Abstract
Background
In patients with degenerative cervical myelopathy (DCM) that have spinal cord compression and sensorimotor deficits, surgical decompression is often performed. However, there is heterogeneity in clinical presentation and post-surgical functional recovery.
Objectives
Primary: a) to assess differences in muscle fat infiltration (MFI) in patients with DCM versus controls, b) to assess association between MFI and clinical disability. Secondary: to assess association between MFI pre-surgery and post-surgical functional recovery.
Study design
Cross-sectional case control study.
Methods
Eighteen patients with DCM (58.6 ± 14.2 years, 10 M/8F) and 25 controls (52.6 ± 11.8 years, 13M/12 F) underwent 3D Dixon fat-water imaging. A convolutional neural network (CNN) was used to segment cervical muscles (MFSS- multifidus and semispinalis cervicis, LC- longus capitis/colli) and quantify MFI. Modified Japanese Orthopedic Association (mJOA) and Nurick were collected.
Results
Patients with DCM had significantly higher MFI in MFSS (20.63 ± 5.43 vs 17.04 ± 5.24, p = 0.043) and LC (18.74 ± 6.7 vs 13.66 ± 4.91, p = 0.021) than controls. Patients with increased MFI in LC and MFSS had higher disability (LC: Nurick (Spearman’s ρ = 0.436, p = 0.003) and mJOA (ρ = -0.399, p = 0.008)). Increased MFI in LC pre-surgery was associated with post-surgical improvement in Nurick (ρ = -0.664, p = 0.026) and mJOA (ρ = -0.603, p = 0.049).
Conclusion
In DCM, increased muscle adiposity is significantly associated with sensorimotor deficits, clinical disability, and functional recovery after surgery. Accurate and time efficient evaluation of fat infiltration in cervical muscles may be conducted through implementation of CNN models.
Introduction
Degenerative cervical myelopathy (DCM) is a progressive disease that could lead to symptoms such as hyperreflexia, proprioceptive loss, weakness, imbalance, and gait disturbances [1,2]. It is the most common cause of spinal cord dysfunction in the elderly [3,4]. The economic burden of surgical hospitalizations for degenerative cervical spine diseases including DCM is a staggering $USD 2 Billion per annum, not accounting for additional costs owing to time lost from work, rehabilitation costs, and nonsurgical treatment costs [5].
Patients may have varying degrees of cord compression on magnetic resonance imaging (MRI) but it is currently unknown if the severity of compression is directly related to symptom severity [6,7]. Moreover, a considerable number of patients undergoing cervical decompression surgery report less than 50% improvement in clinical function as measured by modified Japanese Orthopedic Association (mJOA) [8]. This variability in clinical presentation and response to surgery indicates a multifactorial nature of DCM’s pathophysiology. Several potential pathological mechanisms have been shown to contribute to functional disability in DCM, namely demyelination of spinal cord white matter regions/tracts [9–12], neuronal and volumetric loss of gray matter [13]. Fatty infiltration of cervical spinal musculature is emerging as a potential driver of disability [14]. An improved understanding of specific pathophysiological processes may inform both the clinical assessment of and management for patients with DCM.
Muscle fat infiltration (MFI) is commonly observed in patients with cervical spine diseases including whiplash associated disorders (WAD) from a motor vehicle collision [15], traumatic spinal cord injury [16], and DCM [14]. Increased MFI in cervical flexors (longus capitis/colli and sternocleidomastoid muscles) [17] and extensors (multifidus and semispinalis cervicis) [18,19] is associated with increased pain and clinical disability in patients with WAD. In a smaller clinical cohort of the patients used in this study, we previously showed that in patients with DCM there is an increased MFI in the multifidus muscles that may be associated with clinical disability, as measured by mJOA, and Nurick scales [14]. Changes in muscle composition may occur due to aging [20], pre-existing degenerative changes [15,21], and/or chronic denervation [22–24]. Insidious damage to the spinal cord in patients with DCM may lead to decreased innervation of the cervical muscles resulting in secondary muscle degeneration, observed as MFI. Along with multifidus muscles, other cervical extensors such as semispinalis cervicis and flexors such as longus capitus and longus colli may also be adversely affected. Therefore, a comprehensive assessment of MFI in cervical spine musculature is warranted to understand both the mechanisms that drive clinical disability and heterogeneity in post-surgical symptoms and recovery. It may help to identify specific muscle groups that are affected and inform interventions through targeted physical therapy (flexors/extensors) regimens to facilitate better cervical neuromuscular function [25,26].
One barrier to quantifying muscle injury is the arduous manual segmentation required of each muscle. Recent advances in the use of artificial intelligence in medical imaging have enabled automated segmentation of cervical muscles [27]. Convolutional neural networks (CNN), in particular, permit a rapid and accurate quantification of MFI.
The purpose of this study was to examine 1) muscle degeneration as MFI of the cervical muscles in patients with DCM compared to healthy controls, 2) associations between MFI and clinical disability; and 3) to demonstrate implementation of a recently developed multi-muscle CNN model to segment seven bilateral cervical muscles and quantify MFI. We hypothesized that patients with DCM will have elevated MFI in deep cervical flexors and extensors and increased MFI will relate to worse myelopathy and clinical dysfunction.
Material and methods
Participants
Eighteen patients with DCM (8F/10M, 58.6 ±14.0 years) were recruited from a single academic spine practice. Patients were included if they presented with clinical symptoms of cervical myelopathy such as upper extremity weakness, sensory loss, a lack of hand or leg coordination, or gait instability, in combination with radiographic signs of spinal cord compression. Patients with other neurodegenerative diseases such as Alzheimer’s, multiple sclerosis, spinal tumors or trauma, diabetes, peripheral or vascular neuropathies, or a history of spinal injury or other surgery were excluded. Twenty-five age and sex matched healthy controls (12F/13M, 52.6 ± 11.8 years) were recruited. In addition to the exclusion criteria for patients, controls were screened for current spinal conditions, neck pain or other neurological deficits. Apart from these 43 participants, 6 additional participants were excluded from the analysis due to MRI artifacts during image acquisition- misprescribed field of view [4] and fat-water swapping [2]. All participants provided written informed consent as approved by the Northwestern University institutional review board. A subset of these participants was examined in our preliminary study [14].
Clinical and Health Related Quality of Life Scores (HRQOL)
All participants completed two commonly used clinical scales for myelopathy- mJOA and Nurick. The mJOA scale (ranging from 0–18) assesses sensorimotor dysfunction in upper and lower extremity [28] and the Nurick scale (ranging from 0–4) evaluates ambulatory status [29]. Health related quality of life questionnaires were assessed: Neck Disability Index (NDI), Numerical Rating Scale (NRS) for pain and discomfort, pain interference scale (Pain6a), and Health and Well-Being survey- SF-36 physical (SF-36P) component scores. The NDI evaluates neck pain and its effect on activities of daily living [30]. The NRS scale quantifies pain and discomfort on a scale of 0–10, where 0 = no discomfort/pain, 10 = extreme discomfort/pain [31]. Health and Well-Being survey- SF-36 measures bodily pain, restrictions in physical function and general health due to health problems [32].
A subset of 11 patients with DCM completed these questionnaires at their 6-month follow-up after cervical decompression surgery. In these patients, recovery rate was calculated as (Change in mJOA/(18- Pre-op) *100 [33].
MRI acquisition and assessment
Participants underwent magnetic resonance imaging of the cervical spine using a 3.0 T Siemens (Erlangen, Germany) Prisma scanner. A 64 channel head [40] and a neck coil [24] were used to acquire high-resolution 3D fat-water images of the cervical and upper thoracic spine (C2-T1) with a dual-echo gradient-echo FLASH sequence (2-point Dixon, TR = 6.59 ms, TE1 = 2.45 ms, TE2 = 3.68 ms, flip angle = 12°, field-of-view = 190 mm × 320 mm, slab oversampling of 22% with 36 partitions to prevent aliasing in the superior- inferior direction, in-plane resolution = 0.7 mm × 0.7 mm, slice thickness = 3.0 mm, number of averages = 6, acquisition time = 4 min 23 s).
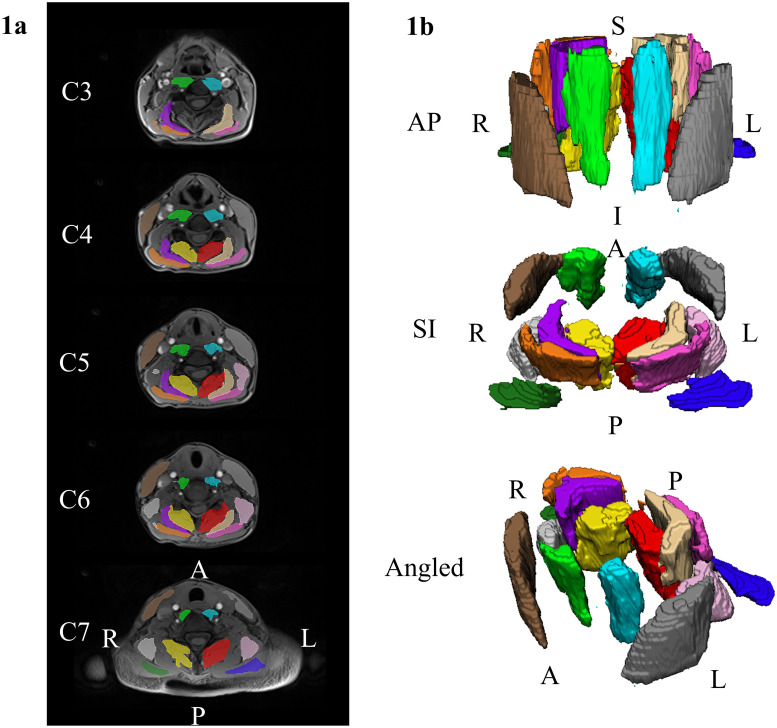
Automated segmentation of the seven bilateral cervical muscle group was performed using a recently trained dense V-net CNN model and the in-phase and out-of-phase images. The model was run using the NiftyNet (Version 0.6.0) open-source deep-learning platform built on TensorFlow (Version 1.15) in Python (Version 3.6) [34,35]. The CNN demonstrated high accuracy and excellent reliability (ICC2,1 > 0.800) for the MFI measures of all muscle groups in an independent testing dataset. The mean absolute error and root mean squared error in MFI measures was less than 2.0% and 3.0%, respectively. The CNN reduces the time to segment a single dataset from 4 to 8 hours down to only seconds (Weber et. al., in review). MFI was calculated as the fat signal/(fat signal + water signal) × 100 using the mean fat and water signal from each of the muscle segmentations. MFI metrics were extracted for the following cervical muscle groups- left and right multifidus and semispinalis cervicis (MFSS), longus colli and longus capitis (LC), semispinalis capitis (SSCap), splenius capitis (SPCap), levator scapula, (LS), sternocleidomastoid (SCM), and trapezius (TR) [Fig 1]. The average MFI of left and right muscles of each muscle group was used for further analysis.
Fig 1. Example renderings of the cervical spine muscle segmentations.
We used a previously developed convolutional neural network (CNN) to segment seven bilateral cervical muscles (14 muscles total). Example segmentations from a randomly selected DCM participant are shown. a) Two-dimensional renderings of the cervical spine segmentations at the C3 through C7 vertebral levels overlaid the axial water images. b) Three-dimensional renderings of the cervical spine muscle segmentations. The muscle groups segmented included the MFSS (left = red, right = yellow, LC (left = light blue, right = light green), SSCap (left = beige, right = purple), SPCap (left = dark pink, right = orange), LS (left = light pink, right = light gray), SCM (left = dark gray, right = brown), and TR (left = dark blue, right = dark green). L = left, R = right, A = anterior, P = posterior, S = superior, I = inferior. MFSS = multifidus and semispinalis cervicis, LC = longus colli and longus capitis, SSCap = semispinalis capitis, SPCap = splenius capitis, LS = levator scapula, SCM = sternocleidomastoid, TR = trapezius.
Statistical analysis
Normality of the data was assessed using the Shapiro-Wilk test [36]. One-way Analysis of Covariance (ANCOVA) was performed to evaluate significant differences in MFI between subject groups with age, sex, and BMI as covariates. Severity of symptoms was defined using mJOA groups- Normal (mJOA = 18), Mild (mJOA = 17, 16 or 15), Moderate (mJOA = 14, 13, 12) [37]. One-way ANCOVA was conducted to assess significant differences in MFI between mJOA groups and Nurick scores controlling for age, sex and BMI in the model. Spearman’s correlation was used to assess the association between clinical or HRQOL scores (mJOA, Nurick, Neck NRS, Arm NRS, NDI, Pain6a, SF-36P) and MFI. Paired sample t-tests were conducted to assess improvement in clinical and HRQOL scores, and Spearman’s correlation was used to evaluate the relationship between clinical scores post-surgery and pre-surgical MFI. Statistical tests were performed using IBM SPSS Statistics (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.) and significance was set at p≤ 0.05.
Results
Participant characteristics- demographic, clinical & HRQOL scores
The patient cohort consisted of 18 subjects (8 females and 10 males) while the control group consisted of 25 subjects (12 females and 13 males); Female: Male (8F:10M) vs (12F:13M) (X2(1) = 0.053, p = 0.818), mean ages 58.6 ± 14.2 years vs 52.6 ± 11.8 years (p = 0.144), mean BMI 26.0 ± 4.1 kg/m2 vs 25.2 ± 3.7 kg/m2 (p = 0.523) respectively. Patients had lower mJOA scores (14.7 ± 1.6, ranging from 12–17 vs 18.0 ± 0, p<0.001), higher Nurick (1.8 ± 0.9, ranging from 1–4 vs 0 ± 0, p<0.001), neck discomfort (4.4 ± 1.8 vs 0.2 ± 0.6, p<0.001), arm discomfort (3.6 ± 2.9 vs 0.2 ± 0.4, p<0.001), NDI (16.89 ± 7.50 vs 1.24 ± 2.05, p<0.001) and Pain-6a (61.02 ± 5.53 vs 41.84 ± 3.68, p<0.001); and lower SF-36P (38.87 ± 9.09 vs 56.49 ± 4.30, p<0.001) as compared to controls [Table 1].
Table 1. Participant’s demographic, clinical and HRQOL characteristics.
| Subjects | Sex | Age (years) | BMI (kg/m2) | mJOA | Nurick | Neck NRS | Arm NRS | NDI | Pain6a | SF-36P |
|---|---|---|---|---|---|---|---|---|---|---|
| Controls | 12F 13M |
52.6 (11.8) | 25.2 (3.7) | 18.0 (0.0) | 0.0 (0.0) | 0.2 (0.6) | 0.2 (0.4) | 1.24 (2.05) | 61.02 (5.53) | 56.49 (4.30) |
| Patients | 8F 10M |
58.6 (14.2) | 26.0 (4.1) | 14.7 (1.6) | 1.8 (0.9) | 4.4 (1.8) | 3.6 (2.9) | 16.89 (7.50) | 41.84 (3.68) | 38.87 (9.09) |
| p-value | 0.818 | 0.144 | 0.523 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
BMI = Body Mass Index, mJOA = modified Japanese Orthopedic Association, NRS = Numerical Rating Scale, Pain6a = Pain Interference Scale, NDI = Neck Disability Index, SF-36P = Health and well-being survey (physical component score).
Mean (SD) and p-value are reported.
Muscle fat infiltration and its association with clinical and HRQOL scores
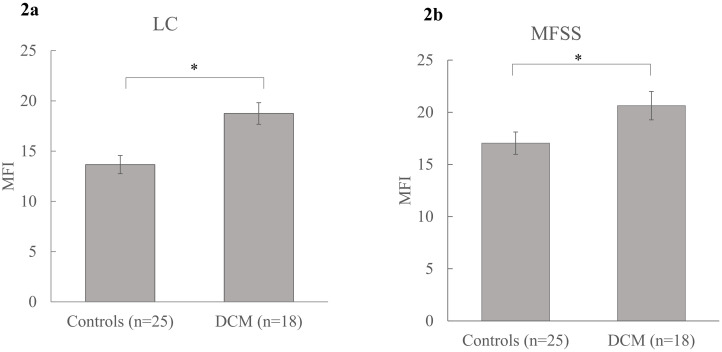
Muscle fat infiltration in the deeper cervical muscle groups such as MFSS, and LC differed significantly between patients with DCM and healthy controls. Specifically, patients with DCM had significantly higher MFI in LC as compared to controls (Right LC- 18.57 ± 7.01 vs 13.27 ± 4.74, p = 0.010, Left LC- 18.91 ± 7.38 vs 14.04 ± 5.20, p = 0.023, Mean LC- 18.74 ± 6.7 vs 13.66 ± 4.91; F (1, 38) = 5.81, p = 0.021, partial η2 = 0.133) after controlling for age, sex and BMI (covariates evaluated at age = 55.12, sex = 0.53 and BMI = 25.50) [Fig 2a]. There was a statistically significant between-subject effect of age (F (1, 38) = 17.19, p<0.001, partial η2 = 0.311) and BMI (F(1, 38) = 6.82, p = 0.013, partial η2 = 0.152) but not sex (F(1, 38) = 1.31, p = 0.260, partial η2 = 0.033) on MFI. Similarly, patients with DCM had significantly higher MFI in MFSS as compared to controls (Right MFSS- 20.58 ± 5.84 vs 16.88 ± 5.34, p = 0.046, Left MFSS- 20.69 ± 5.27 vs 17.20 ± 5.31, p = 0.048, Mean MFSS- 20.63 ±5.43 vs 17.04 ± 5.24; F(1, 35) = 1.38, p = 0.043, partial η2 = 0.138) after controlling for age, sex and BMI (covariates evaluated at age = 55.75, sex = 0.50 and BMI = 25.47) [Fig 2b]. There was a statistically significant between-subject effect of age (F (1, 35) = 11.35, p = 0.002, partial η2 = 0.245) and BMI (F (1, 35) = 9.80, p = 0.004, partial η2 = 0.219) but not sex (F (1, 35) = 1.67, p = 0.205, partial η2 = 0.046) on MFI.
Fig 2. Mean group differences in MFI.
a) MFI in cervical flexors (LC) between patients with DCM and controls; b) MFI in cervical extensors (MFSS) between patients with DCM and controls. Mean (SE) are reported. * denotes significance at p≤0.05. MFI = muscle fat infiltration, LC = longus colli and longus capitis, MFSS = multifidus and semispinalis cervicis.
There were no significant differences in MFI levels between patients with DCM and controls in SPCap (8.91 ± 4.78 vs 8.05 ± 4.74, (p = 0.562)), SSCap (15.58 ± 5.15 vs 14.22 ± 4.92, (p = 0.385)), SCM (8.70 ± 4.90 vs 6.81 ± 3.88, (p = 0.164)), TR (6.66 ± 4.09 vs 5.45 ± 4.14, (p = 0.344)), and LS (5.35 ± 3.50 vs 4.68 ± 3.48, (p = 0.541)) muscle groups [Table 2].
Table 2. Muscle fat infiltration in seven cervical muscle groups.
| MFSS | LC | SPCap | SSCap | SCM | TR | LS | |
|---|---|---|---|---|---|---|---|
| Controls | 17.04 (5.24) | 13.66 (4.91) | 8.05 (4.74) | 14.22 (4.92) | 6.81 (3.88) | 5.45 (4.14) | 4.68 (3.48) |
| Patients | 20.63 (5.43) | 18.74 (6.70) | 8.91 (4.78) | 15.58 (5.15) | 8.70 (4.90) | 6.66 (4.09) | 5.35 (3.50) |
| p-value | 0.043 | 0.021 | 0.562 | 0.385 | 0.164 | 0.344 | 0.5S41 |
MFSS = multifidus and semispinalis cervicis, LC = longus colli and longus capitis, SSCap = semispinalis capitis, SPCap = splenius capitis, LS = levator scapula, SCM = sternocleidomastoid, TR = trapezius.
Mean (SD) and p-values are reported.
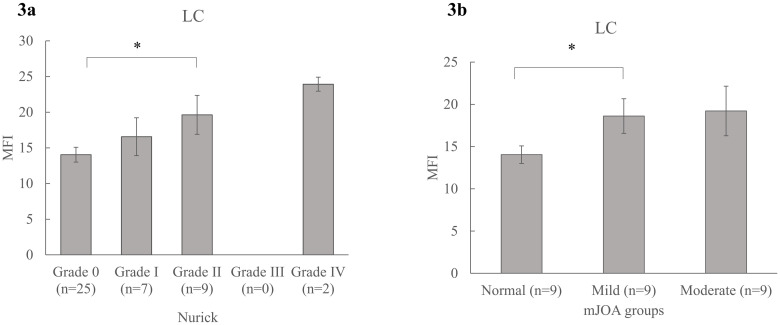
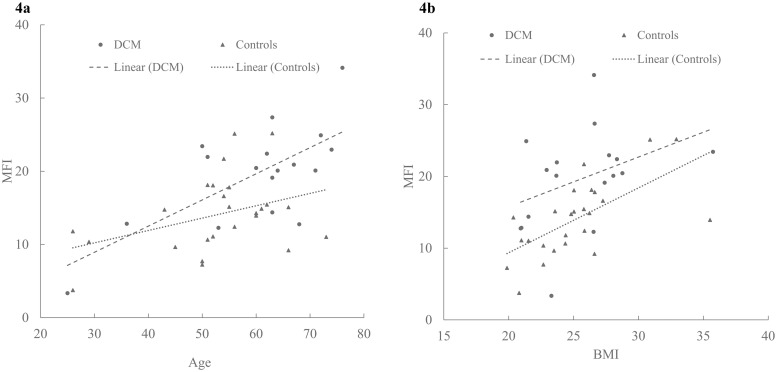
Increased MFI was significantly associated with clinical disability, pain, and physical dysfunction. Patients with elevated Nurick scores had significantly higher MFI in LC (Spearman’s ρ = 0.436 (p = 0.003)), (F (3, 36) = 3.53, p = 0.024, partial η2 = 0.228) [Fig 3a]. Patients with lower mJOA scores had significantly higher MFI in LC (Spearman’s ρ = -0.399 (p = 0.008)). Healthy controls (mJOA = 18, MFI- LC = 13.65 ± 4.90) had lower MFI than patients with mild disability (17 ≥ mJOA ≥ 15, MFI- LC = 18.48 ± 7.52) and moderate disability (14 ≥ mJOA ≥12, MFI- LC = 19.0 ± 6.25), (F (2, 37) = 3.60, p = 0.037, partial η2 = 0.163) after adjusting for age, sex and BMI (covariates evaluated at age = 55.12, sex = 0.53, BMI = 25.50) [Fig 3b]. Increased MFI in MFSS were significantly associated with increasing Nurick scores (ρ = 0.341 (p = 0.031)) and decreasing mJOA scores (ρ = -0.332 (p = 0.036)). Similar associations were observed between MFI and HRQOL scores such as NDI (ρ = 0.432 (p = 0.004)), Pain6a (ρ = 0.335 (p = 0.035)), and SF36-P (ρ = -0.420 (p = 0.026)) [Table 3]. Age and BMI had a significant association with MFI in both healthy controls and patients with DCM. Specifically, MFI levels increased with increasing age and BMI in both groups [Fig 4a and 4b].
Fig 3. Association between MFI and clinical scores.
Mean group differences in MFI across varying severity of clinical disability in patients with DCM as measured by a) Nurick (Grade 0—IV), and b) mJOA groups (Normal = 18, Mild = 17–15, and moderate = 14–12). Mean (SE) are reported. * denotes significance at p≤0.05. MFI = muscle fat infiltration, LC = longus colli and longus capitis, mJOA = modified Japanese Orthopedic Association.
Table 3. Association between muscle fat infiltration, clinical and HRQOL scores.
| mJOA | Nurick | NDI | Neck NRS | Arm NRS | Pain6a | SF-36P | |
|---|---|---|---|---|---|---|---|
| MFI (MFSS) | -0.332 (0.036) | 0.341 (0.031) | 0.346 (0.029) | 0.301 (0.059) | 0.302 (0.060) | 0.335 (0.035) | -0.420 (0.026) |
| MFI (LC) | -0.399 (0.008) | 0.436 (0.003) | 0.432 (0.004) | 0.378 (0.012) | 0.420 (0.005) | 0.557 (0.001) | -0.465 (0.008) |
MFI = Muscle Fat Infiltration, MFSS = multifidus and semispinalis cervicis, LC = longus colli and longus capitis, mJOA = modified Japanese Orthopedic Association, NDI = Neck Disability Index, NRS = Numerical Rating Scale, Pain6a = Pain Interference Scale, SF-36P = Health and well-being survey (physical component score).
Spearman’s ρ (p-value) are reported.
Fig 4. Association between MFI and demographic characteristics.
Scatterplots depicting the relationship between a) MFI and age in patients with DCM and controls; b) MFI and BMI in patients with DCM and Controls. MFI = muscle fat infiltration, BMI = body mass index.
Association with post-surgical recovery
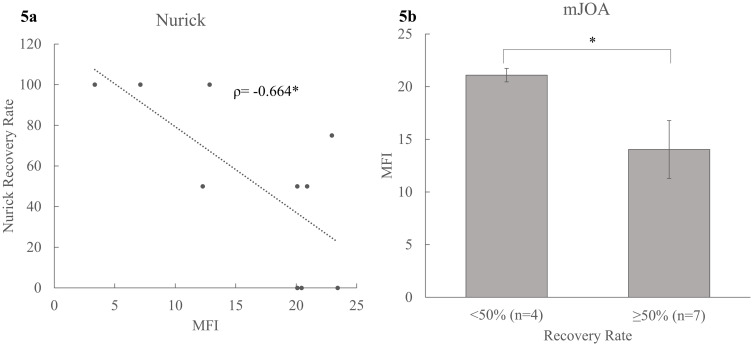
A subset of subjects consisting of 11 patients (4 females and 7 males) with DCM that completed follow up testing after decompression surgery had a mean age of 55.10 ± 15.37 years (ranging from 25–74 years) and BMI of 25.26 ± 3.94 kg/m2. Patients demonstrated significant improvement in their clinical disability after surgery. Nurick scores decreased (0.73 ± 0.65 vs 1.73 ± 0.91, p = 0.004) and mJOA scores increased (14.82 ± 1.90 vs 16.00 ± 1.94, p = 0.029). Higher MFI in LC pre-surgery was associated with post-surgical recovery rate of Nurick (ρ = -0.664 (p = 0.026)) [Fig 5a] and mJOA (ρ = -0.603 (p = 0.049). Similarly, patients who demonstrated ≥50% recovery in mJOA scores had lower MFI (LC) than those with <50% recovery (14.03 ± 7.27 vs 21.09 ±1.28, p = 0.043) [Fig 5b]. However, MFI levels in MFSS before surgery were not associated with post-surgical improvement in Nurick (ρ = 0.139 (p = 0.683)) and mJOA scores (ρ = 0.255 (p = 0.449)).
Fig 5. Association between pre-surgical MFI and post-surgical functional improvement in clinical disability.
a) Scatterplot depicting relation between MFI and Nurick recovery rate, Spearman’s ρ is reported; b) Mean group differences in MFI across mJOA recovery rate dichotomized as <50% and ≥50%. Mean (SE) are reported. * denotes significance at p≤0.05. MFI = muscle fat infiltration, LC = longus colli and longus capitis, mJOA = modified Japanese Orthopedic Association.
Discussion
In this study, we demonstrate that 1a) patients with DCM have higher MFI in deep cervical flexors and extensors as compared to age-and-sex matched healthy controls, 1b) there were no significant group differences in MFI within the more superficial muscles (SPCap, SSCap, SCM, TR, and LS), 2) increased MFI in cervical muscles is associated with higher levels of clinical disability before and after surgery, and 3) multi-muscle segmentation model, a recently developed deep learning CNN can be applied for automated quantification of MFI in patients with DCM. The findings of this study may be useful in understanding underlying pathological mechanisms that drive injury and clinical dysfunction in DCM. It may also help explain the specific sensorimotor deficits commonly observed in patients with comparable radiographic spinal cord compression [6,7]. MRI findings of altered muscle adiposity are present across a number of spinal pathologies. For example, patients with severe WAD have higher MFI in cervical flexors and extensors as compared to healthy controls and patients with mild/moderate WAD [15–19]. Elevated levels of MFI in chronic whiplash may be reduced through a regimen of neck specific exercises [38]. These changes in muscle composition occur concurrently with decreases in neck disability and increases in muscle strength. In patients with disc degeneration and low back pain, patients with lower MFI in multifidus muscles before total disc replacement surgery had better post-surgical outcomes [39], which is similar to the rotator cuff injury literature [40–42].
These studies suggest that MFI may be an important pathophysiological marker in variety of conditions affecting the appendicular skeleton and the axial spine such as rotator cuff injury [40–42], WAD [15–19], disc herniation [43,44], degenerative disc disease [45], and DCM [14], respectively. However, studies on comprehensive examination of cervical muscle composition and its effects on symptomology, diagnostic, and prognostic utility in patients in DCM are limited.
Changes in muscle composition such as increased MFI of the deep, not superficial, flexors and extensors may have direct implications on the function of the cervical spine muscles and mechanics. Deep neck flexors and extensors provide physical support to the spine vertebral column and play an important role in postural biomechanics, proprioception, and fine motor control [46,47]. Additionally, patients with DCM often present with cervical sagittal vertical misalignment resulting in forward head posture (FHP) [48,49], which could reflect excessive loading on a weakened muscular system. Biomechanical modeling of increasing FHP and its influence on cervical muscles showed significant lengthening of the cervical extensors such as MFSS and shortening of the cervical flexors such as LC. As a result of sustained contractions, cervical extensor muscles may weaken [50] and could likely fatigue. Prolonged shortening of the cervical flexors may contribute to generalized disuse atrophy and increased MFI [17,51]. Muscle denervation due to spinal cord compression, and the accompanied increased fatty infiltration, may further diminish the capacity of cervical muscles to maintain dynamic posture and tolerate corresponding biomechanical stresses. Sarcopenia refers to loss of muscle mass and function, is a key part of frailty in the elderly [52]. Numerous studies have shown that increased frailty is associated with adverse clinical outcomes after spine surgery in patients with traumatic spinal cord injury [53], degenerative spine diseases [54–56], and DCM [57]. In this study we found that increased MFI is associated with increasing pain and clinical disability as measured by Nurick, mJOA, Neck NRS, and NDI scores. These findings are consistent with the aforementioned literature and validate the impact of muscle composition and quality on the nature/causes of impairment and clinical dysfunction in patients with DCM. In older adults with disability, fatty infiltration in skeletal muscles may be decreased through physical exercise [20,58]. In chronic WAD, MFI in cervical multifidus was reduced after 10 weeks of neck specific exercises [38]. Similarly, neck specific exercises such as flexor/extensor training may be useful in improving clinical outcomes in patients with DCM and MFI may be a modifiable biomarker for therapeutic interventions.
Changes in fat infiltration may occur with increasing age as lean body mass decreases and body adiposity increases [59]. Our findings demonstrate increase in MFI with increasing age and BMI both in healthy controls and patients. However, statistically significant differences in MFI between groups persisted even after controlling for age and BMI. Therefore, we consider our finding of increased MFI in patients with DCM as a pathological and clinically important change in muscle composition.
In patients with DCM, surgical decompression shows variable and limited neurological improvement [60]; surgical interventions combined with conservative rehabilitation show clinical equipoise [61–63]. We previously demonstrated that increased demyelination (lower magnetization transfer ratios (MTR)) in anterior and lateral cord regions and descending motor tracts such as corticospinal, reticulospinal tracts are associated with poor functional recovery after surgery [64]. Sarcopenia in deep cervical flexors (LC) has been shown to predict poor post-surgical improvement in clinical function in patients with myelopathy [65]. In this study, our preliminary analysis evaluating MFI and post-surgical functional recovery showed that increased pre-surgical MFI in LC muscles is adversely related to post-surgical improvement in clinical scores of mJOA and Nurick. It can be hypothesized that cervical flexor training before and after surgery may promote surgical outcomes and MFI could be a predictive biomarker for better prognosis. However, further large sample investigations are needed to understand and confirm the role of cervical musculature in neurological functional recovery and evaluate the utility of fat-water imaging and MFI in predicting surgical outcome in DCM.
Recent advances in artificial intelligence techniques have led to development of automated tools and application of machine learning algorithms in the field of spinal imaging [27,66,67]. In this study, we utilize a recently developed CNN model that segments seven bilateral cervical muscle groups (14 muscles in total) and measures muscle composition in each muscle group (Weber et. al., in review). This CNN was validated in patients with WAD and shown to be highly time efficient as compared to manual segmentation (drawing regions of interest), accurate and reliable for MFI measures (when tested against different human raters). Conventional MRI techniques (T1, T2 weighted imaging) are excellent in detailed visualization of spinal anatomy in spinal diseases such as DCM, however they do not provide information about specific neuropathophysiological processes such as demyelination, axonal and neuronal loss [68]. Advanced MR techniques such as diffusion tensor, myelin-water, magnetization transfer and fat-water imaging provide several useful quantitative markers of spinal cord injury. Although these MRI based metrics are shown to be associated with clinical impairment and show diagnostic and predictive utility, their translation to clinical use has not been realized [69]. Development and application of CNN models such as the one implemented in this study will be essential to enhance future efficiency and clinical implementation of quantitative MRI techniques.
We acknowledge there are limitations in our study. Firstly, while we have controlled our analysis for confounders such as age, sex, and BMI in assessing differences in MFI; composition of the cervical musculature may also be influenced by other factors such as total lean body mass, physical activity, or neck-specific exercise levels. Secondly, quantification of MFI depends on the accuracy of segmentation of the muscles by the implemented CNN, and subtle differences in field of view during MRI acquisition may affect definition of the muscle boundaries. To address this limitation, we visually screened our database to identify and exclude any such dataset where the CNN may have performed inaccurately. Thirdly, demyelination of the spinal cord regions and white matter tracts may be a prominent pathomechanism in DCM. Here, we studied the role of increased MFI on DCM symptomology in isolation. Additionally, cervical spine misalignment is associated with neck disability in patients with DCM [70], however this study did not control for differences in spinal alignment between participant groups. Future studies that evaluate cumulative impact of cervical spine alignment with cord compression, demyelination, and muscle adiposity are needed as this work shows the early associations that may warrant further investigation. Lastly, while we aimed to include patients with varying degrees of cervical myelopathy, participation of patients with severe myelopathy may be limited due to severity of clinical disability or urgent need of therapeutic interventions.
Conclusion
Compared to healthy controls, patients with DCM have increased fat infiltration in deep cervical flexors and extensor muscles. These adverse changes in muscle composition associate with sensorimotor deficits, physical function, pain, and disability both before and after surgery. MFI could be a potential biomarker for patient assessments, better candidate selection for surgery and prognosis. Future investigations focusing on predictive utility of fat water imaging should compare differential recovery among patients with DCM after surgery. Secondly, this study demonstrates the novel application of machine learning in medical imaging, specifically in automated segmentation of muscles across the cervical spine and quantification of MRI based metric of muscle composition (MFI). We build upon our previous work [14] utilizing this multi-muscle model that can be easily applied to the cervical spine in DCM and other pathologies. Implementation of machine learning could facilitate translation of MRI metrics such as MFI that are otherwise limited to research environments, into clinical practice.
Supporting information
(XLSX)
Data Availability
All relevant data are within the manuscript and its Supporting information files.
Funding Statement
Zachary A. Smith received funding from the National Institute on Neurological Disorders and Stroke (grant K23NS104211). Kenneth A. Weber II received funding from National Institute of Neurological Disorders and Stroke and National Institute of Child Health and Human Development (grants K23NS104211, L30NS108301 and R03HD094577). Andrew C. Smith received funding from National Institute of Child Health and Human Development (grant R03HD094577). Sean Mackey received funding from National Institute of Drug Abuse (grant K24DA029262). James M. Elliott received funding from National Institute of Child Health and Human Development (grants R01HD079076-01 and R03HD094577). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG. Degenerative Cervical Myelopathy: Epidemiology, Genetics, and Pathogenesis. Spine (Phila Pa 1976). 2015;40(12):E675–93. [DOI] [PubMed] [Google Scholar]
- 2.Bakhsheshian J, Mehta VA, Liu JC. Current Diagnosis and Management of Cervical Spondylotic Myelopathy. Global Spine J. 2017;7(6):572–86. doi: 10.1177/2192568217699208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kalsi-Ryan S, Karadimas SK, Fehlings MG. Cervical spondylotic myelopathy: the clinical phenomenon and the current pathobiology of an increasingly prevalent and devastating disorder. Neuroscientist. 2013;19(4):409–21. doi: 10.1177/1073858412467377 [DOI] [PubMed] [Google Scholar]
- 4.Karadimas SK, Gatzounis G, Fehlings MG. Pathobiology of cervical spondylotic myelopathy. Eur Spine J. 2015;24 Suppl 2:132–8. doi: 10.1007/s00586-014-3264-4 [DOI] [PubMed] [Google Scholar]
- 5.Patil PG, Turner DA, Pietrobon R. National trends in surgical procedures for degenerative cervical spine disease: 1990–2000. Neurosurgery. 2005;57(4):753–8; discussion -8. [PubMed] [Google Scholar]
- 6.Ichihara K, Taguchi T, Sakuramoto I, Kawano S, Kawai S. Mechanism of the spinal cord injury and the cervical spondylotic myelopathy: new approach based on the mechanical features of the spinal cord white and gray matter. J Neurosurg. 2003;99(3 Suppl):278–85. doi: 10.3171/spi.2003.99.3.0278 [DOI] [PubMed] [Google Scholar]
- 7.Wen CY, Cui JL, Mak KC, Luk KD, Hu Y. Diffusion tensor imaging of somatosensory tract in cervical spondylotic myelopathy and its link with electrophysiological evaluation. Spine J. 2014;14(8):1493–500. doi: 10.1016/j.spinee.2013.08.052 [DOI] [PubMed] [Google Scholar]
- 8.Zhang JT, Wang LF, Wang S, Li J, Shen Y. Risk factors for poor outcome of surgery for cervical spondylotic myelopathy. Spinal Cord. 2016;54(12):1127–31. doi: 10.1038/sc.2016.64 [DOI] [PubMed] [Google Scholar]
- 9.Hopkins BS, Weber KA 2nd, Cloney MB, Paliwal M, Parrish TB, Smith ZA. Tract-Specific Volume Loss on 3T MRI in Patients With Cervical Spondylotic Myelopathy. Spine (Phila Pa 1976). 2018;43(20):E1204–e9. doi: 10.1097/BRS.0000000000002667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cloney MB, Smith ZA, Weber KA 2nd, Parrish TB. Quantitative Magnetization Transfer MRI Measurements of the Anterior Spinal Cord Region are Associated With Clinical Outcomes in Cervical Spondylotic Myelopathy. Spine (Phila Pa 1976). 2018;43(10):675–80. doi: 10.1097/BRS.0000000000002470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu H, MacMillian EL, Jutzeler CR, Ljungberg E, MacKay AL, Kolind SH, et al. Assessing structure and function of myelin in cervical spondylotic myelopathy: Evidence of demyelination. Neurology. 2017;89(6):602–10. doi: 10.1212/WNL.0000000000004197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suleiman LI, Weber KA 2nd, Rosenthal BD, Bhatt SA, Savage JW, Hsu WK, et al. High-resolution magnetization transfer MRI in patients with cervical spondylotic myelopathy. J Clin Neurosci. 2018;51:57–61. doi: 10.1016/j.jocn.2018.02.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith ZA, Weber KA 2nd, Paliwal M, Hopkins BS, Barry AJ, Cantrell D, et al. Magnetic Resonance Imaging Atlas-Based Volumetric Mapping of the Cervical Cord Gray Matter in Cervical Canal Stenosis. World Neurosurg. 2020;134:e497–e504. doi: 10.1016/j.wneu.2019.10.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cloney M, Smith AC, Coffey T, Paliwal M, Dhaher Y, Parrish T, et al. Fatty infiltration of the cervical multifidus musculature and their clinical correlates in spondylotic myelopathy. J Clin Neurosci. 2018;57:208–13. doi: 10.1016/j.jocn.2018.03.028 [DOI] [PubMed] [Google Scholar]
- 15.Elliott JM, Smith AC, Hoggarth MA, Albin SR, Weber KA 2nd, Haager M, et al. Muscle fat infiltration following whiplash: A computed tomography and magnetic resonance imaging comparison. PLoS One. 2020;15(6):e0234061. doi: 10.1371/journal.pone.0234061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith AC, Parrish TB, Hoggarth MA, McPherson JG, Tysseling VM, Wasielewski M, et al. Potential associations between chronic whiplash and incomplete spinal cord injury. Spinal Cord Ser Cases. 2015;1:15024. doi: 10.1038/scsandc.2015.24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Elliott JM, O’Leary S, Sterling M, Hendrikz J, Pedler A, Jull G. Magnetic resonance imaging findings of fatty infiltrate in the cervical flexors in chronic whiplash. Spine (Phila Pa 1976). 2010;35(9):948–54. doi: 10.1097/BRS.0b013e3181bb0e55 [DOI] [PubMed] [Google Scholar]
- 18.Elliott J, Jull G, Noteboom JT, Darnell R, Galloway G, Gibbon WW. Fatty infiltration in the cervical extensor muscles in persistent whiplash-associated disorders: a magnetic resonance imaging analysis. Spine (Phila Pa 1976). 2006;31(22):E847–55. doi: 10.1097/01.brs.0000240841.07050.34 [DOI] [PubMed] [Google Scholar]
- 19.Smith AC, Albin SR, Abbott R, Crawford RJ, Hoggarth MA, Wasielewski M, et al. Confirming the geography of fatty infiltration in the deep cervical extensor muscles in whiplash recovery. Scientific Reports. 2020;10(1):11471. doi: 10.1038/s41598-020-68452-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marcus RL, Addison O, Kidde JP, Dibble LE, Lastayo PC. Skeletal muscle fat infiltration: impact of age, inactivity, and exercise. J Nutr Health Aging. 2010;14(5):362–6. doi: 10.1007/s12603-010-0081-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Elliott JM, Parrish TB, Walton DM, Vassallo AJ, Fundaun J, Wasielewski M, et al. Does Overall Cervical Spine Pathology Relate to the Clinical Heterogeneity of Chronic Whiplash? Am J Emerg Med. 2020;38(5):869–73. doi: 10.1016/j.ajem.2019.06.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fleckenstein JL, Watumull D, Conner KE, Ezaki M, Greenlee RG Jr., Bryan WW, et al. Denervated human skeletal muscle: MR imaging evaluation. Radiology. 1993;187(1):213–8. doi: 10.1148/radiology.187.1.8451416 [DOI] [PubMed] [Google Scholar]
- 23.Hodges P, Holm AK, Hansson T, Holm S. Rapid Atrophy of the Lumbar Multifidus Follows Experimental Disc or Nerve Root Injury. Spine. 2006;31(25). doi: 10.1097/01.brs.0000248453.51165.0b [DOI] [PubMed] [Google Scholar]
- 24.Dulor JP, Cambon B, Vigneron P, Reyne Y, Nouguès J, Casteilla L, et al. Expression of specific white adipose tissue genes in denervation-induced skeletal muscle fatty degeneration. FEBS Lett. 1998;439(1–2):89–92. doi: 10.1016/s0014-5793(98)01216-2 [DOI] [PubMed] [Google Scholar]
- 25.Blomgren J, Strandell E, Jull G, Vikman I, Röijezon U. Effects of deep cervical flexor training on impaired physiological functions associated with chronic neck pain: a systematic review. BMC Musculoskelet Disord. 2018;19(1):415. doi: 10.1186/s12891-018-2324-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Suvarnnato T, Puntumetakul R, Uthaikhup S, Boucaut R. Effect of specific deep cervical muscle exercises on functional disability, pain intensity, craniovertebral angle, and neck-muscle strength in chronic mechanical neck pain: a randomized controlled trial. J Pain Res. 2019;12:915–25. doi: 10.2147/JPR.S190125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weber KA, Smith AC, Wasielewski M, Eghtesad K, Upadhyayula PA, Wintermark M, et al. Deep Learning Convolutional Neural Networks for the Automatic Quantification of Muscle Fat Infiltration Following Whiplash Injury. Scientific Reports. 2019;9(1):7973. doi: 10.1038/s41598-019-44416-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nagata K, Yoshimura N, Hashizume H, Muraki S, Ishimoto Y, Yamada H, et al. The prevalence of cervical myelopathy among subjects with narrow cervical spinal canal in a population-based magnetic resonance imaging study: the Wakayama Spine Study. Spine J. 2014;14(12):2811–7. doi: 10.1016/j.spinee.2014.03.051 [DOI] [PubMed] [Google Scholar]
- 29.Nurick S. The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Brain. 1972;95(1):87–100. doi: 10.1093/brain/95.1.87 [DOI] [PubMed] [Google Scholar]
- 30.Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14(7):409–15. [PubMed] [Google Scholar]
- 31.Walton DM, Elliott JM, Salim S, Al-Nasri I. A reconceptualization of the pain numeric rating scale: Anchors and clinically important differences. J Hand Ther. 2018;31(2):179–83. doi: 10.1016/j.jht.2017.12.008 [DOI] [PubMed] [Google Scholar]
- 32.Ware JE Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83. [PubMed] [Google Scholar]
- 33.Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Phila Pa 1976). 1981;6(4):354–64. doi: 10.1097/00007632-198107000-00005 [DOI] [PubMed] [Google Scholar]
- 34.Gibson E, Giganti F, Hu Y, Bonmati E, Bandula S, Gurusamy K, et al. Automatic Multi-Organ Segmentation on Abdominal CT With Dense V-Networks. IEEE Trans Med Imaging. 2018;37(8):1822–34. doi: 10.1109/TMI.2018.2806309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gibson E, Li W, Sudre C, Fidon L, Shakir DI, Wang G, et al. NiftyNet: a deep-learning platform for medical imaging. Comput Methods Programs Biomed. 2018;158:113–22. doi: 10.1016/j.cmpb.2018.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ghasemi A, Zahediasl S. Normality tests for statistical analysis: a guide for non-statisticians. Int J Endocrinol Metab. 2012;10(2):486–9. doi: 10.5812/ijem.3505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tetreault L, Kopjar B, Nouri A, Arnold P, Barbagallo G, Bartels R, et al. The modified Japanese Orthopaedic Association scale: establishing criteria for mild, moderate and severe impairment in patients with degenerative cervical myelopathy. Eur Spine J. 2017;26(1):78–84. doi: 10.1007/s00586-016-4660-8 [DOI] [PubMed] [Google Scholar]
- 38.O’Leary S, Jull G, Van Wyk L, Pedler A, Elliott J. Morphological changes in the cervical muscles of women with chronic whiplash can be modified with exercise-A pilot study. Muscle Nerve. 2015;52(5):772–9. doi: 10.1002/mus.24612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Storheim K, Berg L, Hellum C, Gjertsen Ø, Neckelmann G, Espeland A, et al. Fat in the lumbar multifidus muscles - predictive value and change following disc prosthesis surgery and multidisciplinary rehabilitation in patients with chronic low back pain and degenerative disc: 2-year follow-up of a randomized trial. BMC Musculoskelet Disord. 2017;18(1):145. doi: 10.1186/s12891-017-1505-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lansdown DA, Lee S, Sam C, Krug R, Feeley BT, Ma CB. A Prospective, Quantitative Evaluation of Fatty Infiltration Before and After Rotator Cuff Repair. Orthop J Sports Med. 2017;5(7):2325967117718537. doi: 10.1177/2325967117718537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Valencia AP, Lai JK, Iyer SR, Mistretta KL, Spangenburg EE, Davis DL, et al. Fatty Infiltration Is a Prognostic Marker of Muscle Function After Rotator Cuff Tear. The American Journal of Sports Medicine. 2018;46(9):2161–9. doi: 10.1177/0363546518769267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Melis B, Nemoz C, Walch G. Muscle fatty infiltration in rotator cuff tears: descriptive analysis of 1688 cases. Orthop Traumatol Surg Res. 2009;95(5):319–24. doi: 10.1016/j.otsr.2009.05.001 [DOI] [PubMed] [Google Scholar]
- 43.Fortin M, Lazáry À, Varga PP, McCall I, Battié MC. Paraspinal muscle asymmetry and fat infiltration in patients with symptomatic disc herniation. Eur Spine J. 2016;25(5):1452–9. doi: 10.1007/s00586-016-4503-7 [DOI] [PubMed] [Google Scholar]
- 44.Colakoglu B, Alis D. Evaluation of lumbar multifidus muscle in patients with lumbar disc herniation: are complex quantitative MRI measurements needed? J Int Med Res. 2019;47(8):3590–600. doi: 10.1177/0300060519853430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Urrutia J, Besa P, Lobos D, Campos M, Arrieta C, Andia M, et al. Lumbar paraspinal muscle fat infiltration is independently associated with sex, age, and inter-vertebral disc degeneration in symptomatic patients. Skeletal Radiol. 2018;47(7):955–61. doi: 10.1007/s00256-018-2880-1 [DOI] [PubMed] [Google Scholar]
- 46.Boyd-Clark LC, Briggs CA, Galea MP. Muscle spindle distribution, morphology, and density in longus colli and multifidus muscles of the cervical spine. Spine (Phila Pa 1976). 2002;27(7):694–701. [DOI] [PubMed] [Google Scholar]
- 47.Mayoux-Benhamou MA, Revel M, Vallée C, Roudier R, Barbet JP, Bargy F. Longus colli has a postural function on cervical curvature. Surg Radiol Anat. 1994;16(4):367–71. doi: 10.1007/BF01627655 [DOI] [PubMed] [Google Scholar]
- 48.Ames CP, Blondel B, Scheer JK, Schwab FJ, Le Huec JC, Massicotte EM, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976). 2013;38(22 Suppl 1):S149–60. doi: 10.1097/BRS.0b013e3182a7f449 [DOI] [PubMed] [Google Scholar]
- 49.Mohanty C, Massicotte EM, Fehlings MG, Shamji MF. Association of preoperative cervical spine alignment with spinal cord magnetic resonance imaging hyperintensity and myelopathy severity: analysis of a series of 124 cases. Spine (Phila Pa 1976). 2015;40(1):11–6. doi: 10.1097/BRS.0000000000000670 [DOI] [PubMed] [Google Scholar]
- 50.Khayatzadeh S, Kalmanson OA, Schuit D, Havey RM, Voronov LI, Ghanayem AJ, et al. Cervical Spine Muscle-Tendon Unit Length Differences Between Neutral and Forward Head Postures: Biomechanical Study Using Human Cadaveric Specimens. Physical Therapy. 2017;97(7):756–66. doi: 10.1093/ptj/pzx040 [DOI] [PubMed] [Google Scholar]
- 51.Bodine SC. Disuse-induced muscle wasting. Int J Biochem Cell Biol. 2013;45(10):2200–8. doi: 10.1016/j.biocel.2013.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Morley JE. Frailty and sarcopenia in elderly. Wiener klinische Wochenschrift. 2016;128(7):439–45. doi: 10.1007/s00508-016-1087-5 [DOI] [PubMed] [Google Scholar]
- 53.Banaszek D, Inglis T, Marion TE, Charest-Morin R, Moskven E, Rivers CS, et al. Effect of Frailty on Outcome after Traumatic Spinal Cord Injury. J Neurotrauma. 2020;37(6):839–45. doi: 10.1089/neu.2019.6581 [DOI] [PubMed] [Google Scholar]
- 54.Flexman AM, Charest-Morin R, Stobart L, Street J, Ryerson CJ. Frailty and postoperative outcomes in patients undergoing surgery for degenerative spine disease. Spine J. 2016;16(11):1315–23. doi: 10.1016/j.spinee.2016.06.017 [DOI] [PubMed] [Google Scholar]
- 55.Park S, Kim HJ, Ko BG, Chung JW, Kim SH, Park SH, et al. The prevalence and impact of sarcopenia on degenerative lumbar spinal stenosis. Bone Joint J. 2016;98-b(8):1093–8. doi: 10.1302/0301-620X.98B8.37623 [DOI] [PubMed] [Google Scholar]
- 56.Inose H, Yamada T, Hirai T, Yoshii T, Abe Y, Okawa A. The impact of sarcopenia on the results of lumbar spinal surgery. Osteoporos Sarcopenia. 2018;4(1):33–6. doi: 10.1016/j.afos.2018.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wilson JRF, Badhiwala JH, Moghaddamjou A, Yee A, Wilson JR, Fehlings MG. Frailty Is a Better Predictor than Age of Mortality and Perioperative Complications after Surgery for Degenerative Cervical Myelopathy: An Analysis of 41,369 Patients from the NSQIP Database 2010–2018. J Clin Med. 2020;9(11). doi: 10.3390/jcm9113491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Goodpaster BH, Chomentowski P, Ward BK, Rossi A, Glynn NW, Delmonico MJ, et al. Effects of physical activity on strength and skeletal muscle fat infiltration in older adults: a randomized controlled trial. J Appl Physiol (1985). 2008;105(5):1498–503. doi: 10.1152/japplphysiol.90425.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Forbes GB, Reina JC. Adult lean body mass declines with age: some longitudinal observations. Metabolism. 1970;19(9):653–63. doi: 10.1016/0026-0495(70)90062-4 [DOI] [PubMed] [Google Scholar]
- 60.Shiban E, Meyer B. Treatment considerations of cervical spondylotic myelopathy. Neurol Clin Pract. 2014;4(4):296–303. doi: 10.1212/CPJ.0000000000000050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rhee J, Tetreault LA, Chapman JR, Wilson JR, Smith JS, Martin AR, et al. Nonoperative Versus Operative Management for the Treatment Degenerative Cervical Myelopathy: An Updated Systematic Review. Global Spine J. 2017;7(3 Suppl):35s–41s. doi: 10.1177/2192568217703083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kong LD, Meng LC, Wang LF, Shen Y, Wang P, Shang ZK. Evaluation of conservative treatment and timing of surgical intervention for mild forms of cervical spondylotic myelopathy. Exp Ther Med. 2013;6(3):852–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kadaňka Z, Bednařík J, Novotný O, Urbánek I, Dušek L. Cervical spondylotic myelopathy: conservative versus surgical treatment after 10 years. Eur Spine J. 2011;20(9):1533–8. doi: 10.1007/s00586-011-1811-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Paliwal M, Weber KA 2nd, Hopkins BS, Cantrell DR, Hoggarth MA, Elliott JM, et al. Magnetization Transfer Ratio and Morphometrics of the Spinal Cord Associates with Surgical Recovery in Patients with Degenerative Cervical Myelopathy. World Neurosurg. 2020;144:e939–e47. doi: 10.1016/j.wneu.2020.09.148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Thakar S, Arun AA, Aryan S, Mohan D, Hegde AS. Deep flexor sarcopenia as a predictor of poor functional outcome after anterior cervical discectomy in patients with myelopathy. Acta Neurochir (Wien). 2019;161(10):2201–9. doi: 10.1007/s00701-019-03972-8 [DOI] [PubMed] [Google Scholar]
- 66.Azimi P, Yazdanian T, Benzel EC, Aghaei HN, Azhari S, Sadeghi S, et al. A Review on the Use of Artificial Intelligence in Spinal Diseases. Asian Spine J. 2020;14(4):543–71. doi: 10.31616/asj.2020.0147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hopkins BS, Weber KA 2nd, Kesavabhotla K, Paliwal M, Cantrell DR, Smith ZA. Machine Learning for the Prediction of Cervical Spondylotic Myelopathy: A Post Hoc Pilot Study of 28 Participants. World Neurosurg. 2019;127:e436–e42. doi: 10.1016/j.wneu.2019.03.165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Nouri A, Martin AR, Mikulis D, Fehlings MG. Magnetic resonance imaging assessment of degenerative cervical myelopathy: a review of structural changes and measurement techniques. Neurosurg Focus. 2016;40(6):E5. doi: 10.3171/2016.3.FOCUS1667 [DOI] [PubMed] [Google Scholar]
- 69.Martin AR, Aleksanderek I, Cohen-Adad J, Tarmohamed Z, Tetreault L, Smith N, et al. Translating state-of-the-art spinal cord MRI techniques to clinical use: A systematic review of clinical studies utilizing DTI, MT, MWF, MRS, and fMRI. Neuroimage Clin. 2016;10:192–238. doi: 10.1016/j.nicl.2015.11.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Iyer S, Nemani VM, Nguyen J, Elysee J, Burapachaisri A, Ames CP, et al. Impact of Cervical Sagittal Alignment Parameters on Neck Disability. Spine. 2016;41(5):371–7. doi: 10.1097/BRS.0000000000001221 [DOI] [PubMed] [Google Scholar]