The impact of the COVID-19 pandemic on endoscopy services has been profound, triggering a strategic remodelling of service delivery and prompting recommendation of a nationwide senior led triage system in-line with BSG (British Society of Gastroenterology) and JAG (Joint Advisory Group on Gastrointestinal Endoscopy) guidance.1 The anticipated backlog of deprioritised cases during the COVID-19 pandemic represents a daunting challenge to those delivering endoscopy services, particularly given the recent evidence to suggest that for several cancers (including those of the colorectum, oesophagus and stomach), a 3-month delay to diagnosis is predicted to result in a reduction in long-term (10 years) survival of more than 10% in most age groups.1 2 The challenge is compounded further by the pandemic’s effect on training, and therefore the proportion of independent future endoscopists at time of certification of completion of training (CCT).
Impact of COVID-19 on training
COVID-19 has negatively impacted on conventional endoscopy training. Several strategies to address the challenges faced by trainees in the COVID-19 era have been proposed.3 The use of online resources and expert-delivered video endoscopy learning seminars have been suggested as mechanisms to support the delivery of non-technical skills. Educational opportunities may also be enhanced through the utilisation of video conferencing portals.3
Limitations have been placed on the number of personnel in the endoscopy room to protect both patients and staff.1 Whether trainee endoscopists are non-essential personnel in this context remains to be defined.3 Accreditation in diagnostic gastroscopy is required for CCT although colonoscopy is also pursued by most trainees.4 Traditionally, this was already challenging; half of gastroenterology trainees surveyed in 2018 lacked accreditation in colonoscopy as they approached CCT.5 There also exists a disparity between mandatory CCT requirements and the range of endoscopic skills that should equip a trainee for their consultant jobs. Biswas et al report low levels of confidence in one quarter of senior specialist trainees when asked about endoscopic management of gastrointestinal (GI) bleeding; the effect of COVID-19 on endoscopy training is likely to compound this further.6
In the medium-term to long-term there are opportunities to widen the use of capsule endoscopy (CE) procedures for diagnosis and to reduce demands on more invasive endoscopic services.7 The BSG suggest that in addition to small bowel capsule endoscopy (SBCE) this might include upper GI capsule endoscopy (UGICE) for suspected upper GI bleeding/surveillance of varices, as well as colon capsule endoscopy (CCE) in selected symptomatic patients.7
The potential for CCE to reduce the demands on endoscopy services has been explored through the Scottish Capsule Programme in which CCE undertaken in symptomatic faecal immunochemical test positive patients has been estimated to reduce the need for colonoscopy in up to 70% of those referred for investigation.8 In England, a CCE pilot, sponsored by NHS England and NHS Improvement (NHSE&I), is being rolled out in several centres.
As COVID-19 remains prevalent, further strain on endoscopy and training is expected. We believe the proposed strategy to use CE to increase access to endoscopy services provides a unique training opportunity. With the widespread adoption of remote working, the use of video-conferencing platforms such as Microsoft Teams (which allow screen sharing and multiprofessional interaction) and the emerging role of CE in the deceleration and early recovery phases of the COVID-19 pandemic, training in CE should be more accessible than ever.
Small bowel capsule endoscopy training (UK)
Pre-COVID-19, the JAG released a standardised training pathway for SBCE in recognition of rising demand and in line with BSG and European Society of Gastrointestinal Endoscopy guidelines for the investigation for obscure GI bleeding, common GI conditions and surveillance of polyposis syndromes.9–11 Increasing demand was mirrored by trainees for formal training in CE.12 Figure 1 is an adaptation of the current JAG pathway and is the current model adopted by our CE training network.
Figure 1.
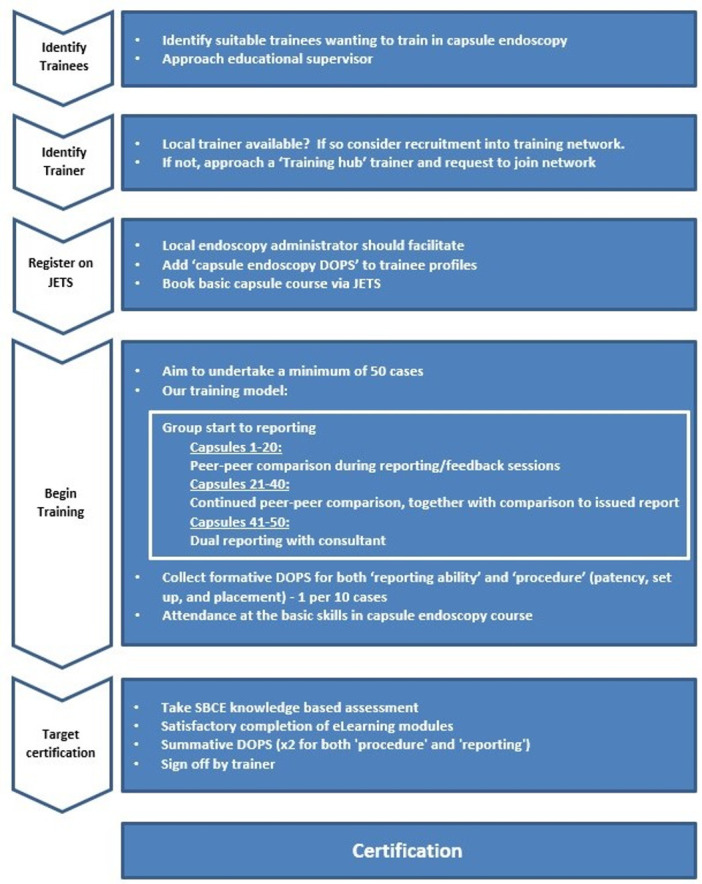
Model currently adopted by our training hub. Adapted from: JAG certification: capsule endoscopy (small bowel). DOPs, directly observed procedures; JAG, Joint Advisory Group on Gastrointestinal Endoscopy; SBCE, small bowel capsule endoscopy.
The JAG approved SBCE certification pathway is based on the American Society for Gastrointestinal Endoscopy training guidance.13 This encompasses a SBCE training course, undertaking a minimum number (50) of cases, collecting both formative and summative directly observed procedures (DOPS) with local trainer sign-off, completion of e-learning modules and successful completion a SBCE knowledge-based assessment. There also exists a standardised training programme for CCE which has been advocated by the BSG and is again based on European and US standards. Training in UGICE is yet to be formalised.
Training opportunities in capsule endoscopy (COVID-19)
Although COVID-19 has limited training opportunities in endoscopic procedures requiring face-to-face contact and tactile assistance, it potentially frees up time for alternative focus of training. Importantly, CE is not included in the current gastroenterology training curriculum. We do not propose that CE training should replace conventional endoscopy training; however, while access to endoscopy training remains limited, there are positive opportunities to train in CE.
Once endoscopy services recover, conventional endoscopy training should take priority; however, we anticipate that trainees will have a unique opportunity to shape their training at this juncture and that ongoing training in CE might well continue as an adjunct.
The ability to report the study and subsequently have training sessions for feedback remotely lends itself perfectly to the limitations faced by trainees in the current climate and could ultimately lead to pre-CCT accreditation in CE. The COVID-19 pandemic has created an environment in which the positioning of CE in investigation pathways may play a role in the recovery plan for endoscopy services. This will create a need for an appropriately trained workforce to meet the demands of a new service model. Existing technology can facilitate the delivery of CE training and it remains to be seen how artificial intelligence based models can facilitate endoscopy training through assisted lesion-detection.14
The lack of a CE service in a trainees’ base hospital need not be a barrier to accessing training using a virtual learning environment. Use of video-conferencing platforms across the NHS facilitates communication between geographically disparate sites willing to offer CE training.
Capsule endoscopy training networks
The endoscopy team in our trust have taken advantage of this unique training opportunity by developing a CE training network. Although this is in its early stages, the proposed model is demonstrated in figures 1 and 2. The Training Hub is led by a group of CE reporters (gastroenterology consultants) and comprises several gastroenterology registrars. The team meets weekly at a time previously occupied by conventional endoscopy training, and trainees are rostered to attend the relevant surrogate multi-disciplinary team (MDT) meetings to maximise output. We have chosen to focus on SBCE pro-term given that this service is well established in our trust.
Figure 2.

Hub and Spoke model depicting the relationship between the ‘Training Hub’ and peripheral/remote ‘Training Centres’.
PillCam Viewer Software was distributed to the trainees and an introductory group tutorial on how to successfully navigate the software, identify key landmarks and structure a report was delivered. A curated set of 20 SBCE studies encompassing a broad set of endoscopic findings (identified by the consultant supervisors) was then distributed to trainees. A ‘group start’ was preferred to a ‘staggered start’ for training purposes to encourage peer-to-peer comparison and peer-driven feedback. Trainees reported the same studies each week in advance of the weekly training session.
Microsoft Teams platform was used, allowing screen sharing and commentary when presenting and discussing cases and capsule studies. While the full team have been on-site for the majority of meetings, social distancing restrictions brought about by COVID-19 have meant that remote dial-in has been the default approach. This has improved efficiency as screen-sharing from individual computers has removed the need to upload multiple studies onto a single unit. Use of information technology in this way is in keeping with the ambition to digitalise secondary care within the NHS as part of the long-term plan, and although a substantial proportion of this effort is directed towards enhancing the patient experience—we believe that the same ambition can be applied to training which will indirectly contribute to good patient care.15 16
The structured approach to training also means that DOPs can be completed on the day of presentation and training portfolios can be kept up-to-date.
Early outcomes of local training network
The group-start approach to training has allowed for the direct comparison of findings between trainees at each weekly meeting. At first, the variation between reports was broad, with a significant degree of over-reporting/misinterpretation of normal findings, heterogeneity of findings in general, and disagreement in recommendations. Over time, reports have become more homogenous in structure, terminology, findings and recommendations. More mature management plans are being constructed and when disagreements arise, the consultant supervisors facilitate further discussion by taking control of the shared image display and providing structured, constructive feedback. Once the 20 preselected CE studies have been completed, we plan to move to a dual-reporting model whereby the trainee and consultant remotely report a live study and compare results.
To date, this has been a success and there are plans to publish outcome data once the desired number of SBCE studies have been successfully reported by our local training group in order to inform other units/networks who wish to adopt such a programme. We hope to inspire an upscaling of such networks to afford trainees in remote trusts the opportunity to continue to progress in their endoscopy training—our outcome data should inform this process further.
Footnotes
Contributors: TEC and AB were involved in the initial drafting of the manuscript. TEC, JF, TT, PC and AB were involved in the final drafting of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: TT has received conference attendance funding from Janssen.
Ethics statements
Patient consent for publication
Not required.
References
- 1. British Society of gastroenterology (Bsg) endoscopy activity and COVID-19: Bsg and JAG guidance – update 22.03.20, 2020. Available: https://www.bsg.org.uk/covid-19-advice/endoscopy-activity-and-covid-19-bsgand-jag-guidance/
- 2. Sud A, Torr B, Jones ME, et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol 2020;21:1035–44. 10.1016/S1470-2045(20)30392-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. FitzPatrick M, Clough J, Harvey P. How can gastroenterology training thrive in a post-COVID world? Frontline Gastroenterol 2021;12:338–41. 10.1136/flgastro-2020-101601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Joint Royal Colleges of Physicians Training Board . Gastroenterology (includes sub-specialty of hepatology). Available: https://www.jrcptb.org.uk/specialties/gastroenterology-includes-sub-specialty-hepatology [Accessed 12 Oct 2020].
- 5. Clough J, FitzPatrick M, Harvey P, et al. Shape of training review: an impact assessment for UK gastroenterology trainees. Frontline Gastroenterol 2019;10:356–63. 10.1136/flgastro-2018-101168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Biswas S, Alrubaiy L, China L, et al. Trends in UK endoscopy training in the Bsg trainees' national survey and strategic planning for the future. Frontline Gastroenterol 2018;9:200–7. 10.1136/flgastro-2017-100848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Penman I, Rees C. British Society of gastroenterology guidance on recommencing gastrointestinal endoscopy in the deceleration and early recovery phases of COVID-19 pandemic. Available: https://www.bsg.org.uk/covid-19-advice/bsg-guidance-on-recommencing-gi-endoscopy-in-the-deceleration-early-recovery-phases-of-the-covid-19-pandemic/ [Accessed 30 Sep 2020]. [DOI] [PMC free article] [PubMed]
- 8. MacLeod C, Wilson P, Watson AJM. Colon capsule endoscopy: an innovative method for detecting colorectal pathology during the COVID-19 pandemic? Colorectal Dis 2020;22:621–4. 10.1111/codi.15134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. JAG certification: capsule endoscopy (small bowel). Available: https://www.thejag.org.uk/CMS/UploadedDocuments/Scheme/Scheme5/Capsule%20endoscopy%20certification%20crtieria%20and%20process%201.1.pdf [Accessed 12 Oct 2020].
- 10. Sidhu R, Sanders DS, Morris AJ, et al. Guidelines on small bowel enteroscopy and capsule endoscopy in adults. Gut 2008;57:125–36. 10.1136/gut.2007.129999 [DOI] [PubMed] [Google Scholar]
- 11. Pennazio M, Spada C, Eliakim R, et al. Small-Bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of gastrointestinal endoscopy (ESGE) clinical guideline. Endoscopy 2015;47:352–86. 10.1055/s-0034-1391855 [DOI] [PubMed] [Google Scholar]
- 12. McAlindon ME, Parker CE, Hendy P, et al. Provision of service and training for small bowel endoscopy in the UK. Frontline Gastroenterol 2012;3:98–103. 10.1136/flgastro-2011-100044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. ASGE Training Committee 2011-2012, Rajan EA, Pais SA, et al. Small-Bowel endoscopy core curriculum. Gastrointest Endosc 2013;77:1–6. 10.1016/j.gie.2012.09.023 [DOI] [PubMed] [Google Scholar]
- 14. Park J, Hwang Y, Nam JH, et al. Artificial intelligence that determines the clinical significance of capsule endoscopy images can increase the efficiency of reading. PLoS One 2020;15:e0241474. 10.1371/journal.pone.0241474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. UK Government . Making it work: harnessing the power of health information technology to improve care in England. Available: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/550866/Wachter_Review_Accessible.pdf [Accessed 13 Dec 2020].
- 16. NHS . The NHS long term plan. Available: http://www.longtermplan.nhs.uk [Accessed 13 Dec 2020].


