Abstract
Cone-beam computed tomography (CBCT) has been widely used in diagnosis of vertical root fractures (VRFs) in recent years. According to the American Association of Endodontists (AAE) classification, there are five types of cracked teeth and VRF is one of them. Due to the variability and overlapping of the cracks and fractures, some narrow fractures on the roots of VRFs could not be detected by CBCT, and some wide cracks on the crown of cracked teeth could be detected by CBCT. In this review, we firstly discussed the value of CBCT in the diagnosis of the AAE five types of cracked teeth and presented CBCT manifestations of some typical cases. Secondly, we summarized the factors influencing the diagnosis of cracks/fractures using CBCT, namely, CBCT device-related factors, patient-related factors, and evaluator-related factors. The possible strategies to improve the diagnostic accuracy in the clinic practice are also discussed in this part. Finally, we compared the differences of root fractures with lateral canals and external root resorption on CBCT images.
Keywords: Cone-beam computed tomography, Diagnosis, Cracked teeth, Vertical root fracture, Cracks/fractures
Introduction
Cracked teeth is a general term for a series types of tooth fracture with quite variable and complicated clinical signs and symptoms. Several different terminologies, definitions, and classifications for cracked teeth have been proposed. The most widely used classification is the American Association of Endodontists (AAE) classification, which divides cracked teeth into five types: craze lines, fractured cusp, cracked tooth, split tooth, and vertical root fracture (VRF).1 It should be noted that these five types are not entirely mutually exclusive. Linear cracks tend to grow and change over time,2,3 and so, one fracture type can progress into another type over time.
The accurate diagnosis of cracked teeth is of great importance because it influences the treatment strategy. It is difficult to reach a definitive diagnosis on the basis of signs and symptoms alone because these are non-specific and mimic the clinical manifestations of endodontic and periodontal disease.2,4–6 The ease of diagnosis also varies according to the position and extent of the fracture.7–10
Cracked teeth is a perplexing diagnostic problem, especially in the early stage. Cracks/fractures in teeth may occur in both the horizontal and vertical directions and may involve the crown and/or root. Conventional periapical radiographs (PRs) can only provide a definite diagnosis of obviously displaced root fractures. Cone-beam computed tomography (CBCT), which provides precise three-dimensional images with high spatial resolution, is now widely used for the diagnosis of VRFs. Many in vitro and in vivo studies have explored the validity of CBCT for the diagnosis of root fractures.11–15 However, no study has systematically reviewed the use of CBCT for the diagnosis of cracked teeth. Therefore, in this review, we first present the typical CBCT presentation of the five types of cracked teeth. Secondly, we summarize and discuss the factors influencing the diagnosis of cracks/fractures using CBCT and discussed the possible strategies to improve the diagnostic accuracy. Finally, we discuss the differential diagnosis of fracture lines with lateral canal and external root resorption on CBCT.
CBCT features of cracked teeth
Except for VRFs, all other AAE fracture types occur in or involve the crown. Therefore, the role of X-ray examination in the diagnosis of these four types of cracked teeth is not as important as in the diagnosis of VRFs. In the case of cracked tooth, split tooth, and VRF, X-ray examination is mainly used to determine whether cracks/fractures are present in the root and to assess the periodontal and periapical bone in a non-destructive fashion.
Craze line
Craze lines are visible cracks that are contained within the enamel. In the posterior teeth, craze lines are usually evident crossing marginal ridges and/or extending along buccal and lingual surfaces. Long vertical craze lines are often found in the anterior teeth.1 These lines are confined to the enamel and are a natural occurrence. Craze lines located on the crown are asymptomatic and narrow.2 These are diagnosed by direct visualization and transillumination, and CBCT is not required.
Fractured cusp
Fractured cusps are usually caused by large intracoronal restoration or devastating occlusal trauma. This type of crack often extends in the mesiodistal and buccolingual directions, commonly involves one or both marginal ridges as well as a buccal or lingual groove, and terminates in the cervical region either parallel to the gingival margin or slightly subgingival.2 Fractured cusps are relatively easy to diagnose, and may be found incidentally on CBCT images (Figure 1). CBCT is occasionally used to determine whether pulp involvement is present and to assess the pulp-periapical status.
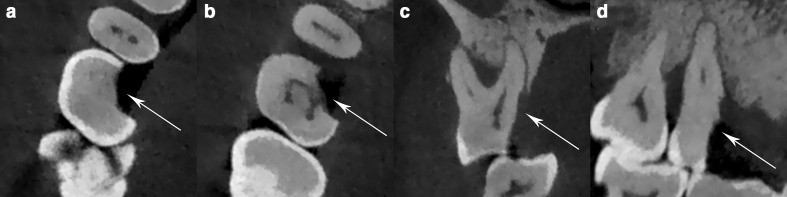
Figure 1.
(a, b) Axial images showing tooth 16 with a complete fracture of the mesiopalatal cusp (arrows). (c, d) Coronal and sagittal reconstruction images showing that the fracture initiates from the crown of the tooth and extends subgingivally (arrows).
Cracked tooth
The term cracked tooth is defined as a crack extending apically from the occlusal surface of the tooth without separation of the two segments. The clinical signs, symptoms, radiographical findings and test results of cracked tooth are highly variable and depend on numerous factors, which makes their diagnosis challenging.4,6 As the crack initiates from the crown, direct inspection combined with staining and transillumination are effective for diagnosis.16 Because this fracture extends in the mesiodistal direction, it is not visible on PRs.2 Even on CBCT, incomplete cracked lines are usually too narrow to be detected. Therefore, CBCT is rarely used to diagnose cracked tooth, and studies evaluating CBCT use in cracked tooth are far less numerous than those evaluating CBCT use in VRFs.17 Nevertheless, as the width of the cracked line is variable, cracked tooth may occasionally be detected on CBCT images (Figure 2). Although the crack can be detected on direct inspection, it is difficult to determine the extent of the crack in this way.3,18,19 Thus, CBCT examination could be used to determine the extent of the crack and assess the pulp-periapical and periodontal status.
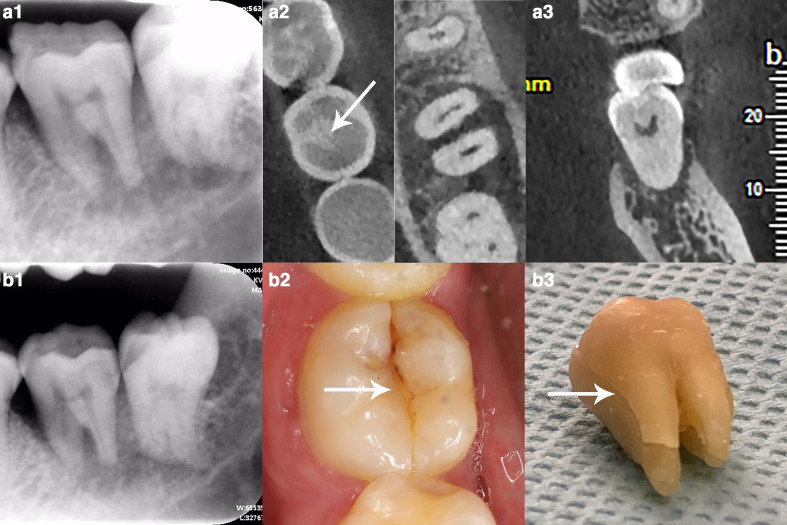
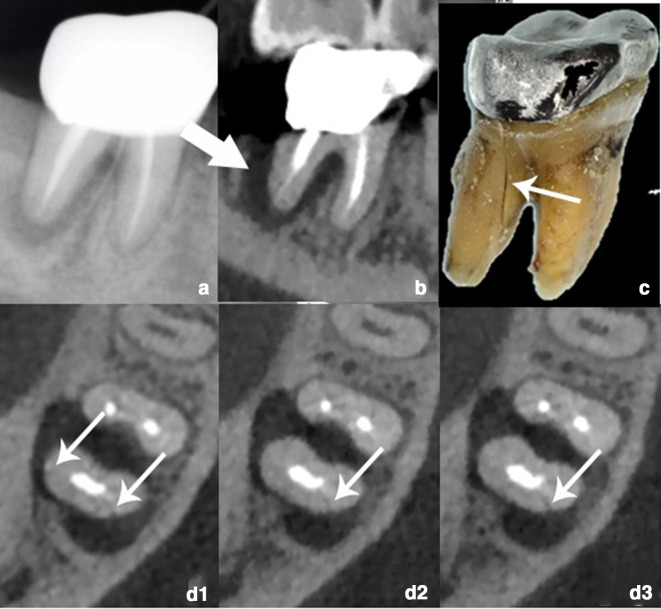
Figure 2.
A case of cracked tooth progressing to split tooth (tooth 36). (a1) Periapical radiograph (PR) showing extensive bone resorption around the root. (a2) Axial image showing a mesiodistal hair-like hypodense line (arrow) that is present on the crown but disappears on the root. (a3) Coronal reconstruction image showing severe buccal and lingual alveolar bone resorption around the root. Cracked tooth with acute inflammation was diagnosed after an incision was made on the periodontal abscess; however, the patient did not undergo further treatment. (b1) PR taken 1 year after the primary referral at our hospital showing more extensive bone resorption around the root. (b2) An obvious mesiodistal fracture line (arrow) can be seen on the occlusal surface. (b3) The extracted tooth has split completely (arrow).
Split tooth
Compared with cracked tooth, split tooth indicates more severe damage and a complete fracture. Split tooth is the end result of the evolution of cracked tooth (Figure 2). Split teeth with obvious separation of segments are easy to identify. For incomplete split tooth, CBCT is sometimes used to determine the extent of root involvement and the periapical and periodontal status. However, in the critical period between cracked stage and split stage, there is no apparent separation of segments. Moreover, endodontically treated split teeth presented serious artefacts; the artefacts make the diagnosis on CBCT more challenging (Figure 3).
Figure 3.
A split tooth (tooth 25). (a1, a2, a3) Axial image showing a mesiodistal hair-like hypodense line (arrow) that is present on the crown but gradually disappears on the root. (a4) Coronal reconstruction images showing a fracture line extend from the occlusal surface to the pulp cavity (arrows). (b1, b2, b3, b4) A fracture line could be found from occlusal surface to the 2/3 root (arrows).
Vertical root fracture
VRFs are defined as a complete or incomplete fracture that initiates from the root at any level and usually extends faciolingually.2 The characteristic clinical findings include a narrow periodontal pocket and crestally located sinus tracts.1 However, it is difficult to reach a definitive diagnosis on the basis of signs and symptoms alone because they are not specific to VRFs and are very similar to endodontic or periodontal disease.2 For the detection of VRFs, two aspects should be carefully noted. First, the fracture line is located on the root, and so, it cannot be directly inspected without periodontal exploration. Therefore, the diagnosis of VRFs is more dependent on X-ray examination than that of the other four types of cracked teeth. Second, like the other four types, the ease of diagnosis of VRFs also varies with the extent of the fracture. Incomplete VRFs and hairline VRFs without obvious separation of the fracture fragments are more difficult to detect than VRFs with extensive displacement of the fracture fragments.20 Some extensively displaced VRFs may even be visualized on PRs. CBCT has been used to overcome the inherent disadvantages of conventional PRs, for example, magnification, distortion, and anatomic superimposition.21 Numerous studies have assessed the utility of CBCT for the detection of VRFs both in vitro and in vivo.11,14,22 However, many subtle VRFs cannot be detected on CBCT.20
CBCT classification of VRFs
Many authors have proposed different terminologies, definitions, and classifications for cracks in teeth.1 Previous classifications were mainly based on the location and extent of cracks/fracture lines and clinical characteristics. As CBCT plays an important role in the diagnosis of VRFs, we propose the following classification of VRFs based on their CBCT appearance: displaced VRFs, subtle VRFs, and hidden VRFs.
Displaced VRFs
Displaced VRFs are complete fractures with obvious separation of the fracture fragments (Figure 4), and they are all easily diagnosed on CBCT.
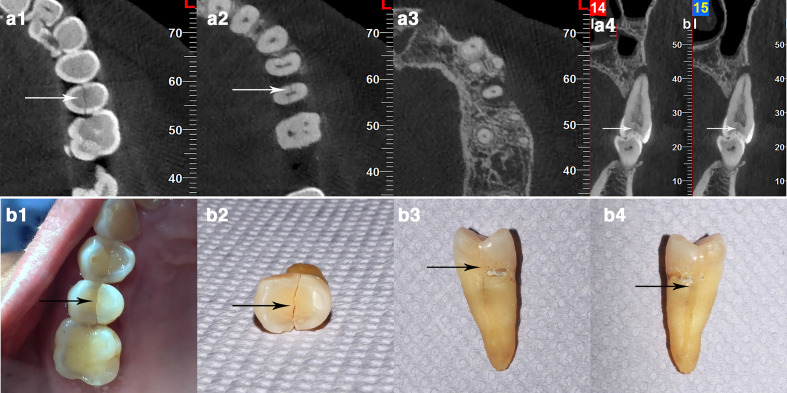
Figure 4.
(a, b) Axial images clearly showing a complete and displaced fracture (arrows) of the mesial root of tooth 36 with alveolar bone resorption around the root. (c) Sagittal reconstruction image showing broadening of the mesial root canal (arrow).
Subtle VRFs
Subtle VRFs are mostly incomplete, narrow or hairline fractures without obvious separation of the fracture fragments (Figure 5). Since the fracture lines are narrow, diagnosis is more difficult than that of displaced VRFs, and the experience of the evaluator considerably influences the diagnostic accuracy.
Figure 5.
(a) PR showing a low-density shadow around the distal root of tooth 46. (b) Sagittal reconstruction image showing alveolar bone resorption around distal root (arrow). (c) The extracted tooth showing the fracture line (arrow). (d1–d3) Subtle irregular hypodense line (arrows) on the distal root without displacement of the two fracture segments.
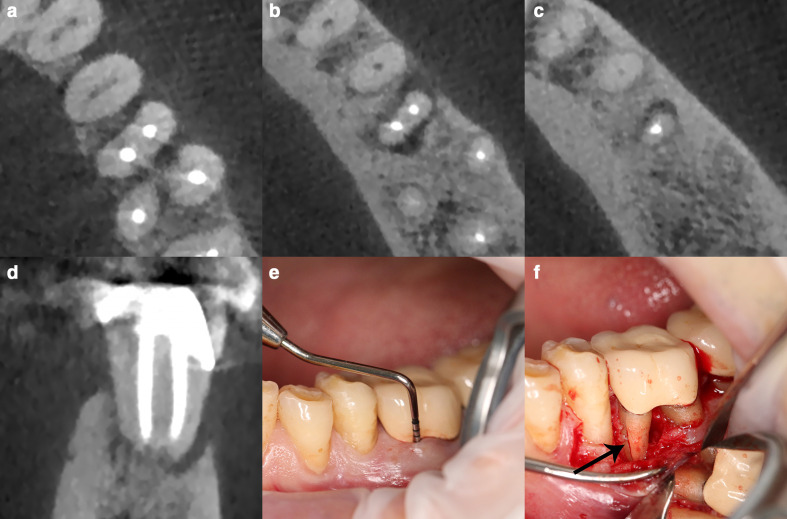
Hidden VRFs
Hidden VRFs cannot be detected on CBCT mainly due to the following reasons: (a) the fracture line is narrower than the voxel size of the CBCT scanner,7 and (b) artefacts induced by endodontic fillings severely interfere with the diagnosis. VRFs are often found in endodontically treated teeth. Artefacts induced by endodontic fillings appear as hypodense lines that mimic or overlap with root fracture lines.23,24 Although this type of VRF cannot be directly demonstrated on CBCT images, localized vertical buccopalatal (lingual) bone loss could be an important indirect diagnostic sign20 (Figure 6).
Figure 6.
(a–c) No obvious fracture lines can be seen in the cervical, middle, and apical thirds of the mesial root of tooth 36 on axial images. (d) Coronal reconstruction image showing vertical alveolar bone resorption on the buccal side. (e) Periodontal examination reveals deep periodontal pockets on the buccal side-of the mesial root measuring approximately 11 mm. (f) Periodontal exploration reveals a longitudinal fracture line on the buccal side-of the mesial root.
Factors influencing use of CBCT to diagnose cracked teeth
Although CBCT offers clear advantages over conventional PRs for the diagnosis of VRFs, the use of CBCT for the detection of VRFs remains controversial.25 In the case of other four types of cracked teeth, CBCT use is limited. Many factors influence the accuracy of diagnosis. These factors can be divided into three categories: CBCT unit-related factors, patient-related factors, and evaluator-related factors. In this section, we also discuss how to improve the diagnosis accuracy (Table 1).
Table 1.
Summary of influence factors and possible strategies improving accuracy in the diagnosis of cracks/fractures using CBCT
| Influence factors | Possible strategies improving accuracy | |
|---|---|---|
| CBCT Unit | Voxel size | Choose smaller voxel size for narrower cracks/fractures |
| FOV | Choose dentoalveolar FOV | |
| Exposure parameter | Increase mAs and number of basis images if possible | |
| Receptor technology | Inherent property of CBCT units, unelectable | |
| Reconstruction algorithm | Inherent property of CBCT units, unelectable | |
| Patient (teeth) |
Motion Artefact | Keep patients as still as possible |
| Beam hardening artefacts | Take off removable metal materials Develop artefact reduction algorithm |
|
| Width of the cracks/fractures | Congenital property of teeth | |
| Observer | Experience | Advance training |
CBCT unit-related factors
The main unit-related factors influencing CBCT image quality are as follows: voxel size, field of view (FOV), exposure parameters (kV, mAs, and number of basis images), receptor technology (flat panels, complementary metal oxide semiconductor, and charge-coupled devices), and reconstruction algorithm. Although there is no standard classification scheme for FOV size, it is useful to categorize FOVs into four ranges: large (>15 cm), medium (10–15 cm), small (8–10 cm), and dentoalveolar (4–6 cm).26 For cracked teeth, the dentoalveolar FOV is preferred. Small FOVs are sometimes used if the dentoalveolar FOV cannot be selected.21 Voxel size mainly ranges from 0.075 to 0.4 mm among the majority of CBCT devices. Exposure parameters, receptor technology, and reconstruction algorithm all depend on the manufacturer and cannot be selected by the dental practitioner.
Voxel size
For the CBCT diagnosis of cracked teeth, voxel size is considered the most important parameter. In the meta-analysis by Corbella et al25 the investigated teeth were divided into four groups based on voxel size, and the authors found that the smaller the voxel, the higher the sensitivity. However, the reported effects of voxel size on the diagnostic accuracy for root fractures varies.10,27,28 We believe that the following two aspects must be considered when evaluating the influence of voxel size on diagnostic accuracy: (a) all other parameters must be constant, and (b) the relationship between voxel size and the width of the crack/fracture line must be taken into account. For example, in the case of a wide fracture line (>300 µm), there may be no differences between voxel sizes of 0.3 and 0.075 mm because these fractures are easy to detect, while in the case of narrow fracture lines (<75 µm), there will be also no difference between voxel sizes of 0.3 and 0.075 mm because these fractures cannot be detected. Finally, in the case of moderate fracture lines, the relationship between voxel size and diagnostic accuracy could be quite complex and variable.10
Field of view
Theoretically, for the same CBCT device, a smaller voxel size is more helpful for the diagnosis of cracks/fractures. In contrast, the FOV size does not influence the resolution of CBCT images. However, many manufacturers couple reductions in voxel size with reductions in FOV size, leading to the false impression that smaller FOVs result in higher-resolution images. In fact, voxel size, not FOV size, is the decisive factor for image resolution. Some researchers have focused on whether the position of the object in the FOV influences diagnostic accuracy because radiation scattering and noise are not homogenously spread across all FOVs.29 Valizadeh et al30 found that the centre of the FOV is the most suitable position for the accurate detection of VRFs in teeth with intracanal posts. Therefore, for particularly small cracks, small FOV and small voxel size should be used and that the tooth should be positioned in the centre of the FOV.31
Exposure parameters, receptor technology, and reconstruction algorithms
Guo et al also found that the detection of VRFs in non-root-filled teeth depended not on voxel size but on the CBCT unit used.10 This suggested the influence of exposure parameters, receptor technology, and reconstruction algorithms. However, these factors are inherent properties of CBCT devices, and cannot be changed during the examination. For devices that allow selection between a low and a high radiation dose for the same FOV and voxel sizes, an adequate increase in mAs and the number of basis images will be helpful for the diagnosis. However, this will also increase the radiation risk for patients. The principle of “as low as reasonably achievable” should always be followed.21
Patient-related factors
In the CBCT diagnosis of VRFs, patient-related factors are common and non-negligible. The two main patient-related factors are artefacts and fracture line width.
Artefacts
Motion artefacts and beam-hardening artefacts are the two most common artefacts in the diagnosis of cracks/fractures. If the patient moves during CBCT examination, the final images usually have motion artefacts such as stripes/streaks, double contours, and overall blurriness.32,33 Spin-Neto et al34 reported movements ≥ 3 mm had a significant impact on image quality and interpretation ability. Although there is no relevant literature on the impact of patient movements in the diagnosis of cracked teeth, reducing motion artefacts is a common consensus.32,34–36 Recently, Santaella et al37 reported there were motion artefact correction systems that could enhance image quality, however, they worked only for CBCT units with aligned detectors and were less effective for those with lateral-offset detectors. Moreover, it is just an in vitro experiment and there are still no in vivo studies on the cracked teeth diagnosis. Therefore, having the patient keep still as much as possible is still an important prerequisite for CBCT examination.
High-density materials, such as metal implants, intracanal posts, metallic crowns, and amalgam restorations, are other main causes of artefacts. The influences vary with the type and position of the material.38,39 Many studies report a decrease in the diagnostic accuracy for VRFs in the presence of endodontic fillings.24,40–42 These materials may cause beam-hardening and streak artefacts that might mimic fracture lines.24,43,44 Artefact-reduction algorithms and filters are applied, however, the results are not satisfactory.45,46 The use of metal artefact reduction (MAR) algorithm and increased of kVp were reported could reduce artefact, however, more studies are still needed in order to assess the influence of them in cracks/fractures detection with metal artefact.47,48 Artefacts and crack/fracture lines may be differentiated as follows: an artefact line is not tridimensional, homogenous, and continuous, and a cracks/fracture line is more likely to have a defined pathway.39
Width of crack/fracture line
The terms crack and fracture can be confusing. According to the review by Rivera,2 the term ‘crack’ implies an incomplete break in a substance, while the term ‘fracture’ implies a complete or incomplete break in a substance. This means that crack lines could be narrower than fracture lines. VRFs might be too narrow in the early stage and may not be detected. Brady et al8 reported a high diagnostic accuracy of CBCT in detecting VRFs ≥ 50 µm in non-endodontically treated teeth. Other in vitro and in vivo studies have reached similar conclusions that the detectability of VRFs on CBCT depends on the fracture width.10 Currently, the smallest voxel size of CBCT devices is 0.075 mm. Therefore, the diagnosis of cracked teeth and early VRFs is still quite difficult. Furthermore, using a smaller voxel size might improve the diagnostic accuracy, but it also increases the radiation dose. Therefore, a balance must be sought between the benefits and potential risks of CBCT.
Evaluator-related factors
The diagnostic accuracy for cracked teeth varies considerably between evaluators, especially for early subtle fractures. Researches usually used inter evaluator agreement (κ values) to compare the consistency of different evaluators and the results vary.8,10,11,14,15,49 An experienced radiologist could have higher accuracy than a junior radiologist.50 For cracked teeth with extensive displacement of the fracture fragments, the diagnosis may be easy, and the influence of the evaluator negligible. However, for early and subtle fractures, the diagnostic accuracy may vary considerably among evaluators. Advance training for those interpreting on CBCT image volumes and offering a CBCT imaging and reporting service are necessary.21
Although CBCT have been adopted to overcome the inherent disadvantages of conventional X-ray radiographs, for example magnification, distortion and anatomic superimposition,51 this does not mean CBCT should be approach of choice if available. Some extensive displaced cracked teeth and periapical or periodontal bone resorption could also be evaluated with 2-dimensional X-ray radiographs. Considering of the radiation risk, CBCT examination is always for further diagnosis when 2-dimensional X-ray radiographs could not provide enough information. Moreover, for patients with CBCT examination, operators should choose the most appropriate parameters of CBCT units to reduce the radiation dose, the principle of “as low as reasonably achievable” should always be followed.21
Differential diagnosis of root fractures with lateral canal and external root resorption
The diagnostic sign of VRF on CBCT is a hypodense (radiolucent) line on the root. In most cases, this sign is characteristic and not easily confused with other diseases. Sometimes, however, lateral canal and external root resorption mimic fracture lines on CBCT images. In this section, we discuss the differential diagnosis of these three conditions.
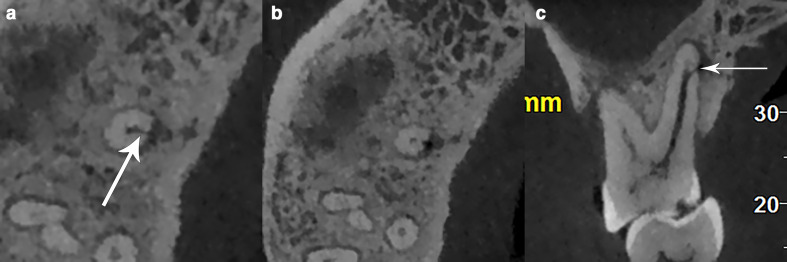
Lateral canal
Lateral canals are a type of accessory canal, which the AAE Glossary of Endodontic Terms (2016)52 defines as “a branch of the main pulp canal or chamber that communicates with the external root surface”. Lateral canals are often found incidentally on CBCT images. When the lateral canal is perpendicular to or almost perpendicular to the main root canal, it may appear as a hypodense line on axial images (Figure 7). Moreover, alveolar bone resorption can be found surrounding lateral canals. Thus, a misdiagnosis of VRF could be made in such patients, especially by inexperienced doctors. A careful inspection of the CBCT images can distinguish lateral canals from fracture lines. On continuous axial images, lateral canals usually appear as a round or elliptical hypodense tubular structure and that gradually move to the root surface; therefore, we come to the conclusion that “movement” is an important feature.53 Although lateral canals appear as hypodense lines, these lines are present on only one or two axial images, are incomplete, and extend from the root canal to one side-of the root surface.
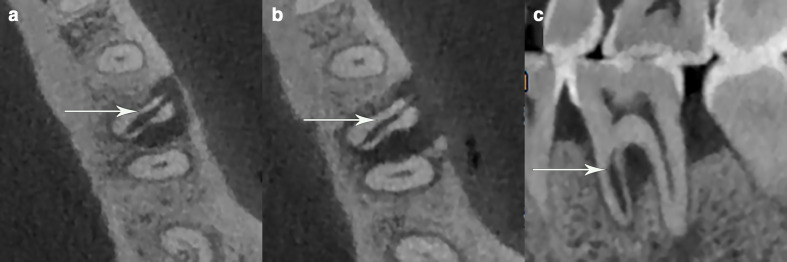
Figure 7.
(a, b) Axial images of tooth 16 showing a hypodense line (arrow) extending from the root canal to the surface of the palatal root, similar to a VRF; however, the hypodense line is present on only one slice and appears as a round hypodense canal closer to the surface of the root on the next axial slice. (c) Coronal reconstruction image clearly showing a lateral canal (arrow) of the palatal root.
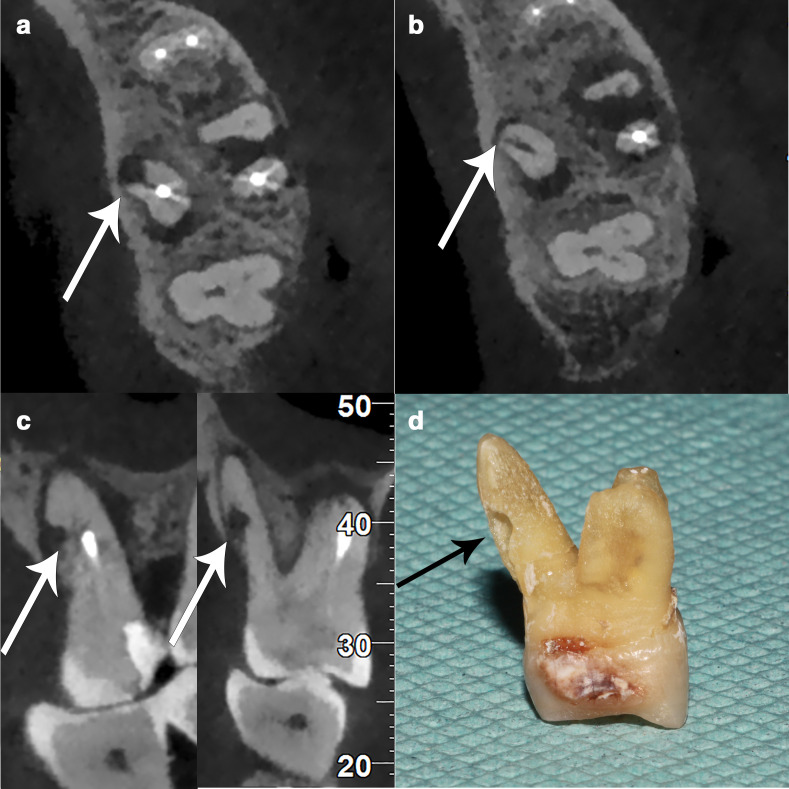
External root resorption
External root resorption usually appears as apical shortening or defects in root surfaces.54 When the resorption and defect of cementum and dentin extend across the pulp, external root resorption might appear as root fracture with two segments on CBCT images (Figure 8), leading to a misdiagnosis. Moreover, bone resorption can usually be found around the root resorption region.
Figure 8.
(a, b) Axial images showing a broad, low-density defect similar with root fracture (arrows). (c) However, sagittal and coronal reconstruction images show an irregular absence of root surface, which indicates external root resorption of palatal root (arrows) and not a vertical root fracture. (d) The extracted tooth shows that the palatal root has external root resorption(arrow).
Comprehensive evaluation of axial, coronal, and sagittal images is crucial, as by integrating the information from these images, external root resorption can be differentiated from root fractures.51,55
Summary
This article summarized the usage of CBCT in the AAE five types of cracked teeth. Except for craze lines, the typical CBCT images of fractured cusps, cracked teeth, split teeth, and vertical root fractures were presented in this article. And we classified VRFs into displaced VRFs, subtle VRFs, and hidden VRFs based on their CBCT manifestations. There are so many factors (device-related factors, patient-related factors, and evaluator-related factors) influence the diagnosis of cracks/fractures using CBCT. Dentoalveolar FOV with small voxel size and increased radiation dose could improve the demonstration for those quite tiny cracked lines theoretically; however, a balance must be sought between the benefits and potential risks for patients in clinic practice. Furthermore, advanced training is necessary for those who interpret the CBCT images. Although there are some similarities between the root fractures with lateral canals and external root resorption on CBCT images, comprehensive evaluation of axial, coronal, and sagittal images could be helpful for the differential diagnosis.
Footnotes
Contributors: Antian Gao contributed to data acquisition, and drafted this manuscript. Dantong Cao contributed to data curation. Zitong Lin contributed to guidance of manuscript writing, and founding acquisition. All authors gave final approval and agree to be accountable for all aspects of the work.
Contributor Information
Antian Gao, Email: gaoantian_1995@163.com.
Dantong Cao, Email: 896999194@qq.com.
Zitong Lin, Email: linzitong_710@163.com.
REFERENCES
- 1.Kahler W. The cracked tooth conundrum: terminology, classification, diagnosis, and management. Am J Dent 2008; 21: 275–82. [PubMed] [Google Scholar]
- 2.Rivera EM, Walton RE. Longitudinal tooth fractures: findings that contribute to complex endodontic diagnoses. Endod Topics 2007; 16: 82–111. doi: 10.1111/j.1601-1546.2009.00243.x [DOI] [Google Scholar]
- 3.Rivera EM, Williamson A. Diagnosis and treatment planning: cracked tooth. Tex Dent J 2003; 120: 278–83. [PubMed] [Google Scholar]
- 4.Seo D-G, Yi Y-A, Shin S-J, Park J-W. Analysis of factors associated with cracked teeth. J Endod 2012; 38: 288–92. doi: 10.1016/j.joen.2011.11.017 [DOI] [PubMed] [Google Scholar]
- 5.Hasan S, Singh K, Salati N. Cracked tooth syndrome: overview of literature. Int J Appl Basic Med Res 2015; 5: 164–8. doi: 10.4103/2229-516X.165376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kang SH, Kim BS, Kim Y. Cracked teeth: distribution, characteristics, and survival after root canal treatment. J Endod 2016; 42: 557–62. doi: 10.1016/j.joen.2016.01.014 [DOI] [PubMed] [Google Scholar]
- 7.Huang C-C, Chang Y-C, Chuang M-C, Lin H-J, Tsai Y-L, Chang S-H, et al. Analysis of the width of vertical root fracture in endodontically treated teeth by 2 micro-computed tomography systems. J Endod 2014; 40: 698–702. doi: 10.1016/j.joen.2013.12.015 [DOI] [PubMed] [Google Scholar]
- 8.Brady E, Mannocci F, Brown J, Wilson R, Patel S. A comparison of cone beam computed tomography and periapical radiography for the detection of vertical root fractures in nonendodontically treated teeth. Int Endod J 2014; 47: 735–46. doi: 10.1111/iej.12209 [DOI] [PubMed] [Google Scholar]
- 9.Neves FS, Freitas DQ, Campos PSF, Ekestubbe A, Lofthag-Hansen S. Evaluation of cone-beam computed tomography in the diagnosis of vertical root fractures: the influence of imaging modes and root canal materials. J Endod 2014; 40: 1530–6. doi: 10.1016/j.joen.2014.06.012 [DOI] [PubMed] [Google Scholar]
- 10.Guo XL, Li G, Zheng JQ, Ma RH, Liu FC, Yuan FS, et al. Accuracy of detecting vertical root fractures in non-root filled teeth using cone beam computed tomography: effect of voxel size and fracture width. Int Endod J 2019; 52: 887–98. doi: 10.1111/iej.13076 [DOI] [PubMed] [Google Scholar]
- 11.Wang P, Yan XB, Lui DG, Zhang WL, Zhang Y, Ma XC. Detection of dental root fractures by using cone-beam computed tomography. Dentomaxillofac Radiol 2011; 40: 290–8. doi: 10.1259/dmfr/84907460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Edlund M, Nair MK, Nair UP. Detection of vertical root fractures by using cone-beam computed tomography: a clinical study. J Endod 2011; 37: 768–72. doi: 10.1016/j.joen.2011.02.034 [DOI] [PubMed] [Google Scholar]
- 13.Kamburoğlu K, Murat S, Yüksel SP, Cebeci ARI, Horasan S. Detection of vertical root fracture using cone-beam computerized tomography: an in vitro assessment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: e74–81. doi: 10.1016/j.tripleo.2009.09.005 [DOI] [PubMed] [Google Scholar]
- 14.Makeeva IM, Byakova SF, Novozhilova NE, Adzhieva EK, Golubeva GI, Grachev VI, et al. Detection of artificially induced vertical root fractures of different widths by cone beam computed tomography in vitro and in vivo. Int Endod J 2016; 49: 980–9. doi: 10.1111/iej.12549 [DOI] [PubMed] [Google Scholar]
- 15.Metska ME, Aartman IHA, Wesselink PR, Özok AR. Detection of vertical root fractures in vivo in endodontically treated teeth by cone-beam computed tomography scans. J Endod 2012; 38: 1344–7. doi: 10.1016/j.joen.2012.05.003 [DOI] [PubMed] [Google Scholar]
- 16.Lee S-H, Lee J-J, Chung H-J, Park J-T, Kim H-J. Dental optical coherence tomography: new potential diagnostic system for cracked-tooth syndrome. Surg Radiol Anat 2016; 38: 49–54. doi: 10.1007/s00276-015-1514-8 [DOI] [PubMed] [Google Scholar]
- 17.Wang S, Xu Y, Shen Z, Wang L, Qiao F, Zhang X, et al. The extent of the crack on artificial simulation models with CBCT and periapical radiography. PLoS One 2017; 12: e0169150. doi: 10.1371/journal.pone.0169150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alassaad SS. Incomplete cusp fractures: early diagnosis and communication with patients using fiber-optic transillumination and intraoral photography. Gen Dent 2011; 59: 132–5. [PubMed] [Google Scholar]
- 19.Tan L, Chen NN, Poon CY, Wong HB. Survival of root filled cracked teeth in a tertiary institution. Int Endod J 2006; 39: 886–9. doi: 10.1111/j.1365-2591.2006.01165.x [DOI] [PubMed] [Google Scholar]
- 20.Zhang L, Wang T, Cao Y, Wang C, Tan B, Tang X, et al. In vivo detection of subtle vertical root fracture in endodontically treated teeth by cone-beam computed tomography. J Endod 2019; 45: 856–62. doi: 10.1016/j.joen.2019.03.006 [DOI] [PubMed] [Google Scholar]
- 21.Patel S, Brown J, Semper M, Abella F, Mannocci F. European society of endodontology position statement: use of cone beam computed tomography in endodontics: European society of endodontology (ESE) developed by. Int Endod J 2019; 52: 1675–8. doi: 10.1111/iej.13187 [DOI] [PubMed] [Google Scholar]
- 22.da Silveira PF, Vizzotto MB, Liedke GS, da Silveira HLD, Montagner F, da Silveira HED. Detection of vertical root fractures by conventional radiographic examination and cone beam computed tomography - an in vitro analysis. Dent Traumatol 2013; 29: 41–6. doi: 10.1111/j.1600-9657.2012.01126.x [DOI] [PubMed] [Google Scholar]
- 23.Schulze R, Heil U, Gross D, Bruellmann DD, Dranischnikow E, Schwanecke U, et al. Artefacts in CBCT: a review. Dentomaxillofac Radiol 2011; 40: 265–73. doi: 10.1259/dmfr/30642039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brito-Júnior M, Santos LAN, Faria-e-Silva AL, Pereira RD, Sousa-Neto MD. Ex vivo evaluation of artifacts mimicking fracture lines on cone-beam computed tomography produced by different root canal sealers. Int Endod J 2014; 47: 26–31. doi: 10.1111/iej.12121 [DOI] [PubMed] [Google Scholar]
- 25.Corbella S, Del Fabbro M, Tamse A, Rosen E, Tsesis I, Taschieri S. Cone beam computed tomography for the diagnosis of vertical root fractures: a systematic review of the literature and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 2014; 118: 593–602. doi: 10.1016/j.oooo.2014.07.014 [DOI] [PubMed] [Google Scholar]
- 26.Brooks SL, Ludlow JB. Cone beam computed tomography in orthodontics: Perspectives on radiation risk. : Kapila S. D, Cone beam computed tomography in orthodontics: Indications, insights, and innovations. New Jersey, PA: John Wiley & Sons Inc; 2014. . 67–80. [Google Scholar]
- 27.Ma RH, Ge ZP, Li G. Detection accuracy of root fractures in cone-beam computed tomography images: a systematic review and meta-analysis. Int Endod J 2016; 49: 646–54. doi: 10.1111/iej.12490 [DOI] [PubMed] [Google Scholar]
- 28.Uzun I, Gunduz K, Celenk P, Avsever H, Orhan K, Canitezer G, et al. Comparing the effect of different voxel resolutions for assessment of vertical root fracture of permanent teeth. Iran J Radiol 2015; 12: e18290. doi: 10.5812/iranjradiol.18290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parsa A, Ibrahim N, Hassan B, van der Stelt P, Wismeijer D. Influence of object location in cone beam computed tomography (newtom 5G and 3D Accuitomo 170) on gray value measurements at an implant site. Oral Radiol 2: 153–9. doi: 10.1007/s11282-013-0157-x [DOI] [Google Scholar]
- 30.Valizadeh S, Vasegh Z, Rezapanah S, Safi Y, Khaeazifard MJ. Effect of object position in cone beam computed tomography field of view for detection of root fractures in teeth with intra-canal posts. Iran J Radiol 2015; 12: e25272. doi: 10.5812/iranjradiol.25272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nikbin A, Dalili Kajan Z, Taramsari M, Khosravifard N. Effect of object position in the field of view and application of a metal artifact reduction algorithm on the detection of vertical root fractures on cone-beam computed tomography scans: An in vitro study. Imaging Sci Dent 2018; 48: 245–54. doi: 10.5624/isd.2018.48.4.245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hanzelka T, Foltán R, Horká E, Sedý J. Reduction of the negative influence of patient motion on quality of CBCT scan. Med Hypotheses 2010; 75: 610–2. doi: 10.1016/j.mehy.2010.07.046 [DOI] [PubMed] [Google Scholar]
- 33.Spin-Neto R, Mudrak J, Matzen LH, Christensen J, Gotfredsen E, Wenzel A. Cone beam CT image artefacts related to head motion simulated by a robot skull: visual characteristics and impact on image quality. Dentomaxillofac Radiol 2013; 42: 32310645. doi: 10.1259/dmfr/32310645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spin-Neto R, Matzen LH, Schropp L, Sørensen TS, Gotfredsen E, Wenzel A. Accuracy of video observation and a three-dimensional head tracking system for detecting and quantifying robot-simulated head movements in cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol 2017; 123: 721–8. doi: 10.1016/j.oooo.2017.02.010 [DOI] [PubMed] [Google Scholar]
- 35.Yeung AWK, Azevedo B, Scarfe WC, Bornstein MM. Patient motion image artifacts can be minimized and re-exposure avoided by selective removal of a sequence of basis images from cone beam computed tomography data sets: a case series. Oral Surg Oral Med Oral Pathol Oral Radiol 2020; 129: e212–23. doi: 10.1016/j.oooo.2019.07.003 [DOI] [PubMed] [Google Scholar]
- 36.Gu J, Bae W, Ye JC. Translational motion correction algorithm for truncated cone-beam CT using opposite projections. J Xray Sci Technol 2017; 25: 927–44. doi: 10.3233/XST-16231 [DOI] [PubMed] [Google Scholar]
- 37.Santaella GM, Wenzel A, Haiter-Neto F, Rosalen PL, Spin-Neto R. Impact of movement and motion-artefact correction on image quality and interpretability in CBCT units with aligned and lateral-offset detectors. Dentomaxillofac Radiol 2020; 49: 20190240. doi: 10.1259/dmfr.20190240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lira de Farias Freitas AP, Cavalcanti YW, Costa FCM, Peixoto LR, Maia AMA, Rovaris K, et al. Assessment of artefacts produced by metal posts on CBCT images. Int Endod J 2019; 52: 223–36. doi: 10.1111/iej.12999 [DOI] [PubMed] [Google Scholar]
- 39.Dutra KL, Pachêco-Pereira C, Bortoluzzi EA, Flores-Mir C, Lagravère MO, Corrêa M. Influence of intracanal materials in vertical root fracture pathway detection with cone-beam computed tomography. J Endod 2017; 43: 1170–5. doi: 10.1016/j.joen.2017.02.006 [DOI] [PubMed] [Google Scholar]
- 40.Patel S, Brady E, Wilson R, Brown J, Mannocci F. The detection of vertical root fractures in root filled teeth with periapical radiographs and CBCT scans. Int Endod J 2013; 46: 1140–52. doi: 10.1111/iej.12109 [DOI] [PubMed] [Google Scholar]
- 41.de Rezende Barbosa GL, Sousa Melo SL, Alencar PNB, Nascimento MCC, Almeida SM. Performance of an artefact reduction algorithm in the diagnosis of in vitro vertical root fracture in four different root filling conditions on CBCT images. Int Endod J 2016; 49: 500–8. doi: 10.1111/iej.12477 [DOI] [PubMed] [Google Scholar]
- 42.Khedmat S, Rouhi N, Drage N, Shokouhinejad N, Nekoofar MH. Evaluation of three imaging techniques for the detection of vertical root fractures in the absence and presence of gutta-percha root fillings. Int Endod J 2012; 45: 1004–9. doi: 10.1111/j.1365-2591.2012.02062.x [DOI] [PubMed] [Google Scholar]
- 43.Schulze R, Heil U, Gross D, Bruellmann DD, Dranischnikow E, Schwanecke U, et al. Artefacts in CBCT: a review. Dentomaxillofac Radiol 2011; 40: 265–73. doi: 10.1259/dmfr/30642039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Salineiro FCS, Kobayashi-Velasco S, Braga MM, Cavalcanti MGP, Fcs S, Mgp C. Radiographic diagnosis of root fractures: a systematic review, meta-analyses and sources of heterogeneity. Dentomaxillofac Radiol 2017; 46: 20170400. doi: 10.1259/dmfr.20170400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.de Rezende Barbosa GL, Sousa Melo SL, Alencar PNB, Nascimento MCC, Almeida SM. Performance of an artefact reduction algorithm in the diagnosis of in vitro vertical root fracture in four different root filling conditions on CBCT images. Int Endod J 2016; 49: 500–8. doi: 10.1111/iej.12477 [DOI] [PubMed] [Google Scholar]
- 46.De Martin E Silva D, Campos CN, Pires Carvalho AC, Devito KL. Diagnosis of mesiodistal vertical root fractures in teeth with metal posts: influence of applying filters in cone-beam computed tomography images at different resolutions. J Endod 2018; 44: 470–4. doi: 10.1016/j.joen.2017.08.030 [DOI] [PubMed] [Google Scholar]
- 47.Bechara BB, Moore WS, McMahan CA, Noujeim M. Metal artefact reduction with cone beam CT: an in vitro study. Dentomaxillofac Radiol 2012; 41: 248–53. doi: 10.1259/dmfr/80899839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Helvacioglu-Yigit D, Demirturk Kocasarac H, Bechara B, Noujeim M. Evaluation and reduction of artifacts generated by 4 different root-end filling materials by using multiple cone-beam computed tomography imaging settings. J Endod 2016; 42: 307–14. doi: 10.1016/j.joen.2015.11.002 [DOI] [PubMed] [Google Scholar]
- 49.Chavda R, Mannocci F, Andiappan M, Patel S. Comparing the in vivo diagnostic accuracy of digital periapical radiography with cone-beam computed tomography for the detection of vertical root fracture. J Endod 2014; 40: 1524–9. doi: 10.1016/j.joen.2014.05.011 [DOI] [PubMed] [Google Scholar]
- 50.Yuan M, Gao AT, Wang TM, Liang JH, Aihemati GB, Cao Y, et al. Using meglumine diatrizoate to improve the accuracy of diagnosis of cracked teeth on cone-beam CT images. Int Endod J 2020; 53: 709–14. doi: 10.1111/iej.13270 [DOI] [PubMed] [Google Scholar]
- 51.Talwar S, Utneja S, Nawal RR, Kaushik A, Srivastava D, Oberoy SS. Role of cone-beam computed tomography in diagnosis of vertical root fractures: a systematic review and meta-analysis. J Endod 2016; 42: 12–24. doi: 10.1016/j.joen.2015.09.012 [DOI] [PubMed] [Google Scholar]
- 52.Ahmed HMA, Neelakantan P, Dummer PMH. A new system for classifying accessory canal morphology. Int Endod J 2018; 51: 164–76. doi: 10.1111/iej.12800 [DOI] [PubMed] [Google Scholar]
- 53.Ji Y, Wen S, Liu S, Zhu M, Yao M, Wang T, et al. Could cone-beam computed tomography demonstrate the lateral accessory canals? BMC Oral Health 2017; 17: 142–9. doi: 10.1186/s12903-017-0430-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Neves FS, Vasconcelos TV, Vaz SLA, Freitas DQ, Haiter-Neto F. Evaluation of reconstructed images with different voxel sizes of acquisition in the diagnosis of simulated external root resorption using cone beam computed tomography. Int Endod J 2012; 45: 234–9. doi: 10.1111/j.1365-2591.2011.01966.x [DOI] [PubMed] [Google Scholar]
- 55.Hassan B, Metska ME, Ozok AR, van der Stelt P, Wesselink PR. Comparison of five cone beam computed tomography systems for the detection of vertical root fractures. J Endod 2010; 36: 126–9. doi: 10.1016/j.joen.2009.09.013 [DOI] [PubMed] [Google Scholar]