Abstract
Coronavirus disease 2019 (COVID-19) pandemic is still a world-class challenge. Inflammation, especially its severe form with excess release of pro-inflammatory cytokines (cytokine storm) which is a life-threatening condition, is among the most important suspects involved in COVID-19 pathogenesis. It has been shown that cytokine storm could cause notable morbidities such as acute respiratory distress syndrome (ARDS) which leads to hypoxia which is significantly associated with mortality of patients with COVID-19. Hypoxia-inducible factor 1α (HIF-1α) which activates following ARDS-induced hypoxia plays a crucial role in pathogenesis of cytokine storm. The expression of tumor necrosis factor α (TNF-α), interleukin 1 β (IL-1β), and IL-6 which are key elements of cytokine storm are by nuclear factor κβ (NFκB). Interestingly, during the hypoxia, HIF-1α activates NFκB to induce expression of pro-angiogenic and pro-inflammatory factors. These released factors starts a autocrine/paracrine loop and causes deterioration of their etiological pathways of expression: cytokine storm and ARDS. To sum up, it seems HIF-1α is an important target to hit to ameliorate the mentioned pathways. Herein, we suggest perfluorocarbons (PFCs) which are among the organofluorine compounds as a possible co-treatment to reduce hypoxemia and then hypoxia. These substances are known for their high gas solving potential that make them able to be used as a synthetic artificial blood product. Due to the potential of PFCs to affect the fountain of important physiopathological pathway such as inflammation a hypoxia through affecting NFκB, they could be considered as multi-target co-treatment for ARD individuals with COVID-19. It is highly suggested to evaluate this hypothesis in following researches.
Keywords: HIF-1α, Perfluorocarbon, Hypoxia, Inflammation, Cytokine storm
Introduction
After more than a year from late 2019, coronavirus disease 2019 (COVID-19) which started a pandemic in Wuhan, Hubei, China is a global health emergency [1] Other than the main and first virus variant identified from China, so far, different variants of SARS-CoV-2 such as the UK one has been identified which has caused a surge in UK [2]. Since further variants may be more invasive than common ones, focusing on potential COVID-19 treatments are still required. COVID-19 has different signs and symptoms in the patients, however, the most common of them is pneumonia [3] In cases with more disease severity, pneumonia will turn to acute respiratory distress syndrome (ARDS) which is a critical condition and patients mostly need critical care [4, 5]. In the patients who are critically ill, different findings such as septic shock [6] and (multi-)organ failure [7] are common which of their causes/consequences could be hypoxia and/or hypoxemia [8, 9]. It is worth mentioning that acute inflammation of the lung, as the main affected organ and the consequent hypoxia that occurred following the inflammation, causes threatening conditions for patients [10–12]. Therefore, getting aid from treatments such as anti-inflammatory agents to reduce the inflammation in a patient with severe COVID-19 seems to be beneficial [3]. Unfortunately, despite the availability of a large number of anti-inflammatory drugs, we cannot merely rely on them to fully control the inflammatory response in the majority of COVID-19 patients. That is why we need to increase our knowledge about the causes of inflammation in COVID-19 and find more effective ways in order to manage the condition.
Hypothesis
COVID-19 has been known to be associated with inflammation and inflammatory reactions which in the lungs could cause hypoxia, and hypoxia could exacerbate the inflammation. Herein, we hypothesize using perfluorocarbon (PFC) along with other anti-inflammatory treatments to restrict the inflammation and prevent organ dysfunction/failure.
Evaluation of hypothesis
Although the inflammatory response has an essential role in protecting cells and tissues against infection, in some cases with COVID-19 over-reaction of the immune system to the inflammation which has been known as cytokine storm could be a destructive response [3, 13, 14] [7, 8]. Studies have shown that in addition to direct viral infection, uncontrolled inflammation and cytokine storm contribute to disease severity during infection. Inflammation is provided with a profound cytokine response in the body and increased levels of inflammatory mediators. Pro-inflammatory cytokines are produced by innate and acquired immune cell involvement after viral infection to remove viruses in the host [15]. As mentioned, in the SARS-CoV-2 infection, severe inflammatory response to the disease especially in the lung tissues might lead to a critical condition for patients [11]. Thus, decreasing the level of inflammatory cytokines produced by inflammatory cells (especially macrophages and neutrophils) in the lung is vital for reducing the injury, and therefore, increase the possibility of patient’s survival rate.
According to previous studies, in the inflamed tissue/organ, the site usually becomes notably hypoxic [10, 12]. Other than inflammation-induced hypoxia, the inflammatory response through severe pneumonia following SARS-CoV-2 infection which could characterize ARDS, might lead to alveolar edema, decreased lung capacity, and eventually, hypoxemia which induces other organs hypoxia [15, 16]. Just as inflammation causes hypoxia in damaged lung tissues due to inflammatory response, hypoxia provides a situation to produce more inflammatory cytokines by immune cells at the same site [15]. This could be correlated with hypoxia-inducible factor 1α (HIF-1α) expression, a critical factor that is activated in hypoxic conditions. HIF-1 is a conserved heterodimer transcription factor that is regulated through the availability and concentration of oxygen [17, 18]. Thus, the expression of HIF-1α at the site of inflammation regulated as a response to inflammation-hypoxia.
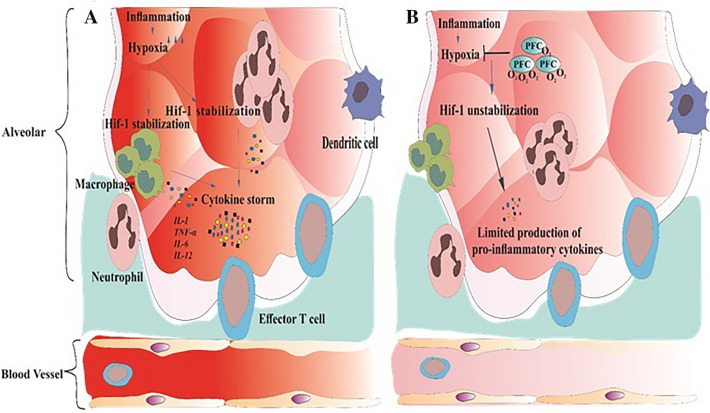
Macrophages and neutrophils as important phagocytic cells which exist in the tissues play a crucial role in the innate immune response against different pathogens such as viruses [9]. Under normal concentration and saturation of oxygen, they express low levels of HIF-1α, but on the other hand, when oxygen demand and/or supply in interrupted HIF-1α expression starts to increase [15]. The transcriptional activity of HIF-1α includes increasing cell survival of as well as stimulating the expression of angiogenic factors such as VEGF as well as pro-inflammatory cytokines (e.g., interleukin 1 β or IL-1β, IL-6, IL-12, and tumor necrosis factor-α) at the site of infection-induced inflammation [19–23]. This increase in the levels of pro-inflammatory cytokines as well as previous levels could lead to deterioration and/or the initiation of cytokine storm which is a serious risk factor for disease severity (Fig. 1a) [3]. Taken together, the processes mentioned above can lead to ARDS and the patient’s death following COVID-19 infection. Moreover, the increased pro-angiogenic factors could induce pathologic angiogenesis which has been seen in the autopsies of patients with COVID-19. Ackerman et al. have found that intussusceptive angiogenesis is a pathologic finding in the COVID-19 patients with ARDS [24, 25].
Fig. 1.
Destabilizing of HIF-1α through PFC administration. a During of infection with coronavirus, the high expression of angiogenic factors such as VEGF as well as pro-inflammatory cytokines (e.g., interleukin 1 β or IL-1β, IL-6, IL-12, and tumor necrosis factor-α) induce the inflammation as a result of the transcriptional activity of HIF-1α. The increasing levels of pro-inflammatory cytokines as well as previous levels lead to the initiation of cytokine storm which is a serious risk factor for disease severity. b PFC might help the body to tackle the hypoxic condition which results in the formation of cytokine storms through HIF-1α activity. PFC utilization is efficient in HIF-1α instability and reduces HIF-1α expression, which causes reduce the inflammation cascade
In view of the foregoing, increased inflammation in the lungs of a severe COVID-19 patient, leading to the hypoxia and its mentioned consequences, brings us this hypothesis that oxygen delivering to inflamed tissues could decrease cytokine storm intensity, and therefore, morbidities (ARDS and organ failure) and mortality. In this regard, perfluorocarbon (PFC) molecules as carriers of remarkable mass of respiratory gases seem to be a great candidate. This is a molecule containing wholly of fluorine and carbon. PFCs have specific features including high gas solubility, low surface tension, fast release, average volatility, high volume quality, good histocompatibility, and the absence of absorption and metabolism in vivo [26]. These features make them to be utilized as oxygen carriers for various purposes such as improving oxygen transport and oxygen delivery to tissues to organ protection [27]. More interestingly, it has been shown that PFCs also is able to reduce HIF-1α expression [28]. Accordingly, PFC utilization is efficient in HIF-1α instability which can reduce the inflammation cascade. Hence, PFCs’ features might help the body to tackle the hypoxic condition which results in the formation of cytokine storms through HIF-1α activity (Fig. 1b). It has been noted that the partial liquid ventilation for ARDS in adults seems not to be useful by a systematic review which only evaluated two eligible studies [29]. On the other hand, it has been suggested that ARDS in the COVID-19 is not similar as ARDS defined in the Berlin criteria which seems to be due to “loss of lung perfusion regulation and hypoxic vasoconstriction” [30].
Conclusion
Due to the severe inflammatory response against SARS-CoV-2, hypoxia will occur at the site of infection-induced inflammation and angiogenesis. Considering HIF-1α expression in hypoxic conditions and consequently, pro-inflammatory cytokines and pro-angiogenic factor upregulation, challenging events including cytokine storm and then ARDS will occur/deteriorate. Therefore, oxygen delivery through PFC to these tissues seems to be efficient, as it might be capable of dissipating HIF-1α expression and further cytokine production. The authors strongly encourage further animal and human studies on this hypothesis.
Funding
This study was not funded.
Declarations
Conflict of interests
The authors declare no actual or potential conflict of interest related to this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Norooznezhad AH, Najafi F, Riahi P, Moradinazar M, Shakiba E, Mostafaei S. Primary symptoms, comorbidities, and outcomes of 431 hospitalized patients with confirmative RT-PCR results for COVID-19. Am J Trop Med Hyg. 2020;103(2):834–837. doi: 10.4269/ajtmh.20-0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirby T. New variant of SARS-CoV-2 in UK causes surge of COVID-19. Lancet Respir Med. 2021;9(2):e20–e21. doi: 10.1016/s2213-2600(21)00005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hantoushzadeh S, Norooznezhad AH. Possible cause of inflammatory storm and septic shock in patients diagnosed with (COVID-19) Arch Med Res. 2020;51(4):347–348. doi: 10.1016/j.arcmed.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kazemi Aski S, Norooznezhad AH, Shamshirsaz AA, et al. Clinical features and risk factors associated with acute respiratory distress syndrome in pregnant women diagnosed with COVID-19: a multi-center case-control study. J Matern Fetal Neonatal Med. 2021;21:1–5. doi: 10.1080/14767058.2021.1872062. [DOI] [PubMed] [Google Scholar]
- 5.Torres Acosta MA, Singer BD. Pathogenesis of COVID-19-induced ARDS: implications for an ageing population. Eur Respir J. 2020;56(3):9. doi: 10.1183/13993003.02049-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dallan C, Romano F, Siebert J, Politi S, Lacroix L, Sahyoun C. Septic shock presentation in adolescents with COVID-19. Lancet Child Adolesc Health. 2020;4(7):e21–e23. doi: 10.1016/s2352-4642(20)30164-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iwasaki M, Saito J, Zhao H, Sakamoto A, Hirota K, Ma D. Inflammation triggered by SARS-CoV-2 and ACE2 augment drives multiple organ failure of severe COVID-19: molecular mechanisms and implications. Inflammation. 2021;44(1):13–34. doi: 10.1007/s10753-020-01337-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pavez N, Kattan E, Vera M, et al. Hypoxia-related parameters during septic shock resuscitation: pathophysiological determinants and potential clinical implications. Ann Trans Med. 2020;8(12):784. doi: 10.21037/atm-20-2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cherian SV, Kumar A, Akasapu K, Ashton RW, Aparnath M, Malhotra A. Salvage therapies for refractory hypoxemia in ARDS. Respir Med. 2018;141:150–158. doi: 10.1016/j.rmed.2018.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fröhlich S, Boylan J, McLoughlin P. Hypoxia-induced inflammation in the lung: a potential therapeutic target in acute lung injury? Am J Respir Cell Mol Biol. 2013;48(3):271–279. doi: 10.1165/rcmb.2012-0137TR. [DOI] [PubMed] [Google Scholar]
- 11.Goh KJ, Choong MC, Cheong EH, et al. Rapid progression to acute respiratory distress syndrome: review of current understanding of critical illness from COVID-19 infection. Ann Acad Med Singap. 2020;49(3):108–118. doi: 10.47102/annals-acadmedsg.202057. [DOI] [PubMed] [Google Scholar]
- 12.Watts ER, Walmsley SR. Inflammation and hypoxia: HIF and PHD isoform selectivity. Trends Mol Med. 2019;25(1):33–46. doi: 10.1016/j.molmed.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 13.Ahmed AU. An overview of inflammation: mechanism and consequences. Front Biol. 2011;6(4):274. doi: 10.1007/s11515-011-1123-9. [DOI] [Google Scholar]
- 14.Opitz B, van Laak V, Eitel J, Suttorp N. Innate immune recognition in infectious and noninfectious diseases of the lung. Am J Respir Crit Care Med. 2010;181(12):1294–1309. doi: 10.1164/rccm.200909-1427SO. [DOI] [PubMed] [Google Scholar]
- 15.Crimi E, Slutsky AS. Inflammation and the acute respiratory distress syndrome. Best Pract Res Clin Anaesthesiol. 2004;18(3):477–492. doi: 10.1016/j.bpa.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 16.Wilkerson RG, Adler JD, Shah NG, Brown R. Silent hypoxia: A harbinger of clinical deterioration in patients with COVID-19. Am J Emerg Med. 2020;38(10):2243.e5–2243.e6. doi: 10.1016/j.ajem.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reyes H, Reisz-Porszasz S, Hankinson O. Identification of the Ah receptor nuclear translocator protein (Arnt) as a component of the DNA binding form of the Ah receptor. Science. 1992;256(5060):1193–1195. doi: 10.1126/science.256.5060.1193. [DOI] [PubMed] [Google Scholar]
- 18.Wang GL, Jiang BH, Rue EA, Semenza GL. Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension. Proc Natl Acad Sci U S A. 1995;92(12):5510–5514. doi: 10.1073/pnas.92.12.5510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nizet V, Johnson RS. Interdependence of hypoxic and innate immune responses. Nat Rev Immunol. 2009;9(9):609–617. doi: 10.1038/nri2607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Colgan SP, Furuta GT, Taylor CT. Hypoxia and innate immunity: keeping up with the HIFsters. Annu Rev Immunol. 2020;38:341–363. doi: 10.1146/annurev-immunol-100819-121537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cramer T, Yamanishi Y, Clausen BE, et al. HIF-1alpha is essential for myeloid cell-mediated inflammation. Cell. 2003;112(5):645–657. doi: 10.1016/s0092-8674(03)00154-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jantsch J, Chakravortty D, Turza N, et al. Hypoxia and hypoxia-inducible factor-1 alpha modulate lipopolysaccharide-induced dendritic cell activation and function. J Immunol. 2008;180(7):4697–4705. doi: 10.4049/jimmunol.180.7.4697. [DOI] [PubMed] [Google Scholar]
- 23.Walmsley SR, Print C, Farahi N, et al. Hypoxia-induced neutrophil survival is mediated by HIF-1alpha-dependent NF-kappaB activity. J Exp Med. 2005;201(1):105–115. doi: 10.1084/jem.20040624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N Engl J Med. 2020;383(2):120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ackermann M, Mentzer SJ, Kolb M, Jonigk D. Inflammation and intussusceptive angiogenesis in COVID-19: everything in and out of flow. Eur Respir J. 2020;56(5):9. doi: 10.1183/13993003.03147-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hou S, Ding H, Lv Q, et al. Therapeutic effect of intravenous infusion of perfluorocarbon emulsion on LPS-induced acute lung injury in rats. PLoS ONE. 2014;9(1):e87826. doi: 10.1371/journal.pone.0087826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Agrawal A, So PW, Penman A, et al. Limited penetration of perfluorocarbon in porcine pancreas preserved by two-layer method with (19)fluorine magnetic resonance spectroscopy and headspace gas chromatography. Cell Transplant. 2010;19(8):1021–1029. doi: 10.3727/096368910x491789. [DOI] [PubMed] [Google Scholar]
- 28.Maillard E, Juszczak MT, Langlois A, et al. Perfluorocarbon emulsions prevent hypoxia of pancreatic β-cells. Cell Transplant. 2012;21(4):657–669. doi: 10.3727/096368911x593136. [DOI] [PubMed] [Google Scholar]
- 29.Galvin IM, Steel A, Pinto R, Ferguson ND, Davies MW. Partial liquid ventilation for preventing death and morbidity in adults with acute lung injury and acute respiratory distress syndrome. Cochrane Database Syst Rev. 2013;2013(7):003707. doi: 10.1002/14651858.CD003707.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gattinoni L, Coppola S, Cressoni M, Busana M, Rossi S, Chiumello D. COVID-19 does not lead to a "typical" acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;201(10):1299–1300. doi: 10.1164/rccm.202003-0817LE. [DOI] [PMC free article] [PubMed] [Google Scholar]