Abstract
Genetic polymorphisms are defined as the presence of two or more different alleles in the same locus, with a frequency higher than 1% in the population. Since the discovery of long non-coding RNAs (lncRNAs), which refer to a non-coding RNA with a length of more than 200 nucleotides, their biological roles have been increasingly revealed in recent years. They regulate many cellular processes, from pluripotency to cancer. Interestingly, abnormal expression or dysfunction of lncRNAs is closely related to the occurrence of human diseases, including cancer and degenerative neurological diseases. Particularly, their polymorphisms have been found to be associated with altered drug response and/or drug toxicity in cancer treatment. However, molecular mechanisms are not yet fully elucidated, which are expected to be discovered by detailed studies of RNA–protein, RNA–DNA, and RNA–lipid interactions. In conclusion, lncRNAs polymorphisms may become biomarkers for predicting the response to chemotherapy in cancer patients. Here we review and discuss how gene polymorphisms of lncRNAs affect cancer chemotherapeutic response. This knowledge may pave the way to personalized oncology treatments.
Keywords: gene polymorphisms, cancer chemotherapy, drug response, drug toxicity, personalized oncology
1. Background
Transcriptomic studies have implicated that up to 90% of eukaryotic genomes are transcribed [1], and the Human Genome Project revealed that only about 1.2% of the human genome encoded proteins, suggesting that a large number of transcripts were non-coding [1]. Non-coding RNAs with more than 200 nucleotides are defined as long non-coding RNAs (lncRNAs). The advent of advanced technologies, such as RNA-Seq and ChIP-Seq, has helped to identify the functions of lncRNAs in embryonic growth, pluripotency, cell cycle, cell differentiation, immune response, and disease development [2], while some of their functions are largely unknown. By interactions with DNA [3], RNA [4], and proteins [5], lncRNAs can participate in pathways of gene regulation. Recent studies have shown that lncRNAs seem to regulate their expression levels in a polymorphism-dependent manner and that they participate in different signal pathways, such as PI3K/AKT/NF-κB, thereby achieving the purpose of influencing the chemotherapy response. Some of them associated with imprinted regions have been extensively studied, such as H19, IPW, and MEG3 [6]. Some well-studied lncRNAs have proved to play a role in epigenetic regulation. For example, HOTAIR, is located in the human homeobox transcription factors C (HOXC) locus, it interacts with polycomb repressive complex 2 (PRC2), thereby repressing the transcription at the HOXD site across 40 kilobases, which may have important implications for gene regulation in development and disease status [7]. Previous studies have shown that lncRNAs can interfere with the miRNA pathway as a sponge [8]. As a new regulatory mechanism, lncRNAs and miRNAs may also form a mutual inhibitory regulatory loop [9]. Additionally, lncRNAs also act as key signal transduction mediators in cancer signaling pathways via the regulation of differentiation, cell proliferation and apoptosis, invasion and metastasis, and chemoresistance [10,11], and alterations in these functions are associated with their gene polymorphisms. Genetic polymorphisms are defined as the presence of two or more different alleles in the same locus, with a frequency of higher than 1% in the population. Single nucleotide polymorphisms (SNPs) are defined as DNA sequence polymorphisms caused by a single nucleotide variation at the genomic level [12]. The genome-wide association study (GWAS) has recognized SNPs as the most common type of genetic variation in the human genome (one per 100–300 nucleotides) [13], associated with cancer tumorigenesis [14]. Recent studies have found that aberrant expression of specific lncRNAs was strongly associated with the earlier diagnosis or prognosis of patients with upper gastrointestinal tumors [14]. In fact, lncRNA-associated SNPs show a strong ability to interfere with the function of lncRNA-regulated genes, which are involved in important signaling pathways and carcinogenesis. Some polymorphisms in lncRNA maternally expressed gene 3 (MEG3) are considered as well-established cancer biomarkers and therapeutic targets due to their association with cancer risk and response to chemotherapy [15]. In this review, we focus on the role of lncRNAs in cancers, particularly the role of lncRNA polymorphisms in response to anti-cancer therapies.
2. lncRNA Polymorphisms in Cancer Chemotherapeutic Response
In recent years, disease association studies have revealed the role of the SNPs of lncRNAs in various diseases. For example, the SNP of SLEAR rs13259960 was associated with susceptibility to systemic lupus erythematosus [16], and the SNP of PART1 rs8176070 was associated with the risk of knee osteoarthritis [17]. Notably, lncRNAs SNPs can significantly affect gene expression and function, leading to alterations in cancer susceptibility, chemotoxicity, and sensitivity. For example, the ANRIL rs1333049 was thought to be associated with the risk of toxicity to platinum-based chemotherapeutic drugs in lung cancer patients [18]. Long intergenic non-coding RNA for kinase activation (LINK-A) rs12095274 might lead to resistance to serine/threonine kinase (AKT) inhibitors in breast cancer patients [19]. Compared with A allele carriers, rs2288947 G allele carriers have a significantly higher risk of bladder cancer susceptibility [20]. Chemotherapy, as one of the important methods of cancer treatment, is of great significance for prolonging the life of patients, but chemotherapy resistance that affects the effectiveness of chemotherapy is still inevitable. Fortunately, some recent studies on lncRNAs polymorphisms bring hope to the fight against chemotherapy resistance. These findings indicate that lncRNAs polymorphisms may have a potential meaning in personalized cancer therapy based on genotypes. Here, we summarize several studies of lncRNAs SNPs relevant to chemotherapy responses to further clarify the potential of lncRNAs as potential biomarkers of cancer risk and predictors of drug resistance as well as toxicity (Table 1).
Table 1.
Known lncRNA polymorphisms affecting drug response in cancer therapy.
| LncRNA | Polymorphisms | Cancer Type | Patient Population | Drug | Effect | Reference |
|---|---|---|---|---|---|---|
| MIR2052 Host Gene (MIR2052HG) | rs4476990 and rs3802201 | Breast cancer | 4658 women with breast cancer, including 252 women experiencing a breast cancer recurrence | Aromatase Inhibitor (AIs) | Regulated ERα expression in the presence of AIs | [21] |
| 4406 controls without recurrence of breast cancer and 252 cases with recurrence | [22] | |||||
| Maternally Expressed 3(MEG3) | rs10132552 | Breast cancer | 144 women with locally advanced invasive breast cancer | Paclitaxel and cisplatin | Associated with good DFS and PCR rate | [23] |
| Nasopharyngeal carcinoma | 505 newly diagnosed nasopharyngeal carcinoma patients | Platinum-based chemotherapy drug | Associated with treatment response and risk of developing anemia | [24] | ||
| rs941576 | Breast cancer | 144 women with locally advanced invasive breast cancer | Paclitaxel and cisplatin | Associated with good DFS | [23] | |
| rs116907618 | Lung cancer | 467 lung cancer patients | Platinum-based chemotherapy drug | Associated with severe gastrointestinal toxicity | [18] | |
| H19 Imprinted Maternally Expressed Transcript(H19) | rs2839698, rs3842761, rs4244809, rs7924316, rs4244809 | Epithelial ovarian cancer (EOC) | 43 platinum-resistant and 138 platinum-sensitive EOC patients | Platinum-based chemotherapy drug | Associated with platinum-based chemoresistance | [25] |
| rs2104725 | Lung cancer | 467 lung cancer patients | Platinum-based chemotherapy drug | Associated with severe gastrointestinal toxicity | [18] | |
| rs2839698 | Associated with severe gastrointestinal or hematologic toxicities | |||||
| antisense non-coding RNA in the INK4 locus (ANRIL) | rs1333049 | Lung cancer | 467 lung cancer patients | Platinum-based chemotherapy drug | Associated with the incidence of severe gastrointestinal toxicity | [18] |
| rs10120688 | Associated with severe hematologic toxicity | |||||
| HOX Transcript Antisense RNA (HOTAIR) | rs7958904 | Lung cancer | 467 lung cancer patients | Platinum-based chemotherapy drug | Associated with the incidence of severe gastrointestinal toxicity | [18] |
| rs1899663 | Associated with severe gastrointestinal toxicity in age ≥ 57 | |||||
| metastasis-associated with lung adenocarcinoma transcript-1 (MALAT1) | rs619586 | Lung cancer | 467 lung cancer patients | Platinum-based chemotherapy drug | Associated with gastrointestinal toxicity | [18] |
| rs3200401 | Metastatic colorectal cancer | 98 colorectal cancer patients | Irinotecan | Associated with Pb derived toxicity and tumor resistance to irinotecan | [26] | |
| cancer susceptibility candidate 8 (CASC8) | rs10505477 | Lung Cancer | 498 lung cancer patients and healthy controls | Platinum-based chemotherapy drug | Associated with platinum-based chemotherapy response and toxicity | [27] |
| Long Intergenic Non-Protein Coding RNA 1139(LINK-A) | rs12095274 | Breast cancer | Breast cancer patients | AKT inhibitors | Leading to resistance to AKT inhibitors | [19] |
| Long intergenic non-protein coding RNA-regulator of reprogramming (Linc-ROR) | rs2027701 | Nasopharyngeal carcinoma | 505 newly diagnosed nasopharyngeal carcinoma patients | Platinum-based chemotherapy drug | Associated with chemoresistance and toxicity | [24] |
2.1. MIR2052HG
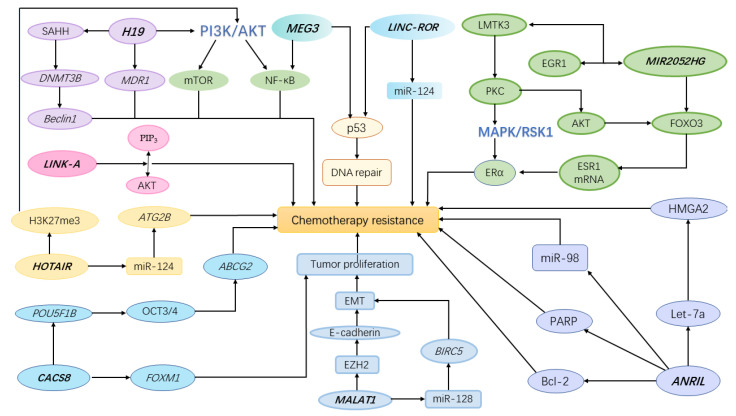
MIR2052HG, located on chromosome 8q21.11, encodes a lncRNA. Previous research results suggested that MIR2052HG was related to estrogen receptor (ER)-positive breast cancer [28], which can be treated with aromatase inhibitors (AIs) by inhibiting the synthesis of estrogen [29]. Compared with 4406 healthy people, it was found that the level of MIR2052HG in 253 breast cancer patients increased, and this change in expression level was regulated by MIR2052HG SNPs [21]. GWAS analysis by Ingle et al. identified six SNPs that were associated with a longer breast cancer-free interval. Among them, rs3802201 was located in an intron of MIR2052HG, which could down-regulate the expression of MIR2052HG and made patients have a longer breast cancer-free interval [21]. In lymphoblastoid cell line (LCL) models, cells with this SNP showed estradiol dose-dependent up-regulation of MIR2052HG expression, which was reversed by an AI (exemestane or anastrozole) [21]. Strikingly, the expression of ESR1 (encoding ERα) was correlated with the expression of MIR2052HG in these LCL models, which was in agreement with the analysis of The Cancer Genome Atlas data of 485 ER-positive breast cancer patients. It is common knowledge that the amplification of ESR1 gene leads to the increased expression of ERα, which is associated with endocrine resistance [29]. This suggested that MIR2051HG may play a role in the resistance of breast cancer patients to AIs. Subsequently, by proteasome inhibitor and ubiquitin analysis experiments, Ingle et al. confirmed that MIR2052HG was involved in the degradation process of ERα in a ubiquitin-dependent and proteasome-mediated mode [21]. In addition, the researchers found that the down-regulation of MIR2052HG could reduce ESR1 mRNA expression by enhancing AKT-mediated decrease of forkhead box O3 (FOXO3), which was a regulator of ESR1 transcription. This finding indicates that the expression of MIR2052HG regulated the level of ERα at both the transcription level and the protein degradation level. Mechanistically, Cairns et al. confirmed that MIR2052HG promoted the transcription of lemur tyrosine kinase-3 (LMTK3) by interacting with early growth response protein 1 (EGR1) [22]. LMTK3 is related to new-onset and intrinsic endocrine resistance in breast cancer [30]. As a direct target of MIR2052HG, LMTK3 regulated downstream protein kinase C (PKC)/AKT/FOXO3 and PKC/MAPK/RSK1/ERα signaling pathways, thereby regulating the expression of ERα and the response to AI [21] (Figure 1). Notably, compared with the wild genotype, the stimulation effect of MIR2052HG SNPs on LMTK3 expression can be reversed by AIs. It showed that MIR2052HG regulated LMTK3 in a SNPs- and AI-dependent way [22]. In conclusion, the expression level of MIR2052HG was influenced by its genetic polymorphisms. Furthermore, different expression levels of MIR2052HG regulate the expression of ERα through transcription and protein degradation mode, which is related to the resistance of ERα-positive breast cancer patients to AIs.
Figure 1.
A schematic showing how polymorphisms affect the response to cancer chemotherapy. SAHH (S-adenosylhomocysteine hydrolase), DNMT3B (DNA Methyltransferase 3 Beta), MDR1 (multidrug resistance 1), PIP3 (phosphatidylinositol 3,4,5-trisphosphate), ATG2B (autophagy-related protein 2 homolog B), POU5F1B (POU Class 5 Homeobox 1B), FOXM1 (Forkhead Box M1), ABCG2 (ATP-binding cassette transporter G2), BIRC5 (Baculoviral IAP Repeat Containing 5), EMT (Epithelial-mesenchymal transition), EZH2 (Enhancer Of Zeste 2 Polycomb Repressive Complex 2 Subunit), HMGA2 (High Mobility Group AT-Hook 2), PARP (Poly(ADP-ribose) polymerase), Bcl-2 (B cell lymphoma-2).
2.2. MEG3
As a lncRNA, Maternally Expressed Gene 3 (MEG3) located on the human chromosome 14q32.3 has an inhibitory effect in a variety of cancers, such as bladder cancer, gastric cancer, and non-small cell lung cancer [31,32,33]. In some pathways associated with cancer, such as TGF-β, PI3K/AKT, mTOR, and WNT/β-catenin pathways, MEG3 plays a regulatory role. Previous studies have shown that MEG3 was down-regulated in ER-positive breast cancer [34] and is also closely related to the chemotherapy response of breast cancer and colorectal cancer [23,35]. Ji et al. found that overexpression of MEG3 increased the sensitivity of cisplatin-resistant cells to cisplatin, which was achieved by suppressing cell proliferation and inducing apoptosis [36]. In non-small cell lung cancer, up-regulation of MEG3 led to an increase in the apoptosis rate of cancer cells. However, cancer cells with MEG3 knockout have a decreased rate of cisplatin-induced apoptosis, and the result is that lung cancer cells enhance cisplatin resistance by activating the WNT/β-catenin signaling pathway [37]. In addition, researchers found that the MEG3 polymorphisms may be a key factor for individual differences in chemotherapy toxicity and sensitivity to treatment [12]. By exploring the response of 505 patients with nasopharyngeal carcinoma after concurrent chemoradiotherapy treatment, it was found that patients with the MEG3 rs10132552 CC genotype had a significantly higher risk of developing anemia (OR = 3.001, 95% CI = 1.355–6.646, p = 0.007), and patients with the rs10132552 CT genotype responded better to chemotherapy (OR = 0.261, 95% CI = 0.089–0.770, p = 0.015). In silico analysis results explained why MEG3 polymorphisms could affect the sensitivity and toxicity of chemotherapy drugs in nasopharyngeal carcinoma patients. The local folding structure of RNA was altered when the T allele on rs10132552 was replaced by the C allele, which then affected the function of MEG3. Likewise, the results of the study by Bayarmaa et al. proved that MEG3 rs10132552 was also related to chemotherapy response in breast cancer patients treated with paclitaxel or cisplatin [23]. In terms of mechanism, MEG3 may inhibit the growth of cancer cells and induce their apoptosis by activating ER stress, nuclear factor-κB (NF-κB), and p53 pathways, and it may eventually affect the response to chemotherapy. Zhang et al. also believed that MEG3 can regulate the expression of a variety of downstream genes of the p53 pathway [38], thereby regulating the proliferation and apoptosis of cancer cells. Additionally, MEG3 genetic polymorphisms were also associated with platinum-based chemotherapy response in lung cancer [39]. In terms of chemotherapy toxicity, Gong et al. found that MEG3 rs116907618 might play an important role in the occurrence of severe gastrointestinal toxicity caused by platinum drugs [18]. Particularly, linkage disequilibrium analysis showed that SNPs of rs10132552 and rs941576 had strong linkage [23]. Thus, the effect of SNP rs941576 on chemotherapy response can be further explored. Based on these results, MEG3 polymorphisms could be used as a potential predictive biomarker for platinum-based adjuvant chemotherapy responses in relevant cancer patients. Moreover, it can also be used for individualized treatment of cancer patients to avoid serious adverse reactions of chemotherapy in some patients.
2.3. H19
H19 plays a dual role of oncogene or tumor suppressor gene, depending on the cancer type and stage of development. In recent years, the impact of H19 on cancer risk and prognosis has attracted researchers’ interest [18,40,41,42]. H19 has recently been found to be an independent posterior factor for low-grade gliomas [43]. As previously reported in the literature, H19 polymorphisms were associated with the risk of several cancers. For instance, H19 rs217727 was found to be associated with oral squamous cell carcinoma [44], osteosarcoma [45], bladder cancer [46], and gastric cancer [47] risk; H19 rs2839698 has been shown to be associated with hepatocellular cancer risk and prognosis [48]. It was noteworthy that H19 was overexpressed in many drug-resistant cancer cell lines, such as cisplatin-resistant ovarian cancer and doxorubicin-resistant breast cancer cells [25,49]. Recently, it was found that H19 was overexpressed in methotrexate-resistant and 5-fluorouracil-resistant choriocarcinoma cells [50]. Methotrexate and 5-fluorouracil are the most important first-line chemotherapeutic agents. Further, studies substantiated that H19 knockdown could reduce drug resistance in cells and promote drug-induced apoptosis in resistant choriocarcinoma cells. In terms of mechanism, the expression levels of p-PI3K, p-AKT, and p-mTOR proteins of H19 knockdown were significantly lower than those of the H19 non-knockdown group, and the PI3K/AKT/mTOR pathway may be the pathway by which H19 exerts chemoresistance [50]. Notably, two H19 SNPs (rs2107425 and rs2839698) were observed to be significantly correlated with platinum-based chemotherapy treatment in lung cancer patients [39]. Among them, H19 rs2839698 T allele carriers had lower sensitivity to platinum-based chemotherapy drugs. In addition, the researchers found that H19 rs2104725 and rs2839698 were both related to gastrointestinal toxicity in platinum-based chemotherapy reactions. Additionally, rs2839698 was also related to severe hematological toxicity [18]. Mechanically, H19 regulates the methylation of the promoter of multidrug resistance 1 (MDR1) gene, thereby inducing the expression of the product p-glycoprotein (encoded by MDR1) and MDR1-related drug resistance in human hepatocellular carcinoma HepG2 cells [42]. MDR1 was also shown to be related to gastrointestinal toxicity caused by platinum-based chemotherapy [51]. Recent studies have found that the H19/SAHH/DNMT3B axis may be critical for tamoxifen resistance in breast cancer patients and then decreasing methylation in the promoter region of Beclin1 [52]. These results corroborated that H19 polymorphisms were related to the drug reaction and toxicity reaction of platinum chemotherapeutic drugs, but its molecular mechanism needs further study.
2.4. CASC8
The gene polymorphisms of CASC8 have been reported to be closely related to the risk and progression of different cancers [53,54]. According to a recent study comparing TC and CC genotypes, gastric cancer patients carrying the rs1562430 TT genotype had a higher risk of death [55]. For rs10505477 TT genotype carriers, cancer risk was higher than TC or CC genotype carriers [56]. In a study of colorectal adenoma, two CASC8 SNPs (rs10505477 and rs6983267) were found to be associated with colorectal adenoma risk, especially in patients without a family history of colorectal cancer [57]. Among them, rs10505477 A genotype carriers and rs6983267 G genotype carriers had a lower risk of developing adenoma. Based on these findings, more attention has been drawn to the effect of CASC8 polymorphisms on chemotherapy responses. Shen et al. have proven that CASC8 rs10505477 was related to the prognosis of gastric cancer patients receiving cisplatin chemotherapy after surgery [58]. Recently, through conducting chemotherapy response and toxicity studies on 467 patients, Gong et al. found for the first time that the SNP of CASC8 rs10505477 was significantly correlated with platinum-based chemotherapy response (adjusted OR = 1.58, 95% CI = 1.05–2.39, p = 0.03) and toxicity (adjusted OR = 0.59, 95% CI = 0.35–0.98, p = 0.04), including severe hematological toxicity and gastrointestinal toxicity [27]. Prior to this, two studies have demonstrated that the CASC8 gene location region overlapped with the POU5F1B gene, also known as POU5F1P1 [58,59]. The protein encoded by POU5F1P1 is functionally similar to the protein encoded by the POU5F1 gene (also known as OCT3 or OCT4) [60]. OCT3/4 has been confirmed to be involved in the chemotherapy resistance of glioblastoma cell lines by affecting the expression of the drug efflux pump gene ABCG2, which encodes breast cancer resistance protein (BCRP) [61]. Non-small cell lung cancer patients with ABCG2 overexpression are resistant to platinum-based chemotherapy [62]. Based on this evidence, Hu et al. surmised that the polymorphisms of CASC8 rs10505477 could affect the efficacy and toxicity of platinum-based chemotherapeutics in patients with lung cancer by adjusting the POU5F1B–OCT3/4-ABCG2 axis. Moreover, in non-small cell lung cancer cells, through Western blotting, researchers found that when CASC8 was knockdown, the level of FOXM1 protein decreased [63]. FOXM1 is an oncogene that promotes cell proliferation and promotes tumor development [64]. Subsequent studies substantiated that there was a positive regulatory relationship between CASC8 and FOXM1. In the three cell lines (A549, H1299, and H460 cells), CASC8 and FOXM1 were both increased in an osimertinib-dependent manner. Silencing CASC8 can increase the sensitivity of NSCLC cells to osimertinib via FOXM1. These findings not only provide new insights for the clinical application of CASC8 polymorphisms in predicting cancer risk and chemotherapy response but also provide new directions for exploring the effect of CASC8 SNPs on chemotherapy.
2.5. LINK-A
LINK-A, also LINC01139, is a lncRNA with increased expression in cancer cell lines. A prior study suggests that highly expressed LINK-A may exhibit resistance to AKT inhibitors in breast cancer [19]. Since up-regulated expression of LINK-A in vivo is regulated by gene amplification and disease-related SNPs, researchers are beginning to focus on the effects of LINK-A SNPs on the development of drug resistance in cancer patients. By analyzing genetic mutations within or adjacent to the LINK-A gene locus in breast cancer patients, Lin et al. found that a SNP mutation located downstream of the LINK-A transcriptional region in breast cancer was associated with LINK-A expression and outcome [19]. In addition, meta-analysis corroborated that the expression of LINK-A was related to its genetic variation, and rs12095274 A allele carriers had higher LINK-A expression levels than G allele carriers. It is known that AKT and phosphatidylinositol 3,4,5-trisphosphate (PIP3) are involved in important signal transduction pathways in cells and play significant roles in cell growth. Therefore, the dysregulation of PI3K and the activation state of its downstream AKT are closely related to many cancers [65,66]. According to previous studies, lncRNA LINK-A can specifically interact with AKT and PIP3 in breast cancer cells [19]. LINK-A promotes the AKT–PIP3 interaction and the activation of downstream enzymes to cause tumor cell resistance to AKT inhibitors. Lin et al. found that the deletion of the PIP3-binding motif of LINK-A reversed the resistance of drug-resistant cells to MK2206 (an AKT inhibitor targeting the AKT pleckstrin homology (PH) domain). This is due to its inability to promote the binding of PIP3 to the PH domain of AKT [67]. Based on these studies, it can be believed that LINK-A rs12095274 A allele carriers are more likely than G allele carriers to develop resistance to AKT inhibitors in breast cancer patients. These genetic polymorphisms may result in poor treatment outcomes and may impact on survival in breast cancer patients. These studies suggest that LINK-A SNPs can be used as a marker to infer the sensitivity of breast cancer patients to AKT inhibitor therapy. Moreover, stratifying breast cancer according to the expression level of LINK-A is an effective way to achieve individualized treatment
2.6. Linc-ROR
Linc-ROR, is an effector of p53, but interestingly, it also has a regulatory effect on p53. The dysfunction of p53 function has been shown to relate to the occurrence and development of breast cancer [68]. Previous studies have suggested that Linc-ROR significantly inhibited p53 in the process of DNA damage, thereby affecting the arrest and apoptosis of cancer cells, which is believed to be the cause of resistance to platinum chemotherapy in cancer patients [24]. In addition, Linc-ROR has also been found to interact with miR-124 and to participate in the resistance of pancreatic cancer to gemcitabine by regulating the miR-124/PTBP1/PKM2 axis [69]. Wang et al. found that the Linc-ROR rs2027701 polymorphisms were associated with the poor efficacy of chemoradiotherapy in lymph nodes, but the mechanism was unclear [24]. Moreover, patients with rs2027701 in one or two variant alleles showed a clear trend of toxic reactions to platinum-based chemotherapy. A recent study confirmed that high Linc-ROR expression leads to doxorubicin resistance in hepatocellular carcinoma [70]. Combined with a finding by Luo et al. that the SNP of rs4801078 affects the expression level of Linc-ROR mRNA [71]. Therefore, it can be speculated that Linc-ROR SNPs may play an important role in chemoresistance by altering Linc-ROR mRNA’s expression level. These findings provide new insights into the function of Linc-ROR polymorphisms in cancer development and chemotherapy.
2.7. MALAT1
In recent years, lncRNA MALAT1 has been proved to be a metastasis and prognosis marker of some cancers, and it was involved in the proliferation, invasion, and apoptosis of cancer cells [26,72]. The increased expression is positively correlated with cancer susceptibility and poor cancer prognosis. A prior study confirmed that mutation of one or two alleles from C to G on rs664589 increased the risk of colorectal cancer metastasis and carcinogenesis [73]. The change in the binding of MALAT1 to miR-194-5p led to an increase in the expression level of MALAT1 rs664589 in the G allele carrier, which leads to this outcome. In addition, the impact of MALAT1 on chemotherapy response is also one of the focuses of researchers, especially its genetic polymorphisms. Lai et al. found that the silence of MALAT1 significantly increased the sensitivity of cancer cells to cisplatin [74]. It has been suggested that rs619586 SNP may change MALAT1 expression by affecting the transcription factor binding site [39], thus affecting chemotherapy toxicity. As one of the effective chemotherapeutic drugs for metastatic colorectal cancer, irinotecan has a wide range of inter-individual toxicity, which is related to the genetic characteristics of patients [75,76,77]. The resistance of tumor cells to irinotecan may be due to the inhibition of DNA topoisomerase I by MALAT1 attenuated irinotecan. As evidence, in metastatic colorectal cancer, researchers found that increased levels of MALAT1 of the cell cycle G1/S and M phases inhibited apoptosis and/or increased the efficiency of DNA repair [26]. Analogously, Li et al. proved that the up-regulation of MALAT1 also led to a decrease in sensitivity to oxaliplatin [74]. Mechanically, MALAT1 knockdown enhanced E-cadherin expression and inhibited oxaliplatin-induced EMT in colorectal cancer cells through EZH2. EZH2 is a critical component of PRC2 [78], which silences E-cadherin during EMT and leads to cancer progression [79]. In addition, as a molecular sponge, MALAT1 interacts with miR-218, also affecting chemotherapy response. After receiving standard FOLFOX treatment, patients with low MALAT1 and high miR-218 expression had a higher survival rate than those with high MALAT1 and low miR-218 expression [74]. In patients with high MALAT1 expression, it was found that MALAT1 binds EZH2 to the CDH1 promoter and inhibits miR-218 during oxaliplatin treatment, indirectly promoting EMT, metastasis, and chemoresistance of colorectal cancer cells. Previous studies revealed that miR-218 could significantly suppress the EMT process and enhance 5-FU–based chemosensitivity in colorectal cancer cells by targeting BIRC5, a key member of the inhibitors of apoptosis gene (IAP) family [80,81]. MALAT1 SNPs influenced the resistance of cancer cells to oxaliplatin through the regulation of their expression level. Moreover, researchers recently proposed that MALAT1 polymorphisms were related to the drug resistance and toxicity of platinum-based chemotherapy drugs in lung cancer patients [82]. To sum up, the regulatory role of MALAT1 polymorphisms in cancer chemotherapy is interesting, and its potential as a biomarker to predict the chemotherapy response of cancer patients is promising.
2.8. ANRIL
As it is located in the genomic hot spot related to disease inheritance—namely, the CDKN2A/B locus—ANRIL has attracted widespread attention [83]. Past studies have shown that ANRIL was involved in the occurrence and development of a variety of cancers, including cancer susceptibility and the proliferation and migration process of cancer cells [84,85]. ANRIL rs1333048 has been confirmed to be a biomarker of breast cancer susceptibility [86]. In addition, rs4977574 and rs10757278 have also been proved to be associated with cancer risk. Studies have confirmed the importance of p16 as a regulator in cancer cells caused by cisplatin. With logistic regression analysis, Gong et al. found that ANRIL rs1333049 was associated with the low incidence of overall toxicity after severe cisplatin treatment in lung cancer patients (p = 0.028) [18]. According to previous studies, ANRIL regulates epigenetic silencing of p14ARF (or p16INK4a), which was an important regulator of cisplatin-induced apoptosis [87,88,89]. This may explain the functional changes associated with ANRIL polymorphisms that can affect the response to platinum-based chemotherapy in cancer patients. Compared with the paclitaxel-resistant group, Xu et al. found that the expression level of ANRIL was significantly increased in paclitaxel-sensitive lung adenocarcinoma cells. Similarly, ANRIL expression was higher after si-ANRIL transfection [90]. It shows that the expression level of ANRIL is related to paclitaxel resistance. Interestingly, rs10757278 SNP may be associated with ANRIL expression levels, as suggested by Huang et al. [86]. Based on the foregoing, it can be speculated that the SNP of rs10757278 affected cisplatin resistance. Further mechanistic studies revealed that ANRIL could significantly modulated the expression of apoptosis-related protein Bcl-2 protein and PARP protein [90]. In paclitaxel-sensitive lung adenocarcinoma cells, the expression of Bcl-2 was increased, but PARP was reduced. It indicates that ANRIL polymorphism-related abnormal expression may result in resistance to paclitaxel chemotherapy by regulating the expression of Bcl-2 and PARP. Another study explained the role of ANRIL in cisplatin resistance in ovarian cancer by down-regulating the expression of let-7a and then up-regulating the expression of HMGA2 [91]. In lung cancer, the development of drug resistance is achieved by inhibiting the expression of miR-98 [92]. All these results indicate that ANRIL polymorphisms are related to the susceptibility to toxicity of cisplatin chemotherapy drugs, and its mechanism might be related to the polymorphisms affecting the centroid secondary structure and minimum free energy of ANRIL [39,93]. The role of ANRIL polymorphisms in chemotherapy response needs to be further investigated, especially in terms of mechanism. However, it cannot be denied that ANRIL polymorphisms have the potential to be biomarkers.
2.9. HOTAIR
HOTAIR is a lncRNA overexpressed in a variety of cancer cells, including lung cancer, hepatocellular carcinoma, and colorectal cancer. It is related to the prognosis of cancer patients [18,94]. A recent study extensively investigated the association of HOTAIR polymorphisms with different cancer risks [95]. The SNPs of rs4759314, rs920778, rs12826786, rs874945, and rs12427129 are all related to cancer risk. Through a study of 467 patients who received platinum chemotherapy, HOTAIR was overexpressed in cisplatin-resistant A549 cells, which were resistant to cisplatin by regulating p21 [26]. High expression of HOTAIR was observed in diffuse large B-cell lymphoma cells and correlated with chemoresistance [96]. It promoted cell growth and inhibited apoptosis by regulating H3K27me3 and activating the PI3K/AKT/NF-κB pathway, which was thought to be the mechanism by which HOTAIR regulates the resistance of large B-cell lymphoma to diffuse prednisone [97]. In addition, HOTAIR was thought to be involved in the resistance of diffuse large B-cell lymphoma to prednisone by regulating miR-130a [98]. Recent studies have shown that HOTAIR affects the chemotherapy resistance of patients with gastrointestinal stromal tumors by combining with miR-130a [99]. It is known that miR-130a-3p has the binding site of ATG2B’s 3′-UTR and encodes an autophagy-related protein [100], thereby regulating chemoresistance [101]. Moreover, HOTAIR rs7958904 may affect platinum-based chemotherapy by affecting the function or expression of HOTAIR. In addition, squamous cell carcinoma patients with HOTAIR rs7958904 were more likely to develop severe hematological toxicity after platinum-based chemotherapy. Even though the mechanism of its action needs further research to prove, we already know that HOTAIR polymorphisms were associated with cancer risk and the toxicity of cisplatin-based chemotherapy.
2.10. Other LncRNAs
In addition to the above, some other important lncRNAs have also been found to play an interesting role in chemotherapy resistance, and their expression levels are regulated by their polymorphisms. The expression of lncRNA TP73 Antisense RNA 1 (TP73-AS1) is high in glioblastoma multiforme, and high expression is positively correlated with poor prognosis [102]. Further studies confirmed that the up-regulation of TP73-AS1 promotes resistance of glioblastoma cancer stem cells to temozolomide by regulating the expression of metabolism-related genes and aldehyde dehydrogenase 1 family member A1 (ALDH1A1). Rs3737589 G genotype carriers had higher expression levels of TP73-AS1 than A genotype carriers [103]. Moreover, the TP73-AS1 polymorphisms have also been revealed to be related to the risk of gastric cancer, in which rs3737589 SNP can be used as a potential biomarker for the prognosis of gastric cancer patients. Previous studies have shown that Growth Arrest Specific 5 (GAS5) is a potential tumor suppressor [104] and is down-regulated in a variety of cancers [105,106,107]. Rs17359906 and rs1951625 G genotype carriers have a higher risk of recurrence than A genotype carriers after chemotherapy [108]. Subsequently, researchers found that the expression level of GAS5 Rs55829688 with CC genotype carriers was significantly higher than that of TT and TC genotype carriers [109]. Recent studies have found that GAS5, as the endogenous “sponge” of miR-221-3p, participates in ABCB1-mediated adriamycin resistance of breast cancer by regulating the miR-221-3p/DKK2/WNT/β-catenin signaling pathway [110]. Similarly, lncRNA Nuclear Paraspeckle Assembly Transcript 1 (NEAT1) was indicated to be lowly expressed in nasopharyngeal carcinoma cells that are resistant to histone deacetylase inhibitors and could improve the resistance of nasopharyngeal carcinoma to histone deacetylase inhibitors by regulating the miR-129/Bcl-2 axis [111]. SNP of rs3825071 affects its expression level [112]. Although there is no direct conclusion to prove the direct effect of these lncRNAs polymorphisms on chemotherapy response, based on the existing evidence, we speculate that the above three lncRNAs polymorphisms also affect chemotherapy resistance and deserve further exploration.
3. Discussion
According to current research, lncRNAs SNPs can be used as potential biomarkers for cancer screening and diagnosis, and even as cancer treatment targets. Recent bioinformatics analysis has shown that H19 can be used as an independent posterior factor of low-grade glioma [43]. In terms of cancer recurrence risk, lncRNA GAS5 rs17359906 and rs1951625 G genotype were significantly associated with high recurrence rates after chemotherapy [108]. The SNPs of KCNQ1OT1 rs7128926 and rs7939976 have been shown to independently predict the recurrence-free survival and overall survival of gastric cancer patients [113]. Currently, chemotherapy is the main treatment method adopted by many cancer patients to prolong life and/or restore health. However, in many cancer patients receiving chemotherapy, there are still important unavoidable challenges, such as significant chemotherapy resistance, including intrinsic and acquired resistance [114]. Therefore, it is imperative to elucidate the mechanism of drug resistance and develop new immunosuppressants for cancer patients. Among chemotherapy resistance, most arise from acquired drug resistance, which is usually related to the expression of the MDR1 gene [115]. The generation and degree of drug resistance vary among individuals, and small mutations in the expression of non-coding genes caused by lncRNAs polymorphisms may play an important role in this process. H19 polymorphisms have been proven to regulate the methylation of the MDR1 promoter in liver cancer cells, resulting in chemotherapy resistance [42]. In recent years, the direct or indirect regulation of the p53 tumor suppressor pathway by lncRNA has also attracted the attention of researchers. P53 participates in all steps of tumor initiation and development by regulating the expression of downstream genes, including DNA replication, transcription, and repair, thereby affecting the chemotherapy resistance of cancer cells [24]. Some lncRNAs polymorphisms also affect chemotherapy response by regulating PI3K/AKT/NF-κB, EMT and miRNA and by other ways (Figure 1).
Additionally, the toxicity of chemotherapy also seriously affects the patients’ survival and quality of life. Blood toxicity, gastrointestinal reactions, and liver and kidney function abnormalities all make cancer patients suffer psychological and physical stress in addition to cancer pain. Therefore, discovering more polymorphisms related to chemotherapy resistance and chemotherapy toxicity has an important practical significance for precise cancer treatment. Based on these study outcomes, lncRNAs are highly expressed in cancer cells, and their polymorphisms are the cause of their abnormal expression and/or structural abnormality. It then affects the function of its downstream genes or proteins, leading to changes in the sensitivity of cancer cells to drugs. It ultimately affects the response to chemotherapy, cancer progression, survival, and recurrence rates of cancer patients. In this review, our focus is limited to the impact of lncRNAs on cancer chemotherapy response and sensitivity since there are only a few studies on lncRNAs polymorphisms on cancer radiotherapy response or other physical therapy. In terms of the relevant mechanism, most of the content is not clear, and further exploration and confirmation are needed. There are also some lncRNAs that are also worthy of further exploration due to their close correlation between polymorphisms and expression levels, for example, TP73-AS1, GAS5, and NEAT1, even though we could not find direct evidence that their regulation of chemoresistance is affected by their polymorphisms.
4. Conclusions
In this review, we analyzed recently identified gene polymorphisms of lncRNAs affecting the response of chemotherapeutic drugs. Because the functional roles of these lncRNAs are largely unresolved, we have limited knowledge of the molecular mechanisms of their polymorphisms. The studies of MIR2052HG, LINK-A, MEG3, and ANRIL have revealed that their polymorphisms may regulate either the expression or the structure of functional lncRNAs, thereby exerting biological effects; however, more mechanisms are expected to be discovered based on detailed studies of RNA-protein and RNA–DNA interactions. In conclusion, the polymorphisms of lncRNAs may serve as a biomarker for predicting the response of cancer patients to chemotherapy. Clinically, suitable chemotherapy drugs can be selected according to the polymorphisms of different patients.
Acknowledgments
Y.-R.L. acknowledges funding from the Shanghai Thousand Talents program and Fudan University.
Author Contributions
Y.-R.L. and Z.G. were involved in the design of the review. M.G. and Z.Z. wrote the first draft of the manuscript. Z.G. and Y.-R.L. provided scientific advice and revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research receives no external funding.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no potential conflicts of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Costa F.F. Non-Coding RNAs, Meet Thy Masters. BioEssays. 2010;32:599–608. doi: 10.1002/bies.200900112. [DOI] [PubMed] [Google Scholar]
- 2.Rinn J.L., Chang H.Y. Genome Regulation by Long Noncoding RNAs. Annu. Rev. Biochem. 2012;81:145–166. doi: 10.1146/annurev-biochem-051410-092902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mas A.M., Huarte M. LncRNA-DNA Hybrids Regulate Distant Genes. EMBO Rep. 2020;21:e50107. doi: 10.15252/embr.202050107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang K., Sun T., Li N., Wang Y., Wang J.-X., Zhou L.-Y., Long B., Liu C.-Y., Liu F., Li P.-F. MDRL LncRNA Regulates the Processing of miR-484 Primary Transcript by Targeting miR-361. PLoS Genet. 2014;10:e1004467. doi: 10.1371/journal.pgen.1004467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang J., Han C., Song K., Chen W., Ungerleider N., Yao L., Ma W., Wu T. The Long-Noncoding RNA MALAT1 Regulates TGF-Beta/Smad Signaling through Formation of a LncRNA-Protein Complex with Smads, SETD2 and PPM1A in Hepatic Cells. PLoS ONE. 2020;15:e0228160. doi: 10.1371/journal.pone.0228160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kanduri C. Long Noncoding RNAs, Lessons from Genomic Imprinting. Biochim. Biophys. Acta. 2016;1859:102–111. doi: 10.1016/j.bbagrm.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 7.Rinn J.L., Kertesz M., Wang J.K., Squazzo S.L., Xu X., Brugmann S.A., Goodnough L.H., Helms J.A., Farnham P.J., Segal E., et al. Functional Demarcation of Active and Silent Chromatin Domains in Human HOX Loci by Noncoding RNAs. Cell. 2007;129:1311–1323. doi: 10.1016/j.cell.2007.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li J.H., Liu S., Zhou H., Qu L.H., Yang J.H. Starbase V2.0, Decoding MiRNA-CeRNA, MiRNA-NcRNA and Protein-RNA Interaction Networks from Large-Scale Clip-Seq Data. Nucleic Acids Res. 2014;42:D92–D97. doi: 10.1093/nar/gkt1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li Q., Zhang C., Chen R., Xiong H., Qiu F., Liu S., Zhang M., Wang F., Wang Y., Zhou X., et al. Disrupting MALAT1/miR-200c Sponge Decreases Invasion and Migration in Endometrioid Endometrial Carcinoma. Cancer Lett. 2016;383:28–40. doi: 10.1016/j.canlet.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 10.Lin C., Yang L. Long Noncoding RNA in Cancer, Wiring Signaling Circuitry. Trends Cell Biol. 2018;28:287–301. doi: 10.1016/j.tcb.2017.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Han P., Li J.W., Zhang B.M., Lv J.C., Li Y.M., Gu X.Y., Yu Z.W., Jia Y.H., Bai X.F., Li L., et al. The LncRNA CRNDE Promotes Colorectal Cancer Cell Proliferation and Chemoresistance Via miR-181a-5p-Mediated Regulation of Wnt/Beta-Catenin Signaling. Mol. Cancer. 2017;16:9. doi: 10.1186/s12943-017-0583-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.He B.S., Sun H.L., Xu T., Pan Y.Q., Lin K., Gao T.Y., Zhang Z.Y., Wang S.K. Association of Genetic Polymorphisms in the LncRNAs with Gastric Cancer Risk in a Chinese Population. J. Cancer. 2017;8:531–536. doi: 10.7150/jca.17519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hurgobin B., Edwards D. SNP Discovery Using a Pangenome, Has the Single Reference Approach Become Obsolete? Biology. 2017;6:21. doi: 10.3390/biology6010021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abdi E., Latifi-Navid S., Latifi-Navid H., Safaralizadeh R. LncRNA Polymorphisms and Upper Gastrointestinal Cancer Risk. Pathol. Res. Pract. 2021;218:153324. doi: 10.1016/j.prp.2020.153324. [DOI] [PubMed] [Google Scholar]
- 15.Ghafouri-Fard S., Taheri M. Expressed Gene 3 (MEG3), A Tumor Suppressor Long Non Coding RNA. Biomed. Pharmacother. 2019;118:109129. doi: 10.1016/j.biopha.2019.109129. [DOI] [PubMed] [Google Scholar]
- 16.Fan Z., Chen X., Liu L., Zhu C., Xu J., Yin X., Sheng Y., Zhu Z., Wen L., Zuo X., et al. Association of the Polymorphism Rs13259960 in Slear with Predisposition to Systemic Lupus Erythematosus. Arthritis Rheumatol. 2020;72:985–996. doi: 10.1002/art.41200. [DOI] [PubMed] [Google Scholar]
- 17.Piskin I., Akcan G., Firat A., Tufan A.C. A Single-Nucleotide Polymorphism (Rs8176070) of LncRNA Part1 May Reflect the Risk for Knee Osteoarthritis. Eur. J. Rheumatol. 2020;7:88–89. doi: 10.5152/eurjrheum.2020.19210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gong W.-J., Peng J.-B., Yin J.-Y., Li X.-P., Zheng W., Xiao L., Tan L.-M., Xiao D., Chen Y.-X., Li X., et al. Association between Well-Characterized Lung Cancer LncRNA Polymorphisms and Platinum-Based Chemotherapy Toxicity in Chinese Patients with Lung Cancer. Acta Pharmacol. Sin. 2017;38:581–590. doi: 10.1038/aps.2016.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin A., Hu Q., Li C., Xing Z., Ma G., Wang C., Li J., Ye Y., Yao J., Liang K., et al. The Link—A LncRNA Interacts with Ptdins(3,4,5)P3 to Hyperactivate AKT and Confer Resistance to AKT Inhibitors. Nat. Cell Biol. 2017;19:238–251. doi: 10.1038/ncb3473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu C., Liu M., Jia D., Tao T., Hao D. LncRNA TINCR SNPS and Expression Levels Are Associated with Bladder Cancer Susceptibility. Genet. Test Mol. Biomarkers. 2021;25:31–41. doi: 10.1089/gtmb.2020.0178. [DOI] [PubMed] [Google Scholar]
- 21.Ingle J.N., Xie F., Ellis M.J., Goss P.E., Shepherd L.E., Chapman J.-A.W., Chen B.E., Kubo M., Furukawa Y., Momozawa Y., et al. Genetic Polymorphisms in the Long Noncoding RNA miR2052HG Offer a Pharmacogenomic Basis for the Response of Breast Cancer Patients to Aromatase Inhibitor Therapy. Cancer Res. 2016;23:7012. doi: 10.1158/0008-5472.CAN-16-1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cairns J., Ingle J.N., Kalari K.R., Shepherd L.E., Kubo M., Goetz M.P., Weinshilboum R.M., Wang L. The LncRNA miR2052HG Regulates Eralpha Levels and Aromatase Inhibitor Resistance through LMTK3 by Recruiting EGR1. Breast Cancer Res. 2019;21:47. doi: 10.1186/s13058-019-1130-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bayarmaa B., Wu Z., Peng J., Wang Y., Xu S., Yan T., Yin W., Lu J., Zhou L. Association of LncRNA MEG3 Polymorphisms with Efficacy of Neoadjuvant Chemotherapy in Breast Cancer. BMC Cancer. 2019;19:877. doi: 10.1186/s12885-019-6077-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang Y., Guo Z., Zhao Y., Jin Y., An L., Wu B., Liu Z., Chen X., Chen X., Zhou H., et al. Genetic Polymorphisms of LncRNA-P53 Regulatory Network Genes Are Associated with Concurrent Chemoradiotherapy Toxicities and Efficacy in Nasopharyngeal Carcinoma Patients. Sci. Rep. 2017;7:8320. doi: 10.1038/s41598-017-08890-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zeng Y., Li T.-L., Zhang H.-B., Deng J.-L., Zhang R., Sun H., Wan Z.-R., Liu Y.-Z., Zhu Y.-S., Wang G. Polymorphisms in IGF2/H19 Gene Locus Are Associated with Platinum-Based Chemotherapeutic Response in Chinese Patients with Epithelial Ovarian Cancer. Pharmacogenomics. 2019;20:179–188. doi: 10.2217/pgs-2018-0153. [DOI] [PubMed] [Google Scholar]
- 26.Lampropoulou D.-I., Aravantinos G., Katifelis H., Lazaris F., Laschos K., Theodosopoulos T., Papadimitriou C., Gazouli M. Long Non-Coding RNA Polymorphisms and Prediction of Response to Chemotherapy Based on Irinotecan in Patients with Metastatic Colorectal Cancer. Cancer Biomarks. 2019;25:213–221. doi: 10.3233/CBM-182383. [DOI] [PubMed] [Google Scholar]
- 27.Hu L., Chen S.-H., Lv Q.-L., Sun B., Qu Q., Qin C.-Z., Fan L., Guo Y., Cheng L., Zhou H.-H. Clinical Significance of Long Non-Coding RNA Casc8 Rs10505477 Polymorphism in Lung Cancer Susceptibility, Platinum-Based Chemotherapy Response, and Toxicity. Int. J. Environ. Res. Public Health. 2016;13:545. doi: 10.3390/ijerph13060545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Melzer D., Perry J.R., Hernandez D., Corsi A.M., Stevens K., Rafferty I., Lauretani F., Murray A., Gibbs J.R., Paolisso G., et al. A Genome-Wide Association Study Identifies Protein Quantitative Trait Loci (PQTLS) PLoS Genet. 2008;4:e1000072. doi: 10.1371/journal.pgen.1000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ma C.X., Reinert T., Chmielewska I., Ellis M.J. Mechanisms of Aromatase Inhibitor Resistance. Nat. Rev. Cancer. 2015;15:261–275. doi: 10.1038/nrc3920. [DOI] [PubMed] [Google Scholar]
- 30.Stebbing J., Filipovic A., Lit L.C., Blighe K., Grothey A., Xu Y., Miki Y., Chow L.W., Coombes R.C., Sasano H., et al. LMTK3 Is Implicated in Endocrine Resistance Via Multiple Signaling Pathways. Oncogene. 2013;32:3371–3380. doi: 10.1038/onc.2012.343. [DOI] [PubMed] [Google Scholar]
- 31.Feng S.Q., Zhang X.Y., Fan H.T., Sun Q.J., Zhang M. Up-Regulation of LncRNA MEG3 Inhibits Cell Migration and Invasion and Enhances Cisplatin Chemosensitivity in Bladder Cancer Cells. Neoplasma. 2018;65:925–932. doi: 10.4149/neo_2018_180125N55. [DOI] [PubMed] [Google Scholar]
- 32.Wei G.H., Wang X. LncRNA MEG3 Inhibit Proliferation and Metastasis of Gastric Cancer via P53 Signaling Pathway. Eur. Rev. Med. Pharmacol. Sci. 2017;21:3850–3856. [PubMed] [Google Scholar]
- 33.Wang C., Nie H., Li Y., Liu G., Wang X., Xing S., Zhang L., Chen X., Chen Y., Li Y. The Study of the Relation of DNA Repair Pathway Genes SNPS and the Sensitivity to Radiotherapy and Chemotherapy of NSCLC. Sci. Rep. 2016;6:26526. doi: 10.1038/srep26526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peng J., Zhang L., Yuan C., Zhou L., Xu S., Lin Y., Zhang J., Yin W., Lu J. Expression Profile Analysis of Long Noncoding RNA in Er-Positive Subtype Breast Cancer Using Microarray Technique and Bioinformatics. Cancer. Manag. Res. 2017;9:891–901. doi: 10.2147/CMAR.S151120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cao X., Zhuang S., Hu Y., Xi L., Deng L., Sheng H., Shen W. Associations between Polymorphisms of Long Non-Coding RNA MEG3 and Risk of Colorectal Cancer in Chinese. Oncotarget. 2016;7:19054–19059. doi: 10.18632/oncotarget.7764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu J., Wan L., Lu K., Sun M., Pan X., Zhang P., Lu B., Liu G., Wang Z. The Long Noncoding RNA MEG3 Contributes to Cisplatin Resistance of Human Lung Adenocarcinoma. PLoS ONE. 2015;10:e0114586. doi: 10.1371/journal.pone.0114586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xia Y., He Z., Liu B., Wang P., Chen Y. Downregulation of MEG3 Enhances Cisplatin Resistance of Lung Cancer Cells through Activation of the Wnt/Beta-Catenin Signaling Pathway. Mol. Med. Rep. 2015;12:4530–4537. doi: 10.3892/mmr.2015.3897. [DOI] [PubMed] [Google Scholar]
- 38.Zhang A., Xu M., Mo Y.Y. Role of the LncRNA-P53 Regulatory Network in Cancer. J. Mol. Cell. Biol. 2014;6:181–191. doi: 10.1093/jmcb/mju013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gong W.J., Yin J.Y., Li X.P., Fang C., Xiao D., Zhang W., Zhou H.H., Li X., Liu Z.Q. Association of Well-Characterized Lung Cancer LncRNA Polymorphisms with Lung Cancer Susceptibility and Platinum-Based Chemotherapy Response. Tumour Biol. 2016;37:8349–8358. doi: 10.1007/s13277-015-4497-5. [DOI] [PubMed] [Google Scholar]
- 40.Lottin S., Adriaenssens E., Dupressoir T., Berteaux N., Montpellier C., Coll J., Dugimont T., Curgy J.J. Overexpression of an Ectopic H19 Gene Enhances the Tumorigenic Properties of Breast Cancer Cells. Carcinogenesis. 2002;23:1885–1895. doi: 10.1093/carcin/23.11.1885. [DOI] [PubMed] [Google Scholar]
- 41.Yang F., Bi J., Xue X., Zheng L., Zhi K., Hua J., Fang G. Up-Regulated Long Non-Coding RNA H19 Contributes to Proliferation of Gastric Cancer Cells. FEBS J. 2012;279:3159–3165. doi: 10.1111/j.1742-4658.2012.08694.x. [DOI] [PubMed] [Google Scholar]
- 42.Tsang W.P., Kwok T.T. Riboregulator H19 Induction of Mdr1-Associated Drug Resistance in Human Hepatocellular Carcinoma Cells. Oncogene. 2007;26:4877–4881. doi: 10.1038/sj.onc.1210266. [DOI] [PubMed] [Google Scholar]
- 43.Xiao Y., Zhu Z., Li J., Yao J., Jiang H., Ran R., Li X., Li Z. Expression and Prognostic Value of Long Non-Coding RNA H19 in Glioma Via Integrated Bioinformatics Analyses. Aging. 2020;12:3407–3430. doi: 10.18632/aging.102819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guo Q.-Y., Wang H., Wang Y. LncRNA H19 Polymorphisms Associated with the Risk of Oscc in Chinese Population. Eur. Rev. Med. Pharmacol. Sci. 2017;21:3770–3774. [PubMed] [Google Scholar]
- 45.He T.-D., Xu D., Sui T., Zhu J.-K., Wei Z.-X., Wang Y.-M. Association between H19 Polymorphisms and Osteosarcoma Risk. Eur. Rev. Med. Pharmacol. Sci. 2017;21:3775–3780. [PubMed] [Google Scholar]
- 46.Hua Q., Lv X., Gu X., Chen Y., Chu H., Du M., Gong W., Wang M., Zhang Z. Genetic Variants in LncRNA H19 Are Associated with the Risk of Bladder Cancer in a Chinese Population. Mutagenesis. 2016;31:531–538. doi: 10.1093/mutage/gew018. [DOI] [PubMed] [Google Scholar]
- 47.Yang C., Tang R., Ma X., Wang Y., Luo D., Xu Z., Zhu Y., Yang L. Tag SNPs in Long Non-Coding RNA H19 Contribute to Susceptibility to Gastric Cancer in the Chinese Han Population. Oncotarget. 2015;6:15311–15320. doi: 10.18632/oncotarget.3840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yang M.L., Huang Z., Wang Q., Chen H.H., Ma S.N., Wu R., Cai W.S. The Association of Polymorphisms in LncRNA-H19 with Hepatocellular Cancer Risk and Prognosis. Biosci. Rep. 2018;38 doi: 10.1042/BSR20171652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhu Q.-N., Wang G., Guo Y., Peng Y., Zhang R., Deng J.-L., Li Z.-X., Zhu Y.-S. LncRNA H19 Is a Major Mediator of Doxorubicin Chemoresistance in Breast Cancer Cells through a Cullin4a-MDR1 Pathway. Oncotarget. 2017;8:91990–92003. doi: 10.18632/oncotarget.21121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yu S., Wu C., Tan Q., Liu H. Long Noncoding RNA H19 Promotes Chemotherapy Resistance in Choriocarcinoma Cells. J. Cell. Biochem. 2019;120:15131–15144. doi: 10.1002/jcb.28775. [DOI] [PubMed] [Google Scholar]
- 51.Chen S., Huo X., Lin Y., Ban H., Lin Y., Li W., Zhang B., Au W.W., Xu X. Association of Mdr1 and Ercc1 Polymorphisms with Response and Toxicity to Cisplatin-Based Chemotherapy in Non-Small-Cell Lung Cancer Patients. Int. J. Hyg. Environ. Health. 2010;213:140–145. doi: 10.1016/j.ijheh.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 52.Wang J., Xie S., Yang J., Xiong H., Jia Y., Zhou Y., Chen Y., Ying X., Chen C., Ye C., et al. The Long Noncoding RNA H19 Promotes Tamoxifen Resistance in Breast Cancer Via Autophagy. J. Hematol. Oncol. 2019;12:81. doi: 10.1186/s13045-019-0747-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu E.-R., Hsieh M.-J., Chiang W.-L., Hsueh K.-C., Yang S.-F., Su S.-C. Association of LncRNA CCAT2 and CASC8 Gene Polymorphisms with Hepatocellular Carcinoma. Int. J. Environ. Res. Public. Health. 2019;16:2833. doi: 10.3390/ijerph16162833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yang B., Thyagarajan B., Gross M.D., Goodman M., Sun Y.V., Bostick R.M. Genetic Variants at Chromosome 8q24, Colorectal Epithelial Cell Proliferation, and Risk for Incident, Sporadic Colorectal Adenomas. Mol. Carcinog. 2014;53:E187–E192. doi: 10.1002/mc.22047. [DOI] [PubMed] [Google Scholar]
- 55.Zhang Y., Wu Y., Jia Z., Cao D., Yang N., Wang Y., Cao X., Jiang J. Long Non-Coding RNA Polymorphisms on 8q24 Are Associated with the Prognosis of Gastric Cancer in a Chinese Population. PeerJ. 2020;8:e8600. doi: 10.7717/peerj.8600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cui Z., Gao M., Yin Z., Yan L., Cui L. Association between LncRNA Casc8 Polymorphisms and the Risk of Cancer, A Meta-Analysis. Cancer Manag. Res. 2018;10:3141–3148. doi: 10.2147/CMAR.S170783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gargallo C.J., Lanas Á., Carrera-Lasfuentes P., Ferrandez Á., Quintero E., Carrillo M., Alonso-Abreu I., García-Gonzalez M.A. Genetic Susceptibility in the Development of Colorectal Adenomas According to Family History of Colorectal Cancer. Int. J. Cancer. 2019;144:489–502. doi: 10.1002/ijc.31858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shen L., Du M., Wang C., Gu D., Wang M., Zhang Q., Zhao T., Zhang X., Tan Y., Huo X., et al. Clinical Significance of POU5F1P1 Rs10505477 Polymorphism in Chinese Gastric Cancer Patients Receving Cisplatin-Based Chemotherapy after Surgical Resection. Int. J. Mol. Sci. 2014;15:12764–12777. doi: 10.3390/ijms150712764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ma G., Gu D., Lv C., Chu H., Xu Z., Tong N., Wang M., Tang C., Xu Y., Zhang Z., et al. Genetic Variant in 8q24 Is Associated with Prognosis for Gastric Cancer in a Chinese Population. J. Gastroenterol. Hepatol. 2015;30:689–695. doi: 10.1111/jgh.12801. [DOI] [PubMed] [Google Scholar]
- 60.Panagopoulos I., Möller E., Collin A., Mertens F. The Pou5f1p1 Pseudogene Encodes a Putative Protein Similar to Pou5f1 Isoform 1. Oncol. Rep. 2008;20:1029–1033. doi: 10.3892/or_00000105. [DOI] [PubMed] [Google Scholar]
- 61.Hosokawa Y., Takahashi H., Inoue A., Kawabe Y., Funahashi Y., Kameda K., Sugimoto K., Yano H., Harada H., Kohno S., et al. Oct-3/4 Modulates the Drug-Resistant Phenotype of Glioblastoma Cells through Expression of ATP Binding Cassette Transporter G2. Biochim. Biophys. Acta. 2015;1850:1197–1205. doi: 10.1016/j.bbagen.2015.01.017. [DOI] [PubMed] [Google Scholar]
- 62.Ota S., Ishii G., Goto K., Kubota K., Kim Y.H., Kojika M., Murata Y., Yamazaki M., Nishiwaki Y., Eguchi K., et al. Immunohistochemical Expression of BCRP and ERCC1 in Biopsy Specimen Predicts Survival in Advanced Non-Small-Cell Lung Cancer Treated with Cisplatin-Based Chemotherapy. Lung Cancer. 2009;64:98–104. doi: 10.1016/j.lungcan.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 63.Jiang X., Guan J., Xu Y., Ren H., Jiang J., Wudu M., Wang Q., Su H., Zhang Y., Zhang B., et al. Silencing of CASC8 Inhibits Non-Small Cell Lung Cancer Cells Function and Promotes Sensitivity to Osimertinib Via FOXM1. J. Cancer. 2021;12:387–396. doi: 10.7150/jca.47863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bella L., Zona S., Nestal G., de Moraes G.N., Lam E.W.-F. FOXM1: A Key Oncofoetal Transcription Factor in Health and Disease. Semin. Cancer Biol. 2014;29:32–39. doi: 10.1016/j.semcancer.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 65.Luo J., Manning B.D., Cantley L.C. Targeting the Pi3k-Akt Pathway in Human Cancer, Rationale and Promise. Cancer Cell. 2003;4:257–262. doi: 10.1016/S1535-6108(03)00248-4. [DOI] [PubMed] [Google Scholar]
- 66.Vivanco I., Sawyers C.L. The Phosphatidylinositol 3-Kinase Akt Pathway in Human Cancer. Nat. Rev. Cancer. 2002;2:489–501. doi: 10.1038/nrc839. [DOI] [PubMed] [Google Scholar]
- 67.Stokoe D., Stephens L.R., Copeland T., Gaffney P.R.J., Reese C.B., Painter G.F., Holmes A.B., McCormick F., Hawkins P.T. Dual Role of Phosphatidylinositol-3,4,5-Trisphosphate in the Activation of Protein Kinase B. Science. 1997;277:567–570. doi: 10.1126/science.277.5325.567. [DOI] [PubMed] [Google Scholar]
- 68.Duffy M.J., Synnott N.C., Crown J. Mutant P53 in Breast Cancer, Potential as a Therapeutic Target and Biomarker. Breast Cancer Res. Treat. 2018;170:213–219. doi: 10.1007/s10549-018-4753-7. [DOI] [PubMed] [Google Scholar]
- 69.Li C., Zhao Z., Zhou Z., Liu R. Linc-ROR Confers Gemcitabine Resistance to Pancreatic Cancer Cells Via Inducing Autophagy and Modulating the miR-124/PTBP1/PKM2 Axis. Cancer Chemother. Pharmacol. 2016;78:1199–1207. doi: 10.1007/s00280-016-3178-4. [DOI] [PubMed] [Google Scholar]
- 70.Zhang Y., Wu W., Sun Q., Ye L., Zhou D., Wang W. Linc-ROR Facilitates Hepatocellular Carcinoma Resistance to Doxorubicin by Regulating Twist1-Mediated Epithelial-Mesenchymal Transition. Mol. Med. Rep. 2021;23:340. doi: 10.3892/mmr.2021.11979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Luo C., Cao J., Peng R., Guo Q., Ye H., Wang P., Wang K., Song C. Functional Variants in Linc-ROR Are Associated with MRNA Expression of Linc-ROR and Breast Cancer Susceptibility. Sci. Rep. 2018;8:4680. doi: 10.1038/s41598-018-22881-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ji P., Diederichs S., Wang W., Boing S., Metzger R., Schneider P.M., Tidow N., Brandt B., Buerger H., Bulk E., et al. MALAT-1, a Novel Noncoding RNA, and Thymosin Beta4 Predict Metastasis and Survival in Early-Stage Non-Small Cell Lung Cancer. Oncogene. 2003;22:8031–8041. doi: 10.1038/sj.onc.1206928. [DOI] [PubMed] [Google Scholar]
- 73.Wu S., Sun H., Wang Y., Yang X., Meng Q., Yang H., Zhu H., Tang W., Li X., Aschner M., et al. MALAT1 Rs664589 Polymorphism Inhibits Binding to miR-194-5p, Contributing to Colorectal Cancer Risk, Growth, and Metastasis. Cancer Res. 2019;79:5432–5441. doi: 10.1158/0008-5472.CAN-19-0773. [DOI] [PubMed] [Google Scholar]
- 74.Li P., Zhang X., Wang H., Wang L., Liu T., Du L., Yang Y., Wang C. MALAT1 is Associated with Poor Response to Oxaliplatin-Based Chemotherapy in Colorectal Cancer Patients and Promotes Chemoresistance through Ezh2. Mol. Cancer Ther. 2017;16:739–751. doi: 10.1158/1535-7163.MCT-16-0591. [DOI] [PubMed] [Google Scholar]
- 75.Ding H.H., Wu W.D., Jiang T., Cao J., Ji Z.Y., Jin J.H., Wang J.J., Song W.F., Wang L.W. Meta-Analysis Comparing the Safety and Efficacy of Metastatic Colorectal Cancer Treatment Regimens, Capecitabine Plus Irinotecan (CAPIRI) and 5-Fluorouracil/Leucovorin Plus Irinotecan (FOLFIRI) Tumour. Biol. 2015;36:3361–3369. doi: 10.1007/s13277-014-2970-1. [DOI] [PubMed] [Google Scholar]
- 76.Ratain M.J. Irinotecan Dosing, Does the Cpt in Cpt-11 Stand for Can’t Predict Toxicity? J. Clin. Oncol. 2002;20:7–8. doi: 10.1200/JCO.2002.20.1.7. [DOI] [PubMed] [Google Scholar]
- 77.Fujita K.-I., Kubota Y., Ishida H., Sasaki Y. Irinotecan, a Key Chemotherapeutic Drug for Metastatic Colorectal Cancer. World J. Gastroenterol. 2015;21:1223–1248. doi: 10.3748/wjg.v21.i43.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cao Q., Yu J., Dhanasekaran S.M., Kim J.H., Mani R.-S., Tomlins S.A., Mehra R., Laxman B., Cao X., Kleer C.G., et al. Repression of E-Cadherin by the Polycomb Group Protein Ezh2 in Cancer. Oncogene. 2008;27:7274–7284. doi: 10.1038/onc.2008.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Luo M., Li Z., Wang W., Zeng Y., Liu Z., Qiu J. Long Non-Coding RNA H19 Increases Bladder Cancer Metastasis by Associating with Ezh2 and Inhibiting E-Cadherin Expression. Cancer Lett. 2013;333:213–221. doi: 10.1016/j.canlet.2013.01.033. [DOI] [PubMed] [Google Scholar]
- 80.Yamasaki T., Seki N., Yoshino H., Itesako T., Hidaka H., Yamada Y., Tatarano S., Yonezawa T., Kinoshita T., Nakagawa M., et al. MicroRNA-218 Inhibits Cell Migration and Invasion in Renal Cell Carcinoma through Targeting Caveolin-2 Involved in Focal Adhesion Pathway. J. Urol. 2013;190:1059–1068. doi: 10.1016/j.juro.2013.02.089. [DOI] [PubMed] [Google Scholar]
- 81.Li P.L., Zhang X., Wang L.L., Du L.T., Yang Y.M., Li J., Wang C.X. MicroRNA-218 is a Prognostic Indicator in Colorectal Cancer and Enhances 5-Fluorouracil-Induced Apoptosis by Targeting Birc5. Carcinogenesis. 2015;36:1484–1493. doi: 10.1093/carcin/bgv145. [DOI] [PubMed] [Google Scholar]
- 82.Fang Z., Chen W., Yuan Z., Liu X., Jiang H. LncRNA-MALAT1 Contributes to the Cisplatin-Resistance of Lung Cancer by Upregulating Mrp1 and Mdr1 Via Stat3 Activation. Biomed. Pharmacother. 2018;101:536–542. doi: 10.1016/j.biopha.2018.02.130. [DOI] [PubMed] [Google Scholar]
- 83.Kong Y., Hsieh C.-H., Alonso L.C. ANRIL: A LncRNA at the CDKN2A/B Locus with Roles in Cancer and Metabolic Disease. Front. Endocrinol. 2018;9:405. doi: 10.3389/fendo.2018.00405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nie F.-Q., Sun M., Yang J.-S., Xie M., Xu T.-P., Xia R., Liu Y.-W., Liu X.-H., Zhang E.-B., Lu K.-H., et al. Long Noncoding RNA Anril Promotes Non-Small Cell Lung Cancer Cell Proliferation and Inhibits Apoptosis by Silencing KLF2 and P21 Expression. Mol. Cancer Ther. 2015;14:268–277. doi: 10.1158/1535-7163.MCT-14-0492. [DOI] [PubMed] [Google Scholar]
- 85.Lin L., Gu Z.-T., Chen W.-H., Cao K.-J. Increased Expression of the Long Non-Coding RNA ANRIL Promotes Lung Cancer Cell Metastasis and Correlates with Poor Prognosis. Diagn. Pathol. 2015;10:14. doi: 10.1186/s13000-015-0247-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Huang X., Zhang W., Shao Z. Association between Long Non-Coding RNA Polymorphisms and Cancer Risk, A Meta-Analysis. Biosci. Rep. 2018;38:BSR20180365. doi: 10.1042/BSR20180365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yap K.L., Li S., Munoz-Cabello A.M., Raguz S., Zeng L., Mujtaba S., Gil J., Walsh M.J., Zhou M.M. Molecular Interplay of the Noncoding RNA Anril and Methylated Histone H3 Lysine 27 by Polycomb CBX7 in Transcriptional Silencing of Ink4a. Mol. Cell. 2010;38:662–674. doi: 10.1016/j.molcel.2010.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yuan X.W., Zhu X.F., Huang X.F., Sheng P.Y., He A.S., Yang Z.B., Deng R., Feng G.K., Liao W.M. P14arf Sensitizes Human Osteosarcoma Cells to Cisplatin-Induced Apoptosis in a P53-Independent Manner. Cancer Biol. Ther. 2007;6:1074–1080. doi: 10.4161/cbt.6.7.4324. [DOI] [PubMed] [Google Scholar]
- 89.Al-Mohanna M.A., Manogaran P.S., Al-Mukhalafi Z., Al-Hussein K.A., Aboussekhra A. The Tumor Suppressor P16(Ink4a) Gene Is a Regulator of Apoptosis Induced by Ultraviolet Light and Cisplatin. Oncogene. 2004;23:201–212. doi: 10.1038/sj.onc.1206927. [DOI] [PubMed] [Google Scholar]
- 90.Xu R., Mao Y., Chen K., He W., Shi W., Han Y. The Long Noncoding RNA Anril Acts as an Oncogene and Contributes to Paclitaxel Resistance of Lung Adenocarcinoma A549 Cells. Oncotarget. 2017;8:39177–39184. doi: 10.18632/oncotarget.16640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Miao J.-T., Gao J.-H., Chen Y.-Q., Chen H., Meng H.-Y., Lou G. LncRNA Anril Affects the Sensitivity of Ovarian Cancer to Cisplatin Via Regulation of Let-7a/HMGA2 Axis. Biosci. Rep. 2019;39:BSR20182101. doi: 10.1042/BSR20182101. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 92.Wang X., Zhang G., Cheng Z., Dai L., Jia L., Jing X., Wang H., Zhang R., Liu M., Jiang T., et al. Knockdown of LncRNA Anril Inhibits the Development of Cisplatin Resistance by Upregulating miR98 in Lung Cancer Cells. Oncol. Rep. 2020;44:1025–1036. doi: 10.3892/or.2020.7685. [DOI] [PubMed] [Google Scholar]
- 93.Cunnington M.S., Koref M.S., Mayosi B.M., Burn J., Keavney B. Chromosome 9p21 Snps Associated with Multiple Disease Phenotypes Correlate with Anril Expression. PLoS Genet. 2010;6:e1000899. doi: 10.1371/journal.pgen.1000899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Nakagawa T., Endo H., Yokoyama M., Abe J., Tamai K., Tanaka N., Sato I., Takahashi S., Kondo T., Satoh K. Large Noncoding RNA Hotair Enhances Aggressive Biological Behavior and is Associated with Short Disease-Free Survival in Human Non-Small Cell Lung Cancer. Biochem. Biophys. Res. Commun. 2013;436:319–324. doi: 10.1016/j.bbrc.2013.05.101. [DOI] [PubMed] [Google Scholar]
- 95.Moazeni-Roodi A., Aftabi S., Sarabandi S., Karami S., Hashemi M., Ghavami S. Genetic Association between Hotair Gene and the Risk of Cancer, An Updated Meta-Analysis. J. Genet. 2020;99:1–16. doi: 10.1007/s12041-020-01214-w. [DOI] [PubMed] [Google Scholar]
- 96.Senousy M.A., El-Abd A.M., Abdel-Malek R.R., Rizk S.M. Circulating Long Non-Coding RNAs Hotair, Linc-P21, GAS5 and Xist Expression Profiles in Diffuse Large B-Cell Lymphoma, Association with R-Chop Responsiveness. Sci. Rep. 2021;11:2095. doi: 10.1038/s41598-021-81715-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Huang X., Qian W., Ye X. Long Noncoding RNAS in Diffuse Large B-Cell Lymphoma, Current Advances and Perspectives. Onco Targets Ther. 2020;13:4295–4303. doi: 10.2147/OTT.S253330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Coiffier B., Sarkozy C. Diffuse Large B-Cell Lymphoma: R-Chop Failure—What to Do? Hematol. Am. Soc. Hematol. Educ. Program. 2016;2016:366–378. doi: 10.1182/asheducation-2016.1.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zhang J., Chen K., Tang Y., Luan X., Zheng X., Lu X., Mao J., Hu L., Zhang S., Zhang X., et al. LncRNA-HOTAIR Activates Autophagy and Promotes the Imatinib Resistance of Gastrointestinal Stromal Tumor Cells through a Mechanism Involving the miR-130a/Atg2b Pathway. Cell Death Dis. 2021;12:367. doi: 10.1038/s41419-021-03650-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kovaleva V., Mora R., Park Y.J., Plass C., Chiramel A.I., Bartenschlager R., Dohner H., Stilgenbauer S., Pscherer A., Lichter P., et al. MiRNA-130a Targets ATG2B and DICER1 to Inhibit Autophagy and Trigger Killing of Chronic Lymphocytic Leukemia Cells. Cancer Res. 2012;72:1763–1772. doi: 10.1158/0008-5472.CAN-11-3671. [DOI] [PubMed] [Google Scholar]
- 101.Jiang B., Xue M., Xu D., Song J., Zhu S. Down-Regulated LncRNA Hotair Alleviates Polycystic Ovaries Syndrome in Rats by Reducing Expression of Insulin-Like Growth Factor 1 Via MicroRNA-130a. J. Cell. Mol. Med. 2020;24:451–464. doi: 10.1111/jcmm.14753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Mazor G., Levin L., Picard D., Ahmadov U., Caren H., Borkhardt A., Reifenberger G., Leprivier G., Remke M., Rotblat B. The LncRNA Tp73-As1 Is Linked to Aggressiveness in Glioblastoma and Promotes Temozolomide Resistance in Glioblastoma Cancer Stem Cells. Cell Death Dis. 2019;10:246. doi: 10.1038/s41419-019-1477-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chen W., Xiao J., Shi L., Lin L., Jiang M., Ge Y., Li Z., Fan H., Yang L., Xu Z. Association of Tp73-As1 Gene Polymorphisms with the Risk and Survival of Gastric Cancer in a Chinese Han Population. Artif. Cells Nanomed. Biotechnol. 2019;47:3814–3822. doi: 10.1080/21691401.2019.1669621. [DOI] [PubMed] [Google Scholar]
- 104.Mourtada-Maarabouni M., Pickard M.R., Hedge V.L., Farzaneh F., Williams G.T. GAS5, a Non-Protein-Coding RNA, Controls Apoptosis and Is Downregulated in Breast Cancer. Oncogene. 2009;28:195–208. doi: 10.1038/onc.2008.373. [DOI] [PubMed] [Google Scholar]
- 105.Qiao H.-P., Gao W.-S., Huo J.-X., Yang Z.-S. Long Non-Coding RNA GAS5 Functions as a Tumor Suppressor in Renal Cell Carcinoma. Asian Pac. J. Cancer Prev. 2013;14:1077–1082. doi: 10.7314/APJCP.2013.14.2.1077. [DOI] [PubMed] [Google Scholar]
- 106.Shi X., Sun M., Liu H., Yao Y., Kong R., Chen F., Song Y. A Critical Role for the Long Non-Coding RNA GAS5 in Proliferation and Apoptosis in Non-Small-Cell Lung Cancer. Mol. Carcinog. 2015;54:E1–E12. doi: 10.1002/mc.22120. [DOI] [PubMed] [Google Scholar]
- 107.Sun M., Jin F.-Y., Xia R., Kong R., Li J.-H., Xu T.-P., Liu Y.-W., Zhang E.-B., Liu X.-H., De W. Decreased Expression of Long Noncoding RNA GAS5 Indicates a Poor Prognosis and Promotes Cell Proliferation in Gastric Cancer. BMC Cancer. 2014;14:319. doi: 10.1186/1471-2407-14-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zhao L., Zheng W., Li C. Association of Long-Chain Non-Coding RNA GAS5 Gene Polymorphisms with Prostate Cancer Risk and Prognosis in Chinese Han Population. Medicine. 2020;99:e21790. doi: 10.1097/MD.0000000000021790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Yan H., Zhang D.-Y., Li X., Yuan X.-Q., Yang Y.-L., Zhu K.-W., Zeng H., Li X.-L., Cao S., Zhou H.-H., et al. Long Non-Coding RNA GAS5 Polymorphism Predicts a Poor Prognosis of Acute Myeloid Leukemia in Chinese Patients Via Affecting Hematopoietic Reconstitution. Leuk. Lymphoma. 2017;58:1948–1957. doi: 10.1080/10428194.2016.1266626. [DOI] [PubMed] [Google Scholar]
- 110.Chen Z., Pan T., Jiang D., Jin L., Geng Y., Feng X., Shen A., Zhang L. The LncRNA-GAS5/miR-221-3p/DKK2 Axis Modulates ABCB1-Mediated Adriamycin Resistance of Breast Cancer Via the Wnt/Beta-Catenin Signaling Pathway. Mol. Ther. Nucleic Acids. 2020;19:1434–1448. doi: 10.1016/j.omtn.2020.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Xue F., Cheng Y., Xu L., Tian C., Jiao H., Wang R., Gao X. LncRNA Neat1/miR-129/Bcl-2 Signaling Axis Contributes to Hdac Inhibitor Tolerance in Nasopharyngeal Cancer. Aging. 2020;12:1417–1488. doi: 10.18632/aging.103427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ji X., Yan Y., Ma N., He G., Wang K., Zhang Y., Yin J., Song C., Wang P., Ye H., et al. Variant of SNPs at LncRNA Neat1 Contributes to Gastric Cancer Susceptibility in Chinese Han Population. Int. J. Clin. Oncol. 2021;26:694–700. doi: 10.1007/s10147-020-01852-1. [DOI] [PubMed] [Google Scholar]
- 113.Yang Z., Yuan L., Yang L., Peng S., Yang P., He X., Bao G. Association Study between Kcnq1 and Kcnq1ot1 Genetic Polymorphisms and Gastric Cancer Susceptibility and Survival in a Chinese Han Population, A Case-Control Study. Ann. Transl. Med. 2021;9:156. doi: 10.21037/atm-20-8052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chang A. Chemotherapy, Chemoresistance and the Changing Treatment Landscape for NSCLC. Lung Cancer. 2011;71:3–10. doi: 10.1016/j.lungcan.2010.08.022. [DOI] [PubMed] [Google Scholar]
- 115.Bukowski K., Kciuk M., Kontek R. Mechanisms of Multidrug Resistance in Cancer Chemotherapy. Int. J. Mol. Sci. 2020;21:605. doi: 10.3390/ijms21093233. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.