Abstract
The aspiration of objects and foreign bodies requires quick and systematic care. During emergent orotracheal intubation, accidental dental crown release can cause a threat to the patient's life. This paper aimed to report a case of foreign body (dental prosthetic crown) aspiration and its management and discuss alternative approaches. An 81-year-old male patient, who was admitted to the hospital's intensive care unit (ICU) for meningitis, presented with altered consciousness, and decreased oxygen saturation. He underwent emergent orotracheal intubation. After intubation, chest radiography was performed to check for proper orotracheal tube positioning and lung expansion. The resultant images revealed the presence of a foreign body within the right lower lobe bronchus in the shape of a dental crown. The foreign body, intubation cannula and basket clamp were successfully removed, followed by reintubation of the patient. The foreign body was a prosthetic upper premolar dental crown (24). While care should be taken to avoid complications, if a foreign body is aspirated during emergent orotracheal intubation, endoscopic removal appears safe and effective. Careful creation, placement, maintenance, and preservation of prosthetic crowns are critically important in elderly patients.
Keywords: Dental prosthetic crown, Pulmonary aspiration, Flexible bronchoscope
Introduction
An increase in life expectancy has led to the search for better rehabilitative treatments; creation, placement, maintenance, and preservation of prosthetic crowns are critically important to promote long-lasting treatment results [1], [2], [3], [4], [5]. Older patients may experience deterioration in oral hygiene, and teeth decay can adversely affect rehabilitation efforts in this population, resulting in fractures or loosening of the crowns [6,7].
Foreign body aspiration is considered a major, emergent complication [8], [9], [10], [11], [12]. While the fate of loosely cemented dental prosthetic crowns may seem trivial, aspiration of the crown into the lower airways represents a medical emergency [9]. When a foreign body remains lodged in the trachea, the risk of suffocation is high, especially when the trachea is partially or totally obstructed. Patients may rapidly develop cyanosis, requiring emergency orotrachealintubation [4,13].
Diagnosis can be made based on the signs and symptoms such as coughing, choking, wheezing, acute dyspnea, and muffled respiratory sounds [14]. Radiographic examination is essential to detect the presence of airway foreign bodies and determine their location [15], [16], [17], [18], [19] because most aspirated dental foreign bodies are radiopaque [20]. However, nonvisualization of a foreign body on radiography does not exclude aspiration, and further investigation is necessary [19]. Although other airways could be affected, the intermediate bronchus is the most commonly affected site in adults [21]. In general, foreign body aspiration requires specific handling and the immediate transportation of the patient to a hospital, especially when maneuvers aimed at expelling the object fail [13,22].
Thus, we aimed to report the aspiration of a foreign body (upper premolar dental prosthetic crown) during emergent orotracheal intubation and the management of such cases. We also discuss alternative approaches.
Clinical report
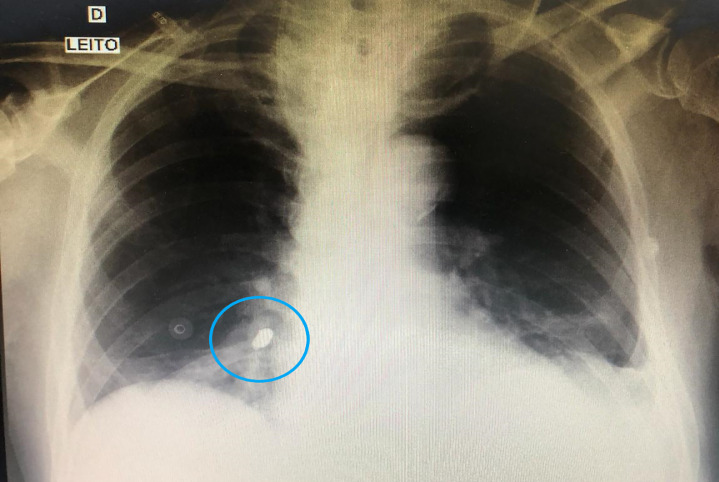
An 81-year-old man was admitted to a hospital's intensive care unit (ICU) for meningitis. He presented with altered consciousness and decreased oxygen saturation, necessitating emergency orotracheal intubation. After intubation, chest radiography was performed to check the orotracheal tube placement and confirm proper lung expansion. Radiography revealed a foreign body shaped like a dental crown located in the right lower lobe bronchus (Fig. 1).
Fig. 1.
Chest radiography showing a foreign body (tooth) (blue circle) in the right lower lobe bronchus.
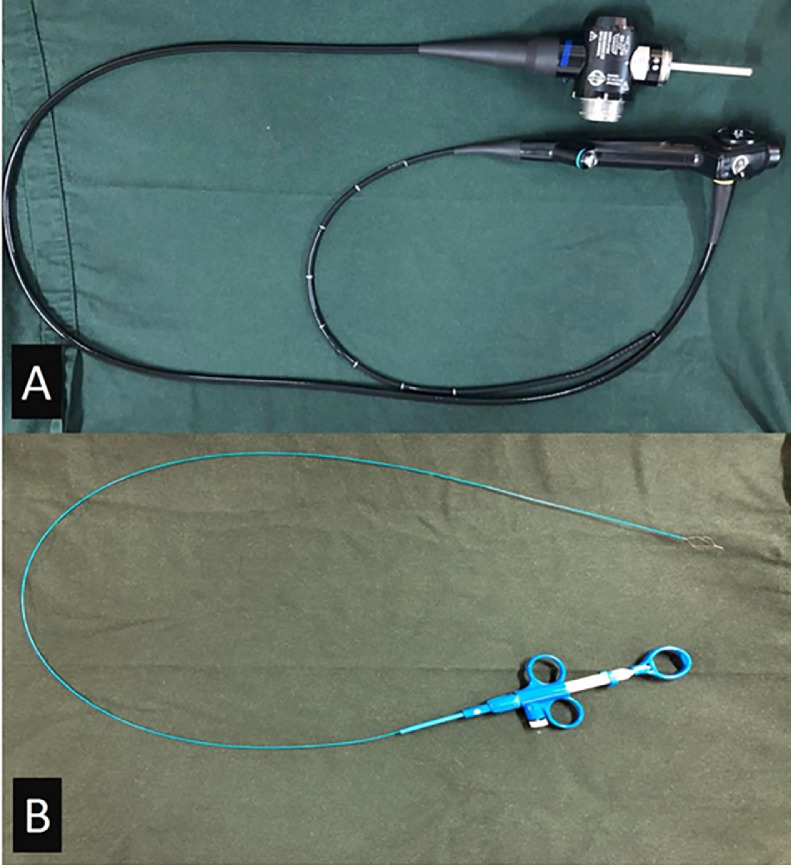
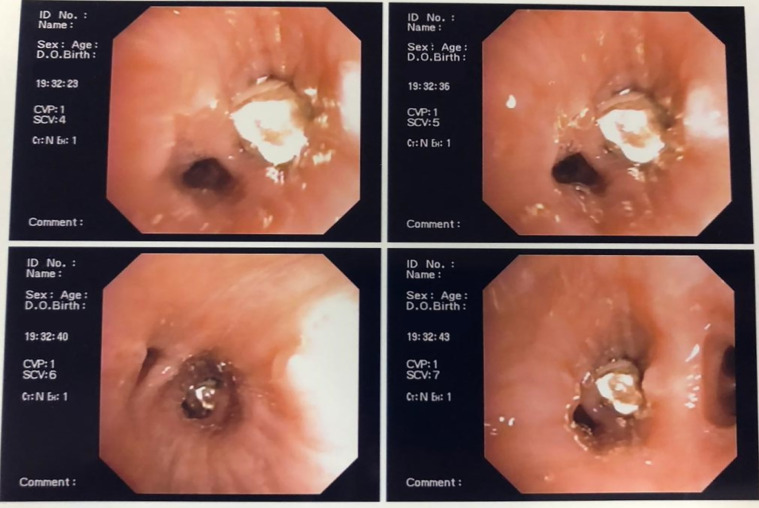
Our plan to remove the foreign body involved accessing the bronchus using an orotracheal intubation cannula coupled with a flexible bronchoscope (Fig. 2A) and basket clamp (Fig. 2B). The scope passed freely through the trachea without altering its caliber and without causing any mucosal lesions. The trachea demonstrated conserved distensibility, indicating a small amount of mucous. A foreign body shaped like a dental prosthetic crown was observed, obliterating the lower lobe bronchus of the right lung (Fig. 3).
Fig. 2.
(A) Flexible bronchoscope (Olympus, BF-P10, Tokyo, Japan); (B) Blasket clamp.
Fig. 3.
Access to the foreign body aided by a flexible bronchoscope and clamp to capture the foreign body.
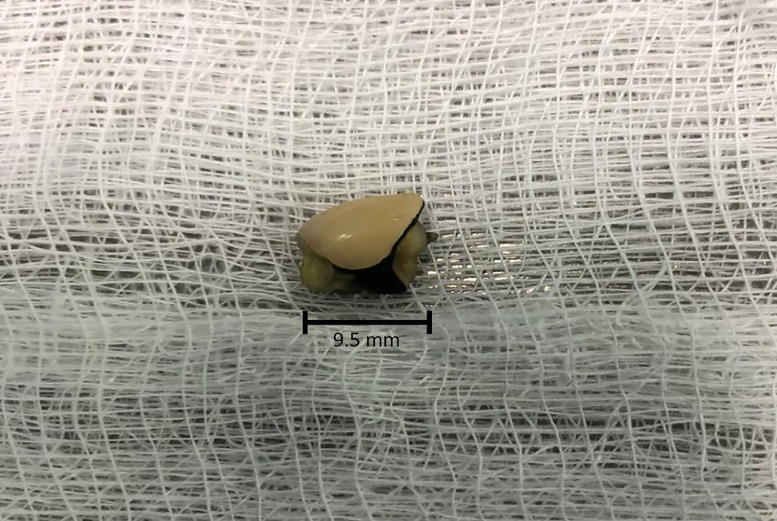
The foreign body was grasped using a basket clamp and removed with the orotracheal intubation cannula. The procedure was successful and without complications. The foreign body was identified as an upper premolar dental prosthetic crown (24) (Fig. 4). After removing the orotracheal intubation cannula, basket clamp, and dental prosthetic crown, the patient was reintubated.
Fig. 4.
Foreign body (single crown) removed using a flexible bronchoscope (crown size 9.5 mm).
The total duration of this intervention, from the identification of the foreign body by the ICU team to foreign body removal and repeat orotracheal intubation, was approximately 1 hour.
Discussion
In this study, we report a case of foreign body aspiration (dental prosthetic crown) during emergency orotracheal intubation. Foreign body aspiration is common in pediatric patients but rare in adults [23,24]. Its main causes among the elderly are trauma, emergency orotracheal intubation, and dental procedures [22,23,25]. Predisposing conditions such as a decrease in (or loss of) consciousness and airway involvement may occur [11,22]. Affected patients may present with chronic cough, fever, hemoptysis, chest pain, and wheezing that could evolve to postobstructive pneumonia and atelectasis [26].
Even though crown aspiration is relatively uncommon, it constitutes a true medical emergency [27], and some successful cases have been reported in the literature [12,14,28,29]. To avoid more severe complications—up to and including even death—individuals may attempt digital seizure when the foreign body is present in the oral cavity or the Heimlich maneuver in cases of aspiration and airway obstruction [1].
Increases in life expectancy have led to the search for better rehabilitative treatments [1,2]. Several factors may be associated with fractures or loosening of the dental prosthetic crowns and include material, occlusal patterns, masticatory load distributions, cement types, oral health and hygiene, presence of carious lesions, tooth preparations and root sizes, old prosthetic crowns, maladjusted pins, endodontic lesions, periodontal disease, and poor prosthetic planning [3,4,6,7].
Procedures like these must be carefully performed, particularly in elderly patients with systemic impairments who are more prone to respiratory problems and intubation due to infections, cardiac and respiratory arrest, pulmonary diseases, or degenerative diseases involving the central nervous system [30].
Prevention remains the best means of avoiding accidental aspiration and ingestion, and some articles have explained how to prevent these adverse outcomes [31], [32], [33], [34], [35], [36]. However, sometimes it is not possible to follow all these recommendations while executing traumatic or emergent procedures. Airway protection mechanisms like cough or laryngeal adductor reflex of the lower airways from foreign body aspiration. Patients undergoing emergent orotracheal intubation may have loose or unaccounted traumatically misplaced teeth or dental crowns. Surgeons should suspect foreign body (in this case, a tooth) aspiration [1,11].
Chest examination and radiography should be performed in patients with dental avulsion, loosening, or prosthetic crown release, especially in those with respiratory alterations or missing dental elements during the accident.
CT scans are more effective than chest radiographs as the thorax shows radiopaque structures and overlays in two-dimensional images [36]. However, a radiopaque foreign body is easily diagnosed based on both CT scans and chest radiographs. In this case report, the patient was diagnosed after chest radiography.
Early diagnosis can help guide treatment and reduce future complications [37,38]. After confirmation of aspiration, the foreign body should be removed using a rigid or flexible bronchoscope [24] to avoid the development of aspiration pneumonia, obstructive pulmonary abscesses, or other complications [10]. A flexible bronchoscope should be the first choice for managing cases of foreign body aspiration because of the low morbidity and high efficacy [36,39,40].
Conclusion
Effective diagnosis is important to prevent further complications in patients who aspirate prosthetic dental crowns. Chest radiography and CT are useful in the diagnosis of this condition, and flexible bronchoscopy should be the first choice for the management of foreign body aspiration.
Footnotes
The authors report no funding resources. The authors would like to thank the CAPES-PRINT-UNESP agreement, which provided the internalization partnership for the paper publication.
Competing Interests: The authors have declared that no competing interests.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2021.05.041.
Contributor Information
Henrique Hadad, Email: henriquehadad@gmail.com.
Laís Kawamata de Jesus, Email: kawamata_lais@hotmail.com.
Pier Paolo Poli, Email: pierpaolo_poli@fastwebnet.it.
Idelmo Rangel Garcia-Júnior, Email: irgcirurgia@gmail.com.
Francisley Ávila Souza, Email: francisley.avila@unesp.br.
Flávio Roberto Garbelini de Oliveira, Email: garbelin@terra.com.br.
Appendix. Supplementary materials
References
- 1.Elgazzar RF, Abdelhady AI, Sadakah AA. Aspiration of an impacted lower third molar during its surgical removal under local anaesthesia. Int J Oral Maxillofac Surg. 2007;36(4):362–364. doi: 10.1016/j.ijom.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 2.Johnson GH, Lepe X, Patterson A, Schäfer O. Simplified cementation of lithium disilicate crowns: retention with various adhesive resin cement combinations. J Prosthet Dent. 2018;119(5):826–832. doi: 10.1016/j.prosdent.2017.07.012. [DOI] [PubMed] [Google Scholar]
- 3.Rosenstiel SF, Land MF, Crispin BJ. Dental luting agents: a review of the current literature. J Prosthet Dent. 1998;80(3):280–301. doi: 10.1016/s0022-3913(98)70128-3. [DOI] [PubMed] [Google Scholar]
- 4.Hill EE. Dental cements for definitive luting: a review and practical clinical considerations. Dent Clin North Am. 2007;51(3):643–658. doi: 10.1016/j.cden.2007.04.002. vi. [DOI] [PubMed] [Google Scholar]
- 5.Rasines Alcaraz MG, Veitz-Keenan A, Sahrmann P, Schmidlin PR, Davis D, Iheozor-Ejiofor Z. Direct composite resin fillings versus amalgam fillings for permanent or adult posterior teeth. Cochrane Database Syst Rev. 2014;(3) doi: 10.1002/14651858.CD005620.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Laske M, Opdam NJM, Bronkhorst EM, Braspenning JCC, Huysmans MCDNJM. Risk factors for dental restoration survival: a practice-based study. J Dent Res. 2019;98(4):414–422. doi: 10.1177/0022034519827566. [DOI] [PubMed] [Google Scholar]
- 7.van de Sande FH, Collares K, Correa MB, Cenci MS, Demarco FF, Opdam N. Restoration survival: revisiting patients' risk factors through a systematic literature review. Oper Dent. 2016;41(S7):S7–S26. doi: 10.2341/15-120-LIT. [DOI] [PubMed] [Google Scholar]
- 8.Madan K, Aggarwal AN, Bhagat H, Singh N. Acute respiratory failure following traumatic tooth aspiration. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2012-008393. bcr2012008393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cossellu G, Farronato G, Carrassi A, Angiero F. Accidental aspiration of foreign bodies in dental practice: clinical management and prevention. Gerodontology. 2015;32(3):229–233. doi: 10.1111/ger.12068. [DOI] [PubMed] [Google Scholar]
- 10.Mohamad I, Mohamad H, Ismail H. Bilateral pulmonary aspiration of teeth and the migration of a foreign body from one main bronchus to another. Med J Malaysia. 2010;65(4):309–310. [PubMed] [Google Scholar]
- 11.Holmes I, Gajurel K, Montoya J. The missing tooth: a curious case of postobstructive pneumonia. Open Forum Infect Dis. 2016;3(2):ofw088. doi: 10.1093/ofid/ofw088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mark NM, Lessing JN, Çoruh B. Crowning achievement: a case of dental aspiration. Radiol Case Rep. 2015;10(4):36–38. doi: 10.1016/j.radcr.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dhadge ND. Tooth aspiration following emergency orotrachealintubation. Respir Med Case Rep. 2016;18:85–86. doi: 10.1016/j.rmcr.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hu X, Lee JS, Pianosi PT, Ryu JH. Aspiration-related pulmonary syndromes. Chest. 2015;147(3):815–823. doi: 10.1378/chest.14-1049. [DOI] [PubMed] [Google Scholar]
- 15.Kim IG, Brummitt WM, Humphry A, Siomra SW, Wallace WB. Foreign body in the airway: a review of 202 cases. Laryngoscope. 1973;83(3):347–354. doi: 10.1288/00005537-197303000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Benjamin B, Vandeleur T. Inhaled foreign bodies in children. Med J Aust. 1974;1(10):355–358. [PubMed] [Google Scholar]
- 17.Seals ML, Andry JM, Kellar PN. Pulmonary aspiration of a metal casting: report of case. J Am Dent Assoc. 1988;117(5):587–588. doi: 10.14219/jada.archive.1988.0050. [DOI] [PubMed] [Google Scholar]
- 18.Mu LC, Sun DQ, He P. Radiological diagnosis of aspirated foreign bodies in children: review of 343 cases. J Laryngol Otol. 1990;104(10):778–782. doi: 10.1017/s0022215100113891. [DOI] [PubMed] [Google Scholar]
- 19.Zerella JT, Dimler M, McGill LC, Pippus KJ. Foreign body aspiration in children: value of radiography and complications of bronchoscopy. J Pediatr Surg. 1998;33(11):1651–1654. doi: 10.1016/s0022-3468(98)90601-7. [DOI] [PubMed] [Google Scholar]
- 20.Tamura N, Nakajima T, Matsumoto S, Ohyama T, Ohashi Y. Foreign bodies of dental origin in the air and food passages. Int J Oral Maxillofac Surg. 1986;15(6):739–751. doi: 10.1016/s0300-9785(86)80116-8. [DOI] [PubMed] [Google Scholar]
- 21.Baharloo F, Veyckemans F, Francis C, Biettlot MP, Rodenstein DO. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest. 1999;115(5):1357–1362. doi: 10.1378/chest.115.5.1357. [DOI] [PubMed] [Google Scholar]
- 22.Alexander G, Attia H. Oral maxillofacial surgery displacement complications. Oral Maxillofac Surg Clin North Am. 2011;23(3):379–386. doi: 10.1016/j.coms.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 23.Rafanan AL, Mehta AC. Adult airway foreign body removal. What's new? Clin Chest Med. 2001;22(2):319–330. doi: 10.1016/s0272-5231(05)70046-0. [DOI] [PubMed] [Google Scholar]
- 24.Boyd M, Chatterjee A, Chiles C, Chin R., Jr. Tracheobronchial foreign body aspiration in adults. South Med J. 2009;102(2):171–174. doi: 10.1097/SMJ.0b013e318193c9c8. [DOI] [PubMed] [Google Scholar]
- 25.Nadjem H, Pollak S, Windisch W, Perdekamp MG, Thierauf A. Tooth aspiration: its relevance in medicolegal autopsies. Forensic Sci Int. 2010;200(1-3):e25–e29. doi: 10.1016/j.forsciint.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 26.Kim E, Noh W, Panchal N. Mortality from an aspiration of dental crown during extraction. Gerodontology. 2017;34(4):498–500. doi: 10.1111/ger.12288. [DOI] [PubMed] [Google Scholar]
- 27.Lopez FA, Burton M. Aspiration of dental crown. J Am Osteopath Assoc. 2018;118(2):124. doi: 10.7556/jaoa.2018.029. [DOI] [PubMed] [Google Scholar]
- 28.Qin H, Qing H, Hu N, Zhu H, Wang J. An all-zirconia crown discovered 2 years following aspiration. J Prosthodont. 2018;27(6):492–495. doi: 10.1111/jopr.12711. [DOI] [PubMed] [Google Scholar]
- 29.Singh G, Gambhir RS, Singh S, Kaur H. Accidental aspiration of dental crowns and retrieval. J Contemp Dent Pract. 2012;13(5):716–718. doi: 10.5005/jp-journals-10024-1215. [DOI] [PubMed] [Google Scholar]
- 30.Souza FÁ, Statkievicz C, Guilhem Rosa AL, da Silveira Bossi F. Management of accidental swallowing in implant dentistry. J Prosthet Dent. 2015;114(2):167–170. doi: 10.1016/j.prosdent.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 31.Rabinstein AA, Wijdicks EF. Warning signs of imminent respiratory failure in neurological patients. Semin Neurol. 2003;23(1):97–104. doi: 10.1055/s-2003-40757. [DOI] [PubMed] [Google Scholar]
- 32.Tiwana KK, Morton T, Tiwana PS. Aspiration and ingestion in dental practice: a 10-year institutional review. J Am Dent Assoc. 2004;135(9):1287–1291. doi: 10.14219/jada.archive.2004.0404. [DOI] [PubMed] [Google Scholar]
- 33.Zitzmann NU, Fried R, Elsasser S, Marinello CP. Aspiration und Verschlucken von Fremdkörpern. Verhalten bei Aspiration oder Verschlucken von Fremdkörpern während der zahnärztlichen Behandlung [The aspiration and swallowing of foreign bodies. The management of the aspiration or swallowing of foreign bodies during dental treatment] Schweiz Monatsschr Zahnmed. 2000;110(6):619–632. [PubMed] [Google Scholar]
- 34.Milton TM, Hearing SD, Ireland AJ. Ingested foreign bodies associated with orthodontic treatment: report of three cases and review of ingestion/aspiration incident management. Br Dent J. 2001;190(11):592–596. doi: 10.1038/sj.bdj.4801046. [DOI] [PubMed] [Google Scholar]
- 35.Bunno M, Kawaguchi M, Yamahara K, Kanda C. Removal of a foreign body (artificial tooth) from the bronchial tree: a new method. Intern Med. 2008;47(19):1695–1698. doi: 10.2169/internalmedicine.47.1173. [DOI] [PubMed] [Google Scholar]
- 36.Lin L, Lv L, Wang Y, Zha X, Tang F, Liu X. The clinical features of foreign body aspiration into the lower airway in geriatric patients. Clin Interv Aging. 2014;9:1613–1618. doi: 10.2147/CIA.S70924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wc Hsu, Ts Sheen, Cd Lin, Ct Tan, Th Yeh, Sy Lee. Clinical experiences of removing foreign bodies in the airway and esophagus with a rigid endoscope: a series of 3217 cases from 1970 to 1996. Otolaryngol Head Neck Surg. 2000;122(3):450–454. doi: 10.1067/mhn.2000.98321. [DOI] [PubMed] [Google Scholar]
- 38.Sopeña B, García-Caballero L, Diz P, De la Fuente J, Fernández A, Díaz JA. Unsuspected foreign body aspiration. Quintessence Int. 2003;34(10):779–781. [PubMed] [Google Scholar]
- 39.Black RE, Johnson DG, Matlak ME. Bronchoscopic removal of aspirated foreign bodies in children. J Pediatr Surg. 1994;29(5):682–684. doi: 10.1016/0022-3468(94)90740-4. [DOI] [PubMed] [Google Scholar]
- 40.Dikensoy O, Usalan C, Filiz A. Foreign body aspiration: clinical utility of flexible bronchoscopy. Postgrad Med J. 2002;78(921):399–403. doi: 10.1136/pmj.78.921.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.