Abstract
Background:
In the year 2020 we observe the world adapting to „new normal“ due to the COVID-19 pandemic, ways of which include physical distancing, hand hygiene, and wearing a face mask. There is no conclusive evidence about ocular manifestations of the new coronavirus infection, but cases of conjunctivitis, keratitis, and episcleritis have been reported in infected individuals.
Objective:
Determining if wearing a face mask during COVID-19 pandemic causes a new onset or deterioration of previously existing dry eye disease (DED).
Methods:
A prospective cohort study included 203 participants, all using surgical facemasks daily due to new regulations during COVID-19 pandemic. Participants completed a survey, containing modified Ocular Surface Disease Index (OSDI) questionnaire. They were divided into groups according to: sex, age, duration of face mask-wear, and existence of prior DED history.
Results:
Our results indicate that women have a statistically higher OSDI score compared to men (14.4 (IQR = 2.4 – 41.7) vs. 5.0 (IQR = 0.0 – 24.4); P = .004). Age did not significantly affect OSDI median values. Group that used masks from 3 to 6 hours/day demonstrated significantly higher OSDI scores compared to <3 hour/day group (15.3 (IQR = 8.3 – 47.7) vs. 8.3 (IQR = 0.0 – 35.1); P = .001). OSDI score was significantly greater in participants with prior DED history compared to those without it (36.1 (IQR = 14.1 – 61.6) vs. 4.2 (IQR = 2.3 – 8.3); P <.001). Participants with prior DED exhibited greater worsening of their disturbances during mask wearing period compared to the ones without previous DED (54.8% vs. 17.7%, Chi-Square 28.3 DF1; P <.001), regardless of daily mask wear duration.
Conclusion:
Our study confirmed the existence of mask-associated dry eye (MADE), most profoundly in females, subjects with a history of prior DED, and if wearing a face mask lasts longer than 3 hours per day. Ophthalmologists should advise their patients of the potential ocular surface health risks related to inadequately fitted facemasks.
Keywords: Dry eye, Face mask, Coronavirus, COVID-19, MADE, Ocular surface
1. BACKGROUND
During December 2019, Wuhan, Hubei province, China, became the center of an outbreak for the pneumonia of unknown cause, raising profound international attention. By January 2020, Chinese scientists had isolated a genetic sequence of the 2019 novel coronavirus (SARS-CoV-2). Widely reported as the COVID-19 (coronavirus disease), this respiratory tract infection had spread from Wuhan China to the rest of the world consequently causing a global pandemic. In the year 2020 we observe the world adapting to „new normal“ due to the COVID-19 pandemic, ways of which include physical distancing, hand hygiene, and wearing a face mask (1).
There is no conclusive evidence about ocular manifestations of the new coronavirus infection, but cases of conjunctivitis, keratitis, and episcleritis have been reported in infected individuals (2-5).
Xia and authors detected SARS-CoV-2 virus from tear and conjunctival secretion samples in one out of thirty enrolled infected patients (6). Although SARS-CoV-2 is not commonly present in tears, ocular manifestations, including dry eye disease (DED), are relatively common among COVID-19 patients and could appear prior to the onset of respiratory symptoms (7, 8).
Different outlooks on the COVID-19 pandemic raised questions about facemasks’ usefulness in protection from the virus, but the World Health Organization, nevertheless, strongly recommends wearing them. Regardless of the face mask type–from fabric to surgical mask and respirator face piece, they are all beneficial in comparison to not wearing one (9). Although different types of facemasks are used in the general population, they all have one thing in common: decreasing the influence of infected individuals from spreading the disease and protecting healthy population from the infection. Studies have demonstrated that physical distancing of 1 m or more, as well as optimal use of eye protection and facemasks in public and health-care settings diminish the risk from COVID-19 infection by reducing the spread of contaminated saliva and droplets from infected individuals (10).
We have noticed an increased number of patients with dry eye symptoms coming to our clinic upon starting to wear a face mask during this pandemic outbreak. Therefore, we have investigated if face mask wear could cause eye irritation or worsening of DED symptoms.
Tear Film and Ocular Surface Dry Eye Workshop II (TFOS DEWS II) report defines DED as a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film, accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles (11).
DED leads to a variety of symptoms, including ocular pain, dryness, itching, and foreign body sensation (12). Evaluation of subjective symptoms of DED using patient-reported outcome questionnaires (with Ocular Surface Disease Index being the most often used), in addition to clinical findings, is beneficial in accurate DED assessment (13).
Current data on mask-associated DED symptoms is very limited. Rare reports on this issue include commentary of patients complaining about DED symptoms worsening while using a face mask (14), and a letter to the editor describing a survey on healthy medical students (15).
Potential reason was described by Giannaccare et al. who have discussed mechanisms that could contribute to the onset or increase in DED symptoms during the use of face masks. They stated that a displacement or incorrect fitting of the face mask could disperse the air around the eyes and potentially cause rapid tears’ evaporation. The authors have found worsening of ocular discomfort symptoms in 10.3%, and the need for daily use of ocular lubricants in 19.6% of survey participants (15). A recent case report illustrated an additional risk of post-operative MADE after cataract surgery under topical anesthesia due to a poorly fitted facemask (16). Similar mechanism was described in a study by Hayirci and authors in the setting of continuous positive airway pressure users (17).
2. OBJECTIVE
The aim of this study was to determining if wearing a face mask during COVID-19 pandemic causes a new onset or deterioration of previously existing dry eye disease (DED).
3. PATIENTS AND METHODS
This research was reviewed by an independent Ethical review board and conforms with the principles and applicable guidelines for the protection of human subjects in biomedical research. This prospective cohort study included 203 participants that were randomly selected among patients who were attending the Ophthalmology Department of the University Hospital Center Sestre milosrdnice (Zagreb, Croatia) during October 2020. All participants wore surgical facemasks during the day. A consent form was signed after detailed information was provided to the subjects. Study followed the tenets of the Declaration of Helsinki. Participants were provided with a survey, containing modified Ocular Surface Disease Index (OSDI) questionnaire (18), with an aim of determining the existence of DED symptoms or deterioration of previous ones, if present, after wearing a face mask during COVID-19 pandemic. Original OSDI questionnaire was modified by adding “while wearing a facemask” to the ending of each question (eg Have you experienced any of the following during the last week while wearing a facemask). We also added three YES/NO questions and one regarding the duration of face masks-wear to our survey:
Did you have any dry eye symptoms (pain, irritation, redness, discomfort...) before you have started to wear a face mask?
If YES, have you used artificial tears or any other lubricant therapy for relieving dry eye symptoms, before you have started to wear a face mask?
Have you noticed the occurrence/worsening of dry eye symptoms after initiation of face mask-wear?
How many hours per day do you wear a face mask?
Study participants filled the surveys by themselves or with investigators’ aid if needed (in elderly subjects). They were divided in groups according to: sex (male/female), age (younger than 40, 41-60, and older than 60 years of age), duration of face mask-wear (less than 3, from 3 to 6, over 6 hours per day), and existence of prior DED history. OSDI index was calculated according to the formula OSDI = (sum of scores) x 25 / (number of questions answered) (18).
Statistical analysis
Neither OSDI score or the patients age were normally distributed according to the Kolmogorov-Smirnov test thus non-parametric tests were used; Mann-Whitney test when comparing two groups, Kruskal-Wallis test when comparing more than two groups. Chi square test was used for comparing categorical variables. All statistical analysis was done in Medcalc (19).
4. RESULTS
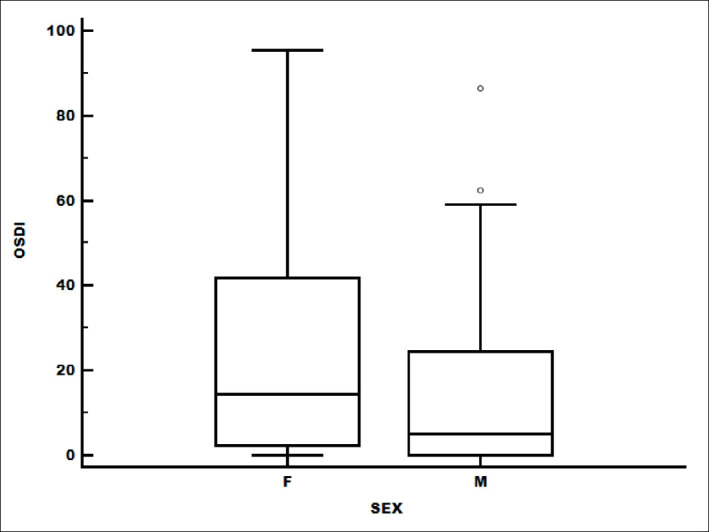
Study included 203 participants with a mean age of 47.4 years, among which 70.9% (144) were women. Our results indicate that women have a statistically higher OSDI score compared to men (14.4 (IQR = 2.4 – 41.7) vs. 5.0 (IQR = 0.0 – 24.4); Mann-Whitney P = .004) (Figure 1).
Figure 1. OSDI score differences according to sex. Females had significantly higher OSDI score than male group. OSDI – Ocular Surface Disease Index, F – female, M – male.
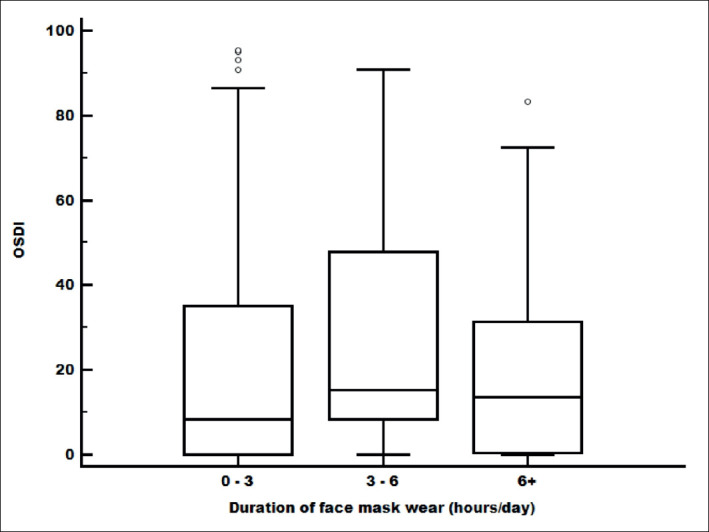
All participants were divided into three groups according to age: younger than 40 years (43.3%), from 40 to 60 years (29.1%), and over 60 years of age (27.6%). OSDI median values do not show significant difference between these three age groups (11.9 (IQR = 0.00 – 32.6), 10.0 (IQR = 2.1 – 22.1) and 15.8 (IQR = 2.3 – 60.7), Kruskal-Wallis P = .077), although the highest average OSDI score was found in the oldest age group (31.1) (Figure 2). We also divided them regarding the duration of face masks wear as follows: <3, 3-6 and >6 hours per day. Overall, there were some differences among groups (Kruskal-Wallis, P = .032). Group that used masks from 3 to 6 hours/day demonstrated significantly higher OSDI scores compared with <3 hours/day group (15.3 (IQR = 8.3 – 47.7) vs. 8.3 (IQR = 0.0 – 35.1); Mann Whitney P = .01) (Figure 3). Wearing a face mask for over 6 hours/day did not show a relevant difference in OSDI compared to other groups.
Figure 2. OSDI score differences according to age. There was no significant difference of OSDI median values. OSDI – Ocular Surface Disease Index.
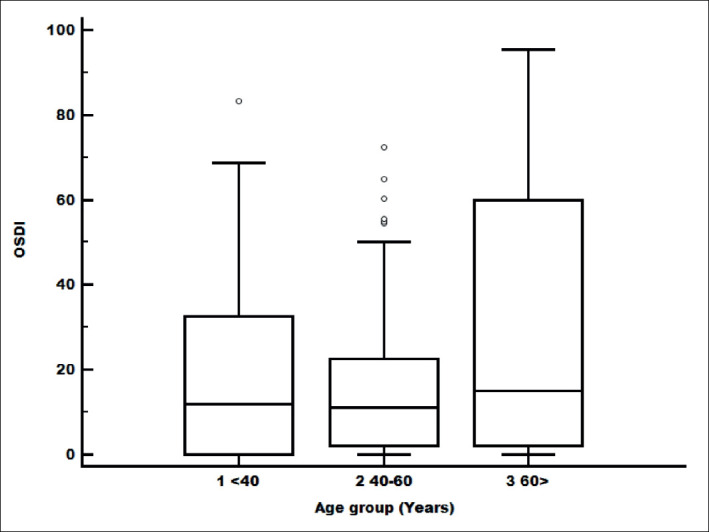
Figure 3. OSDI score differences due to daily face mask-wearing duration. Significantly higher OSDI score was noted in the group wearing masks for 3-6 hours/day, compared to 0-3 hour/day group. OSDI – Ocular Surface Disease Index.
Out of 203 participants, 73 (35.9%) had prior DED symptoms. Their OSDI score was significantly greater than of those without previous history of DED (36.1 (IQR = 14.1 – 61.6) vs. 4.17 (IQR = 0.0 – 18.7); Mann-Whitney P <.001) (Figure 4).
Figure 4. OSDI score according to previous DED history. Prior DED group had significantly higher OSDI score. OSDI – Ocular Surface Disease Index, DED- – No previous history of dry eye disease, DED+- Existence of previous dry eye disease.
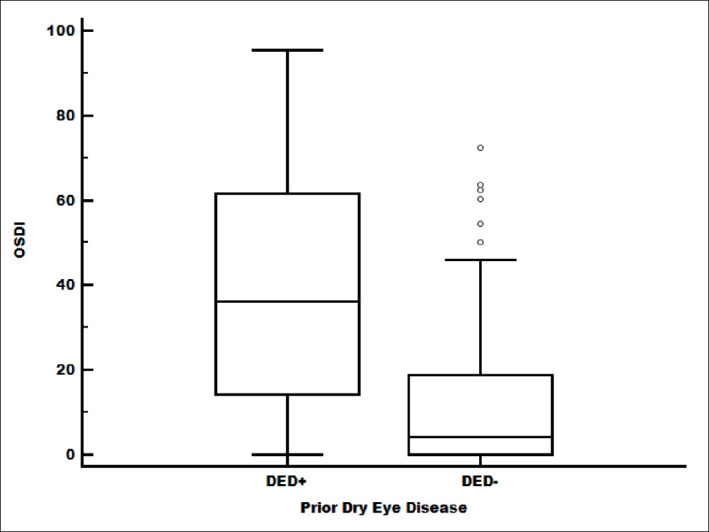
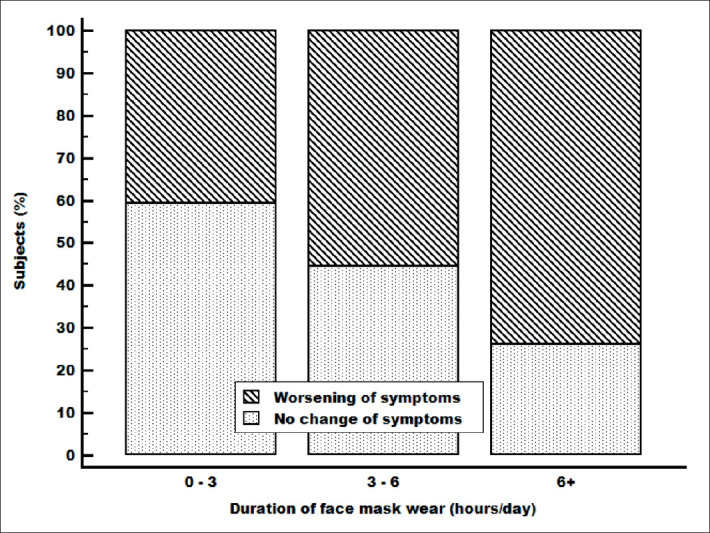
Of 73 participants with prior DED symptoms, 59 (80.8%) were using local eye lubricant therapy and 14 (19.2%) did not. We have not found a significant difference in OSDI scores between these two groups (38.9 (IQR = 15.4 – 62.5) and 18.3 (IQR = 6.3 – 55.0), respectively; Mann-Whitney P =.015). Subjects who reported DED symptoms prior to face mask wear had a significantly greater worsening of their disturbances during mask wearing period compared to the ones without previous dry eye history (54.8% vs. 17.7%, Chi-Square 28.3 DF1; P < .001) (Figure 5). This finding was demonstrated in all groups with previous DED, regardless of daily mask wear duration (Figure 6).
Figure 5. Worsening of the dry eye symptoms during mask-wearing period was significantly more common in participants who previously exhibited DED. DED- – No previous history of dry eye disease, DED+- Existence of previous dry eye disease.
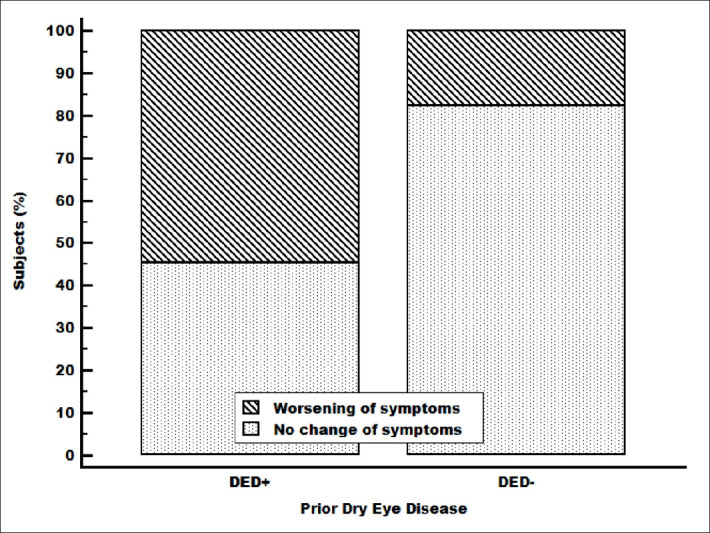
Figure 6. Worsening of the DED symptoms during mask-wear was noted in subjects with prior DED history, regardless of face mask-wearing duration.
5. DISCUSSION
Our results demonstrate that women have a statistically higher OSDI score than men, which concurs with previously reported papers on DED epidemiology (20, 21). The highest average OSDI score was found in the group over 60 years of age, but there was no significant difference of OSDI median values between different age groups. TFOS DEWS II report confirmed that DED prevalence increases significantly and shows a linear association with age, with a greater increase in signs than symptoms per decade (21).
This is the first report which showed that subjects who wore a face mask from 3 to 6 hours/day demonstrated significantly higher OSDI scores compared to those who used the mask less frequently. However, even longer daily mask-wear duration did not result in a relevant OSDI change compared to other groups. This could be due to the fact that the >6 hours/day group was comprised mostly of younger, healthy individuals, required to wear a mask during their work hours.
Subjects with prior DED reported worsening of their symptoms during mask-wearing period regardless of mask-wearing duration. This finding was not present in subjects without previous DED. Although neurosensory abnormalities and reduced corneal sensitivity are now recognized as common features of DED (11), there are also reports of cornea’s neuronal network disruption in the direction of hypersensitivity (22).
A recent study by Tagawa et al. demonstrated corneal hyperalgesia in DED patients with short tear film break-up time (23). The fact that the patients with dry eye might have higher sensitivity for noticing these symptoms could explain the difference between the groups. Also, the group with previous DED history is significantly older than the one without it which alone could account for the distribution of the results in the demonstrated pattern.
6. CONCLUSION
A history of a prior DED, female sex, as well as wearing a face mask longer than 3 hours per day, could contribute to or worsen DED symptoms during face mask-wear. Further studies could investigate different facemasks (eg facemask with valve could be beneficial in preventing MADE due to air blowing in direction of the valve). Ophthalmologists should advise their patients of the potential risks of inadequately fitted facemasks to their ocular surface health.
Acknowledgments:
The authors would like to thank professor Zoran Vatavuk, MD, PhD, FEBO, Head of the Ophthalmology Department at University Hospital Centre Sestre milosrdnice and professor Renata Ivekovic, MD, PhD, FEBO for their support and contribution.
Author’s contribution:
Study concept and design: IK, MB, and IPV. Data collection: : IK, MB, IM, IV, IS, IPV. Analysis and interpretation of data: IK, MB, IM, IV, IS, IPV. Drafting of the manuscript: IK and MB. Critical revision of the manuscript for important intellectual content: IK, MB, IM, IV, IS, IPV. Statistical analysis: IS. Study supervision: IPV.
Conflict of interest:
The authors of this paper certify that they have no conflict of interest to declare, ie they have no affiliations with or involvement in any organization or entity with any financial interest (eg honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, research support, stock ownership, other equity interest, or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
REFERENCES
- 1.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhattacharyya J, Tech M, Prajapat M, Shekhar N, Microbiology P, Avti S, et al. The Lancet Ocular Manifestations and Tear or Conjunctival Swaqb PCR Positivity for 2019-nCoV in Patients With COVID-19: A Systematic Review and Meta-Analysis. 2020 [Google Scholar]
- 3.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Méndez Mangana C, Barraquer Kargacin A, Barraquer RI. Episcleritis as an ocular manifestation in a patient with COVID-19. Acta Ophthalmol. 2020 doi: 10.1111/aos.14484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang X, Chen X, Chen L, Deng C, Zou X, Liu W, et al. The evidence of SARS-CoV-2 infection on ocular surface. Ocul Surf. 2020;18(3):360–362. doi: 10.1016/j.jtos.2020.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020;92(6):589–594. doi: 10.1002/jmv.25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen L, Deng C, Chen X, Zhang X, Chen B, Yu H, et al. Ocular manifestations and clinical characteristics of 535 cases of COVID-19 in Wuhan, China: a cross-sectional study. Acta Ophthalmol. 2020 doi: 10.1111/aos.14472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hong N, Yu W, Xia J, Shen Y, Yap M, Han W. Evaluation of ocular symptoms and tropism of SARS-CoV-2 in patients confirmed with COVID-19. Acta Ophthalmol. 2020 doi: 10.1111/aos.14445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO. Coronavirus disease (COVID-19) advice for the public. [Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
- 10.Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, et al. TFOS DEWS II Definition and Classification Report. Ocul Surf. 2017;15(3):276–283. doi: 10.1016/j.jtos.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 12.Smith JA, Albenz J, Begley C, Caffery B, Nichols K, Schaumberg D, et al. The epidemiology of dry eye disease: report of the Epidemiology Subcommittee of the International Dry Eye WorkShop (2007) International Dry Eye Workshop Ocul Surf 2007 5 2 93 107 10.1016/S1542-0124(12)70082-4. Ocular Surface. 2007;5:93–107. [Google Scholar]
- 13.Okumura Y, Inomata T, Iwata N, Sung J, Fujimoto K, Fujio K, et al. A Review of Dry Eye Questionnaires: Measuring Patient-Reported Outcomes and Health-Related Quality of Life. Diagnostics (Basel) 2020;10(8) doi: 10.3390/diagnostics10080559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moshirfar M, West WB, Jr, Marx DP. Face Mask-Associated Ocular Irritation and Dryness. Ophthalmol Ther. 2020;9(3):397–400. doi: 10.1007/s40123-020-00282-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Giannaccare G, Vaccaro S, Mancini A, Scorcia V. Dry eye in the COVID-19 era: how the measures for controlling pandemic might harm ocular surface. Graefes Arch Clin Exp Ophthalmol. 2020;258(11):2567–2568. doi: 10.1007/s00417-020-04808-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chadwick O, Lockington D. Addressing post-operative Mask-Associated Dry Eye (MADE) Eye (Lond) 2020:1–2. doi: 10.1038/s41433-020-01280-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hayirci E, Yagci A, Palamar M, Basoglu OK, Veral A. The effect of continuous positive airway pressure treatment for obstructive sleep apnea syndrome on the ocular surface. Cornea. 2012;31(6):604–608. doi: 10.1097/ICO.0b013e31824a2040. [DOI] [PubMed] [Google Scholar]
- 18.Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol. 2000;118(5):615–621. doi: 10.1001/archopht.118.5.615. [DOI] [PubMed] [Google Scholar]
- 19. MedCalc Software bv O, Belgium. Medcalc. 11.4 ed.
- 20.Truong S, Cole N, Stapleton F, Golebiowski B. Sex hormones and the dry eye. Clin Exp Optom. 2014;97(4):324–336. doi: 10.1111/cxo.12147. [DOI] [PubMed] [Google Scholar]
- 21.Stapleton F, Alves M, Bunya VY, Jalbert I, Lekhanont K, Malet F, et al. TFOS DEWS II Epidemiology Report. Ocul Surf. 2017;15(3):334–365. doi: 10.1016/j.jtos.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 22.Labetoulle M, Baudouin C, Calonge M, Merayo-Lloves J, Boboridis KG, Akova YA, et al. Role of corneal nerves in ocular surface homeostasis and disease. Acta Ophthalmol. 2019;97(2):137–145. doi: 10.1111/aos.13844. [DOI] [PubMed] [Google Scholar]
- 23.Tagawa Y, Noda K, Ohguchi T, Tagawa Y, Ishida S, Kitaichi N. Corneal hyperalgesia in patients with short tear film break-up time dry eye. Ocul Surf. 2019;17(1):55–59. doi: 10.1016/j.jtos.2018.08.004. [DOI] [PubMed] [Google Scholar]


