Abstract
Despite concerns about the coexistence of overnutrition, undernutrition and micronutrient deficiencies, which is compositely referred to as the triple burden of malnutrition (TBM), little is known about the phenomenon in sub-Saharan Africa (SSA). We, therefore, aimed to examine the prevalence and investigate the factors associated with TBM in SSA. This study uses cross-sectional survey data collected through the Demographic and Health Surveys (DHS) Program from 2010 to 2019. Data from 32 countries in SSA were used for the analysis. The prevalence of TBM were presented in tables and maps using percentages. The predictors of TBM were examined by fitting a negative log-log regression to the data. The results were then presented using adjusted odds ratios (aORs) at 95% Confidence Intervals (CIs). Out of the 169,394 children, 734 (1%) suffered from TBM. The highest proportion of children with TBM in the four geographic regions in SSA was found in western Africa (0.75%) and the lowest in central Africa (0.21%). Children aged 1 [aOR = 1.283; 95% CI = 1.215–1.355] and those aged 2 [aOR = 1.133; 95% CI = 1.067–1.204] were more likely to experience TBM compared to those aged 0. TBM was less likely to occur among female children compared to males [aOR = 0.859; 95% CI = 0.824–0.896]. Children whose perceived size at birth was average [aOR = 1.133; 95% CI = 1.076–1.193] and smaller than average [aOR = 1.278; 95% CI = 1.204–1.356] were more likely to suffer from TBM compared to those who were larger than average at birth. Children born to mothers with primary [aOR = 0.922; 95% CI = 0.865–0.984] and secondary [aOR = 0.829; 95% CI = 0.777–0.885] education were less likely to suffer from TBM compared to those born to mothers with no formal education. Children born to mothers who attended antenatal care (ANC) had lower odds of experiencing TBM compared to those born to mothers who did not attend ANC [aOR = 0.969; 95% CI = 0.887–0.998]. Children born to mothers who use clean household cooking fuel were less likely to experience TBM compared to children born to mothers who use unclean household cooking fuel [aOR = 0.724; 95% CI = 0.612–0.857]. Essentially, higher maternal education, ANC attendance and use of clean cooking fuel were protective factors against TBM, whereas higher child age, low size at birth and being a male child increased the risk of TBM. Given the regional variations in the prevalence and risk of TBM, region-specific interventions must be initiated to ensure the likelihood of those interventions being successful at reducing the risk of TBM. Countries in Western Africa in particular would have to strengthen their current policies and programmes on malnutrition to enhance their attainment of the SDGs.
Keywords: global health, malnutrition, mother-child pairs, Sub-Saharan Africa, triple burden
1. Introduction
Globally, the world is operating on the Sustainable Development Goals (SDGs). Given the importance of promoting zero hunger and nutritional needs of the world’s population, SDG 2.2 envisions ending all forms of malnutrition by 2030 [1]. With this target in mind, there has been a significant decline in malnutrition across the globe [2]. For example, the global prevalence of stunting declined from 29.5% in 2005 to 22.9% in 2016 [3]. Nevertheless, there is still a substantial proportion of people worldwide who are malnourished [2].
Available evidence approximates that 155, and 52 million children under age five are stunted and wasted, respectively [3]. Moreover, the global prevalence of undernourished people is estimated to have increased from 777 million in 2015 to 815 million in 2016 [4], thus making malnutrition and its concomitant issues important public health concern [5]. In addition, malnutrition is reported to be most prevalent in South-East Asia [6] and sub-Saharan Africa [7].
It is important to note that malnutrition is not concerned only with the sufficiency of food but extends to having the appropriate micronutrients [8]. Moreover, evidence suggests that malnutrition coexists with other health events [9,10]. The coexistence of undernutrition along with overweight and obesity within individuals, households and populations and across the life course is what has been referred to as the double burden of malnutrition (DBM) [11]. However, in recent times, there have been concerns about the coexistence of overnutrition, undernutrition and micronutrient deficiencies, which is compositely referred to as the triple burden of malnutrition (TBM) [8].
TBM is a fairly new concept and has, therefore, not received enough scholarship in the current discourse on malnutrition among children under five [12]. Few studies have examined the prevalence and associated factors of TBM. Available evidence from elsewhere in Nepal [12] and India [2,8] have found factors such as maternal age, maternal educational status, caesarean section delivery, birth size of baby, household wealth quintile and place of residence to be significantly associated with TBM. Nonetheless, its prevalence and associated factors in the sub-Saharan African context have not been investigated, even though TBM poses a great threat to the health and wellbeing of children. This presents a gap in the current knowledge about TBM in sub-Saharan Africa (SSA) that ought to be filled. We, therefore, aimed to examine the prevalence and investigate the factors associated with TBM in the sub-Saharan African context. Knowing the prevalence and associated factors of TBM is a step in the right direction towards the attainment of SDG 2.2.
2. Materials and Methods
2.1. Study Design
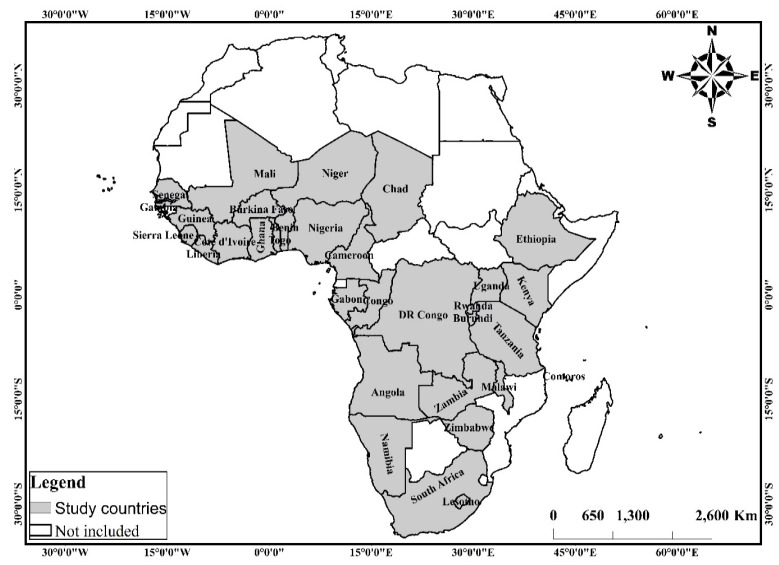
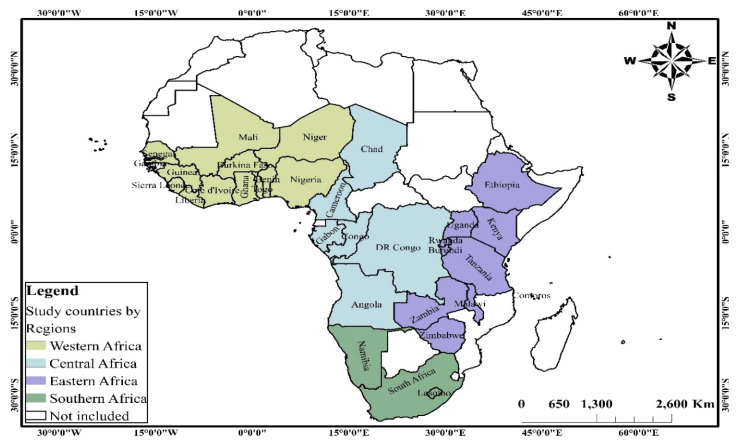
This study uses cross-sectional survey data collected through the Demographic and Health Surveys (DHS) Program from 2010 to 2019. The data of 32 countries in SSA (see Figure 1) in the geographic regions, western, eastern, central and southern Africa (see Figure 2), were obtained for analysis. For each geographic region in SSA, countries were considered based on the availability of data on (i) key anthropometrics and background characteristics including sex, height-for-age z-scores, weight-for-height z-scores, weight-for-age z-scores and anaemia level of children under the age of 5 years and their respective mothers; (ii) household characteristics including the background characteristics of household head and household’s access to basic services such as water, toilet facility and cooking fuel, among others.
Figure 1.
Spatial distribution of the study countries in Sub-Saharan Africa. Source: constructed based on shapefiles from https://tapiquen-sig.jimdofree.com/descargas-gratuitas/mundo/ (1 December 2020) with permission from Carlos Efrain Porto Tapiquen, 2021.
Figure 2.
Spatial distribution of study countries by regions of Sub-Saharan Africa. Source: constructed based on shapefiles from https://tapiquen-sig.jimdofree.com/descargas-gratuitas/mundo/ (1 December 2020) with permission from Carlos Efrain Porto Tapiquen, 2021.
2.2. Data Source, Sampling and Data Collection Procedure
The DHS Program since 1984 has gathered nationally representative data on important population, nutrition and other health indicators of women, men and children at the household level in over 90 low-to-middle-income countries around the world. The program employs standardised protocols and instruments in all its surveys to allow for inter-country comparisons. A two-stage stratified sampling technique involving the demarcation of enumeration areas (clusters) and household selection for interviews was done. Questionnaires are often translated into a country’s major local language, pre-tested and validated before implementation of the surveys. This study included 169,394 child-mother pairs who had complete data for all the variables of interest. We adhered to the strengthening the reporting of observational studies in epidemiology (STROBE) statement for developing this manuscript. The dataset can be accessed freely by download at: https://dhsprogram.com/data/available-datasets.cfm (22 March 2021).
2.3. Measurements
2.3.1. Outcome Variable
The outcome variable TBM was derived from four child malnutrition indicators (stunting, wasting, underweight and anaemia status) and the body mass index (BMI) of their respective mothers. For parsimony and relevance to this study, anaemia levels were measured using four response categories (severe, moderate, mild and not anaemic), which were dichotomized into “anaemic” and “normal”, where anaemic was “severe”, “moderate” and “mild” were combined and coded as “1”, and not anaemic was labelled “normal” and coded “0”. Additionally, following previous studies [13], stunting, wasting, underweight and BMI of the mother were dichotomized and coded as 0 for “normal” and 1 for “stunted”, “wasting”, “underweight” and “obese/overweight”, respectively. Four combinations of these variables—Obese/overweight Mother and Anaemic Child (OM/AC), Obese/overweight Mother and Stunted Child (OM/SC), obese/overweight mother and wasted child (OM/WC), and obese/overweight mother and underweight child (OM/UC)—were made. Following Kumar et al. [2], the binary response variable TBM was measured using response categories “normal” and “TBM”, where the latter included obese/overweight mother with an undernourished child, i.e., children with stunting/wasting/underweight who were also anaemic.
2.3.2. Independent Variables
The independent variables included in this study were considered based on literature and the availability of data. Previous studies [7,13,14,15,16] have documented several variables associated with child malnutrition spanning child, mother and household characteristics and contextual factors. The relevant variables on child characteristics considered include the age of the child in years (0, 1, 2, 3, 4); sex of child (male, female); birth order (1, 2, 3 and above); perceived birth size (larger than average, average, smaller than average, do not know). With regards to the mothers’ characteristics, the relevant variables include the age of mother in years (15–19, 20–24, 25–29, 30–34, 35–49, 40–44, 45–49); educational attainment (no formal, primary, secondary, higher); employment status (no, yes); antenatal care (ANC) visits (no, yes); postnatal care (PNC) visits (No, Yes). The household characteristics considered are the age of household head (“young adults” for those below 35 years, “middle-aged adults” for 35–55 years and “old-aged adults” for those aged 55 years and above [17]; sex of household head (male, female); household size (“small” for those with 1–5 members, “medium” for 6–10 members and “large” for more than 10 members (see [17,18]); wealth status (poor, middle, rich); access to electricity (no, yes); source of drinking water (improved, unimproved [17,18]); type of toilet facility (improved, unimproved [17,18]); and type of cooking fuel (unclean, clean [19,20]). Urbanicity (urban, rural) and geographic region (western Africa, eastern Africa, central Africa and southern Africa) were the contextual variables included in this study.
2.4. Data Analyses
All statistical analyses were performed using the Stata SE version 14.2 (StataCorp, College Station, TX, USA) software. Before analyses were conducted, the data were first declared as survey data using the Stata command “svyset” specifying the cluster, sample weighting and strata variables. This procedure was done to allow for robust estimation of effect sizes by preventing potential clustering and adjusting for oversampling and undersampling. Descriptive statistics (frequencies and percentages) were used to present the distribution of all variables of interest in tables. To enhance visualization and understanding of the study context, the data were then integrated into a geographic information system (GIS) environment and key variables presented in maps. The Chi-square test of independence was then used to assess the associations between the independent variables and the TBM. All independent variables associated with the TBM were tested for multicollinearity and there was no evidence of multicollinearity (see Table S1). The effects of these independent variables on the TBM were then examined by fitting a negative log-log regression to the data. A negative log-log generalized linear regression was deemed plausible considering the skewed distribution of the TBM to the non-affirmation (99%) [19,21,22]. The results were then presented using adjusted odds ratios (aORs) at 95% Confidence Intervals (CIs).
2.5. Ethical Approval
Ethical clearance for DHS reports is taken from the Ethics Committee of ORC Macro Inc. as well as the ethics boards of partner institutions (e.g., ministries of health) of the studied countries. The DHS protocols guarantee that ethical standards for the protection of respondents’ anonymity, privacy and confidentiality are adhered to. Inner City Fund International also ensures that the survey meets the United States Department of Health and Human Services’ regulations for the respect of human subjects. The study used secondary datasets; hence, no further ethical approval was required. The datasets can be accessed freely via download. Further information about the DHS data usage and ethical standards is available at http://goo.gl/ny8T6X (22 March 2021).
3. Results
3.1. Descriptive Analysis on TBM Across Four Geographic Regions in SSA
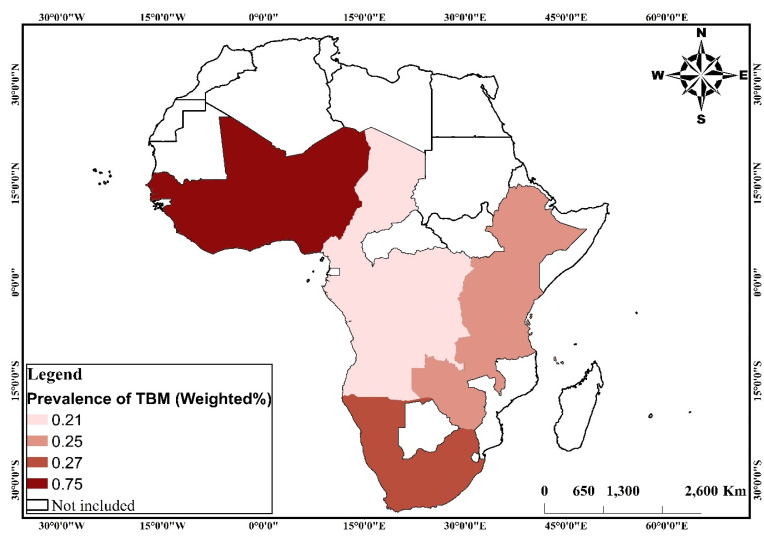
The study included 169,394 children under five from 32 countries in SSA. Variations in sample size for the variables included in this study can be found in Table 1. The highest proportion of children with TBM in the four geographic regions in SSA was found in Western Africa (0.75%) and the lowest in Central Africa (0.21%) (Figure 3). There were variations in the prevalence of TBM across the child, mother, household and contextual factors. Factors that showed significant variations in TBM were the age of the child, sex of the child, birth order, perceived birth size, educational attainment, employment status and ANC. Other statistically significant factors were the age of the household head, sex of household head, household size, wealth status, access to electricity, source of drinking water, type of toilet facility, type of cooking fuel, urbanicity, and geographic region (Table 2).
Table 1.
Distributions of child, mother, household and contextual variables.
| Variable | Weighted n | (%) | Variable | Weighted n | (%) |
|---|---|---|---|---|---|
| OM/WC | Employment status | ||||
| Normal | 166,058 | 98 | No | 59,817 | 37 |
| Wasting | 3335 | 2 | Yes | 100,628 | 63 |
| OM/SC | ANC | ||||
| Normal | 156,387 | 92 | No | 12,262 | 10 |
| Stunting | 13,007 | 8 | Yes | 106,281 | 90 |
| OM/UC | PNC | ||||
| Normal | 162,158 | 96 | No | 63,838 | 59 |
| Underweight | 7236 | 4 | Yes | 45,140 | 41 |
| OM/AC | Household characteristics | ||||
| Normal | 148,790 | 88 | Age of household head | ||
| Anemic | 20,604 | 12 | Young adults | 75,105 | 44 |
| TBM | Middle-aged adults | 73,311 | 43 | ||
| Normal | 168,660 | 99 | Old-aged adults | 20,975 | 12 |
| OM/SC/WC/UC and AC | 734 | 1 | Sex of household head | ||
| Child characteristics | Male | 136,212 | 80 | ||
| Age of child | Female | 33,182 | 20 | ||
| 0 | 34,564 | 20 | Household size | ||
| 1 | 35,793 | 21 | Small | 69,944 | 41 |
| 2 | 33,487 | 20 | Medium | 78,415 | 46 |
| 3 | 33,693 | 20 | Large | 21,035 | 12 |
| 4 | 31,856 | 19 | Wealth status | ||
| Sex of child | Poor | 75,261 | 44 | ||
| Male | 85,523 | 50 | Middle | 33,996 | 20 |
| Female | 83,871 | 50 | Rich | 60,136 | 36 |
| Birth order | Access to electricity | ||||
| 1 | 35,347 | 21 | No | 119,345 | 70 |
| 2 | 81,981 | 48 | Yes | 50,032 | 30 |
| 3 and above | 52,065 | 31 | Source of drinking water | ||
| Perceived birth size | Improved | 109,141 | 64 | ||
| Larger than average | 54,853 | 34 | Unimproved | 60,232 | 36 |
| Average | 78,374 | 49 | Type of toilet facility | ||
| Smaller than average | 24,950 | 16 | Improved | 72,110 | 43 |
| Do not know | 2314 | 1 | Unimproved | 97,246 | 57 |
| Mother characteristics | Type of cooking fuel | ||||
| Age of mother | Unclean | 154,729 | 91 | ||
| 15–19 | 9383 | 6 | Clean | 14,648 | 9 |
| 20–24 | 36,523 | 22 | Contextual | ||
| 25–29 | 47,310 | 28 | Urbanicity | ||
| 30–34 | 36,577 | 22 | Urban | 52,513 | 31 |
| 35–49 | 25,071 | 15 | Rural | 116,881 | 69 |
| 40–44 | 11,200 | 7 | Geographic region | ||
| 45–49 | 3330 | 2 | Western Africa | 63,978 | 38 |
| Educational attainment | Eastern Africa | 69,144 | 41 | ||
| No formal | 67,012 | 40 | Central Africa | 32,899 | 19 |
| Primary | 58,079 | 34 | Southern Africa | 3373 | 2 |
| Secondary | 38,671 | 23 | n | 169,394 | |
| Higher | 5633 | 3 |
NB: Obese/overweight Mother and Anaemic Child = OM/AC; Obese/overweight Mother and Stunted Child = OM/SC, obese/overweight mother and wasted child = OM/WC; obese/overweight mother and underweight child = OM/UC; antenatal care = ANC; postnatal care = PNC.
Figure 3.
Maps showing the prevalence of triple burden of malnutrition in the four geographic regions in Sub-Saharan Africa. Source: constructed based on shapefiles from https://tapiquen-sig.jimdofree.com/descargas-gratuitas/mundo/ (1 December 2020) with permission from Carlos Efrain Porto Tapiquen, 2021. TBM: Triple burden of malnutrition.
Table 2.
Associations between child, mother, household and contextual factors and TBM.
| Variable | TBM (Weighted %) | 95% CIs | p-Value | Variable | TBM (Weighted %) | 95% CIs | p-Value |
|---|---|---|---|---|---|---|---|
| Child characteristics | Household characteristics | ||||||
| Age of child | Age of household head | ||||||
| 0 | 0.26 | 0.21–0.30 | <0.001 | Young adults | 0.37 | 0.32–0.41 | 0.001 |
| 1 | 0.88 | 0.79–0.98 | Middle-aged adults | 0.50 | 0.45–0.55 | ||
| 2 | 0.40 | 0.34–0.48 | Old-aged adults | 0.43 | 0.37–0.55 | ||
| 3 | 0.29 | 0.23–0.35 | Sex of household head | 0.008 | |||
| 4 | 0.30 | 0.24–0.37 | Male | 0.46 | 0.43–0.50 | ||
| Sex of child | Female | 0.31 | 0.26–0.38 | ||||
| Male | 0.56 | 0.51–0.61 | <0.001 | Household size | |||
| Female | 0.31 | 0.27–0.34 | Small | 0.36 | 0.32–0.41 | <0.001 | |
| Birth order | Medium | 0.41 | 0.37–0.46 | ||||
| 1 | 0.31 | 0.25–0.37 | <0.001 | Large | 0.74 | 0.63–0.86 | |
| 2 | 0.39 | 0.34–0.43 | Wealth status | ||||
| 3 and above | 0.59 | 0.53–0.66 | Poor | 0.56 | 0.51–0.62 | <0.001 | |
| Perceived birth size | Middle | 0.42 | 0.36–0.50 | ||||
| Larger than average | 0.27 | 0.22–0.32 | <0.001 | Rich | 0.28 | 0.24–0.32 | |
| Average | 0.47 | 0.42–0.52 | Access to electricity | ||||
| Smaller than average | 0.83 | 0.72–0.95 | No | 0.48 | 0.44–0.53 | <0.001 | |
| Do not know | 0.51 | 0.28–0.90 | Yes | 0.31 | 0.27–0.37 | ||
| Mother characteristics | Source of drinking water | ||||||
| Age of mother | Improved | 0.42 | 0.38–0.46 | 0.038 | |||
| 15–19 | 0.40 | 0.28–0.54 | 0.284 | Unimproved | 0.46 | 0.41–0.52 | |
| 20–24 | 0.33 | 0.28–0.40 | Type of toilet facility | ||||
| 25–29 | 0.42 | 0.36–0.48 | Improved | 0.28 | 0.24–0.32 | <0.001 | |
| 30–34 | 0.46 | 0.39–0.53 | Unimproved | 0.55 | 0.50–0.59 | ||
| 35–49 | 0.55 | 0.46–0.70 | Type of cooking fuel | ||||
| 40–44 | 0.45 | 0.33–0.59 | Unclean | 0.47 | 0.43–0.50 | <0.001 | |
| 45–49 | 0.69 | 0.44–10.3 | Clean | 0.08 | 0.04–0.10 | ||
| Educational attainment | Contextual | ||||||
| No formal | 0.75 | 0.69–0.82 | <0.001 | Urbanicity | |||
| Primary | 0.28 | 0.24–0.33 | Urban | 0.26 | 0.22–0.31 | <0.001 | |
| Secondary | 0.15 | 0.11–0.19 | Rural | 0.51 | 0.47–0.55 | ||
| Higher | 0.20 | 0.10–0.35 | Geographic region | ||||
| Employment status | Western Africa | 0.75 | 0.69–0.82 | <0.001 | |||
| No | 0.51 | 0.45–0.57 | <0.001 | Eastern Africa | 0.25 | 0.22–0.29 | |
| Yes | 0.43 | 0.39–0.47 | Central Africa | 0.21 | 0.16–0.26 | ||
| ANC | Southern Africa | 0.27 | 0.12–0.51 | ||||
| No | 0.91 | 0.75–10.9 | <0.001 | ||||
| Yes | 0.42 | 0.38–0.46 | |||||
| PNC | |||||||
| No | 0.54 | 0.48–0.60 | 0.113 | ||||
| Yes | 0.43 | 0.37–0.50 |
3.2. Multivariate Analysis on the Predictors of TBM
Table 3 shows the results from the negative log-log regression analysis on the predictors of TBM. With the child factors, we found that children aged 1 [aOR = 1.283; 95% CI = 1.215–1.355] and those aged 2 [aOR = 1.133; 95% CI = 1.067–1.204] were more likely to experience TBM compared to those aged 0. TBM was less likely to occur among female children compared to males [aOR = 0.859; 95% CI = 0.824–0.896]. Children whose perceived size at birth was average [aOR = 1.133; 95% CI = 1.076–1.193] and smaller than average [aOR = 1.278; 95% CI = 1.204–1.356] were more likely to suffer from TBM compared to those who were larger than average at birth. In terms of the maternal factors, children born to mothers with primary [aOR = 0.922; 95% CI = 0.865–0.984] and secondary [aOR = 0.829; 95% CI = 0.777–0.885] education were less likely to suffer from TBM compared to those born to mothers with no formal education. Children born to mothers who attended ANC had lower odds of experiencing TBM compared to those born to mothers who did not attend ANC [aOR = 0.969; 95% CI = 0.887–0.998]. With the household factors, children born to mothers who use clean household cooking fuel were less likely to experience TBM compared to children born to mothers who use unclean household cooking fuel [aOR = 0.724; 95% CI = 0.612–0.857]. In terms of the contextual factors, children born to mothers who lived in eastern Africa [aOR = 0.837; 95% CI = 0.789–0.888] and central Africa [aOR = 0.822; 95% CI = 0.768–0.880] had lower odds of suffering from TBM compared to children born to mothers who lived in western Africa.
Table 3.
Negative log-log regression showing relationships between TBM and predictor variables.
| Variable | aOR | Robust SE | p-Value | 95% CIs | |
|---|---|---|---|---|---|
| Child characteristics | |||||
| Age of child (Ref: 0) | |||||
| 1 | 1.283 | 0.036 | <0.001 | 1.215 | 1.355 |
| 2 | 1.133 | 0.035 | <0.001 | 1.067 | 1.204 |
| 3 | 0.996 | 0.043 | 0.928 | 0.916 | 1.084 |
| 4 | 1.013 | 0.051 | 0.792 | 0.918 | 1.118 |
| Sex of child (Ref: male) | |||||
| Female | 0.859 | 0.019 | <0.001 | 0.824 | 0.896 |
| Perceived birth size (Ref: larger than average) | |||||
| Average | 1.133 | 0.030 | <0.001 | 1.076 | 1.193 |
| Smaller than average | 1.278 | 0.039 | <0.001 | 1.204 | 1.356 |
| Do not know | 1.180 | 0.117 | 0.094 | 0.972 | 1.432 |
| Birth order (Ref: 0) | |||||
| 2 | 1.031 | 0.032 | 0.329 | 0.970 | 1.096 |
| 3 and above | 1.062 | 0.037 | 0.084 | 0.992 | 1.136 |
| Mother characteristics | |||||
| Educational attainment (Ref: no formal) | |||||
| Primary | 0.922 | 0.030 | 0.014 | 0.865 | 0.984 |
| Secondary | 0.829 | 0.028 | <0.001 | 0.777 | 0.885 |
| Higher | 0.955 | 0.086 | 0.611 | 0.800 | 1.140 |
| Employment status (Ref: no) | |||||
| Yes | 0.969 | 0.022 | 0.155 | 0.927 | 1.012 |
| ANC (Ref: no) | |||||
| Yes | 0.941 | 0.028 | 0.043 | 0.887 | 0.998 |
| Household characteristics | |||||
| Age of household head (Ref: young adult) | |||||
| Middle-aged adults | 1.020 | 0.026 | 0.451 | 0.969 | 1.073 |
| Old-aged adults | 0.981 | 0.032 | 0.552 | 0.920 | 1.046 |
| Sex of household head (Ref: male) | |||||
| Female | 0.973 | 0.029 | 0.362 | 0.917 | 1.032 |
| Household size (Ref: small) | |||||
| Medium | 0.980 | 0.026 | 0.453 | 0.930 | 1.033 |
| Large | 1.059 | 0.034 | 0.078 | 0.994 | 1.128 |
| Wealth status (Ref: poor) | |||||
| Middle | 0.978 | 0.026 | 0.415 | 0.928 | 1.031 |
| Rich | 0.958 | 0.030 | 0.170 | 0.901 | 1.018 |
| Source of drinking water (Ref: improved) | |||||
| Unimproved | 0.985 | 0.021 | 0.472 | 0.945 | 1.027 |
| Type of toilet facility (Ref: improved) | |||||
| Unimproved | 1.052 | 0.030 | 0.077 | 0.994 | 1.113 |
| Type of Cooking fuel (Ref: unclean) | |||||
| Clean | 0.724 | 0.062 | <0.001 | 0.612 | 0.857 |
| Access to electricity (Ref: no) | |||||
| Yes | 0.992 | 0.031 | 0.785 | 0.932 | 1.054 |
| Contextual factors | |||||
| Urbanicity (Ref: urban) | |||||
| Rural | 1.035 | 0.033 | 0.283 | 0.972 | 1.102 |
| Geographic region (Ref: western Africa) | |||||
| Eastern Africa | 0.837 | 0.025 | <0.001 | 0.789 | 0.888 |
| Central Africa | 0.822 | 0.028 | <0.001 | 0.768 | 0.880 |
| Southern Africa | 0.859 | 0.080 | 0.103 | 0.715 | 1.031 |
4. Discussion
This study examined the prevalence and factors associated with TBM in SSA. At the regional level, Western Africa recorded the highest prevalence of TBM, whereas Central Africa had the lowest prevalence. Additionally, our analysis indicates that children born to mothers who lived in Eastern Africa and Central Africa had lower odds of suffering from TBM compared to children born to mothers who lived in Western Africa. The result is consistent with an earlier study by Akombi et al. [14] that found a high prevalence of wasting and underweight in Western Africa compared to Central Africa. Plausibly, the high prevalence of TBM in Western Africa may be linked to the low rates of exclusive breastfeeding and vaccination for children when compared to Eastern Africa or Central Africa [23,24,25]. For example, Yourkavitch et al. [25] observed from their study that exclusive breastfeeding and vaccination for children were significantly low in Western Africa, and this is further exacerbated by the high levels of stunting in the region. Hence, this may explain the high prevalence of TBM observed with respect to Western Africa. Other studies attribute the high prevalence of TBM in Western Africa to the effects of rapid desertification on food access, availability and production, consequently leading to poor nutritional outcomes for children under five [17,26]. It is also worthy of note that policy differences, as well as other commitments towards addressing malnutrition, could account for sub-regional variations in the prevalence of TBM. For instance, [27] indicate that three out of 16 countries in Western Africa, two out of five in Southern Africa, four out of nine in Central Africa and seven out of 18 in Eastern Africa have multisectoral comprehensive nutrition plans.
Our study also shows that there is a combination of child-related, maternal-related, household and context level factors that were significantly associated with TBM in SSA. Concerning the child-related factors, the analysis showed that the age of the child, sex of the child, birth order and perceived birth size were significantly associated with TBM. Children older than age zero were more likely to experience TBM. This result is substantiated by a recent study from Nepal [2] that found higher child age to be significantly associated with higher risks of TBM. Extant studies have shown that childhood anaemia, faltering growth, stunting, wasting and underweight are more profound in children after age zero [28,29], hence explaining the higher odds of TBM among children aged 1 or 2 as compared to those aged zero.
Consistent with a previous study by Kumar et al. [2], we found that TBM was more likely to occur among children whose perceived size at birth was average or smaller than average. This finding is not surprising given that stunting, underweight, wasting and childhood anaemia are significantly associated with low size at birth [15,30]. In addition, children with low size at birth tend to lack sufficient amounts of nutrients necessary to promote their growth [2]. Hence, such children are more likely to suffer TBM. Contrary to a related study in Nepal [12] that found no significant association between sex of a child and TBM, our study revealed that there was a significant association, with female children having a reduced risk of TBM compared to the males. This can be explained from the perspective of the evolutionary theory that posits that the differences in the genetic composition of males and females (also known as selective male mortality) account for the higher risk of TBM among males compared to female children [31,32,33].
Maternal educational attainment and ANC attendance were the only maternal factors that were significantly associated with TBM among children under five. Compared to children born to mothers with no formal education, those born to mothers with primary and secondary education were less likely to suffer from TBM. Likewise, the odds of TBM were significantly lower among children born to mothers who attended ANC compared to those born to mothers who did not attend ANC. What these findings imply is that maternal education and ANC are strong protective factors to control TBM. The results are congruent to reports from elsewhere [12]. A possible justification for this finding could be that, during ANC, mothers are provided with micronutrient supplementation and fortification such as the folic acid that promotes the health of the mother while meeting the nutritional needs of the child [34], hence reducing the risk of TBM. Furthermore, higher maternal education increases women’s decision-making capacity and also empowers mothers by equipping them with the relevant knowledge concerning the nutritional needs of children [35].
Concerning the household factors, cooking fuel was the only factor that was significantly associated with TBM. Children born to mothers who use clean household cooking fuel were less likely to experience TBM compared to children born to mothers who use unclean household cooking fuel. Similar findings have been reported by Amadu et al. [13] that showed that unclean cooking fuel exacerbated the risk of stunting, wasting and underweight. Available evidence suggests that the use of unclean cooking fuel worsens household air pollution, which can operate through other pathways to impair growth in children and subsequently lead to TBM [36,37]. Therefore, the current findings emphasise the need for sub-Saharan African countries to invest in clean cooking fuel.
4.1. Strengths and Limitations
The strength of this study lies in the robust analytical and statistical methods used. This enhances the trustworthiness of our findings. Additionally, we provide a detailed methodological procedure, hence making our study replicable. The use of a nationally representative dataset makes the findings of this study generalisable to all children under five in SSA. Our findings make a significant contribution to knowledge by being the first to investigate the factors associated with TBM within the sub-Saharan African context. As such, it will set the pace for more research to be done in this regard. Nevertheless, our study has some noteworthy limitations; therefore, an interpretation of the findings should be done with caution.
Given that the DHS dataset employed a cross-sectional design, we cannot establish causality between the various factors (i.e., child-related, maternal, household and contextual factors) and TBM. Additionally, since questions on TBM were self-reported, there could be some recall bias, which is beyond the control of the team. The pooling of the data may be affected by heterogeneity across regions.
4.2. Practical Implications
Not only does our findings contribute to bridging the knowledge gap on TBM in SSA, it also has considerable implications for policy and practice. From our study, it is evident that modifiable maternal and household factors such as maternal education, ANC attendance and use of clean cooking fuel significantly lower the risk of TBM. Therefore, if the sub-region is to attain SDG 2.2 (ending all forms of malnutrition by 2030) and SDG 3.2, then the individual countries should strengthen policies on female education. Additionally, the current findings highlight the essentiality of investing in clean cooking fuel (e.g., electricity, gas, ethanol, solar) for sub-Saharan African countries. Again, the contextual variation indicates that Western Africa must put in serious effort to combat TBM. Free maternal healthcare policies, as seen in the case of Ghana, should be exemplified in other western African countries to achieve the desired reduction in TBM.
5. Conclusions
This study aimed to examine the prevalence and factors associated with TBM in SSA. We conclude that the prevalence of TBM is higher in Western Africa than in any other region. Additionally, the study revealed that a combination of child-related, maternal, household and contextual factors were associated with TBM. Essentially, higher maternal education, ANC attendance and use of clean cooking fuel were protective factors against TBM, whereas higher child age, low size at birth and being a male child increased the risk of TBM. Given the regional variations in the prevalence and risk of TBM, region-specific interventions must be initiated to ensure the likelihood of those interventions being successful at reducing the risk of TBM. Countries in Western Africa in particular would have to strengthen their current policies and programmes on malnutrition and to enhance their attainment of the SDGs.
Abbreviations
| SSA | Sub-Saharan Africa |
| TBM | Triple burden of malnutrition |
| DBM | Double burden of malnutrition |
| ANC | Antenatal care visits |
| PNC | Postnatal care visits |
| SDGs | Sustainable Development Goals |
| DHS | Demographic and Health Surveys |
| OM/AC | Obese/overweight mother and anaemic child |
| OM/SC | Obese/overweight mother and stunted child |
| OM/WC | Obese/overweight mother and wasted child |
| OM/UC | Obese/overweight mother and underweight child |
| STROBE | Strengthening the reporting of observational studies in epidemiology |
| aOR | Adjusted odds ratios |
| OR | Odds ratio |
| CI | Confidence intervals |
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/nu13062050/s1, Table S1: Test of Multicollinearity between All Independent Variables and TBM.
Author Contributions
B.O.A. and I.A. developed the study concept and performed the data analysis. B.O.A., I.A., A.-A.S., J.O., E.D., J.E.H.J., E.B., A.G.A. and S.Y. drafted and revised the manuscript for its intellectual content. All authors have read and agreed to the published version of the manuscript.
Funding
The authors sincerely thank Bielefeld University, Germany for providing financial support through the Institutional Open Access Publication Fund for the article processing charge.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Ethical clearance for DHS reports is taken from the Ethics Committee of ORC Macro Inc. as well as the ethics boards of partner institutions (e.g., ministries of health) of the studied countries. The DHS protocols guarantee that ethical standards for the protection of respondents’ anonymity, privacy and confidentiality are adhered to. Inner City Fund International also ensures that the survey meets the United States Department of Health and Human Services’ regulations for the respect of human subjects. The study used secondary datasets; hence, no further ethical approval was required. The datasets can be accessed freely via download. Further information about the DHS data usage and ethical standards is available at http://goo.gl/ny8T6X (22 March 2021).
Data Availability Statement
The dataset is available on the following website: http://goo.gl/ny8T6X (22 March 2021).
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.United Nations . Sustainable Development Goals. United Nations; New York, NY, USA: 2015. [Google Scholar]
- 2.Kumar P., Chauhan S., Patel R., Srivastava S., Bansod D.W. Prevalence and factors associated with triple burden of malnutrition among mother-child pairs in India: A study based on National Family Health Survey 2015–16. BMC Public Health. 2021;21:1–2. doi: 10.1186/s12889-021-10411-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel R., Srivastava S., Kumar P., Chauhan S. Factors associated with double burden of malnutrition among mother-child pairs in India: A study based on National Family Health Survey 2015–16. Child. Youth Serv. Rev. 2020;1:105256. doi: 10.1016/j.childyouth.2020.105256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Food and Agriculture Organisation The State Of Food Security And Nutrition In The World. Rome: Building Resilience for Peace and Food Security. [(accessed on 7 June 2021)]; Available online: http://www.fao.org/3/I7695e/I7695e.pdf.
- 5.Pal A., Pari A.K., Sinha A., Dhara P.C. Prevalence of undernutrition and associated factors: A cross-sectional study among rural adolescents in West Bengal, India. Int. J. Pediatrics Adolesc. Med. 2017;4:9–18. doi: 10.1016/j.ijpam.2016.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Biswas T., Townsend N., Magalhaes R.S., Islam M.S., Hasan M.M., Mamun A. Current progress and future directions in the double burden of malnutrition among women in South and Southeast Asian countries. Curr. Dev. Nutr. 2019;3:nzz026. doi: 10.1093/cdn/nzz026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bain L.E., Awah P.K., Geraldine N., Kindong N.P., Siga Y., Bernard N., Tanjeko A.T. Malnutrition in Sub–Saharan Africa: Burden, causes and prospects. Pan Afr. Med J. 2013;15:1–8. doi: 10.11604/pamj.2013.15.120.2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meenakshi J.V. Trends and patterns in the triple burden of malnutrition in India. Agric. Econ. 2016;47:115–134. doi: 10.1111/agec.12304. [DOI] [Google Scholar]
- 9.Kulkarni V.S., Kulkarni V.S., Gaiha R. “Double Burden of Malnutrition” Reexamining the Coexistence of Undernutrition and Overweight Among Women in India. Int. J. Health Serv. 2017;47:108–133. doi: 10.1177/0020731416664666. [DOI] [PubMed] [Google Scholar]
- 10.Mondal N., Basumatary B., Kropi J., Bose K. Prevalence of double burden of malnutrition among urban school going Bodo children aged 5-11 years of Assam, Northeast India. Epidemiol. Biostat. Public Health. 2015;12 [Google Scholar]
- 11.Davis J.N., Oaks B.M., Engle-Stone R. The Double Burden of Malnutrition: A Systematic Review of Operational Definitions. Curr. Dev. Nutr. 2020;4:nzaa127. doi: 10.1093/cdn/nzaa127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sunuwar D.R., Singh D.R., Pradhan P.M. Prevalence and factors associated with double and triple burden of malnutrition among mothers and children in Nepal: Evidence from 2016 Nepal Demographic and Health Survey. BMC Public Health. 2020;20:1–11. doi: 10.1186/s12889-020-8356-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amadu I., Seidu A.A., Duku E., Okyere J., Hagan J.E., Hormenu T., Ahinkorah B.O. The Joint Effect of Maternal Marital Status and Type of Household Cooking Fuel on Child Nutritional Status in Sub-Saharan Africa: Analysis of Cross-Sectional Surveys on Children from 31 Countries. Nutrients. 2021;13:1541. doi: 10.3390/nu13051541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akombi B.J., Agho K.E., Merom D., Renzaho A.M., Hall J.J. Child malnutrition in sub-Saharan Africa: A meta-analysis of demographic and health surveys (2006–2016) PLoS ONE. 2017;12:e0177338. doi: 10.1371/journal.pone.0177338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akombi B.J., Agho K.E., Hall J.J., Wali N., Renzaho A., Merom D. Stunting, wasting and underweight in sub-Saharan Africa: A systematic review. Int. J. Environ. Res. Public Health. 2017;14:863. doi: 10.3390/ijerph14080863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akombi B.J., Chitekwe S., Sahle B.W., Renzaho A. Estimating the double burden of malnutrition among 595,975 children in 65 low-and middle-income countries: A meta-analysis of demographic and health surveys. Int. J. Environ. Res. Public Health. 2019;16:2886. doi: 10.3390/ijerph16162886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Armah F.A., Ekumah B., Yawson D.O., Odoi J.O., Afitiri A.R., Nyieku F.E. Access to improved water and sanitation in sub-Saharan Africa in a quarter century. Heliyon. 2018;4:e00931. doi: 10.1016/j.heliyon.2018.e00931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Afitiri A.R., Armah F.A., Ekumah B., Nyieku F.E., Yawson D.O., Odoi J.O. Cumulative effects of environmental factors on household childhood diarrhoea in Ghana. Water Pract. Technol. 2020;15:1032–1049. doi: 10.2166/wpt.2020.083. [DOI] [Google Scholar]
- 19.Armah F.A., Ekumah B., Yawson D.O., Odoi J.O., Afitiri A.R., Nyieku F.E. Predictive probabilities of access to clean cooking: Evidence from the demographic and health surveys in 31 countries in sub-saharan Africa. Environ. Justice. 2019;12:118–131. doi: 10.1089/env.2019.0002. [DOI] [Google Scholar]
- 20.Amegah A.K., Boachie J., Näyhä S., Jaakkola J.J. Association of biomass fuel use with reduced body weight of adult Ghanaian women. J. Expo. Sci. Environ. Epidemiol. 2020;30:670–679. doi: 10.1038/s41370-019-0129-2. [DOI] [PubMed] [Google Scholar]
- 21.Aitkin M.A., Aitkin M., Francis B., Hinde J. Statistical Modelling in GLIM 4. OUP; Oxford, UK: 2005. [Google Scholar]
- 22.Fahrmeir L., Tutz G. Multivariate Statistical Modelling Based on Generalized Linear Models. Springer Science & Business Media; New York, NY, USA: 2013. [Google Scholar]
- 23.Amugsi D.A., Dimbuene Z.T., Kyobutungi C. Correlates of the double burden of malnutrition among women: An analysis of cross sectional survey data from sub-Saharan Africa. BMJ Open. 2019;9:e029545. doi: 10.1136/bmjopen-2019-029545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sámano R., Martínez-Rojano H., Martínez E.G., Jiménez B.S., Rodríguez G.P., Zamora J.P., Casanueva E. Effects of breastfeeding on weight loss and recovery of pregestational weight in adolescent and adult mothers. Food Nutr. Bull. 2013;34:123–130. doi: 10.1177/156482651303400201. [DOI] [PubMed] [Google Scholar]
- 25.Yourkavitch J., Burgert-Brucker C., Assaf S., Delgado S. Using geographical analysis to identify child health inequality in sub-Saharan Africa. PLoS ONE. 2018;13:e0201870. doi: 10.1371/journal.pone.0201870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hollinger F., Staatz J.M. Market and Policy Drivers. FAO, African Development Bank, ECOWAS; Rome, Italy: 2015. Agricultural Growth in West Africa. Pobrano październik. [Google Scholar]
- 27.Development Initiatives Poverty Research Ltd. Country Nutrition Profiles. [(accessed on 6 June 2021)];2020 Available online: https://globalnutritionreport.org/resources/nutrition-profiles/africa/
- 28.Behera S., Bulliyya G. Magnitude of anemia and hematological predictors among children under 12 years in Odisha, India. Anemia. 2016;2016 doi: 10.1155/2016/1729147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Headey D., Menon P., Nguyen P. The Timing of Growth Faltering in India Has Changed Significantly over 1992–2016, with Variations in Prenatal and Postnatal Improvement (P10-005-19) Curr. Dev. Nutr. 2019;3(Suppl.1):nzz034-P10. doi: 10.1093/cdn/nzz034.P10-005-19. [DOI] [Google Scholar]
- 30.Manggala A.K., Kenwa K.W., Kenwa M.M., Jaya A.A., Sawitri A.A. Risk factors of stunting in children aged 24–59 months. Paediatr. Indones. 2018;58:205–212. doi: 10.14238/pi58.5.2018.205-12. [DOI] [Google Scholar]
- 31.Sultana M., Sarker A.R., Sheikh N., Akram R., Ali N., Mahumud R.A., Alam N.H. Prevalence, determinants and health care-seeking behavior of childhood acute respiratory tract infections in Bangladesh. PLoS ONE. 2019;14:e0210433. doi: 10.1371/journal.pone.0210433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Trivers R.L., Willard D.E. Natural selection of parental ability to vary the sex ratio of offspring. Science. 1973;179:90–92. doi: 10.1126/science.179.4068.90. [DOI] [PubMed] [Google Scholar]
- 33.Wamani H., Åstrøm A.N., Peterson S., Tumwine J.K., Tylleskär T. Boys are more stunted than girls in sub-Saharan Africa: A meta-analysis of 16 demographic and health surveys. BMC Pediatrics. 2007;7:1–10. doi: 10.1186/1471-2431-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sandersa D., Hendricksb M., Krollc F., Puoaned T., Ramokoloe V., Swartf R., Tsolekileg L. The triple burden of malnutrition in childhood: Causes, policy implementation and recommendations. Child Adolesc. Health. 2019:145. [Google Scholar]
- 35.Singh K., Bloom S., Brodish P. Gender equality as a means to improve maternal and child health in Africa. Health Care Women Int. 2015;36:57–69. doi: 10.1080/07399332.2013.824971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Islam S., Rana M.J., Mohanty S.K. Cooking, smoking, and stunting: Effects of household air pollution sources on childhood growth in India. Indoor Air. 2021;31:229–249. doi: 10.1111/ina.12730. [DOI] [PubMed] [Google Scholar]
- 37.Upadhyay A.K., Singh A., Kumar K., Singh A. Impact of indoor air pollution from the use of solid fuels on the incidence of life threatening respiratory illnesses in children in India. BMC Public Health. 2015;15:1–9. doi: 10.1186/s12889-015-1631-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset is available on the following website: http://goo.gl/ny8T6X (22 March 2021).