Abstract
Elderly women exhibit a high risk of type 2 diabetes (T2D), but no definitive data exist about the possible role of postmenopausal increases in visceral adiposity, the loss of lean body mass, or decreases in the sum of the lean mass of arms and legs (appendicular skeletal muscle mass (ASMM)). This retrospective, longitudinal study investigated whether body composition (bioelectrical impedance analysis) predicted the development of impaired fasting glucose (IFG) or T2D in a cohort of 159 elderly women (age: 71 ± 5 years, follow-up: 94 months) from southern Italy (Clinical Nutrition and Geriatric Units of the “Mater Domini” University Hospital in Catanzaro, Calabria region, and the “P. Giaccone ”University Hospital in Palermo, Sicily region). Sarcopenia was defined in a subgroup of 128 women according to the EWGSOP criteria as the presence of low muscle strength (handgrip strength <16 kg) plus low muscle mass (reported as appendicular skeletal muscle mass <15 kg). Participants with a low ASMM had a higher IFG/T2D incidence than those with a normal ASMM (17% vs. 6%, p-adjusted = 0.044); this finding was independent of BMI, fat mass, waist circumference, and habitual fat intake (OR = 3.81, p = 0.034). A higher incidence of IFG/T2D was observed in the subgroup with sarcopenia than those without sarcopenia (33% vs. 7%, p-adjusted = 0.005) independent of BMI and fat mass (OR = 6.75, p = 0.007). In conclusion, this study demonstrates that elderly women with low ASMM had a higher probability of developing IFG/T2D. Further studies are needed to confirm these results in men and in other age groups.
Keywords: diabetes, aging, nutrition, body composition, sarcopenia, appendicular skeletal muscle mass
1. Introduction
Despite significant advances in diagnosis, monitoring, and treatments, type 2 diabetes (T2D) and its complications remain among the major causes of morbidity and mortality [1,2,3]. The aging of the population is a significant driver of the diabetes epidemic. The rate of T2D is considerably increased in older adults, with a prevalence ranging from 25% to 35% [4]. Older adults with T2D also have the highest rates of complications [5,6], including cardiovascular events, peripheral neuropathy, and disability [7,8]. Furthermore, it is widely recognized that the association between T2D and the onset of its complications differs significantly according to sex; indeed, this association is stronger in diabetic women than in men [9,10,11,12,13,14,15,16,17,18]. In particular, diabetic women could have a marked clustering of cardiovascular risk factors [9,10,11,12,13,14,15,16,17,18].
A biological reason for the increased risk of T2D and its complications in elderly women might be the propensity for insulin resistance (IR) that is driven by increased visceral adiposity in the postmenopausal period [15]. Adiponectin, which is inversely correlated with estradiol in postmenopausal women, seems to be the most interesting molecule released from fat cells with profound protective actions in the pathogenesis of diabetes mellitus [19]. It has been demonstrated that a decreased adiponectin level caused by obesity-induced IR in the adipose tissue leads to decreased insulin sensitivity in the liver and skeletal muscle and, consequently, to IR-related metabolic phenotypes [19]. At the same time, after menopause, adipose tissue represents the primary source of estrogen production in the body through the aromatization of androgens [20]. Aside from the belief that estrogens impair carbohydrate metabolism, circulating estrogens in postmenopausal women are only viewed as biomarkers of the expanded adipose tissue mass and represent biomarkers for the pathological process that predisposes them to T2D [20,21]. However, overall, prospective studies that measured fat mass (FM) [16,17,22] or lean body mass (LBM) [23,24,25] raised doubts about the prevailing role of adiposity in the pathophysiology of T2D. Although it was demonstrated that individuals with diabetes have both higher FM and lower LBM than nondiabetic people [26], the combination of high FM and high LBM is also associated with an elevated risk of developing T2DM [27]. Interestingly, it was observed that elderly individuals with T2D had both low appendicular LBM and low muscle quality [28], which are two characteristic components of sarcopenia in the elderly [29]. Older people have less appendicular skeletal muscle mass (ASMM) than younger individuals [30]. However, studies assessing the predictive capacity of ASMM to identify the incidence of T2D are lacking.
Therefore, the aim of our study was to investigate whether, in addition to obesity and body composition (total fat mass and fat-free mass), ASMM is able to predict the development of prediabetes (impaired fasting glucose) or diabetes in elderly women.
2. Materials and Methods
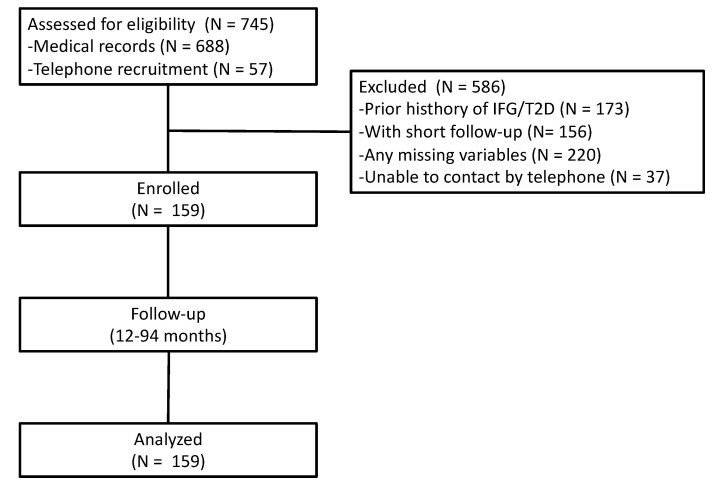
In this multicenter, retrospective cohort study, we selected a population of 745 elderly women (≥65 years) who were consecutive outpatients undergoing health screening tests at the Clinical Nutrition and Geriatric Units of the “Mater Domini” University Hospital in Catanzaro (Italy) and the “P. Giaccone” University Hospital in Palermo (Italy) between October 2012 and April 2021; these patients had at least one follow-up visit. Data that were available from existing databases were obtained for research purposes. Individuals were excluded if they had type 1 or 2 diabetes or had followed a special diet and/or used any dietary supplements in the three months prior to the follow-up visit. All patients included in the study did not suffer from any chronic diseases, such as CKD-EPI stage 2–5 chronic kidney disease, liver cirrhosis, chronic obstructive pulmonary disease, thyroid dysfunction, heart failure ≥NYHA class 2, or any malignant cancer diagnosed in the last 5 years. Additionally, the included patients were not taking anti-obesity, antidiabetics, or psychotropic drugs, according to their medical history, physical examinations, and laboratory tests. Baseline and follow-up clinical characteristics of the population, as well as biochemical parameters, were obtained from their clinical records. Among those initially included, 159 patients completed a full baseline nutritional and biochemical assessment and met all eligibility criteria. Of these patients, 57 completed the enrollment by telephone to confirm their inclusion criteria eligibility (Figure 1).
Figure 1.
Flowchart of the participants in the study. IFG, impaired fasting glucose; T2D, type 2 diabetes.
The study was conducted in accordance with the Declaration of Helsinki and the protocol was approved by the Ethics Committee of the “Mater Domini” University Hospital of Catanzaro, Italy (project identification code no. 23, 21 January 2021) and by the Ethics Committee “Palermo 1” of the Policlinico “P. Giaccone” University Hospital (project identification code no. 3/2015, 11 March 2015). All subjects gave their written informed consent for inclusion before they participated in the study. The data obtained from the cohort of the Palermo center were part of The Nutrition, Cardiovascular Wellness and Diabetes (ABCD_2) project (ISRCTN15840340). This study was a longitudinal observational single-center study of a cohort that was representative of the general population living in Palermo, which is the largest city in Sicily (Italy).
2.1. Diabetes, Impaired Fasting Glucose, and Cardiovascular Risk Factor Assessment
Glucose tolerance was classified according to fasting blood glucose concentrations. In particular, diabetes was diagnosed if the fasting blood glucose concentration was ≥126 mg/dL (7 mmol/L) or antidiabetic treatment was administered; impaired fasting glucose (IFG), a condition of prediabetes, was diagnosed if the fasting blood glucose concentration was in the range of 100–125 mg/dL (5.5–6.9 mmol/L) [31]. Hyperlipidemia was defined as blood concentrations of total cholesterol >200 mg/dL and/or triglycerides >200 mg/dL or the use of lipid-lowering drugs. Hypertension was diagnosed if systolic blood pressure (SBP) was ≥130 mmHg and/or diastolic blood pressure (DBP) ≥85 mmHg or if antihypertensive medications were used. Current smokers who smoked >100 cigarettes in their lifetime and smoke cigarettes every day or some days were considered [32,33].
2.2. Anthropometric and Dietary Intake Assessments
Body weight (BW) and waist and hip circumferences (WC and HC) were obtained from medical records. Body mass index (BMI) was calculated as weight (kg)/height (m)2. Obesity was diagnosed if the BMI was ≥30 kg/m2.
Hand-to-foot bioelectrical impedance analysis (BIA) (BIA-EFG electrofluid graph, Akern srl, Florence, Italy) was performed to estimate the percentage of FM [34], phase angle (pA), and ASMM according to the manufacturer’s equations (Akern, Bodygram Plus software) [14,35]. We considered the following cutoff value for the definition of obesity in women: FM ≥ 35% [36,37]. The ASMM represents the sum of the muscle mass of the arms and legs. According to the European Working Group on Sarcopenia in Older People (EWGSOP), we used a cutoff value for women of 15 kg for diagnosing BIA-derived low ASMM [29].
Sarcopenia was defined as a syndrome that was characterized by progressive and generalized loss of skeletal muscle mass and strength with a risk of adverse outcomes [29]. We used the EWGSOP criteria, which include the presence of low muscle strength (handgrip strength (HGS) <16 kg was defined as low muscle strength) plus low muscle mass reported as ASMM (<15 kg was defined as low ASMM). HGS was measured as previously described [38] using a hydraulic hand dynamometer (Hersteller/manufacturers, SAEHAN Corporation, Masan-Korea).
Dietary intake was assessed via a combination of a validated food frequency questionnaire and a 7-day food record, and it was calculated using the MetaDieta 3.0.1 nutritional software (Metedasrl, San Benedetto del Tronto, Italy) [38,39]. The nutrient database used to calculate the nutrient intake was primarily derived from INRAN (National Institute of Food Research) 2000 and IEO (European Institute of Oncology) 2008.
2.3. Biochemical Evaluation
All laboratory parameters were obtained from medical records. Data relating to blood concentrations of glucose, total cholesterol, high-density lipoprotein (HDL) cholesterol, triglycerides, and creatinine were recorded. Low-density lipoprotein (LDL) cholesterol levels were calculated using Friedewald’s equation [40].
2.4. Statistical Analysis
Data are reported as the means ± standard deviations (SD). For the purposes of this study, a minimum sample size of 150 individuals (Z-statistic) was calculated to find a 10% difference in the incidence of T2D between normal- and low-ASMM groups by considering a cumulative incidence of diabetes in European older adults ranging from 5% to 8% over a 6-year follow-up [41] with 80% power on a two-sided level of significance.
According to the EWGSOP criteria [29,38], we categorized the enrolled population into the following groups: (1) normal ASMM, (2) low ASMM, (3) with sarcopenia, and (4) without sarcopenia. Between-group differences were compared using Student’s unpaired t-test. A Kaplan–Meier estimation of survival curves with Mantel–Cox log-rank univariate analysis was performed to identify any differences in the cumulative risk of developing IFG/T2D between the normal ASMM and low ASMM groups. A multivariate Cox proportional hazard model was used to adjust for potential confounding factors, which were the variables that significantly differed according to the t-test. Categorical variables were analyzed using a Mantel–Haenszel chi-square test to assess the odds ratios. The categorizations of normal ASMM and low ASMM, as well as normal and sarcopenic individuals, were used to construct a two-by-two contingency table. A general linear model (GLM) was used to adjust the prevalence of confounding factors (such as BMI, FM, CV, and dietary fats at baseline). A chi-square test was also used to compare the incidence between the following groups: normal ASMM/high FM, normal ASMM/normal FM, low ASMM/high FM, and low ASMM/normal FM. We then performed a ROC curve to identify the best cut-off of ASMM to detect the onset of IFG/T2D.
All analyses were performed using SPSS 25.0 software for Windows (S. Wacker Drive, Chicago, IL, USA). A two-tailed p-value of <0.05 was considered to be statistically significant.
3. Results
The demographic and clinical characteristics of the participants are presented in Table 1.
Table 1.
Demographic, anthropometric, and clinical characteristics of the cohort.
| Participants (n = 159) |
|
|---|---|
| Age (years) | 71 ± 5 |
| Body weight (kg) | 65.3 ± 11 |
| BMI (kg/m2) | 28 ± 4 |
| Smokers (%) | 8 |
| Physical activity (%) | 52 |
| Hyperlipidemia (%) | 42 |
| Lipid-lowering agents (%) | 24 |
| Hypertension (%) | 65 |
| Antihypertensive agents (%) | 57 |
| Calcium/vitamin D supplementation (%) | 31 |
| BMI-defined obesity (%) | 26 |
| FM-defined obesity (%) | 38 |
| Low ASMM (%) | 45 |
| Sarcopenia * (%) | 9.4 |
| WC (cm) | 92.8 ± 11 |
| HC (cm) | 103.7 ± 10 |
| HGS * (kg) | 19.6 ± 4 |
| SBP (mmHg) | 130 ± 16 |
| DBP (mmHg) | 78 ± 9 |
| Bioimpedance analysis | |
| Rz (Ω) | 554.8 ± 69 |
| Xc (Ω) | 54.0 ± 9 |
| pA (°) | 5.6 ± 0.8 |
| FFM (kg) | 22.1 ± 8.0 |
| FM (%) | 32.9 ± 6.2 |
| ASMM (kg) | 15.4 ± 2.1 |
| Blood concentrations of (mg/dL) | |
| Glucose | 89 ± 8 |
| Creatinine | 0.76 ± 0.2 |
| Total cholesterol | 215 ± 38 |
| HDL cholesterol | 64 ± 16 |
| LDL cholesterol | 131 ± 36 |
| Triglycerides | 106 ± 46 |
Data are given as mean ± SD or prevalence as appropriate. BMI, body mass index; WC, waist circumference; HC, hip circumference; HGS, handgrip strength; SBP, systolic blood pressure; DBP, diastolic blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; Rz, resistance; Xc, reactance; pA, phase angle; FFM, fat-free mass; FM, fat mass; ASMM, appendicular skeletal muscle mass. * Only on 128 participants.
The mean age was 71 ± 5 years. The prevalences of obesity at the baseline were 26% and 38% according to the BMI- and BIA-derived FM% categories, respectively. The prevalence of sarcopenia at the baseline was 9.4% and low ASMM was 45% (Table 1). The characteristics of the population categorized as normal and low ASMM are presented in Table 2.
Table 2.
Characteristics of the cohort that was classified according to appendicular skeletal muscle mass.
| ASMM | p | ||
|---|---|---|---|
| Normal (n = 87) |
Low (n = 72) |
||
| ASMM (range, kg) | 15–22.5 | 10.6–14.9 | |
| Age (years) | 70 ± 4 | 71 ± 6 | 0.36 |
| Body weight (kg) | 71.9 ± 10 | 57.3 ± 6 | <0.001 |
| BMI (kg/m2) | 30.0 ± 4 | 26.0 ± 3 | <0.001 |
| Smokers (%) | 7 | 9 | 0.77 |
| Physical activity (%) | 53 | 51 | 0.86 |
| Hyperlipidemia (%) | 36 | 49 | 0.10 |
| Lipid-lowering agents (%) | 20 | 29 | 0.19 |
| Hypertension (%) | 67 | 64 | 0.74 |
| Antihypertensive agents (%) | 60 | 54 | 0.52 |
| Calcium and vitamin D supplementation (%) | 26 | 36 | 0.30 |
| BMI-defined obesity (%) | 43 | 6 | <0.001 |
| FM-defined obesity (%) | 51 | 22 | <0.001 |
| Sarcopenia * (%) | 0 | 19 | <0.001 |
| WC (cm) | 97.0 ± 12 | 87.6 ± 8 | <0.001 |
| HC (cm) | 107.9 ± 9 | 98.7 ± 8 | <0.001 |
| HGS * (kg) | 20.3 ± 3.9 | 18.8 ± 3.8 | 0.038 |
| SBP (mmHg) | 130 ± 17 | 129 ± 16 | 0.78 |
| DBP (mmHg) | 79 ± 8 | 77 ± 9 | 0.31 |
| Bioimpedance analysis | |||
| Rz (Ω) | 519 ± 58 | 598 ± 57 | <0.001 |
| Xc (Ω) | 53 ± 10 | 56 ± 9 | 0.06 |
| pA (°) | 5.8 ± 0.8 | 5.3 ± 0.7 | <0.001 |
| FM (kg) | 25.6 ± 8.2 | 17.9 ± 4.0 | <0.001 |
| FM (%) | 34.8 ± 6.3 | 30.7 ± 5.1 | <0.001 |
| Blood concentrations of (mg/dL) | |||
| Glucose | 88 ± 8 | 89 ± 7 | 0.54 |
| Creatinine | 0.78 ± 0.2 | 0.73 ± 0.1 | 0.06 |
| Total cholesterol | 217 ± 40 | 212 ± 37 | 0.50 |
| HDL cholesterol | 63 ± 16 | 65 ± 17 | 0.43 |
| LDL cholesterol | 133 ± 38 | 128 ± 35 | 0.38 |
| Triglycerides | 111 ± 52 | 100 ± 38 | 0.11 |
Data are mean ± SD or prevalence. Student’s unpaired t-test or chi-square test as appropriate. ASMM, appendicular skeletal muscle mass; BMI, body mass index; DBP, diastolic blood pressure; FFM, fat-free mass; FM, fat mass; HC, hip circumference; HDL, high-density lipoprotein; HGS, handgrip strength; LDL, low-density lipoprotein; pA, phase angle; Rz, resistance; SBP, systolic blood pressure; WC, waist circumference; Xc, reactance. * Only on 128 participants.
The Cox hazard analysis demonstrated that only low ASMM increased the risk for IFG/T2D (HR 5.30, 95% CI: 1.34–21.04, p < 0.017); BMI, high FM, WC, and the habitual intake of dietary fats were not associated with IFG/T2D onset (Table 3).
Table 3.
Cox proportional hazards models for the risk of impaired fasting glucose/type 2 diabetes.
| Panel A (n = 159) | Multivariate Analysis | |
|---|---|---|
| HR (95% CI) | p | |
| WC | 0.98 (0.91–1.05) | 0.58 |
| BMI | 1.08 (0.84–1.38) | 0.53 |
| High fat mass | 0.94 (0.14–6.43) | 0.95 |
| Low ASMM | 5.30 (1.34–21.04) | 0.017 |
| Fat intake (%) | 1.00 (0.89–1.12) | 0.92 |
| Panel B (n = 128) | Multivariate Analysis | |
| HR (95% CI) | p | |
| BMI | 0.95 (0.80–1.12) | 0.58 |
| High fat mass | 1.70 (0.28–10.07) | 0.55 |
| Sarcopenia | 4.72 (1.38–16.18) | 0.013 |
ASMM, appendicular skeletal muscle mass; BMI, body mass index; CI, confidence interval; HR, hazard ratio; WC, waist circumference.
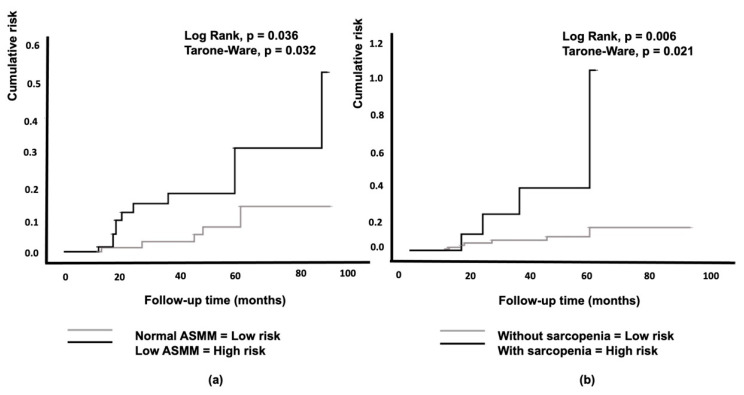
The Kaplan–Meier curves showed that low ASMM was associated with a significantly higher probability of developing IFG/T2D over a period of 94 months compared to normal ASMM conditions (Figure 2a).
Figure 2.
Kaplan–Meier curves for the cumulative risk of impaired fasting glucose/type 2 diabetes according to appendicular skeletal muscle mass (a) and the diagnosis of sarcopenia (b). ASMM, appendicular skeletal muscle mass.
Cox hazard analysis of sarcopenia (ASMM-HGS diagnosed, n = 128 individuals), BMI, and high FM indicated that only sarcopenia was significantly associated with the risk of IFG/T2D (HR 4.72, CI 1.38–16.18, p < 0.013) (Table 3, Figure 2b). Among the obese individuals, the 7-year incidence of diabetes was 8% (data not shown).
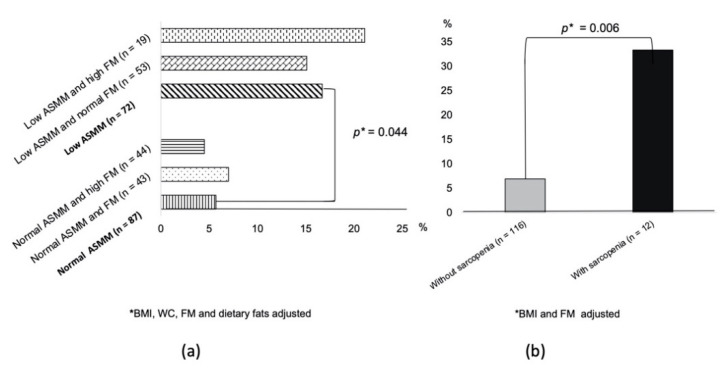
Figure 3a shows that participants with a low ASMM had a higher IFG/T2D incidence than those in the normal ASMM group (17% vs. 6%), which was independent of FM, BMI, WC, and dietary fats (adjusted p = 0.044).
Figure 3.
Incidence of impaired fasting glucose/type 2 diabetes according to appendicular skeletal muscle mass and fat mass categories (a) or the presence of sarcopenia (b).
The OR of low ASMM for IFG/T2D onset was 3.81 (SE 0.55, p = 0.034, CI = 1.09–9.80). In the subgroup with data available on sarcopenia at the baseline (n = 128), elderly women with sarcopenia (Figure 3b) had a higher IFG/T2D incidence than those without sarcopenia (33% vs. 7%, adjusted for BMI and FM p = 0.005). In this subgroup of 128 women, the OR of sarcopenia for IFG/T2D onset was 6.75 (SE 0.71, p = 0.007, CI = 1.66–27.33). Supplemental Table S3 shows the changes in clinical parameters at the follow-up visit. More than 70% of the cohort was weight stable (73% and 83% in normal and low ASMM, respectively, p = 0.24). Figure 3a also shows the prevalence of IFG/T2D according to the different ASMM and FM categories. In particular, analysis using the chi-square test revealed that the final prevalence of IFG/T2D in women with low ASMM was not significantly different between those with high FM and those with normal FM. Furthermore, women with normal ASMM but high FM had the same prevalence of IFG/T2D as women with normal FM. All the clinical characteristics were not significantly different between the four groups according to ANOVA.
The area under the ROC curve for ASMM to predict the onset of IFG/T2D was 0.352 (SE = 0.066, p = 0.04, lower limit 0.224, higher limit 0.481) (figure not shown). An ASMM of 17.1 kg achieved a low sensitivity (10%) but a good specificity (80%) for predicting IFG/T2D.
4. Discussion
Limited research has investigated the impact of muscle mass on the onset of T2D in elderly women; in particular, studies specifically designed to investigate the role of low ASMM in predicting T2D are lacking. In this retrospective study, we observed, for the first time, a significant difference in the incidence of IFG/T2D in a cohort of weight-stable elderly women that were categorized as normal and low ASMM at the baseline using BIA (Figure 3a). In particular, the probability of developing IFG/T2D over a mean follow-up of seven years was higher in women who had a low ASMM than in those with a normal ASMM, independent of the FM size (Figure 2a). Furthermore, women with sarcopenia had a higher probability of developing IFG/T2D than women without sarcopenia (Figure 2b). We found a baseline prevalence of sarcopenia of 9% for the whole study group. This finding is in line with a previous study reporting a prevalence of sarcopenia of 5–13% in 60- to 70-year-old individuals and 11–50% for people aged 80 or older [42]. The issue concerning the role of body composition in influencing the onset of T2D is controversial. Obesity is a key factor, although not the sole factor, in the increasing incidence of diabetes. According to several longitudinal studies, total LBM was positively associated with a high incidence of T2D, but no association remained significant after adjusting for FM [16,17]. In line with these two studies, Hong et al. reported a positive association between FM percentage and the incidence of T2D [22]. Other studies reported a high risk of T2D associated with a high FM size, also after adjusting for LBM [43,44]. The association between muscle indices and incident diabetes in well-functioning older adults living in a community is strongly influenced by their BMI category, especially for women [16]. In fact, in line with our findings, an 11-year follow-up of the Health ABC Study found a 40–60% decrease in the risk of developing T2D among normal-weight women with high muscle mass; however, a high muscle mass was associated with an increased risk of T2D in overweight and obese women [16].
In this study, measures of abdominal and thigh muscle were derived from single-slice CT scans and reported as areas, while total body fat, percentage FM, and total LBM were measured using dual-energy X-ray absorptiometry (DXA) [16]. According to our study, the authors assumed that a low skeletal muscle mass could play a role in the development of “normal-weight metabolic obesity” [16]. Thus, BMI acted as an effect modifier in the association between muscle mass and T2D risk and muscle mass played a crucial role as a preventive factor only in those without excess adiposity. However, it could be assumed that muscle mass is metabolically beneficial for all individuals but, in overweight/obese women, the harmful effects of excess adiposity overpowered the benefits of muscle [16]. However, a greater muscle lipid content was observed to be a characteristic feature of older adults with T2D [45,46]. This means that both intramyocellular lipids and intramuscular adipose tissue deposits can lead to the apparent increase in LBM, and thus explain the positive association between LBM and risk of diabetes in obese women [47].
In supporting the last concept, it was reported that the increased mortality risk for normal-weight patients, compared with overweight patients with T2D, appears to be mediated by their smaller relative muscle size [48]. Furthermore, the Rancho Bernardo Study highlighted that older individuals with sarcopenia have both a reduced LBM and FM compared with individuals without sarcopenia [49]. Considering all the previous studies and our results together, it emerged that if muscle mass was reduced, then normal weight, weight-stable, and sarcopenic subjects were also at risk of diabetes but their risk of diabetes did not depend on FM, as it did for the obese.
Of course, it is well known that CT and MRI are the gold standards for the quantitative estimation of adipose tissue distribution (area) [16]; however, these technologies are costly, have radiation issues, and cannot be routinely available. Therefore, we used a non-invasive and inexpensive method to study the body composition.
In our study, we found a cumulative incidence of IFG/T2D of 11% over 7 years, and it was 8% among obese individuals. This finding is consistent with the 10-year incidence of T2D among Greek women in the ATTICA study [50], as well as the elderly participants in the Hoorn Study [41]. Despite having a high BMI, participants with normal ASMM had a lower incidence of T2D than those with lower BMI but low ASMM. This finding might have been due to the high prevalence of weight-stable individuals, which was more than 70% of the cohort. In fact, a twofold higher risk of T2D was demonstrated in participants whose body weight fluctuated compared with those with stable weight or moderate weight fluctuations over time [51]. Interestingly, overweight/obese but weight-stable elderly women had a lower risk of T2D than overweight/obese women with high body weight variability [52]. Indeed, weight cycling may cause an accumulation of visceral fat that would explain the increased metabolic risk independent of total adiposity [53].
This finding suggests the importance of reducing body weight fluctuations irrespective of the initial BMI in diabetes prevention.
The annual loss of muscle mass was reported to be 1–2% at the age of 50 years onwards [30,54]. By the age of 80, the average muscle loss is approximately 40% of the peak muscle mass that is usually attained at the age of 20 [55]. Older women have been reported to be more sedentary and less active than older men [56]. Since women have a longer life expectancy than men, this fact could imply that sarcopenia represents a greater health concern for women. Additionally, controversies exist about a more adequate way of considering LBM. Relative (percentage of body weight) versus absolute (kg) measures of LBM may have discordant relationships with the development of diabetes, as observed in the Baltimore Longitudinal Study of Aging [23], which included participants of both sexes that were much younger than those of our study. In fact, it was demonstrated that people in the highest quartile of percentage of LBM had the lowest probability of developing T2D; however, the opposite association was observed when the LBM was considered in absolute value. Our study focused on ASMM in elderly women, who are known to exhibit a higher prevalence of sarcopenia [55,57]. This condition could be linked with their low absolute muscle mass; they demonstrated 40% less upper body and 30% less lower body muscle mass than men [55]. Risk factors for the difference in muscle mass between gender are not well defined [58]. Gender differences in hormones are potential factors [58]. In general, older women have more disabilities than older men [58]. It is quite difficult to discriminate between the effects of aging and menopause, as both take place at the same time. With the menopausal transition, the decrease in estrogen seems to be related to an increase in oxidative stress and a decrease in insulin sensitivity, circulating IGF-1, DHEA, GH, and vitamin D, which are all related in some ways to the loss of muscle mass in women [59]. All these previous findings agree with our results demonstrating an important role of ASMM in predicting IGF/T2D in elderly women. As skeletal muscle is responsible for the majority of postprandial glucose disposal in the body, dysfunction of this part of the body might result in substantial whole-body metabolic disorders [60]. Physical inactivity, which is a common feature of aging, is associated with a decline in mitochondrial oxidative function in muscle [61]. This decline involves a reduced capacity to oxidize fatty acids, leading to insulin resistance (IR) and diabetes [62]. The REPOSI study [63], which is a collaborative study involving a network of hospitals in the European Union, demonstrated that women had a worse functional status than men, which could be related to the older age of women than men in that cohort, and it could also be the effect of a possible link between both depression and cognitive impairment and daily living activities [63].
Myostatin and adiponectin play important roles in skeletal muscle function by regulating insulin signaling and energy metabolism [64]. Myostatin is a member of the transforming growth factor beta superfamily and is an autocrine/paracrine inhibitor of skeletal muscle growth and development [65]. Myostatin is increased in sarcopenia [65] and plays a role in diabetic muscle atrophy [66,67]. Adiponectin is secreted mainly from the adipose tissue and has anti-atherogenic and anti-inflammatory actions [68,69]. Serum adiponectin levels increased with aging, and a high adiponectin concentration in the elderly is associated with a low muscle mass and strength [68]. It is not known whether it increases compensatively or due to low FM. Indeed patients with obesity have low serum adiponectin levels [69]. These previous studies could suggest that the skeletal muscle and adipose tissue may crosstalk to control glucose homeostasis. However, it is possible that changes in LBM represent both a risk factor and a consequence of impaired glucose tolerance.
Our study is of relevance considering that the relationship between hyperglycemia and cardiovascular disease (CVD) is a continuum. In the Rotterdam Study [70], among elderly participants with normal blood glucose and without diabetes, people with higher blood glucose levels also had higher arterial stiffness. Additionally, several studies demonstrated that elevated fasting glucose was associated with CVD and mortality in individuals without diabetes [2,71,72,73,74,75,76]. However, in our population, the increase in CV risk could have occurred due to other mechanisms and despite the good control of dyslipidemia using lipid-lowering agents (Table 2). Indeed the population studied was mostly hypertensive (more than 60%, Table 2). This leads to a progressive reduction in the glomerular filtration rate and loss of renal function over time. [77]. These individuals have lifelong exposure to cardiovascular risk [77].
Although the prevalence of sarcopenia increases with age, this condition is potentially reversible. In fact, previous studies showed that physical activity had a positive effect on muscle mass and function in elderly individuals [78,79]. Furthermore, protein intake was associated with a low risk of sarcopenia [60,80,81]. As previously reported [16], overweight/obese older individuals would likely benefit more from losing excess adiposity than building muscle mass, while normal-weight people would likely benefit more from maintenance or building muscle. Thus, increasing physical activity and protein intake could represent an important strategy for the treatment of individuals with a particular phenotype (i.e., sarcopenic, normal-weight individuals with glucose tolerance abnormalities). Thus, performing a BIA assessment would represent a new way to personalize the treatment, at least in the elderly. However, only intervention studies can confirm this hypothesis, which remains speculative.
This study has some limitations. Although evidence clarifying the role of estrogens on muscle mass in elderly women is lacking, it is possible to assume that the different roles of androgens and estrogens contribute to the sex disparity in skeletal muscle morphology and function [82]. Furthermore, adiponectin, which is inversely correlated with estradiol levels, seems to be the most important molecule released from fat cells potentially preventing diabetes in pre- and post-menopausal women [19,83].
However, investigating these effects was not among the objectives of the study and we did not assess their serum levels.
Additionally, we did not include men; therefore, we left some gaps in our understanding of the role of ASMM in diabetes onset. The REPOSI study [63] showed that men were more impaired than women in terms of cumulative illness burden with respect to severity and comorbidity and, in that study, fasting glucose level was higher in men than in women. Future research should include elderly men to improve our knowledge about the link between ASMM and T2D.
Furthermore, due to the lack of some HGS measurements, we assessed the presence of sarcopenia only in a subgroup of the cohort. However, our study encourages more research in the field of sarcopenia to definitively confirm its role in the development of glucose abnormalities. Finally, a greater muscle lipid content was observed to be a characteristic feature of older adults with T2D [45,46], and thus, based on our results, we cannot provide a definitive answer on the role of adipose tissue in predicting the development of T2D.
This study also has some points of strength. By dividing participants into body composition categories, we reduced confounding factors between fat and lean mass indices. It has been suggested that LBM may have a discordant relationship with the development of diabetes [23]. Consequently, we focused on the objective of considering a standardized measure of ASMM. Another strength of the current study includes the availability of a large cohort of women with comprehensive clinical follow-up; thus, undetected T2D cases are less likely to have occurred.
5. Conclusions
In this retrospective study, for the first time, we observed a greater probability of glucose abnormalities in elderly women with low ASMM or sarcopenia than women with normal ASMM. However, further studies are needed to address whether ASMM loss in older individuals, as well as in other age groups and in males, may lead to the development of type 2 diabetes.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/nu13061909/s1. Table S1: Dietary intake assessment of the cohort classified according to appendicular skeletal muscle mass, Table S2: Changes in anthropometric parameters and blood glucose at follow-up according to the diagnosis of IFG/T2D, Table S3: Changes in clinical parameters at follow-up of the cohort classified according to appendicular skeletal muscle mass.
Author Contributions
Conceptualization, C.B., Y.F., R.P., and T.M.; methodology, Y.F., R.P., E.M., and G.B.; formal analysis, A.P. and T.M.; investigation, C.B., Y.F., R.P., and G.B.; writing—original draft preparation, C.B., Y.F., R.P., E.M., and G.B.; writing—review and editing, C.B., S.P., A.P., G.S., S.B., and T.M.; data curation, C.B., Y.F., R.P., G.B., A.S., S.B., and T.M.; supervision, S.B. and T.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Ethics Committee of the “Mater Domini” University Hospital (protocol code number 23 and 21/01/2021) and the “Palermo 1” of the Policlinico “Paolo Giaccone” University Hospital (protocol code numbers 3/2015 and 11/03/2015).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kannel W.B., McGee D.L. Diabetes and Cardiovascular Disease. The Framingham Study. J. Am. Med. Assoc. 1979;241:2035–2038. doi: 10.1001/jama.1979.03290450033020. [DOI] [PubMed] [Google Scholar]
- 2.Barr E.L.M., Zimmet P.Z., Welborn T.A., Jolley D., Magliano D.J., Dunstan D.W., Cameron A.J., Dwyer T., Taylor H.R., Tonkin A.M., et al. Risk of Cardiovascular and All-Cause Mortality in Individuals with Diabetes Mellitus, Impaired Fasting Glucose, and Impaired Glucose Tolerance: The Australian Diabetes, Obesity, and Lifestyle Study (AusDiab) Circulation. 2007;116:151–157. doi: 10.1161/CIRCULATIONAHA.106.685628. [DOI] [PubMed] [Google Scholar]
- 3.Aronson D., Edelman E.R. Coronary Artery Disease and Diabetes Mellitus. Cardiol. Clin. 2014;32:439–455. doi: 10.1016/j.ccl.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cowie C.C., Rust K.F., Ford E.S., Eberhardt M.S., Byrd-Holt D.D., Li C., Williams D.E., Gregg E.W., Bainbridge K.E., Saydah S.H., et al. Full Accounting of Diabetes and Pre-Diabetes in the U.S. Population in 1988–1994 and 2005–2006. Diabetes Care. 2009;32:287–294. doi: 10.2337/dc08-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Y., Burrows N.R., Gregg E.W., Albright A., Geiss L.S. Declining Rates of Hospitalization for Nontraumatic Lower-Extremity Amputation in the Diabetic Population Aged 40 Years or Older: U.S., 1988–2008. Diabetes Care. 2012;35:273–277. doi: 10.2337/dc11-1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirkman M.S., Briscoe V.J., Clark N., Florez H., Haas L.B., Halter J.B., Huang E.S., Korytkowski M.T., Munshi M.N., Odegard P.S., et al. Diabetes in Older Adults. Diabetes Care. 2012;35:2650–2664. doi: 10.2337/dc12-1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Menz H.B., Lord S.R., St George R., Fitzpatrick R.C. Walking Stability and Sensorimotor Function in Older People with Diabetic Peripheral Neuropathy. Arch. Phys. Med. Rehabil. 2004;85:245–252. doi: 10.1016/j.apmr.2003.06.015. [DOI] [PubMed] [Google Scholar]
- 8.Volpato S., Blaum C., Resnick H., Ferrucci L., Fried L.P., Guralnik J.M. Women’s Health and Aging Study Comorbidities and Impairments Explaining the Association between Diabetes and Lower Extremity Disability: The Women’s Health and Aging Study. Diabetes Care. 2002;25:678–683. doi: 10.2337/diacare.25.4.678. [DOI] [PubMed] [Google Scholar]
- 9.Huxley R., Barzi F., Woodward M. Excess Risk of Fatal Coronary Heart Disease Associated with Diabetes in Men and Women: Meta-Analysis of 37 Prospective Cohort Studies. Br. Med. J. 2006;332:73–78. doi: 10.1136/bmj.38678.389583.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yusuf S., Hawken S., Ôunpuu S., Dans T., Avezum A., Lanas F., McQueen M., Budaj A., Pais P., Varigos J., et al. Effect of Potentially Modifiable Risk Factors Associated with Myocardial Infarction in 52 Countries (the INTERHEART Study): Case-Control Study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 11.Haffner S.M., Miettinen H., Stern M.P. Relatively More Atherogenic Coronary Heart Disease Risk Factors in Prediabetic Women than in Prediabetic Men. Diabetologia. 1997;40:711–717. doi: 10.1007/s001250050738. [DOI] [PubMed] [Google Scholar]
- 12.Juutilainen A., Kortelainen S., Lehto S., Rönnemaa T., Pyörälä K., Laakso M. Gender Difference in the Impact of Type 2 Diabetes on Coronary Heart Disease Risk. Diabetes Care. 2004;27:2898–2904. doi: 10.2337/diacare.27.12.2898. [DOI] [PubMed] [Google Scholar]
- 13.Gentile M., Iannuzzo G., Mattiello A., Rubba F., Panico S., Rubba P. Association between Body Shape Index and Small Dense LDL Particles in a Cohort of Mediterranean Women: Findings from Progetto ATENA. J. Clin. Biochem. Nutr. 2017;61:130–134. doi: 10.3164/jcbn.17-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gentile M., Iannuzzo G., Mattiello A., Marotta G., Iannuzzi A., Panico S., Rubba P. Association between Lp (a) and Atherosclerosis in Menopausal Women without Metabolic Syndrome. Biomark. Med. 2016;10:397–402. doi: 10.2217/bmm.16.4. [DOI] [PubMed] [Google Scholar]
- 15.Mauvais-Jarvis F., Clegg D.J., Hevener A.L. The Role of Estrogens in Control of Energy Balance and Glucose Homeostasis. Endocr. Rev. 2013;34:309–338. doi: 10.1210/er.2012-1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Larsen B.A., Wassel C.L., Kritchevsky S.B., Strotmeyer E.S., Criqui M.H., Kanaya A.M., Fried L.F., Schwartz A.V., Harris T.B., Ix J.H., et al. Association of Muscle Mass, Area, and Strength with Incident Diabetes in Older Adults: The Health ABC Study. J. Clin. Endocrinol. Metab. 2016;101:1847–1855. doi: 10.1210/jc.2015-3643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baker C.F., Overvad K., Dahm C.C. Lean Body Mass and Risk of Type 2 Diabetes—A Danish Cohort Study. J. Diabetes Metab. Disord. 2019;18:445–451. doi: 10.1007/s40200-019-00438-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Succurro E., Fiorentino T.V., Miceli S., Perticone M., Sciacqua A., Andreozzi F., Sesti G. Relative Risk of Cardiovascular Disease Is Higher in Women with Type 2 Diabetes, but Not in Those with Prediabetes, as Compared with Men. Diabetes Care. 2020;43:3070–3078. doi: 10.2337/dc20-1401. [DOI] [PubMed] [Google Scholar]
- 19.Mankowska A., Nowak L., Sypniewska G. Adiponectin and Metabolic Syndrome in Women at Menopause. EJIFCC. 2009;19:173–184. [PMC free article] [PubMed] [Google Scholar]
- 20.Bhardwaj P., Au C.C., Benito-Martin A., Ladumor H., Oshchepkova S., Moges R., Brown K.A. Estrogens and breast cancer: Mechanisms involved in obesity-related development, growth and progression. J. Steroid Biochem. Mol. Biol. 2019;189:161–170. doi: 10.1016/j.jsbmb.2019.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mauvais-Jarvis F. Is Estradiol a Biomarker of Type 2 Diabetes Risk in Postmenopausal Women? Diabetes. 2017;66:568–570. doi: 10.2337/dbi16-0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park B.S., Yoon J.S. Relative Skeletal Muscle Mass Is Associated with Development of Metabolic Syndrome. Diabetes Metab. J. 2013;37:458–464. doi: 10.4093/dmj.2013.37.6.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kalyani R.R., Metter E.J., Xue Q.-L., Egan J.M., Chia C.W., Studenski S., Shaffer N.C., Golden S., Al-Sofiani M., Florez H., et al. The Relationship of Lean Body Mass with Aging to the Development of Diabetes. J. Endocr. Soc. 2020;4:bvaa043. doi: 10.1210/jendso/bvaa043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hong S., Chang Y., Jung H.-S., Yun K.E., Shin H., Ryu S. Relative Muscle Mass and the Risk of Incident Type 2 Diabetes: A Cohort Study. PLoS ONE. 2017;12:e0188650. doi: 10.1371/journal.pone.0188650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maliszewska K., Adamska-Patruno E., Goscik J., Lipinska D., Citko A., Krahel A., Miniewska K., Fiedorczuk J., Moroz M., Gorska M., et al. The Role of Muscle Decline in Type 2 Diabetes Development: A 5-Year Prospective Observational Cohort Study. Nutrients. 2019;11:834. doi: 10.3390/nu11040834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heshka S., Ruggiero A., Bray G.A., Foreyt J., Kahn S.E., Lewis C.E., Saad M., Schwartz A.V. Look AHEAD Research Group Altered Body Composition in Type 2 Diabetes Mellitus. Int. J. Obes. 2008;32:780–787. doi: 10.1038/sj.ijo.0803802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rehunen S.K.J., Kautiainen H., Korhonen P.E., Eriksson J.G. A High Lean Body Mass Is Not Protecting from Type 2 Diabetes in the Presence of a High Body Fat Mass. Diabetes Metab. 2021;47:101219. doi: 10.1016/j.diabet.2020.101219. [DOI] [PubMed] [Google Scholar]
- 28.Kalyani R.R., Corriere M., Ferrucci L. Age-Related and Disease-Related Muscle Loss: The Effect of Diabetes, Obesity, and Other Diseases. Lancet Diabetes Endocrinol. 2014;2:819–829. doi: 10.1016/S2213-8587(14)70034-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cruz-Jentoft A.J., Bahat G., Bauer J., Boirie Y., Bruyère O., Cederholm T., Cooper C., Landi F., Rolland Y., Sayer A.A., et al. Sarcopenia: Revised European Consensus on Definition and Diagnosis. Age Ageing. 2019;48:16–31. doi: 10.1093/ageing/afy169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gallagher D., Visser M., De Meersman R.E., Sepúlveda D., Baumgartner R.N., Pierson R.N., Harris T., Heymsfield S.B. Appendicular Skeletal Muscle Mass: Effects of Age, Gender, and Ethnicity. J. Appl. Physiol. 1997;83:229–239. doi: 10.1152/jappl.1997.83.1.229. [DOI] [PubMed] [Google Scholar]
- 31.Association A.D. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2013;36:S67–S74. doi: 10.2337/dc13-S067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention (CDC) Use of Cessation Methods among Smokers Aged 16–24 Years—United States, 2003. MMWR Morb. Mortal. Wkly. Rep. 2006;55:1351–1354. [PubMed] [Google Scholar]
- 33.Psaty B.M., Furberg C.D., Kuller L.H., Bild D.E., Rautaharju P.M., Polak J.F., Bovill E., Gottdiener J.S. Traditional Risk Factors and Subclinical Disease Measures as Predictors of First Myocardial Infarction in Older Adults: The Cardiovascular Health Study. Arch. Intern. Med. 1999;159:1339–1347. doi: 10.1001/archinte.159.12.1339. [DOI] [PubMed] [Google Scholar]
- 34.Pujia A., Mazza E., Ferro Y., Gazzaruso C., Coppola A., Doldo P., Grembiale R.D., Pujia R., Romeo S., Montalcini T. Lipid Oxidation Assessed by Indirect Calorimetry Predicts Metabolic Syndrome and Type 2 Diabetes. Front. Endocrinol. 2019;9:806. doi: 10.3389/fendo.2018.00806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sergi G., De Rui M., Veronese N., Bolzetta F., Berton L., Carraro S., Bano G., Coin A., Manzato E., Perissinotto E. Assessing Appendicular Skeletal Muscle Mass with Bioelectrical Impedance Analysis in Free-Living Caucasian Older Adults. Clin. Nutr. 2015;34:667–673. doi: 10.1016/j.clnu.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 36.Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee. World Health Organ. Tech. Rep. Ser. 1995;854:1–452. [PubMed] [Google Scholar]
- 37.Donini L.M., Poggiogalle E., Del Balzo V., Lubrano C., Faliva M., Opizzi A., Perna S., Pinto A., Rondanelli M. How to Estimate Fat Mass in Overweight and Obese Subjects. Int. J. Endocrinol. 2013:285680. doi: 10.1155/2013/285680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Montalcini T., De Bonis D., Ferro Y., Carè I., Mazza E., Accattato F., Greco M., Foti D., Romeo S., Gulletta E., et al. High Vegetable Fats Intake Is Associated with High Resting Energy Expenditure in Vegetarians. Nutrients. 2015;7:5933–5947. doi: 10.3390/nu7075259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Buscemi S., Rosafio G., Vasto S., Massenti F.M., Grosso G., Galvano F., Rini N., Barile A.M., Maniaci V., Cosentino L., et al. Validation of a Food Frequency Questionnaire for Use in Italian Adults Living in Sicily. Int. J. Food Sci. Nutr. 2015;66:426–438. doi: 10.3109/09637486.2015.1025718. [DOI] [PubMed] [Google Scholar]
- 40.Friedewald W.T., Levy R.I., Fredrickson D.S. Estimation of the Concentration of Low-Density Lipoprotein Cholesterol in Plasma, without Use of the Preparative Ultracentrifuge. Clin. Chem. 1972;18:499–502. doi: 10.1093/clinchem/18.6.499. [DOI] [PubMed] [Google Scholar]
- 41.de Vegt F., Dekker J.M., Jager A., Hienkens E., Kostense P.J., Stehouwer C.D., Nijpels G., Bouter L.M., Heine R.J. Relation of Impaired Fasting and Postload Glucose with Incident Type 2 Diabetes in a Dutch Population: The Hoorn Study. J. Am. Med. Assoc. 2001;285:2109–2113. doi: 10.1001/jama.285.16.2109. [DOI] [PubMed] [Google Scholar]
- 42.von Haehling S., Morley J.E., Anker S.D. An Overview of Sarcopenia: Facts and Numbers on Prevalence and Clinical Impact. J. Cachexia Sarcopenia Muscle. 2010;1:129–133. doi: 10.1007/s13539-010-0014-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Garg S.K., Maurer H., Reed K., Selagamsetty R. Diabetes and Cancer: Two Diseases with Obesity as a Common Risk Factor. Diabetes Obes. Metab. 2014;16:97–110. doi: 10.1111/dom.12124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bellou V., Belbasis L., Tzoulaki I., Evangelou E. Risk Factors for Type 2 Diabetes Mellitus: An Exposure-Wide Umbrella Review of Meta-Analyses. PLoS ONE. 2018;13:e0194127. doi: 10.1371/journal.pone.0194127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Goodpaster B.H., Krishnaswami S., Resnick H., Kelley D.E., Haggerty C., Harris T.B., Schwartz A.V., Kritchevsky S., Newman A.B. Association Between Regional Adipose Tissue Distribution and Both Type 2 Diabetes and Impaired Glucose Tolerance in Elderly Men and Women. Diabetes Care. 2003;26:372–379. doi: 10.2337/diacare.26.2.372. [DOI] [PubMed] [Google Scholar]
- 46.Marcus R.L., Addison O., Dibble L.E., Foreman K.B., Morrell G., Lastayo P. Intramuscular Adipose Tissue, Sarcopenia, and Mobility Function in Older Individuals. J. Aging Res. 2012:629637. doi: 10.1155/2012/629637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Scott D., de Courten B., Ebeling P.R. Sarcopenia: A Potential Cause and Consequence of Type 2 Diabetes in Australia’s Ageing Population? Med. J. Aust. 2016;205:329–333. doi: 10.5694/mja16.00446. [DOI] [PubMed] [Google Scholar]
- 48.Murphy R.A., Reinders I., Garcia M.E., Eiriksdottir G., Launer L.J., Benediktsson R., Gudnason V., Jonsson P.V., Harris T.B. Age, Gene/Environment Susceptibility-Reykjavik Study (AGES-Reykjavik) Adipose Tissue, Muscle, and Function: Potential Mediators of Associations between Body Weight and Mortality in Older Adults with Type 2 Diabetes. Diabetes Care. 2014;37:3213–3219. doi: 10.2337/dc14-0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Castillo E.M., Goodman-Gruen D., Kritz-Silverstein D., Morton D.J., Wingard D.L., Barrett-Connor E. Sarcopenia in Elderly Men and Women: The Rancho Bernardo Study. Am. J. Prev. Med. 2003;25:226–231. doi: 10.1016/S0749-3797(03)00197-1. [DOI] [PubMed] [Google Scholar]
- 50.Koloverou E., Panagiotakos D.B., Pitsavos C., Chrysohoou C., Georgousopoulou E.N., Pitaraki E., Metaxa V., Stefanadis C. ATTICA Study Group 10-Year Incidence of Diabetes and Associated Risk Factors in Greece: The ATTICA Study (2002–2012) Rev. Diabet. Stud. 2014;11:181–189. doi: 10.1900/RDS.2014.11.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kataja-Tuomola M., Sundell J., Männistö S., Virtanen M.J., Kontto J., Albanes D., Virtamo J. Short-Term Weight Change and Fluctuation as Risk Factors for Type 2 Diabetes in Finnish Male Smokers. Eur. J. Epidemiol. 2010;25:333–339. doi: 10.1007/s10654-010-9444-6. [DOI] [PubMed] [Google Scholar]
- 52.French S.A., Folsom A.R., Jeffery R.W., Zheng W., Mink P.J., Baxter J.E. Weight Variability and Incident Disease in Older Women: The Iowa Women’s Health Study. Int. J. Obes. Relat. Metab. Disord. 1997;21:217–223. doi: 10.1038/sj.ijo.0800390. [DOI] [PubMed] [Google Scholar]
- 53.Wallner S.J., Luschnigg N., Schnedl W.J., Lahousen T., Sudi K., Crailsheim K., Möller R., Tafeit E., Horejsi R. Body fat distribution of overweight females with a history of weight cycling. Int. J. Obes. 2004;28:1143–1148. doi: 10.1038/sj.ijo.0802736. [DOI] [PubMed] [Google Scholar]
- 54.Hughes V.A., Frontera W.R., Roubenoff R., Evans W.J., Singh M.A.F. Longitudinal Changes in Body Composition in Older Men and Women: Role of Body Weight Change and Physical Activity. Am. J. Clin. Nutr. 2002;76:473–481. doi: 10.1093/ajcn/76.2.473. [DOI] [PubMed] [Google Scholar]
- 55.Janssen I., Heymsfield S.B., Wang Z.M., Ross R. Skeletal Muscle Mass and Distribution in 468 Men and Women Aged 18–88 Yr. J. Appl. Physiol. 2000;89:81–88. doi: 10.1152/jappl.2000.89.1.81. [DOI] [PubMed] [Google Scholar]
- 56.Lee Y.-S. Gender Differences in Physical Activity and Walking among Older Adults. J. Women Aging. 2005;17:55–70. doi: 10.1300/J074v17n01_05. [DOI] [PubMed] [Google Scholar]
- 57.Goodpaster B.H., Park S.W., Harris T.B., Kritchevsky S.B., Nevitt M., Schwartz A.V., Simonsick E.M., Tylavsky F.A., Visser M., Newman A.B. The Loss of Skeletal Muscle Strength, Mass, and Quality in Older Adults: The Health, Aging and Body Composition Study. J. Gerontol. A Biol. Sci. Med. Sci. 2006;61:1059–1064. doi: 10.1093/gerona/61.10.1059. [DOI] [PubMed] [Google Scholar]
- 58.Newman A.B., Brach J.S. Gender Gap in Longevity and Disability in Older Persons. Epidemiol. Rev. 2001;23:343–350. doi: 10.1093/oxfordjournals.epirev.a000810. [DOI] [PubMed] [Google Scholar]
- 59.Maltais M.L., Desroches J., Dionne I.J. Changes in muscle mass and strength after menopause. J. Musculoskelet Neuronal Interact. 2009;9:186–197. [PubMed] [Google Scholar]
- 60.Montalcini T., Pujia A., Donini L.M., Frittitta L., Galvano F., Natali A., Pironi L., Porrini M., Riso P., Rivellese A.A., et al. A Call to Action: Now Is the Time to Screen Elderly and Treat Osteosarcopenia, a Position Paper of the Italian College of Academic Nutritionists MED/49 (ICAN-49) Nutrients. 2020;12:2662. doi: 10.3390/nu12092662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rimbert V., Boirie Y., Bedu M., Hocquette J.-F., Ritz P., Morio B. Muscle Fat Oxidative Capacity Is Not Impaired by Age but by Physical Inactivity: Association with Insulin Sensitivity. FASEB J. 2004;18:737–739. doi: 10.1096/fj.03-1104fje. [DOI] [PubMed] [Google Scholar]
- 62.McPherron A.C., Lawler A.M., Lee S.J. Regulation of Skeletal Muscle Mass in Mice by a New TGF-Beta Superfamily Member. Nature. 1997;387:83–90. doi: 10.1038/387083a0. [DOI] [PubMed] [Google Scholar]
- 63.Corrao S., Santalucia P., Argano C., Djade C.D., Barone E., Tettamanti M., Pasina L., Franchi C., Eldin T.K., Marengoni A., et al. Gender-differences in disease distribution and outcome in hospitalized elderly: Data from the REPOSI study. Eur. J. Intern. Med. 2014;25:617–623. doi: 10.1016/j.ejim.2014.06.027. [DOI] [PubMed] [Google Scholar]
- 64.Kurose S., Onishi K., Takao N., Miyauchi T., Takahashi K., Kimura Y. Association of serum adiponectin and myostatin levels with skeletal muscle in patients with obesity: A cross-sectional study. PLoS ONE. 2021;16:e0245678. doi: 10.1371/journal.pone.0245678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Léger B., Derave W., De Bock K., Hespel P., Russell A.P. Human Sarcopenia Reveals an Increase in SOCS-3 and Myostatin and a Reduced Efficiency of Akt Phosphorylation. Rejuvenation Res. 2008;11:163B–175B. doi: 10.1089/rej.2007.0588. [DOI] [PubMed] [Google Scholar]
- 66.Allen D.L., Cleary A.S., Speaker K.J., Lindsay S.F., Uyenishi J., Reed J.M., Madden M.C., Mehan R.S. Myostatin, Activin Receptor IIb, and Follistatin-like-3 Gene Expression Are Altered in Adipose Tissue and Skeletal Muscle of Obese Mice. Am. J. Physiol. Endocrinol. Metab. 2008;294:E918–E927. doi: 10.1152/ajpendo.00798.2007. [DOI] [PubMed] [Google Scholar]
- 67.Hittel D.S., Berggren J.R., Shearer J., Boyle K., Houmard J.A. Increased Secretion and Expression of Myostatin in Skeletal Muscle from Extremely Obese Women. Diabetes. 2009;58:30–38. doi: 10.2337/db08-0943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Huang C., Tomata Y., Kakizaki M., Sugawara Y., Hozawa A., Momma H., Tsuji I., Nagatomi R. High circulating adiponectin levels predict decreased muscle strength among older adults aged 70 years and over: A prospective cohort study. Nutr. Metab. Cardiovasc. Dis. 2015;25:594–601. doi: 10.1016/j.numecd.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 69.Rajala M.W., Scherer P.E. Minireview: The adipocyte—At the crossroads of energy homeostasis, inflammation, and atherosclerosis. Endocrinology. 2003;144:3765–3773. doi: 10.1210/en.2003-0580. [DOI] [PubMed] [Google Scholar]
- 70.van Popele N.M., Elizabeth Hak A., Mattace-Raso F.U.S., Bots M.L., van der Kuip D.A.M., Reneman R.S., Hoeks A.P.G., Hofman A., Grobbee D.E., Witteman J.C.M. Impaired Fasting Glucose Is Associated with Increased Arterial Stiffness in Elderly People without Diabetes Mellitus: The Rotterdam Study. J. Am. Geriatr. Soc. 2006;54:397–404. doi: 10.1111/j.1532-5415.2005.00614.x. [DOI] [PubMed] [Google Scholar]
- 71.Coutinho M., Gerstein H.C., Wang Y., Yusuf S. The Relationship between Glucose and Incident Cardiovascular Events. A Metaregression Analysis of Published Data from 20 Studies of 95,783 Individuals Followed for 12.4 Years. Diabetes Care. 1999;22:233–240. doi: 10.2337/diacare.22.2.233. [DOI] [PubMed] [Google Scholar]
- 72.Levitan E.B., Song Y., Ford E.S., Liu S. Is Nondiabetic Hyperglycemia a Risk Factor for Cardiovascular Disease? A Meta-Analysis of Prospective Studies. Arch. Intern. Med. 2004;164:2147–2155. doi: 10.1001/archinte.164.19.2147. [DOI] [PubMed] [Google Scholar]
- 73.Emerging Risk Factors Collaboration. Sarwar N., Gao P., Seshasai S.R.K., Gobin R., Kaptoge S., Di Angelantonio E., Ingelsson E., Lawlor D.A., Selvin E., et al. Diabetes Mellitus, Fasting Blood Glucose Concentration, and Risk of Vascular Disease: A Collaborative Me-ta-Analysis of 102 Prospective Studies. Lancet. 2010;375:2215–2222. doi: 10.1016/S0140-6736(10)60484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lee G., Kim S.M., Choi S., Kim K., Jeong S.-M., Son J.S., Yun J.-M., Park S.M. The Effect of Change in Fasting Glucose on the Risk of Myocardial Infarction, Stroke, and All-Cause Mortality: A Nationwide Cohort Study. Cardiovasc. Diabetol. 2018;17:51. doi: 10.1186/s12933-018-0694-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jin C., Chen S., Vaidya A., Wu Y., Wu Z., Hu F.B., Kris-Etherton P., Wu S., Gao X. Longitudinal Change in Fasting Blood Glucose and Myocardial Infarction Risk in a Population without Diabetes. Diabetes Care. 2017;40:1565–1572. doi: 10.2337/dc17-0610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Piconi L., Quagliaro L., Da Ros R., Assaloni R., Giugliano D., Esposito K., Szabó C., Ceriello A. Intermittent High Glucose Enhances ICAM-1, VCAM-1, E-Selectin and Interleukin-6 Expression in Human Umbilical Endothelial Cells in Culture: The Role of Poly(ADP-Ribose) Polymerase. J. Thromb. Haemost. 2004;2:1453–1459. doi: 10.1111/j.1538-7836.2004.00835.x. [DOI] [PubMed] [Google Scholar]
- 77.Minutolo R., Gabbai F.B., Provenzano M., Chiodini P., Borrelli S., Garofalo C., Sasso F.C., Santoro D., Bellizzi V., Conte G., et al. Cardiorenal prognosis by residual proteinuria level in diabetic chronic kidney disease: Pooled analysis of four cohort studies. Nephrol. Dial. Transplant. 2018;33:1942–1949. doi: 10.1093/ndt/gfy032. [DOI] [PubMed] [Google Scholar]
- 78.Beaudart C., Dawson A., Shaw S.C., Harvey N.C., Kanis J.A., Binkley N., Reginster J.Y., Chapurlat R., Chan D.C., Bruyère O., et al. Nutrition and Physical Activity in the Prevention and Treatment of Sarcopenia: Systematic Review. Osteoporos. Int. 2017;28:1817–1833. doi: 10.1007/s00198-017-3980-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bosaeus I., Rothenberg E. Nutrition and Physical Activity for the Prevention and Treatment of Age-Related Sarcopenia. Proc. Nutr. Soc. 2016;75:174–180. doi: 10.1017/S002966511500422X. [DOI] [PubMed] [Google Scholar]
- 80.Silva T.R., Spritzer P.M. Skeletal Muscle Mass Is Associated with Higher Dietary Protein Intake and Lower Body Fat in Postmenopausal Women: A Cross-Sectional Study. Menopause. 2017;24:502–509. doi: 10.1097/GME.0000000000000793. [DOI] [PubMed] [Google Scholar]
- 81.Ten Haaf D.S.M., Eijsvogels T.M.H., Bongers C.C.W.G., Horstman A.M.H., Timmers S., de Groot L.C.P.G.M., Hopman M.T.E. Protein Supplementation Improves Lean Body Mass in Physically Active Older Adults: A Randomized Placebo-Controlled Trial. J. Cachexia Sarcopenia Muscle. 2019;10:298–310. doi: 10.1002/jcsm.12394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Almeida M., Laurent M.R., Dubois V., Claessens F., O’Brien C.A., Bouillon R., Vanderschueren D., Manolagas S.C. Estrogens and Androgens in Skeletal Physiology and Pathophysiology. Physiol. Rev. 2017;97:135–187. doi: 10.1152/physrev.00033.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ahn S.V., Jung D.H., Yadav D., Kim J.Y., Koh S.B. Relative contribution of obesity and menopause to the association between serum adiponectin and incident metabolic syndrome. Menopause. 2018;25:154–159. doi: 10.1097/GME.0000000000000960. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author.