Abstract
Background
The COVID-19 pandemic has had a profound impact on healthcare systems globally, with a worrying increase in adverse maternal and foetal outcomes. We aimed to assess the changes in maternity healthcare provision and healthcare-seeking by pregnant women during the COVID-19 pandemic.
Methods
We performed a systematic review and meta-analysis of studies of the effects of the pandemic on provision of, access to and attendance at maternity services (CRD42020211753). We searched MEDLINE and Embase in accordance with PRISMA guidelines from January 1st, 2020 to April 17th 2021 for controlled observational studies and research letters reporting primary data comparing maternity healthcare-seeking and healthcare delivery during compared to before the COVID-19 pandemic. Case reports and series, systematic literature reviews, and pre-print studies were excluded. Meta-analysis was performed on comparable outcomes that were reported in two or more studies. Data were combined using random-effects meta-analysis, using risk ratios (RR) or incidence rate ratios (IRR) with 95% confidence intervals (CI).
Findings
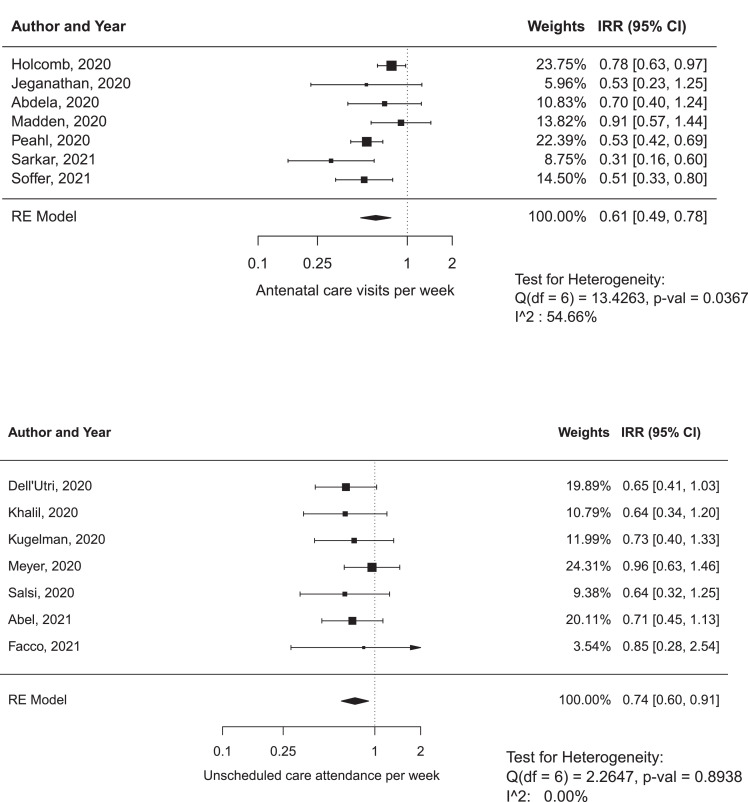
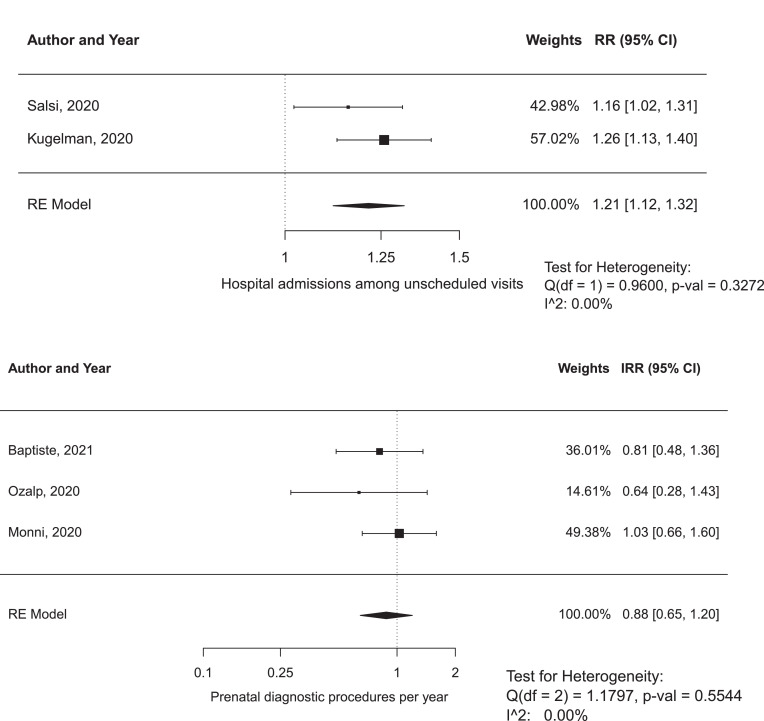
Of 4743 citations identified, 56 were included in the systematic review, and 21 in the meta-analysis. We identified a significant decrease in the number of antenatal clinic visits (IRR 0614, 95% CI 0486–0776, P<00001, I2=54.6%) and unscheduled care visits (IRR 0741, 95% CI 0602–0911, P = 00046, I2=00%) per week, and an increase in virtual or remote antenatal care (IRR 4656 95% CI 7762–2794, P<00001, I2=90.6%) and hospitalisation of unscheduled attendees (RR 1214, 95% CI 1118–1319, P<00001, I2=00%). There was a decrease in the use of GA for category 1 Caesarean sections (CS) (RR 0529, 95% CI 0407–0690, P<00001, I2=00%). There was no significant change in intrapartum epidural use (P = 00896) or the use of GA for elective CS (P = 079)
Interpretation
Reduced maternity healthcare-seeking and healthcare provision during the COVID-19 pandemic has been global, and must be considered as potentially contributing to worsening of pregnancy outcomes observed during the pandemic.
Research in context.
Evidence before this study
During the period of the COVID-19 pandemic significant increases in maternal mortality, stillbirth and maternal depression have been identified. At the same time there has been a reduction in preterm birth in high income settings. The mechanisms underlying the observed changes are unclear, but proposed drivers include the widespread behavioural change associated with national ‘lockdowns’ and other pandemic mitigation measures as well as the restructuring of clinical services that might have led to a reduction of pregnancy care contacts and increased barriers to accessing care.
Added value of this study
This study brings together reports of changes in healthcare usage and provision associated with the COVID-19 pandemic. We show that antenatal care contacts, both planned and emergent, have reduced during the pandemic. The included studies also suggest a reduction in companionship in labour. We also highlight some potentially positive changes – an increase in remote or virtual care provision and reduced postpartum length of stay in hospital. Reassuringly, despite widespread concern at the start of the pandemic response about access to intrapartum analgesia, we have found no evidence of a change in the rate of epidural analgesia associated with the COVID-19 pandemic. A reduction in the use of general anaesthesia for emergency Caesareans was observed.
Implications of all the available evidence
There is a clear change in perinatal outcomes that is contemporaneous with a fall in pregnancy care attendance during the COVID-19 pandemic, especially in low resource settings. While this does not establish a cause, this does support the hypothesis that reduced access to care may have worsened pregnancy outcomes during the pandemic. This finding highlights the need to further investigate the observed changes in perinatal outcomes during the pandemic response while developing robust and equitable maternity care pathways that centre the needs of vulnerable women.
Alt-text: Unlabelled box
1. Introduction
Over the past year maternity services worldwide have faced an unprecedented challenge from the precipitous global spread of the SARS-CoV-2 virus and the attendant societal and healthcare disruption. Initially, the potential effects of this novel virus on pregnancy outcomes, mothers and newborns were a significant concern. Early reports suggested an increase in iatrogenic preterm birth and caesarean birth in infected mothers [1], and there is evidence of an increased risk of maternal intensive care unit (ICU) admission and maternal mortality due to COVID-19 in some settings [2]. Furthermore, multiple reports have raised concerns about the indirect effects of the pandemic on pregnant women and babies, over and above the direct effects of viral infection. An MBRRACE-UK rapid response highlighted an increased number of maternal deaths due to mental health illness, including suicide [3]. Other reports have suggested an increase in the population risk of stillbirth [4,5] but a reduction in overall preterm birth of undetermined mechanism [6], [7], [8], [9]. Our recent meta-analysis has demonstrated an increase in maternal mortality, stillbirth, ruptured ectopic pregnancy and maternal depression during the pandemic [9], and suggested disproportionate adverse effects in lower resource settings.
In response to the pandemic national governments and healthcare providers implemented sweeping changes. In maternity care, face-to-face consultations were widely curtailed with rapid implementation of home blood pressure and blood glucose monitoring programs and telephone antenatal clinics where possible, mostly in high income countries [10]. In many contexts, partners and visitors were restricted from attending outpatient appointments, ultrasound scans or even providing support during intrapartum care [11,12]. Women's healthcare-seeking behaviour has changed; women have reported being less willing to attend hospital due to fear of contracting COVID-19 [13,14]. In addition to misinterpretations of local and national ‘stay at home guidance’, these factors may have impacted on the maternity care provided to mothers during pregnancy and the postpartum period [9]. A similar effect was seen during the Ebola epidemic in West Africa [15].
We undertook a systematic review to evaluate reported changes in maternity care provision and uptake during the global COVID-19 pandemic.
2. Methods
2.1. Overview
A prospective protocol for this systematic review and meta-analysis was developed in accordance with PRISMA guidelines [16] and registered with PROSPERO (CRD42020211753). MEDLINE, Embase and the COVID-19 database were searched electronically, without language restrictions, from 1st January 2020 to 17th April 2021, using combinations of the relevant medical subject heading (MeSH) terms, key words and word variants for pregnancy, antenatal and intrapartum care, and COVID-19 (Supplementary Table 1).
2.2. Search strategy, selection criteria, and data extraction
We included observational studies or research letters reporting primary data on the change in maternity service use (e.g. routine antenatal care attendance or unscheduled attendance) by pregnant women and/or maternity healthcare provision (e.g. virtual antenatal care or postpartum hospital length of stay) during the COVID-19 pandemic, compared to periods before. We excluded case reports and series, guidelines and papers describing mitigation strategies and service adaptation that did not include data on resource use. Two authors reviewed all abstracts and full texts independently (any two of IB, BC and RT), with any conflicts resolved by reference to a third reviewer (AK or EK). Data were then extracted from full texts by two reviewers independently using Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org). Pandemic mitigation response measures were extracted from The Oxford COVID-19 Government Response Tracker [17]. We recorded the maximum restrictions implemented during the study time frame. Quantitative assessment of severity of mitigation measures was recorded according to the Government Response Stringency Index (GRSI) developed by The Blatnavik School of Government, University of Oxford [17].
2.3. Quality assessment
Quality assessment was performed by two reviewers independently (any two of IB, BC and RT) using the Newcastle-Ottawa Scale (NOS), with any conflicts resolved by a third reviewer (AK or EK). According to the scale, each study is judged on three broad perspectives: the selection of the study groups, the comparability of the groups and the ascertainment of outcome of interest [18].
2.4. Statistical analysis
Extracted data were combined in a two stage meta-analysis approach. In the first step, incidence rate ratios (IRR) with their 95% confidence intervals (CI) were estimated from individual studies reporting count data such as number of visits per given time period. Likewise, risk ratios (RR) with 95% CI were estimated from individual studies reporting binary outcome data, such as epidural use. In the second stage, a restricted Maximum Likelihood (REML) random-effects meta-analysis was employed to combine RRs and IRRs from individual studies. Statistical heterogeneity was quantified using the I2 statistic for both analyses; I2 <40% may not be important, 30–60% may represent moderate heterogeneity, 50–90% may represent substantial heterogeneity, and ≥75% represents considerable heterogeneity [19]. Summary statistics were reported as RR for binary outcomes and IRR for count data. Funnel plots displaying the outcome rate from individual studies were created for the exploration of publication bias. Tests for funnel plot asymmetry were not used when the total number of publications included for each outcome was less than ten. In this case, the power of the tests is too low to distinguish chance from real asymmetry [20], [21], [22]. All analyses were conducted using R for Windows software (version 4.0.1) metaphor package.
2.5. Role of the funding source
There was no funding source for this study. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
3. Results
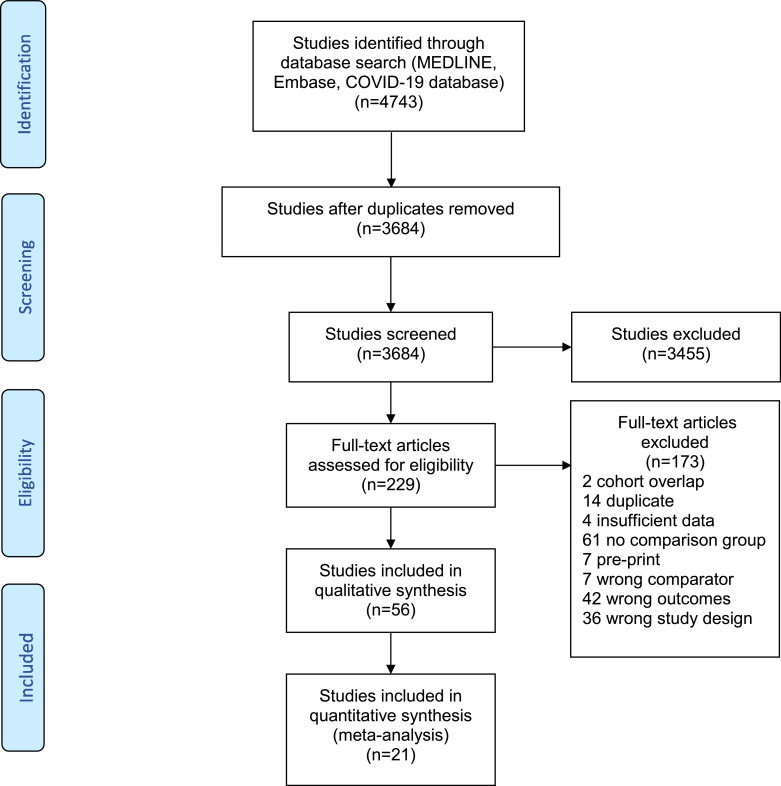
The literature search identified 4743 potentially relevant citations, of which 204 were retrieved for full text review; 56 were included in the qualitative review and 21 in the meta-analysis (Fig. 1, Table 1). Excluded studies and reasons for their exclusion are provided in Supplementary Table 2. The methodological quality of included studies was generally robust, with a median NOS score of 7 out of 9, with only 10 studies scoring less than 7 (Table 2). Importantly, the Comparability domain of the exposed and un-exposed cohorts was good in just over half of cases and the ascertainment of outcomes of interest was of good quality in all studies.
Fig. 1.
PRISMA flow chart.
Table 1.
Characteristics and summary of the findings of the included studies.
| Author (year) | Country | Study Population | GRSI | Country Development Index | Outcomes Reported | Findings in exposed group | NOS Score |
|---|---|---|---|---|---|---|---|
| Abdela (2020) [37] | Ethiopia | Single Centre | 80•56 | LIC | Family planning visits Antenatal clinic attendance Deliveries per week |
Decreased Decreased No change |
7* |
| Abel (2021) [23] | USA | Single Centre | 72.69 | HIC | Obstetric emergency department visits | Decreased | 6* |
| Ahmed (2021) [56] | Bangladesh, Nigeria, South Africa | Multi-centre | Bangladesh: 93.52 Nigeria: 85.65 South Africa:87.96 |
LMIC | Antenatal care (ANC) clinic attendance Family planning clinic attendance Total deliveries Bangladesh Nigeria (two centres) South Africa (two centres) |
Decreased Decreased Decreased Mix Mix |
7* |
| Albert (2020) [72] | Spain | Single Centre | 85•19 | HIC | Report on virtual review of gestational diabetes patients | NA | 5* |
| Anderson (2020) [77] | USA | Single Centre | 72•69 | HIC | Obstetric hospitalisations | Decreased | 7* |
| Baptiste (2021) [32] | USA | Single Centre | 72.69 | HIC | Number of prenatal genetic diagnostic procedures performed Chorionic villus sampling Amniocentesis |
Decreased No change |
9* |
| Bernstein (2021) [33] | USA | Single centre | 72.69 | HIC | Number of in-person visits GA of first prenatal visit GA of dating scan GA of anatomy scan Number of triage visits Total number of ultrasound scans Total number of visits (telehealth and in-person) Total number of no-shows Rates of standard prenatal care metrics (pap smear, genetic screening, GDM screening, GBS screening) Post-partum readmission |
Decreased No change No change Later GA age No change No change Increased No change No change No change |
7* |
| Bertozzi-Villa (2021) [34] |
USA | Single Centre | 72•69 | HIC | Intake obstetric ultrasound scans | Decreased | 7* |
| Bhatia (2020) [48] | UK | Multi-Centre | 79•63 | HIC | General anaesthetic for Caesarean section Regional anaesthesia to general anaesthesia conversion during caesarean section |
Decreased Decreased |
7* |
| Biviá-Rovig (2020) [69] | Spain | Regional (Valencia) | 79•17 | HIC | Cancellation of Antenatal Classes Attendance of Online Classes Cancellation of Appointments due to fear of contagion |
52•2%* 24•4%* 22•5%* |
4* |
| Bornstein (2020) [52] | USA | Multi-Centre | 72•69 | HIC | Postpartum length of stay (hours) CS Postpartum length of stay (hours) VD |
Decreased Decreased |
7* |
| Chen (2020) [59] | China | Regional | 75•46 | UMIC | Online consultations according to severity of pandemic |
||
| Online consultations according to trimester Reason for online consultation |
High rate in severely affected areas for obstetric care-seeking Majority in third trimester Majority for routine care |
7* | |||||
| Dell'Utri (2020) [24] | Italy | Single Centre | 75•46 | HIC | Overall pregnancy related admissions | ||
| Admissions for delivery Postpartum admissions |
Decreased Increased Decreased |
7* | |||||
| Duryea (2021) [35] | USA | Single Centre | 72.69 | HIC | GA at first prenatal visit Total number of prenatal encounters (in-person and virtual) Attendance to prenatal care visits Number of audio-only virtual prenatal visits attended |
Decreased Increased No change Increased |
9* |
| Facco (2021) [36] | USA | Single Centre | 72.69 | HIC | Number of prenatal visits (PNV) Number of postpartum visits (PPV) Length of hospital stay (hours from delivery to discharge) All deliveries VD Maternal post-partum readmission Maternal post-partum emergency department (ED) visits Infant readmission Infant ED visits |
No change No change Decreased Decreased No change Decreased (when stratified for insurance type – only for those with Medicaid insurance) No change Decreased (when stratified for insurance type – only for those with commercial insurance) |
8* |
| Filice (2020) [25] | Italy | Single Centre | 93•52 | HIC | Uptake of toxoplasmosis screening | No change | 7* |
| Futtermann (2020) [26] | USA | Single Centre | 72•69 | HIC | Satisfaction with in-person antenatal appointments Satisfaction with virtual antenatal appointments |
SAPS† score 24 SAPS† score 20 |
9* |
| Gildner (2020) [73] | USA | National Survey | 72•69 | HIC | Changes in birth plan Changes in labour companionship Changes in location Changes in birth plan in hospital |
45•3% reported a change in plan* Qualitative Qualitative Qualitative |
5* |
| Goyal (2020) [13] | India | Single Centre | 100•0 | LMIC | Pregnancy related admissions Antenatal clinic attendance |
Decreased Decreased |
6* |
| Greco (2021) [44] | USA | Single Centre | 72.69 | HIC | Total in-person prenatal hypertensive disorders of pregnancy (HDP) visits Total virtual HDP visits Total number of in-person postpartum HDP visits Total number of no postpartum HDP visits Total number of virtual postpartum HDP visits Diagnosis site of HDP HDP diagnosis timing Post-partum readmission rate |
Decreased No change Decrease Increase Increase (not statistically significant due to 0 in control group) No change No change Increase |
9* |
| Greene (2020) [27] | USA | Single Centre | 72•69 | HIC | Admission to delivery time (hours) Postpartum length of stay (nights) Epidural use |
No change Decreased No change |
8* |
| Gu (2020) [28] | China | Single Centre | 81•02 | UMIC | Outpatient visits per week Hospitalisations per week Emergency Department attendance |
Decreased Decreased Decreased |
9* |
| Holcomb (2020) [29] | USA | Single Centre | 72•69 | HIC | Percentage of appointments conducted virtually Clinic waiting time for in-person visits Clinic attendance for virtual appointments compared to in-person appointments Satisfaction with telemedicine (WHC) Satisfaction with telemedicine (MFM) |
Increased Decreased Higher 95% good or very good* 87% good or very good* |
7* |
| Hui (2020) [30] | Hong Kong | Single Centre | 66•67 | HIC | Rate of hospital births Proportion of women with labour companionship Epidural use Administration of pethidine injections |
Decreased Decreased No change Increased |
5* |
| Hussain (2021) [45] | USA | Single centre | 72.69 | HIC | GA at diagnosis of GDM Total GDM antenatal visits Visits with self-reported blood glucose data (compared to downloaded) Total antenatal GDM ultrasounds In-person and telemedicine attendance |
No change Decreased Increased Decreased Increased |
9* |
| Jeganathan (2020) [70] | USA | Multi-Centre | 72•69 | HIC | Antenatal clinic attendance Antenatal clinic ‘no show’ Antenatal clinic cancellation Antenatal clinic cancellation by patient Patient satisfaction with telemedicine Provider satisfaction with telemedicine |
Decreased Decreased Increased Decreased 86•9% satisfied* 87•8% satisfied* |
8* |
| Justman (2020) [50] | Israel |
Single Centre | 94•44 | HIC | Hospital admissions Triage attendance High risk clinic visits Ultrasound visits Total number of births Epidural use |
Decreased Decreased Decreased Decreased Decreased Increased |
9* |
| KC (2020) [64] | Nepal | Multi-Centre | 96•3 | LMIC | Births per week Attendance at childbirth services by disadvantaged groups Companionship during labour Hand hygiene practices by clinicians during childbirth Clinician use of gloves and gowns during childbirth Intrapartum foetal heart rate monitoring Preparation of equipment used during childbirth Skin to skin after birth |
Decreased Decreased Decreased Increased Decreased Decreased No change Increased |
9* |
| Khalil (2020) [31] | UK | Single Centre | 79•63 | HIC | Antenatal bookings per week Obstetric triage attendance per week Births per week |
Decreased Decreased Decreased |
7* |
| Krishnamurti (2021) [81] | USA | Single Centre | 72.69 | HIC | Women completing the onboarding process for a prenatal care app Use of in-app intimate partner violence (IPV) risk assessment Rates of IPV |
Decreased Increased Increased (non-significant) |
7* |
| Kugelman (2020) [71] | Israel | Single Centre | 94•44 | HIC | Hospitalisation from obstetric triage Admission to Delivery Suite from triage Presentation with reduced foetal movements Presentation with premature rupture of membranes Home birth Admission in second stage of labour Obstetric Emergency Department Visits |
Increased Increased Increased Increased No change No change Decreased |
9* |
| Kumari (2020) [63] | India | Multi-Centre | 100•0 | LMIC | Hospitalisation Referred obstetric emergencies |
Decreased Decreased |
9* |
| Limaye (2020) [43] | USA | Single Centre | 72•69 | HIC | Percentage of telehealth visits | Higher proportion in those with private health insurance | 8* |
| Liu (2020) [62] | China | Multi-Centre | 77•31 | UMIC | Patient request for online consultation Change of planned mode of birth from vaginal to elective caesarean section due to the pandemic Change of planned mode of birth from caesarean section to vaginal delivery due to the pandemic |
75•4% Wuhan, 69•5% Chongqing* 12•7% Wuhan, 6•0% Chongqing* 5•6% Wuhan, 3•1% Chongqing* |
6* |
| Madden (2020) [66] | USA | Multi-centre | 72•69 | HIC | Proportion of antenatal clinic visits conducted virtually Proportion of booked visits that were ‘no shows’ |
Increased Decreased |
7* |
| McDonnell (2020) [38] |
Ireland | Single Centre | 90•74 | HIC | Unbooked mothers presenting in labour Babies born before arrival |
No change No change |
8* |
| Meyer (2020) [39] | Israel | Single Centre | 94•44 | HIC | Referral indications from Emergency Department Duration of treatment until decision Emergency Department referrals Admission in active labour |
No change No change Decreased Increased |
|
| Monni (2020) [53] | Italy | Single Centre | 93•52 | HIC | First trimester prenatal screening Second trimester prenatal screening Third trimester prenatal screening Performance of invasive foetal testing |
Increased No change No change Increased |
7* |
| Moyer (2020) [60] | Ghana | National Survey | 52•78 | LMIC | Missed antenatal visit Plan to deliver in hospital/health centre |
36•2%* Decreased |
6* |
| Ozalp (2020) [54] | Turkey | Single Centre | 77•78 | UMIC | Rate of women accepting offered invasive testing Number of procedures performed Chorionic villus sampling Amniocentesis Cordocentesis |
Decreased Decreased Decreased Increased |
9* |
| Patkar-Kattimani (2021) [49] | UK | Single Centre | 79.63 | HIC | Epidural use Epidural response time <30 min Emergency general anaesthesia rate General anaesthesia for elective CS |
No change No change Reduction Increase |
7* |
| Peahl (2020) [42] | USA | Single Centre | 72•69 | HIC | Average total antenatal clinic visit volume Proportion of antenatal clinic visits conducted virtually Patient satisfaction with telemedicine Provider satisfaction with telemedicine |
Decreased Increased 77•5%* 83•1%* |
8* |
| Racine (2021) [51] | USA | Single Centre | 72.69 | HIC | Likelihood of attending in spontaneous labour Likelihood of need for induction Maternal length of stay Neonatal length of stay Delivery >41 weeks |
Increased Decreased Decreased Decreased Increased |
7* |
| Sarkar (2021) [58] | India | Single Centre | 100 | LMIC | Total antenatal attendance New patients Old patients Total gynaecology outpatient attendance (including infertility, postpartum and termination of pregnancy) |
Decreased Decreased Decreased Decreased |
7* |
| Sakowicz (2021) [74] | USA | Single centre | 72.69 | HIC | Post-partum visit attendance (virtually and in-person) Likelihood of having post-partum depression screening |
Decreased Decreased |
7* |
| Sakowicz (2) (2021) [75] | USA | Single cenre | 72.69 | HIC | Long acting reversible contraceptive use postpartum | Decreased | 8* |
| Salsi (2020) [68] | Italy | Single Centre | 91•67 | HIC | Self-referrals to the Emergency Department Number of admissions Proportion of admissions |
Decreased Decreased Increased |
8* |
| Selinger (2021) [46] | UK | Multi-centre | 79.63 | HIC | Face to face IBD clinic during pregnancy Telephone IBD clinic during pregnancy |
Decreased Increased |
8* |
| Shields (2020) [41] | USA | Single Centre | 72•69 | HIC | Visits per day after conversion to telehealth ‘No shows’ after implementation of telehealth Invasive prenatal testing |
Decreased Decreased No change |
7* |
| Silverman (2020) [67] | USA | Single Centre | 72•69 | HIC | Antenatal clinic attendance | No change | 6* |
| Soffer (2021) [47] | USA | Single Centre | 72.69 | HIC | In-person prenatal care visits Third trimester ultrasound scans Detection of foetal growth restriction (FGR) Telehealth visits GA at diagnosis of FGR |
Decreased Decreased Decreased Increased No change |
7* |
| Sun (2020) [55] | Brazil | Single Centre | 81•02 | UMIC | Delivery within 3 h of admission | Increased | 6* |
| Tadesse (2020) [61] | Ethiopia | Single Centre | 80•56 | LIC | Missed/delayed access to antenatal services Full utilisation of antenatal services Age of patients Education level of patients Urban residency |
55•5%* 29•3%* Positively associated with utilisation Positively associated with utilisation Positively associated with utilisation |
8* |
| Wanyana (2021) [57] | Rwanda | Multi-centre | 90.74 | LIC | ANC first standard visit utilisation rate Deliveries at health facility Mothers in labour referred to higher level for delivery 1ST PNC visit (maternal and infant) utilisation rate 4TH PNC visit (maternal and infant) utilisation rate Vaccination uptake |
Decrease Decrease No change No change Increase Decrease |
7* |
| Weingarten (2021) [40] | USA | Single centre | 72.69 | HIC | Virtual prenatal diabetic visits In person prenatal diabetic visits |
Increased Decreased |
9* |
| Zarasvand (2020) [65] | UK | Single Centre | 79•63 | HIC | Number of face-to-face appointments Number of telephone appointments Use of regional anaesthetic for cerclage placement New referrals to preterm birth services Inappropriate referral percentage |
||
| Total number of clinic appointments | Decreased Increased Increased Increased No change Increased |
7* |
*Results from survey, no comparison group.
†SAPS: Short Assessment of Patient Satisfaction.
GRSI: government response stringency index, NOS: Newcastle-Ottawa Scale.
LIC: lower income country. HIC: high income country. LMIC: lower middle income country. UMIC: upper middle income country. CS: caesarean section. VD: vaginal delivery. WHC: women's health clinic. MFM: maternal foetal medicine, NA: not applicable: .
Table 2.
Quality Assessment of the included studies using the Newcastle-Ottawa Scale (NOS).
| Author | Selection | Comparability | Outcome | Total (max score: 9*) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Represent-ativeness of exposed cohort (max score: *) | Selection of non-exposed (max score: *) | Ascertain-ment of exposure (max score: *) | Demonstration that outcome of interest was not present at start of study (max score: *) | Comparability of cohorts on the basis of design or analysis (max score: ⁑) | Assessment of outcome (max score: *) | Was follow-up long enough for outcomes to occur (max score: *) | Adequacy of follow up (max score: *) | ||
| Abdela (2020) [37] | * | * | * | * | – | * | * | * | 7* |
| Abel (2021) [23] | * | * | * | – | – | * | * | * | 6* |
| Ahmed (2021) [56] | * | * | * | * | – | * | * | * | 7* |
| Albert (2020) [72] | * | – | * | – | – | * | * | * | 5* |
| Anderson (2020) [77] | * | * | * | * | – | * | * | * | 7* |
| Baptiste (2021) [32] | * | * | * | * | ⁑ | * | * | * | 9* |
| Bernstein (2021) [33] | * | * | * | * | – | * | * | * | 7* |
| Bertozzi-Villa (2021) [34] |
* | * | * | * | – | * | * | * | 7* |
| Bhatia (2020) [48] | * | * | * | * | – | * | * | * | 7* |
| Biviá-Rovig (2020) [69] | – | * | * | – | – | – | * | * | 4* |
| Bornstein (2020) [52] | * | * | * | * | – | * | * | * | 7* |
| Chen (2020) [59] | * | * | * | * | – | * | * | * | 7* |
| Dell'Utri (2020) [24] | * | * | * | * | – | * | * | * | 7* |
| Duryea (2021) [35] | * | * | * | * | ⁑ | * | * | * | 9* |
| Facco (2021) [36] | * | * | * | * | * | * | * | * | 8* |
| Filice (2020) [25] | * | * | * | * | – | * | * | * | 7* |
| Futtermann (2020) [26] | * | * | * | * | ⁑ | * | * | * | 9* |
| Gildner (2020) [73] | – | – | * | * | * | – | * | * | 5* |
| Goyal (2020) [13] | – | * | * | * | – | * | * | * | 6* |
| Greco (2021) [44] | * | * | * | * | ⁑ | * | * | * | 9* |
| Greene (2020) [27] | * | * | * | * | * | * | * | * | 8* |
| Gu (2020) [28] | * | * | * | * | ⁑ | * | * | * | 9* |
| Holcomb (2020) [29] | * | * | * | * | – | * | * | * | 7* |
| Hui (2020) [30] | * | * | * | – | – | – | * | * | 5* |
| Hussain (2021) [45] | * | * | * | * | ⁑ | * | * | * | 9* |
| Jeganathan (2020) [70] | * | * | * | * | * | * | * | * | 8* |
| Justman (2020) [50] | * | * | * | * | ⁑ | * | * | * | 9* |
| KC (2020) [64] | * | * | * | * | ⁑ | * | * | * | 9* |
| Khalil (2020) [31] | * | * | * | * | – | * | * | * | 7* |
| Krishnamurti (2021) [81] | * | * | * | – | * | * | * | * | 7* |
| Kugelman (2020) [71] | * | * | * | * | ⁑ | * | * | * | 9* |
| Kumari (2020) [63] | * | * | * | * | ⁑ | * | * | * | 9* |
| Limaye (2020) [43] | * | * | * | * | * | * | * | * | 8* |
| Liu (2020) [62] | – | * | * | – | ⁑ | – | * | * | 6* |
| Madden (2020) [66] | – | * | * | * | * | * | * | * | 7* |
| McDonnell (2020) [38] |
* | * | * | * | * | * | * | * | 8* |
| Meyer (2020) [39] | * | * | * | * | – | * | * | * | 7* |
| Monni (2020) [53] | * | * | * | * | – | * | * | * | 7* |
| Moyer (2020) [60] | – | – | * | * | * | * | * | * | 6* |
| Ozalp (2020) [54] | * | * | * | * | ⁑ | * | * | * | 9* |
| Patkar-Kattimani (2021) [49] | * | * | * | * | – | * | * | * | 7* |
| Peahl (2020) [42] | * | * | * | * | ⁑ | – | * | * | 8* |
| Racine (2021) [51] | * | * | * | * | – | * | * | * | 7* |
| Sarkar (2021) [58] | * | * | * | * | – | * | * | * | 7* |
| Sakowicz (2021) [74] | * | * | * | – | * | * | * | * | 7* |
| Sakowicz (2) (2021) [75] | * | * | * | – | ⁑ | * | * | * | 8* |
| Salsi (2020) [68] | * | * | * | * | * | * | * | * | 8* |
| Selinger (2021) [46] | * | – | * | * | ⁑ | * | * | * | 8* |
| Shields (2020) [41] | * | * | * | * | – | * | * | * | 7* |
| Silverman (2020) [67] | * | * | * | – | – | * | * | * | 6* |
| Soffer (2021) [47] | * | * | * | * | – | * | * | * | 7* |
| Sun (2020) [55] | – | * | * | * | – | * | * | * | 6* |
| Tadesse (2020) [61] | * | – | * | * | ⁑ | * | * | * | 8* |
| Wanyana (2021) [57] | * | * | * | * | – | * | * | * | 7* |
| Weingarten (2021) [40] | * | * | * | * | ⁑ | * | * | * | 9* |
| Zarasvand (2020) [65] | * | * | * | * | – | * | * | * | 7* |
The majority of studies reported findings from a single hospital site or group of facilities relating to specific and highly variable changes in protocols made during the pandemic [13,[23], [24], [25], [26], [37], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39]]. This ranged from the institution of new telehealth services [29,33,35,[40], [41], [42], [43], [44], [45], [46], [47]], altered hospital admission and discharge protocols [27,30,[48], [49], [50]], variance in anaesthetic management [27,36,51,52], and harmonisation of regional antenatal screening services [32,53,54]. Only 14 of the 56 papers reported data from low- or middle-income (LMIC) countries according to World Bank classification [13,28,37,[54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64]]. Lockdown measures in countries included in the studies varied from a GRSI [17] of 6667 to 1000. Comparison periods were most commonly from a similar timeframe in the preceding year/s, with fewer studies reporting data on the months immediately prior to the pandemic response (Table 3). Where two or more studies reported comparable outcomes, meta-analysis was undertaken. Publication bias could not be formally assessed for any of the outcomes due to low number of studies for each outcome.
Table 3.
Characteristics and summary of the findings of studies and outcomes included in the meta-analysis.
| Author (Year) | Pandemic Period | Comparison Period | Events in exposed cohort | Total number in exposed cohort | Events in comparison cohort | Total number in exposed cohort |
|---|---|---|---|---|---|---|
| Abdela (2020) [37] | 23/3/2020–19/4/2020 | 24/02/2020–22/3/2020 |
ANC per week: 60 | n/a | ANC per week: 86 | n/a |
| Abel (2021) [23] |
4/3/2020–1/9/2020 | 01/01/2020–03/03/2020 | Unscheduled visits per week: 554 |
n/a | Unscheduled visits per week: 778 | n/a |
| Baptiste (2021) [32] |
01/01/2020–31/07/2020 | 01/01/2019–31/07/2019 | Prenatal diagnosis procedures per year: 377 | n/a | Prenatal diagnosis procedures per year: 464 | n/a |
| Bhatia (2020) [48] | 01/04/2020–01/07/2020 | 01/04/2019–01/07/2019 |
GA for ELCS: 14 | 1083 | GA for ELCS: 28 | 1059 |
| Dell'Utri (2020) [24] | 23/02/2020 – 24/06/2020 | 23/02/2019 – 24/06/2019 | Unscheduled visits per week: 260 | n/a | Unscheduled visits per week: 403 | n/a |
| Facco (2020) [36] | 01/04/2020–01/07/2020 | 01/04/2019–01/07/2019 | Unscheduled visits per week: 18 |
n/a | Unscheduled visits per week: 22 | n/a |
| Holcomb (2020) [29] | 22/3/2020–31/5/2020 |
23/2/2020–21/3/2020 | ANC per week 1888 Virtual per week 399 |
n/a | ANC per week 2409 Virtual per week 0 |
n/a |
| Hui (2020) [30] | 5/01/2020 – 30/04/2020 | 1/01/2019 – 4/01/2020 | Epidural use: 126 |
954 | Epidural use: 461 | 3577 |
| Jeganathan (2020) [70] | 1/3/2020–30/5/2019 | 1/3/2019–30/5/2019 | ANC per week 42 Virtual per week 21 |
n/a | ANC per week 79 Virtual per week 0 |
n/a |
| Justman (2020) [50] | 01/03/2020 – 30/04/2020 | 01/03/2019 – 30/04/2019 |
Epidural use: 507 | 610 | Epidural use: 572 | 742 |
| Khalil (2020) [31] | 1/2/2020–14/6/2020 | 1/10/2019–31/1/2020 | Unscheduled visits per week: 96 | n/a | Unscheduled visits per week: 119 | n/a |
| Kugelman (2020) [71] | 15/03/2020 – 12/04/2020 | 15/03/2019 – 12/04/2019 | Unscheduled visits per week: 136 Hospital admissions: 257 |
398 | Unscheduled visits per week: 136 Hospital admissions: 279 |
544 |
| Madden (2020) [66] | 17/3/2020 – 12/4/2020 | 9/3/2020–16/3/2020 | ANC per week 378 Virtual per week 187 |
n/a | ANC per week 417 Virtual per week 4 |
n/a |
| Meyer (2020) [39] | 1/2/2020–28/3/2020 | 1/2/2019 – 28/3/2019 | Unscheduled visits per week: 462 | n/a | Unscheduled visits per week: 483 | n/a |
| Monni (2020) [53] | 10/03/2020–18/05/2020 | 10/03/2019–18/05/2019 | Prenatal diagnosis procedures per year: 793 | n/a | Prenatal diagnosis procedures per year: 772 | n/a |
| Ozalp (2020) [54] | 11/03/2020–30/06/2020 | 11/03/2019–30/06/2019 | Prenatal diagnosis procedures per year: 56 | 129 | Prenatal diagnosis procedures per year: 88 | 138 |
| Patkar-Kamminati (2021) [49] |
12/03/2020–11/06/2020 | 01/10/2019–31/12/2019 | GA for ELCS: 4 GA for EMCS: 8 |
172 58 |
GA for ELCS: 2 GA for EMCS: 18 |
186 67 |
| Peahl (2020) [42] | 20/3/2020 – 28/6/2020 | 16/12/2019–20/3/2020 | ANC per week 430 Virtual per week 332 |
ANC per week 805 Virtual per week 97 |
||
| Salsi (2020) [68] | 1/3/2020 – 31/3/2020 | 1/3/2019 – 31/3/2019 | Unscheduled visits per week: 57 Hospital admissions: 164 |
254 | Unscheduled visits per week: 90 Hospital admissions: 223 |
400 |
| Sarkar (2021) [58] | 23/02/2020–31/05/2020 | 12/01/2020–22/03/2020 | ANC per week 99 |
n/a | ANC per week 321 |
n/a |
| Soffer (2021) [47] |
01/04/2020–31/07/2020 | 01/04/2019–31/07/2019 | ANC per week 594 Virtual per week 251 |
1296 | ANC per week 1156 Virtual per week 0 |
1345 |
3.1. Maternity service use
3.1.1. Antenatal clinic attendance
Twenty-five studies [13,26,28,29,33,[35], [36], [37],40,42,[44], [45], [46], [47],50, [56], [57], [58],60,[65], [66], [67], [68], [69], [70]] reported on antenatal clinic attendance during the pandemic using a variety of metrics. In several settings, no alteration was made to the standard antenatal care protocol, but decreased antenatal clinic attendance was reported in the majority of studies; in high income settings a decline in face to face contacts was offset by an increase in remote or virtual clinic appointments and the nature but not the number of the appointments varied [26,29,35,40,[42], [43], [44], [45],47,66,70]. Reports from low resource settings noted a particularly profound reduction in antenatal care contacts. One hospital in Ethiopia noted a fall in antenatal clinic attendance of over 29% [37] (from an average to 86 pregnant women per week to 61) even while delivery rates were maintained, whilst another found that only 293% of (114 out of 389) women giving birth had accessed all recommended antenatal visits [61]. A multicentre study identified reduced antenatal clinic attendance in Bangladesh, Nigeria and South Africa during the pandemic response [56] with similar findings in two additional reports from India [13,58]. Women cited both difficulties in travel and fear of contracting COVID-19 in healthcare settings as their reasons for not attending. A study in Ghana revealed over one third (25 of 71; 362%) missed an antenatal clinic appointment; [60] public transport was seriously restricted during lockdown and virtual appointments were not possible. In contrast, a report from a New York program serving primarily women of low socioeconomic status reported no change in clinic attendance during the pandemic response [67].
Seven studies reported on the number of scheduled antenatal visits in person per week [29,37,42,47,58,66,70]. Quantitative synthesis showed that overall there was a 38.6% drop in care appointments during the pandemic period (pooled IRR: 0614, 95% CI 0486 – 0776; P<00001) (Table 3, Fig. 2a) with evidence of moderate heterogeneity amongst the included studies (I2=54.6%).
Fig. 2.
Forest plots for antenatal care visits per week (2a), unscheduled care attendance per week (2b), hospital admissions amongst unscheduled attendance (2c) and prenatal diagnostic procedures per year (2d).
3.1.2. Antenatal screening
Of particular concern is the impact of the pandemic on routine antenatal screening for infection, anaemia and foetal anomaly, none of which can be offered virtually. In one Italian study, attendance for a variety of routine outpatient encounters was reduced in comparison with the equivalent period in 2019 [25]. The reduction was smallest for antenatal toxoplasmosis screening (740 vs. 1005 visits, 26% reduction), and greatest for non-obstetric outpatient encounters (799 vs. 4253 visits, 81% reduction). One unit in Israel and two from the USA reported reductions in antenatal ultrasound visits during the pandemic period (absolute numbers not given) [33,34,50]. This finding raises concern that women may have been less able to access foetal anomaly screening where desired. In three studies reporting on invasive prenatal genetic testing all noted changes in the timing of presentation and type of procedures performed [32,53,54]. In one study from Turkey, fewer women took up the offer of chorionic villus sampling and amniocentesis - during (n = 56, 434%) compared with before (n = 88, 638%) the pandemic [54]. Nevertheless, more invasive testing in later pregnancy was offered via cordocentesis (n = 6, 11%), raising the possibility that screening tests had been delayed during early pregnancy. One foetal medicine centre in Sardinia, Italy, observed an increase in first trimester screening attendance (70% of population during vs. 50% pre-pandemic) and invasive procedure rates (n = 150 during vs n = 146 pre-pandemic), attributed to increased referrals from other centres that were unable to offer COVID-secure testing [53]. Second and third trimester visits were unaffected. A third study from the US reported a significant decrease in CVS although amniocentesis rates were unchanged, attributed in this case to later referral or access to prenatal screening [32]. Meta-analysis showed a non-significant change in prenatal diagnostic procedures performed per year (pooled IRR: 0880, 95% CI: 0645–1199; P = 0419).
3.1.3. Unscheduled care attendance
In seven studies, quantitative synthesis showed a decrease in unscheduled care attendance at maternity triage, urgent care or obstetric emergency departments, in Italy, Israel, the USA and the UK (pooled IRR 0741, 95% CI: 0602–0911, I2=0%, P = 00046) (Table 4, Fig. 2b).23,24,31,36,39,68,71In the two studies that reported the outcome, from Israel and Italy, the associated risk of hospital admission amongst 1042 pregnant women who presented at the emergency department significantly increased, by 214% (pooled RR 1214, 95% CI: 1118–1319, I2=0%, P<0.0001) (Table 4, Fig. 2c) [68,71]. Variable results were found in three studies that reported on measures of delay in care-seeking during labour. In one report from Brazil of 81 patients in spontaneous labour, the proportion who delivered within three hours of hospital presentation increased from 268% in 2019 to 40% in the equivalent period in 2020 [55]. While one Californian hospital reported no change in mean admission to delivery time, both spontaneous and induced labours were included in the comparison [27]. In a large Irish study no change in births before arrival (BBA) was noted [38].
Table 4.
Results of the quantitative synthesis.
| Outcomes | Studies | Pre-pandemic | Post-pandemic | Pooled estimate †(95% CI) | P | I[2] |
|---|---|---|---|---|---|---|
| Number of antenatal care appointments per week | Holcomb [29] | 2409 | 1888 | IRR 0•614 (0•486 – 0•776) | <0•0001 | 54•6% |
| Jeganathan [70] | 79 | 42 | ||||
| Abdela [37] | 86 | 60 | ||||
| Madden [66] | 417 | 378 | ||||
| Peahl [42] | 805 | 430 | ||||
| Sarkar [58] | 321 | 99 | ||||
| Soffer [47] | 1156 | 594 | ||||
| Number of virtual or over the phone visits per week | Holcomb [29] | 0 | 399 | IRR 46•56 (7•762 – 279•4) | <0•0001 | 90•6% |
| Jeganathan [70] | 0 | 21 | ||||
| Madden [66] | 4 | 187 | ||||
| Peahl [42] | 97 | 332 | ||||
| Soffer [47] | 0 | 251 | ||||
| Number of unscheduled care visits per week | Dell'Utri [24] | 403 | 260 | IRR 0•741 (0•602 – 0•911) | 0•0046 | 0•0% |
| Khalil [31] | 119 | 96 | ||||
| Kugelman [71] | 136 | 99 | ||||
| Meyer [39] | 483 | 462 | ||||
| Salsi [68] | 90 | 57 | ||||
| Abel [23] | 778 | 554 | ||||
| Facco [36] | 22 | 18 | ||||
| Number of prenatal diagnosis procedures per year | Baptiste [32] | 464 | 377 | IRR 0•880 (0•645 – 1•199) | 0•41 | 0•0% |
| Ozalp [54] | 88 | 56 | ||||
| Monni [53] | 772 | 793 | ||||
| Hospital admissions amongst unscheduled care visits | Salsi [68] | 55•7% (223/400) |
64•6% (164/254) | RR 1•214 (1•118 – 1•319) | <0•0001 | 0•0% |
| Kugelman [71] | 51•3% (279/544) |
64•6% (257/398) |
||||
| General anaesthesia for ELCS | Bhatia [48] | 2•6% (28/1059) | 1•3% (14/1083) | RR 0•831 (0•205 – 3•356) | 0•79 | 61•8% |
| Patkar-Kamminati [49] | 1•1% (2/186) | 2•3% (4/172) | ||||
| General anaesthesia for EMCS | Bhatia [48] | 24•3% (118/486) | 12•9% (61/472) |
RR 0•529 (0•407 – 0•690) | <0•0001 | 0•0% |
| Patkar-Kamminati [49] | 26•9% (18/67) |
13•8% (8/58) | ||||
| Epidural use | Hui [30] | 12•9% (461/3577) |
13•2% (126/954) |
RR 1•044 (0•993 – 1•098) | 0•0896 | 37•4% |
| Justman [50] | 77•1% (572/742) |
83•1% (507/610) |
*Individual patient data quantitative synthesis using generalised Poisson regression with random intercepts for studies reporting events per week. Mantel-Haenszel random effects meta-analysis for outcomes reported given a number of dependant events.
IRR: incidence rate ratio, RR: risk ratio, CI: confidence interval.
3.2. Maternity healthcare provision
3.2.1. Virtual antenatal care protocols
Many reports described new provision of virtual services that enabled clinical contact to continue while reducing in-person clinic visits. A wide variety of protocols were described encompassing both routine care and specialist clinics providing care for the hypertensive disorders of pregnancy [44], diabetes [40,45,72], women at risk of preterm birth [65] and women with inflammatory bowel disease [46]. For example, in Nanjing, China, strict screening protocols were introduced for face-to-face antenatal care while telemedicine appointments were offered as an alternative for routine visits, and home monitoring of blood glucose and blood pressure was utilised [28]. For 2458 women studied, the number of in-person visits was significantly reduced from approximately 500 to 200 visits per week, without an associated change in maternal and neonatal outcomes or hospital acquired infections for women with diabetes or high blood pressure.
In one obstetric service in New York, telemedicine via either audio or video link was introduced for most high-risk prenatal care, including gestational diabetes education, genetic counselling and maternal-foetal medicine consultations. The telemedicine protocol included self-monitoring of blood pressure via the provision of automated sphygmomanometers but not foetal heart auscultation, and the majority of contacts were conducted via video link. For 91 women studied, 29% of visits were conducted using telemedicine; patient non-attendance was decreased and both patients (869%) and providers (878%) reported satisfaction with the service [70]. Another New York centre reported conducting 318% (1354 of 4248) of prenatal care visits using video communication within the electronic record accessed by the patients on smart phones or other devices [66], with 92% provider satisfaction when appointments were scheduled appropriately. This group identified that Medicaid patients had higher rates of non-attendance than patients with private insurance. A further New York study reported similar findings: patients with public insurance were less likely to have had at least one telehealth visit (609 vs. 873%, P <0001), although it is not clear if this was patient or insurer driven [43]. One unit in Texas offered audio-only virtual appointments because they predicted that most of their patients lacked access to high-speed internet [29]. By the end of the study period of two weeks, around 25% of prenatal visits were conducted remotely. Average waiting times for women attending in person were reduced (21 min) and a greater proportion of prenatal visits were completed virtually than in person (88% vs 82%, P<0001). The benefits of virtual appointments cited by patients included reduced requirement to use public transport during the pandemic, less time away from work, and less need to arrange childcare assistance. In a relatively more privileged population in Michigan, a prenatal care schedule utilising virtual appointments via either audio or video link was implemented and supported with the distribution of home sphygmomanometers to patients in the third trimester [42]; average weekly clinic visit volume decreased by 332 (316%), and virtual visits increased from 101 to 239 (1366%). Around two-thirds of respondents felt that virtual visits were as safe as in-person visits (648% of patients and 65% of providers), but only 371% of patients and 455% of providers felt that the overall quality of virtual appointments was equivalent to face-to-face visits [42]. Interestingly, there was a discrepancy between patient and provider enthusiasm for continuing virtual visits after the pandemic, with only 403% of patients in favour compared to 922% of providers.
A specialised preterm birth clinic in the UK reported that it reduced face-to-face appointments by 54% from 341 to 157, by increasing their telephone consultations from 0 to 221 (64%) and changing definitions of high- and intermediate-risk referral criteria. By questionnaire, 625% of women indicated they ‘did not mind’ having remote consultations, and 75% were happy or had no preference for telephone over video consultations [65]. A Spanish clinic caring for women with gestational diabetes reduced their face-to-face visits by 886% by using a smartphone app to monitor blood glucose remotely [72].
Five studies reported the number of virtual or over the phone visits per week during, compared to before, the pandemic [29,42,47,66,70]. There was an almost 46-fold increase in the number of virtual appointments during the pandemic period (pooled IRR 4656, 95% CI 7762–2794, P<00001) (Table 4), which balanced the reduction in the number of in-person appointments. There was significant heterogeneity amongst included studies (I2=906%).
3.2.2. Intrapartum analgesia
Quantitative synthesis of two studies found no change in epidural analgesia use during labour (pooled RR 1044, 95% CI 0993–1098, P = 00896) (Table 3) [30,50].
In a study of six UK hospitals with over 17,000 births collectively, the rate of general anaesthesia for caesarean section was reduced from 77% in 2019 to 37% during the equivalent period in 2020, an RR of 050 (95% CI 039 – 063) [48]. A similar proportional reduction in intra-operative conversion from regional to general anaesthesia was observed from 16% (n = 39) to 08% (n = 19). This finding was supported by a second UK based study [49], and pooled analysis showed that general anaesthesia use for category I (the most urgent) caesarean sections were significantly reduced during the pandemic period (pooled RR 0529, 95% CI 0407–0690, P<00001) while general anaesthesia use for elective caesarean was unchanged (pooled RR 0831, 95% CI 0205–3356, P = 079) (Table 4).
3.2.3. Companionship in labour
Three papers reported changes in the proportion of women having personal companionship in labour. In Nepal (20,354 women), the reduction was small (894% to 834%, P = 00014) [64], while in Hong Kong (2138 women) the reduction was large (888% to 218%, P<005) [30]. One paper reported on the number of women anticipating a reduction in support persons present in labour and an associated increase in planned home births [73]. The data could not be pooled as the definition of companionship varied amongst studies – in some contexts family members take an active role in personal care and physical support of the labouring person while in others the role is primarily the provision of social and emotional support. .
3.2.4. Hospital length of stay after birth
Four studies reported length of hospital stay after admission for birth using varying metrics; in all cases, length of stay was reduced after both vaginal births and caesarean sections during the pandemic [27,36,51,52]. In California, the proportion of women (n = 1339) discharged fewer than three nights after caesarean section increased from 118% prior to COVID-19 practice alterations to 409% afterwards (P<00001); after vaginal birth, the proportion of 597 women (n = 597) who stayed only one night in hospital increased from 249% to 485% (P<00001) [27]. In New York, as the number of hospitalised patients with COVID-19 increased, the median postpartum length of stay decreased from a median of 48 to 34 h after vaginal birth (P<00001) and from a median of 74 to 51 h after caesarean section (P<00001) [52].
3.3. Postnatal care
Postnatal care is critical to the long term health of both mother and child – several studies highlighted reduced postpartum visit attendance [58,74], which was in some cases associated with reduced uptake of postnatal long acting contraception (OR 067 (95% CI 053–084)) [75] or probability of receiving screening for postpartum depression (862% vs 455%, P <001) [74]. This was not universal; in Rwanda postnatal care attendance was unaffected even as antenatal care contacts were reduced [57], while for women receiving remote postnatal follow up for hypertension in pregnancy care contacts were actually increased [44].
4. Discussion
This review has provided evidence that pregnant women have altered their healthcare-seeking behaviour during the COVID-19 pandemic, in a variety of contexts, and there has also been rapid and substantive change to maternity care provision globally. There has been a substantial decrease in the number of scheduled and unscheduled antenatal care visits, hospitalisations when urgent care has been sought, a reduction in antenatal care screening uptake (including but not limited to ultrasound and prenatal genetic testing), and delayed attendance at the planned place of care when labour starts. Maternity healthcare provision has also been affected as evidenced by a clear increase in virtual or remote consultations, decrease in face-to-face appointments, and reduction in waiting times; however, people with fewer resources within a population group may have had less access to telehealth, based on data from the USA. Moreover, there was a reduction in companionship allowed during birth, and a reduction in postpartum hospital length of stay, regardless of mode of birth.
The strengths of this review include the comprehensive literature search and rigorous methodology. However, the findings are limited by the heterogeneity of the included studies and the variety of outcomes reported, which frequently precluded meta-analysis. Where substantial heterogeneity was identified in the quantitative synthesis, we must advise caution in reliance on the meta-analysis outcomes. First, there was no information about public health and local healthcare messaging to which people were exposed, although we are unaware of women in any jurisdiction being advised against healthcare-seeking when concerned. Second, although every hospital and care provider will certainly have made changes in response to the COVID-19 pandemic, only a small proportion will have published their experience and outcomes, and not all of these can be guaranteed to have been identified from this search. In particular, despite evidence highlighting the disproportionate impact of the pandemic response on women and children in low resource settings [76], fewer than a third of the included papers originated from low or middle income countries. Third, patient and provider experience of remote antenatal care during the pandemic may not be generalisable to the future post-pandemic world. Patients frequently cited fear of COVID-19 as a key driver for avoiding face-to-face appointments, whether or not virtual care was available, so when this is no longer a concern, the perceived benefits of in-person consultation may vary. Fourth, potential advantages of remote consultation technology to increase flexibility and efficiency in pregnancy care must not compromise patient safety or the development of the essential therapeutic relationship that is core to safety in maternity care. Finally, we do not know the cost implications of the changes observed.
As each individual study reported on specific and highly variable protocols, they are unlikely to be generalisable but, taken together, these studies demonstrate that significant changes in patient and provider behaviour and care provision occurred during the pandemic response. Where positive developments (e.g. increased access to antenatal services via hybrid face-to-face and remote monitoring care pathways or expedited postnatal discharge pathways) have been identified, some of these rapidly developed innovations are likely to result in permanent change.
The altered patient maternity care-seeking and maternity healthcare provision demonstrated in this review must be considered as potentially contributing to worsening of pregnancy outcomes observed during the pandemic [9]. At this point, it is not possible to establish a causal link; where studies did report clinical outcomes for their included cohorts, the findings were mixed. For example, although it would seem plausible that delayed presentation in labour might be associated with worse perinatal outcomes, the small studies that reported on this outcome reported no differences in maternal or neonatal mortality [38,55,71]. One group used their detailed patient records to identify specific complications potentially attributable to, or exacerbated by, delay in seeking care, including anaemia, post-term pregnancy and pregnancy induced hypertension as the most common, and suggested that these relate to an observed increase in ICU admission and maternal mortality during the pandemic in their small cohort [13]. One study explicitly assessed the changes in antenatal care provision in tandem with perinatal outcomes in the same period and found no difference in their high resource setting where a large proportion of antenatal contacts were delivered remotely [35], but this is not applicable to the contexts where antenatal visits were reduced and not mitigated by increased provision of remote or community based services.
This review provides evidence of reduced attendance for antenatal care and reduced uptake of antenatal screening for infection and foetal anomaly [25,32,54]. In addition, there is clear evidence that in some contexts women have avoided seeking urgent care for pregnancy concerns or attending the planned place of birth when labour occurs. All of these changes may introduce additional risk to mothers and babies, and are plausibly linked to the observed worsening of pregnancy outcomes during the pandemic, including an increase in stillbirths [9]. The significant increase in proportion of hospitalisations of those presenting for urgent care could reflect the proportionate increase in mandatory emergency visits, such as labour or rupture of membranes, compared to less urgent presentations, such as emesis or cramps [68,71,77].
Multiple reports considered the changes that occurred in antenatal care provision during the pandemic response. The introduction or upscaling of remote access technologies was a common feature of the pandemic mitigation strategies implemented worldwide, particularly in high and middle income countries. Potential benefits identified included high levels of both patient and provider satisfaction, and a reduction in ‘no shows’ or ‘did not attend’ [29,42,66,69,70]. There are concerns that virtual consultations carried out in effect in the patient's home may make it less possible for pregnant people to disclose concerns for their own or their children's safety, and impair the development of the therapeutic relationship between woman and care providers. There has, for example, been an increase in intimate partner violence (IPV) during the pandemic, primarily directed against women [78], [79], [80]. Krishnamurthi et al. report increased uptake during the pandemic period of an app developed to support IPV reporting [81] but clearly this pathway is only available to women with access to a smartphone. Several groups noted the danger of reducing access for low income or vulnerable women who might be less able to access high speed internet or video capable personal devices.
This review has also identified evidence of change in practice in relation to obstetric anaesthesia and analgesia in labour. The initial concerns that women might be denied access to epidural analgesia in labour because of redeployment of limited anaesthetic staff were not borne out in the studies reporting on this outcome. We did find evidence that the use of general anaesthesia for intrapartum caesarean section was reduced, which must be examined further in relation to outcomes. Both the studies reporting this outcome originated from the UK where full aerosol PPE was recommended by Public Health England for emergency caesarean section under GA but not under spinal. This may not be observed in other settings, although the increased risk of GA to staff would have been known in every healthcare facility. It may be that general anaesthesia was in fact overused in the pre-pandemic times, without benefits for mothers and babies, but it is also possible that reluctance to initiate general anaesthesia in the context of a pandemic respiratory virus could have contributed to delays in time critical emergency deliveries.
Parents and midwives have repeatedly expressed real concern about the impact of reduction in labour companionship on maternal experience and intrapartum outcomes, and this review has shown that labour companionship has significantly reduced in settings as disparate as Nepal and Hong Kong [30,64]. Labour companionship has been shown to affect both birth experience and outcome, and restrictions on companions should be carefully considered. Throughout the pandemic, the NHS in England has issued guidance emphasising the importance of supporting women to have a birth partner of their choice, although there was anecdotal reporting of local restrictions initially [82]. In high income settings fear of birthing alone has been identified as a driver of increased planned home births, in lower resource settings without skilled attendance provision in the community and robust transfer pathways, this could potentially increase unattended birth. In Dessie region in Ethiopia, for example, 393% of women giving birth reported that their carers and attendants were not permitted to enter the hospital with them for the birth [83].
The COVID-19 pandemic has shone a harsh light of racial and social inequality, both within and between societies and regions. While we have identified some potential positive alterations in maternity care provision, it is likely that the majority of these benefits will be available to financially secure women in high income countries able to benefit from digital innovations in care provision. While in high income countries antenatal care has shifted to a hybrid model without sacrificing the number of contacts [29,33,35,36,44,47,65,66] in low resource settings without recourse to alternative models, steep reductions in antenatal care attendance were observed [13,28,37,[56], [57], [58],60,61]. The development of pandemic response and recovery strategies must be sensitive to the needs of the most vulnerable women in their population – whether considering the loan of smart devices to vulnerable women in high income settings or provision of alternate pathways to care. In low resource settings antenatal care attendance must be facilitated by ensuring women have confidence in the safety of healthcare facilities and the means to reach care where transport and mobility restrictions are in place.
Key themes identified by this review – maintaining key preventive care such as antenatal screening and routine care, the importance of clear communication, and considering the needs of those in lower socio-economic groups and lower income countries - are of relevance to all providers of maternity care. These must be considered as locally-responsive and culturally-appropriate care pathways are re-developed during the evolving pandemic response and into the future. They also provide the opportunity to challenge the established norms of maternity care and consider whether ‘returning to normal’ should be our goal.
One of the greatest healthcare lessons of this global pandemic has been that large structural change in maternity services in an extremely short time frame is possible. If length of postpartum stay can be safely and swiftly reduced, why did it take a pandemic to make this happen? Enhanced recovery protocols for obstetric care exist and could be more widely implemented, and innovative models of care make it possible to provide continuity of carer across hospital, clinic and community sites, and help to achieve the recommended 8 antenatal visits as recommended by the World Health Organization [84].
The COVID-19 pandemic has posed an unprecedented challenge to individuals, society and healthcare systems. This systematic review comprises a detailed and rigorous global assessment of changes in maternity healthcare provision, as well as use by pregnant women. It confirms that reduced maternity care-seeking and healthcare provision have occurred globally. These changes must be considered when evaluating whether demonstrable harms to both mothers and babies could have been avoided. We now have an opportunity to examine in depth the effects of this pandemic on maternity healthcare systems and outcomes, harness and refine the examples of excellent practice that have been implemented at pace, and discard or mitigate those that may have increased the risk of adverse outcomes. The strategic choices made now could either reverse or entrench the harms of this pandemic and their disproportionate effects on the poorest and most vulnerable women globally. It is imperative that we put in place mitigation strategies to minimise the collateral harm to mothers and babies in future health system shocks.
Funding
There was no funding received for this study. Therefore, no funder had any involvement in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Contribution and the data sharing statement
BC, IB, RT, EK and AK participated in conceptualisation, data curation, formal analysis, validation, visualisation, writing – original draft, as well as writing, review & editing of the manuscript.
LAM, JvdM, IGU EM, TD, ST, KL and SL participated in the conceptualisation, investigation, visualisation, and writing (original draft, as well as reviewing and editing).
PvD and POB participated in the conceptualisation, investigation, validation, visualisation, and writing (original draft, as well as reviewing and editing).
All authors have read and agreed to the published version of the manuscript.
Data collected for this meta-analysis have already been published in other studies. Data extracted from these published articles will be made available to others upon request. There are no individual participant data due to the nature of this meta-analysis. The protocol is already published and is included as supplementary material. The data will be made available 3 months beginning 3 months and ending 5 years following article publication. The data will be made available to researchers who provide a methodologically sound proposal. Proposals should be directed to akhalil@sgul.ac.uk; to gain access, data requestors will need to sign a data access agreement. Data are available for 5 years following the publication date
Declaration of Competing Interest
Dr Morris reports grants and other from Gedeon Richter, grants and other from Chugai Pharma, personal fees from Pfizer, personal fees from Gedeon Richter, other from Kebomed, from null, outside the submitted work; and President and Trustee, RCOG Trustee, British Menopause Society Chair of Trustees, Group B Strep Support.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2021.100947.
Appendix. Supplementary materials
References
- 1.Khalil A., Kalafat E., Benlioglu C. SARS-CoV-2 infection in pregnancy: a systematic review and meta-analysis of clinical features and pregnancy outcomes. EClinicalMedicine. 2020;25 doi: 10.1016/j.eclinm.2020.100446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allotey J., Stallings E., Bonet M. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370:m3320. doi: 10.1136/bmj.m3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knight M., Bunch K., Cairns A., et al. Saving lives, improving mothers’ care rapid report: learning from SARS-CoV-2-related and associated maternal deaths in the UK March – May 2020. Vol. 31, MBRRACE-UK. 2020. https://www.npeu.ox.ac.uk/news/2013-mbrrace-uk-release-saving-lives-improving-mothers-care-rapid-report [Accessed 28.03.2021]
- 4.Khalil A., von Dadelszen P., Draycott T., Ugwumadu A., O'Brien P., Magee L. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA. 2020;324:705–706. doi: 10.1001/jama.2020.12746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Curtis M., Villani L., Polo A. Increase of stillbirth and decrease of late preterm infants during the COVID-19 pandemic lockdown. Arch Dis Child Fetal Neonatal editor. 2020 doi: 10.1136/archdischild-2020-320682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Been J.V., Burgos Ochoa L., Bertens L.C.M., Schoenmakers S., Steegers E.A.P., Reiss I.K.M. Impact of COVID-19 mitigation measures on the incidence of preterm birth: a national quasi-experimental study. Lancet Public Health. 2020;5 doi: 10.1016/S2468-2667(20)30223-1. e604–e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Philip R.K., Purtill H., Reidy E. Unprecedented reduction in births of very low birthweight (VLBW) and extremely low birthweight (ELBW) infants during the COVID-19 lockdown in Ireland: a ‘natural experiment’ allowing analysis of data from the prior two decades. BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-003075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hedermann G., Hedley P.L., Baekvad-Hansen M. Danish premature birth rates during the COVID-19 lockdown. Arch Dis Child Fetal Neonatal editor. 2021;106:93–95. doi: 10.1136/archdischild-2020-319990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chmielewska B., Barratt I., Townsend R. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob Health. 2021 doi: 10.1016/S2214-109X(21)00079-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jardine J., Relph S., Magee L.A. Maternity services in the UK during the coronavirus disease 2019 pandemic: a national survey of modifications to standard care. BJOG. 2021;128:880–889. doi: 10.1111/1471-0528.16547. [DOI] [PubMed] [Google Scholar]
- 11.Coxon K., Turienzo C.F., Kweekel L. The impact of the coronavirus (COVID-19) pandemic on maternity care in. Europe Midwifery. 2020;88 doi: 10.1016/j.midw.2020.102779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Royal College of Obstetrics and Gynaecology. Coronavirus (COVID-19) Infection in Pregnancy. 2021. https://www.rcog.org.uk/globalassets/documents/guidelines/2021-02-19-coronavirus-covid-19-infection-in-pregnancy-v13.pdf [Accessed 28.03.2021]
- 13.Goyal M., Singh P., Singh K., Shekhar S., Agrawal N., Misra S. The effect of the COVID-19 pandemic on maternal health due to delay in seeking health care: experience from a tertiary center. Int J Gynaecol Obstet. 2021;152:231–235. doi: 10.1002/ijgo.13457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Czeisler M.É., Marynak K., Clarke K.E.N. Delay or Avoidance of medical care because of COVID-19–related concerns — United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250–1257. doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yerger P., Jalloh M., Coltart C.E.M., King C. Barriers to maternal health services during the Ebola outbreak in three West African countries: a literature review. BMJ Global Health. 2020;5 doi: 10.1136/bmjgh-2020-002974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moher D., Liberati A., Tetzlaff J., Altman D.G. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 17.Hale T., Angrist N., Goldszmidt R. A global panel database of pandemic policies (Oxford COVID-19 government response tracker) Nat Hum Behav. 2021 doi: 10.1038/s41562-021-01079-8. [DOI] [PubMed] [Google Scholar]
- 18.Wells G., Shea B., O'Connell D., Peterson J., Welch V., Losos M., et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Internet]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp Accessed 01 January 2021.
- 19.Deeks J.J., Higgins J.P., Altman D.G., obotCSM Group. Cochrane handbook for systematic reviews of interventions. 2019. Analysing data and undertaking meta-analyses; pp. 241–284. [Google Scholar]
- 20.Hunter J.P., Saratzis A., Sutton A.J., Boucher R.H., Sayers R.D., Bown M.J. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J Clin Epidemiol. 2014;67:897–903. doi: 10.1016/j.jclinepi.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 21.Manzoli L., Flacco M.E., D'Addario M. Non-publication and delayed publication of randomized trials on vaccines: survey. BMJ. 2014;348:g3058. doi: 10.1136/bmj.g3058. [DOI] [PubMed] [Google Scholar]
- 22.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abel M.K., Alavi M.X., Tierney C., Weintraub M.R., Avins A., Zaritsky E. Coronavirus disease 2019 (COVID-19) and the incidence of obstetric and gynecologic emergency department visits in an integrated health care system. Obstet Gynecol. 2021;137:581–583. doi: 10.1097/AOG.0000000000004331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dell'Utri C., Manzoni E., Cipriani S. Effects of SARS Cov-2 epidemic on the obstetrical and gynecological emergency service accesses. What happened and what shall we expect now? Eur J Obstet Gynecol Reprod Biol. 2020;254:64–68. doi: 10.1016/j.ejogrb.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Filice C., Poma G.L., Above E. Is the fear of COVID-19 infection the same in all subjects? Int J Infect Dis. 2020;97:331–333. doi: 10.1016/j.ijid.2020.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Futterman I., Rosenfeld E., Toaff M. Addressing disparities in prenatal care via telehealth during COVID-19: prenatal satisfaction survey in East Harlem. Am J Perinatol. 2021;38:88–92. doi: 10.1055/s-0040-1718695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greene N.H., Kilpatrick S.J., Wong M.S., Ozimek J.A., Naqvi M. Impact of labor and delivery unit policy modifications on maternal and neonatal outcomes during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM. 2020;2 doi: 10.1016/j.ajogmf.2020.100234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gu X.-.X., Chen K., Yu H., Liang G.-.Y., Chen H., Shen Y. How to prevent in-hospital COVID-19 infection and reassure women about the safety of pregnancy: experience from an obstetric center in China. J Int Med Res. 2020;48 doi: 10.1177/0300060520939337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Holcomb D., Faucher M.A., Bouzid J., Quint-Bouzid M., Nelson D.B., Duryea E. Patient perspectives on audio-only virtual prenatal visits amidst the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic. Obstet Gynecol. 2020;136:317–322. doi: 10.1097/AOG.0000000000004026. [DOI] [PubMed] [Google Scholar]
- 30.Hui P.W., Ma G., Seto M.T.Y., Cheung K.W. Effect of COVID-19 on delivery plans and postnatal depression scores of pregnant women. Hong Kong Med. 2020 doi: 10.12809/hkmj208774. [DOI] [PubMed] [Google Scholar]
- 31.Khalil A., von Dadelszen P., Kalafat E. Change in obstetric attendance and activities during the COVID-19 pandemic. Lancet Infect Dis. 2021 doi: 10.1016/S1473-3099(20)30779-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baptiste C., Sutton D., Jacob T. 904 Prenatal genetic diagnostic testing during the COVID-19 pandemic. Am J Obstet Gynecol. 2021;224:S560–S561. [Google Scholar]
- 33.Bernstein M., Mei J.Y., Patton E., Negi M. 787 Evaluating standard of care in a reduced prenatal care model in the COVID-19 pandemic. Am J Obstet Gynecol. 2021;224:S490–S491. [Google Scholar]
- 34.Bertozzi-Villa C., Arditi B., Syeda S.K. 1050 Effect of the COVID-19 pandemic on initial obstetric ultrasounds in New York City. Am J Obstet Gynecol. 2021;224:S650–S651. [Google Scholar]
- 35.Duryea E.L., Adhikari E.H., Ambia A., Spong C., McIntire D., Nelson D.B. Comparison between in-person and audio-only virtual prenatal visits and perinatal outcomes. JAMA Netw Open. 2021;4(4) doi: 10.1001/jamanetworkopen.2021.5854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Facco F., Himes K. 993 did health care delivery changes driven by COVID alter pregnancy and postpartum visits? Am J Obstet Gynecol. 2021;224 S615–6. [Google Scholar]
- 37.Abdela S.G., Berhanu A.B., Ferede L.M., van Griensven J. Essential healthcare services in the face of COVID-19 prevention: experiences from a referral hospital in Ethiopia. Am J Trop Med Hyg. 2020;103:1198–1200. doi: 10.4269/ajtmh.20-0464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McDonnell S., McNamee E., Lindow S.W., O'Connell M.P. The impact of the Covid-19 pandemic on maternity services: a review of maternal and neonatal outcomes before, during and after the pandemic. Eur J Obstet Gynecol Reprod Biol. 2020;255:172–176. doi: 10.1016/j.ejogrb.2020.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meyer R., Levin G., Hendin N., Katorza E. Impact of the COVID-19 outbreak on routine obstetrical management. Isr Med Assoc J. 2020;22:483–488. [PubMed] [Google Scholar]
- 40.Weingarten S.J., Clare C.A. 150 Management of diabetes in pregnancy during the COVID-19 pandemic at a New York City hospital. Am J Obstet Gynecol. 2021;224:S103. [Google Scholar]
- 41.Shields A.D., Wagner R.K., Knutzen D., Deering S., Nielsen P.E. Maintaining access to maternal fetal medicine care by telemedicine during a global pandemic. J Telemed Telecare. 2020 doi: 10.1177/1357633X20957468. 10.1177/1357633 × 20957468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peahl A.F., Powell A., Berlin H. Patient and provider perspectives of a new prenatal care model introduced in response to the coronavirus disease 2019 pandemic. Am J Obstet Gynecol. 2021;224 doi: 10.1016/j.ajog.2020.10.008. 384.e1–e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Limaye M.A., Lantigua-Martinez M., Trostle M.E. Differential uptake of telehealth for prenatal care in a large New York City academic obstetrical practice during the COVID-19 pandemic. Am J Perinatol. 2021;38:304–306. doi: 10.1055/s-0040-1721510. [DOI] [PubMed] [Google Scholar]
- 44.Greco P., Hesson A., Clifford C., Sangtani A., Stout M.J., Langen E.S. 801 Hypertensive disorders of pregnancy in a pandemic: care delivery, outcomes, and lessons learned. Am J Obstet Gynecol. 2021;224:S499. [Google Scholar]
- 45.Hussain F.N., Garvey K.L., Karotkin L. 1028 Managing gestational diabetes mellitus with telemedicine during COVID-19: was there an impact on pregnancy outcomes? Am J Obstet Gynecol. 2021;224:S636–S637. [Google Scholar]
- 46.Selinger C.P., Fraser A., Collins P. Impact of the coronavirus infectious disease (COVID-19) pandemic on the provision of inflammatory bowel disease (IBD) antenatal care and outcomes of pregnancies in women with IBD. BMJ Open Gastroenterol. 2021;8 doi: 10.1136/bmjgast-2021-000603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Soffer M.D., Sinnott C., Clapp M.A., Bernstein S.N. 514 Impact of a hybrid model of prenatal care on the diagnosis of fetal growth restriction. Am J Obstet Gynecol. 2021;224:S324–S325. doi: 10.1055/a-1877-8478. [DOI] [PubMed] [Google Scholar]
- 48.Bhatia K., Columb M., Bewlay A. The effect of COVID-19 on general anaesthesia rates for caesarean section. A cross-sectional analysis of six hospitals in the north-west of England. Anaesthesia. 2021;76:312–319. doi: 10.1111/anae.15313. [DOI] [PubMed] [Google Scholar]
- 49.Patkar-Kattimani C., Athod R., Sangtani D. COVID-19 and obstetric anaesthetic services in a tertiary maternity care unit. Int J Obstet Anesth. 2021;45:152–153. doi: 10.1016/j.ijoa.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Justman N., Shahak G., Gutzeit O. Lockdown with a Price: the impact of the COVID-19 Pandemic on Prenatal Care and Perinatal Outcomes in a Tertiary Care Center. Isr Med Assoc J. 2020;22:533–537. [PubMed] [Google Scholar]
- 51.Racine J.L., Hetzel S., Iruretagoyena J.I., Hoppe K.K. 889 Did institutional changes and patient behaviors surrounding COVID-19 affect perinatal outcomes? Am J Obstet Gynecol. 2021;224:S551–S552. [Google Scholar]
- 52.Bornstein E., Gulersen M., Husk G. Early postpartum discharge during the COVID-19 pandemic. J Perinat Med. 2020;48:1008–1012. doi: 10.1515/jpm-2020-0337. [DOI] [PubMed] [Google Scholar]
- 53.Monni G., Corda V., Iuculano A. Prenatal screening diagnosis and management in the era of coronavirus: the Sardinian experience. J Perinat Med. 2020;48:943–949. doi: 10.1515/jpm-2020-0208. [DOI] [PubMed] [Google Scholar]
- 54.Ozalp M., Demir O., Akbas H., Kaya E., Celik C., Osmanagaoglu M.A. Effect of COVID-19 pandemic process on prenatal diagnostic procedures. J Matern Fetal Neonatal Med. 2020:1–6. doi: 10.1080/14767058.2020.1815190. [DOI] [PubMed] [Google Scholar]
- 55.Sun S.Y., Guazzelli C.A.F., de Morais L.R. Effect of delayed obstetric labor care during the COVID-19 pandemic on perinatal outcomes. Int J Gynaecol Obstet. 2020;151:287–289. doi: 10.1002/ijgo.13357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ahmed T., Rahman A.E., Amole T.G. The effect of COVID-19 on maternal newborn and child health (MNCH) services in Bangladesh, Nigeria and South Africa: call for a contextualised pandemic response in LMICs. Int J Equity Health. 2021;20:77. doi: 10.1186/s12939-021-01414-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wanyana D., Wong R., Hakizimana D. Rapid assessment on the utilization of maternal and child health services during COVID-19 in Rwanda. Public Heal action. 2021;11:12–21. doi: 10.5588/pha.20.0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sarkar S., Chowdhury R.R.O.Y., Mukherji J., Samanta M., Bera G. Comparison of attendance of patients pre-lockdown and during lockdown in gynaecology and antenatal outpatient department in a tertiary care hospital of Nadia, West Bengal, India. J Clin Diagnostic Res. 2021;15(2) QC05–8. [Google Scholar]
- 59.Chen M., Liu X., Zhang J. Characteristics of online medical care consultation for pregnant women during the COVID-19 outbreak: cross-sectional study. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-043461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moyer C.A., Sakyi K.S., Sacks E., Compton S.D., Lori J.R., Williams J.E.O. COVID-19 is increasing Ghanaian pregnant women's anxiety and reducing healthcare seeking. Int J Gynecol Obstet. 2021;152:444–445. doi: 10.1002/ijgo.13487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tadesse E. Antenatal care service utilization of pregnant women attending antenatal care in public hospitals during the COVID-19 pandemic period. Int J Womens Health. 2020;12:1181–1188. doi: 10.2147/IJWH.S287534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liu X., Chen M., Wang Y. Prenatal anxiety and obstetric decisions among pregnant women in Wuhan and Chongqing during the COVID-19 outbreak: a cross-sectional study. BJOG. 2020;127:1229–1240. doi: 10.1111/1471-0528.16381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kumari V., Mehta K., Choudhary R. COVID-19 outbreak and decreased hospitalisation of pregnant women in labour. Lancet Glob Heal. 2020;8:e1116–e1117. doi: 10.1016/S2214-109X(20)30319-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.KC A., Gurung R., Kinney M V. Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study. Lancet Glob Heal. 2020;8:e1273–e1e81. doi: 10.1016/S2214-109X(20)30345-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zarasvand S., Bayar E., Adan M. Rapid quality improvement in a preterm birth clinic care pathway during the COVID-19 pandemic. BMJ Open Qual. 2020;9 doi: 10.1136/bmjoq-2020-001049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Madden N., Emeruwa U.N., Friedman A.M. Telehealth uptake into prenatal care and provider attitudes during the COVID-19 pandemic in New York City: a quantitative and qualitative analysis. Am J Perinatol. 2020;37:1005–1014. doi: 10.1055/s-0040-1712939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Silverman M.E., Medeiros C., Burgos L. Early pregnancy mood before and during COVID-19 community restrictions among women of low socioeconomic status in New York City: a preliminary study. Arch Womens Ment Health. 2020;23:779–782. doi: 10.1007/s00737-020-01061-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Salsi G., Seidenari A., Diglio J., Bellussi F., Pilu G., Bellussi F. Obstetrics and gynecology emergency services during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM. 2020;2 doi: 10.1016/j.ajogmf.2020.100214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Biviá-Roig G., La Rosa V.L., Gómez-Tébar M. Analysis of the impact of the confinement resulting from COVID-19 on the lifestyle and psychological wellbeing of Spanish pregnant women: an internet-based cross-sectional survey. Int J Environ Res Public Health. 2020;17:5933. doi: 10.3390/ijerph17165933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jeganathan S., Prasannan L., Blitz M.J., Vohra N., Rochelson B., Meirowitz N. Adherence and acceptability of telehealth appointments for high-risk obstetrical patients during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM. 2020;2 doi: 10.1016/j.ajogmf.2020.100233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kugelman N., Lavie O., Assaf W. Changes in the obstetrical emergency department profile during the COVID-19 pandemic. J Matern Neonatal Med. 2020 doi: 10.1080/14767058.2020.1847072. [DOI] [PubMed] [Google Scholar]
- 72.Albert L., Capel I., García-Sáez G., Martín-Redondo P., Hernando M.E., Rigla M. Managing gestational diabetes mellitus using a smartphone application with artificial intelligence (SineDie) during the COVID-19 pandemic: much more than just telemedicine. Diabetes Res Clin Pract. 2020;169 doi: 10.1016/j.diabres.2020.108396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gildner T.E., Thayer Z.M. Birth plan alterations among American women in response to COVID-19. Heal Expect. 2020;23:969–971. doi: 10.1111/hex.13077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sakowicz A., Imeroni S., Matovina C., Daiter M., Grobman W.A., Miller E.S. 590 Postpartum depression screening during the COVID-19 pandemic. Am J Obstet Gynecol. 2021;224:S371–S372. doi: 10.1016/j.ajogmf.2021.100460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sakowicz A., Matovina C., Imeroni S. 591 The association between COVID-19 related health services changes and postpartum contraception. Am J Obstet Gynecol. 2021;224:S372. [Google Scholar]
- 76.Kumar J., Kumar P. COVID-19 pandemic and health-care disruptions: count the most vulnerable. Lancet Glob Heal. 2021 doi: 10.1016/S2214-109X(21)00098-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Anderson T.S., Stevens J.P., Pinheiro A., Li S., Herzig S.J. Hospitalizations for emergent medical, surgical, and obstetric conditions in Boston during the COVID-19 pandemic. J Gen Intern Med. 2020;35:3129–3132. doi: 10.1007/s11606-020-06027-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hamadani J.D., Hasan M.I., Baldi A.J. Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: an interrupted time series. Lancet Glob Heal. 2020;8:e1380–e1389. doi: 10.1016/S2214-109X(20)30366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Feder G., Lucas d'Oliveira A.F., Rishal P., Johnson M. Domestic violence during the pandemic. BMJ. 2021;372:n722. doi: 10.1136/bmj.n722. [DOI] [PubMed] [Google Scholar]
- 80.Evans M.L., Lindauer M., Farrell M.E. A pandemic within a pandemic — intimate partner violence during Covid-19. N Engl J Med. 2020;383:2302–2304. doi: 10.1056/NEJMp2024046. [DOI] [PubMed] [Google Scholar]
- 81.Krishnamurti T., Davis A.L., Quinn B., Castillo A.F., Martin K.L., Simhan H.N. Mobile remote monitoring of intimate partner violence among pregnant patients during the COVID-19 shelter-in-place order: quality improvement pilot study. J Med Internet Res. 2021;23:e22790. doi: 10.2196/22790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.England N.H.S. Actions for NHS providers; London, UK: 2020. Supporting pregnant women using maternity services during the coronavirus pandemic.https://www.england.nhs.uk/coronavirus/publication/supporting-pregnant-women-using-maternity-services-during-the-coronavirus-pandemic-actions-for-nhs-providers/ [Accessed 28.03.2021] [Google Scholar]
- 83.Assefa K.T., Gashu A.W., Mulualem T.D. North-East Ethiopia; 2020. The impact of COVID-19 infection on maternal and reproductive health care services in governmental health institutions of Dessie town. G.C. medRxiv 2020; 2020.09.20.20198259. [Google Scholar]
- 84.World Health Organisation (WHO). WHO recommendations on antenatal care for a positive pregnancy experience. Geneva, 2016. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.