Abstract
Purpose
To present a case of infectious crystalline keratopathy after corneal cross-linking in a child with delayed wound healing, and its successful management with antibiotic and anti-fungal eye drops.
Observations
A 14-year-old male presented for a second opinion with a non-staining crystalline keratopathy after corneal crosslinking for progressive keratoconus. He reportedly rubbed his eyes vigorously in the post-operative course and had a slowly healing epithelial defect. He was treated with several antibiotic drops and was put on high dose topical difluprednate drops post-procedure for persistent corneal haze. His infection continued to progress until steroids were stopped and he was treated with topical voriconazole. While cultures were negative, the patient's visual acuity and corneal lesions improved significantly after starting voriconazole therapy and stopping steroid drops, pointing to a diagnosis of infectious crystalline keratopathy.
Conclusions and Importance
This is one of the first case reports to describe a primary infectious crystalline keratopathy after a corneal cross-linking procedure, and the first to describe this phenomenon in a child with delayed corneal re-epithelialization. Though corneal cross-linking is a relatively safe procedure, atypical infections like crystalline keratopathy can occur in these patients in the setting of topical steroid use. Atypical organisms such as fungi should always be on the differential, especially for patients with recalcitrant infection in the setting of immunosuppression.
Keywords: Crystalline keratopathy, Cross-linking, Fungal keratitis
1. Introduction
Corneal cross-linking is a procedure developed to halt or slow down the progression of corneal ectatic diseases. The procedure was created in 1998 and involves using riboflavin and ultraviolet (UV) irradiation to increase the stiffness of the cornea.1 Observational studies and randomized control trials (RCTs) have both shown sustained improvement after corneal cross-linking in measurements such as maximum simulated keratometry value (KMax), uncorrected visual acuity (UCVA), and best corrected visual acuity (BCVA).2,3
Corneal cross-linking was approved by the Federal Drug Administration (FDA) in 2016 as a treatment for progressive keratoconus and post-surgical ectasia. Currently, Avedro's KXL System (Waltham, Massachusetts, United States of America) is the only FDA approved device for these indications. The FDA-approved procedure using the Dresden protocol is the gold standard of treatment. Though the procedure is very safe, it does involve removal of the corneal epithelium to allow for application of riboflavin drops. Common complications include delayed epithelial healing, sterile infiltrates, and corneal haze, the latter of which is often transient.2,3
Infectious keratitis is a rare but potentially serious consequence of corneal cross-linking, with a rate of 0.0017% according to one study.4 Infectious keratitis can lead to decreased visual acuity and corneal scarring, sometimes requiring corneal transplantation. Several case reports have shown S.Epidermidis, S. Aureus, Pseudomonas, Acanthamoeba, E. Coli, and Herpes Simplex Virus (HSV) as pathogens implicated in infectious keratitis after corneal cross-linking, with one case report of fungal keratitis in the US with Alternaria, and some reports of Fusarium and Microsporidia internationally.3,5 Presently, there are only two reports of a primary infectious crystalline keratopathy following cross-linking.6,7 In both cases, the patients initially healed well, but presented for their monthly exam with new intrastromal lesions and photophobia. Additionally, Steinwender and colleagues reported one case of infectious crystalline keratopathy in a large series that occurred after the patient had resumed wearing a rigid gas permeable contact lens.8 Risk factors for infectious crystalline keratopathy include immunocompromise, long term steroid use, post-surgical keratitis, contact lens wear, and topical anesthetic abuse.9 Fungal infectious crystalline keratopathy is exceedingly rare, with one study showing 3 out of 18 patients with the condition being of fungal origin.10
The current case report presents an infectious crystalline keratopathy in a child with a prolonged post operative course.
2. Case report
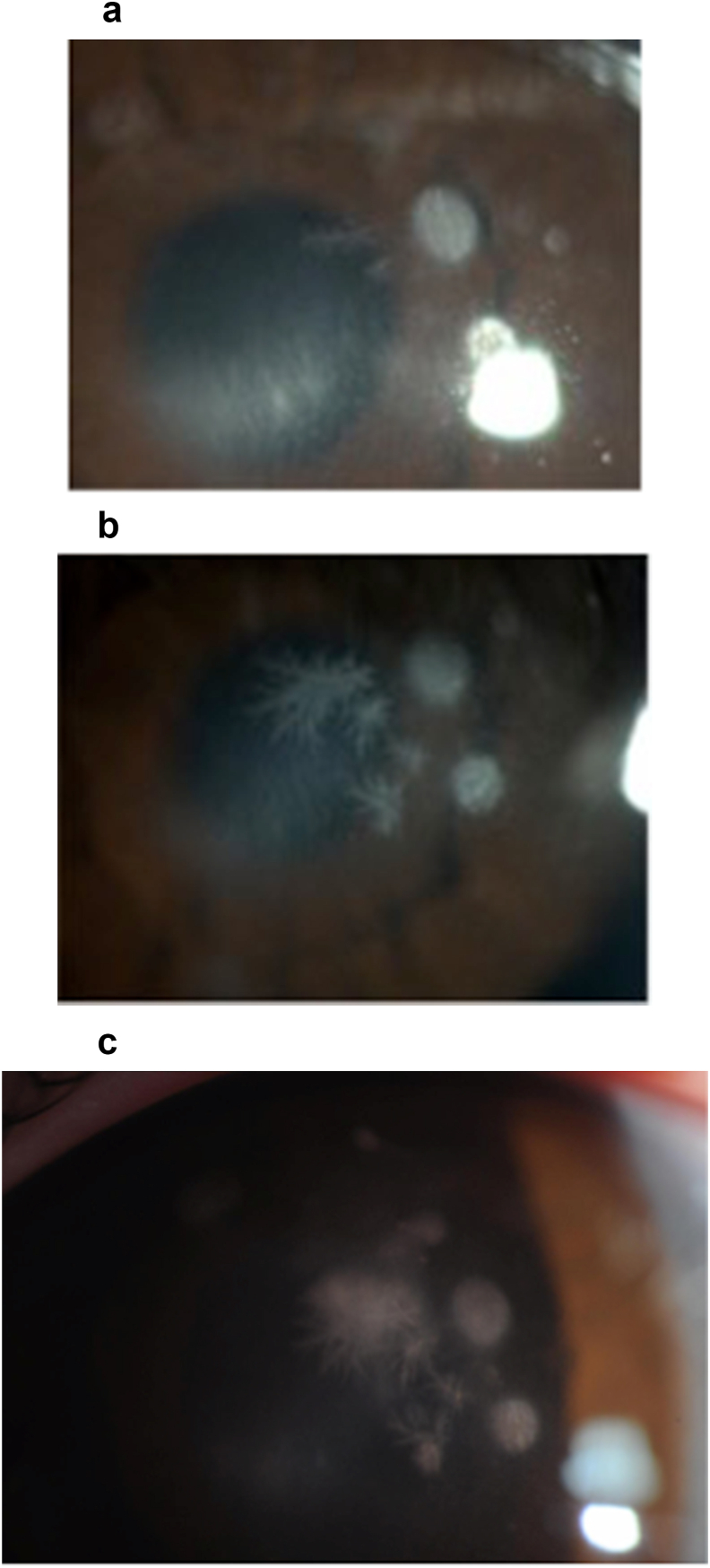
A 14-year-old male with a history of keratoconus and corneal cross-linking in his left eye at an outside hospital, presented to our clinic 19 days post procedure for evaluation of a corneal infection and persistent haze. Per his records from his outside ophthalmologist, the patient had rubbed his eyes continually after surgery and had slow re-epithelialization and haze. He had been taking difluprednate four times a day, and tobramycin three times a day in the left eye. On examination at this initial visit, his uncorrected visual acuity (UCVA) was 20/70–2 and BCVA was 20/40 (−1.25–1.50 × 145) in the left eye. Slit lamp examination showed diffuse corneal haze, several well-demarcated intrastromal opacities (largest measuring 1.5 mm), and a 1.5 mm non-staining intrastromal branching lesion in the left eye (Fig. 1A). The patient had follow up scheduled with his outside ophthalmologist and was asked to return in a month should his symptoms persist.
Fig. 1.
External photographs of patient at initial presentation (A), with worsening 3 weeks after initial presentation (B), and further worsening 3 weeks and 3 days after initial presentation (C).
The patient returned three weeks later with worsening infection. He had stopped the tobramycin two weeks prior per his physician's recommendation and continued on difluprednate. When symptoms worsened, he was asked to start moxifloxacin twice a day, and was told to taper difluprednate to twice a day (from four times a day). On subsequent examination in our office, his UCVA had worsened significantly to 20/250 and BCVA to 20/80. He had increased haze and opacities in the left eye, and the prior small branching lesion was bigger, extending centrally, and appeared more crystalline in structure (Fig. 1B). Given these findings, there was concern for crystalline keratopathy. He was cultured with a 15 blade, which was plated onto blood, chocolate, and sabaraoud's culture plates and sent to the lab. He was then started on fortified vancomycin drops every 1 h and moxifloxacin drops every 1 h. The patient was asked to stop difluprednate. Three days after this appointment, the patient returned with worsening symptoms. He complained of severe pain and eye redness for the first time. On examination, his vision had decreased to UCVA 20/400 in the left eye. He was found to have cell and flare, as well as worsening corneal haze, and growing corneal opacities that were now becoming confluent (Fig. 1C). Cultures to date were negative. voriconazole was added for fungal coverage. He was continued on vancomycin and moxifloxacin drops.
The patient was seen two weeks later with improved vision, BCVA 20/200, and no pain. About four weeks after initiating anti-fungal treatment, prednisolone acetate was added. It was tapered off two months later with improvement in the patient's haze. His antibiotic drops and ultimately voriconazole were stopped nine weeks after his initial presentation to our clinic. Final cultures for bacteria and fungi were negative. Three months after presentation, the patient showed considerable improvement, with UCVA 20/60–1, pinholing to 20/30–2 in the left eye. Slit lamp exam showed only some mild haze in the left eye.
3. Discussion
This is one of the first case reports to detail a primary infectious crystalline keratopathy after a corneal cross-linking procedure, and the first to describe this phenomenon in a child with delayed corneal re-epithelialization on high dose steroids.
Classically, crystalline keratopathy has been seen after penetrating keratoplasties and other more invasive corneal procedures as well as patients who are on chronic steroids. The differential diagnosis for crystalline keratopathy includes infectious causes (usually Strep Viridans, gram positive cocci, and rarely fungus), crystalline dystrophies (e.g. Schnyder Crystalline Corneal Dystrophy, Bietti Crystalline Dystrophy), drug deposition, and errors of protein metabolism (tyrosinemia, cystinosis, and gout).9 The development of lesions in this patient after surgery point to more of an infectious picture. Herpetic epithelial keratitis also has branching lesions, but is epithelial and has terminal bulbs at the end of branches. Our patient's infection was intrastromal and did not stain with fluorescein.
The etiology of crystalline keratopathy in this patient was either a fungal or bacterial organism. Satellite lesions along with central branching lesions that initially did not respond, and actually worsened while the patient was on vancomycin, moxifloxacin, and tobramycin, and improved with the addition of voriconazole lead us to consider a fungal etiology in our differential of infectious organisms. Fungal infections often occur in patients who are immunosuppressed, and this patient had been on a long course of strong steroids after his corneal cross-linking procedure.10 Bacterial crystalline keratopathy, on the other hand, is more common than fungal. If the etiology of his infection was bacterial, his high dose steroids may have limited the efficacy of his topical antibiotic treatment.
Cultures were negative throughout his course, but his infection improved and ultimately resolved with the addition of voriconazole and cessation of his topical steroids. Topical steroids are used after corneal cross-linking procedures to reduce or prevent the development of corneal haze. However, steroid use has been shown to be a risk factor for the development of infectious keratitis.11 This case of infectious crystalline keratopathy in a relatively healthy young patient with keratoconus shows that caution must be taken when prescribing patients steroids after procedures, especially in the setting of a slowly healing epithelial defect. Steroids are an essential part of post-surgical care, but require a high degree of surveillance and low threshold for starting treatment for infection if the patient develops persistent epithelial defects, pain, or infiltrates following a procedure. Infectious etiologies should be considered in patients with prolonged wound healing after crosslinking. Clinicians may wish to culture poor wound healers and consider a faster steroid taper.
Fungal infections should always be on the differential for patients with infectious keratitis who are recalcitrant to treatment with topical antibiotics. Topical voriconazole is well tolerated and is a relatively safe medication to add when treating empirically for fungal keratitis. Voriconazole was chosen over natamycin in this young patient who was prone to rubbing of his eyes and to allergic conjunctivitis due to the fact that the drop is well tolerated.12
Corneal cross-linking is now widely accepted as a safe and effective treatment for progressive keratoconus, particularly in younger patients. As increasing numbers of patients undergo the procedure, we will likely see more total complications. It is important to monitor these complications and report them in order to make providers aware of possible risk factors of corneal cross-linking. While steroids are routinely used after cross-linking, extra care and surveillance should be taken with prolonged use, especially with strong steroids like difluprednate.
4. Conclusions
Practitioners should have a low threshold to suspect infectious keratitis in patients with worsening keratopathy, discomfort or vision in the setting of topical steroid use.
Patient Consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Acknowledgments and disclosures
No funding or grant support. The following authors have no financial disclosures: RK, SS, DT. All authors attest that they meet the current ICMJE criteria for Authorship. No further acknowledgments.
References
- 1.Wollensak G., Spoerl E., Seiler T. Riboflavin/ultraviolet-A-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–627. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 2.Wittig-Silva C., Chan E., Islam F. A randomized, controlled trial of corneal collagen cross-linking in progressive keratoconus: three-year results. Ophthalmology. 2014;121(4):812–821. doi: 10.1016/j.ophtha.2013.10.028. [DOI] [PubMed] [Google Scholar]
- 3.Belin M.W., Lim L., Rajpal R.K. Corneal cross-linking: current USA status: report from the Cornea Society. Cornea. 2018;37:1218–1225. doi: 10.1097/ICO.0000000000001707. [DOI] [PubMed] [Google Scholar]
- 4.Shetty R., Kaweri L., Nuijts R. Profile of microbial keratitis after corneal collagen cross-linking. Biomed Research Int. 2014;2014:340509. doi: 10.1155/2014/340509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGirr S., Andersen D., Halgren J. Alternaria keratitis after corneal crosslinking. Am J Ophthalmol Case Rep. 2020;17:100616. doi: 10.1016/j.ajoc.2020.100616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garcia-Delpech S., Díaz-Llopis M., Udaondo P., Salom D. Fusarium keratitis 3 weeks after healed corneal cross-linking. J Refract Surg. 2010;26(12):994–995. doi: 10.3928/1081597X-20100804-02. [DOI] [PubMed] [Google Scholar]
- 7.Al-Amry M., Mudhaiyan T., Al-Huthail R., Al-Ghadeer H. Infectious crystalline keratopathy after corneal cross-linking. Middle East Afr J Ophthalmol. 2017;24(2):100–102. doi: 10.4103/meajo.MEAJO_346_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steinwender G., Pertl L., El-Shabrawi Y. Complications from corneal cross-linking for keratoconus in pediatric patients. J Refract Surg. 2016;32:68–69. doi: 10.3928/1081597X-20151210-03. [DOI] [PubMed] [Google Scholar]
- 9.Porter A.J., Lee G.A., Jun A.S. Infectious crystalline keratopathy. Surv Ophthalmol. 2018;63(4):480–499. doi: 10.1016/j.survophthal.2017.10.008. [DOI] [PubMed] [Google Scholar]
- 10.Khater T.T., Jones D.B., Wilhemus K.R. Infectious crystalline keratopathy caused by gram-negative bacteria. Am J Ophthalmol. 1997;124(1):19–23. doi: 10.1016/s0002-9394(14)71638-1. [DOI] [PubMed] [Google Scholar]
- 11.Tzamalis A., Romano V., Cheeseman R. 177 et al. Bandage contact lens and topical steroids are risk factors for the development of microbial keratitis after epithelium-off CXL. BMJ Open Ophthalmology. 2019;4(1) doi: 10.1136/bmjophth-2018-000231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al-Badriyeh D., Leung L., Roydhouse T. Prospective open-label study of the administration of two-percent voriconazole eye drops. Antimicrob Agents Chemother. 2009;53:3153–3155. doi: 10.1128/AAC.01700-08. [DOI] [PMC free article] [PubMed] [Google Scholar]