Abstract
American Indian and Alaska Native (AI/AN) youth exhibit multiple health disparities, including high rates of alcohol and other drug (AOD) use, violence and delinquency, and mental health problems. Approximately 70% of AI/AN youth reside in urban areas, where negative outcomes on behavioral health and well-being are often high. Identity development may be particularly complex in urban settings, where youth may face more fragmented and lower density AI/AN communities, as well as mixed racial-ethnic ancestry and decreased familiarity with AI/AN lifeways. This study examines racial-ethnic and cultural identity among AI/AN adolescents and associations with behavioral health and well-being by analyzing quantitative data collected from a baseline assessment of 185 AI/AN urban adolescents from California who were part of a substance use intervention study. Adolescents who identified as AI/AN on their survey reported better mental health, less alcohol and marijuana use, lower rates of delinquency, and increased happiness and spiritual health.
Keywords: racial/ethnic identity, alcohol and drug use/abuse/addiction, delinquency, spirituality, health
It is well known that American Indian and Alaska Native (AI/AN) youth exhibit health disparities across a range of health domains, including high rates of alcohol and other drug (AOD) use (Stanley, Harness, Swaim, & Beauvais, 2014; Substance Abuse and Mental Health Services Administration, 2014), violence and delinquency, physical health morbidity, and poor mental health (Pavkov, Travis, Fox, King, & Cross, 2010; Whitbeck, 2011). Approximately 70% of AI/AN youth reside in urban areas (Norris, Vines, & Hoeffel, 2012), where AI/AN often report negative outcomes related to behavioral health and well-being, including AOD problems and poor physical health (Castor et al., 2006; Dickerson et al., 2012). Acculturative stress directly and indirectly associated with historical trauma experienced by AI/ANs has been linked to these negative behavioral health outcomes (Lane & Simmons, 2011; Whitesell, Beals, Crow, Mitchell, & Novins, 2012; Willmon-Haque & BigFoot, 2008). However, our understanding of how urban AI/AN adolescents form their racial-ethnic and cultural identity and how this identity formation may relate to behavioral health and well-being is limited (House, Stiffman, & Brown, 2006; Kulis, Wagaman, Tso, & Brown, 2013; Lucero, 2010; Walters, 1999).
Racial-ethnic and cultural identity are complex and dynamic in the United States; individuals often identify as belonging to two or more different races, ethnicities, or cultural groups, and “some other race” is now the third most selected racial-ethnic category on the U.S. Census (Ashok, 2016). This is increasingly the case as demographic diversity in the United States continues to rise via immigration, shifting residential patterns, and high rates of racial-ethnic intermarriage (Lee, Martin, Matthews, & Farrell, 2017; Lee & Bean, 2010). This is especially true for the AI/AN population, which has seen high rates of marriage to Whites and other non-AI/AN partners since the 1970s (Eschbach, 1995; Qian & Lichter, 2011). In fact, non-Hispanic White and American Indian adults account for the largest share of multiracial adults in the United States (Cohn, 2015). In addition, racial-ethnic and cultural identity can shift over the life span, especially during the process of identity formation throughout adolescence and young adulthood (Quintana, 2007). Recent longitudinal research has shown that both youth and adults in the United States shift their racial-ethnic identification over time. For example, DeFina and Hannon (2016) found that Latinos, AI/ANs, and those identifying as mixed race were particularly likely to switch their racial identification over time compared with other groups (e.g., African Americans). In addition, Liebler, Porter, Fernandez, Noon, and Ennis (2017) found that individuals identifying as AI/AN in 1 year often switched their status to White in a subsequent year (and vice versa).
We need a better understanding of cultural and racial-ethnic identity among AI/AN populations as it relates to various historical-based traumas, including forced relocation and the attempted genocide (and cultural genocide) of AI/AN populations by the U.S. Government (Evans-Campbell, 2008; Heart, 2003; James, 1992). For the purposes of this study, we define historical trauma as experience (by either the respondent or their parents/grandparents) of systematic attempts to commit genocide and cultural genocide on AI/ANs, including time spent in Indian boarding schools (in the 1950s or before) and forced displacement from tribal lands (Whitbeck, Adams, Hoyt, & Chen, 2004). Urban AI/ANs were directly affected by historical trauma via the Indian Relocation Act of 1956, which encouraged Native Americans to leave their tribal lands and resettle in cities (Burt, 1986); many studies have discovered that resettlement placed enormous stress on AI/ANs, leading to multiple health disparities (see review in Szlemko, Wood, & Thurman, 2006).
Racial-ethnic identity can be particularly complex for AI/ANs living in urban areas (Lucero, 2010; Walters, 1999), due in part to geographic dispersion from other AI/ANs (Hartmann, Wendt, Saftner, Marcus, & Momper, 2014) and the stress of adapting to urban environments (Stumblingbear-Riddle & Romans, 2012). Several studies have identified complex processes of racial-ethnic and cultural identity among AI/AN youth and adults, including urban AI/ANs; these studies indicate that identifying with AI/AN culture may be protective against negative outcomes, such as substance use and antisocial behavior (Kulis, Hodge, Ayers, Brown, & Marsiglia, 2011; LaFromboise, Hoyt, Oliver, & Whitbeck, 2006). Furthermore, existing studies describe a dynamic process of identity development, which may often start with rejection of the identity or internalization of negative stereotypes, and eventually converge on a healthy integration of AI/AN identity (Lucero, 2010). Indeed, some studies have found that identifying both with AI/AN culture and another cultural identity may be especially protective (Szlemko et al., 2006).
We conducted qualitative research with AI/AN adolescents, parents, providers, and elders to help design an intervention focused on urban AI/AN adolescents in California—Motivational Interviewing and Culture for Urban Native American Youth (MICUNAY). This qualitative work emphasized that AI/AN adolescents struggle with cultural disconnection, mixed identity, and racial-ethnic discrimination. We also found that cultural identity and participation in traditional practices are protective for AI/AN youth (Brown, Dickerson, & D’Amico, 2016). The current study continues to address the important issue of identity by focusing on quantitative data collected from a baseline assessment of 185 AI/AN urban adolescents from central, southern, and northern California who were part of a substance use intervention study (Dickerson, Brown, Johnson, Schweigman, & D’Amico, 2016). The baseline assessment included information on racial-ethnic identity, cultural identity scales, adolescents’ participation in traditional practices, and behavioral health and well-being outcomes—including mental and physical health, AOD use, and delinquency.
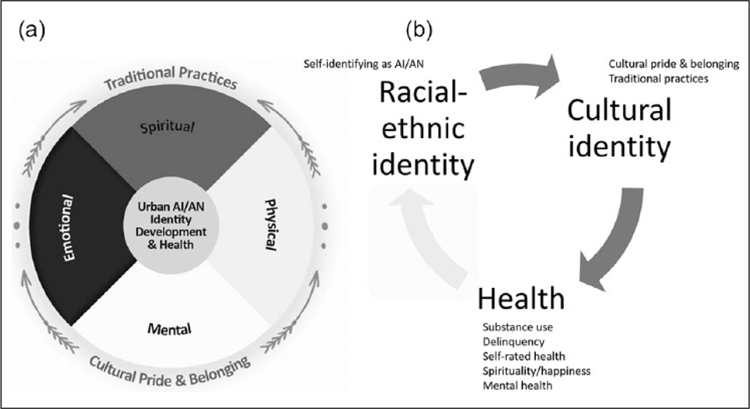
This article explores racial-ethnic identification among AI/AN adolescents by examining whether they explicitly identified as AI/AN or not on their baseline survey and how this identification relates to cultural identity, as well as behavioral health and well-being. We provide a theoretical conceptualization of behavioral health and well-being as it relates to AI/AN racial-ethnic and cultural identity (see Figure 1a and 1b). We acknowledge that debates regarding the theoretical underpinning, empirical science, and definition of racial-ethnic identity and cultural identity persist in the literature (Smith & Silva, 2011). For the purposes of this study, we define racial-ethnic identity as ascribing to oneself the label of being AI/AN, regardless of why the respondent chooses to do so (e.g., they could believe this identity is determined by genetics, growing up on a reservation, assigned by their relatives, etc.). We define cultural identity as exhibiting beliefs or practices that are related (or one believes are related) to a racial-ethnic identity of being AI/AN or a specific tribal identity.
Figure 1.
Indigenous conceptual model of behavioral health and well-being as it relates to the urban setting. (a) AI/AN cultural identity and engagement in traditional practices during development. (b) Theoretical model with variables and assumed causal pathways.
AI/AN = American Indian and Alaska Native.
Given findings across many different racial-ethnic groups showing the positive benefits of association with group members (Smith & Silva, 2011), we expected that the urban adolescents who identified as AI/AN in this study would also report better health outcomes. Other work has indicated that AI/AN cultural identity and participation in traditional practices are both associated with positive behavioral health outcomes (Fleming & Ledogar, 2008; Stone, Whitbeck, Chen, Johnson, & Olson, 2006). We therefore hypothesized that participation in traditional practices and AI/AN cultural pride and belonging would mediate the association between AI/AN self-identification and better health outcomes. Specifically, we expected the psychological and social benefits linked with racial-ethnic identification as AI/AN to benefit adolescents via the positive social interactions and positive sense of self, resulting from participation in culturally linked activities (Donovan et al., 2015).
Method
Sampling and Recruitment
We recruited AI/AN adolescents in northern, central, and southern California in five urban areas (including two locations that were target destinations during the Indian Relocation Act of 1956). Adolescents were recruited from 2014 to 2017 as part of an intervention trial testing MICUNAY, a new AOD use prevention program integrating motivational interviewing with AI/AN traditional practices (Dickerson et al., 2016), and represent more than 60 different tribes. We recruited for the study at community information events and Pow Wows and were also assisted by several AI/AN health and community programs in the five urban areas. We also posted information on AI/AN community-based email lists and on Facebook, and we hired AI/AN recruiters in each community to discuss the project with AI/AN families. In addition, we worked with several community-based organizations across California that serve AI/AN adolescents to help us recruit for the project. To be included, adolescents had to be 14 to 18 years old (inclusive) and either verbally identify as AI/AN or be identified as AI/AN by a family member. Our collaborator, Sacred Path Indigenous Wellness Center (SPIWC), and our community advisory board worked closely with our team to ensure that our recruitment and engagement with these AI/AN urban communities was conducted in a culturally appropriate manner. Our community-based participatory research approach (CBPR) is reflective of a strategy routinely used in National Institutes of Health (NIH)-funded studies of new health interventions (Dickerson et al., 2018; Minkler & Wallerstein, 2011). Data for this article are from the baseline survey, for which adolescents were paid US$25. Further descriptive information on the sample is available in D’Amico et al. (2019); rich qualitative data describing the experiences of youth in this sample in their urban environments are available in Brown et al. (2016).
Measures
Race-ethnicity.
Adolescents verbally self-identified as AI/AN (or were identified as AI/AN by a family member) to be eligible for the study. In a subsequent self-report survey using categories established by NIH, participants were asked to “mark all that apply” for the following categories: American Indian or Alaska Native, Hispanic or Latino/Latina, Asian or Asian American, Native Hawaiian or Pacific Islander, Black or African American, White or Caucasian, and other. We created three categories based on AI/AN self-identification on the survey: (a) identified only as AI/AN, (b) identified as AI/AN and at least one other category, (c) did not identify as AI/AN.
AI/AN traditional practices.
Adolescents reported if they had ever participated in AI/AN traditional practices. The survey listed 24 different activities, along with an “other” option. Adolescents reported the number of times they had engaged in each of the activities in their lifetime (6 response options ranging from “none” to “more than 20 times”). Summing across the 25 activities, we calculated the total number of times each youth had participated in traditional practices. Traditional practice items were based upon extensive research conducted with AI/AN adolescents, parents, and community partners (Kaufman et al., 2014).
Cultural pride and belonging.
We assessed adolescents’ sense of AI/AN cultural pride and sense of belonging with the Multigroup Ethnic Identity Measure (MEIM), which has 12 items (α = .94) in which respondents are asked the degree to which they agree with statements such as, “I have a clear sense of my ethnic background and what it means to me” on a scale from 1 = strongly disagree to 5 = strongly agree (Phinney & Ong, 2007; Ponterotto, Gretchen, Utsey, Stracuzzi, & Saya, 2003). Given that our focus group work indicated that many adolescents were of mixed ethnicity and our focus was on AI/AN identity, we modified items to focus on AI/AN heritage (e.g., “I have clear sense of my AI/AN identity and what it means to me”). We used the mean for all 12 items in analyses.
AOD use.
We assessed AOD use with well-established Monitoring the Future items (Miech, Johnston, Malley, Bachman, & Schulenberg, 2016), which have been used across racial-ethnic groups, including AI/ANs (Plunkett & Mitchell, 2000). Adolescents were asked “how many times have you used or tried …” a variety of substances over the past 3 months (90 days), with six response options ranging from “none” to “more than 20 times.” For this study, we created an indicator of whether adolescents reported any use of alcohol or marijuana. We created this dichotomous indicator as AOD use rates are typically lower in younger adolescents, leading to highly skewed distributions (D’Amico et al., 2016).
Mental health status.
Mental health (e.g., felt downhearted and blue; been very nervous; α = .74) was measured with the well-validated five-item Mental Health Inventory (MHI-5; Stewart, Ware, Sherbourne, & Wells, 1992). Relevant items are reversed, so that a higher total score (transformed to range from 0 to 100) indicates better mental health. The MHI-5 focuses on depression and anxiety symptoms; a score of 60 or higher is considered “good” mental health for adolescents, based on associations of this cut-off with diagnostic criteria for depression and anxiety (Berwick et al., 1991; Kelly, Dunstan, Lloyd, & Fone, 2008), and has been used with AI/ANs in previous research (Pfefferle & Spitznagel, 2009).
Self-rated health.
Health was measured with an item assessing general health on a 5-point scale (1 = poor to 5 = excellent) from the Short-Form Health (SFH) Survey-12 (Ware, Kosinski, & Keller, 1996) in response to the question, “In general, would you say your health is [poor/fair/good/very good/excellent]?” This item has been used across racial-ethnic groups, including AI/ANs (McGee, Liao, Cao, & Cooper, 1999).
Delinquency.
Adolescents were asked “In the past 3 months, how often have you done each of the following things?” with six response options ranging from 1 = none to 6 = more than 20 times. These six items, which have been used with AI/AN youth in previous research (Tucker, Orlando, & Ellickson, 2003) were “Been drunk or high in a public,” “Been suspended or expelled from school,” “Taken something from a store that did not belong to you,” “Been sent out of the classroom for causing trouble,” “Damaged something on purpose that did not belong to you,” “Cheated on a test at school,” “Sold marijuana or hashish (grass, pot, weed),” “Driven a car, motorcycle or other vehicle after drinking alcohol or using drugs,” “Been a passenger in a car or other vehicle with a driver who has been drinking alcohol or using drugs,” and “written things or sprayed paint on walls or sidewalks or cars where you were not supposed to” (Hunter, Miles, Pedersen, Ewing, & D’Amico, 2014). Responses for the 10 items were summed (possible range: 10–60; α = .83).
Spirituality/happiness.
Spirituality and happiness were measured using a subset of 10 items from the 12-item Functional Assessment of Chronic Illness Therapy–Fatigue–Spiritual Questions instrument, or FACIT-SP 12 (Peterman, Fitchett, Brady, Hernandez, & Cella, 2002), which has been used with AI/ANs in previous studies (Dickerson, Annon, Hale, & Funmaker, 2014). Adolescents reported agreement with statements such as “I find comfort in my faith or spiritual beliefs” and “I feel a sense of harmony within myself.” Two items that referred specifically to chronic illness were removed from the scale as they were not relevant for this study. Response options, which ranged from 1 = not at all to 5 = very much were averaged (α = .83), with negative statements reversed such that higher scores indicated greater spirituality and happiness.
Data Analysis
We conducted a complete case analysis, as rates of missing data were low. Of the n = 185 youth who responded to the survey, five records were missing data on either age (n = 1) or the MEIM (n = 4) and were therefore excluded from the analysis. Among the n = 180 retained, mental health and spirituality were missing for n = 1, and delinquency was missing for n = 2; all cases were otherwise complete. See Table 1 for sample demographics.
Table 1.
Sample Demographics (n = 180).
| Characteristic (range) | % or M (SD) |
|||
|---|---|---|---|---|
| AI/AN self-identification | ||||
| AI/AN only (n = 63) |
Mixed (n = 85) |
Did not identify (n = 32) |
Overall (n = 180) |
|
| Female (%) | 55.6 | 51.8 | 43.8 | 51.7 |
| Age | 15.89 (1.35) | 15.56 (1.30) | 15.47 (1.37) | 15.63 (1.33) |
| Good mental health (%) | 79.0 | 70.6 | 46.9 | 69.3 |
| General health (1 = poor, 5 = excellent) | 3.63 (0.94) | 3.73 (0.89) | 3.63 (0.83) | 3.68 (0.89) |
| Any alcohol or marijuana use in past 3 months (%) | 34.9 | 25.9 | 50.0 | 33.3 |
| Frequency of delinquency events (10–60) | 12.75 (4.00) | 12.34 (3.76) | 14.81 (9.04) | 12.93 (5.22) |
| Spirituality/happiness (1–5) | 3.63 (0.75) | 3.76 (0.73) | 3.27 (0.79) | 3.63 (0.76) |
| Traditional practices (lifetime count, 0–525) | 119.4 (102.2) | 100.1 (98.2) | 31.5 (43.6) | 94.66 (97.06) |
| MEIM acculturation/identification (1–5) | 3.60 (0.77) | 3.38 (0.87) | 2.62 (0.67) | 3.32 (0.87) |
Note. Please contact the authors with any questions regarding data or statistical models. AI/AN = American Indian and Alaska Native; MEIM = Multigroup Ethnic Identity Measure.
We used a series of regression models to examine the association of AI/AN self-identity with our behavioral health and well-being outcomes: good mental health, any alcohol or marijuana use in the past 3 months, self-reported physical health, delinquency, and spirituality/happiness (Figure 1b). Mental health and AOD use were binary and modeled with logistic regression (using the LOGISTIC procedure in SAS version 9.4), whereas the other three outcomes were continuous and modeled with linear regression (using the generalized linear model [GLM] procedure). Three models were fit for each outcome.
The first model estimates the association between AI/AN self-identification on the survey and outcomes while controlling for age and gender. Model 2 estimates the same association controlling additionally for participation in traditional practices. Similarly, Model 3 controls for everything in Model 2 and adds cultural pride/belonging. The purpose of the second and third models is to determine whether the association we observe in Model 1 might be due, in whole or in part, to participation in traditional practices and/or cultural pride/belonging, indicating that these other factors could be confounders or mediators of this association (Figure 1b). Postestimation tests were conducted to test for all pairwise differences among the three self-identification groups.
Results
Results from all regression models are in Table 2. Adjusting for gender and age, adolescents who identified as either (a) exclusively AI/AN or (b) AI/AN and another racial-ethnic category (“mixed”) reported better mental health, less frequent alcohol and marijuana use, and fewer delinquent behaviors, in comparison with adolescents who did not identify as AI/AN (see results for Model 1 in Table 2). Table 2 provides details for regression results that reached statistical significance at the p < .05 threshold or below.
Table 2.
Associations of Various Outcomes With AI/AN Self-Identification.
| Outcome | Model | AI/AN self-identification |
Traditional practices (per 10) | MEIM | ||
|---|---|---|---|---|---|---|
| AI/AN only vs. did not identify | Mixed vs. did not identify | AI/AN only vs. mixed | ||||
| Binary | OR (CI) | |||||
| MHI-5 ≥ 60 | 1 | 5.41 [2.03, 14.44]** | 3.23 [1.34, 7.81]** | 1.67 [0.76, 3.70] | — | — |
| 2 | 5.56 [1.98, 15.64]** | 3.31 [1.31, 8.31]* | 1.68 [0.76, 3.72] | 1.00 [0.96, 1.04] | — | |
| 3 | 5.77 [1.96, 16.95]** | 3.41 [1.31, 8.85]* | 1.69 [0.76, 3.76] | 1.00 [0.96, 1.04] | 0.94 [0.57, 1.56] | |
| Alcohol or marijuana use in past 3 months | 1 | 0.36 [0.14, 0.95]* | 0.26 [0.10, 0.66]** | 1.41 [0.66, 3.02] | — | — |
| 2 | 0.29 [0.10, 0.80]* | 0.21 [0.08, 0.57]** | 1.36 [0.63, 2.94] | 1.03 [0.99, 1.07] | — | |
| 3 | 0.29 [0.10, 0.83]* | 0.21 [0.08, 0.59]** | 1.36 [0.63, 2.95] | 1.03 [0.99, 1.07] | 1.00 [0.61, 1.64] | |
| Continuous | b (SE) | |||||
| Self-reported health | 1 | 0.08 [–0.30, 0.46] | 0.14 [–0.22, 0.50] | −0.06 [–0.35, 0.23] | — | — |
| 2 | 0.01 [–0.39, 0.41] | 0.08 [–0.29, 0.46] | −0.07 [–0.36, 0.22] | 0.008 [–0.006, 0.023] | — | |
| 3 | 0.01 [–0.41, 0.42] | 0.08 [–0.30, 0.46] | −0.07 [–0.37, 0.22] | 0.008 [–0.008, 0.024] | 0.01 [–0.18, 0.19] | |
| Delinquency | 1 | −2.21 [–4.43, 0.01]† | −2.49 [–4.59, –0.39]* | 0.28 [–1.42, 1.98] | — | — |
| 2 | −2.88 [–5.19, –0.57]* | −3.03 [–5.19, –0.88]** | 0.15 [–1.54, 1.84] | 0.080 [–0.002, 0.162]† | — | |
| 3 | −2.60 [–5.00, –0.20]* | −2.80 [–5.02, –0.58]* | 0.20 [–1.50, 1.90] | 0.098 [0.006, 0.189]* | −0.48 [–1.57, 0.60] | |
| Spirituality/Happiness | 1 | 0.34 [0.02, 0.66]* | 0.49 [0.18, 0.80]** | −0.15 [–0.40, 0.09] | — | — |
| 2 | 0.21 [–0.13, 0.55] | 0.39 [0.07, 0.70]* | −0.18 [–0.42, 0.06] | 0.014 [0.002, 0.026]* | — | |
| 3 | 0.14 [–0.21, 0.49] | 0.33 [0.01, 0.66]* | −0.21 [0.12]† | 0.009 [–0.004, 0.022] | 0.12 [–0.03, 0.28] | |
Note. All models control for gender and age. Model ns vary from 178 to 180 depending on outcome. n = 5 participants were excluded due to missing age or MEIM. AI/ AN = American Indian and Alaska Native; OR = odds ratio; CI = confidence interval; MEIM = Multigroup Ethnic Identity Measure.
p < .10.
p < .05.
p < .01.
p < .001.
The odds that an adolescent who identified exclusively as AI/AN reported good mental health were 5.41 times higher (95% confidence interval [CI] = [2.03, 14.44]) than those who did not identify as AI/AN. The odds that mixed adolescents reported good mental health were 3.23 times higher (95% CI = [1.34, 7.81]) than adolescents who did not identify as AI/AN. Similarly, adolescents identifying exclusively as AI/AN were only 36% as likely to report any alcohol or marijuana use in the last 30 days versus youth who did not identify as AI/AN (95% CI = [0.14, 0.95]), while mixed adolescents were only 26% as likely to use alcohol or marijuana in the last 30 days compared with nonidentifying youth (95% CI = [0.10, 0.66]).
Furthermore, adolescents who self-identified as mixed reported 2.49 fewer delinquent behaviors (95% CI = [−4.59, −0.39]) than those who did not identify as AI/AN. The pattern for delinquency indicated greater scores for adolescents who identified exclusively as AI/AN, but this did not reach statistical significance (p = .051). Adolescents identifying exclusively as AI/AN and mixed adolescents both showed significantly higher spirituality and happiness compared with those who did not self-identify as AI/AN, scoring on average 0.34 (95% CI = [0.02, 0.66]) and 0.49 points (95% CI = [0.18, 0.80]) higher on the spirituality/happiness scale, respectively. We did not find any statistically significant differences between these groups for self-reported health.
After adjusting for participation in traditional practices (Model 2) and cultural pride/belonging (Model 3), we found similar results. Specifically, odds ratios and regression coefficients showed little change when we entered traditional practices and the MEIM scale (cultural pride/belonging) into the models. Thus, results suggest that differences observed in mental health, AOD use, and delinquency are not explained by participation in traditional practices or cultural pride/belonging and casts doubt on the possibility that traditional practices or pride/belonging mediates the association between these behavioral health/well-being outcomes and self-identification. We did find very small positive associations with both delinquent behaviors and spirituality/happiness and participation in traditional practices; specifically, youth engaging in 10 or more traditional practices over their lifetime showed an average of 0.10 (95% CI = [0.01, 0.19]) additional delinquent behaviors in Model 3 and scored 0.01 (95% CI = [0.00, 0.03]) points higher on the spirituality/happiness scale in Model 2. No associations with the MEIM were statistically significant.
Discussion
This study advances our understanding of racial-ethnic and cultural identity among urban AI/AN adolescents and the relationship of AI/AN self-identification with behavioral health and well-being outcomes. Using a richly described quantitative sample of urban AI/AN adolescents in California, we tested associations between identifying as AI/AN and several behavioral health outcomes and well-being. We also examined effects of participation in traditional practices and cultural pride/belonging on these behavioral health outcomes.
Our results indicated that adolescents identifying as AI/AN only or AI/AN mixed with other racial-ethnic identities on their survey reported better mental health, less delinquency, higher spirituality/happiness, and were less likely to use AOD than adolescents who did not identify as AI/AN. This fits with a large body of previous work documenting the association between AI/AN “enculturation” levels and such diverse outcomes as violent offending, AOD use, mental health, and educational attainment (Fleming & Ledogar, 2008; LaFromboise et al., 2006; Shepherd, Delgado, Sherwood, & Paradies, 2017). Moreover, these associations have been found both in the United States and other locations (such as Australia), with Indigenous populations that have faced marginalization and historical trauma (Dockery, 2010). Furthermore, work on identity development with other racial/ethnic groups has shown that strong group identification is associated with more positive health, psychosocial, and academic outcomes among Latino and African American youth, and these effects seem to be driven by a correlation between group identification and positive affect for one’s racial-ethnic group (Hughes, Kiecolt, Keith, & Demo, 2015; Rivas-Drake et al., 2014).
Of note, previous studies have demonstrated these associations using measures of participation in traditional practices or scales that assess cultural pride and sense of belonging. In our study, surprisingly, participation in traditional practices and AI/AN racial-ethnic belonging (as measured by the MEIM) showed little indication of mediating the association between AI/AN self-identification and better behavioral health and well-being, nor did they show much evidence of independent associations with these outcomes after controlling for self-identification. Rather, AI/AN self-identification itself showed the strongest association with behavioral health and well-being, suggesting that self-identification in this sample of urban AI/AN adolescents may represent aspects of cultural identity not measured by scales such as the MEIM or participation in traditional practices per se. In other words, at least with urban AI/AN adolescents in our California sample, simply identifying as AI/AN seemed to represent a suite of processes connecting culture and identity with resilience that are not easily measured with other common approaches to assessing cultural identity. This raises the question of what determines racial-ethnic identification as AI/AN among urban adolescents, which we suggest should be a topic of future study.
Overall, our findings highlight that all adolescents self-identifying as AI/AN only or AI/AN mixed with other racial-ethnic identities exhibited better health outcomes. A long history of research has described how healthy developmental trajectories for adolescents with multiple racial-ethnic identities involves some manner of reconciling and blending these identities (Renn, 2008). As AI/AN youth show some of the highest racial-ethnic switching from year to year (DeFina & Hannon, 2016; Liebler et al., 2017), it is possible that adolescents in our sample who identified as AI/AN and at least one other ethnicity have achieved successful identity integration or resolution (Ruiz, 1990).
Notably, we estimated the association between AI/AN identity and self-reported health (SRH) to be small at best. This is likely due both to constrained variation in SRH at this age, and the relative instability of SRH in adolescent populations (Boardman, 2006). Also, we found an unexpected (and small) positive relationship between participation in traditional practices and delinquent behaviors. It is possible that this is due to some sort of social iatrogenic effect, as both traditional practices and delinquent behaviors involve group participation (Dishion, Poulin, & Burraston, 2001). However, the small size of this effect and the fact that it only appeared while controlling for several other variables suggest interpretive caution.
Conclusion and Limitations
Our study joins a host of other studies highlighting the importance of racial-ethnic and cultural identity for AOD use and other behavioral health and well-being outcomes (Hughes et al., 2015; Rivas-Drake et al., 2014). It is important to note that we found this association in an urban sample that included three of the major government-designated relocation cities during the Indian Relocation Act of 1956 and that this sample describes a complex psychological and social relationship with AI/AN identity in previous work (Brown et al., 2016). Specifically, we found that endorsement of AI/AN identity in this sample is associated with better health outcomes, regardless of other racial-ethnic identity. This suggests the importance of future work on multiple racial-ethnic identities and the dynamic deployment of these identities in everyday life (e.g., “code-switching”).
Whereas many previous studies suggest that participation in traditional practices or cultural pride and sense of belonging drives the association between racial-ethnic identity and positive outcomes, our results suggest that identification alone may “carry” resilient effects, albeit for unknown reasons. It may be that AI/AN identification is a marker of developmental maturity or “stage” of racial-ethnic identity development and integration. Lack of AI/AN identity in adolescents otherwise identified as AI/AN may be a marker of conflicted identity and perhaps even a warning signal for risk behaviors.
Due to the cross-sectional nature of our study, causal direction (including mediation) is impossible to derive with any certainty due to lack of knowledge about the sequencing of the measured constructs across developmental time. Thus, while we developed a conceptual model of the direction of effects, it is unclear whether (a) identifying as AI/AN itself leads to changes in adolescents’ psychological state, social networks, coping behaviors, or other possible causal pathways to improved mental health, lower likelihood of AOD use, decreased delinquency, and enhanced spirituality; (b) improved behavioral health and well-being somehow makes adolescents more open or accepting of their AI/AN heritage; or (c) both AI/AN self-identification and better behavioral health and well-being are correlated with a third, unidentified variable that is responsible for coincidental changes in both. It is possible that AI/AN identification is more appealing after some degree of maturity or resilience is established—especially among adolescents with conflicted or multiple identities, difficult family relationships with AI/AN parents or other family members. It is also possible that we are seeing some degree of causal pathway from identification as AI/AN and downstream positive effects on health and behavior. Most likely, we are observing a mixture of causal directions; different for different adolescents, and perhaps changing causal directions at different points in the life span.
Some limitations of our sample are that they are comprised of urban AI/AN adolescents in one geographic region of the United States who were recruited mainly through AI/AN community-based organizations and networks. Thus, these adolescents may have had a more cohesive cultural identity than urban AI/AN youth overall. We are also unable to generalize whether these associations would hold for rural or reservation AI/AN youth— especially as differences in context (Brown et al., 2016) and health outcomes (Grossman, Krieger, Sugarman, & Forquera, 1994) for urban versus rural AI/AN populations have been seen in the past—and whether the patterns we found in this small urban sample from California would generalize to a more nationally representative sample of urban AI/AN youth. In addition, our measures of mental and physical health were limited; more comprehensive measurement may have produced different results. Another measurement-related limitation of our study is that although historical trauma is part of our theoretical framework, it was not directly operationalized in this study. Future studies, particularly longitudinal work, should continue to address how historical trauma may affect the well-being of urban and rural AI/AN youth.
Despite limitations, our study has several implications for intervention program design with urban AI/AN youth. First, results highlight that urban AI/AN adolescents may enter intervention programs at vastly different levels or “stages” of cultural identification. Thus, providing some type of cultural discussion and opportunity for cultural experiences in programming is one important way to help urban AI/AN adolescents think more about their AI/AN identity and how this identify fits with who they are as they develop over time (Dickerson et al., 2016). Moreover, adolescents who may not initially identify as AI/AN may experience health protective effects during their path to AI/AN identification, especially if this involves integrating AI/AN identity with one or more additional racial-ethnic identity. Thus, it is important that intervention programs remain open to adolescents at a wide variety of different places in their developmental trajectories of racial-ethnic and cultural identity. Moreover, it is critical to provide adolescents with opportunities to “get to know” their AI/AN roots in a wide variety of ways, and to mentor this process regardless of where it starts. Although this might sound difficult in a group environment, our experience has been that cultural interventions with AI/AN youth work well with youth at these different “starting places.” In fact, youth with more cultural knowledge sometimes become mentors or group experts and help guide other youth.
This study casts new light on racial-ethnic and cultural identity processes among urban AI/AN youth. While further studies—especially in other urban and rural environments—are needed to assess the robustness of the patterns we found, our results support previous research in this area suggesting that cultural identity is an important contributor to AI/AN resilience (Kulis et al., 2011; Kulis et al., 2013; Walters, 1999). Moreover, it suggests that self-identification itself, perhaps independent of traditional practices, cultural pride, or sense of belonging, may be particularly important for urban AI/AN adolescents.
Acknowledgments
We would like to thank our numerous American Indian/Alaska Native community partners, providers, parents, and youth for assisting with and participating in this study.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Work on this article was supported by a grant from the National Institute of Alcohol Abuse and Alcoholism R01AA022066 to Drs. D’Amico and Dickerson, with co-funding from the National Institute on Drug Abuse.
Author Biographies
Ryan A. Brown is a senior social and behavioral scientist at the RAND Corporation, and an anthropologist whose work focuses on novel ways of combining qualitative and quantitative data to explore the drivers of risk-taking and violent behavior. He has extensive experience conducting field research among marginalized youth populations. Brown’s multiple years of ethnographic work focuses on Cherokee and white groups of youth involved in trafficking and using substances both on and off the reservation, including heavy alcohol use.
Daniel L. Dickerson, D.O., M.P.H., (Inupiaq) is an addiction psychiatrist and Associate Research Psychiatrist at UCLA, Integrated Substance Abuse Programs (ISAP). He also provides psychiatric and substance abuse services at American Indian Counseling Center (AICC) in Los Angeles. His research focuses on the development of substance abuse treatment and prevention programs for American Indians and Alaska Natives.
David J. Klein is a senior statistical analyst at the RAND Corporation. He has worked on a wide variety of research projects, mostly in the health field, and has extensive experience with statistical analysis of complex survey data, as well as claims, census, and other sources of data. Recent projects include studies on the evaluation of Medicare CAHPS survey data, discrimination and health disparities, adolescent obesity, parent-child communication, adolescent risk behavior, quality and utilization of health care, use of paid family leave, and medication adherence.
Denis Agniel is an associate statistician at the RAND Corporation who conducts health policy research on topics such as substance use, HIV, and medical informatics. His methodological interests include longitudinal data, multivariate and mixed outcomes, survival analysis, multiple hypothesis testing, nonparametric and semiparametric statistics, and causal inference. Recent projects include estimating the association between opioid misuse and post-surgical opioid prescriptions and personalizing treatment for adolescents with substance use problems.
Carrie L. Johnson (Wahpeton Dakota) is a licensed clinical psychologist and the Director of the Seven Generations Child and Family Counseling Center at United American Indian Involvement in Los Angeles, California. For the last 20 years, Dr. Johnson has provided Behavioral Health services to American Indian and Alaska Natives in Los Angeles County, including mental health treatment, grant writing, and integrating traditional healing into services and evaluation of the services. She is also an experienced trainer and consultant in the effects of intergenerational trauma on American Indian and Alaska Native children, families, and communities.
Elizabeth J. D’Amico is a senior behavioral scientist at the RAND Corporation and a licensed clinical psychologist who is nationally recognized for her work developing, implementing, and evaluating interventions for adolescents. D’Amico has evaluated several motivational interviewing interventions with adolescents and young adults in a variety of settings, including middle schools, primary care, homeless shelters, and teen court. She has also conducted epidemiological work to examine predictors and consequences of adolescent substance use.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Ashok S (2016, August). The rise of the American “others.” The Altantic. Retrieved from https://www.theatlantic.com/politics/archive/2016/08/the-rise-of-the-others/497690/
- Berwick DM, Murphy JM, Goldman PA, Ware JE, Barsky AJ, & Weinstein MC (1991). Performance of a five-item mental health screening test. Medical Care, 29, 169–176. [DOI] [PubMed] [Google Scholar]
- Boardman JD (2006). Self-rated health among U.S. adolescents. Journal of Adolescent Health, 38, 401–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Dickerson DL, & D’Amico EJ (2016). Cultural identity among urban American Indian/Alaska Native youth: Implications for alcohol and drug use. Prevention Science, 17, 852–861. 10.1007/s11121-016-0680-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt LW (1986). Roots of the Native American urban experience: Relocation policy in the 1950s. American Indian Quarterly, 10, 85–99. 10.2307/1183982 [DOI] [Google Scholar]
- Castor ML, Smyser MS, Taualii MM, Park AN, Lawson SA, & Forquera RA (2006). A nationwide population-based study identifying health disparities between American Indians/Alaska Natives and the general populations living in select urban counties. American Journal of Public Health, 96, 1478–1484. 10.2105/ajph.2004.053942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn DV (2015). American Indian and White, but not “multiracial.” Retrieved from http://www.pewresearch.org/fact-tank/2015/06/11/american-indian-and-white-but-not-multiracial/
- D’Amico EJ, Dickerson DL, Brown RA, Klein DJ, Agniel D, & Johnson C (2019). Unveiling an “invisible population”: Health, substance use, sexual behavior, culture, and discrimination among urban American Indian/Alaska Native adolescents in California. Ethnicity and Health. 10.1080/13557858.2018.1562054 [DOI] [PMC free article] [PubMed]
- D’Amico EJ, Tucker JS, Miles JNV, Ewing BA, Shih RA, & Pedersen ER (2016). Alcohol and marijuana use trajectories in a diverse longitudinal sample of adolescents: Examining use patterns from age 11 to 17 years. Addiction, 111, 1825–1835. 10.1111/add.13442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeFina R, & Hannon L (2016). Social status attainment and racial category selection in the contemporary United States. Research in Social Stratification and Mobility, 44(Suppl. C), 91–97. 10.1016/j.rssm.2016.02.006 [DOI] [Google Scholar]
- Dickerson DL, Annon JJ, Hale B, & Funmaker G (2014). Drum-assisted recovery therapy for Native Americans (DARTNA): Results from a pretest and focus groups. Journal of American Indian and Alaska Native Mental Health Research, 21(1), 35–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, Baldwin JA, Belcourt A, Belone L, Gittlsohn J, … Wallerstein N (2018). Encompassing cultural contexts within scientific research methodologies in the development of health promotion interventions, Prevention Science, 10.1007/s11121-018-0926-1 [DOI] [PMC free article] [PubMed]
- Dickerson DL, Brown RA, Johnson CL, Schweigman KD, & D’Amico EJ (2016). Integrating motivational interviewing and traditional practices to address alcohol and drug use among urban American Indian/Alaska Native youth. Journal of Substance Abuse Treatment, 65, 26–35. 10.1016/j.jsat.2015.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, Fisher DG, Reynolds GL, Baig S, Napper LE, & Anglin MD (2012). Substance use patterns among high-risk American Indians/Alaska Natives in Los Angeles County. The American Journal on Addictions, 21, 445–452. 10.1111/j.1521-0391.2012.00258.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, Poulin F, & Burraston B (2001). Peer group dynamics associated with iatrogenic effect in group interventions with high-risk young adolescents. New Directions for Child and Adolescent Development, 2001(91), 79–92. 10.1002/cd.6 [DOI] [PubMed] [Google Scholar]
- Dockery AM (2010). Culture and wellbeing: The case of Indigenous Australians. Social Indicators Research, 99, 315–332. 10.1007/s11205-010-9582-y [DOI] [Google Scholar]
- Donovan DM, Thomas LR, Sigo RLW, Price L, Lonczak H, Lawrence N, … Bagley L (2015). Healing of the canoe: Preliminary results of a culturally grounded intervention to prevent substance abuse and promote tribal identity for Native youth in two pacific northwest tribes. American Indian and Alaska Native Mental Health Research, 22(1), 42–76. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4374439/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eschbach K (1995). The enduring and vanishing American Indian: American Indian population growth and intermarriage in 1990. Ethnic and Racial Studies, 18, 89–108. 10.1080/01419870.1995.9993855 [DOI] [Google Scholar]
- Evans-Campbell T (2008). Historical trauma in American Indian/Native Alaska communities: A multilevel framework for exploring impacts on individuals, families, and communities. Journal of Interpersonal Violence, 23, 316–338. 10.1177/0886260507312290 [DOI] [PubMed] [Google Scholar]
- Fleming J, & Ledogar RJ (2008). Resilience and indigenous spirituality: A literature review. Pimatisiwin, 6(2), 47–64. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2956755/ [PMC free article] [PubMed] [Google Scholar]
- Grossman DC, Krieger JW, Sugarman JR, & Forquera RA (1994). Health status of urban American Indians and Alaska natives: A population-based study. Journal of the American Medical Association, 271, 845–850. 10.1001/jama.1994.03510350055037 [DOI] [PubMed] [Google Scholar]
- Hartmann WE, Wendt DC, Saftner MA, Marcus J, & Momper SL (2014). Advancing community-based research with urban American Indian populations: Multidisciplinary perspectives. American Journal of Community Psychology, 54, 72–80. 10.1007/s10464-014-9643-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heart MYHB (2003). The historical trauma response among Natives and its relationship with substance abuse: A Lakota illustration. Journal of Psychoactive Drugs, 35(1), 7–13. 10.1080/02791072.2003.10399988 [DOI] [PubMed] [Google Scholar]
- House L, Stiffman A, & Brown E (2006). Unraveling cultural threads: A qualitative study of culture and ethnic identity among urban southwestern American Indian youth parents and elders. Journal of Child and Family Studies, 15, 393–407. 10.1007/s10826-006-9038-9 [DOI] [Google Scholar]
- Hughes M, Kiecolt KJ, Keith VM, & Demo DH (2015). Racial identity and well-being among African Americans. Social Psychology Quarterly, 78(1), 25–48. 10.1177/0190272514554043 [DOI] [Google Scholar]
- Hunter SB, Miles JNV, Pedersen ER, Ewing BA, & D’Amico EJ (2014). Temporal associations between substance use and delinquency among youth with a first time offense. Addictive Behaviors, 39, 1081–1086. 10.1016/j.addbeh.2014.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James MA (1992). The state of native America: Genocide, colonization, and resistance. Cambridge, MA: South End Press. [Google Scholar]
- Kaufman CE, Black K, Keane EM, Big Crow CK, Shangreau C, Arthur-Asmah R, … Tuitt N (2014). Planning for a group-randomized trial with American Indian youth. Journal of Adolescent Health Care, 54(3), S59–S63. 10.1016/j.jadohealth.2013.12.028 [DOI] [PubMed] [Google Scholar]
- Kelly MJ, Dunstan FD, Lloyd K, & Fone DL (2008). Evaluating cutpoints for the MHI-5 and MCS using the GHQ-12: A comparison of five different methods. BMC Psychiatry, 8(1), 10.1186/1471-244x-8-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulis S, Hodge D, Ayers SL, Brown EF, & Marsiglia FF (2011). Spirituality and religion: Intertwined protective factors for substance use among urban American Indian youth. The American Journal of Drug and Alcohol Abuse, 38, 444–449. 10.3109/00952990.2012.670338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulis S, Wagaman MA, Tso C, & Brown EF (2013). Exploring indigenous identities of urban American Indian youth of the southwest. Journal of Adolescent Research, 28, 271–298. 10.1177/0743558413477195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaFromboise TD, Hoyt DR, Oliver L, & Whitbeck LB (2006). Family, community, and school influences on resilience among American Indian adolescents in the upper midwest. Journal of Community Psychology, 34, 193–209. 10.1002/jcop.20090 [DOI] [Google Scholar]
- Lane DC, & Simmons J (2011). American Indian youth substance abuse: Community-driven interventions. Mount Sinai Journal of Medicine, 78, 362–372. Retrieved from https://onlinelibrary.wiley.com/doi/abs/10.1002/msj.20262 [DOI] [PubMed] [Google Scholar]
- Lee B, Martin M, Matthews S, & Farrell C (2017). State-level changes in US racial and ethnic diversity, 1980 to 2015: A universal trend? Demographic Research, 37, 1031–1048. Retrieved from https://www.demographic-research.org/volumes/vol37/33/default.htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J, & Bean FD (2010). The diversity paradox: Immigration and the color line in twenty-first century America. New York, NY: Russell Sage Foundation. [Google Scholar]
- Liebler CA, Porter SR, Fernandez LE, Noon JM, & Ennis SR (2017). America’s churning races: Race and ethnicity response changes between census 2000 and the 2010 census. Demography, 54, 259–284. 10.1007/s13524-016-0544-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucero NM (2010). Making meaning of urban American Indian identity: A multistage integrative process. Social Work, 55, 327–336. 10.1093/sw/55.4.327 [DOI] [PubMed] [Google Scholar]
- McGee DL, Liao Y, Cao G, & Cooper RS (1999). Self-reported health status and mortality in a multiethnic US cohort. American Journal of Epidemiology, 149(1), 41–46. 10.1093/oxfordjournals.aje.a009725 [DOI] [PubMed] [Google Scholar]
- Miech RA, Johnston LD, O’Malley PM, Bachman JG, & Schulenberg JE (2016). Monitoring the future national survey results on drug use, 1975–2015: Volume I, secondary school students. Ann Arbor: Institute for Social Research, The University of Michigan. Retrieved from http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2015.pdf [Google Scholar]
- Minkler M, & Wallerstein N (2011). Community-based participatory research for health: From process to outcomes. Hoboken, NJ: John Wiley. [Google Scholar]
- Norris T, Vines PL, & Hoeffel EM (2012). The American Indian and Alaska Native population: 2010 census briefs. Retrieved from http://www.Census.Gov/prod/cen2010/briefs/c2010br-10.pdf
- Pavkov TW, Travis L, Fox KA, King CB, & Cross TL (2010). Tribal youth victimization and delinquency: Analysis of youth risk behavior surveillance survey data. Cultural Diversity and Ethnic Minority Psychology, 16, 123–134. [DOI] [PubMed] [Google Scholar]
- Peterman AH, Fitchett G, Brady MJ, Hernandez L, & Cella D (2002). Measuring spiritual well-being in people with cancer: The functional assessment of chronic illness therapy—Spiritual well-being scale (FACIT-SP). Annals of Behavioral Medicine, 24, 49–58. 10.1207/s15324796abm2401_06 [DOI] [PubMed] [Google Scholar]
- Pfefferle SG, & Spitznagel EL (2009). Children’s mental health service use and maternal mental health: A path analytic model. Children and Youth Services Review, 31, 378–382. 10.1016/j.childyouth.2008.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phinney JS, & Ong AD (2007). Conceptualization and measurement of ethnic identity: Current status and future directions. Journal of Counseling Psychology, 54, 271–281. Retrieved from https://pdfs.semanticscholar.org/1eef/2ee284255e20b7d1e2301c94cd0499690c01.pdf [Google Scholar]
- Plunkett M, & Mitchell CM (2000). Substance use rates among American Indian adolescents: Regional comparisons with monitoring the future high school seniors. Journal of Drug Issues, 30, 575–591. 10.1177/002204260003000305 [DOI] [Google Scholar]
- Ponterotto JG, Gretchen D, Utsey SO, Stracuzzi T, & Saya R (2003). The multigroup ethnic identity measure (MEIM): Psychometric review and further validity testing. Educational and Psychological Measurement, 63, 502–515. 10.1177/0013164403063003010 [DOI] [Google Scholar]
- Qian Z, & Lichter DT (2011). Changing patterns of interracial marriage in a multiracial society. Journal of Marriage and Family, 73, 1065–1084. 10.1111/j.1741-3737.2011.00866.x [DOI] [Google Scholar]
- Quintana SM (2007). Racial and ethnic identity: Developmental perspectives and research. Journal of Counseling Psychology, 54, 259–270. 10.1037/0022-0167.54.3.259 [DOI] [Google Scholar]
- Renn KA (2008). Research on biracial and multiracial identity development: Overview and synthesis. New Directions for Student Services, 2008(123), 13–21. 10.1002/ss.282 [DOI] [Google Scholar]
- Rivas-Drake D, Seaton EK, Markstrom C, Quintana S, Syed M, Lee RM, … Yip T (2014). Ethnic and racial identity in adolescence: Implications for psychosocial, academic, and health outcomes. Child Development, 85(1), 40–57. 10.1111/cdev.12200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz AS (1990). Ethnic identity: Crisis and resolution. Journal of Multicultural Counseling and Development, 18(1), 29–40. 10.1002/j.2161-1912.1990.tb00434.x [DOI] [Google Scholar]
- Shepherd SM, Delgado RH, Sherwood J, & Paradies Y (2017). The impact of Indigenous cultural identity and cultural engagement on violent offending. BMC Public Health, 18(1), 10.1186/s12889-017-4603-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith TB, & Silva L (2011). Ethnic identity and personal well-being of people of color: A meta-analysis. Journal of Counseling Psychology, 58(1), 42–60. 10.1037/a0021528 [DOI] [PubMed] [Google Scholar]
- Stanley LR, Harness SD, Swaim RC, & Beauvais F (2014). Rates of substance use of American Indian students in 8th, 10th, and 12th grades living on or near reservations: Update, 2009–2012. Public Health Reports, 129, 156–163. 10.1177/003335491412900209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart AL, Ware JE, Sherbourne CD, & Wells KB (1992). Psychological distress/well-being and cognitive functioning measures. In Stewart A & Ware JE (Eds.), Measuring functioning and well-being: The medical outcomes study approach (pp. 102–142). Durham, NC: Duke University Press. [Google Scholar]
- Stone RAT, Whitbeck LB, Chen X, Johnson K, & Olson DM (2006). Traditional practices, traditional spirituality, and alcohol cessation among American Indians. Journal of Studies on Alcohol, 67, 236–244. 10.15288/jsa.2006.67.236 [DOI] [PubMed] [Google Scholar]
- Stumblingbear-Riddle G, & Romans JSC (2012). Resilience among urban American Indian adolescents: Exploration into the role of culture, self-esteem, subjective well-being, and social support. American Indian Alaska Native Mental Health Research, 19(2), 1–19. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2014). Results from the 2013 National Survey on Drug Use and Health: Summary of national findings. Rockville, MD: Author. Retrieved from https://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf [PubMed] [Google Scholar]
- Szlemko WJ, Wood JW, & Thurman PJ (2006). Native Americans and alcohol: Past, present, and future. The Journal of General Psychology, 133, 435–451. 10.3200/GENP.133.4.435-451 [DOI] [PubMed] [Google Scholar]
- Tucker JS, Orlando M, & Ellickson PL (2003). Patterns and correlates of binge drinking trajectories from early adolescence to young adulthood. Health Psychology, 22, 79–87. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/12558205 [DOI] [PubMed] [Google Scholar]
- Walters KL (1999). Urban American Indian identity attitudes and acculturation styles. Journal of Human Behavior in the Social Environment, 2, 163–178. 10.1300/J137v02n01_11 [DOI] [Google Scholar]
- Ware JE, Kosinski M, & Keller SD (1996). A 12-item short form health survey: Construction of scales and preliminary tests. Medical Care, 34, 220–233. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/8628042 [DOI] [PubMed] [Google Scholar]
- Whitbeck LB (2011). The beginnings of mental health disparities: Emergent mental disorders among indigenous adolescents. In Carlo G, Crockett LJ & Carranza MA (Eds.), Health disparities in youth and families (pp. 121–149). New York, NY: Springer. [DOI] [PubMed] [Google Scholar]
- Whitbeck LB, Adams GW, Hoyt DR, & Chen X (2004). Conceptualizing and measuring historical trauma among American Indian people. American Journal of Community Psychology, 33, 119–130. 10.1023/B:AJCP.0000027000.77357.31 [DOI] [PubMed] [Google Scholar]
- Whitesell NR, Beals J, Crow CB, Mitchell CM, & Novins DK (2012). Epidemiology and etiology of substance use among American Indians and Alaska Natives: Risk, protection, and implications for prevention. The American Journal of Drug and Alcohol Abuse, 38, 376–382. 10.3109/00952990.2012.694527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willmon-Haque S, & BigFoot SD (2008). Violence and the effects of trauma on American Indian and Alaska Native populations. Journal of Emotional Abuse, 8(1–2), 51–66. 10.1080/10926790801982410 [DOI] [Google Scholar]