Abstract
Although morbidity and mortality rates are declining for acute coronary syndrome (ACS) in most high-income countries, it is rising at an alarming pace for low to middle income countries (LMICs). A major factor that is contributing to the poor clinical outcomes among LMICs is largely due to prehospital treatment delays. This systematic review was conducted to determine the mean length of time from symptom onset to treatment in LMICs and the sociodemographic, clinical and health system characteristics that contribute to treatment delays. We conducted a comprehensive review of the relevant literature published in English between January 1990 through May 2020 using predefined inclusion and exclusion criteria. Twenty-nine studies were included and time to treatment was defined from ACS symptom onset to first medical contact and dichotomized further as less than or >12-hours. The mean time from symptom onset to first medical contact was 12.7 h which ranged from 10-minutes to 96 h. There was consensus among studies that being older, female, illiterate, living in a rural area, and financially limited was associated with longer treatment delays. Lack of a developed emergency transportation system, poor communication and organization between community facilities and interventional facilities were also cited as major contributors for ACS treatment delays. Findings from this systematic review provide future directions to potentially reduce prehospital delays in LMICs and improve ACS outcomes.
Keywords: Acute coronary syndrome, Low to middle income countries, Prehospital treatment delay
1. Introduction
Over the last two decades, mortality rates from acute coronary syndrome (ACS) have markedly declined in high-income countries largely due to lifestyle risk factor reduction and treatment advancements in cardiovascular disease (CVD). Among low-to middle-income countries (LMICs) however, the prevalence of ACS is rising at an alarming pace, accounting for approximately 80% of the burden and 85% of the disability observed worldwide [1], [2], [3], [4]. Despite the disproportionate burden of ACS in LMICs, knowledge of patient characteristics, management and outcomes are primarily composed of data obtained from high-income countries [5].
Inadequate prehospital emergency medical services (EMS) and lack of coordination between facilities contribute to the poorer clinical outcomes observed in most LMICs [6]. In addition, access to interventional cardiology facilities and catheterization laboratories are exceedingly scarce in LMICs with the majority located in large, urban areas [6], [7], [8], [9]. Management guidelines for ST-segment elevation myocardial infarction (STEMI) focus on the avoidance of treatment delays and achieving reperfusion therapy as soon as possible. The best clinical outcomes for a STEMI occurs when the time from first medical contact to diagnosis is within 10 min of arrival at a hospital equipped for reperfusion therapy. Pharmacological interventions such as fibrinolytics have the best patient outcomes if infused within 30 min to one hour of symptom onset, with little efficacy observed after 6 h. Percutaneous coronary intervention (PCI) is most effective when used within 2-hours of symptom onset, although some efficacy is reported up to 12-hours with little improvement reported after 24-hours. Current American Heart Association/American College of Cardiology (AHA/ACC) and European (ESC) guidelines provide strong evidence of superior clinical outcomes, fewer complications and lower mortality if reperfusion therapy efforts are initiated even earlier, within one-hour window of symptom onset [10], [11], [12]. In most LMICs however, the time from symptom onset to treatment is often delayed well beyond the time frame for optimal or effective ACS management and remains a formidable challenge [2], [5].
The purpose of this systematic review was to identify the average length of time from symptom onset to first medical contact in LMICs, and to determine sociodemographic, clinical and health system characteristics that influence prehospital treatment delay for ACS.
2. Methods
2.1. Search strategy
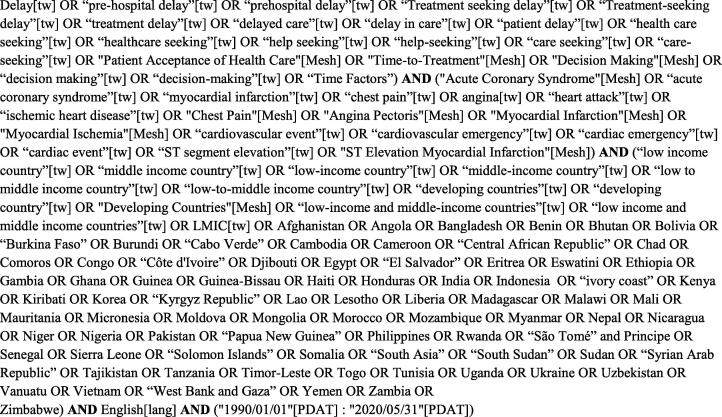
The PRISMA recommendations guided the procedures used in this systematic review [13]. The protocol for the review was registered at PROSPERO (CRD42020202812). A comprehensive literature search was undertaken to identify studies meeting the inclusion criteria. The search strategies were developed and conducted by an experienced medical librarian (SL) with input from the team members. An initial search strategy was drafted for testing in PubMed using keywords from pre-identified sentinel articles related to the study objectives. The draft search results were assessed by the team and terms revised and again tested in PubMed. The search terms were then translated for each additional literature database and grey literature resources appropriate to the study topic. The searches combined controlled vocabulary supplemented with keywords related to the concepts of acute coronary syndrome (e.g. chest pain, angina, ST segment elevation), delayed treatment (treatment seeking delay, time-to-treatment, time factors), and low- to middle-income countries. The search was limited to studies published between January 1, 1990 to May 31, 2020 and in the English language.
Finalized tested searches were undertaken on May 7, 2020. The six bibliographic databases searched were CINAHL, Embase.com, Global Health (Pro Quest), PsycInfo, PubMed, and Web of Science Core Collection. In addition to the grey literature obtained from Embase.com and Web of Science, other grey literature sources searched were Africa Index Medicus, African Journals OnLine, Europe PMC, Google Scholar, Networked Digital Library of Theses and Dissertations, OpenAIRE, Open Grey, ProQuest Dissertations and Theses Global, and Scientific Electronic Library Online (SciELO). Google was hand searched. Search strategy details for PubMed are provided in Fig. 1. Full searches for all databases and grey literature are summarized in the accompanying Supplementary Material.
Fig. 1.
PubMed Search Strategy.
2.2. Inclusion criteria
The following were inclusion criteria: a) studies conducted in low to middle income countries as defined by the World Bank (2016), b) study designs including systematic reviews, meta analyses, cross sectional, observational, case control, randomized controlled trials, prospective and retrospective, c) adults diagnosed with ACS, myocardial infarction with ST- elevation (STEMI), myocardial infarction with non-ST-segment elevation (NSTEMI), unstable angina (UA), and d) time reported from symptom onset to first medical contact was documented.
2.3. Exclusion criteria
Studies were excluded if: a) an admission diagnosis other than ACS, MI, STEMI, NSTEMI or UA b) documentation of symptom onset and time to first medical contact was not reported, c) qualitative or narrative study methodology was used. Characteristics influencing time to treatment and a brief description of the included studies are presented in Table 1.
Table 1.
Factors influencing pre-hospital delay times for acute coronary syndrome in LMICs.
|
Studies where majority had <12 h of pre-hospital delay time | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Study | Design and Setting | Sample Size | Patient Characteristics | Major outcome | Major Findings | Selection | Comparability | Outcome | Rating |
| Ahmed, et al., 2018 [24] |
Cross-sectional, descriptive. 3 tertiary care hospitals in Pakistan |
280 | Mean age 67.9; > 70% male. 130 (n = 46.4%) were diabetic | Time to treatment between diabetics and nondiabetics with STEMI or NSTEMI. | Non-diabetics (n = 54, 36%) mean delay time was 1–3 hrs compared to 3–6 hrs for diabetics (n = 54, 41.5%). Of those presenting after 6 h, majority (n = 66, 88.0%) did not believe that they were experiencing an MI. Self-medication (36.0%) and traffic (22.7%) were major reasons for delay time. | *** ** ** | Good | ||
| Allana, et al., 2015 [33] |
Descriptive, cross-sectional comparative study. 2 tertiary care hospitals in Pakistan | 249 | Males 53.4% and females 46.6%. Mean age men (56.46 ± 11.67); women 55.77 ± 11.77. Women were more likely hypertensive, diabetic, and have prior ACS. | Determine gender differences in time to treatment. | The median prehospital delay time for women was 7 h, compared to 3.5 h among men. Women delayed due to social factors. Men delayed for individual factors. | *** ** ** | Good | ||
| Allana, et al., 2018 [17] |
Comparative, cross-sectional. 2 tertiary care hospitals |
Same as above | Males 53.4% and females 46.6%. Mean age men (56.46 ± 11.67); women 55.77 ± 11.77. | To explore gender differences in ACS symptoms, knowledge of symptoms, and perceived urgency of treatment. | Atypical symptoms were experienced by more women, and perceived symptoms as another cause and not urgent. Only 47.3% (n = 118) had prior knowledge of ACS. Very few 4% (n = 10) were aware of treatment options. | *** ** ** | Good | ||
| Bandara, et al., 2015 [37] |
Observational with one year follow-up. 1 tertiary care hospital in Sri Lanka | 81 | Mean age 61.7 ± 10.7. Males (74%) | Presentation, management, and outcomes of acute STEMI with follow-up over 1-year. | Median time between symptom onset and hospital presentation was 60 min (mean 212 min). Thrombolysis was performed in 73% of patients. The major reason for not providing thrombolysis was prehospital delay time. Median door-to-needle time was 64 min (mean, 98 min). Only 16.9% of patients received thrombolysis within 30 min, and none underwent primary PCI. One-year mortality rate was 12.3%. Only 7.3% received coronary intervention post infarction. |
*** ** ** | Good | ||
| Bezdah, et al., 2020 [19] |
Observational, follow-up at one-year. 1 tertiary care hospital Tunisia. | 445 | Male (79%), mean age 60 ± 12. | Factors influencing first medical contact (FMC). | The average time of FMC was 4.27 ± 5.30 h. Longer FMC among women, elderly, diabetics and those with a history of myocardial infarction. Female gender was the only independent factor related to a longer FMC-delay (adjusted OR = 1.87; P = 0.002). Patients who were carried by an ambulance or seen directly in hospital emergency initially had significantly shorter delay time than those who visited a private doctor. | * * * | Poor | ||
| Dakota, et al., 2020 [26] |
Retrospective, cross-sectional. Jakarta, Indonesia registry database | 1076 | Median age was 55 (range 48–61). Males, 86%, all were acute STEMI and all were transported by ambulance. | Door in (DI) to door out (DO) time, total ischemic time, delay time | Median DI-DO time was 180 min; ischemic time 461 min. Only 63 (n = 6.4%) arrived within 60-minutes. Women had higher risk of longer DI-DO time > 120 min. Slow referral at initial hospitals increased DI-DO time. | *** ** ** | Good | ||
| Dhungel et al., 2018 [18] |
Cross-sectional, observational. 1 tertiary care hospital in Nepal | 79 | All patients undergoing primary PCI; rescue and elective PCIs were excluded. | Door to Balloon time (DTB) and factors that influence it. | The median DTB (DBT) was 79 min. Forty-six (58.2%) had a DTB time less than 90 min. DTB time was significantly shorter with direct visit vs transfer (p = 0.029). No significant DTB differences were found for sociodemographic or clinical variables. | ** * * | Fair | ||
| Doddipalli et al., 2018 [41] |
Prospective, cross-sectional, observational. 1 tertiary cardiac care center in India | 346 | Mean age 55.3 ± 12.1 years; male gender n = 277 (80%), majority lived in rural areas | Factors contributing to longer ischemic times in STEMI patients undergoing primary PCI. | Major factors contributing to longer ischemic included symptom recognition 150.2 ± 140.5 min. and transportation time, much longer if EMS was not utilized. Mortality and poorer outcomes with longer ischemic and DTB time. |
** ** ** | Fair | ||
| George et al., 2017 [20] |
Retrospective, descriptive cross- sectional study. 1 tertiary care center in south India | 96 | Mean age was 55 ± 11 years; male gender n = 78 (81%); majority lived in rural areas (65%), STEMI diagnosis. | Time to treatment and reasons for delay. | The median patient decision delay was 75 min. Median from symptom onset to FMC was 120 min and to referral center 290 min. Longer prehospital delay was associated with rural location and using public transportation. Correct symptom interpretation, rapid progression of symptoms, perceived symptoms as urgent and ambulance use led to shorter prehospital delays. | *** ** ** | Good | ||
| Juwana et al., 2009 [36] |
Prospective, observational, cross-sectional. 1 tertiary care hospital in the Netherlands and Jakarta. | 596 total 568 in Zwolle and 28 in Jakarta |
Mean age was 62.5 years; 75% were male, all patients underwent primary PCI for STEMI diagnosis. | Compare patient characteristics and time to PCI treatment, PCI outcomes, | Time from symptom onset to FMC longer in Indonesian patients than in the Netherlands (413 ± 325 vs. 214 ± 202). DTB time was also longer (189 ± 127 vs. 49 ± 33 min). Indonesian patients were younger, had more severe CAD, smoked, more diabetics and have higher lipid levels. | ** ** ** | Fair | ||
| Khan et al., 2007 [32] |
Prospective, observational, cross-sectional. 1 tertiary care hospital in Pakistan | 720 | First AMI, mean age 54 years ± 12; 78% male. | Pre-hospital delay time in first MI and reasons for delay | The median (IQR) times to presentation was 3.04 (6.0) hours. 34% had FMC 6 h or more after symptoms. Only 36% arrived within 2 h of symptom onset. Two-thirds (66%) did not recognize the AMI symptoms, 81% were not aware of any symptoms of AMI, and only 6% could identify two or more symptoms of heart attack. Lack of knowledge of AMI symptoms and mild chest pain were associated with significantly longer delay times. |
*** ** ** | Good | ||
| Khursheed et al., 2015 [16] | Retrospective chart audit, cross-sectional. 1 tertiary care hospital in Pakistan |
230 | Mean age was 58.9 years ± 13.7, 62.6% (n = 144) were male. | Time to various treatments in ACS | Patients were seen by ED physicians in ≤ 30 min of arrival; 149 patients (74.1%) in ≤ 10 min, 36 (17.9%) in 11–30 min, and 16 (8.0%) after 30 min of triage. 60 patients (26.1%) met criteria for PCI; DTB time was ≤ 90 min in 29 (48%) of patients. | * ** * | Fair | ||
| Kim et al., 2019 [38] |
Retrospective, longitudinal, chart audit, descriptive. 1 rural hospital in Bangladesh | 164 | Mean age was 57.07(±12.40), 75% (n = 123) were male. All were STEMI | Evaluate the in-hospital clinical STEMI outcomes of treated in a rural hospital | The mean pain-to-door time was 472 min (7.87 h ± 12.40). Only 5.49% traveled by EMS which caused significant delay times. Non-thrombolysis group had significantly prolonged pain-to-door time (25.83 ± 29.20 h) when compared to thrombolytic group (4.17 ± 3.86 h). The average door-to-needle time was 38.28 min, and 62.50% (85/136) received streptokinase less than 30 min after arrival. Only 3 patients were referred to PCI capable hospital. The overall in-hospital mortality rate was 19.51%, MACE at 30 days, 23.17% (38/164), respectively. | ** * * | Fair | ||
| Lim et al., 2019 [35] |
Cross-sectional, descriptive. 2 tertiary care hospitals in Malaysia | 222 | Mean age 58 ± 11.9 years. 83.8% (n = 186) were males. | Pre-hospital factors affecting symptom-to-door time among STEMI patients dichotomized as less than 3 hrs and > 3 hrs. | Median symptom-to-door time was 130.5 (IQR 240) min, with 64% of subjects arriving early and 36% arriving late. Only 30.6% males arrived late, compared to 63.9% female patients. Patients who first sought treatment at a primary clinic exhibited a 2.8 greater odds of a longer delay time. Patients’ self-perceptions of their symptoms as cardiac had lower delay time versus those with atypical or recurrent chest pain. | *** ** ** | Good | ||
| Medagama et al., 2015 [40] |
Prospective, cross-sectional observational. 1 tertiary care hospital in Sri Lanka |
265 | Mean age was 63.2 ± 11.1 years; 55.1% (n = 141) were female. | Factors that influence management of ACS. | The median delay from symptom onset to hospital admission was shorter for STEMI patients at 60 min than for UA/NSTEMI patients at 120 min. Longer delays for those seeing a GP initially. Fifty-nine (70.2%) with STEMI underwent fibrinolytic therapy. Only 10 patients (16.9%) received thrombolytic therapy within 30 min, 28 (47.4%) within 60 min, and 39 (66%) within 90 min. Twenty (33.9%) received thrombolytic therapy>90 min after arriving at the hospital. MACE occurred in 11.7% with higher BMI and duration of diabetes the greatest predictors. | *** ** ** | Good | ||
| Mesas et al., 2018 [21] |
Observational, cross-sectional, descriptive. Tertiary care hospital in Brazil. | 50 | Mean age was 59 ± 10.5; 64% (n = 32) were male | Evaluate the individual components of reperfusion time (RT) in patients with STEMI. | The median reperfusion time (RT) was 430 min. Patients treated in intermediate care units showed a significant increase in system delay time; which accounted for 81.1% of RT; only 10% of patients were taken directly to referral center and only 23.5% used an ambulance. Patient delay time was approximately 40 min longer among those who answered, “I didn’t think it was serious.” | * * * | Poor | ||
| Mohan et al., 2018 [30] |
Prospective, cross-sectional, observational. 5 tertiary care hospitals in India | 619 | Age was dichotomized as less than 60 or > 60 years; mean age was 78.6% (n = 487) were males | Identify factors associated with prehospital delay time less than 6 hrs or > 6 hrs. | 58% presented within 6 hrs to the hospital, and 42% after 6 hrs. Prehospital delay > 6 hrs was significantly longer in the elderly, rural residents, when FMC was clinic and illiteracy. Correct symptom interpretation, being diabetic and EKG utilization at FMC reduced prehospital delay. When EKG was performed, approximately 80.7% of the patients received early reperfusion therapy. Ambulance awareness was present in 96% of patients, but only used by 5.3%. | **** ** ** | Good | ||
| Poorhosseini et al., 2019 [22] |
Cross-sectional, descriptive. 1 tertiary care hospital in Iran | 2103 | Mean age was 59.49 ± 11.79 years; 76.4% males. | Assess prehospital delay and it’s contributing factors in STEMI undergoing primary PCI. | Median pain to door (P2D) time was 279 (120–630) minutes. Female gender, being uneducated, self-transportation or referral from another hospital, atypical chest pain and history of hypertension were associated with significantly higher delay times. | *** ** ** | Good | ||
| Sriha et al., 2018 [34] |
Cross-sectional, descriptive. 14 emergency departments (8 academic centers, 7 regional) in Tunisia | 1173 | Mean age was 60 years, 67.4% were males; the majority were UA/NSTEMI (74.2%) | To describe ACS prevalence and management in emergency departments (EDs). | Two hours was the median duration between chest pain onset and ED arrival (IQR: 2–4 h). Pre-hospital delays, starting treatment delays and length of stay were significantly shorter in men, in STEMI cases and among younger patients. Hypertension, active smoking and type 2 diabetes were the most reported risk factors (53%). Emergency medical service transportation was used in 11.9% of cases. Pre-hospital delays, treatment delays and length of stay were significantly shorter in men, in STEMI cases and among younger patients. | *** ** ** | Good | ||
| Xavier et al., 2008 [31] |
Prospective, multicenter registry that included 89 hospitals in 50 cities from 10 regions in India | 20,937 | Mean age was 57.5 ± 12.1 years; STEMI patients were younger 56.3 ± 12.1 years than were those with non-STEMI or unstable angina 59.3 ± 11.8 years). Most patients were from lower middle n = 10, 737 (52.5%) and poor n = 3999 (19.6%) social classes. | Describe associated factors, treatments, and outcomes of patients with acute coronary syndrome | The median time from onset of symptoms to hospital presentation was 6 h. Patients with STEMI were younger and had shorter prehospital delay time than those with non-STEMI or unstable angina. The median time from hospital to thrombolysis was 50 min. Only about 5% used an ambulance. About three-quarters of the patients paid the total hospital costs out of their own pockets. Mortality varied by socioeconomic strata lowest (5.5%) in high income patients and highest (8.2%) in poor patients. | **** ** ** | Good | ||
| Acharya, et al. 2009 [23] |
Cross-sectional, descriptive. 1 tertiary academic referral center in Eastern Nepal |
100 | Age range 36–84, mean 62 ± 10.4; male to female ratio 1.6 to 1; 81% presented with chest pain | Reasons for delayed treatment. | Mean time to treatment was 32-hours; 20 hrs for residing in same city as referral center, 63 hrs for outside city, 39 hrs for seeking care at another facility. Lack of EMS, poor transportation, initial visit at local centers were leading reasons for delayed treatment. | ** * * |
Fair | ||
| Agrawal, et al., 2016 [39] |
Cross-sectional, descriptive. Academic tertiary care center hospital with interventional cardiac care unit in India. | 100 | Mean age was 58.9 years; 75% males; 65% were STEMI and 35% were NSTEMI | Examine patient characteristics of first-time admission for ACS and factors related to treatment delay. | Median time to reach hospital was 24 h with only 27% patients reaching hospital within 6 h. Among patients with STEMI only 43% received fibrinolytic therapy; 56.5% of diabetics presented after 24 h. Lack of EMS, financial constraints, lack of symptom recognition, lack of primary care referral were major reasons for treatment delay. | ** ** ** | Fair | ||
| Bogale, et al., 2019 [25] |
Retrospective, cross-sectional. 1 academic, tertiary care hospital, Ethiopia | 124 | Mean age was 56.3 ± 13.65. Males (75.8%). 72.6% were STEMI, 16.1% NSTEMI, 11.3% UA | Time to treatment and in-hospital mortality outcomes from ACS. | The average time from onset of ACS symptoms to presentation in the emergency department was 3.8 days (91.7 h). In-hospital mortality was 27.4%. LOS was 9.77 ± 6.42 days. Predictors of mortality were age, delay time, hypertension, Killip class III and IV, and STEMI diagnosis. A delay time of > 3 days increased mortality > 5-fold. | *** * ** | Fair | ||
| Desta, et al., 2020 [15] |
Retrospective, cross-sectional. 1 tertiary care hospital, Ethiopia | 151 | Mean age was 59.12 ± 12.98; 72.2% were males; STEMI (n = 110, 72.8%), NSTEMI (n = 23, 15.2%), UA (n = 18, 12%), 74% resided in urban areas. | Time to treatment and ACS outcomes. | The average time between onset of symptoms to hospital admission was 95.85 ± 145.68 h. Five (3.3%) patients presented within one hour onset of symptoms and 43% were admitted within 13–72 h. In-hospital mortality was 24.5%, hypertension was the most frequent (46.4%) ACS risk. Catheterization and PCI were performed in 27.1%, and 3.9%, respectively. Streptokinase was administered in seven (6.3%) patients with STEMI. Heart failure was most common complication (n = 64, 42.2%). | ** ** ** | Fair | ||
| Koirala et al., 2019 [42] |
Retrospective, cross-sectional chart audit. 1 tertiary care hospital in Nepal. | 232 | Mean age was 57.4 ± 12.9; 74.5% male. |
Clinical characteristics and outcomes for STEMI undergoing PCI | The average time of presentation after symptom onset was 17.5 h, earliest being 15 min. 66% of patients presented in less than 12 h of symptoms onset, 21% presented 12- hours of symptoms onset and 13% patients presented late. 87% had primary PCI, 13% had elective PCI. In-hospital mortality was 38.46%. Heart failure was the most common complication. | ** * * | Fair | ||
| Sharma et al., 2019 [29] |
Prospective, cross-sectional, observational. 1 tertiary care hospital in India. | 147 | Mean age was 58.7 ± 11.1 years; 70.7% (n = 104) were male | Characteristics of patients arriving > 12 h for treatment with cardiogenic shock (CS-STEMI) | Median time from symptom onset to care was 24 h (interquartile range 18–48 h); 101 patients (68.7%) presented ≥ 24 h after symptom onset. 53 patients (63.9%) underwent PCI at a median of 36 h (IQ 30–72) after symptom onset. Sixty-three patients (42.9%) died during initial hospitalization, of whom 20 (13.6%) died in the initial 24 h. | *** ** ** | Good | ||
| Shrestha et al., 2011 [27] |
Prospective, cross sectional, observational. 1 tertiary care hospital in Nepal. | 153 | Mean age 62 ± 12 years; the majority were males across STEMI, NSTEMI and UA diagnostic categories | Characteristics and outcomes of patients with ACS | 33% of all patients with ACS presented to the hospital after>48 h of chest pain. 24% of all patients came in within 6 h of the onset of symptoms, nearly one third had STEMI. 52% were illiterate and also had poor access to the hospital because of distance and/or financial constraints and had much longer prehospital delays. Only 20 (34%) received thrombolysis with Streptokinase. Heart failure was more common among those who were illiterate (61% vs. 44%, p less than 0.02). |
** ** * | Fair | ||
| Varwani et al., 2019 [28] |
Retrospective longitudinal. 1 tertiary care private hospital in Kenya. | 230 | Mean age was 60.5 ± 12.8 years. 101 had STEMI, 93 NSTEMI and 36 UA; over 80% were males in the STEMI and NSTEMI/UA groups. | Determine in-hospital and long-term (30-day and one-year) mortality rates of ACS. | Delayed presentation (more than six hours after symptom onset) occurred in 66.1% of patients. 49 received thrombolytic therapy while 19 patients underwent primary percutaneous intervention (PCI). Heart failure was the most common complication. 15 STEMI (14.9%) and three NSTEMI (2.3%) died in hospital. Heart failure most common complication. At the end of 30 days, 7.8% had died, and at the end of one year after event, 13.9% had died and was more common among STEMI. | ** * ** | Fair | ||
| Venkatesan et al., 2018 [14] |
Retrospective, cross-sectional, 1 tertiary care hospital in India | 93 | Majority were over 50 years of age and male. | Identify factors causing delay in treatment among AMI patients and compare the factors between timely and late treatment seeking groups. | Time range to seek care from symptom onset ranged from 10 and 5450 min. 28 patients sought care within 12 h (67%); 40% of male subjects and 83.33% of female subjects delayed treatment. The mean ACS knowledge score was higher among those with timely treatment (12.2745) than those who sought delayed treatment (5.7381). The mean symptom perception was more in timely treatment seeking group (3.6667) than in delayed treatment seeking group (1.3095). The mean perceived seriousness was more in timely treatment seeking group (4.7647) than in delayed treatment seeking group (1.8333). | ** * * | Fair | ||
A meta-analysis was not possible due to the differences in the factors assessed as well as the heterogeneity of inclusion and exclusion criteria among the included studies. Prehospital delay was defined as the time from symptom onset to the first medical contact. The delay time was further dichotomized into less than 12-hours, timely treatment decisions and >12 h, late treatment decisions).
2.4. Study selection
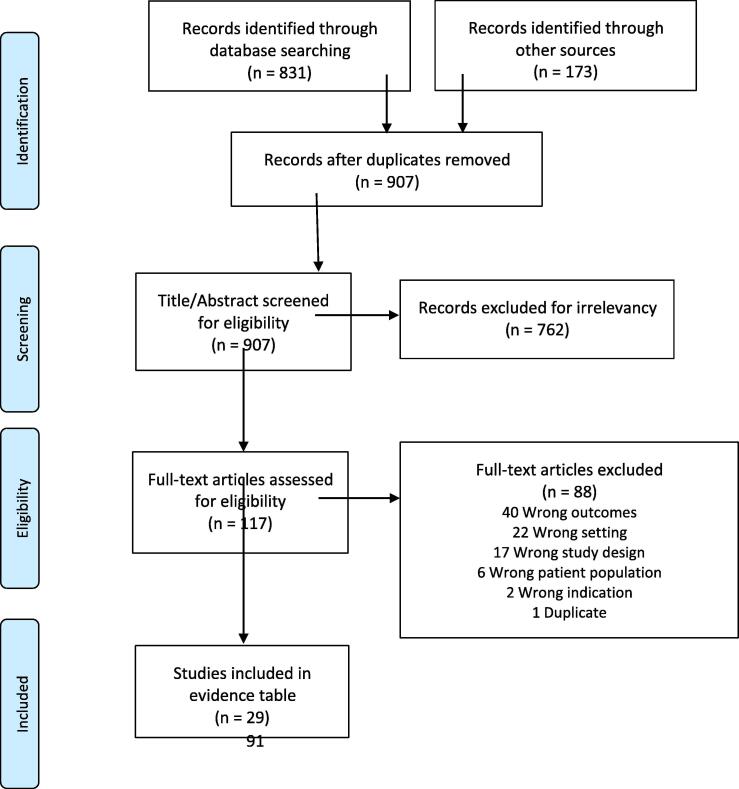
A total of 1004 studies were identified through the database searches, grey literature reviews, and review of article references. All identified citations were collated and uploaded to EndNote X9 and duplicates removed, leaving 907. Of these, 762 were excluded through title and abstract screening by two independent reviewers (LB, RG), leaving 117 eligible for full-text review. During the full-text review, the reviewers independently evaluated each article.
Disagreements between reviewers were resolved by consensus. An additional 88 articles were excluded that did not meet the inclusion criteria, leaving 29 articles that met all eligibility criteria for inclusion in this study. The review and selection processes for the studies are summarized in the diagram in Fig. 2.
Fig. 2.
PRISMA Flow Diagram.
2.5. Studies included in the systematic review
Twenty-nine peer reviewed studies, which comprised 29,731 study subjects with ACS symptoms residing in 14 LMICs, were included in this systematic review. Sample sizes in the studies ranged from 50 to 20,937. The majority of the studies (N = 25) were cross-sectional, observational designs, 4 were longitudinal and there were no randomized controlled trials. Retrospective studies included data retrieved from hospital medical records (N = 9), there were 3 registry databases and in one study the source was not reported. Most studies were single site (N = 22) versus multi-site (N = 7) and the majority were conducted in tertiary care settings (N = 28) compared to rural settings (N = 1). A description of included studies can be found in Table 1.
2.6. Quality assessment of the included studies
The Newcastle-Ottawa Assessment Scale was utilized to measure the quality of each study.
The scale was developed to evaluate the quality of nonrandomized studies. The scale is comprised of a ‘star system' based on three broad criteria: selection of the study groups; the comparability of the groups; and the ascertainment of the exposure or outcome of interest. The scale has an established coding system to rate studies, content validity and interrater reliability. The quality of the studies (good, fair and poor) were evaluated by awarding stars in each domain according to the established guidelines of the Newcastle–Ottawa Scale. A “good” quality score required 3 or 4 stars in selection, 1 or 2 stars in comparability, and 2 or 3 stars in outcomes. A “fair” quality score required 2 stars in selection, 1 or 2 stars in comparability, and 2 or 3 stars in outcomes. A “poor” quality score reflected 0 or 1 star(s) in selection, or 0 stars in comparability, or 0 or 1 star(s) in outcomes. Most of the studies were rated good (n = 14) to fair (n = 13) and 2 were judged as poor.
3. Results
3.1. The mean time from symptom onset to first medical contact
In the current study, the duration of time from symptom onset to first medical contact ranged from less than 10 min [14] to 96 h [15] with a mean of 12.7 h. In three studies, the focus was the delay between arrival to the emergency department and treatment initiation [16] perceptions of treatment urgency for ACS symptoms [17] and the overall time delay to treatment [18]. Four studies reported that all patients sought medical contact within 12 h of symptom onset [19], [20], [21], [22], while 26 studies reported treatment delays of 12 h or more, of these, 7 studies showed that at least 50% of the study population were delayed for 12 h until the initial medical contact [15], [23], [24], [25], [26], [27], [28]. Only 1 study by Sharma and colleagues [29] targeted characteristics of patients arriving over 12-hours from symptom onset to treatment.
3.2. Sociodemographic characteristics and prehospital delay
Age of study participants ranged from 28 to 72 years, and the majority were males. There were several individual patient characteristics that contributed to early treatment within 12-hours. Higher educational status and income were positively associated with the individual's ability to recognize ACS symptoms as cardiac in origin and the perception of the need for urgent medical care [17], [22], [23], [27], [30], [31]. There was also consensus those with awareness or knowledge of ACS symptoms sought earlier treatment from the time of symptom onset [14], [22], [30], [31] compared to those with limited knowledge [24], [32].
3.3. Gender, age and prehospital delay
In the majority of studies, male gender and younger age were associated with earlier treatment of ACS compared to females and older adults, respectively [19], [23], [31], [33], [34], [35]. Several studies reported however, that there were no differences in treatment for ACS due to either gender or age characteristics. [18], [30], [36]. Allana and colleagues [33] reported that the mean time for male patients to seek treatment for ACS symptoms in Pakistan was 3.5 h, while women delayed an average of 7 h or longer. Bezdah and colleagues [19], in a multivariate analysis, showed that female gender was the only independent factor associated with prolonged time from symptom onset to first medical contact (adjusted OR = 1.87; P = 0.002). Females presenting with acute chest pain were typically older than males and they also tended to have more risk factors. Studies that considered comorbidities reported that the frequency of hypertension in women with ACS was 84% and significantly higher than observed in men with ACS (45%). Women with ACS were also more likely to be diabetic, 50% versus 37% compared to men. Similarly, a history of chronic angina was higher in women 64% than the 50% observed in men [37]. Women also had a lower probability of receiving proper treatment for STEMI than men in several studies [26], [38].
Gender related differences concerning the decision to seek treatment were examined by Allana and colleagues (2018). This delay decision among female participants was associated with greater anxiety, lack of knowledge about ACS symptoms or not wanting to trouble others. Males however, were more likely to evade early treatment decisions by assuming that symptoms would eventually subside or they thought the pain was noncardiac in origin [17]. Atypical ACS symptoms were more likely to occur in women and were perceived by many of them as non-cardiac in origin and therefore not requiring urgent medical attention [17], [35].
3.4. Clinical factors
Among the studies that further divided patients into the subcategories within ACS, the great majority presenting to the emergency department were diagnosed to have STEMI (N = 3542, 62.3%), followed by unstable angina (UA) (N = 103, 59%) and NSTEMI (N = 156, 38.5%). In a study of 100 patients in India with no prior histor676of ischemic heart disease or ACS, the median treatment delay time was 24 h, and only 27% reached the hospital within 6 h; 65% of this number were STEMI [39]. Several studies reported that STEMI patients present earlier for treatment than NSTEMI or UA [27], [28], [31], [34], [39], [40].
The type and character of chest pain were also ass985ciated with the length of time before treatment decisions were made by the patient or family to seek medical evaluation. Patients with recurrent, atypical, or mild chest pain and those with a prior myocardial infarction were more likely to delay treatment than those experiencing chest pain for the first time or pain that was severe or rapidly progressing in intensity [14], [19], [20], [30], [32], [35]. For example, individuals experiencing mild chest pain had a 10-fold greater likelihood of delaying the decision to seek treatment (OR 10.05 [95 %CT; 6.50, 15.54]) [32]. In addition, there were lifestyle factors that contributed to treatment seeking behaviors whereby patients who had been smoking were more likely to seek care sooner than nonsmoking individuals [19], [35].
3.4.1. Comorbid conditions and prehospital delay
Several comorbidities were reported to be associated with delayed treatment for ACS. In many of these studies, conventional risk factors for ACS were not reported, but among those that did address this issue found that smoking, hypertension, diabetes and dyslipidemia were the most prevalent [15], [30], [36], [38]. Mohan and colleagues [30], reported that persons with diabetes had a significantly shorter prehospital delay compared to non-diabetic patients (p < 0.047), with no significant association found between other comorbidities and time to treatment. In contrast, Ahmed and colleagues [24] reported that diabetics (n = 54, 41.5%) had a delay time of 3–6 h compared to nondiabetics with a 1–3 h delay (N = 54, 36%). Several other studies also reported similar findings that diabetics had significant delays in arrival time for treatment [19], [39]. With regards to hypertension, two studies reported that patients with hypertension had a significantly delayed time to first medical contact [22], [35] while patients with dyslipidemia had 54% lower odds of delaying hospital arrival [35].
3.4.2. Reperfusion procedures and prehospital delay <12 h
Consistent with the current recommendations [11], [12], those who sought early treatment for ACS or arriving to the hospital within 12-hours of symptom onset were more likely to receive reperfusion therapies than those presenting after 12 h (Table 2). In a study conducted in Nepal where the average arrival time was 24 h after symptom onset, 28 (43%) out of 65 patients arrived within 7.2 h and received thrombolytic therapy, while 37 (57%) did not receive any reperfusion therapy due to late presentation [39]. Whereas, in another study in Sri Lanka with a mean arrival time of less than 6 h, although 71 out of 81 patients (87%) were eligible for thrombolytic therapy only 72.8% (N = 59) received thrombolytic therapy with streptokinase [37]. Regarding door to treatment time in STEMI patients, very few studies met the current AHA/ACC/ESC recommendations that thrombolysis should be administered within 30-minutes and PCI should be within 120 min [11], [12]. In one study however, the time to fibrinolysis from arrival at the emergency room less than or equal to 90 min in 66 patients (58.2%) [18]. In another study, mean door-to-PCI time among 81 STEMI patients was 98-minutes where 10 patients (16.9%) underwent thrombolysis within 30 min, 28 (47.4%) within 60 min and 39 (66%) within 90 min [37].
In a retrospective study of 1076 STEMI patients in Indonesia using the Jakarta Acute Coronary Registry, the median time from symptom onset to treatment was 180 min; only 63 (6.4%) patients arrived within 60-minutes of symptom onset with the majority presenting after 180 min [26]. Notably, the door to PCI time was 70 min, and within the guideline-recommenced time frame of 90-minutes [11], [12]. Doddipalli and colleagues [41] examined 346 patients admitted within 12 h of symptom onset (mean 2.5 h) who were willing to undergo PCI only, of whom 280 (81%) underwent the procedure. The mortality rates were low (1.4%) among those with treatment times less than 90 min, versus 9% in those receiving treatment after 90-minutes. Among a sample of 96 STEMI patients, a median pre- hospital delay of 290 min was reported with 59% arriving for treatment within 6 h (mean 4.8 h). The median time for thrombolysis (N = 61, 63%) was 75 min and 110 min for PCI (N = 8, 13%) [20]. In a comparison of STEMI patients located in the Netherlands (N = 568) and Indonesia (N = 28), the mean time from symptom onset to admission was much shorter in the Netherlands (214 ± 127 min) minutes vs (413 vs. 213 min) in Indonesia. In addition, the Indonesian sample were significantly younger (53.8 ± 11.6 vs 62.9 ± 12.8 years), more likely diabetic (36% vs. 12%), experiencing dyslipidemia (46% vs. 19%), more often smokers (68% vs. 31%) and had more severe cardiovascular disease Killip ≥ 2 on admission (52% vs. 8%) than those residing in the Netherlands [36]. Kim and colleagues [38] observed that the average chest pain duration before treatment for 164 STEMI patients was 7.87 h, of these 136 (83%) underwent thrombolysis, 3 (1.84%) received PCI and 1 was referred for CABG at another facility. In this study, the mean door-to-needle time was 38.28 min, and 62.5% received streptokinase within 30 min of arrival to the hospital. In a study conducted in Sri Lanka on 256 STEMI patients, 73% arrived within 12 h, the range was less than 30 min to 281 min (4.6 hrs.). The mean door-to-needle time was 98-minutes with 10 patients (16.9%) undergoing fibrinolytic therapy using streptokinase within 30-minutes, 28 (47.4%) within 60-min and 39 (66%) within 90-min; notably 20 (33.9%) underwent thrombolysis after 90-min after arriving at the hospital [40].
In a study conducted in Kenya, fewer than 10% of patients presented within one hour of symptom onset, while >35% took longer than 24 h to present to a medical facility. Patients with STEMI presented earlier compared to those with NSTEMI, 46.6% and 23.3% presenting within six hours of symptom onset, respectively. Of the 101 patients admitted with STEMI, 49 received thrombolytic therapy while 19 patients underwent PCI. The mean time intervals to thrombolysis and PCI were 49 (±42) and 137 (±63) minutes, respectively. Target door-to-needle time for thrombolysis of 30 min was met in 26 of the 49 subjects (53.1%) while door-to-balloon time of 90 min was achieved in only 5 of the 19 patients considered for primary PCI (26.3%) [28]. A large multi-site study conducted in India examining 20,937 patients with ACS reported a median time from onset of symptoms to hospital arrival of 6 h. Patients with STEMI were younger and presented to the hospital earlier than those with NSTEMI or UA. Approximately four-fifths of the patients with STEMI received fibrinolytic therapy with a median time from arrival to the hospital to thrombolysis of 50 min [31].
3.4.3. Reperfusion procedures and prehospital delay time exceeding 12-hours
Among studies with arrival times >24 h, fewer participants received reperfusion therapy [15], [25] and those arriving after 12 h were also unlikely to be treated [38], [40]. In a study 151 patients with ACS from Ethiopia, the average time interval from symptom onset to treatment was 96 h, 5 (3.3%) patients presented for treatment within 60 min and 65 (43%) within 13–72 h, the remaining 81 patients presented between 73 and 96 h. Of the 151 patients, 110 (72.8%) were diagnosed to have STEMI followed by NSTEMI in 23 (15.2%) and UA was observed in 18 (12%). Of the patients with STEMI, 13 received reperfusion therapy, thrombolysis was administered in 7 and PCI was done for 6 patients while 6 were referred for CABG at another institution [15]. Kim [38], reported that approximately 79 (34%) of patients presented after 12 h of symptoms onset and had a 13.82 lower-odds of receiving thrombolysis. Koirala [42] in a retrospective chart audit of 232 STEMI patients in Nepal reported a mean duration from symptom onset to treatment was 17.5 h with 153 (66%) presenting before 12 h, approximately 49 (34%) presenting between 12 and 24 h and an additional 30 (13%) beyond 24 h. Despite late presentation for almost half (47%) of the patients treated, almost all (98.2%) received coronary artery stenting with drug eluting stents, and multiple vessel PCI was also conducted in 7 participants. Notably, in this study, the PCI mean time was 7.6 h. In another study conducted in India by Sharma and colleagues [29], 147 STEMI patients were specifically recruited after 12 h of symptom onset with cardiogenic shock, with mean delayed treatment time of 24 h, 33 (22.4%) underwent thrombolysis and 53 patients (63.9%) underwent PCI at a median time of 36 h (IQ 30–72) after symptom onset. Among the 147 patients recruited, 42.9% died during hospitalization, and another 20 (13.6%) died within the first 24 h. In a similar study where the mean time from symptom onset to treatment was 24 h in 153 ACS patients, for those who had a STEMI (N = 38, 58%), only 20 (34%) of STEMI patients underwent thrombolysis with streptokinase; mortality and heart failure was higher among STEMI patients compared to NSTEMI and UA [27].
3.4.4. Major adverse cardiovascular events and prehospital delay time
Among the studies included, 5 of them showed that ACS patients developed major adverse cardiovascular events (MACE), such as heart failure, heart block, ventricular arrythmia, pericardial effusion and stroke primarily after the 12-hour time onset from symptoms to treatment [25], [27], [29], [38], [40], [42]. Patients who arrived at ED after 3 days of symptom onset were 5.52 times more likely to die compared with patients who arrived within 12 h of symptom onset (AOR = 5.52; 95% CI = 1.05–32.22) [15].
3.4.5. System factors and prehospital delay time
Studies were consistent in reporting that patients who initially sought care in a facility that lacked adequately trained physicians and equipment for ACS management were more likely to experience significant treatment delays. Several studies reported that the lack of an organized EMS system was a strong contributor to pre-hospital delay time [27], [31], [38], [40]. Most studies reported that patients came to the emergency department by a taxi or private car and some used public transportation; across studies approximately 5% or less used an ambulance. In one study for example, approximately 87% of patients lived within 10 km of the hospital with ambulance availability, but less than 6% of STEMI patients used these services for transport to the hospital [38]. In another study, Mohan [30] reported that although 96% of patients were aware of ambulance services, only 5.3% of patients used an ambulance for transport. In several other studies, presenting directly to a tertiary facility significantly reduced mean treatment time versus those who were initially seen at a general hospital or by a primary clinician [19], [20], [21], [26], [27], [28], [34], [35], [37], [41]. There was general agreement among studies that a lack of available reperfusion centers outside of major urban areas, limited diagnostic resources (EKG, cardiac enzymes) and adequately trained clinicians to recognize ACS prolonged symptom onset to treatment time [21], [26], [27], [28], [30], [31], [42], [43]. In addition, system factors such as crowding in the emergency departments, and a lack of available bed capacity in reperfusion hospitals also contributed to major delays in treatment time [16].
3.4.6. Other factors and prehospital delay time
There were several other factors that were associated with increased time from symptom onset to treatment. Living in rural geographical areas, difficult road travel (poor road conditions, high traffic volume) and lack of available transportation were reasons for prolonged pre- hospital treat delays in several studies [20], [22], [23], [27], [31], [41], [42]. Limited financial resources and the lack of a national insurance plan in many LMICs requires patients to pay out of pocket for cardiac reperfusion procedures which resulted in little to no access to care [16], [27], [31]. For example, in Pakistan, mortality was significantly lower (5.5%) among high income STEMI patients versus the poorest (8.2%) [31].
4. Discussion
This systematic review supports that pre-hospital treatment delay is a major factor for the higher morbidity and mortality associated with ACS among STEMI patients residing in LMICs [44], [45], [46]. The duration from symptom onset to the decision to seek medical attention and receipt of reperfusion therapy are critically important time points often used to quantify treatment delays [43]. In high-income countries, the decision to seek care is a major factor contributing to prehospital treatment delay for STEMI patients, with transportation having a very limited role except in selected remote settings [9]. In LMICs however, transportation and the lack of adequate EMS services are major reasons for pre-hospital treatment delays.
Patient characteristics, clinical factors and health system influences all contributed to excessive pre-hospital delays among ACS patients residing in LMICs [40], [43]. Greater recognition of these factors by policy makers may help identify alternative strategies that increase the likelihood of earlier treatment decisions. For example, reaching the first point of effective medical care may exceed 2–3 days especially when traveling from rural or remote areas [44]. In urban areas prehospital delay is shorter than in rural areas, but is still reported to exceed 6 h or longer in most instances. This treatment delay is particularly challenging when the first point of contact is a primary care center that lacks essential equipment such as an electrocardiogram (EKG) or a provider who is unable to interpret it correctly resulting in misdiagnosis of ACS symptoms [43].
Ambulance and emergency medical services (EMS) are underdeveloped in LMICs, especially outside of large urban cities [38], [41]. Typically, the mode of transportation for patients experiencing ACS symptoms involves the use of available public transport and private cars [38], [41]. In large urban cities where EMS has been more fully developed and is available, it has contributed to substantial improvements in the timely management of patients with an ACS, but it is estimated that only 5% of patients utilize these services [30], [40]. In addition, the use of an ambulance was cost prohibitive for most patients who are required to pay out of pocket in many LMICs who lack a national insurance program. In addition, many ambulance services did not have the necessary emergency medical equipment required for emergency care [28]
There were a number of factors identified among participants delaying 12 h or longer to seek treatment for ACS symptoms. Clinically, patients with atypical symptoms, those with mild chest pain, gradual in onset or if symptoms subsided on their own, were more likely to delay seeking treatment. Lack of knowledge of ACS symptoms was one of the most prominent reasons reported for treatment delay [14]. Older and illiterate patients with ACS symptoms were more likely to attribute their symptoms to originate from other causes such as gastrointestinal or musculoskeletal problems [34]. Increasing national educational campaigns to improve knowledge about typical and atypical ACS symptoms and the importance of seeking early treatment is central for reducing the high morbidity and mortality in LMICs.
From a health system's perspective, those living in close proximity to and directly admitted to an emergency department [19], [27], [35], [37] with the capacity to provide thrombolytic or PCI [22], [31], [41] were more likely to receive early treatment for ACS symptoms. Settings where EKG machines were readily available and timely used in the evaluation of ACS had significantly lower prehospital delays for referral to reperfusion therapy facilities. One study documented that 80.7% of patients who had an EKG in the prehospital phase received reperfusion therapy compared to 63.3% those who did not have an EKG performed [30]. Another potential strategy to improve EKG diagnostic capability in rural or remote areas that have fewer resources may be the use of telemedicine. The primary care clinic would have the ability to send EKG results to cardiac centers with greater likelihood of a timelier diagnosis and reduced prehospital delay time [48].
Poor travel conditions, lack of suitable roads, traffic congestion, limited access to transportation and vehicle mechanical problems were among the reasons for delay in seeking treatment for ACS in rural locations [23], [24], [27], [30], [31]. A lack of an organized system for collaboration between hospitals and physicians were important roadblocks for more timely treatment for ACS symptoms [21], [30], [35], [40]. A consistent theme in several LMICs was the lack of available insurance or universal coverage for healthcare. Many patients who were unable to pay out of pocket for thrombolytic therapy or PCT procedures had to leave the treatment facility due to financial restraints [16], [27]. There is a urgent need to establish both an emergency medical system infrastructure and health coverage for life-saving treatments in most LMICs in order to improve the morbidity and mortality associated with ACS [47].
Persons residing in LMICs tended to be younger and have more severe CAD than in developed countries [38]. In many instances, this was due to the presence of modifiable risk factors such as smoking. Public and targeted campaigns on primary prevention are urgently needed and could potentially lower morbidity and mortality rates due to ACS [49]. Initiatives targeting younger age children and adolescents through the educational system on the dangers of smoking to prevent them from starting smoking earlier could also be an effective approach [50]. Another strategy could include restrictions in public areas similar to the policies the United States and other European countries have adopted with government and state facilities prohibiting smoking.
The presence of hypertension and diabetes are prominent risk factors for ACS and are more likely to go untreated in LMICs. Public campaigns and screenings to increase awareness of these risk factors may be beneficial. Similar campaigns such as know your numbers has been utilized as a model in some developing countries to increase awareness of cardiovascular risk factors [51]. Screening for prediabetes would identify those at higher risk for developing Type 2 diabetes in the future. Because several studies showed that prehospital delay was longer in diabetics and often was predictable for poorer outcomes, making individuals aware of the close association and higher risk for heart disease may potentially improve morbidity and mortality rates [52].
4.1. Strengths and limitations
This systematic review has both strengths and limitations. A strong and comprehensive search methodology following PRISMA guidelines was a strength. Among the included studies, a clear pattern emerged that men were more likely to have shortened treatment delay and receive reperfusion at higher rates than women. Greater knowledge, higher income and living in an urban area were associated with shorter treatment time with access to care much more limited in rural areas.
There were also several limitations. Due to the heterogeneity of the studies, we were not able to pool the results effectively and analyze the findings using a meta-analysis approach. Most of the studies were retrospective or prospective cohort in design which does not rule out a possible bias. Among the retrospective cohort studies, medical records are subject to errors or missing information and in many of these studies, methods of data collection were not clearly reported or documented. The majority of studies utilized a cross-sectional design, so the long-term effects of treatment provided was not possible. Serum troponin levels were not available or were not taken routinely across studies which may have contributed to an incorrect ACS diagnosis. Single center studies with small sample sizes were included in the systematic review which may have also contributed to bias. In addition, studies conducted in private hospitals or in urban tertiary care facilities may not be generalizable to the population at large in LMICs. Among the prospective studies included, risk of recall bias may have occurred regarding symptom onset which may have potentially confounded the reported pre-hospital delay times. The reliability of the patient or person providing the information regarding symptom onset was not reported in the most studies. The use of validated measures to collect data was not utilized increasing the potential for measurement error. Data was not collected from patients who died at home or in route to the hospital which may have inflated the results in a positive direction. Patients with ACS who were discharged or left against medical advice were not documented in most studies. Exclusion of clinically unstable patients may also have limited the generalizability of the study findings. This is particularly relevant among those who lived in rural areas and had to travel greater distances to receive care or those from lower socioeconomic status with little or no health care access to interventional cardiology facilities.
5. Conclusion
In conclusion, this systematic review provides evidence that pre-hospital delay time remains an important contributor to poorer clinical outcomes and higher mortality in LMICs. As the number of ACS patients is anticipated to dramatically rise in LMICs over the next several decades, there is a growing concern of devising better healthcare structures to improve clinical services. Findings from this systematic review provide direction to reduce prehospital delay in LMICs. Training of multi-disciplinary emergency medical personnel in community hospitals and primary care settings on diagnostic procedures is a vital step. Lack of an organized health care system often delays transfer of ACS patients to cardiac intervention facilities. A country-wide or regional referral plan is urgently needed to insure timely transfer of patients from non-cardiac centers to interventional facilities. Finally, many patients do not seek treatment early because they are not aware of the signs or symptoms of ACS. Health education through the different media outlets will raise awareness of the public on ACS risk factors, accompanying signs and symptoms as well as the need to seek early treatment to improve clinical outcomes.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcha.2021.100823.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Mensah G.A., Roth G.A., Sampson U.K., Moran A.E., Feigin V.L., Forouzanfar M.H., Naghavi M., Murray C.J. GBD 2013 Mortality and Causes of Death Collaborators. Mortality from cardiovascular diseases in sub-Saharan Africa, 1990-2013: a systematic analysis of data from the Global Burden of Disease Study 2013. Cardiovasc. J Afr. 2015 doi: 10.5830/CVJA-2015-036. Mar-Apr;26(2 Suppl 1):S6-10. doi: 10.5830/CVJA-2015-036. PMID: 25962950; PMCID: PMC4557490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roth G.A., Mensah G.A., Johnson C.O., Addolorato G., Ammirati E., Baddour L.M., Barengo N.C., Beaton A.Z., Benjamin E.J., Benziger C.P., Bonny A., Brauer M., Brodmann M., Cahill T.J., Carapetis J., Catapano A.L., Chugh S.S., Cooper L.T., Coresh J., Criqui M., DeCleene N., Eagle K.A., Emmons-Bell S., Feigin V.L., Fernández-Solà J., Fowkes G., Gakidou E., Grundy S.M., He F.J., Howard G., Hu F., Inker L., Karthikeyan G., Kassebaum N., Koroshetz W., Lavie C., Lloyd-Jones D., Lu H.S., Mirijello A., Temesgen A.M., Mokdad A., Moran A.E., Muntner P., Narula J., Neal B., Ntsekhe M., Moraes de Oliveira G., Otto C., Owolabi M., Pratt M., Rajagopalan S., Reitsma M., Ribeiro A.L.P., Rigotti N., Rodgers A., Sable C., Shakil S., Sliwa-Hahnle K., Stark B., Sundström J., Timpel P., Tleyjeh I.M., Valgimigli M., Vos T., Whelton P.K., Yacoub M., Zuhlke L., Murray C., Fuster V. GBD-NHLBI-JACC global burden of cardiovascular diseases writing group. Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 study. J. Am. Coll. Cardiol. 2020 doi: 10.1016/j.jacc.2020.11.010. Dec 22;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. PMID: 33309175; PMCID: PMC7755038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cappuccio F.P., Miller M.A. Cardiovascular disease and hypertension in sub-Saharan Africa: burden, risk and interventions. Intern. Emerg. Med. 2016;11(3):299–305. doi: 10.1007/s11739-016-1423-9. doi: 10.1007/s11739-016-1423-9. Epub 2016 Mar 21. PMID: 27001886; PMCID: PMC4820479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gouda H.N., Charlson F., Sorsdahl K., Ahmadzada S., Ferrari A.J., Erskine H., Leung J., Santamauro D., Lund C., Aminde L.N., Mayosi B.M., Kengne A.P., Harris M., Achoki T., Wiysonge C.S., Stein D.J., Whiteford H. Burden of non-communicable diseases in sub-Saharan Africa, 1990–2017: results from the Global Burden of Disease Study 2017. Lancet Glob Health. 2019 Oct;7(10):e1375–e1387. doi: 10.1016/S2214-109X(19)30374-2. PMID: 31537368. [DOI] [PubMed] [Google Scholar]
- 5.Vedanthan R., Seligman B., Fuster V. Global perspective on acute coronary syndrome: a burden on the young and poor [published correction appears in Circ Res. 2014 Aug 1;115(4):e8] Circ. Res. 2014;114(12):1959–1975. doi: 10.1161/CIRCRESAHA.114.302782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seligman B., Vedanthan R., Fuster V. Acute coronary syndromes in low- and middle-income countries: Moving forward. Int. J. Cardiol. 2016 Aug;217(Suppl):S10–S12. doi: 10.1016/j.ijcard.2016.06.213. Epub 2016 Jun 27 PMID: 27381860. [DOI] [PubMed] [Google Scholar]
- 7.Moran A.E., Tzong K.Y., Forouzanfar M.H., Rothy G.A., Mensah G.A., Ezzati M., Murray C.J., Naghavi M. Variations in ischemic heart disease burden by age, country, and income: the Global Burden of Diseases, Injuries, and Risk Factors 2010 study. Glob. Heart. 2014 Mar;9(1):91–99. doi: 10.1016/j.gheart.2013.12.007. doi: 10.1016/j.gheart.2013.12.007. PMID: 24977114; PMCID: PMC4071302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yuyun M.F., Sliwa K., Kengne A.P., Mocumbi A.O., Bukhman G. Cardiovascular diseases in sub-Saharan Africa compared to high-income countries: an epidemiological perspective. Glob Heart. 2020 Feb 12;15(1):15. doi: 10.5334/gh.403. doi: 10.5334/gh.403. PMID: 32489788; PMCID: PMC7218780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kakou-Guikahue M., N'Guetta R., Anzouan-Kacou J.B., Kramoh E., N'Dori R., Ba S.A., Diao M., Sarr M., Kane A., Kane A., Damorou F., Balde D., Diarra M.B., Djiddou M., Kimbally-Kaki G., Zabsonre P., Toure I.A., Houénassi M., Gamra H., Chajai B., Gerardin B., Pillière R., Aubry P., Iliou M.C., Isnard R., Leprince P., Cottin Y., Bertrand E., Juillière Y., Monsuez J.J., Working Group on Tropical Cardiology Société Française de Cardiologie. Optimizing the management of acute coronary syndromes in sub-Saharan Africa: A statement from the AFRICARDIO 2015 Consensus Team. Arch. Cardiovasc. Dis. 2016 doi: 10.1016/j.acvd.2015.12.005. Jun-Jul;109(6-7):376-83. doi: 10.1016/j.acvd.2015.12.005. Epub 2016 Mar 25. PMID: 27020513. [DOI] [PubMed] [Google Scholar]
- 10.Kushner F.G., Hand M., Smith S.C., Jr, King S.B., 3rd, Anderson J.L., Antman E.M., Bailey S.R., Bates E.R., Blankenship J.C., Casey D.E., Jr, Green L.A., Hochman J.S., Jacobs A.K., Krumholz H.M., Morrison D.A., Ornato J.P., Pearle D.L., Peterson E.D., Sloan M.A., Whitlow P.L., Williams D.O. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2009 Dec 1;54(23):2205–2241. doi: 10.1016/j.jacc.2009.10.015. doi: 10.1016/j.jacc.2009.10.015. Erratum in: J Am Coll Cardiol. 2009 Dec 15;54(25):2464. Erratum in: J Am Coll Cardiol. 2010 Feb 9;55(6):612. Dosage error in article text. PMID: 19942100. [DOI] [PubMed] [Google Scholar]
- 11.Levine G.N., Bates E.R., Blankenship J.C., Bailey S.R., Bittl J.A., Cercek B., Chambers C.E., Ellis S.G., Guyton R.A., Hollenberg S.M., Khot U.N., Lange R.A., Mauri L., Mehran R., Moussa I.D., Mukherjee D., Ting H.H., O'Gara P.T., Kushner F.G., Ascheim D.D., Brindis R.G., Casey D.E., Jr, Chung M.K., de Lemos J.A., Diercks D.B., Fang J.C., Franklin B.A., Granger C.B., Krumholz H.M., Linderbaum J.A., Morrow D.A., Newby L.K., Ornato J.P., Ou N., Radford M.J., Tamis-Holland J.E., Tommaso C.L., Tracy C.M., Woo Y.J., Zhao D.X. ACC/AHA/SCAI Focused Update on Primary Percutaneous Coronary Intervention for Patients With ST-Elevation Myocardial Infarction: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. J. Am. Coll. Cardiol. 2016 Mar 15;67(10):1235-1250. doi: 10.1016/j.jacc.2015.10.005. Epub 2015 Oct 21. Erratum in: J Am Coll Cardiol. 2016 Mar 29;67(12):1506. PMID: 26498666. [Google Scholar]
- 12.Ibanez B., James S., Agewall S., Antunes M.J., Bucciarelli-Ducci C., Bueno H., Caforio A.L.P., Crea F., Goudevenos J.A., Halvorsen S., Hindricks G., Kastrati A., Lenzen M.J., Prescott E., Roffi M., Valgimigli M., Varenhorst C., Vranckx P., Widimský P., ESC Scientific Document Group 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39(2):119–177. doi: 10.1093/eurheartj/ehx393. doi: 10.1093/eurheartj/ehx393. PMID: 28886621. [DOI] [PubMed] [Google Scholar]
- 13.LA Moher D., Tetzlaff J., Altman D.G. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- 14.V.C.K. Venkatesan, S. Madhavi, R SK, P K. A study to explore the factors related to treatment seeking delay among adults diagnosed with acute myocardial infarction at KMCH, Coimbatore, Indian Heart J. 2018 Nov-Dec;70(6):793-801. doi: 10.1016/j.ihj.2018.01.007. PMID: 30580847; PMCID: PMC6306387. [DOI] [PMC free article] [PubMed]
- 15.Desta D.M., Nedi T., Hailu A., Atey T.M., Tsadik A.G., Asgedom S.W., Kasahun G.G., Ayalew E. Treatment outcome of acute coronary syndrome patients admitted to Ayder Comprehensive Specialized Hospital, Mekelle, Ethiopia; A retrospective cross-sectional study. PLoS ONE. 2020 Feb 13;15(2) doi: 10.1371/journal.pone.0228953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khursheed M., Fayyaz J., Feroze A., Shakeel N., Bhatti J.A. Time to treatment in patients of suspected acute coronary syndrome in Pakistan: a clinical audit. Heart Lung. 2015;44(1):63–67. doi: 10.1016/j.hrtlng.2014.08.007. Epub 2014 Oct 1 PMID: 25281530. [DOI] [PubMed] [Google Scholar]
- 17.Allana S., Moser D.D.K., Ali D.T.S., Khan D.A.H. Sex differences in symptoms experienced, knowledge about symptoms, symptom attribution, and perceived urgency for treatment seeking among acute coronary syndrome patients in Karachi Pakistan. Heart Lung. 2018;47(6):584–590. doi: 10.1016/j.hrtlng.2018.06.009. PMID: 30107891. [DOI] [PubMed] [Google Scholar]
- 18.Dhungel S., Malla R., Adhikari C., Maskey A., Rajbhandari R., Sharma R., Nepal H., Rauniyar B., Yadav D., Limbu D., Gautam M., Adhikari A., Dhungel S., Upadhyay H. Door-to-balloon time and the determining factors in a tertiary cardiac center in Nepal. Indian Heart J. 2018 doi: 10.1016/j.ihj.2018.07.011. Dec;70 Suppl 3(Suppl 3):S309-S312. doi: 10.1016/j.ihj.2018.07.011. Epub 2018 Aug 27. PMID: 30595281; PMCID: PMC6309874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bezdah L., Ben Ahmed I., Mrabet A., Saidi O., Ben Romdhane H. Delays in management of ST-segment elevation myocardial infarction. Arch. Cardiovascular Diseases Supplements. 2020;12:25. [Google Scholar]
- 20.George L., Ramamoorthy L., Satheesh S., Saya R.P., Subrahmanyam D.K. Prehospital delay and time to reperfusion therapy in ST elevation myocardial infarction. J. Emerg. Trauma Shock. 2017;10(2):64–69. doi: 10.4103/0974-2700.201580. doi: 10.4103/0974-2700.201580. PMID: 28367010; PMCID: PMC5357880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mesas C.E., Rodrigues R.J., Mesas A.E., Feijó V.B.R., Paraiso L.M.C., Bragatto G.F.G.A., Moron V., Bergonso M.H., Uemura L., Grion C.M.C. Symptoms awareness, emergency medical service utilization and hospital transfer delay in myocardial infarction. BMC Health Serv. Res. 2018;18(1):490. doi: 10.1186/s12913-018-3312-6. doi: 10.1186/s12913-018-3312-6. PMID: 29940942; PMCID: PMC6020233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poorhosseini H., Saadat M., Salarifar M., Mortazavi S.H., Geraiely B. Pre-Hospital Delay and Its Contributing Factors in Patients with ST-Elevation Myocardial Infarction; a Cross sectional Study. Arch. Acad. Emerg. Med. 2019;7(1) e29. PMID: 31432039; PMCID: PMC6637811. [PMC free article] [PubMed] [Google Scholar]
- 23.Acharya P., Adhikari R.R., Bhattarai J., Shrestha N.R., Sharma S.K., Karki P. Delayed presentation of acute coronary syndrome: a challenge in its early management. JNMA J. Nepal Med. Assoc. 2009;48(173):1–4. PMID: 19529049. [PubMed] [Google Scholar]
- 24.Ahmed S., Khan A., Ali S.I., Saad M., Jawaid H., Islam M., Saiyed H., Fatima S., Khan A., Basham M.A., Hussain S.A., Akhtar M., Kausar F., Hussain A., Fatima K. Differences in symptoms and presentation delay times in myocardial infarction patients with and without diabetes: A cross-sectional study in Pakistan. Indian Heart J. 2018;70(2):241–245. doi: 10.1016/j.ihj.2017.07.013. doi: 10.1016/j.ihj.2017.07.013. PMID: 29716701; PMCID: PMC5993922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bogale K., Mekonnen D., Nedi T., Woldu M.A. Treatment Outcomes of Patients with Acute Coronary Syndrome Admitted to Tikur Anbessa Specialized Hospital, Addis Ababa. Ethiopia. Clin Med Insights Cardiol. 2019;13 doi: 10.1177/1179546819839417. 1179546819839417. doi: 10.1177/1179546819839417. PMID: 31024218; PMCID: PMC6472164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dakota I., Dharma S., Andriantoro H., Firdaus I., Danny S.S., Zamroni D., Radi B. “Door-In to Door-Out” Delay in Patients with Acute ST-Segment Elevation Myocardial Infarction Transferred for Primary Percutaneous Coronary Intervention in a Metropolitan STEMI Network of a Developing Country. Int J Angiol. 2020 Mar;29(1):27–32. doi: 10.1055/s-0039-3401046. doi: 10.1055/s-0039-3401046. PMID: 32132813; PMCID: PMC7054060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shrestha N.R., Pilgrim T., Basnet A., Karki P., Cook S., Urban P. Percutaneous coronary intervention for acute coronary syndromes in eastern Nepal: a preliminary report. Swiss Med Wkly. 2013;143 doi: 10.4414/smw.2013.13737. PMID: 23443879. [DOI] [PubMed] [Google Scholar]
- 28.Varwani M.H., Jeilan M., Ngunga M., Barasa A. Outcomes in patients with acute coronary syndrome in a referral hospital in sub-Saharan Africa. Cardiovasc J Afr. 2019;30(1):29–33. doi: 10.5830/CVJA-2018-066. Epub 2018 Dec 4 PMID: 30534849. [DOI] [PubMed] [Google Scholar]
- 29.Sharma Y.P., Krishnappa D., Kanabar K., Kasinadhuni G., Sharma R., Kishore K., Mehrotra S., Santosh K., Gupta A., Panda P. Clinical characteristics and outcome in patients with a delayed presentation after ST-elevation myocardial infarction and complicated by cardiogenic shock. Indian Heart J. 2019;71(5):387–393. doi: 10.1016/j.ihj.2019.11.256. doi: 10.1016/j.ihj.2019.11.256. PMID: 32035521; PMCID: PMC7013184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mohan B., Bansal R., Dogra N., Sharma S., Chopra A., Varma S., Bansal N., Tandon R., Goyal A., Singh B., Chhabra S.T., Aslam N., Wander G.S., Roy A. Factors influencing prehospital delay in patients presenting with ST-elevation myocardial infarction and the impact of prehospital electrocardiogram. Indian Heart J. 2018;70(Suppl 3):S194–S198. doi: 10.1016/j.ihj.2018.10.395. PMID: 30595256; PMCID: PMC6309871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xavier D., Pais P., Devereaux P.J., Xie C., Prabhakaran D., Reddy K.S., Gupta R., Joshi P., Kerkar P., Thanikachalam S., Haridas K.K., Jaison T.M., Naik S., Maity A.K., Yusuf S. CREATE registry investigators. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371(9622):1435–1442. doi: 10.1016/S0140-6736(08)60623-6. PMID: 18440425. [DOI] [PubMed] [Google Scholar]
- 32.Khan M.S., Jafary F.H., Faruqui A.M., Rasool S.I., Hatcher J., Chaturvedi N., Jafar T.H. High prevalence of lack of knowledge of symptoms of acute myocardial infarction in Pakistan and its contribution to delayed presentation to the hospital. BMC Public Health. 2007;9(7):284. doi: 10.1186/1471-2458-7-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Allana S., Khowaja K., Ali T.S., Moser D.K., Khan A.H. Gender differences in factors associated with prehospital delay among acute coronary syndrome patients in Pakistan. J Transcult Nurs. 2015;26(5):480–490. doi: 10.1177/1043659614524787. PMID: 26541388. [DOI] [PubMed] [Google Scholar]
- 34.Sriha Belguith A., Beltaief K., Msolli M.A., Bouida W., Abroug H., Ben Fredj M., Zemni I., Grissa M.H., Boubaker H., ESCor Investigators group, Hsairi M., Nouira S., ESCorT Investigators group Management of acute coronary syndrome in emergency departments: a cross sectional multicenter study (Tunisia) BMC Emerg Med. 2018;18(1):50. doi: 10.1186/s12873-018-0201-6. PMID: 30509187; PMCID: PMC6276213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lim S.C., Rahman A., Yaacob N.M. Pre-Hospital Factors Influencing Time of Arrival at Emergency Departments for Patients with Acute ST-Elevation Myocardial Infarction. Malays J Med Sci. 2019;26(1):87–98. doi: 10.21315/mjms2019.26.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Juwana Y.B., Wirianta J., Ottervanger J.P., Dambrink J.H., van't Hof A.W., Gosselink A.T., Hoorntje J., de Boer M.J., Suryapranata H. Primary coronary intervention for ST-elevation myocardial infarction in Indonesia and the Netherlands: a comparison. Neth. Heart J. 2009;17(11):418–421. doi: 10.1007/BF03086295. PMID: 19949710; PMCID: PMC2779478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bandara R., Medagama A., Munasinghe R., Dinamithra N., Subasinghe A., Herath J., Ratnayake M., Imbulpitiya B., Sulaiman A. Management and outcomes of acute ST-segment-elevation myocardial infarction at a tertiary-care hospital in Sri Lanka: an observational study. BMC Cardiovasc Disord. 2015;15:1. doi: 10.1186/1471-2261-15-1. doi: 10.1186/1471-2261-15-1. PMID: 25592444; PMCID: PMC4361140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim D.Y., Wala Z., Islam S., Islam R., Ahn M. Clinical characteristics and outcomes of ST-segment elevation myocardial infarction in a low income setting in rural Bangladesh. Int J Cardiol Heart Vasc. 2019 May;17(23) doi: 10.1016/j.ijcha.2019.100376. doi: 10.1016/j.ijcha.2019.100376. PMID: 31193421; PMCID: PMC6527896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Agrawal V., Lohiya B.V., Sihag B.K., Prajapati R. Clinical Profile with Angiographic Correlation in Naïve Acute Coronary Syndrome. J Clin Diagn Res. 2016 Sep;10(9):OC10–OC14. doi: 10.7860/JCDR/2016/21166.8519. Epub 2016 Sep 1. PMID: 27790485; PMCID: PMC5071985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Medagama A., Bandara R., De Silva C., Galgomuwa M.P. Management of acute coronary syndromes in a developing country; time for a paradigm shift? An observational study. BMC Cardiovasc Disord. 2015;15:133. doi: 10.1186/s12872-015-0125-y. doi: 10.1186/s12872-015-0125-y. PMID: 26497226; PMCID: PMC4619422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Doddipalli S.R., Rajasekhar D., Vanajakshamma V., Sreedhar Naik K. Determinants of total ischemic time in primary percutaneous coronary interventions: A prospective analysis. Indian Heart J. 2018 Dec;70(Suppl 3):S275–S279. doi: 10.1016/j.ihj.2018.05.005. Epub 2018 May 7. PMID: 30595273; PMCID: PMC6309146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Koirala P., Gajurel R.M., Poudel C.M., Shrestha H., Devkota S., Thapa S. Study of clinical profile and outcomes of Percutaneous Coronary Intervention in ST Elevation Myocardial Infarc- tion. Nepalese Heart J. 2019;16(2):53–57. [Google Scholar]
- 43.Dharma S., Juzar D.A., Firdaus I., Soerianata S., Wardeh A.J., Jukema J.W. Acute myocardial infarction system of care in the third world. Neth Heart J. 2012 Jun;20(6):254–259. doi: 10.1007/s12471-012-0259-9. PMID: 22328356; PMCID: PMC3370084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gupta R., Yusuf S. Challenges in management and prevention of ischemic heart disease in low socioeconomic status people in LLMICs. BMC Med. 2019 Nov 26;17(1):209. doi: 10.1186/s12916-019-1454-y. PMID: 31767015; PMCID: PMC6878693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yusuf S., Rangarajan S., Teo K., Islam S., Li W., Liu L., Bo J., Lou Q., Lu F., Liu T., Yu L., Zhang S., Mony P., Swaminathan S., Mohan V., Gupta R., Kumar R., Vijayakumar K., Lear S., Anand S., Wielgosz A., Diaz R., Avezum A., Lopez-Jaramillo P., Lanas F., Yusoff K., Ismail N., Iqbal R., Rahman O., Rosengren A., Yusufali A., Kelishadi R., Kruger A., Puoane T., Szuba A., Chifamba J., Oguz A., McQueen M., McKee M., Dagenais G., Investigators P.U.R.E. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. 2014 Aug 28;371(9):818–827. doi: 10.1056/NEJMoa1311890. PMID: 25162888. [DOI] [PubMed] [Google Scholar]
- 46.Moser D.K., Kimble L.P., Alberts M.J., Alonzo A., Croft J.B., Dracup K., Evenson K.R., Go A.S., Hand M.M., Kothari R.U., Mensah G.A., Morris D.L., Pancioli A.M., Riegel B., Zerwic J.J. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation. 2006 Jul 11;114(2):168–182. doi: 10.1161/CIRCULATIONAHA.106.176040. Epub 2006 Jun 26 PMID: 16801458. [DOI] [PubMed] [Google Scholar]
- 47.Levine G.N., Bates E.R., Blankenship J.C., Bailey S.R., Bittl J.A., Cercek B., Chambers C.E., Ellis S.G., Guyton R.A., Hollenberg S.M., Khot U.N., Lange R.A., Mauri L., Mehran R., Moussa I.D., Mukherjee D., Ting H.H., O'Gara P.T., Kushner F.G., Ascheim D.D., Brindis R.G., Casey D.E., Jr, Chung M.K., de Lemos J.A., Diercks D.B., Fang J.C., Franklin B.A., Granger C.B., Krumholz H.M., Linderbaum J.A., Morrow D.A., Newby L.K., Ornato J.P., Ou N., Radford M.J., Tamis-Holland J.E., Tommaso C.L., Tracy C.M., Woo Y.J., Zhao D.X. 2015 ACC/AHA/SCAI Focused Update on Primary Percutaneous Coronary Intervention for Patients With ST-Elevation Myocardial Infarction: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. J Am Coll Cardiol. 2016;67(10):1235–1250. doi: 10.1016/j.jacc.2015.10.005. doi: 10.1016/j.jacc.2015.10.005. Erratum in: J Am Coll Cardiol. 2016 Mar 29;67(12):1506. PMID: 26498666. [DOI] [PubMed] [Google Scholar]
- 48.Brunetti N.D., Tarantino N., Dellegrottaglie G., Abatecola G., De Gennaro L., Bruno A.I., Bux F., Gaglione A., Di Biase M. Impact of telemedicine support by remote pre-hospital electrocardiogram on emergency medical service management of subjects with suspected acute cardiovascular disease. Int J Cardiol. 2015 Nov;15(199):215–220. doi: 10.1016/j.ijcard.2015.06.124. Epub 2015 Jul 2 PMID: 26218180. [DOI] [PubMed] [Google Scholar]
- 49.Bala M.M., Strzeszynski L., Topor-Madry R., Cahill K. Mass media interventions for smoking cessation in adults. Cochrane Database Syst. Rev. 2013;6:CD004704. doi: 10.1002/14651858.CD004704.pub3. Update in: Cochrane Database Syst Rev. 2017 Nov 21;11:CD004704. PMID: 23744348. [DOI] [PubMed] [Google Scholar]
- 50.Carson K.V., Ameer F., Sayehmiri K., Hnin K., van Agteren J.E., Sayehmiri F., Brinn M.P., Esterman A.J., Chang A.B., Smith B.J. Mass media interventions for preventing smoking in young people. Cochrane Database Syst Rev. 2017;6(6):CD001006. doi: 10.1002/14651858.CD001006.pub3. PMID: 28574573; PMCID: PMC6481357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Del Brutto O.H., Montalván M., Tettamanti D., Peñaherrera E., Santibáñez R., Pow-Chon-Long F., Del Brutto V.J. The “know your numbers” program in Atahualpa–a pilot study aimed to reduce cardiovascular diseases and stroke burden in rural communities of developing countries. Int J Cardiol. 2013 Oct 3;168(3):3123–3124. doi: 10.1016/j.ijcard.2013.04.049. Epub 2013 May 4 PMID: 23647598. [DOI] [PubMed] [Google Scholar]
- 52.Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, Federici M, Filippatos G, Grobbee DE, Hansen TB, Huikuri HV, Johansson I, Jüni P, Lettino M, Marx N, Mellbin LG, Östgren CJ, Rocca B, Roffi M, Sattar N, Seferović PM, Sousa-Uva M, Valensi P, Wheeler DC; ESC Scientific Document Group. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020 Jan 7;41(2):255–323. doi: 10.1093/eurheartj/ehz486. Erratum. In: Eur Heart J. 2020;41(45):4317. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.