Abstract
A 61-year-old patient presented for syncope and a 1-week history of fever. He was diagnosed with a COVID-19 infection without pulmonary injury associated with an intermediate-risk bilateral pulmonary embolism. Computed tomographic scan and transesophageal echography were performed confirming a mobile in-transit embolus, originating from the right cavities and extending to the right ventricle through the patent foramen ovale. The patient underwent a surgical embolectomy without complications. COVID-19 was found to be the only current risk factor in our patient. This could warrant consideration of extending thromboprophylaxis indication to COVID-19 patients with certain criteria even without hospitalization indication or pulmonary injury.
Keywords: Cardiac thrombus, COVID-19, echocardiography, patent foramen ovale, pulmonary embolism
INTRODUCTION
The COVID-19 infection has spread worldwide over the last year reaching a pandemic level. It is now well recognized that it is associated with an increased risk of acute thrombotic events.[1] A higher incidence in venous thromboembolism has been reported with a hypercoagulability state highly imputed.[2] An entrapped embolus through the patent foramen ovale (PFO) is a very rare finding in common patients. We report such a case in a patient with COVID-19 infection.
CASE REPORT
A 61-year-old man with a medical history of noncomplicated spontaneous phlebitis 5 years ago presented to our hospital for syncope with transient loss of consciousness. He had no risk factor for embolism as was shown on previous thrombophilic blood tests. He benefited from a 6-month treatment with anticoagulant. He described high temperature for 1 week with fatigue with no other symptoms. He had no sign of hemodynamic compromise and his oxygen saturation was 95%. COVID-19 was suspected and the polymerase chain reaction was positive. A computed tomographic angioscan demonstrated no pulmonary infiltrate but found a bilateral pulmonary embolism with a dilated right ventricle [Figure 1a]. High-sensitive troponin-I was at 81 ng/L (normal range <34 ng/L) and B-type natriuretic peptide was in normal range (<125 pg/mL). Transthoracic echocardiography confirmed dilated right cavities with a normokinetic right ventricle and a mild pulmonary artery systolic pressure elevation (33 mmHg). It also indicated an 8 cm mobile in-transit blood clot in the right cavities suspected to be entrapped in the PFO. A synchronized cardiac scan confirmed our hypotheses [Figure 2]. There was no abdominal mass otherwise and no systemic embolism was found. A transesophageal echography was performed. It showed an in-transit mobile embolus originating from the right ventricle, straddling the PFO and extending to the left ventricle [Figure 1b-d].
Figure 1.
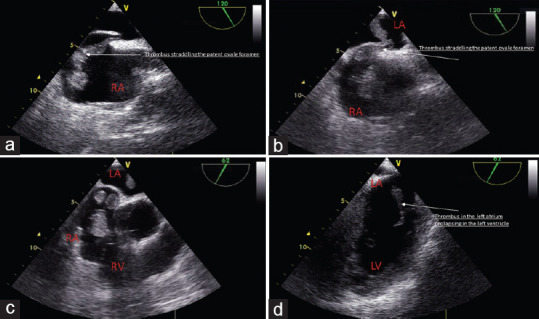
Transesophageal echography showing a thrombus (a) straddling the patent foramen ovale (b), originating from the right cavities (a-c) and extending into the left ventricle (b and d). LA: left atrium, LV: left ventricle, RA: right atrium, LV: left ventricle
Figure 2.
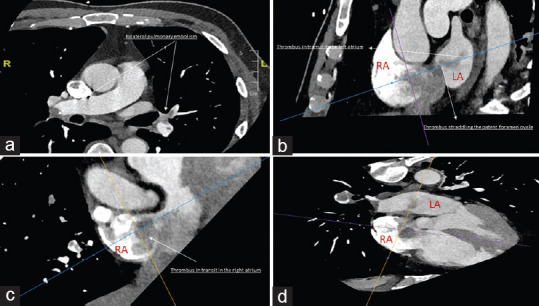
Computed tomography scan showing a bilateral pulmonary embolism (a) with a thrombus in the right cavities (b and c), entrapped in the patent foramen ovale (b) and extending to the left cavities (b and d). LA: left atrium, LV: left ventricle, RA: right atrium, LV: left ventricle
The patient was treated with unfractionated heparin. On the same day, he was urgently transferred to the operating room. A large surgical embolectomy [Figure 3] with a peripheral cardiopulmonary bypass was performed through sternotomy. His condition improved during the 1st days, and he was weaned from any mechanical support or vasopressor drug. He had no clinical sign of stroke. He benefited from a Doppler ultrasonography of the lower extremities on an outpatient basis 2 months later finding no signs of thrombus.
Figure 3.
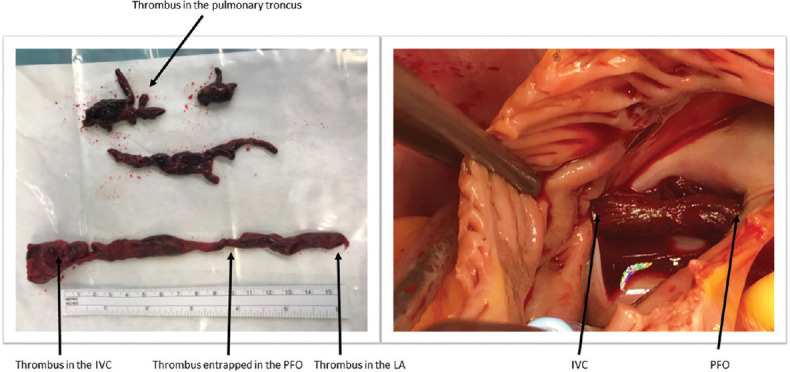
(Left) Images of the thrombus. (Right) Surgical view of the embolus. IVC: Inferior vena cava, LA: right atrium, PFO: Patent foramen ovale
DISCUSSION
A thrombus straddling the PFO is a very rare finding in common patients and is usually associated with a hypercoagulability state such as patients with thrombophilia or cancer.
Lessons from COVID-19–related literature suggest this infection to trigger a pro-inflammatory and thrombotic state, especially in case of severe pulmonary COVID-19 infection.[3] The reasons behind this thrombophilic state remain unclear. Endotheliitis has been evoked with the infection causing an accumulation of inflammatory cells in endothelial cells as a direct consequence of viral involvement.[4] In some other papers, cytokine-mediated microvascular damage or reactive thrombocytosis was proposed.[5] Recent recommendations suggest that all hospitalized COVID-19 patients should receive at least thromboprophylaxis with a prophylactic dose of low-molecular weight heparin.[6,7]
We report a very rare case of an embolus entrapped in the PFO originating from the right ventricle and extending to the left ventricle in a patient with COVID-19 infection and without the pulmonary infiltrate findings. Despite not finding COVID-19 infection features on the pulmonary scan, the patient still developed severe embolism throughout the cardiac cavities with a bilateral pulmonary embolism. This may highlight the importance of extending the indications of prophylaxis to patients with COVID-19 infection even without the need for hospitalization based on selected criteria (age, phlebitis history, other risk factors for thrombosis).[8] A close monitoring by a physician may also be recommended.
CONCLUSION
COVID-19 infection may trigger a thrombophilic state with severe embolic features and extremely rare presentations, independently of pulmonary injury presence warranting new management strategies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Wichmann D, Sperhake JP, Lütgehetmann M, Steurer S, Edler C, Heinemann A, et al. Autopsy findings and venous thromboembolism in patients with COVID-19: A prospective cohort study. Ann Intern Med. 2020;173:268–77. doi: 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klok FA, Kruip MJ, van der Meer NJ, Arbous MS, Gommers DA, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–7. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Danzi GB, Loffi M, Galeazzi G, Gherbesi E. Acute pulmonary embolism and COVID-19 pneumonia: A random association? Eur Heart J. 2020;41:1858. doi: 10.1093/eurheartj/ehaa254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19 Lancet. 2020;395:1417–8. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mei H, Hu Y. Characteristics, causes, diagnosis and treatment of coagulation dysfunction in patients with COVID-19. Zhonghua Xue Ye Xue Za Zhi. 2020;41:185–91. doi: 10.3760/cma.j.issn.0253-2727.2020.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kollias A, Kyriakoulis KG, Dimakakos E, Poulakou G, Stergiou GS, Syrigos K. Thromboembolic risk and anticoagulant therapy in COVID-19 patients: Emerging evidence and call for action. Br J Haematol. 2020;189:846–7. doi: 10.1111/bjh.16727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb J Thromb Haemost. 2020;18:1023–6. doi: 10.1111/jth.14810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marietta M, Ageno W, Artoni A, de Candia E, Gresele P, Marchetti M, et al. COVID-19 and haemostasis: A position paper from Italian society on thrombosis and haemostasis (SISET) Blood Transfus. 2020;18:167–9. doi: 10.2450/2020.0083-20. [DOI] [PMC free article] [PubMed] [Google Scholar]


