Abstract
Isotemporal substitution modelling (ISM) and compositional isotemporal modelling (CISM) are statistical approaches used in epidemiology to model the associations of replacing time in one physical behaviour with time in another. This study’s aim was to use both ISM and CISM to examine and compare associations of reallocating 60 min of sitting into standing or stepping with markers of cardiometabolic health. Cross-sectional data collected during three randomised control trials (RCTs) were utilised. All participants (n = 1554) were identified as being at high risk of developing type 2 diabetes. Reallocating 60 min from sitting to standing and to stepping was associated with a lower BMI, waist circumference, and triglycerides and higher high-density lipoprotein cholesterol using both ISM and CISM (p < 0.05). The direction and magnitude of significant associations were consistent across methods. No associations were observed for hemoglobin A1c, total cholesterol, or low-density lipoprotein cholesterol for either method. Results of both ISM and CISM were broadly similar, allowing for the interpretation of previous research, and should enable future research in order to make informed methodological, data-driven decisions.
Keywords: sedentary behaviour, physical activity, time use, cardiometabolic health
1. Introduction
There is a substantial body of epidemiological evidence linking high sedentary behaviour and lack of physical activity (PA) with morbidity [1,2,3,4] and mortality [2,5,6,7,8]. Recently, there has been an increase in the number of studies that have examined both PA and sedentary behaviour and their impact or associations with health, either by modelling the association of reallocating time from one to another [9,10,11,12,13,14,15,16,17,18,19,20,21,22], or by accounting for the other behaviours as covariates [23,24,25,26].
The term ‘physical behaviours’ refers to any behaviour contributing to the 24-h movement and non-movement conceptual model outlined by Trembley et al. (2017) [27], which represents a consensus project to create clear, common, and accepted terminology and definitions. However, how to treat physical behaviour data when assessing the associations between specific behaviours and health has become a debated topic in recent years [17,28]. Often, data have been treated as continuous and unbounded, as this is the way these behaviours have typically been conceptualised. For example, when assessing the associations of time spent in sedentary behaviour with health, traditionally, one would use minutes or hours spent in sedentary behaviour as the independent variable and then include a PA variable, typically moderate-to-vigorous physical activity (MVPA), as a covariate [29]. However, by doing this, statistical models may not account for the inherent collinearity between time spent sedentary and time spent in PA. Research has shown that collinearity varies between sedentary behaviour and different intensities of PA or non-sedentary behaviours [9,29]. This has led to the development of methodological approaches which aim to address the co-dependence of physical behaviours, which are identified as composites of a finite whole (i.e., a 24-h day). Put simply, changes in one behaviour will affect time allocated to other behaviours.
Isotemporal substitution first addressed the need to recognise the finite nature of time and to understand that in order to change behaviour one must substitute time in that behaviour with time in another [30]. The isotemporal substitution model (ISM) uses data in original, conceptualised units such as hours and uses a specific time period to bind the behaviours into a finite period. Questions have been raised about the suitability of these data in absolute values (i.e., time) to be used in behavioural epidemiology [11]. It has been argued that data that are intrinsically collinear or compositional must be treated as relative values, not absolute [29]. For example, step count is an absolute value, whereas the minutes spent stepping per day are relative to the 24-h day. Compositional isotemporal substitution (CISM) seeks to address these issues for the use of absolute data, such as time spent in different activities [11,29]. It is important to understand the convergence and divergence of these two methodologies regarding associations with health to ensure previous and future evidence is correctly interpreted.
Current evidence, primarily using the ISM approach but not exclusively, has consistently shown beneficial associations with markers of health when time is reallocated from sedentary behaviour to active, non-sedentary behaviours [9,10,11,12,13,14,15,16,17,18,19,20]. Beneficial associations have been reported for post-challenge glucose and insulin [9,12,15,20], chronic-low grade inflammation [16], and other cardiometabolic biomarkers [10,13,14,15], as well as for risk of all-cause mortality [18]. A large proportion of evidence has utilised accelerometers to assess physical behaviours, typically worn at the hip or wrist [31,32], whereby sedentary time is inferred from lack of movement rather than postural allocation. A recent study noted this is a major limitation of the literature concerning sedentary behaviour and health [33]. A handful of studies utilised thigh-worn accelerometers, which have the capability of identifying posture, and modelled the reallocation of time from sitting to standing and stepping [9,12,15,16,19]. These studies all showed inverse associations with markers of health when time was reallocated from sitting to stepping, while three showed inverse associations when time was reallocated from sitting to standing [12,15,16]. Despite this, the evidence utilising thigh-worn accelerometery to examine associations between sitting and health remains limited.
This study’s aim was to use both ISM and CISM to examine and compare associations of reallocating time from sitting to standing or stepping, assessed using thigh-worn accelerometery, with markers of cardiometabolic health.
2. Materials and Methods
2.1. Participants
We performed a pooled analysis of cross-sectional data collected across 3 randomised control trials (RCTs)—the Promotion of Physical activity through structured Education with differing Levels of ongoing Support for people at high risk of type 2 diabetes (T2DM) (PROPELS), Walking Away from Diabetes, and Project STAND (Sedentary Time And Diabetes). Each study recruited individuals from primary care identified as being at high risk of developing T2DM. The protocols for each study have been published previously [34,35,36]. All studies received ethical approval and followed identical standard operating procedures (performed by different research professionals) to collect the dependent and independent variables of interest. All participants provided written informed consent. Each study had its own inclusion and exclusion criteria, as described below.
2.1.1. PROPELS
The PROPELS study (ISRCTN83465245) was a multi-centre 3-arm RCT with 48-month follow-up and data collection completed in July 2019 to evaluate an intervention designed to increase physical activity in an ethnically diverse population at high risk of developing T2DM. Participants were eligible if they were aged 40–74 years and were White European, or aged 25–74 years and were South Asian, had a fasting plasma glucose (≥5.5 to <7.0 mmol/L) or HbA1c (≥6.0 to <6.5%; ≥42 to <48 mmol/mol) value within the prediabetes range [37], and had access to a mobile phone and were willing to use it as part of the study. Data collected at baseline were used for this analysis.
2.1.2. Walking Away from Diabetes (WA)
The WA study (ISRCTN31392913) was a cluster RCT with 36-month follow-up completed in January 2014 which evaluated an intervention designed to increase physical activity in those at high risk of developing T2DM. Participants were eligible if they were aged 18–74 years and scored in the 90th centile of the automated version of the Leicester Risk Assessment tool [38]. Participants were excluded if they had an existing diagnosis of T2DM, were diagnosed with T2DM at a baseline appointment, were taking steroids, or were unable to speak English. Data collected at the 3-year follow-up (2013–2014) were used for this analysis as this was the only time point where activPAL data were collected (see the physical behaviour measurement section).
2.1.3. STAND
The STAND study (ISRCTN08434554) was an RCT with 12-month follow-up completed in 2012 aimed at reducing sitting time in young adults at high risk of developing T2DM. Participants were eligible if they were aged 18–40 years, obese (BMI (body mass index) ≥30 kg/m2 for White Europeans and ≥27.5 kg/m2 for South Asians) or overweight (≥25 kg/m2 and ≥23 kg/m2), with 1 additional risk factor for diabetes (family history of diabetes or cardiovascular disease in a first-degree relative; previous gestational diabetes; polycystic ovarian syndrome; HbA1c ≥5.8% or ≥40 mmol/mol; impaired glucose tolerance and/or impaired fasting glucose) [39]. Data collected at baseline were used for this analysis.
2.2. Sedentary Behaviour and Physical Activity Measurement
Data were collected using the activPAL3™ (PAL Technologies, Glasgow, UK) attached at the midline anterior aspect of the upper thigh with a hypoallergenic dressing. The devices were waterproofed with a nitrile sleeve and wrapped in waterproof hypoallergenic dressing to allow for 24-h wear. Participants were asked to wear the device continuously for up to 7 days in PROPELS and WA and 10 days in Project STAND. The activPAL determines body posture (i.e., sitting/lying and upright activity, standing and stepping) [40]. The activPAL has been shown to be highly accurate in detecting lying, sitting, and upright behaviours [41]. activPAL data (event files) were processed using Processing PAL v1.21 (University of Leicester, UK) [42]. This java application uses a validated algorithm to identify valid waking wear time [43], and it produces summary data based on the identified valid waking wear data. The default algorithm thresholds within the application were used. The processed data were visualised using the heatmaps created within the application to identify any occasions where the algorithm incorrectly coded ‘sleep’ and waking behaviour (e.g., early wake and bedtimes in comparison to other days). On such occasions the self-reported sleep log was referred to, and if necessary, the data were corrected. Participants with ≥4 valid wear days (≥10 h, ≥500 step events (i.e., 1000 steps), ≤95% spent in sitting, standing or stepping) were included in this analysis [43].
2.3. Anthropometric and Blood Pressure Measurement
Blood pressure was measured in a sitting position (Omron, Healthcare, Henfield, UK). In total 3 measurements were taken, with an average of the last 2 calculated. Body weight, body fat percentage, height and waist circumference were measured to the nearest 0.1 kg, 0.5%, 0.5 cm, and 0.1 cm, respectively. Waist circumference was measured at the midline between the iliac crest and the lowest rib. Body mass index (BMI) was calculated as mass (kg)/height2 (m).
2.4. Cardiometabolic Biomarker Measurement
The cardiometabolic outcomes which were measured across all 3 studies were included in this analysis. All biomarkers were assessed by venous sampling, obtained after an overnight fast and analysed in clinical laboratories using validated quality-controlled assays. Analysis was conducted by individuals blinded to the patients’ identity using stable methodologies (the ability of the sample material to maintain its original properties) standardised to external quality assurance values. The biomarkers included were haemoglobin A1c (HbA1c) and lipid profile (total cholesterol, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, triglycerides). A clustered cardiometabolic risk score (CCRS) was generated to assess overall cardiometabolic risk by calculating an average of the standardised ((value–mean)/SD) values for HbA1c, triglycerides, mean of systolic and diastolic blood pressure, HDL cholesterol (inverted), and waist circumference. This method has been reported and validated previously [44,45,46]. Overall, 2 scores were calculated, with 1 including waist circumference and 1 without. This allowed us to examine any mediation effect of change in adiposity for any associations observed for the CCRS. A higher score represents a higher cardiometabolic risk.
2.5. Covariates
Date of birth, sex, ethnicity, and current medication were recorded using an interview-administered questionnaire. Participants who reported taking angiotensin converting enzyme inhibitors, alpha-blockers, angiotensin receptor blockers, beta-blockers, calcium channel blockers, or diuretics/thiazides were classified as taking blood pressure medication. Participants who reported taking statins or fibrates were classified as taking lipid-lowering medication. An Index of Multiple Deprivation (IMD) score was generated using the participants’ home postcodes. These scores are publicly available continuous measures of compound social and material deprivation that are calculated using a variety of data including current income, employment, education, and housing. All covariates were chosen due to their potential influence on cardiometabolic health.
2.6. Statistical Analysis
Analyses were performed using R statistical systems (version 3.4.3, R Foundation for Statistical Computing, Vienna, Austria) and IBM SPSS Statistics 24 (IBM, Armonk, NY, USA). ISM and CISM were conducted to examine the associations of reallocating 60 min of sitting for standing or stepping with markers of cardiometabolic health and adiposity. Dependent (outcome) variables were standardised to allow comparisons. The covariates included in both ISM and CISM were age, sex, ethnicity, IMD score, blood pressure medication, and lipid-lowering medication. Both models report β coefficients which represent a 1-unit (hour) change in a given behaviour, with significance set at an alpha at ≤0.05.
2.6.1. Isotemporal Substitution Modelling
Linear regression models were conducted following an ISM [30]. For the purposes of this analysis, ISM required average waking wear time, standing time, and stepping time to be simultaneously entered into a regression model, with the resulting regression coefficient for standing time and stepping time representing the association of substituting a given unit of sitting time (in this case, 60 min) into each category, respectively. Importantly, the inclusion of average waking wear time ensures the reallocation is modelled within a given time frame—the time participants were awake.
2.6.2. Compositional Isotemporal Substitution Modelling
CISM were conducted using similar methodologies as outlined previously [9,11,47]. CISM uses isometric log ratios (ILRs) to model the physical behaviour composition within real space, allowing conventional statistical models to be conducted. ILRs are calculated for various compositions modelling the reallocations of time from sitting to standing and stepping. In this case, ILRs were calculated to reflect a reallocation of 60 min from sitting to standing and for 60 min from sitting to stepping. These are calculated from the mean physical behaviour composition. These ILRs are then fitted to a multiple linear regression model, which models the reallocation of time spent in one behaviour with another pairwise within a set time frame, in this case waking time when wearing the activPAL device. There were no zero values in the combined dataset, and therefore no recoding had to be undertaken.
2.6.3. Incremental Comparison
In order to assess the dose–response association for reallocating time from one behaviour to another, both ISM and CISM were run to model 5-min reallocations to 60-min reallocations at 5-min intervals. Five-minute reallocations were conducted to replicate, statistically, experimental research that has widely used 5-min changes in behaviour [48,49,50]. This resulted in 12 separate models for ISM and CISM respectively. This was conducted for zBMI only in this instance to explore the convergence and divergence between models more closely. Previous epidemiological work has shown that, when examining cardiometabolic health, the strongest and most consistent associations exist between sedentary time, physical activity, and adiposity [26].
3. Results
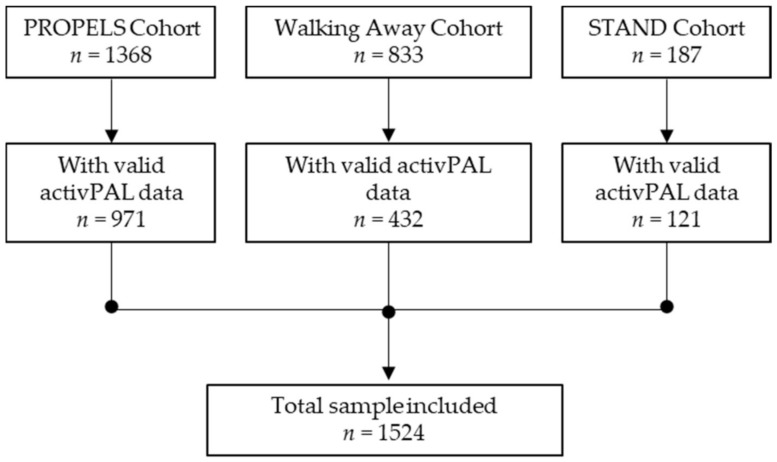
A total of 2388 participants were recruited across the PROPELS, WA, and STAND studies, of which 1524 participants had valid activPAL data and were included in these analyses (sample loss of 36%) (see Figure 1). The mean age was 59.8 years (standard deviation 11.9), 51.7% were male, 72.9% were White European, and the mean BMI was 30.3 kg/m2 (5.72). Basic participant characteristics are included in Table 1. Participants not included in these analyses (N = 864) were younger (58 years of age vs. 60 years of age, p = 0.023) and had a higher HbA1c (5.81% vs. 5.76%, p = 0.008).
Figure 1.
Participant flow diagram.
Table 1.
Participant characteristics.
| Characteristics | All (n = 1524) | PROPELS (n = 971) | WA (n = 432) | STAND (n = 121) |
|---|---|---|---|---|
| Age (years) | 59.8 (11.9) | 59.9 (9.0) | 66.8 (7.4) | 32.8 (5.7) |
| Male (%) | 51.7 | 49.9 | 61.8 | 29.9 |
| White European (%) | 72.9 | 70.5 | 89.1 | 75.2 |
| Body mass index (kg/m2) | 30.3 (5.7) | 29.3 (5.7) | 31.4 (5.3) | 34.4 (5.1) |
| Waist circumference (cm) | 100 (14) | 98 (14) | 103 (13) | 103 (13) |
| Using blood pressure medication (%) | 40.2 | 38.2 | 48.6 | 3.3 |
| Using lipid-lowering medication (%) | 27.9 | 28.3 | 30.1 | 0.8 |
| Current smokers (%) | 9.1 | 8.9 | 7.2 | 19.0 |
| HbA1c (unit %) | 5.8 (0.4) | 5.8 (0.3) | 5.7 (0.5) | 5.5 (0.3) |
| Sitting (min/day) | 548 (112) | 542 (113) | 568 (109) | 530 (107) |
| Standing (min/day) | 286 (96) | 296 (97) | 268 (89) | 277 (91) |
| Stepping (min/day) | 107 (40) | 111 (40) | 101 (38) | 103 (37) |
HbA1c = Haemoglobin A1c, data for continuous variables are reported as mean ± standard deviation.
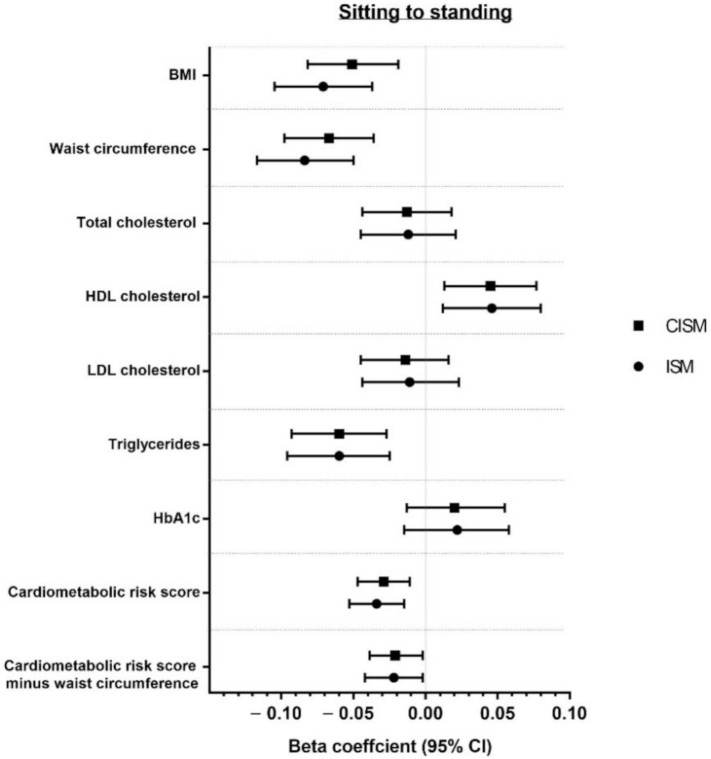
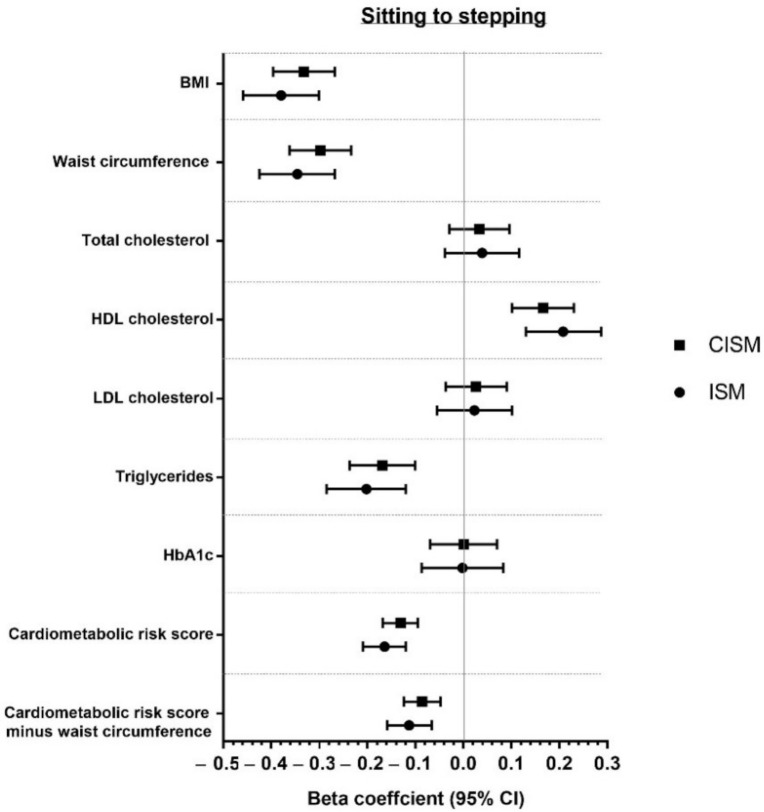
Associations of modelling reallocation of time from sitting to standing and from sitting to stepping for both CISM and ISM are presented in Figure 2 and Figure 3. Associations are also reported in Supplementary Table S1. Overall, both models showed favourable associations when reallocating time from sitting to standing or stepping for BMI, waist circumference, triglycerides, HDL cholesterol, and CCRS (with and without adiposity). The strongest associations for sitting to standing or stepping were for waist circumference and BMI for both models. No significant associations were found for any behavioural reallocation for HbA1c, total cholesterol, or LDL cholesterol in either model.
Figure 2.
Reallocation of 60 min from sitting to standing.
Figure 3.
Reallocation of 60 min from sitting to stepping.
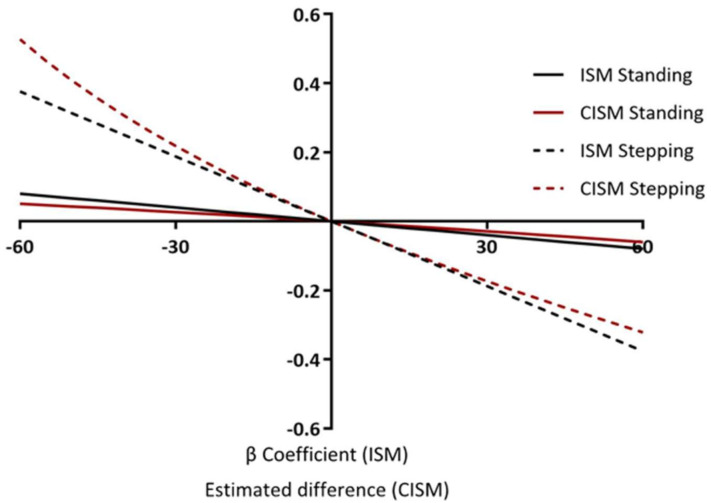
Figure 4 shows the associations of reallocating time from sitting to standing or stepping, and from standing and stepping to sitting for zBMI. Reallocations were made in 5-min increments, starting with 5 min through to 60 min for both ISM and CISM. This demonstrates how the reallocations are asymmetrical for CIMS, yet symmetrical for ISM. Reallocating 60 min of sitting to stepping and of stepping to sitting for zBMI using ISM equates to a β-coefficient of −0.37 (−0.44, −0.29) and 0.37 (0.44, 0.29) respectively, showing perfect symmetry. Whereas, reallocating 60 min of sitting to stepping and of stepping to sitting for zBMI using CISM equates to an estimated difference of −0.23 (−0.27, −0.19) and 0.32 (0.25, 0.38) respectively, which is asymmetrical. The reallocations are also assumed to be linear for ISM, whereas for CISM they are non-linear. For example, ISM shows that the association for reallocating 30 min of sitting to stepping is exactly half the association for reallocating 60 min of sitting with stepping (−0.183 (−0.222, −0.143), −0.365 (−0.444, −0.286)). CIMS, however, shows the association for reallocating 30 min of sitting with stepping is a little more than half of the association for reallocating 60 min of sitting with stepping (−0.122 (−0.146, −0.098), −0.230 (−0.274, −0.185)). The non-linear associations for CISM are further demonstrated when reporting the reallocations from stepping to sitting. For example, the association for reallocating 30 min of stepping with sitting is 45% of the estimated difference for reallocating 60 min of stepping with sitting (0.142 (0.114, 0.170), 0.315 (0.251, 0.378)).
Figure 4.
Incremental reallocations: multiple behavioural reallocations examining 5-min increments on zBMI.
4. Discussion
This study used ISM and CISM analyses to examine the associations of replacing time spent sitting with standing or stepping and with markers of cardiometabolic health. Overall, the findings showed minimal differences in the magnitude of associations between the methods. Both methods demonstrated favourable associations for the reallocation of 60 min of sitting to standing and to stepping for BMI, waist circumference, triglycerides, HDL cholesterol, and CCRS (with and without adiposity). Nevertheless, whilst it was observed that the overall interpretation was similar between models, associations were consistently stronger for ISM models, although these differences were statistically and clinically negligible.
The main difference between methods was in the incremental comparisons, where time was reallocated from sitting to standing or stepping, and vice versa. Here we showed that CISM produced small, yet observable, asymmetrical and non-linear associations when time was reallocated at 5-min increments. ISM produced symmetrical and linear associations. Considering this, the results of modelling the reallocation of larger periods of time may result in larger differences between models, impacting the interpretation of results. However, given the negligible clinical and statistical difference in the magnitude of associations for small reallocations of time, the interpretations of these results are fundamentally similar. However, it is possible that these differences could have an impact on public health messages if the reasons for any differences between models are not better understood. It is therefore advised that future analyses should consider the potential impact of these differences in the interpretation of either ISM or CISM outputs, and perhaps use both methodologies simultaneously. Mechanistic and interventional research is needed to investigate which model provides the better estimation of the ‘true’ association. Furthermore, although minimal differences are observed between models in these analyses, it may be the case that differences are observed in other samples with different mean compositions of behaviour.
One study has compared these methodologies previously; however, this was only done for one variable (body fat percentage) and was in children [22]. Furthermore, a previous study that utilised CISM did include the results of ISM in the supplementary material [9]. However, there was no direct comparison of the results in the main paper. Previous work involving both methods have claimed the superiority of one over the other. Conversely, in the development of CISM, it was stated that ISM violates the compositional properties of time-use data [11]. Although this may be true, no evidence was provided showing the results were in some way incorrect or invalid. The results presented in this study suggest that the use of either method produces broadly comparable results when examining the reallocation of time spent sitting to standing or stepping, assessed with thigh-worn accelerometery, on markers of cardiometabolic health and adiposity. Therefore, the decision as to which methodology to use should be based on the data in use and the research question stipulated, with a consideration of the interpretation of results.
The associations observed here are similar to previous studies that used ISM and CISM to examine association of reallocating time from one physical behaviour to another on markers of cardiometabolic health [15,19,21,51]. Two previous studies that utilised thigh-worn accelerometery to assess physical behaviours showed that reallocating time from sitting to movement was favourably associated with waist circumference, triglycerides, and HDL [15,19]. Reallocating time from sitting to standing was favourably associated with triglycerides and HDL [15]. In older adults, Ryan et al. (2019) showed that modelling the reallocation of time in sedentary behaviour to time in physical activity was favourably associated with total cholesterol and triglycerides [21]. In the current study, favourable associations were observed for reallocating time from sitting to standing and stepping for triglycerides, but not for total cholesterol. Further to this, it was previously shown that, over a 7-year period, reallocating time from sedentary behaviour to MVPA was associated with a reduction in BMI and body fat percentage for older women [51]. This supports the results presented here, because the associations of the reallocation of sitting to standing and stepping were the strongest for BMI and waist circumference.
It is noteworthy that reallocation of time from sitting to standing had favourable associations. Some, but not all, experimental studies support this observation, particularly in those at risk of developing type 2 diabetes [48]. However, this study supports the majority of epidemiological studies conducted to date, which have suggested that whilst standing may have some positive associations, associations are consistently stronger for re-allocation into more intensive forms of movement [46].
This study has several strengths. The measurement of sedentary behaviour and physical activity was with a device that accurately distinguishes between postures (i.e., sitting, standing, and stepping). Widely used and valid health markers were included. The large, heterogeneous, multi-ethnic sample of individuals identified as being at high risk of T2DM accurately reflects individuals likely to receive/benefit from interventions aiming to reducing sitting by increasing movement.
However, this study is not without limitations. The sample is not necessarily generalisable to the general population, meaning results should be treated with caution in non-clinical, healthy populations. There is the potential limitation of pooling three large datasets. However, each study followed the same standard operating procedures when collecting the data. Furthermore, models were adjusted for differences between datasets (i.e., age). Results are cross-sectional; therefore, inferences about causality are not possible. However, the dataset provided a valuable resource with which to test the comparability of the two dominant statistical approaches used to model behavioural reallocation. Similar work is encouraged to replicate these findings in healthy populations across different age and sociodemographic groups.
5. Conclusions
In conclusion, reallocating time from sitting to standing or from sitting to stepping showed beneficial associations with BMI, waist circumference, triglycerides, HDL, and CCRS (with and without adiposity). Results from ISM and CISM are broadly similar, with no differences observed in the direction or magnitude of associations. Minor differences were observed in the symmetry of associations, which requires future research to examine the possible mechanism underpinning these differences, whether it be statistical or physiological. The differences in the symmetry of associations do suggest these methodologies may diverge to a greater extent when larger amounts of time are reallocated, therefore limiting the comparability of these methodologies to smaller reallocations of time. These results allow for appropriate and informed decisions on methodology based on a data-driven approach.
Acknowledgments
The authors would like to thank the participants who volunteered for these studies.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph18126210/s1, Table S1: The associations of reallocating time spent sitting with standing and with stepping.
Author Contributions
Conceptualization, G.J.H.B., J.H., A.V.R., T.Y. and C.L.E.; methodology, G.J.H.B. and J.H.; formal analysis, G.J.H.B. and J.H.; data curation, S.J.H.B., M.J.D., K.K., S.S. and T.Y.; writing—original draft preparation, G.J.H.B.; writing—review and editing, G.J.H.B., J.H., S.J.H.B., M.J.D., A.V.R., K.K., S.S., T.Y. and C.L.E.; visualization, G.J.H.B. and J.H.; supervision, M.J.D., A.V.R., K.K., T.Y. and C.L.E.; funding acquisition, S.J.H.B., M.J.D., K.K., S.S. and T.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by NIHR Collaborations for Leadership in Applied Health Research and Care (CLAHRC) East Midlands and was supported by the NIHR Leicester Biomedical Research Centre.
Institutional Review Board Statement
These studies were conducted according to the guidelines of the Declaration of Helsinki and were approved by the Leicester Research Ethics Committee (ref: 12/EM/0151, 04/05/2012), the Nottingham Research Ethics Committee 2 (ref: 09/H0408/32, 02/03/2009), and the Nottingham National Health Service Research Ethics Committee (ref: 10/H0403/13m 07/05/2010).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ethical restrictions.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Biswas A., Oh P.I., Faulkner G.E., Bajaj R.R., Silver M.A., Mitchell M.S. Sedentary Time and Its Association with Risk for Disease Incidence, Mortality, and Hospitalization in Adults: A Systematic Review and Meta-Analysis. Ann. Intern. Med. 2015;162:123–132. doi: 10.7326/M14-1651. [DOI] [PubMed] [Google Scholar]
- 2.Patterson R., McNamara E., Tainio M., de Sa T.H., Smith A.D., Sharp S.J., Edwards P., Woodcock J., Brage S., Wijndaele K. Sedentary Behaviour and Risk of All-Cause, Cardiovascular and Cancer Mortality, and Incident Type 2 Diabetes: A Systematic Review and Dose Response Meta-Analysis. Eur. J. Epidemiol. 2018;33:811–829. doi: 10.1007/s10654-018-0380-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilmot E.G., Edwardson C.L., Achana F.A., Davies M.J., Gorely T., Gray L.J., Khunti K., Yates T., Biddle S.J.H. Sedentary Time in Adults and the Association with Diabetes, Cardiovascular Disease and Death: Systematic Review and Meta-Analysis. Diabetologia. 2012;55:2895–2905. doi: 10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
- 4.Lee I.M., Shiroma E.J., Lobelo F., Puska P., Blair S.N., Katzmarzyk P.T. Effect of Physical Inactivity on Major Non-Communicable Diseases Worldwide: An Analysis of Burden of Disease and Life Expectancy. Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ku P.-W., Steptoe A., Liao Y., Hsueh M.-C., Chen L.-J. A Cut-Off of Daily Sedentary Time and All-Cause Mortality in Adults: A Meta-Regression Analysis Involving More than 1 Million Participants. BMC Med. 2018;16:74. doi: 10.1186/s12916-018-1062-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ekelund U., Brown W.J., Steene-Johannessen J., Fagerland M.W., Owen N., Powell K.E., Bauman A.E., Lee I.-M. Do the Associations of Sedentary Behaviour with Cardiovascular Disease Mortality and Cancer Mortality Differ by Physical Activity Level? A Systematic Review and Harmonised Meta-Analysis of Data From 850 060 Participants. Br. J. Sports Med. 2018 doi: 10.1136/bjsports-2017-098963. [DOI] [PubMed] [Google Scholar]
- 7.Ekelund U., Steene-Johannessen J., Brown W.J., Fagerland M.W., Owen N., Powell K.E., Bauman A., Lee I.M. Does Physical Activity Attenuate, or Even Eliminate, the Detrimental Association of Sitting Time with Mortality? A Harmonised Meta-Analysis of Data from More Than 1 Million Men and Women. Lancet. 2016;388:1302–1310. doi: 10.1016/S0140-6736(16)30370-1. [DOI] [PubMed] [Google Scholar]
- 8.Ekelund U., Tarp J., Steene-Johannessen J., Hansen B.H., Jefferis B., Fagerland M.W., Whincup P., Diaz K.M., Hooker S.P., Chernofsky A., et al. Dose-Response Associations Between Accelerometry Measured Physical Activity and Sedentary Time and All Cause Mortality: Systematic Review and Harmonised Meta-Analysis. BMJ. 2019;366:l4570. doi: 10.1136/bmj.l4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Biddle G.J.H., Edwardson C.L., Henson J., Davies M.J., Khunti K., Rowlands A.V., Yates T. Associations of Physical Behaviours and Behavioural Reallocations with Markers of Metabolic Health: A Compositional Data Analysis. Int. J. Environ. Res. Public Health. 2018;15:2280. doi: 10.3390/ijerph15102280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buman M.P., Winkler E.A.H., Kurka J.M., Hekler E.B., Baldwin C.M., Owen N., Ainsworth B.E., Healy G.N., Gardiner P.A. Reallocating Time to Sleep, Sedentary Behaviors, or Active Behaviors: Associations with Cardiovascular Disease Risk Biomarkers, NHANES 2005–2006. Am. J. Epidemiol. 2014;179:323–334. doi: 10.1093/aje/kwt292. [DOI] [PubMed] [Google Scholar]
- 11.Dumuid D., Pedisic Z., Stanford T.E., Martin-Fernadez J.-A., Hron K., Maher C.A., Lewis L.K., Olds T. The Compositional Isotemporal Substitution Model: A Method for Estimating Changes in a Health Outcome for Reallocation of Time Between Sleep, Physical Activity and Sedentary Behaviour. Stat. Methods Med Res. 2017;3:1–12. doi: 10.1177/0962280217737805. [DOI] [PubMed] [Google Scholar]
- 12.Edwardson C.L., Henson J., Bodicoat D.H., Bakrania K., Khunti K., Davies M.J., Yates T. Associations of Reallocating Sitting Time into Standing or Stepping with Glucose, Insulin and Insulin Sensitivity: A Cross-Sectional Analysis of Adults at Risk of Type 2 Diabetes. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2016-014267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Falconer C.L., Page A.S., Andrews R.C., Cooper A.R. The Potential Impact of Displacing Sedentary Time in Adults with Type 2 Diabetes. Med. Sci. Sports Exerc. 2015;47:2070–2075. doi: 10.1249/MSS.0000000000000651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hamer M., Stamatakis E., Steptoe A. Effects of Substituting Sedentary Time with Physical Activity on Metabolic Risk. Med. Sci. Sports Exerc. 2014;46:1946–1950. doi: 10.1249/MSS.0000000000000317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Healy G.N., Winkler E.A.H., Owen N., Anuradha S., Dunstan D.W. Replacing Sitting Time with Standing or Stepping: Associations with Cardio-Metabolic Risk Biomarkers. Eur. Heart J. 2015;36:2643–2649. doi: 10.1093/eurheartj/ehv308. [DOI] [PubMed] [Google Scholar]
- 16.Henson J., Edwardson C.L., Bodicoat D.H., Bakrania K., Davies M.J., Khunti K., Talbot D.C.S., Yates T. Reallocating Sitting Time to Standing or Stepping Through Isotemporal Analysis: Associations with Markers of Chronic Low-Grade Inflammation. J. Sports Sci. 2017:1–8. doi: 10.1080/02640414.2017.1405709. [DOI] [PubMed] [Google Scholar]
- 17.Mekary R.A., Ding E.L. Isotemporal Substitution as the Gold Standard Model for Physical Activity Epidemiology: Why It Is the Most Appropriate for Activity Time Research. Int. J. Environ. Res. Public Health. 2019;16:797. doi: 10.3390/ijerph16050797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stamatakis E., Rogers K., Ding D., Berrigan D., Chau J., Hamer M., Bauman A. All-Cause Mortality Effects of Replacing Sedentary Time with Physical Activity and Sleeping Using an Isotemporal Substitution Model: A Prospective Study of 201,129 Mid-Aged and Older Adults. Int. J. Behav. Nutr. Phys. Act. 2015;12:121. doi: 10.1186/s12966-015-0280-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Varela-Mato V., O’Shea O., King J.A., Yates T., Stensel D.J., Biddle S.J., Nimmo M.A., Clemes S.A. Cross-Sectional Surveillance Study to Phenotype Lorry Drivers’ Sedentary Behaviours, Physical Activity and Cardio-Metabolic Health. BMJ Open. 2017;7:e013162. doi: 10.1136/bmjopen-2016-013162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yates T., Henson J., Edwardson C., Dunstan D., Bodicoat D.H., Khunti K. Objectively Measured Sedentary Time and Associations with Insulin Sensitivity: Importance of Reallocating Sedentary Time to Physical Activity. Prev. Med. 2015;76:79–83. doi: 10.1016/j.ypmed.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 21.Ryan D.J., Wullems J.A., Stebbings G.K., Morse C.I., Stewart C.E., Onambele-Pearson G.L. Using Isotemporal Substitution to Predict the Effects of Changing Physical Behaviour on Older Adults’ Cardio-Metabolic Profiles. PLoS ONE. 2019;14:e0224223. doi: 10.1371/journal.pone.0224223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dumuid D., Stanford T.E., Pedisic Z., Maher C., Lewis L.K., Martin-Fernandez J.A., Katzmarzyk P.T., Chaput J.P., Fogelholm M., Standage M., et al. Adiposity and the Isotemporal Substitution of Physical Activity, Sedentary Time and Sleep Among School-Aged Children: A Compositional Data Analysis Approach. BMC Public Health. 2018;18:311. doi: 10.1186/s12889-018-5207-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van der Ploeg H.P., Chey T., Korda R.J., Banks E., Bauman A. Sitting Time and All-Cause Mortality Risk in 222 497 Australian Adults. Arch. Intern. Med. 2012;172:494–500. doi: 10.1001/archinternmed.2011.2174. [DOI] [PubMed] [Google Scholar]
- 24.van der Ploeg H.P., Chey T., Ding D., Chau J.Y., Stamatakis E., Bauman A.E. Standing Time and All-Cause Mortality in a Large Cohort of Australian Adults. Prev. Med. 2014;69:187–191. doi: 10.1016/j.ypmed.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 25.Bakrania K., Edwardson C.L., Khunti K., Bandelow S., Davies M.J., Yates T. Associations Between Sedentary Behaviours and Cognitive Function: Cross-Sectional and Prospective Findings from the UK Biobank. Am. J. Epidemiol. 2017;187:441–454. doi: 10.1093/aje/kwx273. [DOI] [PubMed] [Google Scholar]
- 26.Henson J., Yates T., Biddle S.J., Edwardson C.L., Khunti K., Wilmot E.G. Associations of Objectively Measured Sedentary Behaviour and Physical Activity with Markers of Cardiometabolic Health. Diabetologia. 2013;56:1012–1020. doi: 10.1007/s00125-013-2845-9. [DOI] [PubMed] [Google Scholar]
- 27.Tremblay M.S., Aubert S., Barnes J.D., Saunders T.J., Carson V., Latimer-Cheung A.E., Chastin S.F.M., Altenburg T.M., Chinapaw M.J.M. Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project Process and Outcome. Int. J. Behav. Nutr. Phys. Act. 2017;14:75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Biddle G.J.H., Edwardson C.L., Henson J., Rowlands A.V., Yates T. Reply to Mekary, R.A.; Ding, E.L. Isotemporal Substitution as the Gold Standard Model for Physical Activity Epidemiology: Why It Is the Most Appropriate for Activity Time Research. Int. J. Environ. Res. Public Health 2019, 16, 797. Int. J. Environ. Res. Public Health. 2019;16:2885. doi: 10.3390/ijerph16162885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chastin S.F.M., Palarea-Albaladejo J., Dontje M.L., Skelton D.A. Combined Effects of Time Spent in Physical Activity, Sedentary Behaviors and Sleep on Obesity and Cardio-Metabolic Health Markers: A Novel Compositional Data Analysis Approach. PLoS ONE. 2015;10:e0139984. doi: 10.1371/journal.pone.0139984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mekary R.A., Willett W.C., Hu F.B., Ding E.L. Isotemporal Substitution Paradigm for Physical Activity Epidemiology and Weight Change. Am. J. Epidemiol. 2009;170:519–527. doi: 10.1093/aje/kwp163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Atkin A.J., Gorely T., Clemes S.A., Yates T., Edwardson C., Brage S., Salmon J., Marshall S.J., Biddle S.J. Methods of Measurement in Epidemiology: Sedentary Behaviour. Int. J. Epidemiol. 2012;41:1460–1471. doi: 10.1093/ije/dys118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Healy G.N., Clark B.K., Winkler E.A.H., Gardiner P.A., Brown W.J., Matthews C.E. Measurement of Adults’ Sedentary Time in Population-Based Studies. Am. J. Prev. Med. 2011;41:216–227. doi: 10.1016/j.amepre.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stamatakis E., Ekelund U., Ding D., Hamer M., Bauman A.E., Lee I.-M. Is the Time Right for Quantitative Public Health Guidelines on Sitting? A Narrative Review of Sedentary Behaviour Research Paradigms and Findings. Br. J. Sports Med. 2018;53:377–382. doi: 10.1136/bjsports-2018-099131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilmot E.G., Davies M.J., Edwardson C.L., Gorely T., Khunti K., Nimmo M., Yates T., Biddle S.J. Rationale And Study Design For A Randomised Controlled Trial To Reduce Sedentary Time in Adults at Risk of Type 2 Diabetes Mellitus: Project Stand (Sedentary Time And Diabetes) BMC Public Health. 2011;11:908. doi: 10.1186/1471-2458-11-908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yates T., Davies M.J., Henson J., Troughton J., Edwardson C., Gray L.J., Khunti K. Walking Away from Type 2 Diabetes: Trial Protocol of a Cluster Randomised Controlled Trial Evaluating a Structured Education Programme in Those at High Risk of Developing Type 2 Diabetes. BMC Fam. Pract. 2012;13:46. doi: 10.1186/1471-2296-13-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yates T., Griffin S., Bodicoat D.H., Brierly G., Dallosso H., Davies M.J., Eborall H., Edwardson C., Gillett M., Gray L., et al. PRomotion of Physical Activity Through Structured Education with Differing Levels of Ongoing Support for People at High Risk of Type 2 Diabetes (PROPELS): Study Protocol for a Randomized Controlled Trial. Trials. 2015;16:289. doi: 10.1186/s13063-015-0813-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.National Institute for Health and Care Excellence Type 2 Diabetes: Prevention in People at High Risk. [(accessed on 20 January 2020.)]; Available online: https://www.nice.org.uk/guidance/ph38.
- 38.Gray L.J., Davies M.J., Hiles S., Taub N.A., Webb D.R., Srinivasan B.T., Khunti K. Detection of Impaired Glucose Regulation and/or Type 2 Diabetes Mellitus, Using Primary Care Electronic Data, in a Multiethnic UK Community Setting. Diabetologia. 2012;55:959–966. doi: 10.1007/s00125-011-2432-x. [DOI] [PubMed] [Google Scholar]
- 39.World Health Organisation . Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia: Report of a WHO/IDF Consultation. World Health Organisation; Geneva, Switzerland: 2006. [Google Scholar]
- 40.Edwardson C.L., Winkler E.A.H., Bodicoat D.H., Yates T., Davies M.J., Dunstan D.W., Healy G.N. Considerations when Using the Activpal Monitor in Field-Based Research with Adult Populations. J. Sport Health Sci. 2016 doi: 10.1016/j.jshs.2016.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Edwardson C.L., Rowlands A.V., Bunnewell S., Sanders J., Esliger D.W., Gorely T., O’Connell S., Davies M.J., Khunti K., Yates T. Accuracy of Posture Allocation Algorithms for Thigh- and Waist-Worn Accelerometers. Med. Sci. Sports Exerc. 2016;48:1085–1090. doi: 10.1249/MSS.0000000000000865. [DOI] [PubMed] [Google Scholar]
- 42.GitHub ProcessingPAL. [(accessed on 1 May 2019)]; Available online: https://github.com/UOL-COLS/ProcessingPAL.
- 43.Winkler E.A., Bodicoat D.H., Healy G.N., Bakrania K., Yates T., Owen N., Dunstan D.W., Edwardson C.L. Identifying Adults’ Valid Waking Wear Time by Automated Estimation in Activpal Data Collected with A 24 H Wear Protocol. Physiol. Meas. 2016;37:1653. doi: 10.1088/0967-3334/37/10/1653. [DOI] [PubMed] [Google Scholar]
- 44.Wijndaele K., Orrow G., Ekelund U., Sharp S.J., Brage S., Griffin S.J., Simmons R.K. Increasing Objectively Measured Sedentary Time Increases Clustered Cardiometabolic Risk: A 6 Year Analysis of the Proactive Study. Diabetologia. 2014;57:305–312. doi: 10.1007/s00125-013-3102-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Viitasalo A., Lakka T.A., Laaksonen D.E., Savonen K., Lakka H.M., Hassinen M., Komulainen P., Tompuri T., Kurl S., Laukkanen J.A., et al. Validation of Metabolic Syndrome Score by Confirmatory Factor Analysis in Children and Adults and Prediction of Cardiometabolic Outcomes in Adults. Diabetologia. 2014;57:940–949. doi: 10.1007/s00125-014-3172-5. [DOI] [PubMed] [Google Scholar]
- 46.Yates T., Edwardson C.L., Henson J., Zaccardi F., Khunti K., Davies M.J. Prospectively Reallocating Sedentary Time: Associations with Cardiometabolic Health. Med. Sci. Sports Exerc. 2020;52:844–850. doi: 10.1249/MSS.0000000000002204. [DOI] [PubMed] [Google Scholar]
- 47.Dumuid D., Maher C., Lewis L.K., Stanford T.E., Martin Fernandez J.A., Ratcliffe J., Katzmarzyk P.T., Barreira T.V., Chaput J.P., Fogelholm M., et al. Human Development Index, Children’s Health-Related Quality of Life and Movement Behaviors: A Compositional Data Analysis. Qual. Life Res. 2018;27:1473–1482. doi: 10.1007/s11136-018-1791-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Henson J., Davies M.J., Bodicoat D.H., Edwardson C.L., Gill J.M.R., Stensel D.J., Tolfrey K., Dunstan D.W., Khunti K., Yates T. Breaking Up Prolonged Sitting with Standing or Walking Attenuates the Postprandial Metabolic Response in Postmenopausal Women: A Randomized Acute Study. Diabetes Care. 2016;39:130–138. doi: 10.2337/dc15-1240. [DOI] [PubMed] [Google Scholar]
- 49.Dempsey P.C., Larsen R.N., Sethi P., Sacre J.W., Straznicky N.E., Cohen N.D., Cerin E., Lambert G.W., Owen N., Kingwell B.A., et al. Benefits for Type 2 Diabetes of Interrupting Prolonged Sitting with Brief Bouts of Light Walking or Simple Resistance Activities. Diabetes Care. 2016;39:964–972. doi: 10.2337/dc15-2336. [DOI] [PubMed] [Google Scholar]
- 50.Dunstan D.W., Kingwell B.A., Larsen R., Healy G.N., Cerin E., Hamilton M.T., Shaw J.E., Bertovic D.A., Zimmet P.Z., Salmon J., et al. Breaking Up Prolonged Sitting Reduces Postprandial Glucose and Insulin Responses. Diabetes Care. 2012;35:976–983. doi: 10.2337/dc11-1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pelclova J., Stefelova N., Dumuid D., Pedisic Z., Hron K., Gaba A., Olds T., Pechova J., Zajac-Gawlak I., Tlucakova L. Are Longitudinal Reallocations of Time Between Movement Behaviours Associated with Adiposity Among Elderly Women? A Compositional Isotemporal Substitution Analysis. Int. J. Obes. 2020;44:857–864. doi: 10.1038/s41366-019-0514-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ethical restrictions.