Abstract
Background: With the global attack of Coronavirus Disease 2019 (COVID-19), cases with Post-traumatic Stress Disorder (PTSD) have been increasing steadily, which seriously affects the quality of life of patients and as such, seeking effective treatments is an urgent matter. Narrative Exposure Therapy (NET) is a typical cognitive behavioral therapy targeting trauma-related psychological disorders and may be an effective intervention.
Methods: A total of 111 COVID-19 patients near the discharge stage with positive screening results for posttraumatic stress symptoms (PTSS) were randomly assigned (1:1) to either the study group or the control group. The study group received NET and personalized psychological intervention, while the control group only received personalized psychological intervention. PTSS, depression, anxiety and sleep quality were measured pre- and post-intervention to evaluate the effect of NET. This trial was registered with the International Standard Randomized Clinical Trial Registry (No. ChiCTR2000039369).
Results: NET participants showed a significantly greater PTSS reduction in comparison with the control group after the intervention. Improvement in sleep quality, anxiety and depression after the intervention were pronounced but not significantly different between the two treatment groups.
Limitations: The assessors weren't blinded for the convenience of measurement and protection of participants’ psychological security.
Conclusions: NET likely had a positive impact on PTSS of COVID-19 patients. Clinical staff should consider applying NET to improve the psychological well-being of patients who have experienced an epidemic such as COVID-19.
Keywords: Narrative exposure therapy, COVID-19, Post-traumatic stress symptoms, randomized controlled trial
1. Introduction
Since December 2020, the Coronavirus Disease 2019 (COVID-19) has spread worldwide and the number of infections has increased rapidly. COVID-19 is extremely contagious, fatal, and unpredictable, and it seriously endangers the lives of people. For treatment purposes, patients with mild COVID-19 need to be isolated in a single room for at least 14 days, whereas the critically ill are admitted to ICU with possible rapid deterioration and high mortality. As evidenced in previous studies, acute infectious diseases can lead to anxiety, depression, sleep disorders and post-traumatic stress disorder (PTSD) in survivors (Cheng et al., 2004; Mak et al., 2009; Wu et al., 2005). A study on the psychiatric disorders among the survivors of SARS revealed that 25% of the participants showed signs of PTSD and 15.6% of them had worsening depression (Mak et al., 2009). The Middle East Respiratory Syndrome Coronavirus (MERS) survivors suffered psychological trauma like rumors and discrimination after being discharged from the hospital (Sim, 2016). Patients with COVID-19 were likely to be socially ignored or alienated by the public due to fear of contamination. Recent studies found that the incidence of PTSD symptoms was 14.0% in suspected COVID-19 patients, using Post-traumatic Stress Disorder Checklist-5 (PCL-5) with a sample of 93 (Zhang et al., 2020), and 31% in diagnosed COVID-19 patients, using the Post-traumatic Stress Disorder Self-rating Scale (PTSD-SS) with a sample of 126 (Yuan et al., 2020). Cai et al. (Cai et al., 2020) found that 31% of COVID-19 survivors had stress response, 22.2% of patients had symptoms of depression, and 38.1% of patients had symptoms of anxiety.
PTSD is a debilitating mental illness that can develop after experiencing a traumatic event. There are four typical features of PTSD: a. experiencing or witnessing a traumatic event; b. re-experiencing symptoms of the event, including nightmares and/or flashbacks; c. avoidance of people, situations, or places that are reminders of the event; d. hyperarousal symptoms, including irritability and concentration issues (American Psychological Association, 2013). The occurrence of PTSD can affect the endocrine system, central nervous system and immune system, leading to mental disorders in patients and possible long-term harm in both patients and their families (Herringa, 2017).
Narrative Exposure Therapy (NET) is a short-term cognitive behavioral therapy for trauma-related psychological disorders (Schauer et al., 2011), which is based on neurobiological theories of trauma and memory (Said and King, 2020). NET aims to reduce PTSD symptoms through two alternative mechanisms: one is exposure to traumatic memories and subsequent habituation of the associated emotional response, the other is reconstruction of autobiographical memory and a consistent narrative (Schauer et al., 2011). Existing evidence showed a positive effect when NET was provided to PTSD patients by medical professionals who were not psychologists (Köbach et al., 2017; Neuner et al., 2008; Robjant et al., 2019). NET had a significant effect on improving the mental state of patients who had experienced multiple traumas, such as war, torture or large-scale natural disasters (Cheng et al., 2004; Hecker et al., 2015; Zang et al., 2013). Numerous studies and meta-analyses in different countries (e.g., Europe, Asia and Central Africa) have shown the effectiveness and applicability of NET in various populations such as children, adolescents and women (Crombach and Siehl, 2018; Gwozdziewycs, 2013; Zang et al., 2013). Although NET is not referred to as a first-line treatment in current PTSD treatment guidelines, it is recommended as both prevention and treatment of PTSD in adults, along with cognitive processing theory, prolonged exposure therapy and cognitive therapy for PTSD (National Institute for Health and Care Excellence, 2018).
Due to the new emergency of COVID-19, it is not clear whether NET can be an effective treatment for post-traumatic stress symptoms (PTSS). The purpose of the study was to screen for the prevalence of PTSS among pre-discharged COVID-19 patients and explore the effects of NET on patients experiencing PTSS.
2. Methods
2.1. Study design and participants
This study was a prospective, participant-blinded, randomized controlled trial, which was conducted in three COVID-19 designated hospitals in Xiangyang City, Hubei provinces, China, from February to June, 2020. Permission to conduct the study had been sought from the three medical ethical committees of the above hospitals. Before the study, the patients were informed of the purpose of the research and were assured of the right to refuse to participate or to withdraw from the study at any stage. Informed consent was obtained from each participant before the data collection.
During the COVID-19 epidemic, COVID-19 psychological crisis intervention groups were set up in the above three COVID-19 designated hospitals. Before COVID-19 patients were discharged from the hospitals, they were informed about the crisis intervention and invited to participate in the PTSS screening. Nurses were trained at each hospital to conduct screenings for PTSS among the discharged patients using the PTSD Checklist-Civilian Version (PCL-C). This scale is suitable for medical professionals other than psychologists to evaluate participants, with a cutoff score of 50 suggesting a PTSD diagnosis (Brewin, 2005). Those screening PTSS positive were randomly assigned to personalized psychological intervention or NET.
The inclusion criteria for the research participants included: a. diagnosed with COVID-19 according to the Diagnosis and Clinical Management of 2019 novel coronavirus infected pneumonia (trial version 6 or trial version 7); b. score of PCL-C≥50; c. willing to participate in the study. Exclusion criteria included participants with: a. history of mental illness; b. inability to use the internet.
2.2. Randomization and blindness
The eligible participants were randomized by sortition to either the intervention group or the control group. The drawing of lots for 111 eligible participants was conducted by a research nurse, with 56 in the intervention group and 55 in the control group. The randomization process was blinded to the participants.
2.3. Interventions
2.3.1. Intervention group
The intervention group received both Narrative Exposure Therapy (NET, Schauer et al., 2011) and personalized psychological treatment. A 6-month online follow-up was also provided.
Doctors and nurses with the National Certificate of Psychological Counselor played the role of psychologists. Guided by NET intervention protocol (Schauer et al., 2011), all of the intervention group members have been trained by a doctor who has participated in a NET-training and practiced NET during her usual work in the psychological clinic. The primary responsibility system was adopted and except for special reasons, the participants did not change their psychologists during the intervention. The patients received intervention mainly through the internet in the early stage due to limited public transportation. The members of the psychological crisis intervention groups kept in contact with the participants over mobile phones in order to implement the intervention and assess outcomes after discharge. After social order returned to normal in the later period, the participants voluntarily contacted their designated psychologists and then went to the psychological counseling clinics of the hospitals for in-person treatment. A one-to-one working mode was adopted and the treatment environment was quiet and relatively concealed without being disturbed by others. The NET therapy had a duration of eight weeks, with one or two sessions a week, lasting for 90~120 minutes each time.
The NET intervention included three main sessions: psychoeducation, constructing the life events timeline and starting the narration, with details shown in Table 1 .
Table 1.
Details of NET intervention
| Stage | Intervention content |
| Psychological education | a. Before implementing NET, participants received two courses of psychological education (40 minutes for each course). |
| b. During psychological education, participants were informed that their anxiety, fear, pain, and other negative emotions were normal phenomena. | |
| Constructing the life events timeline | a. The psychologists instructed participants -remotely through the Internet to draw a straight line on a piece of white paper, symbolizing the continuous flow of their life, and to draw a sun at the end, symbolizing the future. |
| b. Participants were asked to paint flowers on the line to represent happy major events in their lives, and stones on the line to represent sad or traumatic events (as shown in Fig. 2). | |
| c. The psychologist encouraged the participants to give a title for each symbol, and to determine the time and place of each event in chronological order. | |
| d. The construction of the life events timeline should have been completed in one treatment session, which dealt with an overview of important life events and the direction of subsequent treatments. | |
| e. In the follow-up treatment, the psychologists discussed in-depth with the participants about their important life events, summarized these events, and helped them to determine the next event. | |
| Starting the narration | a. The chronology of the narration should address all traumatic incidents from birth to the present according to the life events timeline. |
| b. When the participants narrated recent traumatic events, the NET procedure would be explained in detail. | |
| c. In order to recognize when the participants started to discuss a traumatic event and before discussing the traumatic event in detail, the psychologists should have learnt more about the participants’ experiences prior to being diagnosed with COVID-19. | |
| d. The narration of a traumatic event began with the participant's deep recollection and re-experiencing of the event, meaning that they would be exposed to sad or traumatic events again. This process was very slow and painful, so the narration of an event must not be interrupted and must be completed in one treatment session. | |
| e. When the participant was describing the traumatic event, the psychologist recorded the participant's narration and asked in detail about the emotions and feelings when the traumatic event occurred, as well as their current views of the traumatic event. An example of a participant’ s narration is shown in Box1. | |
| f. Before starting each subsequent Narrative Exposure Therapy, the psychologists asked the participants to repeat the contents of the previous treatment session so that they would arouse the events again, and the contents would be modified and supplemented. | |
| g. Since the NET made the participants re-experience the traumatic event, before the end of the treatment session, arousal measures must be limited to reduce negative emotions in the participants. The participants narrated all the major events in their life events timeline to the end, marking the end of treatment. The psychologists’ records of every narration would be saved as the participants’ autobiography. | |
| h. At the end of the treatment, the therapist encouraged the patient to express their views and hopes for the future. The therapist gave the patient a copy of the autobiography. |
As part of the online follow-up, the nurses provided participants with a follow-up after 6-months. Nurses organized the establishment of participant groups, encouraged participants to communicate with each other and answered their questions in a timely manner to help them correctly understand COVID-19. The follow-up group also established a WeChat subscription to learn about COVID-19 prevention and psychological nursing information every week. During the intervention period, if the participants were found to be suicidal or had injured themselves, their family would be immediately contacted and then they would send the participants to specialist hospitals for further treatment.
2.3.2. Control group
The controlled group interventions included personalized psychological treatment and online follow-up.
The psychologists gave individualized psychological interventions based on the participants' symptoms once a week, 40-60 minutes each time. Before intervention, the psychologists needed to establish a trusting and reliable doctor-patient relationship with the participants. During the intervention process, the psychologists guided the participants to express their inner feelings, listened to the inner voices of the participants, and understood the current problems that plagued them. The psychologists guided the participants to think about the above problems, helped them correctly understand COVID-19 and alleviated their feelings of guilt and fear by encouraging participants to communicate with their families and to play an active role in their families, which may help participants integrate into the collective and society. To alleviate the participants' negative emotions, the psychologists taught them the correct psychological adjustment methods, and guided them to vent their negative emotions, such as listening to music, exercising, and chatting.
In addition, the crisis intervention group also provided 6-month online follow-up for the control group.
2.4. Assessments
The primary outcome was PTSS of COVID-19 patients accessed before and after intervention, and the secondary outcomes were their depression, anxiety, and sleep quality.
2.4.1. PTSS
The PTSD Checklist-Civilian Version (PCL-C, Weathers et al., 1993) was used to measure participants’ PTSS pre- and post- intervention. This scale was adapted from the Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), and was specifically used to assess the experience of civilians after trauma during non-war period. The tool has 17 items rated on a 5-point scale ranging from 1-not at all to 5-extremely that assesses three symptom clusters: re-experience, avoidance/numbing and hyper-arousal. The total score ranges from 17 to 85, with scores of 50 or above indicative of probable PTSS (Brewin, 2005). The scale has been found to have reasonably good psychometric properties in different Chinese populations. The internal consistency coefficient was 0.88~0.94, the test-retest reliability was 0.83~0.88, and the factors of the scale explained 65.7% of the total variance, indicating that the Chinese version had satisfactory reliability (Chen et al., 2005). At present, PCL-C is still widely used in the assessment of PTSS for civilians in China.
2.4.2. Depression
The Self-rating Depression Scale (SDS) was used to measure participants’ depression level both before and after the intervention. The SDS is a 20-item questionnaire for assessing experience during the past week, with 10 items indicating negative experiences and 10 items indicating positive experiences. Respondents scored each item based on the frequency, ranging from 1 (never, or sometimes) to 4 (frequently, or always), with higher scores indicating higher depression level (Zung et al., 1965). The SDS has been widely used among Chinese subject, with a Cronbach's α of 0.774 (Lei et al., 2015).
2.4.3. Anxiety
The Self-rating Anxiety Scale (SAS) was used to measure participants’ anxiety pre- and post- intervention. SAS is a 20-item questionnaire used to assess the degree of psychological and physical anxiety within the previous week, with a 4-point Likert scale ranging from 1 (never or sometimes) to 4 (frequently or always). Higher score indicates greater anxiety (Zung, 1971). The SAS has been widely used among Chinese subject, with a Cronbach's α of 0.799 (Lei et al., 2015).
2.4.4. Sleep quality
The Pittsburgh Sleep Quality Index (PQSI) was used to measure participants’ sleep quality pre- and post- intervention. The scale includes 19 items (one item is not scored) with a total score ranging from 0 to 21. Higher scores indicate poorer sleep quality. The PQSI has been widely used among Chinese subject, with a Cronbach's α of 0.87 (Wang et al., 2020).
2.5. Data analyses
Statistical analysis was performed using SPSS 23.0. Frequencies (N), percentages (%), mean and standard deviation (SD) were used to present the characteristics of the participants. The chi-square tests were used for categorical variables and the t-test was used for continuous variables to compare the baseline characteristics of the participants between the intervention group and control group. The explored assessments were analyzed by conducting repeated measures multivariate analysis of variance (MANOVA), followed by post-hoc pairwise comparisons. Effect sizes were calculated with partial eta-squared values. P values of 0.05 or less were considered statistically significant.
3. Results
3.1. Recruitment, attrition, and adherence
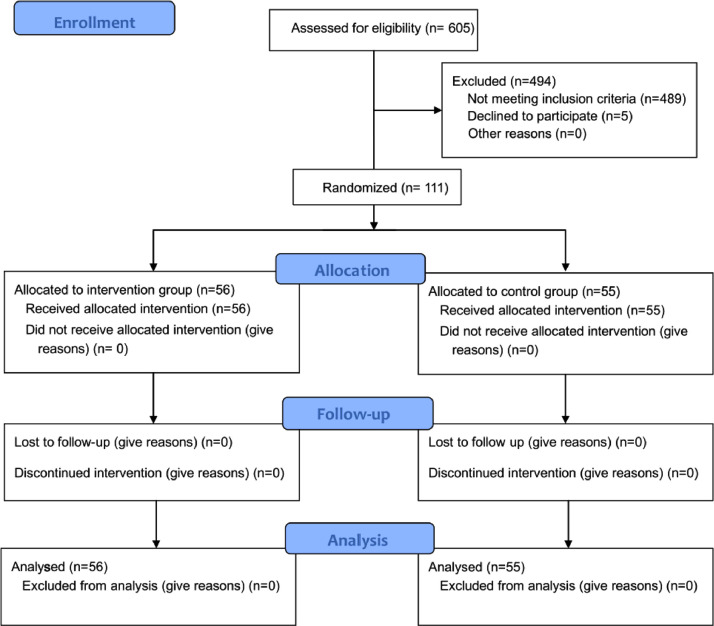
As shown in the flow diagram (Fig. 1 ), 605 discharged COVID-19 patients were approached for eligibility screening. Of these, 116 met the selection criteria and 111 agreed to participate in the study. 111 participants were assigned to two groups randomly (56 in the intervention group and 55 in the control group). During the study process, no participants changed their intervention plan or dropped out, and their data were all complete and analyzed.
Fig. 1.
CONSORT flow diagram of the study
3.2. Characteristics of the participants
The characteristics of the participants are summarized in Table 2 . Most participants were female (62.16%) and their mean age was 46.38 years old. They were isolated for 40.72 days on average and most of them (79.28%) were COVID-19 patients with mild symptoms. Among them, 38 participants had chronic comorbidities, including 18 with hypertension, 12 with diabetes, five with coronary heart disease, four with chronic obstructive pulmonary disease and some with other chronic diseases. No significant differences in the participants’ characteristics were found between the intervention group and the control group.
Table 2.
Characteristics of the participants
| Characteristics | Overall | Control (n=55) | Intervention (n=56) | χ2/t | p |
| Gender (%) | |||||
| Male | 42(37.84) | 20(36.36) | 22(39.29) | 0.101 | 0.951 |
| Female | 69(62.16) | 35(63.67) | 34(60.71) | ||
| Age (means±SD) | 46.38±12.34 | 46.60±12.79 | 46.16±12.01 | 0.187 | 0.852 |
| Marital status (%) | |||||
| Married | 92 | 47 | 45 | 0.508 | 0.476 |
| Single | 19 | 8 | 11 | ||
| Children situation (%) | |||||
| With | 86 | 44 | 42 | 0.398 | 0.528 |
| Without | 25 | 11 | 14 | ||
| Educational level (%) | |||||
| Below middle school | 15 | 7 | 8 | 1.249 | 0.536 |
| Middle school | 31 | 18 | 13 | ||
| Above middle school | 65 | 30 | 35 | ||
| Days in isolation (means±SD) | 40.72±11.99 | 41.02±12.53 | 40.43±11.54 | 0.258 | 0.797 |
| COVID-19 type (%) | |||||
| Mild | 88(79.28) | 45(81.82) | 43(78.79) | 0.428 | 0.513 |
| Severe | 23(20.72) | 10(18.18) | 13(23.31) | ||
| Chronic comorbidities (%) | 38(34.23) | 20(36.36) | 18(32.14) | 0.220 | 0.639 |
3.3. Effects of NET on PTSS
In relation to PTSS, a significant time x group interaction (Table 3 ) was observed for PCL-C (F(1,109)=36.300, p<0.001), and its three dimensions: re-experience (F(1,109)=28.282, p<0.001), voidance/numbing (F(1,109)=8.470, p=0.004), and hyper-arousal (F(1,109)=9.643, p=0.002).
Table 3.
Differences in PCL-C, SDS, SAS and PQSI between the pre-test and post-test groups
| Pre-test | Post-test | Repeated measures MANOVA | |||||||||
| Intervention | Control | Intervention | Control | Group | Time | Group x Time Interaction | |||||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | F | P-value | F | P-value | F | P-value | Effect Size** | |
| PCL-C | 75.2±4.01 | 74.45±4.86 | 49.52±7.32 | 58.65±7.48 | 26.214 | <0.001* | 639.976 | <0.001* | 36.300 | <0.001* | 0.143 |
| re-experience | 21.55±2.05 | 21.42±2.11 | 14.57±3.54 | 18.36±3.02 | 24.517 | <0.001* | 184.689 | <0.001* | 28.282 | <0.001* | 0.115 |
| voidance/numbing | 31.88±2.39 | 31.93±2.55 | 20.68±5.01 | 24.02±5.79 | 9.017 | 0.003* | 286.084 | <0.001* | 8.470 | 0.004* | 0.037 |
| hyper-arousal | 21.77±2.01 | 21.11±2.92 | 14.27±4.3 | 16.27±3.12 | 2.463 | 0.118 | 206.850 | <0.001* | 9.643 | 0.002* | 0.042 |
| PSQI | 15.87±2.85 | 15.84±2.86 | 13.16±2.87 | 14.31±2.86 | 2.089 | 0.15 | 30.519 | <0.001* | 2.390 | 0.124 | 0.011 |
| SAS | 61.11±11.42 | 61.47±11.84 | 51.64±9.5 | 50.7±10.23 | 0.146 | 0.703 | 52.142 | <0.001* | 0.740 | 0.390 | 0.003 |
| SDS | 53.52±11.84 | 54.29±11.51 | 46.89±8.95 | 50.4±8.98 | 2.346 | 0.127 | 14.159 | <0.001* | 0.957 | 0.329 | 0.004 |
* p < 0.05.
Differences by time, group, and time x group were assessed with repeated measures MANOVA.
**Effect size was determined by Partial Eta Squared.
Abbreviations: SD=Standard Deviation; PCL-C=PTSD Checklist-Civilian Version; SDS=Self-rating Depression Scale; SAS=Self-rating Anxiety Scale; PSQI=the Pittsburgh Sleep Quality Index.
Pairwise comparisons at pre-test (NET group vs control group) showed that PCL-C and its three dimensions including re-experience, voidance/numbing and hyper-arousal were not significantly different between groups (p≥0.279). Pairwise comparisons at post-test (NET group vs control group) showed that PCL-C, re-experience, voidance/numbing and hyper-arousal were all significantly lower in NET group (p≤0.001).
Pairwise comparisons over time (pre-test vs post-test) showed that PCL-C and three dimensions at pre-test were all significantly higher than those at post-test in NET group (p<0.001), as well as in control group (p<0.001).
3.4. Effects of NET on depression, anxiety, and sleep quality
In relation to depression, anxiety, and sleep quality, there was no significant time x group interaction (Table 3) observed for SDS (p=0.329), SAS (p=0.390) and PQSI (p=0.124). The main effects of time on SDS, SAS and PQSI were statistically significant (p<0.001), while the main effects of group on SDS, SAS and PQSI were not statistically significant (p>0.05).
4. Discussion
This study has examined the effectiveness of applying NET to treat PTSS in discharged COVID-19 patients. The results indicated that the PTSS were improved to a relatively normal level after both the NET intervention and the control intervention, with a significantly larger level of improvement in the NET group (p<0.001). NET is an evidence-based method to treat survivors of PTSS (Hamblen et al., 2019). Based on the principles of cognitive behavioral therapy (CBT), testimony therapy and exposure therapy, NET follows a systematic treatment protocol that is aimed at constructing a consistent, coherent autobiographical representation of the traumatic event(s) in the patient's life (Raghuraman et al., 2020). NET therapists assisted discharged COVID-19 patients with PTSS to construct their life events timeline and determine their traumatic events. The purpose was to help the patients identify and re-experience the most painful memories in their lives and consequently find hopeful and powerful elements in the traumatic events. Through repeated and detailed descriptions of what happened in a traumatic event, patients with PTSS may become numb to trauma triggers. As a result, the patients reorganized their broken memories into an entire life story with new meanings, where they could gain power to fight against traumatic events and to gain relief from PTSS (Turrini, 2017).
There was no significant difference between NET group and control group regarding improvement of depression, anxiety and sleep disorders (p>0.05). However, both groups showed significant improvement of above symptoms over time (p<0.001). This indicated that patients with PTSS still might benefit improvement of depression, anxiety and sleep disorders from NET, largely consisting with the results of existing studies (Lely et al., 2019; Mørkved and Thorp, 2018). As evidenced in previous studies, PTSS might cause additional psychological and physical disorders, such as depression, anxiety and sleep disorders (Bogic et al., 2015; Park et al., 2019), indicating these combined symptoms may be reduced with the relief of PTSS in patients. Additionally, the results of Weinhold et al. showed that NET could reduce the sleep onset latency and sleep arousal period in patients with PTSS (Weinhold et al., 2017), which may be another explanation for NET to improve sleep quality. In our study, the difference in improvement in depression, anxiety and sleep quality between the two groups was not statistically significant, which was inconsistent with some previous studies. (Alghamdi et al., 2015; Park et al., 2020). This discrepancy might be related to differences in age characteristics of the participants. As reviewed by Lely et al. (2019), treatment results of NET were better for older adults. However, most of participants in our study were middle-aged patients. In addition, most previous studies included wait-list controls whereas the control group in the present trial received personalised psychological treatment and online follow-up. This may have contributed to the reduction of symptoms also in the control group. Besides, the relatively small sample may also lead to this discrepancy.
The practical need for trials such as this is evident and pressing. Currently, the world is facing major public health events. The number of people infected with COVID-19 is increasing every day, and patients are experiencing a series of sufferings such as illness, transmission to others, and disrupted normal lives. Some of them even lost their families and jobs due to COVID-19, resulting in their likely experiencing PTSD. Narrative exposure therapy, as a standardized and programmed intervention with wide applicability, may have a good effect on COVID-19 patients with PTSS, and provide help for patients worldwide.
To our knowledge, this is the first study to apply NET for the treatment of PTSS acquired during major public health events. The evidence produced by this study has significant practical importance in the search for finding effective treatments for PTSS in COVID-19 patients. Since discharged patients were temporarily unable to return to work due to the epidemic, they had enough time to participate in this study. In addition, all interventions were provided for participants free of charge, which led to a 100% participation rate.
Our study also had several limitations worth mentioning. First, the sample size was relatively small as a result of limitations during the COVID-19 epidemic. To determine whether NET can be used as an evidence-based treatment for PTSS after experiencing major public health events, it is necessary to expand the sample and repeat the test to confirm this finding. Second, most participants received intervention from their psychologists remotely through the Internet instead of through an in-person, face-to-face setting, which may have lessened the impact of the treatment. Third, only those who could use the Internet were selected in the early stage of the study, resulting in younger ages of the participants, which may have led to selection bias in this study. Whether NET is applicable to elderly patients with PTSS who have experienced major public health events needs further research. Fourthly, PTSD Checklist for DSM-5 (PCL-5) compiled according to DSM-V has added another symptom (negative changes of cognition and emotion) to PCL-C. Although PCL-5 has its Chinese version, it is still in the exploratory stage and is not widely used in China. Therefore, this study still chose PCL-C as the assessment tool of PTSS, although it was not the latest diagnostic criteria. Fifthly, we did not record sessions during the intervention, mainly due to the inconvenience caused during the COVID-19 pandemic. We were unable to formally monitor or assess treatment competence or adherence and relate these to outcomes. Finally, the assessors were not blinded during the intervention process for the convenience of measurement and protection of participants’ psychological and emotional security.
5. Conclusions
This study demonstrated a positive effect of the NET on PTSS of discharged COVID-19 patients. In addition to re-experience, avoidance/numbing and hyper-arousal symptoms, their sleep quality, depressive and anxiety symptoms have also been improved. After experiencing major public health incidents, it is very easy to cause the occurrence of PTSS, which brings a heavy burden to the country's mental health resources. NET, as a standardized procedure and a multiculturally accepted format, may be an effective intervention method for a wider range of traumatic events and stress events like COVID-19. Clinical staff should consider using it widely in psychological health in epidemic context.
Author statement
All authors have read and approved the contents of the manuscript and agree on the order of ranking.
Data availability statement
The supporting data can be accessed from the corresponding author (Jun Zhang) on reasonable request.
Author contributions
FY and ZG conceived the study. FY, ZJ, SYX, and FGZ designed the study. WXF, XXX, WJ, MDR, KLA and SDW data acquisition. FY, WXF and SYX did statistical analysis. FY, ZJ, and SYX wrote the first draft of this article. All the authors have carefully reviewed the article and approved the final draft.
Funding
This study was not funded.
Declarations of Interest
None to be declared.
Acknowledgments
In this study, three COVID-19 designated hospitals in Xiangyang city, Hubei Province provided free intervention for participants. We would like to thank the members of the psychological crisis team in these three hospitals and all the participants in the post-discharge follow-up group for their contributions to this study.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.06.019.
Appendix. Supplementary materials
References
- Alghamdi M., Hunt N., Thomas S. The effectiveness of Narrative Exposure Therapy with traumatised firefighters in Saudi Arabia: A randomized controlled study. Behav. Res. Ther. 2015;66:64–71. doi: 10.1016/j.brat.2015.01.008. [DOI] [PubMed] [Google Scholar]
- American Psychological Association H. American Psychiatric Publishing; Arlington: 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Bogic M., Njoku A., Priebe S. Long-term mental health of war-refugees: a systematic literature review. BMC Int. Health Hum. Rights. 2015;15 doi: 10.1186/s12914-015-0064-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin C.R. Systematic review of screening instruments for adults at risk of PTSD. J. Trauma Stress. 2005;18:53–62. doi: 10.1002/jts.20007. [DOI] [PubMed] [Google Scholar]
- Cai X., Hu X., Otte E.I., Wang J., An Y., Li Z., Yuan B. Psychological Distress and Its Correlates Among COVID-19 Survivors During Early Convalescence Across Age Groups. Am. J. Geriatr. Psychiatry. 2020;28:1030–1039. doi: 10.1016/j.jagp.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Gao X., Li L., Lu Y., Zhang J. Reliability and Validation of the Symptom Self-Rating Scale of the Post-traumatic Stress Disorder. Chin. Ment. Health J. 2005:13–16. [Google Scholar]
- Cheng S.K.W., Wong C.W., Tsang J., Wong K.C. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS) Psychol. Med. 2004;34:1187–1195. doi: 10.1017/s0033291704002272. [DOI] [PubMed] [Google Scholar]
- Crombach A., Siehl S. Impact and cultural acceptance of the Narrative Exposure Therapy in the aftermath of a natural disaster in Burundi. BMC Psychiatry. 2018;18 doi: 10.1186/s12888-018-1799-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwozdziewycs N. Meta-Analysis of the Use of Narrative Exposure Therapy for the Effects of Trauma Among Refugee Populations. Permanente J. 2013;17:72–78. doi: 10.7812/TPP/12-058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamblen J.L., Norman S.B., Sonis J.H., Phelps A.J., Bisson J.I., Nunes V.D., Megnin-Viggars O., Forbes D., Riggs D.S., Schnurr P.P. A guide to guidelines for the treatment of posttraumatic stress disorder in adults: An update. Psychotherapy. 2019;56:359–373. doi: 10.1037/pst0000231. [DOI] [PubMed] [Google Scholar]
- Hecker T., Hermenau K., Crombach A., Elbert T. Treating Traumatized Offenders and Veterans by Means of Narrative Exposure Therapy. Front. Psychiatry. 2015;6 doi: 10.3389/fpsyt.2015.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herringa R.J. Trauma, PTSD, and the Developing Brain. Curr. Psychiat. Rep. 2017;19 doi: 10.1007/s11920-017-0825-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Köbach A., Schaal S., Hecker T., Elbert T. Psychotherapeutic Intervention in the Demobilization Process: Addressing Combat-related Mental Injuries with Narrative Exposure in a First and Second Dissemination Stage. Clin. Psychol. Psychot. 2017;24:807–825. doi: 10.1002/cpp.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei H., Jing C., Zhuohong Z. Analysis on the relationship between psychological flexibility and the state of anxiety and depression of cancer patients. Chin. J. Behav. Med. Brain Sci. 2015;24:517–520. [Google Scholar]
- Lely J.C.G., Smid G.E., Jongedijk R.A., W. Knipscheer J., Kleber R.J. The effectiveness of narrative exposure therapy: a review, meta-analysis and meta-regression analysis. Eur. J. Psychotraumato. 2019;10 doi: 10.1080/20008198.2018.1550344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak I.W.C., Chu C.M., Pan P.C., Yiu M.G.C., Chan V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiat. 2009;31:318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mørkved N., Thorp S.R. The treatment of PTSD in an older adult Norwegian woman using narrative exposure therapy: a case report. Eur. J. Psychotraumato. 2018;9 doi: 10.1080/20008198.2017.1414561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence, 2018. Post-traumatic stress disorder: NICE guideline. Online verfügbar unter: nice.org.uk/guidance/ng116.
- Neuner F., Onyut P.L., Ertl V., Odenwald M., Schauer E., Elbert T. Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: A randomized controlled trial. J. Consult. Clin. Psych. 2008;76:686–694. doi: 10.1037/0022-006X.76.4.686. [DOI] [PubMed] [Google Scholar]
- Park J., Elbert T., Kim S.J., Park J. The Contribution of Posttraumatic Stress Disorder and Depression to Insomnia in North Korean Refugee Youth. Front. Psychiatry. 2019;10 doi: 10.3389/fpsyt.2019.00211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J.K., Park J., Elbert T., Kim S.J. Effects of Narrative Exposure Therapy on Posttraumatic Stress Disorder, Depression, and Insomnia in Traumatized North Korean Refugee Youth. J. Trauma Stress. 2020;33:353–359. doi: 10.1002/jts.22492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raghuraman S., Stuttard N., Hunt N. Evaluating narrative exposure therapy for post-traumatic stress disorder and depression symptoms: A meta-analysis of the evidence base. Clin. Psychol. Psychot. 2020 doi: 10.1002/cpp.2486. [DOI] [PubMed] [Google Scholar]
- Robjant K., Koebach A., Schmitt S., Chibashimba A., Carleial S., Elbert T. The treatment of posttraumatic stress symptoms and aggression in female former child soldiers using adapted Narrative Exposure therapy – a RCT in Eastern Democratic Republic of Congo. Behav. Res. Ther. 2019;123 doi: 10.1016/j.brat.2019.103482. [DOI] [PubMed] [Google Scholar]
- Said G., King D. Implementing Narrative Exposure Therapy for unaccompanied asylum-seeking minors with post-traumatic stress disorder: A pilot feasibility report. Clin. Child Psychol. P. 2020;25:213–226. doi: 10.1177/1359104519864123. [DOI] [PubMed] [Google Scholar]
- Schauer M., Neuner F., Elbert T. Hogrefe Publishing GmbH; Ashland: 2011. Narrative Exposure Therapy: A Short-Term Treatment for Traumatic Stress Disorders. [Google Scholar]
- Sim M. Psychological trauma of Middle East Respiratory Syndrome victims and bereaved families. Epidemiol. Health. 2016;38 doi: 10.4178/epih.e2016054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Wu B., Tao H., Chai N., Zhao X., Zhen X., Zhou X. Effects and mediating mechanisms of a structured limbs-exercise program on general cognitive function in older adults with mild cognitive impairment: A randomized controlled trial. Int. J. Nurs. Stud. 2020;110 doi: 10.1016/j.ijnurstu.2020.103706. [DOI] [PubMed] [Google Scholar]
- Weathers F., Litz B., Herman D., Juska J., Keane T. Poster session presented at the annual meeting of the International Society for Traumatic Stress Studies. 1993. The PTSD Checklisr (PCL): Reliability, validity, and diagnostic urility. San Antonio, TX. [Google Scholar]
- Weinhold S.L., Göder R., Pabst A., Scharff A., Schauer M., Baier P.C., Aldenhoff J., Elbert T., Seeck-Hirschner M. Sleep recordings in individuals with borderline personality disorder before and after trauma therapy. J. Neural Transm. 2017;124:99–107. doi: 10.1007/s00702-016-1536-3. [DOI] [PubMed] [Google Scholar]
- Wu K.K., Chan S.K., Ma T.M. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS) J. Trauma Stress. 2005;18:39–42. doi: 10.1002/jts.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan B., Cai X., Wang J., Hu X., Li Z., Lu T., An Y. Investigation of psychological stress state of during early convalescence of patients with coronavirus disease 2019 and analysis of its influencing factors. Chin. J. Clin. Neurosurg. 2020;25:531–534. [Google Scholar]
- Zang Y., Hunt N., Cox T. A randomised controlled pilot study: the effectiveness of narrative exposure therapy with adult survivors of the Sichuan earthquake. BMC Psychiatry. 2013;13:41. doi: 10.1186/1471-244X-13-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Liu X., Xue M., Luo L., He G., Feng P., Jiang X., Xie L. The correlation between post-traumatic stress disorder and perceived stress in suspected COVID-19 patients quarantined in hospital. Chin. J. Respiratory Crit. Care Med. 2020;19:325–329. [Google Scholar]
- Zung W.W.K. A Rating Instrument For Anxiety Disorders. Psychosomatics. 1971;12:371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- Zung W.W.K., Richards C., Short M. Self-rating depression scale in an outpatient clinic. Arch. Gen. Psychiatry. 1965;13:508–515. doi: 10.1001/archpsyc.1965.01730060026004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The supporting data can be accessed from the corresponding author (Jun Zhang) on reasonable request.