Abstract
COVID-19 has dominated life in 2020 with, at the time of writing, over 4.9M global cases and >320 000 deaths. The impact has been most intensely felt in acute and critical care environments. However, with most UK elective work postponed, laboratory testing of faecal calprotectin halted due to potential risk of viral transmission and non-emergency endoscopies and surgeries cancelled, the secondary impact on chronic illnesses such as inflammatory bowel disease (IBD) is becoming apparent. Data from the Scottish Biologic Therapeutic Drug Monitoring (TDM) service shows a dramatic drop in TDM testing since the pandemic onset. April 2020 saw a 75.6% reduction in adalimumab testing and a 36.2% reduction in infliximab testing when compared with February 2020 data, a reduction coinciding with the widespread cancellation of outpatient and elective activity. It is feared that disruption to normal patterns of care and disease monitoring of biologic patients could increase the risk of disease flare and adverse clinical outcomes. Urgent changes in clinical practice have been instigated to mitigate the effects of the pandemic on routine clinical care. Further transformations are needed to maintain safe, effective, patient-centred IBD care in the future.
Keywords: inflammatory bowel disease
Introduction
COVID-19, caused by SARS-CoV-2, has dominated life in 2020. At the time of writing, 4.9M global cases of COVID-19 had been confirmed, with >320 000 deaths.1 Up to 20% require hospitalisation, and 5% require critical care.2 3 Healthcare providers have responded by rapidly downscaling non-urgent care and redeploying staff to quickly upscale acute and critical care capacity.4 While the impact of COVID-19 has been most intensely felt in acute and critical care environments, the secondary impact on chronic illnesses such as inflammatory bowel disease (IBD) is becoming apparent.
Early impact of COVID-19 on IBD care
As in China and Italy, most UK elective work has been postponed.4 Laboratory testing of faecal calprotectin (FC) has been halted due to potential viral transmission through faecal shedding.5 Non-emergency endoscopies and surgeries have been postponed. Changes in IBD service design and delivery have been quickly implemented to respond to these challenges. Although some of these may improve IBD care in the future, the short-term impact of COVID-19 remains a concern.
Particular fears were quickly raised about the use of biologics and immunomodulators.6 In April 2020, the British Society of Gastroenterology (BSG) published guidance for patients with IBD and healthcare professionals enabling self-identification to high, moderate or low risk categories for COVID-19-related adverse outcomes.7 Biologic and immunomodulator drugs sit within the ‘moderate risk’ category. Moderately or severely active disease despite the use of ‘moderate risk treatments’ and higher doses of systemic steroids are in the highest risk category. Reflecting this, the guidance strongly advocates the continuation of all prescribed IBD treatments.7 However, disruption to normal patterns of care and disease monitoring of biologic patients could also increase the risk of disease flare and adverse clinical outcomes.
COVID-19 and therapeutic drug monitoring
In the biologics era, treatment paradigms have shifted towards ‘treat-to-target’ strategies emphasising early treatment escalation in the presence of active disease, prevention of gut damage and maintenance of disease remission. Close monitoring of disease is integral to this approach and the COVID-19 pandemic poses a significant challenge to this. Therapeutic drug monitoring (TDM) has become an important tool in monitoring treatment response to commonly used biologics like adalimumab and infliximab. Evidence demonstrating improved outcomes with TDM testing has led to widespread adoption in clinical practice.8 Testing is usually performed in clinic alongside routine blood tests or at attendance for drug infusion. Therefore, changes in TDM testing since the start of the pandemic are likely to be illustrative of the overall effect on clinical care and disease monitoring in this group of patients.
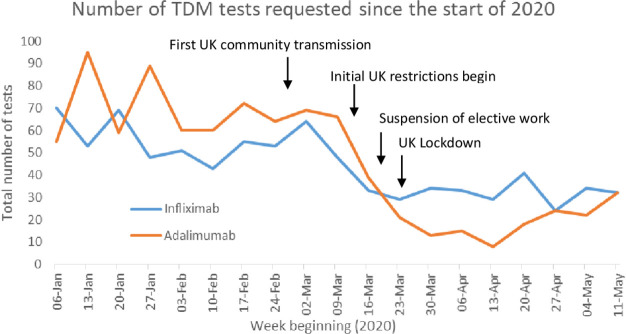
A Scottish TDM service was established in 2018. Over 5600 adalimumab and infliximab samples were processed in 2019 (49.5% increase from 2018); 54.7% tests were performed proactively, an approach used to try and maintain disease remission through attainment of target trough drug levels. Testing numbers have declined sharply since the pandemic began. Adalimumab testing decreased by 23.8% in March, 75.6% in April and 57.8% in the first 2 weeks of May 2020 compared with February 2020 (figure 1). The start of the reduction in tests coincided with the cancellation of elective outpatient activity.
Figure 1.
Trends in Scottish TDM testing over the last 4 months against significant COVID-19 milestones. TDM, therapeutic drug monitoring.
Infliximab testing has also declined, although to a lesser extent with a fall of 13.9% in March, 36.2% in April and 34.7% in the first 2 weeks of May 2020 compared with February 2020 (figure 1). This is worrying as it could be interpreted as a surrogate marker that some hospitals have been unable to maintain routine access to drug treatment during the pandemic or that individuals have missed or stopped treatments due to fear about attending hospital.
The impact of this relaxation in disease monitoring remains to be seen but detrimental outcomes through flare of disease, steroid exposure, hospital admission or IBD-related surgery are a concern.
Short-term mitigation of COVID-19 impact on disease monitoring
Clinical practice has adapted quickly to compensate for the effect of COVID-19. Many examples of service innovation have been forthcoming. Adoption of remote monitoring tools has been the primary focus in the early phase of the response. IBD clinical nurse specialists (CNS) have played a vital role in the design and delivery of changes in practice and it is of fundamental importance that IBD CNS resources are protected.
Locally, we have implemented a number of measures for our patients including:
Expansion in capacity of CNS helpline.
Increased utilisation of telephone consultations.
Adoption of video consultation technology.
An ‘IBD hot clinic’ for one-stop assessment when clinically indicated.
Cohorting of biologic infusions to a ‘clean’ non-COVID site.
Increased biologic dosing in selected patients to decrease infusion frequency and compensate for reduced infusion capacity due to social distancing.
Introduction of phlebotomy clinics for blood monitoring in selected patients.
Launch of remote point of care (POC) FC testing.
Building on this, other initiatives in development include an ‘app’ based interactive consultation platform, which supports autonomous disease monitoring through symptom tracking, encouraging treatment compliance, providing reassurance or prompting contact with the IBD team.
Managing and monitoring of biologics post COVID-19
SARS-CoV-2 has likely irrevocably changed the way we manage patients with IBD. Virtual consultations, if acceptable to patients, will be expanded as traditional face-to-face models of care are downscaled. However, further transformations are needed for safe, effective, patient-centred IBD care while reducing the potential for exposure to SARS-CoV-2. This is especially true for patients receiving biologic treatment for whom blood monitoring, TDM and FC testing capabilities must be re-established as a priority.
Greater collaboration with primary care and community pharmacy offers the potential to develop community hubs for blood monitoring. However, other possibilities also merit consideration and may help empower patient self-management. POC testing is used in many areas of medicine. Most notably, diabetic patients monitor blood sugars at home and titrate their insulin therapy through POC blood sugar monitoring. Biologic TDM has traditionally been performed on a serum sample, taken during a hospital visit, analysed in a laboratory. This creates a significant lag between results and implementation of treatment changes. A validated POC test for infliximab, using serum blood samples, has achieved results within 15 min.9 Similar work demonstrated consistency between standard ELISA and POC testing for anti-infliximab antibodies.10 11 Additionally, an at-home adalimumab testing kit, where a patient obtains a dried blood sample by performing a simple finger prick and posting the sample to the laboratory, has shown good results in a small cohort.12 Adalimumab POC testing may prove useful for community TDM testing, allowing dose optimisation while mitigating the burden of additional hospital attendances. For infliximab, a similar strategy would allow efficient review of dosing prior to treatment, thus optimising the efficacy of the hospital visit. In addition, POC TDM may be of value in the management of acute severe ulcerative colitis (ASUC) requiring infliximab treatment. Evidence suggests that rapid clearance of infliximab can occur during induction therapy for ASUC, likely through excessive faecal loss,13 and data from Kennedy et al 14 demonstrated an association between induction drug levels and long-term clinical outcomes. With results expected in 2024, the TITRATE study is currently recruiting patients with ASUC, examining treatment outcomes associated with POC testing to inform individual dosing regimes, guided by a pharmacokinetic ‘dashboard’ type model.15 Innovations of this type, coupled with POC FC testing,16 could facilitate rapid and objective monitoring of response to induction treatment and may help to minimise steroid exposure and potentially even reduce the need for co-prescription of immunomodulators.
The COVID-19 pandemic has presented an unprecedented need for change in how we manage IBD, resulting in rapid service restructure, balancing safe disease management with protecting patients from the virus. The impact will be lasting and careful analysis of patient outcomes should be undertaken. However, this period also presents an opportunity to embrace modern techniques and new ways of working, highlighting areas for research and development to improve the efficiency and efficacy of IBD patient care and its delivery.
Footnotes
Contributors: SS contributed to the design of the article, analysis and interpretation of the data and drafting of the manuscript. SS was responsible for submission. AD collected the original data and contributed to manuscript revision. JPS contributed to data interpretation and manuscript revision. JM conceptualised the work, contributing to data interpretation and drafting of the initial manuscript, along with revisions of the final article. SS and JM are the guarantors of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1. John Hopkins University & Medicine . COVID-19 Map [Internet]. Baltimore, 2020. Available: https://coronavirus.jhu.edu/map.html [Accessed 20 May 2020].
- 2. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China. summary of a report of 72314 cases from the Chinese centre for disease control and prevention. JAMA 2020;323:p1239–42. [DOI] [PubMed] [Google Scholar]
- 3. Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–20. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Danese S, Ran ZH, Repici A, et al. Gastroenterology department operational reorganisation at the time of covid-19 outbreak: an Italian and Chinese experience. Gut 2020;69:981–3. 10.1136/gutjnl-2020-321143 [DOI] [PubMed] [Google Scholar]
- 5. Chen Y, Chen L, Deng Q, et al. The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J Med Virol 2020:1–8. [DOI] [PubMed] [Google Scholar]
- 6. Mao R, Liang J, Shen J, et al. Implications of COVID-19 for patients with pre-existing digestive diseases. Lancet Gastroenterol Hepatol 2020;5:425–7. 10.1016/S2468-1253(20)30076-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. British Society of Gastroenterology . BSG expanded consensus advice for the management of IBD during the COVID-19 pandemic [Internet]. London, 2020. Available: https://www.bsg.org.uk/covid-19-advice/bsg-advice-for-management-of-inflammatory-bowel-diseases-during-the-covid-19-pandemic/ [Accessed 23 Apr 2020].
- 8. Papamichael K, Cheifetz AS. Use of anti-TNF drug levels to optimise patient management. Frontline Gastroenterol 2016;7:289–300. 10.1136/flgastro-2016-100685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Costa Santos MP, Palmela C, Gouveia C, et al. P736 point-of-care infliximab quantification in inflammatory bowel disease in daily practice. Journal of Crohn's and Colitis 2018;12:S484. 10.1093/ecco-jcc/jjx180.863 [DOI] [Google Scholar]
- 10. Facchin S, Buda A, Cardin R, et al. P475 rapid point-of-care anti-drug antibodies measurement correlates with standardised T tests and facilitate a proactive therapeutic drug monitoring approach in IBD patients on anti-TNF-α maintenance therapy. Journal of Crohn's and Colitis 2019;13:S349–50. 10.1093/ecco-jcc/jjy222.599 [DOI] [Google Scholar]
- 11. Ametzazurra A, Rivera N, Balsa A, et al. FRI0195 Point-of-care monitoring of anti-infliximab antibodies in patients treated with the reference infliximab or ct-p13 in routine clinical practice [abstract]. Annals of the Rheumatic Diseases 2017;76:555. [Google Scholar]
- 12. Berends SE, Bloem K, de Vries A, et al. Monitoring of adalimumab concentrations at home in patients with inflammatory bowel disease using dried blood samples. Ther Drug Monit 2020;42:289–94. 10.1097/FTD.0000000000000686 [DOI] [PubMed] [Google Scholar]
- 13. Brandse JF, van den Brink GR, Wildenberg ME, et al. Loss of infliximab into feces is associated with lack of response to therapy in patients with severe ulcerative colitis. Gastroenterology 2015;149:350–5. 10.1053/j.gastro.2015.04.016 [DOI] [PubMed] [Google Scholar]
- 14. Kennedy NA, Heap GA, Green HD, et al. Predictors of anti-TNF treatment failure in anti-TNF-naive patients with active luminal Crohn's disease: a prospective, multicentre, cohort study. Lancet Gastroenterol Hepatol 2019;4:341–53. 10.1016/S2468-1253(19)30012-3 [DOI] [PubMed] [Google Scholar]
- 15. U.S. National Library of Medicine . TITRATE (inducTIon for acuTe ulceRATivE Colitis) (TITRATE) [Internet]. Maryland, 2020. Available: https://clinicaltrials.gov/ct2/show/NCT03937609 [Accessed 27 Aug 2020].
- 16. Vinding KK, Elsberg H, Thorkilgaard T, et al. Fecal Calprotectin Measured By Patients at Home Using Smartphones-A New Clinical Tool in Monitoring Patients with Inflammatory Bowel Disease. Inflamm Bowel Dis 2016;22:336–44. 10.1097/MIB.0000000000000619 [DOI] [PubMed] [Google Scholar]