Abstract
Background
Tourniquets are widely used in total knee arthroplasty (TKA), but the issue of their safety remains controversial. Previous studies have focused on TKA blood loss, duration of surgery, and hemostatic drugs. The purpose of this meta-analysis was to analyze the effect of tourniquet use on postoperative deep venous thrombosis (DVT).
Methods
PubMed, SCOPUS, Web of Science, Embase, and the Cochrane Library were searched for randomized clinical trials published before April 17, 2020, that compared the effect of tourniquet use on postoperative DVT, knee circumference, D-dimers, and pain measured using the visual analog scale (VAS).
Results
Fourteen clinical trials that included 1321 unique participants were included in the meta-analysis. Among the total, 721 and 600 participants were randomized to the tourniquet and non-tourniquet groups, respectively. The incidence of postoperative thrombosis in the tourniquet group was significantly higher than in the non-tourniquet group (RR 2.30, 95% CI 1.51–3.49, P < 0.0001, I2 = 0%). On the 1st, 3rd, and 5th to 21st days, and 3 to 6 weeks after surgery, the knee circumference difference of the tourniquet group was significantly larger than that of the non-tourniquet group (P < 0.05). However, 4 to 6 months after the surgery, no significant difference in knee circumference was found between the two groups (MD 0.14, 95% CI −0.02–0.31, P = 0.09, I2 = 0%). The VAS score of the tourniquet group was higher than the non-tourniquet group on the 3rd and 5th days after surgery (P < 0.05). However, this difference was not significant (MD 0.31, 95% CI −0.05–0.66, P = 0.09, I2 = 89%).
Conclusion
Results of this meta-analysis indicate that tourniquet application could increase the incidence of postoperative DVT and aggravate postoperative pain and swelling in the short term.
Level of evidence
Level III
Keywords: Total knee arthroplasty, Tourniquet, Thrombosis, Meta-analysis, Complication
Introduction
Total knee arthroplasty (TKA) is a common surgical procedure for painful arthritis of the knee. Its main purpose is to relieve knee pain and restore joint stability and function. TKA has been proven a successful surgical procedure that could restore a significant degree of function in arthritic knees in most cases [1, 2]. Patient satisfaction with the implantation of total knee endoprostheses was about 81.4% [3]. Pneumatic tourniquets have been widely used in various orthopedic surgeries since its introduction by Harvey Cushing in 1904. In TKA, tourniquets have been used for more than a century, aiming to provide a clear surgical field of vision to shorten the operation time and improve the accuracy of the procedure [4, 5]. Although tourniquets are widely used, the complications caused by its alteration of normal physiological state should not be ignored. Examples of these are compartment syndrome, DVT, skin necrosis and neurological complications, and even permanent damage and loss of limb function [6–9]. Tourniquet use is considered as an important cause of DVT [10]. However, several previous meta-analyses have shown no difference in the effects of TKA with and without tourniquet use on postoperative DVT [11, 12], but others believe that the incidence of DVT in the tourniquet group was higher than that in the non-tourniquet group [13, 14]. Compared with the previous meta-analysis, this study included recent studies different from the ones analyzed before, and a few comparisons of knee circumference not seen in previous meta-analyses were also made.
Studies on tourniquet use in TKA are numerous and varied. Conducting a meta-analysis seems to be a good and comprehensive method to analyze these data. The purpose of this study was to evaluate the effect of tourniquet use during unilateral TKA on postoperative DVT, so as to provide guidance for clinical practice.
Material and methods
This meta-analysis was performed in accordance with the guidelines listed in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Search strategy
We systematically searched PubMed, SCOPUS, Web of Science, Embase, and the Cochrane Library for randomized control trials published before April 17. The search was performed using the PICO model [15]. The key words used were “total knee arthroplasty,” “total knee replacement,” “TKA,” “TKR,” “tourniquets,” “tourniquet,” “thrombosis,” “thromboses,” “thrombus,” “blood clot,” and “blood clots.” There was no language or study type restriction, and we manually searched the reference lists of included studies. All articles were imported into a literature management software and screened for duplicates. Two reviewers independently selected the title and abstract of each article and had discussions to resolve the differences. A third reviewer resolved any remaining disagreements.
Inclusion and exclusion criteria
Studies included in this meta-analysis met the following inclusion criteria: (1) randomized controlled trials (RCT), (2) the study compared TKA with and without tourniquet use, (3) osteoarthritis was managed with TKA, and (4) the primary outcome was DVT and the secondary outcomes were knee circumference, D-dimers, and pain.
The exclusion criteria were as follows: (1) bilateral knee replacement, (2) involved other types of surgery (knee arthroscopy, hemiarthroplasty, fracture fixation, etc.), and (3) any non-human studies, regardless of the type or size of prosthesis, anesthesia, and postoperative care. The date of follow-up examinations in individual studies usually varies, so similar follow-up examination time points were systematically combined for analysis (e.g., second to third postoperative day).
Quality assessment
We evaluated the quality of the explicit eligibility criteria, similarity of baseline characteristics, and as well as the revised Jadad scale of the included studies [16]. We resolved disagreements by discussion or adjudication by another reviewer. The revised Jadad scale has a maximum score of 7 points assessed with the following items: (1) random sequence generation (0–2 points), (2) allocation concealment (0–2 points), (3) double-blind design (0–2 points), and (4) the analysis and reasons for withdrawals and dropouts (0–1 point). Studies with a score of at least 4 are considered good quality, and poor-quality studies have a score of less than 3.
Statistical analysis
A meta-analysis was performed with the studies using the Review Manager Database (RevMan version 5.3, Cochrane Collaboration, Copenhagen, Denmark, 2014). Mean differences (MD) were used to weigh the effect size for continuous outcomes, and relative risks (RR) were used for dichotomous outcomes. Funnel plots were used to examine publication bias. We assessed the presence of statistical heterogeneity with the use of a standard Chi square test and the value of I2. It could be considered suggestive of statistical heterogeneity, prompting a random effects modeling estimate if P < 0.1 and I2 > 50%. Otherwise, we used a fixed effects approach.
Result
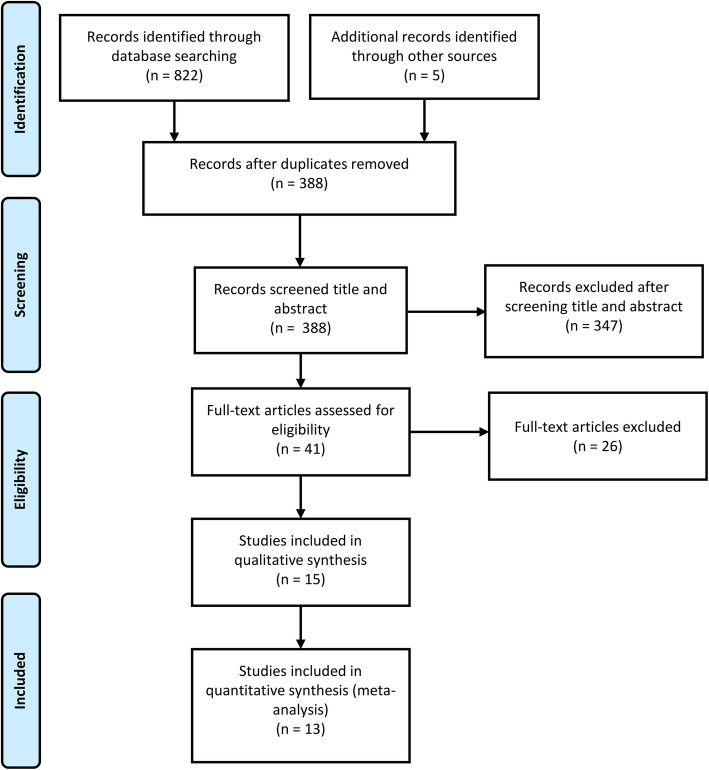
A total of 822 articles were retrieved from the database using our search strategy, and 5 articles were obtained from other review references. After removing 439 duplicate articles, 388 articles were screened. Among these, 347 articles were excluded after reading the titles and abstracts, and 26 articles were excluded after reading the full text. This screening resulted in 15 articles enrolling a total of 1400 patients, all of which compared TKA with and without tourniquet use. After quality evaluation, two studies [17, 18] were excluded due to poor literature quality. Finally, 13 RCTs [19–31], enrolling a total of 1321 patients, were included in the meta-analysis; 721 participants were randomized to the tourniquet group, while 600 were randomized to the non-tourniquet group (Fig. 1). The data extracted from the included studies (age, tourniquet pressure, and operating time) are summarized in Table 1. In the included studies, tourniquets of varying pressures were used, and most of them were deflated after the incision was closed. The type of anesthesia and anticoagulant regimens used in all operations were dependent on the surgeon’s experience and the patient’s needs.
Fig. 1.
Flowchart of search strategy
Table 1.
Characteristics of the included studies
| Author | Year | Age (T/N T) |
Number of patients | T/N T | Tourniquet pressure | Operation time (min) | DVT | K-C | D-d | Pain |
|---|---|---|---|---|---|---|---|---|---|---|
| Abdelsalam | 1995 | 72.0/74.0 | 80 | 40/40 | Twice SBP | <90 | ✓ | ✓ | ||
| Wakankar | 1999 | 72.5/71.8 | 77 | 37/40 | Twice SBP | NA | ✓ | ✓ | ✓ | |
| Aglietti | 2000 | 70.0/68.0 | 20 | 10/10 | 0.8 bar | 90.0 | ✓ | |||
| Vandenbussche | 2002 | 72.5/68.5 | 80 | 40/40 | 350 mmHg | 151.0 | ✓ | ✓ | ||
| Wauke | 2002 | 63.2/61.4 | 37 | 19/18 | SBP+100 mmHg | 75.1 | ✓ | |||
| Li | 2008 | 71.0/70.0 | 80 | 40/40 | SBP+100 mmHg | 73.0 | ✓ | |||
| Zhang | 2010 | 72.0/71.0 | 60 | 30/30 | SBP+100 mmHg | <90 | ✓ | |||
| Yin | 2011 | 63.1/61.9 | 39 | 20/19 | NA | NA | ✓ | |||
| Yin | 2012 | 68.9/67.1 | 40 | 20/20 | NA | NA | ✓ | |||
| Ejaz | 2014 | 68.0/68.0 | 92 | 33/31 | 250 mmHg | 70.0 | ✓ | ✓ | ||
| Mori | 2016 | 72.8/74.6 | 103 | 51/52 | 250 mmHg | 63.6 | ✓ | |||
| Zhang | 2016 | 63.2/65.2 | 230 | 84/82 | SBP+13.3 kPa | 81.7 | ✓ | ✓ | ||
| Zhou | 2017 | 66.8/69.1 | 150 | 72/68 | NA | 77.2 | ✓ | ✓ | ✓ | |
| Wu | 2018 | 67.6/68.1 | 112 | 50/50 | 250 mmHg | 67.2 | ✓ | ✓ | ✓ | |
| Goel | 2019 | 66.0/66.5 | 200 | 100/99 | 300/225 mm Hg | 71.6 | ✓ | ✓ |
T tourniquet, N T non- tourniquet, DVT deep venous thrombosis, NA not available, K-C knee circumference, D-d D-dimers, SBP systolic blood pressure
Quality assessment
The quality assessment of the primary studies is summarized in Table 2. The Jadad scores ranged from 0 to 7. Thirteen of fifteen studies had a Jadad score of at least 4 and thus were considered high quality. Two studies, with a Jadad score of less than 3, were deemed low quality and ultimately excluded.
Table 2.
Quality assessment of RCTs included in the review
| Study | Explicit eligibility criteria | Similarity of baseline characteristics | Revised Jadad score | ||||
|---|---|---|---|---|---|---|---|
| Random sequence generation | Allocation concealment | Double-blind | Withdrawals and dropouts | Sum (4–7 high quality) | |||
| Abdelsalam and Eyres [30] | Yes | Yes | 2 | 1 | 2 | 0 | 5 |
| Wakankar et al. [29] | Yes | Yes | 2 | 1 | 0 | 1 | 4 |
| Aglietti et al. [28] | Yes | Yes | 2 | 1 | 0 | 1 | 4 |
| Vandenbussche et al. [27] | Yes | Yes | 2 | 2 | 2 | 1 | 7 |
| Wauke et al. [26] | Yes | Yes | 2 | 1 | 0 | 1 | 4 |
| Li et al. [31] | Yes | Yes | 2 | 2 | 1 | 1 | 6 |
| Zhang et al. [25] | Yes | Yes | 2 | 2 | 0 | 1 | 5 |
| Zhou et al. [18] | Yes | Yes | 0 | 0 | 0 | 1 | 1 |
| Yin et al. [17] | Yes | Yes | 1 | 1 | 0 | 1 | 3 |
| Ejaz et al. [24] | Yes | Yes | 2 | 2 | 0 | 1 | 5 |
| Mori et al. [23] | Yes | Yes | 2 | 1 | 0 | 1 | 4 |
| Zhang et al. [22] | Yes | Yes | 2 | 0 | 1 | 1 | 4 |
| Zhou et al .[21] | Yes | Yes | 2 | 2 | 0 | 1 | 5 |
| Wu et al. [20] | Yes | Yes | 2 | 2 | 2 | 1 | 7 |
| Goel et al. [19] | Yes | Yes | 2 | 2 | 2 | 1 | 7 |
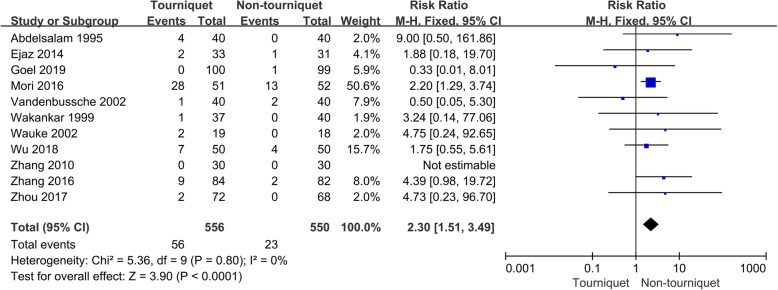
Effects on DVT
Based on the inclusion criteria, a total of 11 trials with 1106 patients provided data of DVT were included in the study (Fig. 2). There was a significant statistical difference in DVT between the tourniquet and non-tourniquet groups (RR 2.30, 95% CI 1.51–3.49, P < 0.0001, I2 = 0%).
Fig. 2.
Occurrence of a deep vein thrombosis
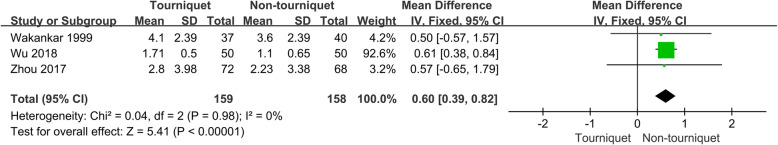
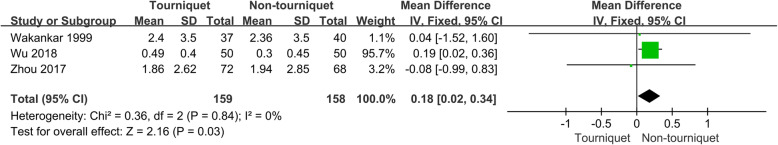
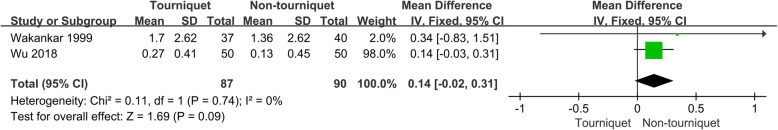
Effects on knee circumference
Four trials provided data of knee circumference, and three of these studies with 317 patients were included in analysis. The meta-analysis showed that the tourniquet group had a significantly larger knee circumference difference than the non-tourniquet group in the 1st, 3rd, and from the 5th to the 21st days, and from the 3rd to the 6th weeks after surgery (P < 0.05) (Figs. 3, 4, 5, and 6). However, 4 to 6 months after the surgery, no significant difference in knee circumference difference was found between the two groups (MD 0.14, 95% CI −0.02–0.31, P = 0.09, I2 = 0%) (Fig. 7).
Fig. 3.
Knee circumference difference, 1st day postop
Fig. 4.
Knee circumference difference, 3rd day postop
Fig. 5.
Knee circumference difference, 5th–7th day postop
Fig. 6.
Knee circumference difference, 3rd–6th week postop
Fig. 7.
Knee circumference difference, 4th–6th month postop
Effects on D-dimers
Three trials provided data of D-dimers, but only one study with 20 patients was included because the two other trials had a revised Jadad scale score of less than 3 and were ruled out. Therefore, a meta-analysis of D-d dimers was not possible.
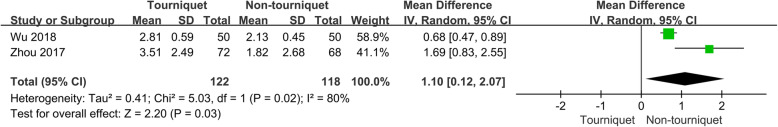
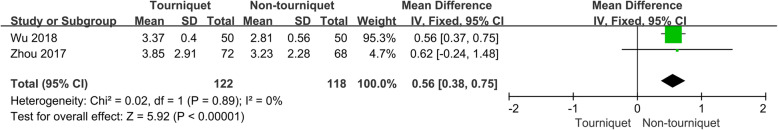
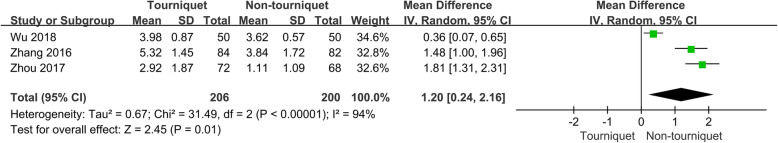
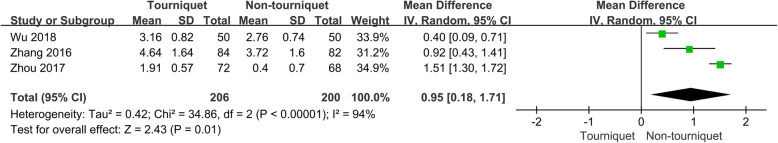
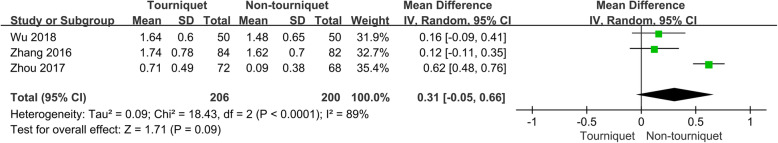
Effects on pain
Eight trials provided data of pain score measured using the visual analog scale (VAS). Three of these studies with 406 patients were included in the analysis. The results show that the VAS score in the tourniquet group was higher than in the non-tourniquet group on the 3rd and 5th days after surgery (P < 0.05) (Figs. 8 and 9). However, there was no significant difference in VAS score between the two groups (MD 0.31, 95% CI −0.05–0.66, P = 0.09, I2 = 89%) (Fig. 10).
Fig. 8.
Pain, 3rd day postop
Fig. 9.
Pain, 5th day postop
Fig. 10.
Pain, 3rd week–1st month postop
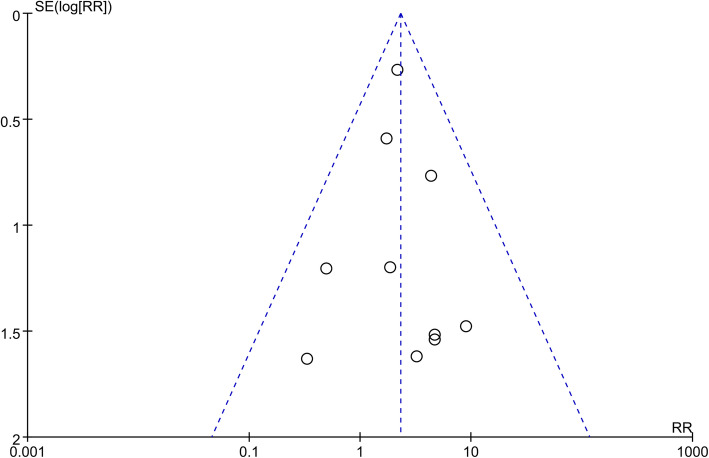
Publication bias
In this study, with DVT after TKA as the main observation index, publication bias was analyzed in 11 studies. All the studies were distributed symmetrically with a small top and a large bottom indicating no significant publication bias in the 11 included studies (Fig. 11).
Fig. 11.
Funnel plot of DVT
Discussion
Tourniquets are widely used in various surgical procedures, but their risks and benefits are still highly controversial. The use of tourniquets achieves a bloodless field for visualization and cement interdigitation [5], but this also gradually exposes its potential disadvantages. A number of reports have studied the effects of tourniquets on the risk of postoperative thrombosis, but their inclusion criteria, operative skill of the surgeons, and number of cases all varied, resulting in varying outcomes as well. Therefore, we included these existing data in the meta-analysis to provide an objective basis for clinical practice. The results showed that tourniquet use in TKA increases the incidence of postoperative DVT and exacerbated knee pain and swelling in the early postoperative period. However, in terms of long-term effects, there were no significant differences in knee swelling and pain between the two groups.
Thrombosis is one of the most common and dangerous postoperative complications. Venous stasis, endothelial injury, and hypercoagulability are the main factors of thrombosis according to Virchow’s triad [32]; this holds true for patients undergoing TKA. Majority of patients receiving TKA are elderly with vascular aging and marked changes in hemorheology accompanied by varying degrees of hypercoagulability. All these factors put the patient’s blood in a state of high coagulation. High pressure and prolonged ligation lead to limb ischemia, and when circulation resumes, ischemia reperfusion leads to secondary injury of endothelial cells [21], temporarily increased blood volume and systemic vascular resistance, induction of hypercoagulability, and activation of fibrinolytic activity [33]. Endothelial cells and skeletal muscles injured by this mechanism of ischemia-reperfusion produce more oxygen free radicals and release inflammatory mediators to promote oxidative stress levels and the inflammatory reaction [33]. Inflammation stimulates thrombosis, which in turn promotes inflammation; these two processes are interdependent and mutually reinforce each other [34]. These mechanisms suggest that tourniquet use may increase the incidence of thrombi, which is consistent with our conclusions. However, the effect of tourniquet on thrombus development remains controversial because many studies have different conclusions. Fukuda et al. [35] showed that tourniquet use in TKA did not increase the incidence of thrombus postoperatively, and the difference between the two groups was not statistically significant. Yi et al. [11] and Alcelik et al. [12] reached the same conclusion. This difference may be related to the inclusion criteria because we included only high-quality literature on unilateral knee replacement.
D-dimers are the degradation product of fibrinolytic enzymes on cross-linked fibrin, indicating the development of thrombus. A D-dimer test could reliably exclude DVT with a negative predictive value of 99% [36]. Since only one study on D-dimers was included, no effective analysis could be performed, but this study also showed that the use of tourniquets increased D-dimer levels [28]. In a similar study, Reikeras et al. [37] found that D-dimer levels increased immediately after tourniquet release. This suggested that tourniquet use in TKA might affect coagulation function and promote thrombosis. D-dimers are affected by many factors, such as surgery, trauma, bleeding, pregnancy, and tumors. As mentioned above, patients may preoperatively have hypercoagulability and hyperfibrinolysis, so elevation of D-dimer is not an independent risk factor for thrombosis after TKA.
Pain and swelling of the knee joint are common symptoms after TKA and can also accompany DVT. Our analysis shows that the use of a tourniquet aggravated postoperative pain and swelling in the short term. Postoperative pain stimulation will lead to sympathetic excitement and a stress response, leading to endocrine disorders and aggravating hypercoagulability. Endothelial cell damage caused by ischemia-reperfusion can aggravate pain, and reactive hyperemia of the affected limb can aggravate swelling [38].
Although our results endorse the absence of tourniquets in TKA, we cannot conclude this by evaluating these indicators alone. The duration of tourniquet use, tourniquet pressure, and operation time all affect the prognosis. Clinicians often use tourniquets based on their own experience to determine the use of time and stress, regardless of the patient’s baseline blood pressure. All of these can have a big impact on the clinical outcome. The use of tourniquets should be considered in combination with other beneficial treatment modalities.
Conclusions
This meta-analysis of randomized placebo-controlled clinical trials suggests that tourniquet application could increase the incidence of postoperative DVT and aggravate postoperative pain and swelling in the short term. Our results indicate that TKA without tourniquet use is superior to TKA with tourniquet use when evaluating postoperative thrombosis, pain, and swelling. However, only a few cases were studied, and the study time span was long; because of this, the application of tourniquets in TKA should not be completely stopped. Therefore, this paper only serves as a clinical reference, which needs to be confirmed by more prospective studies. It is necessary to combine relevant clinical indicators and the experience of the surgeon to decide whether to apply a tourniquet in TKA.
Acknowledgements
Not applicable.
Abbreviations
- TKA
Total knee arthroplasty
- TKR
Total knee replacement
- RCTs
Randomized controlled trials
- VAS
Visual analog scale
- DVT
Deep venous thrombosis
- K-C
Knee circumference
- D-d
D-dimers
- SBP
Systolic blood pressure
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- MD
Mean difference
- CI
Confidence interval
- RR
Relative risk
Authors’ contributions
XJ collected and analyzed data and wrote the manuscript. YH and WFY analyzed data. LJ and JJH helped to draft the manuscript. All authors reviewed the final manuscript. All authors agree to be accountable for all aspects of the work.
Funding
This study was financially supported by Key Research and Development project of Anhui Province (No. 201904b11020032), the National Natural Science Foundation of China Youth Program (No. 81702656), Clinical Research cultivation Program of the Second Affiliated Hospital of Anhui Medical University (No. 2020LCZD20), and Basic and Clinical Cooperative Research Promotion Plan of Anhui Medical University (No. 2020xkjT040).
Availability of data and materials
All data generated or analyzed during this study are included in published articles.
Declarations
Ethics approval and consent to participate
Not applicable
Competing interests
The authors declare that they have no competing interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jia Xie and Hao Yu are listed as co-first authors of the paper.
Contributor Information
Jia Xie, Email: 550387419@qq.com.
Hao Yu, Email: yuhow8023@163.com.
Fangyuan Wang, Email: 332791817@qq.com.
Juehua Jing, Email: jhjpaper@sina.com.
Jun Li, Email: efylijunpaper@163.com.
References
- 1.Dixon MC, Brown RR, Parsch D, Scott RD. Modular fixed-bearing total knee arthroplasty with retention of the posterior cruciate ligament. A study of patients followed for a minimum of fifteen years. J Bone Joint Surg Am. 2005;87(3):598–603. doi: 10.2106/00004623-200503000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Barrington JW, Sah A, Malchau H, Burke DW. Contemporary cruciate-retaining total knee arthroplasty with a pegged tibial baseplate. Results at a minimum of ten years. J Bone Joint Surg Am. 2009;91(4):874–878. doi: 10.2106/JBJS.G.01609. [DOI] [PubMed] [Google Scholar]
- 3.Scott CEH, Howie CR, MacDonald D, Biant LC. Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg (Br) 2010;92:1253–1258. doi: 10.1302/0301-620X.92B9.24394. [DOI] [PubMed] [Google Scholar]
- 4.Kalla TP, Younger A, McEwen JA, Inkpen K. Survey of tourniquet use in podiatric surgery. J Foot Ankle Surg. 2003;42(2):68–76. doi: 10.1016/S1067-2516(03)70004-0. [DOI] [PubMed] [Google Scholar]
- 5.Sato J, Ishii Y, Noguchi H, Takeda M. Safety and efficacy of a new tourniquet system. BMC Surg. 2012;12(1):17. doi: 10.1186/1471-2482-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hirvensalo E, Tuominen H, Lapinsuo M, Heliö H. Compartment syndrome of the lower limb caused by a tourniquet: a report of two cases. J Orthop Trauma. 1992;6(4):469–472. doi: 10.1097/00005131-199212000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Desai K, Dinh TP, Chung S, Pierpont YN, Naidu DK, Payne WG. Upper extremity deep vein thrombosis with tourniquet use. Int J Surg Case Rep. 2015;6C:55–57. doi: 10.1016/j.ijscr.2014.11.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Odinsson A, Finsen V. Tourniquet use and its complications in Norway. J Bone Joint Surg (Br) 2006;88:1090–1092. doi: 10.1302/0301-620X.88B8.17668. [DOI] [PubMed] [Google Scholar]
- 9.Der Spuy LV. Complications of the arterial tourniquet. South Afr J Anaesth Analg. 2012;18(1):14–18. doi: 10.1080/22201173.2012.10872818. [DOI] [Google Scholar]
- 10.Konrad G, Markmiller M, Lenich A, Mayr E, Rüter A. Tourniquets may increase postoperative swelling and pain after internal fixation of ankle fractures. Clin Orthop Relat Res. 2005;(433):189–94. 10.1097/01.blo.0000151849.37260.0a. [DOI] [PubMed]
- 11.Yi S, Tan J, Chen C, Chen H, Huang W. The use of pneumatic tourniquet in total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg. 2014;134(10):1469–1476. doi: 10.1007/s00402-014-2056-y. [DOI] [PubMed] [Google Scholar]
- 12.Alcelik I, Pollock RD, Sukeik M, Bettany-Saltikov J, Armstrong PM, Eimer P. A comparison of outcomes with and without a tourniquet in total knee arthroplasty a systematic review and meta-analysis of randomized controlled trials. J Arthroplast. 2012;27(3):331–340. doi: 10.1016/j.arth.2011.04.046. [DOI] [PubMed] [Google Scholar]
- 13.Jiang FZ, Zhong HM, Hong YC, Zhao GF. Use of a tourniquet in total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Orthop Sci. 2015;20(1):110–123. doi: 10.1007/s00776-014-0664-6. [DOI] [PubMed] [Google Scholar]
- 14.Tai T-W, Lin C-J, Jou IM, Chang C-W, Lai K-A, Yang C-Y. Tourniquet use in total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1121–1130. doi: 10.1007/s00167-010-1342-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.da Costa Santos CM, de Mattos Pimenta CA, Nobre MRC. The PICO strategy for the research question construction and evidence search. Rev Lat Am Enfermagem. 2007;15(3):508–511. doi: 10.1590/S0104-11692007000300023. [DOI] [PubMed] [Google Scholar]
- 16.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 17.Yin JP, Miao HM, Qiao GY, Yi YL. Effects of bone cement and tourniquet on coagulation function during total knee arthroplasty. Chin J Tissue Eng Res. 2012;16:8186–8190. [Google Scholar]
- 18.Zhou W, Liu DH, Ma GT, Gong YK, Liu JS. Relationship between pneumatic tourniquet application in total knee arthroplasty and hypercoagulability. J Clin Rehabilitat Tissue Eng Res. 2011;15:1541–1544. [Google Scholar]
- 19.Goel R, Rondon AJ, Sydnor K, Blevins K, O'Malley M, Purtill JJ, et al. Tourniquet use does not affect functional outcomes or pain after total knee arthroplasty: a prospective, double-blinded, randomized controlled trial. J Bone Joint Surg Am. 2019;101(20):1821–1828. doi: 10.2106/JBJS.19.00146. [DOI] [PubMed] [Google Scholar]
- 20.Wu Y, Lu X, Ma Y, Zeng Y, Xiong H, Bao X, et al. Efficacy and safety of limb position on blood loss and range of motion after total knee arthroplasty without tourniquet: a randomized clinical trial. Int J Surg. 2018;60:182–187. doi: 10.1016/j.ijsu.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 21.Zhou K, Ling T, Wang H, Zhou Z, Shen B, Yang J, et al. Influence of tourniquet use in primary total knee arthroplasty with drainage: a prospective randomised controlled trial. J Orthop Surg Res. 2017;12(1):172. doi: 10.1186/s13018-017-0683-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Q, Dong J, Gong K, Li X, Zheng S, Wen T. Effects of tourniquet use on perioperative outcome in total knee arthroplasty. Chin J Repar Reconstruct Surg. 2016;30(4):421–425. [PubMed] [Google Scholar]
- 23.Mori N, Kimura S, Onodera T, Iwasaki N, Nakagawa I, Masuda T. Use of a pneumatic tourniquet in total knee arthroplasty increases the risk of distal deep vein thrombosis: a prospective, randomized study. Knee. 2016;23(5):887–889. doi: 10.1016/j.knee.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 24.Ejaz A, Laursen AC, Kappel A, Laursen MB, Jakobsen T, Rasmussen S, et al. Faster recovery without the use of a tourniquet in total knee arthroplasty. Acta Orthop. 2014;85(4):422–426. doi: 10.3109/17453674.2014.931197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang FJ, Xiao Y, Liu YB, Tian X, Gao ZG. Clinical effects of applying a tourniquet in total knee arthroplasty on blood loss. Chin Med J. 2010;123(21):3030–3033. [PubMed] [Google Scholar]
- 26.Wauke K, Nagashima M, Kato N, Ogawa R, Yoshino S. Comparative study between thromboembolism and total knee arthroplasty with or without tourniquet in rheumatoid arthritis patients. Arch Orthop Trauma Surg. 2002;122(8):442–446. doi: 10.1007/s00402-002-0404-9. [DOI] [PubMed] [Google Scholar]
- 27.Vandenbussche E, Duranthon LD, Couturier M, Pidhorz L, Augereau B. The effect of tourniquet use in total knee arthroplasty. Int Orthop. 2002;26(5):306–309. doi: 10.1007/s00264-002-0360-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aglietti P, Baldini A, Vena LM, Abbate R, Fedi S, Falciani M. Effect of tourniquet use on activation of coagulation in total knee replacement. Clin Orthop Relat Res. 2000;371:169–177. doi: 10.1097/00003086-200002000-00021. [DOI] [PubMed] [Google Scholar]
- 29.Wakankar HM, Nicholl JE, Koka R, D’Arcy JC. The tourniquet in total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Am. 1999;81(1):30–33. doi: 10.1302/0301-620X.81B1.0810030. [DOI] [PubMed] [Google Scholar]
- 30.Abdelsalam A, Eyres KS. Effects of tourniquet during total knee arthroplasty - a prospective randomized study. J Bone Joint Surg (Br) 1995;77B:250–253. doi: 10.1302/0301-620X.77B2.7706340. [DOI] [PubMed] [Google Scholar]
- 31.Li B, Wen Y, Wu H, Qian Q, Lin X, Zhao H. The effect of tourniquet use on hidden blood loss in total knee arthroplasty. Int Orthop. 2009;33(5):1263–1268. doi: 10.1007/s00264-008-0647-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Virchow R. Phlogose und Thrombose im Gefasssystem. In : Hirsch M, ed. Berlin: Gesammelte Abhandlungen Zur Wissenschaftlichen Medizin; 1856. p. 458–63.
- 33.Leurcharusmee P, Sawaddiruk P, Punjasawadwong Y, Chattipakorn N, Chattipakorn SC. The possible pathophysiological outcomes and mechanisms of tourniquet-induced ischemia-reperfusion injury during total knee arthroplasty. Oxidative Med Cell Longev. 2018;8087598. 10.1155/2018/8087598. [DOI] [PMC free article] [PubMed]
- 34.Jackson SP, Darbousset R, Schoenwaelder SM. Thromboinflammation: challenges of therapeutically targeting coagulation and other host defense mechanisms. Blood. 2019;133(9):906–918. doi: 10.1182/blood-2018-11-882993. [DOI] [PubMed] [Google Scholar]
- 35.Fukuda A, Hasegawa M, Kato K, Shi D, Sudo A, Uchida A. Effect of tourniquet application on deep vein thrombosis after total knee arthroplasty. Arch Orthop Trauma Surg. 2007;127(8):671–675. doi: 10.1007/s00402-006-0244-0. [DOI] [PubMed] [Google Scholar]
- 36.Wells PS, Anderson DR, Rodger M, Forgie M, Kearon C, Dreyer J, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med. 2003;349(13):1227–1235. doi: 10.1056/NEJMoa023153. [DOI] [PubMed] [Google Scholar]
- 37.Reikeras O, Clementsen T. Time course of thrombosis and fibrinolysis in total knee arthroplasty with tourniquet application. Local versus systemic activations. J Thromb Thrombolysis. 2008;28:425. doi: 10.1007/s11239-008-0299-6. [DOI] [PubMed] [Google Scholar]
- 38.Carden DL, Granger DN. Pathophysiology of ischaemia-reperfusion injury. J Pathol. 2000;190(3):255–266. doi: 10.1002/(SICI)1096-9896(200002)190:3<255::AID-PATH526>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in published articles.