Abstract
The COVID-19 pandemic is a worldwide, critical public health challenge and is considered one of the most communicable diseases that the world had faced so far. Response and symptoms associated with COVID-19 vary between the different cases recorded, but it is amply described that symptoms become more aggressive in subjects with a weaker immune system. This includes older subjects, patients with chronic diseases, patients with immunosuppression treatment, and pregnant women. Pregnant women are receiving more attention not only because of their altered physiological and immunological function but also for the potential risk of viral vertical transmission to the fetus or infant. However, very limited data about the impact of maternal infection during pregnancy, such as the possibility of vertical transmission in utero, during birth, or via breastfeeding, is available. Moreover, the impact of infection on the newborn in the short and long term remains poorly understood. Therefore, it is vital to collect and analyze data from pregnant women infected with COVID-19 to understand the viral pathophysiology during pregnancy and its effects on the offspring. In this article, we review the current knowledge about pre-and post-natal COVID-19 infection, and we discuss whether vertical transmission takes place in pregnant women infected with the virus and what are the current recommendations that pregnant women should follow in order to be protected from the virus.
Keywords: SARS-CoV-2, coronavirus, pregnancy outcomes, ACE-2 receptor, immune response, placental antibody transfer
1. Introduction
Pregnancy is an important and “formative period” governed by series of interconnected molecular and cellular mechanisms aimed to promote maternal homeostasis and maintain an optimal fetal-placental interaction while supporting fetal growth [1,2]. Despite being tightly regulated, many factors/events can disrupt this balance and lead to adverse pregnancy outcomes [3,4,5], which may result in failing the pregnancy and in few cases of maternal death [3,4] As per the UNICEF (United Nation United Nations International Children’s Emergency Fund), one pregnant woman or newborn dies every 11 s worldwide [6]. This great risk on pregnant women and babies’ health increases dramatically during pandemics [7].
Pregnant women are considered one of the most susceptible groups in a population, as changes during pregnancy, such as decreased functional residual capacity as well as changes in cellular immunity, can increase the risk of serious illness in response to viral infections and the risk of vertical transmission [8]. Vertical transmission is defined as the possibility of transmission from a mother to her fetus during the antepartum and intrapartum periods or to the neonate during the postpartum period, and it can occur via the placenta, body fluid contact during childbirth, or through direct contact owing to breastfeeding after birth 9. During pregnancy, the placenta acts as a barrier set to avoid transmission of infectious pathogens from the mother to her fetus; however, some infectious agents can cross the placental barrier, leading, in some cases, to congenital infections [9,10].
SARS-CoV-2 is an evolving coronavirus that was declared a pandemic on 11 March 2020 by the World Health Organization [11]. Coronaviruses are enveloped, non-segmented, positive-sense RNA viruses belonging to the family Coronaviridae [12]. A qRT-PCR using a nasopharyngeal swab is proposed as the best form of COVID-19 screening and diagnosis, although findings can be impacted by the sampling process, viral load, and other technical challenges [13]. With about 89,048,345 confirmed cases and 1,930,265 deaths reported by the WHO at the time of writing this review, this virus is easily and quickly spreading in the community [11]. After the first nine months since the COVID-19 pandemic started, a total of 116 million births were registered, and around 57,786 pregnant women in the USA alone were infected with the virus, while 71 lost their lives [14,15]. Unfortunately, many countries have reported a second wave of COVID-19 [16,17,18] with higher frequency of pregnant and post-partum women being infected in the second wave compared to the first one [19]. With the increase in the availability of COVID-19 testing in the developed countries, it has become possible to test more subjects, which has led to an increase in the detection rates of positive cases [20]. More recently, the world has faced new COVID-19 variants that are more transmissible due to mutations on the spike protein 21. The B.1.1.7 variant and B.1.351 variant originated in the United Kingdom and South Africa, respectively [21]. Both strains are considered more contagious and can cause severe disease (up to 30 percent) compared to the first strain [21].
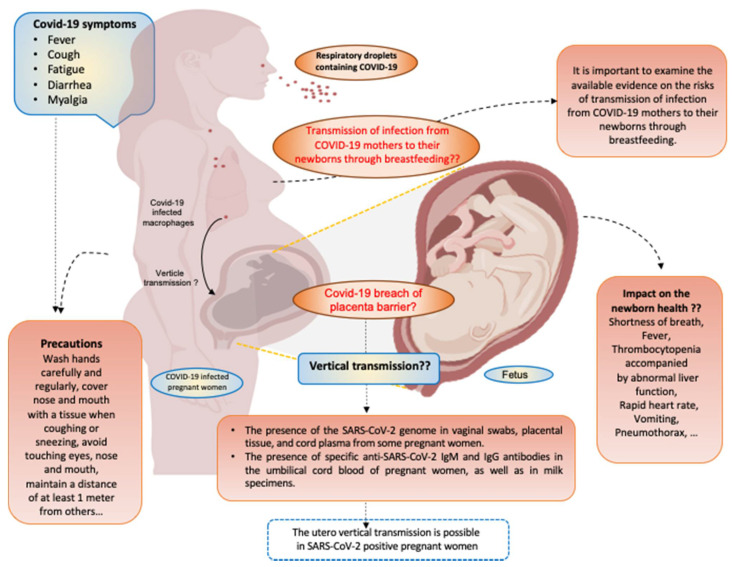
In this review, we assess the current knowledge about pre-and post-natal COVID-19 infection, and we discuss the prevalence, severity, and symptoms of COVID-19 infection and its related immune response during pregnancy. We also discuss the current literature describing whether vertical transmission takes place in pregnant women infected with the virus or not, as well as its potential effect on fetal and neonatal outcomes (summarized in Figure 1).
Figure 1.
COVID-19 infection during pregnancy. Schematic model presenting the relationship between COVID-19 and pregnant women. Pregnant women acquire COVID-19 via respiratory droplets. COVID-19 is spread throughout the maternal vasculature and the symptoms appear after an incubation period of approximately 5.2 days. The most common symptoms of COVID-19 are fever, dry cough, fatigue, diarrhea, and myalgia. The impact of COVID-19 infection on pregnancy outcomes are not established. However, COVID-19 infection effects newborn health (shortness of breath, fever, and thrombocytopenia accompanied by abnormal liver function, rapid heart rate, vomiting, pneumothorax, etc.). So far, the vertical transmission from the woman to her baby may be possible, but no data related to the risks of transmission of COVID-19 infection through breastfeeding were recorded. Specific precautions (wash hands carefully and regularly, cover nose and mouth with a tissue when coughing or sneezing, avoid touching eyes, nose and mouth, maintain a distance of at least 1 m from others, etc.) are needed to protect both the mother and her baby. Figure was created with BioRender.com (accessed date 5 January 2021).
2. Symptoms of COVID-19 Infection during Pregnancy
In general, symptoms of COVID-19 occur after approximately 5.2 days of incubation [22]. Fever, dry cough, and fatigue are the most common symptoms of the infection, although other less common symptoms, including headache, nasal congestion, sore throat, body aches, conjunctivitis, skin rash, diarrhea, loss of taste or smell, and discoloration of fingers or toes, have been reported [23,24,25,26]. Fortunately, most of the reported positive cases of pregnant women showed only mild to moderate symptoms [27,28,29,30,31]. Based on data from the Mexican National Registry of Coronavirus [32], the comparison of COVID-19-related outcomes between 5183 pregnant and 5183 non-pregnant women with COVID-19 demonstrated that the percentage of death, pneumonia, and ICU admission were higher in pregnant women [32], suggesting that pregnancy significantly increases the risk of severe COVID-19 infections [33]. In addition, Black or Hispanic pregnant women are reportedly more affected by COVID-19 compared to others, and diabetic and obese pregnant women are at a higher risk of severe illness [32,34,35]. It is expected that infection by the SARS-CoV-2 virus during pregnancy may increase the risk of maternal and fetal health complications and evolve to severe pneumonia, causing admissions to intensive care units (ICU) [36].
3. Immune Response to COVID-19 Infection in Pregnancy
Special attention has been drawn to pregnant women and their infants in terms of the severity of COVID-19 infection and the possibility of its vertical transmission. Increase in the levels of inflammatory cytokines, such as IL-1, IL-2, IL-7, IL-10, granulocyte-colony stimulating factor, interferon-alfa-inducible protein 10, and tumor necrosis factor alfa, has been reported in blood, vaginal, and placenta samples collected from pregnant women [37,38]. High levels of these mediators can increase the severity of the inflammatory state in women, which may lead to pulmonary edema, severe hypoxia, respiratory failure, and multiple organ failure; in addition, it can cause a fall in T cells and an increase in leukocytes count as well as neutrophil-lymphocyte ratio [39,40]. All these factors have been associated with the severity of the disease and admissions to the ICU [41].
In contrast, others have suggested that the transition to a Th2 anti-inflammatory environment during pregnancy may result in protection from a severe COVID-19 presentation [42,43,44]. It has also been reported that COVID-19-positive pregnant women had reduced anti- COVID-19 IgG titers and were less likely to have detectable neutralizing antibodies compared to non-pregnant women [38].
Seroprevalence studies can detect infections in subjects that test negative on PCR (reviewed in [45]). Several studies were recently published to evaluate the progression of the seroprevalence of SARS-CoV-2 during pregnancy [46]. Cecilia et al. tested 769 serum samples obtained from routine serological testing during the first and third trimesters of pregnancy for specific IgG anti SARS-CoV-2 RBD and S proteins [47]. A high prevalence of COVID-19 was detected [46]. On the other hand, seroprevalence was similar between women in the first trimester of pregnancy and women in the third trimester, suggesting a similar risk of infection, but the proportion of women with symptoms and those who required hospitalization were higher in the third trimester group [47].
4. Vertical Transmission of SARS-CoV-2 and the Role of ACE-2 Receptor
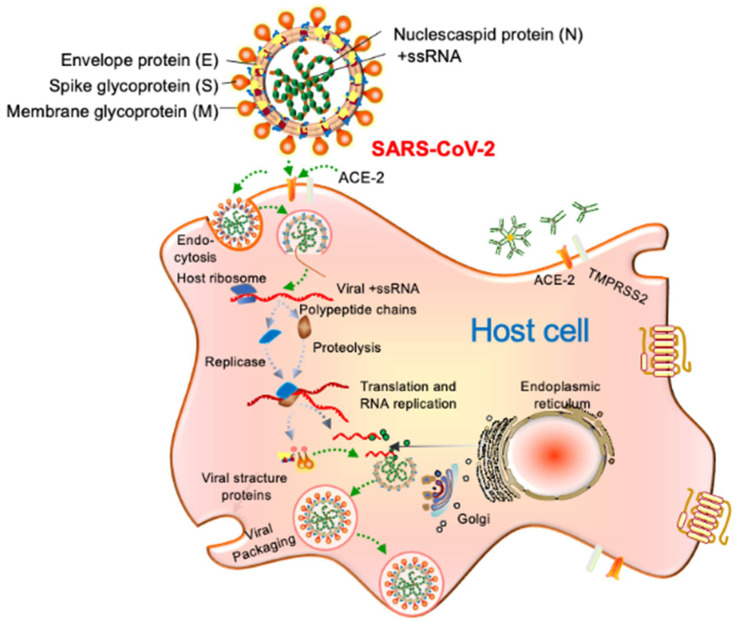
To understand the vertical transmission and pathophysiology of SARS-CoV-2, it is important to discuss the viral structure, attachment to host cells, and replication cycle. A SARS-CoV-2 virion is a positive, single-stranded RNA virus with nucleocapsid and envelope, approximately 50–200 nm in diameter [45,46]. The virion has four structural proteins known as the S (spike), E (envelope), M (membrane), and N (nucleocapsid) proteins; the N protein holds the RNA genome, and the S, E, and M proteins together create the viral envelope 12. The spike glycoprotein-S facilitates the SARS-CoV-2 attachment to the angiotensin-converting enzyme-2 (ACE-2) receptor, and then serine proteases TMPRSS2 contribute to priming the S protein in order for it to fuse with the host cell membrane and replicate (Figure 2) [12,48].
Figure 2.
SARS-CoV-19 structure, host cell entry, and replication model. SARS-CoV-2 binds to host cells through the ACE-2 receptor, and, after uncoating, the components of virion use the host cell’s machinery to produce new viruses. Finally, the SARS-CoV-2 virions are released from the host cell by exocytosis.
Expression of the ACE-2 receptor on the surface of host cells is the hallmark of SARS-CoV-2 susceptibility and infection. To further understand the pathogenesis and vertical transmission of SARS-CoV-2, Jing et al. investigated the expression and activity of ACE-2 during pregnancy and found that the ACE-2 receptor is expressed on various cells, such as on the ovary, uterus, vagina, and on the placenta [49]. Moreover, Carole et al. assessed the ACE-2 expression in the placenta and compared the formalin-fixed placental tissues from 28 women who tested negative for COVID-19 infection as well as placental tissues from a COVID-19-positive woman during the second and third trimester of pregnancy [50]. They found a membranous expression of ACE-2 in the extra villous trophoblast as well as a strong and diffuse membranous staining of cytotrophoblast and syncytiotrophoblast cells of the placental villi [50]. They concluded that the expression of ACE-2 at the maternal–fetal interface is present throughout pregnancy regardless of the COVID-19 status [50].
While the expression of ACE-2 on the placenta supports vertical transmission, other routes of vertical transmission also exist. Recent reports provided evidence of its expression on the venous and arterial endothelium as well as in the smooth muscle of the umbilical cord, which further supports the possibility of COVID-19 vertical transmission [51]. In a recently published study [52], the investigators assessed the viral genome in nasopharyngeal swabs, vaginal swabs, maternal and umbilical cord plasma, placenta and umbilical cord biopsies, amniotic fluids, and milk from 31 mothers with SARS-CoV-2 infection [52]. Specific anti-SARS-CoV-2 antibodies and the expression of genes implicated in placental, maternal, and umbilical cord inflammatory responses were also studied [52].The presence of the SARS-CoV-2 genome was found in one umbilical cord blood and two at-term placentas, one vaginal sample, and in one milk sample [52]. In addition, unique anti-SARS-CoV-2 IgM and IgG antibodies were identified in one umbilical cord blood in pregnant women as well as in one breast milk specimen, and for the documented cases of vertical transmission, SARS-CoV-2 infection was accompanied by a strong inflammatory response [52].
Alzamora et al. reported a patient with a severe presentation of COVID-19 during pregnancy [53]. The patient underwent a cesarean section, and, immediately after delivery, neonatal isolation was performed without delayed cord clamping or skin-to-skin contact [53]. The neonatal nasopharyngeal swab collected 16 hours post-delivery was positive for COVID-19 [53]. A positive throat test obtained from a neonate born to a COVID-19-positive mother was recorded in another study by Wang et al. [51]. The placental and cord blood samples collected at birth were negative, but the baby had near contact with his mother early on, suggesting that the infection was through contact and not vertical transmission [51,54].
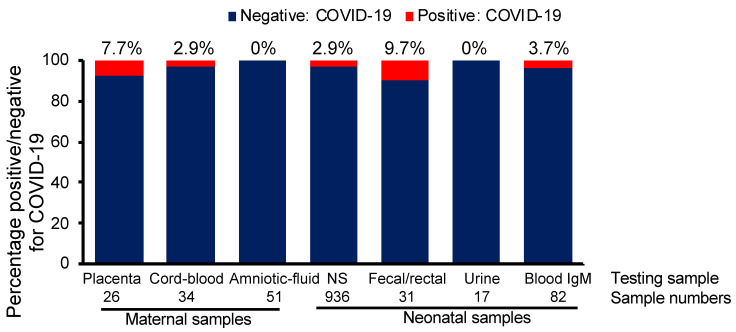
Since the claim of vertical transmission in COVID19-infected mothers is not clear, we decided to analyze a total of 38 studies that assessed COVID-19 and pregnancy (also reviewed in [9]) by using various neonatal samples collected from mothers with COVID-19 infection. We concluded that vertical transmission of COVID-19 in the third trimester seems possible but occurs at very low frequency (Figure 3). The possibility of vertical transmission of COVID-19 was approximately 2.9% based on neonatal nasopharyngeal swab testing and 7.7% and 2.9% by placenta sample and cord blood analysis, respectively, while it was not evident based on amniotic fluid and neonatal urine analysis. In contrast, the highest vertical transmission possibility was observed at 9.7% based on neonatal fecal/rectal samples [9,55]. Although further studies are needed and no concrete assumptions can be taken because of the low number of cases analyzed, the possibility of vertical transmission remains likely, and testing babies born to COVID-19-infected mothers is vital [56].
Figure 3.
Vertical transmission rate of COVID-19 to neonates based on different testing sites and meta-data analysis of 38 studies. IgM, immunoglobulin M; NP, nasopharyngeal; COVID-19, coronavirus disease 2019.
5. COVID-19 Infection and Transplacental Antibody Transfer
The prevailing hypothesis is that antibodies against SARS-CoV-2 can cross the placenta during pregnancy, and several studies have focused on the transplacental antibody transfer [47,57]. In a recent study that enrolled pregnant women with SARS-CoV-2 infection, the authors assessed the SARS-CoV-2 antibodies against the receptor binding domain (RBD) on the S1 subunit of the spike protein and SARS-CoV-2 nucleocapsid (N) antigen using enzyme-linked immunosorbent assay [58]. The antibody analysis of 37 women with SARS-CoV-2 infection showed that only 65% of women showed an anti–receptor binding domain immunoglobin G, and 70% of them showed an anti-nucleocapsid antibody [58]. Additionally, the authors also quantified the SARS-CoV-2 antibodies in cord blood of 77 neonates and showed that only one newborn had detectable immunoglobulin M to the nucleocapsid [58]. This study suggested that the reduced transplacental transfer of anti- SARS-CoV-2 antibodies may predispose the neonates to COVID-19 infection.
Another study showed that while non-SARS-CoV-2-specific antibody transfer to the cord remains intact in COVID-19-infected mothers, SARS-CoV-2-specific antibody transfer is significantly lower in the third trimester of pregnancy, and this was related to a perturbation in the Fc glycosylation profiles [59]. Changes in the Fc glycosylation affect the capacity of the antibody to recruit innate immune effector functions aiming to control the pathogen [60]. On the other hand, Flannery et al. reported an efficient transfer of IgG antibodies from SARS-CoV-2-seropositive women and a positive correlation between maternal and cord antibody concentrations [57].
6. Role of COVID-19 Infection in Fetal and Neonatal Outcomes
The perinatal consequences of maternal infection with COVID-19 are variable, including premature labor, fetal distress, respiratory distress, thrombocytopenia accompanied by impaired liver function, and even death [61]. While maternal and neonatal mortality are rare [62], there is a considerable proportion of women that required ICU due to complication of COVID-19 infection [62]. Previous studies revealed that samples of cord blood, amniotic fluid, placenta, throat swabs collected from neonates, vaginal fluid, and breastmilk samples from subjects infected with COVID-19 and their babies have all been screened negative for the virus [63].
Zhu et al. reported the clinical characteristics and findings of 10 neonates (including 2 twins) born to 9 mothers with confirmed COVID-19 infection in 5 hospitals from January 20 to February 5, 2020 [61]. Those included shortness of breath (n = 6), fever (n = 2), thrombocytopenia accompanied by disrupted liver function (n = 2), rapid heart rate (n = 1), vomiting (n = 1), and pneumothorax (n = 1) [61]. Of these, five neonates were cured and released, one died because of multiple organ failure, and four neonates remained in a healthy state in the hospital [61]. Pharyngeal swab specimens were gathered to test for COVID-19 from 9 of the 10 neonates 1 to 9 days after birth, but all of the samples showed negative findings [61]. Nine infants (ranging from 1 month to 11 months) diagnosed with COVID-19 were tested in another study [64]. Of the nine children, four had fever, two had minor upper respiratory symptoms, one was asymptomatic, and there was no detail on symptoms available for the other two [64]. The time between admission and diagnosis was 1–3 days. All nine babies had at least one infected family member, and the baby’s infection usually happened after the infection of the family member [64]. All nine infants did not require intensive care or artificial ventilation and had no significant complications [65].
The main adverse neonatal outcome found is iatrogenic preterm birth, low birth weight, and admission to the NICU [62]. Chen et al. reported a 20% preterm birth incidence (out of 118 pregnancies), but no vertical transmission [66]. The current evidence suggest that neonates and children do not to develop severe COVID-19, and there is no evidence for congenital abnormalities associated with maternal infection’ however, uncovering neonatal infection is very important, as neonates can remain asymptomatic and serve as a reservoir to COVID-19 contributing, in turn, to community-related infections.
7. Risks of Transmission of SARS-CoV-2 via Breastfeeding
Transmission of viral infections through breastfeeding is well documented for cytomegalovirus, human immunodeficiency virus, and hepatitis B, among others [67]. The current data on the risks of viral transmission from COVID-19-infected mothers to their newborns via breastfeeding is relevant to review. However, the current evidence is very limited, with only a few smaller case series and case studies having been reported to date.
A systematic analysis conducted by Centeno–Tablante et al. included the scientific brief on breastfeeding and COVID-19 released by the WHO on 23 June 2020, revealing that out of 46 COVID-19-positive mothers whose breastmilk samples were checked for SARS-CoV-2, 43 breastmilk samples tested negative for SARS-CoV-2 [68]. Out of the three mothers whose breastmilk tested positive, only one infant tested positive for the virus, although it was not possible to ascertain the path of infection (breast milk or near contact) [68]. All seven colostrum samples obtained from seven mothers who tested positive for SARS-CoV-2 by PCR on a nasopharyngeal swab were negative for COVID-19 in another report by Marin et al. [69]. Another Italian study analyzed the expressed breast milk samples collected from two mothers who tested positive for COVID-19, and the virus was not detected by RT-PCR [70]. A recent systematic analysis was performed to examine existing evidence relevant to the existence of SARS-CoV-2 in COVID-19-infected pregnant women’s breast milk [71]. Eight studies investigating the existence of SARS-CoV-2 RNA in breast milk in 24 COVID-19-positive pregnant women during the third trimester of pregnancy were reported [71]. Biological tests obtained from the upper respiratory tract (throat or nasopharyngeal) of the neonates and placental tissues collected shortly after birth demonstrated negative findings for the presence of SARS-CoV-2 by RT-PCR [71].
However, one study reported the virus in breastmilk samples obtained from one mother who tested positive for four consecutive days before testing negative [72]. In 64 breast milk samples from 18 infected mothers, Chambers et al. analyzed COVID-19; only one breast milk sample was positive for the virus, but the same sample tested negative 2 days earlier and 12 and 41 days later, respectively [73].
Breastmilk samples obtained from mothers infected with COVID-19 tested negative for the virus, but it remains unknown whether the disease was spread via breastfeeding, close contact, or transmission in the few reports where the virus was found in breastmilk and the babies were diagnosed with COVID-19 infection as well.
8. Conclusions
One of these controversial topics that has been unknown to date is COVID-19 vertical transmission. Primary findings suggested no possibility of transmission from mother to fetus, while few recent studies indicated that vertical transmission may occur. The latest literature based on either restricted case studies or small cohort size indicates that it might be possible to vertically transmit the virus from the mother to her baby. In brief, the effect of infection with COVID-19 on the outcomes of pregnancy or health of the offspring is not well known.
In order to confirm the possible intrauterine vertical transmission, further research on larger cohorts of pregnant women in the first or second trimester is needed. Longitudinal studies to assess the long-term effect on babies born to COVID-19-infected mothers are also needed. As newborn babies may catch the virus after delivery, it is also a consideration to temporarily isolate a COVID-19-positive mother from her child, while on the other hand, recommendations from scientific societies advise to provide safety for the newborn baby without compromising the benefit of early contact with the mother. For these reasons, specific precaution measures need to be implemented to save the health and life of the mother and the baby. She should follow the same recommendations as nonpregnant women to minimize the exposure to the virus, including washing hands regularly; covering her nose and mouth with a tissue when coughing or sneezing; avoiding touching her eyes, nose, and mouth; and maintaining social distance.
As the possibility of vertical transmission is very significant in terms of safety and disease prevention for neonatologists and neonatal health care providers, vertical transmission of COVID-19 is a tremendous concern for both patients and caregivers. It is also strongly recommended to inform expectant mothers about the disease process as well as the measures needed to avoid and/or minimize the spread of COVID-19 to their newborns through skin contact. It is also necessary to use the best therapy for pregnant women with COVID-19 infection, taking into consideration those that will not present any harm to the babies’ growth and development. Studies in humans will take a long time to conclude, but preclinical studies using animal models will accelerate our knowledge.
Author Contributions
Conceptualization, M.S. and S.A.K.; writing—original draft preparation, M.S. and S.A.K.; writing—review and editing, M.S., M.K. and S.A.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Sidra Medicine, Qatar, grant number SDR400161 and “The APC was funded by SDR400161”.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kumar P., Magon N. Hormones in pregnancy. Niger. Med. J. 2012;53:179–183. doi: 10.4103/0300-1652.107549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soma-Pillay P., Nelson-Piercy C., Tolppanen H., Mebazaa A. Physiological changes in pregnancy. Cardiovasc. J. Afr. 2016;27:89–94. doi: 10.5830/CVJA-2016-021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Regal J.F., Gilbert J.S., Burwick R.M. The complement system and adverse pregnancy outcomes. Mol. Immunol. 2015;67:56–70. doi: 10.1016/j.molimm.2015.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Okun M.L., Roberts J.M., Marsland A.L., Hall M. How disturbed sleep may be a risk factor for adverse pregnancy outcomes. Obstet. Gynecol. Surv. 2009;64:273–280. doi: 10.1097/OGX.0b013e318195160e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar M., Murugesan S., Singh P., Saadaoui M., Elhag D.A., Terranegra A., Kabeer B.S.A., Marr A.K., Kino T., Brummaier T., et al. Vaginal Microbiota and Cytokine Levels Predict Preterm Delivery in Asian Women. Front. Cell Infect. Microbiol. 2021;11:639665. doi: 10.3389/fcimb.2021.639665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.UNICEF . Surviving Birth: Every 11 Seconds, A Pregnant Woman or Newborn Dies Somewhere Around the World. UNICEF; Causeway Bay, Hong Kong: 2019. [Google Scholar]
- 7.Watson C. Stillbirth rate rises dramatically during pandemic. Nature. 2020;585:490–491. doi: 10.1038/d41586-020-02618-5. [DOI] [PubMed] [Google Scholar]
- 8.Fenizia C., Biasin M., Cetin I., Vergani P., Mileto D., Spinillo A., Gismondo M.R., Perotti F., Callegari C., Mancon A., et al. Analysis of SARS-CoV-2 vertical transmission during pregnancy. Nat. Commun. 2020;11:5128. doi: 10.1038/s41467-020-18933-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kotlyar A.M., Grechukhina O., Chen A., Popkhadze S., Grimshaw A., Tal O., Taylor H.S., Tal R. Vertical transmission of coronavirus disease 2019: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2021;224:35–53. doi: 10.1016/j.ajog.2020.07.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parker E.L., Silverstein R.B., Verma S., Mysorekar I.U. Viral-Immune Cell Interactions at the Maternal-Fetal Interface in Human Pregnancy. Front. Immunol. 2020;11:522047. doi: 10.3389/fimmu.2020.522047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization . WHO Coronavirus Disease (COVID-19) Dashboard. WHO; Geneva, Switzerland: 2020. [Google Scholar]
- 12.Kumar M., Al Khodor S. Pathophysiology and treatment strategies for COVID-19. J. Transl. Med. 2020;18:353. doi: 10.1186/s12967-020-02520-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Udugama B., Kadhiresan P., Kozlowski H.N., Malekjahani A., Osborne M., Li V.Y.C., Chen H., Mubareka S., Gubbay J.B., Chan W.C.W. Diagnosing COVID-19: The Disease and Tools for Detection. ACS Nano. 2020;14:3822–3835. doi: 10.1021/acsnano.0c02624. [DOI] [PubMed] [Google Scholar]
- 14.Woolf S.H., Chapman D.A., Sabo R.T., Weinberger D.M., Hill L., Taylor D.D.H. Excess Deaths from COVID-19 and Other Causes, March–July 2020. JAMA. 2020;324:1562–1564. doi: 10.1001/jama.2020.19545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.UNICEF . Pregnant Mothers and Babies Born during COVID-19 Pandemic Threatened by Strained Health Systems and Disruptions in Services. UNICEF; Causeway Bay, Hong Kong: 2020. [Google Scholar]
- 16.Saito S., Asai Y., Matsunaga N., Hayakawa K., Terada M., Ohtsu H., Tsuzuki S., Ohmagari N. First and second COVID-19 waves in Japan: A comparison of disease severity and characteristics. J. Infect. 2020 doi: 10.1016/j.jinf.2020.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vahidy F.S., Drews A.L., Masud F.N., Schwartz R.L., Askary B.B., Boom M.L., Phillips R.A. Characteristics and Outcomes of COVID-19 Patients during Initial Peak and Resurgence in the Houston Metropolitan Area. JAMA. 2020;324:998–1000. doi: 10.1001/jama.2020.15301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fan G., Yang Z., Lin Q., Zhao S., Yang L., He D. Decreased Case Fatality Rate of COVID-19 in the Second Wave: A study in 53 countries or regions. Transbound. Emerg. Dis. 2020 doi: 10.1111/tbed.13819. [DOI] [PubMed] [Google Scholar]
- 19.Iftimie S., López-Azcona A.F., Vallverdú I., Hernàndez-Flix S., de Febrer G., Parra S., Hernández-Aguilera A., Riu F., Joven J., Camps J., et al. First and second waves of coronavirus disease-19: A comparative study in hospitalized patients in Reus, Spain. medRxiv. 2020 doi: 10.1101/2020.12.10.20246959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. [(accessed on 25 May 2020)]; Available online: https://www.worldometers.info/coronavirus/#countries.
- 21.van Oosterhout C., Hall N., Ly H., Tyler K.M. COVID-19 evolution during the pandemic—Implications of new SARS-CoV-2 variants on disease control and public health policies. Virulence. 2021;12:507–508. doi: 10.1080/21505594.2021.1877066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S.M., Lau E.H.Y., Wong J.Y., et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N. Engl. J. Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khan M.M.A., Khan M.N., Mustagir M.G., Rana J., Haque M.R., Rahman M.M. COVID-19 infection during pregnancy: A systematic review to summarize possible symptoms, treatments, and pregnancy outcomes. medRxiv. 2020 doi: 10.1101/2020.03.31.20049304. [DOI] [Google Scholar]
- 24.Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berghella V., Hughes B. Coronavirus disease 2019 (COVID-19): Pregnancy issues and antenatal care. Walth. UpToDate. 2020 [Google Scholar]
- 26.Hassanipour S., Faradonbeh S.B., Momeni K., Heidarifard Z., Khosousi M.J., Khosousi L., Ameri H., Arab-Zozani M. A systematic review and meta-analysis of pregnancy and COVID-19: Signs and symptoms, laboratory tests, and perinatal outcomes. Int. J. Reprod. Biomed. 2020;18:1005–1018. doi: 10.18502/ijrm.v18i12.8022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Breslin N., Baptiste C., Gyamfi-Bannerman C., Miller R., Martinez R., Bernstein K., Ring L., Landau R., Purisch S., Friedman A.M., et al. Coronavirus disease 2019 infection among asymptomatic and symptomatic pregnant women: Two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am. J. Obstet. Gynecol. MFM. 2020;2:100118. doi: 10.1016/j.ajogmf.2020.100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen L., Li Q., Zheng D., Jiang H., Wei Y., Zou L., Feng L., Xiong G., Sun G., Wang H., et al. Clinical Characteristics of Pregnant Women with Covid-19 in Wuhan, China. N. Engl. J. Med. 2020;382:e100. doi: 10.1056/NEJMc2009226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang L., Jiang Y., Wei M., Cheng B.H., Zhou X.C., Li J., Tian J.H., Dong L., Hu R.H. Analysis of the pregnancy outcomes in pregnant women with COVID-19 in Hubei Province. Zhonghua Fu Chan Ke Za Zhi. 2020;55:166–171. doi: 10.3760/cma.j.cn112141-20200218-00111. [DOI] [PubMed] [Google Scholar]
- 30.Liu Y., Chen H., Tang K., Guo Y. Clinical manifestations and outcome of SARS-CoV-2 infection during pregnancy. J. Infect. 2020 doi: 10.1016/j.jinf.2020.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Juusela A., Nazir M., Gimovsky M. Two cases of coronavirus 2019-related cardiomyopathy in pregnancy. Am. J. Obstet. Gynecol. MFM. 2020;2:100113. doi: 10.1016/j.ajogmf.2020.100113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martinez-Portilla R.J., Sotiriadis A., Chatzakis C., Torres-Torres J., Espino Y.S.S., Sandoval-Mandujano K., Castro-Bernabe D.A., Medina-Jimenez V., Monarrez-Martin J.C., Figueras F., et al. Pregnant women with SARS-CoV-2 infection are at higher risk of death and pneumonia: Propensity score matched analysis of a nationwide prospective cohort (COV19Mx) Ultrasound Obstet. Gynecol. 2021;57:224–231. doi: 10.1002/uog.23575. [DOI] [PubMed] [Google Scholar]
- 33.Oakes M.C., Kernberg A.S., Carter E.B., Foeller M.E., Palanisamy A., Raghuraman N., Kelly J.C. Pregnancy as a risk factor for severe coronavirus disease 2019 using standardized clinical criteria. Am. J. Obstet. Gynecol. MFM. 2021;3:100319. doi: 10.1016/j.ajogmf.2021.100319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mahase E. Covid-19: Pregnant women with virus are more likely to need intensive care, study finds. BMJ. 2020;370:m3391. doi: 10.1136/bmj.m3391. [DOI] [PubMed] [Google Scholar]
- 35.Allotey J., Stallings E., Bonet M., Yap M., Chatterjee S., Kew T., Debenham L., Llavall A.C., Dixit A., Zhou D., et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: Living systematic review and meta-analysis. BMJ. 2020;370:m3320. doi: 10.1136/bmj.m3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen S., Huang B., Luo D.J., Li X., Yang F., Zhao Y., Nie X., Huang B.X. Pregnancy with new coronavirus infection: Clinical characteristics and placental pathological analysis of three cases. Zhonghua Bing Li Xue Za Zhi. 2020;49:418–423. doi: 10.3760/cma.j.cn112151-20200225-00138. [DOI] [PubMed] [Google Scholar]
- 37.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sherer M.L., Lei J., Creisher P., Jang M., Reddy R., Voegtline K., Olson S., Littlefield K., Park H.S., Ursin R.L., et al. Dysregulated immunity in SARS-CoV-2 infected pregnant women. medRxiv. 2020 doi: 10.1101/2020.11.13.20231373. [DOI] [Google Scholar]
- 39.Bouchghoul H., Vigoureux S. Do pregnant women have protective immunity against COVID-19? BJOG. 2020;127:1298–1299. doi: 10.1111/1471-0528.16342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu H., Wang L.L., Zhao S.J., Kwak-Kim J., Mor G., Liao A.H. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. J. Reprod. Immunol. 2020;139:103122. doi: 10.1016/j.jri.2020.103122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ashokka B., Loh M.H., Tan C.H., Su L.L., Young B.E., Lye D.C., Biswas A., Illanes S.E., Choolani M. Care of the pregnant woman with coronavirus disease 2019 in labor and delivery: Anesthesia, emergency cesarean delivery, differential diagnosis in the acutely ill parturient, care of the newborn, and protection of the healthcare personnel. Am. J. Obstet. Gynecol. 2020;223:66–74. doi: 10.1016/j.ajog.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dashraath P., Wong J.L.J., Lim M.X.K., Lim L.M., Li S., Biswas A., Choolani M., Mattar C., Su L.L. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am. J. Obstet. Gynecol. 2020;222:521–531. doi: 10.1016/j.ajog.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aghaeepour N., Ganio E.A., McIlwain D., Tsai A.S., Tingle M., Van Gassen S., Gaudilliere D.K., Baca Q., McNeil L., Okada R., et al. An immune clock of human pregnancy. Sci. Immunol. 2017;2 doi: 10.1126/sciimmunol.aan2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Enninga E.A., Nevala W.K., Creedon D.J., Markovic S.N., Holtan S.G. Fetal sex-based differences in maternal hormones, angiogenic factors, and immune mediators during pregnancy and the postpartum period. Am. J. Reprod. Immunol. 2015;73:251–262. doi: 10.1111/aji.12303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Guo C.C., Mi J.Q., Nie H. Seropositivity rate and diagnostic accuracy of serological tests in 2019-nCoV cases: A pooled analysis of individual studies. Eur. Rev. Med. Pharmacol. Sci. 2020;24:10208–10218. doi: 10.26355/eurrev_202010_23243. [DOI] [PubMed] [Google Scholar]
- 46.Villalain C., Herraiz I., Luczkowiak J., Perez-Rivilla A., Folgueira M.D., Mejia I., Batllori E., Felipe E., Risco B., Galindo A., et al. Seroprevalence analysis of SARS-CoV-2 in pregnant women along the first pandemic outbreak and perinatal outcome. PLoS ONE. 2020;15:e0243029. doi: 10.1371/journal.pone.0243029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Crovetto F., Crispi F., Llurba E., Figueras F., Gomez-Roig M.D., Gratacos E. Seroprevalence and presentation of SARS-CoV-2 in pregnancy. Lancet. 2020;396:530–531. doi: 10.1016/S0140-6736(20)31714-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Valdés G., Neves L.A., Anton L., Corthorn J., Chacón C., Germain A.M., Merrill D.C., Ferrario C.M., Sarao R., Penninger J., et al. Distribution of angiotensin-(1-7) and ACE2 in human placentas of normal and pathological pregnancies. Placenta. 2006;27:200–207. doi: 10.1016/j.placenta.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 49.Yan J., Li R.-Q., Wang H.-R., Chen H.-R., Liu Y.-B., Gao Y., Chen F. Potential influence of COVID-19/ACE2 on the female reproductive system. Mol. Hum. Reprod. 2020;26:367–373. doi: 10.1093/molehr/gaaa030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gengler C., Dubruc E., Favre G., Greub G., de Leval L., Baud D. SARS-CoV-2 ACE-receptor detection in the placenta throughout pregnancy. Clin. Microbiol. Infect. 2020 doi: 10.1016/j.cmi.2020.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang C., Zhou Y.H., Yang H.X., Poon L.C. Intrauterine vertical transmission of SARS-CoV-2: What we know so far. Ultrasound Obstet. Gynecol. 2020;55:724–725. doi: 10.1002/uog.22045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dong L. Possible Vertical Transmission of SARS-CoV-2 From an Infected Mother to Her Newborn. JAMA. 2020;323:1846–1848. doi: 10.1001/jama.2020.4621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Alzamora M.C., Paredes T., Caceres D., Webb C.M., Valdez L.M., Rosa M.L. Severe COVID-19 during Pregnancy and Possible Vertical Transmission. Am. J. Perinatol. 2020;37:861–865. doi: 10.1055/s-0040-1710050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vivanti A.J., Vauloup-Fellous C., Prevot S., Zupan V., Suffee C., Cao J.D., Benachi A., Luca D.D. Transplacental transmission of SARS-CoV-2 infection. Nat. Commun. 2020;11:3572. doi: 10.1038/s41467-020-17436-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Novazzi F., Cassaniti I., Piralla A., Sabatino A.D., Bruno R., Baldanti F. SARS-CoV-2 positivity in rectal swabs: Implication for possible transmission. J. Glob. Antimicrob. Resist. 2020;22:754–755. doi: 10.1016/j.jgar.2020.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kaufman D.A., Puopolo K.M. Infants Born to Mothers With COVID-19-Making Room for Rooming-in. JAMA Pediatr. 2021;175:240–242. doi: 10.1001/jamapediatrics.2020.5100. [DOI] [PubMed] [Google Scholar]
- 57.Flannery D.D., Gouma P., Dhudasia M.B., Mukhopadhyay S., Pfeifer M.R., Woodford E.C., Gerber J.S., Arevalo C.P., Bolton M.J., Weirick M.E. SARS-CoV-2 seroprevalence among parturient women in Philadelphia. Sci. Immunol. 2020;5 doi: 10.1126/sciimmunol.abd5709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Edlow A.G., Li J.Z., Collier A.-R.Y., Atyeo C., James K.E., Boatin A.A., Gray K.J., Bordt E.A., Shook L.L., Yonker L.M. Assessment of Maternal and Neonatal SARS-CoV-2 Viral Load, Transplacental Antibody Transfer, and Placental Pathology in Pregnancies During the COVID-19 Pandemic. JAMA Netw. Open. 2020;3:e2030455. doi: 10.1001/jamanetworkopen.2020.30455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Atyeo C., Pullen K.M., Bordt E.A., Fischinger S., Burke J., Michell A., Slein M.D., Loos C., Shook L.L., Boatin A.A. Compromised SARS-CoV-2-specific placental antibody transfer. Cell. 2021;184:628–642. doi: 10.1016/j.cell.2020.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ackerman M.E. Natural variation in Fc glycosylation of HIV-specific antibodies impacts antiviral activity. J. Clin. Invest. 2013;123:2183–2192. doi: 10.1172/JCI65708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhu H., Wang L., Fang C., Peng S., Zhang L., Chang G., Xia S., Zhou W. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl. Pediatr. 2020;9:51–60. doi: 10.21037/tp.2020.02.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Novoa R.H., Quintana W., Llancarí P., Urbina-Quispe K., Guevara-Ríos E., Ventura W. Maternal clinical characteristics and perinatal outcomes among pregnant women with coronavirus disease 2019. A systematic review. Travel Med. Infect Dis. 2021;39:101919. doi: 10.1016/j.tmaid.2020.101919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yang R., Mei H., Zheng T.Z., Fu Q., Zhang Y.M., Buka S., Yao X., Tang Z.Z., Zhang X.C., Qiu L. Pregnant women with COVID-19 and risk of adverse birth outcomes and maternal-fetal vertical transmission: A population-based cohort study in Wuhan, China. BMC Med. 2020;18:330. doi: 10.1186/s12916-020-01798-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wei M., Yuan J.P., Liu Y., Fu T., Yu X., Zhang Z.-J. Novel Coronavirus Infection in Hospitalized Infants Under 1 Year of Age in China. JAMA. 2020;323:1313–1314. doi: 10.1001/jama.2020.2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hong H., Wang Y., Chung H.T., Chen C.J. Clinical characteristics of novel coronavirus disease 2019 (COVID-19) in newborns, infants and children. Pediatr. Neonatol. 2020;61:131–132. doi: 10.1016/j.pedneo.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen Y., Peng H., Wang L., Zhao Y., Zeng L.K., Gao H., Liu Y.L. Infants Born to Mothers With a New Coronavirus (COVID-19) Front. Pediatr. 2020;8:104. doi: 10.3389/fped.2020.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lawrence R.M., Lawrence R.A. Breast milk and infection. Clin. Perinatol. 2004;31:501–528. doi: 10.1016/j.clp.2004.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kimberlin D.W., Stagno S. Can SARS-CoV-2 Infection Be Acquired In Utero? More Definitive Evidence Is Needed. JAMA. 2020;323:1788–1789. doi: 10.1001/jama.2020.4868. [DOI] [PubMed] [Google Scholar]
- 69.Dietary management of chronic kidney disease patients: Protein-restricted diets supplemented with keto/amino acids. Abstracts from the International Advisory Board Meetings 2003/2004. Am. J. Nephrol. 2005;25(Suppl. 1):1–28. doi: 10.1159/000084130. [DOI] [PubMed] [Google Scholar]
- 70.Aagaard K., Riehle K., Segata J., Ma N., Mistretta T.-A., Coarfa C., Raza S., Rosenbaum S., Veyver I.V.d., Milosavljevic A., et al. A metagenomic approach to characterization of the vaginal microbiome signature in pregnancy. PLoS ONE. 2012;7:e36466. doi: 10.1371/journal.pone.0036466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Martins-Filho P.R., Santos V.S., Santos H.P., Jr. To breastfeed or not to breastfeed? Lack of evidence on the presence of SARS-CoV-2 in breastmilk of pregnant women with COVID-19. Rev. Panam. Salud Publica. 2020;44:e59. doi: 10.26633/RPSP.2020.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cai J.H., Xu J., Lin D.J., Yang Z., Xu L., Qu Z.H., Zhang Y.H., Zhang H., Jia R., Liu P.C. A Case Series of children with 2019 novel coronavirus infection: Clinical and epidemiological features. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chambers C., Krogstad P., Bertrand K., Contreras D., Tobin N.H., Bode L., Aldrovandi G. Evaluation for SARS-CoV-2 in Breast Milk from 18 Infected Women. JAMA. 2020;324:1347–1348. doi: 10.1001/jama.2020.15580. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.