Abstract
Currently, the administration of surfactant to preterm infants with respiratory distress syndrome (RDS) mainly relies on intratracheal instillation; however, there is increasing evidence of aerosolized surfactant being an effective non-invasive strategy. We present a historical narrative spanning sixty years of development of aerosolization systems. We also offer an overview of the pertinent mechanisms needed to create and manage the ideal aerosolization system, with a focus on delivery, distribution, deposition, and dispersion in the context of the human lung. More studies are needed to optimize treatment with aerosolized surfactants, including determination of ideal dosages, nebulizer types, non-invasive interfaces, and breath synchronization. However, the field is rapidly evolving, and widespread clinical use may be achieved in the near future.
Keywords: aerosolized surfactant, nebulize, respiratory distress syndrome, preterm infants
1. Introduction
Respiratory distress syndrome (RDS) secondary to surfactant deficiency is a common problem and major cause of morbidity and mortality in neonates, especially in preterm infants [1]. Outcomes and management of RDS have improved significantly with the discovery of exogenous surfactants and the refinement of instillation strategies. There are currently multiple natural and synthetic exogenous surfactants with comparable benefits and risks [2]. Intratracheal instillation, in various strategies, remains the most widely accepted method of surfactant administration to infants with RDS [3,4]. However, there is increasing evidence suggesting that supraglottic administration via aerosolization is feasible and effective in preterm infants with RDS [5,6,7,8].
2. The Challenging Road towards Successful Clinical Application: Historical Narrative
The clinical success of aerosolized surfactants has been fraught with difficulty. For more than six decades, many attempts to aerosolize an exogenous surface tension reducing agent have been reported. However, within the past decade, multiple reports have demonstrated effective aerosol models for delivering exogenous surfactants in tandem with non-invasive ventilatory support.
The first attempts of an aerosolized surfactant came in a preliminary study in 1964 by Robillard et al., who attempted to administer an aerosol of the synthetic surfactant beta-gamma-dipalmitoyl-L-alpha-lecithin (DPL) to 11 infants with RDS [9]. The eight infants who survived had a modest improvement in their retraction scores. Although these results were not clinically significant, they provided optimism towards aerosolizing surfactants. The second study of this era, Chu et al. in 1967, comprehensively explored an aerosolized DPL via several methods [10]. Using a freon gas carrier, DPL was aerosolized and administered to the excised lungs of 14 infants at autopsy (7 of whom carried the diagnosis of RDS and 7 with normal lungs), with no observed changes to lung elasticity. Subsequently, DPL was aerosolized into the hood of 15 spontaneously breathing live infants. Only half of the infants showed some improvement in their respiratory distress after treatment. In retrospect, this particular form of synthetic surfactant is a rigid crystalline gel at physiologic temperature and also does not have the advantage of surfactant proteins. After these two studies, several decades passed, with advancements in the use of non-invasive respiratory support and instilled surfactant for RDS.
Surfactant, as an aerosol, was revisited by Lewis et al. in 1991 [11]. In an effort to distribute surfactant more uniformly throughout the lungs, Lewis et al. administered aerosolized surfactant to premature lambs for comparison with instilled surfactant. All groups still utilized an endotracheal tube with subsequent ventilator support, and the aerosolized surfactant was released synchronized with inhalation. Lambs treated with aerosolized surfactant demonstrated improvement in their ventilation on par with the instilled surfactant group. Despite this match in clinical outcome, they estimated the dose of aerosolized surfactant deposited in the lungs was only 2 mg/kg. This is markedly less than the instilled surfactant dose of 50 mg/kg, with an estimated 19 mg/kg of surfactant delivered to the lungs.
The promising results of the Lewis et al. lamb study were naturally followed by a proliferation of animal studies, lung cast modeling, and occasional infant feasibility studies. Some studies investigated different nebulizer types, such as Henry et al. in their 1996 study using ultrasonic nebulized surfactant in preterm lambs [12]. While they were able to correlate aerosolized surfactant deposition with better-ventilated regions of lung, the treated lambs did not show improvement in oxygenation. In 1998, Fok et al. also utilized an ultrasonic nebulizer and were able to deliver high levels of surfactant in a rabbit model but found only mediocre clinical improvement [13]. The best explanation for this lack of clinical improvement despite adequate surfactant deposition is surfactant inactivation by the high levels of heat generated by ultrasonic nebulizers.
Unique approaches were attempted to solve the dilemma of delivering effective surfactant to the distal airways, such as the hydroscopic surfactant used in the 1996 rabbit model by Ellyett et al. [14]. This “dried” surfactant would progressively become saturated with water during transit, becoming heavier when in the distal airways to settle there. This was preliminarily successful but not pursued further. In another case, a feasibility study of 20 infants used a specially modified nasopharyngeal tube placed behind the soft palate for jet-nebulized surfactant, with improvement in respiratory outcomes [15].
At the turn of the century, Berggren et al. performed a clinical pilot study in Sweden of nebulized surfactant therapy for neonatal RDS [16]. The study included 34 newborns on continuous positive airway pressure (CPAP) placed into either a treatment group of 480 mg aerosolized poractant alfa via a jet nebulizer or CPAP alone. There were no adverse events noted from aerosolization. However, there was also no documented benefit, with no difference in respiratory outcomes between treatment and control groups, including days on CPAP or need for mechanical ventilation (38% treated vs. 31% controls). Through the 2000s, two new approaches emerged. First, lucinactant, a second-generation synthetic surfactant comprised of two phospholipids, a fatty acid, and a synthetic surfactant protein B (SP-B) peptide replacement, KL4, came to the forefront [5,17,18]. Unlike the surfactant proteins in natural surfactants, the synthetic KL4 is more resistant to the aerosolization process [19]. The second shift in the aerosolization process manifested as a new focus on vibrating membrane nebulizers. Finer et al. in 2010 presented the combination of prophylactic lucinactant and vibrating membrane nebulizers in a safety and feasibility study of 17 infants [5]. The failure rate, defined as intubation, occurred less frequently in infants receiving aerosolized lucinactant (29%) compared to historical controls.
Coming to the most recent years, deliberate combinations of nebulizers, surfactants, and nasopharyngeal interfaces have emerged as a non-invasive approach to aerosolized surfactants. Minocchieri et al. offered a blinded randomized controlled trial of 64 infants in 2019 using the eFlow neonatal vibrating mesh nebulizer to administer poractant alfa via a dedicated nebulizer adapter [6]. They showed a decrease in intubation rates with a relative risk reduction of 0.57 (95% CI: 0.34 to 0.94). The same year, Sood et al. presented an uncontrolled 17 infant safety and feasibility pilot study using the MiniHeart Lo-Flo jet nebulizer via short binasal prongs; the infants tolerated the treatments well, with clinical improvement, as measured by heart rate, pCO2, and blood pH [7]. The most robust example of the customized interface is the 2020 Cummings et al. study, which included 457 infants randomized to standard of care (CPAP) or treatment with aerosolized surfactant via a modified Solarys pneumatically driven nebulizer with the patient interface in a pacifier shape [8]. This multicenter study included both preterm and term infants with respiratory distress on CPAP support, with randomization within the first 12 h of life. The study allowed multiple doses of aerosolized surfactant to be administered as per the clinical team. The primary outcome was endotracheal intubation during the first 4 days of life. There was a decrease in intubation in infants who received surfactant (RR: 0.51 (90% CI: 0.41–0.63)) compared to CPAP alone. The Cummings et al. study is the largest trial that has investigated aerosolized surfactant. More studies, including a systematic review, are currently underway that will provide more insight into the effectiveness of aerosolized surfactant, including prevention of intubation and subsequent mechanical ventilation [20].
3. Nebulizers
The evolution and composition of nebulizers play an important role in the success of aerosolized surfactants. There are three general categories of nebulizers, with subsequent subtypes and modifications within each family. This includes jet nebulizers, ultrasonic nebulizers, and mesh nebulizers. Table 1 summarizes the various nebulizers utilized to aerosolize surfactants in clinical studies in infants.
Table 1.
Summary of aerosolized surfactants and nebulizers utilized in clinical studies in preterm infants.
| Study | Population (n) | Nebulizer (Type) | Interface | Surfactant | Dose | Flow | Particle Size | Comparison | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| Jorch et al., 1994 | 28–35 wk GA (20) | Intersurgical RO252/ME (jet) | Modified nasopharyngeal tube placed behind soft palate | Beractant | 150 mg/kg per treatment | 8 L/min | <4 µm | Pre/post treatment | Significant improvement of A-a gradient, PaCO2, and Silverman score |
| Berggren et al., 2000 | 27–34 wk GA (34) |
Aiolos ® (jet) | Infant Flow System® nasal CPAP | Poractant alfa | 480 mg | 7 L/min | <2 µm | Aerosolized surfactant vs. CPAP alone | No benefit in treatment group |
| Finer et al., 2010 | 28–32 wk GA (17) |
Aeroneb Pro ® (vibrating mesh) | Fisher-Paykel nasal prongs | Lucinactant | 72 mg per treatment | 1 L/min | 1.9 ± 0.3 µm | Pre/post treatment Historic control intubation rate | Mean FiO2 decreased after treatment. 30–32 wk GA infant intubation rate lower than historic control |
| Sood et al., 2019 | 24–36 wk GA (17) |
Low Flow MiniHeart (jet) | Short binasal prongs | Beractant | 100–200 mg/kg per treatment | 2 L/min or less | Not reported | Pre/post treatment | Decrease in heart rate and pCO2; increase in pH |
| Minocchieri et al., 2019 | 29–33.6 wk GA (64) |
eFlow-Neos (vibrating mesh) | Face mask (not specified) | Poractant alfa | 200 mg/kg per treatment | 6–8 L/min | Not reported | Aerosolized surfactant vs. CPAP alone | Decreased intubation rate in treated 32–33.6 wk GA subgroup |
| Cummings et al., 2020 | 23–41 wk GA (457) |
Modified Solarys (pneumatically driven) | Custom pacifier mouthpiece | Calfactant | 210 mg/kg per treatment | 8–10 L/min | 4.5 µm | Aerosolized surfactant vs. usual care | Decreased intubation rate in treated infants |
Jet nebulizers, the oldest, most common, and affordable type, use a pressurized gas, the “jet”, that passes through the liquid drug solution and shears droplets from the surface to form the aerosol. There are many modifiable variables to jet nebulizer output, including the density, pressure, and flow rate of the compressed gas, which influence the aerosol particle size as well as variations in the arrangement of tubing and aerosol containment, allowing continuous aerosol flow or medication release during inhalation only. Disadvantages to jet nebulizers include their inefficiency as their reservoir tends to retain a large proportion of medical solution [21,22,23].
Ultrasonic nebulizers use electrical input through a transducer that converts the energy into high-frequency vibrations, creating a standing wave from which aerosolized droplets are produced. In terms of surfactant administration, ultrasonic nebulizers have the major drawback of heating the solution, presumptively leading to the denaturing of proteins, an important component of effective surfactant [21,23].
Mesh nebulizers are the newest nebulizer device type, emerging as the nebulizer of choice for new pharmaceuticals, distinguished by their efficiency [24]. This nebulizer also uses an electric power source to create high-frequency vibrations to force the medication solution through a fine mesh perforated by tapered holes, generating the aerosol. Variations within this nebulizer class are primarily based on the parameters of the mesh: different material composition of the mesh and varying diameters of the tapered hole openings, containing a range (1000–4000) of holes across the mesh surface. The primary disadvantages of this nebulizer type include blockages of the mesh holes, the difficulty of cleaning it, and the higher cost of the machine compared to other nebulizer types [21,22,23].
4. Delivery, Deposition, Distribution, and Dispersion of Aerosolized Surfactant
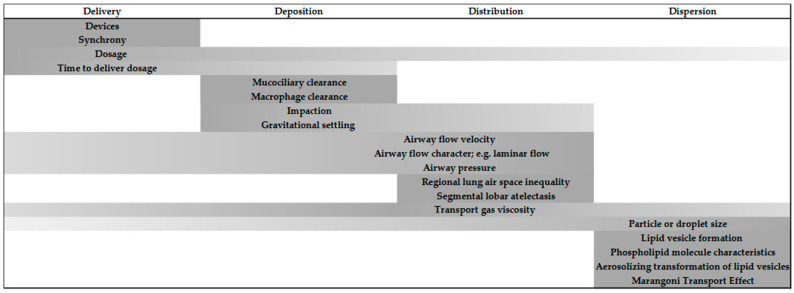
Aerosolized surfactant confronts unique challenges, overcoming deposition in the upper airways and being distributed to the deepest segments of the lung and effectively dispersed within gas-exchanging alveolar tissues. A considerable portion of a delivered therapeutic surfactant dosage is known to be lost before a sufficient amount descends below the alveolar ducts. As little as 1% to 14% of a dosage has been reported to reach the most distal lung parenchyma [25,26]. However, a more recent report using a newborn piglet model introduced atomization rather than nebulization [27]. Their investigational system is a multilumen flexible catheter capable of delivering low airway flow simultaneously with intermittent delivery of surfactant. The median particle size was 40–60 μm. Despite the larger particle size, they demonstrated that 40% of the surfactant is distributed by scintigram in the distal lung regions. They achieved a remarkable supraglottic delivery that overcomes tracheal and large bronchial airway losses to deposition yet provided bilateral lung distribution and alveolar space dispersion. To meet the challenges of surfactant delivery as an aerosol, animal data and in-vitro models have revealed considerable insight into the potential for it to become an effective therapeutic agent. Multiple variables have been determined that provide guidelines for translational considerations in the development and clinical application of aerosolized surfactant for infants (see Figure 1).
Figure 1.
Dynamic processes for the movement of aerosolized surfactant within the human infant lung.
4.1. Delivery of Aerosolized Surfactant
Aerosol delivery is dependent upon the different designs of the many nebulizing devices currently available (see “Nebulizers” above, Table 1). In turn, for surfactant therapy, the various nebulizers generate an aerosol with unique characteristics that are dependent upon the dosage, synchrony with inspired breaths, and desired time for delivery. An immediate goal of aerosolizing exogenous surfactant is to establish an effective supraglottic delivery system in tandem with existing non-invasive ventilatory support and set the stage for surfactant dose distribution to the multiple lobes of the lung. Recognizing that a major portion of the delivered dose is lost to the deep pharyngeal fossa [25,26], an attempt should be made to synchronize the delivery with a majority of spontaneous breaths. Delivery of an aerosol requires consideration for the time needed to complete a dose. This is true whether the delivery is a continuous application or delivery is in synchrony with either mechanically inspired breaths or spontaneous inspiration. Reports of 20 min to 2 h for completion of aerosol dose delivery leave much to be resolved as to the effectiveness [28,29]. Dosage amount per delivery, in milligrams of a phospholipid, varies from 50 to 200 mg/kg in either animal or human subjects, but all have been shown to improve gas exchange as the ultimate test of aerosolization success [11,30].
4.2. Deposition of Aerosolized Surfactant
Much of an aerosolized dosage is lost in the airways due to the velocity of the air stream and the impaction of the droplet against the walls of the trachea and bronchi. Further loss is incurred with gravitational settling upon the ciliated epithelium of the airways [31]. Particles or droplets may be swept proximal by the cilia, or they may be adsorbed in the underlying mucus layer of the ciliated epithelium of the airways. Finally, some dosage is discarded through the clearance action of resident airway macrophages.
4.3. Distribution of Aerosolized Surfactant
Aerosol distribution within the regions of the lung may be gravity-dependent or non-gravity-dependent depending upon the position of the infant. Cunha-Goncalves et al. have demonstrated the impact of subject position in a spontaneously breathing piglet model. The lung dose distribution was higher in the prone position. The influence of gravity was also demonstrated, with the highest dose distribution in the lateral decubitus position for the dependent lung [32]. An immediate goal of aerosolization is to reach as much of each lobe as possible with the surfactant dose. In patients with acute respiratory distress, alternating areas of atelectasis will be factors limiting the effectiveness of an aerosol. Asgharian et al. described a system of aerosol generation using a radiolabeled iron chloride solution to identify lung regions and specific lobes in spontaneously breathing adult rats [33]. They demonstrated distribution and dispersion throughout both lungs, with the greatest concentration of the inhalant deep within peripheral lung parenchyma.
Airway flow has been established as an important factor affecting aerosolized surfactants. An optimal airway flow would minimize deposition in the upper airway and enhance distribution to the deepest regions of the lung. At low gas flow, airway turbulence is minimized and laminar gas flow optimized. Laminar airway flow has been shown to enhance particle and droplet distribution [31]. Using catheter-based laboratory models, Syedain et al. [34] demonstrated that with an air jet nebulizer (Microjet™), they could achieve low airway flow and simultaneously generate surface-active small (4 μm) particles/droplets of commonly used surfactant therapeutic agents. Both observations support known optimization of surfactant distribution to the deepest regions of the lung. Moreover, the clinical implications of their observations are that low airway pressures and jet-nebulized aerosol would be compatible with pressure support mechanical ventilation or non-invasive continuous positive pressure ventilation for preterm infants.
4.4. Dispersion of Aerosolized Surfactant
An additional goal for achieving adequate delivery of an aerosolized surfactant is to gain sufficient dispersion of the dosage deep within the parenchymal lung tissue, resulting in adequate and sustained gas exchange. To this end, Aramendia et al. offered computational, experimental modeling of a delivery system replicating a preterm infant [35]. Their findings served to confirm that adequate dispersion of aerosolized surfactant at the alveolar level is dependent upon the properties of droplet size, airflow driving pressure, and airflow velocity. A perfluorocarbon was used as a proxy for surfactant, and an intratracheal catheter was used to instill a comparable infant surfactant dosage into a droplet-sizing spectrometer. Their data revealed the ideal droplet size to be 3.97 to 4.08 µm at 4 to 5 atm, approximating earlier work showing the optimum droplet size of 3–4 µm, with slightly reduced size at increased driving pressure [34]. From these aerosol dynamics, droplet size remains paramount in studies for maximal distribution and dispersion of a surfactant dosage within lung tissues [30]. Moreover, Borghardt et al., in a review of the pharmacokinetics of inhaled therapies for respiratory diseases, refer to an aerodynamic droplet size of 0.5–5.0 µm as being critical for the delivery of any “lung-dose”, with the greatest potential to be dispersed at the deepest levels of lung parenchyma [36]. Once a fraction of the aerosolized surfactant has reached the lower airways, nearing the end of the ciliated epithelium, it approaches the alveolar ducts. At this point, the remaining surfactant dosage becomes the lung-dose, ready for transport and dispersal as lipid vesicles within the alveolar ducts and alveolar spaces. The lung-dose becomes one portion that remains as aerosolized droplets and another portion that comes in contact with the air-surface liquid interface. Maximizing the surfactant lung-dose will continue to be a clinical goal as newer nebulizers are developed. Presently, means for monitoring lung-dose effect will rely mainly on effective infant pulmonary gas exchange, but evolving lung ultrasound technology promises to add imaging for evidence of greater surfactant lung-dose distribution and dispersion.
5. The Potential Benefit of Aerosolized Surfactant
The major upside of aerosolized surfactant is reducing the need for both intubation and positive pressure ventilation. Adverse events from endotracheal intubations are common in neonates, with incidences ranging from ~20–40% [37,38]. Associated complications include: physiologic changes such as hypoxemia and bradycardia [38,39,40]; oral, airway, and esophageal trauma/injury [37,38,41]; or inappropriate surfactant administration [38,42]. Successful intubation often requires multiple attempts [42,43]; consequently, the higher the number of attempts, the more the risk for adverse events [37], an important consideration with the rising concern for endotracheal intubation proficiency among trainees and providers [44,45,46,47]. In addition, positive pressure ventilation has well documented adverse outcomes, especially in preterm infants [48,49]. Positive pressure ventilation early after birth (even for a few breaths) causes lung injury and blunts the therapeutic effects of the surfactant [50,51]. The initial injury is further exacerbated by continuous and prolonged mechanical ventilation in the neonatal intensive care unit [52,53,54,55,56,57,58]. Other benefits of a nebulized surfactant include avoiding the risks of sedation medications and paralytic agents, often used for intubation in preterm infants [59].
It is unclear if there is a favorable cost–benefit of using aerosolized surfactants. The human studies used high surfactant dosages to account for losses. The duration of administration of aerosolized surfactants is comparable and sometimes longer than surfactant instillation strategies and, currently, not a major advantage. Finally, the recent clinical studies that showed benefit from aerosolized surfactants did not include preterm infants with severe RDS and lacked sufficient numbers of extremely preterm infants, an important consideration for clinical implementation.
6. Conclusions
We presented a historical narrative of the progress seen in the application of aerosolized surfactants over the past six decades. There is rising and promising evidence supporting the use of aerosolized surfactant in preterm infants with mild to moderate RDS. However, there is a paucity of data in infants with severe RDS and the smallest extremely preterm infants. This movement of assessing aerosolized surfactants shows no signs of slowing, with multiple ongoing national clinical trials [60,61,62]. We also summarized in this manuscript the mechanisms of ideal aerosolization strategies, with a focus on delivery, distribution, deposition, and dispersion when applied to the human lung. We believe these are important concepts for neonatologists and clinicians to understand as we translate the evidence to clinical practice in the future. Importantly, more studies are needed to optimize dosage, nebulizer types, non-invasive interfaces, and synchronization before supporting wide use in preterm infants. If an ideal surfactant aerosol can be advanced with non-invasive means of ventilatory support and established efficacy and safety for newborn premature infants, a major therapeutic step forward can be achieved in the near future.
Funding
E.G.A.J. is supported by the Gerber Foundation and by funds from by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1TR001998. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH; T.M.R. is supported by NIH K08HL133459-04 grant.
Conflicts of Interest
The authors declare no conflict of interest. E.G.A.J. participated in the multi-center aerosolized surfactant study ([8]).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Donda K., Vijayakanthi N., Dapaah-Siakwan F., Bhatt P., Rastogi D., Rastogi S. Trends in epidemiology and outcomes of respiratory distress syndrome in the United States. Pediatr. Pulmonol. 2019;54:405–414. doi: 10.1002/ppul.24241. [DOI] [PubMed] [Google Scholar]
- 2.Trembath A., Hornik C.P., Clark R., Smith P.B., Daniels J., Laughon H. Comparative effectiveness of surfactant preparations in premature infants. J. Pediatr. 2013;163:955–960.e951. doi: 10.1016/j.jpeds.2013.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Isayama T., Iwami H., McDonald S., Beyene J. Association of Noninvasive Ventilation Strategies with Mortality and Bronchopulmonary Dysplasia among Preterm Infants: A Systematic Review and Meta-analysis. JAMA. 2016;316:611–624. doi: 10.1001/jama.2016.10708. [DOI] [PubMed] [Google Scholar]
- 4.Isayama T., Chai-Adisaksopha C., McDonald S.D. Noninvasive Ventilation with VS without Early Surfactant to Prevent Chronic Lung Disease in Preterm Infants: A Systematic Review and Meta-analysis. JAMA Pediatr. 2015;169:731–739. doi: 10.1001/jamapediatrics.2015.0510. [DOI] [PubMed] [Google Scholar]
- 5.Finer N.N., Allen Merritt T., Bernstein G., Job L., Mazela J., Segal R. An Open Label, Pilot Study of Aerosurf Combined with nCPAP to Prevent RDS in Preterm Neonates. J. Aerosol. Med. Pulm. Drug Deliv. 2010;23:303–309. doi: 10.1089/jamp.2009.0758. [DOI] [PubMed] [Google Scholar]
- 6.Minocchieri S., Berry C.A., Pillow J.J., CureNeb Study Team Nebulised surfactant to reduce severity of respiratory distress: A blinded, parallel, randomised controlled trial. Arch. Dis. Child Fetal. Neonatal. Ed. 2019;104:F313–F319. doi: 10.1136/archdischild-2018-315051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sood B.G., Cortez J., Kolli M., Sharma A., Delaney-Black V., Chen X. Aerosolized surfactant in neonatal respiratory distress syndrome: Phase I study. Early Hum. Dev. 2019;134:19–25. doi: 10.1016/j.earlhumdev.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 8.Cummings J.J., Gerday E., Minton S., Katheria A., Albert G., Flores-Torres J., Famuyide M., Lampland A., Guthrie S., Kuehn D., et al. Aerosolized Calfactant for Newborns With Respiratory Distress: A Randomized Trial. Pediatrics. 2020;146 doi: 10.1542/peds.2019-3967. [DOI] [PubMed] [Google Scholar]
- 9.Robillard E., Alarie Y., Dagenais-Perusse P., Baril E., Guilbeault A. Microaerosol Administration of Synthetic β-γ-Dipalmitoyl-L-α-Lecithin in the Respiratory Distress Syndrome: A Preliminary Report. Can. Med. Assoc. J. 1964;90:55–57. [PMC free article] [PubMed] [Google Scholar]
- 10.Chu J., Clements J.A., Cotton E.K., Klaus M.H., Sweet A.Y., Tooley W.H., Bradley B.L., Brandorff L.C. Neonatal Pulmonary Ischemia. Pediatrics. 1967;40:709–782. [PubMed] [Google Scholar]
- 11.Lewis J.F., Ikegami M., Jobe A.H., Tabor B. Aerosolized surfactant treatment of preterm lambs. J. Appl. Physiol. 1991;70:869–876. doi: 10.1152/jappl.1991.70.2.869. [DOI] [PubMed] [Google Scholar]
- 12.Henry M.D., Rebello C.M., Ikegami M., Jobe A.H., Langenback E.G., Davis J.M. Ultrasonic Nebulized in Comparison with Instilled Surfactant Treatment of Preterm Lambs. Am. J. Respir. Crit. Care Med. 1996;154:366–375. doi: 10.1164/ajrccm.154.2.8756808. [DOI] [PubMed] [Google Scholar]
- 13.Fai Fok T., Al-Essa M., Dolovich M., Rasid F., Kirpalani H. Nebulisation of surfactants in an animal model of neonatal respiratory distress. Arch. Dis. Child. Fetal Neonatol. Ed. 1998;78:F3–F9. doi: 10.1136/fn.78.1.F3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ellyett K.M., Broadbent R.S., Fawcett E.R., Campbell A.J. Surfactant Aerosol Treatment of Respiratory Distress Syndrome in the Spontaneously Breathing Premature Rabbit. Pediatr. Res. 1996;39:953–957. doi: 10.1203/00006450-199606000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Jorch G., Weller E., Murlat A., Hentschel R. Feasibility study on nebulization of bovine surfactant (SF-RI 1) by pharyngeal continuous positive airway pressure (CPAP) Biol. Neonate. 1994;66 [Google Scholar]
- 16.Berggren E., Liljedahl M., Winbladh B., Andreasson B., Curstedt T., Robertson B., Schollin J. Pilot study of nebulized surfactant therapy for neonatal respiratory distress syndrome. Acta Pediatr. 2000;89:460–464. doi: 10.1111/j.1651-2227.2000.tb00084.x. [DOI] [PubMed] [Google Scholar]
- 17.Lampland A.L., Wolfson M.R., Mazela J., Henderson C., Gregory T.J., Meyers P., Plumm B., Worwa C., Mammel M.C. Aerosolized KL4 surfactant improves short-term survival and gas exchange in spontaneously breathing newborn pigs with hydrochloric acid-induced acute lung injury. Pediatr. Pulmonol. 2014;49:482–489. doi: 10.1002/ppul.22844. [DOI] [PubMed] [Google Scholar]
- 18.Pearson R., Pippins M., Niven R., Johnson M.E. 185 Treatment of RDS Using Aerosolized KL4 Lung Surfactant in Combination with nCPAP. Pediatr. Res. 2005;58:386. doi: 10.1203/00006450-200508000-00214. [DOI] [Google Scholar]
- 19.Donn S., Sinha S. Aerosolized lucinactant: A potential alternative to intratracheal surfactant replacement therapy. Expert Opin. Pharm. 2008;9:475–478. doi: 10.1517/14656566.9.3.475. [DOI] [PubMed] [Google Scholar]
- 20.Gaertner V.D., Bassler D., Ruegger C.M. Does surfactant nebulization prevent early intubation in preterm infants? A protocol for a systematic review and meta-analysis. Syst. Rev. 2021;10:9. doi: 10.1186/s13643-020-01573-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ari A. Jet, Ultrasonic, and Mesh Nebulizers: An Evaluation of Nebulizers for Better Clinical Outcomes. Eurasian J. Pulmonol. 2014;16:1–7. doi: 10.5152/ejp.2014.00087. [DOI] [Google Scholar]
- 22.Gardenhire D.S., Burnett D., Strickland S., Myers T.R. Care AAfR. 4th ed. AARC; Washington, DC, USA: 2017. A Guide to Aerosol Delivery Devices for Respiratory Therapists. [Google Scholar]
- 23.Mazela J., Polin R.A. Aerosol delivery to ventilated newborn infants: Historical challenges and new directions. Eur. J. Pediatr. 2011;170:433–444. doi: 10.1007/s00431-010-1292-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pritchard J.N., Hatley R.H., Denyer J., von Hollen D. Mesh nebulizers have become the first choice for new nebulized pharmaceutical drug developments. Ther. Deliv. 2018;9:121–136. doi: 10.4155/tde-2017-0102. [DOI] [PubMed] [Google Scholar]
- 25.Kohler E., Jilg G., Avenarius S., Jorch G. Lung deposition after inhalation with various nebulisers in preterm infants. Arch. Dis. Child Fetal Neonatal. Ed. 2008;93:F275–F279. doi: 10.1136/adc.2007.121285. [DOI] [PubMed] [Google Scholar]
- 26.Bianco F., Ricci F., Catozzi C., Murgia X., Schlun M., Bucholski A., Hetzer U., Bonelli S., Lombardini M., Pasini E. From bench to bedside: In vitro and in vivo evaluation of a neonate-focused nebulized surfactant delivery strategy. Respir. Res. 2019;20:134. doi: 10.1186/s12931-019-1096-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nord A., Bianco F., Salomone F., Ricci F., Schlun M., Linner R., Cunha-Goncalves D. Nebulization of High-Dose Poractant Alfa in Newborn Piglets on Nasal Continuous Positive Airway Pressure Yields Therapeutic Lung Doses of Phospholipids. Am. J. Perinatol. 2020 doi: 10.1055/s-0040-1721392. [DOI] [PubMed] [Google Scholar]
- 28.Milesi I., Tingay D.G., Zannin E., Bianco F., Tagliabue P., Mosca F., Lavizzari A., Ventura M.L., Zonneveld C.E., Perkins E.J. Intratracheal atomized surfactant provides similar outcomes as bolus surfactant in preterm lambs with respiratory distress syndrome. Pediatr. Res. 2016;80:92–100. doi: 10.1038/pr.2016.39. [DOI] [PubMed] [Google Scholar]
- 29.Bianco F., Pasini E., Nutini M., Murgia X., Stoeckl C., Schlun M., Hetzer U., Bonelli S., Lombardini M., Milesi I., et al. Extended Pharmacopeial Characterization of Surfactant Aerosols Generated by a Customized eFlow Neos Nebulizer Delivered through Neonatal Nasal Prongs. Pharmaceutics. 2020;12:319. doi: 10.3390/pharmaceutics12040319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rey-Santano C., Mielgo V., Gomez-Solaetxe M.A., Ricci F., Bianco F., Salomone F., Loureiro B. Dose-Response Study on Surfactant Nebulization Therapy During Nasal Continuous Positive Airway Pressure Ventilation in Spontaneously Breathing Surfactant-Deficient Newborn Piglets. Pediatr. Crit. Care Med. 2020;21:e456–e466. doi: 10.1097/PCC.0000000000002313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Darquenne C., Schmid O., Kim Prisk G. Aerosols and the Human Lung. World Scientific; Singapore: 2020. [Google Scholar]
- 32.Cunha-Goncalves D., Nord A., Bianco F., Salomone F., Ricci F., Schlun M., Linner R., Perez-de-Sa V. Impact of Body Position on Lung Deposition of Nebulized Surfactant in Newborn Piglets on Nasal Continuous Positive Airway Pressure. Neonatology. 2020;117:467–473. doi: 10.1159/000508349. [DOI] [PubMed] [Google Scholar]
- 33.Asgharian B., Kelly J.T., Tewksbury E.W. Respiratory deposition and inhalability of monodisperse aerosols in Long-Evans rats. Toxicol. Sci. 2003;71:104–111. doi: 10.1093/toxsci/71.1.104. [DOI] [PubMed] [Google Scholar]
- 34.Syedain Z.H., Naqwi A.A., Dolovich M., Somani A. In Vitro Evaluation of a Device for Intra-Pulmonary Aerosol Generation and Delivery. Aerosol. Sci. Technol. 2015;49:747–752. doi: 10.1080/02786826.2015.1067670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aramendia I., Fernandez-Gamiz U., Lopez-Arraiza A., Rey-Santano C., Mielgo V., Basterretxea F.J., Sancho J., Gomez-Solaetxe M.A. Experimental and Numerical Modeling of Aerosol Delivery for Preterm Infants. Int. J. Environ. Res. Public Health. 2018;15:423. doi: 10.3390/ijerph15030423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Borghardt J.M., Kloft C., Sharma A. Inhaled Therapy in Respiratory Disease: The Complex Interplay of Pulmonary Kinetic Processes. Can. Respir. J. 2018;2018:2732017. doi: 10.1155/2018/2732017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hatch L.D., Grubb P.H., Lea A.S., Walsh W.F., Markham M.H., Whitney G.M., Slaughter J.C., Stark A.R., Ely E.W. Endotracheal Intubation in Neonates: A Prospective Study of Adverse Safety Events in 162 Infants. J. Pediatr. 2016;168:62–66.e66. doi: 10.1016/j.jpeds.2015.09.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Foglia E.E., Ades A., Napolitano N., Leffelman J., Nadkarni V., Nishisaki A. Factors Associated with Adverse Events during Tracheal Intubation in the NICU. Neonatology. 2015;108:23–29. doi: 10.1159/000381252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marshall T.A., Deeder R., Pai S., Berkowitz G.P., Austin T.L. Physiologic changes associated with endotracheal intubation in preterm infants. Crit. Care Med. 1984;12:501–503. doi: 10.1097/00003246-198406000-00006. [DOI] [PubMed] [Google Scholar]
- 40.Kelly M.A., Finer N.N. Nasotracheal intubation in the neonate: Physiologic responses and effects of atropine and pancuronium. J. Pediatr. 1984;105:303–309. doi: 10.1016/S0022-3476(84)80137-7. [DOI] [PubMed] [Google Scholar]
- 41.Rentea R.M., St Peter S.D. Neonatal and pediatric esophageal perforation. Semin. Pediatr. Surg. 2017;26:87–94. doi: 10.1053/j.sempedsurg.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 42.O’Donnell C.P., Kamlin C.O., Davis P.G., Morley C.J. Endotracheal intubation attempts during neonatal resuscitation: Success rates, duration, and adverse effects. Pediatrics. 2006;117:e16–e21. doi: 10.1542/peds.2005-0901. [DOI] [PubMed] [Google Scholar]
- 43.Lane B., Finer N., Rich W. Duration of intubation attempts during neonatal resuscitation. J. Pediatr. 2004;145:67–70. doi: 10.1016/j.jpeds.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 44.Easley R.B., Segeleon J.E., Haun S.E., Tobias J.D. Prospective study of airway management of children requiring endotracheal intubation before admission to a pediatric intensive care unit. Crit. Care Med. 2000;28:2058–2063. doi: 10.1097/00003246-200006000-00065. [DOI] [PubMed] [Google Scholar]
- 45.Bismilla Z., Finan E., McNamara P.J., LeBlanc V., Jefferies A., Whyte H. Failure of pediatric and neonatal trainees to meet Canadian Neonatal Resuscitation Program standards for neonatal intubation. J. Perinatol. 2010;30:182–187. doi: 10.1038/jp.2009.152. [DOI] [PubMed] [Google Scholar]
- 46.Parmekar S., Arnold J.L., Anselmo C., Pammi M., Hagan J., Fernandes C.J., Lingappan K. Mind the gap: Can videolaryngoscopy bridge the competency gap in neonatal endotracheal intubation among pediatric trainees? a randomized controlled study. J. Perinatol. 2017;37:979–983. doi: 10.1038/jp.2017.72. [DOI] [PubMed] [Google Scholar]
- 47.Falck A.J., Escobedo M.B., Baillargeon J.G., Villard L.G., Gunkel J.H. Proficiency of pediatric residents in performing neonatal endotracheal intubation. Pediatrics. 2003;112:1242–1247. doi: 10.1542/peds.112.6.1242. [DOI] [PubMed] [Google Scholar]
- 48.Carvalho C.G., Silveira R.C., Procianoy R.S. Ventilator-induced lung injury in preterm infants. Rev. Bras. Ter. Intensiva. 2013;25:319–326. doi: 10.5935/0103-507X.20130054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jobe A.H. Mechanisms of Lung Injury and Bronchopulmonary Dysplasia. Am. J. Perinatol. 2016;33:1076–1078. doi: 10.1055/s-0036-1586107. [DOI] [PubMed] [Google Scholar]
- 50.Bjorklund L.J., Ingimarsson J., Curstedt T., John J., Robertson B., Werner O., Vilstrup C.T. Manual ventilation with a few large breaths at birth compromises the therapeutic effect of subsequent surfactant replacement in immature lambs. Pediatr. Res. 1997;42:348–355. doi: 10.1203/00006450-199709000-00016. [DOI] [PubMed] [Google Scholar]
- 51.Thomson M.A., Yoder B.A., Winter V.T., Giavedoni L., Chang L.Y., Coalson J.J. Delayed extubation to nasal continuous positive airway pressure in the immature baboon model of bronchopulmonary dysplasia: Lung clinical and pathological findings. Pediatrics. 2006;118:2038–2050. doi: 10.1542/peds.2006-0622. [DOI] [PubMed] [Google Scholar]
- 52.Garland J.S. Strategies to prevent ventilator-associated pneumonia in neonates. Clin. Perinatol. 2010;37:629–643. doi: 10.1016/j.clp.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 53.Attar M.A., Donn S.M. Mechanisms of ventilator-induced lung injury in premature infants. Semin Neonatol. 2002;7:353–360. doi: 10.1053/siny.2002.0129. [DOI] [PubMed] [Google Scholar]
- 54.Bancalari E., Gerhardt T. Bronchopulmonary dysplasia. Pediatr. Clin. N. Am. 1986;33:1–23. doi: 10.1016/S0031-3955(16)34967-7. [DOI] [PubMed] [Google Scholar]
- 55.Strong R.M., Passy V. Endotracheal intubation. Complications in neonates. Arch. Otolaryngol. 1977;103:329–335. doi: 10.1001/archotol.1977.00780230051006. [DOI] [PubMed] [Google Scholar]
- 56.Knisely A.S., Leal S.M., Singer D.B. Abnormalities of diaphragmatic muscle in neonates with ventilated lungs. J. Pediatr. 1988;113:1074–1077. doi: 10.1016/S0022-3476(88)80585-7. [DOI] [PubMed] [Google Scholar]
- 57.Powers S.K., Kavazis A.N., Levine S. Prolonged mechanical ventilation alters diaphragmatic structure and function. Crit. Care Med. 2009;37:S347–S353. doi: 10.1097/CCM.0b013e3181b6e760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sassoon C.S. Ventilator-associated diaphragmatic dysfunction. Am. J. Respir. Crit. Care Med. 2002;166:1017–1018. doi: 10.1164/rccm.2207008. [DOI] [PubMed] [Google Scholar]
- 59.Kumar P., Denson S.E., Mancuso T.J., Committee on Fetus and Newborn. Section on Anesthesiology and Pain Medicine Premedication for nonemergency endotracheal intubation in the neonate. Pediatrics. 2010;125:608–615. doi: 10.1542/peds.2009-2863. [DOI] [PubMed] [Google Scholar]
- 60.A Dose-Ranging Study to Determine the Efficacy, Safety and Tolerability of AeroFact. [(accessed on 17 December 2020)]; Available online: https://ClinicalTrials.gov/show/NCT03969992.
- 61.Administration of Surfactant through an Instillation Device Infasurf® (Calfactant) in Neonates—A Pilot Study. [(accessed on 17 December 2020)]; Available online: https://ClinicalTrials.gov/show/NCT04056741.
- 62.Surfactant Nebulization for the Early Aeration of the Preterm Lung. [(accessed on 17 December 2020)]; Available online: https://ClinicalTrials.gov/show/NCT04315636.