Abstract
Outdoor air pollution has been linked to poor sleep health, but limited studies have investigated the relationship between solid cooking fuels and sleep health in adults. Therefore, we analyzed data from the China Health and Retirement Survey (CHARLS), a national survey of about 17,000 residents aged over 45. Participants were restricted to those who participated in CHARLS 2011, 2013 and 2015 (n = 8,668). Sleep health was indicated by self-reported average sleep hours at night and the numbers of unrested days/week in CHARLS 2015. We analyzed cooking fuel types reported and assessed the duration of solid fuels usage as consistent (indicated use in all three surveys or 6 + years) or inconsistent use (indicated use in one or two surveys or 1–4 years). We found consistent use of solid fuels was associated with a shorter sleep duration (OR = 1.17 95% CI 1.01, 1.35 for ≤ 6 h vs. 7–9 h/day) and higher frequencies of feeling unrested (OR = 1.32 95% CI 1.12, 1.55 for ≥ 5 days/week vs. none) compared with cleaner fuels use. The associations for inconsistent solid fuels use and sleep health were in the similar direction but smaller in magnitude. Further research is needed to confirm our findings and evaluate the exposure impact of specific fuel types to inform intervention strategies.
Subject terms: Environmental sciences, Environmental impact, Epidemiology
Introduction
Sleep disorders have been a major public health issue, especially in an aging society, since the elderly are susceptible to age-related changes in circadian rhythm and sleep cycle1. Early awakening fragmented sleep, insufficient sleep, and poor sleep efficiency are common among middle-aged adults and the elderly2,3. Epidemiological studies have shown that sleep disorders and poor sleep quality are associated with a broad range of adverse health outcomes, including cardiovascular disease, hypertension, stroke, cognitive impairment, and depression4–8. Potential mechanisms suggested explaining these associations include that poor sleep health impaired carbohydrate metabolism and endocrine function, activated inflammatory processes, and affected the sympathetic nervous system’s activity to increase blood pressure9–11. An effective intervention on sleep problems may prevent and mitigate the development of other severe chronic diseases.
A variety of physical and psychosocial risk factors have been identified for sleep disorders, including lifestyles such as lack of exercise and smoking12,13, and psychological factors such as job stress and depression14,15. In addition to these individual factors, environmental factors can also affect sleep health. Artificial light at night and noise pollutions have been suggested to disturb sleep16–19. Moreover, accumulating evidence has also suggested that exposures to ambient air pollution, including particulate matter mass concentration (PM10, PM2.5), sulfur dioxide (SO2), nitrogen dioxide (NO2) and carbon monoxide (CO), could affect sleep health20,21 by inducing systemic inflammations in the respiratory tract or central nervous system22,23. Epidemiological evidence has predominantly derived from studies assessing outdoor air pollutions24–27. For example, a most recent study of 395,651 elderly Chinese in Ningbo Province found short-term exposures to outdoor air pollutants, including NO2, SO2, ozone (O3), PM2.5 and PM10 mass concentration were associated with hospital visits for sleep disorders25. Limited studies have investigated the association between indoor air quality and sleep health28. A study evaluating bedroom environment among 63 middle-aged adults in Thailand reported an elevation in 1-year mean PM10 concentration was associated with an increase in apnea–hypopnea and respiratory disturbance indexes29. Two small-scale intervention studies in Peru had reported that the improvement of biomass fuel stoves could improve sleep quality among children30,31. Finally, two recent studies from specific regions of China suggested household air pollution from solid fuel combustion affected poor sleep quality in elderly aged 80 and above32 and that emissions from cooking oil combustion affected sleep quality in middle-aged adults33.
Solid fuels use for cooking activities can be a major source of indoor air pollutants, including PM, NO2, SO2 and CO. At present, about 3 billion people, mostly from low- or middle-income countries, are using solid fuels and kerosene for cooking because of poor financial situation or lack of infrastructure34. According to a survey of 512,891 adults from 10 areas across China during 2004–2008, about half of the participants (52%) reported using coals or charcoal for cooking or heating, especially for rural participants35. In addition, the aging population is rapidly growing in China36. Older adults are likely to spend more time indoor37, and they are vulnerable to ambient pollutions and susceptible to chronic health issues because of a decline in overall physical health38,39. Within this context, we conducted a study to evaluate the association between household use of solid fuels for cooking and sleep health using a large and representative sample of Chinese residents above the age of 45 years.
Materials and methods
Data source
We analyzed data from the China Health and Retirement Longitudinal Study (CHARLS, http://charls.pku.edu.cn/zh-CN), a nationally representative longitudinal survey of about 17,000 Chinese residents ages 45 and older40. The study was launched by Peking University in 2011 which has collected data in 150 counties/districts and 450 villages/resident committees across China every two year. Participants were guided to fill out the self-administered questionnaires by trained researchers. The ethics approval for the CHARLS was granted by the Ethics Review Committee of Peking University and all methods were carried out in accordance with relevant guidelines and regulations. All the participants provided signed informed consent at the time of participation.
Our analysis focused on CHARLS data from 2011 to 2015. Only participants who completed all three waves of surveys (CHARLS 2011, 2013, and 2015) were included in the main analyses to evaluate the duration of exposure prior to outcome assessment (N = 9484). After excluding participants with brain damage or mental retardation and with emotional, nervous, or psychiatric problems that could compromise self-reported data (N = 816), the final sample size for analysis was 8668.
Solid fuels use for cooking
In all three CHARLS surveys from 2011 to 2015, participants were asked: What is their main source of cooking fuel? We classified coal and crop residue/wood burning as solid fuels, and liquefied petroleum gas (LPG), natural gas, marsh gas, and electricity as cleaner fuel types41,42. According to the responses from all three surveys, we further classified solid fuels usage as consistent (indicated use in all three surveys or 6 + years) or inconsistent use (indicated use in one or two surveys only or 1–4 years) prior to sleep outcome assessment in 201541.
Sleep health
In all three CHARLS surveys, participants were asked (1) During the past month, how many hours of actual sleep did you get at night (average hours for one night)? (2) How many days were in accord with the state of feeling unrested from my sleep?42 Sleep health data from 2015 survey was used in the primary analyses to study consistency of solid fuels exposure influences on sleep. Based on the responses, we classified the average hours of sleep into severe insufficient sleep (< 6 h/night), mild insufficient sleep (6–7 h/night), sufficient sleep (7–9 h/night as the reference) and excessive sleep (> 9 h/night), while the number of days feeling unrested were categorized as none or rarely (< 1 day / week), sometimes (1–2 days/week ), moderately (3–4 days/week), and most or all of the time (5–7 days/week)41,42.
Statistical analysis
We conducted multinomial logistic regression to estimate the odds ratio (OR) and 95% confidence interval (CI) for sleep duration or days feeling unrested according to solid fuels usage in cooking, adjusting for potential confounding factors. For sleep duration, sufficient sleep (7–9 h/night) was set as the reference group and for days feeling unrested those reported none or rarely or none (< 1 day) was used as the reference. Our main analyses evaluated the cumulative impacts of exposure on sleep measures. We compared sleep outcomes among consistent (6 + years) or inconsistent solid fuels usage (1–4 years) during the study period with never solid fuels use (or only cleaner fuels use) as the reference. We calculated p value for trend using a continuous exposure variable based on the cumulative years of solid fuels use during the survey periods (value 0, 2, 4, and 6 years assuming each survey wave covered usage in the past two years). In addition, we assessed the cross-sectional associations between solid fuels use and sleep outcomes reported using data from each study wave from 2011 to 2015 separately.
Potential confounders were selected based on literature reviews considering factors associated with choices of cooking fuels use and sleep health and data availability in CHARLS. In all analyses, we adjusted for sex (male or female), age (45–65 or > 65 years), urbanicity of the living place (urban or rural), household economic level estimated by expenditure ( 10,000, 10,000–50,000, 50,000–100,000, > 100,000, RMB), education level (less than high school, high school, college degree or higher), marital status (married and living with a spouse; yes or no), active or passive smoking (yes or no) , and cooking location within household (whether the kitchen is located outside the living room; yes or no). Urban or rural area was classified based on the codes of National Bureau of Statistics of China. The rural–urban fringes and villages were classified into urban areas which include residential households that use solid fuels. Household economic level was measured by overall household expenditure in 2014, including clothing and bedding, traveling expenses, centrally heated fees, consumption of durable goods and electronics, education, medical and fitness expenditures, taxes and donations. Household expenditure has been showed to be a reasonable measure for household economic levels in previous research43,44. Passive smoke exposure was measured by whether other family members in the household had smoking habits. Less than 6.5% participants had at least one missing value of the main potential confounders and they were excluded in the statistical analyses.
In addition, we performed stratified analyses by age (45–65 or > 65 years), sex (male or female), and urbanicity of the residence (urban or rural) when estimating the effect of consistent solid fuels use on sleep health. Sleep problems are more common among older adults and women are more likely to responsible for cooking in Chinese families45. The patterns of exposure and sleep problems might also differ in urban or rural China35. Tests of heterogeneity in multiplicative scale were also performed by assessing the p value of the interaction term for the exposure variable and the potential effect modifier in the regression model.
Moreover, a previous study in CHARLS has suggested that solid fuels use was associated with depression in this population46. We examined the co-occurrence of sleep problems and depression in analyses by classifying participants as who experienced no sleep problems or depression, who only had either sleep problems or depression, and who had both sleep problems and depression using the 2015 survey. Participants were considered to have sleep problems when they experienced insufficient or excessive sleep ( h or h) and high frequency of unrested ( days in a week). Depression symptoms were measured by the self-reported Center for Epidemiologic Studies Depression (CES-D) scale. According to the recommended cut-off46,47, participants were classified as having depression when the CES-D score was 12 or greater.
We re-evaluated our main findings by excluding participants reported use of natural gas in the cleaner fuels reference group concerning NOx emissions from burning natural gas indoors48 and we evaluated the potential effects in each wave. To assess whether selection bias affected our main results, we compared the study characteristics among those who participated in the baseline survey (2011) with those who participated in all three study waves (2011–2015). We performed an inversed probability selection weighting (IPSW) analysis to account for the probability of participation in all three surveys predicted by baseline factors collected in 2011, including the cooking fuel types, sleep health and all covariate data included in the study49.
Finally, we performed a quasi-experimental analysis to estimate the exposure effect on sleep health by studying the change from solid to clean fuel types for cooking during the study period. Among self-reported solid fuel users identified in 2011 (N = 4275), we compared sleep health among those who switched to cleaner fuels assessed in later years (n = 1604) with those who used solid fuels consistently from 2011 to 2015 as the reference (n = 2671). In addition, we also compared the same reference group to those who used solid fuels in 2011 and 2013, and most recently switched to cleaner fuels use reported in 2015 (n = 743).
Results
Summary of selected study characteristics
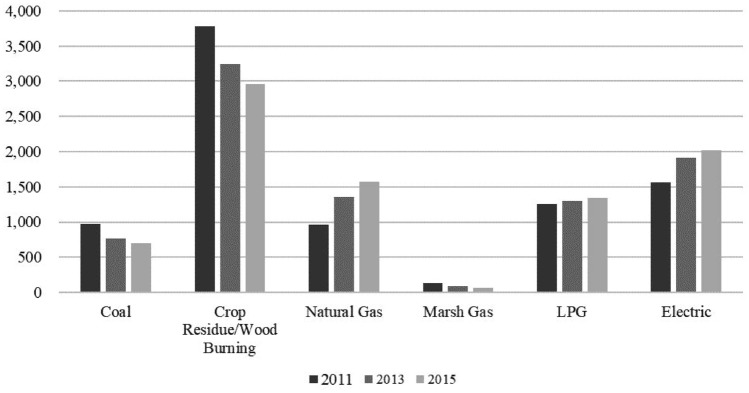
In this population, 64.6% (N = 5604) reported ever using solid fuels while 35.4% (N = 3064) indicated only using cleaner fuels for cooking during the study period. Among the solid fuels users, about half (47.6%) were considered consistent use throughout the study period. The distribution for the specific fuel types reported for cooking is presented in Fig. 1. The usage of solid fuel types, including coal and crop residue or wood burning for cooking has decreased from 2011 to 2015. In comparison, cleaner fuel types use including natural gas and electric have increased.
Figure 1.
The numbers of participants on each fuel type for cooking reported in the three study waves. Coal and crop residue/wood burning were considered as solid fuels in this study. Clean fuels included natural gas, marsh gas, liquefied petroleum gas (LPG) and electric.
The selected characteristics of the study population by solid fuels use groups are presented in Table 1. Participants reporting consistent solid fuels use during the study period were older, had lower education level and household expenditure. As expected, participants living in rural areas were more likely to use solid fuels. More than 90% of participants had a kitchen outside the indoor living area, but those using solid fuels for a longer time were more likely not.
Table 1.
Characteristics of study participants in the CHARLS, 2011–2015.
| Characteristics | Cleaner fuels use only (N = 3064), N (%) | Solid fuels use reported in one or two surveys only (N = 2933), N (%) | Consistent solid fuels use reported in all three surveys (N = 2671), N (%) |
|---|---|---|---|
| Age (years) | |||
| 45–65 | 2265 (74.3) | 2010 (68.9) | 1664 (62.5) |
| Over 65 | 783 (25.7) | 907 (31.1) | 1000 (37.5) |
| Missing | 16 | 16 | 7 |
| Sex | |||
| Male | 1322 (48.4) | 1270 (48.6) | 1165 (49.1) |
| Female | 1420 (51.6) | 1346 (51.4) | 1209 (50.9) |
| Missing | 10 | 7 | 11 |
| Urbanicity of the living place | |||
| Rural | 1003 (36.4) | 1873 (71.5) | 1993 (83.8) |
| Urban | 1755 (63.6) | 746 (28.5) | 385 (16.2) |
| Expenditure in 2015 (RMB) | |||
| ≤ 10,000 | 1845 (61.0) | 2230 (77.1) | 2115 (80.2) |
| 10,000–50,000 | 932 (30.8) | 549 (19.0) | 457 (17.3) |
| 50,000–100,000 | 128 (4.2) | 69 (2.4) | 42 (1.6) |
| 100,000 | 118 (3.9) | 44 (1.5) | 24 (0.9) |
| Missing | 41 | 41 | 33 |
| Educational level | |||
| No formal | 754 (27.4) | 1178 (45.0) | 1282 (53.9) |
| ≤ 12 years | 1872 (67.9) | 1425 (54.5) | 1083 (45.5) |
| ≥ 12 years | 130 (4.7) | 16 (0.6) | 13 (0.6) |
| Missing | 3 | 2 | 0 |
| Marital status | |||
| Married | 2353 (85.3) | 2129 (81.3) | 1997 (84.0) |
| Not married | 405 (14.7) | 490 (18.7) | 381 (16.0) |
| Smoking | |||
| Active | 1229 (41.3) | 1264 (44.3) | 1192 (45.9) |
| Passive | 803 (27.0) | 760 (26.6) | 695 (26.8) |
| Never | 944 (31.7) | 829 (29.1) | 711 (27.4) |
| Missing | 88 | 80 | 73 |
| Cooking location within household | |||
| Yes | 2933 (96.4) | 2713 (93.2) | 2424 (91.8) |
| No | 111 (3.7) | 198 (6.8) | 218 (8.3) |
| Missing | 20 | 22 | 29 |
| Average hours of sleep at night | |||
| 6 | 892 (29.1) | 924 (31.5) | 921 (34.5) |
| 6–7 | 720 (23.5) | 619 (21.1) | 482 (18.1) |
| 7–9 | 1227 (40.1) | 1134 (38.7) | 980 (36.7) |
| 9 | 225 (7.3) | 256 (8.7) | 288 (10.8) |
| The number of unrested days per week | |||
| < 1 | 1522 (55.2) | 1345 (51.4) | 1180 (49.6) |
| 1–2 | 378 (13.7) | 375 (14.3) | 337 (14.2) |
| 3–4 | 389 (14.1) | 364 (13.9) | 355 (14.9) |
| 5–7 | 469 (17.0) | 535 (20.4) | 506 (21.3) |
Associations between solid fuels use and sleep health
Consistent solid fuels use was associated with higher odds for insufficient (OR = 1.17 95% CI 1.01, 1.35) or excessive sleep (OR = 1.22 95% CI 0.97, 1.53) at night compared with participants who cooked with cleaner fuels only, while the associations for sleep duration were null for inconsistent solid fuels use compared with cleaner fuels use.
Consistent solid fuels use reported in three surveys was also associated with higher frequencies of days feeling unrested. The odd ratios were 1.26 (95% CI 1.06, 1.51) for 3–4 days/week and 1.32 (95% CI 1.12, 1.55) for more than 5 unrested days/week among consistent solid fuels users. The associations were in the similar direction but smaller in magnitude for participants indicated solid fuels use in one or two surveys only. The p values for cumulative years of solid fuels use and unrested sleep were all smaller than 0.10 (Table 2).
Table 2.
Associations between solid fuels use for cooking and self-reported sleep health in the CHARLS.
| Outcomes | Inconsistent solid fuels use (reported in 1 or 2 surveys) vs. cleaner fuels use | Consistent solid fuels use (reported in all surveys) vs. cleaner fuels use | P value for cumulative years of exposureb |
|---|---|---|---|
| OR (95% CI)a | OR (95% CI)a | ||
| Average hours of sleep at night | |||
| 6 | 1.04 (0.91, 1.19) | 1.17 (1.01,1.35) | 0.11 |
| 6–7 | 0.96 (0.83, 1.12) | 0.91 (0.77 1.07) | 0.20 |
| 7–9 | Reference | Reference | Reference |
| 9 | 1.03 (0.83, 1.28) | 1.22 (0.97, 1.53) | 0.12 |
| The number of unrested days per week | |||
| 1 | Reference | Reference | Reference |
| 1–2 | 1.12 (0.95, 1.33) | 1.17 (0.98, 1.40) | 0.06 |
| 3–4 | 1.06 (0.90, 1.26) | 1.26 (1.06, 1.51) | 0.01 |
| 5–7 | 1.25 (1.07, 1.46) | 1.32 (1.12, 1.55) | 0.01 |
aAdjusted for age, sex, education, marital status, household expenditure, active or passive smoking, urbanicity, and cooking location within household.
bP value was calculated using the cumulative years of solid fuels use exposure (0, 2, 4, and 6 years) fitted as a continuous variable.
Associations between consistent solid fuels use and sleep health stratified by age, sex and urbanicity
In general, the associations between consistent solid fuels use and impaired sleep health appeared to be stronger for elderly 65 years and older (Table 3). Long-term solid fuels users had 55% greater odds (OR = 1.55, 95% CI 1.04, 2.30) for excessive sleep compared with cleaner fuels users among the elderly, while the effect sizes were closer to null for adults 45–65 years. For unrested days of sleep, the association between consistent solid fuels use and the most severe group of 5–7 unrested days also appeared to be stronger among the elderly (OR = 1.72 95% CI 1.26, 2.33). However, the interaction p values were greater than 0.10 suggested an insufficient statistical precision to conclude an effect modification by age.
Table 3.
Associations between solid fuels use for cooking and slef-reported sleep helath, stratified by age, sex and urbancity.
| Outcomes | Consistent solid fuels use (reported in all surveys) vs. cleaner fuels use only | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Age 45–65 | > 65 years | Interaction p valueb | Men | Women | Interaction p valueb | Rural area | Urban area | Interaction p valueb | |
| OR (95% CI)a | OR (95% CI)a | OR (95% CI)a | OR (95% CI)a | OR (95% CI)a | OR (95% CI)a | ||||
| Average hours of sleep at night | |||||||||
| 6 | 1.14 (0.96, 1.36) | 1.29 (0.98, 1.71) | 0.50 | 1.19 (0.96, 1.47) | 1.16 (0.95, 1.42) | 0.74 | 1.27 (1.05, 1.52) | 0.98 (0.75, 1.28) | 0.09 |
| 6–7 | 0.96 (0.79, 1.16) | 0.81 (0.59, 1.13) | 0.15 | 0.83 (0.66, 1.04) | 1.00 (0.79, 1.27) | 0.11 | 0.94 (0.76, 1.16) | 0.84 (0.63, 1.14) | 0.53 |
| 7–9 | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| 9 | 1.09 (0.82, 1.45) | 1.55 (1.04, 2.30) | 0.38 | 1.39 (1.00, 1.94) | 1.08 (0.79, 1.48) | 0.22 | 1.16 (0.88, 1.52) | 1.15 (0.75, 1.78) | 0.96 |
| The number of unrested days per week | |||||||||
| 1 | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| 1–2 | 1.15 (0.93, 1.42) | 1.18 (0.84, 1.66) | 0.65 | 1.22 (0.95, 1.58) | 1.13 (0.87, 1.46) | 0.35 | 1.28 (1.02, 1.62) | 1.07 (0.76, 1.50) | 0.27 |
| 3–4 | 1.33 (1.08, 1.64) | 1.13 (0.79, 1.62) | 0.36 | 1.30 (0.97, 1.73) | 1.27 (1.00, 1.60) | 0.65 | 1.30 (1.03, 1.63) | 1.24 (0.90, 1.72) | 0.75 |
| 5–7 | 1.20 (0.98, 1.45) | 1.72 (1.26, 2.33) | 0.25 | 1.12 (0.87, 1.43) | 1.49 (1.19, 1.85) | 0.13 | 1.26 (1.03, 1.55) | 1.55 (1.16, 2.07) | 0.26 |
a According to consistent solid fuels use and adjusted for age, sex, education, marital status, household expenditure, active or passive smoking, urbanicity and cooking location within household.
b P value was calculated using the product term between the exposure and the modifying variable.
There were no apparent differences found in analyses stratified by sex (all interaction p values > 0.10). Only for the most severe group of 5–7 unrested days the effect for long-term solid fuels use appeared to be stronger on women than on men (Table 3). Overall, there was no apparent heterogeneity by rural or urban residence observed (Table 3). The estimated effect of consistent solid fuels use and insufficient sleep was stronger among rural residents (OR = 1.27 95% CI 1.05, 1.52; interaction p value = 0.09).
Associations between consistent solid fuels use and co-occurrence of sleep problems and depression
Solid fuels usage in three surveys was associated with sleep problems among participants without depression (OR = 1.19 95% CI 1.03, 1.37). A two-fold higher odd was observed for the co-occurrence of both sleep problems and depression (OR = 2.11 95% CI 1.74, 2.55) among long-term solid fuels users compared with non-users (Table 4).
Table 4.
Associations between solid fuels use for cooking and sleep problem with the co-occurance of depression.
| Outcomesa,b | Cleaner fuels use (2861) | Consistent solid fuels use (reported in all surveys) (2491) | OR (95% CI) c | P value for cumulative years of exposured |
|---|---|---|---|---|
| Without sleep problems and depression | 1406 | 923 | Reference | Reference |
| Sleep problems only | 1084 | 891 | 1.19 (1.03, 1.37) | 0.06 |
| Depression only | 68 | 111 | 1.92 (1.34, 2.74) | < 0.01 |
| With both sleep problems and depression | 303 | 566 | 2.11 (1.74, 2.55) | < 0.01 |
aParticipants defined as having sleep problems when they reported either having insufficient (≤ 6 hrs) or excessive (≥ 9 hrs) sleep durations or higher frequency of feeling unrested (≥ 3 days in a week).
b596 participants with missing data on depression were excluded in the statistical analyses.
cAccording to consistent solid fuels use and adjusted for age, sex, education, marital status, household expenditure, active or passive smoking, urbanicity and cooking location within household.
dP value was calculated using the cumulative years of solid fuels use exposure (0, 2, 4 and 6 years) fitted as a continuous variable.
Sensitivity analyses
Among those who enrolled in 2011, 63.6% also completed the subsequent surveys in 2013 and 2015. Adults less than 65 years, married, living in rural area and solid fuel users at baseline were slightly more likely to have participated in all three surveys (Supplementary Table 1). Our findings remain unchanged using the IPSW-adjusted estimates suggesting that influence from selection bias is minimal (Supplementary Table 2). Our main results also did not markedly change when we excluded natural gas users in the reference group (Supplementary Table 3). The cross-sectional associations between solid fuels use and sleep health in each study wave is presented in Supplementary Table 4. Solid fuels use was associated with higher frequencies of unrested days of sleep in all three waves. For sleep duration, solid fuels use was also associated with excessive sleep in the wave 2011 and wave 2015 and with insufficient sleep in the wave 2011 and 2013 (Supplementary Table 4). Among solid fuel users identified in 2011, those who switched to cleaner fuels during the study period had lower odds for excessive sleep (average sleep hours > 9 h; OR = 0.76 95% CI 0.60, 0.97) in 2015. The point estimates for days feeling unrested were also lower for those who switched to cleaner fuels use but the 95% CIs were wide (Supplementary Table 5).
Discussion
In this study, we analyzed a nationally representative database of adults over 45 years in China with a high proportion of households using solid fuels for cooking. Our findings suggest that a longer duration of using solid fuels for cooking was associated with self-reported poor sleep health as indicated by non-optimal duration of sleep and higher frequencies of unrested days. Some effect sizes observed appear to be stronger for the population 65 years and older, but confirmation of our findings with improved exposure measures and clinically validated sleep outcomes are warranted.
Previous epidemiological studies of air pollution and sleep problems have predominantly focused on outdoor air pollution24,26,27,50 and short-term responses25. Limited studies focused on the association between solid fuels use and sleep health. In children, two intervention studies conducted in Peru that replaced household biomass fuel with cleaner fuel kitchen stoves suggested improved symptoms of sleep apnea and respiratory problems30,31. In adults, the China Hainan Centenarian Cohort Study of 1,616 elderly aged 80 years and older showed that household air pollution from solid fuel combustion increased the risk of having poor sleep quality measured by the Pittsburgh sleep quality index (PSQI)32. Moreover, a cross-sectional study of 2,197 middle-aged adults recruited from employees working in a Machinery Company in Liuzhou, China, reported exposure of emissions from cooking oil combustion affected poor sleep quality measured by PSQI33. Our findings, which are based on a large sample drawn from representative data across multiple regions in China, add to the literature and suggest that solid fuels used for cooking might also contribute to impaired sleep health in middle-aged and elderly Chinese residents.
Studies have shown that solid fuels use could generate elevated indoor exposure to PM, NO2 and SO251,52. A study in Yunnan Province, China, measured indoor NO2 in households from 30 villages found that 24-h averaged NO2 levels reached 132 ppb for households using smokeless coal and 111 ppb for households using smoky coal at home53. A study in India evaluating homes in 51 villages reported the 24-h average PM2.5 concentration of 372 µg/m3 in kitchens where solid fuels were used54. The concentrations of these pollutants were above World Health Organization (WHO) air quality guideline values, which recommend 25 µg/m3 for 24-h mean PM2.5 concentrations and 40 ppb for annual mean NO2 levels55.
The biological mechanism of how indoor air pollutants affect sleep health is still unclear, while some suggestive mechanisms have been proposed. Studies have suggested exposure to PM2.5 can affect neurobehavioral functions of central nervous systems which regulate sleep in human and animal models22,56,57. Long-term exposure to excess air pollutants could also damage intact mucociliary nasal epithelium and increase the risk of respiratory tract inflammation, leading to breathing problems and sleep-disorder23. Excess concentrations of O3, SO2, PM10 and PM2.5 exposure have been demonstrated to increase proinflammatory mediators including interleukin-6, and changes in the inflammatory cytokine levels may affect sleep quality23,58,59. Long-term PM2.5 exposure could also increase the stress level and anxiety or depressive symptoms60,61 and subsequently disrupt normal sleep. Considering the complexity of mixture air pollution, further studies are needed to elucidate the mechanisms of actions for air pollution impacts on sleep disorders.
Previous studies using CHARLS data have suggested shorter nighttime sleep duration < 6 h was associated with a high risk of depressive symptoms in Chinese elderly62, and a higher proportion of current household solid fuels users reported depression symptoms measured by CES-D scale compared with clean fuels users46. The relationship between sleep problems and depression is likely bi-directional63. Our analyses that considered both sleep and depressive symptoms suggested a stronger association for co-occurrence of sleep problems and depression among long-term solid fuels use, while a weaker association was also noted for sleep problems only without depression. Future research of indoor and outdoor air pollution should explore the role of sleep problems as a potential mediating factor that leads to depression or other major chronic diseases in older adults4,64.
Household solid fuels use is the primary pollutant source of indoor air pollution in developing countries34. In China, about 170 million urban residents and 490 million rural residents used solid fuels for cooking according to 2010 census data65. Energy issues have drawn more and more attention. The government and residents have taken measures to promote cleaner fuels like electric, natural gas, liquefied petroleum gas for cooking66. Repeated surveys in CHARLS from 2011 to 2015 also suggested the use of cleaner fuel types has become more common among older residents in China. However, a high cost associated with cleaner fuels use may be a barrier for the low-income households to adopt the change in cooking fuels. Continuing efforts in reducing solid fuels use for low-income rural residents in China are needed.
Our studies have several strengths. First, we analyzed data from a large study with three repeated surveys from a representative sampling of 150 counties/districts in China, including main Chinese provinces and cities. The prevalence of solid fuels use for cooking is high in this population. To our knowledge, there was no similar study focusing on the association between solid fuels use and sleep health in such a large population in China. The repeated surveys also allowed us to evaluate the duration of use and the change from solid to cleaner fuels as the primary household cooking fuels. A range of potential confounding factors were considered in analyses. The large sample size also allowed us to evaluate potential effect modification by age, sex and urbanicity, and study the co-occurrence of sleep problems and depression.
Our study has several limitations. First, we did not have any direct measurements of indoor air pollutant levels from cooking fuels. However, this would require repeated measurements to capture long-term exposure effects, which is less feasible for a large population study. Our analyses primarily addressed cumulative exposure utilizing data from three waves of CHARLS. The cross-sectional association between solid fuels usage and sleep outcomes at each wave might reflect short-term exposure effect, but the results can be sensitive to reverse causality bias. For example, sleep problems can affect the participants’ lifestyles and behaviors. Second, the data we used was primary cooking fuels without considering heating fuels as another exposure source. Solid use for heating is an important source of indoor air pollution, especially for northern China during the winter season. Some household factors, including the kitchen design and ventilation, might modify indoor pollution level from cooking67. The CHARLS database also does not provide outdoor air pollution measures for analyses. Sleep outcomes were self-reported and there was no availability of clinical measures or information regarding sleep medication use. More in-depth assessments of sleep quality, such as the use of polysomnography or objective sleep-scale measures, coupled with novel wearable tools to characterize personal environmental exposure profiles68, could be employed to advance our understanding of the relationship between indoor air pollution and sleep health. Finally, the influence from uncontrolled confounding cannot be ruled out. Some uncontolled variables, such as diets, physical activities, and other social and physical environmental factors, could affect sleep health. These factors, however, might not strongly correlated with the choice of fuels type for cooking after controlling socio-economical differences in the statistical analyses.
Conclusions
In this study based on the three waves of CHARLS from 2011–2015, we found consistent solid fuels use for cooking during the study period was associated with self-reported poor sleep health in Chinese adults 45 years and older. Strategies to promote cleaner fuels for cooking are needed for Chinese elderly residents. Future studies are recommended to investigate the impact of specific fuel types and the biological mechanism linking air pollutants released from solid fuels to sleep disorders etiology.
Supplementary Information
Author contributions
H.Y., J.L., and Z.L. conceived the main idea for the study. H.Y. acquired the dataset from the CHARLS study. H.Y. performed statistical analyses and drafted the manuscript. J.L., and Z.L. supervised the statistical analyses and writing. K.C. and K.J.G.P. contributed to discussions and revisions of the manuscript. All authors read and approved the final manuscript.
Funding
There was no funding for this work.
Data availability
The datasets used and analyzed during the current study are available and assessable from the China Health and Retirement Longitudinal Study (CHARLS, http://charls.pku.edu.cn/zh-CN).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-92452-0.
References
- 1.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–1273. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 2.Suzuki K, Miyamoto M, Hirata K. Sleep disorders in the elderly: Diagnosis and management. J. Gen. Fam. Med. 2017;18:61–71. doi: 10.1002/jgf2.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu Y, Wheaton AG, Chapman DP, Croft JB. Sleep duration and chronic diseases among US adults age 45 years and older: Evidence from the 2010 Behavioral Risk Factor Surveillance System. Sleep. 2013;36:1421–1427. doi: 10.5665/sleep.3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yu K, et al. Association of solid fuel use with risk of cardiovascular and all-cause mortality in rural China. JAMA. 2018;319:1351–1361. doi: 10.1001/jama.2018.2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vandeputte M, de Weerd A. Sleep disorders and depressive feelings: A global survey with the Beck depression scale. Sleep Med. 2003;4:343–345. doi: 10.1016/S1389-9457(03)00059-5. [DOI] [PubMed] [Google Scholar]
- 6.Maung SC, El Sara A, Chapman C, Cohen D, Cukor D. Sleep disorders and chronic kidney disease. World J. Nephrol. 2016;5:224. doi: 10.5527/wjn.v5.i3.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc. Sci. Med. 2010;71:1027–1036. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 8.Bathgate CJ, Fernandez-Mendoza J. Insomnia, short sleep duration, and high blood pressure: Recent evidence and future directions for the prevention and management of hypertension. Curr. Hypertens. Rep. 2018;20:52. doi: 10.1007/s11906-018-0850-6. [DOI] [PubMed] [Google Scholar]
- 9.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. The lancet. 1999;354:1435–1439. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 10.Meier-Ewert HK, et al. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J. Am. Coll. Cardiol. 2004;43:678–683. doi: 10.1016/j.jacc.2003.07.050. [DOI] [PubMed] [Google Scholar]
- 11.Tochikubo O, Ikeda A, Miyajima E, Ishii M. Effects of insufficient sleep on blood pressure monitored by a new multibiomedical recorder. Hypertension. 1996;27:1318–1324. doi: 10.1161/01.HYP.27.6.1318. [DOI] [PubMed] [Google Scholar]
- 12.Wetter DW, Young TB. The relation between cigarette smoking and sleep disturbance. Prev. Med. 1994;23:328–334. doi: 10.1006/pmed.1994.1046. [DOI] [PubMed] [Google Scholar]
- 13.Passos GS, et al. Effects of moderate aerobic exercise training on chronic primary insomnia. Sleep Med. 2011;12:1018–1027. doi: 10.1016/j.sleep.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 14.Nutt D, Wilson S, Paterson L. Sleep disorders as core symptoms of depression. Dialogues Clin. Neurosci. 2008;10:329. doi: 10.31887/DCNS.2008.10.3/dnutt. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kalimo R, Tenkanen L, Härmä M, Poppius E, Heinsalmi P. Job stress and sleep disorders: Findings from the Helsinki Heart Study. Stress Med. 2000;16:65–75. doi: 10.1002/(SICI)1099-1700(200003)16:2<65::AID-SMI834>3.0.CO;2-8. [DOI] [Google Scholar]
- 16.Cho Y, et al. Effects of artificial light at night on human health: A literature review of observational and experimental studies applied to exposure assessment. Chronobiol. Int. 2015;32:1294–1310. doi: 10.3109/07420528.2015.1073158. [DOI] [PubMed] [Google Scholar]
- 17.Obayashi K, Saeki K, Kurumatani N. Association between light exposure at night and insomnia in the general elderly population: The HEIJO-KYO cohort. Chronobiol. Int. 2014;31:976–982. doi: 10.3109/07420528.2014.937491. [DOI] [PubMed] [Google Scholar]
- 18.Halonen JI, et al. Associations between nighttime traffic noise and sleep: The Finnish public sector study. Environ. Health Perspect. 2012;120:1391–1396. doi: 10.1289/ehp.1205026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nassur A-M, et al. The impact of aircraft noise exposure on objective parameters of sleep quality: Results of the DEBATS study in France. Sleep Med. 2019;54:70–77. doi: 10.1016/j.sleep.2018.10.013. [DOI] [PubMed] [Google Scholar]
- 20.Cao B, Chen Y, McIntyre RS. Comprehensive review of the current literature on impact of ambient air pollution and sleep quality. Sleep Med. 2020;79:211–219. doi: 10.1016/j.sleep.2020.04.009. [DOI] [PubMed] [Google Scholar]
- 21.Liu J, Wu T, Liu Q, Wu S, Chen J-C. Air pollution exposure and adverse sleep health across the life course: A systematic review. Environ. Pollut. 2020;262:114263. doi: 10.1016/j.envpol.2020.114263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Calderón-Garcidueñas L, et al. Air pollution and brain damage. Toxicol. Pathol. 2002;30:373–389. doi: 10.1080/01926230252929954. [DOI] [PubMed] [Google Scholar]
- 23.Calderón-Garcidueñas L, et al. Pediatric respiratory and systemic effects of chronic air pollution exposure: Nose, lung, heart, and brain pathology. Toxicol. Pathol. 2007;35:154–162. doi: 10.1080/01926230601059985. [DOI] [PubMed] [Google Scholar]
- 24.Fang SC, et al. Traffic-related air pollution and sleep in the Boston Area Community Health Survey. J Expo Sci Environ Epidemiol. 2015;25:451–456. doi: 10.1038/jes.2014.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tang M, et al. The association of short-term effects of air pollution and sleep disorders among elderly residents in China. Sci. Total Environ. 2020;708:134846. doi: 10.1016/j.scitotenv.2019.134846. [DOI] [PubMed] [Google Scholar]
- 26.Zanobetti A, et al. Associations of PM10 with sleep and sleep-disordered breathing in adults from seven US urban areas. Am. J. Respir. Crit. Care Med. 2010;182:819–825. doi: 10.1164/rccm.200912-1797OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lawrence WR, et al. Association between long-term exposure to air pollution and sleep disorder in Chinese children: The Seven Northeastern Cities study. Sleep. 2018;41:zsy122. doi: 10.1093/sleep/zsy122. [DOI] [PubMed] [Google Scholar]
- 28.Logue JM, Price PN, Sherman MH, Singer BC. A method to estimate the chronic health impact of air pollutants in US residences. Environ. Health Perspect. 2012;120:216–222. doi: 10.1289/ehp.1104035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lappharat S, Taneepanichskul N, Reutrakul S, Chirakalwasan N. Effects of bedroom environmental conditions on the severity of obstructive sleep apnea. J. Clin. Sleep Med. 2018;14:565–573. doi: 10.5664/jcsm.7046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Castañeda, J. L., Kheirandish‐Gozal, L., Gozal, D., Accinelli, R. A. & Pampa Cangallo Instituto de Investigaciones de la Altura Research Group. Effect of reductions in biomass fuel exposure on symptoms of sleep apnea in children living in the peruvian andes: A preliminary field study. Pediatr. Pulmonol.48, 996–999 (2013). [DOI] [PubMed]
- 31.Accinelli RA, et al. Adherence to reduced-polluting biomass fuel stoves improves respiratory and sleep symptoms in children. BMC Pediatr. 2014;14:12. doi: 10.1186/1471-2431-14-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen C, et al. Association between household fuel use and sleep quality in the oldest-old: Evidence from a propensity-score matched case-control study in Hainan, China. Environ. Res. 2020;191:110229. doi: 10.1016/j.envres.2020.110229. [DOI] [PubMed] [Google Scholar]
- 33.Wei F, et al. Association between Chinese cooking oil fumes and sleep quality among a middle-aged Chinese population. Environ. Pollut. 2017;227:543–551. doi: 10.1016/j.envpol.2017.05.018. [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization. Household air pollution and health. https://www.who.int/news-room/fact-sheets/detail/household-air-pollution-and-health (2018).
- 35.Li, J. et al. Epidemiological characteristics of household fuel use in 10 areas of China. Zhonghua liu xing bing xue za zhi= Zhonghua liuxingbingxue zazhi39, 1426 (2018). [DOI] [PubMed]
- 36.Xinhua News. China's senior population may surge from 2025. http://www.xinhuanet.com/english/2019-02/09/c_137808376.htm (2019).
- 37.Almeida-Silva M, Wolterbeek HT, Almeida S. Elderly exposure to indoor air pollutants. Atmos. Environ. 2014;85:54–63. doi: 10.1016/j.atmosenv.2013.11.061. [DOI] [Google Scholar]
- 38.Shumake KL, Sacks JD, Lee JS, Johns DO. Susceptibility of older adults to health effects induced by ambient air pollutants regulated by the European Union and the United States. Aging Clin. Exp. Res. 2013;25:3–8. doi: 10.1007/s40520-013-0001-5. [DOI] [PubMed] [Google Scholar]
- 39.Li J, et al. Characterization and factors associated with sleep quality among rural elderly in China. Arch. Gerontol. Geriatr. 2013;56:237–243. doi: 10.1016/j.archger.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 40.The China Health and Retirement Longitudinal Study. About CHARLS. http://charls.pku.edu.cn/pages/about/111/en.html (2019).
- 41.Yu, H. Solid Fuel-related Indoor Air Pollution and Poor Sleep Quality in Adults Aged 45 Years and Older; a National Longitudinal Study in China, Yale University, (2020).
- 42.The China Health and Retirement Longitudinal Study. China Health and Retirement Longitudinal Study Followup Questionnaire 2015. http://charls.pku.edu.cn/Public/ashelf/public/uploads/document/2015-charls-wave4/application/CHARLS_2015_Questionnaire.pdf (2017).
- 43.Strauss J, Thomas D. Health over the life course. Handb. Dev. Econ. 2007;4:3375–3474. [Google Scholar]
- 44.Shi L, Zhang D. China's new rural cooperative medical scheme and underutilization of medical care among adults over 45: Evidence from CHARLS pilot data. J. Rural Health. 2013;29:s51–s61. doi: 10.1111/jrh.12013. [DOI] [PubMed] [Google Scholar]
- 45.Hou B-D, et al. Cooking fuel choice in rural China: Results from microdata. J. Clean. Prod. 2017;142:538–547. doi: 10.1016/j.jclepro.2016.05.031. [DOI] [Google Scholar]
- 46.Liu, Y., Chen, X. & Yan, Z. Depression in the house: The effects of household air pollution from solid fuel Use in China. (2019). [DOI] [PMC free article] [PubMed]
- 47.Cheng ST, Chan AC. The center for epidemiologic studies depression scale in older Chinese: Thresholds for long and short forms. Int. J. Geriatr. Psychiatry A J. Psychiatry Late Life Allied Sci. 2005;20:465–470. doi: 10.1002/gps.1314. [DOI] [PubMed] [Google Scholar]
- 48.Nicole W. Cooking up indoor air pollution: Emissions from natural gas stoves. Environ. Health Perspect. 2014;122(1):A27. doi: 10.1289/ehp.122-A27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nohr EA, Liew Z. How to investigate and adjust for selection bias in cohort studies. Acta Obstet. Gynecol. Scand. 2018;97:407–416. doi: 10.1111/aogs.13319. [DOI] [PubMed] [Google Scholar]
- 50.Yu H, Chen P, Paige Gordon S, Yu M, Wang Y. The association between air pollution and sleep duration: A Cohort study of freshmen at a University in Beijing, China. Int J Environ Res Public Health. 2019 doi: 10.3390/ijerph16183362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chafe ZA, et al. Household cooking with solid fuels contributes to ambient PM2.5 air pollution and the burden of disease. Environ. Health Perspect. 2014;122:1314–1320. doi: 10.1289/ehp.1206340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Seow WJ, et al. Indoor concentrations of nitrogen dioxide and sulfur dioxide from burning solid fuels for cooking and heating in Yunnan Province, China. Indoor Air. 2016;26:776–783. doi: 10.1111/ina.12251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Du W, Li X, Chen Y, Shen G. Household air pollution and personal exposure to air pollutants in rural China—a review. Environ Pollut. 2018;237:625–638. doi: 10.1016/j.envpol.2018.02.054. [DOI] [PubMed] [Google Scholar]
- 54.Balakrishnan K, et al. Household air pollution exposures of pregnant women receiving advanced combustion cookstoves in India: Implications for intervention. Ann. Glob. Health. 2015;81:375–385. doi: 10.1016/j.aogh.2015.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.World Health Organization. Ambient (outdoor) air pollution. https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (2018).
- 56.Wang S, et al. Association of traffic-related air pollution with children’s neurobehavioral functions in Quanzhou, China. Environ. Health Perspect. 2009;117:1612–1618. doi: 10.1289/ehp.0800023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Guxens, M. & Sunyer, J. A review of epidemiological studies on neuropsychological effects of air pollution. Swiss Med. Wkly.141, w13322 (2012). [DOI] [PubMed]
- 58.Thompson AM, et al. Baseline repeated measures from controlled human exposure studies: Associations between ambient air pollution exposure and the systemic inflammatory biomarkers IL-6 and fibrinogen. Environ Health Perspect. 2010;118:120–124. doi: 10.1289/ehp.0900550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Prather AA, et al. Normative variation in self-reported sleep quality and sleep debt is associated with stimulated pro-inflammatory cytokine production. Biol. Psychol. 2009;82:12–17. doi: 10.1016/j.biopsycho.2009.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pun VC, Manjourides J, Suh H. Association of ambient air pollution with depressive and anxiety symptoms in older adults: Results from the NSHAP study. Environ. Health Perspect. 2017;125:342–348. doi: 10.1289/EHP494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Miller JG, Gillette JS, Manczak EM, Kircanski K, Gotlib IH. Fine particle air pollution and physiological reactivity to social stress in adolescence: The moderating role of anxiety and depression. Psychosom. Med. 2019;81:641–648. doi: 10.1097/PSY.0000000000000714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li Y, et al. Longitudinal association of sleep duration with depressive symptoms among middle-aged and older Chinese. Sci. Rep. 2017;7:11794. doi: 10.1038/s41598-017-12182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Riemann D, Berger M, Voderholzer U. Sleep and depression–results from psychobiological studies: An overview. Biol. Psychol. 2001;57:67–103. doi: 10.1016/s0301-0511(01)00090-4. [DOI] [PubMed] [Google Scholar]
- 64.Yaffe K, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA. 2011;306:613–619. doi: 10.1001/jama.2011.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tang X, Liao H. Energy poverty and solid fuels use in rural China: Analysis based on national population census. Energy Sustain. Dev. 2014;23:122–129. doi: 10.1016/j.esd.2014.08.006. [DOI] [Google Scholar]
- 66.Natural Resources Defense Council. China Dispersed Coal Governance Report 2019.http://coalcap.nrdc.cn/datum/info?id=101&type=2 (2019).
- 67.Akunne AF, Louis VR, Sanon M, Sauerborn R. Biomass solid fuel and acute respiratory infections: The ventilation factor. Int. J. Hyg. Environ. Health. 2006;209:445–450. doi: 10.1016/j.ijheh.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 68.Koelmel JP, et al. Exploring the external exposome using wearable passive samplers-The China BAPE study. Environ. Pollut. 2021;270:116228. doi: 10.1016/j.envpol.2020.116228. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analyzed during the current study are available and assessable from the China Health and Retirement Longitudinal Study (CHARLS, http://charls.pku.edu.cn/zh-CN).