Abstract
Background: When oncologically feasible, avoiding unnecessary splenectomies prevents patients who are undergoing distal pancreatectomy (DP) from facing significant thromboembolic and infective risks. Methods: A systematic search of MEDLINE, Embase, and Web Of Science identified 11 studies reporting outcomes of 323 patients undergoing intended spleen-preserving minimally invasive robotic DP (SP-RADP) and 362 laparoscopic DP (SP-LADP) in order to compare the spleen preservation rates of the two techniques. The risk of bias was evaluated according to the Newcastle–Ottawa Scale. Results: SP-RADP showed superior results over the laparoscopic approach, with an inferior spleen preservation failure risk difference (RD) of 0.24 (95% CI 0.15, 0.33), reduced open conversion rate (RD of −0.05 (95% CI −0.09, −0.01)), reduced blood loss (mean difference of −138 mL (95% CI −205, −71)), and mean difference in hospital length of stay of −1.5 days (95% CI −2.8, −0.2), with similar operative time, clinically relevant postoperative pancreatic fistula (ISGPS grade B/C), and Clavien–Dindo grade ≥3 postoperative complications. Conclusion: Both SP-RADP and SP-LADP proved to be safe and effective procedures, with minimal perioperative mortality and low postoperative morbidity. The robotic approach proved to be superior to the laparoscopic approach in terms of spleen preservation rate, intraoperative blood loss, and hospital length of stay.
Keywords: robotic distal pancreatectomy, laparoscopic distal pancreatectomy, spleen-preserving distal pancreatectomy, minimally-invasive distal pancreatectomy, systematic review, meta-analysis
1. Introduction
The decision on preserving the spleen when performing a distal pancreatectomy (DP) is usually based on the balance between achieving an adequate oncological clearance and avoiding complications related to asplenia. Spleen-preserving DP has therefore been mainly reserved for surgeries performed for benign indications or to excise lesions with a low malignant potential. With the advent of minimally invasive surgery, in the early 1990s, surgeons around the world started to explore the potential of the laparoscopic approach in pancreatic surgery [1,2] and, almost a decade later, of the robotic-assisted technique [3]. Minimally invasive pancreatic surgery has been progressively gaining widespread popularity, and advancements in surgical skills have removed most of the technical restrictions, allowing the safe and effective execution of complex procedures, including laparoscopic spleen-preserving distal pancreatectomy (SP-LADP) [4] and robot-assisted spleen-preserving distal pancreatectomy (SP-RADP) [5].
This systematic review and meta-analysis aims to summarize all of the available evidence regarding spleen-preserving DP and compare results and outcomes of minimally invasive SP-RADP and SP-LADP techniques.
2. Materials and Methods
This systematic review and meta-analysis was conducted in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA 2020 Statement [6]) and was registered on PROSPERO (CRD42021239032).
2.1. Search Strategy
MEDLINE, Embase, and Web Of Science electronic databases were searched using the following terms: “pancrea*” AND “robot*” AND “laparoscop*” AND “sple*”. The last search was run on 1 February 2021 with no language or publication status restrictions. Additional potentially relevant studies were identified from the reference lists of selected studies.
2.2. Study Selection
For inclusion, studies had to (1) include patients undergoing DP for any disease; (2) include procedures performed robotically and laparoscopically; and (3) report data on patients undergoing DP with the intent of preserving the spleen. Case reports, reviews, and communications, as well as non-human studies, were excluded. Two reviewers (G.R. and L.A.) independently screened the results of the electronic search at title and abstract levels. The full texts of the selected references were also retrieved for further analysis and data extraction. When duplicate reports from the same study were identified, only the most recent publication was included.
2.3. Data Extraction and Quality Assessment
Two reviewers (G.R. and L.A.) extracted data from each selected study regarding the first author; publication year; country of origin; study design; number of patients undergoing SP-RADP and SP-LADP; patients characteristics (age, sex, body mass index (BMI)); underlying disease requiring DP; American Society of Anesthesiologists (ASA) score; tumor size; conversion rate; blood loss; pancreatic stump closure technique; splenic vessel preservation and technique (Warshaw vs. Kimura); blood transfusion requirement; length of surgery; data on postoperative morbidity, including prevalence and grading of the clinical severity of postoperative pancreatic fistula (POPF) according to the ISGPS definition [7]; complications and grading according to the Clavien–Dindo classification [8]; re-operation rate; length of stay (LOS); mortality; and length of follow-up. The quality and risk of bias of each included study was evaluated independently by two reviewers (G.R. and L.A.) according to the Newcastle–Ottawa Scale for evaluating the quality of non-randomized studies in meta-analyses [9]. The level of evidence was rated according to the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) system [10]. Any disagreement was resolved through discussion in order to reach consensus across the study team.
2.4. Statistical Analysis and Data Synthesis
The primary outcome was the spleen preservation failure rate. Secondary outcomes included intraoperative blood loss, operative time, prevalence of clinically relevant POPF (grade B/C), prevalence of postoperative complications (Clavien–Dindo [8] grades ≥3), hospital LOS, and mortality. For the analysis, values expressed as median (range) were converted to average ± standard deviation using Wan’s method [11]. To pool proportions, we used random-effects or fixed-effect modelling according to the DerSimonian and Laird method [12,13] to take into account heterogeneity. The presence of heterogeneity among the studies was assessed using Cochran’s Q test and quantified with the I2 inconsistency index, with 25, 50, and 75% considered as thresholds for low, moderate, and high statistical heterogeneity, respectively. Heterogeneity was evaluated by sensitivity analysis [14]. Statistical analyses were performed using Review Manager version 5.3.
3. Results
3.1. Studies Selection
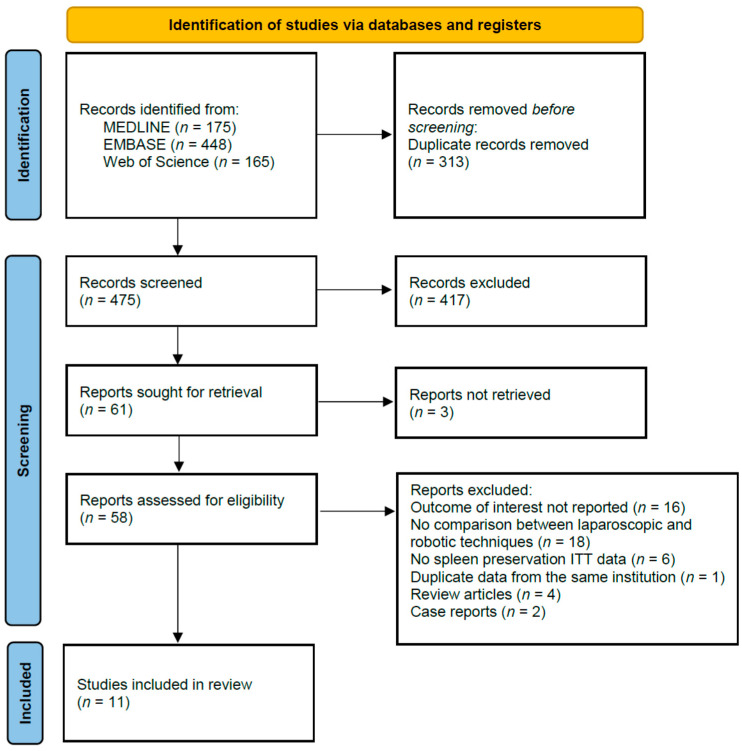
Eleven studies met the inclusion criteria and were included in the systematic review and meta-analysis [15,16,17,18,19,20,21,22,23,24,25] (Figure 1).
Figure 1.
PRISMA flow diagram. ITT: intention-to-treat.
3.2. Studies Characteristics
The characteristics of the selected studies are reported in Table 1. A total of 323 patients undergoing SP-RADP and 362 patients undergoing SP-LADP were included in this meta-analysis. Eight included series (72.7%) were retrospective cohort studies [16,17,18,21,22,23,24,25], two were matched cohort studies (18.2%) [15,19], and one was a case-control study (9.1%) [20]. The reported median follow-up was 27 months (range 6.5–47) for SP-RADP and 33.5 months (range 32–75.5) for SP-LADP. The most frequent indications for surgery were neuroendocrine tumors (NET) in 61 SP-RADP and 52 SP-LADP, mucinous cystic neoplasms in 37 SP-RADP and 28 SP-LADP, intraductal papillary mucinous neoplasms (IPMN) in 15 SP-RADP and 28 SP-LADP, and pseudopapillary tumors in 18 SP-RADP and 17 SP-LADP.
Table 1.
Summary of the selected studies with patients’ characteristics and quality assessment according to the Newcastle–Ottawa scale (NOS). NA: not available.
| Author and Year | Study Type | N Rob/Lap | Age, Years Rob–Lap |
Sex (F) Rob/Lap | Lesion Size, mm Rob–Lap | BMI Rob–Lap | ASA Rob–Lap | NOS Assessment | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Selection | Comparability | Outcome | ||||||||
| Chen et al., 2015 | Matched cohort |
47/33 | 55.6 ± 14.3–55.8 ± 16.2 | 31/21 | 31.25 ± 3.4–29 ± 3.4 | 24.4 ± 2.9–24.8 ± 2.7 | 2.5 ± 0.7–1.91 ± 0.3 | 3 * | 2 * | 3 * |
| Eckhardt et al, 2016 | Cohort | 12/29 | 50.5 ± 14.4–55 ± 16.8 | 8/17 | 22 ± 10.4–38 ± 3 | 24.00 ± 3.4–27.3 ± 4.3 | NA | 3 * | 1 * | 3 * |
| Hong et al, 2020 | Cohort | 31/57 | NA | NA | 36.5 ± 17.4–29.8 ± 19.5 | NA | NA | 3 * | 1 * | 3 * |
| Kang et al, 2011 | Cohort | 20/25 | 44.5 ± 15.9–56.5 ± 13.9 | 12/14 | 35 ± 13–30 ± 14 | 24.2 ± 2.9–23.4 ± 2.6 | NA | 3 * | 1 * | 3 * |
| Liu et al, 2017 | Matched cohort |
76/77 | NA | NA | NA | NA | NA | 3 * | 2 * | 3 * |
| Morelli et al, 2016 | Case-control | 15/15 | 58.2 ± 13.7–49.3 ± 17.1 | 9/13 | 29.9 ± 16.5–26.9 ± 13.5 | 26.4 ± 3.1–26.1 ± 1.9 | 2.40 ± 0.5–2.30 ± 0.5 | 2 * | 2 * | 3 * |
| Nell et al, 2016 | Cohort | 5/9 | NA | NA | NA | NA | NA | 3 * | 1 * | 3 * |
| Najafi et al, 2020 | Cohort | 24/32 | NA | NA | NA | NA | NA | 3 * | 1 * | 3 * |
| Souche et al, 2018 | Cohort | 13/13 | NA | NA | NA | NA | NA | 3 * | 1 * | 3 * |
| Yang et al, 2020 | Cohort | 37/41 | 42.9 ± 14–51.3 ± 14.6 | 23/27 | 27 ± 12–42 ± 33 | 23.5 ± 3.2–24.1 ± 3.4 | 1.41 ± 0.6–1.58 ± 0.8 | 3 * | 1 * | 3 * |
| Zhang et al, 2017 | Cohort | 43/31 | 47.9 ± 10.5–48.7 ± 12.3 | 23/19 | 17.5 ± 2.7–16.5 ± 2.4 | 23.3 ± 2.7–23.9 ± 3.2 | 1.26 ± 0.4–1.39 ± 0.5 | 3 * | 1 * | 3 * |
3.3. Quality Assessment and Publication Bias
The results of the quality assessment of the 11 included studies according to the guidelines of the Newcastle–Ottawa Scale are reported in Table 1.
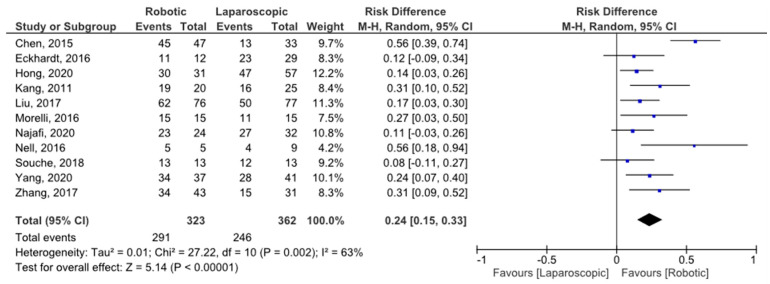
3.4. Spleen Preservation Rate
All selected studies reported the number of procedures intended to be spleen preserving and the spleen preservation failure rate for both the robotic and laparoscopic techniques. The risk difference (RD) of spleen preservation failures was 0.24 (95% CI 0.15, 0.33), favoring the robotic approach and with moderate heterogeneity (I2 = 63%) (Figure 2). Heterogeneity was evaluated by sensitivity analysis, and the results are summarized in Table 2.
Figure 2.
Spleen preservation rate forest plot.
Table 2.
Sensitivity analysis by sequential omission of each individual study. Meta-analysis estimates, given the named study is omitted. CI: confidence interval.
| Study Omitted | Risk Difference [95% CI] (<1 Favors Robotic) |
Test of Heterogeneity |
Quantification of Heterogeneity |
|
|---|---|---|---|---|
| Chi2 | p | |||
| Chen et al, 2015 | 0.19 [0.13, 0.25] | 10.51 | 0.31 | df = 9; I2 = 14% |
| Eckhardt et al, 2016 | 0.25 [0.15, 0.35] | 26.40 | 0.002 | df = 9; I2 = 66% |
| Hong et al, 2020 | 0.25 [0.15, 0.36] | 24.73 | 0.003 | df = 9; I2 = 64% |
| Kang et al, 2011 | 0.23 [0.14, 0.33] | 26.49 | 0.002 | df = 9; I2 = 66% |
| Liu et al, 2017 | 0.25 [0.15, 0.36] | 27.61 | 0.001 | df = 9; I2 = 67% |
| Morelli et al, 2016 | 0.24 [0.14, 0.34] | 27.11 | 0.001 | df = 9; I2 = 67% |
| Najafi et al, 2020 | 0.25 [0.16, 0.35] | 24.78 | 0.003 | df = 9; I2 = 64% |
| Nell et al, 2016 | 0.23 [0.13, 0.32] | 24.15 | 0.004 | df = 9; I2 = 63% |
| Souche et al, 2018 | 0.26 [0.16, 0.25] | 24.49 | 0.004 | df = 9; I2 = 63% |
| Yang et al, 2020 | 0.24 [0.14, 0.34] | 27.30 | 0.001 | df = 9; I2 = 67% |
| Zhang et al, 2017 | 0.23 [0.14, 0.33] | 26.34 | 0.002 | df = 9; I2 = 66% |
3.5. Patient Characteristics and Operative Details
Only four series [16,21,25,26] reported the average ASA score (median value of 1.9, range 1.3–2.5 for SP-RADP; 1.7, range 1.4–2.3 for SP-LADP), while preoperative BMI was described in six series [16,17,19,21,25,26] (median value of 24.1, range 23.3–26.4 for SP-RADP; 24.4, range 23.4–27.3 for SP-LADP). Of the groups reporting the incidence of previous abdominal surgery [16,17,21], 5 out of 15 patients in both groups had had previous surgery in one study [20], with no patients undergoing previous surgery in the other two reports. All other patients’ characteristics are summarized in Table 1.
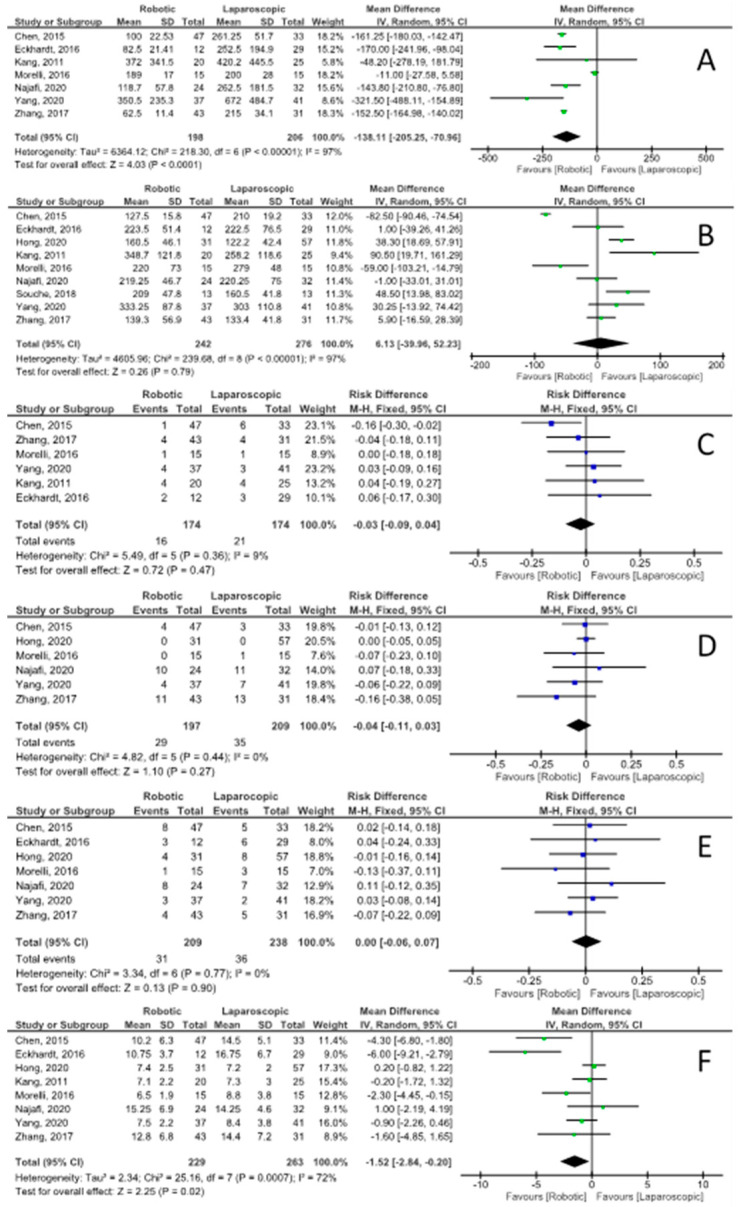
Eight of the included studies [15,16,18,20,21,23,24,25] reported the conversion rate, with an RD of −0.05 (95% CI −0.09, −0.01) and moderate heterogeneity (I2 = 26%) of being converted to “open” technique favoring the robotic approach. Unfortunately, no study described the reason for conversion. The intraoperative blood loss (Figure 3), as reported in seven series [16,17,19,21,22,25,26], was significantly lower for the robotic group, with a mean difference of −138 mL (95% CI −205, −71) and high heterogeneity (I2 = 97%). There was no statistical difference in the operative time between the two groups (Figure 3), reported by nine series [15,16,17,18,20,21,23,24,25], with a mean difference of 6.1 min (95% CI −40, 52) and high heterogeneity (I2 = 97%). Four studies [17,23,24,25] reported the distal pancreatic stump closure technique, which was with an endo-GIA stapler in all cases in both groups. Eight studies [15,16,18,20,21,23,24,25] reported data on spleen preservation techniques, including a total of 211 robotic and 219 laparoscopic procedures. The Kimura technique [26] was adopted in 159 out of the 196 patients (81.1%) undergoing SP-RADP (the remaining 18.9% of patients had the pancreatic resection performed according to the technique described by Warshaw [27]) and in 84 out of the 154 SP-LADP (54.5%), with the Warshaw technique being adopted for the remaining 45.5%.
Figure 3.
Secondary outcomes forest plots: (A) intraoperative blood loss (mL); (B) operative time (min); (C) perioperative blood transfusions; (D) Clavien–Dindo grade ≥3 complications; (E) postoperative pancreatic fistula grade B/C; (F) hospital length of stay (days).
3.6. Postoperative Morbidity and Outcomes
Eight series [15,16,17,18,20,21,24,25] reported the perioperative mortality, with no cases of 30-day deaths. Seven studies [15,16,17,20,21,24,27] described the prevalence of POPF. The RD of clinically relevant POPF (ISGPS grade B/C) was 0.00 (95% CI −0.06, 0.07) with no heterogeneity (I2 = 0%). The RD of Clavien–Dindo grade ≥3 postoperative complications, as reported in six series [16,18,21,22,25,26], was −0.04 (95% CI −0.11, 0.03) with no heterogeneity (I2 = 0%). The mean hospital LOS difference was −1.5 days (95% CI −2.8, −0.2) in favor of SP-RADP and with high heterogeneity (I2 = 0%). Data on overall postoperative complications, Clavien–Dindo grade 1–2 postoperative complications, biochemical leaks, and postoperative bleeding episodes are reported in Table 3.
Table 3.
Risk differences between robotic and laparoscopic spleen-preserving distal pancreatectomies. CI: confidence interval; POPF: postoperative pancreatic fistula.
| Outcome | Studies | Risk Difference [95% CI] (<1 Favors Robotic) |
Test of Heterogeneity | Quantification of Heterogeneity |
|
|---|---|---|---|---|---|
| Chi2 | p | ||||
| Spleen preserving failure | 16–26 | −0.25 [−0.30, −0.19] | 27.22 | 0.002 | df = 10; I2 = 63% |
| Open conversions | 16, 17, 19, 21, 22, 24–26 | −0.05 [−0.09, −0.01] | 9.41 | 0.22 | df = 7; I2 = 26% |
| Overall complications | 16–19, 21, 25, 26 | −0.06 [−0.14, 0.02] | 2.15 | 0.91 | df = 6; I2 = 0% |
| Complications—Clavien–Dindo grade 1–2 | 16, 18, 21 | −0.02 [−0.15, 0.11] | 1.00 | 0.61 | df = 2; I2 = 0% |
| Complications—Clavien–Dindo grade ≥3 | 16, 18, 21, 22, 25, 26 | −0.04 [−0.11, 0.03] | 4.82 | 0.44 | df = 5; I2 = 0% |
| POPF grade B/C | 16–18, 21, 22, 25, 26 | 0.00 [−0.06, 0.07] | 3.34 | 0.77 | df = 6; I2 = 0% |
| Biochemical leaks | 16–18, 21, 26 | −0.04 [−0.14, 0.05] | 1.01 | 0.91 | df = 4; I2 = 0% |
| Intra-/post-operative blood transfusions |
16, 17, 19, 21, 25, 26 | −0.03 [−0.09, 0.04] | 5.49 | 0.36 | df = 5; I2 = 9% |
| Reoperation rate | 16, 17, 21, 22, 26 | 0.01 [−0.05, 0.07] | 3.86 | 0.42 | df = 4; I2 = 0% |
| Hospital length of stay | 16–19, 21, 22, 25, 26 | −1.52 [−2.84, −0.20] | 25.16 | <0.001 | df = 7; I2 = 72% |
3.7. Quality of Evidence
The level of evidence was rated according to GRADE and is summarized in Table 4.
Table 4.
Robotic versus laparoscopic surgery for spleen-preserving distal pancreatectomies. * The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; MD: Mean difference.
| Outcomes | N of Participants (Studies) Follow up |
Certainty of the Evidence (GRADE) | Relative Effect (95% CI) | Anticipated Absolute Effects | |
|---|---|---|---|---|---|
| Risk with Laparoscopic Approach | Risk Difference with Robotic Approach |
||||
| Spleen preservation rate | 685 (11 observational studies) | ⨁⨁◯◯ LOW | RR 1.31 (1.16 to 1.48) |
680 per 1000 | 211 more per 1000 (109 more to 326 more) |
| Blood Loss | 404 (7 observational studies) | ⨁⨁◯◯ LOW | - | Mean blood loss was 233.3 mL | MD 138.11 lower (205.25 lower to 70.96 lower) |
| Operative time | 518 (9 observational studies) | ⨁⨁◯◯ LOW | - | Mean operative time was 206.1 min |
MD 6.13 higher (39.96 lower to 52.23 higher) |
| Pancreatic fistula grade B–C | 447 (7 observational studies) | ⨁⨁◯◯ LOW | RR 1.03 (0.66 to 1.60) |
151 per 1000 | 5 more per 1000 (51 fewer to 91 more) |
| Complications Clavien–Dindo 3–4 |
406 (6 observational studies) | ⨁⨁◯◯ LOW | RR 0.79 (0.52 to 1.20) |
167 per 1000 | 35 fewer per 1000 (80 fewer to 33 more) |
| Hospital length of stay | 492 (8 observational studies) | ⨁⨁◯◯ LOW | - | Mean hospital stay was 9.8 days | MD 1.52 lower (2.84 lower to 0.2 lower) |
| Perioperative bleeding | 143 (3 observational studies) | ⨁⨁◯◯ LOW | RR 0.93 (0.24 to 3.63) |
55 per 1000 | 4 fewer per 1000 (42 fewer to 144 more) |
4. Discussion
To the best of our knowledge, this systematic review and meta-analysis is the first report summarizing all the available evidence on patients undergoing spleen-preserving distal pancreatectomy with robotic and laparoscopic techniques. All published studies comparing these two minimally invasive surgical approaches were screened in order to analyze the intention-to-treat population of patients undergoing DP where the spleen was intended to be preserved and to evaluate whether the surgical technique would have an impact on the spleen preservation success rate.
The spleen holds the largest lymphoid tissue mass in the body, producing early immunoglobulins M and containing macrophages that act as barriers against encapsulated pathogens. Avoiding unnecessary splenectomies prevents those patients undergoing DP from facing significant thromboembolic [28] and infective risks [29]. The most serious post-splenectomy complication is overwhelming post-splenectomy infection (OPSI), which can start with flu-like symptoms but can rapidly progress to septic shock, coma, and disseminated intravascular coagulation [30]. OPSI can represent a major medical emergency, with a mortality rate that can be up to 50–70% [31,32], a yearly incidence of 0.23%, and a lifetime risk of approximately 5%. The risk is greater within the first two years postoperatively but can vary depending on patient risk factors, such as age, immunological status, and indication for splenectomy [33,34]. In order to protect splenectomized individuals from such complications, prophylactic pneumococcal, Haemophilus influenzae type b, meningococcal, and annual influenza vaccinations are usually performed. Despite these risks, splenectomy is routinely performed alongside DP for pancreatic adenocarcinoma in order to achieve an adequate oncological clearance, given the high risk of lymph node involvement [35]. Spleen preservation should be considered in all patients undergoing DP for benign indications or pre-malignant/low-grade tumors, as it has been shown to be a safe procedure that can reduce perioperative morbidity and enable better long-term outcomes [36,37,38,39]. The spleen can be preserved despite the excision of the splenic vessels, as firstly described by Warshaw in 1988 [27], or with splenic vessel preservation, as demonstrated by Kimura et al. almost a decade later [26]. Both approaches have been shown to have comparable short- and long-term results in a recent international multicentric retrospective study [40] and carry fewer complications when performed with a minimally invasive technique. After early experiences of laparoscopic DP [1,2], the minimally invasive approach to pancreatic surgery has progressively gained popularity, with safety and efficacy profiles comparable to open surgery, together with reduced blood loss and a faster recovery time [41,42,43,44,45]. According to the most recent evidence-based guidelines, minimally invasive DP should be considered over open DP for all patients with benign and low-grade malignant tumors [46]. The robotic technique, with its superior accuracy, 3D vision, greater range of motion and precision [47], and excellent safety and efficacy profile in complex oncological surgery [48,49], has been utilized by several surgeons when performing pancreatic procedures [5,50,51].
This meta-analysis showed that the robotic approach is more effective than laparoscopy in allowing spleen preservation during DP, with an RD of spleen preservation failures of 0.24 (95% CI 0.15, 0.33), with reduced intraoperative blood loss (mean difference of −138 mL (95% CI −205, −71)) and similar operative time (mean difference of 6.1 min (95% CI −40, 52)). Patients undergoing SP-RADP were also less likely to experience intraoperative conversion to the “open” technique, with 3/201 open conversions (1.5%) in the robotic group and 15/219 (6.8%) in the laparoscopic group, with an RD of −0.05 (95% CI −0.09, −0.01) [15,16,18,20,21,23,24,25]. It was not possible to identify the proportion of patients where splenic vessel excision (Warshaw technique) was planned preoperatively, but a higher proportion of splenic vessel preservation was observed in patients undergoing SP-RADP (159/196 patients (81.1%)) versus SP-LADP (84/154 (54.5%)). With the exception of cases of tumor proximity or vascular involvement of the splenic vessels, when splenectomy or the Warshaw technique are usually the preferred choices, the Kimura technique is generally the preferred approach. The higher proportion of successful splenic vessel preservations in the robotic group, coupled with the superior spleen preservation rate, could reflect the more precise vascular dissection of the small tributaries of the splenic artery and vein that can be performed robotically. No differences in overall, clinically significant complications (Clavien–Dindo grade ≥3) and POPF were observed between the two groups, but patients undergoing SP-RADP had a significantly shorter hospital LOS, with a mean difference of −1.5 days (95% CI −2.8, −0.2).
Due to the lack of long-term follow-up data, the postoperative morbidity results of the present meta-analysis could underestimate the possible beneficial effects of the robotic approach in terms of expected lower incidence of complications related to the occurrence of splenic infarctions and asplenia-related infections due to the significantly higher proportion of successful splenic and splenic vessel preservation in patients undergoing SP-RADP. Prevalence of overall complications, of Clavien–Dindo grade ≥3 complications, and of clinically relevant POPF were similar to those reported in the literature following minimally invasive DP and open DP [40], with overall complications reported in 31.5% and 45.4%, Clavien–Dindo grade ≥3 complications in 14.7% and 16.7%, and clinically relevant POPF in 14.8% and 15.1% of patients undergoing SP-RADP and SP-LADP, respectively.
Unfortunately, there was no randomized controlled trial directly comparing SP-RADP and SP-LADP that could be included in the present analysis. We performed a sensitivity analysis in order to further investigate the moderate heterogeneity (I2 = 63%) of the main outcome.
In conclusion, both SP-RADP and SP-LADP proved to be safe and effective procedures, with minimal perioperative mortality and low postoperative morbidity. The robotic approach proved to be superior to the laparoscopic approach in terms of spleen preservation rate, intraoperative blood loss, and hospital length of stay. Future prospective and randomized studies with a longer follow-up could better evaluate the possible differences between these two techniques in terms of mid- to long-term complications and outcomes.
Abbreviations
| ASA: | American Society of Anesthesiologists |
| BMI: | body mass index |
| CI: | confidence interval |
| DP: | distal pancreatectomy |
| IPMN: | intraductal papillary mucinous neoplasm |
| LOS: | length of stay |
| NET: | neuroendocrine tumors |
| OPSI: | overwhelming post-splenectomy infection |
| POPF: | postoperative pancreatic fistula |
| RD: | risk difference |
| SP-LADP: | spleen-preserving laparoscopic-assisted distal pancreatectomy |
| SP-RADP: | spleen-preserving robot-assisted distal pancreatectomy |
Author Contributions
Conceptualization, R.M. and G.R.; methodology, G.R.; software, R.M.; validation, R.I.T.; formal analysis, L.A.; resources, L.A.; writing—original draft preparation, G.R.; writing—review and editing, R.M. and R.I.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The data used for this manuscript are available upon request of the reviewers.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gagner M., Pomp A., Herrera M.F. Early experience with laparoscopic resections of islet cell tumors. Surgery. 1996;120:1051–1054. doi: 10.1016/S0039-6060(96)80054-7. [DOI] [PubMed] [Google Scholar]
- 2.Cuschieri A. Laparoscopic surgery of the pancreas. J. R. Coll. Surg. Edinb. 1994;39:178–184. [PubMed] [Google Scholar]
- 3.Melvin W.S., Needleman B., Krause K.R., Ellison E.C. Robotic Resection of Pancreatic Neuroendocrine Tumor. J. Laparoendosc. Adv. Surg. Tech. 2003;13:33–36. doi: 10.1089/109264203321235449. [DOI] [PubMed] [Google Scholar]
- 4.Masson B., Fernández-Cruz L., Sa-Cunha A., Adam J.-P., Jacquin A., Laurent C., Collet D. Laparoscopic Spleen-Preserving Distal Pancreatectomy: Splenic vessel preservation compared with the Warshaw technique. JAMA Surg. 2013;148:246–252. doi: 10.1001/jamasurg.2013.768. [DOI] [PubMed] [Google Scholar]
- 5.Esposito A., Casetti L., De Pastena M., Ramera M., Montagnini G., Landoni L., Bassi C., Salvia R. Robotic spleen-preserving distal pancreatectomy: The Verona experience. Updat. Surg. 2020;73:923–928. doi: 10.1007/s13304-020-00731-8. [DOI] [PubMed] [Google Scholar]
- 6.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bassi C., Marchegiani G., Dervenis C., Sarr M., Abu Hilal M., Adham M., Allen P., Andersson R., Asbun H.J., Besselink M.G., et al. International Study Group on Pancreatic Surgery (ISGPS). The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery. 2017;161:584–591. doi: 10.1016/j.surg.2016.11.014. [DOI] [PubMed] [Google Scholar]
- 8.Dindo D., Demartines N., Clavien P.-A. Classification of Surgical Complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wells G., Shea B., O’Connell D., Peterson J., Welch V., Losos M., Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. [(accessed on 1 June 2021)]; Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 10.Hultcrantz M., Rind D., Akl E.A., Treweek S., Mustafa R.A., Iorio A., Alper B.S., Meerpohl J., Murad M.H., Ansari M.T., et al. The GRADE Working Group clarifies the construct of certainty of evidence. J. Clin. Epidemiol. 2017;87:4–13. doi: 10.1016/j.jclinepi.2017.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wan X., Wang W., Liu J., Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res. Methodol. 2014;14:1–13. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higgins J.P.T., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 13.DerSimonian R., Laird N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 14.Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen S., Zhan Q., Chen J.-Z., Jin J.-B., Deng X.-X., Chen H., Shen B.-Y., Peng C.-H., Li H.-W. Robotic approach improves spleen-preserving rate and shortens postoperative hospital stay of laparoscopic distal pancreatectomy: A matched cohort study. Surg. Endosc. 2015;29:3507–3518. doi: 10.1007/s00464-015-4101-5. [DOI] [PubMed] [Google Scholar]
- 16.Eckhardt S., Schicker C., Maurer E., Fendrich V., Bartsch D.K. Robotic-Assisted Approach Improves Vessel Preservation in Spleen-Preserving Distal Pancreatectomy. Dig. Surg. 2016;33:406–413. doi: 10.1159/000444269. [DOI] [PubMed] [Google Scholar]
- 17.Hong S., Song K.B., Madkhali A.A., Hwang K., Yoo D., Lee J.W., Youn W.Y., Alshammary S., Park Y., Lee W., et al. Robotic versus laparoscopic distal pancreatectomy for left-sided pancreatic tumors: A single surgeon’s experience of 228 consecutive cases. Surg. Endosc. 2020;34:2465–2473. doi: 10.1007/s00464-019-07047-8. [DOI] [PubMed] [Google Scholar]
- 18.Kang C.M., Kim D.H., Lee W.J., Chi H.S. Conventional laparoscopic and robot-assisted spleen-preserving pancreatectomy: Does da Vinci have clinical advantages? Surg. Endosc. 2011;25:2004–2009. doi: 10.1007/s00464-010-1504-1. [DOI] [PubMed] [Google Scholar]
- 19.Liu R., Liu Q., Zhao Z.-M., Tan X.-L., Gao Y.-X., Zhao G.-D. Robotic versus laparoscopic distal pancreatectomy: A propensity score-matched study. J. Surg. Oncol. 2017;116:461–469. doi: 10.1002/jso.24676. [DOI] [PubMed] [Google Scholar]
- 20.Morelli L., Guadagni S., Palmeri M., Di Franco G., Caprili G., D’Isidoro C., Bastiani L., Di Candio G., Pietrabissa A., Mosca F. A Case-Control Comparison of Surgical and Functional Outcomes of Robotic-Assisted Spleen-Preserving Left Side Pancreatectomy versus Pure Laparoscopy. J. Pancreas. 2016;17:30–35. [Google Scholar]
- 21.Najafi N., Mintziras I., Wiese D., Albers M.B., Maurer E., Bartsch D.K. A retrospective comparison of robotic versus laparoscopic distal resection and enucleation for potentially benign pancreatic neoplasms. Surg. Today. 2020;50:872–880. doi: 10.1007/s00595-020-01966-z. [DOI] [PubMed] [Google Scholar]
- 22.Nell S., Brunaud L., Ayav A., Bonsing B.A., Koerkamp B.G., van Dijkum E.J.N., Kazemier G., de Kleine R.H., Hagendoorn J., Molenaar I.Q., et al. Robot-assisted spleen preserving pancreatic surgery in MEN1 patients. J. Surg. Oncol. 2016;114:456–461. doi: 10.1002/jso.24315. [DOI] [PubMed] [Google Scholar]
- 23.Souche R., Herrero A., Bourel G., Chauvat J., Pirlet I., Guillon F., Nocca D., Borie F., Mercier G., Fabre J.-M. Robotic versus laparoscopic distal pancreatectomy: A French prospective single-center experience and cost-effectiveness analysis. Surg. Endosc. 2018;32:3562–3569. doi: 10.1007/s00464-018-6080-9. [DOI] [PubMed] [Google Scholar]
- 24.Yang S.J., Hwang H.K., Kang C.M., Lee W.J. Revisiting the potential advantage of robotic surgical system in spleen-preserving distal pancreatectomy over conventional laparoscopic approach. Ann. Transl. Med. 2020;8:188. doi: 10.21037/atm.2020.01.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang J., Jin J., Chen S., Gu J., Zhu Y., Qin K., Zhan Q., Cheng D., Chen H., Deng X., et al. Minimally invasive distal pancreatectomy for PNETs: Laparoscopic or robotic approach? Oncotarget. 2017;8:33872–33883. doi: 10.18632/oncotarget.17513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kimura W., Inoue T., Futakawa N., Shinkai H., Han I., Muto T. Spleen-preserving distal pancreatectomy with conservation of the splenic artery and vein. Surgery. 1996;120:885–890. doi: 10.1016/S0039-6060(96)80099-7. [DOI] [PubMed] [Google Scholar]
- 27.Warshaw A.L. Conservation of the Spleen With Distal Pancreatectomy. Arch. Surg. 1988;123:550–553. doi: 10.1001/archsurg.1988.01400290032004. [DOI] [PubMed] [Google Scholar]
- 28.Rottenstreich A., Kleinstern G., Spectre G., Da’As N., Ziv E., Kalish Y. Thromboembolic Events Following Splenectomy: Risk Factors, Prevention, Management and Outcomes. World J. Surg. 2018;42:675–681. doi: 10.1007/s00268-017-4185-2. [DOI] [PubMed] [Google Scholar]
- 29.Hansen K., Singer D.B. Asplenic-hyposplenic Overwhelming Sepsis: Postsplenectomy Sepsis Revisited. Pediatr. Dev. Pathol. 2001;4:105–121. doi: 10.1007/s100240010145. [DOI] [PubMed] [Google Scholar]
- 30.Tahir F., Ahmed J., Malik F. Post-splenectomy Sepsis: A Review of the Literature. Cureus. 2020;12:e6898. doi: 10.7759/cureus.6898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sinwar P.D. Overwhelming post splenectomy infection syndrome—Review study. Int. J. Surg. 2014;12:1314–1316. doi: 10.1016/j.ijsu.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 32.Sarangi J., Coleby M., Trivella M., Reilly S. Prevention of post splenectomy sepsis: A population based approach. J. Public Health. 1997;19:208–212. doi: 10.1093/oxfordjournals.pubmed.a024611. [DOI] [PubMed] [Google Scholar]
- 33.Davidson R., Wall R. Prevention and management of infections in patients without a spleen. Clin. Microbiol. Infect. 2001;7:657–660. doi: 10.1046/j.1198-743x.2001.00355.x. [DOI] [PubMed] [Google Scholar]
- 34.Edgren G., Almqvist R., Hartman M., Utter G.H. Splenectomy and the Risk of Sepsis: A population-based cohort study. Ann. Surg. 2014;260:1081–1087. doi: 10.1097/SLA.0000000000000439. [DOI] [PubMed] [Google Scholar]
- 35.Jain G., Chakravartty S., Patel A.G. Spleen-preserving distal pancreatectomy with and without splenic vessel ligation: A systematic review. HPB. 2013;15:403–410. doi: 10.1111/hpb.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shoup M., Brennan M., McWhite K., Leung D.H.Y., Klimstra D., Conlon K.C. The Value of Splenic Preservation with Distal Pancreatectomy. Arch. Surg. 2002;137:164–168. doi: 10.1001/archsurg.137.2.164. [DOI] [PubMed] [Google Scholar]
- 37.Lillemoe K.D., Kaushal S., Cameron J.L., Sohn T.A., Pitt H.A., Yeo C.J. Distal Pancreatectomy: Indications and Outcomes in 235 Patients. Ann. Surg. 1999;229 doi: 10.1097/00000658-199905000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carrère N., Abid S., Julio C.H., Bloom E., Pradère B. Spleen-preserving Distal Pancreatectomy with Excision of Splenic Artery and Vein: A Case-matched Comparison with Conventional Distal Pancreatectomy with Splenectomy. World J. Surg. 2007;31:375–382. doi: 10.1007/s00268-006-0425-6. [DOI] [PubMed] [Google Scholar]
- 39.Jusoh A.C., Ammori B.J. Laparoscopic versus open distal pancreatectomy: A systematic review of comparative studies. Surg. Endosc. 2012;26:904–913. doi: 10.1007/s00464-011-2016-3. [DOI] [PubMed] [Google Scholar]
- 40.Paiella S., De Pastena M., Korrel M., Pan T.L., Butturini G., Nessi C., De Robertis R., Landoni L., Casetti L., Giardino A., et al. Long term outcome after minimally invasive and open Warshaw and Kimura techniques for spleen-preserving distal pancreatectomy: International multicenter retrospective study. Eur. J. Surg. Oncol. 2019;45:1668–1673. doi: 10.1016/j.ejso.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 41.Iacobone M., Citton M., Nitti N. Laparoscopic distal pancreatectomy: Up-to-date and literature review. World J. Gastroenterol. 2012;18:5329–5337. doi: 10.3748/wjg.v18.i38.5329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Merchant N.B., Parikh A.A., Kooby D.A. Should All Distal Pancreatectomies Be Performed Laparoscopically? Adv. Surg. 2009;43:283–300. doi: 10.1016/j.yasu.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 43.Butturini G., Damoli I., Crepaz L., Malleo G., Marchegiani G., Daskalaki D., Esposito A., Cingarlini S., Salvia R., Bassi C. A prospective non-randomised single-center study comparing laparoscopic and robotic distal pancreatectomy. Surg. Endosc. 2015;29:3163–3170. doi: 10.1007/s00464-014-4043-3. [DOI] [PubMed] [Google Scholar]
- 44.Cao H.S.T., Lopez N., Chang D.C., Lowy A.M., Bouvet M., Baumgartner J.M., Talamini M.A., Sicklick J.K. Improved Perioperative Outcomes with Minimally Invasive Distal Pancreatectomy: Results from a population-based analysis. JAMA Surg. 2014;149:237–243. doi: 10.1001/jamasurg.2013.3202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.De Rooij T., Van Hilst J., Van Santvoort H., Boerma D., Boezem P.V.D., Daams F., Van Dam R., DeJong C., Van Duyn E., Dijkgraaf M., et al. Minimally Invasive Versus Open Distal Pancreatectomy (LEOPARD): A Multicenter Patient-blinded Randomized Controlled Trial. Ann. Surg. 2019;269:2–9. doi: 10.1097/SLA.0000000000002979. [DOI] [PubMed] [Google Scholar]
- 46.Asbun H.J., Moekotte A.L., Vissers F.L., Kunzler F., Cipriani F., Alseidi A., D’Angelica M.I., Balduzzi A., Bassi C., Björnsson B., et al. The Miami International Evidence-based Guidelines on Minimally Invasive Pancreas Resection. Ann. Surg. 2020;271:1–14. doi: 10.1097/SLA.0000000000003590. [DOI] [PubMed] [Google Scholar]
- 47.Troisi R.I., Pegoraro F., Giglio M.C., Rompianesi G., Berardi G., Tomassini F., De Simone G., Aprea G., Montalti R., De Palma G.D. Robotic approach to the liver: Open surgery in a closed abdomen or laparoscopic surgery with technical constraints? Surg. Oncol. 2020;33:239–248. doi: 10.1016/j.suronc.2019.10.012. [DOI] [PubMed] [Google Scholar]
- 48.Hu Y., Strong V.E. Robotic Surgery and Oncologic Outcomes. JAMA Oncol. 2020;6:1537–1539. doi: 10.1001/jamaoncol.2020.2996. [DOI] [PubMed] [Google Scholar]
- 49.Ceccarelli G., Andolfi E., Biancafarina A., Rocca A., Amato M., Milone M., Scricciolo M., Frezza B., Miranda E., De Prizio M., et al. Robot-assisted surgery in elderly and very elderly population: Our experience in oncologic and general surgery with literature review. Aging Clin. Exp. Res. 2017;29:55–63. doi: 10.1007/s40520-016-0676-5. [DOI] [PubMed] [Google Scholar]
- 50.Daouadi M., Zureikat A., Zenati M.S., Choudry H., Tsung A., Bartlett D.L., Hughes S.J., Lee K.K., Moser A.J., Zeh H.J. Robot-Assisted Minimally Invasive Distal Pancreatectomy Is Superior to the Laparoscopic Technique. Ann. Surg. 2013;257:128–132. doi: 10.1097/SLA.0b013e31825fff08. [DOI] [PubMed] [Google Scholar]
- 51.Huang B., Feng L., Zhao J. Systematic review and meta-analysis of robotic versus laparoscopic distal pancreatectomy for benign and malignant pancreatic lesions. Surg. Endosc. 2016;30:4078–4085. doi: 10.1007/s00464-015-4723-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used for this manuscript are available upon request of the reviewers.