Abstract
This cohort study compares the incidence of Bell palsy among patients with COVID-19 and those vaccinated against the disease.
SARS-CoV-2, and its clinical manifestation as COVID-19, is an ongoing global pandemic. Patients with COVID-19 can present with numerous otolaryngologic conditions, such as Bell palsy (BP). Bell palsy is a unilateral peripheral facial nerve palsy of sudden onset. Several case reports and series have described peripheral facial nerve palsies associated with COVID-19.1 In addition, since the US Food and Drug Administration’s (FDA) emergency use authorization of several COVID-19 vaccines, there have been media reports of BP associated with vaccination.2 Such concerns could erode vaccine confidence and exacerbate public hesitancy to obtain a COVID-19 vaccine. We used data from a large health research network to estimate the incidence of BP in patients with COVID-19 vs individuals vaccinated against the disease.
Methods
The institutional review board at Case Western Reserve University deemed this cohort study exempt from review and waived the requirement for patient informed consent because deidentified information, aggregated counts, and statistical summaries of electronic medical records were used. These data were collected from 41 health care organizations worldwide and accessed through TriNetX, a global federated research network. Queries were made on April 7, 2021, to identify patients diagnosed with COVID-19 (January 1, 2020, to December 31, 2020) with or without a diagnosis code of BP within 8 weeks of the COVID-19 diagnosis. Among these patients, we identified those with a history of BP. To account for vaccination, the queries were restricted from January 1, 2021, to March 31, 2021. Using TriNetX to evaluate BP as our outcome, we matched 63 551 non-vaccinated patients with COVID-19 to those who were vaccinated against the disease and had no history of COVID-19 infection.
Results
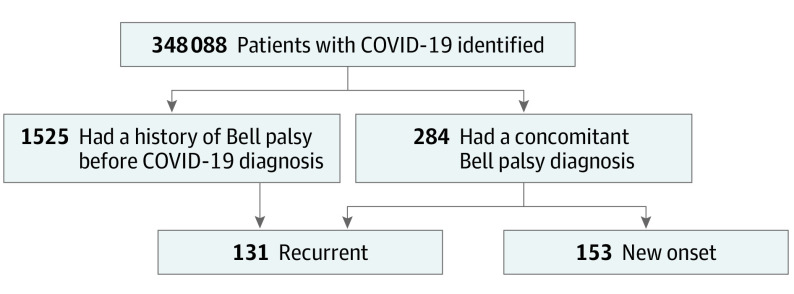
A total of 348 088 patients with COVID-19 were identified in this study. Of these patients, 284 (0.08%) were diagnosed with BP within 8 weeks of the initial COVID-19 diagnosis. One hundred fifty-three of these patients (53.9%) had no history of BP, whereas 131 (46.1%) had a history of BP (Figure). Overall, 1525 patients (0.44%) had a history of BP before receiving the COVID-19 diagnosis, which translates to an 8.6% BP recurrence rate within 8 weeks of COVID-19 diagnosis. After matching patients with COVID-19 to vaccinated individuals (n = 63 551), there was an increased relative risk of 6.8 (95% CI = 3.5-13.2, P < .001) of a diagnosis of BP in those with COVID-19 compared with those who were vaccinated.
Figure. Participant Flow Chart.
Figure shows the study cohort identified using data from TriNetX, a global federated health research network.
Discussion
The annual incidence of BP is 15 to 30 per 100 000 people.3 The recurrence rate in individuals who have had 1 episode of BP is estimated to be 8%. The mechanism of paralysis is thought to be viral, ischemic, and/or immune mediated. The hypothetical mechanism of COVID-19 associated with BP is thought to be molecular mimicry attributable to a neuroimmunologic process between microbial and nerve antigens.4
Two phase 3 COVID-19 vaccine trials consisting of 73 868 participants (36 930 receiving vaccine) reported 8 cases of BP.5,6 Seven cases were in the vaccine groups, which translates to an incidence of 19 per 100 000. The FDA cited insufficient evidence to determine a causal association between COVID-19 vaccinations and BP. This area warrants continued surveillance.
The present analysis found a higher incidence of BP in patients with COVID-19 (0.08%). This translates to approximately 82 per 100 000 patients with COVID-19. The rate of recurrent BP in patients with previous BP at the time of COVID-19 diagnosis was 8.6%. This analysis found a statistically significant higher risk of BP in patients with COVID-19 compared with those who were vaccinated against the disease. The data suggest that rates of BP are higher in patients with COVID-19, and this incidence exceeds the reported incidence of BP in those who have received a COVID-19 vaccine.
This study has limitations, including its retrospective nature and limited period of analysis. Further long-term analysis is necessary to determine the relationship between COVID-19 and the COVID-19 vaccine on BP. We plan to expand on this Research Letter with a more thorough and longer-term analysis.
References
- 1.Goh Y, Beh DLL, Makmur A, Somani J, Chan ACY. Pearls & oy-sters: facial nerve palsy in COVID-19 infection. Neurology. 2020;95(8):364-367. doi: 10.1212/WNL.0000000000009863 [DOI] [PubMed] [Google Scholar]
- 2.Ozonoff A, Nanishi E, Levy O. Bell’s palsy and SARS-CoV-2 vaccines. Lancet Infect Dis. 2021;21(4):450-452. doi: 10.1016/S1473-3099(21)00076-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tiemstra JD, Khatkhate N. Bell’s palsy: diagnosis and management. Am Fam Physician. 2007;76(7):997-1002. [PubMed] [Google Scholar]
- 4.Nepal G, Rehrig JH, Shrestha GS, et al. Neurological manifestations of COVID-19: a systematic review. Crit Care. 2020;24(1):421. doi: 10.1186/s13054-020-03121-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Polack FP, Thomas SJ, Kitchin N, et al. ; C4591001 Clinical Trial Group . Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N Engl J Med. 2020;383(27):2603-2615. doi: 10.1056/NEJMoa2034577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baden LR, El Sahly HM, Essink B, et al. ; COVE Study Group . Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403-416. doi: 10.1056/NEJMoa2035389 [DOI] [PMC free article] [PubMed] [Google Scholar]