Abstract
Purpose:
Quantification of knee motion is essential for assessment of pathologic joint function, such as tracking osteoarthritis progression and evaluating outcomes after conservative or surgical treatment, including total knee arthroplasty. Our purpose was to establish a useful baseline for the kinematic envelope of knee motion in healthy older adults performing movements of daily living.
Methods:
A high-speed stereo radiography system was used to measure the three-dimensional tibiofemoral kinematics of eight healthy people over 55 yr of age (4 women/4 men; age, 61.7 ± 5.4 yr; body mass, 74.6 ± 7.7 kg; body mass index, 26.7 ± 4.4 kg·m−2; height, 168.2 ± 13.7 cm) during seated knee extension, level walking, pivoting, and step descent.
Results:
Internal–external and varus–valgus rotation and anterior–posterior range of motion through stance in normal walking averaged 3.6° ± 1.1°, 2.3° ± 0.6°, and 3.4 ± 1.57 mm, respectively. Average range of motion across subjects was greater during the step-down in both internal–external rotation (average, 6.5° ± 3.1°) and anterior–posterior translation (average, 4.5 ± 1.1). Average internal–external range of motion increased to 13.5° ± 3.6° during pivoting. Range of motion of the knee in varus–valgus rotation was nearly the same for each subject across activities, rarely exceeding 6°.
Conclusions:
Pivoting and step descending during walking had greater internal–external rotation and anterior–posterior translation than normal gait. Internal–external rotation and anterior–posterior translation were shown to have greater activity dependence, whereas varus–valgus rotation was consistent across activities. These results were similar to prior measurements in younger cohorts, though a trend toward reduced range of motion in the older adults was observed.
Keywords: TIBIOFEMORAL, OSTEOARTHRITIS, FLUOROSCOPY, ARTHROPLASTY
The way that we ambulate changes as we age (6,10,37). We tend to slow our pace and use shorter strides while walking when we are older compared with when we were younger (36). In part, this may be due to the adoption of movement strategies to increase stability and prevent falls (20). Some have suggested that these changes in ambulatory mechanics are also protective of the knee (35). Changes in movement strategies are further revealed by higher-demand tasks of ambulation such as pivoting and changing direction (6,11), and during descending a step (30,38). While these studies and others have noted that aging has a significant impact on knee kinematics and demand measured using marker-based motion capture (37), no studies have examined the small relative translations and rotations between the femur and tibia in older adults with no history of knee pathology or shown whether these motions change with age. Thus, it is unclear whether the changes in general lower extremity ambulatory kinematics measured in older adults result in changes in the 6 degree of freedom (DOF) kinematics at the knee.
Although acute knee injury is more likely to occur while we are young (13), degenerative changes in the joint occur much more frequently in older adults. In their review, Litwic et al. (28) reported studies showing severe radiographic changes in only 1% of people age 25 to 34 yr, while incidence in those 75 yr and older was 50%. People with osteoarthritis (OA) in the knee and lower-extremity joints frequently alter their gait and movement kinematics in an attempt to alleviate symptoms of the disease (39). The prevalence of OA and knee pain in older adults is reflected in the high rate of total knee arthroplasty (TKA) surgery (24). Total knee arthroplasty successfully relieves pain and improves function (1,40), however, many patients continue to demonstrate functional limitations after TKA surgery during daily tasks such as walking, and higher-demand tasks such as turning and stair descent (8,22,43). Partly due to these challenges, there have been numerous assessments of 6 DOF TKA kinematics in older adults (5,29,32), and notable analyses of knee kinematics in patients with OA (9,15,25), that have shown differences between patients with OA and TKA and normal knee kinematics in younger subjects. However, there exists no data for comparing OA or TKA kinematics to a population of asymptomatic healthy older adults. Documenting normal changes in knee kinematics with age is necessary for understanding the changes in knee kinematics that occur with OA and TKA.
Measuring in vivo dynamic knee kinematics in 6 DOF with accuracy and precision sufficient to detect small changes in position and orientation is technically challenging and requires advanced radiographic imaging techniques, such as dynamic radiography and fluoroscopy. Errors due to soft tissue artifact largely preclude accurate measurement of varus–valgus (VV), anterior–posterior (AP), superior-inferior (SI), and medial–lateral (ML) tibiofemoral translations (41) using conventional marker-based video motion capture. During normal gait in young adults, the full range of motion (ROM) of the three tibiofemoral translations rarely exceeds 10 mm, while the ROM of VV is generally less than 10° (23,26,34). Acquiring x-ray images with a single fluoroscopy system can capture knee position for motions parallel to the imaging plane (2,21,44); however, image acquisition with two radiographic views (stereo radiography) provides more accurate three-dimensional quantification of knee kinematics in all six DOF (19,26,31,34). This technique has been used to evaluate normal knee kinematics during varied dynamic activities such as normal gait (23,26), landing (33,42), and step-up (27).
Our purpose was to establish a useful baseline for the envelope of knee motion in healthy older adults performing higher-demand movements of daily living. To our knowledge, no other study has assessed normal knee function for a cohort of healthy older subjects similar in age to individuals that are likely candidates for TKA. Additionally, no other study has investigated normal knee kinematics for older people during activities that patients with TKA often report to be troublesome, namely, descending a step and executing a turn during walking. We hypothesized that higher-demand activities would cause greater internal–external (IE) rotation and AP translation than normal gait. We also hypothesized that the amount of motion in DOF that are primarily constrained by soft tissue (IE rotation and AP translation) would be more activity dependent compared with DOF partially constrained by articular geometry (VV rotation, ML and SI translations).
MATERIALS ND METHODS
The in vivo three-dimensional knee kinematics of eight healthy subjects (4 women/4 men; age, 61.7 ± 5.4 yr; body mass, 74.6 ± 7.7 kg; body mass index, 26.7 ± 4.4 kg·m−2; height, 168.2 ± 13.7 cm) were measured using high-speed stereo radiography (HSSR). This study was approved by the University of Denver Institutional Review Board, and all participants provided informed consent. Subjects had no history of injuries or surgeries to the lower limbs. Each subject completed four tasks: 1) unloaded knee extension in which the individuals were seated and slowly extended their knee from high flexion to full extension (seated knee extension); 2) walking at a self-selected pace over approximately 9 m (gait); 3) step down from a 7-inch platform (step down); and 4) turning, consisting of a 90° direction change with the planted foot of the imaged knee (pivot) (Fig. 1).
FIGURE 1—
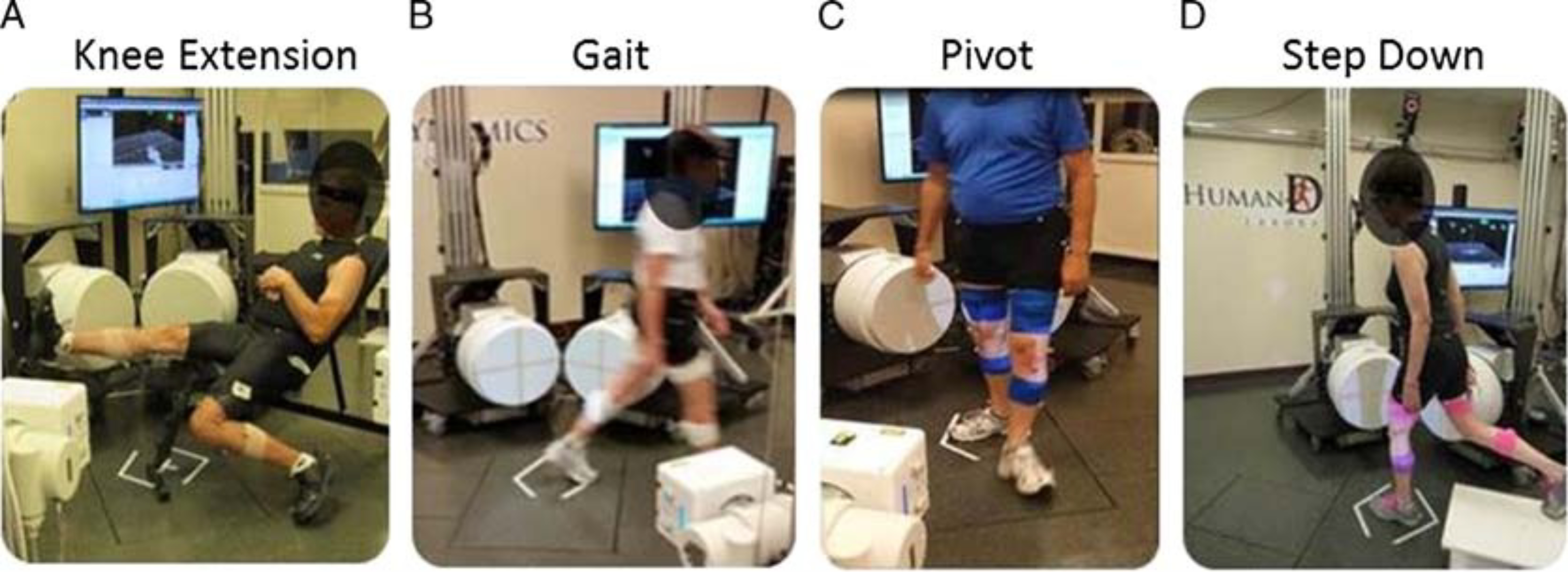
Subjects performing knee extension (A), normal gait (B), gait with a pivot turn (C), and a step down (D).
Knee kinematics were measured using HSSR. The HSSR system is composed of two matching custom radiography systems with 40 cm (16 inches) diameter image intensifiers integrated with high-speed, high-definition (1080 × 1080) digital cameras (17). The HSSR system produces an x-ray pulse only during the brief moment an image is obtained by the camera (“pulsed radiography”). In this way, unnecessary radiation exposure to the subject was minimized (17). Frame rate refers to the actual number of images obtained by HSSR per second. We chose to capture all activities at 100 frames per second except for unloaded knee extension (50 frames per second) based on the frequency content of the motion being recorded. All measurements were obtained with pulsed radiography (pulse width 750 μs, 60 kV, and 63 mA). Image distortion introduced by the image intensifiers was removed by imaging a radio opaque mesh of known dimension, and then forming a transformation to correct distortion from subsequent images of the subjects (XROMM Undistorter, Brown University, RI). The capture volume was calibrated from imaging a custom-calibration cube enclosing 52 steel beads of precisely known position and size (17). The relative bead positions from each two-dimensional image were digitized using a custom-calibration tool (XROMM Calibration Tool, Brown University, RI) and the relative position and orientation of each radiography system determined using a direct linear transformation algorithm (4). In a prior assessment, the mean absolute error of the HSSR system for tracking the bones of the knee was found to be 0.2 ± 0.1 mm in translation and 0.4° ± 0.3° in rotation (17).
After the laboratory data collection, a static bone computed topography (CT) with slice thickness of 1.0 mm was obtained of each subject’s knee. Three-dimensional models of the distal femur and proximal tibia bones were reconstructed from the CT data using ScanIP (Simpleware Inc.). Bone tracking was performed using Autoscoper (Brown University, www.xromm.org (4)), which optimized the positions of the three-dimensional bone models to the two-dimensional stereo radiography images to quantify pose (translation and rotation, Fig. 2).
FIGURE 2—
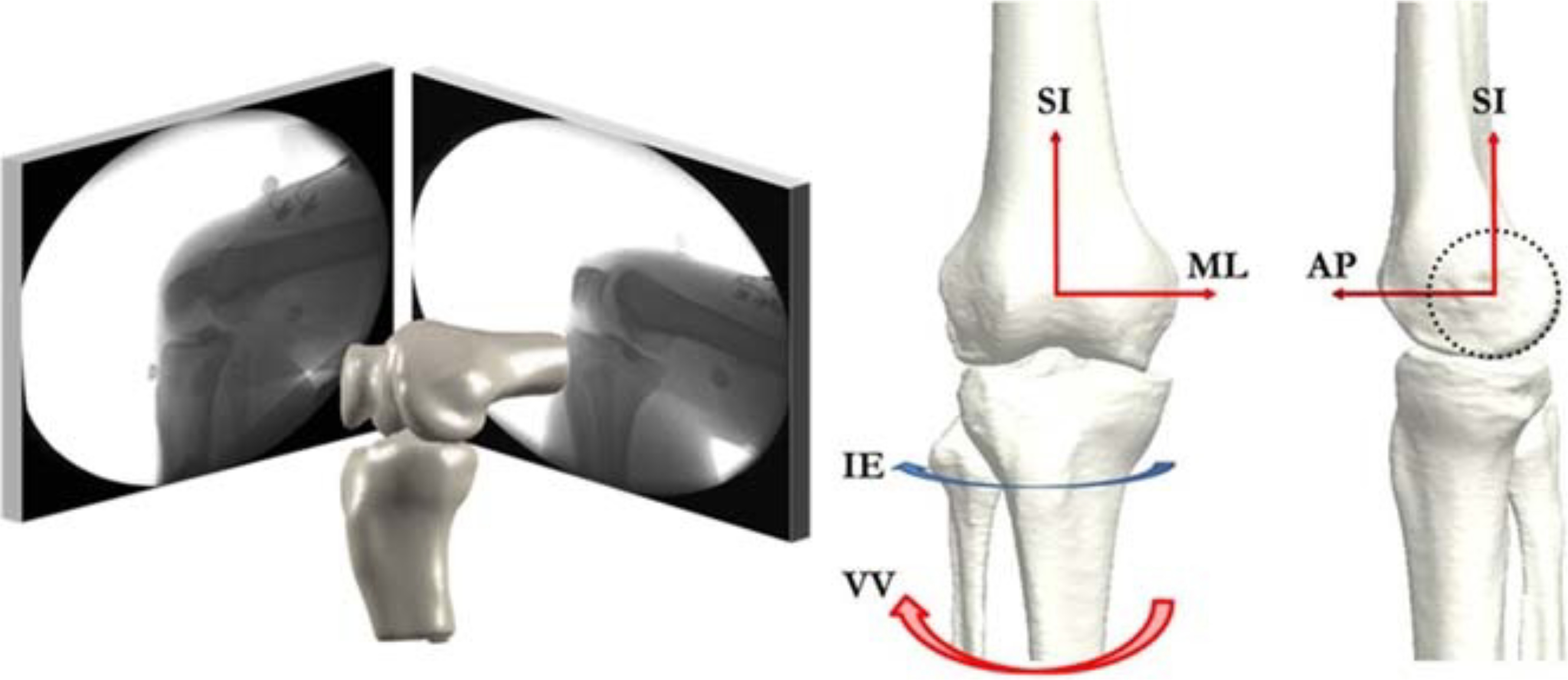
The kinematic pose of the tibia relative to the femur was found through alignment of the projected contours of the reconstructed femur and tibia/fibula bone geometries to the stereo images (left). Coordinate axis show in the reference position of the femur and tibia: superior (+)–inferior (SI), valgus (+)–varus (VV), external (+)–internal (IE), anterior (+)–posterior (AP), medial–lateral (ML) (right).
With the knee in full extension as recorded during the seated knee extension, the origin of the femoral coordinate system for each subject was defined by fitting a cylinder to the medial and lateral posterior condyles, with the center placed at the trochlea (Fig. 2) (16). The ML axis was defined as the line through the long axis of the cylinder, whereas the SI axis was aligned to the posterior aspect of the femur. The AP axis was defined as the cross product of the ML and SI axes. The coordinate system of the tibia was assigned coincident with the femoral coordinate system at full extension (42). Kinematics of the tibia relative to femur were calculated using methods described by Grood and Suntay (14). Kinematics were filtered using a fourth-order low-pass Butterworth filter with a cutoff frequency of 2 Hz for the knee extension, and 8 Hz for all other activities.
Comparisons of the average, SD, and total ROM within each task of IE and VV rotation, and AP translation were made across subjects and activities. Range of motion was calculated as the difference between the maximum and the minimum for each DOF. Paired Student t tests (P < 0.05) and one-way ANOVA (P < 0.05) were used to compare ROM across activities for all subjects.
RESULTS
The subjects exhibited similar knee kinematics relative to each other during unweighted seated knee extension (Fig. 3). At the beginning of the activity with the knee fully flexed, the tibia was internally rotated in all subjects (average, −17.8° ± 5.5° at 100° flexion). As the knee extended, tibia internal rotation decreased until reaching a minimum at full extension. All subjects remained in tibial varus throughout the seated knee extension, with the notable exception of subject 6 who remained valgus (Fig. 3). Tibial location was most anterior at full flexion (average, 5.2 ± 4.3 mm at 100° flexion) and steadily decreased as the knee was extended (average, 0.1 ± 0.4 mm at 0° flexion, Fig. 3).
FIGURE 3—
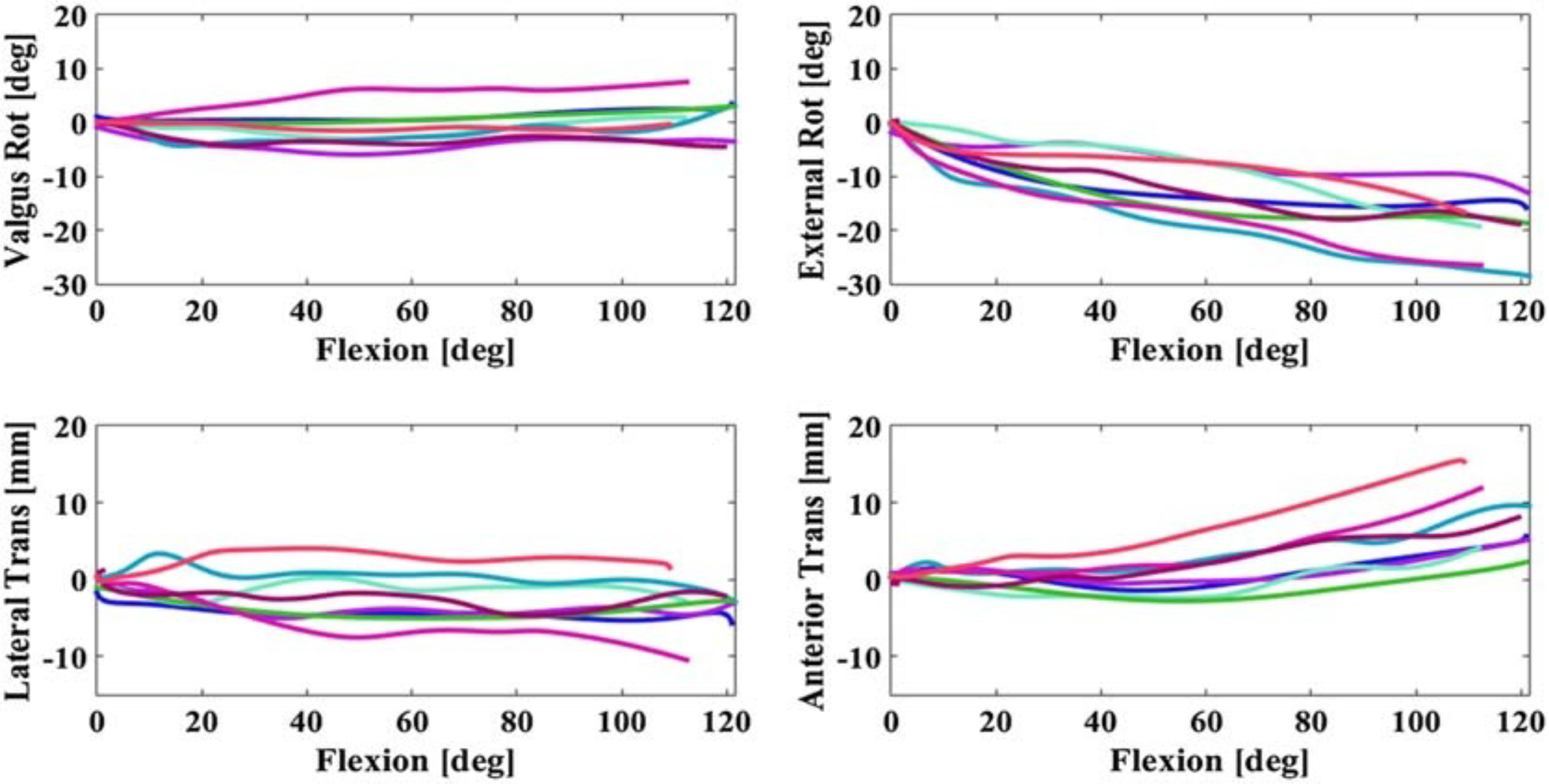
Tibiofemoral kinematics from the seated knee extension showing VV rotation, IE rotation, ML, and AP translation for all eight subjects.
During normal gait, most subjects walked with internal rotation of the tibia (average, −3.6° ± 3.3° from opposite toe off (OTO) to toe off (TO), Fig. 4). Similarly, most subjects (n = 6) walked with a consistent varus angle of the tibia (maximum, −6.0° in subject 2), whereas two subjects demonstrated a valgus angle (maximum, 4.0° in subject 6, Fig. 4). In general, the tibia was located anterior to the femur in early stance (average, 1.3 ± 2.4 mm at OTO) and moved posterior toward TO (average, −0.6 ± 1.48 mm at TO) (Figs. 4 and 5). However, the AP location of the tibia was inconsistent between subjects, with roughly equal numbers posterior and anterior during the stance phase of gait (Fig. 4).
FIGURE 4—
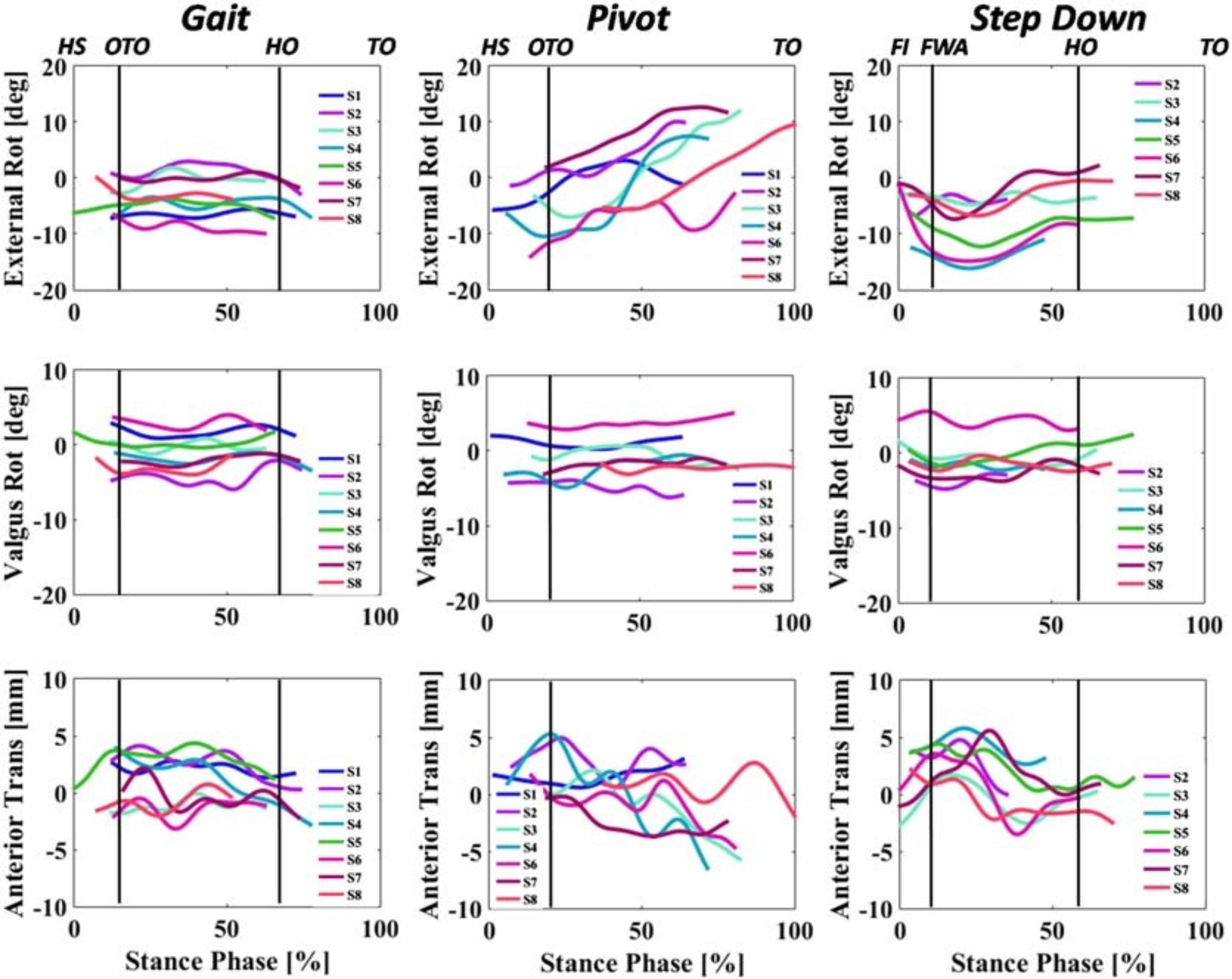
Walking, pivot, and step-down trials showing IE and VV rotation and AP translation. Seven subjects are shown for pivoting and step down because one subject did not complete these trials. In all trials 0% represents heel strike (HS) and 100% represents TO. Average foot-flat (OTO) occurred at 19% and HO at 69% in walking. OTO occurred at 20% of the stance phase during pivot, and FWA was between 7% and 14% for all subjects in step down. FWA, full-weight acceptance.
FIGURE 5—
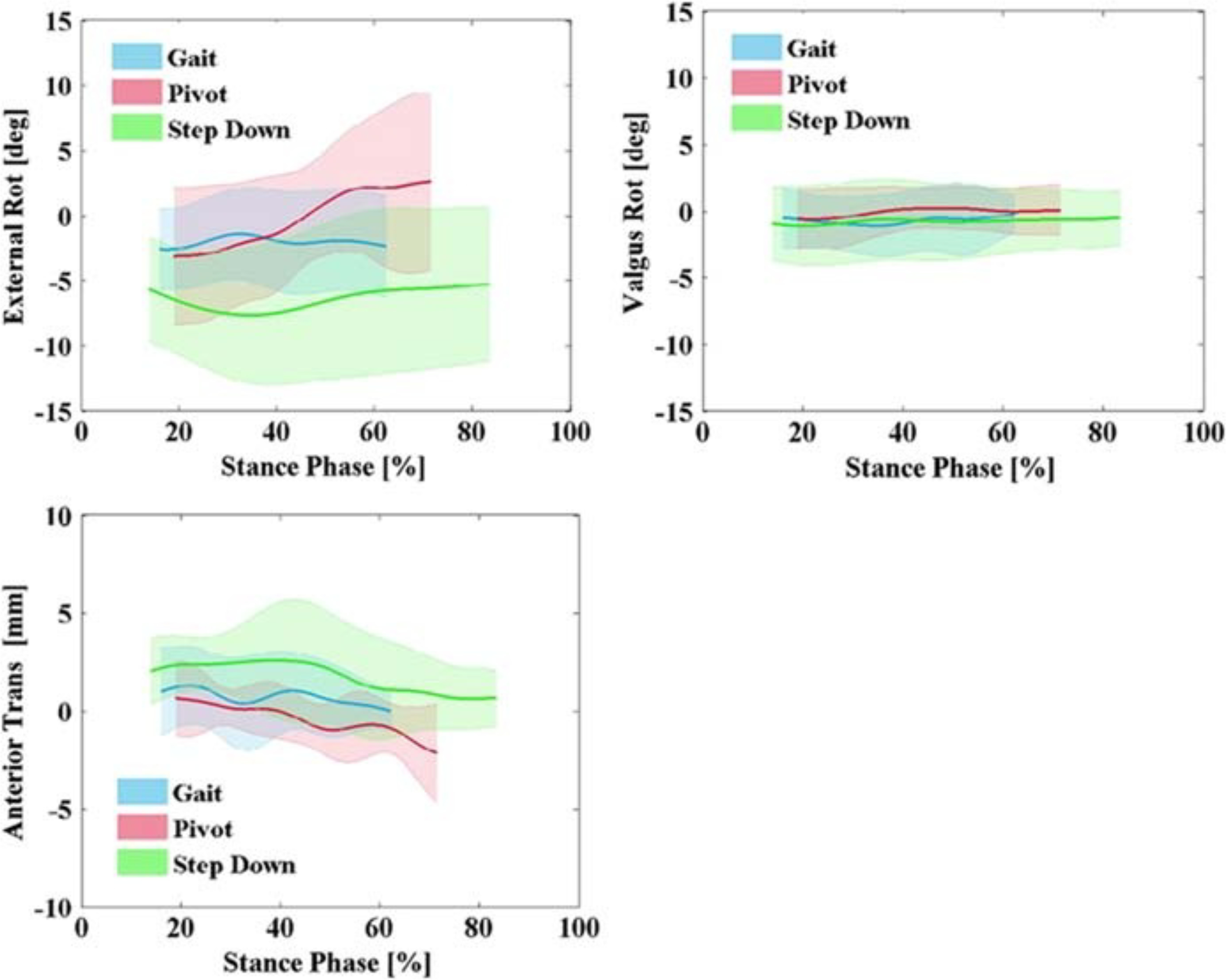
Average and SD for IE rotation, VV rotation, and AP translation for all eight subjects comparing normal gait with pivoting and step descent.
All subjects began the pivot trial in tibial internal rotation (average, at OTO −4.9° ± 5.3°) and completed the turn with greater external rotation (average, at TO 6.6° ± 5.6°) (Figs. 4 and 5). The amount of VV of the subjects was similar to that during seated knee extension and normal gait (Fig. 4). The tibia was posterior to the femur through stance compared with normal gait (Fig. 5).
During the step down, subjects were predominately internally rotated similar to normal gait (Fig. 4). Internal–external at full-weight acceptance was −7.8° ± 4.5° on average. As recorded in the previous activities, all subjects maintained varus except subjects 1 and 6 who were valgus (Fig. 4). Anterior location of the tibia relative to the femur was greater than that during normal gait (e.g., 1.3 mm greater at OTO) and pivot (Fig. 5).
Variability across subjects was largest in IE during the pivot and step-down activities (Fig. 5). Average SD was 4.9° and 4.4° for pivot and step down, whereas SD for normal gait averaged 3.3°. Varus–valgus rotation and variability was similar across all activities, with average SD of 2.6°, 2.5°, and 2.2° for pivoting, step down, and normal gait, respectively. A large portion of the variability was contributed by subject 6—average SD for VV across activities dropped to 1.9°, 1.3°, and 1.6° for pivot, step down, and normal gait, respectively, with subject 6 excluded. Anterior–posterior motion during gait (average, 0.3 mm) was similar to pivot (average, 0.2 mm), whereas the step down elicited greater anterior position of the tibia relative to the femur (average, 1.8 mm, Fig. 5) and similar variability (average, SD 1.7 mm compared with 1.6 and 1.8 mm for gait and pivoting, respectively).
In all subjects, IE, VV, and AP ROM through the stance phase of normal gait were low, averaging 3.6° ± 1.1°, 2.3° ± 0.6°, and 3.4 ± 1.6 mm, respectively (Fig. 6). In particular, the ROM of the knee in VV was nearly the same for each subject across all activities, rarely exceeding 6°. There was no statistical difference in VV rotation as indicated by one-way ANOVA across activities (F(3,20) = 0.43, P = 0.74). (A value of P greater than 0.05 indicates that VV rotation was independent of the subject and type of activity.) However, total IE and AP ROM were more activity and subject dependent as indicated by one-way ANOVA statistical differences across activities (F(3,20) = 9.7, P = 0.0004 and F(3,20) = 6.8, P = 0.002, respectively). During the higher-demand pivot and step-down activities IE and AP ROM were greater than normal gait (Fig. 6). In particular, IE ROM was significantly greater during the pivot than in normal gait (Student t test, P = 0.0005). Although average AP ROM during the pivot was greater than normal gait, the difference was not significant (P = 0.07). Similarly, average ROM across subjects was greater than normal gait during the step down in both IE rotation (average, 6.5° ± 3.1° vs 3.6° ± 1.1°) and AP translation (average, 4.5 ± 1.1 mm vs 3.4 ± 1.57 mm), but was not significant (P = 0.13 and P = 0.14, respectively). IE and AP ROM for the seated knee extension was significantly higher than normal gait (P = 0.009 and P = 0.016, respectively).
FIGURE 6—
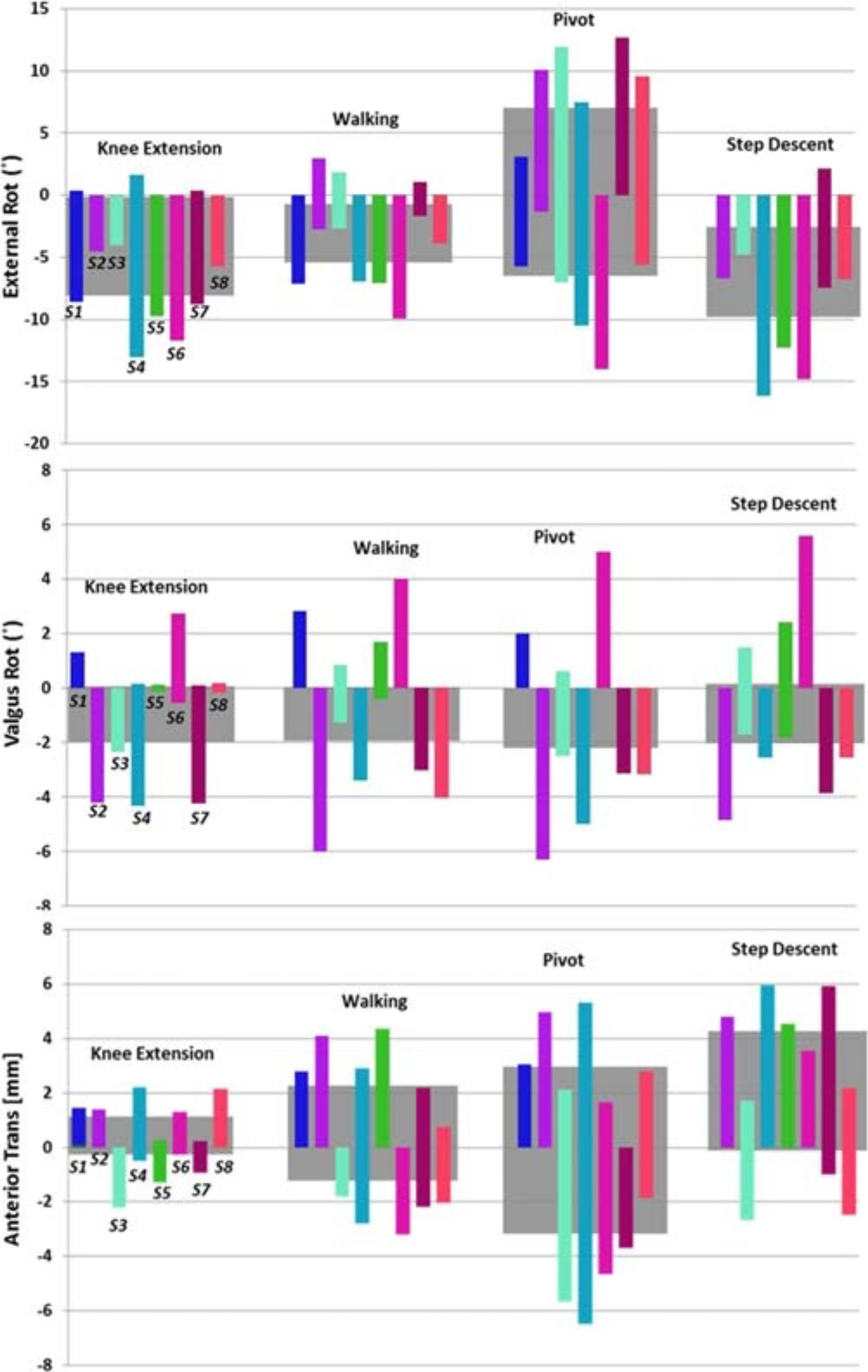
Range of motion for all activities and subjects, IE (top), VV (middle), AP (bottom); the gray shaded areas represent the average ROM of all the subjects for each activity.
DISCUSSION
An HSSR system was used to investigate the kinematics of eight healthy knees in people over 55 yr of age during seated knee extension, normal gait, pivot and step descending to establish a useful baseline for the envelope of knee motion. Step down and pivot produced greater ROM of the knee in IE and AP relative to normal gait, whereas VV remained consistent throughout all activities regardless of demand. The functional ROM of the healthy knee in older adults was similar to previous measurements reported in younger adults and provides a useful baseline kinematic envelope to quantify the impact of pathology and treatment.
Our results for people 55 yr and older were similar to measurements previously reported in younger adults. Although there are currently no studies to compare results during pivot, previous studies have examined seated knee extension, gait, and step down in younger cohorts (21,23,34). The average IE-rotation ROM of our subjects was found to be 20.3° ± 5.3° during seated knee extension, which was slightly higher than healthy knees for subjects recorded by Myers et al. (34), using similar technology with similar accuracy to the HSSR (16.1° ± 6.8°; average, age 30 yr). Likewise, the average AP-translation ROM for the older adults was higher for seated knee extension (9.11 ± 3.8 mm) in comparison to the results reported in Myers et al. (3.3 ± 1.8 mm). These differences might be explained by the greater knee extension ROM in the current study (~110°) as opposed to approximately 85° in Myers et al. (34). The AP-translation ROM for gait was similar between the two studies (3.4 ± 1.6 mm vs 3.9 ± 2.6 mm), possibly reflecting similar knee flexion ROM during walking. Consistent with these results, Kozanek et al. (23) recorded average ROM for AP translation to be approximately 5 mm with dual-plane fluoroscopy of eight healthy individuals between 32 and 49 yr of age during treadmill gait. In addition, the average IE rotation ROM for normal gait in older adults was 3.6° ± 1.1°, which was similar to that reported by Myers et al. (4.2° ± 4.0°) and Komistek et al. (21) (average, 4.4°, ranging from −1.8 to −7.0, subjects age 29 to 44 yr). The average value of IE rotation from OTO to heel off (HO), 3.4° ± 3.3°, was within the range reported by Kozanek et al. (23) (1.6° at heel strike to −7.4° at HO). Results reported by others for VV rotation in seated knee extension (34), gait (23,34), and step down (21) were similar to our results. Taken together, these results suggest that our older group of subjects had very similar patterns of tibiofemoral kinematics to younger cohorts, but with a trend toward reduced active ROM during weight bearing.
The results support our hypotheses that tibiofemoral IE rotation and AP translation depend on the activity being performed more than VV rotation. Average ROM in VV rotation was approximately 3.0° for all three gait activities and the seated knee extension, and there was no statistical difference across activities (F(3,20) = 0.43, P = 0.74). All of our subjects were asymptomatic, had no observable varus thrust during gait, and no measurable limb malalignment on frontal plane long-standing x-ray. Whether our results would remain consistent for pain-free individuals with measurable malalignment or observable varus thrust during gait requires further study. Nevertheless, most subjects maintained a consistent VV pose throughout each activity. For example, subject 6 was in valgus in all activities, whereas subject 2 was in varus (Figs. 3 and 4). Small VV rotations result primarily from the constraint of articular geometry, specifically, asymmetric femoral condylar geometry moving on curved, and asymmetric, tibial articular surfaces (18). Conversely, the ROM of IE rotation and AP translation were different among the activities. For example, the IE-rotation ROM of subject 3 increased from 5.1° for normal gait to 19.0° for the pivot trial (Fig. 6). Likewise for subject 8, AP-translation ROM increased from 1.0 mm during the seated knee extension, to 4.3 mm during normal gait and 7.0 mm during the step down (Fig. 6). IE rotations and AP translations showed greater variation because these degrees of freedom are primarily constrained by soft tissue and correspond to the passive laxity envelope of the joint and muscle forces.
The pivot and step down produced higher demands on the knee than normal gait as characterized by the translational and rotational ROM (34). Across activities, pivot had the greatest IE ROM and variation (13.4° ± 3.6°), closely followed by the step down (6.5° ± 3.2°). The AP location of the tibia had an average ROM of approximately 5.0 mm for the higher-demand activities of pivoting and step descending and 3.4 mm for normal gait. These results agree qualitatively with previous findings showing a progression of demand increasing from seated knee extension to normal gait (34). A progressive increase in demand supports the results of Gaffney et al. (12), which suggest higher joint moment and muscle forces for pivot and step down relative to normal gait.
The knee kinematics of older adults was similar to those reported for subjects after TKA and measured with fluoroscopy (3). When comparisons are made over similar portions of the gait cycle our results for the IE rotation was 3.6° ± 3.3°, whereas for subjects with TKA, the corresponding values were for the IE rotation range between 4° and 7° among different implant groups (3). However, our cohort of older adults demonstrated the common rapid change in IE rotation in the healthy knee from 0° to 20° (i.e., the “screw-home mechanism”) that was found to be absent in previous studies of IE rotation in the knee with medial OA (15) and in patients with TKA (7,45).
A limitation of this study is that the results stemmed from measurement of one trial for each activity and subject. Repeated measurements may have enhanced the results by enabling assessment of intrasubject variability, however this was deemed unjustifiable for the additional x-ray exposure. In addition, the number of subjects might be considered relatively small. However, distinct differences in ROM were found between activities across all subjects, which are similar to the findings of Kozanek et al. and Torry et al. (23,42) who used similar numbers of subjects.
In summary, this study investigated 6 DOF healthy knee kinematics during four activities for a cohort similar in age to most TKA recipients. The higher-demand tasks of pivoting and step descending, as well as a baseline seated knee extension, had greater IE rotation and AP translation than normal gait. Furthermore, IE rotation and AP translation were shown to have greater activity dependence, whereas VV rotation was consistent across activities. These results were similar to prior measurements in younger cohorts, though there was a trend toward reduced ROM in the older adults.
Acknowledgments
Supported by a National Science Foundation Major Research Instrumentation award (12–29148) and by the NIH National Institute of Biomedical Imaging and Bioengineering grant R01EB015497. The results of the present study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. The results of the present study do not constitute endorsement by ACSM.
REFERENCES
- 1.Aglietti P, Buzzi R, De Felice R, Giron F. The Insall–Burstein total knee replacement in osteoarthritis: a 10-year minimum follow-up. J Arthroplasty. 1999;14(5):560–5. [DOI] [PubMed] [Google Scholar]
- 2.Banks SA, Hodge WA. Accurate measurement of three-dimensional knee replacement kinematics using single-plane fluoroscopy. IEEE Trans Biomed Eng. 1996;43(6):638–49. [DOI] [PubMed] [Google Scholar]
- 3.Banks SA, Hodge WA. 2003 Hap Paul Award Paper of the International Society for Technology in Arthroplasty. Design and activity dependence of kinematics in fixed and mobile-bearing knee arthroplasties. J Arthroplasty. 2004;19(7):809–16. [DOI] [PubMed] [Google Scholar]
- 4.Brainerd EL, Baier DB, Gatesy SM, et al. X-ray reconstruction of moving morphology (XROMM): precision, accuracy and applications in comparative biomechanics research. J Exp Zool A Ecol Genet Physiol. 2010;313(5):262–79. [DOI] [PubMed] [Google Scholar]
- 5.Catani F, Ensini A, Belvedere C, et al. In vivo kinematics and kinetics of a bi-cruciate substituting total knee arthroplasty: a combined fluoroscopic and gait analysis study. J Orthop Res. 2009;27(12):1569–75. [DOI] [PubMed] [Google Scholar]
- 6.Chen IH, Yang YR, Cheng SJ, Wang RY. Differences in kinematic and electromyographic characteristics between young and older adults during circular turning. Int J Gerontol. 2013;7(3):162–6. [Google Scholar]
- 7.Collins DJ, Khatib YH, Parker DA, Jenkin DE, Molnar RB. Tibial rotation kinematics subsequent to knee arthroplasty. J Orthop. 2015;12(1):7–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farquhar SJ, Reisman DS, Snyder-Mackler L. Persistence of altered movement patterns during a sit-to-stand task 1 year following unilateral total knee arthroplasty. Phys Ther. 2008;88(5):567–79. [DOI] [PubMed] [Google Scholar]
- 9.Fiacchi F, Zambianchi F, Digennaro V, Ricchiuto I, Mugnai R, Catani F. In vivo kinematics of medial unicompartmental osteoarthritic knees during activities of daily living. Knee. 2014;21(1 Suppl):S10–4. [DOI] [PubMed] [Google Scholar]
- 10.Fukagawa S, Leardini A, Callewaert B, et al. Age-related changes in kinematics of the knee joint during deep squat. Knee. 2012;19(3):208–12. [DOI] [PubMed] [Google Scholar]
- 11.Fuller JR, Adkin AL, Vallis LA. Strategies used by older adults to change travel direction. Gait Posture. 2007;25(3):393–400. [DOI] [PubMed] [Google Scholar]
- 12.Gaffney BM, Harris MD, Davidson BS, Stevens-Lapsley JE, Christiansen CL, Shelburne KB. Multi-joint compensatory effects of unilateral total knee arthroplasty during high-demand tasks. Ann Biomed Eng. 2016;44(8):2529–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gage BE, McIlvain NM, Collins CL, Fields SK, Comstock RD. Epidemiology of 6.6 million knee injuries presenting to United States emergency departments from 1999 through 2008. Acad Emerg Med. 2012;19(4):378–85. [DOI] [PubMed] [Google Scholar]
- 14.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105(2):136–44. [DOI] [PubMed] [Google Scholar]
- 15.Hamai S, Moro-oka TA, Miura H, et al. Knee kinematics in medial osteoarthritis during in vivo weight-bearing activities. J Orthop Res. 2009;27(12):1555–61. [DOI] [PubMed] [Google Scholar]
- 16.Hancock CW, Winston MJ, Bach JM, Davidson BS, Eckhoff DG. Cylindrical axis, not epicondyles, approximates perpendicular to knee axes. Clin Orthop Relat Res. 2013;471(7):2278–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ivester JC, Cyr AJ, Harris MD, Kulis MJ, Rullkoetter PJ, Shelburne KB. A reconfigurable high-speed stereo-radiography system for sub-millimeter measurement of in vivo joint kinematics. J Med Devices. 2015;9(4):041009. [Google Scholar]
- 18.Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Brit. 2000;82(8): 1189–95. [DOI] [PubMed] [Google Scholar]
- 19.Kim SE, Jones SC, Lewis DD, et al. In-vivo three-dimensional knee kinematics during daily activities in dogs. J Orthop Res. 2015;33(11):1603–10. [DOI] [PubMed] [Google Scholar]
- 20.Ko S, Ling SM, Winters J, Ferrucci L. Age-related mechanical work expenditure during normal walking: the Baltimore Longitudinal Study of Aging. J Biomech. 2009;42(12):1834–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Komistek RD, Dennis DA, Mahfouz M. In vivo fluoroscopic analysis of the normal human knee. Clin Orthop Relat Res. 2003;410:69–81. [DOI] [PubMed] [Google Scholar]
- 22.Konig A, Walther M, Kirschner S, Gohlke F. Balance sheets of knee and functional scores 5 years after total knee arthroplasty for osteoarthritis: a source for patient information. J Arthroplasty. 2000;15(3):289–94. [DOI] [PubMed] [Google Scholar]
- 23.Kozanek M, Hosseini A, Liu F, et al. Tibiofemoral kinematics and condylar motion during the stance phase of gait. J Biomech. 2009;42(12):1877–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–5. [DOI] [PubMed] [Google Scholar]
- 25.Li CB, Hosseini A, Tsai TY, Kwon YM, Li GA. Articular contact kinematics of the knee before and after a cruciate retaining total knee arthroplasty. J Orthop Res. 2015;33(3):349–58. [DOI] [PubMed] [Google Scholar]
- 26.Li G, Kozanek M, Hosseini A, Liu F, Van de Velde SK, Rubash HE. New fluoroscopic imaging technique for investigation of 6DOF knee kinematics during treadmill gait. J Orthop Surg Res. 2009;4:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li JS, Hosseini A, Cancre L, Ryan N, Rubash HE, Li G. Kinematic characteristics of the tibiofemoral joint during a step-up activity. Gait Posture. 2013;38(4):712–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105:185–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McClelland JA, Webster KE, Feller JA, Menz HB. Knee kinematics during walking at different speeds in people who have undergone total knee replacement. Knee. 2011;18(3):151–5. [DOI] [PubMed] [Google Scholar]
- 30.Mian OS, Narici MV, Minetti AE, Baltzopoulos V. Centre of mass motion during stair negotiation in young and older men. Gait Posture. 2007;26(3):463–9. [DOI] [PubMed] [Google Scholar]
- 31.Miranda DL, Scwarz JB, Loomis AC, Brainerd EL, Fleming BC, Crisco JJ. Static and dynamic error of a biplanar videoradiography system using marker-based and markerless tracking techniques. J Biomech Eng. 2011;133(12):121002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mizner RL, Snyder-Mackler L. Altered loading during walking and sit-to-stand is affected by quadriceps weakness after total knee arthroplasty. J Orthop Res. 2005;23(5):1083–90. [DOI] [PubMed] [Google Scholar]
- 33.Myers CA, Torry MR, Peterson DS, et al. Measurements of tibiofemoral kinematics during soft and stiff drop landings using biplane fluoroscopy. Am J Sports Med. 2011;39(8):1714–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Myers CA, Torry MR, Shelburne KB, et al. In vivo tibiofemoral kinematics during 4 functional tasks of increasing demand using biplane fluoroscopy. Am J Sports Med. 2012;40(1):170–8. [DOI] [PubMed] [Google Scholar]
- 35.Okamoto N, Breslauer L, Hedley AK, Mizuta H, Banks SA. In vivo knee kinematics in patients with bilateral total knee arthroplasty of 2 designs. J Arthroplasty. 2011;26(6):914–8. [DOI] [PubMed] [Google Scholar]
- 36.Olney SJ, Griffin MP, McBride ID. Temporal, kinematic, and kinetic variables related to gait speed in subjects with hemiplegia: a regression approach. Phys Ther. 1994;74(9):872–85. [DOI] [PubMed] [Google Scholar]
- 37.Pfeiffer JL, Zhang S, Milner CE. Knee biomechanics during popular recreational and daily activities in older men. Knee. 2014;21(3):683–7. [DOI] [PubMed] [Google Scholar]
- 38.Samuel D, Rowe P, Hood V, Nicol A. The biomechanical functional demand placed on knee and hip muscles of older adults during stair ascent and descent. Gait Posture. 2011;34(2):239–44. [DOI] [PubMed] [Google Scholar]
- 39.Schmitt D, Vap A, Queen RM. Effect of end-stage hip, knee, and ankle osteoarthritis on walking mechanics. Gait Posture. 2015;42(3):373–9. [DOI] [PubMed] [Google Scholar]
- 40.Schroder HM, Berthelsen A, Hassani G, Hansen EB, Solgaard S. Cementless porous-coated total knee arthroplasty: 10-year results in a consecutive series. J Arthroplasty. 2001;16(5):559–67. [DOI] [PubMed] [Google Scholar]
- 41.Stagni R, Fantozzi S, Cappello A, Leardini A. Quantification of soft tissue artefact in motion analysis by combining 3D fluoroscopy and stereophotogrammetry: a study on two subjects. Clin Biomech (Bristol, Avon). 2005;20(3):320–9. [DOI] [PubMed] [Google Scholar]
- 42.Torry MR, Shelburne KB, Peterson DS, et al. Knee kinematic profiles during drop landings: a biplane fluoroscopy study. Med Sci Sports Exerc. 2011;43(3):533–41. [DOI] [PubMed] [Google Scholar]
- 43.Walsh M, Woodhouse LJ, Thomas SG, Finch E. Physical impairments and functional limitations: a comparison of individuals 1 year after total knee arthroplasty with control subjects. Phys Ther. 1998;78(3):248–58. [DOI] [PubMed] [Google Scholar]
- 44.You BM, Siy P, Anderst W, Tashman S. In vivo measurement of 3-D skeletal kinematics from sequences of biplane radiographs: application to knee kinematics. IEEE Trans Med Imaging. 2001;20(6):514–25. [DOI] [PubMed] [Google Scholar]
- 45.Yue B, Varadarajan KM, Moynihan AL, Liu F, Rubash HE, Li G. Kinematics of medial osteoarthritic knees before and after posterior cruciate ligament retaining total knee arthroplasty. J Orthop Res. 2011;29(1):40–6. [DOI] [PubMed] [Google Scholar]


