Abstract
Aims
Potentially inappropriate psychotropic medications (PIPMs) prescribed to older adults with psychiatric disorders can inadvertently affect their health. The use of standards and guidelines can ensure prudent prescribing and minimize the risk of morbidities. This study assessed the pattern and prevalence of prescription of PIPMs to older individuals in outpatient psychiatric settings in Saudi Arabia, using the updated 2015 Beers criteria, as well as the probability of polypharmacy.
Methods
The study was conducted in the outpatient psychiatric clinics of the only psychiatric hospital in Jazan region of Saudi Arabia. A retrospective cross-sectional review of electronic medical records was undertaken during 2018 to assess PIPM use and psychotropic polypharmacy. Descriptive statistics were generated and associations between PIPM use and baseline characteristics were assessed using multivariable logistic regression.
Results
Overall, 68% of 1300 older adults received PIPMs, and 77.7% were on psychotropic polypharmacy. Amitriptyline, chlorpromazine, and trifluoperazine were extensively prescribed. Paroxetine (1.2%) and benzodiazepines were prescribed to a smaller proportion of the patients. Elderly with schizophrenia (AOR = 0.046, p < 0.001) and anxiety (AOR = 0.530, p = 0.036) were significantly less likely to have PIPMs than those with dementia. Likewise, elderly with depression and anxiety were less likely to have psychotropic polypharmacy as compared to those with dementia.
Conclusion
A substantial number of the elderly received PIPMs possibly based on implicit criteria. It is therefore important to provide mental health care providers in the region with educational programs to increase their awareness of PIPMs.
Keywords: Psychotropic medications, Elderly, Pharmacist, Polypharmacy, Beers criteria
1. Introduction
The optimal use of prescription medications can improve the quality of patient care. Medications become potentially inappropriate when their harm is substantially more than the benefit (Steinman et al., 2015). The use of such medications in elderly patients increases the likelihood of infirmities, affects their overall performance, raises the risk of emergency department admissions, and increases their dependence on caregivers (Karandikar et al., 2013, Sköldunger et al., 2015, Renom-Guiteras et al., 2018). Moreover, during ageing, a decline in functional capabilities can increase the risk of toxicities (Lavan and Gallagher, 2016). A 30% reduction in the metabolism of some drugs and 50% decrease in renal excretion has been reported in over two-thirds of the population (Klotz, 2009).
To promote effective and safe treatment strategies among elderly, clinicians often rely on tools such as the Beers criteria (Panel et al., 2015) and STOPP criteria (O'Mahony et al., 2015) as there is lack of substantive evidence through clinical trials. The 2015 updated Beers criteria are built on evidence-based information and is an important resource on drugs to be avoided or used cautiously in the elderly to prevent unintended harm. Importantly, the Beers criteria are accepted by the American Geriatrics Society as an invaluable tool providing a list of pharmacotherapeutic agents and drug categories that need to be used with caution or avoided in the elderly (Panel et al., 2015). The Beers criteria emphasize on the risk of using several classes of drugs, which include long-acting benzodiazepines, tricyclic antidepressants, and antimuscarinic medications in the elderly.
In the Kingdom of Saudi Arabia, the prevalence of potentially inappropriate medication to be avoided was high. A study has reported that 43% of the elderly in its sample were prescribed at least one potentially inappropriate medication (Al‐Omar et al., 2013). Furthermore, Alhawassi et al. found that 57.6% of their sample of 4073 older adults were prescribed potentially inappropriate medications (Alhawassi et al., 2019). Potentially inappropriate medication prescriptions in these studies included cardiovascular agents, antiarrhythmics, antidepressants, antipsychotics and benzodiazepines.
Psychiatric morbidities are distinctly manifested in the elderly. They mainly include mood disorders, cognitive impairment, and anxiety. Antidepressants, benzodiazepines, and antipsychotics serve as mainstay psychotropic medications for these disorders. Several weeks of treatment will be required for symptomatic remission which could be accompanied by adverse drug reactions. For example, first-generation antipsychotics (FGAs) cause extrapyramidal effects (Høiberg and Nielsen, 2006), second-generation antipsychotics produce agranulocytosis, and hyperlipidemia (Haddad and Sharma, 2007); hence, their chronic use predisposes the elderly to cardiovascular mortality (Qato et al., 2008). Moreover, about 65% of the elderly experience disequilibrium (Hobeika, 1999, Müjdeci et al., 2012, Lin and Bhattacharyya, 2012, Anson and Jeka, 2016) and the use of inappropriate psychotropic medications augment the risk of fall-related injuries, ultimately impacting their quality of life (Harrison et al., 2018, Bulat and Castle, 2008). Johnell et al. have reported the increased risk of falls with the use of antidepressants (Johnell et al., 2017). Marcum et al. have identified the likelihood of falls among community residing older adults with the use of selective serotonin reuptake inhibitors (SSRIs) to be 1.6 (Marcum et al., 2016), while Du et al. have stated that the likelihood of falls increases six times with the use of SSRIs (Du et al., 2017). In addition, the presence of concurrent diseases requires the simultaneous use of two or more prescription drugs daily (Guaraldo et al., 2011), making them more prone to drug therapy-related problems or leading to exacerbation of adverse drug reactions (Hajjar et al., 2007, Cantlay et al., 2016).
Only a few studies have focused on the use of potentially inappropriate medications in the elderly in the Kingdom of Saudi Arabia. Furthermore, no studies have focused on potentially inappropriate psychotropic medications (PIPMs) in Saudi Arabia. As the elderly are at-risk with the inappropriate use of psychotropic medications, we primarily aimed to assess the pattern of drugs prescribed to older individuals in psychiatric settings. Besides, we also identified the prevalence of PIPMs based on the updated 2015 Beers criteria and determined psychotropic polypharmacy (Panel et al., 2015).
2. Research methods and design
2.1. Study design and setting
This study was a retrospective cross-sectional study conducted by extracting 12-month data from the electronic medical records database.
The health care system in Saudi Arabia encompasses primary, secondary, and tertiary health care hospitals. These health care facilities are government-funded and are accessible to all the citizens and legal residents. Patients with mental health disorders visiting primary health care centers (PHCC) are referred to the psychiatric hospital as PHCC have limited psychiatric health care services (Al Habeeb and Qureshi, 2010, Koenig et al., 2014). Also, tertiary care hospitals only serve as transit paths for patients to the psychiatric hospital. Thus, psychiatric referrals can be from PHCC or general hospitals, as it has a comprehensive setup to provide specialist mental health care services (Al Habeeb and Qureshi, 2010, Koenig et al., 2014). The psychiatric hospital is located on the outskirts of Jazan region catering to the mental health care needs of the residents in the region. The hospital renders consultation, ambulatory, emergency mental health care services, rehabilitation, and substance abuse treatment. A previous study found that 90% of the prescriptions issued from psychiatric outpatient clinics were from this hospital (Meraya et al., 2021). Data were extracted retrospectively from all prescriptions issued from January 2018 to December 2018 in the psychiatric outpatient clinics.
The Institutional Review Board (IRB) of Jazan University reviewed and approved the protocol and all its procedures (IRB No. 6401/1708/1440, dated 04/22/2019).
2.2. Study population
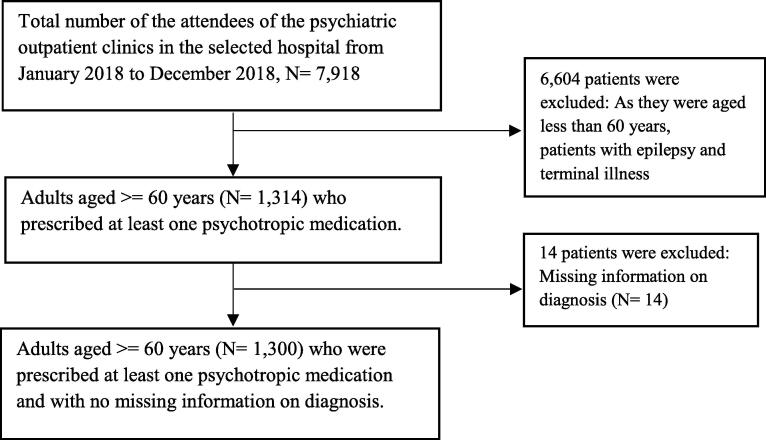
Adults were eligible to be included if their age was ≥60 years, as life transition through retirement takes place at the age of 60 years and above in Saudi Arabia. The total number of attendees to the psychiatric outpatient setting, and the eligibility for inclusion have been depicted in the flow diagram (Fig. 1). Data for ambulatory care patients diagnosed with psychiatric morbidities, based on the International Classifications of Diseases, 10th Revision, Clinical Modification (ICD-10-CM), over 12 months between January and December 2018 were included (Table 1). Older adults seeking treatment for epilepsy or psychiatric patients with terminal illness during the same period were excluded from the study.
Fig. 1.
Selection criteria of patient prescriptions.
Table 1.
Psychiatric morbidities based on the International Classifications of Diseases–10th edition, Clinical Modification (ICD-10-CM).
| Morbidities | ICD-10CM codes |
|---|---|
| Dementia | F00-F09 |
| Schizophrenia | F20-F29 |
| Major depressive disorder | F31.3/F31.5 F32/F33.4 |
| Anxiety | F40/F41.9 |
| Other diagnoses: Substance use | F10-F19 |
| Mood disorders | F30-F31.2, F31.6-F31.9, F34-F39, F44-F44.9 |
| Obsessive-compulsive | F42-F42.9 |
| Stress | F43-F43.9 |
| Other disorders | F45-F69, F99 |
| Mental retardation | F70-F79 |
2.3. Data source and collection
Data were extracted from patients’ electronic medical records by an experienced clinical pharmacist under the guidance of a clinical expert. Psychiatric morbidities were documented using ICD-10-CM, and clinical experts determined prescribing appropriateness after scrutinizing prescription patterns of psychotropic drugs. Medications were adjudged as potentially inappropriate if the psychotropic medication was listed in the 2015 Beers criteria, a recommended guideline of the American Geriatric Society. In addition, the patient’s medication list was also scrutinized to identify psychotropic polypharmacy. We have reviewed all prescriptions received by each patient during 2018. We have identified and counted our outcomes if they were prescribed at least once during 2018.
2.4. Outcome measures
Based on the outpatient data extracted from medical records, (1) the psychotropic medications prescribed were categorized into their therapeutic class as antidepressants, antipsychotics, and antianxiety medications; (2) potentially inappropriate medications in older adults were identified based on the 2015 American Geriatric Society Beers criteria. We emphasized on drugs acting on the central nervous system that have to be avoided in the elderly which include antidepressants alone and in combination (Amitriptyline, amoxapine, clomipramine, desipramine, doxepin, imipramine, nortriptyline, paroxetine, protriptyline, trimipramine), first and second generation antipsychotics (unless the diagnosis was schizophrenia or bipolar), benzodiazepines (short, intermediate and long-acting), meprobamate, nonbenzodiazepines and nonbenzodiazepine receptor agonists (Panel et al., 2015) (3) the use of two or more psychotropic medications from the same therapeutic class or two or more psychotropic medications from different therapeutic classes was defined as polypharmacy (Mojtabai and Olfson, 2010, Tapp et al., 2003, Costa et al., 2017, Kukreja et al., 2013, Meraya, 2020, Meraya et al., 2021).
2.5. Explanatory variables
The explanatory variables were age groups in years, gender, and diagnosed psychiatric disorder identified using ICD-10-CM.
2.6. Statistical analysis
Data were entered into Microsoft Excel and analyzed using Stata 15.1 software (Stata Corp LP, College Station, USA). The categorical variables were represented as frequencies and percentages. We conducted analysis of PPIM in total and assessed polypharmacy in the study sample. Multivariable logistic regressions were carried out to assess the relationship between explanatory variables and the outcome measures. Adjusted models included gender, age, and psychiatric diagnoses. A p-value of <0.05 was considered statistically significant. In all analyses, we used adults with dementia as the reference group, because dementia is a highly disabling disease and often coexist with chronic mental and physical conditions that require multiple treatments (Bhattacharjee et al., 2019, Prince et al., 2014).
3. Results
The review of older adults’ information in the electronic medical records identified 1300 elderly patients, based on fulfillment of our inclusion/exclusion criteria. Of these patients, 58.6% were females and 41.4% were males. Over three-fourths of the elderly were aged less than 75 years, and the remaining one-fourth were over 75 years. Major depressive disorder was diagnosed in 44.2% of the elderly, 21.7% had schizophrenia, 19.6% had anxiety, 9.2% had dementia, and a small proportion were affected with other disorders, which included mood disorders, obsessive–compulsive disorders, and stress-related ailments (Table 2).
Table 2.
Baseline characteristics of elderly patients attending psychiatric setting.
| Characteristics | Total (N = 1300) N (%) |
|---|---|
| Sex | |
| Female | 768 (58.6) |
| Male | 543 (41.4) |
| Age (years) | |
| ≤75 | 961 (76.3) |
| ≥75 | 850 (26.7) |
| Primary psychiatric conditions (ICD-10-CM) | |
| Dementia | 120 (9.2) |
| Schizophrenia | 284 (21.8) |
| Depression | 575 (44.2) |
| Anxiety | 255 (19.6) |
| Other diagnosis | 66 (5.1) |
| Potentially inappropriate medications | |
| Yes | 892 (68.0) |
| No | 419 (32.0) |
| Polypharmacy | |
| Yes | 1019 (77.7) |
| No | 292 (22.3) |
In the elderly receiving psychotropic medications, an overall 68.0% were prescribed PIPMs, and 77.7% were on polypharmacy. Among the psychotropic medications prescribed, tricyclic agents were given to 40.9% of the elderly patients, while tetracyclic agents like maprotiline were prescribed to 3.1%. Only 1.2% of the older adults received paroxetine (Table 3). Second-generation antipsychotics widely prescribed were olanzapine (7.6%) and quetiapine (7.3%), while relatively fewer adults received aripiprazole (2.4%) and clozapine (0.2%). FGAs commonly used were chlorpromazine (15%), trifluoperazine (14.3%), and haloperidol (6.3%). Among sedatives, lorazepam was prescribed to 2.6% of the patients and diazepam was prescribed to 0.2% (Table 3).
Table 3.
Potentially inappropriate medications in older adults attending psychiatric setting using Beers criteria, (N = 1300).
| Medication prescribed | Frequency (%) |
|
|---|---|---|
| Yes | No | |
| Tricyclic antidepressants | ||
| Clomipramine | 13 (1.0) | 1296 (99.0) |
| Imipramine | 33 (2.5) | 1276 (97.5) |
| Amitriptyline | 489 (37.4) | 820 (62.6) |
| Tetracyclic antidepressants | ||
| Maprotiline | 40 (3.1) | 1269 (96.9) |
| Selective serotonin reuptake inhibitors | ||
| Paroxetine | 16 (1.2) | 1293 (98.8) |
| First generation antipsychotics | ||
| Chlorpromazine | 196 (15.0) | 1113 (85.0) |
| Trifluperazine | 187 (14.3) | 1122 (85.7) |
| Haloperidol | 83 (6.3) | 1226 (93.7) |
| Fluphenazine | 5 (0.4) | 1304 (99.6) |
| Flupentixol | 1 (0.1) | 1308 (99.9) |
| Second generation antipsychotics | ||
| Risperidone | 144 (11.0) | 1165 (89.0) |
| Olanzapine | 99 (7.6) | 1210 (92.4) |
| Quetiapine | 96 (7.3) | 1213 (92.7) |
| Sulpiride | 61 (4.7) | 1248 (95.3) |
| Aripiprazole | 32 (2.4) | 1277 (97.6) |
| Amisulpiride | 15 (1.1) | 1294 (98.9) |
| Palperidone | 14 (1.1) | 1295 (98.9) |
| Clozapine | 3 (0.2) | 1306 (99.8) |
| Benzodiazepines | ||
| Lorazepam | 34 (2.6) | 1275 (97.4) |
| Clonazepam | 17 (1.3) | 1292 (98.7) |
| Alprozolam | 19 (1.5) | 1290 (98.5) |
| Diazepam | 3 (0.2) | 1306 (99.8) |
| Nonbenzodiazepine | ||
| Zolpidem | 16 (1.2) | 1293 (98.8) |
| Barbiturates | ||
| Barbitone | 6 (0.5) | 1305 (99.5) |
In the multivariable logistic regression analysis, males (OR = 0.952 [0.712–1.27], p = 0.745) and the elderly above 75 years of age (OR = 0.881 [0.638–1.217], p = 0.445) were less likely to be prescribed a PIPM; however, this was not a statistically significant. In the comparison of diagnoses, the likelihood of the elderly receiving a PIPM for anxiety was one-half times greater than for dementia (OR = 0.530 [0.292–0.959], p = 0.036) and it was statistically significant. Elderly patients aged above 75 years were less likely to be on psychotropic polypharmacy (OR = 0.729 [0.539–0.986], p = 0.04) than those aged less than 75 years. Also, there was a significantly lesser likelihood of the elderly diagnosed with depression (0.415 [0.236–0.73], p = 0.002) and anxiety (0.397 [0.219–0.722], p = 0.002) receiving psychotropic polypharmacy than their counterparts with dementia (Table 4).
Table 4.
Adjusted Odds Ratio (AORs) and 95% Confidence Intervals (CIs) for the explanatory variables using logistic regression on potentially inappropriate psychotropic medications and psychotropic polypharmacy.
| Potentially inappropriate psychotropic medications | ||
|---|---|---|
| Variable | AOR [95% CI] | p-value |
| Gender | ||
| Females | 1 (reference) | |
| Males | 0.952 [0.712–1.27] | 0.745 |
| Age groups | ||
| <75 | 1 (reference) | |
| ≥75 | 0.881 [0.638–1.217] | 0.445 |
| Diagnosis | ||
| Dementia | 1 (reference) | |
| Schizophrenia | 0.046 [0.0257–0.085] | <0.001 |
| Depression | 0.809 [0.460–1.424] | 0.463 |
| Anxiety | 0.530 [0.292–0.959] | 0.036 |
| Other diagnoses | 0.614 [0.278–1.355] | 0.228 |
| Psychotropic polypharmacy | ||
| Variable | AOR [95% CI] | p-value |
| Gender | ||
| Females | 1 (reference) | |
| Males | 1.049 [0.792–1.389] | 0.741 |
| Age group | ||
| <75 | 1 (reference) | |
| >75 | 0.729 [0.539–0.986] | 0.04 |
| Diagnosis | ||
| Dementia | 1 (reference) | |
| Schizophrenia | 0.839 [0.447–1.575] | 0.586 |
| Depression | 0.415 [0.236–0.73] | 0.002 |
| Anxiety | 0.397 [0.219–0.722] | 0.002 |
| Other diagnoses | 0.635 [0.278–1.449] | 0.281 |
4. Discussion
This study identified the use of drugs-to-avoid based on the 2015 updated Beers criteria, and polypharmacy in older psychiatric hospital attendees.
Geriatric depression was identified as the prominent psychiatric disorder in our study population. The World Health Organization reports that depression contributes significantly to the non-fatal loss of health (Organization, 2002). We found only 1.2% of the elderly mentally ill patients prescribed with paroxetine, a first-line SSRI. Our finding concurs with the report of Alosaimi et al. that 1.8% inpatients and 4% outpatients in Saudi Arabia were prescribed paroxetine (Alosaimi et al., 2016). However, the prescription pattern in our setting contrasts with the findings of Bhattacharjee et al. reporting the extensive use of paroxetine (Bhattacharjee et al., 2019). Also, in the United Kingdom and Canada, SSRIs have been used as starting therapy to an extent of 71.4% and 55.2%, respectively. (Tamblyn et al., 2019). We perceive that the prescribers discretion and the patient characteristics could have influenced this differential prescribing pattern.
TCAs are generally unfavorable for the management of major depressive disorders owing to their safety profile. Over 37% of the patients in our study were prescribed amitriptyline, whereas imipramine and clomipramine were prescribed to a lesser extent. The use of amitriptyline in older adults in our study is relatively similar to what have been reported in previous studies. Amitriptyline was prescribed to 41.9% of elderly patients in Brazil, with potentially inappropriate use seen in 31.1% (Fulone and Lopes, 2017). Vicente et al. reported that 34.7% of elderly patients received amitriptyline (Vicente et al., 2015) and Li et al. reported that 15.2% elderly patients were prescribed with TCA (Li et al., 2019). The preference for amitriptyline may be due its effectiveness, long half-life (Kerr et al., 2014), lower cost, and adjustable dosing pattern. However, it is important to emphasize that TCAs can cause pronounced anticholinergic action adding to the perils of the elderly (Gillman, 2007).
Antipsychotics are the third most commonly prescribed psychotropic medication in the elderly (Al Odhayani et al., 2017). In this study, risperidone (11%), olanzapine (7.6%), quetiapine (7.3%), and sulpiride (4.7%) were frequently prescribed for older adults. Second-generation agents have a lesser propensity to cause adverse drug reactions over the first-generation agents. Moreover, we found that the elderly diagnosed with schizophrenia were less likely to receive a PPIM which could minimize their risk of cerebrovascular complications (McKean and Monasterio, 2015), and extrapyramidal symptoms.
Benzodiazepines are not usually recommended in the elderly as they increase the risk of dementia (Takada et al., 2016) and falls (Markota et al., 2016). Incidentally, the use of benzodiazepine and nonbenzodiazepine-receptor agonists like zolpidem were low in our study sample. Also, elderly patients diagnosed with anxiety had a one-half chance of receiving a PIPM compared with dementia. We perceive this to be prudent prescribing as benzodiazepines and nonbenzodiazepine-receptor agonists are to be avoided as per the 2015 Beers criteria owing to their strong sedative effects (Markota et al., 2016). Besides, our findings concur with the results of another Korean study, wherein the use of benzodiazepines in the elderly ranged from 8.7 to 31.9% (Hwang et al., 2017). However, our findings differ from the prescribing pattern elsewhere, wherein the extraordinary use benzodiazepines in older adults has been reported (Steinman et al., 2017, Oktora et al., 2020).
Overall, mentally ill elderly patients were exposed to the risk of receiving a PPIM. The use of specific categories of medications such as tricyclic antidepressants over safer variants such as SSRIs in the elderly might be attributed to the prescribers’ targeting more than one disorder, for example, amitriptyline for depression and insomnia; better symptomatic remission observed in the treated; better tolerability owing to the presence of pharmacogenetic variants; short supply of other drugs, budgetary constraints; public funding of health care, including medicines, making cost criteria important.
The strengths of this study include the collection of information from the only accredited psychiatric hospital in the Jazan region for a sufficiently long period to assess any inappropriate use. A previous study found that 90% of the prescriptions issued from psychiatric outpatient clinics were from this hospital (Meraya et al., 2021). However, our limitations include the use of a retrospective design, which can introduce bias into the findings, as it was not possible to ensure that all the information was available, particularly on the behavior of ambulatory patients. Also, we did not measure and control for other comorbid chronic physical conditions that may affect the psychotropic prescribing patterns. Lastly, we focused on psychotropic polypharmacy but did not consider medications used for comorbidities such as diabetes and hypertension, as they might influence psychotropic prescribing patterns.
5. Conclusion
In the current setting, we identified the use of potentially inappropriate psychotropic medications in elderly patients as well as psychotropic polypharmacy. The risk associated with the use of PIPM in the elderly could be immense due to age-associated changes. Hence, it will be necessary to provide additional medication therapy management practices, involve pharmacists with psychiatric credentialing, sensitize prescribers, and educate patients. Also, instituting educational programs for mental health care providers in the region and providing decision support tools could be of significant benefit.
Financial disclosures
None declared.
Ethical approval
This study was approved by the institutional human research ethics committee IRB No. 6401/1708/1440) dated 22/04/2019).
Ethical approval
Information was collected from electronic medical records after human research ethics committee.
Authors contribution
Both the authors contributed towards the design, analysis, drafting, and critically appraising the article and approve with the final version of the manuscript.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
References
- Al-Omar H.A., Al-Sultan M.S., Abu-Auda H.S. Prescribing of potentially inappropriate medications among the elderly population in an ambulatory care setting in a Saudi military hospital: trend and cost. Geriatr. Gerontol. Int. 2013;13:616–621. doi: 10.1111/j.1447-0594.2012.00951.x. [DOI] [PubMed] [Google Scholar]
- Al Habeeb, A., Qureshi, N. 2010. Mental and social health atlas I in Saudi Arabia: 2007-08. EMHJ-Eastern Mediterranean Health J., 16 (5), 570–577, 2010. [PubMed]
- Al Odhayani, A., Tourkmani, A., alshehri, M., Alqahtani, H., Mishriky, A. 2017. Potentially inappropriate medications prescribed for elderly patients through family physicians. Saudi J. Biol. Sci., 24, 200–207. [DOI] [PMC free article] [PubMed]
- Alhawassi T.M., Alatawi W., Alwhaibi M. Prevalence of potentially inappropriate medications use among older adults and risk factors using the 2015 American Geriatrics Society Beers criteria. BMC Geriatr. 2019;19:154. doi: 10.1186/s12877-019-1168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alosaimi F.D., Alhabbad A., Abalhassan M.F., Fallata E.O., Alzain N.M., Alassiry M.Z., Haddad B.A. Patterns of psychotropic medication use in inpatient and outpatient psychiatric settings in Saudi Arabia. Neuropsychiatr. Dis. Treat. 2016;12:897. doi: 10.2147/NDT.S100405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anson E., Jeka J. Perspectives on aging vestibular function. Front. Neurol. 2016;6:269. doi: 10.3389/fneur.2015.00269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharjee S., Lee J.K., Patanwala A.E., Vadiei N., Malone D.C., Knapp S.M., Lo-Ciganic W.-H., Burke W.J. Extent and predictors of potentially inappropriate antidepressant use among older adults with dementia and major depressive disorder. Am. J. Geriatr. Psych. 2019;27:794–805. doi: 10.1016/j.jagp.2019.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulat T., Castle S.C. Clinical practice algorithms: medication management to reduce fall risk in the elderly-Part 2, summary algorithm. J. Am. Associat. Nurse Practition. 2008;20:1. doi: 10.1111/j.1745-7599.2007.00272.x. [DOI] [PubMed] [Google Scholar]
- Cantlay A., Glyn T., Barton N. Polypharmacy in the elderly. InnovAiT. 2016;9:69–77. [Google Scholar]
- Costa J.D.O., Ceccato M.D.G.B., Melo A.P.S., Acurcio F.D.A., Guimarães M.D.C. Gender differences and psychotropic polypharmacy in psychiatric patients in Brazil: a cross-sectional analysis of the PESSOAS Project. Cadernos de Saúde Pública. 2017;33 doi: 10.1590/0102-311X00168915. [DOI] [PubMed] [Google Scholar]
- Du Y., Wolf I.-K., Knopf H. Association of psychotropic drug use with falls among older adults in Germany. Results of the German Health Interview and Examination Survey for Adults 2008–2011 (DEGS1) PLoS One. 2017;12 doi: 10.1371/journal.pone.0182432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulone I., Lopes L.C. Potentially inappropriate prescriptions for elderly people taking antidepressant: comparative tools. BMC Geriatr. 2017;17:278. doi: 10.1186/s12877-017-0674-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillman, P. 2007. Tricyclic antidepressant pharmacology and therapeutic drug interactions updated. Brit. J. Pharmacol., 151, 737–748. [DOI] [PMC free article] [PubMed]
- Guaraldo L., Cano F.G., Damasceno G.S., Rozenfeld S. Inappropriate medication use among the elderly: a systematic review of administrative databases. BMC Geriatr. 2011;11:79. doi: 10.1186/1471-2318-11-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddad P.M., Sharma S.G. Adverse effects of atypical antipsychotics. CNS Drugs. 2007;21:911–936. doi: 10.2165/00023210-200721110-00004. [DOI] [PubMed] [Google Scholar]
- Hajjar E.R., Cafiero A.C., Hanlon J.T. Polypharmacy in elderly patients. Am. J. Geriatr. Pharmacother. 2007;5:345–351. doi: 10.1016/j.amjopharm.2007.12.002. [DOI] [PubMed] [Google Scholar]
- Harrison S.L., Bradley C., Milte R., Liu E., O’Donnell L.K., Hilmer S.N., Crotty M. Psychotropic medications in older people in residential care facilities and associations with quality of life: a cross-sectional study. BMC Geriatr. 2018;18:60. doi: 10.1186/s12877-018-0752-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobeika, C.P. 1999. Equilibrium and balance in the elderly. Ear Nose Throat J., 78, 558–566. [PubMed]
- Høiberg M., Nielsen B. Antipsychotic treatment and extrapyramidal symptoms amongst schizophrenic inpatients. Nord. J. Psychiatry. 2006;60:207–212. doi: 10.1080/08039480600636296. [DOI] [PubMed] [Google Scholar]
- Hwang S.-H., Han S., Choi H., Park C., Kim S.M., Kim T.H. Trends in the prescription of benzodiazepines for the elderly in Korea. BMC Psych. 2017;17:303. doi: 10.1186/s12888-017-1467-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnell, K., Jonasdottir Bergman, G., Fastbom, J., Danielsson, B., Borg, N., Salmi, P. 2017. Psychotropic drugs and the risk of fall injuries, hospitalisations and mortality among older adults. Int. J. Geriatr. Psych., 32, 414–420. [DOI] [PMC free article] [PubMed]
- Karandikar Y., Chaudhari S., Dalal N., Sharma M., Pandit V. Inappropriate prescribing in the elderly: a comparison of two validated screening tools. J. Clin. Gerontol. Geriatr. 2013;4:109–114. [Google Scholar]
- Kerr G., Aujero M., Richards J., Sayles H., Davis L., Cannon G., Caplan L., Michaud K., Mikuls T. Associations of hydroxychloroquine use with lipid profiles in rheumatoid arthritis: pharmacologic implications. Arthr. Care Res. 2014;66:1619–1626. doi: 10.1002/acr.22341. [DOI] [PubMed] [Google Scholar]
- Pharmacokinetics and drug metabolism in the elderly. Drug Metabol. Rev., 41, 67–76. [DOI] [PubMed]
- Koenig, H.G., Al Zaben, F., Sehlo, M.G., Khalifa, D.A., Al Ahwal, M.S., Qureshi, N.A., Al-Habeeb, A.A. 2014. Mental health care in Saudi Arabia: Past, present and future. Open J. Psych., 4, 113.
- Kukreja S., Kalra G., Shah N., Shrivastava A. Polypharmacy in psychiatry: a review. Mens Sana Monographs. 2013;11:82. doi: 10.4103/0973-1229.104497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavan A.H., Gallagher P. Predicting risk of adverse drug reactions in older adults. Therapeutic Adv. Drug Saf. 2016;7:11–22. doi: 10.1177/2042098615615472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li G., Andrews H.F., Chihuri S., Lang B.H., Leu C.S., Merle D.P., Gordon A., Mielenz T.J., Strogatz D., Eby D.W. Prevalence of potentially inappropriate medication use in older drivers. BMC Geriatr. 2019;19:260. doi: 10.1186/s12877-019-1287-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H.W., Bhattacharyya N. Balance disorders in the elderly: epidemiology and functional impact. The Laryngoscope. 2012;122:1858–1861. doi: 10.1002/lary.23376. [DOI] [PubMed] [Google Scholar]
- Marcum Z.A., Perera S., Thorpe J.M., Switzer G.E., Castle N.G., Strotmeyer E.S., Simonsick E.M., Ayonayon H.N., Phillips C.L., Rubin S. Antidepressant use and recurrent falls in community-dwelling older adults: findings from the Health ABC Study. Ann. Pharmacother. 2016;50:525–533. doi: 10.1177/1060028016644466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markota M., Rummans T.A., Bostwick J.M., Lapid M.I. Benzodiazepine use in older adults: dangers, management, and alternative therapies. Mayo Clin. Proc. 2016;Elsevier:1632–1639. doi: 10.1016/j.mayocp.2016.07.024. [DOI] [PubMed] [Google Scholar]
- McKean A., Monasterio E. Taylor & Francis; 2015. Indications of Atypical Antipsychotics in the Elderly. [DOI] [PubMed] [Google Scholar]
- Meraya, 2020. Psychiatric diagnoses and prescribing patterns of psychotropic polypharmacy among children and adolescents in the Jazan Region, Saudi Arabia. Psych. Clin. Psychopharmacol., 30, 24–30.
- Meraya A.M., Alwhaibi M., Syed M.H., Shwihi A., Mashraqi M., Tripathi R., Buayti Y., Moraya D. Utilization of psychotropic medications and polypharmacy among adults in Jazan Region, Saudi Arabia. Indonesian J. Pharm. 2021;3:205–216. [Google Scholar]
- Mojtabai R., Olfson M. National trends in psychotropic medication polypharmacy in office-based psychiatry. Arch. Gen. Psych. 2010;67:26–36. doi: 10.1001/archgenpsychiatry.2009.175. [DOI] [PubMed] [Google Scholar]
- Müjdeci B., Aksoy S., Atas A. Evaluation of balance in fallers and non-fallers elderly. Brazil. J. Otorhinolaryngol. 2012;78:104–109. doi: 10.5935/1808-8694.20120016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Mahony D., O'Sullivan D., Byrne S., O'Connor M.N., Ryan C., Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44:213–218. doi: 10.1093/ageing/afu145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oktora M.P., Alfian S.D., Bos H.J., Schuiling-Veninga C.C.M., Taxis K., Hak E., Denig P. Trends in polypharmacy and potentially inappropriate medication (PIM) in older and middle-aged people treated for diabetes. British J. Clin. Pharmacol. 2020 doi: 10.1111/bcp.14685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization, W.H. 2002. Proposed working definition of an older person in Africa for the MDS Project. World Health Organization, Geneva.
- Panel, A.G.S.B.C.U.E., Fick, D.M., Semla, T.P., Beizer, J., Brandt, N., Dombrowski, R., Dubeau, C.E., Eisenberg, W., Epplin, J.J., Flanagan, N. 2015. American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J. Am. Geriatr. Soc., 63, 2227–2246. [DOI] [PubMed]
- Prince M., Albanese E., Guerchet M., Prina M. Dementia and risk reduction: an analysis of protective and modifiable factors. World Alzheimer Report. 2014:66–83. [Google Scholar]
- Qato D.M., Alexander G.C., Conti R.M., Johnson M., Schumm P., Lindau S.T. Use of prescription and over-the-counter medications and dietary supplements among older adults in the United States. JAMA. 2008;300:2867–2878. doi: 10.1001/jama.2008.892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renom-Guiteras, A., Thürmann, P.A., Miralles, R., Klaaßen-Mielke, R., Thiem, U., Stephan, A., Bleijlevens, M.H., Jolley, D., Leino-Kilpi, H., Rahm Hallberg, I. 2018. Potentially inappropriate medication among people with dementia in eight European countries. Age Ageing, 47, 68–74. [DOI] [PubMed]
- Sköldunger A., Fastbom J., Wimo A., Fratiglioni L., Johnell K. Impact of inappropriate drug use on hospitalizations, mortality, and costs in older persons and persons with dementia: findings from the SNAC study. Drugs Aging. 2015;32:671–678. doi: 10.1007/s40266-015-0287-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman M.A., Beizer J.L., Dubeau C.E., Laird R.D., Lundebjerg N.E., Mulhausen P. How to use the American Geriatrics Society 2015 Beers Criteria—a guide for patients, clinicians, health systems, and payors. J. Am. Geriatr. Soc. 2015;63:e1–e7. doi: 10.1111/jgs.13701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman M.A., Low M., Balicer R.D., Shadmi E. Epidemic use of benzodiazepines among older adults in Israel: epidemiology and leverage points for improvement. J. Gen. Intern. Med. 2017;32:891–899. doi: 10.1007/s11606-017-4059-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takada M., Fujimoto M., Hosomi K. Association between benzodiazepine use and dementia: data mining of different medical databases. Int. J. Med. Sci. 2016;13:825. doi: 10.7150/ijms.16185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamblyn R., Bates D.W., Buckeridge D.L., Dixon W., Forster A.J., Girard N., Haas J., Habib B., Kurteva S., Li J. Multinational comparison of new antidepressant use in older adults: a cohort study. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-027663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tapp A., Wood A.E., Secrest L., Erdmann J., Cubberley L., Kilzieh N. Combination antipsychotic therapy in clinical practice. Psych. Services. 2003;54:55–59. doi: 10.1176/appi.ps.54.1.55. [DOI] [PubMed] [Google Scholar]
- Vicente, A.R.T., Castro-Costa, É., Diniz, B.S., Firmo, J.O.A., Lima-Costa, M.F., Loyola Filho, A.I.D. 2015. Antidepressant use and associated factors among the elderly: the Bambuí Project. Ciencia saude coletiva, 20, 3797–3804. [DOI] [PubMed]