Abstract
Objectives:
To evaluate and compare the accuracy of high-resolution ultrasound (US) with two different cone beam CT (CBCT) units and clinical assessment for measuring gingival soft tissue thickness in edentulous patients prior to implant placement.
Methods and materials:
The study consisted of 40 maxillary implant sites of 40 healthy patients (20 females, 20 males; mean age, 47.88 years). We prospectively evaluated labial/buccal gingival thickness in 40 implant regions (16 anterior and 24 posterior) by using limited field of view (FOV) CBCT images and US images in comparison to gold standard transgingival probing measurements. One-way analysis of variance (ANOVA) was used to compare mean measurements obtained from CBCT (Morita and Planmeca), US, and transgingival probing. Interclass correlation coefficient (ICC) estimates were calculated based on means with two-way mixed and absolute-agreement model. Bland Altman plot was used to describe agreement between clinical vs US and CBCT measurements by constructing limits of agreement. Statistical significance was set at p < 0.05.
Results:
There was no significant difference between methods used according to mean gingival thickness measurements obtained from the top (p = 0.519) and bottom (p = 0.346) of the alveolar process. US and CBCT measurements highly correlated with clinical measurements for both top and bottom alveolar process gingival thickness (p < 0.001). Distribution of differences between clinical measurements and both CBCT measurements showed statistically significant differences according to 0 (p < 0.05). Distribution of differences between clinical measurements and US measurements did not show statistically significant difference (p > 0.05).
Conclusion:
High-resolution US provided accurate information for the measurement of gingival soft tissue thickness in edentulous patients prior to implant placement.
Keywords: Ultrasonography, Dental implantation, Gingival thickness, Measurement
Introduction
Successful dental implant therapy requires long-term maintenance of both soft and hard tissues surrounding the implant. It is apparent that in order to gain more insight into the factors affecting the success and failure of implant therapy; long-term clinical evaluation of dental implants and their superstructure is necessary. Researchers focused on various parameters including mobility, pain, infection, inflammation and marginal bone levels.1 Recently, soft tissue assessment of implant sites prior to implant placement became an integral part of dental implantation procedures due to the optimization of aesthetics with particular emphasis given to the measurement of soft tissue thickness of marginal bone surrounding the implant.2,3
Gingival tissue thickness and width namely the “gingival biotype” plays an important role in the maintenance of esthetics, function and periodontal health.4,5 Generally, gingival thickness less than 1 mm is considered as a thin biotype, whereas gingival thickness more than 1 mm is considered as a thick biotype.6 Clinically, thin gingival biotypes are correlated with long crowns and scalloped gingival contours. When compared to patients with thick gingival biotype, the incidence of gingival recession is higher in patients with thin gingival biotype and their response to regenerative treatment is less favourable during periodontal and peri-implant tissue procedures. On the other hand, patients with thick gingival biotype show clinically shorter crowns and less scalloped gingival contours. Patients with thick biotype show lower incidence of gingival recession following periodontal and peri-implant treatment procedures along with higher success rates in regenerative treatment.7,8
Various methods have been utilized in order to assess and measure gingival tissue thickness. Assessment of soft tissues by periodontal probing is an essential tool for the measurement of gingival recession, keratinized mucosa and papillary height in routine clinical practice. Besides, the use of periodontal probing was also suggested for the determination of gingival biotype.9 Another invasive technique that is used to assess soft tissue thickness is transgingival probing. After local anaesthesia, periodontal probe or an injection needle is vertically placed on the mucosal surface until touching the bone.10 This technique also has the potential to be used for the determination of alveolar bone level.11
Authors defined another technique called parallel profile radiography that enabled measurement of the buccal gingival tissue of anterior teeth. However, two-dimensional periapical radiography techniques have inherent disadvantages due to projection geometry.12 Today, in order to enable appropriate placement of implants, data obtained by cone beam CT (CBCT) provide a pre-operative view of critical anatomical structures in the jaw along with bone-quality assessment and prosthetic considerations. CBCT has the advantages of acceptable patient dose, ease of usage, fast scanning, cost-effectiveness, and high bone quality images with sub-millimeter accuracy. Disadvantages associated with CBCT include higher patient dose compared to two-dimensional imaging, scatter radiation, limited dynamic range, minimal soft-tissue detail, and beam hardening artifacts caused by dental-care materials and implants.13 Although CBCT images were not suggested as the primary choice for the evaluation of soft tissues, some authors conducted gingival tissue measurements from CBCT images. Main drawback of CBCT measurements is that neighbouring tissues such as lips and cheeks may interfere with gingival tissue, disabling partial, or total radiological visibility, specifically in the labial surfaces. In order to overcome this disadvantage, acrylic lip retractors or wooden spatulas may be used during CBCT imaging. By this non-invasive technique, lip and cheek tissues are retracted and thereby visualization of gingival soft tissues are improved.14–18
Various authors proposed ultrasound (US) to be utilized for gingival tissue thickness measurement as a non-invasive technique.19–23 US imaging has been specifically proposed as an alternative technique that can provide on-site, real-time images at a low cost and without ionizing radiation. In diagnostic US, high-frequency sound waves are transmitted into the body by use of a transducer and echoes from tissue interface are detected and displayed on a screen. Sound waves are emitted via piezoelectric crystals from the US transducer.24 Although, US is frequently used in almost all fields of general medicine, its application in dentistry is limited since high-resolution, small-sized and intra-oral probes were not readily available for dental health. However, recent developments lead to the production of very small-sized probes with high image quality. Schulze et al by using 10 MHz intra-operative probe assessed the effectiveness of US with A-mode and B-mode by comparing to transgingival probing conducted by injection needle at palatal mucosa in 50 volunteers.25 Authors of another study, utilized specific customized soft tissue-matched transducer and signal processing algorithm in order to locate sub-gingival implant and determine its depth in the soft tissue ex vivo.26 In addition, researchers utilized US for the follow-up of dimensional changes in the peri-implant soft tissues after grafting procedures.20,27
To our knowledge, no previous in vivo study compared available techniques including transgingival probing, CBCT and US for the measurement of gingival soft tissue thickness that is an essential part of implant success. Considering the potential differences between various methods utilized to assess gingival soft tissue our objective was to evaluate and compare the accuracy of high-resolution US with two different CBCT units and clinical transgingival probing for measuring soft tissue thickness in edentulous patients prior to implant placement.
Materıals and Methods
This research was conducted in accordance with the Helsinki declaration of 1975 as revised in 2013 and the study protocol was approved by Institutional Review Board of the Başkent University Medicine and Health Science Council (Project no. D-KA-17/13).
Patient selection and data collection
Patients ≥ 18 years of age scheduled for implant surgery were included in the present study. Patients who had systemic chronic disease and had pathology in the implant region were excluded. Informed consent was obtained for each patient. The study consisted of 40 maxillary implant sites of 40 healthy patients (20 females, 20 males; age range, 21–74 years; mean age, 47.88 years) who had been examined at the Ankara University Faculty of Dentistry and Başkent University, Faculty of Dentistry, Ankara, Turkey for missing teeth. Labial/Buccal gingival thickness for each patient was assessed by CBCT, US, and transgingival probing prior to implant surgery. Implant regions were divided into two groups as follows: Group 1 (implant regions including missing incisors and canine – anterior group); and Group 2 (implant regions including missing premolars and molars – posterior group). We prospectively evaluated labial/buccal gingival thickness in 40 implant regions (16 anterior and 24 posterior) by using limited field of view (FOV) CBCT images and US images in comparison with transgingival probing measurements.
CBCT imaging and analysis
CBCT images of 20 patients were obtained by using a Planmeca Promax 3D max CBCT unit (Planmeca, Helsinki, Finland) at 90 kVp, 7mA, and a 0.2 mm voxel size using 55×50 mm limited FOV and CBCT images of the other 20 patients were obtained by using Morita 3D Accuitomo 170® (J Morita, Kyoto, Japan) at 90 kVp, 5mA, and a 0.08 mm voxel size using 40×40 mm limited FOV. CBCT examinations were conducted by placing an acrylic lip retractor (Angle Wider, Swedish Dental Supplies AB, AKARP, Sweden) in order to image the soft tissue with better detail. Prior to image analysis, a calibration session was conducted in order to carry out pilot measurements on 10 CBCT images those were not included in the study. A dentomaxillofacial specialty student under the supervision of an experienced dentomaxillofacial specialist (20 years of clinical experience) performed assessments from multiplanar reformatted and cross-sectional images. For the image interpretation protocol, dedicated softwares of both CBCT units were used. Images were viewed on a 21.3-inch medical diagnostic monitor at 2048×1536 resolution (NEC, Tokyo, Japan) in a dimly lit room. Cross-sectional images were created from the arch that was drawn in the implant region. The longitudinal axis of the nearest tooth adjacent to the implant site was determined and the horizontal intersection point perpendicular to this axis was selected at the cemento-enamel junction level and measurements on CBCT cross-sectional images were conducted 5 mm far away from this intersection point. For each implant site, labial/buccal soft tissue thickness measurements were performed perpendicular to the alveolar process at two different points; top of the alveolar process and bottom of the alveolar process on CBCT images by using measurement tools in mm (Figure 1a–e). Average of 2 measurements were noted for each site. Mucogingival line where attached gingiva ends with alveolar mucosa were determined as the bottom measurement point in order to eliminate misinterpretation of gingival thickness due to lip retraction. The distance between top of alveolar process and bottom of alveolar process was vertically measured in order to evaluate same points as with US images (Figure 1a–e).
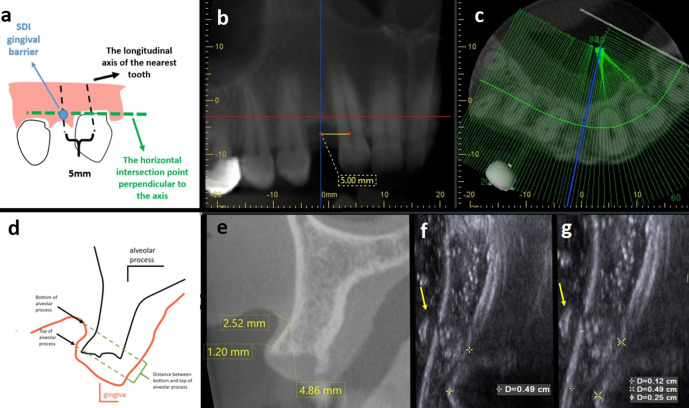
Figure 1.
Gingival soft tissue thickness measurement of the same implant region conducted by CBCT (i-Dixel Software, Morita 3D Accuitomo 170®, J Morita, Kyoto, Japan) and US ACUSON S 2000 (Siemens, Munich, Germany) in mm and cm.) (a) Schematic drawing of reference point determination. Black arrow shows the longitudinal axis of nearest adjacent tooth and 5 mm distance on cemento-enamal junction level; green arrow shows the horizontal intersection point perpendicular to long axis; blue circle and arrow show SDI gingival barrier. (b) Representative panoramic view showing 5 mm distance measurement between longitudinal axis of adjacent tooth; blue line corresponds to selected cross-sectional image. (c) Axial CBCT image: blue line corresponds to selected cross-sectional image. (d) Representative schematic drawing of reference point determination. (e) Representative CBCT image of the drawing shown in (d). Labial/buccal soft tissue thickness measurements were performed perpendicular to alveolar process at two different points; top of the alveolar process and bottom of the alveolar process on CBCT images by using measurement tools in mm. The distance between top of alveolar process and bottom (f) Vertical distance measurement between reference points was found to be 0.49 cm in US image. Hyperechogenic barrier was used as reference point for mesiodistal location of measurement point. Yellow arrow shows hyperechogenic gingival barrier. (g) In US images gingival thickness measurement of top and bottom of alveolar process was 0.12 cm and 0.25 cm, respectively.
US imaging and analysis
US examinations were performed by using an ACUSON S 2000 (Siemens, Munich, Germany) high-resolution ultrasonography by the same researcher who conducted CBCT measurements. Similar to CBCT measurement, the longitudinal axis of the nearest tooth adjacent to the implant site was determined and gingival barrier was placed 5 mm far away from this reference point. Gingiva was dried with air spray and SDI gingival barrier (SDI (North America) Inc., Itasca, IL, USA) was injected on the reference point by using its own syringe and then light cured in fanning motion. Prior to US examination, implant sites were isolated from saliva and the same region measured on CBCT image was detected clinically and marked with SDI gingival barrier as reference poınt. SDI gıngıval barrıer is a 75–80% weighted acrylic monomer, light cure, tissue isolation material specifically used for tooth bleaching by dental professionals (Figure 2a, b). A 15 MHz hockey (stick) probe covered with ultrasonography gel and sterile sheath was performed intraorally on the longitudinal plane, with the probe position changed constantly to obtain sufficient cross-sectional images on the monitor (Figure 2a, b). The transducer was positioned perpendicular to alveolar process in order to enable cross-sectional assessment of the implant site. For the dimensional evaluation of gingival thickness, gingival barrier, seen as hyperechogenic with anechogenic shadow, was used as the reference point on the US images. Once the hyperechogenic barrier was detected, top of the alveolar process was visually determined according to its anatomy and then distance between top of the alveolar process and bottom of the alveolar process was measured vertically on US image and thus bottom of alveolar process point was detected on US images and gingival thickness measurement of the bottom alveolar process was conducted (Figure 1a–g). For each implant site, metric measurement of soft tissue thickness in cm was performed at the same two points, which were calculated on CBCT images. Average of 2 measurements were noted for each site. Figure 3 shows gingival soft tissue thickness measurement of the same implant region conducted by CBCT (i-Dixel Software, Morita 3D Accuitomo 170®, J Morita, Kyoto, Japan) in mm and US ACUSON S 2000 (Siemens, Munich, Germany) in cm. Gingival soft tissue thickness measurement of the same implant region conducted by CBCT and US measurements is shown in Figure 3.
Figure 2.
(a) Gingival barrier placement prior to US examination. Black arrow shows acrylic gingival barrier. (b) A 15 MHz hockey (stick) probe was covered with ultrasonography gel and sterile sheath and the transducer was positioned perpendicular to alveolar process in order to enable cross-sectional assessment of the implant site.
Figure 3.
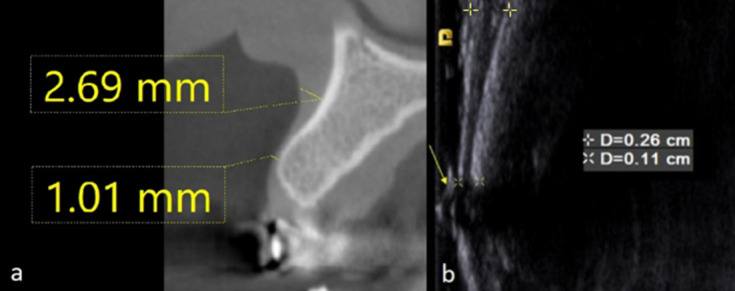
Gingival soft tissue thickness measurement of the same implant region conducted by CBCT (i-Dixel Software, Morita 3D Accuitomo 170®, J Morita, Kyoto, Japan) and US ACUSON S 2000 (Siemens, Munich, Germany) in mm and cm, respectıvely. Gingival soft tissue thickness measurement of the same implant region conducted by CBCT and US. (a) Soft tissue measurement was conducted on CBCT images perpendicular to the alveolar process at two different points: top of alveolar process and bottom of alveolar process. (b) Soft tissue measurement on US images perpendicular to the alveolar process at two different points: top of alveolar process and bottom of alveolar process. Yellow arrow shows hyperechogenic gingival barrier.
Gold standard clinical analysis
Gingival soft tissue thickness of each implant site was also measured clinically at the same reference points. For clinical measurement of gingival soft tissues, same reference point marked with SDI gingival barrier was also used as the reference point. Clinical gingival soft tissue thickness measurement was performed by transgingival probing with the use of an injection needle with a silicon disc stopper and an electronic digital caliper (Allendale Electronics Ltd., Hertfordshire, UK) with fine-pointed jaws and measuring range of 0–200 mm (0–8.0 inch) and a resolution of 0.01 mm (0.0005 inch). Transgingival probing with injection needle were used as gold standard methodology due to it’s higher accuracy when compared to direct gingival tissue thickness measurement.28 The clinical measurements were considered as “gold standard” for the assessment of gingival soft tissue thickness. All measurements obtained from CBCT and US images were then compared with clinical measurements.
Statistical analysis
CBCT (Morita and Planmeca), US, and clinical measurements obtained from top of the alveolar process and bottom of the alveolar process for groups were given as mean ± standart error. Prior to data analysis, in order to assess normal distribution and homogeneity of variance Shapiro-Wilk and Levene Tests were used. One-way analysis of variance (ANOVA) was used to compare mean measurements of CBCT (Morita and Planmeca), US, and transgingival probing. The distribution of the measurement differences of CBCT (Morita and Planmeca), and US, from clinical gold standard was determined by single sample (one) test. Interclass correlation coefficient (ICC) estimates were calculated based on means with two-way mixed and absolute-agreement model. Bland-Altman plot was used to describe agreement between clinical vs US and CBCT measurements by constructing limits of agreement. SPSS v.21 (SPSS Inc., Chicago, IL, USA) and bland package of R (v.3.2.0) statistical software were used for data analysis. Statistical significance was set at p < 0.05.
Results
Mean age was 47 (minimum 21 and maximum 74) for female patients and 48.8 (minimum 30 and maximum 66) for male patients. Descriptive statistics for gingival thickness measurements obtained from top and bottom alveolar process by using different methods were presented as “Mean ± Standard Error” in Table 1. Gingival thickness at the top of the crest ranged between 0.71 and 3.18 mm for clinical measurements, 0.6 and 2.8 mm for US measurements, 0.5 and 2.97 mm for Morita CBCT measurements, and 0.89 and 2.71 mm for Planmeca CBCT measurements. Gingival thickness at the bottom of the crest ranged between 1.14 and 4.12 mm for clinical measurements, 1.3 and 4.2 mm for US measurements, 1.12 and 3.25 mm for Morita CBCT measurements, and 0.89 and 2.71 mm for Planmeca CBCT measurements.
Table 1.
Descriptive statistics as mean and standard error (se) for the anterior and posterior region gingival thickness measurements for different methods. One-way analysis of variance (ANOVA); p < 0.05
| n | Top of Alveolar Process Mean ± SE | Bottom of Alveolar Process Mean ± SE | ||||
|---|---|---|---|---|---|---|
| Clinical Measurement | 40 | 1.72 ± 0.0895 | p = 0.519 | 2.55 ± 0.127 | p = 0.346 | |
| Morita CBCT Planmeca CBCT |
20 | 1.75 ± 0.136 | 2.27 ± 0.149 | |||
| 20 | 1.50 ± 0.126 | 2.69 ± 0.192 | ||||
| US | 40 | 1.69 ± 0.0912 | 2.50 ± 0.111 | |||
| Anterior Region | ||||||
| Top of Alveolar Process | Bottom of Alveolar Process | |||||
| n | Mean ± SE | p = 0.876 | n | Mean ± SE | p = 0.644 | |
| Clinical Measurement | 7 | 1.74 ± 0.188 | 7 | 2.76 ± 0.174 | ||
| Morita CBCT | 7 | 1.63 ± 0.213 | 7 | 2.62 ± 0.172 | ||
| US | 7 | 1.8 ± 0.254 | 7 | 2.54 ± 0.134 | ||
| Clinical Measurement | 9 | 1.66 ± 0,189 | p = 0.924 | 9 | 2.92 ± 0.255 | p = 0.971 |
| Planmeca CBCT | 9 | 1.55 ± 0.205 | 9 | 2.91 ± 0.247 | ||
| US | 9 | 1.64 ± 0.244 | 9 | 2.84 ± 0.226 | ||
| Posterior Region | ||||||
| Top of Alveolar Process | Bottom of Alveolar Process | |||||
| n | Mean ± SE | p = 0.947 | n | Mean ± SE | p = 0.937 | |
| Clinical Measurement | 13 | 1.86 ± 0.168 | 13 | 2.16 ± 0.201 | ||
| Morita CBCT | 13 | 1.81 ± 0.179 | 13 | 2.08 ± 0.193 | ||
| US | 13 | 1.78 ± 0.166 | 13 | 2.17 ± 0.192 | ||
| Clinical Measurement | 11 | 1.57 ± 0.179 | p = 0.903 | 11 | 2.6 ± 0.29 | p = 0.973 |
| Planmeca CBCT | 11 | 1.46 ± 0.165 | 11 | 2.51 ± 0.283 | ||
| US | 11 | 1.53 ± 0.13 | 11 | 2.59 ± 0.24 | ||
According to one-way ANOVA analysis, there was no significant difference between mean differences obtained from different methods, for the top of the alveolar process (p = 0.519) and bottom of the alveolar process (p = 0.346) gingival thickness measurements. Analysis of mean differences between different methods for top and bottom of alveolar gingival thickness measurements according to one-way ANOVA analysis are shown in Figure 4a, b, respectively.
Figure 4.
Analysis of mean differences between methods used. (a) Analysis of mean differences between different methods for the top of alveolar process gingival thickness measurements according to one-way ANOVA analysis. (b) Analysis of mean differences between different methods for the bottom of alveolar process gingival thickness measurements according to one-way ANOVA analysis.
US and CBCT measurements highly correlated with clinical measurements suggesting a positive strong correlation for both top and bottom alveolar process gingival thickness (p < 0.001).
Table 1 shows descriptive statistics as mean and standard error for the anterior and posterior region gingival thickness measurements for different methods. For the anterior region, gingival thickness measurements obtained from CBCT Morita images were compared with those of clinical and US measurements. According to ANOVA analysis, there was no statistically significant difference for the mean differences between different methods for top crest (p = 0.876) and for bottom crest (p = 0.644) gingival thickness. Similarly, anterior region gingival thickness measurements obtained from CBCT Planmeca images were compared with those of clinical and US measurements. According to ANOVA analysis, there was no statistically significant difference for the mean differences between different methods for top crest (p = 0.924) and for bottom crest (p = 0.971).
For the posterior region, gingival thickness measurements obtained from CBCT Morita images were compared with those of clinical and US measurements. No statistically significant difference was observed for the mean differences between different methods for both top crest (p = 0.947) and bottom crest (p = 0.937). In addition, gingival thickness measurements obtained from CBCT Planmeca images were compared with those of clinical and US measurements. There was no statistically significant difference between different methods for top crest (p = 0.903) and bottom crest (p = 0.973) measurements.
Concordance between methods for top crest and bottom crest gingival thickness measurements were also assessed and given in Table 2. Distribution of differences between clinical and Morita CBCT measurements (Clinical and Morita); and clinical and Planmeca CBCT measurements (Clinical and Planmeca) showed statistically significant difference according to 0 (p < 0.05). However, distribution of differences between clinical and US measurements (Clinical and US) did not show statistically significant difference according to 0 (p > 0.05). (Table 2).
Table 2.
Assessment of the distribution of mean differences among groups by single sample (one) test
| Mean Differences | p value | ||
|---|---|---|---|
| Top of Alveolar Process | Clinical-US | 0.032 | 0.51 |
| Clinical-Morita CBCT | −0.075 | 0.018a | |
| Clinical-Planmeca CBCT | 0.1095 | 0.012a | |
| Bottom of Alveolar Process | Clinical-US | 0.0518 | 0.351 |
| Clinical-Morita CBCT | −0.1 | 0.014a | |
| Clinical-Planmeca CBCT | 0.051 | 0.376 |
shows statistically significant differences; p < 0.05.
ICC values calculated for the top alveolar process gingival thickness measurements between clinical and US, between clinical and Morita CBCT and between clinical and Planmeca CBCT were 0.925, 0.984, and 0.967, respectively. ICC values calculated for the bottom alveolar process gingival thickness measurements between clinical and US, between clinical and Morita CBCT and between clinical and Planmeca CBCT were 0.944, 0.981, and 0.979, respectively.
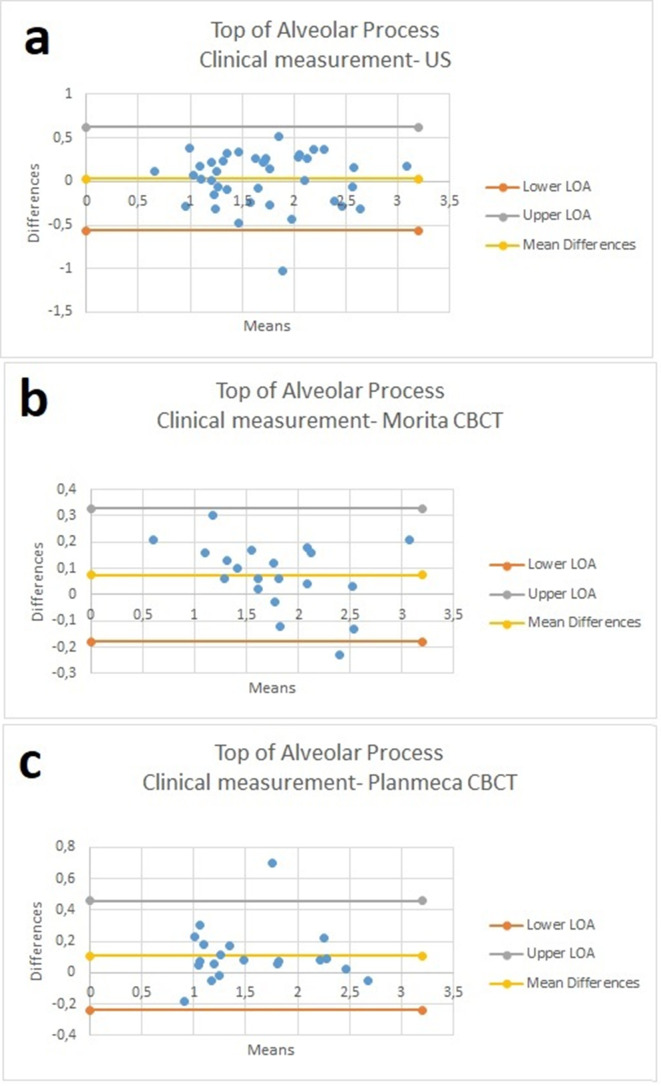
For the measurements performed at the top of alveolar process, mean difference between clinical and US measurements was found to be 0.032. For this difference, measurement of mean and standard variation with 95% CI limits of agreement was −0.56384 and 0.62784 (p = 0.51) (Figure 5a). For the measurements performed at the top of alveolar process, mean difference between clinical and Morita CBCT measurements was found to be 0.075. For this difference, measurement of mean and standard variation with 95% confidence interval limits of agreement was −0.17784 and 0.32784 (p = 0.0189) (Figure 5b). Similarly, mean difference between clinical and Planmeca CBCT measurements for the top of alveolar process was found to be 0.1095. For this difference, measurement of mean and standard variation with 95% CI limits of agreement was −0.23742 and 0.45642 (p = 0.012) (Figure 5c).
Figure 5.
Bland-Altman graphics for the measurements performed at the top of alveolar process. (a) Mean difference between clinical and US measurements was found to be 0.032. (b) Mean difference between clinical and Morita CBCT measurements was found to be 0.075.) (c) Mean difference between clinical and Planmeca CBCT measurements was found to be 0.1095.
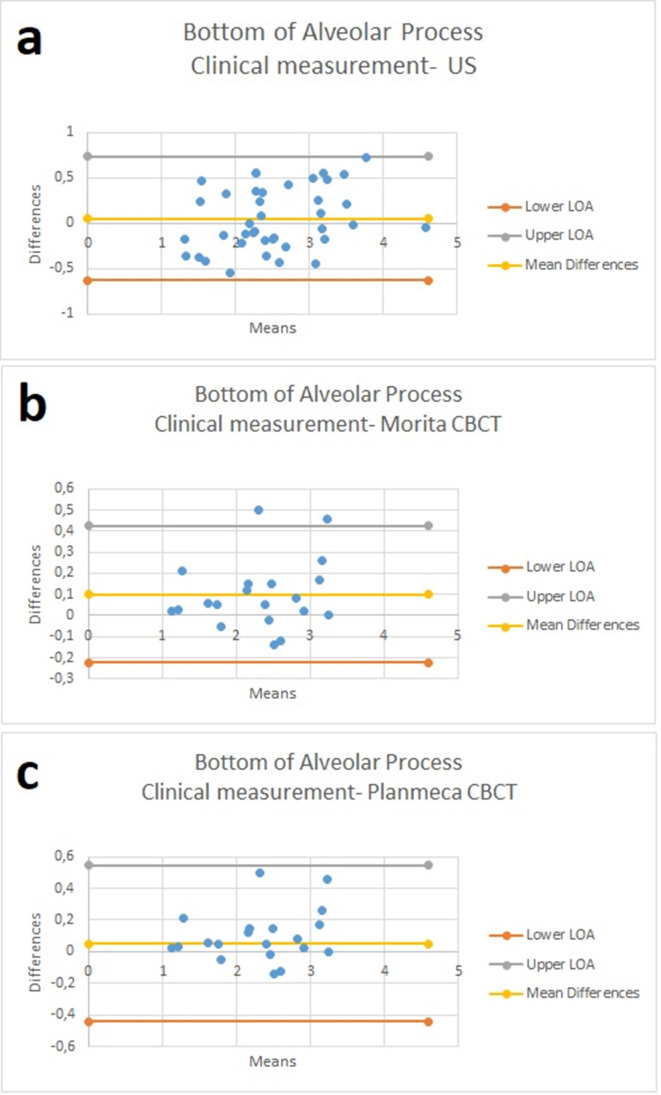
For the measurements performed at the bottom of alveolar process, mean difference between clinical and US measurements was found to be 0.0518. For this difference, measurement of mean and standard variation with 95% confidence interval limits of agreement was −0.62832 and 0.73192 (p = 0.351) (Figure 6a). For the bottom of alveolar process, mean difference between clinical measurement and Morita CBCT measurement was found to be 0.1. For this difference, measurement of mean and standard variation with 95% CI limits of agreement was −0.2234 and 0.4234 (p = 0.014) (Figure 6b). For the bottom of alveolar process, mean difference between clinical measurement and Planmeca CBCT measurement was found to be 0.051. For this difference measurement of mean and standard variation with 95% CI limits of agreement, −0.44292 and 0.54492 (p = 0.376) (Figure 6c).
Figure 6.
Bland-Altman graphics for the measurements performed at the bottom of alveolar process. (a) Mean difference between clinical and US measurements was found to be 0.0518.) (b) Mean difference between clinical measurement and Morita CBCT measurement was found to be 0.1). (c) Mean difference between clinical measurement and Planmeca CBCT measurement was found to be 0.051.
Discussion
In recent years, aesthetic considerations became more important for the rehabilitation of implant patients making measurement of gingival thickness essential prior to surgery. This research was the first to assess and compare high-resolution US and CBCT imaging techniques in comparison to clinical transgingival probing for the assessment of gingival soft tissue thickness in implant patients. We found highly accurate measurements with US imaging for the assessment of gingival soft tissue in terms of gingival thickness measurement at the top and bottom of the alveolar process. We found that for all implant site measurements obtained from high-resolution US images and two different types of CBCT images highly correlated with those of direct clinical measurements. Since measurement site was very limited, mean differences were assessed against 0 and mean differences showed significant difference for both CBCT units at both top crest and bottom crest gingival sites. CBCT performance decreased as gingival thickness decreased. This finding may be attributable to observer performance that is dependent on sub-millimeter measurement sensitivity of CBCT software tools. Invasive techniques like transgingival probing were used for gingival thickness measurement previously, however; it has some disadvantages such as low sensitivity of periodontal probe, discomfort, destruction of tissue and need for local anaesthesia.10 Therefore, CBCT and US imaging may also be preferred due to their non-invasive nature for gingival thickness measurement.11,14,29
CBCT offers the opportunity to evaluate oral structures in three dimensions with submillimeter accuracy; however, when prescribing CBCT its possible benefits should outweigh its potential hazards. Besides, low soft tissue contrast of CBCT is a limitation for gingival thickness assessment.30 In order to overcome this disadvantage, the use of lip retractor is suggested during CBCT imaging that enables better discrimination of periodontal soft and hard tissues and enables better visibility of periodonsium.16 Researchers evaluated the effectiveness of lip retractor for imaging and visualizing dentogingival structures by using CBCT images and reported that without lip retraction, CBCT images only enabled measuring the distance between cementoenamel junction (CEJ) to facial bone crest and width of facial alveolar bone.16 In addition to these measurements, using lip retraction prior to CBCT scans allowed measurement of the distance between the gingival margin to the facial bone crest, the gingival margin to the CEJ, and width of the facial gingiva. It is recommended that cross-sectional imaging be conducted prior to implant placement in order to assist in determining the appropriate size, angulation, and position of dental implants. Today, numerous revolutionary CBCT applications reached the dental market that can address a variety of specific tasks. CBCT has come into common use in the field of dental implantology and; therefore, we utilized two of the frequently preferred and available CBCT units for implant planning.31 Therefore, comparing US measurements with those of CBCT measurements was reasonable in consideration to real clinical conditions. In general, we found that US measurements highly correlated with those of gold standard clinical measurements; however, in the present study, CBCT measurements did not perform as good as US for the gingival soft tissue measurements. As, CBCT is the most frequently used technique for implant planning we also utilized two different CBCT devices with different settings. Obviously, in order to assess a newly introduced diagnostic tool’s clinical versatility (in this case high-resolution US), one should compare it to other commonly used techniques.
A previous study evaluated gingival soft tissue thickness in the maxillary region on fresh cadavers and found no statistically significant differences among transgingival probing and CBCT measurements for facial soft tissue thickness. However, authors found statistically significant differences for the palatal soft tissue thickness among transgingival probing and CBCT measurements.18 Findings of the mentioned study are analogous to our results for facial soft tissue thickness. Palatal soft tissue thickness measurement was out of the scope of our study.
Borges et al. evaluated gingival thickness on 29 patients prior to gingivectomy surgery by transgingival probing, CBCT imaging and SDM ultrasonic device.32 When gingival thickness of incisor and canine region was taken into consideration, no statistically significant differences among CBCT and ultrasonic device measurements were found; however, statistically significant differences were found for transgingival probing (p < 0.05).32 When premolar and molar regions were taken into consideration, authors found no statistically significant differences among CBCT and transgingival probing measurements; however, they found statistically significant differences for ultrasonic device measurements (p < 0.05).32
Authors of another recent study evaluated gingival thickness measurements by transgingival probing and CBCT images obtained with lip retractor, for gingival thickness measurement in maxillary incisors at three different points (1 mm, 3 mm and 5 mm above gingival margin) and similar to our results they found statistically significant correlation between clinical measurements and other methods used (p < .001).14
For gingival thickness determination, US imaging has been specifically proposed as an alternative technique since it provides real-time images without ionizing radiation. Traxler et al. evaluated the effectiveness of US imaging, transgingival probing and anatomical sectioning on gingival thickness measurements on eight fresh human cadavers by using 8 MHz sector transducer and they found no statistically significant differences between US, transgingival probing and anatomical sectioning with 2 mm mean deviation.22 Authors, evaluated conventional A mode and modified B mode US for the determination of mucosal tissue thickness and compared with transgingival probing.25 Prior to examinations they bonded foil coil as reference point on the gingivae of volunteers and used stand-off pads during examinations. When compared to transgingival probing, higher measurements were found for B mode US while lower measurements were found for A mode US. Over measuring for the B mode could be as a result of misinterpretation of the artefacts caused by foil coil. It should also be kept in mind that US is an operator and patient dependent imaging modality.
On porcine mandibles, gingival thickness measurement accuracy and repeatability were evaluated by using 20 MHz US probe, transgingival probing and anatomical sectioning by researchers.23 Their results showed 0.004 ± 0.82 mm limits of agreement for US versus transgingival probing, 0.0047 ± 0.58 mm mm limits of agreement for US versus anatomical sectioning and 0 ± 0.7 mm limits of agreement for transgingival probing versus anatomical sectioning. When repeatability of methods were taken into consideration US imaging performed better with 0.22 mm standard deviation when compared to other methods.23
Researchers evaluated commercially available US probe (SP 7.5, Interson Corp.) on measuring diameters and depths of submerged dental implants on porcine jaws.33 Two titanium dental implants with 3.5 mm and 4.3 mm diameters were placed in porcine mandibles and covered with 1.3 mm width sliced deli turkey in order to simulate soft tissue and porcine specimens were submerged in water tank that allowed rotation and translation of US probe. Their results showed 4.6 ± 0.1 mm and 3.8 ± 0.2 mm mean diameter width for dental implants and 1.4 ± 0.2 mm soft tissue thickness measurement above 3.5 mm diameter implant and 1.5 ± 0.1 mm soft tissue thickness measurement above 4.3 mm diameter dental implant.33
US was found to be a highly accurate and noninvasive technique for periodontal assessment.34 Effective use of 40 MHz US in the assessment of periodontal structures was proven in four patients. No statistical differences between clinical and US measurements were obtained, in respect to probing depth.34 Considering the small sample size used in the mentioned study further research is necessary to fully understand the effectiveness of high-resolution US in the assessment of periodontal structures in vivo. In our study, power analysis and sample size calculation was performed and an adequate number of implant sites were included for clinical, US, and CBCT measurements which strengthened our findings.
On mucosal tissue thickness detection, effectiveness and reproducibility of ultrasonic device were evaluated on four fresh human cadavers maxilla at 100 different sites.34 Ultrasonic measurements were conducted by using 5 MHz frequency probe and micro-CT images were obtained for each specimen as the gold standard. Authors found statistically significant lower measurements for US measurements than micro-CT measurements. They also reported that ultrasonic device proved to be more reliable in measuring soft tissue thickness in the cases where there is less than 5 mm width.27 Our study included soft tissue thickness less than 5 mm width; however, due to in vivo nature of our study design, it was not possible to obtain micro-CT images. In addition, minimal angle changes on probe position may occur during US imaging resulting in differences in soft tissue thickness measurement due to variations on bony part of maxilla and bone surface irregularities.
A recent study, evaluated the effectiveness of a medical ultrasonic array system on imaging dental hard tissues and periodontal attachment and compared US images with CBCT images.35 Researchers measured the distance from gingival margin to cemento-enamel junction, the distance between gingival margin and alveolar process, and the thickness of the alveolar bone at the crest. Authors found lower milimetric measurements for US images when compared to CBCT images.35 CBCT measurements of periodontium cannot be suggested as a gold standard method due to its low soft tissue contrast. Chan et. al. compared US images obtained by using 14 MHz intraoral probe, CBCT images and direct measurements for evaluating facial bone surface and soft tissue, lingual nerve mental foreman and greater palatine foramen on fresh cadavers.36 Their results showed 0.3 ± 0.1 mm mean soft tissue thickness for US, 0.5 ± 0.1 mm mean soft tissue thickness for CBCT and 0.3 ± 0.1 mm mean soft tissue thickness for direct measurements by using caliper accurate to 0.1 mm. Similar to their findings, we also found that US showed similar results with clinical gold standard measurements. Further research should be encouraged in an attempt to assess the effectiveness of various types of US probes with different characteristics in the measurement of gingival soft tissue prior to dental implantation procedures. In our further studies, we will focus on the fusion of US images with those of CBCT images in terms of both gingival thickness and bone quantity and quality assessment of implant regions in fused images.
Conclusion
High-resolution US provides accurate information for the measurement of gingival soft tissue thickness in edentulous patients prior to implant placement. Due to its low cost, non-invasive and non-ionized nature, US imaging is a promising technique, for preoperative gingival soft tissue evaluation in the implant site.
Footnotes
Acknowledgements: This research was presented as specialty thesis at the Department of Dentomaxillofacial Radiology, Faculty of Dentistry, Ankara University, Ankara, Turkey. This study was supported by Ankara University Scientific Research Projects Unit (No:16A0234001) and Başkent University Scientific Research Projects Unit (Project no. D-KA 17/13).
REFERENCES
- 1.Kamburoğlu K, Gülşahı A, Genç Y, Paksoy CS. A comparison of peripheral marginal bone loss at dental implants measured with conventional intraoral film and digitized radiographs. J Oral Implantol 2012; 38: 211–9. doi: 10.1563/AAID-JOI-D-09-00147 [DOI] [PubMed] [Google Scholar]
- 2.Garber DA. The esthetic dental implant: letting restoration be the guide. J Am Dent Assoc 1995; 126: 319–25. doi: 10.14219/jada.archive.1995.0175 [DOI] [PubMed] [Google Scholar]
- 3.Levin L, Pathael S, Dolev E, Schwartz-Arad D. Aesthetic versus surgical success of single dental implants: 1- to 9-year follow-up. Pract Proced Aesthet Dent 2005; 17: 533–8. [PubMed] [Google Scholar]
- 4.Cook DR, Mealey BL, Verrett RG, Mills MP, Noujeim ME, Lasho DJ, et al. Relationship between clinical periodontal biotype and labial plate thickness: an in vivo study. Int J Periodontics Restorative Dent 2011; 31: 345–54. [PubMed] [Google Scholar]
- 5.Fu J-H, Lee A, Wang H-L. Influence of tissue biotype on implant esthetics. Int J Oral Maxillofac Implants 2011; 26: 499–508. [PubMed] [Google Scholar]
- 6.Kan JYK, Morimoto T, Rungcharassaeng K, Roe P, Smith DH. Gingival biotype assessment in the esthetic zone: visual versus direct measurement. Int J Periodontics Restorative Dent 2010; 30: 237–43. [PubMed] [Google Scholar]
- 7.Eghbali A, De Rouck T, De Bruyn H, Cosyn J. The gingival biotype assessed by experienced and inexperienced clinicians. J Clin Periodontol 2009; 36: 958–63. doi: 10.1111/j.1600-051X.2009.01479.x [DOI] [PubMed] [Google Scholar]
- 8.Kois JC. Predictable single-tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent 2004; 25: 895–6. [PubMed] [Google Scholar]
- 9.Kan JYK, Rungcharassaeng K, Umezu K, Kois JC. Dimensions of peri-implant mucosa: an evaluation of maxillary anterior single implants in humans. J Periodontol 2003; 74: 557–62. doi: 10.1902/jop.2003.74.4.557 [DOI] [PubMed] [Google Scholar]
- 10.Wara-aswapati N, Pitiphat W, Chandrapho N, Rattanayatikul C, Karimbux N. Thickness of palatal masticatory mucosa associated with age. J Periodontol 2001; 72: 1407–12. doi: 10.1902/jop.2001.72.10.1407 [DOI] [PubMed] [Google Scholar]
- 11.Song J-E, Um Y-J, Kim C-S, Choi S-H, Cho K-S, Kim C-K, et al. Thickness of posterior palatal masticatory mucosa: the use of computerized tomography. J Periodontol 2008; 79: 406–12. doi: 10.1902/jop.2008.070302 [DOI] [PubMed] [Google Scholar]
- 12.Alpiste-Illueca F. Dimensions of the dentogingival unit in maxillary anterior teeth: a new exploration technique (parallel profile radiograph. Int J Periodontics Restor Dent 2004; 24: 386–96. [PubMed] [Google Scholar]
- 13.Guerrero ME, Jacobs R, Loubele M, Schutyser F, Suetens P, van Steenberghe D. State-Of-The-Art on cone beam CT imaging for preoperative planning of implant placement. Clin Oral Investig 2006; 10: 1–7. doi: 10.1007/s00784-005-0031-2 [DOI] [PubMed] [Google Scholar]
- 14.Silva JNN, Andrade PFde, Sotto-Maior BS, Souza Picorelli Assis NM, Pires Carvalho AC, Devito KL. Influence of lip retraction on the cone beam computed tomography assessment of bone and gingival tissues of the anterior maxilla. Oral Surg Oral Med Oral Pathol Oral Radiol 2017; 123: 714–20. doi: 10.1016/j.oooo.2017.02.005 [DOI] [PubMed] [Google Scholar]
- 15.Barriviera M, Duarte WR, Januário AL, Faber J, Bezerra ACB. A new method to assess and measure palatal masticatory mucosa by cone-beam computerized tomography. J Clin Periodontol 2009; 36: 564–8. doi: 10.1111/j.1600-051X.2009.01422.x [DOI] [PubMed] [Google Scholar]
- 16.Januário AL, Barriviera M, Duarte WR. Soft tissue cone-beam computed tomography: a novel method for the measurement of gingival tissue and the dimensions of the dentogingival unit. J Esthet Restor Dent 2008; 20: 366–73. doi: 10.1111/j.1708-8240.2008.00210.x [DOI] [PubMed] [Google Scholar]
- 17.Ueno D, Sekiguchi R, Morita M, Jayawardena A, Shinpo S, Sato J, et al. Palatal mucosal measurements in a Japanese population using cone-beam computed tomography. J Esthet Restor Dent 2014; 26: 48–58. doi: 10.1111/jerd.12053 [DOI] [PubMed] [Google Scholar]
- 18.Fu J-H, Yeh C-Y, Chan H-L, Tatarakis N, Leong DJM, Wang H-L. Tissue biotype and its relation to the underlying bone morphology. J Periodontol 2010; 81: 569–74. doi: 10.1902/jop.2009.090591 [DOI] [PubMed] [Google Scholar]
- 19.Angelopoulos C, Scarfe WC, Farman AG. A comparison of maxillofacial CBCT and medical CT. Atlas Oral Maxillofac Surg Clin North Am 2012; 20: 1–17. doi: 10.1016/j.cxom.2011.12.008 [DOI] [PubMed] [Google Scholar]
- 20.De Bruyckere T, Eghbali A, Younes F, De Bruyn H, Cosyn J. Horizontal stability of connective tissue grafts at the buccal aspect of single implants: a 1-year prospective case series. J Clin Periodontol 2015; 42: 876–82. doi: 10.1111/jcpe.12448 [DOI] [PubMed] [Google Scholar]
- 21.Eger T, Müller HP, Heinecke A. Ultrasonic determination of gingival thickness. subject variation and influence of tooth type and clinical features. J Clin Periodontol 1996; 23: 839–45. doi: 10.1111/j.1600-051X.1996.tb00621.x [DOI] [PubMed] [Google Scholar]
- 22.Traxler M, Solar P, Ulm C, Gritzmann N. Ultrasonographic measurement of the soft-tissue of the upper jaw. Acta Radiol 1991; 32: 3–5. doi: 10.1177/028418519103200102 [DOI] [PubMed] [Google Scholar]
- 23.Tsiolis FI, Needleman IG, Griffiths GS. Periodontal ultrasonography. J Clin Periodontol 2003; 30: 849–54. doi: 10.1034/j.1600-051X.2003.00380.x [DOI] [PubMed] [Google Scholar]
- 24.Yılmaz D, Kamburoğlu K. Comparison of the effectiveness of high resolution ultrasound with MRI in patients with temporomandibular joint dısorders. Dentomaxillofac Radiol 2019; 48: 20180349. doi: 10.1259/dmfr.20180349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schulze RKW, Curić D, d'Hoedt B. B-Mode versus A-mode ultrasonographic measurements of mucosal thickness in vivo. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 93: 110–7. doi: 10.1067/moe.2002.119465 [DOI] [PubMed] [Google Scholar]
- 26.Culjat MO, Choi M, Singh RS, Grundfest WS, Brown ER, White SN. Ultrasound detection of submerged dental implants through soft tissue in a porcine model. J Prosthet Dent 2008; 99: 218–24. doi: 10.1016/S0022-3913(08)60046-3 [DOI] [PubMed] [Google Scholar]
- 27.Eghbali A, De Bruyn H, Cosyn J, Kerckaert I, Van Hoof T. Ultrasonic assessment of mucosal thickness around implants: validity, reproducibility, and stability of connective tissue grafts at the buccal aspect. Clin Implant Dent Relat Res 2016; 18: 51–61. doi: 10.1111/cid.12245 [DOI] [PubMed] [Google Scholar]
- 28.Sala L, Alonso-Pérez R, Agustin-Panadero R, Ferreiroa A, Carrillo-de-Albornoz A. Comparative in vitro study of two methods for gingival biotype assessment. J Clin Exp Dent 2018; 10: e858–63. doi: 10.4317/jced.55049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chan H-L, Sinjab K, Chung M-P, Chiang Y-C, Wang H-L, Giannobile WV, et al. Non-Invasive evaluation of facial crestal bone with ultrasonography. PLoS One 2017; 12: e0171237. doi: 10.1371/journal.pone.0171237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Suomalainen A, Pakbaznejad Esmaeili E, Robinson S. Dentomaxillofacial imaging with panoramic views and cone beam CT. Insights Imaging 2015; 6: 1–16. doi: 10.1007/s13244-014-0379-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kamburoğlu K, Acar B, Yüksel S, Paksoy CS. CBCT quantitative evaluation of mandibular lingual concavities in dental implant patients. Surg Radiol Anat 2015; 37: 1209–15. doi: 10.1007/s00276-015-1493-9 [DOI] [PubMed] [Google Scholar]
- 32.Borges GJ, Ruiz LFN, de Alencar AHG, Porto OCL, Estrela C. Cone-Beam computed tomography as a diagnostic method for determination of gingival thickness and distance between gingival margin and bone crest. ScientificWorldJournal 2015; 2015: 1–10. doi: 10.1155/2015/142108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Culjat MO, Choi M, Singh RS, White SN. Ultrasound imaging of dental implants Conf proC IEEE. Eng Med Biol Soc 2012; 2012: 456–9. [DOI] [PubMed] [Google Scholar]
- 34.Zimbran A, Dudea S, Dudea D. Evaluation of periodontal tissues using 40MHz ultrasonography. preliminary report. Med Ultrason 2013; 15: 6–9. doi: 10.11152/mu.2013.2066.151.az1ept2 [DOI] [PubMed] [Google Scholar]
- 35.Nguyen K-CT, Le LH, Kaipatur NR, Zheng R, Lou EH, Major PW. High-Resolution ultrasonic imaging of Dento-Periodontal tissues using a Multi-Element phased array system. Ann Biomed Eng 2016; 44: 2874–86. doi: 10.1007/s10439-016-1634-2 [DOI] [PubMed] [Google Scholar]
- 36.Chan H-L, Wang H-L, Fowlkes JB, Giannobile WV, Kripfgans OD. Non-ionizing real-time ultrasonography in implant and oral surgery: a feasibility study. Clin Oral Implants Res 2017; 28: 341–7. doi: 10.1111/clr.12805 [DOI] [PMC free article] [PubMed] [Google Scholar]