Abstract
Rickettsioses are arthropod-borne zoonotic diseases, several of which occur in Australia. This study aimed to assess the exposure levels and risk factors for Rickettsia spp. among Australian wildlife rehabilitators (AWRs) using serology, PCR and a questionnaire. Antibody titres against Spotted Fever Group (SFG), Typhus Group (TG) and Scrub Typhus Group (STG) antigens were determined using an immunofluorescence assay. PCR targeting the gltA gene was performed on DNA extracts from whole blood and serum. Logistic regression was used to identify risk factors associated with seropositivity. Of the 27 (22.1%; 27/122) seropositive participants all were seropositive for SFG, with 5/27 (4.1%) also positive for TG. Of the 27 positive sera, 14.8% (4/27) were further classified as exposure to R. australis, 3.7% (1/27) to R. honei, 3.7% (1/27) to R. felis and 77.8% (21/27) were classified as ‘indeterminate’—most of which (85.7%; 18/21) were indeterminate R. australis/R. honei exposures. Rickettsia DNA was not detected in whole blood or serum. Rehabilitators were more likely to be seropositive if more than one household member rehabilitated wildlife, were older than 50 years or had occupational animal contact. These findings suggest that AWRs are at increased risk of contracting Rickettsia-related illnesses, however the source of the increased seropositivity remains unclear.
Keywords: seroprevalence Rickettsia australis, Rickettsia honei, Rickettsia felis, Rickettsia typhi, Australia, wildlife rehabilitators, spotted fever, typhus
1. Introduction
Rickettsioses are among the oldest known diseases and are caused by bacteria from the genera Rickettsia and Orientia, which are transmitted to humans via arthropod vectors, including ticks, lice, fleas and mites [1]. The genus Rickettsia is comprised of two main antigenic groups; the spotted fever group (SFG), which are primarily transmitted to vertebrate hosts by hard ticks (Ixodidae) [2,3], and the typhus group (TG) transmitted by fleas and lice [4]. Genus Orientia contains two known species; O. tsutsugamushi and O. chuto, transmitted by mites and together form the Scrub Typhus Group (STG) [5]. The salivary glands and faeces of these arthropod vectors may harbour large numbers of rickettsiae, and human infection can occur via bacterial injection during a blood meal, or through faecal contamination of the bite site [6]. The most common clinical presentations of rickettsiosis include headache, rash, fever, chills, muscle aches and an inoculation ’eschar’ (scab) from the bite of a tick [7] or a mite [8]. Severe cases of rickettsiosis can be fatal [9,10]. The similarity of symptoms between rickettsioses and other diseases renders clinical diagnosis challenging. Therefore many cases of human disease probably go unrecognised [11]. In Australia, rickettsial infection is not nationally notifiable, making it difficult to define the distribution of rickettsial diseases and understand the nationwide disease burden attributable to rickettsioses [12].
Rickettsiae of clinical importance from both the STG, SFG and TG have been described in Australia, and several species of SFG rickettsia have been associated with Australian wildlife and their ticks [13]. Scrub typhus, caused by O. tsutsugamushi (STG) is endemic to tropical north Queensland (QLD) and the Torres strait Islands [14], the ‘top end’ of the Northern Territory (NT) [15] and the Kimberley region of Western Australia (WA) [16]. The main reservoir and vector of O. tsutsugamushi in Australia are the larvae of the mite species Leptotrombidium deliense, which parasitise rodents, marsupials, cattle, cats and dogs [17].
Queensland Tick Typhus (QTT), was the first tick-transmitted infection recognised in Australia and is predominantly seen along the eastern seaboard of Australia from Torres Strait to south-eastern Victoria (VIC) [18]. The causative agent of QTT, R. australis (member of SFG), is transmitted by the paralysis tick Ixodes holocyclus, and the common marsupial tick I. tasmani, whose respective vertebrate hosts are bandicoots and native rats [19]. Flinders Island Spotted Fever (FISF), occurring on Flinders Island in Bass Strait, South Australia (SA) and north QLD is caused by R. honei (SFG) [20] and is transmitted by the reptile tick Bothriocroton hydrosauri, whose vertebrate hosts include snakes and blue-tongue lizards [21]. The main arthropod vector of R. felis (also a member of the SFG) causing cat flea typhus [22] is the cat flea (Ctenocephalides felis), the reservoir host of which is yet to be determined, but is thought likely to be the dog [23,24]. Murine typhus is caused by R. typhi, which is currently the only member of the TG recognised in Australia. Rickettsia typhi is transmitted by the fleas of rodents and has been implicated in human disease in WA [25], QLD [26] and Victoria [27].
Over the past 20 years several emerging rickettsioses have been reported in Australia [28]. In 2007, a Rickettsia spp. was identified that was genetically related to R. honei (SFG) and produced similar symptoms to FISF [29]. The agent, subsequently designated Rickettsia honei subsp. marmionii was detected in Haemaphysalis novaeguineae ticks, which typically infest macropods [28], and to date, it has not been found in B. hydrosauri [13]. The associated rickettsiosis was named Australian Spotted Fever owing to its different epidemiology compared to the parent strain R. honei. This subspecies has also been isolated from the blood of chronically ill patients [30]. Several new rickettsia species of unknown pathogenicity have also been described in Australian ticks. Rickettsia gravesii (SFG) has been isolated from the ornate kangaroo tick Amblyomma triguttatum [31], and molecular methods have identified novel rickettsiae in ticks collected from Australian mammals including: koalas (Koala rickettsia from Bothriocroton concolor) [32], Tasmanian devils (Candidatus Rickettsia tasmanensis from I. tasmani) [33] and the marsupial mouse (R. antechini from I. antechini) [13]. Although the pathogenicity of these recently described Rickettsia species is unknown, their potential to cause disease in humans cannot be discounted, particularly for those living in endemic areas and/or in regular contact with Australian wildlife and their ticks.
Although Australia is home to several rickettsia species that are pathogenic to humans, the level of nationwide exposure to Rickettsia spp. within the Australian population is unknown. Clinical studies of chronically ill patients with suspected rickettsia-related illness have reported seroprevalence to SFG as high as 41% [30]. A recent study on Australian veterinarians reported that 16.0% of participants were seropositive for R. felis, 4.6% for R. typhi and 35.1% were seropositive for both organisms [34]. Reports of frequent tick bites and low-grade illness amongst bushland recreationists, prompted a study into the seroprevalence to SFG rickettsia in rogainers, who may spend 6–24 h in the bush whilst participating in the sport [35]. The rogainer group in this study, who frequented areas of WA with a high Rickettsia gravesii prevalence in ticks, had a significantly higher SFG seroprevalence in comparison to the control group (23.1% and 2.1% respectively) and were 14 times more likely to be seropositive for SFG Rickettsia.
Australian wildlife rehabilitators (AWRs) are potentially at risk of contracting rickettsioses because the wildlife for which they care may harbour ticks, fleas, lice and mites, all of which are rickettsial vectors, however the degree of Rickettsia exposure amongst this population is unknown. In a study investigating the zoonotic disease Q fever in a cohort of AWRs, 43.8% of participants reported having been bitten by a tick [36], indicating that AWRs are potentially at risk of rickettsioses. Therefore, the aim of this study was to: (1) determine the level of prior exposure to Rickettsia spp. in a population of AWRs attending a wildlife rehabilitation conference through measurement of SFG, TG and STG antibody titres, (2) investigate the association between seropositivity and risk factors for exposure to Rickettsia spp. to determine potential sources of exposure for wildlife rehabilitators, and (3) identify current infections in this AWR cohort using a PCR assay specific to SFG and TG rickettseae.
2. Results
2.1. Responses and Demographics of Australian Wildlife Rehabilitators
Of the 162 conference attendees who provided blood for the previous study (Mathews et al., 2021) and were subsequently invited to participate in this study, 122 (75.3%) gave consent for their blood sample to be tested for antibody against Rickettsia spp. The median age of the 120/122 participants who disclosed their age was 55 years (range 21–79; IQR 48–62), and the majority of the cohort were female (113/122; 92.6%). All respondents had been actively rehabilitating wildlife for the past five years, and just over half (62/122; 50.8%) had been rehabilitating wildlife for more than 10 years. Almost all participants (118/122; 96.9%) identified their association with wildlife as a rehabilitator; however, 26.3% (31/118) also performed other wildlife-associated roles. These additional roles included veterinary nursing (18/118; 14.8%), wildlife research (5/118; 4.1%) and one participant also worked as a veterinarian (1/118; 1%). Just over half of the cohort resided in the conference host state of New South Wales (NSW; 64/122; 52.5%) followed by VIC (18/122; 14.8%), WA (16/122; 13.1%), QLD (12/122; 9.8%), SA (4/122; 3.3%), Tasmania (TAS; 4/122; 3.3%), NT (2/122; 1.6%) and the Australian Capital Territory (ACT; 2/122; 1.6%). The proportion of AWRs residing in NSW was higher than those in VIC and QLD (52.5%, 14.8% and 9.8% respectively) compared to the available total national population estimates for these states (32.0%, 25.8% and 20.1% respectively). The proportions within the remaining jurisdictions of WA, SA, TAS, ACT and NT (combined 22%) were comparable to the Australian population distribution. According to the available data on population distribution via remoteness area [37], the proportion of the cohort residing in major cities was lower (46.7% vs. 70% respectively), while the proportion residing in inner regional Australia was higher (42% vs. 18% respectively) than the distribution of the general Australian population. The proportion of participants residing in outer regional/remote areas (11.5%; 14/122) was comparable to the population distribution for these remoteness categories (11%).
2.2. Wildlife Rehabilitating Demographics and Practices
The majority of rehabilitators (97/122; 79.5%) spent over 30 weeks per year rehabilitating wildlife and the number of animals (mammals, birds and reptiles) rehabilitated per year ranged from 2 to 1500. For most participants, the location at which the majority of wildlife rehabilitation was undertaken was in their home or someone else’s home (108/122; 88.5%), followed by a wildlife rescue centre/dedicated wildlife hospital (27/122; 22.1%), a veterinary clinic that also treats wildlife (15/122; 12.3%) and a zoo (5/122; 4.1%). Of the 114 AWRs who rehabilitated animals on their own property, 17.5% (20/114) housed animals exclusively within their home, 10.5% (12/114) in outdoor enclosures, while 71.9% (82/122) practiced both housing arrangements. For 79% (97/122) of AWRS, possums and gliders were the most commonly and frequently rehabilitated species, followed by kangaroos and wallabies and flying-foxes which were rehabilitated by 51.6% (63/122), 50.0% (61/122) and 39.34% (48/122) of AWRs respectively. Of the 58.2% (71/122) of participants reporting occupational animal contact, 81.7% (58/71) had been exposed to domestic animals, 73.2% (52/71) to wildlife and 36.6% (26/71) to ruminants.
Biosecurity practices adopted by 120 participants when handling animals and cleaning enclosures are presented in Table 1 (no questionnaire responses for 2 participants). Almost all AWRs practiced prompt hand washing after handling animals (116/120; 96.7%) and cleaning enclosures (117/120; 97.5%); however, 3.3% (4/120) of respondents did not practice any form of biosecurity when performing either activity. The vast majority of AWRs did not meet ‘adequate’ biosecurity requirements in either situation, with only 5.8% (7/120) and 2.5% (3/120) practicing ‘enhanced biosecurity’ when handling animals and cleaning enclosures, respectively.
Table 1.
Biosecurity practices reported by 120 Australian wildlife rehabilitators when handling animals and cleaning enclosures. Results obtained from a survey conducted at the Australian Wildlife Rehabilitation Conference in Sydney in July 2018.
| Biosecurity Practice | Number (%) of Participants When Handling Animals | Number (%) of Participants When Cleaning Enclosures |
|---|---|---|
| Participant report of practice | ||
| No PPE | 4 (3.3) | 4 (3.3) |
| Prompt hand washing | 116 (96.7) | 117 (97.5) |
| Overalls/protective outerwear | 16 (13.3) | 25 (20.8) |
| Disposable gloves | 28 (23.3) | 47 (39.2) |
| Safety glasses | 5 (4.2) | 10 (8.3) |
| Face mask | 3 (2.5) | 7(5.8) |
| Level of biosecurity practice * | ||
| Inadequate | 104 (86.7) | 102 (85.0) |
| Adequate | 9 (7.5) | 15 (12.5) |
| Enhanced | 7 (5.8) | 3 (2.5) |
2.3. Serology
2.3.1. Rickettsia Screening
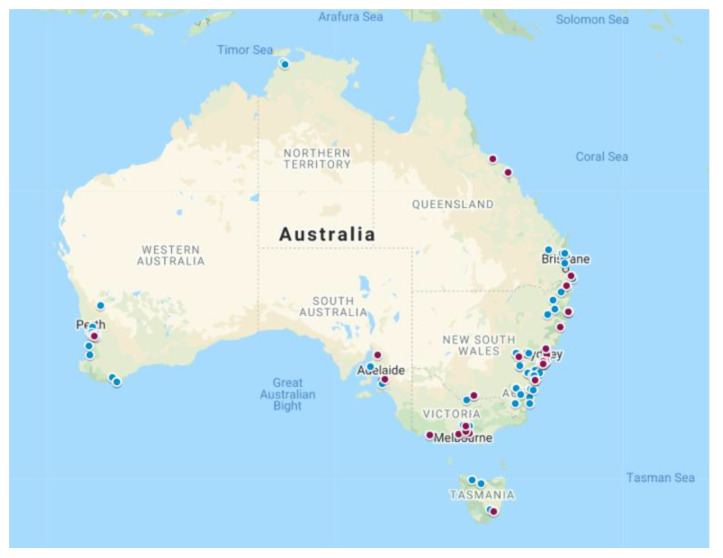
Of the 122 participants, 27 (22.1%; 95% CI 15.1%–30.5%) were seropositive for Rickettsia spp. Of these, just under half (13/27; 48.1%) resided in NSW followed by VIC (7/27; 25.9%), QLD (3/27; 11.1%) and SA (2/27; 7.4%) with TAS and WA returning one seropositive participant each (1/27; 3.7%) (Figure 1, Table 2). Of the 27 seropositive participants, occupational contact with animals (domestic, companion, and wildlife) was reported by 70.1% (19/27). Just under half (12/27; 48.1%) reported having been bitten by a tick. All (27/27; 100%) of the seropositive participants were reactive to SFG, 18.5% (5/27) were reactive to TG and all (27/27; 100%) were non-reactive to STG.
Figure 1.
Location of residence of 122 Australian wildlife rehabilitators participating in rickettsia seroprevalence survey conducted at the Australian Wildlife Rehabilitation Conference in Sydney in July 2018. Maroon denotes seropositive and blue denotes seronegative for Rickettsia spp.
Table 2.
Serological results (reciprocal titres) and antigenic classification of seropositive wildlife rehabilitators participating in a rickettsia seroprevalence survey conducted at the Australian Wildlife Rehabilitation Conference in Sydney in July 2018.
| Spotted Fever Group | Typhus Group | Sample Classification | |||||
|---|---|---|---|---|---|---|---|
| (SFG) | (TG) | ||||||
| Participant | R. australis | R. honei | R. felis | R. typhi | Antigenic Group | Species | State of Residence |
| 96 | ≥2048 | 256 | - | - | SFG | R. australis | VIC |
| 117 + | 1024 | 256 | - | - | SFG | R. australis | NSW |
| 147 | 512 | - | - | - | SFG | R. australis | NSW |
| 161 + | ≥2048 | 512 | - | 256 | SFG | R. australis | NSW |
| 110 + | 512 | ≥2048 | 512 | 256 | SFG | R. honei | NSW |
| 148 | - | - | 256 | - | SFG | R. felis | QLD |
| 6 + | ≥2048 | ≥2048 | 256 | - | SFG | R. australis/R. honei * | NSW |
| 13 | 1024 | 1024 | - | - | SFG | R. australis/R. honei * | VIC |
| 19 | 1024 | 1024 | - | - | SFG | R. australis/R. honei * | VIC |
| 20 + | ≥2048 | ≥2048 | - | - | SFG | R. australis/R. honei * | QLD |
| 27 + | 1024 | 1024 | - | - | SFG | R. australis/R. honei * | NSW |
| 34 | ≥2048 | 1024 | - | - | SFG | R. australis/R. honei * | SA |
| 36 + | 512 | 512 | - | - | SFG | R. australis/R. honei * | QLD |
| 36 + | ≥2048 | ≥2048 | - | 256 | SFG | R. australis/R. honei * | NSW |
| 62 | 256 | 512 | - | - | SFG | R. australis/R. honei * | VIC |
| 83 + | 1024 | 1024 | - | - | SFG | R. australis/R. honei * | NSW |
| 86 + | ≥2048 | ≥2048 | 256 | - | SFG | R. australis/R. honei * | NSW |
| 87 | 512 | 512 | - | - | SFG | R. australis/R. honei * | NSW |
| 94 | 512 | 256 | - | - | SFG | R. australis/R. honei * | VIC |
| 113 | 256 | 256 | - | - | SFG | R. australis/R. honei * | SA |
| 115 | 512 | 512 | - | - | SFG | R. australis/R. honei * | WA |
| 138 + | 256 | 256 | - | - | SFG | R. australis/R. honei * | NSW |
| 158 | 512 | 512 | - | - | SFG | R. australis/R. honei * | VIC |
| 164 | 1024 | 512 | - | - | SFG | R. australis/R. honei * | VIC |
| 40 + | 512 | 1024 | 256 | - | SFG | R. australis/R. honei/R. felis * | NSW |
| 127 + | 512 | 256 | 256 | 256 | SFG/TG | R. australis/R. honei/R. felis/R. typhi * | NSW |
| 172 | 512 | 512 | - | 256 | SFG/TG | R. australis/R. honei/R. typhi * | TAS |
* Indeterminate rickettsial infections, + evidence of self-reported tick bite, Dash (-) = reciprocal antibody titre < 256, VIC—Victoria, NSW—New South Wales, QLD—Queensland, WA—Western Australia, SA—South Australia, TAS—Tasmania.
2.3.2. Rickettsia Species Titration
The results of the titration for Rickettsia species exposure are displayed in Table 2. Twenty-one (21/27; 77.8%) of the serum samples were classified as ‘indeterminate’ due to titres being within twofold of one another. Of these, 18 (18/21; 85.7%) were classified as indeterminate R. australis/R. honei infections, one (1/21; 4.8%) was indeterminate for all three SFG species tested (R. australis/R. honei /R. felis) and the remaining two (2/21; 9.5%) ‘indeterminate’ infections were reactive to both SFG and TG rickettsia. Four (14.8%) of the 27 initial screening seropositive participants were classified as having been exposed to R. australis (4/27; 14.8%), while one was classified as exposed to R. honei (1/27; 3.7%) and one to R. felis. (1/27; 3.7%).
2.4. Rickettsia spp. Serostatus and Investigated Potential Risk Factors
Univariate logistic regression identified five risk factors (out of nine) that were associated with being serologically positive to Rickettsia spp. (p < 0.3) (Table 3), all of which were considered in the multivariable analysis. Three variables were retained in the final model (p < 0.1) (Table 4). Rehabilitators testing seropositive to Rickettsia spp. were 2.4 (95% CI = 0.89–7.32) times more likely to be >50 years of age, more than twice as likely to report occupational contact with animals compared to those without occupational animal contact (OR = 2.2, 95% CI = 0.88–6.16) and were 2.3 (95% CI = 0.95–5.90) times more likely to reside in homes where more than one household member rehabilitated wildlife.
Table 3.
Univariable logistic regression analysis of positive serological result to Rickettsia spp. exposure among Australian wildlife rehabilitators participating in a survey at the Australian Wildlife Rehabilitation Conference in Sydney in July 2018. (p < 0.3).
| Variable Name and Description | Total Number | Seropositive | Seronegative | Odds Ratio | 95% Confidence Intervals | p-Value |
|---|---|---|---|---|---|---|
| State of residence | 122 | 0.365 | ||||
| South West (WA + SA) | 3 | 17 | 1 | |||
| Southeast (VIC + TAS) | 8 | 14 | 3.24 | 0.77–16.99 | 0.125 | |
| Northeast (QLD + NT) | 3 | 11 | 1.55 | 0.25–9.74 | 0.63 | |
| East (NSW + ACT) | 13 | 53 | 1.39 | 0.39–6.58 | 0.637 | |
| Age | 120 | 0.184 * | ||||
| ≤50 | 6 | 33 | 1 | |||
| >50 | 21 | 60 | 1.93 | 0.74–5.67 | ||
| Number of people in household rehabilitating wildlife | 121 | 0.145 * | ||||
| 1 | 13 | 60 | 1 | |||
| >1 | 14 | 34 | 1.90 | 0.80–4.56 | ||
| Total number of animals per year cared for per year | 119 | 0.226 * | ||||
| 0–100 | 18 | 75 | 1 | |||
| >100 | 8 | 18 | 1.85 | 0.67–4.85 | ||
| Occupational animal contact | 122 | 0.140 * | ||||
| No | 8 | 43 | 1 | |||
| Yes | 19 | 52 | 1.96 | 0.81–5.17 | ||
| Tick Bite | 122 | 0.577 | ||||
| No | 14 | 55 | 1 | |||
| Yes | 13 | 40 | 1.27 | 0.56–3.43 | ||
| Association with reptiles | 122 | 0.443 | ||||
| No | 23 | 86 | 1 | |||
| Yes | 4 | 9 | 1.66 | 0.42–5.62 | ||
| Biosecurity practices when handling animals | 120 | 0.220 * | ||||
| None/handwash only | 21 | 61 | 1 | |||
| Handwash and other | 6 | 32 | 0.55 | 0.18–1.42 | ||
| Biosecurity practices when cleaning enclosures | 120 | 0.973 | ||||
| None/handwash only | 15 | 52 | 1 | |||
| Handwash and other | 12 | 41 | 1.02 | 0.42–2.40 |
* p < 0.3, VIC—Victoria, NSW—New South Wales, ACT—Australian Capital Territory, QLD—Queensland, NT—Northern Territory WA—Western Australia, SA—South Australia, TAS—Tasmania.
Table 4.
Final multivariable logistic regression results for exposure to Rickettsia spp. among Australian wildlife rehabilitators participating in a survey at the Australian Wildlife Rehabilitation Conference in Sydney in July 2018. (p < 0.1).
| Variable Name and Description | Total Number | Seropositive | Seronegative | Adjusted Odds Ratio | 95% Confidence Intervals | p-Value |
|---|---|---|---|---|---|---|
| Age | 120 | 0.087 | ||||
| ≤50 | 6 | 33 | 1 | |||
| >50 | 21 | 60 | 2.4 | 0.89–7.32 | ||
| Number of people in household rehabilitating wildlife | 121 | 0.066 | ||||
| 1 | 12 | 60 | 1 | |||
| >1 | 15 | 34 | 2.3 | 0.95–5.90 | ||
| Occupational animal contact | 122 | 0.092 | ||||
| No | 8 | 43 | 1 | |||
| Yes | 19 | 52 | 2.2 | 0.88–6.16 |
2.5. Real-Time PCR (qPCR)
All extraction controls and no-template controls were negative for the β-actin gene ruling out the occurrence of cross-contamination during DNA extraction and PCR set up. For each assay, amplification curves were observed for all positive control DNA samples indicating that the PCR assays were working appropriately. No inhibition was observed when comparing the human β-actin PCR assays of 1/10 diluted and neat whole blood or serum DNA extracts.
Whole Blood and Serum
Of the 122 DNA samples extracted from whole blood, 121 (99.2%) were strongly positive for the β-actin endogenous control gene. Quantification cycles (Cqs) ranged from 19.41–29.25, indicating successful DNA extraction. Of these three (3/121; 2.4%) were positive in the gltA-PCR in the initial screen (Cqs~37), however, these amplifications were not reproducible when repeated in triplicate, and were subsequently considered negative. Of the 122 DNA samples extracted from serum, 91 (79.5%) amplified positive for the β-actin gene (Cq range 28.8–38.8). Of these four (4/91; 4.4%), were positive in the gltA-PCR in the initial screen (Cq’s~38). This finding was not reproducible when these samples were assayed in triplicate, therefore these samples were subsequently considered negative.
3. Discussion
This is the first study to investigate rickettsia exposure in Australian wildlife rehabilitators, a population considered at risk of rickettsioses due to the numerous potential rickettsial species associated with Australian wildlife and their ticks [13,19,28,31,40,41]. This study reports an overall Rickettsia spp. seroprevalence of 22.1% (27/122) in this cohort of AWRs, with all positive sera reactive for SFG rickettsia, and the majority of infections (85.1%; 23/27) attributed to R. australis or R. honei, both of which are transmitted by ticks. All seropositive participants tested negative for O. tsutsugamushi (STG), however none of these participants resided in the tropical regions of WA, NT or QLD where scrub typhus is endemic [14,15,16].
There are very few studies which have investigated exposure to Rickettsia spp. in Australian populations, however the 22.1% seroprevalence observed in the current study is comparable to the 23% SFG seroprevalence found in a study of Australian rogainers who are known to be at an increased risk of tick bites due to their bushland activities, and is considerably higher than the 2.1% SFG seroprevalence observed in the control group of the same study who had minimal tick exposure [35]. In contrast to the current study and the rogainer study in which participants were presumably healthy, another Australian study (using archived patient sera) reported a SFG seroprevalence of 39% and 41% in two cohorts of chronically ill patients (from Melbourne and Adelaide respectively) compared to <6% SFG seroprevalence in the control groups [30]. The elevated SFG seroprevalence of these patients compared to the AWRs and rogainers could be due to sampling bias, in that the patient cohorts were selected on the basis that they were chronically ill with suspected rickettsia infection, whereas the rogainer and AWR populations were presumed healthy. Additionally, the high seroprevalence in the Adelaide patient cohort could be due to the Adelaide region of SA being endemic for spotted fever illnesses [20,42]. However, the explanation for the Melbourne group is unclear because apart from Gippsland [43], there are no other known regions of rickettsia endemicity in Victoria.
Another Australian study on veterinarians attending a veterinary conference reported that overall 16% of participants were seropositive to R. felis (SFG), 4.6% to R. typhi (TG) and 35.1% were classified as ‘indeterminate’ R felis or R. typhi exposures [34]. These findings suggest that Australian veterinarians are at an increased risk of occupational exposure to rickettsia, primarily from exposure to fleas, however the authors were unable to demonstrate a significant association between seropositivity and contact with fleas or animals (companion, large and exotic). Similarly, in the current study no association was found between seropositivity and exposure to animals (ruminants, domestic, wildlife). In contrast to veterinarians, the majority of rickettsial infections in AWRs were tick-associated, and although eight participants exhibited seroreactivity to R. felis and/or R.typhi, only one participant, (who did not identify as a veterinarian and had no occupational animal contact) was classified as having been exposed to R. felis (Table 2). A possible explanation for the greater R. felis and R.typhi seroprevalence in the veterinarian cohort is that this group worked in veterinary clinical practice. While the breakdown of type of animal exposure was not reported in this study, these veterinarians were more likely to be regularly exposed to larger numbers of companion animals than AWRs, in particular cats and dogs, which may act as potential hosts for fleas harbouring R. felis and R typhi [44,45].Although the seropositivity in veterinarians was associated with flea-borne rickettsia and in the current study the majority of exposures were attributable to ticks, well over half of the seropositive participants in both studies (veterinarians 46/73, 63%; AWRs 21/27; 77.8%) were classified as ‘indeterminate’ rickettsial infections highlighting the difficulties in serodiagnosis due to cross reactivity between rickettsia species.
Quantitative PCR may be used to diagnose rickettsioses during the early stages of infection [46], and has also been employed to detect rickettsia DNA in blood samples of chronically ill patients [30]. Given the elevated seroprevalence to SFG rickettsia in this cohort a highly specific gltA-PCR was performed (sensitivity of one copy per reaction (Cq = 35) [47] on DNA extracted from whole blood and serum, to identify AWRs that may have been bacteraemic at the time of blood collection, or those who may have circulating organism due to long standing illness. Although a small number of DNA extracts (from both blood and serum) amplified positive for the gltA-PCR in the initial screen (producing Cqs~38), this amplification was not reproducible when the qPCR reactions on the same samples were repeated in triplicate, and so all samples were considered negative. The severity of rickettsioses is highly variable between individuals, ranging from a mild self-limiting illness to multi-organ failure [9].
The clinical presentation of rickettsioses also varies between pathogens; however common symptoms include fever, malaise, myalgia, headache, rash lymphadenopathy and often a characteristic eschar will be present at the inoculation site [48].Although details of participants’ clinical history were not collected, and it is therefore unknown whether any had been clinically unwell and treated for or diagnosed with rickettsial disease, the absence of rickettsiaemic participants in this study is consistent with the presumption that they were healthy at the time of blood collection. Indeed, they were well enough to attend a wildlife rehabilitator conference, however the possibility of low levels of circulating rickettsiae and underlying illness in these participants cannot be discounted, particularly since estimates of rickettsia DNA concentration of as low as 8.40 × 101 ± 4.19 × 101 copies/mL of blood has been observed in patients with moderately severe disease [49]. The assay for the β-actin gene was performed on DNA samples extracted from serum, with only 91 of these 122 samples (79.5%) amplifying positive for the β-actin gene (Cq range 28.8–38.8). The Cqs of these samples ranged from 28.82–38.8, and overall were considerably higher than those obtained from whole blood DNA extracts (p = 0.007). The higher Cqs and greater number of samples negative for the β-actin gene in the serum DNA extracts is expected, as the level of circulating DNA in the serum of healthy individuals is typically very low [50]. Although for clinical diagnosis, whole blood and serum DNA extracts are considered suitable for PCR, DNA extracted from the buffy coat fraction may have improved the sensitivity of detection of rickettsial DNA, owing to the intracellular lifecycle of rickettisia and the higher concentration of leucocytes found in buffy coat. The samples in this study were collected at variable times between the hours of 9 am and 2 pm. However, daily fluctuations in bacterial load have been observed in peripheral blood samples of patients infected with Rickettsia rickettsia, with peak bacteraemia occurring in early morning [51], therefore taking blood samples earlier in the day may have resulted in greater quantity of rickettsia DNA in the blood and serum.
Although 85.1% (23/27) of rickettsia infections in the current study were attributed R. australis or R. honei, which are both tick-transmitted, no association between reported prior tick bite and seropositivity was identified, and only 47% (11/23) of the seropositive participants reported having been bitten by a tick. Similarly, Abdad, Cook, Dyer, Stenos and Fenwick [35] found no association between SFG seroprevalence and tick bite in rogainers, and other studies have reported that ≤50% of patients with confirmed tick-transmitted rickettsial illness recalled being bitten by a tick [9,52]. These findings indicate that approximately 50% of bites go unrecognised, which may explain the observed lack of association between seropositivity and reported tick bite. The lack of tick bite awareness could be because the individual does not feel the tick attaching due to the local anaesthetic that ticks inject into the skin prior to biting [18], or if the tick detaches before becoming engorged it may go unnoticed. It follows that the number of participants reporting tick bite in this study is likely an underestimation of the true exposure to tick bites.
Alternatively, it is also possible that participants who were seropositive for tick-borne rickettsiae may have been inoculated via means other than a tick bite. Excreta released by ticks during feeding contains high levels of rickettsiae [53] resulting in contamination of the skin and coat of the host animal with rickettsial organisms, hence the rehabilitator could become infected by inhaling aerosolised organisms while handling an animal on which ticks had fed [54]. Although infection via the respiratory route is rarely described as a mode of transmission by ticks, infection in guinea pigs [55], monkeys [56,57] and cases of aerosol transmission of R. rickettsia have also been reported in humans [58,59,60]. Indeed Murine Typhus caused by R. typhi can be acquired through the respiratory route [61] from infected flea faeces [26]. Similarly, rickettsiae present on the skin and coat of animals may be transmitted via inoculation of skin abrasions and contamination of the conjunctiva.
This study utilised IFA methodology to titrate serum samples against antigen preparations from four rickettsia species (R. australis, R. honei, R. felis and R. typhi). Species specific seroreactivity was assigned to six (22.3%) participants, however the majority (21/27;77.7%) of participants were classified as ‘indeterminate’ due to their lack of preferential reactivity to R. australis and R. honei antigens (Table 2). Although IFA is considered the gold standard reference method for rickettsia serodiagnosis [62], serological cross reactivity among the different rickettsial antigens is well documented, particularly between antigens of SFG rickettsia [63]. Similarly, antigenic cross-reactivity is also displayed within the TG [64] and between R. felis (SFG) and R. typhi (TG) [34,65]. This serologic cross-reactivity makes it difficult to infer the rickettsia species responsible for provoking the immune response [66]. Furthermore, extensive R. australis and R. honei serological cross-reactivity may preclude definitive speciation of the infecting rickettsia during clinical diagnosis [67]. It is also possible that serological responses of the ’indeterminate’ participants were from exposure to more than one species, or that these participants had been exposed to species of rickettsia that were not evaluated in this study, such as R. honei subsp. marmionii which is genetically related to R. honei. The high number of ‘indeterminate’ seropositive samples highlights the difficulties in diagnosing rickettsial infections and emphasises the importance of obtaining accurate details regarding a patient’s clinical and epidemiological history to accompany diagnostic testing. Other methodologies offering greater specificity than IFA, such as Western blotting or cross-adsorption [34], may result in a more definitive determination of the species involved in the exposure. However, such analyses were beyond the scope of the current study and are not routinely undertaken.
In this study, a broad range of antibody titres were observed, with eight of the 27 (29.6%) seropositive AWRs displaying titres of 1/2048 (Table 2), which is eight-fold higher than the assigned 1/264 cut-off titre. Additional information regarding how recently these participants had been exposed could have been obtained by the collection of a second serum sample taken several weeks following the initial one to assess whether the antibody titres of these participants were rising, thus demonstrating recent infection, or through antibody subclass analysis including individual IgG and IgM titres (rather than the combined IgA, IgG and IgM conjugate used in this study). The sera in this study were opportunistically obtained from another study, for which the questionnaire accompanying the blood sample related to the zoonotic disease Q fever and did not specifically ask questions regarding symptoms of rickettsial illnesses and, therefore although they were well enough to attend a conference, it is unknown whether these wildlife conference participants were currently experiencing, or had previously suffered from, acute or chronic rickettsia-related illnesses.
Multivariable logistic regression identified three risk factors suggestive of association a positive serostatus. Older participants (>50 years) were 2.4 (95% CI = 0.89–7.32) times more likely to be seropositive than rehabilitators <50 years. A similar association between age and SFG seropositivity was reported in the rogainer study by Abdad, Cook, Dyer, Stenos and Fenwick [35]. The positive association with seropositivity and age in these two studies is possibly due to an increased chance of exposure to rickettsia over time. In contrast Teoh, Hii, Stevenson, Graves, Rees, Stenos and Traub [34] demonstrated that veterinarians >60 years had a decreased risk of exposure to R. felis and R. typhi, which was in line with older veterinarians reporting that they spent less time in clinical practice compared to their middle age and younger counterparts, and therefore had a reduced likelihood of exposure. Rehabilitators reporting occupational contact with animals were 2.2 (95% CI = 0.88–6.16) times more likely to be to Rickettsia spp. seropositive. The source of exposure amongst the veterinarians in the study by Teoh, Hii, Stevenson, Graves, Rees, Stenos and Traub [34] was thought to be from infected fleas located on companion animals, particularly cats and dogs. However, the AWRs in this study were exposed to a wide range of domestic and wildlife species and no association between seropositivity and any particular animal species was identified. The finding that rehabilitators residing in households where more than one person rehabilitated wildlife were more than twice as likely to be seropositive (OR = 2.3, 95% CI = 0.95–5.90) is interesting, and possibly suggestive of a link that could be explained by households with more than one rehabilitator in residence having greater exposure to larger numbers of animals, and therefore their ticks as rickettsial vectors.
Another possibility is that households with more than one rehabilitator are more likely to be involved in outdoor activities such as bushwalking or camping and therefore are more likely to be exposed to ticks. Further studies may indicate how it is that AWRs become exposed to rickettsiae. Future serological studies should focus on targeted questions that may allow for better understanding of how wildlife rehabilitators become exposed to ticks.
Rickettsia are emerging zoonoses and since first described by Ricketts in 1909 [68], the Rickettsia genus has grown to comprise approximately 34 species (http://www.bacterio.cict.fr/qr/rickettsia.html; accessed on 7 February 2021), and contains many novel species of unknown pathogenicity that are yet to be named. Given the recent emergence of R. felis in Australia [45], and the identification and characterisation of three novel rickettsiae over the past three decades including R. gravesii, [69], R. honei [70] and R. honei subsp. marmionii [29], it is possible that the elevated seropositivity observed in this cohort of AWRs (particularly the participants classified as ‘indeterminate’ R. australis/R. honei infections) could be due to exposure to one or more novel rickettsial species not yet discovered, or to a previously described species that is not known to be endemic in Australia.
4. Methods
4.1. Study Design and Participant Recruitment
The serum samples tested in this study were obtained opportunistically from a previous cross-sectional study investigating Coxiella burnetii seroprevalence in AWRs. To be eligible to participate in this study, AWRs were required to be >18 years and to have rehabilitated Australian mammals [36]. Participants from the aforementioned study who elected to receive their Q fever serology results and provided their contact details for this purpose, were invited to participate in the current study via a hyperlink or web address to the secure online platform REDCap (Research Electronic Data Capture) [71,72] hosted at The University of Sydney, where they could access a detailed participant information statement (PIS). Willing participants provided online consent to have their blood sample tested for antibody against Rickettsia spp. and provided their contact details if they wished to be notified of their individual serological results and/or a summary of the project outcomes. For participants supplying a postal address, hard copies of the PIS consent form and a stamped self-addressed envelope were included in the mailout with their Q fever serology results. This research was approved by the Human Research Ethics Committee of the University of Sydney (project number 2018/457).
4.2. Sample Size Calculation
The sample size for this study was calculated using Statulator software [73]. Assuming a nationwide average of 2% seroprevalence to SFG rickettsia (control group in the rogainer study by Abdad, Cook, Dyer, Stenos and Fenwick [35], an expected response rate of 15% (serosurvey of veterinary workers [74]) and a national wildlife rehabilitator population size of 14,358 [36], this study would require a sample size of 103 AWRs for estimating seroprevalence to Rickettsia spp. with 7.0% absolute precision and 95% confidence.
4.3. Questionnaire
The paper-based questionnaire (Supplementary S1) completed by each participant at the time of blood sample collection been previously described [36]. Of relevance to the current study were questions regarding: (i) demographics of the rehabilitator and where they rehabilitated wildlife, (ii) the type of wildlife they rehabilitated and other animals located on or nearby to the caring residence (iii) their rehabilitation and husbandry practices which included a question regarding the frequency of tick bites.
4.4. Laboratory Methods
4.4.1. Blood Sample Collection
Blood samples were collected from participants on each day of the conference. Approximately 8 mL of blood was drawn from the median cubital vein of each participant and divided into serum separator tubes (Interpath, Victoria, Australia) and EDTA blood tubes (Interpath, Victoria, Australia) by a certified phlebotomist or registered doctor. The serum separator tubes were centrifuged at 4000× g for 10 min, after which the serum was removed and stored at −20 °C until transportation to the laboratory. All blood samples were de-identified.
4.4.2. Serology
The serum samples were analysed at the Australian Rickettsial Reference Laboratory (ARRL), Geelong, Australia using an in-house indirect immunofluorescence assay (IFA) accredited by the National Association of Testing Authorities (accreditation No. 14342).
Screening of Sera for Rickettsia spp.
Serum samples were initially screened for reactivity to SFG, TG and STG. Antibodies against SFG were tested using a combined preparation of R. australis, R. honei and R. felis antigens; against TG using R. typhi antigen; and against STG using O. tsutsugamushi (Gilliam and Karp strains) antigen. Sera was diluted 1/128 in 2% casein then approximately 5 µL of was spotted in duplicate onto a glass slide coated with antigens (described above). After incubation at 35 °C for 40 min, the slides were washed with PBS (diluted 1/10) and air-dried before adding a combined conjugate containing fluorescein-labelled goat anti-human IgA + IgG + IgM (H+L). The incubation and wash steps were repeated, the slides were dried and mounted with a coverslip. Each well was visualised using fluorescence microscopy (400×; Axioskop 40; Zeiss). Sera was deemed positive if fluorescence was observed at a dilution of 1/128 and classified according to reactivity to antigenic group (SFG, TG, STG)
Titration of Sera against R. australis, R. honei, R. felis and R. typhi Antigens
Positive sera underwent doubling dilutions (1/128 to 1/1024) in 2% casein. Each dilution was spotted in duplicate onto glass slides coated with individual antigen preparations of R. honei, R. australis, R. felis and R. typhi after which the slides were processed as described above. A minimum titre of 1/256 was required to deem a sample as positive. Species specific seroreactivity within and between serological groups (SFG, TG) was defined when; sera was reactive to only one species, or, if sera was reactive to more than one species, a four-fold minimum difference between antigens of reactive species was required, and in such instances the species with the highest titre was designated as the agent responsible for the infection. Serum from patients returning a titre within these limits was classified as ‘indeterminate’ as it is impossible to determine the causative agent of infection with such titres. All antigens and screening slides were prepared in-house at ARRL as described by Teoh, Hii, Stevenson, Graves, Rees, Stenos and Traub [34] and antibodies were manufactured by KPL/ SeraCare (Milford, MA, USA). Positive and negative human serum samples were included on each slide.
4.4.3. DNA Extraction
Genomic DNA was extracted from whole blood and serum using the Biosprint® 96 One-For-All Vet Kit (Qiagen, Germany) with the following modifications. For whole blood, 200 µL of EDTA blood and 40 mL of Proteinase K was incubated at 56 °C for 30 min. For serum, 160 µL of sample and 40 µL of Proteinase K was incubated at 56 °C for 3 h. Following incubation, 240 µL of each blood lysate and 140 µL of each serum lysate was loaded into a 96 well plate and DNA extractions were performed using the Biosprint® 96 automated extraction system (Thermo Fisher Scientific, Waltham, MA, USA) in accordance with the manufacturer’s instructions. Eight randomly distributed extraction controls (ECs) using PBS in place of serum or blood were included in every 96-well plate.
4.4.4. Real-Time PCR (qPCR)
A qPCR assay (gltA-PCR) using primers targeting a highly conserved region of rickettsial citrate synthase gene gltA [47] was used in an attempt to detect SFG and TG DNA in the serum and whole blood DNA extracts, and human β-actin served as an internal reference gene to verify DNA quality [75]. Rickettsial DNA provided by the ARRL and DNA extracted from a human buccal swab in house served as positive controls for the gltA-PCR and the β-actin PCR, respectively. Both assays were performed in singleplex and each reaction contained 1X SensiFAST No-Rox (Bioline, Alexandria, Australia), primers and probe (concentrations and sequences listed in Table 5), 2 µL of DNA (extracted from blood or serum) and nuclease-free water in a total volume of 10 µL. Assays were performed using a Bio-Rad-CFX Real-Time PCR Thermocycler (Bio-Rad Laboratories Pty Ltd, Gladesville, NSW, Australia) and underwent an initial denaturation at 95 °C for 3 min followed by 40 cycles of denaturation at 95 °C for 10 s, annealing at 60 °C for 40 s. No template controls with nuclease-free water were used in place of sample DNA, and positive control DNA were included in every PCR run. Primers and probes were synthesised by Integrated DNA Technologies (Baulkham Hills, NSW, Australia). Any sample with a quantification cycle (Cq) < 40 was considered positive for β-actin. Samples returning a Cq < 40 for the citrate synthase gene were repeated and deemed positive for gltA-PCR if the same result was reproducible in triplicate. A subset of samples was tested for inhibition by diluting the sample 1/10 and comparing the Cq values.
Table 5.
Sequence and product lengths of target gene primers used to detect SFG and TG DNA (citrate synthase) and human β -actin DNA (internal reference gene to verify DNA quality) in the whole blood and serum DNA extracts of Australian wildlife rehabilitators participating in a survey at the Australian Wildlife Rehabilitation Conference in Sydney in July 2018.
| Target Gene and Primers |
Primer Sequences (5′-3′) | Product Length (bp) |
Final Concentration (nM) |
Reference/ Primer Source |
|---|---|---|---|---|
| Citrate synthase Forward primer Reverse primer Probe |
TCGCAAATGTTCACGGTACTTT TCGTGCATTTCTTTCCATTGTG FAM a- TGCAATAGCAAGAACCGTAGGCTGGATG -BHQ1 b |
74 |
300 300 200 |
Adapted from [47] |
| Human β-actin Forward primer Reverse primer Probe |
CATGCCATCCTGCGTCTGGA CCGTGGCCATCTCTTGCTCG FAM a- CGGGAAATCGTGCGTGACATTAAG-BHQ1 b |
172 |
300 300 200 |
Adapted From [75] |
a 6-Carboxyfluorescein, b Black Hole Quencher-1, SFG—Spotted fever group, TG—Typhus Group.
4.5. Statistical Analysis
4.5.1. Data Management
The serological results of participants were added to a Microsoft Excel (Microsoft Corporation, Washington, DC, USA) spreadsheet alongside their molecular and serological results for processing and subsequently analysed using R statistical program (R Core Team, 2019) [76].
4.5.2. Variables and Risk Factors
The primary outcome variable was whether the AWR was seropositive or seronegative for exposure to Rickettsia spp. (rickettsia serostatus) based on assignment to antigenic groups (SFG, TG, STG). The secondary outcome variable was the classification of species-specific rickettsia infections (R. australis, R. honei, R. felis, R. typhi) in the seropositive participants. Descriptive statistics (mean, median and range for continuous variables, proportions for categorical variables) were generated to obtain information regarding the distribution of each variable. Continuous variables and questions regarding animal exposure and postcode of residence were handled as previously described [36]. Categories with 10% missing data were excluded in the statistical analysis.
Biosecurity practices were based on two questions in which participants indicated how frequently (‘always’, ‘frequently’, ‘occasionally’, ‘rarely’ or ‘never’) they utilised the following infection control practices while handling animals and cleaning enclosures: overalls/protective outerwear, disposable gloves, safety glasses, face mask, and prompt hand washing. The assessment and classification of adequate and enhanced biosecurity in both situations has been previously described [36] and were established by the authors, using recommendations from the Australian Veterinary Association Guidelines for Veterinary Personal Biosecurity [38] in combination with National Wildlife Biosecurity Guidelines [39]. Biosecurity practices were considered inadequate if participants ‘never’ used any form of personal protective equipment (PPE) when handling animals or cleaning enclosures. The use of each type of infection control was considered adequate if ‘always’ or ‘frequently’ was selected. Biosecurity practices were considered adequate if participants ‘always’ or ‘frequently’ used overalls/protective outerwear and practiced prompt hand washing when handling animals, and additionally wore disposable gloves when cleaning enclosures. Biosecurity practices were considered to be enhanced if participants ‘always’ or ‘frequently’ used overalls/protective outerwear, practiced prompt hand washing and wore disposable gloves when handling animals, and if all five methods of infection control were practiced when cleaning enclosures.
Potential risk factors for the outcome variable rickettsia serostatus were age, state of residence, remoteness area, total years rehabilitating wildlife, total weeks per year rehabilitating wildlife, rehabilitating wildlife on own property, number of people in household rehabilitating wildlife, wildlife species rehabilitated during rehabilitation career, total number of animals rehabilitated per year, association with reptiles, tick bite, occupational animal contact, biosecurity practices when handling animals and when cleaning enclosures.
4.5.3. Modelling
Univariable logistic regression was undertaken to identify associations between potential risk factors and serostatus (positive, negative). Risk factors with p < 0.3 in the univariable analysis were progressed to multivariable analysis after evaluating the strength of association between these risk factors using the Cramer’s V statistic. When the Cramer’s V statistic for a pair of risk factors was >0.7 only the variable which was more biologically plausible was included in subsequent multivariable analysis. Multivariate modelling was performed using backward selection where the variable with the least significance (Wald test) was removed sequentially. Variables with p-values < 0.1 were retained in the final model.
5. Conclusions
This is the first study to investigate the level of exposure to Rickettsia spp. in rehabilitators of Australian wildlife. An elevated overall seroprevalence to Rickettsia spp. compared to control groups in other Australian studies was observed, with most exposures in the seropositive participants attributable to tick-borne SFG rickettsia. The activities associated with tick exposure in AWRs are unclear; nonetheless, these findings have significant health implications especially given that ticks can transmit a number of clinically important rickettsiae. The elevated seroprevalence to Rickettisa spp. observed in this cohort suggests that Australian wildlife rehabilitators would benefit from targeted education programs aimed at raising their awareness of arthropod-borne infections. Such programs should include information regarding potential exposure pathways, clinical symptoms of rickettsial disease, and, recommendations of appropriate precautionary measures that may be implemented to minimise exposure risk to arthropod-borne diseases. For example, rickettsial pathogens could be included as a key infectious disease of concern in the National Wildlife Biosecurity Guidelines issued by Wildlife Health Australia [39].
Acknowledgments
The authors thank the AWRC 2018 organising committee for allowing us to conduct this research at the conference, the wildlife rehabilitators who participated in this study. We would also acknowledge Cathie Savage, whose MVPH study provided a basis for the questionnaire, Liana Bonner for her assistance at the AWRC conference and the Australian Rickettsial Reference Laboratory for conducting the IFAs.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/pathogens10060745/s1, S1 Q fever in AWR Serosurvey _V11_15-5-18.
Author Contributions
Conceptualization, K.O.M., D.P., J.M.N., P.A.S. and K.L.B.; Methodology, K.O.M., D.P., J.M.N., P.A.S., K.L.B., J.S., S.G., N.W. and C.N.; Validation, J.S.; Formal Analysis, K.O.M., J.S. and J.-A.T.; Investigation, K.O.M., J.M.N., K.L.B. and N.W.; Writing—Original Draft Preparation, K.O.M.; Writing—Review & Editing, D.P., J.M.N., P.A.S., K.L.B., J.S., S.G., N.W. and C.N.; Supervision, D.P., J.M.N., K.L.B., and J.-A.T.; Project Administration, K.L.B.; Funding Acquisition, D.P., J.M.N., K.L.B., S.G. and N.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research was partially funded by a Marie Bashir Institute 2017 Zoonoses Node Seed Funding Grant Funding and NHMRC project grant APP1049558.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Human Research Ethics Committee of the University of Sydney (2018/457; approved 21st June 2018).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data available on request due to privacy restrictions.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Walker D.H. Rickettsiae. In: Baron S., editor. Medical Microbiology. University of Texas; Austin, TX, USA: 1996. [PubMed] [Google Scholar]
- 2.Blanton L.S. The Rickettsioses: A practical update. Infect. Dis. Clin. N. Am. 2019;33:213–229. doi: 10.1016/j.idc.2018.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luce-Fedrow A., Mullins K., Kostik A.P., John H.K.S., Jiang J., Richards A.L. Strategies for detecting rickettsiae and diagnosing rickettsial diseases. Futur. Microbiol. 2015;10:537–564. doi: 10.2217/fmb.14.141. [DOI] [PubMed] [Google Scholar]
- 4.Azad A.F., Beard C.B. Rickettsial pathogens and their arthropod vectors. Emerging Infect. Dis. 1998;4:179–186. doi: 10.3201/eid0402.980205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Izzard L., Fuller A., Blacksell S., Paris D.H., Richards A.L., Aukkanit N., Nguyen C., Jiang J., Fenwick S., Day N.P.J., et al. Isolation of a Novel Orientia Species (O. chutosp. nov.) from a Patient Infected in Dubai. J. Clin. Microbiol. 2010;48:4404. doi: 10.1128/JCM.01526-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.NSW Department of Health Typhus (Epidemic, Murine and Other Rickettsial Diseases) Fact Sheet. [(accessed on 4 February 2019)]; Available online: https://www.health.nsw.gov.au/Infectious/factsheets/Pages/Typhus.aspx#.
- 7.McBride W.J., Hanson J.P., Miller R., Wenck D. Severe Spotted Fever Group Rickettsiosis, Australia. Emerg. Infect. Dis. 2007;13:1742–1744. doi: 10.3201/eid1311.070099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu G., Walker D.H., Jupiter D., Melby P.C., Arcari C.M. A review of the global epidemiology of scrub typhus. PLoS Negl. Trop. Dis. 2017;11:e0006062. doi: 10.1371/journal.pntd.0006062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stewart A., Smith S., Binotto E., McBride W.J.H., Hanson J. The epidemiology and clinical features of rickettsial diseases in North Queensland, Australia: Implications for patient identification and management. PLoS Negl. Trop. Dis. 2019;13:e0007583. doi: 10.1371/journal.pntd.0007583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sexton D.J., King G. Fatal queensland tick typhus. J. Infect. Dis. 1990;162:779–780. doi: 10.1093/infdis/162.3.779. [DOI] [PubMed] [Google Scholar]
- 11.Biggs H.M., Behravesh C.B., Bradley K.K., Dahlgren F.S., Drexler N.A., Dumler J.S., Folk S.M., Kato C.Y., Lash R.R., Levin M.L., et al. Diagnosis and Management of Tickborne Rickettsial Diseases: Rocky Mountain Spotted Fever and Other Spotted Fever Group Rickettsioses, Ehrlichioses, and Anaplasmosis. MMWR. Recomm. Rep. 2016;65:1. doi: 10.15585/mmwr.rr6502a1. [DOI] [PubMed] [Google Scholar]
- 12.National Notifiable Diseases Surveillance System Disease notification Rates, Australia, 1991 to 2020 and Year-to-Date Notifications for 2021. Commun. Dis. Intell. [(accessed on 15 March 2021)];2021 Available online: http://www9.health.gov.au/cda/source/rpt_3.cfm.
- 13.Graves S., Stenos J. Rickettsioses in Australia. Ann. N. Y. Acad. Sci. 2009;1166:151–155. doi: 10.1111/j.1749-6632.2009.04530.x. [DOI] [PubMed] [Google Scholar]
- 14.Faa A.G., McBride W.J., Garstone G., Thompson R.E., Holt P. Scrub Typhus in the Torres Strait Islands of North Queensland, Australia. Emerg. Infect. Dis. 2003;9:480–482. doi: 10.3201/eid0904.020509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Whelan P.I., Ralph A., Currie B.J., Raines M. Scrub typhus in the Northern Territory: Exceeding the boundaries of Litchfield National Park. Commun. Dis. Intell. Q. Rep. 2004;28:267–269. doi: 10.33321/cdi.2004.28.29. [DOI] [PubMed] [Google Scholar]
- 16.Graves S., Nack Z., Jones S., Wang L. Rickettsia serosurvey in Kimberley, Western Australia. Am. J. Trop. Med. Hyg. 1999;60:786–789. doi: 10.4269/ajtmh.1999.60.786. [DOI] [PubMed] [Google Scholar]
- 17.Mullen G.R., O’Connor B.M. Mites (Acari) In: Mullen G.R., Durden L.A., editors. Medical and Veterinary Entomology. 3rd ed. Academic Press; Cambridge, MA, USA: 2019. pp. 533–602. [Google Scholar]
- 18.Graves S.R., Stenos J. Tick-borne infectious diseases in Australia. Med. J. Aust. 2017;206:320. doi: 10.5694/mja17.00090. [DOI] [PubMed] [Google Scholar]
- 19.Raby E., Pearn T., Marangou A.G., Merritt A.J., Murray R.J., Dyer J.R., Graves S.R. New Foci of Spotted Fever Group Rickettsiae Including Rickettsia honei in Western Australia. Trop. Med. Infect. Dis. 2016;1:5. doi: 10.3390/tropicalmed1010005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Unsworth N.B., Stenos J., McGregor A.R., Dyer J.R., Graves S.R. Not only ’Flinders Island’ spotted fever. Pathology. 2005;37:242–245. doi: 10.1080/00313020500099247. [DOI] [PubMed] [Google Scholar]
- 21.Barker S.C., Walker A.R. Ticks of Australia. The species that infest domestic animals and humans. Zootaxa. 2014;3816:1–144. doi: 10.11646/zootaxa.3816.1.1. [DOI] [PubMed] [Google Scholar]
- 22.Williams M., Izzard L., Graves S.R., Stenos J., Kelly J.J. First probable Australian cases of human infection with Rickettsia felis (cat-flea typhus) Med. J. Aust. 2011;194:41–43. doi: 10.5694/j.1326-5377.2011.tb04145.x. [DOI] [PubMed] [Google Scholar]
- 23.Hii S.F., Kopp S.R., Abdad M.Y., Thompson M.F., O’Leary C.A., Rees R.L., Traub R.J. Molecular Evidence Supports the Role of Dogs as Potential Reservoirs for Rickettsia felis. Vector Borne Zoonotic Dis. 2011;11:1007–1012. doi: 10.1089/vbz.2010.0270. [DOI] [PubMed] [Google Scholar]
- 24.Ng-Nguyen D., Hii S.-F., Hoang M.-T.T., Nguyen V.-A.T., Rees R., Stenos J., Traub R.J. Domestic dogs are mammalian reservoirs for the emerging zoonosis flea-borne spotted fever, caused by Rickettsia felis. Sci. Rep. 2020;10:4151. doi: 10.1038/s41598-020-61122-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beaman M.H., Marlnovltch N. Murlne typhus in metropolitan Perth. Med. J. Aust. 1999;170:93–94. doi: 10.5694/j.1326-5377.1999.tb126896.x. [DOI] [PubMed] [Google Scholar]
- 26.Graves S.R., Dwyer B., Banks J., King G.K. A case of murine typhus in Queensland. Med. J. Aust. 1992;156:650–651. doi: 10.5694/j.1326-5377.1992.tb121464.x. [DOI] [PubMed] [Google Scholar]
- 27.Jones S.L., Athan E., O’Brien D., Graves S.R., Nguyen C., Stenos J. Murine typhus: The first reported case from Victoria. Med. J. Aust. 2004;180:482. doi: 10.5694/j.1326-5377.2004.tb06032.x. [DOI] [PubMed] [Google Scholar]
- 28.Parola P., Paddock C.D., Socolovschi C., Labruna M.B., Mediannikov O., Kernif T., Abdad M.Y., Stenos J., Bitam I., Fournier P.-E., et al. Update on Tick-Borne Rickettsioses around the World: A Geographic Approach. Clin. Microbiol. Rev. 2013;26:657–702. doi: 10.1128/CMR.00032-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Unsworth N.B., Stenos J., Graves S.R., Faa A.G., Cox G.E., Dyer J.R., Boutlis C.S., Lane A.M., Shaw M.D., Robson J., et al. Flinders Island Spotted Fever Rickettsioses Caused by “marmionii” Strain of Rickettsia honei, Eastern Australia. Emerg. Infect. Dis. 2007;13:566–573. doi: 10.3201/eid1304.050087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Unsworth N., Graves S., Nguyen C., Kemp G., Graham J., Stenos J. Markers of exposure to spotted fever rickettsiae in patients with chronic illness, including fatigue, in two Australian populations. Q. J. Med. 2008;101:269–274. doi: 10.1093/qjmed/hcm149. [DOI] [PubMed] [Google Scholar]
- 31.Owen H., Clark P., Stenos J., Robertson I., Fenwick S. Potentially pathogenic spotted fever group rickettsiae present in Western Australia. Aust. J. Rural. Health. 2006;14:284–285. doi: 10.1111/j.1440-1584.2006.00831.x. [DOI] [PubMed] [Google Scholar]
- 32.Vilcins I.E., Old J.M., Deane E.M. Detection of a spotted fever group Rickettsia in the tick Ixodes tasmani collected from koalas in Port Macquarie, Australia. J. Med. Entomol. 2008;45:745–750. doi: 10.1093/jmedent/45.4.745. [DOI] [PubMed] [Google Scholar]
- 33.Izzard L., Graves S., Cox E., Fenwick S., Unsworth N., Stenos J. Novel Rickettsia in Ticks, Tasmania, Australia. Emerg. Infect. Dis. 2009;15:1654–1656. doi: 10.3201/eid1510.090799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teoh Y.T., Hii S.F., Stevenson M.A., Graves S., Rees R., Stenos J., Traub R.J. Serological evidence of exposure to Rickettsia felis and Rickettsia typhi in Australian veterinarians. Parasites Vectors. 2017;10:129. doi: 10.1186/s13071-017-2075-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abdad M.Y., Stenos J., Fenwick S.G., Cook A., Dyer J. Seroepidemiological Study of Outdoor Recreationists’ Exposure to Spotted Fever Group Rickettsia in Western Australia. Am. J. Trop. Med. Hyg. 2014;91:584–588. doi: 10.4269/ajtmh.14-0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mathews K.O., Toribio J.-A., Norris J.M., Phalen D., Wood N., Graves S.R., Sheehy P.A., Bosward K.L. Coxiella burnetii seroprevalence and Q fever in Australian wildlife rehabilitators. One Health. 2021;12:100197. doi: 10.1016/j.onehlt.2020.100197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.National Rural Health Alliance The Little Book of Rural Health Numbers. [(accessed on 17 February 2020)]; Available online: https://www.ruralhealth.org.au/book/demography.
- 38.Australian Veterinary Association Guidelines for Veterinary Personal Biosecurity. [(accessed on 31 July 2019)]; Available online: https://www.ava.com.au/library-resources/other-resources/veterinary-personal-biosecurity/
- 39.Wildlife Health Australia National Wildlife Biosecurity Guidelines. Version 1.0. [(accessed on 31 July 2019)];2018 Available online: https://www.wildlifehealthaustralia.com.au/Portals/0/Documents/ProgramProjects/National_Wildlife_Biosecurity_Guidelines.PDF.
- 40.Graves S.R., Dwyer B., McColl D., McDade J. Flinders Island spotted fever: A newly recognised endemic focus of tick typhus in Bass Strait: Part 2. Serological investigations. Med. J. Aust. 1991;154:99–104. doi: 10.5694/j.1326-5377.1991.tb120994.x. [DOI] [PubMed] [Google Scholar]
- 41.Vilcins I.-M.E., Old J.M., Deane E.M. Molecular detection of Rickettsia, Coxiella and Rickettsiella DNA in three native Australian tick species. Exp. Appl. Acarol. 2009;49:229–242. doi: 10.1007/s10493-009-9260-4. [DOI] [PubMed] [Google Scholar]
- 42.Dyer J.R., Einsiedel L., Ferguson P.E., Lee A.S., Gordon D.L., Unsworth N.B., Graves S.R. A new focus of Rickettsia honei spotted fever in South Australia. Med. J. Aust. 2005;182:231–234. doi: 10.5694/j.1326-5377.2005.tb06673.x. [DOI] [PubMed] [Google Scholar]
- 43.Dwyer B.W., Graves S.R., Yung A.P., Doherty R.R., McDonald M.I., McDonald J.K. Spotted fever in East Gippsland, Victoria: A previously unrecognised focus of rickettsial infection. Med. J. Aust. 1991;154:121–125. doi: 10.5694/j.1326-5377.1991.tb120998.x. [DOI] [PubMed] [Google Scholar]
- 44.Barrs V., Beatty J., Wilson B., Evans N., Gowan R., Baral R., Lingard A., Perkovic G., Hawley J. Lappin Prevalence of Bartonella species, Rickettsia felis, haemoplasmas and the Ehrlichia group in the blood of cats and fleas in eastern Australia. Aust. Vet. J. 2010;88:160–165. doi: 10.1111/j.1751-0813.2010.00569.x. [DOI] [PubMed] [Google Scholar]
- 45.Schloderer D., Owen H., Clark P., Stenos J., Fenwick S.G. Rickettsia felis in fleas, Western Australia. Emerg. Infect. Dis. 2006;12:841–843. doi: 10.3201/eid1205.051458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paris D.H., Dumler J.S. State of the art of diagnosis of rickettsial diseases: The use of blood specimens for diagnosis of scrub typhus, spotted fever group rickettsiosis, and murine typhus. Curr. Opin. Infect. Dis. 2016;29:433–439. doi: 10.1097/QCO.0000000000000298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stenos J., Unsworth N.B., Graves S.R. A Highly Sensitive and Specific Real-Time Pcr Assay for the Detection of Spotted Fever and Typhus Group Rickettsiae. Am. J. Trop. Med. Hyg. 2005;73:1083–1085. doi: 10.4269/ajtmh.2005.73.1083. [DOI] [PubMed] [Google Scholar]
- 48.Parola P., Paddock C.D., Raoult D. Tick-Borne Rickettsioses around the World: Emerging Diseases Challenging Old Concepts. Clin. Microbiol. Rev. 2005;18:719. doi: 10.1128/CMR.18.4.719-756.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kaplowitz L.G., Lange J.V., Fischer J.J., Walker D.H. Correlation of Rickettsial Titers, Circulating Endotoxin, and Clinical Features in Rocky Mountain Spotted Fever. Arch. Intern. Med. 1983;143:1149–1151. doi: 10.1001/archinte.1983.00350060073012. [DOI] [PubMed] [Google Scholar]
- 50.Gal S., Fidler C., Lo Y., Taylor M., Han C., Moore J., Harris A., Wainscoat J. Quantitation of circulating DNA in the serum of breast cancer patients by real-time PCR. Br. J. Cancer. 2004;90:1211–1215. doi: 10.1038/sj.bjc.6601609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kato C., Chung I., Paddock C. Estimation of Rickettsia rickettsii copy number in the blood of patients with Rocky Mountain spotted fever suggests cyclic diurnal trends in bacteraemia. Clin. Microbiol. Infect. 2016;22:394–396. doi: 10.1016/j.cmi.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 52.Willis G., Lodo K., McGregor A., Howes F., Williams S., Veitch M. New and old hotspots for rickettsial spotted fever acquired in Tasmania, 2012–2017. Aust. N. Z. J. Public Health. 2019;43:389–394. doi: 10.1111/1753-6405.12918. [DOI] [PubMed] [Google Scholar]
- 53.Reháçek J. Ecological relationships between ticks and rickettsiae. Eur. J. Epidemiol. 1989;5:407–413. doi: 10.1007/BF00140130. [DOI] [PubMed] [Google Scholar]
- 54.O’Connor L.F., Kelly H.A., Lubich J.M., Lindsey R.J., McComish M.J. A cluster of murine typhus cases in Western Australia. Med. J. Aust. 1996;165:24–26. doi: 10.5694/j.1326-5377.1996.tb124812.x. [DOI] [PubMed] [Google Scholar]
- 55.Kenyon R.H., Kishimoto R.A., Hall W.C. Exposure of guinea pigs to Rickettsia rickettsii by aerosol, nasal, conjunctival, gastric, and subcutaneous routes and protection afforded by an experimental vaccine. Infect. Immun. 1979;25:580–582. doi: 10.1128/iai.25.2.580-582.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Saslaw S., Carlisle H.N. Aerosol infection of monkeys with Rickettsia rickettsii. Bacteriol. Rev. 1966;30:636–645. doi: 10.1128/br.30.3.636-645.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wolf G.L., Cole C.R., Carlisle H.N., Saslaw S. The pathogenesis of Rocky Mountain spotted fever in monkeys, infected by inhalation. Arch. Pathol. 1967;84:486–494. [PubMed] [Google Scholar]
- 58.Calia F.M., Bartelloni P.J., McKinney R.W. Rocky Mountain Spotted Fever: Laboratory infection in a vaccinated individual. JAMA. 1970;211:2012–2014. doi: 10.1001/jama.1970.03170120056014. [DOI] [PubMed] [Google Scholar]
- 59.Johnson J.E., Kadull P.J. Rocky Mountain Spotted Fever Acquired in a Laboratory. N. Engl. J. Med. 1967;277:842–847. doi: 10.1056/NEJM196710192771603. [DOI] [PubMed] [Google Scholar]
- 60.Oster C.N., Burke D.S., Kenyon R.H., Ascher M.S., Harber P., Pedersen C.E. Laboratory-Acquired Rocky Mountain Spotted Fever: The hazard of aerosol transmission. N. Engl. J. Med. 1977;297:859–863. doi: 10.1056/NEJM197710202971604. [DOI] [PubMed] [Google Scholar]
- 61.Saint E.G., Drummond A.F., Thorburn I.O. Murine typhus in Western Australia. Med. J. Aust. 1954;2:731–737. doi: 10.5694/j.1326-5377.1954.tb66921.x. [DOI] [PubMed] [Google Scholar]
- 62.La Scola B., Raoult D. Laboratory diagnosis of rickettsioses: Current approaches to diagnosis of old and new rickettsial diseases. J.Clin. Microbio. 1997;35:2715–2727. doi: 10.1128/jcm.35.11.2715-2727.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hechemy K.E., Raoult D., Fox J., Han Y., Elliott L.B., Rawlings J. Cross-reaction of immune sera from patients with rickettsial diseases. J. Med. Microbiol. 1989;29:199–202. doi: 10.1099/00222615-29-3-199. [DOI] [PubMed] [Google Scholar]
- 64.La Scola B., Rydkina L., Ndihokubwayo J.-B., Vene S., Raoult D. Serological Differentiation of Murine Typhus and Epidemic Typhus Using Cross-Adsorption and Western Blotting. Clin. Diagn. Lab. Immunol. 2000;7:612–616. doi: 10.1128/CDLI.7.4.612-616.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Teoh Y.T., Hii S.F., Graves S., Rees R., Stenos J., Traub R.J. Evidence of exposure to Rickettsia felis in Australian patients. One Health. 2016;2:95–98. doi: 10.1016/j.onehlt.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Delisle J., Moncayo A.C., Bouyer D.H., Mendell N.L., Bloch K.C., Stull-Lane A. Human Infections by Multiple Spotted Fever Group Rickettsiae in Tennessee. Am. J. Trop. Med. Hyg. 2016;94:1212–1217. doi: 10.4269/ajtmh.15-0372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Baird R.W., Lloyd M., Stenos J., Ross B.C., Stewart R.S., Dwyer B. Characterization and comparison of Australian human spotted fever group rickettsiae. J. Clin. Microbiol. 1992;30:2896–2902. doi: 10.1128/jcm.30.11.2896-2902.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ricketts H.T. A micro-organism which apparently has a specific relationship to Rocky Mountain spotted fever: A preliminary report. J. Am. Med. Assoc. 1909;52:379–380. doi: 10.1001/jama.1909.25420310039002. [DOI] [Google Scholar]
- 69.Abdad M.Y., Abdallah R.A., Karkouri K.E., Beye M., Stenos J., Owen H., Fournier P.-E. Rickettsia gravesii sp. nov.: A novel spotted fever group rickettsia in Western Australian Amblyomma triguttatum triguttatum ticks. Int. J. Syst. Evol. Microbiol. 2017;67:3156–3161. doi: 10.1099/ijsem.0.001865. [DOI] [PubMed] [Google Scholar]
- 70.Stenos J., Roux V., Walker D., Raoult D. Rickettsia honei sp. nov., the aetiological agent of Flinders Island spotted fever in Australia. Int. J. Syst. Bacteriol. 1998;48:1399–1404. doi: 10.1099/00207713-48-4-1399. [DOI] [PubMed] [Google Scholar]
- 71.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Harris P.A., Taylor R., Minor B.L., Elliott V., Fernandez M., O’Neal L., McLeod L., Delacqua G., Delacqua F., Kirby J., et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dhand N.K., Khatkar M.S. Statulator: An Online Statistical Calculator. Sample Size Calculator for Estimating a Single Propor-tion. [(accessed on 7 May 2019)]; Available online: http://statulator.com/SampleSize/ss1P.html.
- 74.Sellens E., Bosward K.L., Norris J.M., Wood N., Heller J., Graves S., Gidding H.F. Coxiella burnetii seroprevalence in unvaccinated veterinary workers in Australia: Evidence to support Q fever vaccination. Zoonoses Public Health. 2020;67:79–88. doi: 10.1111/zph.12658. [DOI] [PubMed] [Google Scholar]
- 75.Mediannikov O., Fenollar F., Socolovschi C., Diatta G., Bassene H., Molez J.-F., Sokhna C., Trape J.-F., Raoult D. Coxiella burnetii in Humans and Ticks in Rural Senegal. PLoS Negl. Trop. Dis. 2010;4:e654. doi: 10.1371/journal.pntd.0000654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.R Core Team R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. [(accessed on 18 December 2018)]; Available online: http://www.R-project.org/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data available on request due to privacy restrictions.