Abstract
Background
There is strong evidence regarding the efficacy and effectiveness of the BNT162b2 vaccine in preventing symptomatic infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). There is a relative paucity of data regarding its effectiveness in the prevention of asymptomatic infection.
Methods
In this real-world observational study, we identified a subpopulation of individuals in a large health maintenance organization who were repeatedly tested for SARS-CoV-2 infection by polymerase chain reaction (PCR). We included these individuals in the study cohort and compared those who were vaccinated with BNT162b2 mRNA vaccine to unvaccinated individuals. A positive SARS-CoV-2 PCR test result was used as the outcome. The follow-up period was from January 1, 2021, until February 11, 2021.
Results
A total of 6286 individuals were included in the cohort. Seven days after the second vaccine dose, a rate of 6 positive PCR tests per 10 000 person-days was recorded, compared with a rate of 53 positive tests per 10 000 person-days for the unvaccinated group. The estimated vaccine effectiveness against infection with SARS-CoV-2 virus after 2 vaccine doses was 89% (95% CI, 82%–94%). The estimated effectiveness 2 weeks after the first vaccine dose was 61% (95% CI, 49%–71%).
Conclusions
In this study, vaccination with BNT162b2 reduced infection rates among individuals who underwent screening by frequent SARS-CoV-2 PCR testing. Using a cohort of frequently tested individuals reduced the indication bias for the PCR testing, which enabled estimation of infection rates.
Keywords: asymptomatic infection, COVID-19, observational study, SARS-CoV-2, vaccine effectiveness
The effectiveness of BNT162b2 vaccine in prevention of asymptomatic infection is unclear. Among individuals who were repeatedly tested for SARS-CoV-2 infection by PCR, we found that the estimated vaccine effectiveness against SARS-CoV-2 virus after two vaccine doses was 89%.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has afflicted more than 129 million persons worldwide and caused more than 2.8 million deaths as of the end of March 2021 [1]. The Pfizer BNT162b2 mRNA vaccine was the first to receive emergency authorization, first in the United Kingdom, then in the United States and globally at the beginning of December 2020. Since then, more than 100 million doses of this vaccine have been administered worldwide [2].
The efficacy of the BNT162b2 vaccine was demonstrated in a large phase III randomized controlled clinical trial showing 95% protection against confirmed symptomatic disease 7 days after the second dose and 52.4% before receiving the second dose [3]. Several observational real-world clinical studies later demonstrated similar vaccine effectiveness [4–6]. However, these studies lacked active laboratory surveillance among both vaccinated and unvaccinated individuals, missing diagnoses of asymptomatic cases and possibly overestimating the protection conferred by the vaccine.
The proportion of individuals with asymptomatic SARS-CoV-2 is hard to estimate and best requires prospective, regular screening of a defined population. In a systematic review that summarized 79 reports, the proportion of people who were infected with SARS-CoV-2 and remained asymptomatic throughout infection was 20% (95% CI, 17%–25%), while the proportion was 31% (95% CI, 26%–37%) in 7 studies in which active screening for SARS-CoV-2 was performed [7]. While evidence suggests that the risk for transmission of SARS-CoV-2 from asymptomatic individuals is significantly lower compared with presymptomatic or symptomatic cases [7–12], understanding vaccine effectiveness on asymptomatic infection is important for public health policy development.
Vaccine protection against asymptomatic SARS-CoV-2 has been estimated in several studies. In the Moderna mRNA vaccine clinical study, participants underwent nasopharyngeal polymerase chain reaction (PCR) testing before each dose and were shown to have a 67% decrease in asymptomatic infection following the first dose (0.1% vs 0.3%) [13]. In a large study from Israel, in which almost 600 000 vaccinated individuals were compared with a matched group of unvaccinated individuals, vaccine effectiveness was 92% at 7 days following the second vaccine dose for all documented symptomatic and asymptomatic infections [4]. In this study, the proxy for an asymptomatic infection was a positive PCR without documented symptoms; however, this methodology does not overcome bias of different test-seeking behaviors. In addition, Israeli public health policy exempts fully vaccinated individuals from undergoing PCR tests after being exposed to an individual with a confirmed SARS-CoV-2 infection or when entering the country, which may further bias the results of observational studies that use the entire population as their cohort. This may result in overestimation of vaccine effectiveness due to underdiagnosis of asymptomatic infections among vaccinated individuals. A recent study from England that followed a cohort of health care workers who underwent regular screening [14] demonstrated vaccine effectiveness of 85% 7 days after the second vaccine dose for both symptomatic and asymptomatic infections.
To further estimate vaccine protection against any SARS-CoV-2 infection, we conducted this observational study using a historical cohort of individuals repeatedly tested for SARS-CoV-2 before and after receiving the BNT162b2 vaccine.
METHODS
Setting and Data Source
The Meuhedet Health Maintenance Organization (MHMO) serves 1.2 million members in Israel. The Israeli National Health Insurance Act of 1994 requires that all citizens be registered with 1 of 4 HMOs, which in turn are obliged to insure every citizen wishing to join, irrespective of sex, age, physical condition, or any other criterion. Citizens can move freely among the HMOs, which operate in every region.
MHMO’s comprehensive database stores members’ medical data from all health care providers, including dates of vaccination with the BNT162b2 vaccine and all COVID-19 PCR test results since the beginning of the pandemic.
We identified a subpopulation of MHMO members who were repeatedly tested for SARS-CoV-2 infection using PCR tests. We used these individuals as the cohort for the study, using BNT162b2 mRNA vaccine as the exposure and a positive SARS-CoV-2 PCR test result as the outcome.
The follow-up period started on January 1, 2021, and ended on February 11, 2021 (6 weeks). Data were extracted on February 17, 2021. This study was approved by MHMO’s institutional review board (number 03-17-02-21), and investigators were exempt from requesting informed consent. One author, D.S., has a potential conflict of interest.
Study Participants
We extracted all SARS-CoV-2 PCR tests and SARS-CoV-2 serological assays for MHMO members since the beginning of the pandemic.
Inclusion Criteria
Individuals aged 16 years or older who had at least 2 PCR tests during November, at least 2 PCR tests during December, and at least 1 PCR test during January were included.
Exclusion Criteria
Individuals who tested positive by either a PCR test or a serological assay before the beginning of the follow-up period (January 1, 2021) were excluded. We also excluded individuals who tested positive by a serological assay during the follow-up period, as we could not determine their exact infection date. Thirteen individuals had a positive serological assay during the study period. One of them was vaccinated twice before the positive serology test, 2 were vaccinated once before the test, and 10 were not vaccinated. The following serological assays were used: LIAISON SARS-CoV-2 S1/S2 IgG, DiaSorin (Italy), or SARS-CoV-2 IgG II Quant, Abbott (IL, USA). Both assays identify antibodies against the spike protein and cannot distinguish prior vaccination from past infection. In general, physicians in MHMO were discouraged from ordering serology tests for vaccinated individuals.
The participants were included in the analysis until the date of their first positive SARS-CoV-2 PCR test or the last negative test within the follow-up period. The outcome was the result of this test.
For each patient, we collected BNT162b2 vaccination dates, SARS-CoV-2 PCR tests during the follow-up period, and demographic data: sex, age, and population sector by place of residence (general Jewish, Arab, or ultra-orthodox Jewish), given that in Israel different ethno-cultural groups tend to reside in different, usually clearly defined, areas.
Exposure Periods
In order to estimate vaccine effectiveness during different postvaccination periods, we calculated infection rates separately for the following:
Before the first vaccination (including vaccination day).
From 14 days after the first vaccine dose until the day of the second vaccine dose.
One to 6 days following the second vaccine dose.
Seven or more days following the second vaccine dose.
The participants were included in the analysis of the different periods according to the timing of their vaccination within the study period. The days before the first vaccine dose of an individual were added to the first period, from 14 days after the first vaccine until the second vaccine was the second period, the first 6 days following the second vaccine dose were added to the third period, and the remaining days in the cohort of this individual were added to the fourth period. An individual could contribute days to 1 or more periods.
Statistical Methods
For each period, we summarized exposure days of all individuals in each of the 4 periods, and we counted individuals with a positive PCR test as cases. We calculated infection rates per 10 000 person-days (PD) for each period and then calculated risk ratios for vaccinated individuals compared with unvaccinated. We estimated the vaccine effectiveness as 1 minus the risk ratio.
In order to overcome possible variation of infection rates across the different population sectors, we calculated infection rates separately for each sector.
The incidence infection rates in Israel increased at the beginning of the follow-up period from a moving 7-day average of 4728 new cases per day on January 1, 2021, to a peak of >8000 new cases per day from January 14 to January 20. The rate slowly subsided while remaining above 6500 new cases per day until February 7, reaching a rate of 5822 new cases per day at the end of the follow-up period on February 11, 2021 [15]. In view of this variation, we performed a sensitivity analysis and calculated the rates in 2-week-long intervals: January 1–14, January 15–28, and January 29–February 11.
We used the chi-square test to examine the association between categorical variables and analysis of variance (ANOVA) to analyze the differences among means. Analyses were conducted with IBM SPSS, version 27. Two-tailed P values are reported, and α = .05 was used for CI calculations.
RESULTS
The Participants
A total of 6286 individuals met the inclusion criteria and were eligible for the study. During the study period, 2941 of them received 2 doses of BNT162b2 vaccine, 1445 received only 1 dose, and 1900 were not vaccinated at all (Table 1). The mean age of the 2-dose vaccinated group was significantly higher than the mean age of individuals who received a single vaccine dose or none (52 ± 17 years vs 41 ± 21 years and 36 ± 19 years respectively; P < .001). A total of 1055 individuals (17%) were 65 years old or older. Significantly more PCR tests were performed from November 1, 2020, until the end of the follow-up period for the fully vaccinated group compared with individuals who were vaccinated with a single dose or none (13 tests vs 9 tests and 10 tests, respectively; P < .001). Fifty-three percent of the women (1961 of 3685) were vaccinated with 2 doses compared with 38% of the men (980 of 2601; P < .001). Vaccination rates also significantly varied between the different sectors in our cohort (P < .001).
Table 1.
Characteristics of Participants According to Their Vaccination Status at the End of Follow-up
| Unvaccinated | Vaccinated With 1 Dose | Vaccinated With 2 Doses | P Value | |
|---|---|---|---|---|
| Overall | 1900 | 1445 | 2941 | |
| Women, No. (%) | 1007 (53) | 717 (50) | 1961 (67) | <.001 |
| Mean age ± SD, y | 36 ± 19 | 41 ± 21 | 52 ± 17 | <.001 |
| Age ≥65 y, No. (%) | 165 (9) | 205 (14) | 685 (23) | <.001 |
| Sectors, No. (%) | <.001 | |||
| General Jewish | 1189 (63) | 966 (67) | 2255 (77) | |
| (n = 4410) | ||||
| Ultra-orthodox Jewish | 525 (28) | 338 (23) | 314 (11) | |
| (n = 1177) | ||||
| Arabs | 186 (10) | 141 (10) | 372 (13) | |
| (n = 699) | ||||
| Mean No. of PCR testsa ± SD | 10 ± 3.7 | 9 ± 3.1 | 13 ± 3.6 | <.001 |
Abbreviation: PCR, polymerase chain reaction.
aPerformed from November 1, 2020, to the end of the follow-up period.
Exposure Days and Outcome
There were 190 084 exposure days for the study cohort, with a mean number of exposure days (SD) for individuals of 30 (11.5). Table 2 summarizes the exposure days for each of the vaccination periods. There were 382 positive SARS-CoV-2 PCR tests in the first period (unvaccinated individuals), with a calculated rate of 53 cases per 10 000 PD. Fourteen or more days after the first vaccine dose, there were 59 cases, a rate of 21 cases per 10 000 PD (effectiveness, 61%; 95% CI, 49%–71%). During the first 6 days following the second dose, only 16 cases were recorded, a rate of 9 cases per 10 000 PD (effectiveness, 82%; 95% CI, 71%–89%). In the period that started a week after the second vaccine dose, 15 cases were recorded, with a rate of 6 cases per 10 000 PD (effectiveness, 89%; 95% CI, 82%–94%) (Table 2).
Table 2.
Incidence Infection Rates of SARS-CoV-2 and BNT162b2 Vaccine Effectiveness
| No. of Exposure Days | PCR-Positive Cases | Incidence Rate per 10 000 Person-Days | Rate Reduction Compared With Unvaccinated (95% CI), % | |
|---|---|---|---|---|
| Before the 1st vaccine (= unvaccinated) | 71 797 | 382 | 53 | NA |
| ≥14 d following the 1st dose | 28 727 | 59 | 21 | 61 (49–71) |
| 1–6 d following the 2nd dose | 16 921 | 16 | 9 | 82 (71–89) |
| ≥7 d following the 2nd dose | 26 260 | 15 | 6 | 89 (82–94) |
Abbreviations: PCR, polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Effectiveness Across Different Subpopulations and Time Periods
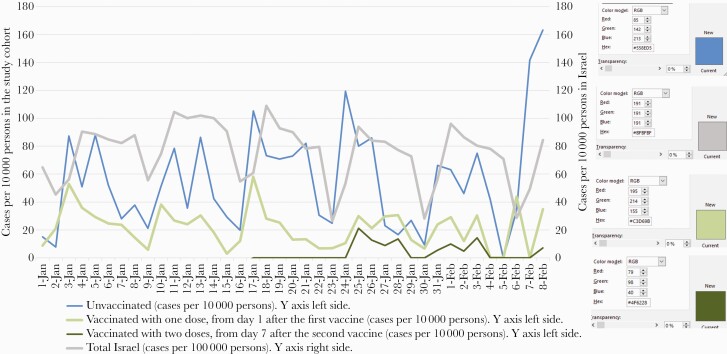
Infection rates varied significantly across the different populations. The Arab and general Jewish population had similar infection rates for the unvaccinated group (35 and 36 cases per 10 000 PD, respectively), compared with 112 cases per 10 000 PD for the unvaccinated ultra-orthodox Jewish population. Table 3 summarizes the infection rate ratios and effectiveness separately for the ultra-orthodox Jewish population and the rest of the cohort. Vaccine effectiveness 7 days after the second vaccine dose was 90% for the ultra-orthodox Jewish (95% CI, 68%–97%; n = 1177) and 86% for the rest of the cohort (95% CI, 75%–92%; n = 5109). A sensitivity analysis for 3 periods of 2 weeks was performed in order to overcome a possible bias from temporal trends. This analysis was limited due to the low number of cases and exposure days for some of the analyzed periods. However, the effectiveness trend was clear for all 3 periods. Figure 1 presents the daily incidence rates of positive PCR tests in Israel (per 100 000 people) [15, 16] and in the study cohort (per 10 000 people).
Table 3.
Incidence Infection Rates of SARS-CoV-2 and BNT162b2 Vaccine Effectiveness According to Population Sectors
| No. of Exposure Days | PCR- Positive Cases | Incidence Rate per 10 000 Person-Days | Rate Reduction Compared With Unvaccinated (95% CI), % | |
|---|---|---|---|---|
| Arabs and general Jewish population (n = 5109) | ||||
| Before the 1st vaccine (= unvaccinated) | 55 250 | 197 | 36 | NA |
| ≥14 d following the 1st dose | 25 457 | 48 | 19 | 47 (28–61) |
| 1–6 d following the 2nd dose | 15 153 | 13 | 9 | 76 (58–86) |
| ≥7 d following the 2nd dose | 23 674 | 12 | 5 | 86 (75–92) |
| Ultra-orthodox Jewish populations (n = 1177) | ||||
| Before the 1st vaccine (= unvaccinated) | 16 547 | 185 | 112 | NA |
| ≥14 d following the 1st dose | 3270 | 11 | 34 | 70 (45–84) |
| 1–6 d following the 2nd dose | 1768 | 3 | 17 | 85 (53–95) |
| ≥7 d following the 2nd dose | 2586 | 3 | 12 | 90 (68–97) |
Abbreviations: PCR, polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Figure 1.
Daily incidence rates of positive SARS-CoV-2 PCR tests in Israel compared with the study cohort groups. The last 3 days of the study period are not presented as the total amount of days at risk in the cohort was <2000 person-days. Abbreviations: PCR, polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
DISCUSSION
In a cohort of individuals who underwent frequent SARS-CoV-2 PCR testing, we found that the rate of positive SARS-CoV-2 PCR tests in the vaccinated group was reduced by 61% from 14 days after the first vaccination and by 89% from 7 days after the second vaccination. The frequent PCR testing in our cohort enabled estimation of infections, whether symptomatic or asymptomatic. The reduction ratio remained constant between the individuals in ultra-orthodox Jewish towns, which had higher incidence rates of COVID-19 infection, and the other cohort participants. The large cohort with its large age variance suggests that these results may be applicable in different population groups.
A study that assessed the effectiveness of the BNT162b2 vaccine among 600 000 individuals showed a 92% reduction in positive PCR tests [4]. Another study that monitored daily symptom reporting with immediate same-day testing allowed for prompt (<24 hours) detection and investigation of exposed or symptomatic health care workers and showed that among 4081 vaccinated health care workers in Israel, 22 (0.54%) developed COVID-19 1–10 days (median, 3.5 days) after the first vaccine dose [17]. An additional analysis estimated vaccine effectiveness at 51% for the BNT162b2 vaccine in reducing positive PCR rates 13–24 days following vaccination with the first dose [6]. These studies were limited in their ability to assess asymptomatic SARS-CoV-2 infection rates due to different test-seeking behaviors that result in different rates of PCR testing by vaccinated and unvaccinated individuals. A study of health care workers from California, half of whom had mandatory weekly PCR screening after the first and second vaccinations, showed that the absolute risk of testing positive for SARS-CoV-2 after vaccination was 1.19% among health care workers who had mandatory screening. However, among health care workers who received the second dose 2 or more weeks before, there was a positivity rate of 0.05% [18]. Another study of health care workers undergoing weekly PCR testing showed 90% effectiveness 2 weeks after the second vaccination and 80% 14 days after the first vaccination [19]. A recent study that followed health care workers who underwent routine bimonthly PCR screening demonstrated 85% effectiveness 7 days after the second vaccine dose [14]. This compares with 89% 7 days after the second vaccination and 61% after the first vaccination in our study. The temporal trend of the daily infection incidence rate of the unvaccinated group mirrors the pattern of the incidence rate of the total Israeli population (Figure 1). Fewer tests were performed during weekends, causing weekly fluctuations. The rates in the unvaccinated group in our cohort were 10 times higher compared with the total population, which suggests that the study cohort was a high-risk group. This assumption is supported by the cohort demographics: 17.7% of our cohort was from the ultra-orthodox population, who had a higher incidence of SARS-CoV-2 than the general population [15]. In addition, the frequent PCR testing in this cohort may partially explain the higher incidence rate of SARS-CoV-2 compared with the total population of Israel, as it has been shown that 20%–31% of individuals with SARS-CoV-2 infection are asymptomatic [7].
The strengths of this study include full data collection and comprehensive countrywide assessment in different population groups. The entry criteria required at least 2 PCR tests in November, 2 tests in December, and 1 in January, ensuring that the cohort was composed mainly of frequently screened individuals. The repeated testing reduces the false-negative rate of a single test, thus decreasing the likelihood of missing an asymptomatic infection. Misclassification into the vaccinated or unvaccinated group is unlikely as all interactions were recorded in our electronic medical record (EMR) at the time of vaccination regardless of the vaccination location. The EMR also ensured full data collection of PCR test results from all laboratories. The limitations of this study include the observational nature of the study design. We do not know the reason why individuals within our cohort chose to be vaccinated (or not) or why they had repeated PCR testing. From Table 1, we see significant differences between the 3 groups (unvaccinated, partially vaccinated, and fully vaccinated). The age difference between vaccinated and unvaccinated individuals resulted from the fact that the study period overlapped the beginning of the Israeli vaccination campaign, when vaccine availability was initially limited to older citizens. This table also shows that the ultra-orthodox Jewish sector was vaccinated at lower rates; however, the calculated effectiveness for this sector did not differ from the other sectors (Table 3). The number of PCR tests per individual was significantly higher for the fully vaccinated group (Table 1). Consequently, there is a lower chance of missing an infection in this group, which could cause bias, reducing the calculated effectiveness. We were unable to validate the reason for the repeated PCR testing, and it is possible that some of the tests were performed by symptomatic individuals. During the study period, PCR tests were free and widely available in Israel and did not require a physician’s referral. In the ultra-orthodox community, young adults continued to study in high schools and religious institutions during the outbreak; the repeated testing in this group could be related to outbreak investigation or symptomatic infection. Thus, the increased effectiveness of the vaccine seen in the ultra-orthodox population might be an artifact. The cohort’s limited size and short follow-up period did not allow for a multivariate analysis or estimation of vaccination effectiveness in reducing infection in different age groups. In addition, due to the high uptake of the second vaccination, we could not assess the long-term effectiveness of a single dose.
CONCLUSIONS
In this real-world setting, vaccination greatly reduced infection rates among individuals who underwent screening by frequent SARS-CoV-2 PCR testing. A prospective clinical trial needs to be undertaken in order to confirm this finding and establish long-term protection from asymptomatic infection following the first and second vaccine doses.
Acknowledgments
Author contributions. G.Z. and D.S. contributed equally to this research.
Patient consent. This database study was approved by the local ethical committee, which decided that patient consent was not required.
Availability of data. De-identified participant data and statistical analysis will be made available via the corresponding author for a year from publication.
Financial support. No funding was received for this analysis.
Potential conflicts of interest. D.S. reports receiving personal fees from Pfizer, outside the submitted work (advisory board on Trumenba) and consultation fees from GSK and Gilead. The other authors, G.Z., R.B., I.K., F.H.S., I.K., D.M., and A.D.H., declare no competing interests. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Worldometers.info. 2021. Available at: https://www.worldometers.info/coronavirus. Accessed 28 February 2021.
- 2. Our world in data. 2021. Available at: https://ourworldindata.org/covid–vaccinations. Accessed 28 February 2021.
- 3. Polack FP, Thomas SJ, Kitchin N, et al. ; C4591001 Clinical Trial Group. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N Engl J Med 2020; 383:2603–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dagan N, Barda N, Kepten E, et al. BNT162b2 mRNA COVID-19 vaccine in a nationwide mass vaccination setting. N Engl J Med 2021; 384:1412–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Amit S, Regev–Yochay G, Afek A, et al. Early rate reductions of SARS-CoV-2 infection and COVID-19 in BNT162b2 vaccine recipients. Lancet 2021; 397:875–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chodick G, Tene L, Patalon T, et al. Assessment of effectiveness of 1 dose of BNT162b2 vaccine for SARS-CoV-2 infection 13 to 24 days after immunization. JAMA Netw Open 2021; 4:e2115985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Buitrago–Garcia D, Egli–Gany D, Counotte MJ, et al. Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: a living systematic review and meta-analysis. PLoS Med 2020; 17:e1003346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang Y, He Y, Tong J, et al. Characterization of an asymptomatic cohort of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infected individuals outside of Wuhan, China. Clin Infect Dis 2020; 71:2132–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Arons MM, Hatfield KM, Reddy SC, et al. ; Public Health–Seattle and King County and CDC COVID-19 Investigation Team. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med 2020; 382:2081–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Johansson MA, Quandelacy TM, Kada S, et al. SARS-CoV-2 transmission from people without COVID-19 symptoms. JAMA Netw Open 2021; 4:e2035057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gao M, Yang L, Chen X, et al. A study on infectivity of asymptomatic SARS-CoV-2 carriers. Respir Med 2020; 169:106026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sayampanathan AA, Heng CS, Pin PH, et al. Infectivity of asymptomatic versus symptomatic COVID-19. Lancet 2021; 397:93–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. FDA Vaccines and Related Biological Products Advisory Committee. mRNA–1273 sponsor briefing document addendum. 2020. Available at: https://www.fda.gov/media/144453/download. Accessed 28 February 2021.
- 14. Hall VJ, Foulkes S, Saei A, et al. COVID-19 vaccine coverage in health–care workers in England and effectiveness of BNT162b2 mRNA vaccine against infection (SIREN): a prospective, multicentre, cohort study. Lancet 2021;397:1725–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Israeli Ministry of Health. COVID-19 dashboard. Available at: https://datadashboard.health.gov.il/COVID-19/general. Accessed 27 February 2021.
- 16. Central Bureau of Statistics, Israel. Population of Israel on the eve of 2021 [in Hebrew]. 2021. Available at: https://www.cbs.gov.il/he/mediarelease/Pages/2020/%D7%90%D7%95%D7%9B%D7%9C%D7%95%D7%A1%D7%99%D7%99%D7%AA–%D7%99%D7%A9%D7%A8%D7%90%D7%9C–%D7%91%D7%A4%D7%AA%D7%97%D7%94–%D7%A9%D7%9C–%D7%A9%D7%A0%D7%AA–2021–.aspx. Accessed 26 March 2021.
- 17. Amit S, Beni SA, Biber A, et al. Postvaccination COVID-19 among healthcare workers, Israel. Emerg Infect Dis 2021; 27:1220–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Keehner J, Horton LE, Pfeffer MA, et al. SARS-CoV-2 Infection after Vaccination in Health Care Workers in California. N Engl J Med 2021; 384:1774–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Thompson MG, Burgess JL, Naleway AL, et al. Interim estimates of vaccine effectiveness of BNT162b2 and mRNA-1273 COVID-19 vaccines in preventing SARS-CoV-2 infection among health care personnel, first responders, and other essential and frontline workers – eight U.S. locations, December 2020–March 2021. MMWR Morb Mortal Wkly Rep 2021; 70:495–500. [DOI] [PMC free article] [PubMed] [Google Scholar]