Abstract
Type 2 diabetes mellitus (T2DM) is an increasing global public health problem, and its prevalence is expected to rise in coming decades. Dipeptidyl peptidase-4 (DPP-4) is a therapeutic target for the management of T2DM, and its inhibitors prevent the degradation of glucose-dependent insulinotropic peptide and glucagon-like peptide 1, and thus, maintain their endogenous levels and lower blood glucose levels. Various medicinal plant extracts and isolated bioactive compounds exhibit DPP-4 inhibitory activity. In this review, we discussed different natural sources that have been shown to have anti-diabetic efficacy with a particular emphasis on DPP-4 inhibition. Furthermore, the effect of DPP-4 inhibition on pancreatic beta cell function, skeletal muscle function, and the glucose-lowering mechanisms were also discussed. We believe that scientists looking for novel compounds with therapeutic promise against T2DM will be able to develop antidiabetic drugs using these natural sources.
Keywords: diabetes, dipeptidyl peptidase-4, medicinal plants, natural compounds
1. Introduction
Type 2 diabetes mellitus (T2DM) is a metabolic condition marked by a prolonged hyperglycemic state caused by a combination of underlying defects, which include insulin tolerance in muscle and liver, and reduced insulin production by pancreatic beta cells [1,2]. T2DM is the most prevalent form of diabetes and accounts for about 91% of all cases, and the disease has been predicted to affect about 366 million people by 2030 [3]. T2DM is marked by enhanced blood glucose (BG) levels and microvascular and macrovascular complications that substantially enhance disease-associated morbidity and mortality, and epidemiological data show that people with diabetes are at slightly higher risk of developing various types of cancer, and musculoskeletal, cardiovascular, and psychiatric disorders [4,5,6,7]. Dipeptidyl peptidase-4 (DPP-4) has emerged as a target in T2DM, and as a result, its inhibitors are attracting increased research interest. DPP-4 accelerates the degradations of the incretin hormones glucagon-like peptide 1 (GLP-1) and glucose-dependent insulinotropic peptide (GIP) by removing a dipeptide from their N termini, resulting in altered glucose homeostasis. Interestingly, DPP4 knockout mice are resistant to diet-induced obesity and have better postprandial glucose balances than their counterparts [8,9].
Insulin controls the metabolism of carbohydrates, fats, and proteins [10], and thus, any defects in insulin synthesis or its activities cause severe metabolic complications. Insulin is produced by pancreatic beta cells, and as T2DM progresses, beta cell functions decline due to rising hyperglycemia and insulin resistance. This cellular decline can start early during the course of T2DM and worsens due to compensatory overload, which accelerates disease progression. Beta cell dysfunction results from deficient glucose sensing, and thus, insulin release, which increases glucose concentrations [11,12].
Many plants have been used to treat diabetes, and interest in medicinal plants as a source of medicines has increased [13,14]. Herbal medicines are considered to importantly complement oral hypoglycemic agents for the management of T2DM, and to have played important roles in the management of diabetes in several countries by preventing diabetic complications and fixing metabolic irregularities [15,16]. We undertook the present review to provide an update on the latest advances made to develop DPP-4 inhibitors derived from natural resources.
2. Dipeptidyl Peptidase-4
DPP-4 (also termed cluster of differentiation 26, CD26) is a serine exopeptidase, a 220 kDa homodimeric type II transmembrane glycoprotein, found on the surfaces of different cell types. DPP-4 cleaves X-proline dipeptides from polypeptides including chemokines, neuropeptides, and peptide hormones at their N-termini, and is expressed in a variety of tissues, including endothelial cells in various vascular beds, which makes it particularly accessible to peptide substrates in gut, stomach, kidney, and liver [17]. The DPP4 gene encodes a 766-amino-acid protein and is located on chromosome 2q23 in man [18]. After being synthesized, DPP4 is immediately integrated into plasma membranes. It is a type II surface protein, which means most of the structure, including its C-terminal domain, is located in the extracellular domain. However, DPP4 can be released from the membrane in response to certain stimuli, such as insulin resistance, tumor necrosis factor-alpha, and chronic low-grade inflammation, resulting in its soluble form [19].
3. Incretin Hormones
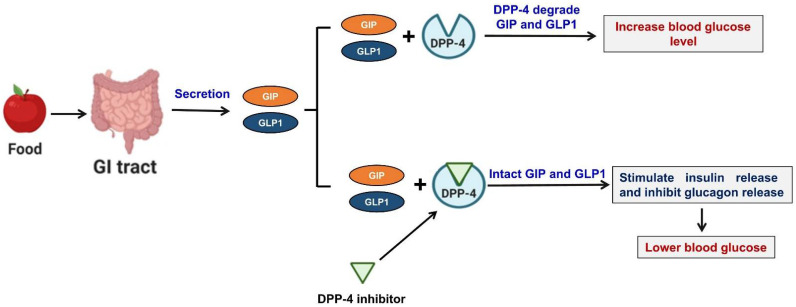
Incretins are a class of metabolic hormones that stimulate a drop in BG levels. Incretin deficiency/resistance plays a vital role in the progression of T2DM. GLP-1 and GIP are the two main human incretins that control the maintenance of glucose homeostasis. GLP-1 is released by intestinal endocrine L-cells, which are often found in ileum and colon, whereas GIP is secreted by intestinal K-cells in the more proximal regions (duodenum and jejunum) of the small intestine [20]. In response to nutrient consumption and/or enhanced BG levels, GLP-1 and GIP are released from the gastrointestinal tract. These two incretins enhance the action of insulin, inhibit the release of glucagon, and reduce liver glucose production, which in healthy individuals lowers BG levels. GLP-1 and GIP are the best-characterized DPP-4 substrates in terms of metabolic effects. In T2DM, endogenous GLP-1 is quickly degraded by DPP-4, and thus, its insulinotropic function is lost. On the other hand, preventing this degradation results in higher GLP-1 levels and enhanced pancreatic islet response, and improved glucose homeostasis. DPP-4 also effectively cleaves GIP, and inhibiting DPP-4 enhances GIP levels and its effects [20]. Therefore, DPP-4 is viewed as an important therapeutic target for the management of T2DM (Figure 1).
Figure 1.
Proposed mechanism of DDP-4 inhibition. In response to nutrient intake and/or an enhanced BG level, incretins (GLP-1 and GIP) are released from the gastrointestinal tract. These two incretins enhance insulin synthesis and secretion and inhibit the release of glucagon, and thus, reduce BG levels in healthy individuals. However, in T2DM, DPP-4 rapidly degrades both incretins and renders them inactive. DPP-4 inhibitors act by preventing DPP-4-induced incretin degradation, increasing intact GLP-1 and GIP levels, and improving glucose homeostasis.
4. Commercialized DPP-4 Inhibitors for the Treatment of Diabetes
GLP-1 and GIP both control insulin release in a glucose-dependent manner. However, endogenous GLP-1 and GIP have plasma half-lives of ~7 and 1 to 2 min, respectively, due to their rapid enzymatic deactivations by DPP-4. The biological activities of these two peptides are determined by the Xaa-pro and Xaa-ala sequences, which also act to prevent non-specific proteolysis [21,22]. Several DPP-4 inhibitors, such as gliptin, are currently approved for the treatment of T2DM. The first DPP-4 inhibitor approved by the FDA was sitagliptin [23], which was followed by vildagliptin [24], saxagliptin [25], alogliptin [26], and linagliptin [27]. More recently, the following inhibitors were approved; anagliptin [28], gemigliptin [29], and teneligliptin [30] in 2012; evogliptin [31], omarigliptin [32], and trelagliptin [33] in 2015; and gosogliptin [34] in 2016. While their binding characteristics and pharmacokinetic properties vary, all DPP-4 inhibitors are orally active, selective for DPP-4, and have a high affinity for the enzyme [35]. Table 1 lists commercialized DPP-4 inhibitors along with their brand name and approval year.
Table 1.
Commercial DPP-4 inhibitors.
| S.No. | DDP-4 Inhibitor | Brand Name | Year of Approval |
|---|---|---|---|
| 1. | Sitagliptin | Januvia | 2006 |
| 2. | Vildagliptin | Galvus | 2007 |
| 3. | Saxagliptin | Onglyza | 2009 |
| 4. | Alogliptin | Nesina and Vipidia | 2010 |
| 5. | Linagliptin | Tradjenta, Trajenta | 2011 |
| 6. | Anagliptin | Suiny | 2012 |
| 7. | Gemigliptin | Zemiglo | 2012 |
| 8. | Teneligliptin | Tenelia | 2012 |
| 9. | Evogliptin | Suganon | 2015 |
| 10. | Omarigliptin | Marizev | 2015 |
| 11. | Trelagliptin | Zafatek | 2015 |
| 12. | Gosogliptin | Satyor | 2016 |
5. DPP-4 Inhibition and Pancreatic Beta Cell Function
DPP-4 antagonists provide long-term, reliable, and effective treatments for T2DM that provide strong glycemic control. GLP-1 and GIP act on G-protein coupled receptors, which are expressed on pancreatic beta and alpha cells and in peripheral tissues, to lower glucose levels [20]. GLP-1 enhances insulin secretion, insulin gene transcription, and insulin biosynthesis by acting on pancreatic beta cells [36].
T2DM causes a gradual reduction in beta cell activity, and thus, to reverse insulin secretory defects, beta cell activity must be restored. Given that GLP-1 has been reported to induce the proliferation and inhibit the apoptosis of beta cells in rodents and to induce beta cell differentiation from human precursor cells [37,38], it seems safe to assume that DPP-4 inhibition enhances GLP-1 levels, and thus, improves beta cell mass and survival. Animal studies have shown that DPP-4 inhibitor promotes islet neogenesis, beta cell regeneration, and/or improved insulin biosynthesis, and thereby preserves or increases beta cell numbers [37,39]. Accordingly, histological analysis of pancreases after DPP-4 inhibitor treatment revealed elevated numbers of islets and beta cells [37].
DPP-4 inhibition has been shown to reduce T2DM-induced beta cell dysfunction and apoptosis in in vitro and in pre-clinical studies. DPP-4 is present in mouse and human islets, and inhibiting islet DPP-4 activity has been shown to have a direct stimulatory effect on GLP-1-dependent insulin secretion [40,41]. A similar effect was demonstrated in db/db diabetic mice after 2 weeks of des-F-sitagliptin treatment, which resulted in enhanced insulin exocytosis by beta cells [42]. In addition, DPP-4 inhibition has been related to beta cell mass and functional increases in several T2DM models [43,44], and the transcriptional activations of anti-apoptotic and pro-survival genes have also been linked to these positive effects in beta cells [45]. Furthermore, the DPP-4 inhibitor linagliptin has been shown to protect isolated human islets from gluco- and lipotoxicity [46], and interestingly, vildagliptin has been shown to have antioxidant properties, as evidenced by dose-dependent reductions in nitric oxide concentrations in serum and pancreatic homogenates of diabetic rats [47].
6. DPP-4 Inhibitors Improve Blood Glucose Response
DPP-4 inhibitors have been shown to decrease BG levels in T2DM patients by continuous glucose monitoring (CGM) [48,49,50]. In addition, various randomized controlled trials have shown by CGM that DPP-4 inhibitors suppress BG levels more efficiently than other agents such as sulfonylureas [51,52] or sodium glucose cotransporter 2 inhibitors [53,54,55] when used in combination with insulin administration [56,57]. DPP-4 inhibitors that enhance insulin secretion and decrease prandial glucagon levels have been shown to improve BG levels [49], and reductions in prandial glucagon levels are considered to underlie improvements in BG levels by DPP-4 inhibitors [58]. Vildagliptin was reported to lower postprandial glucagon levels and improve hyperglycemia in T2DM patients [58], and DPP-4 inhibitors were observed to increase the abilities of alpha and beta cells to detect and respond to hypoglycemia [59]. Furthermore, DPP-4 inhibitors can improve both hyperglycemia and hypoglycemia [60,61]. Moreover, when DPP-4 inhibitors block persistent glucagon oversecretion [58], glucagon responds normally to a drop in BG level and ameliorates hypoglycemia [59]. Overall, these studies show that DPP-4 inhibitors can improve hypoglycemia/hyperglycemia and BG levels in T2DM patients.
7. DPP-4 Inhibition and Skeletal Muscle Function
Skeletal muscles (SM) comprise the largest organ in the body, and thus, process the largest amounts of administered drugs [62]. Furthermore, muscle has recently been reported to release DPP-4 [63]. SM cell cultures were observed to release DPP-4 during differentiation [64], and DPP-4 activity in the bathing medium from intact SM was found to be enhanced by whey protein in situ [65]. DPP-4 inhibitors were also found to reduce SM loss in T2DM patients [66]. Recently, sitagliptin was reported to increased muscle mass and muscle/fat ratio in T2DM [67], and natural DPP-4 inhibitors such as chrysin and galangin were reported to promote SM cell proliferation [68,69]. Furthermore, in a diabetic animal model, myricetin administration reduced DDP-4 expression in muscle [70]. Overall, these studies revealed that DPP-4 inhibitors have a positive effect on SM, increasing SM cell proliferation and the muscle/fat ratio in diabetic patients.
8. DDP-4 Inhibitors from Natural Sources
Nature is a plentiful source of medicinal herbs, and several natural foods that contain bioactive components with health benefits are commonly used as herbal remedies for many life-threatening diseases [71,72,73]. Herbal remedies offered a valuable resource for pharmacological agents for diabetes even before insulin and other pharmacological drugs were discovered, and have become an increasingly important aspect of searches for curative and adjunctive treatments [74]. Below, we detail plants with extracts that inhibit DPP-4 and their corresponding IC50 values; a summary is also provided as a list in Table 2.
Table 2.
Plants extracts that inhibit DPP-4 and their IC50 values.
| S.No. | Plant Name | Family | Plant Part Used | Solvent/Extract Types | IC50 Value | Reference |
|---|---|---|---|---|---|---|
| 1. | Urena lobata | Malvaceae | Roots and leaves | Ethanol | 1.65 mg/mL | [76] |
| 2. | Castanospermum austral | Fabaceae | Seed | Ethanol | 13.96 µg/mL | [80] |
| 3. | Fagonia cretica | Zygophyllaceae | Aerial parts | Crude | 38.1 μg/mL | [81] |
| 4. | Hedera nepalensis | Araliaceae | Aerial parts | Crude | 17.2 μg/mL | [81] |
| 5. | Eugenia jambolana | Myrtaceae | Fruit | Fruit extract | 278.94 µg/mL | [82] |
| 6. | Pterocarpus marsupium | Leguminosae | Heartwood | Heartwood extract | 273.73 µg/mL | [82] |
| 7. | Chenopodium quinoa Willd | Amaranthaceae | Protein hydrolysates | - | 0.88 mg/mL | [83] |
| 8. | Allium sativum | Alliaceae | Garlic bulb | Methanol | 70.9 µg/mL | [85] |
| 9. | Pilea microphylla | Urticaceae | Leaves | Ethanol | 520.4 µg/mL | [86] |
| 10. | Mangifera indica | Anacardiaceae | Leaves | Methanol | 182.7 µg/mL | [88] |
| 11. | Psidium guajava | Myrtaceae | Leaves | Ethanol | 380 μg/mL | [92] |
| 12. | Melicope glabra | Rutaceae | Leaves | Chloroform | 169.40 μg/mL | [93] |
| 13. | Emblica officinalis | Phyllanthaceae | Fruit | Fruit extract | 3770 μg/mL | [97] |
| 14. | Berberis aristata | Berberidaceae | Bark | Methanol | 14.4 µg/mL | [98] |
| 15. | Camellia sinensis | Theaceae | Leaves | Ethanol | 227 µg/mL | [100] |
| 16. | Prunus amygdalus | Rosacease | Seed | Methanol | 162.9 µg/mL | [102] |
| 17. | Avena sativa | Poaceae | Seed | Seed flour | 0.99 mg/mL | [99] |
| 18. | Anogeissus latifolia | Combretaceae | Bark | Water | 754 µg/mL | [79] |
| 19. | Aegle marmelos | Rutaceae | Leaves | Water | 790 µg/mL | [79] |
| 20. | Helichrysum arenarium | Asteraceae | Flowers | Methanol | 41.2 µg/mL | [104] |
8.1. Urena lobata
Urena lobata (Caesar weed or Congo jute) is a traditional herb found in many countries and has promising biological activities. U. lobata root extract had antihyperglycemic effects on streptozotocin-induced diabetic rats [75], and in vitro, an ethanolic extract of U. lobata showed 4-fold greater DPP-4 inhibitory activity (IC50 = 1.65 mg/mL) than water extract (IC50: 6.49 mg/mL) [76].
8.2. Anogeissus latifolia and Aegle marmelos
Anogeissus latifolia and Aegle marmelos are members of the Combretaceae and Rutaceae families, respectively, and are used traditionally to treat diabetes, hemorrhages, diarrhea, asthma, dysentery, skin diseases, leprosy, and hepatopathy [77,78]. A. latifolia and A. marmelos extracts inhibited DPP-4 with IC50 values of 754 and 790 µg/mL, respectively, and improved glucose homeostasis and insulin release in high-fat diet (HFD)-diabetic rats [79].
8.3. Castanospermum austral
Castanospermum austral (also called black bean) is an herb that grows in Australian coastal regions and rainforests. C. australe seed extract inhibited DPP-4 with an IC50 of 13.96 µg/mL, while the control compound diprotin A had an IC50 of 1.543 µg/mL. In addition, in a T2DM animal model, C. australe seed extract lowered BG levels, prevented hyperinsulinemia, and increased glucose tolerance [80].
8.4. Fagonia cretica and Hedera nepalensis
Fagonia cretica (FC) belongs to the Zygophyllaceae (Caltrop) family, and Hedera nepalensis is a member of the family Araliaceae and is found in Nepal and Bhutan, Afghanistan, Pakistan, India, China, Myanmar, Thailand, and Vietnam. The crude extracts of FC and H. nepalensis strongly inhibited DPP-4 with IC50 values of 38.1 and 17.2 μg/mL, respectively. Four compounds (quinovic acid, quinovic acid-3β-O-β-d-glycopyranoside, quinovic acid-3β-O-β-d-glucopyranosyl-(28→1)-β-d-glucopyranosyl ester, and stigmasterol) isolated from FC had IC50 values of 30.7, 57.9, 23.5, and >100 µg/mL, respectively [81].
8.5. Eugenia jambolana and Pterocarpus marsupium
Eugenia jambolana is an evergreen, tropical, fruit-producing tree found in South Asia and South America, while Pterocarpus marsupium is native to India, Nepal, and Sri Lanka. Both P. marsupium and E. jambolana had potent inhibitory effects on DPP-4 with IC50 values of 273.73 and 278.94 µg/mL, respectively [82].
8.6. Chenopodium quinoa Willd
Quinoa (Chenopodium quinoa Willd) is a flowering plant of the amaranth genus Amaranthaceae. Quinoa is a gluten-free grain that has a greater protein content than other grains including wheat, rice, maize, oat, and barley. Analysis of quinoa protein hydrolysate revealed potent DPP-4 inhibitory activity (IC50 0.88 mg/mL) [83].
8.7. Allium sativum
Allium sativum (garlic), a member of the Alliaceae family, is widely used as a spice and as a treatment for a variety of diseases and physiological conditions [84]. Its bulb extract inhibits DPP-4 activity (IC50 70.9 µg/mL) and enhances SM cell proliferation [85].
8.8. Pilea microphylla
Pilea microphylla (the gunpowder plant) is an annual herb found in Florida, Mexico, and tropical Central and Southern America. In vitro, P. microphylla inhibited DPP-4 with an IC50 of 520.4 µg/mL. In addition, in an HFD/streptozotocin-induced diabetic rat, P. microphylla reduced plasma glucose and prevented beta cell destruction [86].
8.9. Mangifera indica
Mangifera indica (MI) is an ayurvedic herb that belongs to the Anacardiaceae family. MI leaf extract has been shown to have hypoglycemic properties [87]. The extract of its leaves was tested in vitro for DPP-4 inhibitory activity, and the results reveal an IC50 of 182.7 µg/mL [88]. The main phytochemical in MI is mangiferin. In HFD/streptozotocin-induced diabetic rat, lower serum DPP-4 levels were associated with improved insulin resistance and improved beta cell function [89].
8.10. Lilium longiflorum
Lilium longiflorum (Liliaceae) bulbs are used as food ingredients and herbal medicines in East Asia. Treatment with the ethyl acetate fraction of L. longiflorum was shown to inhibit DPP-4. Five compounds were purified from the ethyl acetate fraction of L. longiflorum, and compounds 2 and 5 were found to exhibit DPP-4 inhibitory activity with IC50 values of 46.19 and 63.26 µM, respectively [90].
8.11. Coreopsis lanceolata
Coreopsis lanceolata is a perennial herb of the Compositae family. A methanol extract of the flowers of C. lanceolata was found to inhibit DPP-4 activity by 87.2%. Among the various compounds isolated, compounds 2–4, 6, and 7 inhibited DPP-4 in a concentration-dependent manner, with IC50 values ranging from 9.6 to 64.9 µM [91], which suggests that flowers of C. lanceolata and their active components have potential for the treatment of T2DM.
8.12. Psidium guajava L.
Psidium guajava L. (Guava) is a member of the Myrtle family (Myrtaceae). Guava leaves have a long history of use in traditional and conventional medicine that spread from South America to tropical Asia and Africa. Ethanolic guava leaf extract (IC50 380 μg/mL) and flavonol glycosides isolated from the extract inhibited DPP-4 in a dose-dependent manner [92].
8.13. Melicope glabra
Melicope glabra is a tree of the Rutaceae family herb and an important source of flavonoids and coumarins. The plant is native to Sumatra, Peninsular Malaysia, Singapore, Java, and Borneo. The chloroform extract of the leaves of M. glabra effectively inhibited DPP-4 with an IC50 of 169.40 μg/mL. Computational analysis showed that compounds (8) and (7) in this extract are potent DPP-4 inhibitors based on their binding affinities and extensive interactions with important DPP-4 residues [93]. The phytochemical profiles of these compounds indicated their potential as DPP-4 inhibitors.
8.14. Hibiscus rosa-sinensis
Hibiscus rosa-sinensis (HRS) is a tropical flowering plant that is common in Asia and is used in herbal medicine to treat a variety of ailments, such as cough, diarrhea, and diabetes. An ethanol extract of HRS significantly inhibited DPP-4 activity, increased insulin release, and thus, improved glucose tolerance in type 2 diabetic rats [94].
8.15. Annona squamosa
Annona squamosa, commonly called ‘Ata’, is a small tree that belongs to the Annonaceae family and is native to Bangladesh. This herb is well known for its various medicinal properties, which include antioxidant, anti-diabetic, and hepatoprotective effects [95]. Hot water extract of A. squamosa was recently reported to promote cellular glucose absorption and the secretion/action of insulin, and to suppress DPP-4 activity [96].
8.16. Emblica officinalis
Emblica officinalis, commonly known as Indian gooseberry (amla), is a member of the Phyllanthaceae family and used as a folk medicine to treat various diseases, including diabetes. Amla fruit extract inhibited DPP-4 (IC50 3770 μg/mL) and alpha-glucosidases and exhibited antioxidant properties [97].
8.17. Berberis aristata
Berberis aristata belongs to the Berberidaceae family and is a shrub native to the Himalayas in India and Nepal. The roots of this plant have antibacterial, anti-inflammatory, analgesic, antioxidant, and hepatoprotective properties, and its crude bark extract inhibited DPP-4 activity with an IC50 of 14.4 µg/mL [98].
8.18. Avena sativa
Avena sativa, also called the common oat, is a member of the Poaceae family and is widely cultivated in Western China as a staple food. A. sativa is considered a functional food due to its health-promoting properties. Oat flour was found to inhibit DPP-4 with an IC50 of 0.99 mg/mL [99].
8.19. Camellia sinensis
Camellia sinensis is a member of the Theaceae family and native to China and Southeast Asia. The principal component of C. sinensis is caffeine, which acts as a secondary metabolite. Extract of C. sinensis leaves inhibited DPP-4 activity with an IC50 value of 227 µg/mL [100].
8.20. Vitis thunbergii var. taiwaniana
The leaves and fruit of the small-leaf grape (Vitis thunbergii var. taiwaniana, VTT) are smaller than those of Vitis vinifera (standard grape). VTT is used in folk medicine to treat hepatitis, jaundice, diarrhea, and arthritis, and ethanol extracts of the stems and leaves of VTT inhibited DPP-4 activity by 26 and 11%, respectively. The VTT ethanol extracts treatment improved the impaired glucose tolerance of diet-induced obese animals [101].
8.21. Prunus amygdalus
Prunus amygdalus (also called badaam) is a member of the Rosacease family and is widely distributed in India, especially in the Himalayan region. P. amygdalus has several health benefits, which include antioxidative, lipid-reducing, anti-cancer, anti-inflammatory, and immunostimulatory effects. P. amygdalus extract inhibited DPP-4 activity with an IC50 of 162.9 µg/mL [102].
8.22. Ferula assa-foetida
Ferula assa-foetida is an herbaceous plant of the Apiaceae family and has a number of medicinal properties. The ethanolic fraction of F. assa-foetida inhibited DPP-4 activity by 24.5% [103].
8.23. Helichrysum arenarium
Helichrysum arenarium is a perennial herbaceous plant of the Asteraceae family and is native to Europe. In European folk medicine, the medicinal properties of this plant are attributed to its choleretic, cholagogic, hepatoprotective, and detoxifying activities. H. arenarium methanol extract inhibited DPP-4 enzymatic activity with an IC50 of 41.2 µg/mL [104].
9. Natural Phytochemicals
Natural products are an exceptionally rich resource for drug discovery, drug development, and clinical medicine [105]. A summary of natural compounds with DPP-4 inhibitory activity and their corresponding IC50 values is provided in Table 3.
Table 3.
Natural compounds with DPP-4 inhibition and their corresponding IC50 values.
| S.No. | Phytochemicals | IC50 Values | References |
|---|---|---|---|
| 1. | Alkaloids | ||
| Berberine | 13.3 µM | [106] | |
| 2. | Flavonoids | ||
| Cyanidin 3-O-glucoside | 125.1 µM | [108] | |
| Anthocyanins | 0.07 µM | [107] | |
| Emodin | 5.76 µM | [109] | |
| Rutin | 485 µM | [110] | |
| Isoquercetin | 96.8 µM | [114] | |
| Cirsimaritin | 0.43 µM | [112] | |
| Hispidulin | 0.49 µM | [112] | |
| Naringenin | 2.5 µM | [112] | |
| Quercetin | 4.02 nmol/mL | [113] | |
| Galangin | 40.13 µM | [69] | |
| Kaempferol 7-O-α-l-rhamnoside | 20.81 µM | [115] | |
| Vitexin | 33.12 µM | [115] | |
| Rutin | 32.93 µM | [115] | |
| 3. | Phenols | ||
| Hopeaphenol | 401 µM | [101] | |
| (+)-vitisin A | 90.75 µM | [101] | |
| (−)-vitisin B | 15.3 µM | [101] | |
| Resveratrol | 0.6 nM | [107] | |
| Luteolin | 0.12 µM | [107] | |
| Apigenin | 0.14 µM | [107] | |
| Flavone | 0.17 µM | [107] | |
| Coumarins | 54.83 nmol/mL | [113] | |
| Myricetin | 4.8 μM | [70] | |
| 4. | Glycosides | ||
| Kaempferol-3-O-β-gulcopyranosyl-(1→2)-β-galactopyranosyl-7-O-α-rhamnopyranoside | 27.89 μM | [121] | |
| 36.52 μM | |||
| Kaempferol-3-O-β-gulcopyranosyl-(1→2)-[α-rhamnopyranosyl (1→6)]-β-galactopyranosyl-7-O-α rhamnopyranoside | 37.01 μM | [121] | |
| Kaempferol-3-O-α-rhamnosyl (1→6)-O-β-galactopyranoside-7-O-α-rhamnopyranoside | 23.1 μM | [104] | |
| Chalconaringenin 2′-O-β-Dglucopyranoside | 24.3 μM | [104] | |
| Aureusidin 6-O-β-d-glucopyranoside | |||
| Quercetin-3-O-β-d-glucosyl-7-O-α-rhamnoside | 0.194 µg/mL | [122] | |
| Isorhamnetin-7-O-β-neohesperidoside | 0.573 µg/mL | [122] | |
| Isorhamnetin-3-O-β-d-glucoside | 0.345 µg/mL | [122] | |
| Kaempferol-40-methoxy-3,7-O-α-dirhamnoside | 0.281 µg/mL | [122] |
9.1. Alkaloids
Coptis chinensis (family: Ranunculaceae) is a goldthread species native to China. Its rhizomes contain the isoquinoline alkaloids berberine, palmatine, and coptisine and are used in traditional Chinese medicine. In vitro, berberine has a strong DPP-4 inhibitory effect with an IC50 value of 13.3 µM [106]. Molecular docking results show 7-deoxy-6-epi-castanospermine derived from C. australe inhibited DPP-4 with the same potency as berberine [80].
9.2. Flavonoids
The beneficial health effects of fruits and vegetables have been linked to their high flavonoid contents. DPP-4 activity was potently inhibited by anthocyanins isolated from blueberry/blackberry wine blends with an IC50 of 0.07 µM [107]. Cyanidin 3-O-glucoside inhibited DPP-4 with an IC50 of 125.1 µM [108].
Emodin obtained from Rheum palmatum inhibited DPP-4 in vitro with an IC50 of 5.76 µM [109]. Citrus flavonoids have also been shown to have DPP-4 inhibitory activity; rutin was the most active inhibitor with an IC50 of 485 µM [110]. Naringin is abundant in orange peel and has been shown to inhibit DPP-4 in vitro and in vivo and to enhance insulin levels, and thus, is considered an option for the low-cost treatment of diabetes [111].
Rosemary and marjoram extracts were found to inhibit DPP-4 with IC50 values of 16 and 29 µM, respectively, and the isolated flavonoids cirsimaritin, hispidulin, and naringenin inhibited DDP-4 activity with IC50 values of 0.43, 0.49, and 2.5 µM, respectively [112].
Quercetin is a plant-derived flavonol that has been shown to regulate hyperglycemia and oxidative stress. Molecular docking studies showed that quercetin and galangin bind strongly with DPP-4 and inhibit its activity with IC50 values of 4.02 and 40.13 µM, respectively [69,113]. Furthermore, isoquercetin from Apocynum cannabinum inhibited DPP-4 with an IC50 of 96.8 µM [114].
Smilax china plants are found in tropical and temperate regions worldwide, especially in East Asia and North America. Its flavonoids kaempferol 7-O-α-l-rhamnoside, vitexin, and rutin were shown to inhibit DPP-4 with IC50 values of 20.81, 33.12, and 32.93 µM, respectively [115].
9.3. Terpenoids
Polyathia longifolia (PL) is used in traditional Indian medicine as a febrifuge and treatment for indigestion. PL has been shown to possess anticancer, antimicrobial, immune-modulating, and anti-ulcer properties [116], and 16-hydroxycleroda-3,13-dien-15,16-olide from PL was found to inhibit DPP-4 activity and to lower BG levels in diabetic mice [117].
The chloroform extract of Inonotus obliquus mycelium was also found to inhibit DPP-4. Nineteen compounds were isolated from I. obliquus mycelium powders. Molecular docking showed that compounds 5, 8, 9, 14, and 15 could be the active compounds responsible for DPP-4 inhibition [118].
9.4. Phenols
VTT-derived hopeaphenol, (+)-vitisin A, and (−)-vitisin B inhibited DPP-4 with IC50 values of 401, 90.75, and 15.3 μM, respectively [101]. Resveratrol, luteolin, apigenin, and flavone potently inhibit DPP-4 with IC50 values of 0.6 ± 0.4 nM, 0.12 ± 0.01, 0.14 ± 0.02, 0.17 ± 0.01 μM, respectively, which were lower than the IC50 of the diprotin A control (4.21 ± 2.01 μM) [107].
Coumarins are heterocyclic molecules and have been associated with a variety of health benefits, which include antithrombotic, anti-inflammatory, and vasodilatory effects. Coumarins inhibited DPP-4 with an IC50 of 54.83 nmol/mL [113]. In a molecular docking study, curcumin was found to bind strongly with DPP-4, and in vitro curcumin inhibited DPP-4 activity by up to 50% [119].
Macrotyloma uniflorum (horsegram) is a legume grown mainly in dry regions of Australia, Burma, India, and Sri Lanka and contains high concentrations of myricetin, which has been shown to have anti-hyperglycemic properties. Myricetin also inhibited DPP-4 (IC50 of 4.8 μM), and thus, increased serum GLP-1 and insulin levels and ameliorated the manifestations of T2DM [70].
9.5. Glycosides
Foods contain a wide range of bioactive molecules, and their different scaffolds and functionalities make them the most important source of possible leads for drug discovery. Virtual screening of a polyphenol-rich food database for potential DPP-4 inhibitors resulted in the identification of chrysin, and an in vitro enzyme assay showed that chrysin inhibits DPP-4 in a concentration-dependent manner [120].
Lentils are the edible seeds of Lens culinaris (family Fabaceae), a pulse crop, and have long been grown for human consumption in Europe, the Middle East, Africa, and Asia. Three flavonol glycosides, kaempferol-3-O-β-gulcopyranosyl-(1→2)-β-galactopyranosyl-7-O-α-rhamnopyranoside, kaempferol-3-O-β-gulcopyranosyl-(1→2)-[α-rhamnopyranosyl (1→6)]-β-galactopyranosyl-7-O-α-rhamnopyranoside, and robinin (kaempferol-3-O-α-rhamnosyl (1→6)-O-β-galactopyranoside-7-O-α-rhamnopyranoside) isolated from L. culinaris seeds were found to inhibit DPP-4 activity in a dose-dependent manner with IC50 values of 27.89, 36.52, and 37.01 μM, respectively; molecular docking analysis revealed that these compounds readily fit within the DPP-4 active sites [121].
In Egyptian folk medicine, the herb Cleome droserifolia is used to treat diabetes, stomach aches, skin allergies, and open wounds. Five major flavonol glycosides were isolated from an aqueous extract of C. droserifolia, and four of these, quercetin-3-O-β-d-glucosyl-7-O-α-rhamnoside, isorhamnetin-7-O-β-neohesperidoside, isorhamnetin-3-O-β-d-glucoside, and kaempferol-40-methoxy-3,7-O-α-dirhamnoside, showed significant DPP-4 inhibition with IC50 values of 0.194, 0.573, 0.345, and 0.281 µg/mL, respectively. In addition, these compounds inhibited aldose reductase and reduced oxidative stress, suggesting their potential use for addressing problems associated with diabetes [122].
The flavonol glycosides (chalconaringenin 2′-O-β-d glucopyranoside and aureusidin 6-O-β-d-glucopyranoside) derived from H. arenarium inhibited DPP-4 with IC50 values of 23.1 and 24.3 μM, respectively [104].
10. Bioactive Peptides
The herbaceous annual plant Phaseolus vulgaris (PV) is cultivated globally for its edible dry seeds or unripe berries. Protein fractions derived from PV were found to inhibit DPP-4 activity by 96.7%. In addition, bioactive peptides were isolated from a protein isolate of PV. EGLELLLLLLAG, AKSPLF, and FEELN peptides inhibited DPP-4 more effectively in silico with free binding energy values of −9.8, −9.6, and −9.5 kcal/mol, respectively, than the reference compound sitagliptin (−8.67 kcal/mol) [123]. In another study, protein digests and pure peptides derived from Mexican black and Brazilian Carioca beans inhibited DPP-4 with IC50 values ranging from 0.03 to 0.87 mg dry weight/mL [124]. These studies suggest that peptides derived from bean protein isolates can inhibit DPP-4.
Oryza sativa L. (rice) bran protein hydrolysates inhibited DPP-4 enzyme with an IC50 of 1.45 ± 0.13 mg/mL [125]. When Umamizyme G and Bioprase SP were used to defat and hydrolyze rice bran protein fractions, dipeptides digested with Umamizyme G inhibited DPP-4 with an IC50 of 2.3 ± 0.1 mg/mL [126]. Proteins derived from Amaranthus hypochondriacus were subjected to simulated gastrointestinal digestion, and this resulted in the formation of bioactive peptides that suppressed DPP-4 in a concentration-dependent manner with an IC50 of 1.1 mg/mL [127]. Glycine max (soybean) and Lupinus albus (lupin) protein hydrolysates contain bioactive peptides, and Soy 1 (IAVPTGVA) and Lup 1 (LTFPGSAED) effectively inhibited DPP-4 with IC50 values of 106 and 228 µM, respectively [128]. Gastrointestinal digestion of proteins derived from Phalaris canariensis (canary) seeds inhibited DPP-4 by 43.5% [129], and enzymatic digestion of quinoa proteins with papain also resulted in DPP-4 inhibition with an IC50 of 0.88 ± 0.05 mg/mL [83]. In a study that used quinoa protein to simulate duodenal digestion, the fraction collected after 120 min of digestion most inhibited DPP-4 with an IC50 of 0.84 ± 0.07 mg protein/mL [130].
DPP-4 inhibitory activity was found in peptides isolated from tuna cooking juice hydrolyzed by the enzymes protease XXIII (PR) and orientase (OR). The amino acid sequences of three peptides isolated from PR and OR hydrolysates were PGVGGPLGPIGPCYE (1412.7 Da), CAYEWQRPVDRIR (1690.8 Da), and PACGGFYISGRPG (1304.6 Da), and all three inhibited DPP-4 in a dose-dependent manner [131]. GPAE (372.4 Da) and GPGA (300.4 Da) peptide sequences obtained from Atlantic salmon skin gelatin also potently inhibited DPP-4 [132]. Several peptide sequences in an aqueous Palmaria palmata protein extract hydrolyzed with Corolase PP inhibited DPP-4, and three of these peptides (ILAP, LLAP, and MAGVDHI), when purified, potently inhibited DPP-4 with IC50 values ranging from 43.40 to 159.37 µM [133]. In addition, peptides obtained from oats, buckwheat, and barley inhibited DPP-4 with IC50 values from 0.13 to 8.15 mg/mL, and LQAFEPLR inhibited DPP4 in vitro with an IC50 value of 103.5 µM [99]. The bioactive peptides that inhibit DPP-4 and their corresponding IC50 values have been listed in Table 4.
Table 4.
Bioactive peptides with DPP-4 inhibition and their corresponding IC50 values.
| S.No. | Plant | Peptide Sequence | IC50 Value | References |
|---|---|---|---|---|
| 1. | Phaseolus vulgaris | KTYGL | 0.03 mg DW/mL | [124] |
| KKSSG | 0.64 mg DW/mL | [124] | ||
| GGGLHK | 0.61 mg DW/mL | [124] | ||
| CPGNK | 0.87 mg DW/mL | [124] | ||
| 2. | Oryza sativa | IP | 2.3 ± 0.1 mg/ml | [126] |
| 3. | Glycine max | IAVPTGVA | 106 µM | [128] |
| 4. | Lupinus albus | LTFPGSAED | 228 µM | [128] |
| 5. | Palmaria palmata | ILAP | 43.40 µM | [133] |
| LLAP | 53.67 µM | [133] | ||
| MAGVDHI | 159.37 µM | [133] | ||
| 6. | Avena sativa | LQAFEPLR | 103.5 µM | [99] |
11. Conclusions
At the molecular level, DPP4 inhibitors work by preventing the degradation of GIP and GLP1, and thus, preserve their endogenous levels and reduce BG levels. Nature has many herbal plants that have long been used to treat diabetes. In this review article, we detail the medicinal plants and their bioactive compounds that inhibit DPP-4 activity. Of these compounds, resveratrol, quercetin, and coumarins are highly effective DPP-4 inhibitors with IC50 values in the nanomolar range. Other compounds (flavonoids and phenolics) have the additional benefit of being present in a variety of functional foods. DPP-4 inhibitors improve pancreatic beta cell function and enhance SM cell proliferation. Studies on natural DPP-4 inhibitors offer a powerful means of developing novel treatments for T2DM, and it is hoped this review will help researchers searching for safer, natural DPP-4 inhibitors for the treatment of diabetes.
Abbreviations
T2DM: type 2 diabetes mellitus, BG: blood glucose, DPP-4: dipeptidyl peptidase-4, GLP-1: glucagon-like peptide 1, GIP: glucose-dependent insulinotropic peptide, SM: skeletal muscles, HFD: high-fat diet, FC: Fagonia cretica, MI: Mangifera indica, HRS: Hibiscus rosa-sinensis, VTT: Vitis thunbergii var. taiwaniana, PL: Polyathia longifolia, PV: Phaseolus vulgaris, PR: protease XXIII, OR: orientase.
Author Contributions
Conceptualization, S.S. and I.C.; writing—original draft preparation, S.S. and K.A.; writing—review and editing, E.-J.L., S.-S.A., and J.-H.L.; funding acquisition, I.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Korean Ministry of Education (grant no. 2020R1A6A1A03044512) and by the NRF funded by the Korean government (MSIP: grant nos. NRF-2021R1A2C2004177 and NRF-2019R1C1C1006542).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Campbell R.K. Fate of the beta-cell in the pathophysiology of type 2 diabetes. J. Am. Pharm. Assoc. 2009;49:S10–S15. doi: 10.1331/JAPhA.2009.09076. [DOI] [PubMed] [Google Scholar]
- 2.Surampudi P.N., John-Kalarickal J., Fonseca V.A. Emerging Concepts in the Pathophysiology of Type 2 Diabetes Mellitus. Mt. Sinai J. Med. A J. Transl. Pers. Med. 2009;76:216–226. doi: 10.1002/msj.20113. [DOI] [PubMed] [Google Scholar]
- 3.Wild S., Roglic G., Green A., Sicree R., King H. Global Prevalence of Diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 4.Giovannucci E., Harlan D.M., Archer M.C., Bergenstal R.M., Gapstur S.M., Habel L.A., Pollak M., Regensteiner J.G., Yee D. Diabetes and Cancer: A consensus report. Diabetes Care. 2010;33:1674–1685. doi: 10.2337/dc10-0666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sozen T., Center A.P.A.E.E., Basaran N.C., Tinazli M., Ozisik L. Musculoskeletal problems in diabetes mellitus. Eur. J. Rheumatol. 2018;5:258–265. doi: 10.5152/eurjrheum.2018.18044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leon B.M., Maddox T.M. Diabetes and cardiovascular disease: Epidemiology, biological mechanisms, treatment recommendations and future research. World J. Diabetes. 2015;6:1246–1258. doi: 10.4239/wjd.v6.i13.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Atram A.A. A review of the bidirectional relationship between psychiatric disorders and diabetes mellitus. Neurosciences. 2018;23:91–96. doi: 10.17712/nsj.2018.2.20170132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Conarello S.L., Li Z., Ronan J., Roy R.S., Zhu L., Jiang G., Liu F., Woods J., Zycband E., Moller D.E., et al. Mice lacking dipeptidyl peptidase IV are protected against obesity and insulin resistance. Proc. Natl. Acad. Sci. USA. 2003;100:6825–6830. doi: 10.1073/pnas.0631828100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marguet D., Baggio L., Kobayashi T., Bernard A.-M., Pierres M., Nielsen P.F., Ribel U., Watanabe T., Drucker D.J., Wagtmann N. Enhanced insulin secretion and improved glucose tolerance in mice lacking CD26. Proc. Natl. Acad. Sci. USA. 2000;97:6874–6879. doi: 10.1073/pnas.120069197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gianani R. Beta cell regeneration in human pancreas. Semin. Immunopathol. 2010;33:23–27. doi: 10.1007/s00281-010-0235-7. [DOI] [PubMed] [Google Scholar]
- 11.Cerf M.E. Beta Cell Dysfunction and Insulin Resistance. Front. Endocrinol. 2013;4:37. doi: 10.3389/fendo.2013.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saisho Y. β-cell dysfunction: Its critical role in prevention and management of type 2 diabetes. World J. Diabetes. 2015;6:109–124. doi: 10.4239/wjd.v6.i1.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kooti W., Farokhipour M., Asadzadeh Z., Ashtary-Larky D., Asadi-Samani M. The role of medicinal plants in the treatment of diabetes: A systematic review. Electron. Physician. 2016;8:1832–1842. doi: 10.19082/1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.KAMESWARA R.B., Giri R., Kesavulu M., Apparao C. Herbal medicine: In the management of diabetes mellitus. Manphar Vaidya Patrika. 1997;1:33–35. [Google Scholar]
- 15.Chang C.L.T., Lin Y., Bartolome A.P., Chen Y.-C., Chiu S.-C., Yang W.-C. Herbal Therapies for Type 2 Diabetes Mellitus: Chemistry, Biology, and Potential Application of Selected Plants and Compounds. Evid. Based Complement. Altern. Med. 2013;2013:1–33. doi: 10.1155/2013/378657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gao Y., Zhang Y., Zhu J., Li B., Li Z., Zhu W., Shi J., Jia Q., Li Y. Recent progress in natural products as DPP-4 inhibitors. Futur. Med. Chem. 2015;7:1079–1089. doi: 10.4155/fmc.15.49. [DOI] [PubMed] [Google Scholar]
- 17.Fukasawa K.M., Sahara N., Harada M., Kondo Y., Nagatsu I. Immunohistochemical localization of dipeptidyl aminopeptidase IV in rat kidney, liver, and salivary glands. J. Histochem. Cytochem. 1981;29:337–343. doi: 10.1177/29.3.6787113. [DOI] [PubMed] [Google Scholar]
- 18.Matteucci E., Giampietro O. Dipeptidyl peptidase-4 (CD26): Knowing the function before inhibiting the enzyme. Curr. Med. Chem. 2009;16:2943–2951. doi: 10.2174/092986709788803114. [DOI] [PubMed] [Google Scholar]
- 19.Lee S.A., Kim Y.R., Yang E.J., Kwon E.J., Kim S.H., Kang S.H., Park D.B., Oh B.C., Kim J., Heo S.T., et al. CD26/DPP4 levels in peripheral blood and T cells in patients with type 2 diabetes mellitus. J. Clin. Endocrinol. Metab. 2013;98:2553–2561. doi: 10.1210/jc.2012-4288. [DOI] [PubMed] [Google Scholar]
- 20.Seino Y., Fukushima M., Yabe D. GIP and GLP-1, the two incretin hormones: Similarities and differences. J. Diabetes Investig. 2010;1:8–23. doi: 10.1111/j.2040-1124.2010.00022.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Juillerat-Jeanneret L. Dipeptidyl peptidase IV and its inhibitors: Therapeutics for type 2 diabetes and what else? J. Med. Chem. 2014;57:2197–2212. doi: 10.1021/jm400658e. [DOI] [PubMed] [Google Scholar]
- 22.Deacon C.F. Dipeptidyl peptidase 4 inhibitors in the treatment of type 2 diabetes mellitus. Nat. Rev. Endocrinol. 2020;16:642–653. doi: 10.1038/s41574-020-0399-8. [DOI] [PubMed] [Google Scholar]
- 23.Plosker G.L. Sitagliptin: A review of its use in patients with type 2 diabetes mellitus. Drugs. 2014;74:223–242. doi: 10.1007/s40265-013-0169-1. [DOI] [PubMed] [Google Scholar]
- 24.Keating G.M. Vildagliptin: A review of its use in type 2 diabetes mellitus. Drugs. 2014;74:587–610. doi: 10.1007/s40265-014-0199-3. [DOI] [PubMed] [Google Scholar]
- 25.Dhillon S. Saxagliptin: A Review in Type 2 Diabetes. Drugs. 2015;75:1783–1796. doi: 10.1007/s40265-015-0473-z. [DOI] [PubMed] [Google Scholar]
- 26.Keating G.M. Alogliptin: A review of its use in patients with type 2 diabetes mellitus. Drugs. 2015;75:777–796. doi: 10.1007/s40265-015-0385-y. [DOI] [PubMed] [Google Scholar]
- 27.Lajara R. Use of the dipeptidyl peptidase-4 inhibitor linagliptin in combination therapy for type 2 diabetes. Expert Opin. Pharmacother. 2012;13:2663–2671. doi: 10.1517/14656566.2012.741591. [DOI] [PubMed] [Google Scholar]
- 28.Nishio S., Abe M., Ito H. Anagliptin in the treatment of type 2 diabetes: Safety, efficacy, and patient acceptability. Diabetes Metab. Syndr. Obes. 2015;8:163–171. doi: 10.2147/DMSO.S54679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim S.H., Lee S.H., Yim H.J. Gemigliptin, a novel dipeptidyl peptidase 4 inhibitor: First new anti-diabetic drug in the history of Korean pharmaceutical industry. Arch. Pharmacal Res. 2013;36:1185–1188. doi: 10.1007/s12272-013-0171-x. [DOI] [PubMed] [Google Scholar]
- 30.Scott L.J. Teneligliptin: A review in type 2 diabetes. Clin. Drug Investig. 2015;35:765–772. doi: 10.1007/s40261-015-0348-9. [DOI] [PubMed] [Google Scholar]
- 31.McCormack P.L. Evogliptin: First Global Approval. Drugs. 2015;75:2045–2049. doi: 10.1007/s40265-015-0496-5. [DOI] [PubMed] [Google Scholar]
- 32.Biftu T., Sinha-Roy R., Chen P., Qian X., Feng D., Kuethe J.T., Scapin G., Gao Y.D., Yan Y., Krueger D., et al. Omarigliptin (MK-3102): A novel long-acting DPP-4 inhibitor for once-weekly treatment of type 2 diabetes. J. Med. Chem. 2014;57:3205–3212. doi: 10.1021/jm401992e. [DOI] [PubMed] [Google Scholar]
- 33.Kaku K. First novel once-weekly DPP-4 inhibitor, trelagliptin, for the treatment of type 2 diabetes mellitus. Expert Opin. Pharmacother. 2015;16:2539–2547. doi: 10.1517/14656566.2015.1099630. [DOI] [PubMed] [Google Scholar]
- 34.Sharma R., Sun H., Piotrowski D.W., Ryder T.F., Doran S.D., Dai H., Prakash C. Metabolism, excretion, and pharmacokinetics of ((3,3-difluoropyrrolidin-1-yl)((2S,4S)-4-(4-(pyrimidin-2-yl)piperazin-1-yl)pyrrol idin-2-yl)methanone, a dipeptidyl peptidase inhibitor, in rat, dog and human. Drug Metab. Dispos. 2012;40:2143–2161. doi: 10.1124/dmd.112.047316. [DOI] [PubMed] [Google Scholar]
- 35.Deacon C.F. Dipeptidyl peptidase-4 inhibitors in the treatment of type 2 diabetes: A comparative review. Diabetes Obes. Metab. 2011;13:7–18. doi: 10.1111/j.1463-1326.2010.01306.x. [DOI] [PubMed] [Google Scholar]
- 36.Meloni A.R., DeYoung M.B., Lowe C., Parkes D.G. GLP-1 receptor activated insulin secretion from pancreatic β-cells: Mechanism and glucose dependence. Diabetes Obes. Metab. 2013;15:15–27. doi: 10.1111/j.1463-1326.2012.01663.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pospisilik J.A., Martin J., Doty T., Ehses J.A., Pamir N., Lynn F.C., Piteau S., Demuth H.U., McIntosh C.H., Pederson R.A. Dipeptidyl peptidase IV inhibitor treatment stimulates β-cell survival and islet neogenesis in streptozotocin-induced diabetic rats. Diabetes. 2003;52:741–750. doi: 10.2337/diabetes.52.3.741. [DOI] [PubMed] [Google Scholar]
- 38.Ahren B., Foley J.E. Improved glucose regulation in type 2 diabetic patients with DPP-4 inhibitors: Focus on alpha and beta cell function and lipid metabolism. Diabetologia. 2016;59:907–917. doi: 10.1007/s00125-016-3899-2. [DOI] [PubMed] [Google Scholar]
- 39.Argun-Kurum G., Kaya-Dagistanli F., Ozturk M. DPP4 inhibitor induces beta cell regeneration and DDR-1 protein expression as an endocrine progenitor cell marker in neonatal STZ-diabetic rats. Pharmacol. Rep. 2019;71:721–731. doi: 10.1016/j.pharep.2019.03.008. [DOI] [PubMed] [Google Scholar]
- 40.Omar B.A., Liehua L., Yamada Y., Seino Y., Marchetti P., Ahren B. Dipeptidyl peptidase 4 (DPP-4) is expressed in mouse and human islets and its activity is decreased in human islets from individuals with type 2 diabetes. Diabetologia. 2014;57:1876–1883. doi: 10.1007/s00125-014-3299-4. [DOI] [PubMed] [Google Scholar]
- 41.Bugliani M., Syed F., Paula F.M.M., Omar B.A., Suleiman M., Mossuto S., Grano F., Cardarelli F., Boggi U., Vistoli F., et al. DPP-4 is expressed in human pancreatic beta cells and its direct inhibition improves beta cell function and survival in type 2 diabetes. Mol. Cell. Endocrinol. 2018;473:186–193. doi: 10.1016/j.mce.2018.01.019. [DOI] [PubMed] [Google Scholar]
- 42.Nagamatsu S., Ohara-Imaizumi M., Nakamichi Y., Aoyagi K., Nishiwaki C. DPP-4 inhibitor des-F-sitagliptin treatment increased insulin exocytosis from db/db mice beta cells. Biochem. Biophys. Res. Commun. 2011;412:556–560. doi: 10.1016/j.bbrc.2011.07.119. [DOI] [PubMed] [Google Scholar]
- 43.Duttaroy A., Voelker F., Merriam K., Zhang X., Ren X., Subramanian K., Hughes T.E., Burkey B.F. The DPP-4 inhibitor vildagliptin increases pancreatic beta cell mass in neonatal rats. Eur. J. Pharmacol. 2011;650:703–707. doi: 10.1016/j.ejphar.2010.10.062. [DOI] [PubMed] [Google Scholar]
- 44.Takeda Y., Fujita Y., Honjo J., Yanagimachi T., Sakagami H., Takiyama Y., Makino Y., Abiko A., Kieffer T.J., Haneda M. Reduction of both beta cell death and alpha cell proliferation by dipeptidyl peptidase-4 inhibition in a streptozotocin-induced model of diabetes in mice. Diabetologia. 2012;55:404–412. doi: 10.1007/s00125-011-2365-4. [DOI] [PubMed] [Google Scholar]
- 45.Han S.J., Choi S.E., Kang Y., Jung J.G., Yi S.A., Kim H.J., Lee K.W., Kim D.J. Effect of sitagliptin plus metformin on beta-cell function, islet integrity and islet gene expression in Zucker diabetic fatty rats. Diabetes Res. Clin. Pract. 2011;92:213–222. doi: 10.1016/j.diabres.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 46.Shah P., Ardestani A., Dharmadhikari G., Laue S., Schumann D.M., Kerr-Conte J., Pattou F., Klein T., Maedler K. The DPP-4 inhibitor linagliptin restores beta-cell function and survival in human isolated islets through GLP-1 stabilization. J. Clin. Endocrinol. Metab. 2013;98:E1163–E1172. doi: 10.1210/jc.2013-1029. [DOI] [PubMed] [Google Scholar]
- 47.Akarte A.S., Srinivasan B.P., Gandhi S. Vildagliptin selectively ameliorates GLP-1, GLUT4, SREBP-1c mRNA levels and stimulates beta-cell proliferation resulting in improved glucose homeostasis in rats with streptozotocin-induced diabetes. J. Diabetes Complicat. 2012;26:266–274. doi: 10.1016/j.jdiacomp.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 48.Tanaka S., Suzuki K., Aoki C., Niitani M., Kato K., Tomotsune T., Aso Y. Add-on treatment with teneligliptin ameliorates glucose fluctuations and improves glycemic control index in Japanese patients with type 2 diabetes on insulin therapy. Diabetes Technol. Ther. 2014;16:840–845. doi: 10.1089/dia.2014.0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mori Y., Taniguchi Y., Miyazaki S., Yokoyama J., Utsunomiya K. Effects of add-on treatment with sitagliptin on narrowing the range of glucose fluctuations in Japanese type 2 diabetes patients receiving insulin therapy. Diabetes Technol. Ther. 2013;15:237–240. doi: 10.1089/dia.2012.0214. [DOI] [PubMed] [Google Scholar]
- 50.Ishikawa-Tanaka T., Hosojima M., Kabasawa H., Kaseda R., Yasukawa R., Yata Y., Kuwahara S., Kono E., Takata T., Iino N., et al. Effects of DPP-4 Inhibitors on Blood Glucose Variability in Japanese Patients with Type 2 Diabetes on Maintenance Hemodialysis: A Prospective Observational Exploratory Study. Diabetes Ther. 2020;11:2845–2861. doi: 10.1007/s13300-020-00928-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Suzuki R., Eiki J.I., Moritoyo T., Furihata K., Wakana A., Ohta Y., Tokita S., Kadowaki T. Effect of short-term treatment with sitagliptin or glibenclamide on daily glucose fluctuation in drug-naive Japanese patients with type 2 diabetes mellitus. Diabetes Obes. Metab. 2018;20:2274–2281. doi: 10.1111/dom.13364. [DOI] [PubMed] [Google Scholar]
- 52.Kim G., Oh S., Jin S.M., Hur K.Y., Kim J.H., Lee M.K. The efficacy and safety of adding either vildagliptin or glimepiride to ongoing metformin therapy in patients with type 2 diabetes mellitus. Expert Opin. Pharmacother. 2017;18:1179–1186. doi: 10.1080/14656566.2017.1353080. [DOI] [PubMed] [Google Scholar]
- 53.Kwak S.H., Hwang Y.C., Won J.C., Bae J.C., Kim H.J., Suh S., Lee E.Y., Lee S., Kim S.Y., Kim J.H. Comparison of the effects of gemigliptin and dapagliflozin on glycaemic variability in type 2 diabetes: A randomized, open-label, active-controlled, 12-week study (STABLE II study) Diabetes Obes. Metab. 2020;22:173–181. doi: 10.1111/dom.13882. [DOI] [PubMed] [Google Scholar]
- 54.Cho K.Y., Nomoto H., Nakamura A., Kawata S., Sugawara H., Takeuchi J., Nagai S., Tsuchida K., Omori K., Yokoyama H., et al. Favourable effect of the sodium-glucose co-transporter-2 inhibitor canagliflozin plus the dipeptidyl peptidase-4 inhibitor teneligliptin in combination on glycaemic fluctuation: An open-label, prospective, randomized, parallel-group comparison trial (the CALMER study) Diabetes Obes. Metab. 2020;22:458–462. doi: 10.1111/dom.13879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fuchigami A., Shigiyama F., Kitazawa T., Okada Y., Ichijo T., Higa M., Hiyoshi T., Inoue I., Iso K., Yoshii H., et al. Efficacy of dapagliflozin versus sitagliptin on cardiometabolic risk factors in Japanese patients with type 2 diabetes: A prospective, randomized study (DIVERSITY-CVR) Cardiovasc. Diabetol. 2020;19:1. doi: 10.1186/s12933-019-0977-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lyu F.P., Huang B.K., Su W.J., Yan F.F., Zeng J.Y., Chen Z., Zhang Y.X., Wang S.H., Huang Y.X., Zhang M.L., et al. Efficacy of Vildagliptin Added to Continuous Subcutaneous Insulin Infusion (CSII) in Hospitalized Patients with Type 2 Diabetes. Diabetes Ther. 2020;11:701–710. doi: 10.1007/s13300-020-00758-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Okajima F., Emoto N., Kato K., Sugihara H. Effect of Glycemic Control on Chylomicron Metabolism and Correlation between Postprandial Metabolism of Plasma Glucose and Chylomicron in Patients with Type 2 Diabetes Treated with Basal-bolus Insulin Therapy with or without Vildagliptin. J. Atheroscler. Thromb. 2017;24:157–168. doi: 10.5551/jat.32409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ahren B., Foley J.E., Ferrannini E., Matthews D.R., Zinman B., Dejager S., Fonseca V.A. Changes in prandial glucagon levels after a 2-year treatment with vildagliptin or glimepiride in patients with type 2 diabetes inadequately controlled with metformin monotherapy. Diabetes Care. 2010;33:730–732. doi: 10.2337/dc09-1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ahren B., Schweizer A., Dejager S., Dunning B.E., Nilsson P.M., Persson M., Foley J.E. Vildagliptin enhances islet responsiveness to both hyper- and hypoglycemia in patients with type 2 diabetes. J. Clin. Endocrinol. Metab. 2009;94:1236–1243. doi: 10.1210/jc.2008-2152. [DOI] [PubMed] [Google Scholar]
- 60.Li F.F., Shen Y., Sun R., Zhang D.F., Jin X., Zhai X.F., Chen M.Y., Su X.F., Wu J.D., Ye L., et al. Effects of Vildagliptin Add-on Insulin Therapy on Nocturnal Glycemic Variations in Uncontrolled Type 2 Diabetes. Diabetes Ther. 2017;8:1111–1122. doi: 10.1007/s13300-017-0303-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fonseca V., Schweizer A., Albrecht D., Baron M.A., Chang I., Dejager S. Addition of vildagliptin to insulin improves glycaemic control in type 2 diabetes. Diabetologia. 2007;50:1148–1155. doi: 10.1007/s00125-007-0633-0. [DOI] [PubMed] [Google Scholar]
- 62.Gupta R.C., Dettbarn W.-D., Milatovic D. Handbook of Toxicology of Chemical Warfare Agents. Elsevier; Amsterdam, The Netherlands: 2009. Skeletal Muscle; pp. 509–531. [Google Scholar]
- 63.Kluess H.A. Dipeptidyl Peptidase IV as a Muscle Myokine. Front. Physiol. 2020;11:148. doi: 10.3389/fphys.2020.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Raschke S., Eckardt K., Bjorklund Holven K., Jensen J., Eckel J. Identification and validation of novel contraction-regulated myokines released from primary human skeletal muscle cells. PLoS ONE. 2013;8:e62008. doi: 10.1371/journal.pone.0062008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Neidert L.E., Al-Tarhuni M., Goldman D., Kluess H.A., Jackson D.N. Endogenous dipeptidyl peptidase IV modulates skeletal muscle arteriolar diameter in rats. Physiol. Rep. 2018;6 doi: 10.14814/phy2.13564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bouchi R., Fukuda T., Takeuchi T., Nakano Y., Murakami M., Minami I., Izumiyama H., Hashimoto K., Yoshimoto T., Ogawa Y. Dipeptidyl peptidase 4 inhibitors attenuates the decline of skeletal muscle mass in patients with type 2 diabetes. Diabetes Metab. Res. Rev. 2018;34 doi: 10.1002/dmrr.2957. [DOI] [PubMed] [Google Scholar]
- 67.Ishii S., Nagai Y., Kato H., Fukuda H., Tanaka Y. Effect of the Dipeptidyl Peptidase-4 Inhibitor Sitagliptin on Muscle Mass and the Muscle/Fat Ratio in Patients With Type 2 Diabetes. J. Clin. Med. Res. 2020;12:122–126. doi: 10.14740/jocmr4078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kalhotra P., Chittepu V.C.S.R., Osorio-Revilla G., Gallardo-Velazquez T. Chrysin in Combination with Insulin Promotes Glucose Uptake in Skeletal Muscle Cell: Impact of Combination Therapy in Diabetes Myopathy (P01-031-19) Curr. Dev. Nutr. 2019;3:nzz028-P01. doi: 10.1093/cdn/nzz028.P01-031-19. [DOI] [Google Scholar]
- 69.Kalhotra P., Chittepu V., Osorio-Revilla G., Gallardo-Velazquez T. Discovery of Galangin as a Potential DPP-4 Inhibitor That Improves Insulin-Stimulated Skeletal Muscle Glucose Uptake: A Combinational Therapy for Diabetes. Int. J. Mol. Sci. 2019;20:1228. doi: 10.3390/ijms20051228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lalitha N., Sadashivaiah B., Ramaprasad T.R., Singh S.A. Anti-hyperglycemic activity of myricetin, through inhibition of DPP-4 and enhanced GLP-1 levels, is attenuated by co-ingestion with lectin-rich protein. PLoS ONE. 2020;15:e0231543. doi: 10.1371/journal.pone.0231543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lee E.J., Shaikh S., Ahmad K., Ahmad S.S., Lim J.H., Park S., Yang H.J., Cho W.K., Park S.J., Lee Y.H., et al. Isolation and Characterization of Compounds from Glycyrrhiza uralensis as Therapeutic Agents for the Muscle Disorders. Int. J. Mol. Sci. 2021;22:876. doi: 10.3390/ijms22020876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Howes M.J.R., Quave C.L., Collemare J., Tatsis E.C., Twilley D., Lulekal E., Farlow A., Li L., Cazar M.E., Leaman D.J. Molecules from nature: Reconciling biodiversity conservation and global healthcare imperatives for sustainable use of medicinal plants and fungi. Plants People Planet. 2020;2:463–481. doi: 10.1002/ppp3.10138. [DOI] [Google Scholar]
- 73.Baig M.H., Jan A.T., Rabbani G., Ahmad K., Ashraf J.M., Kim T., Min H.S., Lee Y.H., Cho W.K., Ma J.Y., et al. Methylglyoxal and Advanced Glycation End products: Insight of the regulatory machinery affecting the myogenic program and of its modulation by natural compounds. Sci. Rep. 2017;7:5916. doi: 10.1038/s41598-017-06067-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ekor M. The growing use of herbal medicines: Issues relating to adverse reactions and challenges in monitoring safety. Front. Pharmacol. 2014;4:177. doi: 10.3389/fphar.2013.00177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Onoagbe I., Negbenebor E., Ogbeide V., Dawha I., Attah V., Lau H., Omonkhua A. A study of the anti-diabetic effects of Urena lobata and Sphenostylis stenocarpa in streptozotocin-induced diabetic rats. Eur. J. Sci. Res. 2010;43:6–14. [Google Scholar]
- 76.Purnomo Y., Soeatmadji D.W., Sumitro S.B., Widodo M.A. Anti-diabetic potential of Urena lobata leaf extract through inhibition of dipeptidyl peptidase IV activity. Asian Pac. J. Trop. Biomed. 2015;5:645–649. doi: 10.1016/j.apjtb.2015.05.014. [DOI] [Google Scholar]
- 77.Ramachandran S., Faisal T.K., Anjumary J., Rajasekaran A., Asokkumar K., Annadurai K., Arivukkarasu R., Sharma R.K., Shankar M.B. Comparative evaluation of hypoglycemic and hypolipidemic activity of various extract of Anogeissus latifolia bark in streptozotocin-induced diabetic rats. J. Complement. Integr. Med. 2017;14 doi: 10.1515/jcim-2016-0130. [DOI] [PubMed] [Google Scholar]
- 78.Baliga M.S., Thilakchand K.R., Rai M.P., Rao S., Venkatesh P. Aegle marmelos (L.) Correa (Bael) and its phytochemicals in the treatment and prevention of cancer. Integr. Cancer Ther. 2013;12:187–196. doi: 10.1177/1534735412451320. [DOI] [PubMed] [Google Scholar]
- 79.Ansari P., Hannon-Fletcher M.P., Flatt P.R., Abdel-Wahab Y.H.A. Effects of 22 traditional anti-diabetic medicinal plants on DPP-IV enzyme activity and glucose homeostasis in high-fat fed obese diabetic rats. Biosci. Rep. 2021;41 doi: 10.1042/BSR20203824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bharti S.K., Krishnan S., Kumar A., Rajak K.K., Murari K., Bharti B.K., Gupta A.K. Antihyperglycemic activity with DPP-IV inhibition of alkaloids from seed extract of Castanospermum australe: Investigation by experimental validation and molecular docking. Phytomedicine. 2012;20:24–31. doi: 10.1016/j.phymed.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 81.Saleem S., Jafri L., Haq I.U., Chang L.C., Calderwood D., Green B.D., Mirza B. Plants Fagonia cretica L. and Hedera nepalensis K. Koch contain natural compounds with potent dipeptidyl peptidase-4 (DPP-4) inhibitory activity. J. Ethnopharmacol. 2014;156:26–32. doi: 10.1016/j.jep.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 82.Kosaraju J., Dubala A., Chinni S., Khatwal R.B., Satish Kumar M.N., Basavan D. A molecular connection of Pterocarpus marsupium, Eugenia jambolana and Gymnema sylvestre with dipeptidyl peptidase-4 in the treatment of diabetes. Pharm. Biol. 2014;52:268–271. doi: 10.3109/13880209.2013.823550. [DOI] [PubMed] [Google Scholar]
- 83.Nongonierma A.B., Le Maux S., Dubrulle C., Barre C., FitzGerald R.J. Quinoa (Chenopodium quinoa Willd.) protein hydrolysates with in vitro dipeptidyl peptidase IV (DPP-IV) inhibitory and antioxidant properties. J. Cereal Sci. 2015;65:112–118. doi: 10.1016/j.jcs.2015.07.004. [DOI] [Google Scholar]
- 84.Bayan L., Koulivand P.H., Gorji A. Garlic: A review of potential therapeutic effects. Avicenna J. Phytomed. 2014;4:1–14. [PMC free article] [PubMed] [Google Scholar]
- 85.Kalhotra P., Chittepu V., Osorio-Revilla G., Gallardo-Velazquez T. Phytochemicals in Garlic Extract Inhibit Therapeutic Enzyme DPP-4 and Induce Skeletal Muscle Cell Proliferation: A Possible Mechanism of Action to Benefit the Treatment of Diabetes Mellitus. Biomolecules. 2020;10:305. doi: 10.3390/biom10020305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bansal P., Paul P., Mudgal J., Nayak P.G., Pannakal S.T., Priyadarsini K.I., Unnikrishnan M.K. Antidiabetic, antihyperlipidemic and antioxidant effects of the flavonoid rich fraction of Pilea microphylla (L.) in high fat diet/streptozotocin-induced diabetes in mice. Exp. Toxicol. Pathol. 2012;64:651–658. doi: 10.1016/j.etp.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 87.Aderibigbe A.O., Emudianughe T.S., Lawal B.A. Evaluation of the antidiabetic action of Mangifera indica in mice. Phytother. Res. 2001;15:456–458. doi: 10.1002/ptr.859. [DOI] [PubMed] [Google Scholar]
- 88.Yogisha S., Raveesha K.A. Dipeptidyl Peptidase IV inhibitory activity of Mangifera indica. J. Nat. Prod. 2010;3:9. [Google Scholar]
- 89.Suman R.K., Mohanty I.R., Maheshwari U., Borde M.K., Deshmukh Y.A. Natural dipeptidyl peptidase-IV inhibitor mangiferin mitigates diabetes- and metabolic syndrome-induced changes in experimental rats. Diabetes Metab. Syndr. Obes. 2016;9:261–272. doi: 10.2147/DMSO.S109599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kim B.R., Thapa P., Kim H.M., Jin C.H., Kim S.H., Kim J.B., Choi H., Han A.R., Nam J.W. Purification of Phenylpropanoids from the Scaly Bulbs of Lilium Longiflorum by CPC and Determination of Their DPP-IV Inhibitory Potentials. ACS Omega. 2020;5:4050–4057. doi: 10.1021/acsomega.9b03649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kim B.R., Paudel S.B., Nam J.W., Jin C.H., Lee I.S., Han A.R. Constituents of Coreopsis lanceolata Flower and Their Dipeptidyl Peptidase IV Inhibitory Effects. Molecules. 2020;25:4370. doi: 10.3390/molecules25194370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Eidenberger T., Selg M., Krennhuber K. Inhibition of dipeptidyl peptidase activity by flavonol glycosides of guava (Psidium guajava L.): A key to the beneficial effects of guava in type II diabetes mellitus. Fitoterapia. 2013;89:74–79. doi: 10.1016/j.fitote.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 93.Quek A., Kassim N.K., Ismail A., Latif M.A.M., Shaari K., Tan D.C., Lim P.C. Identification of Dipeptidyl Peptidase-4 and alpha-Amylase Inhibitors from Melicope glabra (Blume) T. G. Hartley (Rutaceae) Using Liquid Chromatography Tandem Mass Spectrometry, In Vitro and In Silico Methods. Molecules. 2020;26:1. doi: 10.3390/molecules26010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ansari P., Azam S., Hannan J.M.A., Flatt P.R., Abdel Wahab Y.H.A. Anti-hyperglycaemic activity of H. rosa-sinensis leaves is partly mediated by inhibition of carbohydrate digestion and absorption, and enhancement of insulin secretion. J. Ethnopharmacol. 2020;253:112647. doi: 10.1016/j.jep.2020.112647. [DOI] [PubMed] [Google Scholar]
- 95.Li W.L., Zheng H.C., Bukuru J., De Kimpe N. Natural medicines used in the traditional Chinese medical system for therapy of diabetes mellitus. J. Ethnopharmacol. 2004;92:1–21. doi: 10.1016/j.jep.2003.12.031. [DOI] [PubMed] [Google Scholar]
- 96.Ansari P., Flatt P.R., Harriott P., Abdel-Wahab Y.H.A. Evaluation of the Antidiabetic and Insulin Releasing Effects of A. squamosa, Including Isolation and Characterization of Active Phytochemicals. Plants. 2020;9:1348. doi: 10.3390/plants9101348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Majeed M., Majeed S., Mundkur L., Nagabhushanam K., Arumugam S., Beede K., Ali F. Standardized Emblica officinalis fruit extract inhibited the activities of alpha-amylase, alpha-glucosidase, and dipeptidyl peptidase-4 and displayed antioxidant potential. J. Sci. Food Agric. 2020;100:509–516. doi: 10.1002/jsfa.10020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Chakrabarti R., Bhavtaran S., Narendra P., Varghese N., Vanchhawng L., Mohamed Sham Shihabudeen H., Thirumurgan K. Dipeptidyl peptidase-IV inhibitory activity of Berberis aristata. J. Nat. Prod. 2011;4:158–163. [Google Scholar]
- 99.Wang F., Yu G., Zhang Y., Zhang B., Fan J. Dipeptidyl Peptidase IV Inhibitory Peptides Derived from Oat (Avena sativa L.), Buckwheat (Fagopyrum esculentum), and Highland Barley (Hordeum vulgare trifurcatum (L.) Trofim) Proteins. J. Agric. Food Chem. 2015;63:9543–9549. doi: 10.1021/acs.jafc.5b04016. [DOI] [PubMed] [Google Scholar]
- 100.Ekayanti M., Sauriasari R., Elya B. Dipeptidyl peptidase IV inhibitory activity of fraction from white tea ethanolic extract (Camellia sinensis (L.) Kuntze) ex vivo. Pharmacogn. J. 2018;10:190–193. doi: 10.5530/pj.2018.1.32. [DOI] [Google Scholar]
- 101.Lin Y.S., Chen C.R., Wu W.H., Wen C.L., Chang C.I., Hou W.C. Anti-alpha-glucosidase and Anti-dipeptidyl Peptidase-IV Activities of Extracts and Purified Compounds from Vitis thunbergii var. taiwaniana. J. Agric. Food Chem. 2015;63:6393–6401. doi: 10.1021/acs.jafc.5b02069. [DOI] [PubMed] [Google Scholar]
- 102.Kumar V., Sachan R., Rahman M., Sharma K., Al-Abbasi F.A., Anwar F. Prunus amygdalus extract exert antidiabetic effect via inhibition of DPP-IV: In-silico and in-vivo approaches. J. Biomol. Struct. Dyn. 2020:1–15. doi: 10.1080/07391102.2020.1775124. [DOI] [PubMed] [Google Scholar]
- 103.YARIZADE A., KUMLEH H.H., Niazi A. In vitro antidiabetic effects of ferula assa-foetida extracts through dipeptidyl peptidase iv and α-glucosidase inhibitory activity. IN VITRO. 2017;10 doi: 10.22159/ajpcr.2017.v10i5.16648. [DOI] [Google Scholar]
- 104.Morikawa T., Ninomiya K., Akaki J., Kakihara N., Kuramoto H., Matsumoto Y., Hayakawa T., Muraoka O., Wang L.B., Wu L.J., et al. Dipeptidyl peptidase-IV inhibitory activity of dimeric dihydrochalcone glycosides from flowers of Helichrysum arenarium. J. Nat. Med. 2015;69:494–506. doi: 10.1007/s11418-015-0914-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cragg G.M., Newman D.J. Natural products: A continuing source of novel drug leads. Biochim. Biophys. Acta. 2013;1830:3670–3695. doi: 10.1016/j.bbagen.2013.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Al-masri I.M., Mohammad M.K., Tahaa M.O. Inhibition of dipeptidyl peptidase IV (DPP IV) is one of the mechanisms explaining the hypoglycemic effect of berberine. J. Enzym. Inhib. Med. Chem. 2009;24:1061–1066. doi: 10.1080/14756360802610761. [DOI] [PubMed] [Google Scholar]
- 107.Fan J., Johnson M.H., Lila M.A., Yousef G., de Mejia E.G. Berry and Citrus Phenolic Compounds Inhibit Dipeptidyl Peptidase IV: Implications in Diabetes Management. Evid. Based Complement. Altern. Med. 2013;2013:479505. doi: 10.1155/2013/479505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cásedas G., Les F., González-Burgos E., Gómez-Serranillos M.P., Smith C., López V. Cyanidin-3-O-glucoside inhibits different enzymes involved in central nervous system pathologies and type-2 diabetes. S. Afr. J. Bot. 2019;120:241–246. doi: 10.1016/j.sajb.2018.07.001. [DOI] [Google Scholar]
- 109.Wang Z., Yang L., Fan H., Wu P., Zhang F., Zhang C., Liu W., Li M. Screening of a natural compound library identifies emodin, a natural compound from Rheum palmatum Linn that inhibits DPP4. PeerJ. 2017;5:e3283. doi: 10.7717/peerj.3283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gupta A., Jacobson G.A., Burgess J.R., Jelinek H.F., Nichols D.S., Narkowicz C.K., Al-Aubaidy H.A. Citrus bioflavonoids dipeptidyl peptidase-4 inhibition compared with gliptin antidiabetic medications. Biochem. Biophys. Res. Commun. 2018;503:21–25. doi: 10.1016/j.bbrc.2018.04.156. [DOI] [PubMed] [Google Scholar]
- 111.Parmar H.S., Jain P., Chauhan D.S., Bhinchar M.K., Munjal V., Yusuf M., Choube K., Tawani A., Tiwari V., Manivannan E., et al. DPP-IV inhibitory potential of naringin: An in silico, in vitro and in vivo study. Diabetes Res. Clin. Pract. 2012;97:105–111. doi: 10.1016/j.diabres.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 112.Bower A.M., Real Hernandez L.M., Berhow M.A., de Mejia E.G. Bioactive compounds from culinary herbs inhibit a molecular target for type 2 diabetes management, dipeptidyl peptidase IV. J. Agric. Food Chem. 2014;62:6147–6158. doi: 10.1021/jf500639f. [DOI] [PubMed] [Google Scholar]
- 113.Singh A.K., Patel P.K., Choudhary K., Joshi J., Yadav D., Jin J.O. Quercetin and Coumarin Inhibit Dipeptidyl Peptidase-IV and Exhibits Antioxidant Properties: In Silico, In Vitro, Ex Vivo. Biomolecules. 2020;10:207. doi: 10.3390/biom10020207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zhang L., Zhang S.-T., Yin Y.-C., Xing S., Li W.-N., Fu X.-Q. Hypoglycemic effect and mechanism of isoquercitrin as an inhibitor of dipeptidyl peptidase-4 in type 2 diabetic mice. RSC Adv. 2018;8:14967–14974. doi: 10.1039/C8RA00675J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zhao B.T., Le D.D., Nguyen P.H., Ali M.Y., Choi J.S., Min B.S., Shin H.M., Rhee H.I., Woo M.H. PTP1B, alpha-glucosidase, and DPP-IV inhibitory effects for chromene derivatives from the leaves of Smilax china L. Chem. Biol. Interact. 2016;253:27–37. doi: 10.1016/j.cbi.2016.04.012. [DOI] [PubMed] [Google Scholar]
- 116.Katkar K.V., Suthar A.C., Chauhan V.S. The chemistry, pharmacologic, and therapeutic applications of Polyalthia longifolia. Pharmacogn. Rev. 2010;4:62–68. doi: 10.4103/0973-7847.65329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Huang P.K., Lin S.R., Riyaphan J., Fu Y.S., Weng C.F. Polyalthia Clerodane Diterpene Potentiates Hypoglycemia via Inhibition of Dipeptidyl Peptidase 4. Int. J. Mol. Sci. 2019;20:530. doi: 10.3390/ijms20030530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Geng Y., Lu Z.M., Huang W., Xu H.Y., Shi J.S., Xu Z.H. Bioassay-guided isolation of DPP-4 inhibitory fractions from extracts of submerged cultured of Inonotus obliquus. Molecules. 2013;18:1150–1161. doi: 10.3390/molecules18011150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Huang P.K., Lin S.R., Chang C.H., Tsai M.J., Lee D.N., Weng C.F. Natural phenolic compounds potentiate hypoglycemia via inhibition of Dipeptidyl peptidase IV. Sci. Rep. 2019;9:15585. doi: 10.1038/s41598-019-52088-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kalhotra P., Chittepu V., Osorio-Revilla G., Gallardo-Velazquez T. Structure(-)Activity Relationship and Molecular Docking of Natural Product Library Reveal Chrysin as a Novel Dipeptidyl Peptidase-4 (DPP-4) Inhibitor: An Integrated In Silico and In Vitro Study. Molecules. 2018;23:1368. doi: 10.3390/molecules23061368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kim B.R., Kim H.Y., Choi I., Kim J.B., Jin C.H., Han A.R. DPP-IV Inhibitory Potentials of Flavonol Glycosides Isolated from the Seeds of Lens culinaris: In Vitro and Molecular Docking Analyses. Molecules. 2018;23:1998. doi: 10.3390/molecules23081998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Abdel Motaal A., Salem H.H., Almaghaslah D., Alsayari A., Bin Muhsinah A., Alfaifi M.Y., Elbehairi S.E.I., Shati A.A., El-Askary H. Flavonol Glycosides: In Vitro Inhibition of DPPIV, Aldose Reductase and Combating Oxidative Stress are Potential Mechanisms for Mediating the Antidiabetic Activity of Cleome droserifolia. Molecules. 2020;25:5864. doi: 10.3390/molecules25245864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Mojica L., de Mejia E.G. Optimization of enzymatic production of anti-diabetic peptides from black bean (Phaseolus vulgaris L.) proteins, their characterization and biological potential. Food Funct. 2016;7:713–727. doi: 10.1039/C5FO01204J. [DOI] [PubMed] [Google Scholar]
- 124.Mojica L., Luna-Vital D.A., Gonzalez de Mejia E. Characterization of peptides from common bean protein isolates and their potential to inhibit markers of type-2 diabetes, hypertension and oxidative stress. J. Sci. Food Agric. 2017;97:2401–2410. doi: 10.1002/jsfa.8053. [DOI] [PubMed] [Google Scholar]
- 125.Hatanaka T., Uraji M., Fujita A., Kawakami K. Anti-oxidation activities of rice-derived peptides and their inhibitory effects on dipeptidylpeptidase-IV. Int. J. Pept. Res. Ther. 2015;21:479–485. doi: 10.1007/s10989-015-9478-4. [DOI] [Google Scholar]
- 126.Hatanaka T., Inoue Y., Arima J., Kumagai Y., Usuki H., Kawakami K., Kimura M., Mukaihara T. Production of dipeptidyl peptidase IV inhibitory peptides from defatted rice bran. Food Chem. 2012;134:797–802. doi: 10.1016/j.foodchem.2012.02.183. [DOI] [PubMed] [Google Scholar]
- 127.Velarde-Salcedo A.J., Barrera-Pacheco A., Lara-Gonzalez S., Montero-Moran G.M., Diaz-Gois A., de Mejia E.G., de la Rosa A.P.B. In vitro inhibition of dipeptidyl peptidase IV by peptides derived from the hydrolysis of amaranth (Amaranthus hypochondriacus L.) proteins. Food Chem. 2013;136:758–764. doi: 10.1016/j.foodchem.2012.08.032. [DOI] [PubMed] [Google Scholar]
- 128.Lammi C., Zanoni C., Arnoldi A., Vistoli G. Peptides Derived from Soy and Lupin Protein as Dipeptidyl-Peptidase IV Inhibitors: In Vitro Biochemical Screening and in Silico Molecular Modeling Study. J. Agric. Food Chem. 2016;64:9601–9606. doi: 10.1021/acs.jafc.6b04041. [DOI] [PubMed] [Google Scholar]
- 129.Estrada-Salas P.A., Montero-Moran G.M., Martinez-Cuevas P.P., Gonzalez C., de la Rosa A.P.B. Characterization of antidiabetic and antihypertensive properties of canary seed (Phalaris canariensis L.) peptides. J. Agric. Food Chem. 2014;62:427–433. doi: 10.1021/jf404539y. [DOI] [PubMed] [Google Scholar]
- 130.Vilcacundo R., Martínez-Villaluenga C., Hernández-Ledesma B. Release of dipeptidyl peptidase IV, α-amylase and α-glucosidase inhibitory peptides from quinoa (Chenopodium quinoa Willd.) during in vitro simulated gastrointestinal digestion. J. Funct. Foods. 2017;35:531–539. doi: 10.1016/j.jff.2017.06.024. [DOI] [Google Scholar]
- 131.Huang S.L., Jao C.L., Ho K.P., Hsu K.C. Dipeptidyl-peptidase IV inhibitory activity of peptides derived from tuna cooking juice hydrolysates. Peptides. 2012;35:114–121. doi: 10.1016/j.peptides.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 132.Li-Chan E.C., Hunag S.L., Jao C.L., Ho K.P., Hsu K.C. Peptides derived from atlantic salmon skin gelatin as dipeptidyl-peptidase IV inhibitors. J. Agric. Food Chem. 2012;60:973–978. doi: 10.1021/jf204720q. [DOI] [PubMed] [Google Scholar]
- 133.Harnedy P.A., O’Keeffe M.B., FitzGerald R.J. Purification and identification of dipeptidyl peptidase (DPP) IV inhibitory peptides from the macroalga Palmaria palmata. Food Chem. 2015;172:400–406. doi: 10.1016/j.foodchem.2014.09.083. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.