Abstract
Cardiovascular diseases (CVD) comprise the leading cause of mortality worldwide, accounting for 3 in 10 deaths. Individuals with certain risk factors, including tobacco use, obesity, low levels of physical activity, type 2 diabetes mellitus, racial/ethnic minority status and low socioeconomic status, experience higher rates of CVD and are, therefore, considered priority populations. Technological devices such as computers and smartphones are now routinely utilized in research studies aiming to prevent CVD and its risk factors, and they are also rampant in the public and private health sectors. Traditional health behavior interventions targeting these risk factors have been adapted for technology-based approaches. This review provides an overview of technology-based interventions conducted in these priority populations as well as the challenges and gaps to be addressed in future research. Researchers currently possess tremendous opportunities to engage in technology-based implementation and dissemination science to help spread evidence-based programs focusing on CVD risk factors in these and other priority populations.
Keywords: Cardiovascular disease, Technology-based interventions, Vulnerable populations, Risk factors, Health behaviors
Cardiovascular diseases (CVD) comprise the leading cause of mortality worldwide, accounting for approximately 17.5 million deaths in 2012, including 7.4 million from ischemic heart disease and 6.7 million from stroke.1 These statistics translate to 3 in every 10 deaths.1 Compared to low- and middle-income countries, high-income countries are burdened by a higher percentage of deaths from CVD and other non-communicable diseases, largely due to the longer lifespan and lower prevalence of communicable diseases in these countries.1
Technological devices, such as computers and smartphones, are now routinely utilized in research studies aimed at preventing CVD and its risk factors.2 Although these devices are becoming increasingly available in low- and middle-income countries, few studies using technology to prevent CVD have been conducted in these less affluent areas.3 Therefore, this review will focus on research conducted in high-income countries.
Within high-income countries, certain segments of the population face relatively higher CVD risk and are thus considered to be “priority populations.” In particular, individuals with the following risk factors (Fig 1) experience higher rates of CVD: tobacco use, obesity, low levels of physical activity (PA), type 2 diabetes mellitus (T2DM), racial/ethnic minority status, and low socioeconomic status (SES). Technology-based health behavior interventions are adaptable and often tailored to match the needs and characteristics of these specific populations (Fig 2). For example, a health behavior intervention based on the social cognitive theory might focus on smoking cessation for tobacco users, healthy eating habits and PA promotion for individuals with T2DM, and all three of these health behaviors for racial/ethnic minorities with high rates of these behaviors.
Fig 1 –
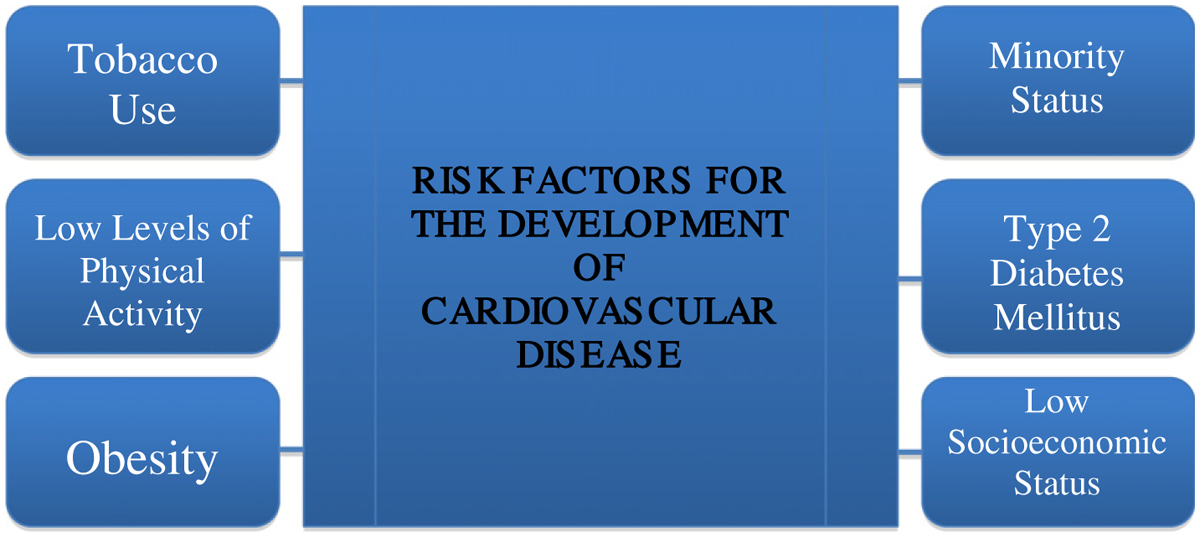
Populations at high-risk for cardiovascular disease.
Fig 2 –
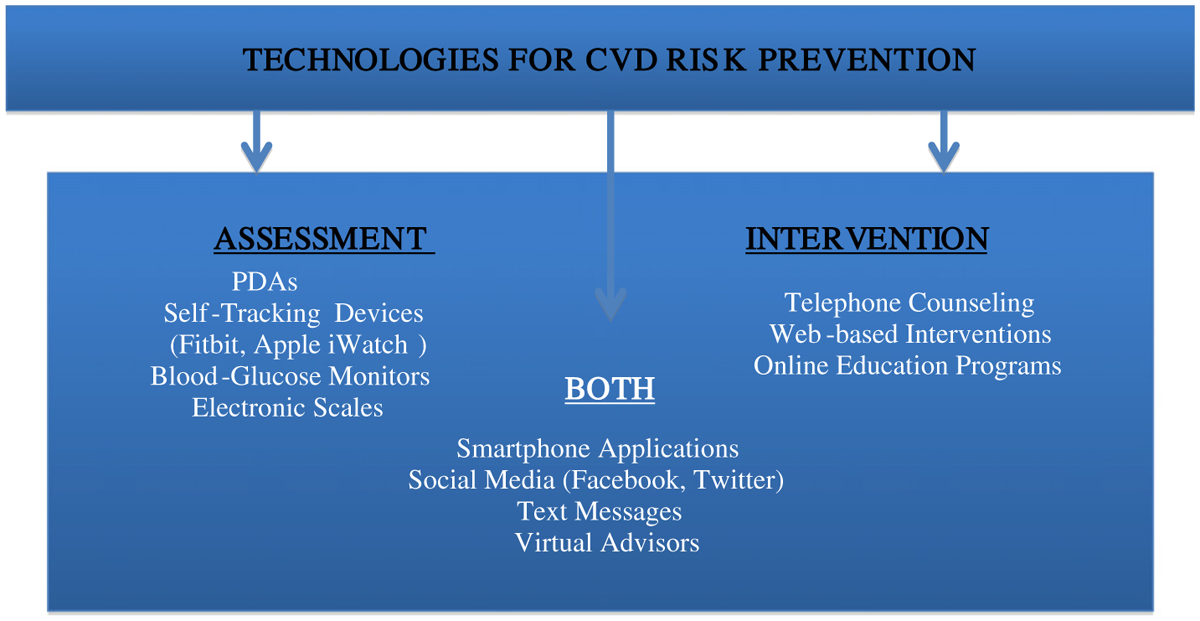
Technologies utilized for assessment and intervention within populations at high-risk of cardiovascular disease.
Technology-based health behavior tools are appealing for many reasons, including their adaptability, expansive reach, cost-effectiveness, objective data collection capacity, and facilitation of real-time data collection and feedback (i.e., ecological momentary assessment and intervention). The following sections describe some of the adaptations that have been made to technology-based CVD prevention interventions to meet the needs of these priority populations as well as the outcomes extracted from these studies. It attempts to summarize best practices thus far and identify important gaps that remain for future research studies to explore or resolve.
Tobacco Use
Tobacco use has been the leading cause of CVD and preventable premature death for the past four decades and has therefore been the target of health behavior change interventions more than any other single behavior.4 Technology-based smoking cessation interventions have been tested in numerous randomized controlled trials and have also become mainstream in the government, public and private sectors.
Telephone counseling for smoking cessation (referred to as Quitlines) marked the first major use of technology to help smokers quit, and this method continues to be one of the most utilized and evidence-based approaches.5 Telephone counseling is currently delivered in multiple languages, and most Quitlines provide free access to additional cessation information and services, including telephone-based support and advice from an experienced cessation counselor, a personalized quit plan and self-help materials, social support and strategies to help them cope with cravings, cessation services and other resources offered near their residence, and/or access to the latest information about cessation medications.6 Quitlines have continued to thrive despite the development of more technologically advanced smoking cessation delivery methods, which raises the question of whether or not these newer methods provide incremental benefits.
Smoking cessation websites emerged with the increasing utilization of the Internet for health information and services.7 These websites contain facts/statistics about smoking and its health risks, questionnaires for smokers to complete to help them determine their stage of change, tips and tools to help smokers prepare to quit, strategies for them to use in the quitting process, and relapse prevention tools to help them remain tobacco free.
More recently, other technology-based approaches such as text messaging, smartphone applications (apps), and social media (e.g., Facebook) have expanded the reach and accessibility of smoking cessation interventions and support. For example, researchers and government-funded organizations have developed programs that enable smokers to reach out for real-time text-based support from smoking cessation counselors and/or other smokers trying to quit by texting keywords or codes.2
Countless smoking cessation apps with various features to help smokers quit, such as self-monitoring of cravings and numbers of cigarettes per day smoked, have been developed by research teams, government-funded organizations, and private companies alike.8 Other programs have been delivered via Facebook to reach smokers who prefer to engage with their existing social media platform in their quitting journey.9
Combining many of the aforementioned methods is the Tobacco Control Research Branch of the National Cancer Institute’s comprehensive (Smokefree.gov (http://smokefree.gov) program, which “provides free, accurate, evidence-based information and professional assistance to help support the immediate and long-term needs of people trying to quit smoking”.8 Smokefree.gov provides multiple options to help smokers quit according to their preferences, including an extensive website with cessation information and tools; live online instant messaging support; a mobile text messaging service with 24/7 encouragement, advice, and tips; two smartphone app options (for teens and adults) with tips, tools, goal-setting, and self-monitoring; and referrals to local or national quitlines. The Smokefree.gov website also provides information about healthy eating habits, exercise, and mood management to help smokers adopt an overall healthy lifestyle, which may help them quit and avoid relapses. Moreover, Smokefree.gov offers tailored versions of these programs for specific populations: women (including pregnant women), veterans, teens, and Spanish-speaking smokers.8
This review only touches on the extensive work of technology-based interventions for smoking cessation. Although it is the most developed area of behavior change interventions for CVD prevention, it still has many gaps that need to be filled. For example, helping smokers to navigate their environmental surroundings and social situations to make smoking the more difficult behavior to engage in would constitute novel uses of behavioral economics.
Furthermore, although the overall smoking prevalence rate has declined significantly in the past few decades, certain segments of the population continue to face higher rates of tobacco use and more difficulty quitting. In particular, individuals with certain racial/ethnic backgrounds (e.g., African Americans), mental health disorders, fewer years of education, and lower SES are more likely to smoke and less likely to successfully quit.3 Therefore, technology-based smoking cessation interventions should be designed or tailored to reach these and other underserved and vulnerable populations, who have apparently not responded as successfully to traditional cessation approaches and may benefit from these alternative approaches. More research is needed to determine whether or not technology-based approaches would be more helpful.10
Insufficient PA
Less than 50% of adults in the US meet public health guidelines for recommended levels of PA.11 In effect, insufficient PA rivals and is expected to soon surpass smoking as the most important CVD risk factor.12–16 Technology-based assessments and interventions for PA have proliferated since the dawn of technologies such as pedometers for PA self-monitoring17 and telephone counseling for PA motivation enhancement.18
Technology-based assessments have enabled more objective and accurate tracking of PA behaviors than traditional self-report measures.19 These devices are constantly evolving as the engineering within them becomes increasingly accurate and reliable. Accelerometers are still considered the gold standard in PA assessment but are utilized almost exclusively by PA researchers since the data they collect are complicated to extract and interpret.20 In the public domain, traditional pedometers are being quickly replaced by wireless self-tracking devices such as the Fitbit, Jawbone UP, Garmin vivo, Apple iWatch, and Nike Fuelband, among numerous others, and the latest smartphones incorporate accelerometers and GPS tracking to track users’ PA behaviors and encourage them to carry or essentially wear their phones.21,22
Self-tracking devices are thriving in a society full of individuals increasingly interested in these wearable technologies that enable them to better understand and take control of their own health.23 A Pew Internet Research Survey conducted in August through September 2012 via telephone found that 21% of respondents reported using some form of technology to track their health data.24 This number has undoubtedly grown substantially in the past few years. The latest versions of these devices incorporate social connectivity and social media features that encourage users to challenge their friends with the same devices to achieve certain goals and benchmarks, compete with each other, and share their goals and accomplishments on social media platforms. Many of these built-in features are rooted in classic social psychology strategies known to improve effort and performance in exercise and sports (e.g., social facilitation).25 These wireless tracking devices have been increasingly incorporated into PA research as evidence supporting their validity and reliability has increased.22,26–28
Technology-based PA interventions have incorporated strategies to address the most commonly stated barriers to engaging in leisure time PA, including a perceived lack of time, motivation, social support, knowledge, and convenient places to be active, among others.29 Modeled after traditional evidence-based PA interventions, technology-based interventions strive to incorporate multiple behavioral adherence strategies such as self-monitoring, social support, and goal-setting.28 Telephone counseling sessions with health coaches or nurses are still utilized in research and clinical settings.18 However, more modern delivery channels such as websites, automated text messaging systems, mobile applications, and social media platforms (e.g., Facebook, Twitter) have essentially dominated the public and private sector PA promotion market and become increasingly commonplace in research settings.30 One recently completed study was designed based on behavioral theory and integrated intervention elements across multiple technology-based touch points, including Facebook, text messaging, smartphone apps, blogs, and e-mail in order to give participants the option of utilizing one or more devices according to their personal preferences.31
Since accumulating multiple, shorter bouts of PA improves health as much as engaging in sustained bouts of PA and may be more convenient and feasible for individuals who are short on leisure time, encouraging individuals to break-up their sedentary time with short bouts of PA have gained popularity.32,33 Notifications, such as buzzers or vibrations, reminding users to break up long periods of sedentary time by standing up and/or going for short walks are built-in features on many wearable devices and can be easily programmed in to computers or smartphones (e.g., using a simple clock or timer feature).
Encouraging individuals to focus on the immediate rewards of PA (e.g., energy boost, enjoyment, mood/affect improvement) rather than on the delayed, long-term effects (e.g., decreased risk of CVD, longer lifespan) may help increase their motivation for daily PA.34 Technology-based approaches naturally capitalize on this approach, as they are equipped to provide immediate feedback and positive reinforcement upon meeting PA goals and benchmarks.
Individuals with certain demographic characteristics, including female sex, minority race/ethnicity, low educational attainment, and low SES, are more likely to report insufficient PA and also suffer from higher rates of CVD; therefore, PA interventions have and should continue to focus on meeting the unique needs of these high-risk populations.35 Recent data suggest that an equally high percentage (approximately 90% as of April 2015)36 of high-risk individuals own a cellular phone as those from lower-risk groups, so reaching them via phone or text is feasible. Decreasing sedentary behavior in addition to increasing PA is another area of rapidly growing interest and apparent importance in the activity-related CVD prevention literature.37–39
Obesity
Obesity is one of the leading risk factors for CVD, and traditional behavior weight management is intensive and expensive.1 Although other variables factor in to the weight management equation, obesity treatment programs typically focus primarily on diet and exercise because they exert the most influence on weight and are modifiable behaviors.40 Some programs emphasize one of these behaviors over the other. For example, diet is often emphasized during the weight loss phase, whereas exercise is emphasized in the weight maintenance phase of weight loss/maintenance programs.40
Over the last 10 years, technology-based interventions, which can increase accessibility and reach while promoting evidence-based weight loss strategies at lower cost, have proliferated in the treatment of overweight and obesity.41–48 A variety of technological components have been included in weight loss interventions. Interactive computer or web-based weight loss interventions are most common,42,48 but mobile technologies such as phones for text messaging and smartphone applications have more recently gained popularity.43,45 Other technological devices tested have included a personal digital assistant (PDA), wireless and electronic weighing scales, and virtual groups.41,44,45
Technology-based interventions for obesity treatment have seamlessly incorporated behavioral change strategies. For example, websites, automated “health coaching” text messaging systems, mobile applications, and wireless weighing scales facilitate self-monitoring. Individuals using a self-monitoring app are more likely to consistently enter complete days of dietary data than individuals using pencil and paper approaches.49 PDAs have similarly shown better adherence to self-monitoring of food intake and physical activity than paper diaries.50,51 Self-weighing using Wi-Fi scales and graphic email feedback has been associated with frequent self-monitoring and weight loss.52
Computer-tailored feedback is another feature that allows for more individualization of counseling delivered in real-time through text or email messages.53,54 Receiving tailored versus non-tailored messages has led to greater weight loss.54 In addition to or in lieu of a counselor, technology-based interventions have tested the provision of social support through online communities. For example, among individuals randomized to a mobile media intervention, engagement in a social network such as Twitter was related to weight loss.55 In another study, using Facebook resulted in weight loss but only among those who also received text messages and personalized feedback and identified a support person, suggesting that delivering weight loss content alone via social networking sites may not be sufficient to drive changes in behavior.56
In general, technology-based interventions have led to greater weight loss than minimal intervention but have produced less weight loss than in-person treatment.42,48 However, as with in-person treatment, greater use of the program is associated with better weight loss results.47,53 Hence, finding innovative ways to increase and sustain adherence and motivation through technology may be key to keeping individuals engaged in treatment.
Currently, most studies on technology-based intervention on obesity have focused on weight loss, but interest in their use in long-term weight loss maintenance is growing.46 Employing technology-based approaches holds particular promise for weight loss maintenance when in-person intervention contact is minimal to none. For example, weight loss is more likely to be sustained in interventions with a technology component compared with minimal or no personal contact during the maintenance or follow-up phase.57,58 More studies are needed to determine the effectiveness of technology-based tools in preventing weight regain.
Type 2 Diabetes Mellitus
Certainly T2DM has been identified as a major risk factor for CVD, to the extent that T2DM status is included as a factor in the Framingham Risk Score as well as the Pooled Cohort Equation.59 Individuals with impaired glucose tolerance or T2DM levels of fasting glucose have more than double the risk of CVD mortality as individuals with normal glucose tolerance.60 Patients with T2DM, therefore, should be considered a population of particularly high priority to target in order to prevent CVD.
One of the most important self-management behaviors for T2DM is monitoring blood glucose. This behavior in particular has important clinical utility; a meta-analysis showed that simply tracking glucose significantly improves long-term glycated hemoglobin (HbA1c).61 This is a behavior especially amenable to technological approaches; accordingly, a large array of literature has emerged exploring the feasibility and effectiveness of different technological approaches to glucose monitoring and sharing glucose levels with health care providers.
One review examined the effectiveness of telemedicine approaches to glucose monitoring, including studies in which technology (web or texting) was used both to share glucose levels with providers and to give patients feedback on their data.
Across studies, T2DM participants who monitored their glucose and shared it via the web or text with their providers had significantly greater reductions in HbA1c than controls receiving usual care.62 One study showed that more data uploads were associated with greater improvements in HbA1c, suggesting a dose response.63 A recent meta-analysis specifically examined smartphone apps for managing T2DM, and, overall, found a meaningful reduction in HbA1c (−0.8%) in T2DM patients using apps.64
While there is some evidence that telemedicine approaches to glucose monitoring reduce cost and burden for patients, it can increase burden for providers, who may not be compensated for the time they spend reviewing uploaded glucose logs. One possible solution is the use of computerized software that is programmed to review logs and generate automated responses. A cluster randomized trial of 26 primary care practices assessed the efficacy of using the WellDoc System, which provided patients with a Bluetooth-enabled glucose monitor that transmitted data to a smartphone software program.65 The software program in turn gives automated feedback on how to correct glucose levels outside the normal range, asks questions about medication, diet, and other influential factors, and generates a quarterly treatment plan. Treatment plans were also sent to health care providers to review. Intervention participants showed greater reductions in A1c than controls after one year. A smaller trial of the software also showed that participants using the software were more likely to have medication errors identified, and found that providers were satisfied with the program and found it saved time compared to reviewing traditional logbooks.66
The use of technology thus appears very promising in T2DM management, though there are of course questions and complications that remain. As with all technological interventions, the success of the approach depends on the comfort and knowledge base of the population using it. Most T2DM cases are typically diagnosed between ages 45 and 65 years,67 a demographic that is showing increased use of technology (particularly smartphones) but which may not be as tech savvy as a younger generation. Additionally, in regards to which technological innovations may benefit providers by supplying more information, it remains unclear how providers should be expected to view and process this information given their busy schedules and reimbursement systems. The available data, however, suggests that telemedicine approaches to T2DM management could improve clinical outcomes for patients, thus the use of telemedicine will likely increase and should be considered and incorporated into health care plans and standard treatment approaches.
Racial/Ethnic Minority Status
Compared to non-Hispanic whites, prevalence rates of CVD risk factors, such as overweight/obesity, physical inactivity, and poor nutrition, are higher among non-Hispanic Blacks, Latinos, and other racial and ethnic minority groups.68–75 Therefore, racial and ethnic minorities are considered priority populations for interventions promoting behaviors associated with CVD prevention, including weight management, PA, and nutrition.
Technology has long been used to engage hard to reach populations by utilizing different communication channels (e.g., television and radio) for health promotion. For example, Risica and colleagues76 conducted a cable TV-based weight control study (SisterTalk) for black women. In order to design an appropriately tailored approach, they conducted extensive formative research and developed community partnerships for program implementation.77 The study found initial program effectiveness, although only dietary changes were sustained.76
Newer technologies provide engaging platforms for health promotion research in minority racial and ethnic populations, enabling program delivery through text messaging, websites, and social media. Text messaging has been successfully used to promote PA and weight management among non-Hispanic blacks,78,79 although little information regarding the cultural adaptation of such messages has been provided.
A recent intervention to promote PA within a small sample of non-Hispanic black women combined the use of Facebook and text messaging.80 The cultural tailoring of this intervention was based on the research team’s previous experiences conducting research among non-Hispanic black women as well as literature related to PA determinants specific to this population and tailoring for minority populations. Tailoring included emphasizing the prevalence of physical inactivity and related morbidity among non-Hispanic blacks, discussing social norms and barriers specific to this population, and using visual materials (e.g., photographs, images) that matched the population’s characteristics. Despite the small sample size (N=29), the study found significant differences between the intervention and control group in objectively measured sedentary time and increased light and moderate intensity lifestyle PA.80
Technology also offers the opportunity of tailoring intervention content, and various studies have taken advantage of this feature. For example, the Seamos Saludables study used a computer expert system to tailor PA messages for Latinas.81 This intervention was adapted for Latinas through a series of focus groups and cognitive interviews.82 The study found a significantly greater increase in minutes/week of moderate to vigorous PA in the intervention versus control group.83 The knowledge acquired through this formative research was used to develop a web-based physical activity intervention for Latinas (Muevete Alabama), which allows participants to set goals and track their PA.84 Steinberg recently used interactive voice response technology to facilitate self-monitoring in a study for weight loss among Black women, which resulted in high adherence and greater weight loss.85
The use of novel technologies in interventions to promote CVD prevention behaviors among racial and ethnic minorities is still sparse, but it is growing rapidly. While many of the studies discussed in this review are pilot studies and thus underpowered, their preliminary results are promising. Further research with larger samples and enough power to detect changes is necessary. Additionally, although using a variety of technological devices and tools used to promote CVD preventive behaviors among Latinos and non-Hispanic blacks is encouraging, research should also explore the application of technology to promote CVD preventive behaviors among other at-risk racial and ethnic minorities.
Socioeconomic Status
Low SES has consistently been associated with a high prevalence of CVD risk factors, including smoking, physical inactivity, and poor nutrition.71,86,87 Nevertheless, a paucity of research on the adaptation of technology-based interventions for CVD preventive behaviors among groups with low SES exists. While older technologies, such as the telephone, have been used in interventions to promote CVD preventive behaviors among low SES populations,88–90 few studies have used text messaging, social media, and other newer technologies for such purposes. Moreover, when they are conducted, the process taken to tailor the materials for low SES populations is rarely described.
Nevertheless, a few studies have explored the use of websites for health education among low SES populations. Neuenschwander and colleagues91 found that a web-delivered nutrition education program for individuals with low income was as effective as an in-person program, with the added benefits of ease of dissemination and reduced costs. The researchers conducted two stages of cognitive interviews to ensure comprehension and ease of use within a sample of low-income adults.91 A more recent study also used a website to deliver nutritional information to low-income women.92 The program was initially designed for a college population and then adapted for low-income women through a process including cognitive interviews and surveys. The intervention resulted in increased use of food management skills, such as budgeting and meal planning.92
According to national data, 92% of adults in the US in 2015 reported owning a cellphone. The use of cellphones is widespread among most demographic groups, including individuals with low SES. For example, 86% of individuals who had less than high school education and 86% of individuals with household income of less than $30,000 owned a cellphone in 2015.36 In recognition of the high prevalence of cellphone ownership among people with low SES, Vidrine and colleagues adapted and enhanced a standard care smoking cessation intervention by adding text-based components and counseling phone calls.93 One of the most innovative strategies used in studies promoting CVD preventive behaviors among individuals with low SES is the use of virtual advisors to promote walking, such as in the Compass study.94 Initial research stages included twelve months of formative participatory research to design an appropriate model for mostly Latino older adults with low income and low literacy levels. The study found significantly different increases in minutes per week of walking between the intervention and control groups. Additionally, participants remained engaged with the program even after the study ended.94
Overall, research related to the adaptation and application of technology-based interventions to promote CVD preventive behaviors among individuals with low SES is scarce. Nevertheless, the success of existing studies is encouraging and suggests the need for more research in the area. Formative research, including cognitive interviews and participatory research, emerged as a common strategy used to adapt programs for low SES populations and should continue to be used in future research endeavors in this important area.
Summary
In sum, technology-based health behavior interventions have been adapted to address the CVD risk factors most relevant to the high-risk and vulnerable populations within high-income countries identified in this review. A major challenge with future research in this area will be keeping up with the constantly evolving technologies on the market so that results are not irrelevant by the time they are published.95 Confidentiality and privacy issues also constitute an area of growing interest and concern as these technologies often toe the privacy and confidentiality lines.96
The so-called technology divide has for the most part fallen within high-income countries, enabling equal access to technology-based interventions across individuals with all racial/ethnic backgrounds and SES. Researchers are primed for a unique time to engage in technology-based implementation and dissemination science to help spread evidence-based programs focusing on CVD risk factors in these and other priority populations.97 As these programs continue to develop and establish effectiveness, researchers will be tasked with determining whether they are more efficiently useful as replacements of other types of interventions or if they should be used to enhance existing interventions (e.g., face-to-face visits, in-person groups). Comparative effectiveness trials and cost-effectiveness analyses may be particularly useful methods of reaching those conclusions. Moreover, as the proportion of deaths due to CVD and other non-communicable diseases are increasing in low- and middle-income countries, researchers should focus on learning more about the acceptability and feasibility of technology-based health behavior interventions adapted for these populations.
Acknowledgement
The authors greatly appreciate the technical assistance of Britany Schnelby, B.A., who helped with the Figures and References.
Abbreviations and Acronyms
- CVD
Cardiovascular disease
- PA
Physical activity
- PDA
Personal digital assistant
- HbA1c
Glycated hemoglobin
- SES
Socioeconomic status
- T2DM
Type 2 diabetes mellitus
Footnotes
Statement of conflict of interest
There is no conflict of interest of any of the listed authors.
Disclosures: None
REFERENCES
- 1.World Health Organization. Fact Sheets: Cardiovascular Diseases (CVDs). 2015.
- 2.Whittaker R, McRobbie H, Bullen C, Borland R, Rodgers A, Gu Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev. 2012;11. [DOI] [PubMed] [Google Scholar]
- 3.Jamal A, Agaku IT, O’Connor E, King BA, Kenemer JB, Neff L. Current cigarette smoking among adults–United States, 2005–2013. MMWR Morb Mortal Wkly Rep. 2014;63(47):1108–1112. [PMC free article] [PubMed] [Google Scholar]
- 4.Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet. 2014;384:45–52. [DOI] [PubMed] [Google Scholar]
- 5.Stead LF, Hartmann-Boyce J, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2013;8. [DOI] [PubMed] [Google Scholar]
- 6.Center for Disease Control and Prevention. Telephone Quitlines: A Resource for Development, Implementation, and Evaluation. 2004. [http://www.cdc.gov/tobacco/quit_smoking/cessation/quitlines/pdfs/quitlines.pdf].
- 7.Fox S The Social Life of Health Information 2011. Washington, DC: Pew Internet & American Life Project. 2011. [Google Scholar]
- 8.United States Department of Health and Human Services, National Institutes of Health, National Cancer Institute, USA.gov. Smoke Free: Quit Guide. http://smokefree.gov/apps-quitguide.
- 9.Jacobs MA, Cobb CO, Abroms L, Graham AL. Facebook apps for smoking cessation: a review of content and adherence to evidence-based guidelines. J Med Internet Res. 2014;16(9):e205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen YF, Madan J, Welton N, et al. Effectiveness and cost-effectiveness of computer and other electronic aids for smoking cessation: a systematic review and network meta-analysis. Health Technol Assess. 2012;16(38):1–205. [DOI] [PubMed] [Google Scholar]
- 11.Tucker JM, Welk GJ, Beyler NK. Physical Activity in U.S. Adults: Compliance with the Physical Activity Guidelines for Americans. Am J Prev Med. 2011;40(4):454–461. [DOI] [PubMed] [Google Scholar]
- 12.Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arena R, Harrington RA, Despres JP. A message from modern-day healthcare to physical activity and fitness: welcome home! Prog Cardiovasc Dis. 2015;57(4):293–295. [DOI] [PubMed] [Google Scholar]
- 14.Myers J, McAuley P, Lavie CJ, Despres JP, Arena R, Kokkinos P. Physical activity and cardiorespiratory fitness as major markers of cardiovascular risk: their independent and interwoven importance to health status. Prog Cardiovasc Dis. 2015;57(4):306–314. [DOI] [PubMed] [Google Scholar]
- 15.DeFina LF, Haskell WL, Willis BL, et al. Physical activity versus cardiorespiratory fitness: two (partly) distinct components of cardiovascular health? Prog Cardiovasc Dis. 2015;57(4):324–329. [DOI] [PubMed] [Google Scholar]
- 16.Lopez-Jimenez F, Simha V, Thomas RJ, et al. A summary and critical assessment of the 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: filling the gaps. Mayo Clin Proc. 2014;89(9):1257–1278. [DOI] [PubMed] [Google Scholar]
- 17.Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: A systematic review. JAMA. 2007;298(19):2296–2304. [DOI] [PubMed] [Google Scholar]
- 18.Goode AD, Reeves MM, Eakin EG. Telephone-Delivered Interventions for Physical Activity and Dietary Behavior Change: An Updated Systematic Review. Am J Prev Med. 2012;42(1):81–88. [DOI] [PubMed] [Google Scholar]
- 19.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical Activity in the United States Measured by Accelerometer. Med Sci Sports Exerc. 2008;40:181–188. [DOI] [PubMed] [Google Scholar]
- 20.Westerterp K Assessment of physical activity: a critical appraisal. Eur J Appl Physiol. 2009;105(6):823–828. [DOI] [PubMed] [Google Scholar]
- 21.Bort-Roig J, Gilson ND, Puig-Ribera A, Contreras RS, Trost SG. Measuring and influencing physical activity with smartphone technology: a systematic review. Sports Med. 2014;44(5):671–686. [DOI] [PubMed] [Google Scholar]
- 22.Ferguson T, Rowlands AV, Olds T, Maher C. The validity of consumer-level, activity monitors in healthy adults worn in free-living conditions: a cross-sectional study. Int J Behav Nutr Phys Act. 2015;12(42):015–0201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Klasnja P, Pratt W. Healthcare in the pocket: Mapping the space of mobile-phone health interventions. J Biomed Inform. 2012;45(1):184–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fox S, Duggan M. Tracking for Life. Pew Research Center’s Internet & American Life Project. 2013. [http://www.pewinternet.org/2013/01/28/tracking-for-health/].
- 25.Weinberg RS, Gould D. Foundations of Sport and Exercise Psychology, 6E. Human Kinetics. 2014. [Google Scholar]
- 26.Dontje ML, de Groot M, Lengton RR, van der Schans CP, Krijnen WP. Measuring steps with the Fitbit activity tracker: an inter-device reliability study. J Med Eng Technol. 2015;39(5):286–290. [DOI] [PubMed] [Google Scholar]
- 27.Diaz KM, Krupka DJ, Chang MJ, et al. Fitbit®: An accurate and reliable device for wireless physical activity tracking. Int J Cardiol. 2015;185:138–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lyons EJ, Lewis ZH, Mayrsohn BG, Rowland JL. Behavior change techniques implemented in electronic lifestyle activity monitors: a systematic content analysis. J Med Internet Res. 2014;16(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sherwood NE, Jeffery RW. The behavioral determinants of exercise: Implications for physical activity interventions. Annu Rev Nutr. 2000;20(1):21–44. [DOI] [PubMed] [Google Scholar]
- 30.Stephens J, Allen J. Mobile Phone Interventions to Increase Physical Activity and Reduce Weight: A Systematic Review. J Cardiovasc Nurs. 2013;28(4):320–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patrick K, Marshall SJ, Davila EP, et al. Design and implementation of a randomized controlled social and mobile weight loss trial for young adults (project SMART). Contemp Clin Trials. 2014;37(1):10–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garber CE, Blissmer B, Deschenes MR, et al. Quantity and Quality of Exercise for Developing and Maintaining Cardiorespiratory, Musculoskeletal, and Neuromotor Fitness in Apparently Healthy Adults: Guidance for Prescribing Exercise. Med Sci Sports Exerc. 2011;43(7):1334–1359. [DOI] [PubMed] [Google Scholar]
- 33.Linke S, Gallo L, Norman G. Attrition and adherence rates of sustained vs. intermittent exercise interventions. Ann Behav Med. 2011;42:197–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Segar M, Eccles J, Richardson C. Rebranding exercise: closing the gap between values and behavior. Int J Behav Nutr Phys Act. 2011;8(1):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burton NW, Khan A, Brown WJ. How, where and with whom? Physical activity context preferences of three adult groups at risk of inactivity. Br J Sports Med. 2012;46(16):1125–1131. [DOI] [PubMed] [Google Scholar]
- 36.Anderson M Technology Device Ownership: 2015. Pew Research Center’s Internet & American Life Project. 2015. [http://www.pewinternet.org/data-trend/mobile/device-ownership/].
- 37.Hamilton MT, Healy GN, Dunstan DW, Zderic TW, Owen N. Too little exercise and too much sitting: Inactivity physiology and the need for new recommendations on sedentary behavior. Curr Cardio Risk Rep. 2008;2(4):292–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ford ES, Caspersen CJ. Sedentary behaviour and cardiovascular disease: a review of prospective studies. Int J Epidemiol. 2012;41(5):1338–1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carlson SA, Fulton JE, Pratt M, Yang Z, Adams EK. Inadequate physical activity and health care expenditures in the United States. Prog Cardiovasc Dis. 2015;57(4):315–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barlow SE, Dietz WH. Obesity Evaluation and Treatment: Expert Committee Recommendations. Pediatrics. 1998;102(3):e29–e29. [DOI] [PubMed] [Google Scholar]
- 41.Raaijmakers LC, Pouwels S, Berghuis KA, Nienhuijs SW. Technology-based interventions in the treatment of overweight and obesity: A systematic review. Appetite. 2015;95:138–151. [DOI] [PubMed] [Google Scholar]
- 42.Wieland LS, Falzon L, Sciamanna CN, et al. Interactive computer-based interventions for weight loss or weight maintenance in overweight or obese people. Cochrane Database Syst Rev. 2012;8:CD007675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aguilar-Martinez A, Sole-Sedeno JM, Mancebo-Moreno G, Medina FX, Carreras-Collado R, Saigi-Rubio F. Use of mobile phones as a tool for weight loss: a systematic review. J Telemed Telecare. 2014;20(6):339–349. [DOI] [PubMed] [Google Scholar]
- 44.Thomas JG, Bond DS. Review of innovations in digital health technology to promote weight control. Curr Diab Rep. 2014;14(5):485. [DOI] [PubMed] [Google Scholar]
- 45.Bacigalupo R, Cudd P, Littlewood C, Bissell P, Hawley MS, Buckley Woods H. Interventions employing mobile technology for overweight and obesity: an early systematic review of randomized controlled trials. Obes Rev. 2013;14(4):279–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee S, Lindquist R. A review of technology-based interventions to maintain weight loss. Telemed J E Health. 2015;21(3):217–232. [DOI] [PubMed] [Google Scholar]
- 47.Neve M, Morgan PJ, Jones PR, Collins CE. Effectiveness of web-based interventions in achieving weight loss and weight loss maintenance in overweight and obese adults: a systematic review with meta-analysis. Obes Rev. 2010;11(4):306–321. [DOI] [PubMed] [Google Scholar]
- 48.Hutchesson MJ, Rollo ME, Krukowski R, et al. eHealth interventions for the prevention and treatment of overweight and obesity in adults: a systematic review with meta-analysis. Obes Rev. 2015;16(5):376–392. [DOI] [PubMed] [Google Scholar]
- 49.Wharton CM, Johnston CS, Cunningham BK, Sterner D. Dietary self-monitoring, but not dietary quality, improves with use of smartphone app technology in an 8-week weight loss trial. J Nutr Educ Behav. 2014;46(5):440–444. [DOI] [PubMed] [Google Scholar]
- 50.Burke LE, Conroy MB, Sereika SM, et al. The effect of electronic self-monitoring on weight loss and dietary intake: a randomized behavioral weight loss trial. Obesity (Silver Spring). 2011;19(2):338–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Acharya SD, Elci OU, Sereika SM, Styn MA, Burke LE. Using a personal digital assistant for self-monitoring influences diet quality in comparison to a standard paper record among overweight/obese adults. J Am Diet Assoc. 2011;111(4):583–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bertz F, Pacanowski CR, Levitsky DA. Frequent Self-Weighing with Electronic Graphic Feedback to Prevent Age-Related Weight Gain in Young Adults. Obesity (Silver Spring). 2015;23(10):2009–2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Haapala I, Barengo NC, Biggs S, Surakka L, Manninen P. Weight loss by mobile phone: a 1-year effectiveness study. Public Health Nutr. 2009;12(12):2382–2391. [DOI] [PubMed] [Google Scholar]
- 54.Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss program. Arch Intern Med. 2006;166(15):1620–1625. [DOI] [PubMed] [Google Scholar]
- 55.Turner-McGrievy GM, Tate DF. Weight loss social support in 140 characters or less: use of an online social network in a remotely delivered weight loss intervention. Transl Behav Med. 2013;3(3):287–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Napolitano MA, Hayes S, Bennett GG, Ives AK, Foster GD. Using Facebook and text messaging to deliver a weight loss program to college students. Obesity (Silver Spring). 2013;21(1):25–31. [DOI] [PubMed] [Google Scholar]
- 57.Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA. 2008;299(10):1139–1148. [DOI] [PubMed] [Google Scholar]
- 58.Harvey-Berino J, Pintauro S, Buzzell P, Gold EC. Effect of internet support on the long-term maintenance of weight loss. Obes Res. 2004;12(2):320–329. [DOI] [PubMed] [Google Scholar]
- 59.Kannel WB, McGee DL. Diabetes and glucose tolerance as risk factors for cardiovascular disease: the Framingham study. Diabetes Care. 1979;2(2):120–126. [DOI] [PubMed] [Google Scholar]
- 60.Tominaga M, Eguchi H, Manaka H, Igarashi K, Kato T, Sekikawa A. Impaired glucose tolerance is a risk factor for cardiovascular disease, but not impaired fasting glucose. The Funagata Diabetes Study. Diabetes Care. 1999;22(6):920–924. [DOI] [PubMed] [Google Scholar]
- 61.Allemann S, Houriet C, Diem P, Stettler C. Self-monitoring of blood glucose in non-insulin treated patients with type 2 diabetes: a systematic review and meta-analysis. Curr Med Res Opin. 2009;25(12):2903–2913. [DOI] [PubMed] [Google Scholar]
- 62.Azar M, Gabbay R. Web-based management of diabetes through glucose uploads: has the time come for telemedicine? Diabetes Res Clin Pract. 2009;83(1):9–17. [DOI] [PubMed] [Google Scholar]
- 63.McMahon GT, Gomes HE, Hickson Hohne S, Hu TM, Levine BA, Conlin PR. Web-based care management in patients with poorly controlled diabetes. Diabetes Care. 2005;28(7):1624–1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabet Med. 2011;28(4):455–463. [DOI] [PubMed] [Google Scholar]
- 65.Quinn CC, Shardell MD, Terrin ML, Barr EA, Ballew SH, Gruber-Baldini AL. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care. 2011;34(9):1934–1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Quinn CC, Clough SS, Minor JM, Lender D, Okafor MC, Gruber-Baldini A. WellDoc mobile diabetes management randomized controlled trial: change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technol Ther. 2008;10(3):160–168. [DOI] [PubMed] [Google Scholar]
- 67.Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: national health interview survey, 2012. Vital Health Stat 10. 2014(260):1–161. [PubMed] [Google Scholar]
- 68.Fitzgerald KR. Review of article: Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010 by Katherine M. Flegal, PhD; Margaret D. Carroll, MSPH; Brian K. Kit, MD; Cynthia L. Ogden, PhD (JAMA 2012;307:491–7). J Vasc Nurs. 2013;31(3):131–132. [DOI] [PubMed] [Google Scholar]
- 69.Wilson-Frederick SM, Thorpe RJ Jr, Bell CN, Bleich SN, Ford JG, LaVeist TA. Examination of race disparities in physical inactivity among adults of similar social context. Ethn Dis. 2014;24(3):363–369. [PMC free article] [PubMed] [Google Scholar]
- 70.Neighbors CJ, Marquez DX, Marcus BH. Leisure-time physical activity disparities among Hispanic subgroups in the United States. Am J Public Health. 2008;98(8):1460–1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kirkpatrick SI, Krebs-Smith SM, Dodd KW, Reedy J. Income and race/ethnicity: drivers of adherence to dietary guidance among the US population. FASEB J. 2011:25. [Google Scholar]
- 72.Schneiderman N, Chirinos DA, Aviles-Santa ML, Heiss G. Challenges in preventing heart disease in hispanics: early lessons learned from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Prog Cardiovasc Dis. 2014;57(3):253–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lopez-Jimenez F, Lavie CJ. Hispanics and cardiovascular health and the “Hispanic Paradox”: what is known and what needs to be discovered? Prog Cardiovasc Dis. 2014;57(3):227–229. [DOI] [PubMed] [Google Scholar]
- 74.Pratt M, Perez LG, Goenka S, et al. Can population levels of physical activity be increased? Global evidence and experience. Prog Cardiovasc Dis. 2015;57(4):356–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Daviglus ML, Pirzada A, Talavera GA. Cardiovascular disease risk factors in the Hispanic/Latino population: lessons from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Prog Cardiovasc Dis. 2014;57(3):230–236. [DOI] [PubMed] [Google Scholar]
- 76.Risica PM, Gans KM, Kumanyika S, Kirtania U, Lasater TM. SisterTalk: final results of a culturally tailored cable television delivered weight control program for Black women. Int J Behav Nutr Phys Act. 2013;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gans KM, Kumanyika SK, Lovell HJ, et al. The development of SisterTalk: a cable TV-delivered weight control program for black women. Prev Med. 2003;37(6):654–667. [DOI] [PubMed] [Google Scholar]
- 78.Gerber BS, Stolley MR, Thompson AL, Sharp LK, Fitzgibbon ML. Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: a feasibility study. Health Informatics J. 2009;15(1):17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kim BH, Glanz K. Text Messaging to Motivate Walking in Older African Americans A Randomized Controlled Trial. Am J Prev Med. 2013;44(1):71–75. [DOI] [PubMed] [Google Scholar]
- 80.Joseph RP, Keller C, Adams MA, Ainsworth BE. Print versus a culturally-relevant Facebook and text message delivered intervention to promote physical activity in African American women: a randomized pilot trial. BMC Womens Health. 2015;15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Marcus BH, Dunsiger SI, Pekmezi DW, et al. The Seamos Saludables Study A Randomized Controlled Physical Activity Trial of Latinas. Am J Prev Med. 2013;45(5):598–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pekmezi D, Dunsiger S, Gans K, et al. Rationale, design, and baseline findings from Seamos Saludables: A randomized controlled trial testing the efficacy of a culturally and linguistically adapted, computer- tailored physical activity intervention for Latinas. Contemp Clin Trials. 2012;33(6):1261–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Marcus BH, Dunsiger SI, Pekmezi D, et al. Twelve-month physical activity outcomes in Latinas in the Seamos Saludables trial. Am J Prev Med. 2015;48(2):179–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Benitez TJ, Cherrington AL, Joseph RP, et al. Using Web-Based Technology to Promote Physical Activity in Latinas: Results of the Muevete Alabama Pilot Study. Comput Inform Nurs. 2015;33(7):315–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Steinberg DM, Levine EL, Lane I, et al. Adherence to Self-Monitoring via Interactive Voice Response Technology in an eHealth Intervention Targeting Weight Gain Prevention Among Black Women: Randomized Controlled Trial. J Med Internet Res. 2014;16(4):105–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Giles-Corti B, Donovan RJ. Socioeconomic status differences in recreational physical activity levels and real and perceived access to a supportive physical environment. Prev Med. 2002;35(6):601–611. [DOI] [PubMed] [Google Scholar]
- 87.Margerison-Zilko C, Cubbin C. Socioeconomic Disparities in Tobacco-Related Health Outcomes Across Racial/Ethnic Groups in the United States: National Health Interview Survey 2010. Nicotine Tob Res. 2013;15(6):1161–1165. [DOI] [PubMed] [Google Scholar]
- 88.Albright CL, Pruitt L, Castro C, Gonzalez A, Woo S, King AC. Modifying physical activity in a multiethnic sample of low-income women: One-year results from the IMPACT (increasing motivation for physical activity) project. Ann Behav Med. 2005;30(3):191–200. [DOI] [PubMed] [Google Scholar]
- 89.Samuel-Hodge CD, Johnston LF, Gizlice Z, et al. A pilot study comparing two weight loss maintenance interventions among low-income, mid-life women. BMC Public Health. 2013;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Parker DR, Windsor RA, Roberts MB, et al. Feasibility, cost, and cost-effectiveness of a telephone-based motivational intervention for underserved pregnant smokers. Nicotine Tob Res. 2007;9(10):1043–1051. [DOI] [PubMed] [Google Scholar]
- 91.Neuenschwander LM, Abbott A, Mobley AR. Comparison of a Web-Based vs In-Person Nutrition Education Program for Low-Income Adults. J Acad Nutr Diet. 2013;113(1):120–126. [DOI] [PubMed] [Google Scholar]
- 92.Lohse B, Belue R, Smith S, Wamboldt P, Cunningham-Sabo L. About Eating: An Online Program With Evidence of Increased Food Resource Management Skills for Low-Income Women. J Nutr Educ Behav. 2015;47(3):265–272. [DOI] [PubMed] [Google Scholar]
- 93.Vidrine DJ, Fletcher FE, Danysh HE, et al. A randomized controlled trial to assess the efficacy of an interactive mobile messaging intervention for underserved smokers: Project ACTION. BMC Public Health. 2012;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.King AC, Bickmore TW, Campero MI, Pruitt LA, Yin JL. Employing Virtual Advisors in Preventive Care for Under-served Communities: Results From the COMPASS Study. J Health Commun. 2013;18(12):1449–1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Woods D, Dekker S. Anticipating the effects of technological change: A new era of dynamics for human factors. Theor Issues Ergon Sci. 2000;1(3):272–282. [Google Scholar]
- 96.Haig SV. Ethical choice in the medical applications of information theory. Clin Orthop Relat Res. 2010;468(10):2672–2677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Finch CF. Implementation and dissemination research: the time has come! Br J Sports Med. 2011;45(10):763–764. [DOI] [PubMed] [Google Scholar]


