Abstract
The blood–brain barrier (BBB) is a highly selective cellular monolayer unique to the microvasculature of the central nervous system (CNS), and it mediates the communication of the CNS with the rest of the body by regulating the passage of molecules into the CNS microenvironment. Limitation of passage of substances through the BBB is mainly due to tight junctions (TJ) and adherens junctions (AJ) between brain microvascular endothelial cells. The importance of actin filaments and microtubules in establishing and maintaining TJs and AJs has been indicated; however, recent studies have shown that intermediate filaments are also important in the formation and function of cell–cell junctions. The most common intermediate filament protein in endothelial cells is vimentin. Vimentin plays a role in blood–brain barrier permeability in both cell–cell and cell–matrix interactions by affecting the actin and microtubule reorganization and by binding directly to VE-cadherin or integrin proteins. The BBB permeability increases due to the formation of stress fibers and the disruption of VE–cadherin interactions between two neighboring cells in various diseases, disrupting the fiber network of intermediate filament vimentin in different ways. Intermediate filaments may be long ignored key targets in regulation of BBB permeability in health and disease.
Keywords: blood–brain barrier, vimentin, tight junctions, adherens junctions, endothelial permeability
1. Introduction
Specialized endothelial cells covering the inner surfaces of the blood and lymph capillaries as a monolayer act as barriers, separating the blood or lymph fluid from the tissues [1]. The blood–brain barrier (BBB) is an endothelial cell-based, very specialized barrier system, which has great importance in providing brain homeostasis, regulating substance transport from blood to brain, and protecting the brain from pathogens and toxins [2]. The different cell types in the microenvironment of the endothelial cells, the basal lamina and the mechanical stimuli that cells are exposed to due to blood flow and vascular movement affect both the endothelial cell–matrix and the cell–cell interactions [3,4]. Therefore, these external stimuli cause the rearrangement of cytoskeleton proteins, controlling the structure of cellular junctions and the regulation of the endothelial barrier function. Although actin and microtubules are the cytoskeleton proteins whose role in the endothelial barrier function has been studied the most, the role of the intermediate filaments has been recognized only recently. The main purpose of this review is to underline that researchers should not ignore the role of this extensive nanofibrillar network that connects the plasma membrane with the nucleus, while investigating BBB function in health and disease.
2. Blood–Brain Barrier (BBB) Structure and Function
2.1. Brain Vascular Architecture
The primary function of the circulatory system is to provide the nutrients and oxygen required for all tissues and organs of the body, and to remove cellular and metabolic wastes via the bloodstream. Since the central nervous system (CNS) is a specialized and critical system, in which vital functions are managed for the body, it requires an extremely stable microenvironment. For this reason, the structure and the barrier function of the circulatory system in the CNS also differs from that in the periphery, constructing the blood–brain barrier (BBB). BBB maintains ion homeostasis in the brain, prevents the brain from toxic and foreign substances and pathogens in the bloodstream [5,6,7]. The endothelial cells lining the peripheral blood vessels can have wide intercellular spaces, and their basement membranes are not continuous (Figure 1). While mass transport through the peripheral vessels mainly takes place by diffusion via intercellular space, BBB in brain micro vessels directs mass transfer to transcellular, paracellular and enzymatic pathways [8,9,10]. Brain microvascular endothelial cells (BMECs) reduce paracellular permeability by forming a large number of tight junctions (TJ), along with some adherens junctions (AJ) with adjacent BMECs. A continuous basement membrane also reduces transcytosis. Since BMECs have specific transporters, such as hexose transporters, amino acid transporters and monocarboxylic acid transporters, only molecules like glucose, glutamate and lactate that are recognized can pass transcellularly [11,12]. Some special cellular enzymes like acetylcholinesterase, alkaline phosphatase, γ -glutamyl transpeptidase and monoamine oxidases in BMECs were shown to inactivate some drugs, and neurotransmitters pass only transcellularly, which constitutes an enzymatic barrier [13]. Many previous studies on BBB permeability have focused on cell–cell junctions and paracellular permeability. However, to maintain the low permeability characteristic of the BBB, it has been shown that transcytosis must also be at a low rate, and the important effects of this mechanism on the BBB permeability has been demonstrated [14,15]. Ben-Zvi et al. have shown that the Mfds2a (major facilitator superfamily domain containing 2a) membrane protein expressed in CNS endothelium suppresses transcytosis [15]. The essential omega-3 fatty acid docosahexaenoic acid (DHA) transport is carried out by Mfds2a-mediated transport [16]. DHA prevents the formation of functional caveolae domains on the membrane. Thus, the formation of caveolae, which are invaginations of the plasma membrane, is prevented, and caveolae-mediated transcytosis is suppressed [14].
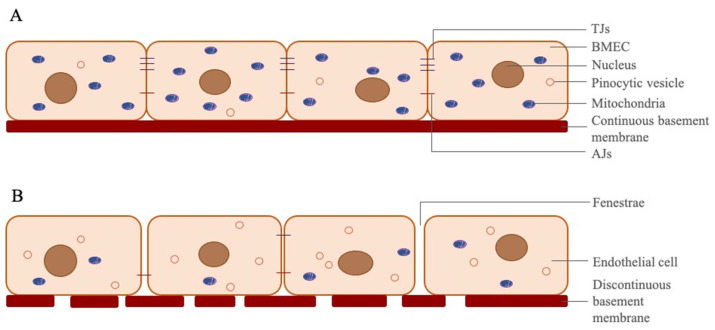
Figure 1.
Differences between BMECs and peripheral endothelial cells. (A) BMECs line along a continuous basement membrane in cerebral capillaries. These cells have tight and adherens junctions to prevent paracellular transition of the molecules in bloodstream. BMECs have 5–6 times more mitochondria than peripheral endothelial cells, due to which transition of the molecules occurs mostly transcellularly in cerebral microvascular capillaries, and BMECs need more ATP than other endothelial cells. They have less pinocytic vesicles than peripheral endothelial cells to reduce transport of unwanted molecules via pinocytosis. (B) Peripheral endothelial cells, which have fenestrae, more pinocytic vesicles and less mitochondria, line along a discontinuous basement membrane in peripheral capillaries. These cells have fewer TJs and AJs, and sometimes have wide intracellular gaps to allow transition of molecules via diffusion.
2.2. BBB Structure
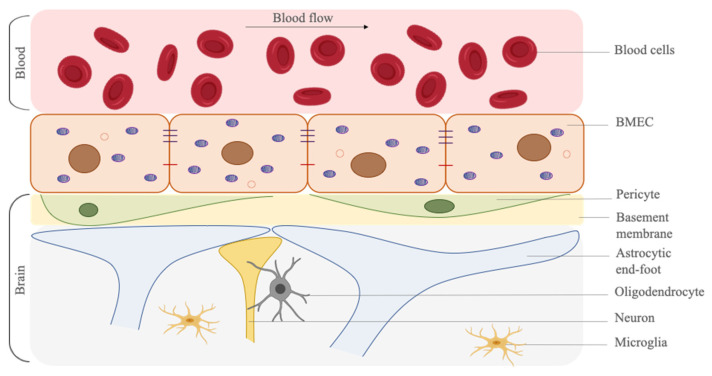
BMECs are specialized cells that limit the movement of substances between the blood and the brain. However, there are also different cell types that support this structure and enhance the barrier function. These supporting cells are perivascular astrocytes, brain microvascular pericytes, oligodendrocytes, neurons and microglia. In addition to the cells, the basal membrane structure is also responsible for supporting the barrier structure and maintaining its functionality [17,18] (Figure 2). Perivascular astrocytes ensheathe the microvascular structure and support the integrity of the BBB. Brain microvascular pericytes directly control the endothelial cell behavior, as well as the vessel shape, by their contractile properties. Moreover, oligodendrocytes, neurons and microglia are also responsible for the BBB function; however, their mechanisms of action on BBB are not well-explained yet.
Figure 2.
Schematic representation of the blood–brain barrier and the supportive cell types on the barrier function. BMECs form the lining of the brain microvasculature and they interact with multiple cells. Brain microvascular pericytes are embedded in the basal membrane and astrocytic end-feet surround brain micro vessels. Neurons, oligodendrocytes and microglia are also found in perivascular space. Created with BioRender.com (accessed on 21 May 2021).
Endothelial cells are found in all vascular structures in the body and line the luminal surface of the vessel. Their main function is to regulate the transmission of molecules in the bloodstream to the surrounding tissues. BMECs are the most important component of the BBB barrier structure. They have many differences (e.g., fewer pinocytotic vesicles and fenestrae, more mitochondria and cell–cell junction proteins) from the peripheral endothelial cells [19,20,21]. All these differences ensure that paracellular and transcellular permeability from BMECs is lower than that of microvascular endothelial cells in the periphery.
BMECs are in constant communication with astrocytic end-feet and pericytes [22]. Pericytes, characterized by α-smooth muscle actin (α-sma), control the diameter of the capillaries by contracting and regulate the blood flow [2,23]. The area of pericytes covering the capillaries is inversely proportional to the capillary permeability [24]. Apart from regulating the capillary diameter and blood flow rate, pericytes also have crucial functions like controlling endothelial cell proliferation, regulating angiogenesis, secretion of extracellular matrix proteins and growth factors and regulating tight junction proteins [25,26].
Astrocytes cover almost the entire vascular surface with their cytoplasmic extensions, called end-foot [24,27]. Growth factors produced from astrocytes have an inducing effect on the barrier characteristics of BMECs [28]. Astrocytes contribute to the physical (by helping the formation of TJ’s), transcellular (by expression of specialized carrier proteins, e.g., P-glycoprotein) and enzymatic (by inducing of specialized enzyme systems, such as γ -glutamyl transpeptidase) barrier structures [29,30].
The basement membrane secreted by BMECs, astrocytes and pericytes is the extracellular matrix (ECM) that is mainly associated with cell surfaces [31]. It supports the cells with its layer-like structure of approximately 100 nm thickness [32]. It holds different cell groups together, regulates the signaling processes between different cells by associating with its ECM proteins (collagen IV, laminin, nidogen and perlecan) and regulates the barrier function by taking place between BMECs and astrocytes [17,31,33].
2.3. Tight and Adherens Junctions
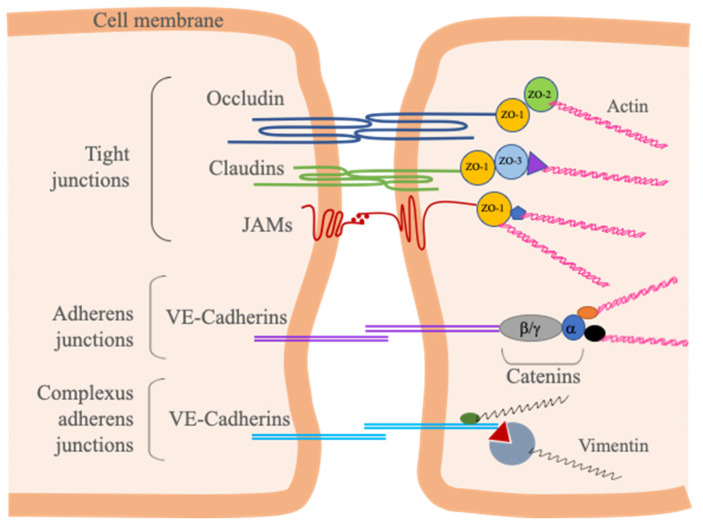
BMECs carry out the regulation of permeability through TJs and AJs. TJs located in the apical end of the lateral side of BMECs can even limit the passage of soluble substances by tightly connecting two neighboring cells like a zipper [34]. Proteins involved in the structure of TJs are divided into two, as transmembrane and cytoplasmic proteins. The transmembrane proteins occludin, claudins and junction adhesion proteins (JAMs) interact with cytoplasmic scaffolding proteins, which are Zonula Occludens 1–2 and 3 (ZO-1/2/3), members of membrane-associated guanylate kinase (MAGUK) protein family, actin cytoskeleton and associated proteins (Figure 3) [35,36,37].
Figure 3.
Major TJ and AJ proteins between adjacent BMECs. Transmembrane TJ proteins (Occludin, Claudins and JAMs) associate and bind to each other across the intercellular cleft. These proteins link to the F-actin cytoskeleton via zonula occludens proteins (ZO-1/2/3) and α-catenin. The most important component of BMEC AJs, VE-Cadherin, binds to the F-actin via catenins (α-catenin, β-catenin, γ-catenin, p120-catenin) and vimentin. VE-Cadherin is also the component of complexus adherens junctions, and links to vimentin by desmosomal plakoglobin/desmoplakin or p0071 linker proteins.
AJs, which are not as tight as TJs, are adhesive structures; however, they also support TJs by connecting adjacent cells to each other [38]. Apart from initiating and stabilizing cell–cell adhesion, AJs have many other functions, such as regulating the actin cytoskeleton, providing cell signaling and transcriptional regulation [39,40]. If the structure of AJs that forms the connections between cadherin superfamily and actin bounded catenin is disrupted, the barrier structure is also disturbed. AJs and TJs have close functional interdependence [35,36,37].
Different than epithelial cells, endothelial cells do not have desmosomes that connect the intermediate filament network of adjacent epithelial cells. Instead, intermediate filaments are linked to AJs in endothelial cells through a complex called complexus adherens (Figure 3) [41]. These desmosome-like complexes link vimentin to VE-cadherin by desmosomal plakoglobin/desmoplakin or p0071 linker proteins [42,43]. Since desmosomes are known to provide junction stability and maintain tissue integrity in other cell types [44], in the lack of desmosomal junctions, it is plausible that AJs take over this duty by connecting intracellular intermediate filament networks through complexus adherens.
3. Endothelial Cytoskeleton
Endothelial cells line the vessel wall that contact with blood and protect the blood vessel and the surrounding tissue against mechanical stimuli originated from blood flow [45]. Besides maintaining the barrier function, these cells have some other roles, such as remaining to attach onto the matrix as a monolayer, maintaining a flat endothelial morphology to prevent turbulent flow, and covering the damaged area by proliferating and migrating rapidly when damage occurs in the vascular structure [46,47]. Endothelial cells need cytoskeletal proteins to perform all these tasks. Like other mammalian cells, the endothelial cell cytoskeleton consists of three filamentous proteins: actin microfilaments, microtubules and intermediate filaments [46,48,49]. These structures are in constant communication with each other directly or indirectly.
3.1. Actin Filaments
The actin protein is found in the endothelial cells in monomer form as globular actin (G-actin), or as filamentous actin (F-actin), which is the polymerized form (7 nm diameter) of G-actin monomers [50]. G- and F-actin are in balance in the cell, and these two types of actin protein react to cellular stimuli by rapidly polymerizing and depolymerizing with the help of actin-binding proteins and actin regulating proteins [51,52]. According to the ratio of G- and F-actin in the cytoskeleton, the cellular functions of actin are regulated. F-actin is involved in cell shape, polarity, cell–cell and cell–matrix interactions, cell migration and cellular transport mechanisms [53,54]. F-actins form membrane cytoskeleton, stress fibers and cortical actin ring (also called cortical actin rim) structures in endothelial cells [48].
Membrane cytoskeleton is a layer approximately 100 nm thick, attached to the cell membrane and is a separate structure from the cortical actin ring consisting of longer F-actin bundles [55]. However, these two structures are in communication with each other. The cortical actin ring structure provides a centrifugal force to the cell, supporting and stabilizing the cell membrane outward [55,56]. Thus, cell–cell and cell–matrix interactions are supported. Membrane cytoskeleton and cortical actin ring join TJ and AJ proteins and structures that form cell–matrix adhesion complexes, providing the formation and protection of the endothelial barrier (Figure 4). The first interaction between neighboring endothelial cells occurs with the help of lamellopodia, filopodia and junction-associated intermittent lamellipodia (JAIL) [53,57]. The space between two neighboring cells is reduced with the help of these cellular protrusions, and the first adhesion complexes are formed by the homophilic interaction between the extracellular amino termini of the VE-cadherins [53,58,59]. The carboxyl termini in the cytosolic part of the VE-cadherins are connected to the actin cytoskeleton via intracellular anchoring molecules, such as p120-catenin, α-catenin, β-catenin and γ-catenin, and actin-binding proteins, such as α-actinin and vinculin, and thus the two cells are interconnected [48,60,61]. There is a reorganization between F-actin that makes up the cortical actin ring and stress fibers. For example, during inflammation, stress fibers increase in endothelial cells with the increase in cytosolic Ca2+, decrease in cAMP, and activation of RhoA/Rho kinase pathway [48,62]. These stress fibers increase intracellular tension and with the reorganization of the adhesion complex structure, gaps occur in the intercellular connections [63]. Cells pull out from each other and barrier permeability increases. Therefore, the cortical actin ring is required for a linear and continuous AJ structure, hence a barrier structure with low permeability.
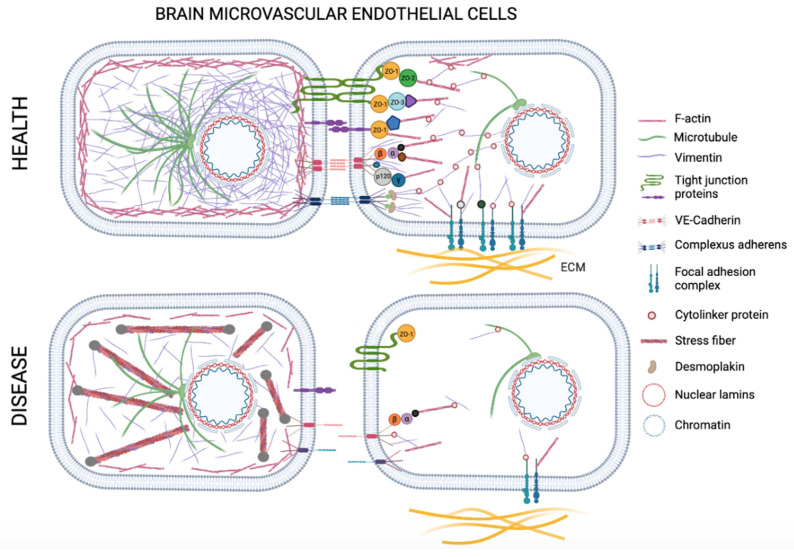
Figure 4.
Schematic representation of the cytoskeleton and the interactions of transmembrane proteins with cytoskeleton proteins and the nucleus in brain microvascular endothelial cells (BMECs) in health and disease. In healthy conditions cortical actin ring supports and stabilizes the cell membrane outward. Cytoskeleton and cortical actin ring join cell–cell and cell–matrix adhesion complexes. Microtubules interact with actin directly or indirectly through intermediate filament proteins or signal molecules. Vimentin intermediate filament provides structural support and mechanical integrity to the cells. Transmembrane tight junction proteins, adherens junction and complexus adherens proteins associate and bind to each other across the intercellular cleft. These proteins link to the cell cytoskeleton directly or via cytolinker proteins. In disease conditions vimentin network is destroyed, the cell loses actin organization, and stress fibers increase in endothelial cells creating higher contractility. The adhesion complex structure reorganizes, and because of the loosening of cell–cell and cell–matrix junctions, gaps occur in the intercellular connections. Cells pull out from each other and barrier permeability increases. Created with BioRender.com (accessed on 21 May 2021).
3.2. Microtubules
Microtubules are 25 nm-diameter fibers consisting of approximately 13 parallel protofilaments composed of alpha and beta-tubulin subunits [64,65,66]. Microtubules are located radially and densely in the center of the cell and their density decreases towards the cell membrane (Figure 4) [67]. Most of the microtubules are attached to the centrosomes; however, non-centrosomal microtubules are also found in the cytosol [68]. Microtubules are involved in many important processes, such as cell migration, spreading, division, polarization, cytoplasmic transport of signal molecules and vesicles and changing the shape of the cell [67,69]. Microtubules are in a constant state of reorganization by polymerizing and depolymerizing rapidly [48]. They interact with actin directly or indirectly through intermediate filament proteins or signal molecules. In the initial phase of endothelial barrier dysfunction, it has recently been observed that microtubules have a higher effect than actin filaments [70]. Depolymerization of microtubules occurs much faster than the reorganization of F-actin when a stress factor is applied to the cell. Even with minimal depolymerization of peripheral microtubules, increased permeability has been shown without actin reorganization or changes in cell morphology [71]. As a result of the depolymerization of microtubules, it has also been shown that the barrier function is impaired by causing stress fiber formation with RhoA activation [48,72].
3.3. Intermediate Filaments
Intermediate filaments (IFs) are the toughest of all three classes of cytoskeleton elements. They provide a template between the plasma membrane and the nucleus with an extensive surface area for cellular organelles and other plasma elements. They are mostly associated with desmosomes and focal adhesions on the plasma membrane, providing mechanical integrity [73]. The role of actin filaments and microtubules on cell–cell interactions and the permeability of the endothelial barrier has been investigated in detail; for a long time, only these structures among the cytoskeleton proteins were thought to be effective on the barrier function. It has been shown that intermediate filaments also have important functions in providing this regulation [74,75,76]. However, still, the role of intermediate filaments has not been studied thoroughly and their effects are not fully elucidated.
Intermediate filaments are tissue-specific, where they show different protein expressions depending on the tissue type or developmental stage. Many IFs were shown to be upregulated in regenerating tissues, and they were shown to have critical roles in the embryonic development [77].
The most abundant intermediate filament protein in microvascular endothelial cells is vimentin [78,79]. Vimentin is a type III intermediate filament protein and is expressed in cells of mesenchymal origin. The vimentin protein can be found in non-filamentous form in the cytoplasm, on the membrane and extracellular site of the cell [79,80,81]. Non-filamentous vimentin is involved in cell–cell interactions, immune activation, homeostasis, tissue repair and relationship with pathogens [79]. Filamentous vimentin is approximately 10 nm in diameter and provides structural support and mechanical integrity to the cells [82,83]. In addition to being responsible for maintaining the shape of the cell, it plays a major role in protecting the vascular cells and tissue against various mechanical factors, such as shear stress or contractile forces [84,85,86]. Lack of vimentin was shown to lead to decreased contractile properties and inhibits the differentiation of embryonic stem cells (ESCs) into endothelial phenotype in vitro. VIM −/− ESCs also showed altered cell–cell interactions and failed to form embryoid bodies [82,83]. Therefore, filamentous vimentin indirectly plays an important role in the formation and regulation of the actin fibers. Vimentins are stable structures that are bound to focal adhesions in cell–matrix interactions by cytoskeleton linker proteins (Figure 4). They increase the resistance of the cells against shear stress by reinforcing the attachment of cells to the matrix [76,87,88]. As vimentin filaments are stretched more, they become more resistant to further deformation due to hierarchical interactions of their coiled-coil subunits. This property is called “strain stiffening” or “strain hardening” [89]. The ability of filamentous vimentin to stretch beyond its original length also prompts its role as an important mechanosensor anchored to focal adhesions, activating the major mechanosensory molecule, focal adhesion kinase (FAK), deforming the nucleus, and transferring the outside mechanical stimuli to the nuclear lamins that are the main form of intermediate filaments within the nucleus [90]. Lamins re-organize the chromatin structure within the nucleus, therefore direct the intracellular transcriptional machinery according to the mechanical stimuli, which is also a phenomenon termed as “mechanoepigenetics” [91]. α-Catenin acts as the main mechanosensor protein in AJs that regulate the cadherin-specific mechanotransduction transmitting the external mechanical information to the nucleus through vimentin network [42,92].
An interesting study by Reinitz et al. has shown that while human umbilical vein endothelial cells (HUVECs) change their morphology and elongate in the direction of physiological shear stress, human brain microvascular endothelial cells (HBMECs) do not show any change in cell morphology or orientation under the same flow conditions [93]. The same group has also shown that HBMECS also resist elongation in response to curvature, as opposed to HUVECs [94]. Their observations suggest that brain microvascular endothelial cells show a unique property of the BBB, where these cells are resistant to actin modeling and elongation under shear and strain to minimize total length of cell–cell junctions. Unfortunately, they did not investigate the vimentin modelling characteristics. Another recent in vitro study that used traction force microscopy to evaluate structural changes in human brain endothelial cells on geometrically defined surfaces has shown that increased cellular traction levels (due to stress fiber generation) are accompanied by increased permeability, whereas when the cortical actin is stabilized, the permeability drops [95]. Since it is well documented that the cytoskeletal organization and cellular shape, as well as the cortical actin structure is particularly maintained by intermediate filaments and their linker proteins that bind to microtubules and microfilaments [77], the unique role of vimentin network for the integrity of BBB becomes more pronounced. Particularly the linker protein plectin has binding domains that can cross-link with all three types of cytoskeleton elements. The non-polar nature of intermediate filaments as opposed to polar microfilaments and microtubules gives them the ability to de-polymerize and re-polymerize allowing routine reassembly of their network [73]. It has been shown that actin filaments re-orient first in response to mechanical strain, followed by microtubules [96]. The slowest response of intermediate filaments might also be pointing out to the stabilization of the whole cytoskeletal adaptation mechanism by intermediate filaments.
Quinlan et al. propose the existence of a separate desmosome–intermediate filament network in epithelial cells that is circumferential and that explains the mechanosensor role of intermediate filaments transducing external stimuli to nucleus through linker of nucleoskeleton and cytoskeleton (LINC) complex [97]. Since endothelial cells lack desmosomes, AJs replace the main mechanosensor role in endothelial cells. Interaction of cadherins with actin through α-catenin is the main actor for sensing of the external mechanical force, while presence of vimentin improves stability and transduction [42].
4. Potential Roles of Intermediate Filaments on BBB Permeability in Disease
It has been shown that, as a result of many pathological conditions (e.g., genetic factors, trauma, infection, neurodegenerative diseases, brain tumor, ischemic/hemorrhagic shock, environmental toxins) junctions between adjacent endothelial cells are affected, and BBB dysfunction develops [98,99]. Specific stressors, such as cytokines (e.g., TNF-α, IL-6) and chemokines (e.g., CCL3, CXCL12) released from damaged cells, free radicals and hypoxic conditions that may occur as a result of ischemia, anemia or brain tumors cause the formation of stress fibers by actin reorganization in endothelial cells [100,101,102,103,104]. With the increased acto-myosin activity in the cell, the cytoskeleton tension increases, and the cells are pulled away from each other as a result of contraction; thus hyperpermeability increases [98]. Many studies have shown that BBB permeability changes as a result of actin reorganization [105,106,107,108,109,110]. It is now known that actin reorganization can occur from disturbances in the organization of the intermediate filament network, as well as directly from structural changes of F-actins and microtubules [111]. In order to create internal tension in the cell, an acto-myosin system and intermediate filament network are required [76]. Besides, in a cell that lacks a healthy intermediate filament network, stress fibers begin to deform with F-actin reorganization because intracellular tension is not sufficiently provided, and a discontinuous AJ structure and BBB dysfunction emerge because cortical actin structure is disrupted [112].
It has been shown that a continuous AJ structure is provided by the binding of the actin-bound VE-cadherins to the network structure of mechanically stable cage-like vimentins via plectins [76]. Gregor et al. indicated that in fibroblasts that do not have plectin cytoskeleton linker protein that binds intermediate filaments to actin, microtubules, organelles and focal adhesions, the intermediate filament network was disrupted and therefore the mechanosensory mechanism in the cell was attenuated [112]. Plectin deficiency was also linked to disruption of AJs and TJs, as well as increased contractility [76]. These studies show that linker proteins are essential for many functions of intermediate filaments that allow the cells respond and adapt to stress. When the intermediate filament network is destroyed, the cell loses tensegrity or actin organization, which will have significant effects on tumor formation, hypertension or delayed wound healing, as well as reduction of BBB integrity. Vimentin is also often related with motility in several cell types, because of its control over cellular contractility. Recently, vimentin was associated with epithelial–mesenchymal transition (EMT), and metastasis in cancer [113,114]. Since cellular motility is not expected in preservation of BBB integrity, stabilization of the vimentin and the whole cytoskeletal network by the linker proteins is necessary in order to avoid barrier disruption.
Changes in cell–cell adhesion are associated with the phosphorylation of adhesion complex members [115]. Vimentin filaments reorganize by phosphorylation, which is a transient posttranslational modification [116,117]. Polymerization and depolymerization of vimentin are essential processes for cell cycle, cell migration, cell spreading and cell signaling. For example, the phosphorylation of vimentin is required to separate cells from each other during the cytokinesis [118]. However, as a result of the disassembly of vimentin, the junctions between cells related to VE-cadherin are weakened (Figure 4) [119]. Due to activation of various protein kinases, such as Protein Kinase A (PKA), Protein Kinase C (PKC), RhoA Kinase (ROCK), the head domain of vimentin is phosphorylated and depolymerization is triggered [120,121,122]. PKC is activated by inflammation mediators, such as bradykinin platelet-activating factor and thrombin, and phorbol esters, leading to disruption in the BBB [119,123,124].
Shear stress induced by fluid flow causes vimentin network to redistribute around the nucleus and the periphery near cell junctions. Tensegrity model explains the distribution of contractile forces and dissipation of energy by intermediate filament structure and the related cross-linking proteins, such as plectins, that connect intermediate filaments with microtubules and microfilaments [125]. Low levels of shear stress have been shown to have protective effects on BBB. It was shown that cerebral endothelial cells form tight junctions and improved barrier function in vitro under shear stress [126], whereas disturbed fluid flow causes BBB breakdown [127]. Our lab’s own experience also has shown that brain vascular endothelial cells show higher levels of TJ (ZO-1 and Claudin-5) and AJ (VE-Cadherin) mRNA expressions under physiological levels of flow induced shear, while there is significant decrease in expression levels of these mRNAs when the flow conditions simulate hypertension (Data not published). Besides hypertension, disturbed fluid flow can be associated to many different pathological conditions including dementia, Alzheimer’s, epilepsy and ischemia [127].
Besides flow induced shear, other forms of mechanical stress also alter BBB permeability. Exposure to repeated low-level blast overpressure, that is commonly experienced in athletes and military personnel was shown to disrupt BBB in a mouse model [128].
In a study showing the role of intermediate filaments in endothelial permeability, it was determined that the organization of the intermediate filaments was disrupted by a drug called Withaferin A (WFA) that is known to cause phosphorylation of vimentin; there was no noticeable change in actin distribution [75]. However, the fact that there was an increase in BBB permeability shows that the phosphorylation of vimentin directly affects the barrier function. In the same study, it was shown that the junctions between endothelial cells were not loosened by the inhibition of phosphorylation of vimentin [75]. Although the cell–cell junctions are not damaged, the increase in BBB permeability may indicate that vimentin influences transcellular permeability as well as paracellular permeability. Apart from that, vimentin affects the expression and organization of surface molecules that are critical for adhesion [129].
In addition to being involved in cell–cell junctions, vimentin is also a component of focal adhesion complexes that provide cell–matrix interactions (Figure 4) [130,131]. In the absence of vimentin, spatial organization of focal adhesions are altered, the resistance of endothelial cells to shear stress decreases and cell–matrix adhesion deteriorates [76,87,88].
It is known that hypoxic conditions, such as in injury, amyotrophic lateral sclerosis (ALS), carbon monoxide poisoning, respiratory arrest, low blood pressure or stroke, change the actin cytoskeleton structure by activation of mitogen-activated protein kinase (MAPK) and Rho Kinase signaling pathways in endothelial cells [74]. Vimentin phosphorylation occurs in rat pulmonary microvascular endothelial cells (RPMECs) exposed to hypoxic conditions, and endothelial cell permeability increases if the intermediate filament network is disrupted [74]. It has been shown in RPMECs that intermediate filaments collapse around the nucleus, redistribute and polymerize in the cell periphery and create a stabilized continuous network in response to hypoxia. Hypoxia also increases the ratio of insoluble/soluble vimentin; vimentin de-phosphorylates, and hypoxia-induced heat shock protein (HSP27) stabilizes the intermediate filament network [74]. Similar vimentin re-organization in brain capillary endothelial cells was also reported [132]. This organization is comparable to the response of vimentin network against shear stress, where the cell–cell junctions are protected against the environmental stressor through establishment of a strong morphological belt in the cellular periphery.
Histamine is a neurotransmitter produced by histaminergic neurons, mast cells and microglia in the brain [133]. It has been shown that histamine is increased during CNS diseases, such as Parkinson’s Disease, schizophrenia, trauma, ischemia and sleep-wake disorders, and is accumulated in different amounts in various parts of the brain [134]. In the study of Shasby et al., histamine increased the phosphorylation of vimentin with the adhesion complexes of AJ, VE-cadherin, β- and γ-catenin; additionally, histamine disrupted the VE-cadherin-vimentin interaction, and therefore obstructed the AJ structure on human umbilical vein endothelial cells (HUVECs) [115]. Consequently, it is thought that cell–cell interactions that are disrupted as a result of the increased phosphorylation of vimentin and AJ complexes during diseases that cause histamine increase may cause BBB dysfunction.
Most of the studies investigating the effects of intermediate filaments on endothelial permeability have been done on intracellular filamentous vimentin. However, it is known that besides the filamentous vimentin in the brain microvascular endothelium, there is also non-filamentous vimentin on the cell surface [135]. Surface vimentin can facilitate internalization of virus and bacteria and infection of cells [81,136,137]. It was shown that the surface vimentin binds to the invasion protein (IbeA) of Escherichia coli K1 and internalin family of surface protein (InlF) of Listeria monocytogenes, both bacteria that are associated with meningitis, indicating the important role of vimentin on invasion of pathogens to the CNS through BBB [137]. Huang et al., indicated that bacterial meningitis has three characteristic properties, NF-κB activation, pathogen invasion and polymorphonuclear neutrophil transmigration (PMNT) across the BBB. In their study, it is shown that vimentin, which is an NF-κB regulator, IbeA induced NF-κB activation, pathogen invasion and PMNT across the BBB, is reduced in vimentin −/− mice [138]. Vimentin deficient mice also showed resistance to Streptococcus agalactiae induced meningitis [139]. Paradoxically, depolymerization of the filamentous vimentin in the case of inflammation can loosen the intercellular junctions and increase BBB permeability, while the surface vimentin may also help infection. Enterovirus A71, which is the cause of foot and mouth disease and encephalitis, was also shown to increase BBB permeability, as well as vimentin expression [140]. It has been shown that in case of an inflammation, vimentins of both brain vascular endothelial cells and lymphocytes reorganize and adhere strongly, and they facilitate the trans-endothelial migration of lymphocytes through BBB [141].
5. Concluding Remarks
Although researchers do not regard the effects of intermediate filaments on cell–cell interactions as much as F-actin and microtubules, studies in this field actually show how effective intermediate filaments are in regulation and integrity of BBB. Intermediate filaments constitute a scaffolding within the cytoskeleton that determines the cellular organization and stabilizes the cell–cell junctions for maintaining the integrity of BBB. As many neurodegenerative diseases, as well as traumatic injuries and infections are associated with disturbed homeostasis and altered hemodynamics within the central nervous system, role of intermediate filament network and the linker proteins to maintain the cell and junction stability is highly pronounced. Particularly, the contribution of intermediate filaments as mechanosensors, and their role in the orchestrated organization of actin cortex and microtubules in reaction to blood flow induced shear must be studied in more detail in vitro and in vivo in order to shed light on their role in BBB functions in health and disease. Use of novel imaging techniques like electron cryotomography, traction force microscopy or Förster resonance energy transfer (FRET) might provide an opportunity to examine the signal transduction pathways in molecular level in the crosstalk of intermediate filaments with the cell–cell junctions and other cytoskeleton/nucleoskeleton molecules. Vimentin-targeted therapeutic strategies might play an important role for controlling and even ameliorating the central nervous system pathologies.
Acknowledgments
The supports of EuroCellNet COST Action CA15214 and The Scientific and Technological Research Council of Turkey (TÜBİTAK) [grant number 216M542] are acknowledged.
Author Contributions
Conceptualization, writing, figure design and drawing E.B.; conceptualization, writing, figure design, and editing A.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yazdani S., Jaldin-Fincati J.R., Pereira R.V., Klip A. Endothelial cell barriers: Transport of molecules between blood and tissues. Traffic. 2019;20:390–403. doi: 10.1111/tra.12645. [DOI] [PubMed] [Google Scholar]
- 2.Daneman R., Prat A. The Blood-Brain Barrier. Cold Spring Harb. Perspect. Biol. 2015;7:a020412. doi: 10.1101/cshperspect.a020412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cucullo L., Hossain M., Puvenna V., Marchi N., Janigro D. The role of shear stress in blood-brain barrier endothelial physiology. BMC Neurosci. 2011;12:40. doi: 10.1186/1471-2202-12-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chow B.W., Gu C. The molecular constituents of the blood-brain barrier. Trends Neurosci. 2015;38:598–608. doi: 10.1016/j.tins.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Misra A., Ganesh S., Shahiwala A., Shah S.P. Drug delivery to the central nervous system: A review. J. Pharm. Pharm. Sci. 2003;6:252–273. [PubMed] [Google Scholar]
- 6.Gawdi R., Emmady P.D. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2020. Physiology, blood brain barrier. [PubMed] [Google Scholar]
- 7.Ayloo S., Gu C. Transcytosis at the blood-brain barrier. Curr. Opin. Neurobiol. 2019;57:32–38. doi: 10.1016/j.conb.2018.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cornford E.M., Hyman S. Blood-Brain barrier permeability to small and large molecules. Adv. Drug Deliv. Rev. 1999;36:145–163. doi: 10.1016/S0169-409X(98)00082-9. [DOI] [PubMed] [Google Scholar]
- 9.Stamatovic S.M., Keep R.F., Andjelkovic A.V. Brain endothelial cell-cell junctions: How to “open” the blood brain barrier. Curr. Neuropharmacol. 2008;6:179–192. doi: 10.2174/157015908785777210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaya M., Ahishali B. Basic physiology of the blood-brain barrier in health and disease: A brief overview. Tissue Barriers. 2021;9:1840913. doi: 10.1080/21688370.2020.1840913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Upadhyay R.K. Transendothelial transport and its role in therapeutics. Int. Sch. Res. Not. 2014;2014:309404. doi: 10.1155/2014/309404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khan N.U., Miao T., Ju X., Guo Q., Han L. 6-Carrier-Mediated transportation through BBB. In: Gao H., Gao X., editors. Brain Targeted Drug Delivery System. Academic Press; Cambridge, MA, USA: 2019. pp. 129–158. [DOI] [Google Scholar]
- 13.Wilhelm I., Fazakas C., Krizbai I.A. In vitro models of the blood-brain barrier. Acta Neurobiol. Exp. 2011;71:113–128. doi: 10.55782/ane-2011-1828. [DOI] [PubMed] [Google Scholar]
- 14.Andreone B.J., Chow B.W., Tata A., Lacoste B., Ben-Zvi A., Bullock K., Deik A.A., Ginty D.D., Clish C.B., Gu C. Blood-brain barrier permeability is regulated by lipid transport-dependent suppression of caveolae-mediated transcytosis. Neuron. 2017;94:581–594. doi: 10.1016/j.neuron.2017.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ben-Zvi A., Lacoste B., Kur E., Andreone B.J., Mayshar Y., Yan H., Gu C. Mfsd2a is critical for the formation and function of the blood–brain barrier. Nature. 2014;509:507–511. doi: 10.1038/nature13324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tjakra M., Wang Y., Vania V., Hou Z., Durkan C., Wang N., Wang G. Overview of crosstalk between multiple factor of transcytosis in blood brain barrier. Front. Neurosci. 2020;13:1436. doi: 10.3389/fnins.2019.01436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xu L., Nirwane A., Yao Y. Basement membrane and blood-brain barrier. Stroke Vasc. Neurol. 2019;4:78–82. doi: 10.1136/svn-2018-000198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bell A.H., Miller S.L., Castillo-Melendez M., Malhotra A. The neurovascular unit: Effects of brain insults during the perinatal period. Front. Neurosci. 2020;13:1452. doi: 10.3389/fnins.2019.01452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hawkins R.A., O’Kane R.L., Simpson I.A., Viña J.R. Structure of the blood-brain barrier and its role in the transport of amino acids. J. Nutr. 2006;136:218S–226S. doi: 10.1093/jn/136.1.218S. [DOI] [PubMed] [Google Scholar]
- 20.Engelhardt B., Sorokin L. The blood-brain and the blood-cerebrospinal fluid barriers: Function and dysfunction. Semin. Immunopathol. 2009;31:497–511. doi: 10.1007/s00281-009-0177-0. [DOI] [PubMed] [Google Scholar]
- 21.Baeten K.M., Akassoglou K. Extracellular matrix and matrix receptors in blood-brain barrier formation and stroke. Dev. Neurobiol. 2011;71:1018–1039. doi: 10.1002/dneu.20954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bertrand L., Cho H.J., Toborek M. Blood-Brain barrier pericytes as a target for HIV-1 infection. Brain. 2019;142:502–511. doi: 10.1093/brain/awy339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu Q., Yang Y., Fan X. Microvascular pericytes in brain-associated vascular disease. Biomed. Pharmacother. 2020;121:109633. doi: 10.1016/j.biopha.2019.109633. [DOI] [PubMed] [Google Scholar]
- 24.Herndon J., Tome M.E., Davis T.P. Primer on Cerebrovascular Diseases. Elsevier; Amsterdam, The Netherlands: 2017. Development and maintenance of the blood-brain barrier; pp. 51–56. [Google Scholar]
- 25.Ribatti D., Nico B., Crivellato E. The role of pericytes in angiogenesis. Int. J. Dev. Biol. 2011;55:261. doi: 10.1387/ijdb.103167dr. [DOI] [PubMed] [Google Scholar]
- 26.Winkler E.A., Bell R.D., Zlokovic B.V. Central nervous system pericytes in health and disease. Nat. Neurosci. 2011;14:1398–1405. doi: 10.1038/nn.2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wong A.D., Ye M., Levy A.F., Rothstein J.D., Bergles D.E., Searson P.C. The blood-brain barrier: An engineering perspective. Front. Neuroeng. 2013;6:7. doi: 10.3389/fneng.2013.00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spampinato S.F., Bortolotto V., Canonico P.L., Sortino M.A., Grilli M. Astrocyte-Derived paracrine signals: Relevance for neurogenic niche regulation and blood-brain barrier integrity. Front. Pharmacol. 2019;10:1346. doi: 10.3389/fphar.2019.01346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Banerjee S., Bhat M.A. Neuron-Glial interactions in blood-brain barrier formation. Annu. Rev. Neurosci. 2007;30:235–258. doi: 10.1146/annurev.neuro.30.051606.094345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mercier C., Masseguin C., Roux F., Gabrion J., Scherrmann J.M. Expression of P-glycoprotein (ABCB1) and Mrp1 (ABCC1) in adult rat brain: Focus on astrocytes. Brain Res. 2004;1021:32–40. doi: 10.1016/j.brainres.2004.06.034. [DOI] [PubMed] [Google Scholar]
- 31.Blanchette M., Daneman R. Formation and maintenance of the BBB. Mech. Dev. 2015;138:8–16. doi: 10.1016/j.mod.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 32.Nag S. The Blood-Brain Barrier: Biology and Research Protocols. Volume 89 Springer Science & Business Media; Berlin/Heidelberg, Germany: 2003. [Google Scholar]
- 33.Thomsen M.S., Routhe L.J., Moos T. The vascular basement membrane in the healthy and pathological brain. J. Cereb. Blood Flow Metab. 2017;37:3300–3317. doi: 10.1177/0271678X17722436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aijaz S., Balda M.S., Matter K. Tight junctions: Molecular architecture and function. Int. Rev. Cytol. 2006;248:261–298. doi: 10.1016/S0074-7696(06)48005-0. [DOI] [PubMed] [Google Scholar]
- 35.Luissint A.-C., Artus C., Glacial F., Ganeshamoorthy K., Couraud P.-O. Tight junctions at the blood brain barrier: Physiological architecture and disease-associated dysregulation. Fluids Barriers CNS. 2012;9:23. doi: 10.1186/2045-8118-9-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Redzic Z. Molecular biology of the blood-brain and the blood-cerebrospinal fluid barriers: Similarities and differences. Fluids Barriers CNS. 2011;8:3. doi: 10.1186/2045-8118-8-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hashimoto Y., Campbell M. Tight junction modulation at the blood-brain barrier: Current and future perspectives. Biochim. Biophys. Acta Biomembr. 2020;1862:183298. doi: 10.1016/j.bbamem.2020.183298. [DOI] [PubMed] [Google Scholar]
- 38.Tariq H., Bella J., Jowitt T.A., Holmes D.F., Rouhi M., Nie Z., Baldock C., Garrod D., Tabernero L. Cadherin flexibility provides a key difference between desmosomes and adherens junctions. Proc. Natl. Acad. Sci. USA. 2015;112:5395–5400. doi: 10.1073/pnas.1420508112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hartsock A., Nelson W.J. Adherens and tight junctions: Structure, function and connections to the actin cytoskeleton. Biochim. Biophys. Acta Biomembr. 2008;1778:660–669. doi: 10.1016/j.bbamem.2007.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abdullahi W., Tripathi D., Ronaldson P.T. Blood-Brain barrier dysfunction in ischemic stroke: Targeting tight junctions and transporters for vascular protection. Am. J. Physiol. Cell Physiol. 2018;315:C343–C356. doi: 10.1152/ajpcell.00095.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wallez Y., Huber P. Endothelial adherens and tight junctions in vascular homeostasis, inflammation and angiogenesis. Biochim. Biophys. Acta Biomembr. 2008;1778:794–809. doi: 10.1016/j.bbamem.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 42.Angulo-Urarte A., van der Wal T., Huveneers S. Cell-Cell junctions as sensors and transducers of mechanical forces. Biochim. Biophys. Acta Biomembr. 2020;1862:183316. doi: 10.1016/j.bbamem.2020.183316. [DOI] [PubMed] [Google Scholar]
- 43.Schmelz M., Franke W. Complexus adhaerentes, a new group of desmoplakin-containing junctions in endothelial cells: The syndesmos connecting retothelial cells of lymph nodes. Eur. J. Cell Biol. 1993;61:274–289. [PubMed] [Google Scholar]
- 44.Hatzfeld M., Keil R., Magin T.M. Desmosomes and intermediate filaments: Their consequences for tissue mechanics. Cold Spring Harb. Perspect. Biol. 2017;9:a029157. doi: 10.1101/cshperspect.a029157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Krüger-Genge A., Blocki A., Franke R.-P., Jung F. Vascular endothelial cell biology: An update. Int. J. Mol. Sci. 2019;20:4411. doi: 10.3390/ijms20184411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Blose S.H. Biology of Endothelial Cells. Springer; Cham, Switzerland: 1984. The endothelial cytoskeleton; pp. 141–154. [Google Scholar]
- 47.Peng Z., Shu B., Zhang Y., Wang M. Endothelial response to pathophysiological stress. Arterioscler. Thromb. Vasc. Biol. 2019;39:e233–e243. doi: 10.1161/ATVBAHA.119.312580. [DOI] [PubMed] [Google Scholar]
- 48.Prasain N., Stevens T. The actin cytoskeleton in endothelial cell phenotypes. Microvasc. Res. 2009;77:53–63. doi: 10.1016/j.mvr.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shahzad K.A., Qin Z.J., Li Y., Xia D.L. The roles of focal adhesion and cytoskeleton systems in fluid shear stress-induced endothelial cell response. Biocell. 2020;44:137–145. doi: 10.32604/biocell.2020.08500. [DOI] [Google Scholar]
- 50.Cooper G.M. The Cell: A Molecular Approach. Volume 2 Sinauer Associates; Sunderland, MA, USA: 2000. Structure and organization of actin filaments. [Google Scholar]
- 51.Lee S.H., Dominguez R. Regulation of actin cytoskeleton dynamics in cells. Mol. Cells. 2010;29:311–325. doi: 10.1007/s10059-010-0053-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang X., Tao T., Song D., Mao H., Liu M., Wang J., Liu X. Calreticulin stabilizes F-actin by acetylating actin and protects microvascular endothelial cells against microwave radiation. Life Sci. 2019;232:116591. doi: 10.1016/j.lfs.2019.116591. [DOI] [PubMed] [Google Scholar]
- 53.Schnittler H., Taha M., Schnittler M.O., Taha A.A., Lindemann N., Seebach J. Actin filament dynamics and endothelial cell junctions: The ying and yang between stabilization and motion. Cell Tissue Res. 2014;355:529–543. doi: 10.1007/s00441-014-1856-2. [DOI] [PubMed] [Google Scholar]
- 54.Rasool S., Geethakumari A.M., Biswas K.H. Role of actin cytoskeleton in E-cadherin-based cell-cell adhesion assembly and maintenance. J. Indian Inst. Sci. 2021;101:51–62. doi: 10.1007/s41745-020-00214-0. [DOI] [Google Scholar]
- 55.Belvitch P., Htwe Y.M., Brown M.E., Dudek S. Current Topics in Membranes. Volume 82. Elsevier; Amsterdam, The Netherlands: 2018. Cortical actin dynamics in endothelial permeability; pp. 141–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chugh P., Paluch E.K. The actin cortex at a glance. J. Cell Sci. 2018;131:jcs186254. doi: 10.1242/jcs.186254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Abu Taha A., Schnittler H.-J. Dynamics between actin and the VE-cadherin/catenin complex: Novel aspects of the ARP2/3 complex in regulation of endothelial junctions. Cell Adhes. Migr. 2014;8:125–135. doi: 10.4161/cam.28243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vestweber D. VE-Cadherin: The major endothelial adhesion molecule controlling cellular junctions and blood vessel formation. Arterioscler. Thromb. Vasc. Biol. 2008;28:223–232. doi: 10.1161/ATVBAHA.107.158014. [DOI] [PubMed] [Google Scholar]
- 59.Cao J., Schnittler H. Putting VE-cadherin into JAIL for junction remodeling. J. Cell Sci. 2019;132:jcs222893. doi: 10.1242/jcs.222893. [DOI] [PubMed] [Google Scholar]
- 60.Bazzoni G., Dejana E. Endothelial cell-to-cell junctions: Molecular organization and role in vascular homeostasis. Physiol. Rev. 2004;84:869–901. doi: 10.1152/physrev.00035.2003. [DOI] [PubMed] [Google Scholar]
- 61.Lee N.P., Mruk D., Lee W.M., Cheng C.Y. Is the cadherin/catenin complex a functional unit of cell-cell actin-based adherens junctions in the rat testis? Biol. Reprod. 2003;68:489–508. doi: 10.1095/biolreprod.102.005793. [DOI] [PubMed] [Google Scholar]
- 62.Karki P., Birukov K.G. Rho and reactive oxygen species at crossroads of endothelial permeability and inflammation. Antioxid. Redox Signal. 2019;31:1009–1022. doi: 10.1089/ars.2019.7798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang W., Zhu L., An C., Wang R., Yang L., Yu W., Li P., Gao Y. The blood brain barrier in cerebral ischemic injury—Disruption and repair. Brain Hemorrhages. 2020;1:34–53. doi: 10.1016/j.hest.2019.12.004. [DOI] [Google Scholar]
- 64.Lee T.Y., Gotlieb A.I. Microfilaments and microtubules maintain endothelial integrity. Microsc. Res. Tech. 2003;60:115–127. doi: 10.1002/jemt.10250. [DOI] [PubMed] [Google Scholar]
- 65.Wade R.H., Hyman A.A. Microtubule structure and dynamics. Curr. Opin. Cell Biol. 1997;9:12–17. doi: 10.1016/S0955-0674(97)80146-9. [DOI] [PubMed] [Google Scholar]
- 66.Janke C., Magiera M.M. The tubulin code and its role in controlling microtubule properties and functions. Nat. Rev. Mol. Cell Biol. 2020;21:307–326. doi: 10.1038/s41580-020-0214-3. [DOI] [PubMed] [Google Scholar]
- 67.Alieva I.B. Role of microtubule cytoskeleton in regulation of endothelial barrier function. Biochemistry. 2014;79:964–975. doi: 10.1134/S0006297914090119. [DOI] [PubMed] [Google Scholar]
- 68.Alieva I.B., Zemskov E.A., Kireev I.I., Gorshkov B.A., Wiseman D.A., Black S.M., Verin A.D. Microtubules growth rate alteration in human endothelial cells. J. Biomed. Biotechnol. 2010;2010:671536. doi: 10.1155/2010/671536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Garcin C., Straube A. Microtubules in cell migration. Essays Biochem. 2019;63:509–520. doi: 10.1042/EBC20190016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shakhov A.S., Verin A.D., Alieva I.B. Reorganization of endothelial cells cytoskeleton during formation of functional monolayer in vitro. Cell Tissue Biol. 2014;8:138–151. doi: 10.1134/S1990519X14020096. [DOI] [Google Scholar]
- 71.Alieva I.B., Zemskov E.A., Smurova K.M., Kaverina I.N., Verin A.D. The leading role of microtubules in endothelial barrier dysfunction: Disassembly of peripheral microtubules leaves behind the cytoskeletal reorganization. J. Cell Biochem. 2013;114:2258–2272. doi: 10.1002/jcb.24575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Weber A., Iturri J., Benitez R., Zemljic-Jokhadar S., Toca-Herrera J.L. Microtubule disruption changes endothelial cell mechanics and adhesion. Sci. Rep. 2019;9:14903. doi: 10.1038/s41598-019-51024-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Godsel L.M., Hobbs R.P., Green K.J. Intermediate filament assembly: Dynamics to disease. Trends Cell Biol. 2008;18:28–37. doi: 10.1016/j.tcb.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 74.Liu T., Guevara O.E., Warburton R.R., Hill N.S., Gaestel M., Kayyali U.S. Regulation of vimentin intermediate filaments in endothelial cells by hypoxia. Am. J. Physiol. Cell Physiol. 2010;299:C363–C373. doi: 10.1152/ajpcell.00057.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Liu T., Ghamloush M.M., Aldawood A., Warburton R., Toksoz D., Hill N.S., Tang D.D., Kayyali U.S. Modulating endothelial barrier function by targeting vimentin phosphorylation. J. Cell. Physiol. 2014;229:1484–1493. doi: 10.1002/jcp.24590. [DOI] [PubMed] [Google Scholar]
- 76.Osmanagic-Myers S., Rus S., Wolfram M., Brunner D., Goldmann W.H., Bonakdar N., Fischer I., Reipert S., Zuzuarregui A., Walko G. Plectin reinforces vascular integrity by mediating crosstalk between the vimentin and the actin networks. J. Cell Sci. 2015;128:4138–4150. doi: 10.1242/jcs.172056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sjöqvist M., Antfolk D., Suarez-Rodriguez F., Sahlgren C. From structural resilience to cell specification—Intermediate filaments as regulators of cell fate. FASEB J. 2021;35:e21182. doi: 10.1096/fj.202001627R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Päll T., Pink A., Kasak L., Turkina M., Anderson W., Valkna A., Kogerman P. Soluble CD44 interacts with intermediate filament protein vimentin on endothelial cell surface. PLoS ONE. 2011;6:e29305. doi: 10.1371/journal.pone.0029305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ramos I., Stamatakis K., Oeste C.L., Pérez-Sala D. Vimentin as a multifaceted player and potential therapeutic target in viral infections. Int. J. Mol. Sci. 2020;21:4675. doi: 10.3390/ijms21134675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Danielsson F., Peterson M.K., Caldeira Araújo H., Lautenschläger F., Gad A.K.B. Vimentin diversity in health and disease. Cells. 2018;7:147. doi: 10.3390/cells7100147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Patteson A.E., Vahabikashi A., Goldman R.D., Janmey P.A. Mechanical and non-mechanical functions of filamentous and non-filamentous vimentin. BioEssays. 2020;42:2000078. doi: 10.1002/bies.202000078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Boraas L.C., Ahsan T. Lack of vimentin impairs endothelial differentiation of embryonic stem cells. Sci. Rep. 2016;6:30814. doi: 10.1038/srep30814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hu J., Li Y., Hao Y., Zheng T., Gupta S.K., Parada G.A., Wu H., Lin S., Wang S., Zhao X., et al. High stretchability, strength, and toughness of living cells enabled by hyperelastic vimentin intermediate filaments. Proc. Natl. Acad. Sci. USA. 2019;116:17175–17180. doi: 10.1073/pnas.1903890116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mendez M.G., Restle D., Janmey P.A. Vimentin enhances cell elastic behavior and protects against compressive stress. Biophys. J. 2014;107:314–323. doi: 10.1016/j.bpj.2014.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dave J.M., Bayless K.J. Vimentin as an integral regulator of cell adhesion and endothelial sprouting. Microcirculation. 2014;21:333–344. doi: 10.1111/micc.12111. [DOI] [PubMed] [Google Scholar]
- 86.Van Engeland N.C.A., Suarez Rodriguez F., Rivero-Müller A., Ristori T., Duran C.L., Stassen O.M.J.A., Antfolk D., Driessen R.C.H., Ruohonen S., Ruohonen S.T., et al. Vimentin regulates notch signaling strength and arterial remodeling in response to hemodynamic stress. Sci. Rep. 2019;9:12415. doi: 10.1038/s41598-019-48218-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bhattacharya R., Gonzalez A.M., DeBiase P.J., Trejo H.E., Goldman R.D., Flitney F.W., Jones J.C. Recruitment of vimentin to the cell surface by β3 integrin and plectin mediates adhesion strength. J. Cell Sci. 2009;122:1390–1400. doi: 10.1242/jcs.043042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tsuruta D., Jones J.C. The vimentin cytoskeleton regulates focal contact size and adhesion of endothelial cells subjected to shear stress. J. Cell Sci. 2003;116:4977–4984. doi: 10.1242/jcs.00823. [DOI] [PubMed] [Google Scholar]
- 89.Goldman R.D., Grin B., Mendez M.G., Kuczmarski E.R. Intermediate filaments: Versatile building blocks of cell structure. Curr. Opin. Cell Biol. 2008;20:28–34. doi: 10.1016/j.ceb.2007.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Terriac E., Schutz S., Lautenschlager F. Vimentin intermediate filament rings deform the nucleus during the first steps of adhesion. Front. Cell Dev. Biol. 2019;7:106. doi: 10.3389/fcell.2019.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Missirlis Y.F. Mechanoepigenetics. Front. Cell Dev. Biol. 2016;4:113. doi: 10.3389/fcell.2016.00113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yonemura S., Wada Y., Watanabe T., Nagafuchi A., Shibata M. α-Catenin as a tension transducer that induces adherens junction development. Nat. Cell Biol. 2010;12:533–542. doi: 10.1038/ncb2055. [DOI] [PubMed] [Google Scholar]
- 93.Reinitz A., DeStefano J., Ye M., Wong A.D., Searson P.C. Human brain microvascular endothelial cells resist elongation due to shear stress. Microvasc. Res. 2015;99:8–18. doi: 10.1016/j.mvr.2015.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ye M., Sanchez H.M., Hultz M., Yang Z., Bogorad M., Wong A.D., Searson P.C. Brain microvascular endothelial cells resist elongation due to curvature and shear stress. Sci. Rep. 2014;4:1–6. doi: 10.1038/srep04681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.O’Connor B.B., Grevesse T., Zimmerman J.F., Ardoña H.A.M., Jimenez J.A., Bitounis D., Demokritou P., Parker K.K. Human brain microvascular endothelial cell pairs model tissue-level blood-brain barrier function. Integr. Biol. 2020;12:64–79. doi: 10.1093/intbio/zyaa005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zielinski A., Linnartz C., Pleschka C., Dreissen G., Springer R., Merkel R., Hoffmann B. Reorientation dynamics and structural interdependencies of actin, microtubules and intermediate filaments upon cyclic stretch application. Cytoskeleton. 2018;75:385–394. doi: 10.1002/cm.21470. [DOI] [PubMed] [Google Scholar]
- 97.Quinlan R.A., Schwarz N., Windoffer R., Richardson C., Hawkins T., Broussard J.A., Green K.J., Leube R.E. A rim-and-spoke hypothesis to explain the biomechanical roles for cytoplasmic intermediate filament networks. J. Cell Sci. 2017;130:3437–3445. doi: 10.1242/jcs.202168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Shi Y., Zhang L., Pu H., Mao L., Hu X., Jiang X., Xu N., Stetler R.A., Zhang F., Liu X. Rapid endothelial cytoskeletal reorganization enables early blood-brain barrier disruption and long-term ischaemic reperfusion brain injury. Nat. Commun. 2016;7:1–18. doi: 10.1038/ncomms10523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Abbott N.J., Friedman A. Overview and introduction: The blood-brain barrier in health and disease. Epilepsia. 2012;53:1–6. doi: 10.1111/j.1528-1167.2012.03696.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Corre I., Paris F., Huot J. The p38 pathway, a major pleiotropic cascade that transduces stress and metastatic signals in endothelial cells. Oncotarget. 2017;8:55684–55714. doi: 10.18632/oncotarget.18264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Mittal M., Siddiqui M.R., Tran K., Reddy S.P., Malik A.B. Reactive oxygen species in inflammation and tissue injury. Antioxid. Redox Signal. 2014;20:1126–1167. doi: 10.1089/ars.2012.5149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zieseniss A. Hypoxia and the modulation of the actin cytoskeleton—Emerging interrelations. Hypoxia. 2014;2:11–21. doi: 10.2147/HP.S53575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Campos S.B., Ashworth S.L., Wean S., Hosford M., Sandoval R.M., Hallett M.A., Atkinson S.J., Molitoris B.A. Cytokine-induced F-actin reorganization in endothelial cells involves RhoA activation. Am. J. Physiol. Ren. Physiol. 2009;296:F487–F495. doi: 10.1152/ajprenal.00112.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Yang C., Hawkins K.E., Doré S., Candelario-Jalil E. Neuroinflammatory mechanisms of blood-brain barrier damage in ischemic stroke. Am. J. Physiol. Cell Physiol. 2019;316:C135–C153. doi: 10.1152/ajpcell.00136.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shakhov A.S., Dugina V.B., Alieva I.B. Structural features of actin cytoskeleton required for endotheliocyte barrier function. Biochemistry. 2019;84:358–369. doi: 10.1134/S0006297919040035. [DOI] [PubMed] [Google Scholar]
- 106.Lai C.-H., Kuo K.-H., Leo J.M. Critical role of actin in modulating BBB permeability. Brain Res. Rev. 2005;50:7–13. doi: 10.1016/j.brainresrev.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 107.Nag S. Role of the endothelial cytoskeleton in blood-brain-barrier permeability to protein. Acta Neuropathol. 1995;90:454–460. doi: 10.1007/BF00294805. [DOI] [PubMed] [Google Scholar]
- 108.Huot J., Houle F., Marceau F., Landry J. Oxidative stress-induced actin reorganization mediated by the p38 mitogen-activated protein kinase/heat shock protein 27 pathway in vascular endothelial cells. Circ. Res. 1997;80:383–392. doi: 10.1161/01.RES.80.3.383. [DOI] [PubMed] [Google Scholar]
- 109.Weiss N., Miller F., Cazaubon S., Couraud P.-O. The blood-brain barrier in brain homeostasis and neurological diseases. Biochim. Biophys. Acta Biomembr. 2009;1788:842–857. doi: 10.1016/j.bbamem.2008.10.022. [DOI] [PubMed] [Google Scholar]
- 110.Kása A., Csortos C., Verin A.D. Cytoskeletal mechanisms regulating vascular endothelial barrier function in response to acute lung injury. Tissue Barriers. 2015;3:e974448. doi: 10.4161/21688370.2014.974448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Jiu Y., Peränen J., Schaible N., Cheng F., Eriksson J.E., Krishnan R., Lappalainen P. Vimentin intermediate filaments control actin stress fiber assembly through GEF-H1 and RhoA. J. Cell Sci. 2017;130:892–902. doi: 10.1242/jcs.196881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Gregor M., Osmanagic-Myers S., Burgstaller G., Wolfram M., Fischer I., Walko G., Resch G.P., Jörgl A., Herrmann H., Wiche G. Mechanosensing through focal adhesion-anchored intermediate filaments. FASEB J. 2014;28:715–729. doi: 10.1096/fj.13-231829. [DOI] [PubMed] [Google Scholar]
- 113.Yamashita N., Tokunaga E., Iimori M., Inoue Y., Tanaka K., Kitao H., Saeki H., Oki E., Maehara Y. Epithelial paradox: Clinical significance of coexpression of E-cadherin and vimentin with regard to invasion and metastasis of breast cancer. Clin. Breast Cancer. 2018;18:e1003–e1009. doi: 10.1016/j.clbc.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 114.Strouhalova K., Přechová M., Gandalovičová A., Brábek J., Gregor M., Rosel D. Vimentin intermediate filaments as potential target for cancer treatment. Cancers. 2020;12:184. doi: 10.3390/cancers12010184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Shasby D.M., Ries D.R., Shasby S.S., Winter M.C. Histamine stimulates phosphorylation of adherens junction proteins and alters their link to vimentin. Am. J. Physiol. Lung Cell. Mol. Physiol. 2002;282:L1330–L1338. doi: 10.1152/ajplung.00329.2001. [DOI] [PubMed] [Google Scholar]
- 116.Battaglia R.A., Delic S., Herrmann H., Snider N.T. Vimentin on the move: New developments in cell migration. F1000Research. 2018;7:1796. doi: 10.12688/f1000research.15967.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Shi A., Tao Z., Li R., Wang Y., Wang X., Zhao J. Vimentin and post-translational modifications in cell motility during cancer-a review. Eur. Rev. Med. Pharm. Sci. 2016;20:2603–2606. [PubMed] [Google Scholar]
- 118.Yasui Y., Goto H., Matsui S., Manser E., Lim L., Nagata K.-I., Inagaki M. Protein kinases required for segregation of vimentin filaments in mitotic process. Oncogene. 2001;20:2868–2876. doi: 10.1038/sj.onc.1204407. [DOI] [PubMed] [Google Scholar]
- 119.Waschke J., Golenhofen N., Kurzchalia T.V., Drenckhahn D. Protein kinase C-mediated endothelial barrier regulation is caveolin-1-dependent. Histochem. Cell Biol. 2006;126:17–26. doi: 10.1007/s00418-005-0140-7. [DOI] [PubMed] [Google Scholar]
- 120.Chen M., Li R., Yin W., Wang T., Kang Y.J. Copper promotes migration of adipose-derived stem cells by enhancing vimentin-Ser39 phosphorylation. Exp. Cell Res. 2020;388:111859. doi: 10.1016/j.yexcr.2020.111859. [DOI] [PubMed] [Google Scholar]
- 121.Sin W.C., Chen X.Q., Leung T., Lim L. RhoA-Binding kinase α translocation is facilitated by the collapse of the vimentin intermediate filament network. Mol. Cell. Biol. 1998;18:6325–6339. doi: 10.1128/MCB.18.11.6325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Eriksson J.E., He T., Trejo-Skalli A.V., Härmälä-Braskén A.S., Hellman J., Chou Y.H., Goldman R.D. Specific in vivo phosphorylation sites determine the assembly dynamics of vimentin intermediate filaments. J. Cell Sci. 2004;117:919–932. doi: 10.1242/jcs.00906. [DOI] [PubMed] [Google Scholar]
- 123.Wu B., McDermott J.S., Krajewski J.L., Knopp K.L., Nisenbaum E.S., Cummins T.R., Tan Z.-Y. Extracellular signal-regulated kinases mediate the enhancing effects of inflammatory mediators on resurgent currents in dorsal root ganglion neurons. Mol. Pain. 2019;15:174480691983710. doi: 10.1177/1744806919837104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Mehta D., Malik A.B. Signaling mechanisms regulating endothelial permeability. Physiol. Rev. 2006;86:279–367. doi: 10.1152/physrev.00012.2005. [DOI] [PubMed] [Google Scholar]
- 125.Wang N., Stamenovic D. Mechanics of vimentin intermediate filaments. J. Muscle Res. Cell Motil. 2002;23:535–540. doi: 10.1023/A:1023470709071. [DOI] [PubMed] [Google Scholar]
- 126.Partyka P.P., Godsey G.A., Galie J.R., Kosciuk M.C., Acharya N.K., Nagele R.G., Galie P.A. Mechanical stress regulates transport in a compliant 3D model of the blood-brain barrier. Biomaterials. 2017;115:30–39. doi: 10.1016/j.biomaterials.2016.11.012. [DOI] [PubMed] [Google Scholar]
- 127.Bouhrira N., DeOre B.J., Sazer D.W., Chiaradia Z., Miller J.S., Galie P.A. Disturbed flow disrupts the blood-brain barrier in a 3D bifurcation model. Biofabrication. 2020;12:025020. doi: 10.1088/1758-5090/ab5898. [DOI] [PubMed] [Google Scholar]
- 128.Heyburn L., Abutarboush R., Goodrich S., Urioste R., Batuure A., Wheel J., Wilder D.M., Arun P., Ahlers S.T., Long J.B. Repeated low-level blast acutely alters brain cytokines, neurovascular proteins, mechanotransduction, and neurodegenerative markers in a rat model. Front. Cell. Neurosci. 2021;15:26. doi: 10.3389/fncel.2021.636707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ivaska J., Pallari H.-M., Nevo J., Eriksson J.E. Novel functions of vimentin in cell adhesion, migration, and signaling. Exp. Cell Res. 2007;313:2050–2062. doi: 10.1016/j.yexcr.2007.03.040. [DOI] [PubMed] [Google Scholar]
- 130.Ostrowska-Podhorodecka Z., Ding I., Lee W., Tanic J., Abbasi S., Arora P.D., Patteson A.E., Janmey P.A., McCulloch C.A. Vimentin tunes cell migration on collagen by controlling β1 integrin activation and clustering. J. Cell Sci. 2021;134:jcs254359. doi: 10.1242/jcs.254359. [DOI] [PubMed] [Google Scholar]
- 131.Leube R.E., Moch M., Windoffer R. Intermediate filaments and the regulation of focal adhesion. Curr. Opin. Cell Biol. 2015;32:13–20. doi: 10.1016/j.ceb.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 132.Kuntz M., Mysiorek C., Pétrault O., Boucau M.-C., Aijjou R., Uzbekov R., Bérézowski V. Transient oxygen-glucose deprivation sensitizes brain capillary endothelial cells to rtPA at 4 h of reoxygenation. Microvasc. Res. 2014;91:44–57. doi: 10.1016/j.mvr.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 133.Rocha S.M., Pires J., Esteves M., Graça B., Bernardino L. Histamine: A new immunomodulatory player in the neuron-glia crosstalk. Front. Cell. Neurosci. 2014;8:120. doi: 10.3389/fncel.2014.00120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Nuutinen S., Panula P. Histamine in Inflammation. Springer; Cham, Switzerland: 2010. Histamine in neurotransmission and brain diseases; pp. 95–107. [DOI] [PubMed] [Google Scholar]
- 135.Xu B., de Waal R.M., Mor-Vaknin N., Hibbard C., Markovitz D.M., Kahn M.L. The endothelial cell-specific antibody PAL-E identifies a secreted form of vimentin in the blood vasculature. Mol. Cell. Biol. 2004;24:9198–9206. doi: 10.1128/MCB.24.20.9198-9206.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Yu Y.T.-C., Chien S.-C., Chen I.Y., Lai C.-T., Tsay Y.-G., Chang S.C., Chang M.-F. Surface vimentin is critical for the cell entry of SARS-CoV. J. Biomed. Sci. 2016;23:14. doi: 10.1186/s12929-016-0234-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Zou Y., He L., Huang S.-H. Identification of a surface protein on human brain microvascular endothelial cells as vimentin interacting with Escherichia coli invasion protein IbeA. Biochem. Biophys. Res. Commun. 2006;351:625–630. doi: 10.1016/j.bbrc.2006.10.091. [DOI] [PubMed] [Google Scholar]
- 138.Huang S.-H., Chi F., Peng L., Bo T., Zhang B., Liu L.-Q., Wu X., Mor-Vaknin N., Markovitz D.M., Cao H. Vimentin, a novel NF-κB regulator, is required for meningitic Escherichia coli K1-induced pathogen invasion and PMN transmigration across the blood-brain barrier. PLoS ONE. 2016;11:e0162641. doi: 10.1371/journal.pone.0162641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Deng L., Spencer B.L., Holmes J.A., Mu R., Rego S., Weston T.A., Hu Y., Sanches G.F., Yoon S., Park N. The group B Streptococcal surface antigen I/II protein, BspC, interacts with host vimentin to promote adherence to brain endothelium and inflammation during the pathogenesis of meningitis. PLoS Pathog. 2019;15:e1007848. doi: 10.1371/journal.ppat.1007848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Wang W., Sun J., Wang N., Sun Z., Ma Q., Li J., Zhang M., Xu J. Enterovirus A71 capsid protein VP1 increases blood-brain barrier permeability and virus receptor vimentin on the brain endothelial cells. J. Neurovirol. 2020;26:84–94. doi: 10.1007/s13365-019-00800-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Nieminen M., Henttinen T., Merinen M., Marttila-Ichihara F., Eriksson J.E., Jalkanen S. Vimentin function in lymphocyte adhesion and transcellular migration. Nat. Cell Biol. 2006;8:156–162. doi: 10.1038/ncb1355. [DOI] [PubMed] [Google Scholar]