Abstract
Purpose
The immediate application of a dentin-bonding agent after tooth preparation and before impression-taking (immediate dentin sealing [IDS]) has been suggested to provide several advantages concerning bacterial microleakage, hypersensitivity, and bonding quality. We reviewed the literature and clarified certain aspects related to each step of IDS application.
Materials and Methods
The search strategy comprised an electronic research in MEDLINE, Cochrane, Ovid and Scopus for studies published from January 1990 to December 2020 regarding the IDS technique and including both in vitro and clinical studies.
Results
After exclusion of irrelevant or duplicate articles, 88 articles focusing on aspects of the IDS technique were assessed. IDS seems to be advantageous with regard to bond strength, gap formation, bacterial microleakage, and dentin hypersensitivity. However, issues arising from interaction with impression materials, the provisional phase, and conditioning methods before cementation require further investigation.
Conclusion
There are no documented reasons preventing clinicians applying IDS in their everyday practice. On the contrary, the presented technique seems to be beneficial in certain aspects regarding indirect restorations.
Keywords: IDS, indirect restorations, restorative dentistry, review
Introduction
Indirect restorations (even if they are more expensive and time-consuming compared with direct restorations) provide reduced polymerization shrinkage;1 better esthetic, physical, and mechanical properties by post-curing the restoration with light/heat; ideal occlusal morphology; interproximal contacts and wear compatibility with opposing teeth.1,2 Indirect restorations can also aid the restoration of deep preparations with gingival margins located in dentin.3
Restorative dentistry is opposed to the wastage of tooth tissue. Hence, minimally invasive restorations such as inlays, onlays, and laminate veneers are employed. However, regardless of the amount of tooth substance removed, exposure of dentin tubules is inevitable.4 Given the inadequate sealing provided by interim cementation materials, exposed dentin is confronted with bacterial microleakage, as well as chemical and mechanical stimuli transmitted during impression-taking, rinsing, drying, function, and removal of provisional materials.5
To counterbalance the above-mentioned issues and prevent potential pulp damage, the immediate application of a dentin-bonding agent (DBA) after tooth preparation and before impression-taking was introduced in the early-1990s by Pashley et al.6 This method, which is also referred to as “prehybridization”, “dual bonding technique”, and “resin coating technique”, was established with the term “immediate dentin sealing” (IDS).7 In conventional procedures, sealing of the dentin tubules takes place at the bonding stage of the final restoration (delayed dentin sealing [DDS]).8 Thus, during provisionalization, exposed dentin leaves a potential pathway for bacterial infiltration. Conversely, in the IDS technique, dentin adhesives are applied before the provisional phase, which presents benefits with regard to bacterial microleakage, dentin hypersensitivity, gap formation, and bond strength.9
Because articles elaborating all aspects regarding IDS and providing a unanimous protocol are lacking,10 in this study we reviewed the literature and clarified certain clinical procedures related to each step of IDS application.
Materials and Methods
We searched for evidence-based research articles on IDS published from January 1990 until December 2020 using MEDLINE, Cochrane, Ovid and Scopus databases. After initial screening of the literature, the terms “immediate dentin sealing”, “dual bonding technique”, “resin coating technique”, and “prehybridization” were used as key words. Supplementary manual research was also conducted.
Peer-reviewed articles, articles written in English, and articles regarding the IDS technique in human, permanent teeth were the inclusion criteria. Articles not written in English, duplicates, and articles not focusing on aspects of the IDS technique or in vitro studies including primary or bovine teeth were excluded from further evaluation.
The search identified 26.222 articles. After a gradual screening of titles, abstracts, and full texts, all articles were evaluated independently by two reviewers (T.S. and D.P.) for their appropriateness. Discrepancies between the two reviewers were discussed until consensus was reached.
Results
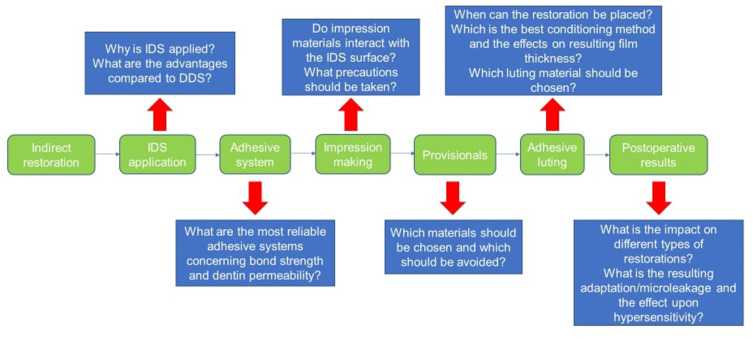
After exclusion of irrelevant or duplicated articles, 88 articles were included in this review. Information regarding the type of study, study design, and main findings are depicted in Table 1. For better understanding and segmentation of the available literature, we divided the articles and presented the information in accordance with the chronological steps of the technique and corresponding clinical appointments (Figure 1).
Table 1.
Characteristics of Articles Included in the Present Review in Publication Order
| Authors and Year of Publication | Type of Study | Tested Parameters | Study Design | Main Findings |
|---|---|---|---|---|
| Pashley et al 19926 | In vitro | Dentin permeability | Tested the sealing ability of 6 DBAs (Prisma Universal Bond 2, Scotchbond 2, Superbond C&B, Amalgam Bond, Gluma, Clearfil PhotoBond) in crown preparations. | Application of a DBA seems a simple procedure to protect the pulp from microleakage. |
| Paul et al 199712 | Case report | Technique presentation | - | - |
| Nikaido et al 2003136 | In vitro | Bond strength | Compared μTBS of a single-step DBA (RZ-II) in direct and indirect use. | RZ-II proved to be a useful resin coating material for crown preparation. |
| Jayasooriya et al 200331 | In vitro | Βond strength | Evaluated the effect of a DBA (Clearfil SE Bond/Single Bond) with/without an LVR (Protect liner F) on μTBS of a resin cement (Panavia F) to dentin in indirect composite restorations and compared it with direct restorations. | Addition of an LVR significantly improved μTBS in indirect restorations but direct restorations performed better. |
| Magne et al 20059 | In vitro | Βond strength | Compared IDS and DDS techniques using a three-step etch-and-rinse DBA (Optibond FL). | IDS had a superior μTBS compared with that of DDS, and reached that obtained using a direct restoration. |
| Magne 200511 | Review | – | Presented the technical details and clinical advantages of IDS. | IDS improved the bond strength, reduced bacterial infiltration and hypersensitivity, and has a positive impact on preservation of dental tissues, patient comfort, and restoration survival. |
| Stavridakis et al 200556 | In vitro | DBA thickness | Investigated the thickness of two three-step-total-etch DBAs (Optibond FL, Syntac Classic) and the effect of two conditioning methods (APA with aluminum oxide, prophy paste with a rotary brush) on it. | Film thickness was dependent on the material and location. |
| Islam et al 2006117 | In vitro | Bond strength | Evaluated μTBS of a resin cement (Chemiace II) to resin-coated dentin using a single-step coating material (Hybrid Bond) on teeth prepared for indirect composite crowns. | Hybrid Bond significantly improved μTBS of Chemiace II to dentin in indirect composite crowns. |
| Maruoka et al 200696 | In vitro | Microleakage | Evaluated coronal leakage of endodontically treated incisors sealed with Clearfil SE Bond + Protect Liner F or RZII. | Both coatings reduced dye penetration but Clearfil SE Bond + Protect Liner F eliminated it completely. |
| Frankenberger et al 200746 | In vitro | Bond strength | Evaluated μTBS of class-I composite inlays luted with different adhesives (XP Bond/Syntac/Optibond FL), temporary cements, cleaning methods (scaler, air polishing with Prophypearls/ClinPro powder) and curing modes. | Dentin contamination with interim cement negatively influenced the bond quality. IDS increased the internal bond strength of all adhesives tested. |
| De Andrade et al 200798 | In vitro | Marginal adaptation/bond strength | Evaluated marginal adaptation and bond strength of composite indirect restorations bonded with dual-cure resin cement (RelyX ARC) after sealing dentin with a DBA (Sigle Bond) associated or not with an LVR (Protect Liner F) | Previous sealing of dentin with a DBA, followed by a second application just before the cementation, is an effective technique for maintaining marginal adaptation and bond strength. |
| Magne et al 200719 | In vitro | Βond strength | Tested μTBS after IDS application (Optibond FL/SE Bond) at 2, 7 and 12 weeks of delay until restoration placement. | No influence upon bond strength by ≤12 weeks of elapsed time before definitive restoration placement. |
| Udo et al 200732 | In vitro | Βond strength | Tested the μTBS of different combinations of sealing materials (Clearfil SE Bond + Protect Liner F/Clearfil Flow FX) and resin cements (Panavia F2.0, Clearfil DC Core Automix). | Use of materials with high ultimate tensile strength in the resin coating and cementation led to enhanced bond strength between them. |
| Okuda et al 200767 | In vitro | Βond strength | Evaluated the effect of a DBA (Clearfil Protect Bond) with/without an LVR (Protect Liner F) on μTBS in indirect composite restorations and compared it with direct restorations. | Addition of an LVR improved the bond strength but direct restorations continued to perform better. |
| Ariyoshi et al 200868 | In vitro | Bond strength | Evaluated the effect of resin coating (Clearfil SE Bond/Clearfil SE Bond+ Clearfil Flow FX) on μTBS of composite cores to pulpal floor dentin. | Resin coating enhanced the dentin bond strength of indirect composite cores to pulpal floor dentin and Clearfil SE Bond+ Clearfil Flow FX group exhibited the highest μTBS values. |
| Santoz-Daroz et al 200866 | In vitro | Bond strength | Investigated μTBS of a resin cement (Panavia F) to dentin after application of seven DBAs (AdheSE, Clearfil Protect Bond, One-Up Bond F, Single Bond, Tyrian SPE/One-step Plus, Xeno III, Unifil Bond) with/without an LVR (Protect Liner F). | The bond strength of the resin cement to dentin was enhanced if an LVR was applied over the DBA. |
| Schenke et al 200897 | In vitro | Marginal integrity | Investigated the marginal integrity of partial ceramic crowns bonded using IDS (Excite + Tetric Flow/Clearfil Se Bond + Protect Liner F/Syntac Classic + Tetric Flow) or DDS and compared the results with marginal sealing provided by self-adhesive cement (RelyX Unicem). | Among IDS and DDS groups, the former yielded better marginal integrity. However, RelyX Unicem had the lowest microleakage. |
| Terry et al 2009137 | Review | - | Technique presentation | - |
| Duarte et al 20093 | In vitro | Microleakage, Βond strength | Compared the effect of total-etch (Adper Single Bond) and self-etch (Adper Prompt L-Pop) DBAs on bond strength and microleakage of an inlay composite restoration. | Both DBAs favored IDS with regard to bond strength but did not influence microleakage. |
| Dillenburg et al 200948 | In vitro | Βond strength, Conditioning method | Evaluated different conditioning methods (APA with aluminum oxide, 37% phosphoric acid, combination of both) applied on two-step etch-and-rinse DBAs (Adper Single Bond 2, Prime&Bond NT) contaminated by interim cement. | IDS could improve the bond strength if its surface was conditioned with APA aluminum oxide + 37% phosphoric acid and a second layer of DBA was applied afterwards. |
| Magne and Nielsen 200927 | In vitro | Interaction with impression materials | Investigated the interactions between impression materials (Impregum soft, Extrude) and DBAs (Optibond FL, Clearfil SE Bond) used for IDS. | Polyether was contraindicated for impression-taking. Polyvinylsiloxane was recommended only after air-blocking and pumicing of the IDS surface. |
| Lee and Park 2009138 | In vitro | Bond strength | Evaluated the effect of IDS (AdheSE), thinning of the DBA by air-blowing before cementation, and light-curing the DBA before cementation on the bond strength of resin inlays. | A combination of the three variables tested improved the bond strength. |
| Hu and Zhu 2010103 | Split-mouth clinical study | Hypersensitivity | Assessed the sensitivity perceived by 25 male patients 1 week as well as 1, 6, 12 and 24 months after cementation of a three-unit fixed restoration. | Post-cementation hypersensitivity was reduced significantly after IDS application. |
| Choi and Cho 2010116 | In vitro | Βond strength | Evaluated the differences in shear bond strength to dentin using IDS (Clearfil SE Bond, Adapter Single Bond 2) compared with DDS. | IDS with Clearfil SE Bond yielded superior shear bond strength compared with that obtained with DDS. |
| Magne et al 2011139 | In vitro | Fatigue strength | Evaluated the fatigue strength of compromised molars restored with CAD/CAM composite resin inlays/onlays (Paradigm MZ100) with/without fiber-reinforced IDS (Ribbond) | There was no benefit of using fiber reinforcement under molars with a compromised cusp. Cusp-protecting onlay was the best solution. |
| Helvey 20117 | Review | – | Evaluated the development of bonding materials and techniques. | Combining different bonding techniques led to IDS creation. |
| Kitayama et al 201195 | In vitro | Microleakage | Investigated the effect of a DBA (Clearfil Protect Bond) + LVR (Clearfil Majesty Flow) and occlusal loading on microleakage of a CAD/CAM ceramic restoration cemented with resin cement (Clearfil Esthetic Cement). | Resin coating reduced microleakage. |
| Magne et al 201170 | In vitro | Bond strength | Evaluated the effect of different opaque resin applications (IDS alone-Optibond FL)/IDS + opaque/IDS mixed with opaque) on bond strength. | An opaque resin for masking discolored resin reduced the bond strength. |
| Medina et al 201299 | In vitro | Marginal adaptation | Evaluated the effect of different material combinations used in the resin coating technique (Single Bond 2/Sigle Bond 2+Scotch Bond Multi-Purpose/Sigle Bond 2+Filtek Flow/Scotch Bond Multi-Purpose/Clearfil S3/Clearfil S3+Bond Clearfil SE Bond/Clearfil S3+Protect Liner F/Clearfil SE Bond+ Protect Liner F) on the marginal adaptation of indirect restorations with gingival margins in enamel and cement. | The most appropriate resin coating combinations were the groups that used a liner. |
| Rocca et al 2012133 | Clinical technique | - | - | Reinforcement of an endodontically treated tooth by incorporating a fiber-reinforced composite (FRC) layer into the resin coating of the tooth preparation, allows the use of FRCs in combination with any kind of restorative material for an adhesive overlay/endocrown. |
| Sahin et al 20125 | In vitro | Dentin permeability | Tested dentin permeability after IDS application with five DBAs (Single Bond 2, Adper Prompt L-Pop, Clearfil Protect Bond, Clearfil S3 Bond, G-Bond) and a dentin desensitizer (Gluma). | Only one-step self-etch G-Bond and two-step self-etch Clearfil Protect Bond provided more effective sealing than the original smear layer. |
| Schoenbaum et al 201235 | Clinical technique | Provisionalization | - | Provisionalization involving silicone and separating medium was efficacious for ≤6 weeks. |
| Sailer et al 201245 | In vitro | Βond strength | Evaluated the effect of a dentin desensitizer (Gluma) and three DBAs (Syntac, Clearfil SE Bond, ED Primer) on the bond strength of dentin cemented with a shelf-adhesive resin cement (RelyX Unicem) and two conventional resin cements (variolink II, Panavia 21). | Resin sealing of dentin had a beneficial effect on the shear bond strength of the self-adhesive resin cement tested. |
| Dalby et al 201273 | In vitro | Βond strength | Investigated the effect of IDS with four DBAs (Optibond FL, One Coat Bond, Single Bond, Go!) on the shear bond strength of ceramic restorations luted with a self-adhesive resin cement (RelyX Unicem). | IDS did not influence the shear bond strength of the restoration luted with RelyX Unicem. |
| Bruzi et al 201330 | In vitro | Interaction with impression materials | Investigated the interactions between DBAs used for IDS (Optibond FL, Scotchbond Universal, Optibond XTR, Filtek LS) and impression materials (Express STD, Impregum F). | Interactions were not observed if a liner was applied over the DBA. |
| Spohr et al 201357 | In vitro | Film thickness | Evaluated the thickness of the material used for IDS (Clearfil SE Bond, Clearfil SE Bond + Protect Liner F) on full-crown preparations and its influence on the fracture load of the restorations. | Film thickness was dependent upon the position under the crown and may increase the fracture load of the restoration. |
| Perugia et al 2013140 | Case report | – | Used IDS in indirect restorations of dental fractures in children. | IDS protected the pulp from bacterial infiltration and formed a hybrid layer that had excellent adhesive properties. |
| Medina et al 2014100 | In vitro | Nanoleakage | Evaluated the nanoleakage patterns in indirect composite restorations bonded to dentin using different combinations of resin coating materials (Single Bond 2+ Scotch Bond Multi-Purpose/Single Bond 2+ Filtek Flow/Clearfil S3/Clearfil S3 +Protect Liner/Clearfil SE Bond+ Protect Liner), after thermal and load cycling. | The combination of a two-step self-etch DBA with an LVR presented a superior behavior and revealed less nanoleakage compared to the other groups. |
| Magne 201418 | IAAD Working Instructions | - | - | - |
| Ghiggi et al 201428 | In vitro | Interaction with impression materials | Evaluated the interactions between the materials used for IDS (Clearfil SE Bond, Clearfil SE Bond + Protect Liner F) and impression materials (Express XT, Impregum) as well as the effect of additional polymerization with glycerin jelly and treatment with alcohol. | Application of glycerin jelly and alcohol prevented the interaction of Clearfil CE Bond with Express XT and Protect Liner F with Impregum; however, these treatments could not completely prevent the interaction of Clearfil SE Bond with Impregum, or Protect Liner F with Express XT. |
| Falkensammer et al 201449 | In vitro | Bond strength, Conditioning method | Evaluated alterations in the bond strength after application of different conditioning methods (polishing with fluoride-free pumice paste, APA with silicoated aluminum oxide, glycine or calcium carbonate). | Polishing and APA with aluminum oxide or glycine were efficient conditioning methods. APA with aluminum oxide left significant surface alterations. Calcium carbonate was contraindicated. |
| Oliveira et al 2014119 | In vitro | Cuspal deflection, Fracture resistance | Investigated the effect of IDS (Clearfil SE Bond/Clearfil SE Bond + Protect Liner F) on the cuspal deflection and fracture resistance of teeth with composite resin inlays. | IDS did not affect fracture resistance. IDS with Clearfil SE Bond alone provided cuspal deflection similar to that in a sound tooth. LVR addition did not reduce the cuspal deflection further. |
| Özcan 201555 | In vitro | Bond strength | Investigated the effect of mechanical and air-particle cleansing protocols (APA with 50μm at 2, 3.5 bar/30μm at 2, 3.5 bar/prophylaxy paste/pumice-water slurry at 1500 rpm for 15 sec) of provisional cement on IDS surface. | Provisional cement remnants on the IDS surface could best be removed by cleansing methods using air-abrasion for a short duration of 5 sec. |
| Rocca et al 2015141 | Review | - | - | IDS is a crucial step of the indirect restoration fabrication procedure. |
| Giannini et al 201574 | In vitro | Bond strength, Cement type | Evaluated the effect of IDS (Clearfil SE Bond + Clearfil Majesty Flow) on the dentin bond strength of five resin cements (RelyX Unicem, RelyX Unicem 2, Clearfil SA Cement, G-Cem, Panavia F2.0). | The increase in bond strength was dependent upon the resin cement type. IDS improved the bond strength of Panavia 2.0, RelyX Unicem, RelyX Unicem 2, but did not influence Clearfil SA Cement or G-Cem. |
| Leesungbok et al 201589 | In vitro | Bond strength | Tested the effect of IDS (All Bond II) on bond strength of ceramic restorations under various thermocycling periods (1, 2, 7, and 14 days). | Ceramic restorations should be bonded within 1 week after IDS. |
| Nawarek et al 201520 | Review | – | Described the sealing ability of DBAs used for IDS. | Two-step self-etch and three-step total-etch adhesives sealed dentin very well. |
| van der Breemer et al 201582 | Systematic review | – | Evaluated the available literature concerning the cementation of glass–ceramic restorations with an additional focus on IDS. | There were no clinical studies regarding IDS. Possible benefits mainly concern favorable μTBS values. |
| De Rose et al 2015101 | In vitro | Internal adaptation | Evaluated the effect of immediate endodontic sealing (Clearfil SE Bond + Majesty Flow/Majesty Posterior) and the composite viscosity on internal adaptation of the final restoration. | Immediate endodontic sealing significantly improved internal adaptation compared with that using delayed endodontic sealing, and composite viscosity did not affect internal adaptation. |
| Nikaido et al 2015142 | Review | - | - | The resin coating technique can minimize pulp irritation, improve the bond strength between a resin cement and tooth, and enhance interfacial adaptation of the restorations. |
| Goldeberg et al 2016143 | In vitro | Fatigue resistance | Evaluated the accelerated fatigue resistance of thick CAD/CAM composite resin overlays luted with three different bonding methods (IDS Optibond FL+ luting cement Herculite XRV/IDS Optibond FL luting cement Nexus 3/direct luting with Optibond FL+Nexus 3) | Light-polymerizing luting composites in combination with IDS are not contraindicated with thick restorations. |
| Da Silva et al 201634 | In Vitro | Bond Strength | Compared the effect of a resin-based provisional material (Clip F) on μTBS to human dentin developed using DDS and IDS. | Adhesion to dentin was negatively influenced in the IDS procedure when a resin-based provisional material was applied. Isolation with a water-soluble gel was recommended. |
| Gresnigt et al 201686 | In vitro | Fracture strength | Investigated the effect of DDS and IDS (Optibond FL) on the fracture strength of lithium-disilicate laminate veneers. | When laminate veneers were bonded to a large dentin substrate, IDS improved the adhesion and, therefore, the fracture strength. |
| Santana et al 201675 | In vitro | Βond strength | Investigated the effect of simulated pulpal pressure and IDS (Clearfil SE Bond) on μTBS of indirect composite restorations luted with four resin cements (RelyX Unicem, Clearfil SA Luting, RelyX ARC, Panavia F). | Regardless of the simulated pulpal pressure, IDS increased the bond strength of Panavia F, Clearfil SA Luting and RelyX Unicem, but did not influence RelyX ARC. |
| Qanungo et al 2016144 | Review | – | Reviewed the available literature concerning IDS between 1990 and 2014. | IDS was recommended for indirect bonded restorations. |
| El-Damanhoury and Gaintantzopoulou 201683 | In vitro | Fracture resistance | Investigated the effect of IDS (Syntac) and optical powder removal on the fracture resistance of premolar endocrowns. | IDS did not improve the fracture resistance of premolar endocrowns. |
| Belleflamme et al 201784 | Retrospective clinical study | - | Evaluated documented cases of endocrowns performed using IDS. | The study supported the use of IDS which contributed to the high success rate in terms of debonding (2%). |
| Lima et al 2017145 | In vitro | Bond strength | Assessed the bond strength of a resin cement (RelyX ARC) when IDS (Adper Scotchbond Multi-Purpose) was contaminated by different temporary cements (Provy/RelyX Temp NE/Provitemp). | Provitemp temporary cement sealing increased microshear bond strength of the resin cement on dentin treated with IDS. Residues of Provy and Provitemp were observed on the sealed dentin. |
| Leite et al 201710 | Case Report | - | - | The incorporation of IDS in indirect restorations provided better marginal fit, reduced marginal infiltration and postoperative Sensitivity. |
| Brigagao et al 201744 | In vitro | Bond strength, Interim cement | Evaluated the effect of IDS (Scotchbond Universal) and interim cement on the bond strength of a conventional (RelyX ARC) and a self-adhesive (RelyX U200) resin cement. | Immediate application of a DBA before interim cement promoted the highest bond strength for both resin cements tested. |
| Ishii et al 201778 | In vitro | Βond strength | Investigated the bonding state of metal-free CAD/CAM onlay restorations fabricated by two resin blocks (Lava Ultimate, VITA ENAMIC) and one glass–ceramic block (VITABLOCS Mark II) after loading, with/without IDS (Scotchbond Universal + Filtek Supreme Ultra Flowable Restorative). | IDS improved the bond reliability of metal-free CAD/CAM onlay restorations. |
| van der Breemer et al 201779 | In vitro | Fracture strength | Investigated the effect of IDS (Clearfil SE Bond + Tetric Evoflow) on the fracture strength of two indirect restorative materials (Lithium disilicate: IPS e.max, multi-phase resin composite: Lava Ultimate). | IDS significantly improved the fracture resistance of lithium disilicate but not that of a multi-phase resin composite. |
| Yazigi et al 201777 | In vitro | Fracture strength | Investigated the effect of IDS (total-etch/selective-etch) on the fracture strength of CAD/CAM occlusal veneers. | Selective etching of enamel was as efficacious as total-etching. IDS was recommended if dentin was exposed. |
| Nikaido et al 201817 | Review | - | - | Coating materials have the potential to reinforce sound tooth,leading to the maximum preservation of tooth structures. |
| Augusti et al 201847 | In vitro | Bond strength | Investigated the influence of different cleaning techniques (Hand-scaler/Alumina air-abrasion/Glycine powder air-abrasion/D-Limonene chemical solvent) upon microshear bond strength of a composite resin cement (Nexus Universal adhesive luting cement) to a pre-hybridized dentinal substrate (Optibond FL) exposed to two different temporary materials (TempBond NE/TempBond Clear) | IDS protected freshly-cut dentin from the adverse effects of temporary materials. Glycine air-abrasion was suggested when a temporary resin cement is adopted. |
| Ferreira-Filho et al 201821 | In vitro | Bond strength | Evaluated the immediate and 3-month water-storage behavior of four DBAs (Xeno V, Clearfil SE Bond, XP Bond, Optibond FL) used for IDS. | After 7 days, IDS groups yielded higher μTBS than that of the control group (without IDS), except for XP Bond and Clearfil SE Bond. After 3 months, IDS groups did not differ significantly from control group. |
| Hironaka et al 201839 | In vitro | Bond strength, Interim cement | Investigated the effect of IDS (Clearfil SE Bond+ Protect Liner F) and interim cement (Temp Bond NE) on the bond strength of indirect restorations luted with a dual-cure resin cement (Panavia F 2.0). | IDS provided higher μTBS values, whereas the interim cement did not interfere with bond quality if IDS was applied. |
| Murata et al 201860 | In vitro | Bond strength | Evaluated the effect of different IDS applications (thin layer/slope-shaped/base-shaped) on the bond strength of CAD/CAM ceramic inlays subjected to loading. | IDS improved μTBS as well as the bonding reliability and durability of the restorations tested. The slope-shaped group yielded the highest performance. |
| Redoul et al 201881 | In vitro | Bond strength | Evaluated the bond strength of glass–ceramic overlays luted using different bonding techniques (Panavia V5 + IDS-Optibond FL/Panavia V5 without IDS/Heated composite + IDS). | Panavia V5 + IDS yielded the best resistance to shear forces. IDS increased the bond strength. |
| Fouda 2019146 | Randomized Control Clinical Trial | Hypersensitivity | Compared IDS and DDS effect on Hypersensitivity of teeth prepared for indirect composite restorations using Visual Analog Scale. | Inter-operative and post-cementation hypersensitivity reduced by using the IDS protocol with a self-etch adhesive. |
| Anzlovar et al 201954 | In vitro | Bond strength | Evaluated the influence of chemical and physical processes at the resin-composite and composite-cement interface on the bond strength between these two components. | Concentration of free radicals at the surface of the resin composite is only relevant immediately after the polymerisation to the bond strength between the resin composite and the composite cement. |
| Khakiani et al 201929 | Ex vivo | Interaction with impression materials | Evaluated the interactions between IDS (Adper Single Bond 2/Clearfil SE Bond) and two impression materials (Aquasil/Impregum Soft) after air-blocking alone or combined with pumicing. | Air-blocking and pumicing should be applied with silicone impressions. Polyether was not recommended with IDS. |
| Sinjari et al 201933 | In vitro | Interaction with impression materials | Evaluated the interactions between two impression materials (Extrude medium/Impregum Penta) and IDS (Optibond FL). Specimens subjected to two cleaning protocols before impression-taking (prophy paste/prophy paste + Marseille soap). | Regardless of the impression material used, complete elimination of any interaction was observed in the prophy paste + Marseille-soap group. |
| Hayashi et al 2019147 | In vitro | Βond strength | Investigated the effect of IDS (Clearfil Universal Bond + Clearfil Majesty ES Flow) and temporary restoration materials (Protemp4 Temporization material, TempBond NE) on the bond strength of CAD/CAM ceramic crowns after loading. | IDS increased the bond strength, whereas temporary restoration did not affect it at all. IDS without a temporary restoration yielded the maximum bond reliability. |
| van der Breemer et al 201950 | In vitro | Βond strength | Evaluated the effect of different IDS combinations (one layer-Optibond FL, two layers-Optibond FL, one layer-Optibond FL + LVR- Grand IO Flow) and conditioning methods (pumice rubbing/pumice rubbing + tribochemical-silica coating) at two water-storage times (1 week/6 months). | Dentin exposure during clinical procedures for indirect restorations benefited from IDS application, which was shown to result in higher bond strength. Significant differences were not found between cleaning with pumice alone or pumice followed by tribochemical-silica coating. |
| van der Breemer et al 201951 | In vitro | Βond strength | Evaluated the effect of two DBAs (Clearfil SE Bond/Optibond FL) used for three IDS combinations (one layer/two layers/one layer + LVR) and two surface-conditioning methods (pumice/pumice + silica coating) on the bond strength of a resin cement (Variolink II) to dentin. | Regardless of the combination, IDS improved the bond strength compared with DDS. Significant differences among the conditioning methods tested were not observed. |
| van der Breemer et al 2019148 | Randomized clinical trial | Survival, success rate, and quality of survival of partial ceramic restorations | Investigated the survival, success rate, and quality of survival of partial ceramic restorations (IPS e.max) in vital molars bonded using IDS (Clearfil SE Bond + Clearfil Majesty Flow) after 3 years of function. | Ceramic restorations with IDS did not yield differences in the success rate or survival rate after 3 years of function. |
| Rigos et al 201980 | In vitro | Βond strength | Evaluated the bond strength of pretreated monolithic zirconia bonded to dentin using IDS (Optibond FL) and two self-adhesive resin cements (Panavia F2.0/Permacem Dual Smartmix). | Bonding strategies for monolithic zirconia restorations could potentially benefit from IDS regardless of the adhesive luting agent system used. |
| Gresnigt et al 201987 | Prospective clinical trial | Survival, success rate, patient satisfaction | Evaluated the survival, success rate, and satisfaction regarding laminate veneers received by 104 patients, in which IDS was done, after 11 years of function. | IDS significantly benefited teeth with >50% of dentin exposure. |
| van der Breemer et al 2019102 | Prospective randomized clinical trial | Tooth sensitivity, patient satisfaction | Investigated tooth sensitivity and patient satisfaction regarding partial ceramic restorations in 30 patients, bonded using IDS (Clearfil SE Bond + Clearfil Majesty Flow). | IDS was not superior with regard to tooth sensitivity or patient satisfaction after 1 year of function. |
| Akehashi et al 201969 | In vitro | Βond strength | Investigated the bond strength provided by different combinations of resin materials used for IDS (Clearfil SE Bond 2 + Protect Liner F/Clearfil Majesty LV/Panavia V5) in indirect composite restorations luted with a dual-cure resin cement (Panavia V5/Panavia F2.0). | μTBS values of the combination Clearfil SE Bond2 + Panavia V5 and cementation with Panavia F2.0 were identical with those of a direct composite restoration. |
| Rozan et al 2020149 | In vitro | Bond strength and Internal adaptation | Assessed the effect of the resin-coating technique (G-Premio Bond/Clearfil SE Bond 2+Clearfil Majesty ES Flow) on bond strength and internal adaptation of CAD/CAM inlays luted with different resin cements (PelyX Ultimate/G-CEM LinkForce/Panavia V5). | Resin coating did not influence the bond strength of RelyX Ultimate, whereas resin coating increased the bond strength of G-CEM LinkForce and Panavia V5. |
| Cesca et al 2020150 | In vitro | Tensile load | Compared direct/indirect resin composite copings for perio-overdentures, luted using DDS or IDS (Syntac+ Variolink II/Tetric Ceram). | IDS group yielded significantly higher tensile load. |
| Sag and Bektas 2020118 | In vitro | Bond strength | Compared bond strength of different resin cements (RelyX Unicem/RelyX Ultimate Clicker) on an indirect composite (Solidex) and a resin nanoceramic CAD/CAM block (Lava Ultimate) with or without IDS (Clearfil SE Bond+ Filtek Ultimate). | IDS improved bond strength of indirect restorations. |
| Ashy et al 20208 | In vitro | Marginal adaptation and internal adaptation | Investigated marginal adaptation and internal adaptation of ceramic inlay restorations bonded using IDS (All-Bond Universal) or DDS. | Luted ceramic inlays had a superior marginal adaptation immediately after cementation and a superior internal adaptation after thermocycling if using IDS compared with using DDS. However, marginal adaptation after thermocycling was not significantly different between the two techniques. |
| Shafiei et al 2020120 | In vitro | Fracture resistance | Investigated the effect of dentin pretreatment with polyanthocyanidin (PA) combined with IDS (Futurabond) or DDS on the fracture resistance of premolar ceramic inlays luted with a self-adhesive resin cement (BiFix SE) | IDS with/without PA increased the fracture strength of premolars. The combination of both reached the level of a sound tooth. |
| Hofsteenge et al 202088 | In vitro | Aging and Fracture strength | Evaluated the effect of aging, fracture strength, failure mode, and repairability on lithium-disilicate inlays and onlays in relation with IDS (Optibond FL) or DDS. | IDS application and the preparation design influenced the fracture strength, respectively. IDS application did not interact with the effect of the preparation design on fracture strength. |
| van der Breemer et al 202176 | Prospective clinical trial | Clinical performance | Assessed the clinical performance of 765 partial glass–ceramic posterior restorations (IPS e.max) luted with a conventional photo-activated resin composite in conjunction with IDS (Clearfil SE Bond). | Partial glass–ceramic posterior restorations treated with IDS had an excellent medium-term prognosis. |
Abbreviations: DBA, dentin-bonding agent; LVR, low-viscosity resin; μTBS, microtensile bond strength; IDS, immediate dentin sealing; DDS, delayed dentin sealing; APA, airborne particle abrasion.
Figure 1.
Questions regarding each clinical step of the restorative protocol containing the IDS technique and determination of the sections discussed in this review.
Abbreviations: IDS, immediate dentin sealing; DDS, delayed dentin sealing.
Each section of this manuscript answers a crucial question regarding the treatment approach as well as the technical details of IDS application. First, the rationale supporting selection of the technique is analyzed. Moreover, we cite all available evidence for the most appropriate adhesive systems; interaction with impression materials; provisional restorations; surface conditioning; material selection for adhesive luting and film thickness; restorative materials; microleakage/marginal adaptation; time of restoration placement; and hypersensitivity.
IDS Protocol
The IDS technique rests upon four fundamental principles.11 First, only fresh-cut, contaminant-free dentin provides the optimum substrate for bonding. In any other case, the bond strength is inferior.12,13 Second, if the DBA and overlaying composite are light-cured together, the hybrid layer may collapse due to the pressure from the composite or restoration placement.14–16 Thus, precuring the DBA results in a better bond strength. Third, IDS and delayed restoration placement permit maturation of the dentin bond in an environment free of occlusal forces and overlaying composite shrinkage.71,72 Fourth, IDS reduces fluid and bacterial penetration.
The clinical advantages emerging from the aforementioned include11 (i) patient comfort during provisionalization, less need for anesthesia at the cementation appointment, and reduced post-cementation sensitivity; (ii) increased bond strength and retention, especially for tapered teeth with short clinical crowns and minimum removal of tooth tissue;17 (iii) independent treatment and conditioning of dentin and enamel that maximizes the overall performance of both tissues according to their individual characteristics.
According to Magne,9,18 the first step of IDS is to distinguish dentin from enamel. For this purpose, a preliminary etching of 2–3 s is undertaken at the whole tooth surface. After thorough rinsing, enamel acquires a “frosty” appearance, whereas dentin is more “glossy”. Then, using a diamond bur (in etch-and-rinse systems) or a carbide tungsten bur (in self-etch systems), a fresh layer of dentin is exposed, over which a thick layer of a DBA is applied and light-polymerized according to manufacturer instructions. In the case of unfilled adhesive, a supplementary layer of flowable resin is recommended or alternatively, a regular composite to correct geometry, eliminate undercuts, or elevate the preparation. After that, the DBA is polymerized additionally through glycerin gel (air-blocking) to reduce the oxygen-inhibition layer (OIL) and rinsed with air/water spray. To remove excess adhesive, enamel margins may need to be corrected with a diamond bur.
Before the impression procedure with elastomeric materials, the tooth preparation is pumiced softly with a rubber cup for OIL reduction and, after that it is isolated with a separating medium (eg, petroleum jelly) to avoid locking of the interim restoration. With regard to placement of the final restoration, the sealed surface must be air-abraded and the enamel etched with phosphoric acid (H3PO4). Finally, the restoration is luted with a resin-based cement. However, materials and protocols are evolving constantly, so the above-mentioned guidelines may deviate. The key element is to follow the basic steps and integrate the new materials simultaneously following manufacturer instructions.
Type of Adhesive System
In adhesive dentistry, there are always attempts to simplify bonding steps to reduce “chair time” and make clinical procedures less technique-sensitive. However, a conventional three-step total-etch DBA claimed to be the most reliable long-term option is recommended by Magne9 for IDS. Scholars have reported19,20 that older three-step etch-and-rinse systems and two-step self-etch systems are superior to single-step systems with regard to durability, aging, and bond strength. Furthermore, older adhesives form a more hydrophobic resin coating, which is desirable for IDS efficacy.19 Single-step self-etching adhesives have been accused of being susceptible to degradation if water stored because of the increased hydrophilicity of their interface.21 It has also been suggested that, for vital teeth with positive pulpal pressure, the penetration of dentinal fluid through polymerized adhesive layers may deteriorate hermetic dentin sealing if simplified adhesive systems are employed.5
Duarte et al3 revealed that both total-etch adhesives and self-etch adhesives favored IDS achieving a significantly higher bond strength than that using the conventional approach (without IDS). Conversely, Ferreira-Filho et al,21 in an attempt to investigate the behavior of four adhesive systems (one-step self-etch Xeno V; two-step self-etch Clearfil SE Bond; two-step etch-and-rinse XP Bond; three-step etch-and-rinse Optibond FL), found no differences in microtensile bond strength among the adhesives tested and the control group (without IDS) after 3 months of water storage.
It is clear that the adhesive system applied influences the permeability of sealed dentin, not to mention that there are adhesives reported to be less effective than the original smear layer.22–24 Sahin et al5 attempted to identify the hydraulic conductance of dentin after application of five materials (two-step self-etch Clearfil Protect Bond; all-in-one self-etch adhesive Adper Prompt L-Pop; one-component self-etch adhesives Clearfil S3 Bond and G-Bond; etch-and-rinse adhesive Single Bond 2; one dentin desensitizer Gluma). They reported that none of the adhesives examined achieved hermetic dentin sealing. However, G-Bond and Clearfil Protect Bond managed more efficacious sealing than the original smear layer. The results of that study are in agreement with data from another study23 demonstrating that Clearfil Protect Bond had the lowest fluid permeability, followed by G-Bond (which manifested lower but statistically similar permeability with that using Clearfil S3 Bond).
Although a few studies have compared the efficacy of different DBAs used for IDS, conventional systems (three-step-total-etch, two-step-self-etch) are recommended because their clinical efficacy has been substantiated by many studies in recent decades. Adherence to manufacturer instructions is of the utmost importance.
Interaction with Impression Materials
Several issues arise regarding the contamination of a resin coating surface by elastomeric impression materials. If light-cured, DBAs present a superficial OIL.25 The thickness of the OIL is ~40 μm and can inhibit the polymerization of elastomeric impression materials.25,26 Magne and Nielsen27 demonstrated a substantial layer of unpolymerized resin in specimens in which IDS had been applied without further surface treatment, regardless of the type of DBA or impression material used. This, in turn, led to defective impressions. Those findings are in agreement with data from Ghiggi et al,28 who observed diverse interaction types among resin materials and impression materials: silicone showed incomplete polymerization and polyether, although polymerized, attempted to adhere to the resin present on the surface. It is speculated that the chemical composition of vinylpolysiloxane and polyethers accounts for their different interactions with resin materials.28 Specifically, for vinyl polysiloxane, the monomers present in the OIL may react with the platinum salt (the catalyst in the polymerization reaction). As a result, a small portion of the light impression material remains unpolymerized over the resin materials. For polyethers, the initiator agent is cation that can react with the free radicals of monomers from the surface of resin materials (ionic polymerization). Furthermore, the hydrophilicity of polyethers, their higher stiffness, and their lower resistance to tear in comparison with those of vinyl polysiloxane favors superficial adhesion to the resin surface, and so defective impressions emerge. The hydrophilic monomer hydroxyethylmethacrylate, which is present in the adhesive resin of some DBAs, has been also accused of causing residual inhibition.27
Based on the knowledge that reducing/eliminating the OIL would lead to the abovementioned issues being resolved, several cleaning protocols after IDS application and before impression-taking have been suggested. Magne and Nielsen27 advocated that the residues of impression materials could be reduced with additional polymerization of the DBA with glycerin jelly (air-blocking) and pumicing (gentle application of a pumice water mix with a soft rubber prophy cup and slow-speed handpiece at 500 rpm), but only with silicone impression materials. A polyether was not recommended with IDS because of the high incidence of faulty impressions (unpolymerized impression material, adhesion, tearing). Those findings are in agreement with an in vitro study by Khakiani et al.29
Bruzi et al30 suggested that covering the IDS layer with a liner (flowable/composite) resolves the issue of interaction with impression materials. Coating the DBA with flowable resin enhances subsequent polymerization of the OIL in uncured adhesives thanks to the diffusion of free radicals from the flowable resin.31,32
Ghiggi et al28 compared the air-blocking technique with the use of a cotton pellet soaked in alcohol. They concluded that both methods were equally efficient in preventing interaction with impression materials.
Sinjari et al,33 in an attempt to identify a safe protocol for clinical surfaces, evaluated the application of prophy paste treatment (surface carefully cleaned with a handpiece, coping brush, and prophy paste at 500 rpm under a water spray for 15 s) and of a surfactant agent (Marseille soap) on the IDS surface before impression-taking with silicone and polyether. The researchers demonstrated a reduction of residues in prophy groups and their total disappearance in prophy + Marseille-soap groups for the two impression materials tested.
Given that OIL elimination is the key factor for a defect-free impression, researchers have focused attention on double polymerization of the DBA with glycerin gel and the several cleaning protocols suggested in literature. Even if polyether as an impression material is disapproved by most authors, the protocol of Sinjari et al (prophy paste + Marseille soap) offers cautious optimism regarding the choice of impression material.
Interaction with Provisional Materials
With regard to the choice of interim material and cement, resin-based ones should be avoided.9,34 Direct acrylic-based provisional materials cannot seal preparations hermetically, which results in contamination of the IDS surface and loss of retention.35 Conversely, regardless of OIL removal, direct bis-acryl-based provisional materials and resin-based interim cements bond strongly to the IDS substrate.35 Hence, removal of the provisional material proves to be demanding and sometimes it must be cut-off the tooth, which jeopardizes the integrity of tooth preparation.35 Even after persistent mechanical cleaning and conditioning with 37% phosphoric acid, the presence of interim-material residue on dentin has been identified in studies using scanning electron microscopy36,37 and atomic force microscopy.38 This is the reason why Magne9 strongly recommends isolation of the tooth preparation with a thick layer of a separating medium (petroleum jelly) during fabrication of the provisional material.
The presence of interim-material residues after cleaning has been documented. The question is whether the remaining residues affect the bond strength to such an extent that makes bonding insufficient.39 Some authors have reported a reduction in the bond strength of resin materials only after use of eugenol-containing cements,40,41 whereas other scholars have not discriminated the type of interim cement.42 To counteract the drawbacks of eugenol (interaction with initiators, loss of retention, microleakage43), one could propose its replacement by carboxylic acids. Nevertheless, a considerable reduction in bond strength after adhesive cementation has also been observed with non-eugenol formulations.13 It has been demonstrated that if IDS is applied, regardless of the use of eugenol-containing or eugenol-free provisional luting agents,43 interim materials do not influence the adhesion quality of resin cements.39,43–46
Schoenbaum et al35 suggested the “reverse spot bonding technique” for provisional cementation. This technique relies on the bonding of the provisional material in only a small area of the IDS-prepared tooth, away from the margins. This serves efficient cleaning of the surface at the cementation appointment. A small portion of fast-setting condensation silicone is placed in the middle of the preparation, covering 2–3 mm of the sealed surface. Then, a separating medium is applied on the entire surface of the preparation. The silicone increment is removed to leave a small active bonding area while the remaining portion of the sealed surface does not bond to the bis-acryl material thanks to the presence of the separating film.
Interim restoration should protect the underlying tooth surface and not endanger the integrity of the preparation after its removal. Application of a separating medium combined with spot bonding seems to serve the above-mentioned requirements. Moreover, resin-based temporary cements should be avoided,47 unless isolation using a water-soluble gel has been applied beforehand.34
Conditioning Methods
A contaminant-free substrate is a necessity for optimum bonding. Therefore, selection of the appropriate conditioning method is of utmost importance. Magne et al9 employed air-borne particle abrasion (APA) with aluminum oxide, whereas Dillenburg et al48 demonstrated that additional etching with phosphoric acid had a positive impact on conditioning sealed dentin. In another study,49 polishing with fluoride-free pumice paste and APA with silicoated aluminum oxide or glycin proved to be equally efficient methods, whereas APA with calcium carbonate was contraindicated due to its higher roughness along with the lower bond strength following its application. van den Breemer et al50,51 observed that neither cleaning with pumice nor pumicing with an additional tribochemical silica coating affected the bond strength. Although they could not identify the optimum combination of IDS/conditioning method, they suggested a thick IDS layer conditioned with silica coating. Silica coating expands the adhesive surface area via deposition of silica particles. This action permits superior mechanical retention52 and cleans the surface, thereby enabling chemical co-polymerization of the resin-based cement with IDS.50 With regard to sandblasting with alumina, loss of filling particles is likely49 as is a reduction of the resin-to-resin bond strength.51,53 Although as outlined above there are conflicting results, contrary to pumicing with a rotary brush, access to difficult parts of the preparation achieved by sandblasting is desirable.
There is an array of conditioning methods/materials, and further investigation on their potential influence on the IDS surface is required. However, it seems that methods ensuring physical removal of a few micrometers (such as APA) from the resin surface which is in contact with oral fluids should be implemented54 at limited application duration since it enhances diffusion of resin cements.55 After cleansing, dentin surface needs to be reactivated by adhesive resin.55
Film Thickness
The risk of re-exposure of dentin after conditioning is substantive, and is dependent not only on the conditioning method but also on the thickness of the IDS film.56 Film thickness is dependent on the product and its location on the tooth (greater in concave areas than in convex areas).56 The higher film thickness in concave areas is attributed to the tendency of the adhesive to “pool” at the inner angles of the preparation. Low thickness in the border of the preparation is desirable because a high one would expose the adhesive to the oral cavity, with subsequent degradation.57
Stavridakis et al56 suggested the use of a filled DBA to prevent dentin re-exposure after conditioning. Hashimoto et al58 observed an increase in the bond strength after application of multiple layers of adhesive (≤4 layers), whereas Ito et al59 concluded that the separate polymerization of each layer improved the quality of dentin adhesion. The IDS layer has been found to affect cement thickness.60 A thicker IDS film contributes to better distribution of stress, yields a superior bond strength, and provides more stable bonding,50,60,61 whereas elimination of undercuts becomes easier.51 However, if applying a multi-layering technique, one should pay attention to the “ideal” thickness of the adhesive system used and follow manufacturer instructions closely.62
A supplementary layer of a low-viscosity resin (LVR) over the DBA is recommended,57 especially if unfilled DBAs are used.11 Free radicals from the LVR interact with the uncured resin or the acidic monomers from the OIL63 to improve the polymerization of the adhesive system.31 Moreover, an LVR reduces the permeability of adhesives and improves coupling with the resin cement.64 Even if resin–dentin interfaces degrade over time, an LVR protects the underlying hybrid layer and preserves the integrity of the dentin seal.65 An LVR can act as an “absorbing cushion” of the contraction stress generated during resin cement polymerization and, thus, modify the failure pattern63,66 (the formation of a resistant hybridization process contributes to the preservation of the bonded interface area if a fracture occurs). Hence, an improved bond strength has been recorded when adding an LVR31,67,68 although it seems that selection of the LVR type can affect the performance of the restoration.69 In general, the use of materials with high ultimate strength for cementation and coating is recommended.32 In the case of discolored dentin, application of an opaque resin over the DBA reduces the bond strength likely due to the limited mechanical properties of the liner.70 If masking is needed, use of a separate layer of opaque resin is preferred to mixing with the DBA.70
A thick IDS layer is crucial to prevent dentin re-exposure after conditioning. Addition of an LVR provides an array of advantages and so its application is imperative in the case of unfilled DBAs.
Interaction with Luting Cements
IDS manifests the highest retentive stress if combined with resin cements. Thus, IDS is indicated in cases of a short clinical crown height and high angle of convergence. IDS provides efficient retention with glass ionomer cements as well, but under no circumstances should it be used with zinc phosphate.71,72 Dalby et al73 found that IDS did not affect the bond strength of the self-adhesive resin cement RelyX Unicem. In a similar study74 that tested several self-adhesive resin cements, IDS was found to influence the bond strength of the resin cement depending on its type (bond-strength values of Panavia F2.0, RelyX Unicem and RelyX Unicem2 were improved, but no effects were reported for Clearfil SA Cement and G-Cem). It has been also demonstrated that even if simulated pulpal pressure negatively affects the quality of resin–dentin interfaces, IDS increases the bond strength of self-adhesive and conventional resin cements.75 IDS also interacts well if luted with conventional light-cured composites, as indicated by the excellent medium-term prognosis of partial ceramic restorations in a recent clinical study.76
IDS has been demonstrated to improve the bond strength of resin cements (conventional or self-adhesive). Conventional resin cements are recommended in the literature for their superior properties with regard to bond strength, bond-degradation behavior, susceptibility to aqueous aging, and water absorption.
Interaction with Preparation Design
The survival rate of minimally invasive restorations is influenced by the preparation design, restoration thickness and geometry, restorative material, occlusal loading, and bonding procedures.77 Several studies77–82 investigating different types of restorations and restorative materials have shown that IDS enhances the bond strength, fracture resistance, and bond reliability of the restorations tested. With regard to endocrowns, El-Damanhoury and Gaintantzopoulou83 showed that IDS does not improve their fracture resistance. However, a clinical study demonstrated the high success rate of endocrowns in terms of debonding when IDS is applied.84 The survival rate of laminate veneers decreases if bonded to dentin.85 In the case of limited dentin exposure (less than one-quarter of the bonding surface), IDS has no influence on them.86 However, with >50% of dentin exposure, laminate veneers benefit significantly from IDS.87 In a recent study, Hofsteenge et al88 investigated the influence of IDS on the fracture strength of different preparation designs (inlays–overlays). Even though IDS in conjunction with an overlay preparation resulted in the highest fracture strength, the authors concluded that the IDS application did not interact with the effect of the preparation design on fracture strength.
Time of Restoration Placement
With IDS, there is leeway in the dentin bond to develop in a stress-free environment and, thus, to be optimal.11 Magne19 advocates that IDS favors delayed restoration placement for ≤12 weeks. Leesungbok et al89 investigated the influence of IDS on the dentin bond strength of a lithium-disilicate ceramic under various thermocycling periods (1, 2, 7 and 14 days). They identified a reduction in bond strength after 1 week and a greater one (characterized by a larger area of detached cement and exposed dentin) after 2 weeks. Thus, the authors strongly recommend the final bonding to be within 1 week after IDS application.
The IDS concept counts on the success of the bond between the resin coating and luting agent, which is similar to the one for resin-to-resin repair.19 Placement of a provisional restoration for ≤2 weeks does not endanger the resin-to-resin bond, and van den Waals interactions, and micro-mechanical interlocking can account for it.9,90,91 However, to achieve this, the existing adhesive layer must be conditioned.9 Even if it is claimed that a delayed restoration placement is attainable when IDS is applied, the final restoration should be delivered as soon as possible.
Microleakage/Adaptation of the Final Restoration
The adhesive layer–dentin interface constitutes the most vulnerable part of the bonded restoration, so micro-leakage remains a major concern if a restoration is thermally and occlusally stressed.3 There is a wide variation concerning acceptable values for marginal discrepancy: they range from 20–40 μm to 160 μm.92–94 Duarte et al3 demonstrated that even if IDS favored bond strength, micro-leakage was not improved. Conversely, several studies have shown that if the DBA is combined with an LVR, a smaller gap formation in the dentin–restoration interface is observed,31,95–99 even if subjected to loading.95,100 A variant of IDS undertaken in the access cavity of teeth subjected to endodontic treatment (immediate endodontic sealing) has been shown to reduce coronal leakage, which is the major cause of failure.101 In a recent study, Ashy et al8 identified a better marginal adaptation immediately after cementation and a better internal adaptation after thermocycling, when IDS was applied, compared with that using the conventional method (DDS). However, there was no significant difference in marginal adaptation after thermocycling among the two techniques examined. Therefore, IDS seems to reduce microleakage, whereas a DBA combined with an LVR provides more predictable outcomes.
Hypersensitivity
During the provisional phase and after cementation of the final restoration, it is common for the patient to experience an unpleasant symptom characterized by a short, sharp pain upon thermal and chemical stimuli.102 Several factors can account for this effect: over-heating and dehydration during preparation, bacterial micro-leakage, or fluid movement through dentin tubules.21 Although dentin hypersensitivity usually resolves within 24 months,102 its persistence can overwhelm the patient and put the clinician’s reputation at risk. Hu and Zhu103 undertook a sensitivity assessment 1 week as well as 1, 6, 12 and 24 months after cementation of a three-unit full-coverage restoration on vital abutment teeth. They identified a significant improvement in patients to whom IDS was applied at 1 week and 1 month after cementation, whereas no differences between IDS and DDS groups were found at the end of 6, 12 and 24 months. Conversely, van der Breemer102 detected no difference among IDS and DDS, an anticipated result given the minimally invasive design used for partial ceramic restorations in their study. Hence, the amount of tooth tissue removed plays an important part in the degree of postoperative sensitivity.104 A distance of 0.5 mm from the pulp can cause a pulpal reaction in 60% of cases, whereas a similar situation occurs in 5% of teeth in which >1 mm of dentin has been preserved.105
Early sealing of dentin tubules provided by the IDS technique seems to reduce sensitivity during the provisional phase and after cementation. This is a promising strategy for enhancing comfort and treatment satisfaction.
Discussion
Systematic reviews showing a significant difference in terms of longevity between direct and indirect composite restorations are lacking.106,107 Nevertheless, indirect composite restorations are recommended in the case of endodontically treated teeth.108 Such restorations also overcome the problems related to polymerization shrinkage or inadequate curing, thereby providing better mechanical properties, occlusal morphology, and proximal contacts.2,109 Although these restorations constitute a large workload in everyday practice, clear protocols regarding the handling of prepared tissues and materials used to obtain optimum results are lacking. We reviewed the literature to provide clinically oriented answers to questions regarding crucial procedures related to each step of indirect restorations, from the preparation appointment until restoration delivery and maintenance.
Some types of indirect restorations interact entirely with enamel,110 whereas others demand more aggressive preparation that inevitably leads to dentin exposure.111 Knowledge of the anatomic and morphologic differences between these two tissues is fundamental to handle them appropriately. Enamel is mainly made of the mineral hydroxyapatite (which is crystalline calcium phosphate) and it contains virtually no water.112 Dentin has a higher percentage of organic matter and is perforated by dentinal tubules that contain odontoblasts and transmit thermal stimuli, pressure, and pain.113 Pulp and dentin are embryologically, histologically, and functionally identical tissue; this leads to the belief that they should not be studied as separate tissues but must be viewed as a pulp–dentin complex.114 Consequently, leaving dentin exposed is akin to an “open pathway” towards the pulp, which endangers tooth vitality because microorganisms can reach the pulp tissue if it is not sealed adequately.102 This assumption is supported by the findings of Sailer et al,115 who found that loss of vitality of an abutment tooth was the most frequent biologic complication for metal–ceramic crowns. This finding supports the use of a technique that seals dentin hermetically.
One could claim that application of an adhesive at the preparation appointment would diminish its bonding capacity at the final cementation appointment. However, studies have shown that teeth on which DDS is carried out demonstrate inferior bond strength,31,67,68,82,86,116–118 whereas IDS favors delayed restoration placement19 and provides bond strength and cuspal deflection similar to that observed in direct composite-restored teeth.9,69,119,120 Direct restorations yield higher bond strength in comparison with that using indirect restorations,121 so techniques such as IDS that enhance the bonding capacity of indirect procedures should be adopted. Moreover, IDS does not increase the number of clinical appointments but is incorporated in the necessary steps of an indirect restoration.
An aspect that should be clarified is the mechanism that defines composite-to-composite bond. Although one might assume that chemical bonding of free radicals is the main factor that determines the subsequent bond,122 other mechanisms play a more crucial role. Concentration of free radicals declines as the material ages and according to Anzlovar et al54 they play a minor role within 24 hours and they are completely eliminated after 2.5 days. Mechanisms such as micromechanical interlocking and interpretating network matrices (IPN) seem to play a major role.91,123,124 For the latter to be formed, monomers of the resin cement are diffused into the composite resin and polymerized, and it is the depth of this penetration that determines bond strength.91,124,125 Factors such as the increased polarity of the surface due to contact with water reduces the diffusion potential and this is why implementation of methods that remove a few microns of the composite layer should be applied.54
The literature recommends multiple coatings of a DBA and additional application of an LVR in the case of an unfilled adhesive system.57–59 Hence, another issue that requires further clarification is the impact of the thickness of the DBA film on appropriate seating and marginal adaptation of the restoration. The above-mentioned thickness varies depending on the topography of the tooth preparation,56,57 but it is captured with impression-taking and, therefore, the fit of the final restoration is not influenced.11 Addition of these coatings might raise concerns regarding different material interfaces. However, composite resins have a modulus of elasticity that is close to that of dental tissues,126 thereby eliminating the risk of nonuniform stress distribution if there is a vast difference between restorative materials.127 If a composite restoration instead of a ceramic restoration is chosen, this risk is reduced further.
Another concern regarding IDS pertains to interaction with impression materials. However, this matter will probably not concern future generations because intraoral scanning technologies have yielded results that are equal (or even superior) to those of conventional impression techniques.128 Currently, this technology is indicated in short-span restorations and represents a challenge regarding edentulous arches.129
Complete elimination of the provisional material is difficult. Hence, penetration of the adhesive monomers into dentin could prove to be inadequate.44 Occlusion of dentin tubules with interim materials has been identified, as has a subsequent reaction of zinc-oxide remnants with the acidic primer of some adhesive systems.130 Therefore, the early sealing of dentin tubules with a DBA could prevent their obstruction by interim residues, as well as the inhibition of adhesion-system polymerization due to eugenol diffusion from interim material into dentin.43 Removal of the provisional restoration endangers the integrity of tooth preparation, so it should be done with caution.35 Techniques that pursue spot bonding of the provisional material must evolve and be carried out for an optimum result. Nevertheless, novel digital technology/protocols tend to eliminate the need for provisional restorations. Silva et al131 proposed a technique in which digital design and three-dimensional-printed guides provide the opportunity for cementing restorations immediately after preparation completion.
IDS is a substantiated technique mainly according to many in vitro studies. Among the 88 studies included in this review, 64 are vitro studies and only 12 are clinical surveys. More clinical trials, preferably randomized ones (which are considered the “gold standard” for evaluation of interventions132) are needed to further support the efficacy of this technique and clarify certain aspects regarding it. Moreover, implementation of novel materials and techniques should be tested. A technique has been described where a fiber network has been incorporated in the IDS.70,133 The rationale behind this choice is that in case of a vertical crack, its propagation may be stopped by the fiber network. Fibers and their incorporation in dental restorations are a promising field and their use is growing in cases that demand cusp replacement to enhance the performance of conventional restorative composite resins in terms of fracture resistance.134,135
Conclusions
The IDS technique seems to be advantageous with regard to bond strength, gap formation, bacterial microleakage, and dentin hypersensitivity. However, issues arising from interaction with impression materials, the provisional phase, and conditioning methods before cementation require further investigation. There are no documented reasons preventing clinicians applying IDS in their everyday practice.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Barone A, Derchi G, Rossi A, Marconcini S, Covani U. Longitudinal clinical evaluation of bonded composite inlays: a 3-Year Study. Quintessence Int (Berl). 2008;39(1):65–71. [PubMed] [Google Scholar]
- 2.Duquia Rde C, Osinaga PW, Demarco FF, Conceicao EN. Cervical microleakage in MOD restorations: in vitro comparison of indirect and direct composite. Oper Dent. 2006;31(6):682–687. doi: 10.2341/05-132 [DOI] [PubMed] [Google Scholar]
- 3.Duarte S Jr., de Freitas CR, Saad JR, Sadan A. The effect of immediate dentin sealing on the marginal adaptation and bond strengths of total-etch and self-etch adhesives. J Prosthet Dent. 2009;102(1):1–9. doi: 10.1016/S0022-3913(09)00073-0 [DOI] [PubMed] [Google Scholar]
- 4.Jud C, Schaff F, Zanette I, Wolf J, Fehringer A, Pfeiffer F. Dentinal tubules revealed with X-ray tensor tomography. Dent Mater. 2016;32(9):1189–1195. doi: 10.1016/j.dental.2016.06.021 [DOI] [PubMed] [Google Scholar]
- 5.Sahin C, Cehreli ZC, Yenigul M, Dayangac B. In vitro permeability of etch-and-rinse and self-etch adhesives used for immediate dentin sealing. Dent Mater J. 2012;31(3):401–408. doi: 10.4012/dmj.2011-217 [DOI] [PubMed] [Google Scholar]
- 6.Pashley EL, Comer RW, Simpson MD, Horner JA, Pashley DH, Caughman WF. Dentin permeability: sealing the dentin in crown preparations. Oper Dent. 1992;17(1):13–20. [PubMed] [Google Scholar]
- 7.Helvey GA. Adhesive dentistry: the development of immediate dentin sealing/selective etching bonding technique. Compend Contin Educ Dent. 2011;32(9):22,24–32, 34–5; quiz 36, 38. [PubMed] [Google Scholar]
- 8.Ashy LM, Marghalani H, Silikas N. In vitro evaluation of marginal and internal adaptations of ceramic inlay restorations associated with immediate vs delayed dentin sealing techniques. Int J Prosthodont. 2020;33(1):48–55. doi: 10.11607/ijp.6372 [DOI] [PubMed] [Google Scholar]
- 9.Magne P, Kim TH, Cascione D, Donovan TE. Immediate dentin sealing improves bond strength of indirect restorations. J Prosthet Dent. 2005;94(6):511–519. doi: 10.1016/j.prosdent.2005.10.010 [DOI] [PubMed] [Google Scholar]
- 10.Leite M, Lopes LG, de Souza D, Carvalho M. Immediate dentin sealing with self-etch dentin bonding agent for indirect restoration. World J Dent. 2017;8(6):490–495. doi: 10.5005/jp-journals-10015-1492 [DOI] [Google Scholar]
- 11.Magne P. Immediate dentin sealing: a fundamental procedure for indirect bonded restorations. J Esthet Restor Dent. 2005;17(3):144–154; discussion 155. doi: 10.1111/j.1708-8240.2005.tb00103.x [DOI] [PubMed] [Google Scholar]
- 12.Paul SJ, Scharer P. The dual bonding technique: a modified method to improve adhesive luting procedures. Int J Periodontics Restorative Dent. 1997;17(6):536–545. [PubMed] [Google Scholar]
- 13.Paul SJ, Scharer P. Effect of provisional cements on the bond strength of various adhesive bonding systems on dentine. J Oral Rehabil. 1997;24(1):8–14. doi: 10.1046/j.1365-2842.1997.00484.x [DOI] [PubMed] [Google Scholar]
- 14.Dietschi D, Magne P, Holz J. Bonded to tooth ceramic restorations: in vitro evaluation of the efficiency and failure mode of two modern adhesives. Schweiz Monatsschr Zahnmed. 1995;105(3):299–305. [PubMed] [Google Scholar]
- 15.Magne P, Douglas WH. Porcelain veneers: dentin bonding optimization and biomimetic recovery of the crown. Int J Prosthodont. 1999;12(2):111–121. [PubMed] [Google Scholar]
- 16.Dietschi D, Herzfeld D. In vitro evaluation of marginal and internal adaptation of class II resin composite restorations after thermal and occlusal stressing. Eur J Oral Sci. 1998;106(6):1033–1042. doi: 10.1046/j.0909-8836.1998.eos106609.x [DOI] [PubMed] [Google Scholar]
- 17.Nikaido T, Tagami J, Yatani H, et al. Concept and clinical application of the resin-coating technique for indirect restorations. Dent Mater J. 2018;37(2):192–196. doi: 10.4012/dmj.2017-253 [DOI] [PubMed] [Google Scholar]
- 18.Magne P. IDS: Immediate Dentin Sealing (IDS) for tooth preparations. J Adhes Dent. 2014;16(6):594. doi: 10.3290/j.jad.a33324 [DOI] [PubMed] [Google Scholar]
- 19.Magne P, So WS, Cascione D. Immediate dentin sealing supports delayed restoration placement. J Prosthet Dent. 2007;98(3):166–174. doi: 10.1016/S0022-3913(07)60052-3 [DOI] [PubMed] [Google Scholar]
- 20.Nawareg MM, Zidan AZ, Zhou J, Chiba A, Tagami J, Pashley DH. Adhesive sealing of dentin surfaces in vitro: a review. Am J Dent. 2015;28(6):321–332. [PMC free article] [PubMed] [Google Scholar]
- 21.Ferreira-Filho RC, Ely C, Amaral RC, et al. Effect of different adhesive systems used for immediate dentin sealing on bond strength of a self-adhesive resin cement to dentin. Oper Dent. 2018;43(4):391–397. doi: 10.2341/17-023-L [DOI] [PubMed] [Google Scholar]
- 22.Chersoni S, Suppa P, Grandini S, et al. In vivo and in vitro permeability of one-step self-etch adhesives. J Dent Res. 2004;83(6):459–464. doi: 10.1177/154405910408300605 [DOI] [PubMed] [Google Scholar]
- 23.Sauro S, Pashley DH, Montanari M, et al. Effect of simulated pulpal pressure on dentin permeability and adhesion of self-etch adhesives. Dent Mater. 2007;23(6):705–713. doi: 10.1016/j.dental.2006.06.010 [DOI] [PubMed] [Google Scholar]
- 24.Gregoire G, Joniot S, Guignes P, Millas A. Dentin permeability: self-etching and one-bottle dentin bonding systems. J Prosthet Dent. 2003;90(1):42–49. doi: 10.1016/s0022-3913(03)00258-0 [DOI] [PubMed] [Google Scholar]
- 25.Rueggeberg FA, Margeson DH. The effect of oxygen inhibition on an unfilled/filled composite system. J Dent Res. 1990;69(10):1652–1658. doi: 10.1177/00220345900690100501 [DOI] [PubMed] [Google Scholar]
- 26.Erickson RL. Mechanism and clinical implications of bond formation for two dentin bonding agents. Am J Dent. 1989;2:117–123. [PubMed] [Google Scholar]
- 27.Magne P, Nielsen B. Interactions between impression materials and immediate dentin sealing. J Prosthet Dent. 2009;102(5):298–305. doi: 10.1016/S0022-3913(09)60178-5 [DOI] [PubMed] [Google Scholar]
- 28.Ghiggi PC, Steiger AK, Marcondes ML, Mota EG, Burnett LHJ, Spohr AM. Does immediate dentin sealing influence the polymerization of impression materials? Eur J Dent. 2014;8(3):366–372. doi: 10.4103/1305-7456.137650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khakiani MI, Kumar V, Pandya HV, Nathani TI, Verma P, Bhanushali NV. Effect of immediate dentin sealing on polymerization of elastomeric materials: an ex vivo randomized controlled trial. Int J Clin Pediatr Dent. 2019;12(4):288–292. doi: 10.5005/jp-journals-10005-1657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bruzi G, Carvalho MA, Maia HP, Giannini M, Magne P. Are there combinations of resin liners and impression materials not compatible with IDS technique? Am J Esthet Dent. 2013;3(3):200–208. [Google Scholar]
- 31.Jayasooriya PR, Pereira P, Nikaido T, Tagami J. Efficacy of a resin coating on bond strengths of resin cement to dentin. J Esthet Restor Dent. 2003;15(2):105–113; discussion 113. doi: 10.1111/j.1708-8240.2003.tb00325.x [DOI] [PubMed] [Google Scholar]
- 32.Udo T, Nikaido T, Ikeda M, et al. Enhancement of adhesion between resin coating materials and resin cements. Dent Mater J. 2007;26(4):519–525. doi: 10.4012/dmj.26.519 [DOI] [PubMed] [Google Scholar]
- 33.Sinjari B, D’Addazio G, Murmura G, et al. Avoidance of interaction between impression materials and tooth surface treated for immediate dentin sealing: an in vitro study. Materials (Basel). 2019;12(20):3454. doi: 10.3390/ma12203454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.da Silva CJR, Gonçalves ICS, Botelho MPJ, Guiraldo RD, Lopes MB, Ja G. Interactions between resin‑based temporary materials and immediate dentin sealing. Appl Adhes Sci. 2016;4(3). [Google Scholar]
- 35.Schoenbaum TR, Ercus S, Snowden J. Reverse spot bonding: a novel technique for provisionalization with immediate dentin sealing. Compend Contin Educ Dent. 2012;33(5):374–377. [PubMed] [Google Scholar]
- 36.Takimoto M, Ishii R, Iino M, et al. Influence of temporary cement contamination on the surface free energy and dentine bond strength of self-adhesive cements. J Dent. 2012;40(2):131–138. doi: 10.1016/j.jdent.2011.11.012 [DOI] [PubMed] [Google Scholar]
- 37.Watanabe EK, Yatani H, Ishikawa K, Suzuki K, Yamashita A. Pilot study of conditioner/primer effects on resin-dentin bonding after provisional cement contamination using SEM, energy dispersive x-ray spectroscopy, and bond strength evaluation measures. J Prosthet Dent. 2000;83(3):349–355. doi: 10.1016/s0022-3913(00)70139-9 [DOI] [PubMed] [Google Scholar]
- 38.Ribeiro JC, Coelho PG, Janal MN, Silva NR, Monteiro AJ, Fernandes CA. The influence of temporary cements on dental adhesive systems for luting cementation. J Dent. 2011;39(3):255–262. doi: 10.1016/j.jdent.2011.01.004 [DOI] [PubMed] [Google Scholar]
- 39.Hironaka NGL, Ubaldini ALM, Sato F, Giannini M, Terada RSS, Pascotto RC. Influence of immediate dentin sealing and interim cementation on the adhesion of indirect restorations with dual-polymerizing resin cement. J Prosthet Dent. 2018;119(4):678e1–678 e8. doi: 10.1016/j.prosdent.2018.02.001 [DOI] [PubMed] [Google Scholar]
- 40.Yap AU, Shah KC, Loh ET, Sim SS, Tan CC. Influence of eugenol-containing temporary restorations on bond strength of composite to dentin. Oper Dent. 2001;26(6):556–561. [PubMed] [Google Scholar]
- 41.Bayindir F, Akyil MS, Bayindir YZ. Effect of eugenol and non-eugenol containing temporary cement on permanent cement retention and microhardness of cured composite resin. Dent Mater J. 2003;22(4):592–599. doi: 10.4012/dmj.22.592 [DOI] [PubMed] [Google Scholar]
- 42.Leirskar J, Nordbo H. The effect of zinc oxide-eugenol on the shear bond strength of a commonly used bonding system. Endod Dent Traumatol. 2000;16(6):265–268. doi: 10.1034/j.1600-9657.2000.016006265.x [DOI] [PubMed] [Google Scholar]
- 43.Erkut S, Kucukesmen HC, Eminkahyagil N, Imirzalioglu P, Karabulut E. Influence of previous provisional cementation on the bond strength between two definitive resin-based luting and dentin bonding agents and human dentin. Oper Dent. 2007;32(1):84–93. doi: 10.2341/06-27 [DOI] [PubMed] [Google Scholar]
- 44.Brigagao VC, Barreto LFD, Goncalves KAS, et al. Effect of interim cement application on bond strength between resin cements and dentin: immediate and delayed dentin sealing. J Prosthet Dent. 2017;117(6):792–798. doi: 10.1016/j.prosdent.2016.09.015 [DOI] [PubMed] [Google Scholar]
- 45.Sailer I, Oendra AE, Stawarczyk B, Hammerle CH. The effects of desensitizing resin, resin sealing, and provisional cement on the bond strength of dentin luted with self-adhesive and conventional resincements. J Prosthet Dent. 2012;107(4):252–260. doi: 10.1016/S0022-3913(12)60070-5 [DOI] [PubMed] [Google Scholar]
- 46.Frankenberger R, Lohbauer U, Taschner M, Petschelt A, Nikolaenko SA. Adhesive luting revisited: influence of adhesive, temporary cement, cavity cleaning, and curing mode on internal dentin bond strength. J Adhes Dent. 2007;9(Suppl 2):269–273. [PubMed] [Google Scholar]
- 47.Augusti D, Re D, Özcan M. Removal of temporary cements following an immediate dentin hybridization approach: a comparison of mechanical and chemical methods for substrate cleaning. J Adhes Sci Technol. 2018;32(7):693–704. doi: 10.1080/01694243.2017.1381015 [DOI] [Google Scholar]
- 48.Dillenburg AL, Soares CG, Paranhos MP, Spohr AM, Loguercio AD, Burnett LH Jr. Microtensile bond strength of prehybridized dentin: storage time and surface treatment effects. J Adhes Dent. 2009;11(3):231–237. [PubMed] [Google Scholar]
- 49.Falkensammer F, Arnetzl GV, Wildburger A, Krall C, Freudenthaler J. Influence of different conditioning methods on immediate and delayed dentin sealing. J Prosthet Dent. 2014;112(2):204–210. doi: 10.1016/j.prosdent.2013.10.028 [DOI] [PubMed] [Google Scholar]
- 50.van den Breemer C, Ozcan M, Cune MS, Ayres AA, Van Meerbeek B, Gresnigt M. Effect of immediate dentin sealing and surface conditioning on the microtensile bond strength of resin-based composite to dentin. Oper Dent. 2019;44(6):E289–E298. doi: 10.2341/18-052-L [DOI] [PubMed] [Google Scholar]
- 51.van den Breemer CR, Ozcan M, Pols MR, Postema AR, Cune MS, Gresnigt MM. Adhesion of resin cement to dentin: effects of adhesive promoters, immediate dentin sealing strategies, and surface conditioning. Int J Esthet Dent. 2019;14(1):52–63. [PubMed] [Google Scholar]
- 52.Ozcan M, Barbosa SH, Melo RM, Galhano GA, Bottino MA. Effect of surface conditioning methods on the microtensile bond strength of resin composite to composite after aging conditions. Dent Mater. 2007;23(10):1276–1282. doi: 10.1016/j.dental.2006.11.007 [DOI] [PubMed] [Google Scholar]
- 53.Rodrigues SA Jr., Ferracane JL, Della Bona A. Influence of surface treatments on the bond strength of repaired resin composite restorative materials. Dent Mater. 2009;25(4):442–451. doi: 10.1016/j.dental.2008.09.009 [DOI] [PubMed] [Google Scholar]
- 54.Anžlovar A, Kiteska B, Cevc P, Kopač I. The role of an interfacial interpenetrating polymer network formation on the adhesion of resin composite layers in immediate dentin sealing. Int J Adhes Adhes. 2019;90:9–14. doi: 10.1016/j.ijadhadh.2019.01.009 [DOI] [Google Scholar]
- 55.Özcan M. Effect of mechanical and air-particle cleansing protocols of provisional cement on immediate dentin sealing layer and subsequent adhesion of resin composite cement. J Adhes Sci Technol. 2015;29(24):2731–2743. doi: 10.1080/01694243.2015.1087254 [DOI] [Google Scholar]
- 56.Stavridakis MM, Krejci I, Magne P. Immediate dentin sealing of onlay preparations: thickness of pre-cured dentin bonding agent and effect of surface cleaning. Oper Dent. 2005;30(6):747–757. [PubMed] [Google Scholar]
- 57.Spohr AM, Borges GA, Platt JA. Thickness of immediate dentin sealing materials and its effect on the fracture load of a reinforced all-ceramic crown. Eur J Dent. 2013;7(4):474–483. doi: 10.4103/1305-7456.120682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hashimoto M, Sano H, Yoshida E, et al. Effects of multiple adhesive coatings on dentin bonding. Oper Dent. 2004;29(4):416–423. [PubMed] [Google Scholar]
- 59.Ito S, Tay FR, Hashimoto M, et al. Effects of multiple coatings of two all-in-one adhesives on dentin bonding. J Adhes Dent. 2005;7(2):133–141. [PubMed] [Google Scholar]
- 60.Murata T, Maseki T, Nara Y. Effect of immediate dentin sealing applications on bonding of CAD/CAM ceramic onlay restoration. Dent Mater J. 2018;37(6):928–939. doi: 10.4012/dmj.2017-377 [DOI] [PubMed] [Google Scholar]
- 61.Choi KK, Condon JR, Ferracane JL. The effects of adhesive thickness on polymerization contraction stress of composite. J Dent Res. 2000;79(3):812–817. doi: 10.1177/00220345000790030501 [DOI] [PubMed] [Google Scholar]
- 62.D’Arcangelo C, Vanini L, Prosperi GD, et al. The influence of adhesive thickness on the microtensile bond strength of three adhesive systems. J Adhes Dent. 2009;11(2):109–115. [PubMed] [Google Scholar]
- 63.Figueiredo Reis A, Giannini M, Ambrosano GM, Chan DC. The effects of filling techniques and a low-viscosity composite liner on bond strength to class II cavities. J Dent. 2003;31(1):59–66. doi: 10.1016/s0300-5712(02)00122-7 [DOI] [PubMed] [Google Scholar]
- 64.Carvalho RM, Pegoraro TA, Tay FR, Pegoraro LF, Silva NR, Pashley DH. Adhesive permeability affects coupling of resin cements that utilise self-etching primers to dentine. J Dent. 2004;32(1):55–65. doi: 10.1016/j.jdent.2003.08.003 [DOI] [PubMed] [Google Scholar]
- 65.Duarte RM, de Goes MF, Montes MA. Effect of time on tensile bond strength of resin cement bonded to dentine and low-viscosity composite. J Dent. 2006;34(1):52–61. doi: 10.1016/j.jdent.2005.03.002 [DOI] [PubMed] [Google Scholar]
- 66.Santos-Daroz CB, Oliveira MT, Goes MF, Nikaido T, Tagami J, Giannini M. Bond strength of a resin cement to dentin using the resin coating technique. Braz Oral Res. 2008;22(3):198–204. doi: 10.1590/s1806-83242008000300002 [DOI] [PubMed] [Google Scholar]
- 67.Okuda M, Nikaido T, Maruoka R, Foxton RM, Tagami J. Microtensile bond strengths to cavity floor dentin in indirect composite restorations using resin coating. J Esthet Restor Dent. 2007;19(1):38–46; discussion 47–8. doi: 10.1111/j.1708-8240.2006.00062.x [DOI] [PubMed] [Google Scholar]
- 68.Ariyoshi M, Nikaido T, Foxton RM, Tagami J. Microtensile bond strengths of composite cores to pulpal floor dentin with resin coating. Dent Mater J. 2008;27(3):400–407. doi: 10.4012/dmj.27.400 [DOI] [PubMed] [Google Scholar]
- 69.Akehashi S, Takahashi R, Nikaido T, Burrow MF, Tagami J. Enhancement of dentin bond strength of resin cement using new resin coating materials. Dent Mater J. 2019;38(6):955–962. doi: 10.4012/dmj.2018-328 [DOI] [PubMed] [Google Scholar]
- 70.Magne P, Paranhos MP, Hehn J, Oderich E, Boff LL. Selective masking for thin indirect restorations: can the use of opaque resin affect the dentine bond strength of immediately sealed preparations? J Dent. 2011;39(10):707–709. doi: 10.1016/j.jdent.2011.07.005 [DOI] [PubMed] [Google Scholar]
- 71.Johnson GH, Hazelton LR, Bales DJ, Lepe X. The effect of a resin-based sealer on crown retention for three types of cement. J Prosthet Dent. 2004;91(5):428–435. doi: 10.1016/S0022391304000770 [DOI] [PubMed] [Google Scholar]
- 72.Patel P, Thummar M, Shah D, Pitti V. Comparing the effect of a resin based sealer on crown retention for three types of cements: an in vitro study. J Indian Prosthodont Soc. 2013;13(3):308–314. doi: 10.1007/s13191-013-0269-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dalby R, Ellakwa A, Millar B, Martin FE. Influence of immediate dentin sealing on the shear bond strength of pressed ceramic luted to dentin with self-etch resin cement. Int J Dent. 2012;2012:310702. doi: 10.1155/2012/310702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Giannini M, Takagaki T, Bacelar-Sa R, et al. Influence of resin coating on bond strength of self-adhesive resin cements to dentin. Dent Mater J. 2015;34(6):822–827. doi: 10.4012/dmj.2015-099 [DOI] [PubMed] [Google Scholar]
- 75.Santana VB, de Alexandre RS, Rodrigues JA, Ely C, Reis AF. Effects of immediate dentin sealing and pulpal pressure on resin cement bond strength and nanoleakage. Oper Dent. 2016;41(2):189–199. doi: 10.2341/15-150-L [DOI] [PubMed] [Google Scholar]
- 76.Van den Breemer CRG, Buijs GJ, Cune MS, et al. Prospective clinical evaluation of 765 partial glass-ceramic posterior restorations luted using photo-polymerized resin composite in conjunction with immediate dentin sealing. Clin Oral Investig. 2021;25(3):1463–1473. doi: 10.1007/s00784-020-03454-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yazigi C, Kern M, Chaar MS. Influence of various bonding techniques on the fracture strength of thin CAD/CAM-fabricated occlusal glass-ceramic veneers. J Mech Behav Biomed Mater. 2017;75:504–511. doi: 10.1016/j.jmbbm.2017.08.016 [DOI] [PubMed] [Google Scholar]
- 78.Ishii N, Maseki T, Nara Y. Bonding state of metal-free CAD/CAM onlay restoration after cyclic loading with and without immediate dentin sealing. Dent Mater J. 2017;36(3):357–367. doi: 10.4012/dmj.2016-289 [DOI] [PubMed] [Google Scholar]
- 79.van den Breemer CRG, Ozcan M, Cune MS, van der Giezen R, Kerdijk W, Gresnigt MMM. Effect of immediate dentine sealing on the fracture strength of lithium disilicate and multiphase resin composite inlay restorations. J Mech Behav Biomed Mater. 2017;72:102–109. doi: 10.1016/j.jmbbm.2017.04.002 [DOI] [PubMed] [Google Scholar]
- 80.Rigos AE, Dandoulaki C, Kontonasaki E, Kokoti M, Papadopoulou L, Koidis P. Effect of immediate dentin sealing on the bond strength of monolithic zirconia to human dentin. Oper Dent. 2019;44(4):E167–E179. doi: 10.2341/18-198-L [DOI] [PubMed] [Google Scholar]
- 81.Reboul T, Hoang Thai HA, Cetik S, Atash R. Comparison between shear forces applied on the overlay-dental tissue interface using different bonding techniques: an in vitro study. J Indian Prosthodont Soc. 2018;18(3):212–218. doi: 10.4103/jips.jips_165_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.van den Breemer CR, Gresnigt MM, Cune MS. Cementation of glass-ceramic posterior restorations: a systematic review. Biomed Res Int. 2015;2015:148954. doi: 10.1155/2015/148954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.El-Damanhoury HM, Gaintantzopoulou M. The effect of immediate dentin sealing and optical powder removal method on the fracture resistance of CAD/CAM-fabricated endocrowns. Int J Comput Dent. 2016;19(2):135–151. [PubMed] [Google Scholar]
- 84.Belleflamme MM, Geerts SO, Louwette MM, Grenade CF, Vanheusden AJ, Mainjot AK. No post-no core approach to restore severely damaged posterior teeth: an up to 10-year retrospective study of documented endocrown cases. J Dent. 2017;63:1–7. doi: 10.1016/j.jdent.2017.04.009 [DOI] [PubMed] [Google Scholar]
- 85.Burke FJ. Survival rates for porcelain laminate veneers with special reference to the effect of preparation in dentin: a literature review. J Esthet Restor Dent. 2012;24(4):257–265. doi: 10.1111/j.1708-8240.2012.00517.x [DOI] [PubMed] [Google Scholar]
- 86.Gresnigt MM, Cune MS, de Roos JG, Ozcan M. Effect of immediate and delayed dentin sealing on the fracture strength, failure type and Weilbull characteristics of lithiumdisilicate laminate veneers. Dent Mater. 2016;32(4):e73–81. doi: 10.1016/j.dental.2016.01.001 [DOI] [PubMed] [Google Scholar]
- 87.Gresnigt MMM, Cune MS, Schuitemaker J, et al. Performance of ceramic laminate veneers with immediate dentine sealing: an 11 year prospective clinical trial. Dent Mater. 2019;35(7):1042–1052. doi: 10.1016/j.dental.2019.04.008 [DOI] [PubMed] [Google Scholar]
- 88.Hofsteenge JW, Hogeveen F, Cune MS, Gresnigt MMM. Effect of immediate dentine sealing on the aging and fracture strength of lithium disilicate inlays and overlays. J Mech Behav Biomed Mater. 2020;110:103906. doi: 10.1016/j.jmbbm.2020.103906 [DOI] [PubMed] [Google Scholar]
- 89.Leesungbok R, Lee SM, Park SJ, et al. The effect of IDS (immediate dentin sealing) on dentin bond strength under various thermocycling periods. J Adv Prosthodont. 2015;7(3):224–232. doi: 10.4047/jap.2015.7.3.224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Suh BI. Oxygen-inhibited layer in adhesion dentistry. J Esthet Restor Dent. 2004;16(5):316–323. doi: 10.1111/j.1708-8240.2004.tb00060.x [DOI] [PubMed] [Google Scholar]
- 91.Papacchini F, Dall’Oca S, Chieffi N, et al. Composite-to composite microtensile bond strength in the repair of a microfilled hybrid resin: effect of surface treatment and oxygen inhibition. J Adhes Dent. 2007;9(1):25–31. [PubMed] [Google Scholar]
- 92.Fransson B, Oilo G, Gjeitanger R. The fit of metal-ceramic crowns, a Clinical Study. Dent Mater. 1985;1(5):197–199. doi: 10.1016/s0109-5641(85)80019-1 [DOI] [PubMed] [Google Scholar]
- 93.McLean JW, von Fraunhofer JA. The estimation of cement film thickness by an in vivo technique. Br Dent J. 1971;131(3):107–111. doi: 10.1038/sj.bdj.4802708 [DOI] [PubMed] [Google Scholar]
- 94.Grajower R, Zuberi Y, Lewinstein I. Improving the fit of crowns with die spacers. J Prosthet Dent. 1989;61(5):555–563. doi: 10.1016/0022-3913(89)90275-8 [DOI] [PubMed] [Google Scholar]
- 95.Kitayama S, Nasser NA, Pilecki P, et al. Effect of resin coating and occlusal loading on microleakage of class II computer-aided design/computer-aided manufacturing fabricated ceramic restorations: a Confocal Microscopic Study. Acta Odontol Scand. 2011;69(3):182–192. doi: 10.3109/00016357.2010.549504 [DOI] [PubMed] [Google Scholar]
- 96.Maruoka R, Nikaido T, Ikeda M, Ishizuka T, Foxton RM, Tagami J. Coronal leakage inhibition in endodontically treated teeth using resin-coating technique. Dent Mater J. 2006;25(1):97–103. doi: 10.4012/dmj.25.97 [DOI] [PubMed] [Google Scholar]
- 97.Schenke F, Hiller KA, Schmalz G, Federlin M. Marginal integrity of partial ceramic crowns within dentin with different luting techniques and materials. Oper Dent. 2008;33(5):516–525. doi: 10.2341/07-131 [DOI] [PubMed] [Google Scholar]
- 98.de Andrade OS, de Goes MF, Montes MA. Marginal adaptation and microtensile bond strength of composite indirect restorations bonded to dentin treated with adhesive and low-viscosity composite. Dent Mater. 2007;23(3):279–287. doi: 10.1016/j.dental.2006.01.028 [DOI] [PubMed] [Google Scholar]
- 99.Medina AD, de Paula AB, de Fucio SBP, Puppin-Rontani RM, Correr-Sobrinho LC, Sinhoreti MAC. Marginal adaptation of indirect restorations using different resin coating protocols. Braz Dent J. 2012;23(6):672–678. doi: 10.1590/S0103-64402012000600008 [DOI] [PubMed] [Google Scholar]
- 100.Medina ADC, de Paula AB, Naufel FS, Puppin-rontani RM, Correr-Sobrinho L, Sinhoreti MA. Nanoleakage in indirect composite restorations using different combinations of resin coating technique. Appl Adhes Sci. 2014;2(5):5. doi: 10.1186/2196-4351-2-5 [DOI] [Google Scholar]
- 101.De Rose L, Krejci I, Bortolotto T. Immediate endodontic access cavity sealing: fundamentals of a new restorative technique. Odontology. 2015;103(3):280–285. doi: 10.1007/s10266-014-0174-1 [DOI] [PubMed] [Google Scholar]
- 102.van den Breemer C, Gresnigt M, Ozcan M, Kerdijk W, Cune MS. Prospective randomized clinical trial on the survival of lithium disilicate posterior partial crowns bonded using immediate or delayed dentin sealing: short-term results on tooth sensitivity and patient satisfaction. Oper Dent. 2019;44(5):E212–E222. doi: 10.2341/18-047-C [DOI] [PubMed] [Google Scholar]
- 103.Hu J, Zhu Q. Effect of immediate dentin sealing on preventive treatment for postcementation hypersensitivity. Int J Prosthodont. 2010;23(1):49–52. [PubMed] [Google Scholar]
- 104.Edelhoff D, Sorensen JA. Tooth structure removal associated with various preparation designs for posterior teeth. Int J Periodontics Restorative Dent. 2002;22(3):241–249. [PubMed] [Google Scholar]
- 105.Camps J, Dejou J, Remusat M, About I. Factors influencing pulpal response to cavity restorations. Dent Mater. 2000;16(6):432–440. doi: 10.1016/s0109-5641(00)00041-5 [DOI] [PubMed] [Google Scholar]
- 106.Angeletaki F, Gkogkos A, Papazoglou E, Kloukos D. Direct versus indirect inlay/onlay composite restorations in posterior teeth. A systematic review and meta-analysis. J Dent. 2016;53:12–21. doi: 10.1016/j.jdent.2016.07.011 [DOI] [PubMed] [Google Scholar]
- 107.da Veiga AM, Cunha AC, Ferreira DM, et al. Longevity of direct and indirect resin composite restorations in permanent posterior teeth: a systematic review and meta-analysis. J Dent. 2016;54:1–12. doi: 10.1016/j.jdent.2016.08.003 [DOI] [PubMed] [Google Scholar]
- 108.Shu X, Mai QQ, Blatz M, Price R, Wang XD, Zhao K. Direct and indirect restorations for endodontically treated teeth: a systematic review and meta-analysis, IAAD 2017 consensus conference paper. J Adhes Dent. 2018;20(3):183–194. doi: 10.3290/j.jad.a40762 [DOI] [PubMed] [Google Scholar]
- 109.Wassell RW, Walls AW, McCabe JF. Direct composite inlays versus conventional composite restorations: three-year clinical results. Br Dent J. 1995;179(9):343–349. doi: 10.1038/sj.bdj.4808919 [DOI] [PubMed] [Google Scholar]
- 110.Nattress BR, Youngson CC, Patterson CJ, Martin DM, Ralph JP. An in vitro assessment of tooth preparation for porcelain veneer restorations. J Dent. 1995;23(3):165–170. doi: 10.1016/0300-5712(95)93574-l [DOI] [PubMed] [Google Scholar]
- 111.Goodacre CJ, Campagni WV, Aquilino SA. Tooth preparations for complete crowns: an art form based on scientific principles. J Prosthet Dent. 2001;85(4):363–376. doi: 10.1067/mpr.2001.114685 [DOI] [PubMed] [Google Scholar]
- 112.Chai H. On the mechanical properties of tooth enamel under spherical indentation. Acta Biomater. 2014;10(11):4852–4860. doi: 10.1016/j.actbio.2014.07.003 [DOI] [PubMed] [Google Scholar]
- 113.Arana-Chavez VE, Massa LF. Odontoblasts: the cells forming and maintaining dentine. Int J Biochem Cell Biol. 2004;36(8):1367–1373. doi: 10.1016/j.biocel.2004.01.006 [DOI] [PubMed] [Google Scholar]
- 114.Kawashima N, Okiji T. Odontoblasts: specialized hard-tissue-forming cells in the dentin-pulp complex. Congenit Anom (Kyoto). 2016;56(4):144–153. doi: 10.1111/cga.12169 [DOI] [PubMed] [Google Scholar]
- 115.Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: single crowns (SCs). Dent Mater. 2015;31(6):603–623. doi: 10.1016/j.dental.2015.02.011 [DOI] [PubMed] [Google Scholar]
- 116.Choi YS, Cho IH. An effect of immediate dentin sealing on the shear bond strength of resin cement to porcelain restoration. J Adv Prosthodont. 2010;2(2):39–45. doi: 10.4047/jap.2010.2.2.39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Islam MR, Takada T, Weerasinghe DS, et al. Effect of resin coating on adhesion of composite crown restoration. Dent Mater J. 2006;25(2):272–279. doi: 10.4012/dmj.25.272 [DOI] [PubMed] [Google Scholar]
- 118.Sag BU, Bektas OO. Effect of immediate dentin sealing, bonding technique, and restorative material on the bond strength of indirect restorations. Braz Dent Sci. 2020;23(2). doi: 10.14295/bds.2020.v23i2.1923 [DOI] [Google Scholar]
- 119.Oliveira L, Mota EG, Borges GA, Burnett LH Jr., Spohr AM. Influence of immediate dentin sealing techniques on cuspal deflection and fracture resistance of teeth restored with composite resin inlays. Oper Dent. 2014;39(1):72–80. doi: 10.2341/12-100-L [DOI] [PubMed] [Google Scholar]
- 120.Shafiei F, Aghaei T, Jowkar Z. Effect of proanthocyanidin mediated immediate and delayed dentin sealing on the strength of premolars restored with composite resin inlay. J Clin Exp Dent. 2020;12(3):e235–e241. doi: 10.4317/jced.55942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zorba YO, Ilday NO, Bayindir YZ, Demirbuga S. Comparing the shear bond strength of direct and indirect composite inlays in relation to different surface conditioning and curing techniques. Eur J Dent. 2013;7(4):436–441. doi: 10.4103/1305-7456.120679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Özcan M. Effect ofdelayinlayeringontheincrementaladhesionofindirectdental composite resins. Int J Adhes Adhes. 2012;39:15–20. [Google Scholar]
- 123.Ferracane JL, Stansbury JW, Burke FJ. Self-adhesive resin cements - chemistry, properties and clinical considerations. J Oral Rehabil. 2011;38(4):295–314. doi: 10.1111/j.1365-2842.2010.02148.x [DOI] [PubMed] [Google Scholar]
- 124.Papacchini F, Dall’Oca S, Chieffi N, et al. Composite-to-composite microtensile bond strength in the repair of a microfilled hybrid resin: effect of surface treatment and oxygen inhibition. J Adhes Dent. 2006;8(6). [PubMed] [Google Scholar]
- 125.Vallittu PK. Interpenetrating Polymer Networks (IPNs) in dental polymers and composites. J Adhes Sci Technol. 2009;23(7–8):961–972. doi: 10.1163/156856109X432785 [DOI] [Google Scholar]
- 126.Benetti AR, Peutzfeldt A, Lussi A, Flury S. Resin composites: modulus of elasticity and marginal quality. J Dent. 2014;42(9):1185–1192. doi: 10.1016/j.jdent.2014.07.004 [DOI] [PubMed] [Google Scholar]
- 127.Afroz S, Tripathi A, Chand P, Shanker R. Stress pattern generated by different post and core material combinations: a Photoelastic Study. Indian J Dent Res. 2013;24(1):93–97. doi: 10.4103/0970-9290.114959 [DOI] [PubMed] [Google Scholar]
- 128.Tomita Y, Uechi J, Konno M, Sasamoto S, Iijima M, Mizoguchi I. Accuracy of digital models generated by conventional impression/plaster-model methods and intraoral scanning. Dent Mater J. 2018;37(4):628–633. doi: 10.4012/dmj.2017-208 [DOI] [PubMed] [Google Scholar]
- 129.Bohner L, Gamba DD, Hanisch M, et al. Accuracy of digital technologies for the scanning of facial, skeletal, and intraoral tissues: a systematic review. J Prosthet Dent. 2019;121(2):246–251. doi: 10.1016/j.prosdent.2018.01.015 [DOI] [PubMed] [Google Scholar]
- 130.Watanabe EK, Yamashita A, Imai M, Yatani H, Suzuki K. Temporary cement remnants as an adhesion inhibiting factor in the interface between resin cements and bovine dentin. Int J Prosthodont. 1997;10(5):440–452. [PubMed] [Google Scholar]
- 131.Silva BPD, Stanley K, Gardee J. Laminate veneers: preplanning and treatment using digital guided tooth preparation. J Esthet Restor Dent. 2020;32(2):150–160. doi: 10.1111/jerd.12571 [DOI] [PubMed] [Google Scholar]
- 132.Sargeant JM, Kelton DF, O’Connor AM. Study designs and systematic reviews of interventions: building evidence across study designs. Zoonoses Public Health. 2014;61(Suppl 1):10–17. doi: 10.1111/zph.12127 [DOI] [PubMed] [Google Scholar]
- 133.Rocca GT, Rizcalla N, Krejci I. Fiber-reinforced resin coating for endocrown preparations: a technical report. Oper Dent. 2013;38(3):242–248. doi: 10.2341/12-139-TR [DOI] [PubMed] [Google Scholar]
- 134.Fennis WM, Tezvergil A, Kuijs RH, et al. In vitro fracture resistance of fiber reinforced cusp-replacing composite restorations. Dent Mater. 2005;21(6):565–572. doi: 10.1016/j.dental.2004.07.019 [DOI] [PubMed] [Google Scholar]
- 135.Bijelic-Donova J, Keulemans F, Vallittu PK, Lassila LVJ. Direct bilayered biomimetic composite restoration: the effect of a cusp-supporting short fiber-reinforced base design on the chewing fracture resistance and failure mode of molars with or without endodontic treatment. J Mech Behav Biomed Mater. 2020;103:103554. doi: 10.1016/j.jmbbm.2019.103554 [DOI] [PubMed] [Google Scholar]
- 136.Nikaido T, Nakaoki Y, Ogata M, Foxton R, Tagami J. The resin-coating technique. Effect of a single-step bonding system on dentin bond strengths. J Adhes Dent. 2003;5(4):293–300. [PubMed] [Google Scholar]
- 137.Terry AD, Powers JM, Paul SJ. Immediate dentin sealing technique. Dent Today. 2009;28(9):140–141. [PubMed] [Google Scholar]
- 138.Lee JI, Park SH. The effect of three variables on shear bond strength when luting a resin inlay to dentin. Oper Dent. 2009;34(3):288–292. doi: 10.2341/08-82 [DOI] [PubMed] [Google Scholar]
- 139.Magne P, Boff LL, Oderich E, Cardoso AC. Computer-aided-design/computer-assisted-manufactured adhesive restoration of molars with a compromised cusp: effect of fiber-reinforced immediate dentin sealing and cusp overlap on fatigue strength. J Esthet Restor Dent. 2012;24(2):135–146. doi: 10.1111/j.1708-8240.2011.00433.x [DOI] [PubMed] [Google Scholar]
- 140.Perugia C, Ferraro E, Docimo R. Immediate dentin sealing in indirect restorations of dental fractures in paediatric dentistry. Eur J Paediatr Dent. 2013;14(2):146–149. [PubMed] [Google Scholar]
- 141.Rocca GT, Rizcalla N, Krejci I, Dietschi D. Evidence-based concepts and procedures for bonded inlays and onlays. Part II. Guidelines for cavity preparation and restoration fabrication. Int J Esthet Dent. 2015;10(3):392–413. [PubMed] [Google Scholar]
- 142.Nikaido T, Inoue G, Takagaki T, Takahashi R, Sadr A, Tagami J. Resin coating technique for protection of pulp and increasing bonding in indirect restoration. Curr Oral Health Rep. 2015;2(2):81–86. doi: 10.1007/s40496-015-0046-y [DOI] [Google Scholar]
- 143.Goldberg J, Guth JF, Magne P. Accelerated fatigue resistance of thick CAD/CAM composite resin overlays bonded with light- and dual-polymerizing luting resins. J Adhes Dent. 2016;18(4):341–348. doi: 10.3290/j.jad.a36515 [DOI] [PubMed] [Google Scholar]
- 144.Qanungo A, Aras MA, Chitre V, Mysore A, Amin B, Daswani SR. Immediate dentin sealing for indirect bonded restorations. J Prosthodont Res. 2016;60(4):240–249. doi: 10.1016/j.jpor.2016.04.001 [DOI] [PubMed] [Google Scholar]
- 145.Lima MF, Maciel CM, Correia AMO, Griza S, Mendonça AAMD. Effect of temporary cements on the bond strength of a resin cement to a pre-hybridized dentin. Bioscience J. 2017;33(1):247–256. doi: 10.14393/BJ-v33n1a2017-34668 [DOI] [Google Scholar]
- 146.Fouda HOT. Post-Operative Hyper-Sensitivity Assessment After Immediate versus Delayed Dentine Sealing in Indirect Tooth Colored Restorations: Randomized Controlled Clinical Trial. Cairo University; 2019. [Google Scholar]
- 147.Hayashi K, Maeno M, Nara Y. Influence of immediate dentin sealing and temporary restoration on the bonding of CAD/CAM ceramic crown restoration. Dent Mater J. 2019;38(6):970–980. doi: 10.4012/dmj.2018-313 [DOI] [PubMed] [Google Scholar]
- 148.van den Breemer CRG, Cune MS, Ozcan M, Naves LZ, Kerdijk W, Gresnigt MMM. Randomized clinical trial on the survival of lithium disilicate posterior partial restorations bonded using immediate or delayed dentin sealing after 3 years of function. J Dent. 2019;85:1–10. doi: 10.1016/j.jdent.2019.02.001 [DOI] [PubMed] [Google Scholar]
- 149.Rozan S, Takahashi R, Nikaido T, Tichy A, Tagami J. CAD/CAM-fabricated inlay restorations: can the resin-coating technique improve bond strength and internal adaptation? Dent Mater J. 2020;39(6):941–949. doi: 10.4012/dmj.2019-309 [DOI] [PubMed] [Google Scholar]
- 150.Cesca R, Colombo V, Ernst B, Gallo LM, Ozcan M. Tensile strength and failure types of direct and indirect resin composite copings for perio-overdentures luted using different adhesive cementation modalities. Materials (Basel). 2020;13(16):3517. doi: 10.3390/ma13163517 [DOI] [PMC free article] [PubMed] [Google Scholar]