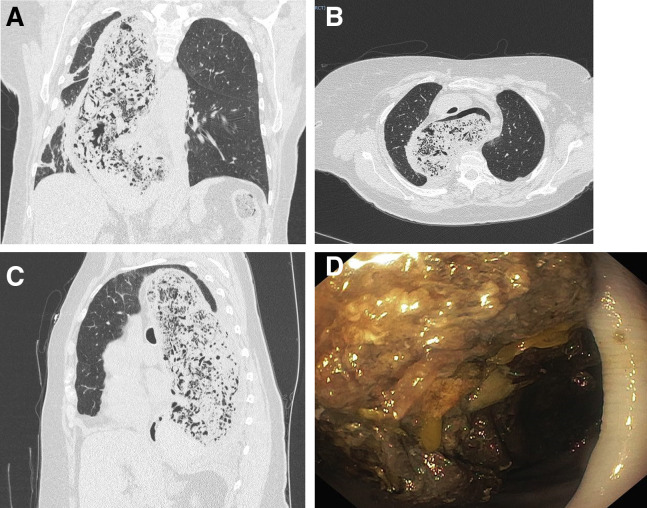
Question: A 75-year old woman presented to the emergency department with a history of epigastric discomfort and rapidly worsening thoracic pain. She had no fever or cough. On physical examination, she appeared overweight (102 kg, height 162 cm). Laboratory examination revealed normal cardiac troponin levels and slight increase in inflammatory markers (C-reactive protein and neutrophil-lymphocyte ratio). As a nasal screening swab was positive for coronavirus 2019 (COVID-19) infection, she was transferred to the COVID isolation ward. A subsequent computed tomography scan of the chest showed no interstitial lung disease. However, the presence of a monstrous esophageal dilatation with sigmoid shape and dislodgment of the surrounding structures was seen. The esophagus appeared full of solid content compatible with accumulated undigested food residues (Figure A–C).
The patient was then referred to our gastroenterology unit. Upper endoscopy was performed under general anesthesia with endotracheal intubation. Endoscopic esophageal findings are shown in Figure D.
What is the most likely diagnosis and how should it be managed?
Look on page 1112 for the answer and see the Gastroenterology web site ( www.gastrojournal.org ) for more information on submitting your favorite image to Clinical Challenges and Images in GI.
Answer to: Image 1 (Page 1111): Type II Achalasia
The patient was suffering from type II achalasia, which was refractory to previous endoscopic and surgical treatment. In detail, she had undergone three endoscopic pneumatic dilation sessions in 2005 and ultimately laparoscopic Heller-Dor myotomy in 2015. In 2018, an esophageal high-resolution manometry was unsuccessful, probably because the catheter did not reach the stomach in the sigmoid dilated esophagus.
We treated our patient with prolonged fasting and nasoesophageal tube placement at 35 cm from the incisors teeth. Multiple daily irrigations with saline solution were performed without apparent benefit. Three endoscopic sessions were then performed to clean the entire esophagus from the huge amount of feces-like food residues.
We believe that 2 reasons were behind this ominous presentation. First, the patient suffered from poorly controlled hypothyroidism for which she was taking levothyroxine per os. Laboratory examination revealed high levels of thyrotropin (103 μU/mL) and low levels of free thyroxine (<2.5 pg/mL) and free tri-iodothyronine (1.5 pg/mL). Her severe hypothyroidism was probably due to the inability of oral levothyroxine to reach the stomach, thus decreasing the subjective awareness of her own clinical condition. Second, she was edentulous and this affected the chewing phase, favoring episodes of food impaction and accumulation of food in the esophagus. Surprisingly, she did not experience weight loss and her general nutritional status was good.
Achalasia is an uncommon esophageal motility disorder, usually characterized by dysphagia to solids and liquids, chest pain, regurgitation, and weight loss. High-resolution esophageal manometry is the gold standard test for the diagnosis. Diagnostic findings include distal esophageal aperistalsis and integrated relaxation pressure of >15 mm Hg. Achalasia is classified as type 1 classic, type 2 compartmentalized high pressure in esophageal body, and type 3 spastic.1
In the last few years, peroral endoscopic myotomy is the most frequent endoscopic intervention for achalasia leading to outcomes that are comparable with those of laparoscopic Heller myotomy. Additional interventions are represented by pneumatic dilation and botulinum toxin injection. Esophagectomy is the last option to manage end-stage achalasia.2 , 3
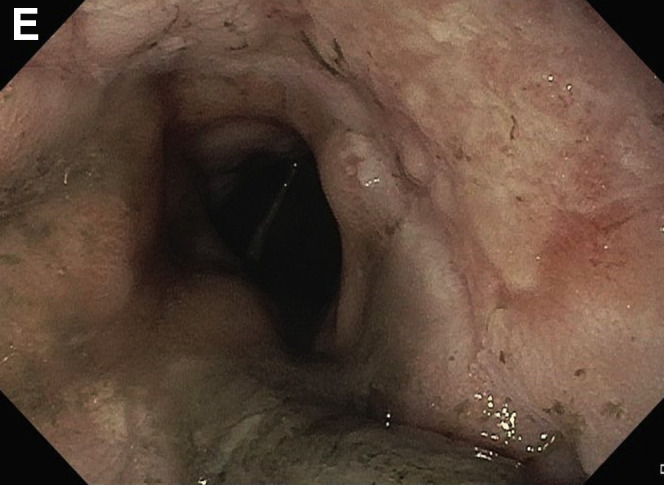
Peroral endoscopic myotomy was not considered for our patient because of the patent cardia (Figure E), the lack of manometric data, and the poor expected outcome in sigmoid esophagus. She was referred to the endocrinologist for further therapeutic workup. Moreover, dental prosthesis implantation was recommended.
Bilal Hameed, Uma Mahadevan, and Kay Washington, Section Editors
Footnotes
Conflicts of interest The authors disclose no conflicts.
For submission instructions, please see theGastroenterologyweb site(www.gastrojournal.org).
References
- 1.Weusten B.L.A.M., Barret M., Bredenoord A.J. Endoscopic management of gastrointestinal motility disorders - part 1: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020;52:498–515. doi: 10.1055/a-1160-5549. [DOI] [PubMed] [Google Scholar]
- 2.Familiari P., Greco S., Volkanovska A. Achalasia: current treatment options. Expert Rev Gastroenterol Hepatol. 2015;9:1101–1114. doi: 10.1586/17474124.2015.1052407. [DOI] [PubMed] [Google Scholar]
- 3.Hammad A., Lu V.F., Dahiya D.S. Treatment challenges of sigmoid-shaped esophagus and severe achalasia. Ann Med Surg (Lond) 2020;61:30–34. doi: 10.1016/j.amsu.2020.11.077. [DOI] [PMC free article] [PubMed] [Google Scholar]