly relevant to decision‐making during, and planning for, any future outbreaks of COVID‐19 or other disease pandemics.
Objectives
Objective 1: to assess the effects of interventions aimed at supporting the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic.
Objective 2: to identify barriers and facilitators that may impact on the implementation of interventions aimed at supporting the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic.
Methods
Criteria for considering studies for this review
Types of studies
To address objective 1, we included quantitative evidence from the following.
Randomised trials: experimental studies in which people are allocated to different interventions using methods that are random. We included cluster‐randomised trials, in which randomisation is at the level of the site, where a study has at least two intervention sites and two control sites (EPOC 2017a).
Non‐randomised trials: experimental studies in which people are allocated to different interventions using methods that are not random (EPOC 2017a).
Controlled before‐after studies: studies in which observations are made before and after the implementation of an intervention, both in a group that receives the intervention and in a control group that does not (EPOC 2017a).
Interrupted time series studies: studies that use observations at multiple time points before and after an intervention (the ‘interruption’). The design attempts to detect whether the intervention has had an effect significantly greater than any underlying trend over time. For inclusion, these studies must have a clearly defined point in time when the intervention occurred, and at least three data points before and three after the intervention (EPOC 2017a).
We planned to include evidence from non‐randomised studies as the planning and conduct of randomised studies is likely to be highly challenging during disease epidemics and pandemics. However, evidence from non‐randomised studies has an increased risk of bias; in particular there are a number of confounding factors that may influence whether an individual receives one or other intervention. In relation to interventions to support the mental health and resilience of health and social care professionals, important confounding factors were likely to include the setting that the healthcare professional is working in, the type and grade of health professional, and the length of time that the individual has worked within the disease epidemic or pandemic. Furthermore, there are known differences between men and women in the reporting of mental health symptoms and treatment rates for symptoms such as depression and anxiety, therefore gender may have been a confounding domain (MHF 2016). There is also a growing body of evidence that socioeconomic status may be associated with an increased chance of developing mental health problems (WHO 2014a), and this could be an important confounding factor in some studies. If these important confounding factors were not controlled for within the non‐randomised study, we planned to judge the study to be at high risk of bias.
We excluded evidence from non‐randomised studies in which the interventions were not assigned by the investigators, including prospective and retrospective cohort and case‐control studies.
To address objective 2, we included any papers that described barriers or facilitators to implementation of an intervention. Papers could report a qualitative, quantitative or descriptive study. We classified papers that:
reported a pre‐planned qualitative method of data collection (e.g. interviews) as 'qualitative studies';
reported a pre‐planned quantitative method of data collection (e.g. cohort study) as 'quantitative studies';
reported a pre‐planned study that combined qualitative and quantitative methods of data collection as 'mixed methods studies';
described factors relating to implementation of an intervention, but that did not report a pre‐planned or systematic method of data collection as 'descriptive studies'.
Our classification of studies was based on the type of data extracted and used for our qualitative evidence synthesis, rather than on the pre‐planned study design; for example, we classified a mixed methods study from which we only used qualitative data as a 'qualitative study', and we classified a quantitative study from which we only used descriptive data as a 'descriptive study'.
We excluded secondary research (systematic reviews and evidence syntheses). However, where we found relevant secondary research studies, we considered any primary studies included in these reviews, and included any that met our inclusion criteria.
Types of participants
We included studies in which participants were (or had been) health and social care professionals working at the front line during disease outbreaks, epidemics or pandemics, from the year 2002 onwards. Within this review we use the term 'frontline workers' as an abbreviation to refer to health and social care professionals working at the front line during disease outbreaks, epidemics or pandemics. Operational definitions of key terms are below.
Disease epidemics or pandemics
We only included studies relating to epidemics or pandemics that have occurred from the year 2002 onwards. We categorised evidence as 'epidemic' or 'pandemic' according to the WHO categorisation (WHO 2020a), and other evidence as 'outbreak'.
We included studies conducted during or after an epidemic or pandemic.
We included infectious diseases that were categorised by WHO 2020a as “pandemic or epidemic diseases”, if outbreaks occurred in 2002 or later. These may have included:
chikungunya
cholera
Crimean‐Congo haemorrhagic fever
Ebola virus disease
Hendra virus infection
influenza (pandemic, seasonal, zoonotic)
Lassa fever
Marburg virus disease
meningitis
Middle East respiratory syndrome (MERS)
monkeypox
Nipah virus infection
novel coronavirus (2019‐nCoV)
plague
Rift Valley fever
severe acute respiratory syndrome (SARS)
smallpox
tularaemia
yellow fever
Zika virus disease
We excluded studies relating to diseases that have not been listed by WHO 2020a as a pandemic or epidemic disease. This included studies relating to the following diseases: insect‐borne diseases, including (but not limited to): dengue fever, malaria, leishmaniasis, measles, hepatitis, hand foot and mouth disease, mumps, polio, Creutzfeldt–Jakob disease (CJD) and HIV/AIDS.
The decision to focus on epidemics or pandemics from the year 2002 onwards was made pragmatically, with the aim of limiting the necessary searching, in order to ensure feasibility of carrying out this review rapidly. We considered the year 2002 appropriate as the outbreak of SARS occurred in 2003, meaning that we would capture studies undertaken in response to SARS, as well as more recent outbreaks of the Ebola virus and MERS (originated 2012). A similar justification for date restriction was used in a Cochrane qualitative evidence synthesis that focused on infection control during infectious respiratory diseases (Houghton 2020).
Health and social care professionals
We included studies in which the participant is any person who works in a health or social care setting in a professional capacity, or who provides health or social care within community settings deployed at the ‘front line’. This included, but was not limited* to the following.
Doctors
Nurses and midwives
Allied health and social care professionals, including all those currently regulated by the UK's Health and Care Professions Council (HCPC 2016). This includes: art therapists, biomedical scientist, chiropodists/podiatrists, clinical scientists, dietitians, hearing aid dispensers, occupational therapists, operating department practitioners, orthoptists, paramedics, physiotherapists/physical therapists, practitioner psychologists, prosthetists/orthotists, radiographers, social workers, speech and language therapists.
Students of any of the above listed professions
Health and social care assistants
*The list given here is not comprehensive of all health and social care professionals. For professional groups included in search strategy see Appendix 1 (row 12‐18), Appendix 2 (row 34‐72), and Appendix 3 (row 14‐21).
We planned to include health and social care professionals who returned to practice after a period of absence (> 3 months), for example, following a career break or retirement.
We also included students in education to become health and social care professionals where they enter paid clinical or social care practice early in order to work during the epidemic or pandemic.
We included volunteers who delivered frontline health or social care services; for example, medical or nursing staff volunteering to assist in different countries. To be included, the volunteer had to be working in a professional role, as listed above.
We excluded studies including only other people who may have frontline roles, but who are not providing health and social care, such as cleaners, porters and biomedical waste management handlers, or volunteers undertaking tasks such as delivery of medicines. We acknowledge that there are equity issues here and that evidence relating to 'non‐professional' frontline workers is of high importance. However, this was beyond the scope of this rapid review; in future updates we will consider expanding inclusion criteria in order to include this important group of workers.
Frontline
We defined 'frontline' as working in any role that brings the person into direct contact (e.g. providing care to) or indirect contact (e.g. managing a team of people who are providing care), or potential contact (e.g. working on the same ward or setting) with a patient with the disease of interest, or where the patient is suspected of having the disease (e.g. displays symptoms but disease not yet confirmed), or is considered to be at high risk of contracting the disease (e.g. working in environments where it is considered necessary for staff to wear PPE), or where the staff member is considered to be at risk of contracting the disease.
We included studies in which there is a mix of different frontline workers, if the majority were health and social care professionals. For example, where an intervention is given to all staff within a particular setting, and these staff include a mix of health and social care professionals and other frontline workers, such as cleaners, porters or receptionists. If possible, we included data from only the subgroup of health and social care professionals, but if these data were not available, we included the mixed frontline worker data and planned to explore the inclusion of this within sensitivity analyses.
We excluded:
studies focused on the mental health and resilience of health and social care professionals, where these people were not working at the front line of disease epidemics or pandemics; and
studies focused on the psychological, mental health, resilience of patients, or a combination of any or all of these.
Types of interventions
We included any intervention that was aimed at addressing mental health or resilience, or both, in the staff identified above. This could include, but was not limited to, the following.
Workplace interventions
Workplace structure and routine interventions, for example, regular breaks, shorter working hours, regular team meetings, mentorship, relaxation or recreation areas in workplaces
Provision of information, guidance, or training, for example, on dealing with difficult situations
Interventions to support basic daily needs
Interventions promoting or supporting healthy lifestyle and self‐care, for example, eating, sleeping, exercising, following a routine, avoiding excess social media, staying in touch with family and friends, engaging in enjoyable activities
Relaxation techniques, for example, progressive muscle relaxation, meditation
Psychological support interventions
Therapist‐delivered psychological interventions, delivered individually or in groups, and face‐to‐face or by text or video call, including professional psychological or counselling support, CBT and psychotherapy
Guided self‐help strategies, such as online CBT, online/web well‐being and sleep apps, and mindfulness programmes. For inclusion, guided interventions had to describe the type of support offered (e.g. telephone, online, video)
Non‐guided self‐help strategies, such as online/computer, audio or book‐based self‐guided interventions (these can also include self‐guided CBT, mindfulness, mediation, and exercises such as writing down worries)
Workplace‐based psychological support strategies, such as peer support networks, employee wellness programmes, and psychological first aid
Pharmacological interventions
Medication for depression, anxiety, sleep other mental disorders, or a combination of any or all of these.
We categorised included interventions using the headings and subgroups listed above, with the addition of new subgroups if necessary. We included multifaceted interventions that comprised a combination of interventions or strategies, including, but not limited to, those listed above.
To address objective 1, within the review of effectiveness we included studies with any comparator intervention. We categorised these as:
no intervention;
standard care;
placebo or attention control intervention; and
other active intervention(s).
We anticipated that it was possible that 'standard care' in some studies could be the same as 'no intervention'. We planned to note this, and combine these studies if it was clear that participants had received no intervention aimed at addressing mental health or resilience.
Types of outcome measures
Objective 1: review of effectiveness
As outlined in Description of the condition, there are a wide range of mental health‐related symptoms that someone may experience, and a range of impacts on the individual and their ability to function effectively within the work environment. The outcomes considered critical to this review included measures of general mental health, as these are anticipated to be of critical importance to frontline health and social care professionals, and measures of resilience as this is a measure of the ability to cope with negative effects of stress or adversity, relates to dysfunction at work, and is considered of key importance to this review, which focused on the effects of anticipated high levels of stress in the workplace. Outcomes critical to this review therefore included the following.
-
General mental health, measured by:
Symptom Checklist 90 Revised (SCL‐90‐R)
General Health Questionnaire (GHQ‐12 or GHQ‐28)
Short Form‐36 questionnaire (SF‐36)
-
Resilience, measured by:
Wagnild and Young Resilience Scale
Connor‐Davidson Resilience Scale (CD‐RISC)
Brief Resilience Scale
Baruth Protective Factors Inventory (BPFI)
Resilience Scale for Adults (RSA)
Brief Resilience Coping Scale (BRCS)
Additional important outcomes included the following.
-
Psychological symptoms of anxiety, depression or stress:
-
anxiety, measured by:
Generalized Anxiety Disorder 7‐Item (GAD‐7)
Self‐Rating Anxiety Scale (SAS)
State‐Trait Anxiety Inventory
Spielberger Trait Anxiety Inventory
Kessler Psychological Distress Scale
Depression, Anxiety and Stress Scale – 21 Items (DASS‐21)
-
depression, measured by:
Patient Health Questionnaire‐9 (PHQ‐9)
Beck Depression Inventory
Center for Epidemiologic Studies Depression Scale (CES‐D)
-
stress, measured by:
Parker and DeCotiis Scale (job‐related stress)
SARS‐Related Stress Reactions Questionnaire
Perceived Stress Scale (PSS‐10)
-
-
Burnout, measured by:
Oldenburg Burnout Inventory (OLBI)
Maslach Burnout Inventory questionnaire (MBIQ)
Effects on workplace staffing, measured by:
absenteeism/presenteeism
staff retention/turnover
Mental health disorders caused by distressing events, measured by:
post‐traumatic stress disorder (PTSD) – Stanford Acute Stress Reaction (SASR)
Impact of Event Scale (IES, IES‐R)
Davidson Trauma Scale
Vicarious Traumatization Questionnaire
PTSD Checklist‐Civilian Version (PCL‐C)
Chinese Impact of Event Scale—Revised (CIES–R)
Harm, adverse events or unintended consequences arising from the interventions
We noted where studies report costs; referrals, for example to mental health team; or alcohol or substance use.
We included other tools that assess these domains where those named specifically in the list above were not measured.
We did not use measuring or reporting of outcomes within studies as a criterion for inclusion within the review.
We were interested in outcomes that were recorded at the end of the intervention period ('immediate' time point) and outcomes recorded at a 'follow‐up' time point. If possible, we planned to categorise follow‐up outcomes as short‐term (< 3 to 6 months), medium‐term (> 6 to 12 months) and longer‐term (> 12 months) follow‐up.
Objective 2: qualitative evidence synthesis
To be included, qualitative studies had to report findings relating to barriers and facilitators to the implementation of interventions aimed at improving the resilience and mental health of frontline health and social care professionals. We defined a barrier as any factor that may impede the delivery of an intervention. We defined a facilitator as any factor that contributes to the implementation of an intervention (Bach‐Mortensen 2018).
Search methods for identification of studies
We used one search strategy for identifying studies eligible for a broader review on this topic (New Reference), and for identifying studies relevant to each of the objectives addressed by this Cochrane Review.
Electronic searches
An information specialist (JDC) developed a comprehensive search strategy for MEDLINE (Appendix 1), combining uncontrolled vocabulary terms and MeSH for (a) resilience and mental health interventions AND (b) health and social care personnel AND (c) pandemics, epidemics and health outbreaks; this has been peer reviewed in accordance with PRESS guidelines (McGowan 2016). We adapted and ran the search for each of the following major electronic databases on 28 May 2020.
MEDLINE Ovid (from 1946 to 28 May 2020; Appendix 1).
Cochrane Database of Systematic Reviews (CDSR) and Cochrane Central Register of Controlled Trials (CENTRAL; 2020 Issue 5) in the Cochrane Library (Appendix 2)
Embase Ovid (from 1974 to 28 May 2020; Appendix 3)
Several indexes in Web of Science: Web of Science Indexes (Science Citation Index Expanded (SCIEXPANDED), Social Sciences Citation Index (SSCI), Conference Proceedings Citation Index‐ Science (CPCI‐S), Conference Proceedings Citation Index‐ Social Science & Humanities (CPCI‐SSH); Appendix 4).
PsycINFO Ovid (from 1806 to 28 May 2020; Appendix 5).
CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature; from 1982 to 28 May 2020; Appendix 6).
Global Index Medicus databases (www.globalindexmedicus.net/; Appendix 7).
WHO Library Database (WHO IRIS (Institutional Repository for Information Sharing, apps.who.int/iris) last searched 28 May 2020; Appendix 8).
We ran searches from the year 2002 onwards, with no language restrictions.
Searching other resources
We also conducted systematic supplementary searches (last search date 28 May 2020) to identify other potentially relevant studies including:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov; Appendix 9);
Google Scholar (first 250 relevant entries) via 2Dsearch (www.2dsearch.com/; Appendix 10).
We attempted to search the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/en; Appendix 11), but were unable to complete this (see Differences between protocol and review).
Where our searching identified relevant systematic reviews or qualitative evidence synthesis we handsearched the list of included studies. Due to the rapid nature of this review, we did not conduct additional handsearching. This included handsearching of reference lists of included studies and forward citation searching. These should be considered for future updates of this review.
Data collection and analysis
The methods for conducting and reporting this review followed the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2020a), the Handbook for Synthesizing Qualitative Research (Sandelowski 2007), and guidance from the Cochrane Qualitative and Implementation Methods Group (CQIMG, Noyes 2020), CQIMG supplemental methods papers (Noyes 2018), and Cochrane Effective Practice and Organisation of Care (EPOC; EPOC 2019).
Selection of studies
One review author ran the targeted searches and excluded any obviously irrelevant titles and abstracts. Pairs of review authors independently applied selection criteria to abstracts; this stage was managed in Covidence. Pairs of review authors independently applied the selection criteria to the full papers, and 'tagged’ included studies as relevant to the Cochrane Review. Disagreements between review authors were resolved through discussion, involving a third review author.
Objective 1: review of effectiveness
We did not impose any restrictions according to language. Where titles and abstracts were in languages other than English, we used Google‐Translate to enable screening. Where studies published in languages other than English were considered at the full‐paper stage, we involved a review author or advisory group member with appropriate language skills. The review authors and advisory group are fluent in a wide range of languages (including Arabic, Bengali, French, German, Hindi, Italian, Marathi, Portuguese, Spanish). If necessary, we planned that selection criteria would be applied by one review author, with a second review author checking the translated text of included studies.
Objective 2: qualitative evidence synthesis
Studies included in the qualitative evidence synthesis were limited to those published in English, due to the potential problems associated with translations of concepts across different languages, and the rapid nature of this planned synthesis and need for additional resources if studies in languages other than those that the review author team are proficient in are to be included in qualitative synthesis (Downe 2019). Studies in languages other than English that otherwise meet the criteria for inclusion in the qualitative evidence synthesis were placed in 'studies awaiting assessment', and should be considered for inclusion in future updates of this review.
Ongoing, unpublished and preprint papers
Any studies that met the eligibility criteria, but that are still ongoing, or for which no results data are yet available, we listed as an 'ongoing' study. Reports of studies that were available as unpublished studies or preprint publications (not yet peer‐reviewed) were treated as included studies, but the publication status was noted and we planned to explore the effect of inclusion using sensitivity analysis.
Reporting of search results
We reported search results using PRISMA (Moher 2009).
Where there was a potentially relevant abstract, but we were unable to find a full paper, we listed this as a 'study awaiting assessment'. Where there was a relevant abstract for which there was no full paper, for example a conference abstract, we planned to include this study and attempt to contact study authors to obtain further data.
We listed any studies excluded at the full‐paper stage in a table of excluded studies, and provided reasons for exclusion.
Data extraction and management
We brought together multiple reports of the same study at data extraction and considered all publications related to that study. Where there was conflicting information between different reports of the same study, we planned to base our extraction on the designated 'main' publication. Where there was a protocol and also a report of a completed study, we designated the report of the completed study as the 'main' publication, referring to both for data extraction but using the main publication if there was conflicting information relating to a study.
Objective 1: review of effectiveness
One review author (AP) systematically extracted data from all papers using a predeveloped data extraction form, within Microsoft Excel. We planned to pilot the extraction form on at least five studies prior to use, but this was not done as we only identified one study. All data extraction was cross‐checked by a second review author (AE), and any disagreements resolved through discussion.
We extracted and categorised data on the following items.
Year
Study design
Aim
Inclusion criteria
Geographical setting (countries)
Epidemic/pandemic ‐ disease, phase of disease outbreak (during outbreak/de‐escalation)
Setting (hospital, care home, community, etc.)
Participant characteristics – number of participants/dropouts, demographic variables of included participants, type (profession) of staff. We will categorise participant populations using the list above (see Types of participants), with additional categories if required. We will note when participants are people who returned to practice or were students who entered a professional role early
Intervention characteristics – described using TIDieR framework (Hoffmann 2014). We will categorise interventions according to whether the intervention involves changes at the level of individual staff members, groups of staff members (e.g. teams), an organisation (e.g. at the hospital level), or policy (e.g. National Health System (NHS) or government policy)
Comparator characteristics
Assessed outcomes
Baseline and follow‐up results data (mean and standard deviation, or other summary statistics as appropriate) for relevant outcomes. We will extract data for an 'immediate' time point – recorded at the end of the intervention period; and for a 'follow‐up' time point. Where multiple follow‐up time points are available we will extract data that reflect the following time points: short‐term (< 3 to 6 months), medium‐term (> 6 to 12 months) and longer‐term (> 12 months).
Analysis: presented analysis/es
For non‐randomised studies we planned to extract data on intervention effects, levels of precision and confounders adjusted for. We planned to document whether the following potentially confounding factors were controlled for: setting that the healthcare professional is working in, the type and grade of healthcare professional, and the length of time that the individual has worked within the disease epidemic or pandemic, gender and socioeconomic status.
Objective 2: qualitative evidence synthesis
One review author (PC) systematically extracted data from all papers using a predeveloped data extraction form, within Microsoft Excel. This was cross‐checked by a second review author (JC), and any disagreements were resolved through discussion, involving a third review author (AP) if necessary.
We extracted and categorised data on the following items.
Year
Study design
Aim
Geographical setting (countries)
Epidemic/pandemic ‐ disease, phase of disease outbreak (during outbreak/de‐escalation)
Type (profession) of staff and length of time in the profession
Whether staff have previous experience of working in the front line during an epidemic/pandemic
Details of who the frontline staff were providing care for
Type of interventions implemented
Study fidelity with a specific focus on whether the interventions were tailored or modified, or both, in different contexts
Details of any adverse events or unintended consequences
Barriers and facilitators to implementation (direct quotes)
Sampling of studies
Qualitative evidence synthesis aims for variation in concepts rather than an exhaustive sample, and large amounts of study data can impair the quality of the analysis. Once we had identified all studies that were eligible for inclusion, we assessed whether their number or data richness was likely to represent a problem for the analysis, and whether we should consider selecting a sample of studies (EPOC 2017b). Due to the relatively low number of included studies, discussion amongst review authors (PC, JC, AP) led to the decision not to select a sample of studies, but instead to extract data from all included studies.
Qualitative data management
One review author (PC or JC) extracted and coded data identified as a barrier or facilitator to the implementation of interventions (author, year, country, direct quotes, page numbers) verbatim, which a second review author (PC or JC) independently checked. We resolved any ambiguity identified through discussion with other members of the review team.
We used the best fit framework synthesis approach, which combines deductive and inductive thematic approaches to identifying barriers and facilitators (Carroll 2011). The first step involved a deductive approach, employing a predefined list of 39 constructs, grouped into five domains, from the Consolidated Framework for Implementation Research guide (CFIR 2020), see Table 4. We coded data against this framework. The second step involved an inductive approach to develop themes and subthemes from data that could not be categorised using the predefined codes.
2. Consolidated Framework for Implementation Research (CFIR) constructs.
| Domain | Constructsa |
| Intervention characteristics | Intervention source |
| Evidence strength and quality | |
| Relative advantage | |
| Adaptability | |
| Trialability | |
| Complexity | |
| Design quality and packaging | |
| Cost | |
| Outer settings | Patient needs and resources |
| Cosmopolitanism | |
| Peer pressure | |
| External policy and incentives | |
| Inner setting | Structural characteristics |
| Networks and communications | |
| Culture | |
| Implementation climate | |
| Tension for change | |
| Compatibility | |
| Relative priority | |
| Organisational incentives and rewards | |
| Goals and feedback | |
| Learning climate | |
| Readiness for implementation | |
| Leadership engagement | |
| Available resources | |
| Access to knowledge and information | |
| Characteristics of individuals | Knowledge and beliefs about the intervention |
| Self‐efficacy | |
| Individual stage of change | |
| Individual identification with organisation | |
| Other personal attributes | |
| Process | Planning |
| Engaging | |
| Opinion leaders | |
| Formally appointed internal implementation leaders | |
| Champions | |
| External change agents | |
| Executing | |
| Reflecting and evaluating |
aFrom CFIR 2020. For descriptions of each construct, see www.cfirguide.org/constructs.
Assessment of risk of bias in included studies
Objective 1: review of effectiveness
We used the Cochrane 'Risk of bias' tool for randomised trials (Higgins 2017). Two review authors (AP and AE) independently completed assessments, with disagreements resolved through discussion.
Had we included any non‐randomised studies, we had planned to use ROBINS‐I tool for non‐randomised studies of interventions (Sterne 2016), following the guidance in Chapter 25 of the Cochrane Handbook for Systematic Reviews of Interventions, and in section 25.5 for assessing the risk of bias in interrupted time series studies (Sterne 2020).
Assessment of methodological limitations
Objective 2: qualitative evidence synthesis
One review author (AP) assessed methodological limitations, using the tool relevant to the type of individual study (see below). A second review author (PC) checked all assessments, and any disagreements were resolved through discussion.
Qualitative studies
We used the Critical Appraisal Skills Programme (CASP) for qualitative studies to assess the methodological limitations of studies with a qualitative design (CASP 2018). We answered each of the questions from Section A and B of the tool (i.e. questions 1 to 9), giving a response of 'yes', 'no' or 'cannot tell'. We considered the 'hints' listed within the tool, and we noted our reasons for each response. We also made a judgement on the overall assessment of the limitations of the study as follows:
where the assessments for most items in the tool were 'yes' ‐ no or few limitations;
where the assessments for most items in the tool were 'yes' or 'cannot tell' ‐ minor limitations;
where the assessments for one or more questions in the tool were 'no' ‐ major limitations.
Descriptive studies
We used the WEIRD (Ways of Evaluating Important and Relevant Data) tool to assess the methodological limitations of descriptive studies (Lewin 2019). We answered each of the questions from the tool, giving a response of 'yes', 'no' or 'unclear', with consideration of the subquestions for each criterion. We combined question 5 ("Is the information accurate (source materials other than empirical studies)?" and question 6 ("Is the information accurate (empirical studies only)?") into one question ("5/6 Is the information accurate? (non‐empirical/empirical studies)"). We noted our justification for each assessment. Based on our assessment for each tool item, we made a judgement on the overall assessment of the limitations of the source as follows:
where the assessments for most items in the tool were 'yes' ‐ no or few limitations;
where the assessments for most items in the tool were 'yes' or 'unclear' ‐ minor limitations;
where the assessments for one or more questions in the tool were 'no' ‐ major limitations.
Measures of treatment effect
Objective 1: review of effectiveness
We planned to carry out meta‐analyses of pairwise comparisons for outcomes where direct evidence was available. We planned to estimate pooled effect sizes (with 95% confidence intervals (CI)) using data from individual arms of included studies, and to estimate risk ratios for binary outcomes and mean differences for continuous outcomes (or standardised mean differences if different studies used different measures of the same outcomes). We would have meta‐analysed complex study designs (multi‐arm, cluster and cross‐over) following established guidance (Higgins 2020b).
We planned to conduct the synthesis of non‐randomised studies according to the guidance in Chapter 24 of the Cochrane Handbook for Systematic Reviews of Interventions (Reeves 2020). Where possible, we would meta‐analyse adjusted effect sizes. We planned to meta‐analyse randomised and non‐randomised studies separately.
For outcomes relating to effects on workplace staffing, we planned only to conduct meta‐analysis where we would analyse this as dichotomous data. For example, using data for the proportion of participants who have a period of absenteeism during the intervention period, those who are absent at the end of the intervention period, and/or those who have a period of absenteeism before stated follow‐up assessment points. If time‐to‐event data were presented (e.g. for absenteeism) we planned to only include these if we could convert these and analyse as dichotomous data. If count data were presented (e.g. number of periods of absenteeism) we planned not to include these unless we could determine the number of participants to whom these data relate (e.g. the number of participants who had at least one period of absenteeism).
Unit of analysis issues
For the quantitative evidence synthesis, where studies had two or more active intervention groups eligible for inclusion within the same comparison (against a control, placebo, or no‐treatment group), we intended to 'share' the control group data between the multiple pair‐wise comparisons in order to avoid double‐counting of participants within an analysis. Where we included studies that used a cluster‐randomised design, we planned to treat the group (or cluster) as the unit of allocation, and follow methods for analysis of cluster‐randomised trials as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2020b), with advice from a statistician (AE).
Dealing with missing data
For the quantitative evidence synthesis: where studies appeared to have measured outcome data that are relevant to our critical outcomes of general mental health and resilience, but these are missing from identified reports, we planned to contact study authors by email. This included requests where the study report did not provide means or standard deviations (or data from which these can be calculated by the review authors). Where we did not obtain the missing data, or where there were missing data relating to other outcomes, we intended to highlight this within our narrative synthesis. We intended to only analyse available data and did not plan to input missing data with replacement values.
For the qualitative evidence synthesis, where studies appeared to have missing data we noted this, but did not contact study authors due to the rapid nature of this review.
Assessment of heterogeneity
Within the quantitative evidence synthesis, we planned to assess heterogeneity by visually inspecting forest plots and assessing I2 statistics (Higgins 2003), with random‐effects models used to address potential heterogeneity. We intended to consider an I² value of more than 50% to indicate substantial heterogeneity.
Assessment of reporting biases
As this is a rapid review, we did not use any formal methods to assess the risk of reporting biases.
Data synthesis
Objective 1: review of effectiveness
We planned to conduct pairwise meta‐analyses using Review Manager 2020 for all primary and secondary outcomes listed above, for comparisons of:
intervention versus no intervention
intervention versus standard care
intervention versus placebo or attention control
and for outcomes measures:
immediately after the end of intervention
at follow‐up. If data are available, we will present data for short‐term (< 3 to 6 months), medium‐term (> 6 to 12 months) and longer‐term (> 12 months) follow‐up.
We did not plan to conduct any meta‐analyses for comparisons of one active intervention with another intervention.
We planned to summarise and tabulate important clinical and methodological characteristics of all included studies (including randomised and non‐randomised studies). Where study results were pooled within meta‐analysis, we intended to judge our certainty in each pooled outcome using the GRADE approach (Schünemann 2020). We created a 'Summary of findings' table for the comparison of 'intervention versus no intervention'. We did not create planned 'Summary of findings' tables for 'intervention versus standard care' or 'intervention versus placebo or attention control', as we included no studies with this comparison. Our 'Summary of findings' table includes results relating to the following outcomes.
General mental health
Resilience
Anxiety
Depression
Stress
Burnout
Absenteeism
We planned to include in the 'Summary of findings' table, results measured immediately at the end of the intervention and at one‐year follow‐up (if data were available).
We planned to structure our main narrative summary of findings first by the intervention, using the predefined broad intervention headings listed under Types of interventions, second by comparison group, and third by outcome. Within the narrative we intended to refer to the study participants, and to areas of similarity or differences (clinical heterogeneity) between the studies. For the included study, for which there were no data suitable for inclusion in meta‐analysis, we provided a brief table summarising results reported by the study, and referred to these tabulated data within a narrative synthesis. Had we had suitable data, we had planned to comment on whether there were agreements or disagreements between our meta‐analysis and studies not included in meta‐analysis, with reference to the risk of bias of studies.
For any outcomes not included in the 'Summary of findings' table, we planned to provide a brief narrative synthesis of key findings. We also planned to provide a brief narrative synthesis of key findings of studies that had comparisons of one active intervention with another active intervention. We followed the Synthesis Without Meta‐analysis (SWiM) in systematic reviews reporting guideline (Campbell 2020).
Objective 2: qualitative evidence synthesis
We brought evidence relating to barriers and facilitators together using a narrative synthesis supported by Summary of Qualitative Findings (SoQF) tables and figures organised around the five major domains that may influence an intervention’s implementation, as reported in the Consolidated Framework of Implementation Research (CFIR 2020). These five factors included:
intervention characteristics;
outer settings (i.e. environmental factors);
inner settings (i.e. organisational factors);
individual characteristics;
implementation process characteristics.
We used the GRADE‐CERQual approach to assess our confidence in each finding (Lewin 2018), reaching agreement through discussion. GRADE‐CERQual assesses confidence in the evidence, based on the following four key components.
Methodological limitations of included studies: the extent to which there are concerns about the design or conduct of the primary studies that contributed evidence to an individual review finding. For this component we considered the assessment of methodological limitations, using the CASP or WEIRD tool, for each study that contributed to a review finding. We considered whether the inclusion of evidence from studies judged to have minor or major limitations reduced our confidence in the findings, and recorded these decisions within our evidence profiles.
Coherence of the review finding: an assessment of how clear and cogent the fit is between the data from the primary studies and a review finding that synthesises those data. By cogent, we mean well supported or compelling.
Adequacy of the data contributing to a review finding: an overall determination of the degree of richness and quantity of data supporting a review finding.
Relevance of the included studies to the review question: the extent to which the body of evidence from the primary studies supporting a review finding is applicable to the context (perspective or population, phenomenon of interest, setting) specified in the review question.
After assessing each of the four components, we made a judgement about the overall confidence in the evidence supporting the review finding. We judged confidence as 'high', 'moderate', 'low', or 'very low'. The final assessment was based on consensus among the review authors. All findings started as high confidence and we then downgraded the findings if we had important concerns regarding any of the GRADE‐CERQual components.
Overarching synthesis
We planned to produce a brief narrative synthesis that brings the findings from the quantitative and qualitative syntheses together, but due to lack of evidence from the quantitative synthesis we did not complete the planned formal overarching synthesis (see Differences between protocol and review).
Subgroup analysis and investigation of heterogeneity
Had we conducted the planned quantitative evidence synthesis: we would have explored differences between subgroups based on the following.
Type of intervention (including whether intervention is targeted at individual/group/organisation/policy)
Duration of intervention delivery (one‐off, < 3 months, 3 to 6 months, > 6 months)
Disease (type of disease and specific epidemic/pandemic, and mode of disease transmission (direct/indirect))
Geographical location (countries)
Type of staff (profession)
Sensitivity analysis
Objective 1: review of effectiveness
Had we conducted the planned quantitative evidence analyses, we would have explored the effect on results of excluding non‐randomised studies. In addition, for analyses of our primary outcomes, we would have explored the effect on results if only evidence from studies judged to be at low risk of bias (on all assessed domains) had been included within the analyses.
Objective 2: qualitative evidence synthesis
We considered how each study's methodological limitations may affect our review findings (Noyes 2020; Appendix 12).
Results
Description of studies
Results of the search
Results of the search are summarised in Figure 1. We considered 3315 abstracts, and applied inclusion criteria to 137 full texts. We excluded 111 papers: 41 as they did not meet our criteria (see Characteristics of excluded studies); 38 as they were systematic reviews and therefore did not meet our inclusion criteria; and there was insufficient information to determine inclusion for 32 studies and these were classed as 'awaiting classification', and further information is being sought from study authors (see Characteristics of studies awaiting classification). This left 26 papers that met our criteria for inclusion; 16 studies (23 papers) of these were completed studies and three are ongoing studies.
1.
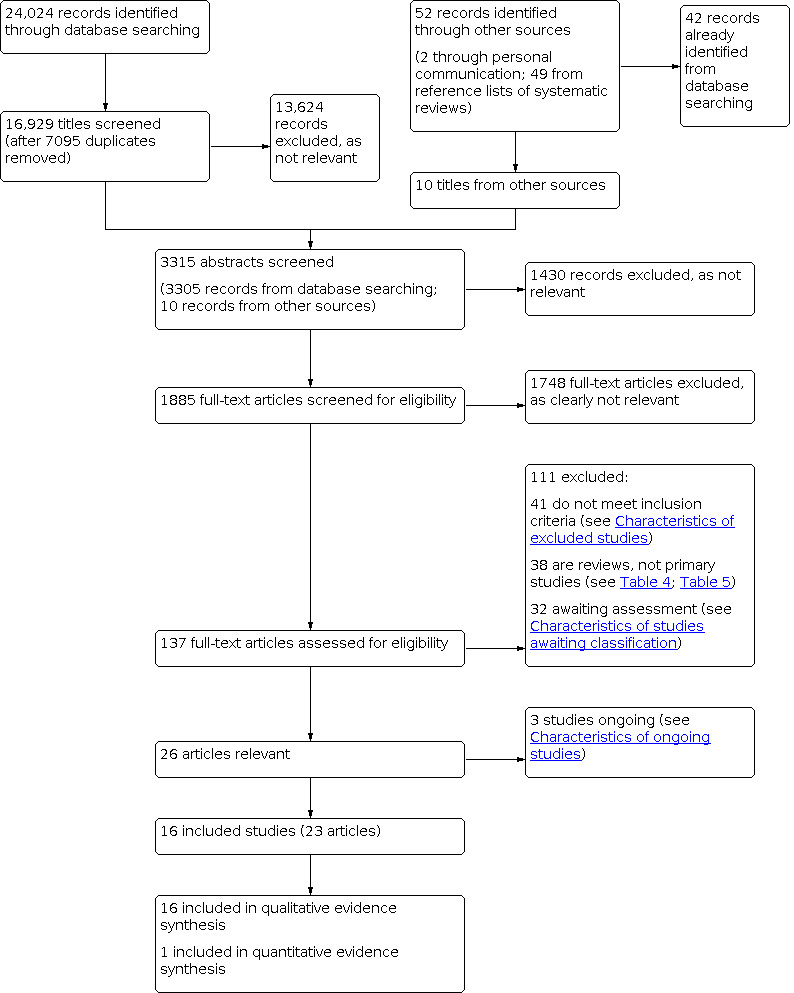
Study flow diagram
Included studies
We included 16 studies (Belfroid 2018; Blake 2020; Brown‐Johnson 2020; Cao 2020; Carvalho 2019; Chang 2006; Chen 2020; Cheung 2015; Cunningham 2017; De Jong 2019; Ferranti 2016; Klomp 2020; Lee 2005; Schreiber 2019; Son 2019; Waterman 2018).
Objective 1: review of effectiveness
One of the 16 studies that met our criteria for inclusion in the review of effectiveness (De Jong 2019). De Jong 2019 was a mixed methods study comprising both a qualitative (interview) study and a cluster‐randomised trial. The evidence from the randomised trial was eligible for inclusion in the review of effectiveness. This randomised trial had the following key features (further details are in Characteristics of included studies).
Participants
From 129 randomised ‘peripheral health units’ (the clusters), 408 participants were recruited. Participants (intervention and control group, respectively) comprised nurses (35.4% and 44.1%), community health workers (9.7% and 5.9%), midwives (7.3% and 7.9%), maternal health assistants (38.8% and 36.1%), and other (vaccinator, laboratory assistant etc.; 8.7% and 5.9%). There were more women than men (80.5% and 87.1%).
Participants were staff members from 'peripheral health units' in Sierra Leone, and were recruited in 2017. This study occurred after the 2014 to 2016 Ebola epidemic in Sierra Leone.
Intervention
The intervention was considered to be a workplace intervention, as it comprised a training session ‐ psychological first aid training ‐ aimed at providing staff members with the skills to help people in post‐Ebola Sierra Leone. The control group received no intervention during the period of the study (but did receive the intervention after the end of the study period, i.e. was a ‘waiting list’ control).
Outcomes
This study assessed only one outcome relevant to this review, measured using questions from the Professional Quality of Life Scale (ProQOL‐5), which we considered to be relevant to our outcome of burnout (see section of Assessment of risk of bias in included studies for further details of this outcome).
Objective 2: qualitative evidence synthesis
We classified the following 7 out of 16 studies as qualitative studies.
Study design
Six of these had a qualitative study design: Belfroid 2018, Chen 2020, Cunningham 2017 and De Jong 2019* conducted interviews; Lee 2005 conducted focus groups (and administered a survey that was developed based on focus groups' results); and Son 2019 collected qualitative data in the form of "short anonymous notes" that were thematically analysed.
Cao 2020 had a mixed method design, reporting results from quantitative questionnaires and qualitative interviews assessed after a period of work when participants had access to the intervention, but from which only data from the qualitative component were used within the evidence synthesis.
We classified the following nine out of 16 studies as descriptive studies.
Waterman 2018 had a mixed method design, describing the implementation and evaluation of an intervention, including a qualitative interview component and a cohort study where outcome assessment was recorded before and after an intervention. However, the data extracted and used for the qualitative evidence synthesis was descriptive, rather than coming directly from the analysis or synthesis of the qualitative or quantitative data.
Five of these studies described the implementation or evaluation of an intervention, or both: Blake 2020 and Ferranti 2016 described the development, implementation and evaluation of an intervention; Brown‐Johnson 2020 briefly described the implementation and evaluation of an intervention; Klomp 2020 described the implementation and evaluation of a range of different training programmes; and Schreiber 2019 described the implementation of an intervention programme.
Cheung 2015 was a commentary relating to an intervention: provided a personal account of an aid worker, including views and experiences relating to psychosocial support.
Carvalho 2019 and Chang 2006 had quantitative study designs, but included some descriptive data relevant to our review question. Carvalho 2019 was a cohort study in which participants were assessed before and after an intervention; the design of this study did not meet our criteria for inclusion in the review of effectiveness, and the presented results comprised quantitative data from self‐assessment questionnaires. However, the quantitative study results were followed by a discussion that explored participants' reasons for questionnaire responses and this descriptive information was relevant to our qualitative evidence synthesis (for example, there is a discussion around what factors relating to the intervention may have enhanced participants' confidence). Chang 2006 conducted a survey that aimed to examine components of an intervention and links with mental health outcomes; this study design did not meet our criteria for inclusion in the review of effectiveness, with the presented results comprising quantitative data, including analyses to explore the relationship between different domains (specifically the "relationship between social capital and emotional exhaustion and job tension"). However, following the presentation of results data there was a discussion aimed at exploring potential reasons for the identified relationships, and this included a descriptive exploration of potential barriers and facilitators to reduced emotional exhaustion and job tension (for example, there are discussions around workplace communication, workplace design, and encouragement and incentives to engage workers). The review authors discussed both of these quantitative studies in detail and reached consensus that the descriptive data within the discussion were relevant to the qualitative evidence synthesis.
*Note that while De Jong 2019 had a mixed method design, incorporating a randomised trial and qualitative interviews, we only used data from the qualitative interviews within the qualitative evidence synthesis, and we therefore classify it here as having a qualitative study design.
Participants
Details of the study participants are provided in the Characteristics of included studies.
Thirteen of the 16 studies clearly reported the number of participants. There were a total of 1268 participants, with studies ranging from 13 to 253 participants. The number of participants included in two studies was unclear or not reported (Brown‐Johnson 2020; Klomp 2020). One study was a field report based on the experiences of the one study author (Cheung 2015).
The majority included a mix of different healthcare professionals (sometimes including students), of whom most were generally doctors or nurses (Belfroid 2018; Blake 2020; Brown‐Johnson 2020; Cao 2020; Chang 2006; Cunningham 2017; Waterman 2018). De Jong 2019 included a range of healthcare professionals (nurses, midwives, mental health clinicians, social workers) and people in other roles (e.g. volunteers, burial teams, administrators, technicians, teachers, caregivers). Carvalho 2019 included a range of different healthcare professionals and also non‐professionals (e.g. cleaning and security staff). Lee 2005 only included nurses, and Ferranti 2016 only included undergraduate nursing students. The type of healthcare staff was unclear or not reported in Chen 2020, Klomp 2020, Schreiber 2019 and Son 2019. In Cheung 2015 the study author was an international aid worker, reflecting on staff who were "frontline local and overseas workers".
Disease, year and country
Severe acute respiratory syndrome (SARS) 2003
Two studies focused on the 2003 outbreak of SARS in Taiwan (Chang 2006; Lee 2005).
Ebola virus disease 2014 to 2016
Nine studies focused on the 2014 to 2016 outbreak of Ebola virus disease (Belfroid 2018; Carvalho 2019; Cheung 2015; Cunningham 2017; De Jong 2019; Ferranti 2016; Klomp 2020; Schreiber 2019; Waterman 2018). However, although focused on this outbreak, Klomp 2020 refers to data from 2009 onwards. The intervention delivered by Waterman 2018 continued after the country in which it was being implemented was declared Ebola‐free.
Studies were carried out in Liberia (Cheung 2015), Netherlands (Belfroid 2018), Sierra Leone (Waterman 2018), Spain (Carvalho 2019), USA (Ferranti 2016; Klomp 2020), and West Africa (Schreiber 2019). de Jong 2019 recruited from both Liberia and Sierra Leone. Cunningham 2017 recruited participants from Canada and the USA who had worked with Ebola patients in Guinea, Liberia and Sierra Leone.
Middle East respiratory syndrome (MERS) 2015
One study focused on the 2015 outbreak of MERS in South Korea (Son 2019).
COVID‐19 December 2019 to April 2020 pandemic
Four studies focused on the COVID‐19 pandemic, conducted between January and April 2020 (Blake 2020; Brown‐Johnson 2020; Cao 2020; Chen 2020).
Cao 2020 and Chen 2020 were conducted in China; Blake 2020 in the UK; Brown‐Johnson 2020 in the USA.
Interventions
Workplace interventions
We considered six of the studies to deliver 'workplace interventions'.
One study focused on a multifaceted workplace intervention, which comprised some components relating to workplace structure and routine interventions, and some components relating to training (Belfroid 2018).
In three studies the intervention was a training course. In two studies this was largely designed to prepare people for working in a disease epidemic or pandemic (Carvalho 2019; Ferranti 2016). The training provided by Ferranti 2016 was designed to increase knowledge, rather than specifically address mental health outcomes, although the impact on "concern" and "confidence" was measured. In one study the training was 'psychological first aid training', designed to help workers have the skills and knowledge to help people who had been adversely affected by Ebola (De Jong 2019).
In one study the intervention was the use of "PPE portraits", aimed at "humanising" patient care (Brown‐Johnson 2020).
In one study the intervention was "social capital", which was defined as relating to social interaction and trust (Chang 2006). The study authors argue that, as an intervention, "social capital would aid medical organizations in managing crises such as SARS" and describe administrative procedures such as designing workplaces to encourage social interaction and "adopting hiring procedures to ensure new employees add social capital to the organization".
Interventions to support basic daily needs
No studies focused specifically on interventions to support basic daily needs.
Psychological support interventions
We considered eight studies to focus on 'psychological support interventions'. Cao 2020 provided access to a 'hotline service' aimed at providing psychological support; Chen 2020 provided access to online courses, a 'hotline' service and group activities aimed at releasing stress; Cheung 2015 described a range of different psychosocial support interventions; Lee 2005 provided a range of psychiatric interventions, including debriefing groups, a 'hotline' counselling service and individual psychotherapy; Schreiber 2019 investigated the 'Anticipate, Plan and Deter Responder Risk and Resilience model'; Son 2019 described "a special program for their employees to share what they were emotionally experiencing and issues that troubled them", which was held in the workplace, led by trained department heads; and Waterman 2018 was focused on cognitive behavioural therapy (CBT). Cunningham 2017 explored the use of 'narrative medicine' as a psychological support intervention in which creative means, such as writing down thoughts or using the visual arts to express experiences, are used by frontline workers to help them understand their experiences; use of this strategy appears to have relied solely on the initiative of individual participants, and there was no 'delivery' of this intervention.
We considered five of these eight psychological support interventions to incorporate 'therapist‐delivered psychological interventions' (Cao 2020; Chen 2020; Cheung 2015; Lee 2005; Waterman 2018), but all were delivered as part of a workplace‐based strategy. We considered the interventions by Son 2019 and Schreiber 2019 to be workplace‐based strategies; and we considered that of Cunningham 2017 to be a non‐guided self‐help strategy.
Pharmacological interventions
No studies focused on pharmacological interventions.
Multifaceted interventions
Two studies focused on a multifaceted intervention. Blake 2020 implemented a digital learning package, described as a "a comprehensive package to support psychological well‐being", which included components relating to the workplace, basic daily needs and psychological support interventions. Klomp 2020 delivered a multicomponent training package that included pre‐ and post‐deployment initiatives (before/after deployment to work within the Ebola outbreak in West Africa), training and screening.
Ongoing studies
We identified three ongoing studies (for details see Characteristics of ongoing studies). All of these are focused on frontline workers during the COVID‐19 pandemic. Two are randomised trials: one is investigating a work‐based intervention ('peer champion support', NCT04373382), and one a psychological support intervention (CBT, NCT04362358). One is an observational (non‐comparative) study investigating a dietary supplement (Ayurvedic kadha, NCT04387643).
Studies awaiting classification
Thirty‐two studies are awaiting classification (for details see Characteristics of studies awaiting classification). Twenty are ongoing studies being carried out during the COVID‐19 pandemic, or studies referred to within commentaries or other papers, for which we currently have insufficient information to determine whether they meet our inclusion criteria (Albott 2020; NCT04379063; Banerjee 2020a; Benzarti 2020; NCT04363671; Cheng 2020; NCT04389476; Chung 2020; Cole 2020; Goh 2020; Jiang 2020; Li 2020; NCT04377165; Schulte 2020; Shen 2020a; NCT04367857; NCT04379336; Xiao 2020; Yau 2020; Zhang 2020); nine are completed studies, from disease outbreaks other than COVID‐19, for which we have identified abstracts, or limited information, only, and are seeking further information from study authors (Brusin 2003; ChiCTR‐TRC‐11001268; Fu 2004; James 2020; Khee 2004; Masumbuko 2020; Mehtar 2016; Saul 2016; Siddle 2016); and three require translation (Casado‐Mejia 2016; Keita 2017; Liu 2015).
Excluded studies
Reasons for exclusion of 41 studies are described in Characteristics of excluded studies. There was considerable discussion around the eligibility of 19 of these studies as they did briefly describe an intervention aimed at supporting the mental health or resilience of frontline healthcare professionals during a disease epidemic or pandemic. However, whilst a brief description of an intervention was provided, we judged that there were no relevant data relating to implementation (specifically barriers and facilitators to implementation) and so we excluded these studies. However, we have extracted a list of interventions reported in these studies (see Table 5).
3. Candidate interventions and strategies to support resilience and mental health reported in excluded studies.
| Interventions | |||||
| Author (year) | Workplace | Support basic daily needs | Psychological | Pharmacological | Other |
| Banerjee 2020 | ‐ |
|
|
‐ |
|
| Barrett 2020 | ‐ | ‐ | ‐ | ‐ |
(ucd.ie/medicine/capsych/mindreading) |
| Behan 2020 | ‐ | ‐ |
|
‐ | ‐ |
| Bohan 2020 | ‐ | ‐ |
|
‐ |
|
| Booth 2005 | ‐ | ‐ |
|
‐ |
|
| Chou 2010 |
|
|
|
‐ |
|
| Fukuti 2020 |
|
|
|
‐ |
|
| Greenberg 2015 |
|
‐ |
|
|
‐ |
| Liu 2020 |
|
‐ |
|
‐ |
|
| Meyer 2018 |
|
‐ |
|
‐ |
|
| Singh 2020 | ‐ |
|
|
|
‐ |
| Sprang 2015 |
|
‐ | ‐ | ‐ | ‐ |
| Taylor 2019 | ‐ | ‐ |
|
‐ |
|
| Vymetal 2011 |
|
‐ |
|
‐ |
|
| Wald 2020 |
|
|
|
‐ | ‐ |
| WHO 2014b |
|
|
|
‐ | ‐ |
| WHO 2020b |
|
|
|
|
|
| WHO 2020d |
|
‐ | ‐ | ‐ | ‐ |
| Yuen‐Tsang 2004 | ‐ | ‐ | ‐ | ‐ |
|
| CBT: cognitive behavioural therapy; CBTi: cognitive behavioural therapy for insomnia; EMDR: eye movement desensitisation and reprocessing; HCW: healthcare workers; HSCWs: health and social care workers; MBCT: mindfulness‐based cognitive therapy; MBSR: mindfulness‐based stress reduction; OT: occupation therapy; OTC: over the counter; PC: palliative care; PFA: psychological first aid; PPE: personal protective equipment; TRiM: Trauma Risk Management programme | |||||
Excluded reviews
We considered 38 of the excluded studies to be reviews of primary studies; 15 of these did not clearly report systematic review methods (listed in Table 6 as 'narrative literature reviews'); 14 reported systematic review methods, but did not aim to investigate the effectiveness of interventions to support mental health or resilience of frontline workers (listed in Table 6). The remaining nine reported systematic review methods and aimed (at least in part) to investigate the effectiveness of interventions to support mental health or resilience of frontline workers (listed in Table 7). We noted three systematic reviews to have similar aims, inclusion criteria and search dates to this Cochrane Review (Cabello 2020; Robertson 2020; Stuijfzand 2020), although all are described as 'rapid' systematic reviews (see Agreements and disagreements with other studies or reviews). We handsearched the references to included studies from all of these excluded reviews.
4. Excluded reviews: narrative literature reviews and systematic reviews not focused on interventions.
| Review | Pandemic/epidemic studied | Stated study aim |
| Narrative literature reviews | ||
| Balasubramanian 2020 | COVID‐19 | To consolidate pre‐existing self‐care tips and mental health resources, summarise webinars and teleconference proceedings from hard‐hit areas, and discussions with experts in the field, which will serve as a resource to mitigate the short‐ and long‐term psychological effects of the current pandemic |
| Bansal 2020 | COVID‐19 | To understand the stressors that COVID‐19 is placing on clinicians can assist in recognising what is needed to return to a point of wellness |
| Benedek 2007 | Disasters | To review the spectrum of emotional and behavioUral consequences of traumatic events as part of understanding the effects of disaster work on public health responders. To outline evidence‐based psychopharmacologic and psychotherapeutic interventions for post‐traumatic distress reactions and psychiatric disorders, and to discuss public health intervention models for the assessment and management of distress responses and mental disorders in first‐responder communities |
| Chakraborty 2020 | COVID‐19 |
|
| Chersich 2020 | COVID‐19 | In this review we describe the infection risks and mental health challenges that healthcare workers face in the COVID‐19 pandemic and propose interventions to counter these in Africa. |
| Duan 2020 | COVID‐19 | Summarises the psychological interventions for people affected by COVID‐19 in China |
| Duncan 2020 | Disasters | This article briefly looks at previous pandemics and disasters that have affected healthcare systems, as well as the 2020 COVID‐19 pandemic, and considers how nurse leaders can support staff and show organisational resilience during such emergencies. The article also discusses how nurse leaders can develop their own resilience. |
| Galbraith 2020 | Virus epidemics or pandemics | To describe and discuss the mental health of doctors during disease outbreaks, and the need of strong leadership and support |
| Shah 2020 | Virus epidemics or pandemics | Our review article focused on:
|
| Shultz 2016 | Ebola virus disease | This review examines how fear‐related behaviours were implicated in:
|
| Spokane 2011 | Not clearly stated | Discuss the phases and stages, social ecology, and individual reactions to disasters. A case study is presented, followed by mental health interventions and counselling psychology’s role in these interventions at both the individual and systemic levels |
| Stanley 2012 | Disasters | The research included in this review was published between 2000 and 2011, capturing a snapshot of the last decade of relevant research on the psychological impact of disaster |
| Tsamakis 2020 | COVID‐19 | The impact of COVID‐19‐related anxiety in cardiology, paediatrics, oncology, dermatology, neurology and mental health and how it affects treatments is discussed |
| Walton 2020 | Not clearly stated | This paper details the effects on staff and addresses some of the organisational, team and individual considerations for supporting staff (pragmatically) during this pandemic. |
| Weiss 2020 | COVID‐19 | In this paper, we adapt Maslow’s needs framework to systematically address trainee well‐being during the COVID‐19 pandemic and identify potential interventions to meet trainee needs at the program, institution, and extra‐institutional levels. |
| Systematic reviews, not focused on effectiveness of interventions to support mental health or resilience of healthcare workers | ||
| Allan 2020 | Virus epidemics or pandemics | To estimate the prevalence of common mental health disorders in HCWs based in hospitals where pandemic‐affected patients were treated |
| Aoyagi 2015 | Influenza | To estimate the proportion of healthcare workers (HCWs) willing to work during an influenza pandemic and identify associated risk factors |
| Ayanore 2019 | Health crises in Sub‐Saharan Africa | To examine the literature on health workforce, surveillance, and health governance issues for health systems strengthening |
| Baduge 2018 | Ebola | To describe the evidence to‐date regarding strategies that achieve emergency nurses’ and EDs' preparedness to manage EVD risk |
| Brooks 2016 | Disasters | To identify social and occupational factors affecting the psychological impact of disasters on responders |
| Brooks 2018 | SARS | To conduct a systematic literature review to identify social and occupational factors affecting the psychological well‐being of healthcare workers involved in the severe acute respiratory syndrome (SARS) crisis. |
| Connor 2014 | Disasters | Emergency response relies on the assumption that essential healthcare services will continue to operate and be available to provide quality patient care during and after a patient surge. The observed successes and failures of healthcare systems during recent mass‐casualty events and the concern that these assumptions are not evidence‐based prompted this review. |
| Ejeta 2015 | Disasters | The goal of this systematic review was to search and summarise evidence by assessing the application of behavioral theories to disaster and emergency health preparedness across the world. |
| Etkind 2020 | Virus epidemics or pandemics | To synthesize evidence for the role and response of palliative care and hospice teams to viral epidemics/pandemics and inform the COVID‐19 pandemic response |
| Gardner 2015 | SARS | To conduct a critical review of the English language literature on the psychological impact of SARS for survivors |
| Gowing 2017 | Disasters | To review both qualitative and quantitative research to gain a current understanding of research conducted and the current state of knowledge. The review will be used to inform future research and the development of knowledge which can be used by health services, professionals, or disaster planners to better prepare health professionals and support staff for disasters (includes pandemics) |
| Kisely 2020 | Virus outbreaks | To examine the psychological effects on clinicians of working to manage novel viral outbreaks, and successful measures to manage stress and psychological distress |
| Vyas 2016 | Ebola | To examine the potential psychological impact of deploying in support of the USA response to Ebola in West Africa by systematic review and meta‐analysis |
| Zuercher 2020 | Virus epidemics or pandemics | The purpose of this rapid review is to provide an overview of MHP prevalence rates during and after large epidemics of the past two decades. We aim to provide a broad picture of MHP that may arise across a wide range of populations including a) the general public, b) HCW, and c) and virus disease survivors. |
| EVD: Ebola virus disease; HCW: healthcare worker; MHP: mental health problems | ||
5. Excluded reviews: systematic reviews covering interventions to support mental health or resilience of healthcare professionals during disease pandemics.
| Review | Pandemic/epidemic studied | Stated review aim | Number of included studies | Description of interventions included in review | Key findings relevant to mental health & resilience | Notes |
| Bell 2020 | Virus epidemics or pandemics | We aimed to estimate the additional burden of working directly with infected patients during epidemic and pandemic health emergencies. | 74 | "In terms of protective factors that reduced the chance of poor mental health or psychological distress, social support, team cohesion or organisational support were identified by numerous studies" | "Although a recent anecdotal report noted clinicians did not find mental health support particularly useful during COVID‐19 response (Chen et al 2020) several studies found that participants reported formal psychological support services to be a useful source of support (Goulia et al 2010; Lee et al 2005; Meyer et al 2018; Smith et al 2017; von Strauss et al 2017). One study specifically asked whether staff needed ‘psychological treatment’ and 8.6% of healthcare workers dealing with COVID‐19 reported they did (Liu et al 2020). Conversely, however, Chung and Yeung (2020) reported that only 2% of staff responding to COVID‐19 requested psychological support and all “were reassured after a single phone contact by the psychiatric nurse” although this was a notably small study with just 69 participants." | 'Rapid' review |
| Cenat 2020 | Ebola |
|
11 (11 programmes identified) | 11 mental health and psychological support programmes were identified; 4 programmes were aimed at staff and volunteers; 2 programmes were in Ebola treatment centres and 1 in the community. The activities of the programmes varied greatly, including training, support and supervision. | At least 3 of the identified programmes were focused on frontline workers but others were community/paediatric based. Concludes that culturally adapted MHPSS programmes may have positive effects both for adults and children affected by EVD, as well as the relation between emotional impacts of EVD and the implementation of preventive measures. | |
| Devnani 2012 | Influenza and SARS | To determine the state of the evidence concerning the willingness of healthcare professionals to work during an influenza public health emergency, to identify the gaps for future investigation, and to facilitate evidence‐based influenza public health emergency planning. | 32 | Interventions to improve willingness to work in a pandemic | Factors associated with a willingness to work during an influenza public health emergency include: being male, being a doctor or nurse, working in a clinical or emergency department, working full‐time, prior influenza education and training, prior experience working during an influenza emergency, the perception of value in response, the belief in duty, the availability of PPE, and confidence in one’s employer. Factors found to be associated with less willingness were: being female, being in a supportive staff position, working part‐time, the peak phase of the influenza emergency, concern for family and loved ones, and personal obligations. Interventions that resulted in the greatest increase in the healthcare professional’s willingness to work were preferential access to Tamiflu for the healthcare professional and his/ her family, and the provision of a vaccine for the individual and his/her family. | |
| Koh 2010 | Acute respiratory infectious diseases | To synthesise evidence relating to the risk perceptions and workplace strategies of HCWs to EARIDs in acute hospital and community healthcare settings; and to make recommendation for practice that will protect them and their patients/clients. | 16 (2 qualitative, 14 quantitative) | One paper is reported as finding that: “57.1% of the respondents perceived psychological support during the outbreak to be important and around 60% perceived psychological support after the event to be important” | Quant ‐ Concerned with 3 categories of risk perception: health, social and acceptance of risk. Strategies employed to mitigate risk were behaviour towards patients, compliance towards preventative measures and organisational strategies. Qualitative ‐ similar to quantitative. Risks to personal health, social but HCWs were still willing to care for patients. | Joanna Briggs review |
| Muller 2020 | COVID‐19 | To identify, assess and summarise available research on the mental health impact of the COVID‐19 pandemic on HCWs, including a) changes over time, b) prevalence of mental health problems and risk/resilience factors, c) strategies and resources used by healthcare providers to protect their own mental health, d) perceived need and preferences for interventions, and e) healthcare workers’ understandings of their own mental health during the pandemic. Our second aim was to describe the interventions assessed in the literature to prevent or reduce negative mental health impacts on healthcare workers who are at work during the covid‐19 pandemic. | 59 | "Six studies reported on the implementation of interventions to prevent or reduce mental health problems caused by the covid‐19 pandemic among healthcare workers": 2 involved a series of "organisational adjustments" including shortened shifts and a telephone hotline; 1 was a telephone hotline to provide immediate psychological support; 1 "collegial support and building individual strategies through one‐hour video “support calls”"; 1 was an online app that allowed requests for psychological support; and 1 was an "onsite, in‐person psychological crisis measure". | Most studies did not report comparative data on mental health symptoms before the pandemic or in the general population. There seems to be a mismatch between risk factors for adverse mental health outcomes among HCWs in the current pandemic, their needs and preferences, and the individual psychopathology focus of current interventions. | 'Rapid' review |
| Cabello 2020 | Virus epidemics or pandemics | To examine the impact of providing healthcare during or after health emergencies caused by viral epidemic outbreaks on HCWs' mental health, and to assess the available evidence base regarding interventions to reduce such impact. | 61 | 5 intervention studies: educational interventions (2 studies), multifaceted interventions combining training and implementation of organisational changes (2 studies), provision of psychological support (1 study) | HCWs commonly present high levels of anxiety, depression, PTSD, acute disorder and burnout, both during and after the outbreaks. 5 interventions identified but low evidence that they mitigate development of mental health problems | 'Rapid' review |
| Robertson 2020 | Virus epidemics or pandemics | a) What may be expected regarding the psychological impact of the COVID‐19 outbreak on HCWs? b) What interventions could be considered in order to protect and support the mental health and well‐being of HCWs during the crisis? | 32 | Psychological support, organisational interventions | "We did not identify any effectiveness studies in our literature search. Rather, interventions were recommended according to identified needs and coping strategies, risk and protective factors, and experience, and therefore were all SORT level 3 evidence. While some articles prioritised early recognition and individual psychological support, others placed emphasis on organisational interventions to support HCWs." | 'Rapid' review |
| Spoorthy 2020 | COVID‐19 | This review aimed to review the literature about mental health problems faced by HCW during the COVID‐19 pandemic. | 6 | Factors responsible for the reduction in stress included personal and organisational factors; coping measures are briefly outlined. | Current research focused on assessing several aspects of mental health affected in HCW due to COVID‐19. Several sociodemographic variables like gender, profession, age, place of work, department of work and psychological variables like poor social support, self‐efficacy were associated with increased stress, anxiety, depressive symptoms, insomnia in HCW. There is increasing evidence that suggests that COVID‐19 can be an independent risk factor for stress in HCW. | |
| Stuijfzand 2020 | Virus epidemics or pandemics | This rapid review synthesises the evidence on the psychological impact of pandemics/epidemics on the mental health of HCPs, what factors predict this impact, and the evidence of prevention/intervention strategies to reduce this impact. | 48 | Five studies investigating the effect of preventative programmes or interventions addressing mental health outcomes in HCPs were included. These included preventative program, computerised simulation sessions, computer‐based resilience training, psychological first aid training, and brief CBT group program. | Results show that exposed HCPs working with patients during an epidemic/pandemic are at heightened risk of mental health problems in the short and longer term, particularly: psychological distress, insomnia, alcohol/drug misuse, and symptoms of posttraumatic stress disorder (PTSD), depression, anxiety, burnout, anger, and higher perceived stress. These mental health problems are predicted by organizational, social, personal, and psychological factors and may interfere with the quality of patient care. Few evidence‐based early interventions exist so far. | 'Rapid' review |
| EARID: emerging acute respiratory infectious diseases; EVD: Ebola virus disease; HCP: healthcare provider/professional; HCW: healthcare worker; MHPSS: mental health and psychosocial support; PTSD: post‐traumatic stress disorder; PPE: personal protective equipment; SARS: severe acute respiratory syndrome; SORT: Strength of Recommendation Taxonomy | ||||||
Risk of bias in included studies
Objective 1: review of effectiveness
We assessed the one randomised trial (De Jong 2019), using Cochrane's 'Risk of bias' tool (Higgins 2017). Details of this are provided in Table 8. Assessment of the risk of bias of this study was limited by the lack of a registered study protocol, and lack of detail about some areas of the methods. In addition, we identified some concerns relating to potential risk of bias in the outcome comprising questions from the Professional Quality of Life Scale, which we considered relevant to our outcome of burnout. The Professional Quality of Life Scale is a 30‐item scale; however, the study authors state that due to "difficulties in understanding and responding to 20 of the items" during piloting, they used only 10 items. While it states that "The 10 selected items were 6 items from the Compassion Fatigue Scale (items 3, 12, 20, 22, 24, and 30) and 4 items from the Burnout Scale (items 2, 3, 5, and 7)", exploration of the scale (ProQOL‐5), indicates that these questions were from the Compassion Satisfaction (not Fatigue) and Burnout Scale. Although there is evidence for the validity of the Professional Quality of Life Scale, and the associated subscales, we are uncertain about the risk of bias associated with the use of incomplete scales, and the combination of individual questions from different subscales. Furthermore, we identified some concerns relating to the methods of quantitative analysis. The analysis attempts to account for clustering by including Peripheral Health Unit (PHU, the cluster‐level variable) as a fixed effect in addition to a fixed effect for randomised allocation. This method is not recommended as it fails to reflect the clustering in the study design and underestimates the variability of the intervention effect. These problems could have been addressed if PHU had been fitted as a random effect (this would not change the reported point estimate but would widen the confidence intervals). The study authors did not publish intraclass correlation coefficients, which could have enabled us to reanalyse the data, and so the underestimated variability must be considered when interpreting the results.
6. Assessment of risk of bias of quantitative studies using the Cochrane 'Risk of bias' tool (RoB 1).
| Study:De Jong 2019 | ||
| Biasa | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Cluster‐randomised trial. Lack of information about randomisation |
| Allocation concealment (selection bias) | Unclear risk | As above, lack of information about randomisation and concealment |
| Blinding of participants and personnel (performance bias) | High risk | Due to nature of intervention, participants were not blinded. Control group did not receive any attention control intervention |
| Blinding of outcome assessment (detection bias) | Low risk | "Twelve trained assessors, who were blind to the group participants were assigned to, administered the instruments." |
| Incomplete outcome data (attrition bias) | High risk | Authors state: "Seventy‐one (34.5%) people in the program group did not attend the PFA training, mainly due to practical reasons including heavy rainfall in Sierra Leone during the days of the trainings. In the control group, 4 (2.0%) people received PFA when they should not have received it. We performed both completers and intention‐to‐treat analysis, but we judged the completers analysis as the main outcome analysis since we considered it most relevant to examine the training effects of PFA training in individuals who were actually trained. In addition, we considered attrition bias unlikely since the reason for most people not having received the condition they were assigned to (PFA or control) was external (extreme weather conditions)." Although the study authors conclude that attrition bias was unlikely; there was a high proportion of dropouts, and dropouts were likely to involve whole clusters (or certainly some clusters were likely to be more affected than others) due to the impact of the weather. Geographical factors were likely to have affected the dropouts, and consequently the demographics of the dropouts and the completers could vary substantially. Furthermore the completers' analyses were all different from the intention‐to‐treat analyses, with the direction of difference the same. We therefore judged this to be high risk for attrition bias. |
| Selective reporting (reporting bias) | Unclear risk | No evidence of pre‐registered protocol, so not possible to know if there has been selective reporting. For example, only certain subscales of the Psychological Quality of Life scale are reported; it is unclear whether the decision to only collect these data was pre‐planned. |
| PFA: psychological first aid | ||
aAssessed using Cochrane 'Risk of bias' tool for randomised trials (RoB 1) (Higgins 2017).
Assessment of methodological limitations
Objective 2: qualitative evidence synthesis
We assessed the methodological limitations of the seven qualitative studies using the CASP checklist for qualitative studies (CASP 2018). These studies included six with a qualitative study design (Belfroid 2018; Chen 2020; Cunningham 2017; De Jong 2019; Lee 2005; Son 2019), and one that had a mixed method, from which we used data from the qualitative component (Cao 2020). Details of these assessments are provided in Table 9 and Appendix 13.
7. Assessment of methodological limitations using CASP tool for qualitative studies.
| Study | CASP criteria | |||||||||
| 1. Was there a clear statement of the aims of the research? | 2. Is a qualitative methodology appropriate? | 3. Was the research design appropriate to address the aims of the research? | 4. Was the recruitment strategy appropriate to the aims of the research? | 5. Were the data collected in a way that addressed the research issue? | 6. Has the relationship between researcher and participants been adequately considered? | 7. Have ethical issues been taken into consideration? | 8. Was the data analysis sufficiently rigorous? | 9. Is there a clear statement of findings? | Overall assessment | |
| Belfroid 2018 | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | Yes | Yes | No or few limitations |
| Cao 2020 | Yes | Yes | Cannot tell | Yes | Yes | Cannot tell | Cannot tell | Cannot tell | Yes | Minor limitations |
| Chen 2020 | No | Yes | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Yes | Major limitations |
| Cunningham 2017 | Yes ‐ partly | Yes | Cannot tell | Yes | Yes | Yes | Yes | Yes | Yes | No or few limitations |
| De Jong 2019 | Yes | Yes | Yes | Cannot tell | Yes | Cannot tell | Yes | Yes | Yes | No or few limitations |
| Lee 2005 | Yes | Yes | Yes | Yes | Cannot tell | No | Cannot tell | Cannot tell | Yes ‐ partly | Minor limitations |
| Son 2019 | Yes | Yes | Cannot tell | No | Cannot tell | No | Cannot tell | Yes | Yes | Minor limitations |
| CASP: Critical Appraisal Skills Programme for qualitative studies (CASP 2018) | ||||||||||
We assessed the methodological limitations of the nine descriptive studies using the WEIRD checklist (Lewin 2019). These studies included one that had a mixed method (Waterman 2018), and two with a quantitative study design (Carvalho 2019 ‐ cohort study; Chang 2006 ‐ survey), from which we extracted descriptive data, rather than the quantitative evidence. Details of these assessments are provided in Table 10 and Appendix 14.
8. Assessment of methodological limitations using WEIRD tool for descriptive studies.
| Study | WEIRD criteria | ||||||||||
| 1. Is there a clearly stated aim, objective or purpose for the source material? | 2. Is there a clear description of the source of the information reported (transparency)? | 3. Is there a clear description of the programme or intervention or policy or reform on which the source material focuses? | 4. Is there a clear description of the context/s to which the information described in the source material relates? | 5/6. Is the information accurate? (Non‐empirical/empirical studies) | 7. Is the evidence representative? | 8. Are any limitations of the information and/or methods discussed in the source material? | 9. Is evidence provided to support any findings or conclusions made? | 10. Are relevant rights and ethics considerations described? | 11. Are any interests declared and any potential conflicts of interest noted? | Overall assessment | |
| Blake 2020 | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | No or few limitations |
| Brown‐Johnson 2020 | Yes | Unclear | Yes | No | Unclear | Unclear | No | No | Unclear | Yes | Major limitations |
| Carvalho 2019 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Unclear | Minor limitations |
| Chang 2006 | Yes | Yes | Yes | Yes | No | No | Yes | No | Unclear | Unclear | Major limitations |
| Cheung 2015 | Yes | No | No | Yes | Yes | No | Unclear | Yes ‐ partly | Unclear | Unclear | Major limitations |
| Ferranti 2016 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Unclear | Unclear | Minor limitations |
| Klomp 2020 | No | No | Unclear | No | Unclear | Unclear | No | Unclear | Unclear | Yes | Major limitations |
| Schreiber 2019 | Yes | Yes | Yes | Unclear | Unclear | Unclear | No | Yes | Unclear | Unclear | Minor limitations |
| Waterman 2018 | Yes | Yes | Yes | Yes | Yes | Unclear | No | Yes | Unclear | Yes | Minor limitations |
| WEIRD: Ways of Evaluating Important and Relevant Data tool (Lewin 2019) | |||||||||||
Based on the assessment of each tool item (either WEIRD or CASP), we judged the overall assessment of the limitations of the studies to be:
no or few limitations ‐ four studies (Belfroid 2018; Blake 2020; Cunningham 2017; De Jong 2019);
minor limitations ‐ seven studies (Cao 2020; Carvalho 2019; Ferranti 2016; Lee 2005; Schreiber 2019; Son 2019; Waterman 2018);
major limitations ‐ five studies (Brown‐Johnson 2020; Chen 2020; Chang 2006; Cheung 2015; Klomp 2020).
Effects of interventions
Summary of findings 1. Workplace intervention compared to no intervention to support mental health and resilience of health and social care professionals during a disease outbreak.
| Workplace intervention compared to no intervention to support mental health and resilience of health and social care professionals during a disease outbreak | |||
|
Patient or population: health and social professionals Settings: any setting in which there is a disease outbreak, epidemic or pandemic Intervention: workplace intervention Comparison: no treatment | |||
| Outcomes | Impact | No of Participants (studies) | Certainty of the evidence (GRADE) |
| General mental health (critical outcome) | ‐ | No studies | Insufficient evidence |
| Resilience (critical outcome) | ‐ | No studies | Insufficient evidence |
| Psychological symptoms of anxiety, depression or stress | ‐ | No studies | Insufficient evidence |
|
Burnout (10 questions from ProQOL scale; assessed immediately post‐intervention and at 6‐month follow‐up) |
It is uncertain whether workplace interventions improve burnout as the certainty of the evidence is very low | 408 (1 study)a | ⊕⊝⊝⊝ Very lowb,c,d |
| Effects on workplace staffing ‐ absenteeism | ‐ | No studies | Insufficient evidence |
| ProQOL: Professional Quality of Life | |||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | |||
aStudy is De Jong 2019. The workplace intervention comprised training for frontline workers in how to deliver psychological first aid to people affected by the Ebola epidemic in Sierra Leone. bDowngraded by one level due to serious imprecision, as evidence was available from one study only. cDowngraded by one level due to high risk of bias due to the analysis not accounting for the cluster randomisation, high risk of incomplete outcome bias with dropouts potentially affected by geographical factors, and lack of blinding and no attention control intervention. dDowngraded by one level due to serious indirectness as we had concerns regarding the validity of use of the ProQOL scale.
Summary of findings 2. Summary of qualitative findings.
| Summary of review findings | Studies contributing to the review finding | GRADE‐CERQual assessment of confidence in the evidence | Explanation of GRADE‐CERQual assessment |
| CFIR Domain 1: intervention characteristics | |||
| Finding 1. Flexible interventions that were culturally appropriate, adaptable and/or able to be tailored to meet local needs were seen as key to successful implementation. | Blake 2020; Brown‐Johnson 2020; Cheung 2015; De Jong 2019; Ferranti 2016; Schreiber 2019; Waterman 2018 | Moderate confidence | Downgraded because we had moderate concerns regarding methodological limitations. We had no or very minor concerns about coherence, relevance and adequacy. |
| Finding 2. Interventions characterised as having a low level of complexity were seen as easier to implement. | Blake 2020; Brown‐Johnson 2020; Ferranti 2016; Son 2019 | Low confidence | Downgraded because we had moderate concerns regarding coherence, relevance and adequacy. We had minor concerns about methodological limitations. |
| Finding 3: Intervention costs and associated costs of implementing the intervention were seen as both hindering and facilitating implementation. | Blake 2020; De Jong 2019 | Low confidence | Downgraded because we had moderate concerns regarding, coherence, relevance and adequacy. We had no concerns about the methodological limitations. |
| CFIR Domain 2: outer setting (i.e. environmental factors) | |||
| Finding 4: Lack of awareness about the needs and resources of frontline workers was seen as a barrier to implementation. This included lack of awareness of frontline workers' of their own needs, and lack of awareness of organisations who employed and supported frontline workers. | Belfroid 2018; Cao 2020; Chang 2006; Chen 2020; Cheung 2015; Cunningham 2017; De Jong 2019; Ferranti 2016; Klomp 2020; Lee 2005; Schreiber 2019; Waterman 2018 | Moderate confidence |
Downgraded because we had moderate concerns regarding methodological limitations. We had minor concerns about coherence, relevance and adequacy. |
| Finding 5. Awareness of mental health needs by governments and political leaders was identified as a facilitator. | Cheung 2015; Klomp 2020 | Very low confidence | Downgraded because we had serious concerns about the methodological limitations of these studies, and moderate concerns regarding relevance and adequacy. |
| Finding 6. Networking between organisations involved in providing frontline services, and co‐ordinating multiple external organisations in a crisis was seen as both a barrier and a facilitator to implementation. | Blake 2020; Cheung 2015; De Jong 2019 | Low confidence | Downgraded because we had moderate concerns regarding coherence, relevance and adequacy. We had minor concerns about the methodological limitations. |
| CFIR Domain 3: inner setting (i.e. organisational factors) | |||
| Finding 7. Effective communication, and cohesion through horizontal and vertical networks, was seen to strengthen social capital and improve team resilience and was considered to be a key factor in implementation. | Belfroid 2018; Blake 2020; Cao 2020; Chang 2006; Cheung 2015; Cunningham 2017; Klomp 2020; Lee 2005 | Moderate confidence | Downgraded because we had moderate concerns regarding methodological limitations, and no or very minor concerns about coherence, relevance and adequacy. |
| Finding 8. Organisational incentives and rewards for frontline workers were seen as important in facilitating and engaging student healthcare workers and frontline staff with the intervention. | Belfroid 2018; Chang 2006; Ferranti 2016; Waterman 2018 | Low confidence | Downgraded because we had moderate concerns regarding coherence, relevance and adequacy. We had minor concerns about the methodological limitations. |
| Finding 9. A positive learning climate for everyone involved in implementation of an intervention was seen to facilitate implementation. | Belfroid 2018; Brown‐Johnson 2020; Carvalho 2019; Chang 2006; Cheung 2015; Cunningham 2017; De Jong 2019; Lee 2005 | Moderate confidence | Downgraded because we had moderate concerns regarding methodological relevance. We had no or very minor concerns about coherence, relevance and adequacy. |
| Finding 10. Resource constraints, including lack of equipment, staff time and skills, were described as hindering implementation. | Belfroid 2018; Brown‐Johnson 2020; Cao 2020; Chang 2006; Chen 2020; Cunningham 2017; De Jong 2019; Waterman 2018 | Moderate confidence | Downgraded because we had moderate concerns regarding methodological limitations, and no or very minor concerns about coherence, relevance and adequacy. |
| Finding 11. Education, training, and access to information for frontline workers was considered an important step underpinning the readiness for implementation, and was seen to act as a barrier or facilitator depending on the quality provided. | Belfroid 2018; Chang 2006; Chen 2020; Cheung 2015; De Jong 2019; Ferranti 2016 | Low confidence | Downgraded because we had moderate concerns regarding methodological limitations, relevance and adequacy. We had minor concerns about coherence. |
| CFIR Domain 4: individual characteristics (of frontline health and social care professionals) | |||
| Finding 12. Frontline workers' knowledge and beliefs about the intervention were seen to act as either a barrier or facilitator to implementation. | Belfroid 2018; Blake 2020; Carvalho 2019; Chen 2020; Cunningham 2017; De Jong 2019; Waterman 2018 | Moderate confidence | Downgraded because we had moderate concerns regarding adequacy. We had no or very minor concerns about methodological limitations, coherence and relevance. |
| Finding 13. Frontline workers' confidence in their ability to deliver and implement an intervention was seen as an important factor in successful implementation. | Belfroid 2018; Brown‐Johnson 2020; Carvalho 2019; Cunningham 2017; Ferranti 2016 | Low confidence | Downgraded because we had moderate concerns regarding coherence, relevance and adequacy. We had minor concerns about methodological limitations. |
| Finding 14. Individual personal characteristics and attributes of frontline professionals, such as their attitudes and motivation, were seen to act as either a barrier or facilitator to implementation. | Belfroid 2018; Chang 2006; Cheung 2015; Cunningham 2017; De Jong 2019; Lee 2005; Waterman 2018 | Low confidence | Downgraded because we had moderate concerns regarding methodological limitations, relevance and adequacy. |
| CFIR Domain 5: implementation process characteristics | |||
| Finding 15. Planning to prepare individual frontline workers and organisations to implement changes was often reported to be overlooked, resulting in frontline workers feeling rushed and unprepared. Strategic plans at the level of the individual healthcare worker and organisation were considered to facilitate the success of the implementation. | Belfroid 2018; Brown‐Johnson 2020; Cao 2020; Chang 2006; Chen 2020; Ferranti 2016; Klomp 2020; Waterman 2018 | Low confidence | Downgraded because we had moderate concerns regarding methodological limitations, and adequacy. We had no or very minor concerns about coherence and relevance. |
| Finding 16. Meaningful engagement of people involved in the delivery of interventions to support mental health, and forming strong collaborations with champions and opinion leaders, was seen to positively impact on implementation. | Belfroid 2018; Blake 2020; Brown‐Johnson 2020; Cunningham 2017; Klomp 2020; Lee 2005; Son 2019; Waterman 2018 | Low confidence | Downgraded because we had moderate concerns regarding methodological limitations and adequacy. We had minor concerns regarding coherence and relevance. |
| Finding 17. The opportunity for frontline workers to reflect on, evaluate or take part in a debriefing session was seen to promote a sense of safety, and to support a shared learning which facilitated the implementation process. | Belfroid 2018; Blake 2020; Carvalho 2019; Cunningham 2017; De Jong 2019; Klomp 2020 | Low confidence | Downgraded because we had moderate concerns regarding relevance and adequacy. We had minor concerns regarding methodological limitations and coherence. |
| CERQual: Confidence in the Evidence from Reviews of Qualitative research; CFIR: Consolidated Framework for Implementation Research | |||
Objective 1: review of effectiveness
Workplace interventions
One cluster‐randomised study (De Jong 2019; 408 participants), compared the effect of a workplace intervention ‐ training in psychological first aid ‐ with no treatment, for healthcare professionals working immediately after the Ebola outbreak. They reported only one outcome relevant to this review, individual questions from the Professional Quality of Life Scale, which we considered a measure of burnout; however, due to the use of individual questions from the scale only, we noted concerns relating to risk of bias of this reported outcome. Table 11 shows the results for this outcome, reported by De Jong 2019. This was a cluster‐randomised trial, but the analysis presented did not take clustering into account appropriately and there was insufficient reporting of results to enable us to re‐estimate the variability associated with the reported effect size (see section on Risk of bias in included studies for further details). Based on the data published in the paper, we are uncertain about the effect of training in psychological first aid on burnout as the certainty of the evidence was very low (see Table 1).
9. Quantitative findings.
| Quantitative findings:De Jong 2019 | |||
| Completers' ‐ Professional Quality of Life Scale (burnout) | |||
|
PFA group (n = 135) Mean (SD) |
Control group (n = 198) Mean (SD) |
Mean difference (95% CI) | |
| Baseline | 37.07 (5.73) | 36.36 (5.69) | |
| Post‐assessment | 36.87 (5.52) | 36.30 (5.51) | 0.07 (‐1.21 to 1.35) |
| Follow‐up | 36.79 (6.10) | 36.58 (5.52) | 0.51 (‐0.81 to 1.83) |
| Intention‐to‐treat ‐ Professional Quality of Life Scale (burnout) | |||
|
PFA group (n = 206) Mean (SD) |
Control group (n = 202) Mean (SD) |
Mean difference (95% CI) | |
| Baseline | 36.49 (5.66) | 36.36 (5.66) | |
| Post‐assessment | 36.40 (5.49) | 36.40 (5.53) | −0.17 (0.00 to 0.97) |
| Follow‐up | 36.57 (5.89) | 36.57 (5.48) | −0.04 (‐1.23 to 1.15) |
| CI: confidence interval; PFA: psychological first aid; SD: standard deviation | |||
We identified no other studies exploring the effect of workplace interventions.
Interventions to support basic daily needs
We identified no quantitative studies that explored the effect of interventions to support basic daily needs.
Psychological support interventions
We identified no quantitative studies that explored the effect of psychological support interventions.
Pharmacological interventions
We identified no quantitative studies that explored the effect of pharmacological interventions.
Multifaceted interventions
We identified no quantitative studies that explored the effect of multifaceted interventions.
Objective 2: qualitative evidence synthesis
Our findings are presented in the 'Summary of qualitative findings' table (Table 2). This table also provides our GRADE‐CERQual assessment of confidence in the review finding as well as a brief explanation of this assessment. More detailed assessment of how we applied GRADE‐CERQual is summarised in the GRADE‐CERQual evidence profiles (Appendix 12).
All 16 included studies described barriers and facilitators that influenced the implementation of interventions to support the resilience and mental health of frontline health and social care professionals (Belfroid 2018; Blake 2020; Brown‐Johnson 2020; Cao 2020; Carvalho 2019; Chang 2006; Chen 2020; Cheung 2015; Cunningham 2017; De Jong 2019; Ferranti 2016; Klomp 2020; Lee 2005; Schreiber 2019; Son 2019; Waterman 2018). We identified multiple factors within each study, and we mapped these to 17 constructs across five domains based on the CFIR (Table 4).
In the following section, we present the findings that were reported within each CFIR domain, supported by key examples for barriers and facilitators (see Appendix 12 for all findings below).
CFIR Domain 1: intervention characteristics
Finding 1. Flexible interventions that were culturally appropriate, adaptable and/or able to be tailored to meet local needs were seen as key to successful implementation
We have moderate confidence in this evidence (Appendix 12).
Several studies described the ability of an intervention to be flexible or adapted for the local context as a facilitator (Blake 2020; Brown‐Johnson 2020; Cheung 2015; De Jong 2019; Ferranti 2016; Schreiber 2019; Waterman 2018).
Studies highlighted the importance of adapting training and training materials to promote effective use of the intervention. De Jong 2019 described the importance of adapting the PFA (psychological first aid) facilitators' manual in two different settings ‐ Liberia and Sierra Leone ‐ during the Ebola outbreak. In the Liberian context: "the content itself was perceived to be appropriate and not to require adaptation. Trainers said the only modifications they made to the material were in terms of language and adapting the role plays and other exercises to be suitable for the group being trained. Although the original manual was used to deliver PFA [psychological first aid]training, additional emphasis was given to safe entry into communities, self‐care, and active listening skills. These elements were felt to be especially important".
However, in Sierra Leone, the study authors report that the intervention needed to be adapted, and "greatly reduced to fit into the 95‐min time slot" (p7)" so that it could be integrated into a broader training programme that was in place. Several respondents also, "noted the need to ensure that the training was culturally appropriate in terms of community entry, how to approach a distressed individual, and in the language and case studies used" (De Jong 2019, p8).
Adapting training and training materials was not always enough to ensure seamless implementation of the intervention. For example, Waterman 2018 commented that "although the materials were adapted for lower literacy levels, many participants still struggled to understand the workbooks. This meant that the sessions were often interrupted and some participants were less able to complete homework tasks and contribute to group discussions...‘It was very challenging to teach CBT to people that could not speak or read English...I had to give them a lot of assistance and sometimes they still wouldn’t understand, even when I explained in the local language’" (Waterman 2018, p32).
The importance of contextualising interventions was also highlighted with Cheung 2015 stressing the need to understand "the cultural background of the community is crucial in order to implement appropriate support to address local psychosocial issues and concerns. It is important, not only for psychosocial workers, but also those are responsible for conducting contact tracing and health education in the community, to be well informed" (p74). Waterman 2018 also pointed out that there may be differing cultural conceptualisations of mental health problems..."CBT is new here and many people struggled to understand the concepts. . . some people didn't get the point in coming because they didn't see their problems in the same way we did" (p32).
Finding 2. Interventions characterised as having a low level of complexity were seen as easier to implement
We have low confidence in this evidence (Appendix 12).
Four studies linked the difficulty and complexity of understanding and delivering an intervention to implementation success (Blake 2020; Brown‐Johnson 2020; Ferranti 2016; Son 2019).
Interventions that were perceived by frontline workers as having a low burden (i.e. interventions perceived as 'simple', easy to teach and accessible) were considered easier to implement. Blake 2020 reported high usability scores for their multifaceted digital intervention aimed at improving psychological well‐being of healthcare workers because it required "no prior knowledge or training, and the mode of delivery is via web link, with the intention that the resource would be utilised independently and individually by healthcare workers (or healthcare students and academics) at a time and location of their choosing" (p11).
Finding 3: Intervention costs and associated costs of implementing the intervention was seen as both hindering and facilitating implementation
We have low confidence in this evidence (Appendix 12).
Two studies discussed the impact of costs of the intervention on implementation success (Blake 2020; De Jong 2019). De Jong 2019 pointed out that the cost‐benefit of different interventions required careful consideration arguing that "there are clear advantages to training non‐specialists to provide psychosocial support during emergencies, and PFA, as outlined in manuals and training materials, has all the elements of an effective approach. However, the perception that it is a cheap and easy option has led to very short training programmes, with minimal follow‐up support" (p9). Conversely, interventions that were made freely available online, with 'acceptable cost implications', or those that integrated the intervention using well‐known digital platforms were perceived as beneficial to implementation (Blake 2020).
CFIR Domain 2: outer setting (i.e. environmental factors)
Finding 4. Lack of awareness about the needs and resources of frontline workers was seen as a barrier to implementation.
This included lack of awareness of frontline workers of their own needs, and lack of awareness of organisations who employed and supported frontline workers. We have moderate confidence in this evidence (Appendix 12).
Twelve studies described a lack of awareness regarding frontline staff needs, coupled with failure of frontline workers to recognise that they needed help, or organisations struggling to provide timely support (Belfroid 2018; Cao 2020; Chang 2006; Chen 2020; Cheung 2015; Cunningham 2017; De Jong 2019; Ferranti 2016; Klomp 2020; Lee 2005; Schreiber 2019; Waterman 2018).
Frontline health and social care workers in a pandemic or epidemic often have a dual role. They are expected successfully to deliver and implement an intervention to support resilience and mental health, but they were often the target population of these interventions (i.e. the 'patient'). For example, in De Jong 2019 the authors report that "most of the PFA providers interviewed had been selected for training because their role involved contact with distressed individuals, but some were selected because they were working in very distressing situations and were in need of emotional support themselves. In the absence of any kind of stress management programmes, they were selected for PFA training to help them learn ways to cope with the situation they were working in" (p8).
Organisations that considered the specific health needs and desired health outcomes for frontline workers were more likely to implement change effectively (Cao 2020). However, Belfroid 2018 pointed out that "when preparing for outbreaks, healthcare organizations focus mainly on the medical, hygienic, and organizational aspects, whereas the human factors are ignored" (p217).
One nurse observed that they didn't feel that their needs were considered: "I missed the entire psychosocial aspect around it. I thought that was a shortcoming.... At least to sit around the table and listen to what the needs are" (Belfroid 2018, p216).
Other studies described how frontline workers were often reluctant to seek help because of the negative beliefs about help‐seeking and the stigma associated with mental health within their organisation(Belfroid 2018; Chen 2020; Waterman 2018). As Chen 2020 states "implementation of psychological intervention services encountered obstacles, as medical staff were reluctant to participate in the group or individual psychology interventions provided to them" (e15). Other staff failed to recognise that they needed help with their mental health. For example, "individual nurses showed excitability, irritability, unwillingness to rest, and signs of psychological distress, but refused any psychological help and stated that they did not have any problems" (Chen 2020 e15).
Several studies pointed out that some organisations attempted to support their staff by providing targeted solutions. For example; adjusting work schedules (Cao 2020); improving the work environment, by providing accommodation or space to rest, leisure activities, or healthy food, for example, so that frontline workers had more time (Belfroid 2018; Chen 2020; Cunningham 2017); developing protocols for the use and management of PPE to reduce stress (Chen 2020); or providing mental health specialists who "regularly visited the rest area to listen to difficulties or stories encountered by staff at work, and provide support accordingly" (Chen 2020, e15). These organisational efforts to encourage self‐care, providing adequate spaces to rest; and implementing early mental health interventions all sought to improve quality of care, both for themselves and for their patients. However, it was clear from the studies that many of these solutions were often implemented as a reactive strategy.
Finding 5. Awareness of mental health needs by governments and political leaders was identified as a facilitator
We have very low confidence in this evidence (Appendix 12).
Two studies described a positive influence on implementation of political awareness and a willingness to support the mental health needs of frontline workers by policy makers and other well‐placed external agencies, by bringing together multiple stakeholders to work collaboratively (Cheung 2015; Klomp 2020).
Cheung 2015, for example, stated that "I was, in fact, quite surprised to so often hear about the importance of mental health being mentioned by high officials during government coordination meetings for the EVD [Ebola virus disease] operation. The heightened awareness of mental well‐being among the government and political leaders, and committed local mental health professionals, better and more training among health workers, and assistance from international experts and agencies, all provided the best breeding ground for development of longer term, community based mental health and psychosocial support systems" (p75).
Finding 6. Networking between organisations involved in providing frontline services, and co‐ordinating multiple external organisations in a crisis, was seen as both a barrier and a facilitator to implementation
We have low confidence in this evidence (Appendix 12).
Three studies described the various challenges and benefits of networking outside of the frontline workers' organisation (Blake 2020; Cheung 2015; De Jong 2019).
De Jong 2019 reported that, as the Ebola crisis deepened, more organisations became involved on the frontline, providing services. The authors described this as "creating challenges for coordination and making it difficult to control the quality of the training being delivered. There were instances of poor‐quality training being offered, and of the same people being trained multiple times by different organisations" (p8). However, Cheung 2015 described the value of "bringing together all actors in the region to support the collaboration and exchange lessons learnt" (p74).
CFIR Domain 3: inner setting (i.e. organisational factors)
Finding 7. Effective communication, and cohesion through horizontal and vertical networks, was seen to strengthen social capital and improve team resilience and was considered to be a key factor in implementation
We have moderate confidence in this evidence (Appendix 12).
Eight studies described the importance of networks, communications and connectedness within an organisation (Belfroid 2018; Blake 2020; Cao 2020; Chang 2006; Cheung 2015; Cunningham 2017; Klomp 2020; Lee 2005).
Communication, camaraderie and peer support were frequently cited as building a sense of community that positively impacted on the effectiveness of the intervention. Belfroid 2018 described the "…importance of creating feelings of safety and connectedness, providing reliable information, and showing organizational involvement and facilitation of the exchange of experiences between those involved (p217)".
The role of high‐quality communication across the organisation is clear. Effective communication is essential in order to achieve a shared understanding and to build cohesion within and across healthcare providers. Belfroid 2018 reported that "Interviewees who worked in a healthcare organization that did not have clear and unambiguous protocols said that this caused stress and uncertainty. These HCWs [healthcare workers] felt confused because of undefined roles and tasks." (p214). High‐quality communications contributes to effective implementation, as Lee 2005 observed: "...importance of providing timely, clear and updated information to nursing staff with regard to new handling procedures, patient numbers, and the like. In addition, tension between doctors and nurses interfered with teamwork. To address this, meetings of doctors and nurses should be held frequently so that their shared tasks can be identified, conflicts reduced and teamwork strengthened" (p357).
Other studies described the value of having supportive horizontal (social) networks. One healthcare worker in Cunningham 2017 said “I think the biggest coping mechanism was just talking about and encouraging the folks that I lived with and worked with to talk about what was going on, sharing our feelings, and I think we were really a great support for one another.” (2) (p57).Waterman 2018 highlighted the impact of these networks on implementation stating that "Many participants had already met each other in previous parts of this stepped intervention and formed friendships. This greatly enhanced cohesiveness among some of the groups, a factor that has been shown to influence the effectiveness of group CBT and the facilitation of a safe space to share .." (p32).
Strong vertical (formal) networks also had a positive relationship with implementation. For example, Lee 2005 described the pivotal role of a team leader who "had to bridge the gap between the hospital command center and the nurses. As a consequence, she sustained much stress. She had to be sensitive to members’ emotional status and respond accordingly to maintain high morale. Prior to this event, the team leader (H.‐L.L.) and the psychiatrist (S.‐H.L.) had worked collaboratively on another occasion. Because of this past partnership, the team leader was able to call for psychiatric help immediately when she noticed the increased irritability, inattention and withdrawal of some team members" (p357).
One study emphasised the importance of maximising social capital and fostering approaches to facilitate ways in which frontline workers could stay connected and informed to build a sense of ‘community’ that may contribute to implementation effectiveness: Chang 2006 described five approaches including "(1) designing workplaces so there is ample interaction among employees: Work space orientation, cubicle height, break room location, traffic flow patterns, etc., should all be examined with respect to increasing levels of communication and propinquity; (2) facilitating employee participation: Encouragement and incentives should be given to involve individuals in the larger institutional context via knowledge of specialty jargon, engagement in social functions, and acquisition of an oral history of the hospital; (3) taking steps to ensure a culture within the hospital that is supportive of social capital: Steps should be taken to implement an obvious, strategic plan that is preventive, not reactive. Best and worst‐case scenarios should be examined to cushion unexpected shocks during crisis outbreaks; (4) adopting hiring procedures to ensure new employees add social capital to the organization; and (5) emphasizing trust at the employee level" (p32).
Finding 8. Organisational incentives and rewards for frontline workers were seen as important in facilitating and engaging student healthcare workers and frontline staff with the intervention
We have low confidence in this evidence (Appendix 12).
Four studies reported the advantages of using incentives to facilitate and engage workers. Three reported on frontline professionals (Belfroid 2018; Chang 2006; Waterman 2018), and one on student healthcare workers (Ferranti 2016).
Waterman 2018 observed that "being provided with treatment itself did not seem to be motivation enough; group participants expected refreshments, and although they were reimbursed for travel, this did not provide substantial motivation" (p32). Ferranti 2016 noted a "substantial decrease in the number of student participants who completed the final survey from the base‐line measurement time point. This decrease aligned with the level of course credit or bonus points provided to students, indicating greater student motivation to complete the full program when credit was awarded in meaningful ways to students. Giving extra credit points could also be a limitation of the program findings as it may not be representative of students who did not need extra credit (i.e. students with better course grades). The challenge with implementing consistent bonus points was having differing courses over two separate semesters" (p603).
Finding 9. A positive learning climate for everyone involved in implementation of an intervention was seen to facilitate implementation
We have moderate confidence in this evidence (Appendix 12).
Eight studies identified creating a positive and safe learning climate as supporting implementation (Belfroid 2018; Brown‐Johnson 2020; Carvalho 2019; Chang 2006; Cheung 2015; Cunningham 2017; De Jong 2019; Lee 2005). Ensuring that all team members felt valued, and a part of the change process was an essential component. Belfroid 2018: "...protocols were often developed with the entire team, which made them feel that their opinion was important. They also felt that their supervisors valued their opinions" (p215). Chang 2006 pointed out that "social interaction alone is not enough; trust is also required in order to aid in discussing problems, obtaining affective and emotional support, sharing information, understanding the collective goals and proper ways of acting, and exchanging ideas in combating SARS and other similar crises" (p30). Allowing sufficient time and space for reflective thinking and evaluation was also an important part of building a safe learning climate. For example, Waterman 2018 found that "participants benefited from having a space to discuss their experiences with their peers and promote their capacity for self‐care" (p162).
Finding 10. Resource constraints, including lack of equipment, staff time and skills, were described as hindering implementation
We have moderate confidence in this evidence (Appendix 12).
A key factor underpinning organisational readiness for implementation was the availability of resources to deliver and implement an intervention (Belfroid 2018; Brown‐Johnson 2020; Cao 2020; Chang 2006; Chen 2020; Cunningham 2017; De Jong 2019; Waterman 2018).
A variety of resource constraints were described as hindering implementation, including lack of appropriate PPE (Brown‐Johnson 2020), lack of time (clinician and administration; Brown‐Johnson 2020), and competing demands for time as a result of an increased workload, or insufficient staffing levels, or both (Cao 2020), or a lack of experienced staff (De Jong 2019). Waterman 2018 describes having to reduce the number of training sessions, which meant having to condense the training. Consequently, "the participants wanted to drop off because they couldn't understand the sessions. I had less time to explain some important parts" (Waterman 2018, p32). Another study reported that resources required to implement the intervention that were readily available in a resource‐rich country were not always available (Cunningham 2017). Resource constraints were not just limited to the outset of a pandemic, but were also evident during the recovery phase, when healthcare workers had returned: "within the first few months, and specifically first 21 days following their return, some respondents voiced that they desired more psychosocial follow up from the organizations for which they worked: 'We were supposed to have been given some decompression time by the company that I went with and I did not experience any of that, so...you know, you're ‐ you're plucked down back in your environment and...pretty much left to figure it out for yourself' " (Cunningham 2017, p44).
Finding 11. Education, training and access to information for frontline workers was considered an important step in underpinning the readiness for implementation, and was seen to act as a barrier or facilitator depending on the quality provided
We have low confidence in this evidence (Appendix 12).
An important factor described in six studies, and closely linked to readiness for implementation, was the provision of education, training, and access to information about the intervention (Belfroid 2018; Chang 2006; Chen 2020; Cheung 2015; De Jong 2019Ferranti 2016). These were key in getting frontline workers to engage and embrace the intervention. Failure to provide high‐quality training negatively impacted on implementation as pointed out by De Jong 2019, "the limited training time had an impact on quality. For example, some short ToTs [training of trainer sessions] did not include any content on how to plan and deliver a training session. There was considerable variation in whether trainers received supervision as they delivered their first PFA training courses to others, or refresher training after they had started to train others... nature and quality of both the supervision and refresher training varied considerably ….providers who had not received supervision would have welcomed it, and trainers also felt that it was necessary...‘This will help everybody to know where the gaps are because if you have been trained and are not being supervised, you just continue to go you think that all is well. Probably there might be a gap you don’t know and if you would have been supervised the gap will be filled’ (Trainer, Liberia) ‘If you only come and train me today and you go, never to come and monitor what I’m doing, whether it’s right or not, it means that your training is in vain’ (Provider, Liberia)" (p8).
Access to knowledge and accurate information including facts about the disease and prevention was essential to support implementation. Cheung 2015 stated that a "lack of information and fear breed more rumours. This was the reason behind us including a short session to sensitise the frontline workers, including those who are responsible for contact tracing, health education and potential psychosocial support through telephone hotlines, about local perceptions and rumours related to the current outbreak" (p72). Other studies pointed out that frontline workers "in organizational crisis situations, ... face highly ambiguous situations and complex uncertainty" which can be overcome by providing timely information to reduce this additional stress (Chang 2006, p30). Frontline workers also benefited from "clear and simple protocols [that] helped them remain calm by using the instructions provided" (Belfroid 2018, p214).
CFIR Domain 4: individual characteristics (of frontline health and social care professionals)
Finding 12. Frontline workers' knowledge and beliefs about the intervention were seen to act as either a barrier or facilitator to implementation
We have moderate confidence in this evidence (Appendix 12).
Seven studies described knowledge and skill in using the intervention, coupled with healthcare workers' beliefs in the intervention as barriers and facilitators (Belfroid 2018; Blake 2020; Carvalho 2019; Chen 2020; Cunningham 2017; De Jong 2019; Waterman 2018). Four studies reported that a lack of knowledge of underlying principles or rationale for adopting the intervention, or inadequate knowledge of how to implement the intervention was a significant barrier, which could "lead health care workers to a false sense of security, which can pose a real risk to them" (Carvalho 2019, p259). One study pointed out that: "when people combine new skills with existing attitudes and beliefs, without having an empathic approach, there is a danger they could become involved in situations they are ill‐equipped to handle, and potentially do harm. For example, in Sierra Leone, it is common (and perhaps expected) that one would comfort a distressed person by promising that everything will be fine. This use of false reassurance ‘ultimately undermines the credibility and is counter‐productive’ (De Jong 2019, p9).
On the other hand, several studies described the enthusiastic use and adoption of an intervention as a result of a positive experience. Examples of frontline workers sharing their experiences about using the intervention in public or small groups were described, and reported as facilitating the implementation of the intervention (Blake 2020; Cunningham 2017; Waterman 2018). Blake 2020 reports that "following engagement with the package, they had already taken further actions (‘intervention enactment’) to emotionally support colleagues and family members, considered training in psychological first aid (PFA), called a telephone helpline, or engaged with advice around coping with emotions." (p12) and that frontline workers were observed "sharing the information in the following ways: circulating the package link around their clinical teams, colleagues and students; sharing the resource with external professional networks via email, print media, websites and social media; including a link to the digital package within their organisation’s COVID‐19 Staff Health and well‐being provisions; uploading the package to internal educational resource portals; printing posters and guidance documents (that were signposted from within the package) and placing them in shared areas such as staffrooms or noticeboards" (p13).
Finding 13. Frontline workers' confidence in their ability to deliver and implement an intervention was seen as an important factor in successful implementation
We have low confidence in this evidence (Appendix 12).
Frontline workers' self‐confidence was closely linked with their ability to deliver and implement an intervention (Belfroid 2018; Brown‐Johnson 2020; Carvalho 2019; Cunningham 2017; Ferranti 2016). Those who felt that they were well trained, and exhibited confidence in their own abilities, were more likely to use the intervention, even in challenging circumstances. As one nurse working in a university hospital reports "Well, we are well‐trained. Bring it on!" (Belfroid 2018, p215).
Finding 14. Individual personal characteristics and attributes of frontline professionals, such as their attitudes and motivation, were seen to act as either a barrier or facilitator to implementation
We have low confidence in this evidence (Appendix 12).
Seven studies reported that frontline professionals' characteristics could act as a barrier or a facilitator to the implementation of the intervention (Belfroid 2018; Chang 2006; Cheung 2015; Cunningham 2017; De Jong 2019; Lee 2005; Waterman 2018).
Multiple individual factors were described as an obstacle to implementation, including a lack of autonomy (Belfroid 2018), limited motivation to engage with the intervention (Waterman 2018), and competing needs of participants, for example, finding paid employment (Waterman 2018). Other studies reported that experience was also a significant barrier with: "providers with one to five years of professional experience scored significantly higher than their colleagues on the burnout scale when means of subgroups were compared. Also during the interviews, providers with less humanitarian experience expressed more bitterness and anger" (Cunningham 2017, p46). Experience also played an important role in the quality of the intervention that was delivered, as noted in De Jong 2019: "Respondents typically had little prior experience of MHPSS [Mental Health and Psychosocial Support] interventions and no experience of PFA. The ToTs were often short and rarely included content designed to develop training skills...The process of hearing and understanding new information – which may conflict with existing beliefs, attitudes, and behaviours – takes time, and additional time is needed to integrate this new material into a personal frame of understanding in order to teach it to someone else....As a result, the PFA training delivered during the EVD outbreak was of variable quality" (De Jong 2019, p9).
Literacy levels were also highlighted as a relevant factor. Waterman 2018 notes that "at the time of this study, the literacy rate in Sierra Leone was 65.72%. Although materials were adapted to be more appropriate for a lower literate population, validated adaptations of CBT materials for low‐literacy populations in general are lacking ... This likely must have impacted on participants' ability to engage with the sessions, and may therefore have reduced the effectiveness of the intervention overall" (p163).
Two studies reported that the willingness of a healthcare worker to volunteer was linked to successful implementation (Belfroid 2018; Cunningham 2017). Cunningham 2017 refers to this as their "psychological make‐up" and states that "women and men who volunteered, then, to help EVD patients may have been less prone to symptoms of [stress] by even showing a willingness to work in this context…" (p45). Lee 2005 (p356) reports that frontline workers could change their attitudes: "..some [workers] changed their attitudes and started facing their work more positively".
CFIR Domain 5: implementation process characteristics
Finding 15. Planning to prepare individual frontline workers and organisations to implement changes was often reported to be overlooked, resulting in frontline workers feeling rushed and unprepared. Strategic plans at the level of the individual healthcare worker and organisation were considered to facilitate the success of the implementation process
We have low confidence in this evidence (Appendix 12).
Planning effective implementation was reported as a barrier in four studies (Belfroid 2018; Brown‐Johnson 2020; Ferranti 2016; Waterman 2018) and as a facilitator in five studies (Belfroid 2018; Cao 2020; Chang 2006; Chen 2020; Klomp 2020).
Frontline workers reported that there was a lack of pre‐implementation planning, leading to concerns that the organisation was not fully prepared (Belfroid 2018). As Belfroid 2018 pointed out: "some HCWs regretted that they were unprepared for the fear and anxiety that they experienced. They said that training and simulation exercises focused mainly on technical guidance related to the pathogen and the transmission routes only. They focused on preventing transmission, whereas no attention was paid to mental well‐being in the preparation phase or during training sessions" (p216). They also expressed their concern at what they perceived as poor co‐ordination (Ferranti 2016); or being stressed at having to rush their preparations (Belfroid 2018). Brown‐Johnson reported that "preparing PPE Portraits or other humanizing approaches in anticipation of surges would have been much preferred" (p2241).
Chang 2006 argued that "steps should be taken to implement an obvious, strategic plan that is preventive, not reactive. Best and worst‐case scenarios should be examined to cushion unexpected shocks during crisis outbreaks" (p32). Evidence of different types of planning and preparation were described; including planning at the level of the individual healthcare worker; the organisation and both at the individual and organisational level. Studies pointed to the role of pre‐job training and the value of pre‐deployment assessment so that it gives "potential deployers the opportunity to proactively explore and prepare for some unintended consequences in the field. This includes fatigue or distress that might negatively impact their work and family dynamics while deployed. The intent was to improve their professional and personal success and happiness in the field" (Klomp 2020, p74). Other studies reported that organisations would only admit a high‐risk infectious patient once all of the preparatory work had been completed, and the relevant healthcare staff had been fully briefed (Belfroid 2018; Chen 2020).
Finding 16. Meaningful engagement of people involved in the delivery of interventions to support mental health, and forming strong collaborations with champions and opinion leaders, was seen to positively impact on implementation
We have low confidence in this evidence (Appendix 12).
Eight studies described the importance of early engagement with frontline workers who were tasked with delivering the intervention (Belfroid 2018; Blake 2020; Brown‐Johnson 2020; Cunningham 2017; Klomp 2020; Lee 2005; Son 2019; Waterman 2018). Engagement was multi‐level; described across all levels of an organisation and also negotiated externally and involved new users (Blake 2020), champions (Blake 2020; Cunningham 2017; Lee 2005), and local opinion leaders (Belfroid 2018; Brown‐Johnson 2020; Klomp 2020; Waterman 2018). Waterman 2018 described the benefit of engaging 'new users' stating that: "CBT was a new experience for them and a new process of learning...the more interested ones answered more questions and were faster to manage their depression" (p32).
Three studies reported that engaging frontline workers who were committed to the intervention to act as advocates or champions helped to embed the intervention (Blake 2020; Cunningham 2017; Lee 2005). For example, Lee 2005 describes the reduction in anxiety of the psychiatric team when volunteering to support members of the SARS team because of the help of the SARS team leader who "arranged an independent, safe and quiet meeting place for the debriefing groups and took proper protective measures to make all the participants, including the psychiatrists and psychologists, feel secure and relaxed" (p357).
Frontline workers also described the value of involving opinion leaders in the implementation of an intervention in three studies (Belfroid 2018; Brown‐Johnson 2020; Waterman 2018). One study described the influence of traditional healers in Sierra Leone who: "often command more respect than trained health personnel who are less familiar" (p163). The study authors concluded that the ability of local opinion leaders to influence attitudes and behaviours was key to successful implementation stating that "involving traditional healers in the development and delivery of mental health interventions in the future may provide more holistic care for the clients, as well as promoting engagement through sources they trust" (Waterman 2018, p163).
Finding 17. The opportunity for frontline workers to reflect on, evaluate or take part in a debriefing session was seen to promote a sense of safety, and to support a shared learning which facilitated the implementation process
We have low confidence in this evidence (Appendix 12).
Debriefing allows dedicated time for individual frontline workers, teams and their organisation to reflect on what aspects of the intervention worked well and those that did not. As Carvalho 2019 points out: "debriefing was used during and after every training session, trying to reinforce good points in the performance and change those that could be improved, promoting reflective learning" (p260).
A lack of ongoing review or evaluation about the progress of the implementation negatively impacted on the implementation process. For example, in De Jong 2019: "Wherever you go they say a lot of trainings have been done .... But you find out that no supervision has been done nor evaluation has been done ... some people come in and say they are doing PFA but ... you ask a few questions and they cannot even understand and yet they say they have done PFA. So you realise the quality of PFA has been diluted because of lack of supervision, and lack of proper monitoring and evaluation of the process" (p9).
Frontline workers reported that having time to reflect on, or take part in a debriefing session (before or after) the intervention was implemented was beneficial, and gave them the opportunity to build on skills and knowledge, and a chance to share input and feedback with their peers (Belfroid 2018; Blake 2020; Carvalho 2019; Cunningham 2017; De Jong 2019; Klomp 2020). Pre‐arrival briefings were described as allowing frontline workers to "prepare mentally" (Belfroid 2018, p214). They reported that the majority of "healthcare organizations had a debriefing after the dismissal of each patient, which the HCWs appreciated because it served as an outlet, and protocols could be adjusted if necessary" (p214). De Jong 2019 states that "staff who received this PFA training showed greater understanding of applying psychosocial support strategies in response to scenarios of patients affected by acute crisis. That this effect was apparent only at follow‐up rather than immediately post‐training may suggest that the opportunity to put learning into practice was key in establishing this capability (p9)". Frontline workers also observed that they felt "safe seeing their organization continuously reviewing and improving procedures, securing the availability of all necessary materials, and taking steps to obtain the safest personal protective equipment possible" (Belfroid 2018, p214).
Debriefing and evaluation was also important to the organisation, particularly when implementation activities had ceased. Klomp 2020 reports that: "benefit of the outreach was that it served as a consistent, unobtrusive vehicle through which the CDC could emphasize the organization’s gratitude for personal and professional sacrifices and contributions made during the Ebola response. It reminded them about the meaningfulness of their professional contributions in the field and provided an additional opportunity for deployers to connect with supportive resources, if needed" (p74).
Discussion
See Table 1 for a summary of the main findings from the review of effectiveness (objective 1), and Table 2 for a summary of the main findings from the qualitative evidence synthesis (objective 2).
Summary of main results
We included 16 studies that reported implementation of an intervention aimed at supporting the resilience and mental health of frontline health and social care professionals during disease outbreaks (SARS: 2 studies; Ebola: 9 studies; MERS: 1 study, COVID‐19: 4 studies). The interventions studied included workplace interventions (such as training, structure and communication: 6 studies); psychological support interventions (such as counselling and psychology services: 8 studies); and multifaceted interventions (2 studies).
Effectiveness of interventions (objective 1)
We only identified one study that investigated the effect of an intervention to support the resilience and mental health of frontline health and social care professionals. We do not know whether training frontline workers to deliver psychological first aid has any effect on burnout because the certainty of this evidence is very low. Conclusions are limited by study quality.
We included no other quantitative studies that investigated the effect of any other intervention to support the resilience and mental health of frontline health and social care professionals.
Qualitative evidence synthesis (objective 2)
We identified 17 findings, from 16 studies, that described barriers and facilitators to the implementation of interventions aimed at supporting the resilience and mental health of frontline health and social care professionals, mapped across the five domains of the CFIR framework. Key findings are summarised below.
Barriers to implementation (2 findings)
Finding 4. Lack of awareness about the needs and resources of frontline workers was seen as a barrier to implementation. This included lack of awareness of frontline workers of their own needs, and lack of awareness of organisations that employed and supported frontline workers (Belfroid 2018; Cao 2020; Chang 2006; Chen 2020; Cheung 2015; Cunningham 2017; De Jong 2019; Ferranti 2016; Klomp 2020; Lee 2005; Schreiber 2019; Waterman 2018; moderate confidence).
Finding 10. Resource constraints, including lack of equipment, staff time and skills, were described as hindering implementation (Belfroid 2018; Brown‐Johnson 2020; Cao 2020; Chang 2006; Chen 2020; Cunningham 2017; De Jong 2019; Waterman 2018; moderate confidence).
Facilitators to implementation (9 findings)
Finding 1. Flexible interventions that were culturally appropriate, adaptable and/or able to be tailored to meet local needs were seen as key to successful implementation (Blake 2020; Brown‐Johnson 2020; Cheung 2015; De Jong 2019; Ferranti 2016; Schreiber 2019; Waterman 2018; moderate confidence).
Finding 2. Interventions characterised as having a low level of complexity were seen as easier to implement (Blake 2020; Brown‐Johnson 2020; Ferranti 2016; Son 2019; low confidence).
Finding 5. Awareness of mental health needs by governments and political leaders was identified as a facilitator (Cheung 2015; Klomp 2020; very low confidence).
Finding 7. Effective communication, and cohesion through horizontal and vertical networks, was seen to strengthen social capital and improve team resilience and was considered to be a key factor in implementation (Belfroid 2018; Blake 2020; Cao 2020; Chang 2006; Cheung 2015; Cunningham 2017; Klomp 2020; Lee 2005; moderate confidence).
Finding 8. Organisational incentives and rewards for frontline workers were seen as important in facilitating and engaging student healthcare workers and frontline staff with the intervention (Belfroid 2018; Chang 2006; Ferranti 2016; Waterman 2018; low confidence).
Finding 9. A positive learning climate for everyone involved in implementation of an intervention was seen to facilitate implementation (Belfroid 2018; Brown‐Johnson 2020; Carvalho 2019; Chang 2006; Cheung 2015; Cunningham 2017; De Jong 2019; Lee 2005; moderate confidence).
Finding 13. Frontline workers' confidence in their ability to deliver and implement an intervention was seen as an important factor in successful implementation (Belfroid 2018; Brown‐Johnson 2020;Carvalho 2019; Cunningham 2017; Ferranti 2016; low confidence).
Finding 16. Meaningful engagement of people involved in the delivery of interventions to support mental health, and forming strong collaborations with champions and opinion leaders, was seen to positively impact on implementation (Belfroid 2018; Blake 2020; Brown‐Johnson 2020;Cunningham 2017;Klomp 2020; Lee 2005;Son 2019; Waterman 2018; low confidence).
Finding 17. The opportunity for frontline workers to reflect on, evaluate or take part in a debriefing session was seen to promote a sense of safety, and support a shared learning, which facilitated the implementation process (Belfroid 2018; Blake 2020;Carvalho 2019; Cunningham 2017;De Jong 2019; Klomp 2020; low confidence).
Combined barriers and facilitators (6 findings)
Finding 3. Intervention costs and associated costs of implementing the intervention was seen as both hindering and facilitating implementation (Blake 2020; De Jong 2019; low confidence).
Finding 6. Networking between organisations involved in providing frontline services, and co‐ordinating multiple external organisations in a crisis was seen as both a barrier and a facilitator to implementation (Blake 2020; Cheung 2015; De Jong 2019; low confidence).
Finding 11. Education, training, and access to information for frontline workers was considered an important step underpinning the readiness for implementation, and was seen to act as a barrier or facilitator depending on the quality provided (Belfroid 2018; Chang 2006; Chen 2020; Cheung 2015; De Jong 2019; Ferranti 2016; low confidence).
Finding 12. Frontline workers' knowledge and beliefs about the intervention were seen to act as either a barrier or facilitator to implementation (Belfroid 2018; Blake 2020; Carvalho 2019; Chen 2020; Cunningham 2017; De Jong 2019; Waterman 2018; moderate confidence).
Finding 14. Individual personal characteristics and attributes of frontline professionals, such as their attitudes and motivation, were seen to act as either a barrier or facilitator to implementation (Belfroid 2018; Chang 2006; Cheung 2015; Cunningham 2017; De Jong 2019; Lee 2005; Waterman 2018; low confidence).
Finding 15. Planning to prepare individual frontline workers and organisations to implement changes was often reported to be overlooked, resulting in frontline workers feeling rushed and unprepared. Strategic plans at the level of the individual healthcare worker and organisation were considered to facilitate the success of the implementation (Belfroid 2018; Brown‐Johnson 2020; Cao 2020; Chang 2006; Chen 2020; Ferranti 2016; Klomp 2020; Waterman 2018; low confidence).
Overall completeness and applicability of evidence
This review includes studies focused on interventions aimed at supporting the resilience and mental health of health and social care professionals working at the front line during disease outbreaks, epidemics or pandemics, from the year 2002 onwards. We used detailed operational definitions to judge eligibility. However, in some cases it was difficult to establish what constitutes an intervention, whether it can really be defined as an intervention or something else, for example, a behaviour or reaction to a given context. We found that in several cases, prompted by the urgent desire to share study findings during what was perceived as periods of healthcare crisis, studies were reported within brief commentaries, letters or editorials. Whilst we had a comprehensive search strategy and methods, this manner of reporting reduces our confidence that we found all relevant research.
Many of the included studies reported on interventions that had been deployed at short notice in response to the start of an epidemic or pandemic. The urgency with which interventions were implemented meant that some of the key steps in intervention delivery such as planning, assessing readiness for change, appropriateness of the intervention, and how best to engage participants in the intervention were not possible or not reported. The immediacy of implementation arguably limits completeness and is itself a significant barrier to successful intervention implementation. It would seem evident that in some studies the implementation of an intervention was in response to the start of an epidemic or pandemic. The urgency brought about by this situation seems to have resulted in ad hoc solutions and strategies, rather than evidence‐based interventions, often attempted in the spirit of 'something is better than nothing'. In some cases, the interventions that have been implemented could be considered 'common sense' reactions to a situation, rather than carefully selected evidence‐based interventions that are known to provide solutions to given problems in specific contexts. It is possible that interventions may have been delivered differently or indeed, entirely different interventions may have been deemed more suitable, had time for reflection, pre‐delivery, been possible. Furthermore, the perceived urgency, and need to implement 'something' to support frontline workers, means that the priority was arguably delivery of the intervention, rather than formal evaluation of the effect or impact of the intervention. Consequently, many of the studies included in this review are unlikely to have had preconceived protocols, or clearly formed research questions, participants or outcomes, and this inevitably impacts on the completeness of the study information and results data.
Participants in the majority of studies were healthcare professionals (mainly doctors and nurses). In some cases the profession of the participants was unclear, with studies referring to wider populations of hospital workers. Despite a comprehensive search, we found only one study that stated that social workers were amongst the recruited professionals (De Jong 2019), but we found no studies specifically focused on social care professionals, and no studies that considered health or social care professionals who were returning to practice after a period of absence (this group of professionals being actively recruited to return to work during the COVID‐19 crisis). This suggests that there is currently a gap in evidence relating to the resilience and mental health of social care professionals and professionals returning to practice in order to work at the front line during disease epidemics or pandemics.
Many of the studies provided an in‐depth description of the local context in which frontline workers were operating. The context was often perceived to be one of 'disaster', with challenging working environments that were considered difficult and stressful to be in. When extracting data relating to the barriers and facilitators to successful implementation of interventions it was at times difficult to distinguish between the barriers and facilitators to operating in such a challenging work environment, and the barriers and facilitators to implementing an intervention to support the mental health of the people in that environment.
During our searching we identified, and excluded, several studies that specifically related to 'preparedness' for disease epidemics and pandemics, and also studies relating to interventions to support the resilience and mental health of frontline workers during other healthcare crises (for example, after natural disasters or terrorist attacks). Whilst these studies did not meet the predefined criteria for our review, we anticipate that systematic synthesis of these studies would enhance the completeness of evidence to inform decisions relating to the effectiveness and barriers and facilitators to implementation of interventions to support resilience and mental health of frontline workers.
While this review synthesises evidence from a range of disease outbreaks, epidemics and pandemics, it was carried out in response to the COVID‐19 pandemic. It is therefore important to consider the applicability of evidence from different diseases, and interventions delivered in a wide range of contexts, to COVID‐19. As COVID‐19 is a global pandemic, evidence arising from all geographical contexts is likely to have some relevance. Thus, whilst some of the evidence relating to the need for culturally appropriate training, and differing cultural conceptualisations of mental health (see, for example, Finding 1: flexible interventions that were culturally appropriate, adaptable and/or able to be tailored to meet local needs were seen as key to successful implementation) may not be generalisable to all global settings, it is likely to be applicable in some local contexts. The nature of the transmission of COVID‐19, and the resultant governmental restrictions on international and national travel and movement in many parts of the world, may limit the applicability of some evidence. For example, evidence relating to the deployment of 'aid workers' or volunteers from one part of the world to another, such as occurred during the Ebola outbreak. However, we found that many barriers and facilitators were common to several studies, and that these arose from a number of different disease outbreaks, highlighting similarities and increasing our confidence that many of the findings are directly applicable to the COVID‐19 pandemic.
While we identified barriers and facilitators that were common to several studies, these came from studies that focused on specific types of interventions (as well as specific diseases and settings, as discussed above). This created challenges during the synthesis of qualitative evidence, and the decision to summarise evidence across studies may have lost some important links to specific interventions, diseases and settings. While the identified barriers and facilitators were common to several studies, which all had varied interventions, it is possible that some findings may potentially be more applicable to some interventions than others.
Certainty/confidence in the evidence
As discussed above, we identified a range of limitations to the evidence included in this review. We only identified one quantitative study, and we have very low certainty in the evidence arising from this, meaning that we are unable to reach any conclusions about the effectiveness of interventions to support resilience and mental health of frontline health and social care professionals during or after disease epidemics or pandemics. While we found a number of consistent findings relating to barriers and facilitators to implementation of interventions to support resilience and mental health, our confidence in the evidence of the majority of these findings was low or very low (11 of 17 findings). We did not have high confidence in any of the findings. We had moderate confidence in six of our 17 findings (see Table 2).
Potential biases in the review process
Despite the rapid nature of this review, we aimed to search electronic databases comprehensively. However there were some limitations to our searching of other resources. We encountered problems searching the WHO ICTRP database, meaning that we were unable to complete our planned search of this database and we have missed some ongoing studies. During the COVID‐19 pandemic there were rapid publications of many papers, which presented challenges to identification of all relevant papers relating to COVID‐19. While we handsearched lists of included studies from relevant systematic reviews and narrative literature reviews, we did not conduct any additional handsearching. This included handsearching of reference lists of included studies and forward citation searching. This may mean that we failed to identify some studies relating to COVID‐19. However, due to the timescale of the pandemic and this review, it is most likely that these would be ongoing studies and ‐ as such ‐ failure to identify these should not have impacted on the conclusions made within this first version of this review. It will be important to identify all of these for future updates of this review. Furthermore, we identified and included a number of preprint publications, which had not yet been peer‐reviewed. Future updates should include the peer‐reviewed versions of these preprints.
Several of the studies included in the qualitative evidence synthesis were not presented as 'standard' reports of qualitative studies, with descriptions of study designs, interventions, participants and barriers and facilitators to implementation provided within narrative commentaries. Decisions to include these papers sometimes involved subjective decision making. Decisions were made through discussion between two or three review authors, and we aimed for transparent reporting of these decisions. Whilst we aimed for inclusivity, the nature of the narrative reporting of some studies within commentaries and editorials means that there is a risk that we may have excluded some potentially relevant studies during the title and abstract screening stages. Furthermore, there is therefore a risk that some of our decisions relating to these 'narrative' papers were influenced by the comprehensiveness of reporting of study details and results, and that we may have excluded some potentially relevant studies that were reported within narrative texts. Where we were uncertain we aimed to err on the side of caution and categorised studies as 'awaiting classification', in order to seek further information from the authors. Due to the timescale of this review, those studies where we require further information remain as 'awaiting classification'; had we had a longer period of time within which to complete this review, inclusion decisions could have been finalised and additional studies may have been included in this review.
We aimed to adopt rigorous methods, and two independent review authors did complete the majority of review tasks, with differences resolved through discussion (e.g. applying selection criteria, data extraction, assessment of risk of bias of quantitative studies). However, due to the rapid nature of this review, for the assessment of methodological limitations of qualitative studies and the final application of GRADE‐CERQual, a single review author conducted the assessments and entered data into Review Manager 5 (Review Manager 2020). All these assessments were checked by a second review author. However, we acknowledge that this approach is not as rigorous as using two independent review authors, and this may potentially have introduced bias into the review.
Our review question and objectives were focused on interventions delivered 'during' or 'following' a disease outbreak, epidemic or pandemic. Our eligibility criteria therefore excluded studies focused on 'preparedness', as we considered this to occur 'before' the disease outbreak. This led to a need to judge the time point at which an intervention was delivered in relation to a disease outbreak, and this was at times challenging. Furthermore, we also excluded a number of studies that focused on interventions to support the mental health and resilience of frontline workers during a range of health emergencies (often including, but not limited to, disease pandemics). While we adhered to our pre‐planned eligibility criteria and objectives, we felt that we were potentially excluding a number of key studies that could offer important evidence; for example, evidence relating to barriers and facilitators of the planning process, such as advance planning and resource allocation in preparation for a disease pandemic. We do not consider that this will have introduced bias into the review process, however it is possible that we have excluded important components of wider evidence, meaning that results and conclusions are not based on all relevant evidence. We recommend that future updates of this review consider expanding the inclusion criteria to include the body of evidence relating to preparation for disease outbreaks, epidemics or pandemics, and evidence from health emergencies other than disease outbreaks, epidemics or pandemics (e.g. natural disasters).
Reflexivity
While this review was carried out rapidly (within four months), we adopted systematic and rigorous methods at all stages of the review process. The review protocol was developed with input from an international advisory group and was reviewed and approved by Cochrane (see Appendix 15). The author team were assembled quickly to respond to a call from the Scottish Government for proposals for rapid research studies that had the potential to inform the government's response to the COVID‐19 crisis. The author team were all experienced in systematic reviews, with expertise in a range of different types of reviews, including Cochrane quantitative reviews and qualitative evidence syntheses. Members of the author team had research expertise relating to mental health, and represented a wide range of healthcare professionals (with the majority of the author team being based at the Scottish Government‐funded 'Nursing, Midwifery and Allied Health Professions Research Unit'). A wider advisory group was also quickly assembled. This group comprised people who proactively contacted the lead review author to offer support to the review (either after seeing the registered title for a Cochrane rapid review, or seeing Scottish Government funding announcement), and members recruited though the Cochrane Consumers COVID‐19 rapid review panel. This group represents diverse professional and geographical backgrounds, including frontline healthcare professionals within the COVID‐19 pandemic and earlier epidemics (e.g. Ebola). All members of the team had an interest in synthesising the evidence in relation to the impact of COVID‐19 on the mental health and well‐being of health and social care professionals, in order to urgently identify optimal ways of supporting frontline workers who are working in highly stressful circumstances. However, while there was engagement and involvement of this group at the start of the review, with considerable input at the protocol stage, and with some individual members providing substantial input during the searching and selection of studies stage, the involvement during stages of data extraction and synthesis was considerably less. This was due to the review team lacking the time to maintain communication and involvement with this group of people. However, all group members were invited to comment on a pre‐publication version of the review, and a number of changes were made in response to these peer‐review comments.
Throughout this review, members of the review team and the wider advisory group were aware of making decisions that excluded evidence that could potentially be highly relevant to identifying effective interventions to support the mental health and resilience of frontline workers. The team had several discussions throughout the review process about these exclusions, with particular concerns relating to the exclusion of evidence relating to 'non‐professional' frontline workers (e.g. cleaners, porters), the exclusion of evidence relating to preparedness for disease epidemics and pandemics, and the exclusion of evidence arising from health emergencies other than disease outbreaks, epidemics or pandemics. The rapid timeline for this review led to the decision that it was not possible to expand the scope of the review; however these exclusions remained a concern to the author team and advisory group, and expanding the scope of this review during future updates is considered important.
The review team experienced a number of challenges in reaching decisions about inclusion of some papers, particularly papers that were describing barriers and facilitators to implementation of an intervention, but for which there was not a clear pre‐planned study design. Review authors reported that they found that some decisions were complex, and made difficult by lack of information, and that they were sometimes uncertain as to whether some narrative reports were describing results of a study that investigated an intervention. At the early, screening, stage of the review, multiple review authors were involved, and this prompted a number of discussions between review authors who raised concerns about whether or not they were applying inclusion criteria consistently. However, the lack of time and need to complete this stage rapidly limited opportunities for in‐depth discussion between the whole team.
The review team were aware that the rapid nature of the review did impact on opportunities for reflection, particularly during the qualitative evidence synthesis. While two review authors did independently extract and code the qualitative data, and final codes were agreed through discussion, these review authors both felt that they had limited opportunities to pause, reflect and discuss the themes arising from the review in depth. This stage of qualitative evidence synthesis would have been useful, promoting opportunities for sense checking, reflection and rumination over findings. Several of the workplace interventions that were identified were multifaceted and were not specifically, or only, aimed at supporting the mental well‐being and resilience of the frontline workers. Often these interventions were also aimed at improving patient care and patient outcomes, and the 'benefit' to the frontline workers was perhaps secondary. The multifaceted nature of these interventions, which could potentially act on an individual frontline worker, a wider workforce, an organisation, and on patients, created challenges to extracting barriers and facilitators to an intervention. Sometimes review authors found it difficult to unpick whether identified barriers and facilitators were relevant to the impact of the intervention on the mental health and resilience of frontline workers. As stated earlier, the lack of time limited opportunities to reflect on these issues and the impact on the themes and findings arising from the evidence.
Agreements and disagreements with other studies or reviews
As outlined in Excluded studies and Table 7, our searching identified three systematic reviews that had similar (although not the same) aims, inclusion criteria and search dates to this Cochrane Review (Cabello 2020; Robertson 2020; Stuijfzand 2020). Our review is in broad agreement with these other systematic reviews: Cabello 2020 identified five studies that "described different interventions to reduce the mental health impact of viral outbreaks in HCWs [healthcare workers]". These studies included one that we included (Schreiber 2019); and two that were specifically focused on preparedness for a disease outbreak and two that did not have study designs that met our criteria for inclusion and that were therefore excluded from our review. Cabello 2020 concludes that there is "limited evidence regarding the impact of interventions", which is in agreement with our findings. Robertson 2020 did not identify any effectiveness studies, but concluded that there were a number of workplace, social, and individual factors that could be risk and protective factors for mental health conditions. While wider in focus than 'interventions', these factors include similar themes as are covered within our qualitative evidence synthesis (such as the need for flexibility and effective communication). Stuijfzand 2020 identified five studies that investigated the effect of "preventative programmes or interventions". These reviews included two studies that we included (De Jong 2019; Waterman 2018), one that we excluded based on study design (Chen 2006), and two that we excluded as they were focused on preparedness (Marrs 2020; Maunder 2010). In agreement with our review, and that of Cabello 2020 and Robertson 2020, Stuijfzand 2020 concluded that "few evidence‐based early interventions exist so far".
Authors' conclusions
Implications for practice.
There is a lack of evidence from studies carried out during or after disease outbreaks, epidemics or pandemics that can inform the selection of interventions that are beneficial to the resilience and mental health of frontline health and social care professionals. Alternative sources of evidence, such as evidence arising from other healthcare crises, and general evidence relating to the effectiveness of interventions to support mental well‐being during stressful situations, should therefore be used to inform decision making. When selecting interventions aimed at supporting the mental health of frontline health and social care workers, organisational, social, personal, and psychological factors may all be important.
Based on findings from the review that we have moderate confidence in, we have developed the following set of questions that may support the selection and successful implementation of interventions to support the mental health and resilience of frontline health and social care professionals.
Selecting an intervention
Is the intervention flexible, with ability to be tailored to meet local needs?
Are the needs and resources of the frontline workers known (known to the frontline workers and to their employers/organisations)?
Planning organisational factors
Are there effective networks of communication (both formal and social networks)?
Is there a positive, safe and supportive learning environment for the frontline workers (for example, for learning new skills related to caring for patients with the disease)?
Is there adequate resourcing, including necessary equipment, staff time and skills, for the intervention?
Individual characteristics of frontline staff
Do frontline staff have adequate knowledge relating to, and belief in, the intervention?
Based on findings from the review that we have low or very low confidence in, we have identified the following additional factors that may have implications for practice.
Complexity of the intervention (low‐complexity interventions may be easier to implement)
Intervention costs and associated costs of implementing the intervention
Government and political leaders' awareness of mental health needs of frontline workers
Networking and co‐ordination of different relevant organisations
Organisational incentives and rewards for frontline workers may facilitate engagement in the intervention
Education, training and access to information for frontline workers about the intervention)
Confidence of people delivering the intervention
Individual personal characteristics of workers, such as attitudes and motivation
Strategic planning prior to implementation of an intervention or changes to practice
Meaningful engagement of, and collaborations with, people involved in the delivery of the intervention, and opinion leaders who can champion the intervention
Providing frontline workers with opportunities to reflect on the implementation of an intervention
It is important to note that these implications are based on findings based on the implementation of a range of different interventions, delivered in a variety of contexts. As such, the importance of these factors may differ with different interventions and in different settings.
Implications for research.
We have found a lack of research evidence relating to the effectiveness of interventions to support the resilience and mental health of frontline workers during disease epidemics or pandemics. Given the ongoing COVID‐19 pandemic and the recognised negative impact on frontline workers, research to determine the effectiveness of interventions to support the resilience and mental health of frontline health and social care workers during disease epidemics or pandemics is a high priority.
Despite the continued challenges of the global COVID‐19 pandemic, this provides unique opportunities for robust evaluation of interventions. It is essential that any future studies are developed with appropriately rigorous planning, including development, peer review and transparent reporting of research protocols, following guidance and standards for best practice (e.g. SPIRIT and CONSORT reporting guidelines for randomised trial protocols and studies), and planning for appropriate follow‐up. Given the large numbers of health and social care workers who will have experienced stress and anxiety associated with frontline COVID‐19 work, it is important to work in partnership with these people to identify and prioritise interventions and outcomes of greatest importance. In doing so, careful consideration will need to be given to the burden placed on frontline workers, planning research so that it is not perceived to place additional workload or stress on individuals, organisations or on limited resources.
There are a range of different types of interventions that could be researched. There is currently no empirical evidence of effectiveness to help prioritise interventions for research. Interventions that have been implemented during disease epidemics or pandemics include workplace and psychological support interventions. It will be important to consider issues such as intervention acceptability, required resources, cost, theoretical justification, feasibility, and potential for harm when selecting interventions to research. Many of the potential interventions will be complex; this makes clear description of the intervention essential, in order that (if effective) it can be replicated in other settings.
Participants in the majority of studies were healthcare professionals (mainly doctors and nurses). We found no studies focused on social care professionals, and no studies that considered health or social care professionals who were returning to practice after a period of absence (this group of professionals being actively recruited to return to work during the COVID‐19 crisis). Future research should be planned to address the mental health and resilience of social care workers, professionals returning to practice after a period of absence, and students entering practice early during a disease pandemic. Furthermore, although this rapid review focused specifically on health and social care professionals, the majority of a health and social care workforce will be employed within wider roles, such as administration (e.g. receptionist), domestic services (e.g. cleaner), or support services (e.g. porter); within the UK this is estimated to be more than 90% of the workforce (NHS England 2020). The health and well‐being of all of these frontline workers is fundamental to the response to the COVID‐19 pandemic, and any adverse effects on these workers will have a profound impact at multiple levels, from the individual worker to the entire health and social care system. Future research should consider the mental health and resilience of this wider workforce. We recommend that future updates of this Cochrane Review consider expanding the inclusion criteria to include evidence relating to this wider group of workers. Given the relatively low volume of evidence included in this Cochrane Review, we also recommend that within future updates consideration is given to expanding the eligibility criteria to include evidence relating to preparedness of disease outbreaks, and relevant evidence arising from other health emergencies (such as natural disasters).
Given the uncertainties relating to COVID‐19, and the potential for other global disease pandemics in the future, research should consider the long‐term sustainability of interventions, and long‐term outcomes. Outcomes assessed should include the resilience and mental health of individuals, as well as the functioning of organisations, and the wider impact on patient care.
History
Review first published: Issue 11, 2020
Acknowledgements
This systematic review is supported by an Advisory Group. The following Advisory Group members read and provided comments on drafts of the protocol, and were invited to comment on a draft of the completed review (listed alphabetically): Ms Laura Boeira, Veredas Institute, Brazil; Dr Andrew Booth, University of Sheffield, UK; Mr James Chan, Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences, University of Oxford; Stoke Mandeville Hospital, Buckinghamshire Healthcare NHS Trust; Dr Mark Delicata, Victoria Hospital, Kirkcaldy, NHS Fife, UK; Dr David Gillespie, Royal Infirmary Edinburgh, NHS Lothian, UK; Dr Sohil Khan, Griffith University, Australia; Dr Terry Quinn, Institute of Cardiovascular and Medical Sciences, University of Glasgow, UK; Prof AG Radhika, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India; Prof Valéry Ridde, French Institute for Research on Sustainable Development, Paris; Dr Lesley Robertson, University of the Witwatersrand, Johannesburg, South Africa; Dr Abi Sriharan, Dalla Lana School of Public Health, University of Toronto; Prof Balendra Pratap Singh, King George’s Medical University, India; and Dr Ali Zamlout, Tishreen University, Latakia, Syria. The following additional members joined the Advisory Group after the protocol was finalised, and were invited to comment on a draft of the completed review: Mr Justin Williams, University of Aberdeen, UK and Dr Latha T, MAHE Manipal, Karntaka, India. In addition, the following members of the Advisory Group contributed to screening and identification of studies for inclusion in the review: Ms Laura Boeira, Prof AG Radhika, Dr Latha T and Dr Ali Zamlout.
Robin Featherstone, Cochrane, provided peer review feedback and comments on the search strategy for this review.
A complete draft of this review was peer reviewed by: EPOC editors (Claire Glenton, Signe Flottorp, Simon Lewin), Liz Paulsen (EPOC Managing Editor); Cochrane EMD editor (Rachel Richardson) and Cochrane EMD Managing Editors (Helen Wakeford and Clare Dooley). Peer referees: Andrew Rix (retired organisational and work psychologist), Professor Graeme D Smith (Professor of Nursing, School of Health Sciences, Caritas Institute of Higher Education, Hong Kong), Karen Daniels, Professor Abdullah E Laher (Department of Emergency Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa).
Text from the 'EPOC qualitative evidence synthesis: protocol and review template’ has been used for this review (EPOC 2019).
Appendices
Appendix 1. MEDLINE (Ovid) search strategy
1. exp mental fatigue/ or exp stress, psychological/ or resilience, psychological/ or exp occupational stress/
2. depression/ or anxiety/
3. mental health/ or anxiety disorders/ or panic disorder/ or exp "bipolar and related disorders"/ or mood disorders/ or depressive disorder/ or depressive disorder, major/ or depressive disorder, treatment‐resistant/ or "trauma and stressor related disorders"/ or adjustment disorders/ or stress disorders, traumatic/ or exp psychological trauma/ or stress disorders, post‐traumatic/ or stress disorders, traumatic, acute/
4. adaptation, psychological/ or help‐seeking behavior/
5. substance‐related disorders/ or alcohol‐related disorders/ or alcoholic intoxication/ or alcoholism/ or "tobacco use disorder"/
6. ((mental or psychological or psychosocial or psycho‐social or emotional) adj3 (condition$ or health or care or condition or factor or help or state or status or stability or instability)).tw.
7. (((post‐traumatic or posttraumatic or trauma$) adj3 (disorder or neurosis or psychos$ or syndrome)) or PTSD or traumati?ed or traumatic).tw.
8. motivation/
9. (depress$ or anxious$ or anxiety or panic$ or hysteria or stress or (chronic adj2 fatigue) or suicid$ or ((affective$ or mood or mental) adj2 (disorder$ or health))).tw.
10. (burnout or burn‐out or cope or coping or adaption or catastrophi?ing or depersonali?ation or resilience or hope$ or anger or apath$ or bereave$ or grief or sadness or distress$ or fear$ or frustrat$ or guilt or shame or hope$ or loneliness or sadness or motivat$ or confusion or empathy or ((unable or difficult$) adj3 (sleep$ or focus$)) or eagerness or enthusiasm or goodwill or keenness or resolve or toughness or volition or well‐being or wellbeing or willing$ or willpower or wish$).tw.
11. or/1‐10
12. health personnel/ or allied health personnel/ or community health workers/ or emergency medical technicians/ or home health aides/ or licensed practical nurses/ or nursing assistants/ or operating room technicians/ or physical therapist assistants/ or exp physician assistants/ or exp anesthetists/ or audiologists/ or caregivers/ or "coroners and medical examiners"/ or exp dental staff/ or dentists/ or emergency medical dispatcher/ or epidemiologists/ or exp health facility administrators/ or infection control practitioners/ or medical laboratory personnel/ or exp medical staff/ or exp nurses/ or exp nursing staff/ or nutritionists/ or occupational therapists/ or optometrists/ or exp personnel, hospital/ or pharmacists/ or physical therapists/ or exp physicians/
13. students/ or exp students, health occupations/ or volunteers/ or hospital volunteers/
14. ((clinical or healthcare or health care or (operating adj3 (room or theat$ or department$)) or hospital or laborator$ or biomedical or medical or surgical or pharmacy or social or community) adj3 (auxilliar$ or practitioner$ or professional$ or provider$ or worker$ or personnel or dispenser$ or aides or workforce or consultant$ or student$ or technician$ or scientist$ or volunteer$)).tw.
15. (an?esthesiologist$ or an?esthetist or cardiologist$ or dermatologist$ or diabetologist$ or doctor$ or endocrinologist$ or epileptologist$ or gastroenterologist$ or (general adj2 practitioner) or GP or geriatrician$ or gerontologist$ or gyn?ecologist$ or h?ematologist$ or (h?ematolog$ adj2 specialist$) or hepatologist$ or immunologist$ or (infectious adj2 diseas$ adj2 specialist$) or intensivist$ or internist$ or medic or medics or neonatologist$ or nephrologist$ or neurologist$ or obstetrician$ or oncologist$ or ((cancer or malignancy) adj2 specialist$) or ophthalmologist$ or (orthop?edic adj2 specialist$) or orthop?edist$ or otolaryngologist$ or pathologist$ or p?ediatric$ or perinatologist$ or pharmacist$ or phlebologist$ or physiatrist$ or physician$ or podiatrist$ or psychiatrist$ or pulmonologist$ or radiologist$ or rheumatologist$ or surgeon$ or urologist$ or urogyn?ecolog$ or vaccinologist$).tw.
16. ((allied health adj3 (professional$ or personnel or worker$ or practitioner$)) or NMAHP$ or AHP$).tw.
17. (nurse$ or midwife$ or midwives$ or (health adj2 visitor$) or (art adj2 therapist) or chiropodist$ or podiatrist$ or dietician$ or (hearing adj2 aid$ adj2 dispenser$) or ((physical or occupational) adj2 therapist$) or orthoptist$ or paramedic$ or physiotherapist$ or psychologist$ or prosthetist$ or orthotist$ or radiographer$ or ((speech adj2 language adj2 (therapist$ or pathologist$)) or SLT$)).tw.
18. ((key or frontline or front‐line) adj3 (staff or worker$ or workforce or personnel or volunteer$ or professional$)).tw.
19. or/12‐18
20. disease outbreaks/ or epidemics/ or pandemics/
21. (((health$ or disease$) adj5 (disaster$ or catastrophe$ or crises or crisis)) or outbreak$ or pandemic$ or epidemic$).tw.
22. ebolavirus/ or influenza, human/ or severe acute respiratory syndrome/ or pneumonia, viral/ or coronavirus infections/
23. meningitis, bacterial/
24. cholera/
25. exp influenzavirus a/ or exp influenzavirus b/ or influenzavirus c/
26. chikungunya virus/ or chikungunya fever/ or exp dengue/ or rift valley fever/ or yellow fever/ or zika virus infection/ or lassa fever/
27. exp hemorrhagic fevers, viral/
28. coronavirus/ or betacoronavirus/ or middle east respiratory syndrome coronavirus/ or sars virus/ or monkeypox/ or smallpox/
29. exp henipavirus/ or henipavirus infections/
30. (((h?emorrhagic or yellow or rift valley or lassa) adj3 fever) or ebola or ebolavirus or ((nipah or marburg or hendra or zika) adj2 virus)).tw.
31. (chikungunya or cholera or smallpox or small pox or monkeypox or plague or tularaemia).tw.
32. ((avian or bird or fowl) adj5 (influenza or flu or plague)).tw.
33. ((bacterial adj2 meningitis) or (meningococcal adj2 diseas$)).tw.
34. (severe acute respiratory syndrome or SARS or coronavirus or Middle East respiratory syndrome or MERS‐CoV or ((atypical or influenza or viral or virus) adj3 (pneumonia or bronchopneumonia or infection))).tw.
35. (coronavirus$ or corona virus$ or HCoV$ or ncov$ or covid$ or sars‐cov$ or sarscov$ or sars‐coronavirus$).tw.
36. or/20‐35
37. 11 and 19 and 36
38. (200$ or 201$ or "2020").dp. or 20020101:20301231.(ep).
39. 37 and 38
Appendix 2. CDSR (Cochrane Database of Systematic Reviews) and CENTRAL (Cochrane Central Register of Controlled Trials) in the Cochrane Library search strategies
#1 MeSH descriptor: [Mental Fatigue] explode all trees
#2 MeSH descriptor: [Stress, Psychological] explode all trees
#3 MeSH descriptor: [Depersonalization] this term only
#4 MeSH descriptor: [Depression] this term only
#5 MeSH descriptor: [Anxiety] this term only
#6 MeSH descriptor: [Mental Health] this term only
#7 MeSH descriptor: [Anxiety Disorders] this term only
#8 MeSH descriptor: [Panic Disorder] this term only
#9 MeSH descriptor: [Bipolar and Related Disorders] explode all trees
#10 MeSH descriptor: [Mood Disorders] this term only
#11 MeSH descriptor: [Depressive Disorder] this term only
#12 MeSH descriptor: [Depressive Disorder, Major] this term only
#13 MeSH descriptor: [Depressive Disorder, Treatment‐Resistant] this term only
#14 MeSH descriptor: [Trauma and Stressor Related Disorders] this term only
#15 MeSH descriptor: [Adjustment Disorders] this term only
#16 MeSH descriptor: [Stress Disorders, Traumatic] this term only
#17 MeSH descriptor: [Psychological Trauma] explode all trees
#18 MeSH descriptor: [Stress Disorders, Post‐Traumatic] this term only
#19 MeSH descriptor: [Stress Disorders, Traumatic, Acute]
#20 MeSH descriptor: [Adaptation, Psychological] this term only
#21 MeSH descriptor: [Help‐Seeking Behavior] this term only
#22 MeSH descriptor: [Motivation] this term only
#23 MeSH descriptor: [Resilience, Psychological] this term only
#24 MeSH descriptor: [Substance‐Related Disorders] this term only
#25 MeSH descriptor: [Alcohol‐Related Disorders] this term only
#26 MeSH descriptor: [Alcoholic Intoxication] this term only
#27 MeSH descriptor: [Alcoholism] this term only
#28 MeSH descriptor: [Tobacco Use Disorder] this term only
#29 ((mental or psychological or psychosocial or psycho‐social or emotional) near/3 (condition* or health or care or condition or factor or help or state or status or stability or instability)):ti,ab,kw (Word variations have been searched)
#30 (((post‐traumatic or posttraumatic or trauma*) near/3 (disorder or neurosis or psychos* or syndrome)) or PTSD or traumati?ed or traumatic):ti,ab,kw (Word variations have been searched)
#31 (depress* or anxious* or anxiety or panic* or hysteria or stress or (chronic near/2 fatigue) or suicid* or ((affectiv* or mood or mental) near/2 (disorder* or health))):ti,ab,kw (Word variations have been searched)
#32 (burnout or burn‐out or cope or coping or adaption or catastrophi?ing or depersonali?ation or resilience or exhaust* or hope* or anger or apath* or bereave* or grief or sadness or distress* or fear* or frustrat* or guilt or shame or hope* or loneliness or sadness or motivat* or confusion or empathy or ((unable or difficult*) near/3 (sleep* or focus*)) or eagerness or enthusiasm or goodwill or keenness or resolve or toughness or volition or well‐being or wellbeing or willing* or willpower or wish*):ti,ab,kw (Word variations have been searched)
#33 {or #1‐#32}
#34 MeSH descriptor: [Health Personnel] this term only
#35 MeSH descriptor: [Allied Health Personnel] this term only
#36 MeSH descriptor: [Community Health Workers] this term only
#37 MeSH descriptor: [Emergency Medical Technicians] this term only
#38 MeSH descriptor: [Home Health Aides] this term only
#39 MeSH descriptor: [Licensed Practical Nurses] this term only
#40 MeSH descriptor: [Nursing Assistants] this term only
#41 MeSH descriptor: [Operating Room Technicians] this term only
#42 MeSH descriptor: [Physical Therapist Assistants] this term only
#43 MeSH descriptor: [Physician Assistants] explode all trees
#44 MeSH descriptor: [Anesthetists] explode all trees
#45 MeSH descriptor: [Audiologists] this term only
#46 MeSH descriptor: [Caregivers] this term only
#47 MeSH descriptor: [Coroners and Medical Examiners] this term only
#48 MeSH descriptor: [Dental Staff] explode all trees
#49 MeSH descriptor: [Dentists] this term only
#50 MeSH descriptor: [Emergency Medical Dispatcher] this term only
#51 MeSH descriptor: [Epidemiologists] this term only
#52 MeSH descriptor: [Health Facility Administrators] explode all trees
#53 MeSH descriptor: [Infection Control Practitioners] this term only
#54 MeSH descriptor: [Medical Laboratory Personnel] this term only
#55 MeSH descriptor: [Medical Staff] explode all trees
#56 MeSH descriptor: [Nurses] explode all trees
#57 MeSH descriptor: [Nursing Staff] explode all trees
#58 MeSH descriptor: [Nutritionists] this term only
#59 MeSH descriptor: [Occupational Therapists] this term only
#60 MeSH descriptor: [Optometrists] this term only
#61 MeSH descriptor: [Personnel, Hospital] explode all trees
#62 MeSH descriptor: [Pharmacists] this term only
#63 MeSH descriptor: [Physical Therapists] this term only
#64 MeSH descriptor: [Physicians] explode all trees
#65 MeSH descriptor: [Students] this term only
#66 MeSH descriptor: [Students, Health Occupations] explode all trees
#67 MeSH descriptor: [Volunteers] this term only
#68 ((clinical or healthcare or health care or (operating near/3 (room or theat* or department*)) or hospital or laborator* or biomedical or medical or surgical or pharmacy or social or community) near/3 (auxilliar* or practitioner* or professional* or provider* or worker* or personnel or dispenser* or aides or workforce or consultant* or student* or technician* or scientist* or volunteer*)):ti,ab,kw (Word variations have been searched)
#69 (an?esthesiologist* or an?esthetist* or cardiologist* or dermatologist* or diabetologist* or doctor* or endocrinologist* or epileptologist* or gastroenterologist* or (general near/2 practitioner) or GP or geriatrician* or gerontologist* or gyn?ecologist* or h?ematologist* or (h?ematolog* near/2 specialist*) or hepatologist* or immunologist* or (infectious near/2 diseas* near/2 specialist*) or intensivist* or internist* or medic or medics or neonatologist* or nephrologist* or neurologist* or obstetrician* or oncologist* or ((cancer or malignancy) near/2 specialist*) or ophthalmologist* or (orthop?edic near/2 specialist*) or orthop?edist* or otolaryngologist* or pathologist* or p?ediatric* or perinatologist* or pharmacist* or phlebologist* or physiatrist* or physician* or podiatrist* or psychiatrist* or pulmonologist* or radiologist* or rheumatologist* or surgeon* or urologist* or urogyn?ecolog* or vaccinologist*):ti,ab,kw (Word variations have been searched)
#70 ((allied health near/3 (professional* or personnel or worker* or practitioner*)) or NMAHP* or AHP*):ti,ab,kw (Word variations have been searched)
#71 (nurse* or midwife* or midwives* or (health near/2 visitor*) or (art near/2 therapist) or chiropodist* or podiatrist* or dietician* or (hearing near/2 aid* near/2 dispenser*) or ((physical or occupational) near/2 therapist*) or orthoptist* or paramedic* or physiotherapist* or psychologist* or prosthetist* or orthotist* or radiographer* or ((speech near/2 language near/2 (therapist* or pathologist*)) or SLT*)):ti,ab,kw (Word variations have been searched)
#72 ((key or frontline or front‐line) near/3 (staff or worker* or workforce or personnel or volunteer* or professional*)):ti,ab,kw (Word variations have been searched)
#73 {or #34‐#72}
#74 MeSH descriptor: [Disease Outbreaks] this term only
#75 MeSH descriptor: [Epidemics] this term only
#76 MeSH descriptor: [Pandemics] this term only
#77 (((health* or disease*) near/5 (disaster* or catastrophe* or crises or crisis)) or outbreak* or pandemic* or epidemic*):ti,ab,kw (Word variations have been searched)
#78 MeSH descriptor: [Ebolavirus] this term only
#79 MeSH descriptor: [Influenza, Human] this term only
#80 MeSH descriptor: [Severe Acute Respiratory Syndrome] this term only
#81 MeSH descriptor: [Pneumonia, Viral] this term only
#82 MeSH descriptor: [Coronavirus Infections] explode all trees
#83 MeSH descriptor: [Meningitis, Bacterial] this term only
#84 MeSH descriptor: [Cholera] this term only
#85 MeSH descriptor: [Influenzavirus B] explode all trees
#86 MeSH descriptor: [Influenzavirus A] explode all trees
#87 MeSH descriptor: [Influenzavirus C] this term only
#88 MeSH descriptor: [Chikungunya Virus] this term only
#89 MeSH descriptor: [Chikungunya Fever] this term only
#90 MeSH descriptor: [Dengue] explode all trees
#91 MeSH descriptor: [Rift Valley Fever] this term only
#92 MeSH descriptor: [Yellow Fever] this term only
#93 MeSH descriptor: [Zika Virus Infection] this term only
#94 MeSH descriptor: [Lassa Fever] this term only
#95 MeSH descriptor: [Hemorrhagic Fevers, Viral] explode all trees
#96 MeSH descriptor: [Coronavirus] this term only
#97 MeSH descriptor: [Betacoronavirus] this term only
#98 MeSH descriptor: [Middle East Respiratory Syndrome Coronavirus] this term only
#99 MeSH descriptor: [SARS Virus] this term only
#100 MeSH descriptor: [Monkeypox] this term only
#101 MeSH descriptor: [Smallpox] this term only
#102 MeSH descriptor: [Henipavirus] explode all trees
#103 MeSH descriptor: [Henipavirus infections] this term only
#104 (((h?emorrhagic or yellow or rift valley or lassa) near/3 fever) or ebola or ebolavirus or ((nipah or marburg or hendra or zika) near/2 virus)):ti,ab,kw (Word variations have been searched)
#105 (chikungunya or cholera or smallpox or small pox or monkeypox or plague or tularaemia):ti,ab,kw (Word variations have been searched)
#106 ((avian or bird or fowl) near/5 (influenza or flu or plague)):ti,ab,kw (Word variations have been searched)
#107 ((bacterial near/2 meningitis) or (meningococcal near/2 diseas*)):ti,ab,kw (Word variations have been searched)
#108 (severe acute respiratory syndrome or SARS or coronavirus or ((atypical or influenza or viral or virus) near/3 (pneumonia or bronchopneumonia or infection))):ti,ab,kw (Word variations have been searched)
#109 (coronavirus* or corona virus* or HCoV* or ncov* or covid* or sars‐cov* or sarscov* or sars‐coronavirus*):ti,ab,kw (Word variations have been searched)
#110 {or #74‐#109}
#111 #32 and #73 and #110 with Cochrane Library publication date Between Jan 2002 and May 2020.
Appendix 3. Embase (Ovid) search strategy
1. wellbeing/
2. exp burnout/ or exp job stress/
3. compassion fatigue/
4. mental health/ or anxiety disorder/ or acute stress disorder/ or anxiety neurosis/ or catastrophizing/ or distress syndrome/ or generalized anxiety disorder/ or "mixed anxiety and depression"/ or posttraumatic stress disorder/ or attitude to death/ or psychological adjustment/ or depersonalization/ or physically induced stress/
5. bipolar disorder/ or bipolar depression/
6. adjustment/ or adjustment disorder/ or psychological adjustment/
7. exp adaptive behavior/ or behavioral stress/ or exp coping behavior/ or help seeking behavior/ or motivation/ or psychological resilience/
8. drug dependence/ or alcoholism/ or drug craving/ or drug misuse/ or tobacco dependence/ or alcoholic intoxication/ or exp "tobacco use"/ or smoking/ or smoking habit/ or tobacco consumption/
9. ((mental or psychological or psychosocial or psycho‐social or emotional) adj3 (condition$ or health or care or condition or factor or help or state or status or stability or instability)).tw.
10. (((post‐traumatic or posttraumatic or trauma$) adj3 (disorder or neurosis or psychos$ or syndrome)) or PTSD or traumati?ed or traumatic).tw.
11. (depress$ or anxious$ or anxiety or panic$ or hysteria or stress or (chronic adj2 fatigue) or suicid$ or ((affectiv$ or mood or mental) adj2 (disorder$ or health))).tw.
12. (burnout or burn‐out or cope or coping or adaption or catastrophi?ing or depersonali?ation or resilience or exhaust$ or hope$ or anger or apath$ or bereave$ or grief or sadness or distress$ or fear$ or frustrat$ or guilt or shame or hope$ or loneliness or sadness or motivat$ or confusion or empathy or ((unable or difficult$) adj3 (sleep$ or focus$)) or eagerness or enthusiasm or goodwill or keenness or resolve or toughness or volition or well‐being or wellbeing or willing$ or willpower or wish$).tw.
13. or/1‐12
14. health care personnel/ or exp advanced practice provider/ or exp anesthesist/ or care coordinator/ or exp dental personnel/ or epidemiologist/ or health workforce/ or hospital personnel/ or hospital volunteer/ or medical staff/ or lay health worker/ or medical personnel/ or coroner/ or medical assistant/ or exp medical registrar/ or medical specialist/ or medical staff/ or physician/ or physician assistant/ or hospital physician/ or internist/ or surgeon/ or mental health care personnel/ or orthotist/ or perfusionist/ or exp prosthetist/ or transplant coordinator/
15. paramedical personnel/ or clinical laboratory personnel/ or health practitioner/ or exp midwife/ or exp nurse/ or nursing assistant/ or nursing staff/ or occupational therapist/ or occupational therapy assistant/ or operating room personnel/ or paramedical profession/ or exp paramedical student/ or exp pharmacist/ or pharmacy technician/ or phlebotomist/ or physiotherapist/ or physiotherapist assistant/ or exp radiographer/ or rescue personnel/
16. exp laboratory personnel/ or exp health student/
17. ((clinical or healthcare or health care or (operating adj3 (room or theat$ or department$)) or hospital or laborator$ or biomedical or medical or surgical or pharmacy or social or community) adj3 (auxilliar$ or practitioner$ or professional$ or provider$ or worker$ or personnel or dispenser$ or aides or workforce or consultant$ or student$ or technician$ or scientist$ or volunteer$)).tw.
18. (an?esthesiologist$ or an?esthetist$ or cardiologist$ or dermatologist$ or diabetologist$ or doctor$ or endocrinologist$ or epileptologist$ or gastroenterologist$ or (general adj2 practitioner) or GP or geriatrician$ or gerontologist$ or gyn?ecologist$ or h?ematologist$ or (h?ematolog$ adj2 specialist$) or hepatologist$ or immunologist$ or (infectious adj2 diseas$ adj2 specialist$) or intensivist$ or internist$ or medic or medics or neonatologist$ or nephrologist$ or neurologist$ or obstetrician$ or oncologist$ or ((cancer or malignancy) adj2 specialist$) or ophthalmologist$ or (orthop?edic adj2 specialist$) or orthop?edist$ or otolaryngologist$ or pathologist$ or p?ediatric$ or perinatologist$ or pharmacist$ or phlebologist$ or physiatrist$ or physician$ or podiatrist$ or psychiatrist$ or pulmonologist$ or radiologist$ or rheumatologist$ or surgeon$ or urologist$ or urogyn?ecolog$ or vaccinologist$).tw.
19. ((allied health adj3 (professional$ or personnel or worker$ or practitioner$)) or NMAHP$ or AHP$).tw.
20. (nurs$ or midwife$ or midwives$ or (health adj2 visitor$) or (art adj2 therapist) or chiropodist$ or podiatrist$ or dietician$ or (hearing adj2 aid$ adj2 dispenser$) or ((physical or occupational) adj2 therapist$) or orthoptist$ or paramedic$ or physiotherapist$ or psychologist$ or prosthetist$ or orthotist$ or radiographer$ or ((speech adj2 language adj2 (therapist$ or pathologist$)) or SLT$)).tw.
21. ((key or frontline or front‐line) adj3 (staff or worker$ or workforce or personnel or volunteer$ or professional$)).tw.
22. or/14‐21
23. epidemic/ or pandemic/
24. (((health$ or disease$) adj5 (disaster$ or catastrophe$ or crises or crisis)) or outbreak$ or pandemic$ or epidemic$).tw.
25. ebolavirus/ or influenza/ or exp influenza a/ or influenza b/ or influenza c/ or pandemic influenza/ or swine influenza/
26. severe acute respiratory syndrome/ or coronavirus infection/ or virus pneumonia/
27. chikungunya virus/ or chikungunya/ or dengue/ or dengue hemorrhagic fever/ or exp hemorrhagic fever/ or Zika fever/ or exp Zika virus/
28. betacoronavirus/ or coronavirinae/ or betacoronavirus 1/ or middle east respiratory syndrome coronavirus/ or exp sars‐related coronavirus/
29. monkeypox/ or monkeypox virus/ or smallpox/ or smallpox virus/
30. henipavirus/ or exp henipavirus infection/
31. (((h?emorrhagic or yellow or rift valley or lassa) adj3 fever) or ebola or ebolavirus or ((nipah or marburg or hendra or zika) adj2 virus)).tw.
32. (chikungunya or cholera or smallpox or small pox or monkeypox or plague or tularaemia).tw
33. ((avian or bird or fowl) adj5 (influenza or flu or plague)).tw.
34. ((bacterial adj2 meningitis) or (meningococcal adj2 diseas$)).tw.
35. (severe acute respiratory syndrome or SARS or coronavirus or Middle East respiratory syndrome or MERS‐CoV or ((atypical or influenza or viral or virus) adj3 (pneumonia or bronchopneumonia or infection))).tw.
36. (coronavirus$ or corona virus$ or HCoV$ or ncov$ or covid$ or sars‐cov$ or sarscov$ or sars‐coronavirus$).tw.
37. or/23‐36
38. 13 and 22 and 37
39. limit 38 to yr="2002 ‐Current"
Appendix 4. Web of Science Indexes
Web of Science Indexes ((Science Citation Index Expanded (SCIEXPANDED), Social Sciences Citation Index (SSCI), Conference Proceedings Citation Index‐ Science (CPCI‐S), Conference Proceedings Citation Index‐ Social Science & Humanities (CPCI‐SSH) search strategy
#1 TS=((mental or psychological or psychosocial or “psycho‐social” or emotional) NEAR/3 (condition* or health or care or condition or factor or help or state or status or stability or instability))
#2 TS=(((“post‐traumatic” or posttraumatic or trauma*) NEAR/3 (disorder or neurosis or psychos* or syndrome)) or PTSD or traumati?ed or traumatic)
#3 TS=(depress* or anxious* or anxiety or panic* or hysteria or stress or (chronic NEAR/2 fatigue) or suicid* or ((affectiv* or mood or mental) NEAR/2 (disorder* or health)))
#4 TS=(burnout or “burn‐out” or cope or coping or adaption or catastrophi?ing or depersonali?ation or resilience or exhaust* or hope* or anger or apath* or bereave* or grief or sadness or distress* or fear* or frustrat* or guilt or shame or hope* or loneliness or sadness or motivat* or confusion or empathy or ((unable or difficult*) NEAR/3 (sleep* or focus*)) or eagerness or enthusiasm or goodwill or keenness or resolve or toughness or volition or well‐being or wellbeing or willing* or willpower or wish*)
#5 #1 OR #2 OR #3 OR #4
#6 TS=((clinical or healthcare or “health care” or (operating NEAR/3 (room or theat* or department*)) or hospital or laborator* or biomedical or medical or surgical or pharmacy or social or community) NEAR/3 (auxilliar* or practitioner* or professional* or provider* or worker* or personnel or dispenser* or aides or workforce or consultant* or student* or technician* or scientist* or volunteer*))
#7 TS=(an?esthesiologist* or an?esthetist* or cardiologist* or dermatologist* or diabetologist* or doctor* or endocrinologist* or epileptologist* or gastroenterologist* or (general NEAR/2 practitioner) or GP or geriatrician* or gerontologist* or gyn?ecologist* or h?ematologist* or (h?ematolog* NEAR/2 specialist*) or hepatologist* or immunologist* or (infectious NEAR/2 diseas* NEAR/2 specialist*) or intensivist* or internist* or medic or medics or neonatologist* or nephrologist* or neurologist* or obstetrician* or oncologist* or ((cancer or malignancy) NEAR/2 specialist*) or ophthalmologist* or (orthop?edic NEAR/2 specialist*) or orthop?edist* or otolaryngologist* or pathologist* or p?ediatric* or perinatologist* or pharmacist* or phlebologist* or physiatrist* or physician* or podiatrist* or psychiatrist* or pulmonologist* or radiologist* or rheumatologist* or surgeon* or urologist* or urogyn?ecolog* or vaccinologist
#8 TS=((“allied health” NEAR/3 (professional* or personnel or worker* or practitioner*)) or NMAHP* or AHP*)
#9 TS=(nurs* or midwife* or midwives* or (health NEAR/2 visitor*) or (art NEAR/2 therapist) or chiropodist* or podiatrist* or dietician* or (hearing NEAR/2 aid* NEAR/2 dispenser*) or ((physical or occupational) NEAR/2 therapist*) or orthoptist* or paramedic* or physiotherapist* or psychologist* or prosthetist* or orthotist* or radiographer* or ((speech NEAR/2 language NEAR/2 (therapist* or pathologist*)) or SLT*))
#10 TS=((key or frontline or “front‐line”) NEAR/3 (staff or worker* or workforce or personnel or volunteer* or professional*))
#11 #6 OR #7 OR #8 OR #9 OR #10
#12 TS=(((health* or disease*) NEAR/5 (disaster* or catastrophe* or crises or crisis)) or outbreak* or pandemic* or epidemic*)
#13 TS= (((h?emorrhagic or yellow or rift valley or lassa) NEAR/3 fever) or ebola or ebolavirus or ((nipah or marburg or hendra or zika) NEAR/2 virus))
#14 TS= (chikungunya or cholera or smallpox or small pox or monkeypox or plague or tularaemia)
#15 TS=((avian or bird or fowl) NEAR/5 (influenza or flu or plague))
#16 TS=((bacterial NEAR/2 meningitis) or (meningococcal NEAR/2 diseas*))
#17 TS=(“severe acute respiratory syndrome” or SARS or coronavirus or ((atypical or influenza or viral or virus) NEAR/3 (pneumonia or bronchopneumonia or infection)))
#18 TS=(coronavirus* or “corona virus*” or HCoV* or ncov* or covid* or sars‐cov* or sarscov* or "sars‐coronavirus*”)
#19 #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18
#20 #5 OR #11 OR #19 [Timespan=2002‐2020]
Appendix 5. PsycINFO (Ovid) search strategy
PsycINFO (Ovid) search strategy
1. fatigue/ or compassion fatigue/
2. stress/ or occupational stress/ or post‐traumatic stress/ or psychological stress/ or stress reactions/ or psychological endurance/
3. trauma/ or emotional trauma/
4. major depression/ or late life depression/ or recurrent depression/ or "depression (emotion)"/
5. anxiety disorders/ or generalized anxiety disorder/ or panic attack/ or panic disorder/ or guilt/ or anxiety/ or agitation/ or shame/ or motivation/
6. emotional states/ or bereavement/ or catastrophizing/ or dissatisfaction/ or distress/ or doubt/ or emotional trauma/ or fear/ or frustration/ or helplessness/ or homesickness/ or hopelessness/ or loneliness/ or pessimism/ or regret/ or restlessness/ or sadness/ or sympathy/
7. "resilience (psychological)"/ or "adaptability (personality)"/ or cognitive reserve/ or coping behavior/
8. drug abuse/ or drug usage/ or addiction/ or exp alcohol abuse/ or alcoholism/ or alcohol abuse/
9. ((mental or psychological or psychosocial or psycho‐social or emotional) adj3 (condition$ or health or care or condition or factor or help or state or status or stability or instability)).tw.
10. (((post‐traumatic or posttraumatic or trauma$) adj3 (disorder or neurosis or psychos$ or syndrome)) or PTSD or traumati?ed or traumatic).tw.
11. (depress$ or anxious$ or anxiety or panic$ or hysteria or stress or (chronic adj2 fatigue) or suicid$ or ((affectiv$ or mood or mental) adj2 (disorder$ or health))).tw.
12. (burnout or burn‐out or cope or coping or adaption or catastrophi?ing or depersonali?ation or resilience or exhaust$ or hope$ or anger or apath$ or bereave$ or grief or sadness or distress$ or fear$ or frustrat$ or guilt or shame or hope$ or loneliness or sadness or motivat$ or confusion or empathy or ((unable or difficult$) adj3 (sleep$ or focus$)) or eagerness or enthusiasm or goodwill or keenness or resolve or toughness or volition or well‐being or wellbeing or willing$ or willpower or wish$).tw.
13. or/1‐12
14. health personnel/ or allied health personnel/ or occupational therapists/ or physical therapists/ or speech therapists/ or medical personnel/ or dentists/ or military medical personnel/ or exp nurses/ or pharmacists/ or physicians/ or gynecologists/ or internists/ or neurologists/ or obstetricians/ or pathologists/ or pediatricians/ or psychiatrists/ or surgeons/ or clinicians/ or mental health personnel/ or clinical psychologists/ or psychiatric nurses/ or psychiatric social workers/ or psychiatrists/ or psychotherapists/ or social workers/ or psychiatric social workers/
15. nursing students/ or medical students/ or volunteers/
16. ((clinical or healthcare or health care or (operating adj3 (room or theat$ or department$)) or hospital or laborator$ or biomedical or medical or surgical or pharmacy or social or community) adj3 (auxilliar$ or practitioner$ or professional$ or provider$ or worker$ or personnel or dispenser$ or aides or workforce or consultant$ or student$ or technician$ or scientist$ or volunteer$)).tw.
17. (an?esthesiologist$ or an?esthetist$ or cardiologist$ or dermatologist$ or diabetologist$ or doctor$ or endocrinologist$ or epileptologist$ or gastroenterologist$ or (general adj2 practitioner) or GP or geriatrician$ or gerontologist$ or gyn?ecologist$ or h?ematologist$ or (h?ematolog$ adj2 specialist$) or hepatologist$ or immunologist$ or (infectious adj2 diseas$ adj2 specialist$) or intensivist$ or internist$ or medic or medics or neonatologist$ or nephrologist$ or neurologist$ or obstetrician$ or oncologist$ or ((cancer or malignancy) adj2 specialist$) or ophthalmologist$ or (orthop?edic adj2 specialist$) or orthop?edist$ or otolaryngologist$ or pathologist$ or p?ediatric$ or perinatologist$ or pharmacist$ or phlebologist$ or physiatrist$ or physician$ or podiatrist$ or psychiatrist$ or pulmonologist$ or radiologist$ or rheumatologist$ or surgeon$ or urologist$ or urogyn?ecolog$ or vaccinologist$).tw.
18. ((allied health adj3 (professional$ or personnel or worker$ or practitioner$)) or NMAHP$ or AHP$).tw.
19. (nurs$ or midwife$ or midwives$ or (health adj2 visitor$) or (art adj2 therapist) or chiropodist$ or podiatrist$ or dietician$ or (hearing adj2 aid$ adj2 dispenser$) or ((physical or occupational) adj2 therapist$) or orthoptist$ or paramedic$ or physiotherapist$ or psychologist$ or prosthetist$ or orthotist$ or radiographer$ or ((speech adj2 language adj2 (therapist$ or pathologist$)) or SLT$)).tw.
20. ((key or frontline or front‐line) adj3 (staff or worker$ or workforce or personnel or volunteer$ or professional$)).tw.
21. or/14‐20
22. epidemics/ or pandemics/
23. (((health$ or disease$) adj5 (disaster$ or catastrophe$ or crises or crisis)) or outbreak$ or pandemic$ or epidemic$).tw.
24. exp influenza/
25. (((h?emorrhagic or yellow or rift valley or lassa) adj3 fever) or ebola or ebolavirus or ((nipah or marburg or hendra or zika) adj2 virus)).tw.
26. (chikungunya or cholera or smallpox or small pox or monkeypox or plague or tularaemia).tw.
27. ((avian or bird or fowl) adj5 (influenza or flu or plague)).tw.
28. ((bacterial adj2 meningitis) or (meningococcal adj2 diseas$)).tw.
29. (severe acute respiratory syndrome or SARS or coronavirus or ((atypical or influenza or viral or virus) adj3 (pneumonia or bronchopneumonia or infection))).tw.
30. (coronavirus$ or corona virus$ or HCoV$ or ncov$ or covid$ or sars‐cov$ or sarscov$ or sars‐coronavirus$).tw.
31. or/22‐30
32. 13 and 21 and 31
33. limit 32 to yr="2002 ‐Current"
Appendix 6. CINAHL EBSCO search strategy
CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature) search strategy
S1 (MH "Burnout, Professional") OR (MH "Stress, Occupational")
S2 (MH "Mental Fatigue") OR (MH "Compassion Fatigue")
S3 (MH "Mental Health") OR (MH "Anger") OR (MH "Anxiety") OR (MH "Catastrophization") OR (MH "Anticipatory Anxiety") OR (MH "Depression")
S4 (MH "Stress Disorders, Post‐Traumatic") OR (MH "Anxiety Disorders") OR (MH "Depression, Reactive") OR (MH "Panic Disorder") OR (MH "Bipolar Disorder") OR (MH "Psychological Trauma") OR (MH "Avoidance (Psychology)") OR (MH "Denial (Psychology)") OR (MH "Agitation") OR (MH "Depersonalization") OR (MH "Helplessness, Learned") OR (MH "Self‐Injurious Behavior") OR (MH "Self Neglect") OR (MH "Powerlessness") OR (MH "Suicide") OR (MH "Repression") OR (MH "Acting Out") OR (MH "Denial (Psychology)") OR (MH "Repression") OR (MH "Regression (Psychology)") OR (MH "Anger") OR (MH "Apathy") OR (MH "Grief") OR (MH "Compassion") OR (MH "Fear") OR (MH "Frustration") OR (MH "Guilt") OR (MH "Shame") OR (MH "Hopelessness") OR (MH "Hope") OR (MH "Sadness") OR (MH "Suffering") OR (MH "Motivation")
S5 (MH "Empathy") OR (MH "Optimism") OR (MH "Courage") OR (MH "Pessimism") OR (MH "Confidence")
S6 (MH "Alcoholism") OR (MH "Alcohol Abuse") OR (MH "Alcoholic Intoxication") OR (MH "Substance Abuse") OR (MH "Substance Dependence") OR (MH "Smoking")
S7 TI ((mental or psychological or psychosocial or psycho‐social or emotional) N3 (condition* or health or care or condition or factor or help or state or status or stability or instability)) OR AB ((mental or psychological or psychosocial or psycho‐social or emotional) N3 (condition* or health or care or condition or factor or help or state or status or stability or instability))
S8 TI (((post‐traumatic or posttraumatic or trauma*) N3 (disorder or neurosis or psychos* or syndrome)) or PTSD or traumati?ed or traumatic) OR AB (((post‐traumatic or posttraumatic or trauma*) N3 (disorder or neurosis or psychos* or syndrome)) or PTSD or traumati?ed or traumatic)
S9 TI (depress* or anxious* or anxiety or panic* or hysteria or stress or (chronic N2 fatigue) or suicid* or ((affectiv* or mood or mental) N2 (disorder* or health))) OR AB (depress* or anxious* or anxiety or panic* or hysteria or stress or (chronic N2 fatigue) or suicid* or ((affectiv* or mood or mental) N2 (disorder* or health)))
S10 TI (burnout or burn‐out or cope or coping or adaption or catastrophi?ing or depersonali?ation or resilience or exhaust* or hope* or anger or apath* or bereave* or grief or sadness or distress* or fear* or frustrat* or guilt or shame or hope* or loneliness or sadness or motivat* or confusion or empathy or ((unable or difficult*) N3 (sleep* or focus*)) or eagerness or enthusiasm or goodwill or keenness or resolve or toughness or volition or well‐being or wellbeing or willing* or willpower or wish*) OR AB (burnout or burn‐out or cope or coping or adaption or catastrophi?ing or depersonali?ation or resilience or exhaust* or hope* or anger or apath* or bereave* or grief or sadness or distress* or fear* or frustrat* or guilt or shame or hope* or loneliness or sadness or motivat* or confusion or empathy or ((unable or difficult*) N3 (sleep* or focus*)) or eagerness or enthusiasm or goodwill or keenness or resolve or toughness or volition or well‐being or wellbeing or willing* or willpower or wish*)
S11 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10
S12 (MH "Health Personnel") OR (MH "Allied Health Personnel") OR (MH "Audiologists") OR (MH "Cardiopulmonary Technicians") OR (MH "Dialysis Technicians") OR (MH "Dietitians") OR (MH "Emergency Medical Technicians") OR (MH "Infection Preventionists") OR (MH "Interns and Residents") OR (MH "Laboratory Personnel+") OR (MH "Medical Assistants") OR (MH "Occupational Therapy Assistants") OR (MH "Ophthalmic Technologists") OR (MH "Physical Therapist Assistants") OR (MH "Physician Assistants") OR (MH "Radiology Personnel+") OR (MH "Respiratory Therapists") OR (MH "Social Workers") OR (MH "Speech‐Language Pathologists") OR (MH "Speech‐Language Pathology Assistants") OR (MH "Surgical Technologists") OR (MH "Orthopedic Technologists") OR (MH "Community Health Workers") OR (MH "Coroners and Medical Examiners") OR (MH "Dentists") OR (MH "Expert Clinicians+") OR (MH "Health Personnel, Unlicensed") OR (MH "Medical Staff, Hospital+") OR (MH "Psychotherapists") OR (MH "Psychologists") OR (MH "Midwives+") OR (MH "Novice Clinicians+") OR (MH "Advanced Practice Nurses") OR (MH "Nurse Anesthetists") OR (MH "Nurse Midwives") OR (MH "Nurses") OR (MH "Nurse Practitioners+") OR (MH "Nurse Consultants") OR (MH "Nurse Liaison") OR (MH "Nurse Counselors") OR (MH "Nurse Psychotherapists") OR (MH "Case Managers") OR (MH "Nursing Leaders") OR (MH "Staff Nurses") OR (MH "Emergency Nurse Practitioners") OR (MH "Infection Preventionists") OR (MH "Gerontologic Nurse Practitioners") OR (MH "Pediatric Nurse Practitioners+") OR (MH "Nursing Assistants") OR (MH "Operating Room Personnel") OR (MH "Anesthetists") OR (MH "Anesthesiologists") OR (MH "Surgical Technologists") OR (MH "Nursing Staff, Hospital") OR (MH "Cardiologists") OR (MH "Endocrinologists") OR (MH "Dermatologists") OR (MH "Gastroenterologists") OR (MH "Geriatricians") OR (MH "Neonatologists") OR (MH "Neurologists") OR (MH "Oncologists") OR (MH "Ophthalmologists") OR (MH "Nephrologists") OR (MH "Optometrists") OR (MH "Pathologists+") OR (MH "Pediatricians") OR (MH "Physiatrists") OR (MH "Physicians, Emergency") OR (MH "Psychiatrists") OR (MH "Pulmonologists") OR (MH "Radiologists") OR (MH "Rheumatologists") OR (MH "Surgeons") OR (MH "Urologists") OR (MH "Transplant Coordinators")
S13 (MH "Students, Medical") OR (MH "Students, Midwifery") OR (MH "Students, Nursing+") OR (MH "Students, Allied Health+") OR (MH "Volunteer Workers")
S14 TI ((clinical or healthcare or health care or (operating N3 (room or theat* or department*)) or hospital or laborator* or biomedical or medical or surgical or pharmacy or social or community) N3 (auxilliar* or practitioner* or professional* or provider* or worker* or personnel or dispenser* or aides or workforce or consultant* or student* or technician* or scientist* or volunteer*)) OR AB ((clinical or healthcare or health care or (operating N3 (room or theat* or department*)) or hospital or laborator* or biomedical or medical or surgical or pharmacy or social or community) N3 (auxilliar* or practitioner* or professional* or provider* or worker* or personnel or dispenser* or aides or workforce or consultant* or student* or technician* or scientist* or volunteer*))
S15 TI (an?esthesiologist* or an?esthetist* or cardiologist* or dermatologist* or diabetologist* or doctor* or endocrinologist* or epileptologist* or gastroenterologist* or (general N2 practitioner) or GP or geriatrician* or gerontologist* or gyn?ecologist* or h?ematologist* or (h?ematolog* N2 specialist*) or hepatologist* or immunologist* or (infectious N2 diseas* N2 specialist*) or intensivist* or internist* or medic or medics or neonatologist* or nephrologist* or neurologist* or obstetrician* or oncologist* or ((cancer or malignancy) N2 specialist*) or ophthalmologist* or (orthop?edic N2 specialist*) or orthop?edist* or otolaryngologist* or pathologist* or p?ediatric* or perinatologist* or pharmacist* or phlebologist* or physiatrist* or physician* or podiatrist* or psychiatrist* or pulmonologist* or radiologist* or rheumatologist* or surgeon* or urologist* or urogyn?ecolog* or vaccinologist*) OR AB (an?esthesiologist* or an?esthetist* or cardiologist* or dermatologist* or diabetologist* or doctor* or endocrinologist* or epileptologist* or gastroenterologist* or (general N2 practitioner) or GP or geriatrician* or gerontologist* or gyn?ecologist* or h?ematologist* or (h?ematolog* N2 specialist*) or hepatologist* or immunologist* or (infectious N2 diseas* N2 specialist*) or intensivist* or internist* or medic or medics or neonatologist* or nephrologist* or neurologist* or obstetrician* or oncologist* or ((cancer or malignancy) N2 specialist*) or ophthalmologist* or (orthop?edic N2 specialist*) or orthop?edist* or otolaryngologist* or pathologist* or p?ediatric* or perinatologist* or pharmacist* or phlebologist* or physiatrist* or physician* or podiatrist* or psychiatrist* or pulmonologist* or radiologist* or rheumatologist* or surgeon* or urologist* or urogyn?ecolog* or vaccinologist*)
S16 TI ((allied health N3 (professional* or personnel or worker* or practitioner*)) or NMAHP* or AHP*) OR AB ((allied health N3 (professional* or personnel or worker* or practitioner*)) or NMAHP* or AHP*)
S17 TI (nurs* or midwife* or midwives* or (health N2 visitor*) or (art N2 therapist) or chiropodist* or podiatrist* or dietician* or (hearing N2 aid* N2 dispenser*) or ((physical or occupational) N2 therapist*) or orthoptist* or paramedic* or physiotherapist* or psychologist* or prosthetist* or orthotist* or radiographer* or ((speech N2 language N2 (therapist* or pathologist*)) or SLT*)) OR AB (nurs* or midwife* or midwives* or (health N2 visitor*) or (art N2 therapist) or chiropodist* or podiatrist* or dietician* or (hearing N2 aid* N2 dispenser*) or ((physical or occupational) N2 therapist*) or orthoptist* or paramedic* or physiotherapist* or psychologist* or prosthetist* or orthotist* or radiographer* or ((speech N2 language N2 (therapist* or pathologist*)) or SLT*))
S18 TI ((key or frontline or front‐line) N3 (staff or worker* or workforce or personnel or volunteer* or professional*)) OR AB ((key or frontline or front‐line) N3 (staff or worker* or workforce or personnel or volunteer* or professional*))
S19 S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18
S20 (MH "Disease Outbreaks")
S21 TI (((health* or disease*) N5 (disaster* or catastrophe* or crises or crisis)) or outbreak* or pandemic* or epidemic*) OR AB (((health* or disease*) N5 (disaster* or catastrophe* or crises or crisis)) or outbreak* or pandemic* or epidemic*)
S22 (MH "Influenza, Human+") OR (MH "Ebola Virus") OR (MH "Zika Virus") OR (MH "Pneumonia, Viral") OR (MH "Coronavirus") OR (MH "Middle East Respiratory Syndrome Coronavirus") OR (MH "SARS Virus") OR (MH "Coronavirus Infections") OR (MH "Middle East Respiratory Syndrome") OR (MH "Severe Acute Respiratory Syndrome")
S23 (MH "Hemorrhagic Fevers, Viral+")
S24 TI (((h?emorrhagic or yellow or rift valley or lassa) N3 fever) or ebola or ebolavirus or ((nipah or marburg or hendra or zika) N2 virus)) OR AB (((h?emorrhagic or yellow or rift valley or lassa) N3 fever) or ebola or ebolavirus or ((nipah or marburg or hendra or zika) N2 virus))
S25 TI (chikungunya or cholera or smallpox or small pox or monkeypox or plague or tularaemia) OR AB (chikungunya or cholera or smallpox or small pox or monkeypox or plague or tularaemia)
S26 TI ((avian or bird or fowl) N5 (influenza or flu or plague)) OR AB ((avian or bird or fowl) N5 (influenza or flu or plague))
S27 TI ((bacterial N2 meningitis) or (meningococcal N2 diseas*)) OR AB ((bacterial N2 meningitis) or (meningococcal N2 diseas*))
S28 TI (severe acute respiratory syndrome or SARS or coronavirus or ((atypical or influenza or viral or virus) N3 (pneumonia or bronchopneumonia or infection))) OR AB (severe acute respiratory syndrome or SARS or coronavirus or ((atypical or influenza or viral or virus) N3 (pneumonia or bronchopneumonia or infection)))
S29 TI (coronavirus* or corona virus* or HCoV* or ncov* or covid* or sars‐cov* or sarscov* or sars‐coronavirus*) OR AB (coronavirus* or corona virus* or HCoV* or ncov* or covid* or sars‐cov* or sarscov* or sars‐coronavirus*)
S30 S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29
S31 S11 AND S19 AND S30 [Limiters ‐ Publication Year: 2002‐2020]
Appendix 7. Global Index Medicus databases search strategy
Global Index Medicus databases search strategy
(tw:((((clinical OR health* OR medical OR surgical OR biomedical OR social OR community OR frontline) AND (staff OR worker* OR workforce OR volunteer* OR professional* OR personnel)) OR “allied health” OR therapist* OR nurs* OR clinician* OR physician* OR physiotherap* OR surgeon* OR pharmac* OR AHP* OR NMAHP*))) AND (ti:((depress* OR anxious* OR anxiety OR panic* OR stress OR (mental AND health) OR psychological OR psychosocial OR “psycho‐social” OR emotional OR “post‐traumatic” OR posttraumatic OR wellbeing OR burnout OR “burn‐out” OR cope OR coping OR depersonali* OR resilience))) AND (tw:((((health* OR disease*) AND (disaster* OR catastrophe* OR crises OR crisis)) OR outbreak* OR pandemic* OR epidemic*)))
Appendix 8. WHO Library Database (WHO IRIS)
WHO Library Database (WHO IRIS)
All in IRIS: “wellbeing OR coping OR resilience OR burnout OR depression OR depressed OR anxiety OR depersonalisation OR post‐traumatic OR stress OR preparedness”
Advanced Filters>Title: staff; personnel; workforce; workers; nurse; doctors; outbreak; pandemic; epidemic
Appendix 9. US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov search strategy
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov search strategy
( doctors OR physician OR staff OR surgeon OR specialist OR worker OR workforce OR personnel OR volunteer OR professional OR NMAHP OR AHP ) AND ( stress OR post‐traumatic OR wellbeing OR burnout OR coping OR depersonalisation OR resilience ) AND ( outbreak OR epidemic ) AND AREA[StudyFirstPostDate] EXPAND[Term] RANGE[01/01/2000, 06/12/2030]
Appendix 10. Google scholar (via 2Dsearch)
Google Scholar (via 2Dsearch)
(pandemic|epidemic|"disease outbreak")(healthcare ( workforce|personnel|NMAHP|"frontline staff"| professionals| workers|"social care"))(resilience|burnout|wellbeing|"mental health"|cope|"mental fatigue"|"post traumatic"|PTSD)
Appendix 11. World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) search strategies
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) search strategies (Last search attempted on 28 May 2020). At the time of searching, the ICTRP database was not accessible because of the high traffic generated by the virus outbreak. Repeated attempts were made to conduct searches over the succeeding months.
1. stress AND outbreak OR post‐traumatic AND outbreak OR wellbeing AND outbreak OR burnout AND outbreak OR coping AND outbreak OR depersonalisation AND outbreak OR resilience
2. stress AND epidemic OR post‐traumatic AND epidemic OR wellbeing AND epidemic OR burnout AND epidemic OR coping AND epidemic OR depersonalisation AND epidemic OR resilience
3. stress AND pandemic OR post‐traumatic AND pandemic OR wellbeing AND pandemic OR burnout AND pandemic OR coping AND pandemic OR depersonalisation AND pandemic OR resilience
Appendix 12. GRADE‐CERQual evidence profiles
| Finding | Studies contributing | Assessment for each GRADE‐CERQualcomponent | Overall GRADE‐CERQualassessment and explanation | |||
|
Methodological limitations |
Coherence | Relevance | Adequacy | |||
| 1. Flexible interventions that were culturally appropriate, adaptable and/or able to be tailored to meet local needs were seen as key to successful implementation. |
Blake 2020; Brown‐Johnson 2020; Cheung 2015; De Jong 2019; Ferranti 2016; Schreiber 2019; Waterman 2018 |
Moderate concerns as 2 studies had major limitations |
No or very minor concerns |
Minor concerns as studies had a good geographical spread and reported across several settings | No or very minor concerns as the finding was based on 7 studies, 4 of which included reasonably thick data |
Moderate confidence Downgraded because we had moderate concerns regarding methodological limitations. We had no or very minor concerns about coherence, relevance and adequacy. |
| 2. Interventions characterised as having a low level of complexity were seen as easier to implement. |
Blake 2020; Brown‐Johnson 2020; Ferranti 2016; Son 2019 |
Minor concerns as 1 study had major limitations | Moderate concerns about the fit between the data from primary studies and the review finding | Moderate concerns as studies had limited geographical spread and reported across limited settings | Moderate concerns as the finding was based on 4 studies; 3 of these studies had moderately thin data |
Low confidence Downgraded because we had moderate concerns regarding coherence, relevance and adequacy. We had minor concerns about methodological limitations. |
| 3. Intervention costs and associated costs of implementing the intervention were seen as both hindering and facilitating implementation. |
Blake 2020; De Jong 2019 |
No concerns | Moderate concerns about the fit between the data from primary studies and the review finding | Moderate concerns as studies had limited geographical spread and reported across limited settings | Moderate concerns as the finding was based on 2 studies with moderately thin data |
Low confidence Downgraded because we had moderate concerns regarding, coherence, relevance and adequacy. We had no concerns about the methodological limitations. |
| 4. Lack of awareness about the needs and resources of frontline workers was seen as a barrier to implementation. This included lack of awareness of frontline workers' of their own needs, and lack of awareness of organisations who employed and supported frontline workers. |
Belfroid 2018; Cao 2020; Chang 2006; Chen 2020; Cheung 2015; Cunningham 2017; De Jong 2019; Ferranti 2016; Klomp 2020; Lee 2005; Schreiber 2019; Waterman 2018 |
Moderate concerns as 3 studies had major limitations | Minor concerns about the fit between the data from primary studies and the review finding | Minor concerns as studies had a good geographical spread and reported across several settings | Minor concerns as the finding was based on 12 studies, 5 of which included reasonably thick data |
Moderate confidence Downgraded because we had moderate concerns regarding methodological limitations. We had minor concerns about coherence, relevance and adequacy. |
| 5. Awareness of mental health needs by governments and political leaders was identified as a facilitator. |
Cheung 2015; Klomp 2020 |
Serious concerns as both studies judged to have major limitations | Minor concerns about the fit between the data from primary studies and the review finding | Moderate concerns as studies had limited geographical spread and reported across limited settings | Moderate concerns as the finding was based on 2 studies with moderately thin data |
Very low confidence Downgraded because we had serious concerns about the methodological limitations of these studies, and moderate concerns regarding relevance and adequacy. |
| 6. Networking between organisations involved in providing frontline services, and co‐ordinating multiple external organisations in a crisis was seen as both a barrier and a facilitator to implementation. |
Blake 2020; Cheung 2015; De Jong 2019 |
Minor concerns as 1 study had major limitations | Moderate concerns about the fit between the data from primary studies and the review finding | Moderate concerns as studies had limited geographical spread and reported across limited settings | Moderate concerns as the finding was based on 3 studies with moderately thin data |
Low confidence Downgraded because we had moderate concerns regarding coherence, relevance and adequacy. We had minor concerns about the methodological limitations. |
| 7. Effective communication, and cohesion through horizontal and vertical networks, was seen to strengthen social capital and improve team resilience and was considered to be a key factor in implementation. |
Belfroid 2018; Blake 2020; Cao 2020; Chang 2006; Cheung 2015; Cunningham 2017; Klomp 2020; Lee 2005 |
Moderate concerns as 3 studies had major limitations | No or very minor concerns about the fit between the data from primary studies and the review finding | Minor concerns as studies had a good geographical spread and reported across several settings | No or very minor concerns as the finding was based on 8 studies, 4 of which included reasonably thick data |
Moderate confidence Downgraded because we had moderate concerns regarding methodological limitations, and no or very minor concerns about coherence, relevance and adequacy. |
| 8. Organisational incentives and rewards for frontline workers were seen as important in facilitating and engaging student healthcare workers and frontline staff with the intervention |
Belfroid 2018; Chang 2006; Ferranti 2016; Waterman 2018 |
Minor concerns as 1 study had major limitations | Moderate concerns about the fit between the data from primary studies and the review finding | Moderate concerns as studies had limited geographical spread and reported across limited settings | Moderate concerns as the finding was based on 4 studies with moderately thin data |
Low confidence Downgraded because we had moderate concerns regarding coherence, relevance and adequacy. We had minor concerns about the methodological limitations. |
| 9. A positive learning climate for everyone involved in implementation of an intervention was seen to facilitate implementation. |
Belfroid 2018; Brown‐Johnson 2020; Carvalho 2019; Chang 2006; Cheung 2015; Cunningham 2017; De Jong 2019; Lee 2005 |
Moderate concerns as 3 studies had major limitations | No or very minor concerns about the fit between the data from primary studies and the review finding | Minor concerns as studies had a good geographical spread and reported across several settings | Minor concerns as the finding was based on 8 studies, 5 of which included reasonably thick data |
Moderate confidence Downgraded because we had moderate concerns regarding methodological relevance. We had no or very minor concerns about coherence, relevance and adequacy. |
| 10. Resource constraints, including lack of equipment, staff time and skills, were described as hindering implementation. |
Belfroid 2018; Brown‐Johnson 2020; Cao 2020; Chang 2006; Chen 2020; Cunningham 2017; De Jong 2019; Waterman 2018 |
Moderate concerns as 2 studies had major limitations |
No or very minor concerns about the fit between the data from primary studies and the review finding | Minor concerns as studies had a good geographical spread and reported across several settings | Minor concerns as the finding was based on 8 studies, 5 of which included reasonably thick data |
Moderate confidence Downgraded because we had moderate concerns regarding methodological limitations, and no or very minor concerns about coherence, relevance and adequacy. |
| 11. Education, training, and access to information for frontline workers was considered an important step underpinning the readiness for implementation, and was seen to act as a barrier or facilitator depending on the quality provided. |
Belfroid 2018; Chang 2006; Chen 2020; Cheung 2015; De Jong 2019; Ferranti 2016 |
Moderate concerns as 3 studies had major limitations | Minor concerns about the fit between the data from primary studies and the review finding | Moderate concerns as studies had limited geographical spread and was reported across limited settings | Moderate concerns as the finding was based on 6 studies with moderately thin data |
Low confidence Downgraded because we had moderate concerns regarding methodological limitations, relevance and adequacy. We had minor concerns about coherence. |
| 12. Frontline workers knowledge and beliefs about the intervention were seen to act as either a barrier or facilitator to implementation. |
Belfroid 2018; Blake 2020; Carvalho 2019; Chen 2020; Cunningham 2017; De Jong 2019; Waterman 2018 |
Minor concerns as 1 study had major limitations | No or very minor concerns about the fit between the data from primary studies and the review finding | Minor concerns as studies had a good geographical spread and reported across several settings | Moderate concerns as the finding was based on 7 studies, 3 with moderately thin data |
Moderate confidence Downgraded because we had moderate concerns regarding adequacy. We had no or very minor concerns about methodological limitations, coherence and relevance. |
| 13. Frontline workers' confidence in their ability to deliver and implement an intervention was seen as an important factor in successful implementation. |
Belfroid 2018; Brown‐Johnson 2020; Carvalho 2019; Cunningham 2017; Ferranti 2016 |
Minor concerns as 1 study had major limitations | Moderate concerns about the fit between the data from primary studies and the review finding | Moderate concerns as studies had limited geographical spread and was reported across limited settings | Moderate concerns as the finding was based on 5 studies all with moderately thin data |
Low confidence Downgraded because we had moderate concerns regarding about coherence, relevance and adequacy. We had minor concerns about methodological limitations. |
| 14. Individual personal characteristics and attributes of frontline professionals, such as their attitudes and motivation, were seen to act as either a barrier or facilitator to implementation. |
Belfroid 2018; Chang 2006; Cheung 2015; Cunningham 2017; De Jong 2019; Lee 2005; Waterman 2018 |
Moderate concerns as 2 studies had major limitations | No or very minor concerns about the fit between the data from primary studies and the review finding | Moderate concerns as studies had limited geographical spread and was reported across limited settings | Moderate concerns as the finding was based on 7 studies, 3 of which had moderately thin data |
Low confidence Downgraded because we had moderate concerns regarding methodological limitations, relevance and adequacy. |
| 15. Planning to prepare individual frontline workers and organisations to implement changes was often reported to be overlooked, resulting in frontline workers feeling rushed and unprepared. Strategic plans at the level of the individual healthcare worker and organisation were considered to facilitate the success of the implementation. |
Belfroid 2018; Brown‐Johnson 2020; Cao 2020; Chang 2006; Chen 2020; Ferranti 2016; Klomp 2020; Waterman 2018 |
Moderate concerns as 4 studies had major limitations | No or very minor concerns about the fit between the data from primary studies and the review finding | Minor concerns as studies had a good geographical spread and reported across several settings | Moderate concerns as the finding was based on 8 studies, 4 with moderately thin data |
Low confidence Downgraded because we had moderate concerns regarding methodological limitations and adequacy. We had no or very minor concerns about coherence and relevance. |
| 16. Meaningful engagement of people involved in the delivery of interventions to support mental health, and forming strong collaborations with champions and opinion leaders, were seen to positively impact on implementation. |
Belfroid 2018; Blake 2020; Brown‐Johnson 2020; Cunningham 2017; Klomp 2020; Lee 2005; Son 2019; Waterman 2018 |
Moderate concerns as 2 studies had major limitations | Minor concerns about the fit between the data from primary studies and the review finding | Minor concerns as studies had limited geographical spread and was reported across limited settings | Moderate concerns as the finding was based on 8 studies, of which 3 studies had moderately thin data |
Low confidence Downgraded because we had moderate concerns regarding methodological limitations and adequacy. We had minor concerns regarding coherence and relevance. |
| 17. The opportunity for frontline workers to reflect on, evaluate or take part in a debriefing session was seen to promote a sense of safety, and support shared learning which facilitated the implementation process. |
Belfroid 2018; Blake 2020; Carvalho 2019; Cunningham 2017; De Jong 2019; Klomp 2020 |
Minor concerns as 1 study had major limitations | Minor concerns about the fit between the data from primary studies and the review finding | Moderate concerns as studies had limited geographical spread and was reported across limited settings | Moderate concerns as the finding was based on 6 studies, of which 3 studies had moderately thin data |
Low confidence Downgraded because we had moderate concerns regarding relevance and adequacy. We had minor concerns regarding methodological limitations and coherence. |
Appendix 13. CASP assessments, with support for judgement
| Study | 1. Was there a clear statement of the aims of the research? | 2. Is a qualitative methodology appropriate? | 3. Was the research design appropriate to address the aims of the research? | 4. Was the recruitment strategy appropriate to the aims of the research? | 5. Were the data collected in a way that addressed the research issue? | 6. Has the relationship between researcher and participants been adequately considered? | 7. Have ethical issues been taken into consideration? | 8. Was the data analysis sufficiently rigorous? | 9. Is there a clear statement of findings? | Overall assessment |
| Belfroid 2018 |
Yes "The aim of this study was to gain insight into how healthcare organizations can prepare for meeting the needs of their healthcare personnel. We did this by studying the experiences of HCWs who dealt with patients with suspected Ebola virus disease." |
Yes |
Yes Design was "in‐depth interviews", which is appropriate to the stated aims. |
Yes "We invited HCWs who had cared for a patient with suspected Ebola or were part of the team that had prepared for admission of such patients in several university hospitals in the Netherlands. We also invited HCWs from regional ambulance services who had transported a patient with suspected Ebola." |
Yes "The interviews lasted 25 min to 1 h. Each interview started with a short explanation about the goal of the study. The interviews were semi‐structured. We used an interview guide that included a topic list about HCWs’ potential needs from a systematic literature review of outbreak preparedness (A. Huis et al., unpublished data)." |
Cannot tell There is insufficient information on the role of the researcher and potential bias or influence |
Yes "The Medical Ethics Committee of the University Medical Center Utrecht assessed the study and concluded that it was exempt from their approval." |
Yes "A thematic analysis was applied and the main themes extracted from the data. Patterns in the data were identified with an iterative process in research group meetings." Quotes are provided to support each of the themes identified. |
Yes Key themes are presented and discussed. Limitations are stated |
No or few limitations |
| Cao 2020 |
Yes "The objectives of the present study were to examine COVID‐19‐related stress and its immediate psychological impact among medical workers in the fever clinic." |
Yes |
Cannot tell Methods are appropriate: "Qualitative and quantitative evaluations via telephone" "Fixed guiding words helped medical workers understand the meaning of the interview. Open qualitative interviews were conducted in the first step, followed by quantitative questionnaires. Hotline workers stopped the interview if necessary to provide essential support." However it is unclear whether or not the interviews and evaluations formed part of the psychological support intervention. |
Yes "Thirty‐seven medical workers in the first batch and 68 medical workers in the second batch were to stay and work in the hospital continuously for 2‐3 weeks and then leave the fever clinic......All medical workers at fever clinic during that time period were eligible for the study,.." |
Yes "Qualitative and quantitative evaluations" |
Cannot tell The relationship between the research project and the 'hotline' is unclear. Hotline workers may have been listening in to the interview: "Hotline workers stopped the interview if necessary to provide essential support." Some interviews seem to have been initiated by the hotline workers and some by the participants. When describing the qualitative interview questions it is stated that "The administrator of the hotline provided continuous feedback on findings to the Department of Emergency, the Medical Affairs Office and the labor union..." The relationship between the researcher, participants, the intervention provider and external bodies are therefore unclear. |
Cannot tell Paper states: "The study was approved by the ethics committee of the hospital. Oral informed consent was obtained before the interview began." However it is unclear if ethical issues relating to the relationship issues described above have been considered. |
Cannot tell Lack of information about how qualitative evidence was analysed. |
Yes Findings are described in 2 papers. |
Minor limitations |
| Chen 2020 |
No The aim is not clearly stated. It appears that the interviews were carried out in order to explore reasons why "medical staff were reluctant to participate" in a psychological intervention service. |
Yes Qualitative methodology is appropriate to explore reasons for non‐participation in an intervention. |
Cannot tell Few details are provided about the research design. |
Cannot tell No information about recruitment strategy. |
Cannot tell Only details given are that "a 30‐min interview survey with 13 medical staff" was carried out. |
Cannot tell Lack of detail |
Cannot tell Lack of detail |
Cannot tell No information about data analysis |
Yes Key findings are briefly listed. |
Major limitations |
| Cunningham 2017 |
Yes ‐ partly There is a clear study aim relating to experiences of narrative medicine: "to examine how expatriate healthcare providers used narrative methods to process their experiences working with Ebola patients and whether these processes were therapeutic". The study aim for the first part of the interview study is not very clear, and it is stated that the aim of the qualitative interviews was to "validate findings" from the survey. The results from the first phase provided evidence relating to interventions, and this was not clearly stated as the aim of that part of the study, but it was a specific question in the interview guide ("What are some coping mechanisms that you used and use to manage the memories of experiences while working in the Ebola response? Please describe what you did while working in West Africa as well as after you returned.") |
Yes The aim was to explore experiences. |
Cannot tell Although interviews were appropriate to explore experiences; the extent to which the participants were familiar with "narrative medicine" is not clear. It is not clear whether this is an 'intervention' that frontline workers were encouraged to use or not. |
Yes The participants comprised respondents to a survey (linked study) who consented to being interviewed. |
Yes The full interview guide is provided. |
Yes This is discussed, and potential bias acknowledged: "It should also be noted that TC worked as an EVD [Ebola virus disease] volunteer and thus brings a unique perspective, as well as bias to this analysis." |
Yes Approval granted from "Institutional Review Board approval from Columbia University Medical Center" |
Yes Methods are described for qualitative analysis. Six people were involved in the analyses. |
Yes Key themes and subthemes are stated. |
No or few limitations |
| De Jong 2019 |
Yes "The aim of the study reported here is to understand how the PFA approach was used during the Ebola outbreak in Sierra Leone and Liberia, and to learn lessons from this which can be applied in other emergency contexts to strengthen the psychosocial support offered by first responders." |
Yes Qualitative interviews are appropriate. |
Yes |
Cannot tell Purposive sampling technique was used. However "unfortunately, many of the key individuals had since left West Africa and could not be interviewed." ‐ this may affect the results collected. |
Yes Interviews were audio‐recorded |
Cannot tell "In each country, data collection was led by a research coordinator (third and 4th authors) who recruited the research assistants locally. In Sierra Leone, 4 research assistants were recruited who both conducted and transcribed the interviews. In Liberia, 4 research assistants were recruited to conduct interviews, plus 4 transcribers. The data collection process was supported by the lead researcher (first author) who trained the research assistants and transcribers, and provided additional supervision and support to research coordinators, research assistants and transcribers during the first week of data collection. The lead researcher and the research coordinators conducted the key informant interviews". Lack of information about the relationship between researchers/interviewers and participants, and whether use of different interviewers for interviews with different groups of participants may have affected data collected. |
Yes "This study was given favourable ethical approval by Queen Margaret University Edinburgh Research Ethics Committee, the Office of the Sierra Leone Ethics and Scientific Review Committee, and the University of Liberia Pacific Institute for Research Review Board (UL‐PIRE)" |
Yes "The first author developed a coding scheme involving three levels with which excerpts of the data could be labelled........The lead researcher then worked with two other analysts (second and fifth authors) to trial the coding scheme, discuss discrepancies, and make modifications... following which all three coders worked on coding the transcripts using the on‐line analysis package, Dedoose. Once the coding was complete, the same team worked on the data analysis. The draft results were shared with and discussed by the entire research team at a workshop in January 2017, following which they were revised and finalised." |
Yes Clear themes and subthemes are provided, supported by quotations. |
No or few limitations |
| Lee 2005 |
Yes "to understand the needs and experiences of frontline female nurses in order to provide better psychiatric services in future epidemics." |
Yes |
Yes "Nurses were interviewed in small groups of 4 to 6. The interviews followed a semistructured schedule derived from previously identified issues. Based on the analysis of the interview protocols, the SARS Team Questionnaire was developed. Twenty‐six (87%) female nurses who gave informed consent to participate in the survey then completed this questionnaire." |
Yes The population was the "SARS team of nursing staff", which comprised "Thirty female senior nurses from the emergency department". Participants were recruited from this group of 30, on a voluntary basis. |
Cannot tell There is information about the design and use of the "SARS Team Questionnaire, and the quantitative analysis of this. However, there is little information about the interviews/focus groups and how data were collected and analysed. |
No It is not stated who conducted the interviews, however it is inferred that the author team included the SARS "team leader" and "psychiatrist." This suggests that the researchers may have had roles in the SARS team from whom participants were recruited. This relationship could impact on the study and results. |
Cannot tell No information |
Cannot tell There is a lack of information about data analysis. Results presented are largely quantitative, from the survey, rather than the qualitative evidence from the interviews. |
Yes‐ partly There is a clear statement of results from the survey (questions were developed from initial interviews), but these are not fully supported by qualitative evidence. |
Minor limitations |
| Son 2019 |
Yes "to reflect actual experiences of hospital workers by using qualitative data collected in real time during the 2015 MERS outbreak in South Korea." |
Yes "Qualitative methodology was adopted to investigate the negative emotion and stress of hospital workers during an outbreak, and the triggers behind those emotions and stress." |
Cannot tell Unclear ‐ not a standard qualitative design, and only a small amount of data per participant: "At the end of the program's session, the participants were encouraged to leave a short, anonymous note (1 note per participant) on the “Let It Out” panel prepared by the session moderator. In these notes, hospital workers wrote about their emotions, stress, and trigger events that were most representative of what they verbally communicated during the session...........After the implementation of the program sessions was ended, the “Let It Out” panels were gathered at the center, where the short notes were then removed from the panels and collected. Overall, 156 short notes were collected and electronically transcribed for analysis." |
No Lack of information about recruitment. It is inferred that a much larger number of people attended the training, but only 156 "left a note". It is acknowledged that "it is possible that the experiences of hospital workers who left a short note and those who did not leave a note are not entirely consistent. For example, the latter might have had a greater workload and felt more emotionally distressed and therefore unable or unwilling to participate in the program..." |
Cannot tell See previous ‐ unusual data collection method, with only small amount of data per participant. |
No "Department heads.....implemented the program to their respective departments as they played the role of the moderator". The role or influence of the department head as monitor is not discussed. |
Cannot tell Lack of information |
Yes A detailed analysis method is described. |
Yes Themes and subthemes are described clearly, supported by evidence. |
Minor limitations |
Appendix 14. WEIRD assessments, with support for judgement
| Study | 1. Is there a clearly stated aim, objective or purpose for the source material? | 2. Is there a clear description of the source of the information reported (transparency)? | 3. Is there a clear description of the programme or intervention or policy or reform on which the source material focuses? | 4. Is there a clear description of the context/s to which the information described in the source material relates? | 5/6. Is the information accurate? (non‐empirical/empirical studies) | 7. Is the evidence representative? | 8. Are any limitations of the information and/or methods discussed in the source material? | 9. Is evidence provided to support any findings or conclusions made? | 10. Are relevant rights and ethics considerations described? | 11. Are any interests declared and any potential conflicts of interest noted? | Overall assessment |
| Blake 2020 |
Yes "The aim of this study was to synthesise evidence‐based information to rapidly develop and evaluate a digital learning package to support psychological well‐being for all healthcare workers." |
Yes "This study was based on a three‐step process, including public involvement activities, content and technical development with iterative peer review, delivery (number of users accessing the package plus Twitter engagement within 7 days of launch) and evaluation. Each step is reported separately as a distinct element of the study, combining methods and results." |
Yes There is a description, and the full digital learning package is available online: www.nottingham.ac.uk/toolkits/play |
Yes The intervention was developed in response to the COVID‐19 pandemic. |
Yes Methods and results are presented in some detail for each step of the intervention development and evaluation. |
Unclear The authors state that "This digital package is considered to be appropriate for any UK healthcare professional as well as healthcare academics and students, with much of the content having international relevance." However, the digital package was evaluated with healthcare workers and students who were recruited via professional networks over a 3‐day period, during the COVID‐19 pandemic. It is unclear whether this will have resulted in a representative sample. |
Yes "Since this project was a rapid response to COVID‐19, with a need for immediate package implementation, the evaluation was limited to a small sample of healthcare workers from the UK. There is scope for further evaluation studies to investigate healthcare workers’ perceptions towards and use of the package and any resulting changes in actions (e.g. communication, team approaches, self‐care and managing emotions)." |
Yes Data were collected on use of the digital package, and 55 participants took part in a "fidelity assessment." |
Yes "The authors adhered to the British Psychological Society (BPS) Code of Human Research Ethics." |
Yes "This research received no external funding—it was conducted as a rapid response to the COVID‐19 pandemic." "The authors declare no conflict of interest." |
No or few limitations |
| Brown‐Johnson 2020 |
Yes "In preparation for a larger evaluation of the effectiveness of PPE Portraits on patient and provider experience, we collected initial qualitative data on implementation barriers and facilitators during the chaotic surge preparation activities of March and April 2020. We share practical lessons for implementing similar programs for others to use." |
Unclear Lack of information |
Yes There is a description of the intervention ("PPE portraits") and a figure describing the process of using these. |
No "Stanford Express Care is piloting PPE [personal protective equipment] Portraits for the newly created drive‐thru COVID‐19 testing. Similarly, the inpatient palliative care team at UMass Memorial Medical Center has begun using PPE Portraits in caring for seriously ill patients in the hospital, regardless of infection status." No further information about the context is provided. |
Unclear Lack of information about how the information was collected or analysed. |
Unclear Lack of information about context, participants and the collection of data makes this difficult to judge. |
No No limitations discussed |
No One brief quote is provided. No other evidence is provided. |
Unclear No information |
Yes "The authors declare that they do not have a conflict of interest". |
Major limitations |
| Carvalho 2019 |
Yes "The purpose of this study was to assess the impact of multi‐professional simulation‐based training on the risk perception and preparedness of health care workers (registered nurses, doctors and ancillary staff) who care for patients assessed to be at risk or confirmed to have Ebola, level 3 – 4 biohazard." |
Yes A "prospective before – after study" is described. |
Yes There is a written description of the "multi‐professional simulation‐based training" |
Yes There is a description of the "population and field of study." |
Yes Study results are presented for: "two different self‐questionnaires: one for self‐assessment, which was completed before and after the course was performed, and another for satisfaction to be completed after the course" |
No Participation was voluntary, so evidence only applies to the population who volunteer to participate and who "provided informed consent, completed the course and self‐completed any of the three questionnaires." All participants came from the same hospital. |
Yes "This study has some limitations that should be considered. The main ones are the small sample size, especially in the participant groups of doctors and stretcher bearers, and those data come from only one hospital, which could affect the generalization of our results." |
Yes Empirical data from questionnaires are provided. |
Yes "The Ethics Committee of Hospital Clinic in Barcelona approved the study (HCB/2014/1072). Participants who agreed to participate signed an informed consent form after receiving all the information and instructions about the study." |
Unclear No conflict of interest statement. Funding statement: "Capes Foundation Ministry of Education of Brazil for research fellowship (Eva Carvalho, Doctoral Fellow Capes – Proc.No. BEX 2715139– ). The funder had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript." |
Minor limitations |
| Chang 2006 |
Yes "The purpose of this study is to examine whether social capital can enhance an individual’s ability in reducing emotional exhaustion and job tension when medical professionals encounter a crisis such as SARS." Two hypotheses were also developed from published evidence/theories: "Hypothesis 1: Social interaction is negatively related to (a) emotional exhaustion and (b) job tension. Hypothesis 2: Trust is negatively related to (a) emotional exhaustion and (b) job tension." |
Yes Data were collected through a survey. The methods of this are described. |
Yes There is a theoretical description, based on previous research, of "social capital, emotional exhaustion and job tension", and the key dimensions of social capital are described. |
Yes The context described is the SARS crisis in Taiwan in 2003. |
No The data collected were levels of agreement relating to "seven statements that reflected two key dimensions of social capital (social interaction and trust)", and statements aimed at measuring social interaction, trust, emotional exhaustion and job tension. The validity of these measures was explored and the results are reported. However this study has used a survey to explore questions relating to the relationship between social capital and outcomes ‐ the authors acknowledge: "this research is based on cross‐sectional data. Therefore, the direction of causality cannot be established. Future research should consider adopting longitudinal data to further test the causal order of the factors." |
No The respondents all came from 4 medical centres in Taiwan. Response rate was 53% (211 out of 400 questionnaires analysed). There is evidence of some imbalance ‐ e.g. 75% were female. Only a small proportion had actually cared for SARS patients: "Fifty‐one per cent of the sample respondents had at least some temporary contact with SARS patients, 16 per cent cared for SARS patients, and 33 per cent did not have contact with SARS patients". The authors acknowledge that these findings may not be generalisable to other countries or cultures, especially as "Cultural differences also influence the creation of social capital. Factors such as deference to authority, stoicism, fatalism, societal cohesiveness, and social homogeneity could affect how trust and social capital are built and maintained." |
Yes Limitations are discussed. |
No Conclusions and implications suggesting that "social capital would aid medical organizations in managing crises such as SARS" are made, and specific recommendations are made. But given the acknowledged limitations, such conclusions do not appear to be fully supported. |
Unclear No information |
Unclear No information |
Major limitations |
| Cheung 2015 |
Yes "This field report will summarise some of these psychosocial issues: fear in local communities and among aid workers, the spreading of rumours, health measures interfering with traditional rituals, and stigmatisation. It will also offer some suggestions for dealing with these issues." |
No This is a report of "the experience and lessons learnt by the author." |
No The author refers to a number of psychosocial support strategies which she encountered/observed, but there is not a clear description of the elements of these. |
Yes There is a description of the local communities in Liberia, with examples given, based on reports from the author and other aid workers. |
Yes There is a description of the local communities in Liberia, with examples given, based on reports from the author and other aid workers. |
No The information was not systematically collected, and is based on the author's memory, beliefs and opinion. |
Unclear Lack of information |
Yes ‐ partly There are some documents/evidence cited in support of the author's conclusions. |
Unclear No information |
Unclear No information. It is reported that the author "works as a clinical psychologist for the Hong Kong Red Cross. She has coordinated and provided emergency mental health and psychosocial support response and preparedness programmes in Hong Kong, Bhutan, and various rural and disaster‐affected counties in China" |
Major limitations |
| Ferranti 2016 |
Yes "To describe the development, implementation, and evaluation of the EVD Just‐in‐Time Teaching (JiTT) educational program." |
Yes The methods of development, implementation and evaluation are described. |
Yes The training programme is described. |
Yes The University, and links with Ebola treatment, are described. |
Yes Survey results are presented. |
No The authors acknowledge that there are limitations to the generalisability of this evidence. |
Yes The limitations are discussed, including the number of dropouts who did not complete the final survey, and limited generalisability of findings. |
Yes Conclusions are supported by the survey findings. |
Unclear No information |
Unclear No information |
Minor limitations |
| Klomp 2020 |
No There is no clear aim. It is stated that "The accompanying special report highlights innovative pre‐deployment training initiatives, customized screening processes, and post‐deployment outreach efforts intended to protect and support the public health professionals fighting Ebola." |
No There is not a clear description. The report contains a variety of information from different sources, and it is not clear how this information was selected or put together. |
Unclear There are descriptions of a variety of different training initiatives. However, it is not clear how these relate to each other (e.g. who attended different training etc). |
No It is not clear what the roles of the Ebola responders were. Some of the evidence appears to relate to responses to other health emergencies, e.g. in relation to "post‐deployment outreach" it is stated that: "the resilience team contacted hundreds of CDC professionals when they returned from deployment to the 2005 Marburg Hemorrhagic, Fever outbreak, the 2005 Hurricane Katrina response, and the 2010 Haiti earthquake. During the 2014–2016 Ebola outbreak in West Africa, the CDC formalized post‐deployment outreach processes......" |
Unclear There is insufficient information to judge accuracy of the results presented in the text (e.g. it is reported that "approximately 100 individuals completed the three‐day DSRT training during the Ebola response" and that pre‐ and post‐assessments were carried out. Average scores and change scores, and confidence intervals are provided in the text for some outcomes, but there is a lack of information about participants, methods or analysis. Figures 2 and 3 contain data but it is unclear what the date relate to). |
Unclear Lack of information means it is not possible to judge this. |
No No limitations are discussed. |
Unclear There is some evidence provided, but there are insufficient details about this. |
Unclear No information |
Yes "The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention and/or the Agency for Toxic Substances and Disease Registry. The authors have no conflicts of interest to declare." |
Major limitations |
| Schreiber 2019 |
Yes "This paper describes the APD model and how the PsySTART‐R system is integrated to provide objective “self‐triage” metrics for HCWs. Furthermore, this report documents initial piloting of the PsySTART‐R self‐triage system component in a disaster training exercise and a realworld event, and a case example of the full APD model implementation during the 2014–2015 Ebola response." |
Yes The information comes from a number of different "case descriptions". The one relevant to this Cochrane Review is "Implementation of the full APD system during the ebola response in West Africa 2014–2015" |
Yes There is a clear description of the "The Anticipate, Plan and Deter (APD) Responder Risk and Resilience Model" which "was developed to provide a new, evidence‐informed method for understanding and managing psychological impacts among HCWs [healthcare workers], including strategies to manage the full range of risk and resilience in the responder workforce and their families" and "The PsySTART‐Responder Self Triage System (PsySTARTR)" which "is a mobile‐optimized web‐based application that prompts responders to indicate which of 19 traumatic stress risk factors they experienced over a given operational period." |
Unclear There is little information given specifically about the context in which the intervention was implemented; report states that "Ebola medical providers from one US‐based medical effort were trained in the full APD model" but few further details are provided. |
Unclear There is a narrative description, and examples, relating to the implementation of the intervention, but no presentation of results. |
Unclear Insufficient information about the collection of data. |
No No limitations are discussed. |
Yes "A retrospective, qualitative, completely de‐identified analysis of 186 self‐triage encounters from the PsySTART‐R system was conducted using data from the first two groups of HCWs deployed to Africa to assist with Ebola." Data from this analysis are provided to support conclusions. |
Unclear No information |
Unclear No information |
Minor limitations |
| Waterman 2018 |
Yes Three papers report different aspects of this implementation and evaluation study which "trained ETC staff to provide a three‐phase cognitive behavioural therapy (CBT)–based intervention for common mental health problems to fellow ETC staff and explored the effectiveness of this intervention." |
Yes The study is clearly described. |
Yes The CBT intervention, and processes, are clearly described. |
Yes The source material relates to Sierra Leone during the Ebola outbreak. |
Yes A range of different information is presented, with relevant data in text and tables. |
Unclear The evidence is relevant to Sierra Leone and the Ebola outbreak. It may not be more widely generalisable. |
No A number of limitations are discussed, including the lack of control group; limited sample of participants; the fact that "Sierra Leone was declared EVD [Ebola virus disease] free during the second phase of our intervention, so by phase 3 the risk within the country itself had dramatically reduced, which may have led to a natural improvement in peoples’ mental health"; lack of validated CBT materials for low‐literacy populations and use of measures only validated in Western cultures; and "Despite making cultural adaptations to the materials, the intervention was delivered independent of other care systems and without collaboration with traditional healers." |
Yes A wide variety of evidence is provided within 3 different papers. |
Unclear It is unclear whether ethical approval was sought for all aspects of this study, but for the qualitative component it is stated that "Ethical approval was received by the Medical Director of South London and Maudsley NHS Trust." |
Yes "No potential conflict of interest was reported by the author(s)." |
Minor limitations |
Appendix 15. Protocol
Date protocol accepted: 22 July 2020
Objectives
We plan to assess the effects of interventions and factors affecting implementation of interventions aimed at supporting the resilience and mental health of frontline health and social care professionals during a disease outbreak, epidemic or pandemic and following de‐escalation.
We will address the following two key objectives.
What are the effectiveness of interventions to support the resilience and mental health of these frontline health and social care professionals, during a disease outbreak, epidemic or pandemic, and after de‐escalation?
What are the barriers and facilitators that may impact on the implementation of interventions to support the resilience and mental health of these frontline health and social care professionals, during a disease outbreak, epidemic or pandemic, and after de‐escalation?
The methods for conducting and reporting this review will follow the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2020a), the Handbook for Synthesizing Qualitative Research (Sandelowski 2007), and guidance from the Cochrane Qualitative and Implementation Methods Group (CQIMG) (Noyes 2020) and CQIMG supplemental methods papers, Noyes 2018), and Cochrane Effective Practice and Organisation of Care (EPOC) (EPOC 2019).
Methods
Types of studies
To address objective 1, we will include quantitative evidence from the following types of studies.
Randomised trials, i.e. experimental studies in which people are allocated to different interventions using methods that are random. We will include cluster‐randomised trials, in which randomisation is at the level of the site, where a study has at least two intervention sites and two control sites (EPOC 2017a).
Non‐randomised trials, i.e. experimental studies in which people are allocated to different interventions using methods that are not random (EPOC 2017a).
Controlled before‐after study, i.e. studies in which observations are made before and after the implementation of an intervention, both in a group that receives the intervention and in a control group that does not (EPOC 2017a).
Interupted time series study, i.e. studies that use observations at multiple time points before and after an intervention (the ‘interruption’). The design attempts to detect whether the intervention has had an effect significantly greater than any underlying trend over time. For inclusion, these studies must have a clearly defined point in time when the intervention occurred, and at least three data points before and three after the intervention (EPOC 2017a).
We will include evidence from non‐randomised studies as the planning and conduct of randomised studies is likely to be highly challenging during disease epidemics and pandemics. However, evidence from non‐randomised studies has an increased risk of bias; in particular there are a number of confounding factors which may influence whether an individual receives one or other intervention. In relation to interventions to support the mental health and resilience of health and social care professionals, important confounding factors are likely to include the setting that the healthcare professional is working in, the type and grade of health professional, and the length of time that the individual has worked within the disease epidemic/pandemic. Furthermore, there are known differences between men and women in the reporting of mental health symptoms and treatment rates for symptoms, such as depression and anxiety, and gender may therefore be a confounding domain (MHF 2016). There is also a growing body of evidence that socioeconomic status may be associated with an increased chance of developing mental health problems (WHO 2014a), and this could be an important confounding factor in some studies. If these important confounding factors are not controlled for within the non‐randomised studies, we will judge the study to be at high risk of bias.
We will exclude evidence from studies in which the interventions are not assigned by the investigators, including prospective and retrospective cohort and case‐control studies.
To address objective 2, we will include qualitative evidence from:
primary qualitative studies (e.g. ethnography, case studies, and process evaluations);
mixed methods studies, where the qualitative data are reported separately.
We will exclude secondary research (systematic reviews and evidence syntheses). However, where we find relevant secondary research studies, we will consider any primary studies, and include any that meet our inclusion criteria.
Types of participants
We will include studies in which participants are (or have been) health and social care professionals working at the frontline during disease outbreaks, epidemics or pandemics, from the year 2002 onwards.
Operational definitions of key terms are below.
Disease epidemics or pandemics
We will only include studies relating to epidemics or pandemics which have occurred from the year 2002 onwards. Declarations of epidemics or pandemics are not always clear. Outbreaks of disease may or may not be categorised as an epidemic, by the World Health Organization (WHO) or local governments or health service organisations. We will adopt an inclusive approach and not require a formal declaration of epidemic or pandemic; we will accept authors' definitions or categorisation, and include evidence relating to outbreaks of disease, even if this has not been formally declared as an epidemic. We will categorise evidence as “epidemic” or “pandemic” according to the WHO categorisation (WHO 2020a), and other evidence as “outbreak”.
We will include studies conducted during and/or after an epidemic/pandemic.
We will include infectious diseases that are categorised by WHO 2020a as “pandemic or epidemic diseases”, if outbreaks have occurred in 2002 or later. These may include the following.
Chikungunya
Cholera
Crimean‐Congo haemorrhagic fever
Ebola virus disease
Hendra virus infection
Influenza (pandemic, seasonal, zoonotic)
Lassa fever
Marburg virus disease
Meningitis
Middle East respiratory syndrome (MERS)
Monkeypox
Nipah virus infection
Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2)
Plague
Rift Valley fever
Severe acute respiratory syndrome (SARS)
Smallpox
Tularaemia
Yellow fever
Zika virus disease
We will exclude studies relating to diseases which have not been listed by WHO 2020a as a pandemic or epidemic disease. This includes studies relating to the following diseases: insect‐borne diseases, including (but not limited to): dengue fever, malaria, leishmaniasis, measles, hepatitis, hand, foot and mouth disease, mumps, polio, CJD and HIV/AIDS.
The decision to focus on epidemics or pandemics from the year 2002 onwards was made pragmatically, with the aim of limiting the necessary searching, in order to ensure feasibility of carrying out this review rapidly. The year 2002 was considered appropriate as the outbreak of SARS was in 2003, meaning that we would capture studies undertaken in response to SARS, as well as more recent outbreaks of the Ebola virus and MERS (originated 2012). A similar justification for date restriction was used in the Cochrane qualitative evidence synthesis focused on infection control during infectious respiratory diseases (Houghton 2020).
Health and social care professionals
We will include studies in which the participant is any person who works in a health or social care setting in a professional capacity, or who provides health or social care within community settings deployed at the ‘frontline’. This includes, but is not limited to the following.
Doctors
Nurses and midwives
Allied health and social care professionals currently regulated by the Health and Care Professions Council (HCPC 2016). This includes: art therapists, biomedical scientists, chiropodists/podiatrists, clinical scientists, dietitians, hearing aid dispensers, occupational therapists, operating department practitioners, orthoptists, paramedics, physiotherapists/physical therapists, practitioner psychologists, prosthetists/orthotists, radiographers, social workers, speech and language therapists.
Students of any of the above listed professions
Health and social care assistants
We will include health and social care professionals who returned to practice after a period of absence (> 3 months), for example, following a career break or retirement.
We will also include students in education to become health and social care professionals where they enter paid clinical/social care practice early in order to work during the epidemic/pandemic.
We will include volunteers who delivered frontline health or social care services; for example, medical or nursing staff volunteering to assist in different countries. To be included, the volunteer has to be working in a professional role, as listed above.
We will exclude studies including only other people who may have frontline roles, but who are not providing health and social care, such as cleaners and biomedical waste management handlers, or volunteers undertaking tasks such as delivery of medicines.
Frontline
We will define “frontline” as working in any role which brings the person into direct contact (e.g. providing care to) or indirect contact (e.g. managing a team of people who are providing care), or potential contact (e.g. working on the same ward, or setting) with a patient with the disease of interest, or where the patient is suspected of having the disease (e.g. displays symptoms but disease is not yet confirmed) or is considered to be at high risk of contracting the disease (e.g. working in environments where it is considered necessary for staff to wear personal protective equipment (PPE)), or where the staff member is considered to be at risk of contracting the disease.
We will include studies in which there are a mix of different frontline workers, if the majority are health and social care professionals. For example, where an intervention is given to all staff within a particular setting, and these staff include a mix of health and social care professionals and other frontline workers, such as cleaners, porters or receptionists. If possible, we will include data from only the subgroup of health and social care professionals, but if these data are not available, we will include the mixed frontline worker data and plan to explore the inclusion of this within sensitivity analyses.
We will exclude:
studies focused on the mental health and resilience of health and social care professionals, where these people were not working at the frontline of disease epidemics or pandemics; and
studies focused on the psychological, mental health and/or resilience of patients.
Types of interventions
We will include any intervention which is aimed at addressing mental health and/or resilience in the staff identified above. This may include, but is not limited to, the following.
Workplace interventions
Workplace structure and routine interventions, e.g. regular breaks, shorter working hours, regular team meetings, mentorship, relaxation/recreation areas in workplaces
Provision of information, guidance, or training, e.g. on dealing with difficult situations
Interventions to support basic daily needs
Interventions promoting or supporting healthy lifestyle and self‐care: eating, sleeping, exercising, following a routine, avoiding excess social media, staying in touch with family and friends, doing things that are enjoyable
Relaxation techniques, e.g. progressive muscle relaxation, meditation
Psychological support interventions
Therapist‐delivered psychological interventions, delivered individually or in groups, and face‐to‐face or by text or videocall, including professional psychological or counselling support, cognitive behavioural therapy (CBT) and psychotherapy
Guided self‐help strategies, such as online CBT, online/web well‐being and sleep apps, and mindfulness programmes
Non‐guided self‐help strategies, such as self‐guided mediation, and writing down worries
Workplace‐based psychological support strategies, e.g. peer support networks, employee wellness programmes, and psychological first aid
Pharmacological interventions
Medication for depression, anxiety, sleep and/or other mental disorders
We will categorise included interventions using the headings and subgroups listed above, with the addition of new subgroups if necessary. We will include multifaceted interventions which comprise a combination of interventions or strategies, including, but not limited to, those listed above.
To address objective 1, within the review of effectiveness, we will include studies with any comparator intervention. We will categorise these as:
no intervention;
standard care;
placebo or attention control intervention;
other active intervention(s).
We anticipate that it is possible that "standard care" in some studies could be the same as "no intervention". We will note this, and combine these studies if it is clear that participants have received no intervention aimed at addressing mental health or resilience.
Types of outcome measures
Objective 1: review of effectiveness
As outlined in Description of the condition, there are a wide range of mental‐health related symptoms which someone may experience, and a range of impacts on the individual and their ability to function effectively within the work environment. The outcomes considered critical to this review include measures of general mental health, as these are anticipated to be of critical importance to the frontline health and social care professionals, and measures of resilience as this is a measure of the ability to cope with negative effects of stress or adversity, relates to dysfunction at work, and is considered of key importance to this review which is focused on the effects of anticipated high levels of stress in the workplace. Outcomes critical to this review therefore include:
General mental health ‐ Symptom Checklist 90 Revised (SCL‐90‐R), General Health Questionnaire (GHQ‐12 or GHQ‐28), Short Form‐36 questionnaire (SF‐36)
Resilience ‐ measured by: Wagnild and Young Resilience Scale, Connor‐Davidson Resilience Scale (CD‐RISC), Brief Resilience Scale, Baruth Protective Factors Inventory (BPFI), Resilience Scale for Adult (RSA), Brief Resilience Coping Scale (BRCS)
Additional important outcomes include the following.
(a) Psychological symptoms of anxiety, depression or stress:
Anxiety – Generalized Anxiety Disorder 7‐Item (GAD‐7), Self‐Rating Anxiety Scale (SAS), State‐Trait Anxiety Inventory, Spielberger Trait Anxiety Inventory, Kessler Psychological Distress Scale, Depression, Anxiety and Stress Scale – 21 Items (DASS‐21)
Depression – Patient Health Questionnaire‐9 (PHQ‐9), Beck Depression Inventory, Center for Epidemiologic Studies Depression Scale (CES‐D)
Stress – Parker and DeCotiis Scale (job‐related stress), SARS‐Related Stress Reactions Questionnaire, Perceived Stress Scale (PSS‐10)
(b) Burnout:
measured by: Oldenburg Burnout Inventory (OLBI), Maslach Burnout Inventory questionnaire (MBIQ)
(c) Effects on workplace staffing:
Absenteeism/presenteeism
Staff retention/turnover
(c) Mental health disorders caused by distressing events:
Post‐traumatic stress disorder (PTSD) – Stanford Acute Stress Reaction (SASR), Impact of Event Scale (IES, IES‐R), Davidson Trauma Scale, Vicarious Traumatization Questionnaire, PTSD Checklist‐Civilian Version (PCL‐C), Chinese Impact of Event Scale—Revised (CIES–R
(d) Harm, adverse events or unintended consequences arising from the interventions
We will note where studies report costs, referrals, for example to mental health team, or alcohol/substance use.
We will include other tools which assess these domains where those named specifically in the list above are not measured.
Measuring or reporting of outcomes within studies will not be used as a criteria for inclusion within the review.
We are interested in outcomes which are recorded at the end of the intervention period ('immediate' time point) and outcomes recorded at a 'follow‐up' time point. If possible, we will categorise follow‐up outcomes as short‐term (< 3 to 6 months), medium‐term (> 6 months to 12 months) and longer‐term (> 12 months) follow‐up.
Objective 2: qualitative evidence synthesis
To be included, qualitative studies have to report findings relating to barriers and facilitators to the implementation of interventions aimed at improving the resilience and mental health of frontline health and social care professionals. We define a barrier as any factor that may impede the delivery of an intervention. We define a facilitator as any factor that contributes to the implementation of an intervention (Bach‐Mortensen 2018).
Search methods for identification of studies
One search strategy will be used for searching for studies for a series of systematic reviews on this topic (New Reference), and for identifying studies relevant to each of the objectives addressed by this Cochrane Review.
Electronic searches
A comprehensive search strategy has been developed for MEDLINE by an information specialist (JDC) (Appendix 1), combining uncontrolled vocabulary terms and Medical Subject Heading (MeSH) for (a) resilience and mental health interventions AND (b) health and social care personnel AND (c) pandemics, epidemics and health outbreaks and has been peer‐reviewed in accordance with PRESS guidelines (McGowan 2016). The search will be adapted for each of the following major electronic databases.
Cochrane Database of Systematic Reviews (CDSR) and Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane Library
MEDLINE (Ovid)
Embase (Ovid)
Web of Science: Web of Science Indexes ((Science Citation Index Expanded (SCIEXPANDED), Social Sciences Citation Index (SSCI), Conference Proceedings Citation Index‐ Science (CPCI‐S), Conference Proceedings Citation Index‐ Social Science & Humanities (CPCI‐SSH)
PsycINFO (Ovid)
CINAHL (Cumulative Index to Nursing and Allied Health Literature) (EBSCO)
Global Index Medicus databases (www.globalindexmedicus.net/)
WHO Library Database (WHO IRIS) (Institutional repository for Information Sharing, apps.who.int/iris/)
-
COVID‐19 systematic search strategies and resources, including (Shokraneh 2020):
PubMed for Recent Published Literature on COVID‐19 (live strategy and results: tinyurl.com/uwbsvo2
medRxiv and bioRxiv search strategies for Unpublished Studies on COVID‐19: connect.medrxiv.org/relate/content/181
US National Institutes of Health Ongoing Trials Register (www.clinicaltrials.gov) on COVID‐19 (live strategy and results): tinyurl.com/t9vwzfo
Google Scholar for Published and Unpublished Literature on COVID‐19 (live strategy and results): tinyurl.com/spj6oox
Cochrane COVID‐19 Study Register: covid‐19.cochrane.org/
We will run the searches from year 2002 onwards, with no language restrictions.
Searching other resources
We will also conduct systematic supplementary searches to identify other potentially relevant studies including:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov) and World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/en);
targeted handsearches of key organisational websites (e.g. international governmental and non‐governmental (third sector) websites);
Google scholar (first 250 relevant entries).
Where our searching identifies relevant systematic reviews or qualitative evidence synthesis we will handsearch the list of included studies. Due to the rapid nature of this review, we will not conduct additional handsearching. This includes handsearching of reference lists of included studies and forward citation searching. These should be considered for future updates of this review.
Selection of studies
One review author will run the targeted searches and will exclude any obviously irrelevant titles and abstracts. Pairs of review authors will independently apply selection criteria to abstracts; this stage will be managed in Covidence. Pairs of review authors will independently apply the selection criteria to the full papers, and 'tag’ included studies as relevant to objectives 1 and 2. Disagreements between review authors will be resolved through discussion, involving a third review author.
We will restrict the publication date from 2002 onwards.
Objective 1: review of effectiveness
We will not impose any restrictions according to language. Where titles and abstracts are in languages other than English, we will use Google‐Translate to enable screening. If studies published in languages other than English are considered at the full‐paper stage, or are included, we will involve a review author, advisory group member, or seek a volunteer with appropriate language skills. The review authors and advisory group are fluent in a wide range of languages (including Arabic, Bengali, French, German, Hindi, Italian, Marathi, Portuguese, Spanish). If necessary, selection criteria will be applied by one review author, with a second review author checking the translated text of included studies.
Objective 2: qualitative evidence synthesis
We will limit studies included in the qualitative evidence synthesis to those published in English, due to the the potential problems associated with translations of concepts across different languages, and the rapid nature of this planned synthesis and need for additional resources if studies in languages other than those that the review author team are proficient in are to be included in qualitative synthesis (Downe 2019). We will place studies in languages other than English, which otherwise meet the criteria for inclusion in the qualitative evidence synthesis, in 'studies awaiting assessment', and consider them for inclusion in future updates of this review.
Ongoing, unpublished and preprint papers
For any studies meeting the eligibility criteria, but which are still ongoing, or for which no results data are yet available, we will list as an "ongoing" study. We will treat reports of studies that are available as unpublished studies or preprint publications (not yet peer‐reviewed) as included studies, but we will note the publication status and explore the effect of inclusion using sensitivity analysis.
Reporting of search results
We will report search results using PRISMA (Moher 2009).
Where there is a potentially relevant abstract, but we are unable to find a full paper, we will list this in the 'Characteristics of studies awaiting classification' tables. Where there is a relevant abstract for which there is no full paper, for example a conference abstract, we will include this study and attempt to contact study authors to obtain further data.
We will list any studies excluded at the full paper stage in the 'Characteristics of excluded studies' tables, with reasons for exclusion given.
Data extraction and management
We will bring together multiple reports of the same study, and at data extraction we will consider all publications related to that study. Where there is conflicting information between different reports of the same study we will identify this, but will base our extraction on the designated "main" publication. Where there is a protocol and also report of a completed study, we will designate the report of the completed study as the "main" publication, referring to both for data extraction but using the main publication if there is conflicting information relating to a study.
Objective 1: review of effectiveness
One review author will systematically extract data from all papers using a pre‐developed data extraction form, within Microsoft Excel. We will pilot the extraction form on at least five studies prior to use. All data extraction will be cross checked by a second review author, and any disagreements resolved through discussion, involving a third review author if necessary.
We will extract and categorise data on the following items.
Year
Study design
Aim
Inclusion criteria
Geographical setting (countries)
Epidemic/pandemic ‐ disease, phase of disease outbreak (during outbreak/de‐escalation)
Setting (hospital, care home, community, etc.)
Participant characteristics – number of participants/dropouts, demographic variables of included participants, type (profession) of staff. We will categorise participant populations using the list above (see Types of participants), with additional categories if required. We will note when participants are people who: returned to practice or were students who entered a professional role early
Intervention characteristics – described using TIDieR framework (Hoffmann 2014). We will categorise interventions according to whether the intervention involves changes at the level of individual staff members, groups of staff members (e.g. teams), an organisation (e.g. at the hospital level), or policy (e.g. NHS or government policy)
Comparator characteristics
Assessed outcomes
Baseline and follow‐up results data (mean and standard deviation, or other summary statistics as appropriate) for relevant outcomes. We will extract data for an 'immediate' time point – recorded at the end of the intervention period; and for a 'follow‐up' time point. Where multiple follow‐up time points are available, we will extract data which reflect the following time points: short‐term (< 3 months to 6 months), medium‐term (> 6 to 12 months) and longer‐term (> 12 months).
Analysis: presented analysis/ses
For non‐randomised studies we will extract data on intervention effects, levels of precision and confounders adjusted for. We will document whether the following potentially confounding factors were controlled for: setting that the healthcare professional is working in, the type and grade of health professional, and the length of time that the individual has worked within the disease epidemic/pandemic, gender and socioeconomic status.
Objective 2: qualitative evidence synthesis
One review author will systematically extract data from all papers using a pre‐developed data extraction form, within Microsoft Excel. This will be cross checked by a second review author, and any disagreements resolved through discussion, involving a third review author, if necessary.
We will extract and categorise data on the following items.
Year
Study design
Aim
Geographical setting (countries)
Epidemic/pandemic ‐ disease, phase of disease outbreak (during outbreak/de‐escalation)
Type (profession) of staff and length of time in the profession
Whether staff have previous experience of working in the frontline during an epidemic/pandemic
Details of who the frontline staff were providing care for
Type of interventions implemented
Study fidelity with a specific focus on whether the interventions were tailored and/or modified in different contexts
Details of any adverse events/unintended consequences
Sampling of studies
Qualitative evidence synthesis aims for variation in concepts rather than an exhaustive sample, and large amounts of study data can impair the quality of the analysis. Once we have identified all studies that are eligible for inclusion, we will assess whether their number or data richness is likely to represent a problem for the analysis, and will consider selecting a sample of studies (EPOC 2017b).
We will use a similar sampling approach to that used by Houghton 2020, based on a 3‐step sampling frame (Ames 2017), in order to reach agreement on a final sample of studies:
we will include studies that cover a range of epidemic/pandemic diseases, including those focused on coronaviruses (i.e. MERS, SARS, COVID‐19) and those with alternative modes of disease transmission;
we will assess the data richness of the remaining studies, using the EPOC 2017b purposeful sampling frame (see Table 12);
we will consider the spread of frontline health and social care professionals and the types of interventions studied.
10. Purposeful sampling frame based on the richness of the data in the included studies.
| Measurea | Example | |
| 1 | Very little qualitative data presented that relate to the synthesis objective. Those findings that are presented are fairly descriptive. | For example, a mixed‐methods study using open‐ended survey questions or a more detailed qualitative study where only part of the data relate to the synthesis objective |
| 2 | Some qualitative data presented that relate to the synthesis objective | For example, a limited number of qualitative findings from a mixed‐methods or qualitative study |
| 3 | A reasonable amount of qualitative data that relate to the synthesis objective | For example, a typical qualitative research article in a health services journal |
| 4 | A good amount and depth of qualitative data that relate to the synthesis objective | For example, a qualitative research article in a social sciences journal with more context and setting descriptions |
| 5 | A large amount and depth of qualitative data that relate in depth to the synthesis objective | For example, from a detailed ethnography or a published qualitative article with the same objectives as the synthesis |
aFrom EPOC 2017b.
Qualitative data management
We will extract data identified as a barrier or facilitator to the implementation of interventions (author, year, country, direct quotes, page numbers) verbatim and coded by one review author (PC or JC), and independently checked by a second review author (BD). Any ambiguity identified will be resolved through discussion with other members of the review team.
We will use the best fit framework synthesis approach, which combines deductive and inductive thematic approaches to identifying barriers and facilitators (Carroll 2011). The first step will involve a deductive approach, employing a predefined list of 39 constructs, grouped into five domains, from the Consolidated Framework for Implementation Research guide (CFIR 2020) (see Table 4). We will code data against this framework. The second step will involve an inductive approach to develop themes and subthemes from data that cannot be categorised using the predefined codes.
Assessment of risk of bias in included studies
Objective 1: review of effectiveness
We will use:
Cochrane ROB tool for randomised trials (RoB 1) (Higgins 2017)
ROBINS‐I tool for non‐randomised studies of interventions (Sterne 2016). We will follow the guidance in Chapter 25 of the CochraneHandbook for Systematic Reviews of Interventions, and in section 25.5 for assessing the risk of bias in interrupted time series studies (Sterne 2020).
Assessments will be completed by one review author, and checked by a second review author. Any disagreements will be resolved through discussion, involving a third review author if necessary.
Assessment of methodological limitations
Objective 2: qualitative evidence synthesis
We will use tools appropriate to the design of the study, i.e.:
the Critical Appraisal Skills Programme for qualitative studies (CASP 2018)
Mixed Methods Appraisal Tool for mixed method studies (Pluye 2009)
SQUIRE 2.0 (Standards for Quality Improvement Reporting Excellence) checklist (SQUIRE 2018) for appraising quality of quality improvement studies
Assessments will be carried out independently by two review authors. Any disagreements will be resolved through discussion, involving a third review author if necessary.
Measures of treatment effect
Objective 1: review of effectiveness
We will carry out meta‐analyses of pairwise comparisons for outcomes where direct evidence is available. We will estimate pooled effect sizes (with 95% confidence intervals) using data from individual arms of included trials. We will estimate risk ratios for binary outcomes and mean differences for continuous outcomes (or standardised mean differences if different measures of the same outcomes have been used in different trials). We will meta‐analyse complex trial designs (multi‐arm, cluster and crossover) following established guidance (Higgins 2020a).
We will conduct the synthesis of non‐randomised studies according to the guidance in Chapter 24 of the CochraneHandbook for Systematic Reviews of Interventions (Reeves 2020). Where possible, we will meta‐analyse effect sizes. We will meta‐analyse randomised and non‐randomised studies separately.
For outcomes relating to effects on workplace staffing, we will only conduct meta‐analysis where we can analyse this as dichotomous data. For example, using data for the proportion of participants who have a period of absenteeism during the intervention period, those who are absent at the end of the intervention period, and/or those who have a period of absenteeism before stated follow‐up assessment points. If time‐to‐event data are presented (e.g. for absenteeism) we will only include these if we can convert these and analyse as dichotomous data. If count data are presented (e.g. number of periods of absenteeism) we will not include these unless we can determine the number of participants whom these data relate to (e.g. the number of participants who had at least one period of absenteeism).
Unit of analysis issues
For the quantitative evidence synthesis: where studies have two or more active intervention groups eligible for inclusion within the same comparison (against a control, placebo, or no treatment group), we intend to 'share' the control group data between the multiple pair‐wise comparisons in order to avoid double counting of participants within an analysis. Where we include studies which have used a cluster‐randomised design, we will treat the group (or cluster) as the unit of allocation, and follow methods for analysis of cluster‐randomised trials as described in the CochraneHandbook for Systematic Reviews of Interventions (Higgins 2020a), with advice from a statistician (AE).
Dealing with missing data
For the quantitative evidence synthesis: where studies appear to have measured outcome data that are relevant to our critical outcomes of general mental health and resilience, but these are missing from identified reports, we will contact study authors by email. This will include requests where the study report does not provide means or standard deviations (or data from which these can be calculated by the review authors). Where we do not obtain the missing data, or where there are missing data relating to other outcomes, we will highlight this within our narrative synthesis. We will only analyse available data and do not plan to input missing data with replacement values.
For the qualitative evidence synthesis: where studies appear to have missing data we will note this, but will not contact study authors due to the rapid nature of this review.
Assessment of heterogeneity
Within the quantitative evidence synthesis: we will assess heterogeneity by visually inspecting Forest plots and assessing I2 statistics, with random‐effects models used to address potential heterogeneity. We will consider an I² value of more than 50% to indicate substantial heterogeneity.
Assessment of reporting biases
As this is a rapid review, we will not use any formal methods to assess the risk of reporting biases.
Data synthesis
Objective 1: review of effectiveness
We plan to conduct pairwise meta‐analysis for all primary and secondary outcomes listed above (Review Manager 2020), for comparisons of:
intervention versus no intervention
intervention versus standard care
intervention versus placebo or attention control
and for outcome measures:
immediately after the end of intervention
at follow‐up. If data are available, we will present data for short‐term (< 3 months to 6 months), medium‐term (> 6 months to 12 months) and longer‐term (> 12 months) follow‐up.
We do not plan to conduct any meta‐analyses for comparisons of one active intervention with another intervention.
We will summarise and tabulate important clinical and methodological characteristics of all included studies (including randomised and non‐randomised studies). Where study results have been pooled within meta‐analysis, we will judge our confidence in each pooled outcome using the GRADE approach. We will create 'Summaries of findings' tables for comparisons of: (1) intervention versus no intervention; (2) Intervention versus standard care; and (3) intervention versus placebo or attention control. These 'Summaries of findings' tables will include results relating to the following outcomes.
General mental health
Resilience
Anxiety
Depression
Stress
Burnout
Absenteeism
The 'Summaries of findings' tables will include results measured immediately at the end of the intervention and at 1‐year follow‐up (if data are available).
We will structure our main narrative summary of findings first by the intervention, using the predefined broad intervention headings listed under 'Types of interventions', and second by comparison group, and third by outcome. Within the narrative we will refer to the study participants, and to areas of similarity and/or differences (clinical heterogeneity) between the studies. Where there are studies which are relevant to a particular comparison and outcome, but for which there are no data suitable for inclusion in meta‐analysis, we will provide a brief table summarising results reported by the study, and refer to this tabulated data within a narrative synthesis. We will comment on whether there are agreements or disagreements between our meta‐analysis and studies not included in meta‐analysis, with reference to the risk of bias of studies.
For outcomes not included in the 'Summaries of findings' tables, we will provide a brief narrative synthesis of key findings. We will also provide a brief narrative synthesis of key findings of studies which have comparisons of one active intervention with another active intervention. We will follow the Synthesis Without Meta‐analysis (SWiM) in systematic reviews reporting guideline (Campbell 2020).
Objective 2: qualitative evidence synthesis
We will bring together evidence relating to barriers and facilitators using a narrative synthesis supported by Strength of Qualitative Findings (SoQF) tables and figures organised around the five major domains that may influence an intervention’s implementation, as reported in the Consolidated Framework of Implementation Research (CFIR 2020). This may include factors related to:
intervention characteristics;
inner settings (i.e. organisational factors);
outer settings (i.e. environmental factors);
individual characteristics;
implementation process characteristics.
Two review authors will use the GRADE‐CERQual approach to assess our confidence in each finding (Lewin 2018).
CERQual assesses confidence in the evidence, based on the following four key components.
Methodological limitations of included studies: the extent to which there are concerns about the design or conduct of the primary studies that contributed evidence to an individual review finding.
Coherence of the review finding: an assessment of how clear and cogent the fit is between the data from the primary studies and a review finding that synthesises those data. By cogent, we mean well supported or compelling.
Adequacy of the data contributing to a review finding: an overall determination of the degree of richness and quantity of data supporting a review finding.
Relevance of the included studies to the review question: the extent to which the body of evidence from the primary studies supporting a review finding is applicable to the context (perspective or population, phenomenon of interest, setting) specified in the review question.
After assessing each of the four components, we will make a judgement about the overall confidence in the evidence supporting the review finding. We will judge confidence as high, moderate, low, or very low. The final assessment will be based on consensus among the review authors. All findings start as high confidence and will then be graded down if there are important concerns regarding any of the CERQual components.
Overarching synthesis
We will produce a brief narrative synthesis which brings the findings from the quantitative and qualitative syntheses together. The aim of this integrated synthesis will be to explore why interventions to support mental health and resilience of frontline health and social care professionals may, or may not, be effective, and to inform future decisions about how to design and implement effective interventions. We will integrate the findings from the quantitative and qualitative evidence syntheses within a matrix. This will comprise a table which lists each type of intervention explored, a brief summary of evidence of effectiveness, and any potential barriers or facilitators to implementation of that intervention which were identified, and our confidence in this evidence.
Subgroup analysis and investigation of heterogeneity
Within the quantitative evidence synthesis we will explore differences between subgroups based on:
type of intervention (including whether intervention is targeted at: individual/group/organisation/policy);
duration of intervention delivery (one‐off, < 3 months, 3 to 6 months, > 6 months);
disease (type of disease and specific epidemic/pandemic, and mode of disease transmission (direct/indirect));
geographical location (countries);
type of staff (profession).
Sensitivity analysis
Objective 1: review of effectiveness
For all analyses, we will explore the effect on results of excluding non‐randomised studies. In addition, for analyses of our primary outcomes, we will explore the effect on results if only evidence from studies judged to be at low risk of bias (on all assessed domains) is included within the analyses.
Objective 2: qualitative evidence synthesis
For the sample of studies that are selected, we will consider how each study's methodological limitations may affect our review findings (Noyes 2020).
Review team reflexivity
The author team were assembled quickly to respond to a call from the Scottish Government for proposals for rapid research studies which had the potential to inform the government's response to the COVID‐19 crisis. The author team were all experienced in systematic reviews, with expertise in a range of different types of reviews, including Cochrane quantitative reviews and qualitative evidence syntheses. Members of the author team had research expertise relating to mental health, and represented a wide range of healthcare professionals (with the majority of the author team being based at the Scottish government‐funded 'Nursing, Midwifery and Allied Health Professions Research Unit').
A wider advisory group was also quickly assembled. This group comprised people who proactively contacted the lead review author to offer support to the review (either after seeing the registered title for a Cochrane rapid review, or seeing Scottish Government funding announcement), and members recruited though the Cochrane Consumers Covid‐19 rapid review panel. This group represents diverse professional and geographical backgrounds, including frontline healthcare professionals within the Covid‐19 pandemic and earlier epidemics (e.g. Ebola).
All members of the team have an interest in synthesising the evidence in relation to the impact of COVID‐19 on the mental health and well‐being on health and social care professionals, in order to urgently identify optimal ways of supporting frontline workers who are working in highly stressful circumstances.
Contributions of authors
AP and PC have developed the review questions, and written drafts of this protocol. AP will lead the quantitative evidence synthesis. PC will lead the qualitative evidence synthesis.
JDC has written the search strategy. JDC will run the search, and contribute to screening of studies.
JC, BD, KM, AE, SH, DM, JM and MM have all read and commented on drafts of this protocol. JC, BD, and KM will contribute to study selection and data extraction. AE and SH will provide statistical expertise and support. DM, JM and MM will provide content expertise relating to health and social care workers and mental health and well‐being.
Acknowledgements
This systematic review is supported by an Advisory Group. The following Advisory Group members have read and provided comments on drafts of this protocol (listed alphabetically):
Ms Laura Boeira, Veredas Institute, Brazil
Dr Andrew Booth, University of Sheffield, UK
Mr James Chan, Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences, University of Oxford; Stoke Mandeville Hospital, Buckinghamshire Healthcare NHS Trust
Dr Mark Delicata, Victoria Hospital, Kirkcaldy, NHS Fife, UK
Dr David Gillespie, Royal Infirmary Edinburgh, NHS Lothian, UK
Dr Sohil Khan, Griffith University, Australia
Dr Terry Quinn, Institute of Cardiovascular and Medical Sciences, University of Glasgow, UK
Prof A.G. Radhika, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India
Prof Valéry Ridde, French Institute for Research on Sustainable Development, Paris
Dr Lesley Robertson, University of the Witwatersrand, Johannesburg, South Africa
Dr Abi Sriharan, Dalla Lana School of Public Health, University of Toronto
Prof Balendra Pratap Singh, King George’s Medical University, India
Dr Ali Zamlout, Tishreen University, Latakia, Syria
Text from the 'EPOC Qualitative Evidence synthesis: protocol and review template’ has been used within this protocol (EPOC 2019).
Declarations of interest
Alex Pollock: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. Employed within a post at the NMAHP Research Unit which is supported by the Chief Scientist Office, Scottish Government. No other known conflict of interest.
Pauline Campbell: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. No other known conflict of interest.
Joshua Cheyne: no known conflict of interest.
Julie Cowie: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. No other known conflict of interest.
Bridget Davis: no known conflict of interest.
Kris McGill: no known conflict of interest.
Andrew Elders: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. No other known conflict of interest.
Suzanne Hagen: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. Employed within a post at the NMAHP Research Unit which is supported by the Chief Scientist Office, Scottish Government. No other known conflict of interest.
Jacqueline McCallum: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. No other known conflict of interest.
Doreen McClurg: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. Employed within a post at the NMAHP Research Unit which is supported by the Chief Scientist Office, Scottish Government. No other known conflict of interest.
Margaret Maxwell: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. Employed within a post at the NMAHP Research Unit which is supported by the Chief Scientist Office, Scottish Government. No other known conflict of interest.
Internal sources
No sources of support supplied
External sources
Scottish Government's Chief Scientist Office (CSO), UKGrant funding. CSO ID: COV/GCU/Portfo
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Belfroid 2018.
| Study characteristics | ||
| Methods |
Design: qualitative study using semi‐structured in‐depth interviews (25‐60 min) Country: The Netherlands Study aim: to gain insight into how healthcare organisations can prepare to meet the needs of their HCWs by capturing the experiences of HCWs with patients with suspected EVD Study recruitment details: invited HCWs who cared for/or transported patients with suspected EVD to take part Setting: regional ambulance services and 5 university hospitals appointed to deal with the admission of patients with suspected EVD Epidemic/pandemic disease: EVD Phase of disease outbreak: after the pandemic |
|
| Participants |
Total study population: 23
Inclusion criteria: HCWs who had cared for a patient with suspected EVD or were part of the team that had prepared for admission of such patients in several university hospitals. Also invited HCWs from regional ambulance services who had transported a patient with suspected EVD.
Exclusion criteria: none reported
Type (profession) of staff: nurses (n = 13), physicians (n = 6), manager (logistics) (n = 1), ambulance nurses (n = 3) Length of time in the profession: 4‐38 years' experience in their current profession Previous experience of working in the frontline during an epidemic/pandemic: not reported Details of who the frontline staff were providing care for: 99 patients assessed for risk of EVD, 14 of whom were admitted in strict isolation. All tests proved negative for EVD. |
|
| Interventions |
1. Multicomponent training and feedback (n = 23)
|
|
| Outcomes |
Outcomes: experiences were categorised into three themes, which were experiences related to
Data collection: interviews with HCWs in the Netherlands dealing with patients with suspected EVD during the 2014‐2015 EVD outbreak. These interviews took place from May to October in 2016. |
|
| Funding | Funding statement: work was carried out with financial support from the Dutch Ministry of Health, Welfare and Sport Conflict of interest: none declared | |
| Notes | Included in the review of qualitative evidence synthesis. Classified as a 'qualitative study', as this has a qualitative study design. Methodological assessment: assessed using CASP tool Overall assessment: no or few limitations. For details of assessment see Table 9, and for support for judgements see Appendix 13. |
|
Blake 2020.
| Study characteristics | ||
| Methods |
Design: describes the development and evaluation of a digital intervention Country: UK Study aim: 4 aims to
Study recruitment details: 3‐step development process using Agile methodology that involved public involvement at each stage. Combination of approaches used to recruit individuals (HCWs and students) to input at various stages of the project (see Steps 1‐3 below) including self‐identified through the professional networks of the project team and email Setting: university Epidemic/pandemic disease: COVID‐19 Phase of disease outbreak: during the outbreak |
|
| Participants |
Total study population: different at different stages of development (see steps 1‐3 below). 55 completed evaluation
Inclusion criteria: all UK healthcare employees
Exclusion criteria: not reported
Type (profession) of staff: the intervention is aimed at all UK healthcare employees. HCWs were involved in all stages of development
Length of time in the profession: not reported Previous experience of working in the frontline during an epidemic/pandemic: not reported Details of who the frontline staff were providing care for: not reported |
|
| Interventions |
1. Intervention: E‐package ‐ digital learning package (n = 55)
|
|
| Outcomes |
Outcomes: intervention was evaluated using a series of assessments
Data collection: data were collected 1 week after package release |
|
| Funding | Funding statement: no external funding Conflict of interest: study authors declared no conflicts | |
| Notes | Included in the review of qualitative evidence synthesis. Classified as a 'descriptive study', as this study describes the development, implementation and evaluation of an intervention. Methodological assessment: assessed using WEIRD tool Overall assessment: no or few limitations. For details of assessment see Table 10, and for support for judgements see Appendix 14. |
|
Brown‐Johnson 2020.
| Study characteristics | ||
| Methods |
Design: quality improvement study describes barriers and facilitators to the implementation of PPE portraits over a 2‐day pilot Country: USA Study aim: to see if PPE portraits (disposable portrait picture stickers ‐ 4" × 5" (approx 10 cm x 12.5 cm) can improve ("humanise") patient care Study recruitment details: "collected initial qualitative data ...between March and April 2020" Setting: hospital Epidemic/pandemic disease: COVID‐19 Phase of disease outbreak: during the outbreak |
|
| Participants |
Total study population: not reported
Inclusion criteria: not reported
Exclusion criteria: not reported
Type (profession) of staff: physician, shift nurses, medical assistants Length of time in the profession: not reported Previous experience of working in the frontline during an epidemic/pandemic: not reported Details of who the frontline staff were providing care for: not reported |
|
| Interventions |
1. PPE portraits (n = not reported)
|
|
| Outcomes | Outcomes: evaluated HCW provider experience Data collection: not reported | |
| Funding | Funding statement: not reported Conflict of interest: study authors declared no conflicts | |
| Notes | Study authors report that this study is the pilot in preparation for "a larger evaluation of the effectiveness of PPE Portraits on patient and provider experience" Included in the review of qualitative evidence synthesis. Classified as a 'descriptive study', as this study describes the implementation and evaluation of an intervention. Methodological assessment: assessed using WEIRD tool Overall assessment: major limitations. For details of assessment see Table 10, and for support for judgements see Appendix 14. |
|
Cao 2020.
| Study characteristics | ||
| Methods |
Design: qualitative interviews and quantitative questionnaires Country: China Study aim: "to examine COVID‐19‐related stress and its immediate psychological impact among medical workers in the fever clinic, to help improve the management of the stress of medical workers and maintain their physiological‐psychological well‐being during the pandemic" Study recruitment details: a special 24‐h 'fever clinic' was set up within the ED of the Peking Union Medical College Hospital. "Doctors and nurses for this fever clinic were handpicked by the Emergency Department based on their experience and their adaptability and tenacity under pressure shown in their past works." These workers: "stay and work in the hospital continuously for 2‐3 weeks and then leave the fever clinic; they then quarantined and convalesced in a vocational resort for two weeks. During their rotation in the fever clinic, a separate apartment building with an individual dormitory in the hospital was offered to each of them" 105 medical workers were at the fever clinic during the period of the study; 102 agreed to participate. Setting: hospital Epidemic/pandemic disease: COVID‐19 Phase of disease outbreak: during the outbreak |
|
| Participants |
Total study population: 102 medical workers (37 from the 'first batch' and 69 from the 'second batch' of medical workers within the fever clinic)
Inclusion criteria: "All medical workers at fever clinic during that time period were eligible for the study"
Exclusion criteria: none stated
Type (profession) of staff: "40 (39.2%) doctors, 54 (52.9%) nurses, and 8 (7.8%) laboratory technicians handling specimens from patients." Length of time in the profession: "a median of 6 (3, 13) years of work experience" Previous experience of working in the frontline during an epidemic/ pandemic: not reported Details of who the frontline staff were providing care for: patients entered a fever clinic within an ED for triaging patients during the COVID‐19 outbreak |
|
| Interventions |
1. Psychological support (n = 102)
|
|
| Outcomes |
Outcomes:
Data collection: IES‐R and sources of distress were measured at the end of the period of duty "PHQ‐9 and MBI were administered at the end of their duty", for the first batch of workers only ("duty" was a period of 2‐3 weeks working on the fever clinic") |
|
| Funding | Funding statement: "J.C. and J.W. received funding support from PUMCH (pumch‐2016‐3.3 and ZC201902261, respectively)." "The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report." (PUMCH ‐ Peking Union Medical College Hospital). Conflict of interest: not reported | |
| Notes | It is unclear whether the "qualitative interview" from which results are reported formed part of the intervention (i.e. the interview took place as part of the 'hotline' service); or whether this occurred in addition to the hotline service. Included in the review of qualitative evidence synthesis. Classified as a 'qualitative study', as qualitative data from this mixed‐method study were used. Methodological assessment: assessed using CASP tool Overall assessment: minor limitations. For details of assessment see Table 9, and for support for judgements see Appendix 13. |
|
Carvalho 2019.
| Study characteristics | ||
| Methods |
Design: prospective before‐after (cohort) study ‐ relevant data are descriptive data within the discussion around the cohort study results Country: Spain Study aim: to assess the impact of multi‐professional simulation‐based training on the risk perception and preparedness of HCWs who care for patients assessed to be at risk or confirmed to have EVD (level 3–4 biohazard) Study recruitment details: course was offered to all ICU staff (registered nurses, nursing assistants and doctors) plus any staff who could be involved in their care (e.g. stretcher bearers and cleaning and security personnel) Setting: hospital clinic, which was designated to admit and treat EVD patients. As such hospital protocols for managing potential EVD patients were updated, and a multi‐professional simulation‐based course to train HCWs implemented Epidemic/pandemic disease: EBV Phase of disease outbreak: > 1 phase |
|
| Participants |
Total study population: 58
Inclusion criteria: ICU staff
Exclusion criteria: not reported
Type (profession) of staff: registered nurses (n = 22), cleaning staff (n = 11), nursing assistants (n = 9), security staff (n = 5) doctors (n = 4), 'stretcher bearer' (n = 1) Length of time in the profession: < 5 years (n = 5), 5‐9 years (n = 9), 10‐14 years (n = 10), 15‐19 years (n = 4), 20‐24 years (n = 11), > 25 years+ (n = 13) Previous experience of working in the frontline during an epidemic/pandemic: not reported although study authors report that 13/52 had experience with infected patients requiring high isolation Details of who the frontline staff were providing care for: potential EVD patients. No other details reported |
|
| Interventions |
1. Multiprofessional simulation training (n = 58)
|
|
| Outcomes | Outcomes: 2 self‐reported questionnaires: self‐assessment questionnaire and a satisfaction questionnaire Data collection: baseline and post‐intervention (2 weeks later) | |
| Funding | Funding statement: Capes Foundation Ministry of Education of Brazil for research fellowship Conflict of interest: not reported | |
| Notes | Included in the review of qualitative evidence synthesis. Classified as a 'descriptive study', as descriptive data were used from the report of this cohort study. Methodological assessment: assessed using WEIRD tool Overall assessment: minor limitations. For details of assessment see Table 10, and for support for judgements see Appendix 14. |
|
Chang 2006.
| Study characteristics | ||
| Methods |
Design: survey ‐ relevant data are descriptive data within the discussion around the quantitative survey results Country: Taiwan Study aim: examined whether two components of social capital (social interaction and trust) can enhance an individual’s ability in reducing emotional exhaustion and job tension when medical professionals encounter a crisis such as SARS. Study recruitment details: 400 surveys were sent to medical professionals across the 4 medical centres and staff were asked to respond anonymously Setting: 4 medical centres (hospitals), each had complete facilities, such as negative air pressure isolation wards, and specially trained staff working exclusively in taking care of SARS patients Epidemic/pandemic disease: SARS Phase of disease outbreak: during the outbreak |
|
| Participants |
Total study population: 244 questionnaires return but, only 211 questionnaires were usable
Inclusion criteria: not reported
Exclusion criteria: not reported
Type (profession) of staff: registered nurses (67%), resident doctors (33%) Length of time in the profession: not reported Previous experience of working in the frontline during an epidemic/pandemic: not reported Details of who the frontline staff were providing care for: SARS patients. Study authors report that 51% participants had some temporary contact with SARS patients; 16% cared for SARS patients, and 33% did not have contact with SARS patients |
|
| Interventions |
1. Social capital (social interaction and trust)
|
|
| Outcomes |
Outcomes: questionnaires were developed based on authors previous research. 7 statements were generated
Data collection: data were collected once |
|
| Funding | Funding statement: not reported Conflict of interest: not reported | |
| Notes | Included in the review of qualitative evidence synthesis. Classified as a 'descriptive study', as descriptive data were used from the report of this survey‐based study. Methodological assessment: assessed using WEIRD tool Overall assessment: major limitations. For details of assessment see Table 10, and for support for judgements see Appendix 14. |
|
Chen 2020.
| Study characteristics | ||
| Methods |
Design: interviews Country: China Study aim: to examine why "medical staff were reluctant to participate in the group or individual psychology interventions provided to them". Study recruitment details: no details provided Setting: hospital ("Second Xiangya Hospital — workplace of the chairman of the Psychological Rescue Branch of the Chinese Medical Rescue Association— and the Institute of Mental Health, the Medical Psychology Research Center of the Second Xiangya Hospital, and the Chinese Medical and Psychological Disease Clinical Medicine Research Center") Epidemic/pandemic disease: COVID‐19 Phase of disease outbreak: during the outbreak |
|
| Participants |
Total study population: 13
Inclusion criteria: not reported (medical staff who had refused/not participated in an offered psychological assistance intervention)
Exclusion criteria: not reported
Type (profession) of staff: "medical staff" Length of time in the profession: not reported Previous experience of working in the frontline during an epidemic/pandemic: not reported Details of who the frontline staff were providing care for: "The hospital has set up a 24‐h fever clinic, two mild suspected infection patient screening wards, and one severe suspected infection patient screening ward." |
|
| Interventions |
1. Psychological support intervention
|
|
| Outcomes | 30‐min interview survey ‐ no further details | |
| Funding | Funding statement: not reported Conflict of interest: "We declare no competing interests" | |
| Notes | Included in the review of qualitative evidence synthesis. Classified as a 'qualitative study', as this study had a qualitative study design. Methodological assessment: assessed using CASP tool Overall assessment: major limitations. For details of assessment see Table 9, and for support for judgements see Appendix 13. |
|
Cheung 2015.
| Study characteristics | ||
| Methods |
Design: case study (field report) Country: Liberia Study aim: to summarise some of the psychosocial issues in the field and to offer some suggestions for dealing with these issues Study recruitment details: study author was deployed as an International Federation of Red Cross and Red Crescent Societies psychosocial delegate to Liberia for the EVD outbreak in July and August 2014. Part of the role was to provide psychosocial support for HCWs. Setting: community Epidemic/pandemic disease: EVD Phase of disease outbreak: during the pandemic |
|
| Participants |
Total study population: not reported
Inclusion criteria: not reported
Exclusion criteria: not reported
Type (profession) of staff: "frontline local and overseas workers" Length of time in the profession: not reported Previous experience of working in the frontline during an epidemic/pandemic: not reported Details of who the frontline staff were providing care for: patients, families, members of the local and aid workers |
|
| Interventions |
1. Psychosocial support: (n = not reported)
|
|
| Outcomes | Outcomes: descriptions of fear among HCWs, stress, and stigmatisation Data collection: field report so data collection on‐going | |
| Funding | Funding statement: not reported Conflict of interest: not reported | |
| Notes | Included in the review of qualitative evidence synthesis. Classified as a 'descriptive study', as this was a commentary relating to an intervention. Methodological assessment: assessed using WEIRD tool Overall assessment: major limitations. For details of assessment see Table 10, and for support for judgements see Appendix 14. |
|
Cunningham 2017.
| Study characteristics | ||
| Methods |
Design: qualitative study (interviews) Country: Sierra Leone Study aim:
Study recruitment details: potential participants were invited to complete an online survey; 1 of the questions asked for consent for a subsequent interview. 63 people completed the survey, of whom 27 consented to be interviewed, and 20 were interviewed Setting: unclear Epidemic/pandemic disease: EVD Phase of disease outbreak: after the pandemic |
|
| Participants |
Total study population: 20 participants were interviewed; 19 interviews were analysed
Inclusion criteria: any healthcare provider who provided direct, hands‐on, care to patients or corpses infected with EVD; use of "narrative methods" while working with EVD patients
Exclusion criteria: none stated
Type (profession) of staff: expatriate humanitarian and HCWs (including volunteers) from USA and nurses and physicians from Canada. This included nurses, physicians and nurse practitioners. "Six nurses, nine physicians and five nurse practitioners were interviewed". Length of time in the profession: "The group represented a mean of 15.7 years of professional experience (nurses 15.7, doctors 19.3, and nurse practitioners 10.3 years experience). 74% of the interview respondents had at least 6 years of professional experience prior to their work with EVD patients. 1 provider interviewed skewed the mean time working for the EVD response because this provider had spent 1 year in the response as compared to most other providers who spent, on average, 42 days." Previous experience of working in the frontline during an epidemic/pandemic: "All but the least experienced providers (0‐5 years' experience, n = 2) had experience providing medical care in a humanitarian setting." Details of who the frontline staff were providing care for: patients and their families affected by EVD |
|
| Interventions | 1. Narrative medicine: (n = 20)
|
|
| Outcomes | Outcomes: ProQOL 5; interviews to explore use of narrative medicine Data collection: after return from deployment to Sierra Leone | |
| Funding | Funding statement: not reported Conflict of interest: not reported | |
| Notes | Included in the review of qualitative evidence synthesis. Classified as a 'qualitative study', as this study had a qualitative study design. Note: this qualitative study is presented within a PhD thesis. The thesis also includes an online survey (n = 58), which "aimed to assess the prevalence of compassion fatigue, compassion satisfaction and burnout among expatriate Ebola aid workers". A subgroup of the participants from the survey were interviewed (n = 20). In 1 of the thesis chapters the methods are described as a "mixed methods descriptive study incorporating quantitative and qualitative data." The part of the study relevant for inclusion in this Cochrane review is the qualitative study, and therefore data presented here relate only to this component. Methodological assessment: assessed using CASP tool Overall assessment: no or few limitations. For details of assessment see Table 9, and for support for judgements see Appendix 13. |
|
De Jong 2019.
| Study characteristics | ||
| Methods |
Design: mixed methods, including cluster‐randomised trial and qualitative interviews Country: Sierra Leone and Liberia Study aim: to systematically evaluate PFA Study recruitment details:
Setting: community Epidemic/pandemic disease: EVD virus disease Phase of disease outbreak: after the pandemic |
|
| Participants |
Total study population: for the qualitative study ‐ 73 participants (23 trainers, 36 providers and 14 key informants). For the randomised trial ‐ 408 participants
Inclusion criteria:
Exclusion criteria: not reported Type (profession) of staff:
Length of time in the profession:
Previous experience of working in the frontline during an epidemic/pandemic:
Details of who the frontline staff were providing care for: people directly affected by EVD |
|
| Interventions | 1. Training in delivery of psychological first aid: (n = 206)
2. Control group (no intervention): (n = 202) |
|
| Outcomes |
Qualitative study Semi‐structured interviews "explored how PFA training was delivered during the EVD crisis, whether fidelity to the original model was maintained, and the trainers’ reflections on the process of rolling out the training" Randomised trial Outcomes: self‐report questionnaires for
Data collection: baseline, "3 months post‐assessment" (timed to follow shortly after the PFA training for the PFA group), 6 months post‐assessment |
|
| Funding | Elrha’s Research for Health in Humanitarian Crises (R2HC) Programme (Grant number 21163). (The R2HC programme is funded by the UK Government (DFID), the Wellcome Trust, and the UK National Institute for Health Research (NHIR).) "Additional funding was obtained at the United States Agency for International Development (USAID) through the Advancing Partners & Communities project, implemented by JSI Research &Training Institute, Inc., in collaboration with FHI 360 under Cooperative Agreement No. AID‐OAA‐A‐12‐00047." |
|
| Notes | Included in the review of quantitative evidence ‐ randomised trial Included in the review of qualitative evidence synthesis ‐ classified as a 'qualitative study', as data were extracted from the qualitative component of this mixed‐method study. Methodological assessment
Overall assessment: no or few limitations. For details of assessment see Table 9, and for support for judgements see Appendix 13. |
|
Ferranti 2016.
| Study characteristics | ||
| Methods |
Design: development, implementation and evaluation (survey) of an intervention Country: USA Study aim: to describe the development, implementation, and evaluation of the EVD Just‐in‐Time Teaching (JiTT) educational program Study recruitment details: undergraduate student nurses enrolled in our pre licensure Bachelor of Science in nursing (BSN) program in Fall 2014 and Spring 2015. Setting: university, which is located "on the same campus as Emory University Hospital and is also adjacent to the Centers for Disease Control and Prevention (CDC). Both the CDC and Emory Healthcare are key partners for the clinical and public health education of our student nurses. The treatment of patients with EVD at Emory University Hospital, combined with our CDC colleagues’ response to the EVD epidemic in Africa and the status of Atlanta being a major international transportation hub, necessitated a swift response by key public health faculty and administration of the NHWSN [Nell Hodgson Woodruff School of Nursing] to educate our students and fellow faculty colleagues and staff members about EVD." Epidemic/pandemic disease: EVD Phase of disease outbreak: after the pandemic |
|
| Participants |
Total study population: 233
Inclusion criteria: all enrolled undergraduate students
Exclusion criteria: none
Type (profession) of staff: nursing students Length of time in the profession: not applicable Previous experience of working in the frontline during an epidemic/pandemic: not applicable Details of who the frontline staff were providing care for: not applicable |
|
| Interventions | 1. Just‐in‐Time Teaching: (n = 233)
|
|
| Outcomes | Outcomes: knowledge scores (13 EVD items) Data collection: baseline and two post‐tests (immediately after the training and 5 weeks later) | |
| Funding | Funding statement: not reported Conflict of interest: not reported | |
| Notes | Included in the review of qualitative evidence synthesis. Classified as a 'descriptive study', as this study described the development, implementation and evaluation of an intervention.
Description of implementation factors is based on empirical data. Methodological assessment: assessed using WEIRD tool Overall assessment: minor limitations. For details of assessment see Table 10, and for support for judgements see Appendix 14. |
|
Klomp 2020.
| Study characteristics | ||
| Methods |
Design: describes the CDC multiple approaches to safeguarding mental health of EVD responders, and the implementation of these interventions Country: West Africa Study aim: to report on the different approaches intended to protect and support the public health professionals fighting EVD Study recruitment details: not reported Setting: community Epidemic/pandemic disease: EVD Phase of disease outbreak: > 1 phase of the pandemic |
|
| Participants |
Total study population: unclear. Multiple interventions are described and one small study, which has approximately 100 participants but study authors report that since 2009, over 400 individuals have completed this unique resilience‐focused training.
Inclusion criteria: not reported
Exclusion criteria: not reported
Type (profession) of staff: not reported Length of time in the profession: not reported Previous experience of working in the frontline during an epidemic/pandemic: "Between November 19, 2014 and December 31, 2016, there were 3,770 deployments by CDC staff in response to the EVD outbreak in West Africa.... almost 500 of the total deployments were by repeat employers". Details of who the frontline staff were providing care for: patients with EVD |
|
| Interventions |
1. Multicomponent resilience training: (n = X)
|
|
| Outcomes | Outcomes: the pre‐deployment assessment battery comprised of CD‐RISC, K‐10 and PC‐PTSD; Participants taking part in DSRT were given a series of pre‐ and post‐training assessments: knowledge of resilience‐enhancing principles and processes; knowledge of basic disaster site safety principles and processes; sense of self‐efficacy as measured by a 10‐item General Self‐Efficacy scale; overview of course content and general effectiveness of the training via a standard training assessment form. Data collection: "Pre‐training assessments of their RESILIENCE knowledge, Deployment SAFETY knowledge, and perceived SELF EFFICACY were administered to DSRT course participants immediately before training began. At the conclusion of the training, the three assessments were administered to participants again" | |
| Funding | Funding statement: not reported Conflict of interest: study authors declared no conflicts | |
| Notes | Included in the review of qualitative evidence synthesis. Classified as a 'descriptive study', as this study described the implementation and evaluation of an intervention. Note: some quantitative data are presented. However this is pre‐ and post‐training measures (2 time points), so does not meet criteria for inclusion within quantitative evidence synthesis. Methodological assessment: assessed using WEIRD tool Overall assessment: major limitations. For details of assessment see Table 10, and for support for judgements see Appendix 14. |
|
Lee 2005.
| Study characteristics | ||
| Methods |
Design: qualitative study and a survey. Small groups of nurses (4‐6 per group) were interviewed using semi‐structured interviews at the end of the "mission". This was followed with a 72‐item SARS team questionnaire Country: Taiwan Study aim: to understand the needs and experiences of frontline female nurses in order to provide better psychiatric services Study recruitment details: not reported Setting: tertiary medical centre designated to provide care for SARS patients during the outbreak Epidemic/pandemic disease: SARS Phase of disease outbreak: during the pandemic |
|
| Participants |
Total study population: 26
Inclusion criteria: SARS team of nursing staff was organised and cared for SARS patients in the ED. Team selection was made by both the director of the nursing department and the head nurse of the ED based on the nurses’ clinical performance, physical conditions, adaptability, willingness and their family’s considerations.
Exclusion criteria: not reported
Type (profession) of staff: nurses Length of time in the profession: 5‐12 years (mean = 6.5, S.D. = 1.98) Previous experience of working in the frontline during an epidemic/pandemic: not reported Details of who the frontline staff were providing care for: SARS patients |
|
| Interventions |
1. Debriefing intervention: (n = 26)
|
|
| Outcomes |
Outcomes: 72‐item questionnaire, which assessed 6 areas
Data collection: retrospectively collected at the end of the "mission" |
|
| Funding | Funding statement: not reported Conflict of interest: not reported | |
| Notes | Included in the review of qualitative evidence synthesis. Classified as a 'qualitative study', as this study had a qualitative study design. Methodological assessment: assessed using CASP tool Overall assessment: minor limitations. For details of assessment see Table 9, and for support for judgements see Appendix 13. |
|
Schreiber 2019.
| Study characteristics | ||
| Methods |
Design: data from aggregated PsySTART‐R Triage encounters reported as part of a case study, and implementation of the intervention is described during the EVD response Country: USA and West Africa Study aim: to describe the pilot work using the self‐triage system component in Alameda County’s Urban Shield and the Philippines’ Typhoon Haiyan, and then reports a case example of the full 'Anticipate, Plan and Deter' (APD) model implementation in West Africa’s EVD epidemic Study recruitment details: 186 self‐triage encounters among 45 clinical staff included in the first 2 deployed groups responding to EVD in West Africa for a 2‐month period at the end of 2014, reflecting approximately 75% of the total deployed force Setting: "different sites" in West Africa Epidemic/pandemic disease: EVD Phase of disease outbreak: during the pandemic |
|
| Participants |
Total study population: 45
Inclusion criteria: not reported
Exclusion criteria: not reported
Type (profession) of staff: "clinical staff"/"Ebola medical providers from one U.S.‐based medical effort". Length of time in the profession: not reported Previous experience of working in the frontline during an epidemic/pandemic: not reported Details of who the frontline staff were providing care for: not reported |
|
| Interventions |
1. Anticipate, Plan and Deter Responder Risk and Resilience model (n = X)
|
|
| Outcomes | Outcomes: number of self‐triage encounters Data collection: collected every 24 operational cycles | |
| Funding | Funding statement: sponsored by the Office of the Secretary of Defense for Health Affairs Conflict of interest: not reported | |
| Notes | Included in the review of qualitative evidence synthesis. Classified as a 'descriptive study', as this study described the implementation of an intervention. Methodological assessment: assessed using WEIRD tool Overall assessment: minor limitations. For details of assessment see Table 10, and for support for judgements see Appendix 14. |
|
Son 2019.
| Study characteristics | ||
| Methods |
Design: qualitative study using content analysis Country: South Korea Study aim: to reflect actual experiences of hospital workers by using qualitative data collected in real time during the 2015 MERS outbreak in South Korea Study recruitment details: not reported Setting: local community hospital designated as a treatment centre for MERS patients Epidemic/pandemic disease: MERS‐CoV Phase of disease outbreak: during the outbreak |
|
| Participants |
Total study population: 156 hospital workers
Inclusion criteria: not reported
Exclusion criteria: not reported
Type (profession) of staff: not reported Length of time in the profession: not reported Previous experience of working in the frontline during an epidemic/pandemic: not reported Details of who the frontline staff were providing care for: 5 MERS patients |
|
| Interventions | 1. "Let It Out": (n = 156 short notes)
|
|
| Outcomes | Outcomes: expressions of emotions (i.e. anger, anxiety, fear, sadness, disgust, and shame/guilt) and stress. Event themes that triggered those emotions and stress were also identified in thematic analysis Data collection: notes were collected after each session | |
| Funding | Funding statement: supported by the Institute of Health and Environment and the National Research Foundation of Korea Grant funded by the Korean Government (No.21B20151213037) Conflict of interest: not reported | |
| Notes | Included in the review of qualitative evidence synthesis. Classified as a 'qualitative study', as this study had a qualitative study design. Methodological assessment: assessed using CASP tool Overall assessment: minor limitations. For details of assessment see Table 9, and for support for judgements see Appendix 13. |
|
Waterman 2018.
| Study characteristics | ||
| Methods |
Design: implementation and evaluation of intervention. Qualitative interviews with intervention providers Country: Sierra Leone Study aims:
Study recruitment details: study comprised 3 phases of intervention. Participants completing 1 phase were screened and, if appropriate, referred to the next phase. In addition a number of new participants entered the study direct into Phase 2. In addition, 9 people involved in delivery of the group CBT were recruited for an interview to explore barriers and enablers. Setting: ETCs set up across Sierra Leone and staffed by a combination of national and international HCWs Epidemic/pandemic disease: EVD Phase of disease outbreak: during the outbreak |
|
| Participants |
Total study population: people trained to facilitate group CBT: 12 (9 were interviewed). Phase 1: 3273 invited to attend. 1533 attended. Phase 2: 1170 referred from phase 1 + 1720 joined at this point. Total participants attending sessions = 2533. Phase 3: 523 screened, 298 referred, 253 attended intervention, 157 completing post‐intervention assessment.
Inclusion criteria: ETC staff member from 1 of the 6 ETCs within Sierra Leone
Exclusion criteria: none stated
Type (profession) of staff: not reported for Phase 1 or 2. For Phase 3 ‐ "136 were unemployed (53.80%), 80 were employed (31.60%) and 32 (12.60%) were students." Profession not stated Length of time in the profession: not reported Previous experience of working in the frontline during an epidemic/pandemic: not reported Details of who the frontline staff were providing care for: patients attending ETCs. There were 6 ETCs ‐ 5 were 100‐bed facilities and 1 had 62 beds |
|
| Interventions | 1. Name of intervention: (Phase 1, n = 1533; Phase 2, n = 2533; Phase 3, n = 157 completers; attended all 3 phases, n = 75)
|
|
| Outcomes |
Outcomes: 7‐item well‐being screening tool concerning stress, sleep, anxiety, depression, relationship difficulties, behavioural changes and PTSD
Data collection: 7‐item well‐being screening tool was assessed before Phase 1 Other outcomes were measured at the start of Phase 2, at the start of Phase 3, and 2 weeks after completion of Phase 3. "Participants who had been the most symptomatic at Phase 1 were re‐screened using GAD7 and PHQ9 2 months after the completion of Phase 2". In addition there was data from 9 interviews (45‐60 min long). |
|
| Funding | Funding statement: financial support was received from the UK Public Health Rapid Support Team, funded by the UK Government, the UK Department for International Development and the Maudsley Charity. This report is independent research by the UK Public Health Rapid Support Team Conflict of interest: study authors report no conflict of interest | |
| Notes | Included in the review of qualitative evidence synthesis. Classified as a 'descriptive study', as descriptive data were used from this mixed‐method study. Methodological assessment: assessed using WEIRD tool Overall assessment: minor limitations. For details of assessment see Table 10, and for support for judgements see Appendix 14. |
|
AHP: allied health professional; CASP: Critical Appraisal Skills Programme; CBT: cognitive behavioural therapy; CDC: Centers for Disease Control and Prevention; CD‐RISC: Connor Davidson Resilience Scale; DSRT: Deployment Safety Resilience Team; ED: emergency department; ETC: Ebola treatment centres; EVD: Ebola virus disease; GAD‐7: General Anxiety Disorder‐7; HCW: healthcare worker; ICU: intensive care unit; IES(‐R): Impact of Event Scale (‐Revised); K‐10: Kessler Psychological Distress Scale (10‐item); MERS: Middle East respiratory syndrome; MBI: Maslach Burn‐out Inventory; PC‐PTSD: Primary Care Post‐traumatic Stress Disorder Screen; PFA: psychological first aid; PHQ‐9: Patient Health Questionnaire‐9; PPE: personal protective equipment; PPI: personal and public involvement; ProQOL 5: Professional Quality of Life scale; PTSD: post‐traumatic stress disorder; SARS: severe acute respiratory syndrome; SD: standard deviation; VRE: virtual reality environment; WEIRD: Ways of Evaluating Important and Relevant Data; WHO: World Health Organization
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Banerjee 2020 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| Barrett 2020 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| Barroso 2017 | Not relevant study design (secondary data analysis); focus on preparedness |
| Battista 2019 | No Intervention |
| Behan 2020 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| Bell 2017 | No intervention |
| Bergeron 2006 | No Intervention |
| Bohan 2020 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| Booth 2005 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| Chalk 2017 | No intervention |
| Chan 2004 | No intervention |
| Chan‐Yeung 2004 | No intervention |
| Chilton 2016 | No intervention |
| Chou 2010 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| Chung 2005 | No intervention |
| Corley 2010 | No intervention |
| Everly 2014 | Focused on preparedness |
| Fukuti 2020 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| Gershon 2016 | Focused on preparedness |
| Greenberg 2015 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| Liu 2020 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| Maltzman 2011 | Not specific to pandemic/epidemic |
| Marrs 2020 | Focused on preparedness |
| Maunder 2010 | Focused on preparedness |
| Meyer 2018 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| NCT04324190 | Not focused on health professionals |
| Shen 2020b | Not focused on mental health/resilience |
| Singh 2020 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| Soma 2020 | Not focused on mental health/resilience |
| Sprang 2015 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| Tam 2004 | No intervention |
| Taylor 2019 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| Vymetal 2011 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| Wald 2020 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| WHO 2014b | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| WHO 2015 | Not focused on HCWs mental health/resilience |
| WHO 2020b | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| WHO 2020d | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| WHO 2020e | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
| Xi 2019 | Not focused on health professionals |
| Yuen‐Tsang 2004 | Not relevant study design. The paper does briefly describe an intervention, which has been extracted and is summarised in Table 5. |
HCW: healthcare worker
Characteristics of studies awaiting classification [ordered by study ID]
Albott 2020.
| Methods | An overview paper. Describes psychological resilience intervention ‐ peer support model ("Battle buddies") for HCWs |
| Participants | Study population: HCWs |
| Interventions | 1. Rapidly deployable psychological resilience intervention founded on a peer support model (Battle Buddies) developed by the United States Army. 3 levels of support:
|
| Outcomes | Not specifically stated but focus is on resilience |
| Notes | Study authors refer to a project that "will stratify medical school departments affected by COVID‐19 between groups A (early‐start group) and B (delayed‐start group) based on administrative implementation of the intervention". They also provide a figure (see Figure 5) in the paper of a stratified‐start observational study of effects of a psychological resilience intervention for COVID‐19 HCWs |
Banerjee 2020a.
| Methods | Toolkit based on the model of the Zika virus preparedness toolkit (see Nair 2020) for use in COVID‐19 |
| Participants | Study population: no details |
| Interventions |
1. Community‐based toolkit for psychosocial management and preparedness. Multi‐component stepwise intervention
|
| Outcomes | Not reported |
| Notes | Further information should be sought from authors about the toolkit and who it is aimed at and whether there are any other published/unpublished data available |
Benzarti 2020.
| Methods | Qualitative study, Central Maghreb (Tunisia, Algeria, Morocco) |
| Participants |
Study population: 382 Inclusion criteria: health professionals in the Maghreb Central "regarding their experience of the first 6 weeks of fighting the COVID‐19 pandemic" Exclusion criteria: |
| Interventions | 1. National response plans ‐ details not fully reported. There is also mention of "assistant motivation programs" |
| Outcomes |
Outcomes: not reported Data collection: "first six weeks" |
| Notes | Translation required. Further details about the intervention will be sought from the translated paper. |
Brusin 2003.
| Methods | PhD thesis to "to develop a Post Disaster Assignment Recovery Manual" |
| Participants | Participant details not reported Inclusion criteria: mental health clinicians Exclusion criteria: not reported |
| Interventions | 1. Manual. Delivered over 8 days aims to provide disaster mental health clinicians with (a) tools for assessment of stress reactions; (b) an opportunity to develop and apply appropriate stress management and self‐care techniques to address stress reactions; and (c) an opportunity for the development of a narrative about their disaster mental health experience, which then might be integrated into their worldview. |
| Outcomes |
Outcomes: not reported Data collection: not reported |
| Notes | Abstract only. Contacted author to see whether we can obtain a copy of the PhD thesis, and need to clarify whether the manual is for in epidemic/pandemic scenario |
Casado‐Mejia 2016.
| Methods | Qualitative, interpretative and phenomenological study to " to understand the motivations and emotional experiences of this group and to identify the facilitators of and obstacles to its operation" |
| Participants |
Study population: 23 Inclusion criteria: key informants of the team members trained to deliver care during Ebola crisis Exclusion criteria: not reported |
| Interventions | 1. Not reported |
| Outcomes |
Outcomes: teamwork, motivations and emotions and elements affecting the team's operation Data collection: not reported |
| Notes | Translation required. Further details about the intervention will be sought from the translated paper. |
Cheng 2020.
| Methods | Describes the design of a short‐term social media, peer‐support project developed and carried out by a group of experienced mental health professionals, organised to offer peer psychological support from overseas to healthcare professionals on the frontline of COVID‐19, China |
| Participants | Study population: not applicable Inclusion criteria: HCWs from Wuhan Exclusion criteria: not reported |
| Interventions | 1. Social media peer support and crisis intervention (n = approximately 300)
|
| Outcomes | Outcomes: "did not collect formal outcome data.....but total number of the counseling group was stable at around 300 members throughout the whole course of the project" Data collection: not collected |
| Notes | Limited details about evaluation. Authors contacted for further information. |
ChiCTR‐TRC‐11001268.
| Methods | Parallel randomised trial; Hong Kong, China |
| Participants |
Study population: 900 Inclusion criteria: first responders, including fire fighters, police, ambulance officers, rescuers and auxiliary medical personnel with and without previous trauma exposure Exclusion criteria: individuals with psychiatric history or current diagnosis of psychiatric disorders will be screened out and referred for professional mental health services |
| Interventions |
1. Psychological first aid. A model widely used and adopted as a community‐based intervention for reducing post‐disaster psychological distress in a form of 7 h of training delivered in 1 day 2. Wait‐list control |
| Outcomes |
Primary outcomes: participants’ knowledge in disaster mental health, knowledge in PFA, self‐efficacy in delivering help in times of emergencies and actual helping behaviour Secondary outcomes: participants’ psychological well‐being, psychological distress and coping responses to stressful events and life satisfaction using a series of measurement tools including: GHQ‐28 (Chinese version), DASS‐21 (Chinese version), IES‐R, Brief COPE, Trauma History Questionnaire, MSPSS Data collection: baseline, 3‐ and 6‐month follow‐up |
| Notes | The trial is reported as completed, however we have only identified one published abstract. Further information sought from authors. |
Chung 2020.
| Methods | Unclear |
| Participants |
Study population: 69 Inclusion criteria: unclear (hospital staff) Exclusion criteria: not stated |
| Interventions | 1. Support of You (SOY) |
| Outcomes |
Outcomes: PHQ‐9 Data collection: via online questionnaire |
| Notes | This study may be ongoing. Study design is unclear. Further information from the authors is required. |
Cole 2020.
| Methods |
Design: description of an intervention, and intervention implementation Country: UK Study aim: to share our service design and pathway of care with other IAPT services who may also seek to support hospital frontline staff within their associated NHS Trusts and in doing so, lay the foundations of a co‐ordinated response Study recruitment details: not applicable Setting: hospital Epidemic/pandemic disease: COVID‐19 Phase of disease outbreak: during the outbreak |
| Participants |
Study population:
Inclusion criteria: ‘frontline workers’ across health and social care provisions of Homerton University Hospital Foundation Trust. This includes, but is not limited to, doctors, nurses, midwives, paramedics, social workers, care workers and volunteers. Support will also be offered to those who uphold the sector without a clinical input such as cleaners, administrators and security personnel.
Exclusion criteria: not reported
Type (profession) of staff: not applicable Length of time in the profession: not applicable Previous experience of working in the frontline during an epidemic/pandemic: not applicable Details of who the frontline staff were providing care for: not applicable |
| Interventions |
1. Homerton Covid Psychological Support’ (HCPS): (n = X)
|
| Outcomes | Outcomes: no data have been collected but a process evaluation study is planned to measure PHQ‐9, GAD‐7, WSAS and TSQ. Findings with regard to the pilot evaluation of the 20minCareSpace intervention offered during phase 2 will be included in the overall pilot evaluation being conducted by University College London (Scior 2020) Data collection: no data collected |
| Notes | Planned process evaluation study has been reported by authors; authors contacted for further information |
Fu 2004.
| Methods | Randomised trial |
| Participants | Study population: no details available |
| Interventions | 1. the effect of psychological behaviour training on mental health of the HCWs in SARS ward |
| Outcomes | No details available |
| Notes | No abstract available. Further information sought from authors |
Goh 2020.
| Methods | Short online survey (3 questions); Singapore |
| Participants |
Study population: 80 Inclusion criteria: "first 2 batches of front‐line HCWs who completed their 10‐day work cycle". Frontline HCWs included doctors, nurses and allied health professionals Exclusion criteria: not reported |
| Interventions | 1. Morale boosters (e.g. food and drink, appreciation from patients, general public and senior members of staff, medical subsidies) and initiatives such as GrabCare |
| Outcomes |
Outcome: changes in anxiety levels before and after starting work in the National Centre for Infectious Diseases Data collection: unclear |
| Notes | The study design is unclear and further information from authors is required. |
James 2020.
| Methods | Qualitative study |
| Participants | Study population: HCWs ‐ no other details reported |
| Interventions | 1. Limited details but study authors report the value of the "implementation of the CPES programme" |
| Outcomes |
Outcomes: barriers and facilitators to the delivery of healthcare during Ebola outbreak in West Africa Data collection: not reported |
| Notes | Abstract only. Full text not available at present. Further information sought from authors |
Jiang 2020.
| Methods | Description of a crisis intervention, China |
| Participants | Study population: medical workers, patients, and others affected to overcome any psychological difficulties |
| Interventions | 1. Based on the "Guidelines for the Psychological Assistance Hotline during the Prevention and Control of New Coronavirus Pneumonia''. Initiated via remote (telephone and internet) and on‐site medical services. |
| Outcomes |
Outcomes: describe some of the challenges and strategies following COVID‐19 outbreak Data collection: first few months following the start of the pandemic |
| Notes | Short communication with limited details about the intervention delivered and limited information about the evaluation of the intervention. Further details sought from authors. |
Keita 2017.
| Methods | Cross‐sectional and descriptive "to report the psychosocial experience of patients having recovered from Ebola virus infection and other persons affected by it psychologically in Conakry (Guinea), and to describe the psychological methods implemented for their care" |
| Participants | Study population: 68 patients who were affected psychologically were seen in the psychiatric department of Donka national hospital for psychological support on request from the NGO, Save the Children |
| Interventions | 1. Psychological debriefing, followed by supportive psychotherapy and CBT, with use of antidepressants in some cases, were the therapeutic means deployed. |
| Outcomes |
Outcomes: not reported Data collection: seen between May and August 2014 |
| Notes | Unclear whether any of the patients were HCWs, and if so, whether there are separate data available. Translation required. Further details about the intervention will be sought from the translated paper. |
Khee 2004.
| Methods | Qualitative study |
| Participants | Study population: healthcare providers |
| Interventions | 1. During the time of the study and in the midst of the outbreak, the psychology team developed a programme for mental health among healthcare providers. The programme consisted of group session therapy where a total of 16 groups were developed mainly comprised of nurses and physicians. |
| Outcomes |
Outcomes: not reported Data collection: unclear ‐ themes from therapy sessions are presented |
| Notes | Further details about the intervention and implementation are required as no information reported in the paper, only the "themes" from the analysis. Further information sought from authors. |
Li 2020.
| Methods | No details available, China |
| Participants | No details available |
| Interventions | 1. Traditional Chinese medicine specifically Sini Powder |
| Outcomes | No details available |
| Notes | No abstract available. Translation required. Further information sought from authors |
Liu 2015.
| Methods | No details available |
| Participants | Study population: no details available |
| Interventions | 1. Traditional Chinese medicine, baduanjing exercise on physical and mental condition of international medical team members fighting against Ebola virus |
| Outcomes | No details available |
| Notes | No abstract available. Translation required. Further information sought from authors |
Masumbuko 2020.
| Methods | Descriptive study, Democratic Republic of the Congo (DRC) |
| Participants |
Study population: medical students (n = 355) and community participants (n = 319) evaluated the campaign Inclusion criteria: outreach was conducted in November 2018, involving 600 students and reaching 5000‐10,000 community members Exclusion criteria: not reported |
| Interventions | 1. Student‐led educational campaign to increase community awareness and engagement in EVD control efforts, with evaluation of student and community satisfaction. Medical students were identified as "trusted local health agents" |
| Outcomes |
Outcomes: satisfaction scores Data collection: not reported |
| Notes | Abstract only. Full text not available at present. Authors contacted for further information about mental health outcomes |
Mehtar 2016.
| Methods | Not reported |
| Participants |
Study population: 215 HCWs Inclusion criteria: not reported Exclusion criteria: not reported |
| Interventions | 1. Educational intervention. A 1‐week, basic infection‐control course on containing Ebola was prepared. The course was structured to provide formal lectures but mainly to engage the students in problem solving, group discussion and peer‐presentations to assess their ability to teach others |
| Outcomes |
Outcomes: challenges, and non‐evidence based rituals Data collection: not reported |
| Notes | Limited details available. Not clear what was delivered on the course. It is not clear what the mental health outcomes are, although the authors note "challenges and "fear of the unknown". Further information about outcomes, intervention and study design is required. |
NCT04363671.
| Methods | Qualitative study based on interpretative phenomenological analysis to explore the experience of adolescents, doctors and psychologists regarding emergency changes in the methods of their follow‐up by setting up teleconsultation in the context of the COVID‐19 epidemic |
| Participants |
Study population: 30 (15 adolescents followed in consultation, day hospital or full hospitalisation and 15 health professionals) Inclusion criteria:
Exclusion criteria: none reported |
| Interventions | 1. Teleconsultation. Remote care using teleconsultation |
| Outcomes | Primary outcomes: to describe the experience of reorganisation of care during the COVID‐19 epidemic and acceptability of teleconsultation for the adolescents and the therapists by exploring the themes emerging from analysis of the content of the interviews |
| Notes | Trial registration: NCT04363671 Estimated completion date: December 2020 |
NCT04367857.
| Methods | Cohort |
| Participants |
Study population: 1000 Inclusion criteria: New York‐Presbyterian (NYP) healthcare personnel employee or affiliate aged 18+ years, able to understand and read English Exclusion criteria: participants aged < 18 years, mentally and/or physically unable to complete study requirements |
| Interventions |
1. Prior positive PCR and recovered. Prior positive PCR result, fully recovered, back at work and symptom‐free for ≥ 14 days 2. Never tested, history of COVID‐19 symptoms and recovered. Never tested and history of COVID‐19 symptoms and symptom‐free for > 14 days 3. Never tested and current COVID‐19 symptoms. Never tested and current COVID‐19 symptoms (e.g. referred by a provider or clinic) 4. Never tested and asymptomatic. Never tested and asymptomatic for COVID‐19 symptoms, including asymptomatic HCW |
| Outcomes |
Primary outcomes: percentage of HCWs with positive serological markers to describe patterns in exposure, re‐infection, clinical symptom, serological responses among HCWs based on their baseline serological status over a 1‐year period Data collection: baseline and at 12 months after initial collection visit |
| Notes | Trial registration: NCT04367857 Estimated completion date: October 2021 Not clear if there are mental health outcomes planned. Authors contacted for study protocol |
NCT04377165.
| Methods | Multicentre randomised trial, randomisation at the level of the Aged Care Facilities, Australia |
| Participants |
Study population: 9000 Inclusion criteria: age HCW, aged 18‐90 years Exclusion criteria: none reported |
| Interventions |
1. Gamification group. Participants will get the full 'gamified' app, including the newsfeed (i.e.) receives the app with the addition of a gamification competent, this will include rewarding experiences for staff doing safety behaviours and well‐being behaviours. The gamification function will allow users to earn points for actions completed. The gamification function has links to resources for infection control, watching or completing tasks or playing games to earn points. Points can be viewed at a facility level, state level or national level. 2. Newsfeed. Participants will get the app with newsfeed only (i.e.) participants will receive current and accurate information from an app. |
| Outcomes |
Primary outcomes: sick leave Secondary outcomes: handwashing behaviour (based on amount of soap/sanitiser), number of self‐tests, amount of disinfectant used, number of COVID‐19 infections, number of flu and gastroenteritis outbreaks, COVID‐19 awareness training, awareness of PPE training, levels of PPE material used, well‐being and self‐efficacy using a self‐reported survey Data collection: baseline and at 4 weeks post‐randomisation |
| Notes | Trial registration: NCT04377165 Recent note on the trial register that this trial has been terminated because of recruitment issues. Further information from authors sought |
NCT04379063.
| Methods | Observational (longitudinal survey) |
| Participants |
Study population: 10,000 Inclusion criteria: any physician who is currently practicing in Canada, whether they hold a full, provisional, or post‐graduate in‐training license Exclusion criteria: non‐physician healthcare providers, medical students, physicians without an active license to practice will be excluded |
| Interventions | Not reported |
| Outcomes |
Primary outcomes: MBI, HADS Secondary outcomes: PTSD checklist, PTGI‐SF Data collection: baseline and primary outcomes will be measured monthly until there is a month with no new cases; secondary outcomes will be measured monthly for the first 12 months. |
| Notes | Trial registration: NCT04379063 Estimated completion date: May 2022 Further information should be sought from the author to get more details on the study design |
NCT04379336.
| Methods | Parallel randomised trial; South Africa |
| Participants |
Study population: 500 Inclusion criteria: adults aged ≥ 18 years, HCW or other frontline staff currently in contact with, or anticipated to be in contact with, patients with SARS‐CoV‐2 infection, able and willing to provide informed consent, contactable by mobile for follow‐up Exclusion criteria: known allergy to (components of) the BCG vaccine or serious reaction to prior BCG administration, known active TB or any other active or uncontrolled condition that, in the opinion of the investigator or designee, makes participation unsafe or makes it difficult to collect follow‐up data over the study period, HIV‐1 infection, symptoms of respiratory tract infection which, in the opinion of the investigator or designee, is likely to interfere with the objectives of the study, medical history of any of the following immunocompromised states (neutropenia, lymphopenia, solid organ of bone marrow transplantation, active solid or non‐solid malignancy or lymphoma in the previous 2 years, pregnancy or breastfeeding) or current treatment with the following medicines (chemotherapy, anti‐cytokine therapies, current treatment with oral or IV steroids for > 3 months), any experimental unproven treatment against SARS‐CoV‐2 infection) |
| Interventions |
1. Bacille Calmette‐Guérin (BCG) vaccine. BCG vaccine will be given intradermally in the upper arm after randomisation 2. Placebo comparator. Placebo injection (0.9% NaCl) will be given intradermally in the upper arm after randomisation |
| Outcomes |
Primary outcomes: incidence of HCWs hospitalised due to COVID‐19 Secondary outcomes: incidence of SARS‐CoV‐2 infection, incidence of upper respiratory tract infections, days of unplanned absenteeism due to COVID‐19 or any reason, incidence of hospitalisation of HCW for any reason, incidence of ICU admission of HCW due to COVID‐19 or any reason, incidence of death of HCW due to COVID‐19 or any reason, prevalence of latent TVB infection, incidence of active TB of HCW, compare the effect of latent TB on morbidity and mortality due to COVID‐19, incidence of treatment related adverse events Data collection: baseline and at varying intervals across 52 weeks |
| Notes | Trial registration: NCT04379336 Estimated completion date: April 2021 The intervention is not aimed at mental health, but has absenteeism as an secondary outcome and may therefore capture mental health‐related absenteeism. More information required |
NCT04389476.
| Methods | Observational ‐ prospective case only; Taiwan |
| Participants |
Study population: 2500 Inclusion criteria: medical staff in high contact with patients; other personnel in low contact with patients; patients and community residents. Participants should be aged > 20 years Exclusion criteria: participants aged < 20 years and/or unable to complete assessments |
| Interventions | 1. Standardised crisis management and coping protocol plan |
| Outcomes |
Outcomes: "Acute and chronic psychological impacts". No other details available Data collection: time‐frame 3 years |
| Notes | The study design is unclear, and the description of the intervention is limited. Further information from the authors is required |
Saul 2016.
| Methods | Narrative summary; USA |
| Participants |
Study population: 24 Inclusion criteria: mental health, health and allied health professionals who work with populations that have "endured severe adversities and trauma, such as domestic and political violence, extreme poverty, armed conflict, epidemics, and natural disasters" Exclusion criteria: not reported |
| Interventions |
1. Brief immersion training programme 2 modules delivered across 2 weeks
|
| Outcomes | Not reported |
| Notes | Limited details reported about participants included in the intervention and participant mental health outcomes (if any) are unclear. Authors also mention that this is part of a larger study. Further information about outcomes, intervention and study design is required. |
Schulte 2020.
| Methods | Descriptive study reporting on the use of support calls |
| Participants | Study population: redeployed faculty staff who were asked to care for adult patients with COVID‐19 |
| Interventions | 1. Virtual support calls ("Initiated a new program of optional 1‐h group support video calls to help our faculty address their challenges, listen to how they are coping, and describe lessons learned. These calls are voluntary, informal, and facilitated by the Vice Chair for Faculty Development, who is a board‐certified executive coach. The calls are advertised as part of daily faculty e‐mail updates") |
| Outcomes |
Outcomes: number and sex of faculty participants attending Data collection: over 2‐week interval |
| Notes | Limited evaluation reported. Further information sought from authors |
Shen 2020a.
| Methods |
Design: survey Country: China Study aim: to discuss the psychological stress of nurses working in the ICU during COVID‐19 Study recruitment details: not reported Setting: ICU designated for the treatment of severe COVID‐19 patients. The ward has a total of 20 beds and 102 nurses from the local hospital and other hospitals in the provinces and cities outside of Wuhan City Epidemic/pandemic disease: COVID‐19 Phase of disease outbreak: during the pandemic |
| Participants |
Total study population: 85
Inclusion criteria: not reported
Exclusion criteria: not reported
Type (profession) of staff: nurses Length of time in the profession: not reported Previous experience of working in the frontline during an epidemic/pandemic: not reported Details of who the frontline staff were providing care for: patients with COVID‐19 on the ICU |
| Interventions | 1. Early psychological intervention: (n = 85)
|
| Outcomes | Outcomes: symptoms (e.g. decreased appetite or indigestion, fatigue, nervousness, crying), issues sleeping, suicidal thoughts Data collection: not reported |
| Notes | Limited evaluation reported. Further information sought from authors |
Siddle 2016.
| Methods | Cross‐sectional (pre‐and post‐) survey, USA |
| Participants |
Study population: 159 Inclusion criteria: ED staff Exclusion criteria: not reported |
| Interventions | 1. Effects of targeted training on ED staff's Ebola‐related perceptions and attitudes |
| Outcomes |
Outcomes: questions about risk, roles, willingness to provide care, preparedness, and the contributions of media, training, or time to opinion change using a Likert agree‐disagree scale Data collection: pre‐training and post‐training |
| Notes | Abstract only. Full text not available at present. Authors contacted for further information |
Xiao 2020.
| Methods | "An observational and cross‐sectional clinical study" |
| Participants |
Study population: 180 Inclusion criteria: medical staff (doctors, nurses) working in respiratory medicine (fever clinics or ICU) from several provinces who treated patients with COVID‐19 infection in January‐February 2020 Exclusion criteria: none reported |
| Interventions | 1. Social support. No other details described |
| Outcomes |
Outcomes: levels of anxiety, self‐efficacy, stress, sleep quality, and social support were measured using the SAS, the GSES, the SASR questionnaire, the PSQI, and the SSRS Data collection: unclear |
| Notes | The study authors report "two hypotheses tested in this study were hypothesis 1, that the social support given to the medical staff directly affected their sleep quality, and hypothesis 2, that social support affected sleep quality by reducing anxiety and stress and by increasing self‐efficacy as intermediate variables." However, it is not clear how they have collected these data or whether the data have been imputed based on structural equation modelling or whether there were baseline and follow‐up data. More information from the authors is required. |
Yau 2020.
| Methods | Narrative paper with a section describing the behaviour changes of healthcare providers, Malaysia |
| Participants | Study population: healthcare providers |
| Interventions | 1. Describe a series of behaviour changes of healthcare providers including a brief psychological intervention |
| Outcomes |
Outcomes: not reported Data collection: not reported |
| Notes | Study authors cite an unpublished paper stating that "Shoesmith and James, had created such an intervention in 2018 named Brief Psychological Interventions for the Malaysian Setting (Unpublished), and the same intervention was adapted for use during COVID‐19." Further information sought from authors |
Zhang 2020.
| Methods | Description of a crisis intervention model utilising internet technology, China |
| Participants |
Study population: not applicable
Inclusion criteria: new model, one of West China Hospital, integrates physicians, psychiatrists, psychologists and social workers into Internet platforms to carry out psychological intervention to patients, their families and medical staff
Exclusion criteria: not reported
Type (profession) of staff: not reported Length of time in the profession: not reported Previous experience of working in the frontline during an epidemic/pandemic: not reported Details of who the frontline staff were providing care for: not reported |
| Interventions |
1. Online psychological interventions: (n = not reported)
|
| Outcomes | Outcomes: none reported Data collection: not reported |
| Notes | Limited evaluation reported. Further information sought from authors |
BCG: Bacille Calmette‐Guérin; CBT: cognitive behavioural therapy; CD‐RISC: Connor‐Davidson Resilience Scale; COPE: Coping Orientation to Problems Experienced; DASS‐21: Depression Anxiety Stress Scales – short version; ED: emergency department; EVD: Ebola virus Disease; GAD‐7: General Anxiety Disorder‐7; GSES: General Self‐Efficacy Scale; IGHQ‐28: General Health Questionnaire; HADS: Hospital Anxiety and Depression Scale; HCW: healthcare worker; IAPT: Improving Access to Psychological Therapies; ICU: intensive care unit; IES‐R: Impact of Event Scale‐Revised; IV: intravenous; MBI: Maslach Burnout Inventory; MSPSS: Multidimensional Scale of Perceived Social Support; NGO: non‐governmental organisation; NHS: National Health Service; NICE: National Institute for Health and Care Excellence; PCR: polymerase chain reaction; PFA: psychological first aid; PHQ‐9: Patient Health Questionnaire‐9; PPE: personal protective equipment; PSQI: Pittsburgh Sleep Quality Index; PTGI‐SF: Post‐Traumatic Growth Inventory; PTSD: post‐traumatic stress disorder; SARS: severe acute respiratory syndrome; SAS: Self‐Rating Anxiety Scale; SASR: Stanford Acute Stress Reaction; SSRS: Social Support Rate Scale; TB: tuberculosis; TSQ: Traumatic Screening Questionnaire; WSAS: Work and Social Adjustment Scale
Characteristics of ongoing studies [ordered by study ID]
NCT04362358.
| Study name | Online cognitive behavioral therapy (CBT) for stress disorders in health workers involved in the care of patients during the COVID‐19 epidemic (REST) |
| Methods | Parallel randomised trial Aim: to evaluate the efficacy of the online CBT programme we have developed to specifically address immediate perceived stress in health workers, as well as the prevention of mental health problems at 3‐ and 6‐month follow‐up |
| Participants | 120 Inclusion criteria: health worker aged between 18‐70, able to understand French Exclusion criteria: PSS < 16, suicidal ideation assessed as < 3 on the item 9 of the PHQ‐9 and legally able to provide consent |
| Interventions |
1. Online CBT. 7 sessions of CBT online + possibility to contact the psychological hotline 2. Online bibliotherapy programme. Online bibliotherapy programme on the Ma Santé website. Also with explanatory sheets and tools to improve stress management and the possibility of contacting the Psychological Hotline |
| Outcomes |
Primary outcomes: PSS Data collection: baseline, up to 8 weeks treatment, 3‐ and 6‐month follow‐up |
| Starting date | May 2020 |
| Contact information | Luisa Weiner, University Hospital, Strasbourg, France. Email: luisa.weiner@chru‐strasbourg.fr |
| Notes | Trial registration: NCT04362358 Estimated completion date: October 2021 Authors contacted to see whether a protocol is available |
NCT04373382.
| Study name | Peer champion support for hospital staff during and after the COVID‐19 pandemic |
| Methods | Randomised, cluster, stepped‐wedge trial ("Five clusters of clinical units and departments constructed in order to approximate the following goals: similar number of staff, comparable COVID‐19 exposure, similar mix of staff by discipline and gender, number of clusters small enough to allow for the PRC intervention to be provided with at least 6 months of implementation within the two‐year study after cross‐over occurs. The Enriched survey intervention will be a RCT design with equal allocation (1:1) to both the express and enriched surveys") Aim: to test if the well‐being of hospital workers facing a novel coronavirus outbreak is improved by adding either of 2 interventions: Peer Resilience Champions or enriched feedback. |
| Participants | 1000 Inclusion criteria: employee, physician, scientist, employee of a contractor or retail business, learning, or volunteer of Sinai Health at time of recruitment; able to read and respond to a survey in English; access to a computer or device connected to the internet and be able to use the device Exclusion criteria: none listed |
| Interventions |
1. Peer Resilience Champion support. An interdisciplinary team of professionals (Peer Resilience Champion) who actively monitor for early signs of heightened stress within clinical teams, liaise between staff and senior management to improve organisational responsiveness, and provide direct support and teaching (under the supervision of experts in resilience, infection control, and professional education) 2. No Peer Resilience Champion support. Will not receive the Peer Resilience Champion support until they cross‐over into the Peer Resilience Champion support arm. 3. Enriched feedback. Individuals will receive feedback based on answers to questionnaires that will hopefully help provoke self‐reflection. 4. Express feedback. Individuals who will not receive feedback from the survey |
| Outcomes |
Primary outcomes: MBI: Emotional Exhaustion Scale Data collection: not reported |
| Starting date | June 2020 |
| Contact information | Robert Maunder, Mount Sinai Hospital, Canada. Email: Robert.maunder@sinaihealth.ca |
| Notes | Trial registration: NCT04373382 Estimated completion date: February 2022 Authors contacted to see whether a protocol is available |
NCT04387643.
| Study name | Protecting health care workers during the COVID‐19 outbreak |
| Methods | Observational Aim: to determine the experience of health care workers who had Ayurveda kadha before starting as front‐line workers |
| Participants | 52 Inclusion criteria: frontline HCWs aged 18‐60 years, working in COVID‐19 environment, HCWs who have had Ayurveda herb combination over "for at least 10 days" Exclusion criteria: unwilling to consent, "inability to participate" |
| Interventions | 1. Dietary supplement: Ayurvedic kadha. Kadha (also called Kwath and Kashaya) is a type of ayurvedic formulation prepared by boiling herbs in water. Water and herbs are main ingredients of these preparations. The preparation of Kadha uses dry herbs, which are dried under the sun or in the shade, as directed for the individual herb. Then, the herbs are pounded to form a coarse powder |
| Outcomes |
Primary outcomes: self‐reported health issues, self‐reported psychological issues Secondary outcomes: self‐reported coping with high demanding work in COVID‐19 duties, self‐reported, self‐help measures used Data collection: baseline and at 30 days |
| Starting date | March 2020 |
| Contact information | Sahil Singhal, Samta Ayurveda Prakoshtha, India |
| Notes | Trial registration: NCT04387643 Estimated completion date: April 2020 Authors contacted to see whether any publications or unpublished is available |
CBT: cognitive behavioural therapy; MBI: Maslach Burnout Inventory; PHQ‐9: Patient Health Questionnaire‐9; PSS: Perceived Stress Scale; RCT: randomised controlled trial
Differences between protocol and review
Searching other resources
We attempted to search the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/en; Appendix 11), but were unable to complete this. This was because at the time of searching, the ICTRP database was not accessible due to the high traffic generated by the COVID‐19 outbreak. We made repeated attempts to conduct searches over the succeeding months, with a final (unsuccessful) attempt in September 2020.
We planned to handsearch a number of COVID‐19 systematic search strategies and resources, as recommended by Shokraneh 2020, and we planned to conduct targeted handsearches of key organisational websites (e.g. international governmental and non‐governmental (third sector) websites). These were not conducted as systematic searches. Instead we relied on knowledge of our international advisory group members to signpost us to potentially relevant evidence, many of whom were regularly accessing and handsearching living sources of evidence relating to COVID‐19.
Types of studies
In our protocol we stated that, to address objective 2, we would include:
"evidence from:
primary qualitative studies (e.g. ethnography, case studies, and process evaluations)
mixed methods studies, where the qualitative data are reported separately"
During our searching and selection of studies that contained evidence relating to barriers and facilitators to implementation of interventions, we recognised that there was relevant evidence in a number of papers that described ‐ or commented on ‐ the development, implementation and/or evaluation of an intervention. This evidence could arise from studies with pre‐planned qualitative (e.g. interviews) or quantitative (e.g. cohort study) methods of data collection, or from papers that described factors relating to implementation of an intervention, but that did not have a pre‐planned or systematic method of data collection. We have amended the wording of the criteria stated under 'Types of studies' and have classified the included papers as either 'quantitative', 'qualitative', 'mixed method' or 'descriptive', providing definitions of these terms.
Sampling of studies
We considered selecting a sample of studies (EPOC 2017b), but reached the decision not to select a sample of studies. Had we sampled studies, we would have used a similar sampling approach to that used by Houghton 2020, based on a three‐step sampling frame (Ames 2017), in order to reach agreement on a final sample of studies we planned to:
include studies that cover a range of epidemic/pandemic diseases, including those focused on coronaviruses (i.e. MERS, SARS, COVID‐19) and those with alternative modes of disease transmission;
assess the data richness of the remaining studies, using the EPOC 2017b purposeful sampling frame (see Table 12);
-
consider the
spread of frontline health and social care professionals
types of interventions studied.
Assessment of methodological limitations
Objective 2: qualitative evidence synthesis
We planned to use a series of different tools, selected according to the design of the study, i.e. the Critical Appraisal Skills Programme for qualitative studies (CASP) (CASP 2018), Mixed Methods Appraisal Tool for mixed method studies (Pluye 2009), and SQUIRE 2.0 (Standards for Quality Improvement Reporting Excellence) checklist for appraising quality of quality improvement studies (SQUIRE 2018).
However, for some included studies the design of the study was not clear, and we therefore used the WEIRD (Ways of Evaluating Important and Relevant Data) tool to assess methodological limitations of these studies, as this tool has been developed to assess the limitations of 'non‐conventional' evidence sources (Lewin 2019).
To avoid use of multiple different quality appraisal tools, we made the decision to use CASP 2018 for qualitative studies and the WEIRD tool for all other studies included within the qualitative evidence synthesis (Lewin 2019).
We used the method for providing an overall assessment of the limitations proposed for the WEIRD tool, to reach an overall judgement on the limitations of all studies included within the qualitative evidence synthesis.
Overarching synthesis
We planned to produce a brief narrative synthesis that brings the findings from the quantitative and qualitative syntheses together, but due to lack of evidence from the quantitative synthesis we did not complete the planned formal overarching synthesis. Had we included an overarching synthesis, the aim of this integrated synthesis would have been to explore why interventions to support mental health and resilience of frontline health and social care professionals may, or may not, be effective, and to inform future decisions about how to design and implement effective interventions. We had planned to integrate the findings from the quantitative and qualitative evidence syntheses within a matrix. This would have comprised a table that lists each type of intervention explored, a brief summary of evidence of effectiveness, and any potential barriers or facilitators to implementation of that intervention that were identified, and our confidence in this evidence.
Contributions of authors
Alex Pollock (AP) and Pauline Campbell (PC) developed the review questions, and wrote drafts of the protocol. AP led the quantitative evidence synthesis, with AE conducting second review author tasks and providing statistical expertise. PC led the qualitative evidence synthesis, with JC conducting second review author tasks. Joshua Cheyne (JDC) wrote the search strategy, ran the search, and contributed to title screening. Julie Cowie (JC), Bridget Davis (BD), Kris McGill (KM), Andrew Elders (AE), Suzanne Hagen (SH), Doreen McClurg (DM), Jacqueline McCallum (JM), and Margaret Maxwell (MM) all read and commented on drafts of the protocol. JC, BD, KM and Claire Torrens (CT) contributed to study selection and data extraction. BD, DM, JM, MM and CT provided additional content expertise relating to health and social care workers and mental health and well‐being. AP and PC wrote the final review; all authors read and commented on a draft version.
Sources of support
Internal sources
No sources of support supplied
External sources
-
Scottish Government's Chief Scientist Office (CSO), UK
Grant funding. CSO ID: COV/GCU/Portfolio
Declarations of interest
Alex Pollock: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. Employed within a post at the NMAHP Research Unit, which is supported by the Chief Scientist Office, Scottish Government. No other known conflict of interest
Pauline Campbell: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. No other known conflict of interest
Joshua Cheyne: no known conflict of interest
Julie Cowie: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. No other known conflict of interest
Bridget Davis: employed as paid researcher for this grant. No other known conflict of interest.
Jacqueline McCallum: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. No other known conflict of interest
Kris McGill: no known conflict of interest
Andrew Elders: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. Employed within a post at the NMAHP Research Unit, which is supported by the Chief Scientist Office, Scottish Government. No other known conflict of interest
Suzanne Hagen: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. Employed within a post at the NMAHP Research Unit, which is supported by the Chief Scientist Office, Scottish Government. No other known conflict of interest
Doreen McClurg: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. Employed within a post at the NMAHP Research Unit, which is supported by the Chief Scientist Office, Scottish Government. DM was the chair of the Pelvic, Obstetric and Gynaecological Physiotherapy Professional Network of the Chartered Society of Physiotherapists in the UK and was the Chair of the International Continence Society Physiotherapy Committee. No other known conflict of interest
Claire Torrens: employed by the Priory Hospital Group, Glasgow and previously delivered modules within BSc Mental Health Nursing at the University of Stirling. No known conflict of interest
Margaret Maxwell: grant holder on funding from the Chief Scientist Office, Scottish Government to support this review. Employed within a post at the NMAHP Research Unit, which is supported by the Chief Scientist Office, Scottish Government. No other known conflict of interest
New
References
References to studies included in this review
Belfroid 2018 {published data only}
- Belfroid E, Van Steenbergen J, Timen A, Ellerbroek P, Huis A, Hulscher M. Preparedness and the importance of meeting the needs of healthcare workers: a qualitative study on Ebola. Journal of Hospital Infection 2018;98(2):212-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Blake 2020 {published data only}
- Blake H, Bermingham F, Johnson G, Tabner A. Mitigating the psychological impact of COVID-19 on healthcare workers: a digital learning package. International Journal of Environmental Research and Public Health 2020;17(2997):1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brown‐Johnson 2020 {published data only}
- Brown-Johnson C, Vilendrer S, Heffernan MB, Winter S, Khong T, Reidy J, et al. PPE Portraits-a way to humanize personal protective equipment. Journal of General Internal Medicine 2020;35(7):2240-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cao 2020 {published data only}
- Cao J, Wei J, Zhu H, Duan Y, Geng W, Hong X, et al. A study of basic needs and psychological wellbeing of medical workers in the fever clinic of a tertiary general hospital in Beijing during the COVID-19 outbreak. Psychotherapy and Psychosomatics 2020;30:1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong X, Cao J, Wei J, Duan Y, Zhao X, Jing J, et al. The stress and psychological impact of the COVID-19 outbreak on medical workers at the fever clinic of a tertiary general hospital in Beijing: a cross-sectional study. SSRN [Preprint] 2020. [DOI: ] [DOI] [PMC free article] [PubMed]
Carvalho 2019 {published data only}
- Carvalho E, Castro P, Leon E. Multi‐professional simulation and risk perception of health care workers caring for Ebola‐infected patients. Nursing in Critical Care 2019;24(5):256-62. [DOI] [PubMed] [Google Scholar]
Chang 2006 {published data only}
- Chang K, Gotcher DF, Chan Y. Does social capital matter when medical professionals encounter the SARS crisis in a hospital setting? Health Care Management Review 2006;31(1):26-33. [DOI] [PubMed] [Google Scholar]
Chen 2020 {published data only}
- Chen Q, Lian M, Li Y, Guo J, Fei D, Wang L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020;7(4):E15-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cheung 2015 {published data only}
- Cheung EY. An outbreak of fear, rumours and stigma: psychosocial support for the Ebola virus disease outbreak in West Africa. Intervention 2015;13(1):70-6. [Google Scholar]
Cunningham 2017 {published data only}
- Cunningham T, Rosenthal D, Catallozzi M. Narrative medicine practices as a potential therapeutic tool used by expatriate Ebola caregivers. Intervention 2017;15(2):106-19. [Google Scholar]
- Cunningham T. The use and role of narrative practices to mitigate compassion fatigue among expatriate health workers during the Ebola outbreak of 2013-2016. Dissertation Abstracts International: Section B: The Sciences and Engineering 2017;77:11-B(E).
De Jong 2019 {published data only}
- De Jong J. Strengthening evidence for the scaling of psychological first aid in humanitarian settings. www.elrha.org/project/strengthening-evidence-scaling-psychological-first-aid-humanitarian-settings/ (accessed prior to 8 October 2020).
- Horn R, O'May F, Esliker R, Gwaikolo W, Woensdregt L, Ager A. The myth of the 1-day training: the effectiveness of psychosocial support capacity-building during the Ebola outbreak in West Africa. Global Mental Health 2019;6:e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psychological first aid in the Ebola outbreak in West Africa. Research Snapshot, Research for Health in Humanitarian Crises (r2hc), www.elrha.org/wp-content/uploads/2020/03/8.-Elrha-R2HC_Research-Snapshot_19873-Psychological-First-Aid.pdf (accessed prior to 8 October 2020).
- Sijbrandij M, Horn R, Esliker R, O’May F, Reiers R, Ruttenberg L, et al. The effect of psychological first aid training on knowledge and understanding about psychosocial support principles: a cluster-randomized controlled trial. International Journal of Environmental Research and Public Health 2020;17:484. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ferranti 2016 {published data only}
- Ferranti EP, Wands L, Yeager KA, Baker B, Higgins MK, Lupo J, et al. Implementation of an educational program for nursing students amidst the Ebola virus disease epidemic. Nursing Outlook 2016;64(6):597-603. [DOI] [PMC free article] [PubMed] [Google Scholar]
Klomp 2020 {published data only}
- Klomp RW, Jones L, Watanabe E, Thompson WW. CDC's multiple approaches to safeguard the health, safety, and resilience of Ebola responders. Prehospital and Disaster Medicine 2020;35(1):69-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 2005 {published data only}
- Lee S, Juang Y, Su Y, Lee H, Lin Y, Chao C. Facing SARS: psychological impacts on SARS team nurses and psychiatric services in a Taiwan general hospital. General Hospital Psychiatry 2005;27(5):352-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schreiber 2019 {published data only}
- Schreiber M, Cates DS, Formanski S, King M. Maximizing the resilience of healthcare workers in multi-hazard events: lessons from the 2014–2015 Ebola response in Africa. Military Medicine 2019;184:114-20. [DOI] [PubMed] [Google Scholar]
Son 2019 {published data only}
- Son H, Lee W, Jun K, Hyun S, Lee KS, You M. Examination of hospital workers' emotional responses to an infectious disease outbreak: lessons from the 2015 MERS Co-V outbreak in South Korea. Disaster Medicine and Public Health Preparedness 2019;13(3):504-10. [DOI] [PubMed] [Google Scholar]
Waterman 2018 {published data only}
- Cole CL, Waterman S, Hunter EC, Bell V, Greenberg N, Rubin GJ, et al. Effectiveness of small group cognitive behavioural therapy for anxiety and depression in Ebola treatment centre staff in Sierra Leone. International Review of Psychiatry 2020 Apr 17 [Epub ahead of print]. [DOI: 10.1080/09540261.2020.1750800] [DOI] [PubMed]
- Waterman S, Cole C, Greenberg N, Rubin GJ, Beck A. A qualitative study assessing the feasibility of implementing a group cognitive–behavioural therapy-based intervention in Sierra Leone. British Journal of Psych International 2019;16(2):31-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waterman S, Hunter EC, Cole CL, Evans LJ, Greenberg N, Rubin GJ, et al. Training peers to treat Ebola centre workers with anxiety and depression in Sierra Leone. International Journal of Social Psychiatry 2018;64(2):156-65. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Banerjee 2020 {published data only}
- Banerjee D. The COVID-19 outbreak: crucial role the psychiatrists can play. Asian Journal of Psychiatry 2020;50(102014):1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barrett 2020 {published data only}
- Barrett E, Dickson M, Hayes-Brady C, Wheelock H. Storytelling and poetry in the time of coronavirus. Irish Journal of Psychological Medicine 2020 May 14 [Epub ahead of print]. [DOI: 10.1017/ipm.2020.36] [DOI] [PMC free article] [PubMed]
Barroso 2017 {published data only}
- Barroso S. A model for emerging infectious disease/disaster preparedness training for nursing students. Dissertation Abstracts International: Section B: The Sciences and Engineering 2017;78:3-B(E).
Battista 2019 {published data only}
- Battista M-C, Loignon C, Benhadj L, Nouvet E, Murthy S, Fowler R, et al. Priorities, barriers, and facilitators towards international guidelines for the delivery of supportive clinical care during an Ebola outbreak: a cross-sectional survey. Viruses 2019;11(194):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Behan 2020 {published data only}
- Behan C. The benefits of meditation and mindfulness practices during times of crisis such as COVID-19. Irish Journal of Psychological Medicine 2020 May 14 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
Bell 2017 {published data only}
- Bell SA, Munro-Kramer ML, Eisenberg MC, Williams G, Amarah P, Lori JR. “Ebola kills generations”: qualitative discussions with Liberian healthcare providers. Midwifery 2017;45:44-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bergeron 2006 {published data only}
- Bergeron SM, Cameron S, Armstrong-Stassen M, Pare K. Diverse implications of a national health crisis: a qualitative exploration of community nurses' SARS experiences. Canadian Journal of Nursing Research 2006;38(2):42-54. [PubMed] [Google Scholar]
Bohan 2020 {published data only}
- Bohan E, Hannigan L, Walsh M. Mind YOUR mind on the frontline: self-care handbook. Addressing the psychological needs of frontline and healthcare staff in response to the COVID-19 outbreak. www.fedvol.ie/_fileupload/Corona/Self-Care%20Handbook%20-%20Addressing%20the%20Psychological%20Needs%20of%20Frontline%20and%20Healthcare%20Staff%20in%20Response%20to%20the%20COVID-19%20Outbreak.pdf 2020.
Booth 2005 {published data only}
- Booth CM, Steward TE. Severe acute respiratory syndrome and critical care medicine: the Toronto experience. Critical Care Medicine 2005;33(1 Suppl):S53-S60. [DOI] [PubMed] [Google Scholar]
Chalk 2017 {published data only}
- Chalk M. The psychological effects of working at an Ebola treatment centre. British Journal of Nursing 2017;26(3):178-9. [DOI] [PubMed] [Google Scholar]
Chan 2004 {published data only}
- Chan AO, Huak CY. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occupational Medicine 2004;54(3):190-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chan‐Yeung 2004 {published data only}
- Chan-Yeung M. Severe acute respiratory syndrome (SARS) and healthcare workers. International Journal of Occupational and Environmental Health 2004;10(4):421-7. [DOI] [PubMed] [Google Scholar]
Chilton 2016 {published data only}
- Chilton JM, McNeill C, Alfred D. Survey of nursing students' self-reported knowledge of Ebola virus disease, willingness to treat, and perceptions of their duty to treat. Journal of Professional Nursing 2016;32(6):487-93. [DOI] [PubMed] [Google Scholar]
Chou 2010 {published data only}
- Chou T-L, Ho L-Y, Wang K-Y, Kao C-W, Yang M-H, Fan P-L. Uniformed service nurses' experiences with the severe acute respiratory syndrome outbreak and response in Taiwan. Nursing Clinics of North America 2010;45(2):179-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chung 2005 {published data only}
- Chung BP, Wong TK, Suen ES, Ching JW. SARS: caring for patients in Hong Kong. Journal of Clinical Nursing 2005;14(4):510-7. [DOI] [PubMed] [Google Scholar]
Corley 2010 {published data only}
- Corley A, Hammond NE, Fraser JF. The experiences of health care workers employed in an Australian intensive care unit during the H1N1 influenza pandemic of 2009: a phenomenological study. International Journal of Nursing Studies 47;5:577-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Everly 2014 {published data only}
- Everly GS, Lee McCabe O, Semon NL, Thompson CB, Links JM. The development of a model of psychological first aid for non-mental health trained public health personnel: the Johns Hopkins RAPID-PFA. Journal of Public Health Management and Practice 2014;5:S24-9. [DOI] [PubMed] [Google Scholar]
Fukuti 2020 {published data only}
- Fukuti P, Uchoa CL, Mazzoco MF, Corchs F, Kamitsuji S, De Rossi L, et al. How institutions can protect the mental health and psychosocial well-being of their healthcare workers in the current COVID-19 pandemic. Clinics 2020;75(e1963):1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gershon 2016 {published data only}
- Gershon R, Dernehl LA, Nwankwo E, Zhi Q, Qureshi K. Experiences and psychosocial impact of West Africa Ebola deployment on US health care volunteers. PLoS Currents 2016;September 21:8. [DOI: 10.1371/currents.outbreaks.c7afaae124e35d2da39ee7e07291b6b5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Greenberg 2015 {published data only}
- Greenberg N, Wessely S, Wykes T. Potential mental health consequences for workers in the Ebola regions of West Africa - a lesson for all challenging environments. Journal of Mental Health 2015;24(1):1-3. [DOI] [PubMed] [Google Scholar]
Liu 2020 {published data only}
- Liu Y, Wang H, Chen J, Zhang X, Yue X, Ke J, et al. Emergency management of nursing human resources and supplies to respond to coronavirus disease 2019 epidemic. International Journal of Nursing Sciences 2020;7(2):135-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maltzman 2011 {published data only}
- Maltzman S. An organizational self-care model: practical suggestions for development and implementation. Counseling Psychologist 2011;39(2):303-19. [Google Scholar]
Marrs 2020 {published data only}
- Marrs R, Horsley TL, Hackbarth D, Landon E. High consequence infectious diseases training using interprofessional simulation and TeamSTEPPS. American Journal of Infection Control 2020;48:615-20. [DOI] [PubMed] [Google Scholar]
Maunder 2010 {published data only}
- Maunder RG, Lancee WJ, Mae R, Vincent L, Peladeau N, Beduz MA, et al. Computer-assisted resilience training to prepare healthcare workers for pandemic influenza: a randomized trial of the optimal dose of training. BMC Health Services Research 2010;10:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Meyer 2018 {published data only}
- Meyer D, Sell K, Schoch-Spana M, Shearer MP, Chandler H, Thomas E, et al. Lessons from the domestic Ebola response: improving health care system resilience to high consequence infectious diseases. American Journal of Infection Control 2018;46(5):533-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT04324190 {published data only}
- NCT04324190. DIgital online SuPport for COVID-19 StrEss (DISPOSE). ClinicalTrials.gov/show/NCT04324190 (first received 27 March 2020).
Shen 2020b {published data only}
- Shen Y, Cui Y, Li N, Tian C, Chen M, Zhang Y-W, et al. Emergency responses to COVID-19 outbreak: experiences and lessons from a general hospital in Nanjing, China. Cardiovascular and Interventional Radiology 2020;43:810-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Singh 2020 {published data only}
- Singh M, Sharda S, Gautam, M, Hawa R. Optimal sleep health among frontline healthcare workers during the COVID-19 pandemic. Canadian Journal of Anaesthesia 2020;May 18:1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Soma 2020 {published data only}
- Soma M, Jacobson I, Brewer J, Blondin A, Davidson G, Singham S. Operative team checklist for aerosol generating procedures to minimise exposure of healthcare workers to SARS-CoV-2. International Journal of Pediatric Otorhinolaryngology 2020;134(110075):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sprang 2015 {published data only}
- Sprang G, Silman M. Using professional organizations to prepare the behavioral health workforce to respond to the needs of pediatric populations impacted by health-related disasters: guiding principles and challenges. Disaster Medicine and Public Health Preparedness 2015;9(6):642-9. [DOI] [PubMed] [Google Scholar]
Tam 2004 {published data only}
- Tam CW, Pang EP, Lam LC, Chiu HF. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychological Medicine 2004;34(7):1197-204. [DOI] [PubMed] [Google Scholar]
Taylor 2019 {published data only}
- Taylor G. Perspectives of Sierra Leoneans healthcare workers' mental health during the Ebola outbreak. Dissertation Abstracts International: Section B: The Sciences and Engineering 2019;80:11-B(E).
Vymetal 2011 {published data only}
- Vymetal S, Deistler A, Bering R, Schedlich C, Rooze M, Orengo F, et al. European Commission project: European guideline for target group-oriented psychosocial aftercare-implementation. Prehospital and Disaster Medicine 2011;26(3):234-6. [DOI] [PubMed] [Google Scholar]
Wald 2020 {published data only}
- Wald HS. Optimizing resilience and wellbeing for healthcare professions trainees and healthcare professionals during public health crises - practical tips for an 'integrative resilience' approach. Medical Teacher 2020;42(7):744-55. [DOI] [PubMed] [Google Scholar]
WHO 2014b {published data only}
- World Health Organization. Psychological first aid during Ebola virus disease outbreaks. www.who.int/mental_health/emergencies/psychological_first_aid_ebola/en/ 2014.
WHO 2015 {published data only}
- World Health Organization. Enhanced capacity building training for frontline staff on building trust and communication: facilitator’s guide, July 2015. www.who.int/csr/en/ 2015.
WHO 2020b {published data only}
- World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak, 18 March 2020. www.who.int/publications/i/item/mental-health-and-psychosocial-considerations-during-the-covid-19-outbreak 2020.
WHO 2020d {published data only}
- World Health Organization. COVID-19: operational guidance for maintaining essential health services during an outbreak: interim guidance, 25 March 2020. apps.who.int/iris/handle/10665/331561 2020.
WHO 2020e {published data only}
- World Health Organization Regional office for the Eastern Mediterranean. WHO interim guidance note: health workforce response to the COVID-19 pandemic: April 2020. apps.who.int/iris/handle/10665/331949?locale-attribute=pt& 2020.
Xi 2019 {published data only}
- Xi Y, Chen R, Gillespie AL, He Y, Jia C, Shi K, et al. Mental health workers perceptions of disaster response in China. BMC Public Health 2019;19(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yuen‐Tsang 2004 {published data only}
- Yuen-Tsang AW, Tsien-Wong TB. Universities and civic responsibility - an actualisation of the university-community partnership model through the Anti-SARS Project in Hong Kong. Asia Pacific Journal of Social Work and Development 2004;14(1):19-32. [Google Scholar]
References to studies awaiting assessment
Albott 2020 {published data only}
- Albott CS, Wozniak JR, McGlinch BP, Wall MH, Gold BS, Vinogradov S. Battle Buddies: rapid deployment of a psychological resilience intervention for healthcare workers during the COVID-19 pandemic. Anesthesia and Analgesia 2020;131(1):43-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Banerjee 2020a {published data only}
- Banerjee D, Nair VS. Handling the COVID-19 pandemic: proposing a community based toolkit for psycho-social management and preparedness. Asian Journal of Psychiatry 2020;51(102152):1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Benzarti 2020 {published data only}
- Benzarti S, Achouri MY, Nouira S, Mlouki I, Yahia F, Ben Abdelaziz A, et al. Counter-COVID- 19 pandemic strategy in the Maghreb Central. Qualitative study of the perceptions of health professionals. Tunisie Medicale 2020;98(4):266-82. [PubMed] [Google Scholar]
Brusin 2003 {published data only}
- Brusin LK. Addressing stress reactions in disaster mental health clinicians: a post-disaster assignment recovery manual. Dissertation Abstracts International: Section B: The Sciences and Engineering 2003.
Casado‐Mejia 2016 {published data only}
- Casado-Mejia R, Brea-Ruiz MT, Torres-Enamorado D, Albar-Marin MJ, Botello-Hermosa A, Santos-Casado M, et al. Motivations and emotional experiences of the first hospital multidisciplinary team trained to care for people with Ebola in Andalusia, Spain (2014-2016) [Motivaciones y experiencias emocionales del primer equipo multidisciplinario hospitalario entrenado para atender casos de Ebola en Andalucia (2014-2016)]. Gaceta Sanitaria 2016;30(4):242-9. [DOI] [PubMed] [Google Scholar]
Cheng 2020 {published data only}
- Cheng P, Xia G, Pang P, Wu B, Jiang W, Li Y-T, et al. COVID-19 epidemic peer support and crisis intervention via social media. Community Mental Health Journal 2020;56:786-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
ChiCTR‐TRC‐11001268 {published data only}
- ChiCTR-TRC-11001268. Effectiveness of psychological first aid training in improving self-efficacy and mental health outcomes for Chinese emergency responders: a randomized controlled trial. apps.who.int/trialsearch/Trial2.aspx?TrialID=ChiCTR-TRC-11001268 (first received 24 March 2011).
Chung 2020 {published data only}
- Chung JP, Yeung W-S. Staff mental health self-assessment during the COVID-19 outbreak. East Asian Archives of Psychiatry 2020;30:34. [DOI] [PubMed] [Google Scholar]
Cole 2020 {published data only}
- Cole EL, Waterman S, Stott J, Saunders R, Buckman JE, Pilling S, et al. Adapting IAPT services to support frontline NHS staff during the COVID-19 pandemic: the Homerton Covid Psychological Support (HCPS) pathway. discovery.ucl.ac.uk/id/eprint/10096883/1/adapting_iapt_services_to_support_frontline_nhs_staff_during_the_covid19_pandemic_the_homerton_covid_psychological_support_hcps_pathway.pdf 2020. [DOI: 10.1017/S1754470X20000148] [DOI] [PMC free article] [PubMed]
Fu 2004 {published data only}
- Fu XL, Wang ZQ, Zhu ZH, Zhu HW. A randomed controlled study on the effect of psychological behavior training on mental health of the healthcare workers in SARS ward. International Journal of Psychology 39;5-6:191. [Google Scholar]
Goh 2020 {published data only}
- Goh SS, Chia MY. Anxiety and morale in front-line healthcare workers during the coronavirus disease 2019 (COVID-19) outbreak at the National Screening Centre in Singapore. Annals of the Academy of Medicine 2020;49(4):259-62. [PubMed] [Google Scholar]
James 2020 {published data only}
- James PB, Wardle J, Steel A, Adams J, Bah AJ, Sevalie S. Providing healthcare to Ebola survivors: a qualitative exploratory investigation of healthcare providers' views and experiences in Sierra Leone. Global Public Health 2020;15(9):1380-95. [DOI] [PubMed] [Google Scholar]
Jiang 2020 {published data only}
- Jiang X, Deng L, Zhu Y, Ji H, Tao L, Yang D, et al. Psychological crisis intervention during the outbreak period of new coronavirus pneumonia from experience in Shanghai. Psychiatry Research 2020;286:112903. [DOI] [PMC free article] [PubMed] [Google Scholar]
Keita 2017 {published data only}
- Keita MM, Doukoure M, Chantereau I, Sako FB, Traore FA, Soumaoro K, et al. Survivors of epidemic recent disease Ebola virus in psychiatric hospital service national Donka in Guinea: psychopathological and psychotherapeutic study. Evolution Psychiatrique 2017;82(1):127-42. [Google Scholar]
Khee 2004 {published data only}
- Khee KS, Lee LB, Chai OT, Loong CK, Ming CW, Kheng TH. The psychological impact of SARS on healthcare providers. Critical Care and Shock 2004;7(2):99-106. [Google Scholar]
Li 2020 {published data only}
- Li YF, Zhang YG, Niu JT, Si XL, Yan XK. Analysis of TCM in prevention and treatment of post-traumatic stress disorder induced by COVID-19. Chinese Traditional and Herbal Drugs 2020;51(5):1130-8. [Google Scholar]
Liu 2015 {published data only}
- Liu B, Zhu Y, Huang S. Influence of TCM baduanjing exercise on physical and mental condition of international medical team members fighting against Ebola virus. Chinese Nursing Research 2015;29(7C):2629-30. [Google Scholar]
Masumbuko 2020 {published data only}
- Masumbuko CK, Hawkes MT. Ebola crisis in Eastern Democratic Republic of Congo: student-led community engagement. Pathogens and Global Health 2020;114(4):218-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mehtar 2016 {published data only}
- Mehtar S. The impact of education on reducing Ebola virus disease transmission in healthcare facilities. International Journal of Infectious Diseases 2016;45 Suppl 1:66-7. [Google Scholar]
NCT04363671 {published and unpublished data}
- NCT04363671. Adolescents and health professionals faced with the necessity for changing to remote care during the COVID-19 outbreak quarantine (AdoPro-Cov19). clinicaltrials.gov/ct2/show/NCT04363671 (first received 27 April 2020).
NCT04367857 {published and unpublished data}
- NCT04367857. ARMOR Study: COVID-19 seroprevalence among healthcare workers. clinicaltrials.gov/ct2/show/NCT04367857 (first received 29 April 2020).
NCT04377165 {published and unpublished data}
- NCT04377165. Innovative tool to limit spread of SARS-CoV-2 in residential aged care facilities. ClinicalTrials.gov/show/NCT04377165 (first received 6 May 2020).
NCT04379063 {published and unpublished data}
- NCT04379063. COVID-19 pandemic short interval national survey gauging psychological distress (COPING). www.clinicaltrials.gov/ct2/show/NCT04379063 (first received 7 May 2020).
NCT04379336 {published data only}
- NCT04379336. BCG vaccination for healthcare workers in COVID-19 pandemic. clinicaltrials.gov/ct2/show/NCT04379336 (first received 7 May 2020).
NCT04389476 {published data only}
- NCT04389476. The impact and coping strategy of COVID-19 among Taiwan society and medical and nursing institutes. clinicaltrials.gov/ct2/show/record/NCT04389476?view=record (first received 15 May 2020).
Saul 2016 {published data only}
- Saul J, Simon W. Building resilience in families, communities, and organizations: a training program in global mental health and psychosocial support. Family Process 55;4:689-99. [DOI] [PubMed] [Google Scholar]
Schulte 2020 {published data only}
- Schulte EE, Bernstein CA, Cabana MD. Addressing faculty emotional responses during the coronavirus 2019 pandemic. Journal of Pediatrics 2020;222:13-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shen 2020a {published data only}
- Shen X, Zou X, Zhong X, Yan J, Li L. Psychological stress of ICU nurses in the time of COVID-19. Critical Care 2020;24(1):200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Siddle 2016 {published data only}
- Siddle J, Tolleson-Rinehart S, Brice J. Survey of emergency department staff on disaster preparedness and training for Ebola virus disease. American Journal of Disaster Medicine 2016;11(1):5-18. [DOI] [PubMed] [Google Scholar]
Xiao 2020 {published data only}
- Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Medical Science Monitor: International Journal of Experimental and Clinical Research 2020;26(e923549):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yau 2020 {published data only}
- Yau EK, Ping NP, Shoesmith WD, James S, Hadi NM, Loo JL. The behaviour changes in response to COVID-19 Pandemic within Malaysia. Malaysian Journal of Medical Sciences 2020;27(2):45-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2020 {published data only}
- Zhang M, Zhou M, Tang F, Wang Y, Nie H, Zhang L, et al. Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: a model of West China Hospital. Precision Clinical Medicine 2020;3(1):3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
NCT04362358 {published and unpublished data}
- NCT04362358. Online cognitive behavioral therapy (CBT) for stress disorders in health workers involved in the care of patients during the COVID-19 epidemic (REST). clinicaltrials.gov/ct2/show/NCT04362358 (first received 24 April 2020).
NCT04373382 {published and unpublished data}
- NCT04373382. Peer champion support for hospital staff during and after the COVID-19 pandemic. clinicaltrials.gov/ct2/show/NCT04373382 (first received 4 May 2020).
NCT04387643 {published and unpublished data}
- NCT04387643. Protecting health care workers during the COVID-19 outbreak. clinicaltrials.gov/ct2/show/NCT04387643 (first received 14 May 2020).
Additional references
Allan 2020
- Allan SM, Bealey R, Birch J, Cushing T, Parke S, Sergi G, et al. The prevalence of common and stress-related mental health disorders in healthcare workers based in pandemic-affected hospitals: a rapid systematic review and meta-analysis. European Journal of Psychotraumatology 2020;11(1):1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ames 2017
- Ames HM, Glenton C, Lewin S. Parents' and informal caregivers' views and experiences of communication about routine childhood vaccination: a synthesis of qualitative evidence. Cochrane Database of Systematic Reviews 2017, Issue 2. Art. No: CD011787. [DOI: 10.1002/14651858.CD011787.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Aoyagi 2015
- Aoyagi Y, Beck CR, Dingwall R, Nguyen-Van-Tam JS. Healthcare workers' willingness to work during an influenza pandemic: a systematic review and meta-analysis. Influenza and Other Respiratory Viruses 2015;9(3):120-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ayanore 2019
- Ayanore MA, Amuna N, Aviisah M, Awolu A, Kipo-Sunyehzi DD, Mogre V, et al. Towards resilient health systems in Sub-Saharan Africa: a systematic review of the English language literature on health workforce, surveillance, and health governance issues for health systems strengthening. Annals of Global Health 2019;85(1):113, 1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bach‐Mortensen 2018
- Bach-Mortensen AM, Lange BC, Montgomery P. Barriers and facilitators to implementing evidence-based interventions among third sector organisations: a systematic review. Implementation Science 2018;13(1):103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baduge 2018
- Baduge M, Morphet J, Moss C. Emergency nurses' and department preparedness for an ebola outbreak: a (narrative) literature review. International Emergency Nursing 2018;38:41-9. [DOI] [PubMed] [Google Scholar]
Balasubramanian 2020
- Balasubramanian A, Paleri V, Bennett R, Paleri V. Impact of COVID‐19 on the mental health of surgeons and coping strategies. Head and Neck 2020;42(7):1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bansal 2020
- Bansal P, BingemannTA, Greenhawt M, Mosnaim G, Nanda A, Oppenheimer J, et al. Clinician wellness during the COVID-19 pandemic: extraordinary times and unusual challenges for the allergist/immunologist. Journal of Allergy and Clinical Immunology 2020;8(6):1781-90. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bell 2020
- Bell V, Wade D. Mental health of clinical staff working in high-risk epidemic and pandemic health emergencies: a rapid review of the evidence and meta-analysis. medRxiv [Preprint] 2020. [DOI: ] [DOI] [PMC free article] [PubMed]
Benedek 2007
- Benedek DM, Fullerton C, Ursano RJ. First responders: mental health consequences of natural and human-made disasters for public health and public safety workers. Annual Review of Public Health 2007;28:55-68. [DOI] [PubMed] [Google Scholar]
British Psychological Society 2020
- British Psychological Society Covid 19 Staff Wellbeing Group. The psychological needs of healthcare staff as a result of the coronavirus pandemic: guidance. www.bps.org.uk/sites/www.bps.org.uk/files/News/News%20-%20Files/Psychological%20needs%20of%20healthcare%20staff.pdf 2020.
Brooks 2016
- Brooks SK, Dunn R, Amlot R, Greenberg N, Rubin GJ. Social and occupational factors associated with psychological distress and disorder among disaster responders: a systematic review. BMC Psychology 2016;4:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brooks 2018
- Brooks SK, Dunn R, Amlot R, Rubin GJ, Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. Journal of Occupational and Environmental Medicine 2018;60(3):248-57. [DOI] [PubMed] [Google Scholar]
Cabello 2020
- Cabello IR, Echavez JF, Serrano-Ripoll MJ, Fraile-Navarro D, Roque MA, Moreno GP, et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review. medRxiv [Preprint] 2020. [DOI: ] [DOI] [PMC free article] [PubMed]
Campbell 2020
- Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ 2020;368:l6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carroll 2011
- Carroll C, Booth A, Cooper K. A worked example of "best fit" framework synthesis: a systematic review of views concerning the taking of some potential chemopreventive agents. BMC Medical Research Methodology 2011;11(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
CASP 2018
- Critical Appraisal Skills Programme (CASP). Critical Appraisal Skills Programme Checklists. casp-uk.net/#!casp-tools- checklists/c18f82018) 2018.
CDC 2011
- Centre for Disease Control and Prevention. Section 11: Epidemic disease occurrence. In: Principles of Epidemiology in Public Health Practice. 3rd edition. CDC Division of scientific education and professional development, 2011:www.cdc.gov/csels/dsepd/ss1978/lesson1/section11.html. [Google Scholar]
CDC 2020a
- Centers for Diseases Control and Prevention. Employees: how to cope with job stress and build resilience during the COVID-19 pandemic. www.cdc.gov/coronavirus/2019-ncov/community/mental-health-non- healthcare.html 2020.
CDC 2020b
- Centers for Disease Control and Prevention. Coping with stress. www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html 2020.
Cenat 2020
- Cenat JM, Mukunzi JN, Noorishad P-G, Rousseau C, Derivois D, Bukaka J. A systematic review of mental health programs among populations affected by the Ebola virus disease. Journal of Psychosomatic Research 2020;131(109966):1-11. [DOI] [PubMed] [Google Scholar]
CFIR 2020
- Consolidated Framework for Implementation Research. Consolidated Framework for Implementation Research (CFIR) guide. cfirguide.org 2020.
Chakraborty 2020
- Chakraborty N. The COVID‐19 pandemic and its impact on mental health. Progress in Neurology & Psychiatry 2020;24(2):21-4. [Google Scholar]
Chen 2006
- Chen R, Chou KR, Huang YJ, Wang TS, Liu SY, Ho LY. Effects of a SARS prevention programme in Taiwan on nursing staff's anxiety, depression and sleep quality: a longitudinal survey. International Journal of Nursing Studies 2006;43(2):215-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chersich 2020
- Chersich MF, Gray G, Fairlie L, Eichbaum Q, Mayhew S, Allwood B, et al. COVID-19 in Africa: care and protection for frontline healthcare workers. Globalization and Health 2020;16(1):46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Connor 2014
- Connor B. When and why health care personnel respond to a disaster: the state of the science. Prehospital & Disaster Medicine 2014;29(3):270-4. [DOI] [PubMed] [Google Scholar]
Covidence [Computer program]
- Veritas Health Innovation Covidence. Version accessed 28 May 2020. Melbourne, Australia: Veritas Health Innovation. Available at covidence.org.
Devnani 2012
- Devnani M. Factors associated with the willingness of health care personnel to work during an influenza public health emergency: An integrative review. Prehospital and Disaster Medicine 2012;27(6):551-66. [DOI] [PubMed] [Google Scholar]
Downe 2019
- Downe S, Finlayson KW, Lawrie TA, Lewin SA, Rosenbaum S, Barreix M, et al. Qualitative evidence synthesis (QES) for guidelines: paper 1 – using qualitative evidence synthesis to inform guideline scope and develop qualitative findings statements. Health Research Policy and Systems 2019;17:Article number: 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Duan 2020
- Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry 2020;7(4):300-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Duncan 2020
- Duncan DL. What the COVID-19 pandemic tells us about the need to develop resilience in the nursing workforce. Nursing Management 2020;27(3):22-7. [DOI] [PubMed] [Google Scholar]
Ejeta 2015
- Ejeta LT, Ardalan A, Paton D. Application of behavioral theories to disaster and emergency health preparedness: a systematic review. PLoS Currents 2015;1:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
EPOC 2017a
- Cochrane Effective Practice and Organisation of Care (EPOC). EPOC Resources for review authors. What study designs can be considered for inclusion in an EPOC review and what should they be called? epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/Resources-for-authors2017/what_study_designs_should_be_included_in_an_epoc_review.pdf (accessed 5 May 2020).
EPOC 2017b
- Cochrane Effective Practice and Organisation of Care (EPOC). EPOC resources for review authors. EPOC qualitative evidence syntheses guidance on when to sample and how to develop a purposive sampling frame. epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/Resources-for-authors2017/qes_guidance_on_sampling.pdf (accessed 4 June 2020).
EPOC 2019
- Glenton C, Bohren MA, Downe S, Paulsen EJ, Lewin S, Cochrane Effective Practice and Organisation of Care (EPOC). EPOC qualitative evidence synthesis: protocol and review template. epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/Resources-for-authors2017/epoc_qes_protocol_and_review_template.pdf (accessed 29 June 2020).
Erren 2013
- Erren TC, Herbst C, Koch MS, Fritschi L, Foster RG, Driscoll TR, et al. Adaptation of shift work schedules for preventing and treating sleepiness and sleep disturbances caused by shift work. Cochrane Database of Systematic Reviews 2013, Issue 7. Art. No: CD010639. [DOI: 10.1002/14651858.CD010639] [DOI] [Google Scholar]
Etkind 2020
- Etkind SN, Bone AE, Lovell N, Cripps RL, Harding R, Higginson IJ, et al. The role and response of palliative care and hospice services in epidemics and pandemics: a rapid review to inform practice during the COVID-19 pandemic. Journal of Pain and Symptom Management 2020;60(1):e31-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Galbraith 2020
- Galbraith N, Boyda D, McFeeters D, Hassan T. The mental health of doctors during the COVID-19 pandemic. BJPsych Bulletin 2020 Apr 28 [Epub ahead of print]. [DOI: 10.1192/bjb.2020.44] [DOI] [PMC free article] [PubMed]
Gardner 2015
- Gardner PJ, Moallef P. Psychological impact on SARS survivors: critical review of the English language literature. Canadian Psychology 2015;56(1):123-35. [Google Scholar]
Giga 2018
- Giga SI, Fletcher IJ, Sgourakis G, Mulvaney CA, Vrkljan BH. Organisational level interventions for reducing occupational stress in healthcare workers. Cochrane Database of Systematic Reviews 2018, Issue 4. Art. No: CD013014. [DOI: 10.1002/14651858.CD013014] [DOI] [Google Scholar]
Gowing 2017
- Gowing JR, Walker KN, Elmer SL, Cummings EA. Disaster preparedness among health professionals and support staff: what is effective? an integrative literature review. Prehospital and Disaster Medicine 2017;32(3):321-8. [DOI] [PubMed] [Google Scholar]
Harmer 2017
- Harmer CJ, Duman RS, Cowen PJ. How do antidepressants work? New perspectives for refining future treatment approaches. Lancet Psychiatry 2017;4(5):409-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
HCPC 2016
- Health and Care Professions Council. Returning to practice. www.hcpc-uk.org/resources/guidance/returning-to-practice/ 2016.
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2017
- Higgins JP, Altman DG, Sterne JA, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017). Cochrane, 2017. Available from www.training.cochrane.org/handbook.
Higgins 2020a
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane, 2020. Available from www.training.cochrane.org/handbook.
Higgins 2020b
- Higgins JP, Eldridge S, Li T, editor(s). Chapter 23: Including variants on randomized trials. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane, 2020. Available from www.training.cochrane.org/handbook.
Hoffmann 2014
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. [DOI] [PubMed] [Google Scholar]
Houghton 2020
- Houghton C, Meskell P, Delaney H, Smalle M, Glenton C, Booth A, et al. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2020, Issue 4. Art. No: CD013582. [DOI: 10.1002/14651858.CD013582] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jackson 2007
- Jackson D, Firtko A, Edenborough M. Personal resilience as a strategy for surviving and thriving in the face of workplace adversity: a literature review. Journal of Advanced Nursing 2007;60(1):1-9. [DOI] [PubMed] [Google Scholar]
Kang 2020
- Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 2020;7(3):e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kausto 2019
- Kausto J, Verbeek JH, Ruotsalainen JH, Halonen JI, Virta LJ, Kankaanpää E. Self-certification versus physician certification of sick leave for reducing sickness absence and associated costs. Cochrane Database of Systematic Reviews 2019, Issue 5. Art. No: CD013098. [DOI: 10.1002/14651858.CD013098.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kisely 2020
- Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ 2020;369(m1642):1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Koh 2010
- Koh Y, Hegney D, Drury V. A comprehensive systematic review of healthcare workers' perceptions of risk from exposure to emerging acute respiratory infectious diseases and the perceived effectiveness of strategies used to facilitate healthy coping in acute hospital and community healthcare settings. JBI Library of Systematic Reviews 2010;8(23):917-71. [DOI] [PubMed] [Google Scholar]
Kuehnl 2019
- Kuehnl A, Seubert C, Rehfuess E, Elm E, Nowak D, Glaser J. Human resource management training of supervisors for improving health and well-being of employees. Cochrane Database of Systematic Reviews 2019, Issue 9. Art. No: CD010905. [DOI: 10.1002/14651858.CD010905.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kunzler 2020
- Kunzler AM, Helmreich I, Chmitorz A, König J, Binder H, Wessa M, et al. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database of Systematic Reviews 2020, Issue 7. Art. No: CD012527. [DOI: 10.1002/14651858.CD012527.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kuster 2017
- Kuster AT, Dalsbø TK, Luong Thanh BY, Agarwal A, Durand‐Moreau QV, Kirkehei I. Computer-based versus in-person interventions for preventing and reducing stress in workers. Cochrane Database of Systematic Reviews 2017, Issue 8. Art. No: CD011899. [DOI: 10.1002/14651858.CD011899.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewin 2018
- Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implementation Science 2018;13 Suppl 1:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewin 2019
- Lewin S, Langlois E, Tuncalp Ö, Portela A, the COMMVAC Project Team. WEIRD (Ways of Evaluating Important and Relevant Data) tool: questions to guide assessment / critical appraisal of programme descriptions, implementation descriptions and other mainly descriptive types of evidence. Norwegian Institute of Public Health; epoc.cochrane.org/resources/epocresources-review-authors 2019;1.1.
Liira 2014
- Liira J, Verbeek JH, Costa G, Driscoll TR, Sallinen M, Isotalo LK, et al. Pharmacological interventions for sleepiness and sleep disturbances caused by shift work. Cochrane Database of Systematic Reviews 2014, Issue 8. Art. No: CD009776. [DOI: 10.1002/14651858.CD009776.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Liira 2016
- Liira H, Knight AP, Sim MG, Wilcox HM, Cheetham S, Aalto MT. Workplace interventions for preventing job loss and other work related outcomes in workers with alcohol misuse. Cochrane Database of Systematic Reviews 2016, Issue 9. Art. No: CD012344. [DOI: 10.1002/14651858.CD012344] [DOI] [Google Scholar]
Lubans 2016
- Lubans D, Richards J, Hillman C, Faulkner G, Beauchamp M, Nilsson M, et al. Physical activity for cognitive and mental health in youth: a systematic review of mechanisms. Pediatrics 2016;138(3):e20161642. [DOI] [PubMed] [Google Scholar]
Lynch 2020
- Lynch P. New resources to help health care workers cope with COVID-19-related stress. www.univadis.co.uk/viewarticle/new-resources-to-help-health-care-workers-cope- with-covid-19-related-stress-717806?topic=covid-19 2020.
Maunder 2006
- Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerging Infectious Diseases 2006;12(12):1924-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
McGowan 2016
- McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. Journal of Clinical Epidemiology 2016;75:40-6. [DOI] [PubMed] [Google Scholar]
MHF 2016
- Mental Health Foundation. Fundamental facts about mental health. www.mentalhealth.org.uk/publications/fundamental-facts-about-mental-health-2016 (accessed 29 June 2020).
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Medicine 2009;6(7):e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Muller 2020
- Muller AE, Hafstad EV, Himmels JP, Smedslund G, Flottorp S, Stensland S, et al. The mental health impact of the COVID-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatry Research 2020;293:1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Naghieh 2015
- Naghieh A, Montgomery P, Bonell CP, Thompson M, Aber JL. Organisational interventions for improving wellbeing and reducing work-related stress in teachers. Cochrane Database of Systematic Reviews 2015, Issue 4. Art. No: CD010306. [DOI: 10.1002/14651858.CD010306.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nair 2020
- Nair V, Sekar K, Thomas P. Knowledge among nursing students on Zika preparedness. Acta Scientific Neurology 2020;3(3):17-21. [Google Scholar]
NHS England 2020
- NHS Health Education England. Roles in the wider healthcare team UK. www.healthcareers.nhs.uk/explore-roles/wider-healthcare-team/roles-wider-healthcare-team (accessed July 2020).
Nieuwenhuijsen 2014
- Nieuwenhuijsen K, Faber B, Verbeek JH, Neumeyer‐Gromen A, Hees HL, Verhoeven AC, et al. Interventions to improve return to work in depressed people. Cochrane Database of Systematic Reviews 2014, Issue 12. Art. No: CD006237. [DOI: 10.1002/14651858.CD006237.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Noyes 2018
- Noyes J, Booth A, Cargo M, Flemming K, Garside R, Hannes K, et al. Cochrane Qualitative and Implementation Methods Group guidance series-paper 1: introduction. Journal of Clinical Epidemiology 2018;97:35-8. [DOI] [PubMed] [Google Scholar]
Noyes 2020
- Noyes J, Booth A, Cargo M, Flemming K, Harden A, Harris J, et al. Chapter 21: Qualitative evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane, 2020. Available from www.training.cochrane.org/handbook.
Pachito 2018
- Pachito DV, Eckeli AL, Desouky AS, Corbett MA, Partonen T, Rajaratnam SM, et al. Workplace lighting for improving alertness and mood in daytime workers. Cochrane Database of Systematic Reviews 2018, Issue 3. Art. No: CD012243. [DOI: 10.1002/14651858.CD012243.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pluye 2009
- Pluye P, Gagnon MP, Griffiths F, Johnson-Lafleur J. A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in mixed studies reviews. International Journal of Nursing Studies 2009;46(4):529-46. [DOI] [PubMed] [Google Scholar]
ProQOL‐5
- Stamm BH. The Concise ProQOL Manual. 2nd edition. Pocatello, USA: ProQOL.org, 2010. [Google Scholar]
Reeves 2020
- Reeves BC, Deeks JJ, Higgins JP, Shea B, Tugwell P, Wells GA. Chapter 24: Including non-randomized studies on intervention effects. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane, 2020. Available from www.training.cochrane.org/handbook.
Review Manager 2020 [Computer program]
- The Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.4. Copenhagen: The Cochrane Collaboration, 2020.
Robertson 2016
- Robertson HD, Elliot AM, Burton C, Iversen P, Murchie P, Porteuous T, et al. Resilience of primary healthcare professionals: a systematic review. British Journal of General Practice 2016;66(647):e423-e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Robertson 2020
Ruotsalainen 2015
- Ruotsalainen JH, Verbeek JH, Mariné A, Serra C. Preventing occupational stress in healthcare workers. Cochrane Database of Systematic Reviews 2015, Issue 4. Art. No: CD002892. [DOI: 10.1002/14651858.CD002892.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sandelowski 2007
- Sandelowski M, Barraso J. Handbook for Synthesizing Qualitative Research. New York: Springer Publishing, 2007. [Google Scholar]
Schünemann 2020
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane, 2020. Available from www.training.cochrane.org/handbook.
Scior 2020
- Scior K, Clements H. Proposed Pilot and Formative Evaluation of 20minCareSpace. Unpublished manuscript 2020.
Shah 2020
- Shah K, Kamrai D, Mekala H, Mann B, Desai K, Patel RS. Focus on mental health during the coronavirus (COVID-19) pandemic: applying learnings from the past outbreaks. Cureus 2020;12(3):e7405. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shanafelt 2020
- Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA 2020;323(21):2133-4. [DOI: 10.1001/jama.2020.5893] [DOI] [PubMed] [Google Scholar]
Shokraneh 2020
- Shokraneh F. Keeping up with studies on COVID-19: systematic search strategies and resources. BMJ 2020;369:m1601. [DOI] [PubMed] [Google Scholar]
Shultz 2016
- Shultz JM, Cooper JL, Baingana F, Oquendo MA, Espinel Z, Althouse BM, et al. The role of fear-related behaviors in the 2013–2016 West Africa Ebola virus disease outbreak. Current Psychiatry Reports 2016;18(104):1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Slanger 2016
- Slanger TE, Gross JV, Pinger A, Morfeld P, Bellinger M, Duhme AL, et al. Person-directed, non-pharmacological interventions for sleepiness at work and sleep disturbances caused by shift work. Cochrane Database of Systematic Reviews 2016, Issue 8. Art. No: CD010641. [DOI: 10.1002/14651858.CD010641.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Spokane 2011
- Spokane AR, Inman AG, Weatherford RD, Davidson AK, Straw R. Ecologically based, culturally concordant responding following disasters: the counseling psychologist’s role. Counseling Psychologist 2011;39(8):1128–59. [Google Scholar]
Spoorthy 2020
- Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic-a review. Asian Journal of Psychiatry 2020;51(102119):1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
SQUIRE 2018
- Standards for Quality Improvment Reporting Excellence. www.squire-statement.org/ 2018.
Stanley 2012
- Stanley SA, Bulecza S, Gopalani SV. Psychological impact of disasters on communities. Annual Review of Nursing Research 2012;30:89-123. [DOI] [PubMed] [Google Scholar]
Sterne 2016
- Sterne JA, Hernan MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non- randomised studies of interventions. BMJ 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2020
- Sterne JA, Hernán MA, McAleenan A, Reeves BC, Higgins JP. Chapter 25: Assessing risk of bias in a non-randomized study. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane, 2020. Available from www.training.cochrane.org/handbook.
Strathdee 2015
- Strathdee G. A defining moment in mental health care. www.england.nhs.uk/blog/geraldine-strathdee-8/ 2015.
Stuijfzand 2020
- Stuijfzand S, Deforges C, Sandoz V, Sajin C-T, Jaques C, Elmers J, et al. Psychological impact of an epidemic/pandemic on the mental health of healthcare professionals: a rapid review. BMC Public Health 2020;20:1-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Suijkerbuijk 2017
- Suijkerbuijk YB, Schaafsma FG, Van Mechelen JC, Ojajärvi A, Corbière M, Anema JR. Interventions for obtaining and maintaining employment in adults with severe mental illness, a network meta-analysis. Cochrane Database of Systematic Reviews 2017, Issue 9. Art. No: CD011867. [DOI: 10.1002/14651858.CD011867.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tsamakis 2020
- Tsamakis K, Triantafyllis AS, Tsiptosios D, Spartalis E, Mueller C, Tsamakis C, et al. COVID-19 related stress exacerbates common physical and mental pathologies and affects treatment (Review). Experimental and Therapeutic Medicine 2020;20:159-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Verbeek 2018
- Verbeek L, Ruotsalainen J, Laitinen J, Korkiakangas E, Lusa S, Mänttäri S, et al. Interventions to enhance recovery in healthy workers; a scoping review. Occupational Medicine 2019;69(1):54-63. [DOI] [PubMed] [Google Scholar]
Vogel 2017
- Vogel N, Schandelmaier S, Zumbrunn T, Ebrahim S, De Boer WE, Busse JW, et al. Return-to-work coordination programmes for improving return to work in workers on sick leave. Cochrane Database of Systematic Reviews 2017, Issue 3. Art. No: CD011618. [DOI: 10.1002/14651858.CD011618.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vyas 2016
- Vyas KJ, Delaney EM, Webb-Murphy JA, Johnston SL. Psychological Impact of deploying in support of the US response to Ebola: a systematic review and meta-analysis of past outbreaks. Military Medicine 2016;181(11/12):e1515-e31. [DOI] [PubMed] [Google Scholar]
Walton 2020
- Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. European Heart Journal: Acute Cardiovascular Care 2020;9(3):241-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Weiss 2020
- Weiss PG, Li S-TT. Leading change to address the needs and well-being of trainees during the COVID-19 pandemic. Academic Pediatrics 2020;20(6):735-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2002
- Department of Mental Health and Substance Dependence, World Health Organization. Prevention and promotion in mental health. Available from who.int/mental_health/media/en/545.pdf (accessed 4 June 2020).
WHO 2004
- World Health Organization. Promoting mental health. Concepts, emerging evidence, practice. Summary report. who.int/mental_health/evidence/en/promoting_mhh.pdf (accessed 4 June 2020).
WHO 2014a
- World Health Organization and Calouste Gulbenkian Foundation. Social determinants of mental health. who.int/social_determinants/sdh_definition/en/ (accessed 29 June 2020).
WHO 2018
- World Health Organization and United Nations High Commissioner for Refugees. WHO Mental Health Gap Action Programme (mhGAP). who.int/mental_health/mhgap/en/ 2018.
WHO 2019a
- World Health Organization. Mental health in the workplace. Information sheet. who.int/mental_health/in_the_workplace/en/ (accessed 5 June 2020).
WHO 2019b
- World Health Organization. Burn-out an “occupational phenomenon”: International Classification of Diseases. www.who.int/mental_health/evidence/burn-out/en/ 2019.
WHO 2020a
- World Health Organization. Emergencies. www.who.int/emergencies/diseases/en/ 2020.
WHO 2020c
- Kluge HH. WHO announces COVID-19 outbreak a pandemic. euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic 2020.
Zuercher 2020
- Zürcher SJ, Kerksieck P, Adamus C, Burr C, Lehmann AI, Huber FK, et al. Prevalence of mental health problems during virus epidemics in the general public, health care workers and survivors: a rapid review of the evidence. medRxiv [Preprint] 2020. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Pollock 2020
- Pollock A, Campbell P, Cowie J, Davis B, Elders A, Hagen S, et al. Effective interventions to support the resilience and mental health of frontline health and social care staff during a global health crisis and following de-escalation. (RECOVER: REsilience and mental wellbeing of frontline COVid-19 workers a series of Evidence Reviews). PROSPERO 2020 CRD42020187884. Available from: www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020187884 2020.


