Abstract
Simple Summary
Colorectal cancer (CRC) is the second cause of cancer death worldwide. Irinotecan is a drug widely used in CRC treatment. Unfortunately, colonic bacteria decompose the metabolite of irinotecan back to the active form of the drug resulting in severe side-effects of the treatment, such as diarrhea. The present work demonstrated that new apple pectin (PC) enhanced cytostatic action of irinotecan and, at the same time, reduced the activity of bacterial enzymes responsible for the appearance of side-effects in patients. Thus, novel pectin PC constitutes a promising candidate for an adjunct to irinotecan therapy that might alleviate its side-effects, increasing its therapeutic efficacy.
Abstract
Colorectal cancer (CRC) is the second cause of cancer death worldwide. The composition and enzymatic activity of colonic microbiota can significantly affect the effectiveness of CRC chemotherapy. Irinotecan is a drug widely used to treat colon cancer. However, the transformation of a drug-glucuronide (SN-38G) back to its active form (SN-38) by bacterial β-glucuronidase (GUS) constitutes the primary reason for the observed intestinal toxicity of irinotecan. It was demonstrated that novel enzymatically extracted apple pectin (PC) might be a promising candidate for an adjunct to irinotecan therapy. PC itself reduced the viability of HCT 116 and Caco-2 colorectal cancer cells, induced apoptosis, and increased intracellular reactive oxygen species production. Moreover, PC enhanced the cytotoxic and proapoptotic effect of irinotecan (at concentrations below its IC50), i.e., synergistic effect was recorded. Additionally, PC exhibited potent anti-inflammatory properties and prevented adhesion of prototype adherent-invasive E. coli (AIEC) LF82 strain and laboratory K-12C600 strain to colon cancer cells. PC was also identified to be an effective inhibitor of bacterial GUS activity. Altogether, novel apple pectin was identified as a promising candidate for a supplement to irinotecan therapy that might alleviate its side-effects via inhibition of bacterial GUS and thus increasing its therapeutic efficacy.
Keywords: colon cancer, pectin, irinotecan, apoptosis, inflammation, E. coli, bacterial β-glucuronidase, side-effects alleviation
1. Introduction
Colorectal cancer (CRC) takes the third position among the most frequently occurring cancers worldwide [1]. As reported by International Agency for Cancer Research of the World Health Organization (WHO) in 2020 more than 1.9 million new CRC cases were diagnosed and over 900,000 deaths were recorded [1]. In the great majority, CRC appears as a sporadic disease, typically diagnosed in patients over 50 and usually linked to environmental factors, such as western-type diet rich in red meat, fat, and sugar [2]. About 10% of CRC cases develop due to inherited syndromes, such as familial adenomatous polyposis and Lynch syndrome [2]. Moreover, the higher risk of CRC has been observed in patients with inflammatory bowel disease, such as ulcerative colitis and Crohn’s disease [3]. Local inflammation may modulate the pathogenesis of CRC, mostly via the complex network of inflammation mediators, such as cytokines, produced both by cancer cells themselves and by various types of cells constituting tumor microenvironment [4]. Additionally, the progression of CRC can be influenced by colonic microbiota [5,6] that is altered in cancer patients as compared to the healthy subjects [7,8]. The microbiota was also shown to modulate the response of tumor cells to chemotherapy [9,10].
The treatment options of CRC depend on the stage of disease. For locally advanced colon or rectal tumors concomitant combination of surgery and chemotherapy is recommended, while in metastatic CRC, chemotherapy appears to be preferable [11]. Irinotecan is a derivative of an alkaloid, camptothecin. Irinotecan hydrolysis by patients’ carboxylesterases yields its active form, SN-38, an inhibitor of topoisomerase I [12]. This drug is a common component of cytotoxic combinations recommended as a treatment for CRC patients, such as FOLFIRI (fluorouracil, leucovorin, and irinotecan) or FOLFOXIRI (fluorouracil, leucovorin, oxaliplatin, and irinotecan) [13,14]. Common side-effects of irinotecan include diarrhea, nausea, and vomiting [15,16]. SN-38 is metabolized via glucuronidation in the liver to irinotecan glucuronide (SN-38G) that enters the small intestine via biliary excretion [17]. Unfortunately, bacteria in the colon produce β-glucuronidase (GUS) that decomposes SN-38G back to its active form (SN-38), which is toxic for intestinal epithelium [18], causing the adverse effects of chemotherapy.
Pectin constitutes a significant component of dietary fiber. This structural acidic heteropolysaccharide is a component of plant cell walls [19]. The basic structural skeleton of pectin is a linear polymer of galacturonic acid (GalUA). In native pectin molecule, some distinct structural regions are present. In rhamnogalacturonan I (RG I), the backbone consists of repeating dimers of GalUA and rhamnose, and is substituted with side chains composed of galactose and arabinose. Sidechains of rhamnogalacturonan II (RG II) contain atypical, rare monosaccharides, including L-fucose, apiose, and acids: aceric, glucuronic, ketodeoxyoctonic (KDO), and 3-deoxy-lyxo-2-heptulopyranosylaric (DHA). Structural differences may depend on the plant source of the polysaccharide. Commercially available pectins are usually prepared from citrus peels or apple pomace by hot acid extraction [20]. Pectins extracted using this method are, in comparison with the native molecule, depleted in RG I and RG II that are considered to be crucial for prebiotic, immunomodulatory, and anticancer potency of pectins [21,22]. Recently, Wikiera et al. [23] developed an effective method for enzymatic isolation of apple pectins using limited doses of endo-cellulase and endo-xylanase. This procedure protects native molecules, especially its neutral sugars that are not damaged during isolation [23]. Pectin studied in the present work (PC) was enzymatically extracted from apple pomace using endo-cellulase from filamentous fungus Trichoderma viride. Its detailed structure was previously described [23], and its biological properties were partially characterized [24].
In the present work, we studied the influence of enzymatically obtained pectin, PC, on colon cancer cells and compared its properties to commercially available modified citrus pectin, SolC. It was assumed that PC is going to exhibit intrinsic anticancer activity. Next, due to presumed anticancer properties of PC, the enhancement of the anticancer activity of irinotecan (i.e., synergistic effect) was expected when the drug would be applied together with PC. Additionally, considering the crucial role of colonic microbiota in causing irinotecan-induced diarrhea, we supposed that enzymatically obtained pectin might alleviate side-effects of irinotecan both via inhibition of bacterial GUS in the colon or providing an additional substrate for the enzyme. The results presented below confirmed all of the above hypotheses.
2. Materials and Methods
2.1. Chemicals
SN-38 (7-ethyl-10-hydroxy-camptothecin), an active metabolite of irinotecan, was from Sigma-Aldrich (Poznan, Poland). PectaSol-C (SolC) low molecular weight modified citrus pectin with a documented antitumor activity [25] was purchased from ecoNugenics (Santa Rosa, C, USA). Stock solutions of pectins were prepared at a concentration of 10 mg/mL in double-distilled water. About 50 mM stock solution of SN-38 was prepared in dimethyl sulfoxide (DMSO) and stored at −20 °C. Stock solutions were diluted in a culture medium just before the experiments.
2.2. Pectin Isolation
Macromolecular apple pectin was extracted from dried apple pomace using cellulase (endo-β-1,4-glucanase, EC 3.2.1.4) produced by filamentous fungus Trichoderma viride (Sigma-Aldrich, Poznan, Poland, Cat. No. C9422). Isolation was performed with 50 U enzyme per 1 g of pomace, at pH 5.0, in 40 °C, for 10 h, according to a method described by Wikiera et al. 2016 [23]. The detailed characteristics of the obtained pectin are presented in the previous works [23,24].
2.3. Cell Culture
The experiments were performed on the human colon cancer cell lines HCT-116 and Caco-2 (obtained from ATCC collection). The cells were cultivated in medium DMEM-F12 (PAA) supplemented with fetal bovine serum (10% FBS for HCT 116 and 20% for Caco-2; Eurx) and 1% antibiotics (10,000 μg/mL streptomycin and 10,000 units/mL penicillin; Sigma-Aldrich (Poznan, Poland), at 37 °C in a humidified atmosphere with 5% CO2, under standard conditions. In addition, the medium for Caco-2 cells contained non-essential amino acid solution (1×) (Sigma-Aldrich, Poznan, Poland). The medium was changed twice a week. Confluent cultures were passaged using 0.25% trypsin. All experimental procedures were carried out in the log-phase of cell growth.
2.4. Cell Viability Assay
SRB assay. The sulforhodamine B (SRB, Sigma-Aldrich, Poznan, Poland) assay was performed, as previously described [26], with modifications. Briefly, 15,000 cells were seeded in 96-well plates and allowed for a 24-h attachment period (at 37 °C). Then, the cells were treated with the studied pectins (0.05–0.5 mg/mL with or without 5 nM SN-38) for 48 h. Control wells only contained medium. The further procedure was carried out as previously described [27]. Cytotoxicity of DMSO to the cells was found to be negligible. All experiments were repeated three times.
MTT assay. Cells were seeded on 96-well plates in the concentration of 150,000 cells/mL. About 24 h later, the medium was removed, and a fresh medium containing tested pectins (0.05–0.5 mg/mL with or without 5 nM SN-38) was added. The control wells contained DMSO diluted in a medium. The plates were incubated for 48 h at 37 °C in a humidified atmosphere with 5% CO2. Then, the medium was removed, and cells were washed with physiological saline (1 × PBS; Sigma-Aldrich, Poznan, Poland). In the next step of the experiment MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) in the concentration of 0.5 mg/mL (diluted in RPMI 1640 without phenol red; Sigma-Aldrich, Poznan, Poland) was added to each well. The plates were incubated for at least 2 h yielding purple MTT formazan crystals in the wells. The incubation with MTT was followed by the dissolution of crystals in the mixture of acidic isopropanol (isopropanol:HCl, v/v 1:0.04). The absorbance of the obtained product was read at 570 nm using a microplate reader. Survival rate was expressed as the percentage of cell survival and calculated from the ratio (A570 of treated cells/A570 of control cells) × 100%. The experiments were repeated three times.
2.5. Isobolographic Analysis
By the CompuSyn software (ComboSyn Inc., Paramus, NJ, USA) according to the classic median-effect equation, as described by Chou and Martin, the combination index (CI) values were calculated [28].
| (1) |
where: (Dx)1 is the dose of drug 1 alone that inhibits a system by x%, (Dx)2 is the dose of drug 2 alone that inhibits a system by x%, and (D)1 + (D)2 are the doses of drug 1 and 2 in combination that also inhibit a system by x%. CI values below 1 represent synergism, CI values equal to 1 indicate additive effect (i.e., no interaction), and CI values above 1 point to antagonism.
2.6. Flow Cytometry Analysis
In order to study the cell cycle, apoptosis, and intracellular level of reactive oxygen species (ROS), flow cytometry was applied. In these studies, the cells in concentration 150,000 cells/mL were seeded onto 12-well plates 24 h before the experiment. Then, the medium was removed, and a fresh medium containing the compounds (0.2 mg/mL pectins with or without 5 nM SN-38) was added. The plates were incubated for 48 h at 37 °C in a humidified atmosphere with 5% CO2.
The apoptosis was investigated using an Annexin-V apoptosis assay (BioLegend, San Diego, CA, USA) and propidium iodide (PI) solution (100 μg/mL; Sigma-Aldrich, Poznan, Poland). The cells were collected and centrifuged for 3 min at 235× g. After supernatant removal, the cells were washed with PBS and centrifuged once again. In the next step, the pellet of cells was suspended in cold Annexin-V binding buffer and stained with FITC-labeled Annexin-V and PI in the dark for 20 min at 37 °C. After this time, the final volume of Annexin-V binding buffer was added to the samples.
In order to analyze the cell cycle, collected cells were centrifuged for 3 min at 235× g (room temperature). After supernatant removal the cells were fixed with hypotonic buffer containing PI 100 µg/mL in PBS; 5 mg/l of citric acid; 1:9 Triton-X solution; RNase 100 µg/mL in PBS. The samples were incubated for 20 min (room temperature) in the dark and then stored on ice till they were measured.
The level of ROS in the cells treated with studied compounds was quantified using 2′,7′-dichlorofluorescein diacetate (DCFH-DA, Sigma-Aldrich, Poznan, Poland), a cell-permeable fluorogenic probe. The experiments were performed after 72 h of incubation with given compounds. The cells were harvested and centrifuged, washed with PBS, and centrifuged again. The pellet was resuspended in a culture medium and a cell-permeable non-fluorescent probe 2′,7′-dichlorofluorescein diacetate (DCFH-DA, Sigma-Aldrich, Poznan, Poland) in a final concentration of 30 µM was added. The samples were incubated in darkness for 30 min at 37 °C and then stored on ice till they were measured. DCFH-DA is hydrolyzed by cellular esterases into its polar form DCFH. Due to the intracellular ROS and other peroxides DCFH undergoes oxidation and turns into highly a fluorescent form 2′,7′-dichlorofluorescein (DCF).
Cytometric analyses were performed immediately using an Aria III flow cytometer (Becton Dickinson, Franklin Lakes, NJ, USA) with the FITC configuration (488 nm excitation; emission: LP mirror 503, BP filter 530/30) or PE configuration (547 nm excitation; emission: 585 nm) and at least 10,000 cells were counted.
2.7. Caspase-3 Activation Assay
The activity of caspase-3 was analyzed using a commercially available kit (GenScript Biotech, Leiden, the Netherlands). Cells were seeded (800,000 cells/well) onto a 6-well plate in 2 mL of medium and incubated for 24 h at 37 °C. Then, the cells were treated with PC or SolC alone (at 0.2 mg/mL), and in combination with SN-38 (5 nM). After incubation with studied compounds for 48 h cells were scraped and centrifuged (2000× g, 5 min, 25 °C). After cell lysis, spectrophotometric detection (A405) of the chromophore p-nitroanilide (pNA) was used to measure caspase-3 activity. The relative increase of caspase-3 activity was determined by calculating the ratio of the absorbance of pNA in the studied sample (treated with the compound) to the control (with no compound). Experiments were performed in triplicate.
2.8. Enzyme-Linked Immunosorbent Assay (ELISA)
HCT 116 cells were seeded in 96-well plates in the concentration of 150,000 cells/mL. The colorectal cancer cells were treated with 5 μM of lipopolysaccharide (LPS; trinitrophenol-lipopolysaccharide from E. coli O111:B4, Sigma-Aldrich, Poznan, Poland) added at the time of seeding. A fresh medium containing the compounds (0.2 mg/mL) was added after 24 h. After incubation with the studied compounds for 48 h interleukin 6 (IL-6) and cyclooxygenase 2 (COX-2) in the cancer cell culture lysates were quantified using ELISA (Human COX-2 ELISA Kit; Sigma-Aldrich, Poznan, Poland; IL-6 Human ELISA Kit-ThermoFisher Scientific, Waltham, MA, USA). ELISA was performed according to the manufacturer’s instructions. Each plate test was repeated three times.
2.9. E. coli Strains
Tests were performed on two reference strains. A prototype adherent-invasive E. coli (AIEC) LF82 (O83: H1) strain, kindly provided by Dr. Arlette Darfeuille-Michaud, Université d’Auvergne, France, and laboratory E. coli K-12C600 strain. E. coli strains were routinely cultured overnight in Luria broth (LB) with shaking at 37 °C.
2.10. Adherence Assay
Overnight E. coli cultures in LB medium were harvested and suspended in PBS to the optical density 6 × 108 CFU/mL established spectrophotometrically at 600 nm. HCT 116 or Caco-2 cells were washed three times with pre-warmed PBS, and 200 µL of pectin solutions in PBS at concentrations 0.125, 0.25, and 0.5 mg/mL were added to the cells following 200 µL of E. coli suspensions. Cells untreated with pectins and infected with E. coli served as a positive control. Then the cells were incubated for two hours at 37 °C in a humid atmosphere with 5% CO2. At 2 h post-infection, cells were washed three times with PBS and lysed with 0.1% Triton X-100. Serial dilutions of bacterial lysates were plated onto nutrient agar and incubated overnight at 37 °C to count bacterial colonies (CFU). The assay was repeated three times in duplicate. The results are presented as the percentage of E. coli adhering to cells concerning negative control established to be 100%.
Wright-Giemsa staining. Intestinal epithelial cells were cultured on slides in the wells of a 24-well plate. After 2 h of E. coli adherence with the epithelial cells, the cells were washed three times and fixed with 4% formaldehyde for 10 min at room temperature. After washing off the formaldehyde, cells were stained with Wright-Giemsa for 30 min. The dye was rinsed off, and the slides were dried. Adhesion images were taken under a light microscope at 100× magnification.
2.11. E. coli Proliferation
The impact of apple pectins on E. coli proliferation was assessed by mixing 75 µL of E. coli suspensions in PBS at the optical density 6 × 108 CFU/mL obtained from overnight cultures in LB with the equal volumes of pectins solutions in PBS at concentrations 0.125, 0.25, and 0.5 mg/mL. According to the adherence assay, the plate was incubated for two hours at 37 °C in an atmosphere with 5% CO2. The proliferation of E. coli was measured spectrophotometrically at 600 nm and compared to the growth of E. coli at time zero established to be 100%.
2.12. β-Glucuronidase (GUS) Activity Assay
Overnight E. coli LF82 and K-12C600 cultures in 3 mL of tryptic soy broth (TSB) were supplemented with 0.3 µM 4-nitrophenyl β-D-glucuronide (PNPG; Sigma-Aldrich, Poznan, Poland) one hour before the end of the incubation to induce GUS synthesis. Then, the cultures were centrifuged (16,000× g; 10 min; 4 °C). Bacterial cell pellets were washed twice in cold 100 mM sodium phosphate buffer (pH 6.8), followed by suspension in 1 mL of cold phosphate buffer, and mixing with 0.1 mm silica glass beads. The samples were then beaten in BeadBugTM microtube homogenizer five times for 30 sec each, with 30-sec incubations on ice in between. The tubes were centrifuged for 10 min, 16,000× g at 4 °C, and bacterial extracts were collected and stored on ice. Bacterial extracts were prewarmed at 37 °C, and samples of 75 µL were mixed in microtitrate plate with prewarmed equal volumes of the 10 mM PNPG in phosphate buffer. The yellow 4-nitrophenol product was recorded in a spectrophotometer after 60 min of incubation at 37 °C at 405 nm. The 4-nitrophenol concentration was determined from a standard curve according to Aich et al. [29]. Protein concentrations in bacterial extracts were determined with a bicinchoninic acid kit (Pierce, Waltham, MA, USA). GUS activity was calculated as follows: 4-nitrophenol concentration/100 mg/mL protein × 60 min. The effect of pectins SolC and PC on E. coli GUS activity was assayed as described above. SolC and PC solutions in PBS at final concentrations of 0.25, 0.5, and 0.7 mg/mL were mixed with an appropriate amount of E. coli lysates and 10 mM PNPG in the wells of a 96-well plate and incubated at 37 °C for 18 h.
2.13. Statistical Analysis
All of the experiments were repeated three times. Data represent the mean ± standard deviation (SD) of at least three replications. The Student’s t-test was applied and p-values less than 0.05 were considered to achieve statistical significance.
3. Results
3.1. Anticancer Activity of Pectins
3.1.1. Cytotoxicity of Pectins
The influence of two pectins on colon cancer cell viability was assessed. Commercially available pectin PectaSol-C (SolC) was compared to PC that had been enzymatically extracted from apple pomace using endo-cellulase. SolC is derived from water-insoluble citrus pectin modified by pH/temperature treatment to increase its water solubility and anticancer properties [25].
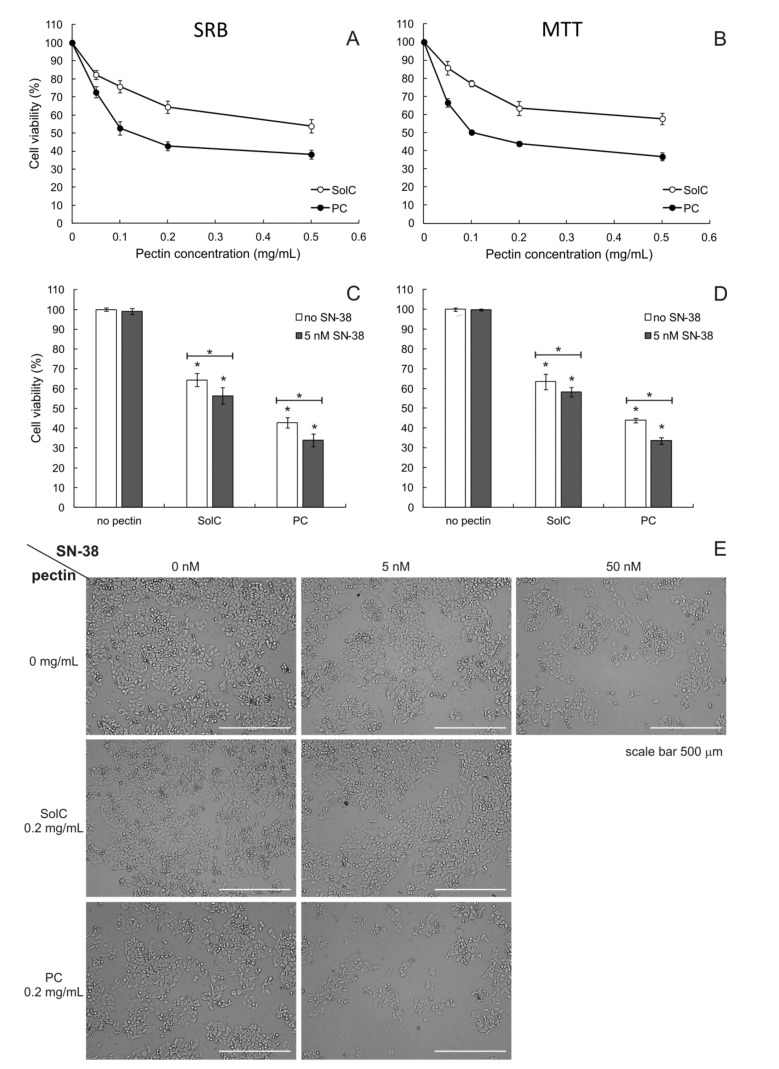
Both pectins were revealed to possess anticancer activity against human colorectal carcinoma HCT 116 cells (Figure 1A,B), as shown by the results of SRB as well as MTT assays. In both types of assays, PC exhibited significantly greater cytotoxic activity as compared to SolC (p < 0.05 for all concentrations tested). IC50 values obtained for PC were 0.098 ± 0.011 mg/mL and 0.103 ± 0.014 mg/mL for SRB and MTT assay, respectively. In the case of SolC, the SRB assay yielded an IC50 value of 0.590 ± 0.019 mg/mL, whereas the MTT assay gave IC50 equal to 0.640 ± 0.018 mg/mL. The appearance of HCT 116 cells cultures treated with 0.2 mg/mL of pectins is presented in Figure 1E.
Figure 1.
SRB (A) and MTT (B) cytotoxicity assay of pectins and 0.2 mg/mL pectins in combination with SN-38 (C,D) for SRB and MTT, respectively) in HCT 116 cells (incubation time 48 h). Light microscopy images (magnification 10×) of HCT 116 cells (E) treated with pectins (0.2 mg/mL) and/or 5 nM SN-38. The means of three experiments ± SD are presented (* p < 0.05). Statistical significance was checked between the studied probes and controls (no pectin) and between probes containing only pectin and pectin combined with SN-38. In panels A and B all measurements were significantly different from the control (not marked on the graph for the sake of clarity).
Cytotoxic activity of the studied pectins was also studied in human colorectal adenocarcinoma cells Caco-2 (Figure S1). The results of SRB and MTT cell viability assays revealed that PC was more toxic to Caco-2 cells than SolC, similarly as in the case of HCT 116 cells. IC50 values calculated for SolC were 0.440 ± 0.016 mg/mL (SRB) and 0.490 ± 0.015 mg/mL (MTT) that were slightly lower than that obtained in HCT 116 cells. On the other hand, IC50 values obtained for PC in Caco-2 cells, 0.210 ± 0.009 mg/mL for SRB and 0.270 ± 0.013 mg/mL for MTT, were almost twice higher than in HCT 116 cells. Therefore, it was concluded that the difference in cytotoxicity between SolC and PC was more pronounced in the case of HCT 116 cell line than in Caco-2.
3.1.2. Cytotoxicity of Pectins Combined with SN-38
Additionally, the anticancer activity of pectins was studied in the presence of SN-38, an active form of irinotecan—the drug commonly used to treat colon cancer. Its IC50 value in HCT 116 cell line was found to be 10.2 ± 0.8 nM (3.5 x 10−6 mg/mL). Figure 1E presents the appearance of cell cultures treated with 5 and 50 nM of SN-38 as well as with the mixtures of 0.2 mg/mL of pectin and 5 nM of SN-38. It can be noticed that in the case of PC:SN-38 combination the number of HCT 116 cells is reduced to a greater degree than in case of the treatment with SN-38 (at 5 nM) alone. Figure 1C,D present the results of the SRB and MTT assay, respectively. Cell viability was significantly reduced in the presence of both 0.2 mg/mL of SolC and PC. In addition, the combination of pectins with a low concentration of SN-38 reduced cell viability even more. The isobolographic analysis was employed to evaluate the possible synergy between the anticancer drug and pectins. Dose and effect data obtained from SRB assay for pure compounds and for two-component combinations (pectin:SN-38) were subjected to CompuSyn analysis (Table 1). The cytotoxic effects of PC and SN-38 were synergistic as demonstrated by the combination index (CI) values well below 1. On the other hand, no synergy was detected between SolC and SN-38, their effect was purely additive.
Table 1.
Combination of pectins with SN-38 against HCT 116 cell growth.
| Concentration (mg/mL) | Ratio | Combination Index (CI) | |
|---|---|---|---|
| SN-38 | SolC | ||
| 1.96 × 10−6 | 0.2 | 102,000:1 | 1000 |
| SN-38 | PC | ||
| 0.96 x 10−6 | 0.1 | 104,400:1 | 0.822 |
| 1.96 x 10−6 | 0.2 | 102,000:1 | 0.779 |
| 3.92 x 10−6 | 0.5 | 127,550:1 | 0.792 |
Dose and effect data were obtained from the sulforhodamine B (SRB) assay (mean values of three experiments) and analyzed by CompuSyn software (ComboSyn Inc., Paramus, NJ, USA). CI values were calculated by CompuSyn software. CI = 1 indicates additive effect, CI < 1—synergism, and CI > 1—antagonism.
3.2. Proapoptotic Activity of Pectins
3.2.1. Annexin V/PI Double Staining Assay
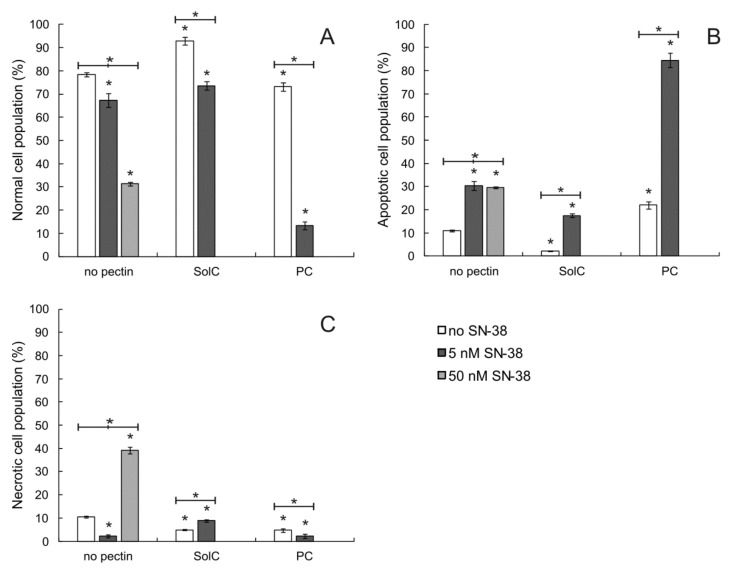
After confirming the anticancer properties of SolC and PC, it was checked whether the treatment of colon cancer cells with the studied pectins led to cellular death by apoptosis. Therefore, Annexin V/PI double staining assay was performed in HCT 116 cells. Typical dot plots obtained during the assay are presented in Figure S2. As shown in Figure 2, PC at 0.2 mg/mL slightly increased the number of apoptotic cells as compared to the control not treated by the pectin. Such an effect was not observed for SolC tested at the same concentration. The application of SN-38 also resulted in a significant increase of apoptotic cell population, both at 5 and 50 nM concentration. The drug when applied in the highest concentration also caused necrosis of HCT 116 cells. The apoptosis-inducing activity of pectins was also tested in combination with SN-38 at the concentration of 5 nM. It was observed (Figure 2B) that in the case of PC the number of cells undergoing apoptosis was much bigger as compared to the probe treated with SN-38 only (p < 0.05). On the other hand, the combined SolC:SN-38 treatment resulted in lower number of apoptotic cells as compared to the probe treated with SN-38 alone (p < 0.05). It was concluded that PC augmented the proapoptotic activity of SN-38.
Figure 2.
The proportion of normal (A), apoptotic (B), and necrotic (C) cell populations as recorded by Annexin-V apoptosis assay in HCT 116 cells treated with pectins (0.2 mg/mL) and/or SN-38 for 48 h. The means of three experiments ± SD are presented (* p < 0.05). Statistical significance was checked between the studied probes and controls (no pectin), and between probes containing only pectin and pectin combined with SN-38. Cells were recognized as viable (Annexin-V and PI negative), apoptotic (Annexin-V positive and PI negative), and necrotic (Annexin-V and PI positive) based on the measurement of cell-associated fluorescence of FITC-Annexin-V conjugate and PI.
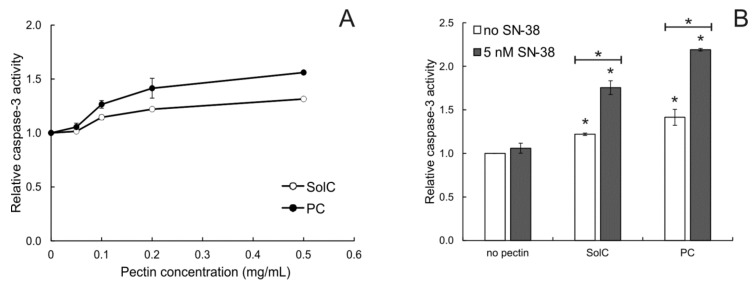
3.2.2. Caspase-3 Activation
Additionally, the ability of pectins to activate the apoptosis-involved protease, caspase-3, was investigated (Figure 3). Caspase-3 is an enzyme associated with the initiation of the apoptotic cascade. Its activation ultimately leads to the execution of the program of cell death. Both studied pectins activated this enzyme in concentrations higher than 0.1 mg/mL. The addition of 5 nM of SN-38 to the cells also treated with 0.2 mg/mL of pectin significantly enhanced the activity of caspase-3. SN-38 used alone at 5 nM did not, however, cause any activation of caspase-3. This experiment additionally confirmed the proapoptotic properties of the studied pectins and demonstrated that PC enhanced the ability of SN-38 (applied in concentration below IC50) to induce cell death.
Figure 3.
Relative caspase-3 activity in HCT 116 cells treated with pectins (A) and 0.2 mg/mL pectins in combination with SN-38. (B) for 48 h. The means of three experiments ± SD are presented (* p < 0.05). Statistical significance was checked between the studied probes and controls (no pectin), and between probes containing only pectin and pectin combined with SN-38. In panel A only the measurements for 0.05 mg/mL of SolC and PC were not significantly different from the control (not marked on the graph for the sake of clarity).
3.3. The Influence of Pectins on Cell Cycle
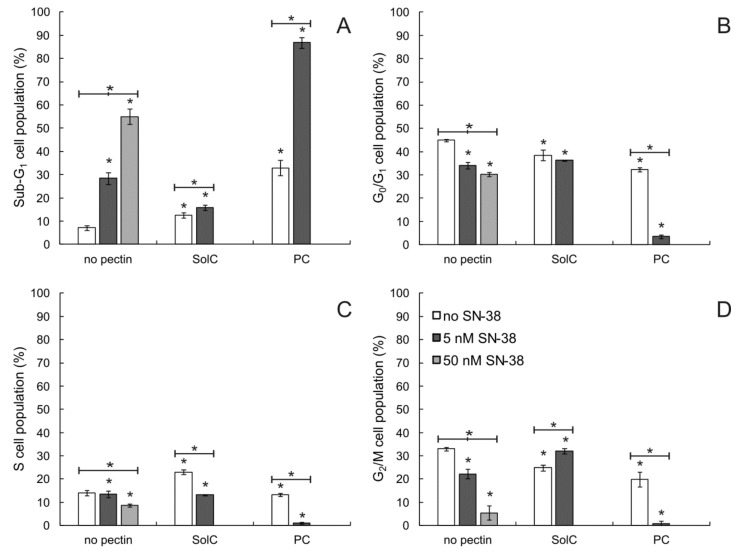
The influence of pectins on the cell cycle of HCT 116 cells was also tested (see Figure 4 and Figure S3 for the histograms). The cytometric evaluation indicated that both pectins at the concentration of 0.2 mg/mL elevated sub-G1 cellular fraction (dead cells), with PC being significantly more active than SolC. The number of dead cells was also elevated when HCT 116 cells were treated with SN-38, the higher concentration of the drug inevitably causing the more pronounced effect. The most interesting observation was made for the PC:SN-38 mixture. When the cells were treated by the two compounds in combination, the very strong increase of sub-G1 cellular fraction occurred that was accompanied by the reduction of the abundance of all other fractions. On this basis, it was concluded that PC enhanced the cytotoxic potential of SN-38.
Figure 4.
Cell cycle-dependent DNA content in HCT 116 cells treated with 0.2 mg/mL of pectins and /or SN-38 for 48 h. Sub-G1 population (A)—dead cells, G0/G1 (B)—mononuclear cells, S (C)—DNA replication, G2/M (D)—mitosis. Statistical significance was checked between the studied probes and controls (no pectin) as well as between probes containing only pectin and pectin combined with SN-38. * p < 0.05.
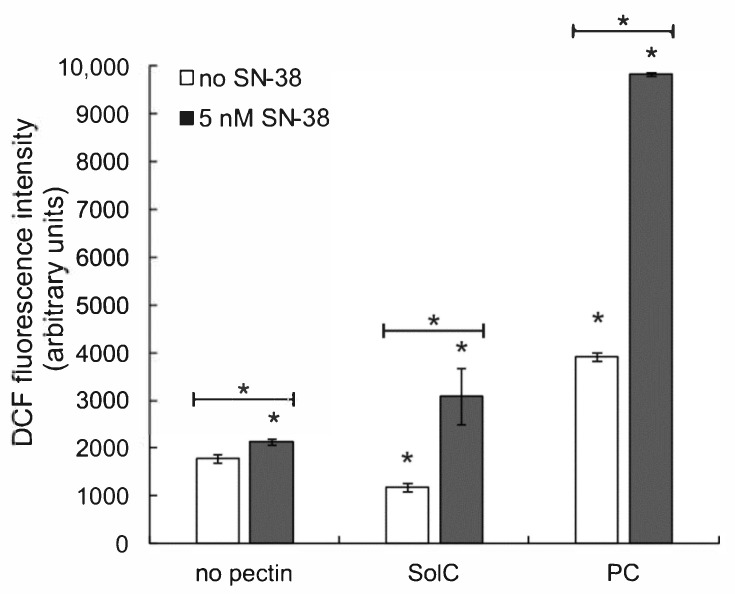
3.4. The Effect of Pectins on Reactive Oxygen Species (ROS) Production
The assay based on the detection of intracellular ROS by the fluorescent probe DCF was applied to quantify the generation of ROS in the presence of the studied pectins. As shown in Figure 5. the treatment of HCT 116 cells with SolC at 0.2 mg/mL concentration resulted in a slight decrease in ROS level, whereas PC applied at the same concentration elevated the production of ROS by cancer cells. SN-38 (at 5 nM) gently increased ROS level. When the anticancer drug was combined with pectins, the increase in ROS generation was observed, by more than 60% in the case of SolC and almost 4.5-fold in the case of PC. The conclusion was drawn that SolC itself possessed some antioxidative properties, in contrast to PC that was prooxidative. On the other hand, both pectins strengthened ROS production induced by SN-38.
Figure 5.
ROS level in HCT 116 cells treated with 0.2 mg/mL pectins and/or 5 nM SN-38 for 48 h. The means of three experiments ± SD are presented (* p < 0.05). Statistical significance was checked between the studied probes and controls (no pectin) as well as between probes containing only pectin and pectin combined with SN-38.
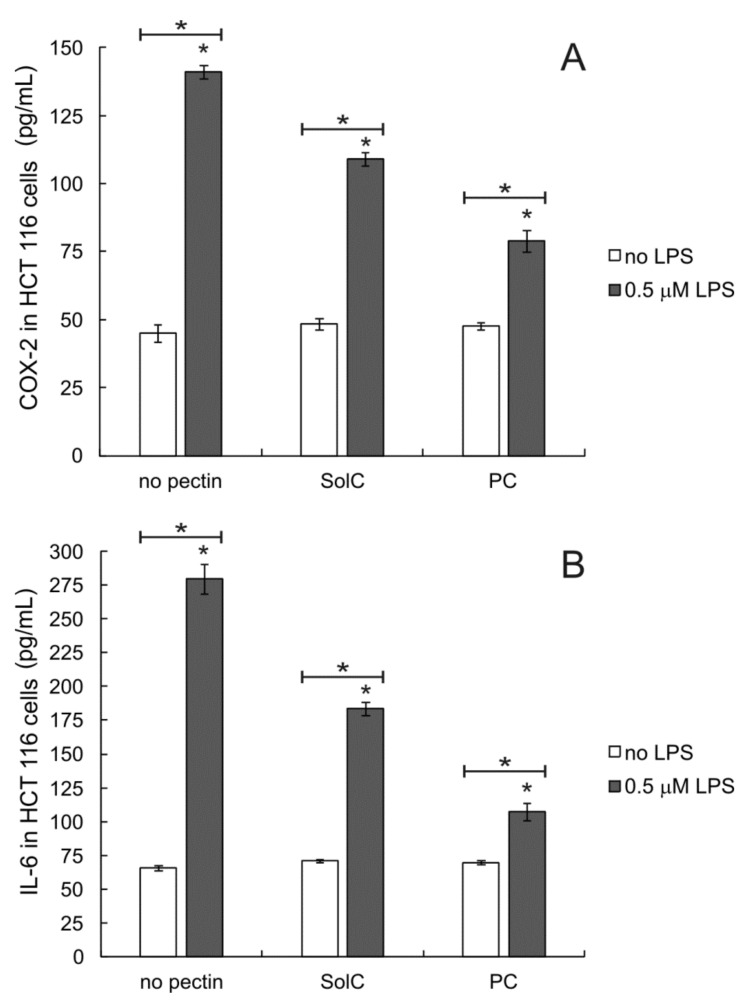
3.5. Anti-Inflammatory Activity of Pectins
To check whether the studied pectins could modify the cellular inflammatory response HCT 116 cells were pretreated by 5 μM of bacterial lipopolysaccharide (LPS, endotoxin) for 24 h before the experiment to induce inflammation. After the treatment with pectins the amounts of cyclooxygenase 2 (COX-2) and interleukin 6 (IL-6) were quantified in cell culture lysates. As presented in Figure 6 in not-stimulated cells pectins tested at 0.2 mg/mL had no influence on either COX-2 or IL-6 levels. As expected, the treatment of colon cancer cells by LPS induced inflammatory response resulting in the substantial increase of COX-2 and IL-6 produced by the cells (Figure 6A and Figure 6B, respectively). The addition of any of the studied pectins resulted in the reduction of LPS-induced levels of both inflammation markers. The effect of PC was more pronounced than that of SolC (statistical significance (p < 0.05) was obtained both in the case of COX-2 and IL-6). It was demonstrated that both studied pectins were able to modulate the inflammatory response of colon cancer cells.
Figure 6.
Amount of COX-2 (A) and IL-6 (B) in HCT 116 cells treated with 0.2 mg/mL pectins and/or 0.5 μM LPS. Cells were pretreated with LPS for 24 h and then incubated with pectins for 48 h. The means of three experiments ± SD are presented (* p < 0.05). Statistical significance was checked between the studied probes and controls (no pectin) as well as between probes containing only pectin and pectin combined with LPS.
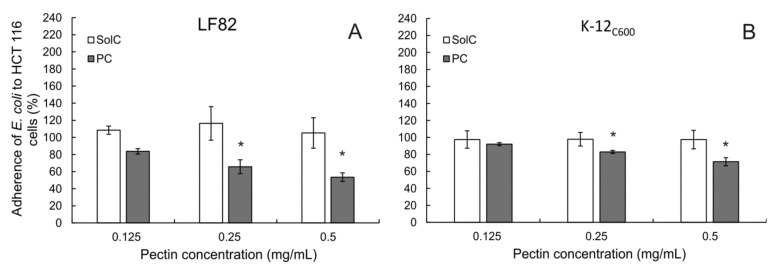
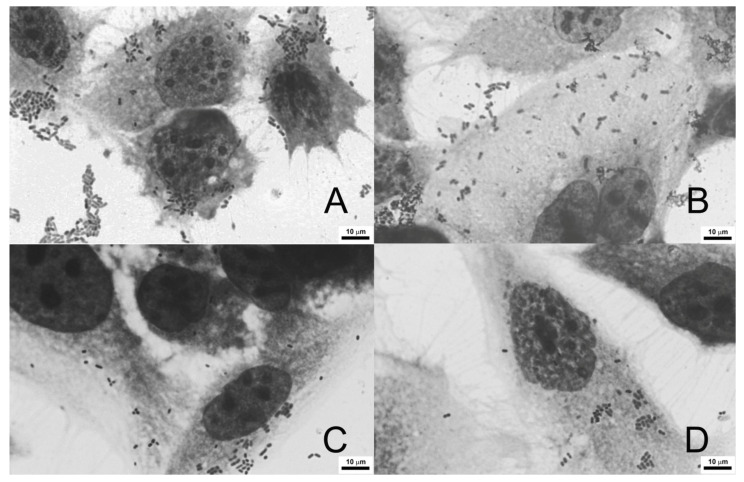
3.6. Adherence of E. coli to Colon Cancer Cells
Since colonic microbiota is known to affect colorectal cancer initiation and progression, adherence of bacteria E. coli to cancer cells in the presence of the studied pectins was monitored. Two bacterial strains were employed, a laboratory E. coli K-12C600 strain, and an adherent-invasive E. coli (AIEC) LF82 strain. The latter was isolated from a patient with Crohn’s disease. SolC did not influence the ability of either LF82 (Figure 7A) or K-12C600 (Figure 7B) strains to adhere to HCT 116 cells. On the other hand, PC in concentrations 0.25 mg/mL or higher significantly reduced the adherence of both E. coli strains to cancer cells. The observed effect seemed slightly stronger in AIEC E. coli than in the control laboratory strain. It was also confirmed that none of the studied pectins influenced cancer cell viability (Figure S5) and E. coli proliferation (Figure S6) under experimental conditions. The same experiment was performed in human colorectal adenocarcinoma cells Caco-2 (Figure S4), and it showed virtually the same results. Representative pictures of E. coli LF82 strain adhering to untreated Caco-2 cells and in the presence of PC at different concentrations are shown in Figure 8. It was therefore found that PC was able to reduce adherence of E. coli to colon cancer cells.
Figure 7.
E. coli LH82 (A) and K-12C600 strains (B) adherence to HCT 116 cells in the presence of pectins during 2 h of incubation. The means of three experiments ± SD are presented. Statistical significance (* p < 0.05) was checked between the studied probes and controls (no pectin) assumed to be 100%.
Figure 8.
Adherence of E. coli (LF82 strain) to Caco-2 cells. Representative pictures of bacteria adhering to untreated Caco-2 cells (A), and treated with PC at concentration of 0.125 mg/mL (B), 0.25 mg/mL (C), and 0.5 mg/mL, (D). Wright-Giemsa stain, 100× magnification.
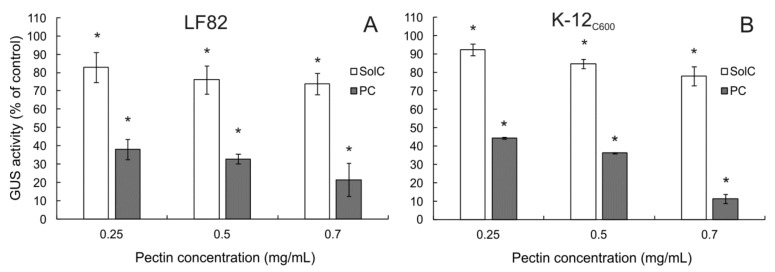
3.7. The Effect of Pectins on β-Glucuronidase (GUS) Activity
Colonic bacteria may influence intestinal toxicity of irinotecan by enzymatic decomposition of SN-38G back to highly cytotoxic SN-38. The influence of pectins on the activity of β-glucuronidase produced by E. coli strains was tested. As shown in Figure 9, both studied pectins reduced GUS activity in a concentration-dependent manner. PC exhibited much stronger enzyme-inhibiting potency as compared to SolC. It was concluded that pectins might potentially alleviate irinotecan-induced diarrhea by reducing enzymatic transformation of the drug in the colon.
Figure 9.
The influence of pectins on GUS activity in E. coli LH82 (A) and K-12C600 lysates (B). Pectin solution were mixed with 0.5 U of E. coli GUS and incubated for 18 h. The means of three experiments ± SD are presented (* p < 0.05). Statistical significance was checked between the studied probes and controls (no pectin) assumed to be 100%.
4. Discussion
In the present work, it was demonstrated that both studied pectins, PC and SolC, significantly reduced the viability of two colon cancer cell lines, HCT 116 and Caco-2. In both types of cells, enzymatically isolated apple pectin (PC) exhibited greater cytotoxicity in comparison to commercially available modified citrus pectin (SolC). Previous studies on PC revealed its ability to reduce proliferation, cell adhesion, and invasion of human adenocarcinoma HT-29 and melanoma B16F10 cells [24]. Pectin treatment was much more destructive to colon cancer cells than to melanoma cells. At the same time, it was shown that PC (tested in concentrations up to 1 mg/mL) exerted virtually no effect on proliferation and adhesion of normal mouse fibroblasts L929 [24]. Anticancer activity of various pectins has been already recognized for several years (see [21,30] for a review). Pectins isolated from ginseng [31] and potato [32] were demonstrated to exert an antiproliferative effect on colon cancer cells (HT-29). Interestingly, it seems that anticancer activity of commercial pectin preparations was limited while enzymatically modified pectins, especially the ones rich in RG I regions, significantly reduced the proliferation of various cancer cell lines [33,34].
Moreover, PC but not SolC was demonstrated to act synergistically with SN-38 in reducing colon cancer cells viability. Pectins have not been reported to potentiate the activity of this drug before. In contrast, the augmentation of the antiproliferative effect of irinotecan toward HCT 116 cells was observed in case of flavopiridol [35]. On the other hand, the synergistic anticancer effect of modified citrus pectin preparation and paclitaxel [36], as well as doxorubicin [37] was recorded in ovarian and prostate cancer cell lines, respectively.
To understand better the mechanism of anticancer properties of pectins, their ability to induce apoptosis in colon cancer cells was studied. It was shown that PC but not SolC significantly increased the size of the apoptotic cell population. Both pectins activated caspase-3, an effector caspase in the apoptotic pathway. Cell cycle analysis demonstrated both pectins elevated sub-G1 cellular fraction that is composed of cellular debris as well as late apoptotic and necrotic cells. SN-38, tested at low concentrations, also induced apoptosis in HCT 116 cells and raised the abundance of sub-G1 cellular fraction but it did not activate caspase-3. The most interesting findings came from the analysis of HCT 116 cells treated with PC and SN-38 simultaneously. Strong increases of apoptotic cell population, as well as sub-G1 cellular fraction, suggested that PC augmented proapoptotic and cytostatic properties of this anticancer drug. Proapoptotic activity of pectins have been already demonstrated for many types of pectin preparations in a variety of experimental settings, e.g., in ovarian cancer (SolC [36]), prostate cancer (fractionated pectin powder [38], SolC [39]) as well as in colon cancer (pectic oligosaccharides [40], sweet potato [41], ginger [31], and beetroot pectin [33]). Modified citrus pectin was recorded to increase caspase-3 activity and to modify the cell cycle of ovarian cancer cells in a similar way as observed for apple pectin PC in the present work [36]. In the same study, the synergy of pectin and paclitaxel in apoptosis induction was observed. However, the same pectin preparation induced G2/M phase arrest, activation of caspase-3, and the cleavage of poly (ADP-ribose) polymerase (PARP) in urinary bladder cancer cells [42]. Since dietary pectins are not digested before they reach the distal portion of the gastrointestinal tract, they cannot reach circulation. Pectins are known to bind strongly to the mucous layer of the intestine, and in this way, they can modulate the function of epithelial cells. Avivi-Green et al. [43] fed rats in which carcinogenesis had been chemically induced a high-pectin diet and observed an increased apoptotic index of their colon crypt cells that was likely to result in reduced tumor volumes in comparison with rats fed with a standard diet. It has been presumed that proapoptotic, and more generally, anticancer activity of pectins was related to their interaction with galectin-3 (Gal-3). Gal-3 is a lectin that specifically binds β-galactosides. It is present in a variety of cells and often over-expressed in cancer (see [44,45] for a review). Gal-3 specifically binds many intra- and extracellular proteins mediating numerous biological processes including the ones necessary for cancer growth, transformation, invasion, and metastasis. The studies trying to identify the structural features of pectin needed for proapoptotic activity pointed to the importance of an ester-based cross-link within the pectin molecule [38] as well as to the high content RG-I regions (rich in neutral sugars) within the pectin preparation [33].
The proapoptotic properties of chemical compounds are often associated with their ability to increase the level of reactive oxygen species (ROS) within cells. This possibility was tested in the case of the studied pectins. It was found that PC but not SolC (both at 0.2 mg/mL) increased ROS content in colon cancer cells. SN-38, when applied alone at the concentration of 5 nM increased ROS level only slightly. The SN-38-induced increase in ROS content was pretty elevated when the drug was combined with SolC and considerably raised in the case of the PC:SN-38 combination. Enzymatically isolated pectin, PC, has been previously demonstrated to effectively scavenge free radicals, and its antioxidative potency was more significant as compared to commercial apple pectin [24]. Antioxidative activity of various types of pectins has been widely reported (see [46] for a review). However, it should be taken into consideration that the laboratory-detected ability of a compound to scavenge free radicals does not have to translate into its ROS-mitigating behavior in the cellular environment. Modified citrus pectin has been recently demonstrated to increase ROS production in prostate cancer cells that contributed to their increased radiosensitivity in the presence of pectin [47]. Both citrus and apple pectins were observed to increase ROS release in breast cancer cells and to induce apoptosis via the mitochondrial pathway [48].
Local inflammation in the colon has been associated with a higher risk of CRC development [5]. Therefore, it was decided to investigate the ability of the studied pectins to modulate the inflammatory response of colon cancer cells. Since HCT 116 cells express Toll-Like Receptor 4 (TLR4) [49,50], LPS produced by E. coli was used to induce inflammatory processes in these cells. Interaction of TLR4 with LPS switches on the signaling pathway in which many components (including nuclear factor NFκB) are engaged and that triggers the expression of pro-inflammatory cytokines (e.g., IL-6) and enzymes, like COX-2 [51,52]. The results showed that LPS induced a significant increase in both IL-6 and COX-2 levels produced by HCT 116 cells. In the presence of pectins the levels of both proteins significantly decreased. The immunomodulatory effect was, however, much more pronounced in the case of PC than SolC. The interplay of pectins with various components of LPS/TLR4-induced pathways has already been observed. Citrus pectin caused the decrease of expression of inducible nitric oxide synthase (iNOS) and COX-2 in LPS-activated macrophages [53]. An apple oligogalactan suppressed both the expression and activity of COX-2 in LPS-stimulated colon carcinoma cells [54]. In the same experimental setting modified apple polysaccharides significantly decreased LPS-induced expression of TLR4, COX-2, matrix metallopeptidases (MMP) 2 and 9, iNOS, as well as prostaglandin E2 [55]. Oral application of pectins was also demonstrated to alleviate LPS-induced shock in mice [56] and to decrease the expression of pro-inflammatory markers in model mouse colitis [57]. The direct interaction of pectins with TLR4, thus competing with LPS binding, was proposed to constitute the molecular basis for the modulation of the inflammatory process by pectins [55,58]. Interestingly, the sugar profile and structure of RG II region present in PC molecule (but not in SolC) highly resemble the structure of O-antigen of LPS [59,60].
Pectins are characterized by high adhesion to the intestinal mucous layer. They can both affect the function of epithelial cells and form the protective barrier against colonization by opportunistic microflora [61]. Additionally, they form a favorable environment for the normal microbiome and constitute the source of nutrients for bacteria populating the colon [62]. The disruption of gut microbiome equilibrium, called dysbiosis, often precedes the development of certain pathological conditions, from mild as irritable bowel syndrome to severe such as CRC. Colonic microbiota of CRC patients has been shown to differ from healthy individuals colonic flora [8,9]. Therefore, the impact of PC and SolC on the adherence of E. coli to colorectal cancer cells was studied. Two bacterial strains have been applied, laboratory K-12C600 strain, and adherent-invasive E. coli (AIEC) LF82 strain, isolated from a Crohn’s disease patient. SolC did not change the adherence of E. coli to HCT 116 and Caco-2 cells, whereas PC significantly diminished the adherence of bacteria to colon cancer cells. Moreover, the inhibitory action of PC seemed to be stronger in AIEC E. coli than in laboratory strain. The inhibitory effect of pectic oligosaccharides (POS) on the adhesion of pathogenic bacterial strains has been demonstrated in numerous studies. In human colon adenocarcinoma epithelial cells HT-29 POS from citrus significantly reduced the adherence of Vibrio cholerae [63], several enteropathogenic as well as verotoxigenic E. coli strains [64], and Shiga-toxin-producing E. coli O157:H7 [65]. Although orange peel POS did not affect Campylobacter jejuni adhesion, they reduced its invasion into intestinal epithelial cells Caco-2 [66]. In the study on POS produced from apple pomace, Wilkowska et al. [67] presented evidence for their inhibitory effect on adhesion of pathogenic strains of E. coli, Listeria monocytogenes, and Salmonella typhimurium to Caco- 2 cells. In contrast, the adhesion of probiotic bacterial strains to the intestine epithelium was increased in the presence of pectins. Similarly, pectin-like oligosaccharides from Panax ginseng roots was shown to reduce adhesion of Helicobacter pylori Actinobacillus actinomycetemcomitans, Propionibacterium acnes, and Staphylococcus aureus to human gastric adenocarcinoma cells with no inhibitory effects against non-pathogenic Lactobacillus acidophilus, E. coli, and Staphylococcus epidermidis [68]. These studies pointed to the beneficial effects of pectins in maintaining healthy microbiota.
The composition and enzymatic activity of colonic microbiota can significantly affect the effectiveness of chemotherapy [10,11]. On the other hand, chemotherapeutic drugs can influence intestinal microbiota [69]. Decomposition of a drug-glucuronide back to an active form of the drug by bacterial β-glucuronidase constitutes the major reason for the observed intestinal toxicity of irinotecan [18] but also other xenobiotics [70]. The application of GUS inhibitors as an adjuvant to irinotecan therapy has been proposed and demonstrated to be effective in alleviating the drug-induced gut damage and diarrhea [71,72]. For this reason, it was decided to investigate the effect of the studied pectins on the activity of GUS produced by two E. coli strains, laboratory strain and the one isolated of Crohn’s disease patient. Both SolC and PC were demonstrated to inhibit GUS activity. However, the reduction caused by PC was much stronger as compared to SolC. The analysis of previous studies dealing with the influence of pectins on bacterial GUS revealed lots of inconsistencies. Depending on the type of pectin and experimental setting pectins were reported to increase [73,74], to have no effect [75,76,77], or to reduce GUS activity [78,79,80,81]. Based on the results obtained in the present study, it was concluded that PC strongly inhibited the enzymatic activity of E. coli GUS and might therefore reduce the backward transformation of SN-38G to SN-38.
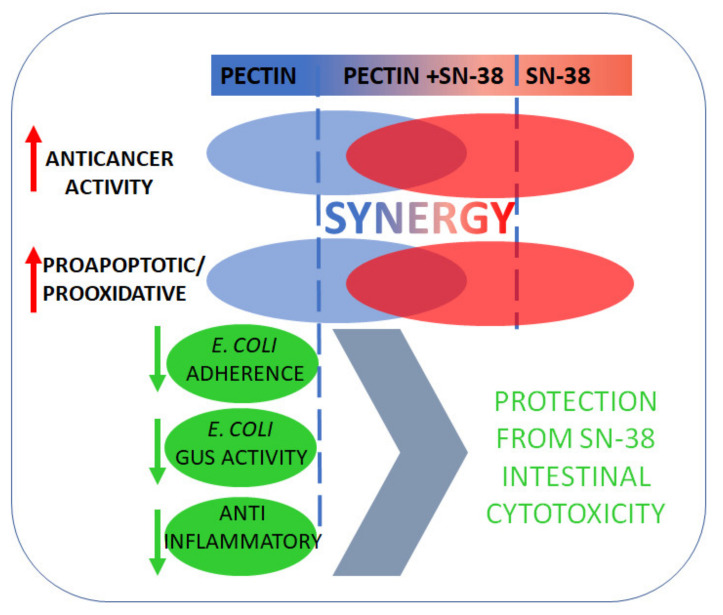
5. Conclusions
The novel pectin, PC, obtained by enzymatic extraction of apple pomace, demonstrated to possess superior anticancer activity as compared to the modified citrus pectin, SolC. The key findings of the present study are summarized in Figure 10. PC reduced colon cancer cell viability, induced apoptosis, and increased intracellular ROS production. Moreover, the enhancement of the cytotoxic and proapoptotic effects of low concentrations of irinotecan was observed in the presence of PC. Additionally, novel apple pectin exhibited potent anti-inflammatory properties, prevented adhesion of E. coli to colon cancer cells, as well as inhibited the activity of bacterial GUS. With the reservation that the conclusions are based on the in vitro study only, it was demonstrated that novel pectin might be a promising candidate for an adjunct to irinotecan therapy that might alleviate its side effects and thus increase its therapeutic efficacy.
Figure 10.
Schematic representation of activities of novel apple pectin in colon cancer cells.
Acknowledgments
The authors are grateful to A. Uryga for skilled technical help.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/cancers13122952/s1. Figure S1: SRB (A) and MTT (B) cytotoxicity assay of pectins in Caco-2 cells (incubation time 48 h). Figure S2: Typical dot plots of Annexin V/PI double staining apoptosis assay in HCT 116 cells. Figure S3: Typical histograms of DNA content (stained with PI) in HCT 116 cells treated with 0.2 mg/mL of pectins and/or SN-38 for 48 h. Sub-G1 population—dead cells, G0/G1—mononuclear cells, S—DNA replication, G2/M—mitosis. Figure S4: E. coli LH82 (A) and K-12C600 strains (B) adherence to Caco-2 cells in the presence of pectins during 2 h of incubation. Figure S5: MTT (B) cytotoxicity assay of pectins in HCT-116 (A) and Caco-2 cells (B) during 2 h of incubation. Figure S6: E. coli LH82 (A) and K-12C600 strains (B) proliferation during 2 h of incubation in the presence of pectins.
Author Contributions
Conceptualization, K.Ś.-P., B.S., A.W., O.W., A.P.-Ł.; data curation, A.P.-Ł., J.M., K.Ś.-P., A.W., M.S., B.S.; formal analysis, A.P.-Ł., J.M., K.Ś-P., A.W., M.S., B.S., O.W.; funding acquisition, K.Ś.-P.; investigation, A.P.-Ł., J.M., K.Ś.-P., A.W., M.S., B.S., O.W.; methodology, A.P.-Ł., K.Ś.-P., M.S., B.S., project administration, K.Ś.-P.; supervision, K.Ś.-P.; validation, K.Ś.-P., B.S., M.S., and O.W.; visualization, A.P.-Ł., K.Ś.-P.; B.S., O.W.; writing—original draft, A.P.-Ł., O.W., B.S., and K.Ś.-P.; writing—review and editing, K.Ś.-P., B.S., A.W., O.W., A.P.-Ł. All authors have read and agreed to the published version of the manuscript.
Funding
This study was financed from the funds granted by the Ministry of Science and Higher Education in the Regional Initiative of Excellence program for the years 2019–2022, project number RID.Z501.20.013, the amount of funding 140 000.00 PLN.
Data Availability Statement
Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cancer Today. [(accessed on 14 March 2021)]; Available online: https://gco.iarc.fr/today/fact-sheets-cancers.
- 2.Recio-Boiles A., Cagir B. Stat Pearls. StatPearls Publishing; Treasure Island, FL, USA: 2021. Colon Cancer. [PubMed] [Google Scholar]
- 3.Fantini M.C., Guadagni I. From inflammation to colitis-associated colorectal cancer in inflammatory bowel disease: Pathogenesis and impact of current therapies. Dig. Liver Dis. 2021;53:558–565. doi: 10.1016/j.dld.2021.01.012. [DOI] [PubMed] [Google Scholar]
- 4.Peddareddigari V.G., Wang D., Dubois R.N. The tumor microenvironment in colorectal carcinogenesis. Cancer Microenviron. 2010;3:149–166. doi: 10.1007/s12307-010-0038-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin C., Cai X., Zhang J., Wang W., Sheng Q., Hua H., Zhou X. Role of gut microbiota in the development and treatment of colorectal cancer. Digestion. 2019;100:72–78. doi: 10.1159/000494052. [DOI] [PubMed] [Google Scholar]
- 6.Heo G., Lee Y., Im E. Interplay between the gut microbiota and inflammatory mediators in the development of colorectal cancer. Cancers. 2021;13:734. doi: 10.3390/cancers13040734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hibberd A.A., Lyra A., Ouwehand A.C., Rolny P., Lindegren H., Cedgard L., Wettergren Y. Intestinal microbiota is altered in patients with colon cancer and modified by probiotic intervention. BMJ Open Gastroenterol. 2017;4:e000145. doi: 10.1136/bmjgast-2017-000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karwowska Z., Szemraj J., Karwowski B. Microbiota alterations in gastrointestinal cancers. Appl. Sci. 2020;10:585. doi: 10.3390/app10020585. [DOI] [Google Scholar]
- 9.Lehouritis P., Cummins J., Stanton M., Murphy C.T., McCarthy F.O., Reid G., Urbaniak C., Byrne W.L., Tangney M. Local bacteria affect the efficacy of chemotherapeutic drugs. Sci. Rep. 2015;5:14554. doi: 10.1038/srep14554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alexander J.L., Wilson I.D., Teare J., Marchesi J.R., Nicholson J.K., Kinross J.M. Gut microbiota modulation of chemotherapy efficacy and toxicity. Nat. Rev. Gastroenterol. Hepatol. 2017;14:356–365. doi: 10.1038/nrgastro.2017.20. [DOI] [PubMed] [Google Scholar]
- 11.Kanemitsu Y., Shitara K., Mizusawa J., Hamaguchi T., Shida D., Komori K., Ikeda S., Ojima H., Ike H., Shiomi A., et al. Primary tumor resection plus chemotherapy versus chemotherapy alone for colorectal cancer patients with asymptomatic, synchro-nous unresectable metastases (JCOG1007; iPACS): A randomized clinical trial. J. Clin. Oncol. 2021;39:1098–1107. doi: 10.1200/JCO.20.02447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rivory L.P. Irinotecan (CPT-11): A brief overview. Clin. Exp. Pharmacol. Physiol. 1996;23:1000–1004. doi: 10.1111/j.1440-1681.1996.tb01158.x. [DOI] [PubMed] [Google Scholar]
- 13.Van Cutsem E., Cervantes A., Adam R., Sobrero A., van Krieken J.H., Aderka D., Aranda Aguilar E., Bardelli A., Benson A., Bodoky G., et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann. Oncol. 2016;27:1386–1422. doi: 10.1093/annonc/mdw235. [DOI] [PubMed] [Google Scholar]
- 14.Yoshino T., Arnold D., Taniguchi H., Pentheroudakis G., Yamazaki K., Xu R.H., Kim T.W., Ismail F., Tan I.B., Yeh K.H., et al. Pan-Asian adapted ESMO consensus guidelines for the management of patients with metastatic colorectal cancer: A JSMO-ESMO Initiative Endorsed by CSCO, KACO, MOS, SSO and TOS. Ann. Oncol. 2018;29:44–70. doi: 10.1093/annonc/mdx738. [DOI] [PubMed] [Google Scholar]
- 15.Gibson R.J., Stringer A.M. Chemotherapy-induced diarrhoea. Curr. Opin. Support. Palliat. 2009;3:31–35. doi: 10.1097/SPC.0b013e32832531bb. [DOI] [PubMed] [Google Scholar]
- 16.Stein A., Voigt W., Jordan K. Review: Chemotherapy-induced diarrhea: Pathophysiology, frequency and guideline-based management. Ther. Adv. Med. Oncol. 2010;2:51–63. doi: 10.1177/1758834009355164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guthrie L., Gupta S., Daily J., Kelly L. Human microbiome signatures of differential colorectal cancer drug metabolism. NPJ Biofilms Microbiomes. 2017;3:1–8. doi: 10.1038/s41522-017-0034-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsieh Y.T., Chen K.C., Cheng C.M., Cheng T.L., Tao M.H., Roffler S.R. impediments to enhancement of CPT-11 anticancer activity by E. coli directed beta-glucuronidase therapy. PLoS ONE. 2015;10:e0118028. doi: 10.1371/journal.pone.0118028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Willats W.G.T., Mccartney L., Mackie W., Knox J.P. Pectin: Cell biology and prospects for functional analysis. Plant. Mol. Biol. 2001;47:9–27. doi: 10.1023/A:1010662911148. [DOI] [PubMed] [Google Scholar]
- 20.Morris G.A., Binhamad H.A.S. Isolation and characterisation of pectin. In: Kontogiorgos V., editor. Pectin: Technological and Physiological Properties. Springer Nature; Basingstoke, UK: 2020. pp. 61–82. [DOI] [Google Scholar]
- 21.Eliaz I., Raz A. Pleiotropic effects of modified citrus pectin. Nutrients. 2019;11:2619. doi: 10.3390/nu11112619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beukema M., Faas M.M., de Vos P. The effects of different dietary fiber pectin structures on the gastrointestinal immune barrier: Impact via gut microbiota and direct effects on immune cells. Exp. Mol. Med. 2020;52:1364–1376. doi: 10.1038/s12276-020-0449-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wikiera A., Mika M., Starzyńska-Janiszewska A., Stodolak B. Endo-Xylanase and endo-cellulase-assisted extraction of pectin from apple pomace. Carbohydr. Polym. 2016;142:199–205. doi: 10.1016/j.carbpol.2016.01.063. [DOI] [PubMed] [Google Scholar]
- 24.Wikiera A., Grabacka M., Byczyński Ł., Stodolak B., Mika M. Enzymatically extracted apple pectin possesses antioxidant and antitumor activity. Molecules. 2021;26:1434. doi: 10.3390/molecules26051434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hossein G., Halvaei S., Heidarian Y., Dehghani-Ghobadi Z., Hassani M., Hosseini H., Naderi N., Sheikh Hassani S. Pectasol-C modified citrus pectin targets galectin-3-induced STAT3 activation and synergize paclitaxel cytotoxic effect on ovarian cancer spheroids. Cancer Med. 2019;8:4315–4329. doi: 10.1002/cam4.2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Skehan P., Storeng R., Scudiero D., Monks A., Mcmahon J., Vistica D., Warren J.T., Bokesch H., Kenney S., Boyd M.R. New colorimetric cytotoxicity assay for anticancer-drug screening. J. Natl. Cancer Inst. 1990;82:1107–1112. doi: 10.1093/jnci/82.13.1107. [DOI] [PubMed] [Google Scholar]
- 27.Palko-Labuz A., Sroda-Pomianek K., Uryga A., Kostrzewa-Suslow E., Michalak K. Anticancer activity of baicalein and luteolin studied in colorectal adenocarcinoma LoVo cells and in drug-resistant LoVo/Dx cells. Biomed. Pharmacother. 2017;88:232–241. doi: 10.1016/j.biopha.2017.01.053. [DOI] [PubMed] [Google Scholar]
- 28.Chou T.C., Martin N. CompuSyn for Drug Combinations: PC Software and User’s Guide: A Computer Program for Quantitation of Synergism and Antagonism In Drug Combinations, and the Determination of IC50 and ED50 and LD50 Values. ComboSyn Inc.; Paramus, NJ, USA: 2005. [Google Scholar]
- 29.Aich S., Delbaere L.T.J., Chen R. Continuous spectrophotometric assay for β-glucuronidase. Biotechniques. 2001;30:846–850. doi: 10.2144/01304rr02. [DOI] [PubMed] [Google Scholar]
- 30.Leclere L., van Cutsem P., Michiels C. Anti-cancer activities of pH- or heat-modified pectin. Front. Pharmacol. 2013;4:128. doi: 10.3389/fphar.2013.00128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cheng H., Li S., Fan Y., Gao X., Hao M., Wang J., Zhang X., Tai G., Zhou Y. comparative studies of the antiproliferative effects of ginseng polysaccharides on HT-29 human colon cancer cells. Med. Oncol. 2011;28:175–181. doi: 10.1007/s12032-010-9449-8. [DOI] [PubMed] [Google Scholar]
- 32.Cheng H., Zhang Z., Leng J., Liu D., Hao M., Gao X., Tai G., Zhou Y. The inhibitory effects and mechanisms of rhamnogalacturonan I pectin from potato on HT-29 colon cancer cell proliferation and cell cycle progression. Int. J. Food Sci. Nutr. 2013;64:36–43. doi: 10.3109/09637486.2012.694853. [DOI] [PubMed] [Google Scholar]
- 33.Maxwell E.G., Colquhoun I.J., Chau H.K., Hotchkiss A.T., Waldron K.W., Morris V.J., Belshaw N.J. Modified sugar beet pectin induces apoptosis of colon cancer cells via an interaction with the neutral sugar side-chains. Carbohydr. Polym. 2016;136:923–929. doi: 10.1016/j.carbpol.2015.09.063. [DOI] [PubMed] [Google Scholar]
- 34.Naqash F., Masoodi F.A., Rather S.A., Wani S.M., Gani A. Emerging concepts in the nutraceutical and functional properties of pectin—A review. Carbohydr. Polym. 2017;168:227–239. doi: 10.1016/j.carbpol.2017.03.058. [DOI] [PubMed] [Google Scholar]
- 35.Motwani M., Jung C., Shah M.A., Schwartz G.K., Sirotnak F.M., She Y., Gonen M. Augmentation of apoptosis and tumor regression by flavopiridol in the presence of CPT-11 in HCT116 colon cancer monolayers and xenografts. Clin. Cancer Res. 2001;7:4209–4219. [PubMed] [Google Scholar]
- 36.Hossein G., Keshavarz M., Ahmadi S., Naderi N. Synergistic effects of PectaSol-C modified citrus pectin an inhibitor of galectin-3 and paclitaxel on apoptosis of human SKOV-3 ovarian cancer cells. Asian Pac. J. Cancer Prev. 2013;14:7561–7568. doi: 10.7314/APJCP.2013.14.12.7561. [DOI] [PubMed] [Google Scholar]
- 37.Tehranian N., Sepehri H., Mehdipour P., Biramijamal F., Hossein-Nezhad A., Sarrafnejad A., Hajizadeh E. Combination effect of PectaSol and doxorubicin on viability, cell cycle arrest and apoptosis in DU-145 and LNCaP prostate cancer cell lines. Cell. Biol. Int. 2012;36:601–610. doi: 10.1042/CBI20110309. [DOI] [PubMed] [Google Scholar]
- 38.Jackson C.L., Dreaden T.M., Theobald L.K., Tran N.M., Beal T.L., Eid M., Gao M.Y., Shirley R.B., Stoffel M.T., Kumar M.V., et al. Pectin induces apoptosis in human prostate cancer cells: Correlation of apoptotic function with pectin structure. Glycobiology. 2007;17:805–819. doi: 10.1093/glycob/cwm054. [DOI] [PubMed] [Google Scholar]
- 39.Yan J., Katz A. PectaSol-C modified citrus pectin induces apoptosis and inhibition of proliferation in human and mouse androgen-dependent and-independent prostate cancer cells. Integr. Cancer Ther. 2010;9:197–203. doi: 10.1177/1534735410369672. [DOI] [PubMed] [Google Scholar]
- 40.Olano-Martin E., Rimbach G.H., Gibson G.R., Rastall R.A. Pectin and pectic-oligosaccharides induce apoptosis in in vitro human colonic adenocarcinoma cells. Anticancer Res. 2003;23:341–346. [PubMed] [Google Scholar]
- 41.Ogutu F.O., Mu T.H., Sun H., Zhang M. Ultrasonic modified sweet potato pectin induces apoptosis like cell death in colon cancer (HT-29) cell line. Nutr. Cancer. 2018;70:136–145. doi: 10.1080/01635581.2018.1406123. [DOI] [PubMed] [Google Scholar]
- 42.Fang T., Liu D., Ning H.M., Liu D., Sun J.Y., Huang X.J., Dong Y., Geng M.Y., Yun S.F., Yan J., et al. Modified citrus pectin inhibited bladder tumor growth through downregulation of galectin-3. Acta Pharmacol. Sin. 2018;39:1885–1893. doi: 10.1038/s41401-018-0004-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Avivi-Green C., Madar Z., Schwartz B. Pectin-enriched diet affects distribution and expression of apoptosis-cascade proteins in colonic crypts of dimethylhydrazine-treated rats. Int. J. Mol. Med. 2000;6:689–698. doi: 10.3892/ijmm.6.6.689. [DOI] [PubMed] [Google Scholar]
- 44.Dumic J., Dabelic S., Flogel M. Galectin-3: An open-ended story. Biochim. Biophys. Acta. 2006;1760:616–635. doi: 10.1016/j.bbagen.2005.12.020. [DOI] [PubMed] [Google Scholar]
- 45.Newlaczyl A.U., Yu L.G. Galectin-3—A jack-of-all-trades in cancer. Cancer Lett. 2011;313:123–128. doi: 10.1016/j.canlet.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 46.Minzanova S., Mironov V., Arkhipova D., Khabibullina A., Mironova L., Zakirova Y., Milyukov V. Biological activity and pharmacological application of pectic polysaccharides: A review. Polymers. 2018;10:1407. doi: 10.3390/polym10121407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Conti S., Vexler A., Hagoel L., Kalich-Philosoph L., Corn B.W., Honig N., Shtraus N., Meir Y., Ron I., Eliaz I., et al. Modified citrus pectin as a potential sensitizer for radiotherapy in prostate cancer. Integr. Cancer Ther. 2018;17:1225–1234. doi: 10.1177/1534735418790382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Salehi F., Behboudi H., Kavoosi G., Ardestani S.K. Oxidative DNA damage induced by ROS-modulating agents with the ability to target DNA: A comparison of the biological characteristics of citrus pectin and apple pectin. Sci. Rep. 2018;8:1–16. doi: 10.1038/s41598-018-32308-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Davoodi H., Hashemi S.R., Seow H.F. Increased NFκ-B activity in HCT116 colorectal cancer cell line harboring TLR4 Asp299Gly variant. Iran. J. Allergy Asthma Immunol. 2012;11:121–132. [PubMed] [Google Scholar]
- 50.Chung Y.H., Kim D. Enhanced TLR4 expression on colon cancer cells after chemotherapy promotes cell survival and epithelial-mesenchymal transition through phosphorylation of GSK3β. Anticancer Res. 2016;36:3383–3394. [PubMed] [Google Scholar]
- 51.Lu Y.C., Yeh W.C., Ohashi P.S. LPS/TLR4 signal transduction pathway. Cytokine. 2008;42:145–151. doi: 10.1016/j.cyto.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 52.Luo C., Zhang H. The Role of proinflammatory pathways in the pathogenesis of colitis-associated colorectal cancer. Mediat. Inflamm. 2017;2017:5126048. doi: 10.1155/2017/5126048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chen C.H., Sheu M.T., Chen T.F., Wang Y.C., Hou W.C., Liu D.Z., Chung T.C., Liang Y.C. Suppression of endotoxin-induced proinflammatory responses by citrus pectin through blocking LPS signaling pathways. Biochem. Pharmacol. 2006;72:1001–1009. doi: 10.1016/j.bcp.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 54.Li Y., Fan L., Sun Y., Zhang D., Yue Z., Niu Y., Meng J., Yang T., Liu W., Mei Q. An apple oligogalactan suppresses endotoxin-induced cyclooxygenase-2 expression by inhibition of LPS pathways. Int. J. Biol. Macromol. 2013;61:75–81. doi: 10.1016/j.ijbiomac.2013.06.048. [DOI] [PubMed] [Google Scholar]
- 55.Zhang D., Li Y.H., Mi M., Jiang F.L., Yue Z.G., Sun Y., Fan L., Meng J., Zhang X., Liu L., et al. Modified apple polysaccharides suppress the migration and invasion of colorectal cancer cells induced by lipopolysaccharide. Nutr. Res. 2013;33:839–848. doi: 10.1016/j.nutres.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 56.Ishisono K., Yabe T., Kitaguchi K. Citrus pectin attenuates endotoxin shock via suppression of Toll-Like Receptor signaling in Peyer’s patch myeloid cells. J. Nutr. Biochem. 2017;50:38–45. doi: 10.1016/j.jnutbio.2017.07.016. [DOI] [PubMed] [Google Scholar]
- 57.Sabater C., Molina-Tijeras J.A., Vezza T., Corzo N., Montilla A., Utrilla P. Intestinal anti-inflammatory effects of artichoke pectin and modified pectin fractions in the dextran sulfate sodium model of mice colitis. artificial neural network modelling of inflammatory markers. Food Funct. 2019;10:7793–7805. doi: 10.1039/C9FO02221J. [DOI] [PubMed] [Google Scholar]
- 58.Tan H., Chen W., Liu Q., Yang G., Li K. Pectin Oligosaccharides ameliorate colon cancer by regulating oxidative stress- and inflammation-activated signaling pathways. Front. Immunol. 2018;9:1504. doi: 10.3389/fimmu.2018.01504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cochet F., Peri F. The role of carbohydrates in the lipopolysaccharide (LPS)/Toll-Like Receptor 4 (TLR4) signalling. Int. J. Mol. Sci. 2017;18:2318. doi: 10.3390/ijms18112318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mazgaeen L., Gurung P. Recent advances in lipopolysaccharide recognition systems. Int. J. Mol. Sci. 2020;21:379. doi: 10.3390/ijms21020379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wong T.W., Colombo G., Sonvico F. Pectin matrix as oral drug delivery vehicle for colon cancer treatment. AAPS PharmSciTech. 2011;12:201–214. doi: 10.1208/s12249-010-9564-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ferrario C., Statello R., Carnevali L., Mancabelli L., Milani C., Mangifesta M., Duranti S., Lugli G.A., Lodge J.B., Viappiani S., et al. How to feed the mammalian gut microbiota: Bacterial and metabolic modulation by dietary fibers. Front. Microbiol. 2017;8:1749. doi: 10.3389/fmicb.2017.01749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang S., Wang J., Mou H., Luo B., Jiang X. Inhibition of adhesion of intestinal pathogens (Escherichia coli, Vibrio cholerae, Campylobacter jejuni, and Salmonella typhimurium) by common oligosaccharides. Foodborne Pathog. Dis. 2015;12:360–365. doi: 10.1089/fpd.2014.1835. [DOI] [PubMed] [Google Scholar]
- 64.Rhoades J., Manderson K., Wells A., Hotchkiss A.T., Jr., Gibson G.R., Formentin K., Beer M., Rastall R.A. Oligosaccharide-mediated inhibition of the adhesion of pathogenic Escherichia coli strains to human gut epithelial cells in vitro. J. Food Prot. 2008;71:2272–2277. doi: 10.4315/0362-028X-71.11.2272. [DOI] [PubMed] [Google Scholar]
- 65.Di R., Vakkalanka M.S., Onumpai C., Chau H.K., White A., Rastall R.A., Yam K., Hotchkiss A.T., Jr. Pectic oligosaccharide structure-function relationships: Prebiotics, inhibitors of Escherichia coli O157:H7 adhesion and reduction of Shiga toxin cytotoxicity in HT29 cells. Food Chem. 2017;227:245–254. doi: 10.1016/j.foodchem.2017.01.100. [DOI] [PubMed] [Google Scholar]
- 66.Ganan M., Collins M., Rastall R., Hotchkiss A.T., Chau H.K., Carrascosa A.V., Martinez-Rodriguez A.J. Inhibition by pectic oligosaccharides of the invasion of undifferentiated and differentiated Caco-2 cells by Campylobacter jejuni. Int. J. Food Microbiol. 2010;137:181–185. doi: 10.1016/j.ijfoodmicro.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 67.Wilkowska A., Nowak A., Antczak-Chrobot A., Motyl I., Czyżowska A., Paliwoda A. Structurally different pectic oligosaccharides produced from apple pomace and their biological activity in vitro. Foods. 2019;8:365. doi: 10.3390/foods8090365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lee J.H., Shim J.S., Lee J.S., Kim M.K., Chung M.S., Kim K.H. Pectin-like acidic polysaccharide from Panax ginseng with selective antiadhesive activity against pathogenic bacteria. Carbohydr. Res. 2006;341:1154–1163. doi: 10.1016/j.carres.2006.03.032. [DOI] [PubMed] [Google Scholar]
- 69.Lin X.B., Dieleman L.A., Ketabi A., Bibova I., Sawyer M.B., Xue H., Field C.J., Baracos V.E., Ganzle M.G. Irinotecan (CPT-11) chemotherapy alters intestinal microbiota in tumour bearing rats. PLoS ONE. 2012;7:e39764. doi: 10.1371/journal.pone.0039764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dashnyam P., Mudududdla R., Hsieh T.J., Lin T.C., Lin H.Y., Chen P.Y., Hsu C.Y., Lin C.H. β-Glucuronidases of opportunistic bacteria are the major contributors to xenobiotic-induced toxicity in the gut. Sci. Rep. 2018;8:1–12. doi: 10.1038/s41598-018-34678-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wallace B.D., Wang H., Lane K.T., Scott J.E., Orans J., Koo J.S., Venkatesh M., Jobin C., Yeh L.A., Mani S., et al. Alleviating cancer drug toxicity by inhibiting a bacterial enzyme. Science. 2010;330:831–835. doi: 10.1126/science.1191175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bhatt A.P., Pellock S.J., Biernat K.A., Walton W.G., Wallace B.D., Creekmore B.C., Letertre M.M., Swann J.R., Wilson I.D., Roques J.R., et al. Targeted inhibition of gut bacterial β-glucuronidase activity enhances anticancer drug efficacy. Proc. Natl. Acad. Sci. USA. 2020;117:7374–7381. doi: 10.1073/pnas.1918095117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ross J.K., Leklem J.E. The effect of dietary citrus pectin on the excretion of human fecal neutral and acid steroids and the activity of 7alpha-dehydroxylase and beta-glucuronidase. Am. J. Clin. Nutr. 1981;34:2068–2077. doi: 10.1093/ajcn/34.10.2068. [DOI] [PubMed] [Google Scholar]
- 74.Borisenkov M.F., Bakutova L.A., Latkin D.S., Golovchenko V.V., Vityazev F.V. Interaction of microbial β-glucuronidase with vegetable pectins. J. Agric. Food Chem. 2011;59:9922–9926. doi: 10.1021/jf202307r. [DOI] [PubMed] [Google Scholar]
- 75.Bauer H.G., Asp N.G., Dahlqvist A., Fredlund P.E., Nyman M., Oste R. Effect of two kinds of pectin and guar gum on 1,2-dimethylhydrazine initiation of colon tumors and on fecal beta-glucuronidase activity in the rat. Cancer Res. 1981;41:2518–2523. [PubMed] [Google Scholar]
- 76.Ohno K., Narushima S., Takeuchi S., Itoh K., Itoh T., Hioki K., Nomura T. Effect of bacterial metabolism in the intestine on colorectal tumors induced by 1,2-dimethylhydrazine in transgenic mice harboring human prototype c-Ha-ras genes. J. Exp. Clin. Cancer Res. 2001;20:51–56. [PubMed] [Google Scholar]
- 77.Chen H.L., Lin Y.M., Wang Y.C. Comparative effects of cellulose and soluble fibers (pectin, konjac glucomannan, inulin) on fecal water toxicity toward Caco-2 cells, fecal bacteria enzymes, bile acid, and short-chain fatty acids. J. Agric. Food Chem. 2010;58:10277–10281. doi: 10.1021/jf102127k. [DOI] [PubMed] [Google Scholar]
- 78.Lindop R., Tasman-Jones C., Thomsen L.L., Lee S.P. Cellulose and pectin alter intestinal beta-glucuronidase (EC 3.2.1.31) in the rat. Br. J. Nutr. 1985;54:21–26. doi: 10.1079/BJN19850088. [DOI] [PubMed] [Google Scholar]
- 79.Ohkami H., Tazawa K., Yamashita I., Shimizu T., Murai K., Kobashi K., Fujimaki M. Effects of apple pectin on fecal bacterial enzymes in azoxymethane-induced rat colon carcinogenesis. Jpn. J. Cancer Res. 1995;86:523–529. doi: 10.1111/j.1349-7006.1995.tb02429.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tazawa K., Okami H., Yamashita I., Ohnishi Y., Kobashi K., Fujimaki M. Effects of apple pectin on fecal enzyme activities and prostaglandin E2 levels in azoxymethane-induced rat colon carcinogenesis. In: Ohigashi H., Osawa T., Terao J., Watanabe S., Yoshikawa T., editors. Food Factors for Cancer Prevention. Springer; Tokyo, Japan: 1997. pp. 178–181. [DOI] [Google Scholar]
- 81.Rao C.V., Chou D., Simi B., Ku H., Reddy B.S. Prevention of colonic aberrant crypt foci and modulation of large bowel microbial activity by dietary coffee fiber, inulin and pectin. Carcinogenesis. 1998;19:1815–1819. doi: 10.1093/carcin/19.10.1815. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing is not applicable to this article.