Abstract
Background: Acute coronary syndrome (ACS) is a major cause of death all over the world. STEMI represents a type of myocardial infarction with acute ST elevation. We aimed to assess the predictive power of potential RNA panel expression in acute coronary syndrome. Method: We used in silico data analysis to retrieve RNAs related to glycerophospholipid metabolism dysregulation and specific to ACS that results in the selection of Alpha/Beta hydrolase fold domain4 (ABHD4) mRNA and its epigenetic regulators (Foxf1 adjacent noncoding developmental regulatory RNA (FENDRR) lncRNA, miRNA-221, and miRNA-197). We assessed the expression of the serum RNA panel in 68 patients with ACS, 21 patients with chest pain due to non-cardiac causes, and 21 healthy volunteers by quantitative real-time polymerase chain reaction. Results: The study data showed significant down regulation in the expression of the serum levels of FENDRR lncRNA and miRNA-221-3p by 120-fold and 22-fold in Unstable angina (UA) in comparison with healthy volunteers, and by 8.6-fold and 2-fold in ST segment elevation myocardial infarction (STEMI) patients versus UA; concomitant upregulation in the expression of ABHD4 mRNA and miRNA-197-5p by 444-fold and 10-fold in UA compared with healthy volunteers, and by 1.54-fold and 4.5-fold in STEMI versus unstable angina. Performance characteristics analysis showed that the ABHD4-regulating RNA panel were potential biomarkers for prediction of ACS. Moreover, there was a significant association between the 2 miRNAs and ABHD4 mRNA and the regulating FENDRR lncRNA. Conclusion: Collectively, ABHD4 mRNA regulating RNA panel based on putative interactions seems to be novel non-invasive biomarkers that could detect ACS early and stratify severity of the condition that could improve health outcome.
Keywords: acute coronary syndrome, RNA, diagnosis, serum, troponin, bioinformatics, glycerophospholipid
1. Introduction
Acute coronary syndrome is a prime reason of hospital admission and death worldwide [1]. Myocardial infarction definition necessitates necrosis of the cardiac myocytes with abnormal levels of plasma cardiac troponin [2,3]. Early diagnosis of ACS allows early reperfusion therapy, resulting in decrease in the death rate [4]. Diagnostic biomarkers of ACS have widely emerged through the study of known myocardial proteins [5]. Currently, many biomarkers as cardiac myoglobin, creatine kinase-MB, and troponins are widely used in the clinical diagnosis with unfortunately many false elevations due to skeletal muscle injury. From these biomarkers, troponins are now considered as the corner stone in ACS diagnosis but it has the following limitations: (1) it begins to increase within 3–4 h after the incidence of myocardial ischemia, limiting ACS diagnosis within first 1–2 h, (2) it is elevated in the chronic renal failure patients and has limited use in myocardial re-infarction due to its long half time [6,7]. Yet, the need to find novel biomarkers with high accuracy is always present, to allow earlier diagnosis with decreased mortality and complications [8,9]. Dysregulation of lipid metabolism leads to several chronic diseases especially cardiovascular disease. Shedding the light on the enzymatic mechanisms controlling lipid metabolism is crucial for successful innovative diagnostics and drug discovery in human diseases. Alpha/Beta hydrolase fold domain containing (ABHD) proteins family have common roles in lipid metabolism [10]. They include proteases, esterases, lipases, dehalogenases, and epoxide hydrolases [11]. ABHD protein family members have the ability to metabolize different glycerophospholipid types that act as key intermediates in cellular signaling and neurotransmission [12]. Recently, ABHD protein family mutations have been linked to inborn errors of lipid metabolism with subsequent complications. ABHD protein family is considered as a predictor of plasma phospholipid levels in humans [13].
Plasma glycerophospholipid and lysophosphatidic acids (LysoPAs) are crucial lipid mediators, and the main risk factors for cardiovascular diseases including ACS [14]. LysoPA stimulates the adhesion of molecules and chemokines expression in the endothelial cells, the smooth muscle cells migration, and platelets activation [15]. Several studies highlighted the activations of phospholipase A2 and phospholipase D15 in myocardial ischemia [16]. Alpha/Beta Hydrolase Domain-Containing Protein 4 (ABHD4) gene is a main regulator of phospholipid metabolism in mammals having hydrolase and lysophospholipase activity [17]. ABHD4 deacylates N-acylphosphatidylethanolamines and N-acylphosphatidylserines to hydrolyze saturated and unsaturated N-acyl chains. ABHD4 (–/–) mice show decrease in brain glycerophosphoethanolamine and lysophosphatidylserines [18].
miRNAs are known to regulate important complex gene regulatory pathways related to the development of cardiovascular system [19].Certain patterns of miRNA expression plays a prime role in myocardial infarction, in addition to the fact that many cardiac miRNAs are dysregulated in patients with ACS [20,21]. Several miRNAs have been studied in ACS, such as miRNA-208a, miRNA-126, miRNA-122-5p, miRNA-19a, and miRNA-1, which have been recognized as new biomarkers in early ACS diagnosis [22]. So, further studies of the relation between target genes and miRNA are needed for better comprehension of MI pathology and potential biomarker discovery. Additionally, dysregulation of lncRNA expression is involved in many diseases including cancers [23] and cardiovascular diseases [24]. For example, Mirt1 lncRNA [25], lncRNA KCNQ1OT1 [26], and aHIF lncRNA and ANRIL lncRNA [27] have been related to myocardial infarction.
In this study, we used in silico data analysis to explore a new mechanistic signaling pathway based on putative interactions between RNAs in ACS. We chose ABHD4-regulating RNA panel related to glycerophospholipid metabolism and related to ACS that could be a potential biomarker in early ACS diagnosis and detection of myocardial ischemia in unstable angina with low troponin level or in STEMI patients with high troponin level. We measured the expression of the serum RNA panel in ACS patients group, patients presented with chest pain due to non-cardiac causes, and healthy volunteers.
We have selected ABHD4 mRNA as a crucial player in glycerophospholipid metabolism gene highly correlated with cardiovascular complications, especially ACS based on two approaches. Firstly, bioinformatics analysis was used to confirm the expression of ABHD4 mRNA in ACS based on novelty, gene ontology enrichment that confirm its correlation with lipid metabolism regulation, and the basal expression in heart. Taken together, the public microarray gene expression databases confirmed such selection. The second approach was a literature review [1,2,3,4] of the limited data available about the role of ABHD family as predictor of glycerophospholipid in humans, which has a strong correlation with ACS. Both bioinformatics analysis and literature review suggested a possible role of ABHD4 mRNA in ACS. Afterwards, we retrieved data about miRNA regulation of ABHD4 mRNA and identified (miRNA-197-5p and miRNA-221-3p) based on both in silico data and literature review [28,29,30,31,32,33] that affirm that the chosen miRNAs were linked to lipid metabolism regulation as previously confirmed in ACS, targeting ABHD4 mRNA. Lastly, we aim to construct an integrated and genetically linked mRNA–miRNA–lncRNA panel to increase the chance of usefulness of the chosen panel in ACS management and novel implications for targeting ABHD enzymes in the treatment or prevention of lipid-metabolism-related disease, especially ACS. We have selected FENDRR lncRNA based on both in silico data that confirm complementarity binding between the selected RNA panel members and literature search that highlighted its role in inflammation, fibrosis, and cardiovascular diseases [34,35].
2. Materials and Methods
2.1. Study Population
This study is approved by the Ain Shams ethical committee, faculty of medicine. All the patients were recruited from the cardiovascular (CVS) department, Ain Shams University in the period from November 2017 till October 2018. The study includes 68 acute coronary syndrome patients including UA (n = 21), STEMI (n = 31) patients, and NSTEMI (n = 16); 21 patients with non-cardiac chest pain based on the output of coronary angiography; and 21 healthy volunteers with normal ECG and no history of CVS disease seeking routine health checkups with matched sex and age to the patients’ groups. Informed consent was taken from all participants.
ACS was diagnosed through assessing cardiac troponin levels, creatine kinase-MB (CK-MB) together with clinical symptoms consistent with ACS within 6 h of chest pain and underwent primary Percutaneous Coronary Intervention (PCI). ACS was diagnosed on the basis of ischemic symptoms, a pathological Q wave, and an increased cTnI (cardiac troponin I) with CK-MB expression according to American College of Cardiology/American Heart Association (2018 ESC/ACC/AHA/WHF Fourth Universal Definition) guidelines. Subjects with end-stage renal failure, liver disease, cardiomyopathy, hemorrhagic disorders, immunological diseases, chemotherapy or radiotherapy, or inflammatory bowel disease, chronic myopathy and cancer were excluded from the study.
Blood samples were collected in the first 6 h of chest pain onset. Continuous assessment of CK-MB and hs-cTnT were done. Samples were centrifuged at 4000 rpm for 20 min, and the sera samples were kept in aliquots and stored at −70 °C into DNase-/RNase-free eppendorf tubes.
2.2. In Silico Data Analysis
We have chosen ABHD4 gene as it is linked to glycerophospholipid metabolism and ACS from GeneCards®: The Human Gene Database and Human Protein Atlas database based on novelty and basal expression in normal heart (Supplementary Figures S1–S4). Then, based on high complementarity binding site numbers, relation to lipid metabolism regulation, and relation to coronary syndrome and expression in heart, miRNA-221-3p and miRNA-197-5p miRNAs were selected through miRWalk database. Pathway enrichment analysis of both miRNAs ensured their relation to lipid metabolism, apoptosis, cytokines, and inflammation that are closely linked to ACS (Supplementary Figures S5–S10). Finally, FENDRR lncRNA was selected as a master control player of the previously selected genes through non-code database. Sequence alignment was done between the FENDRR lncRNA and the selected miRNAs to confirm the in silico prediction (Supplementary Figures S11–S20).
2.3. Purification of Total RNA Including miRNAs from Sera Samples and Quantitaive Real Time PCR (RT-qPCR)
Total RNA was purified from the sera samples by miRNEasy extraction kit (Qiagen, Hilden, Germany) according to the kit manual. Concentration & purity of RNA was analyzed by NanoDrop (Thermo Scientific, Waltham, MA, USA) and with Invitrogen™ Qubit™ 3.0 Fluorometer (Termo Fisher, Waltham, MA, USA). Equal amounts of RNA were used for reverse transcription (RT) using the TaqMan miRNA Reverse Transcription Kit and for amplification by qPCR, using TaqMan MicroRNA Assays of the selected miRNAs, ABHD4 Taqman probe and TaqMan universal mastermix (Applied Biosystems, Foster City, CA; Termo Fisher, Waltham, MA, USA), U6 sn RNA, and endogenous control.
FENDRR lncRNA in the sera samples were assessed using miScript II RT Kit (Qiagen, Hilden, Germany) to synthesize cDNA, followed by RT2 SYBR Green ROX qPCR Mastermix (Qiagen, Germany) and ACTB-1/beta actin (Hs-ACTB-1-RT2 QuantiTect Primer Assays, Qiagen, Germany) as endogenous control. Each sample was assessed in duplicate. Spike-in control cel-miRNA-39 (Qiagen, Germantown, MD, USA) was used for the normalization of miRNAs. Relative quantification of RNA panel expression was calculated by RQ = 2−∆∆Ct using Livak method. RT-qPCR was done using Applied Biosystems 7500 FAST Real Time PCR system (Applied Biosystems, Foster City, CA, USA) thermal cycler with data analysis taking into consideration the negative expression if Ct value was more than 36 (details in Supplementary Materials).
2.4. Statistical Analysis
Data was statistically analyzed using software package of statistical analysis version 25(SPSS25): median for non-parametric data, while mean ± SD for symmetrically distributed raw numerical data. One-way ANOVA, cross-tabulation chi-square test for number and percentage calculation, and Spearman correlation test were used as appropriate. The receiver operating characteristic (ROC) curve was used to evaluate the predictive value of the RNA panel in acute coronary syndrome.
3. Results
3.1. Biochemical and Clinical Markers in the Investigated Groups
Concerning the clinical and laboratory data (age, sex, smoking, hypertension, diabetes mellitus, and serum LDL, HDL, and total cholesterol), we did not find significant difference in the ACS, non-cardiac chest pain, and control groups (p > 0.05). On the contrary, we found highly significant difference in body mass index and serum levels of triglycerides, and creatinine among the three investigated groups (p < 0.05) (Supplementary Table S1).
3.2. Expression of the Serum RNAs Molecular Network
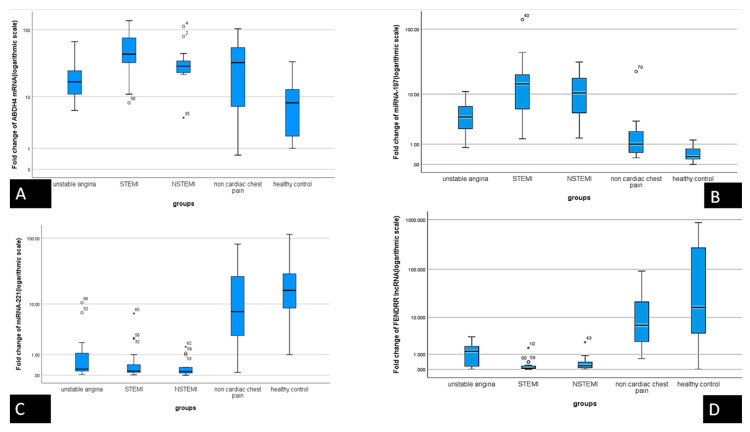
Serum levels of the chosen molecular network RNAs were assessed in samples of the 3 different groups to validate our retrieved in silico data. The expression was assessed through fold change (RQ) values. There was down regulation in the expression of FENDRR lncRNA and miRNA-221 with concomitant upregulation in the level of ABHD4 mRNA and miRNA-197 in the ACS group compared with both non-cardiac chest pain group and healthy volunteers (p < 0.001) (Table 1, Figure 1A–D).
Table 1.
Differential expression of different parameters among the study groups, in addition to patients with unstable angina versus STEMI.
| i | Median | F | p | ||
|---|---|---|---|---|---|
| miRNA-221-3p | unstable angina | 21 | 0.2300 | a 13.053 | a 0.000 |
| STEMI | 31 | 0.1500 | b 0.00 | ||
| NSTEMI | 16 | 0.1300 | c 0.874 | ||
| non cardiac chest pain | 21 | 7.5000 | |||
| healthy control | 21 | 16.4000 | |||
| miRNA 197-5p | unstable angina | 21 | 4.0395 | a 7.473 | a 0.000 |
| STEMI | 31 | 14.6000 | b 0.001 | ||
| NSTEMI | 16 | 10.4500 | c 0.001 | ||
| non cardiac chest pain | 21 | 1.0000 | |||
| healthy control | 21 | 0.3000 | |||
| ABHD4 mRNA | unstable angina | 21 | 8.80000 | a 9.142 | a 0.000 |
| STEMI | 31 | 7.80000 | b 0.01 | ||
| NSTEMI | 16 | 21.40000 | c 0.103 | ||
| non cardiac chest pain | 21 | 0.04000 | |||
| healthy control | 21 | 0.01000 | |||
| FENDRR lncRNA | unstable angina | 21 | 1.30000 | a 8.994 | a 0.000 |
| STEMI | 31 | 0.06000 | b 0.00 | ||
| NSTEMI | 16 | 0.17000 | c 0.968 | ||
| non cardiac chest pain | 21 | 6.65000 | |||
| healthy control | 21 | 16.50000 | |||
| Creatine kinase-MB (CK-MB) | unstable angina | 21 | 17.00 | a 10.947 | a 0.000 |
| STEMI | 31 | 44.00 | b 0.128 | ||
| NSTEMI | 16 | 29.50 | c 0.1 | ||
| non cardiac chest pain | 21 | 33.00 | |||
| healthy control | 21 | 8.00 | |||
| Cardiac Troponin | unstable angina | 21 | 17.00 | a 79.243 | a 0.000 |
| STEMI | 31 | 44.00 | b 0.154 | ||
| NSTEMI | 16 | 29.50 | c 0.1 | ||
| non cardiac chest pain | 21 | 33.00 | |||
| healthy control | 21 | 8.00 | |||
a Statistics among all groups, b Statistics UA versus healthy control, c UNA versus STEMI, p-value > 0.05 is considered statistically non-significant, and p-value < 0.05 is considered statistically significant. F: One Way Anova. STEMI: ST segment elevation in myocardial infarction.
Figure 1.
Differential analysis of the results in BOXPLOT represents serum RNA panel expression based on fold change in gene expression at logarithmic scale as measured by qRT-PCR among the groups of the study. (A) ABHD4 mRNA, (B) MiRNA-197-5p, (C) miRNA-221-3p, and (D) FENDRR lncRNA. The median is represented by line inside the box while the 1st and 3rd quartiles are represented by the top and bottom lines of the box, respectively, and the 5th and 95th percentiles are at the top and bottom whiskers, respectively. *, ° different markers for “out” values (small circle) and “far out” or as SPSS calls them “Extreme values” (marked with a star). SPSS uses a step of 1.5 × IQR (Interquartile range).
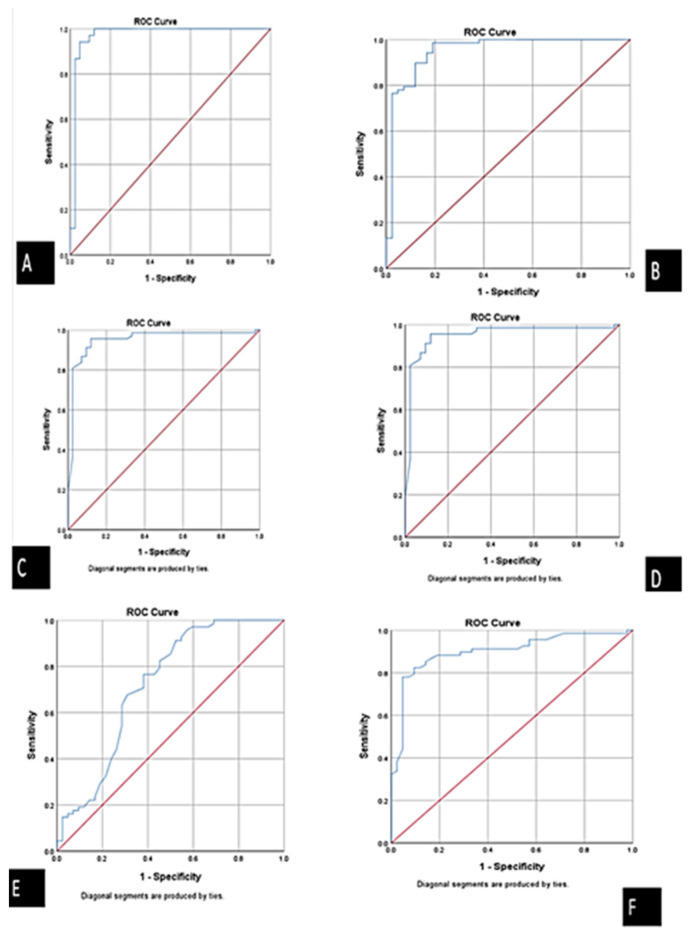
Using ROC curve analysis, we compared the ACS group to both chest pain group due to non-cardiac causes and healthy volunteer group. We found that the best cutoff values were 2.1 for ABHD4 mRNA (AUC = 0.972), 2.55 for FENDRR lncRNA (AUC =0.949), 2.02 for miRNA-221-3p (AUC = 0.958), and 1.7 for miRNA-197-5p (AUC = 0.949). The measured sensitivities were 94.4%, 93.3%, 95.4%, and 89.3%, respectively. The aforementioned results point out that these optimal cutoff values could be used to discriminate between ACS from non-cardiac chest pain patients and healthy participants (Table 2, Figure 2A–F, Figure 3 and Figure 4).
Table 2.
Performance characteristics of serum laboratory biomarkers.
| Biomarker | Sensitivity | Specificity | PPV (Positive Predictive Value) |
NPV (Negative Predictive Value) |
Accuracy |
|---|---|---|---|---|---|
| ABHD4 mRNA | 94.4% | 97.4% | 98.5% | 90.5% | 95.4% |
| FENDRR lncRNA | 93.3% | 90.5% | 82.4% | 76% | 93.3% |
| miRNA-221-3p | 95.4% | 86.7% | 91.2% | 92.9% | 91.8% |
| miRNA-197-5p | 89.3% | 97.1% | 98.5% | 81% | 91.8% |
| Cardiac troponin | 93.1% | 73.1% | 79.4% | 90.5% | 83.6% |
Figure 2.
Receiver operator characteristics (ROC) curve presents the diagnostic accuracy of the ABHD4 RNA panel discriminating between ACS and control. (A) ABHD4 mRNA, (B) MiRNA-197-5p, (C) miRNA-221-3p, and (D) FENDRR lncRNA, (E) CK-MB, and (F) cardiac troponin.
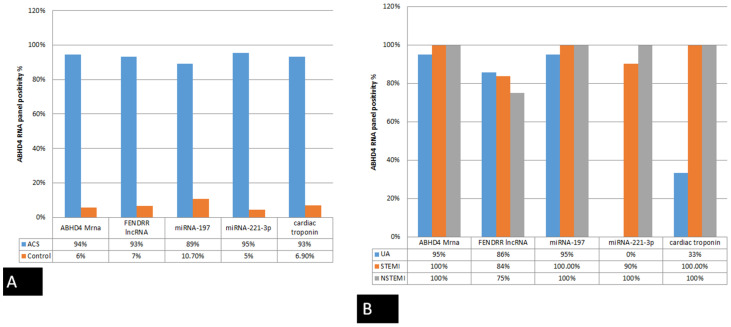
Figure 3.
Bar chart shows the positivity rate of the studied parameter: (A) between ACS patients and control (non-cardiac and healthy controls), and (B) the diagnostic value of the studied parameters in discriminating UA from STEMI and NSTEMI.
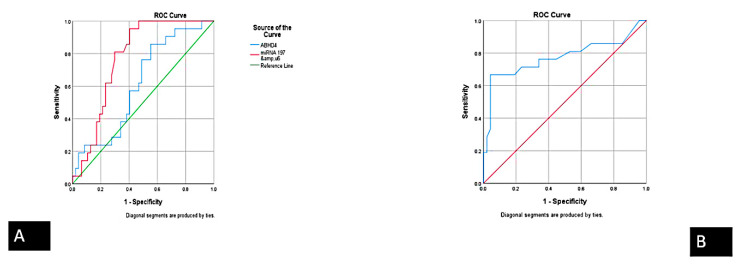
Figure 4.
Receiver operator characteristics (ROC) curve presents the diagnostic accuracy of the ABHD4 RNA panel discriminating between UA and STEMI: (A) ABHD4 mRNA and miRNA-197-5p a (B) FENDRR lncRNA.
Additionally, the expression pattern for ABHD4 mRNA regulating RNA panel in unstable angina and acute STEMI were compared with healthy participants. The serum levels of FENDRR lncRNA and miRNA-221-3p were increased by 120-fold and 22-fold in unstable angina compared with healthy participants, and by 8.6-fold and 2-fold in STEMI compared with unstable angina. Moreover, there was a concomitant upregulation in the expression of ABHD4 mRNA and miRNA-197-5p by 444-fold and 10-fold in unstable angina compared with healthy participants, and by 1.54-fold and 4.5-fold in STEMI compared with UA, respectively. Additionally, at an optimal cut-off value of 13.55, 7.07, and 0.25 for ABHD4 mRNA, miRNA-197-5p, and FENDRR lncRNA expression levels could potentially distinguish UA from patients with STEMI (AUC: 0.615, 0.773, and 0.774, respectively) (Figure 3) with sensitivity of 77.2%, 81%, and 71.4% and specificity of 52%, 70.2%, and 76.6%, respectively (Table 2, Figure 3A,B and Figure 4).
Contrary to the limited elevation of cardiac troponin levels in only 33% of UA patients, ABHD4 mRNA regulating RNA panel were markedly elevated in 94%, 93%, and 89% for ABHD4 mRNA, FENDRR lncRNA, and miRNA-197-5p, respectively, of UA patients (Figure 4A,B). For acute STEMI patients, myocardial infarction was verified by persistent ST-segment changes and significant increase in cardiac troponin in all patients, similar to the marked differential expression of ABHD4 mRNA regulating RNA in the STEMI patients compared with healthy controls (Figure 3 and Figure 4).
3.3. Correlation between Serum ABHD4 Regulating RNAs and Cardiac Troponin among the Study Groups
On the other hand, there was significant inverse correlation between ABHD4 mRNA and both FENDRR lncRNA and miRNA-221-3p (p < 0.000). Furthermore, there was significant positive correlation between ABHD4 mRNA and miRNA-197 (p < 0.000) (Table 3).
Table 3.
Correlation between ABHD4 RNA panel and cardiac troponin among the study groups.
| MiRNA-221 | MiRNA-197 | ABHD4 | FENDRR | Troponin | |||
|---|---|---|---|---|---|---|---|
| Spearman’s rho | miRNA-221-3p | Correlation Coefficient | 1.000 | –0.614 ** | –0.596 ** | 0.678 ** | –0.586 ** |
| Sig. (2-tailed) | 0.000 | 0.000 | 0.000 | 0.000 | |||
| N | 110 | 110 | 110 | 110 | 110 | ||
| miRNA 197-5p | Correlation Coefficient | –0.614 ** | 1.000 | 0.589 ** | –0.586 ** | 0.641 ** | |
| Sig. (2-tailed) | 0.000 | 0.000 | 0.000 | 0.000 | |||
| N | 110 | 110 | 110 | 110 | 110 | ||
| ABHD4 mRNA | Correlation Coefficient | –0.596 ** | 0.589 ** | 1.000 | –0.587 ** | 0.596 ** | |
| Sig. (2-tailed) | 0.000 | 0.000 | 0.000 | 0.000 | |||
| N | 110 | 110 | 110 | 110 | 110 | ||
| FENDRR lncRNA | Correlation Coefficient | 0.678 ** | –0.586 ** | –0.587 ** | 1.000 | –0.643 ** | |
| Sig. (2-tailed) | 0.000 | 0.000 | 0.000 | 0.000 | |||
| N | 110 | 110 | 110 | 110 | 110 | ||
| Cardiac Troponin | Correlation Coefficient | –0.586 ** | 0.641 ** | 0.596 ** | –0.643 ** | 1.000 | |
| Sig. (2-tailed) | 0.000 | 0.000 | 0.000 | 0.000 | |||
| N | 110 | 110 | 110 | 110 | 110 | ||
** Correlation is significant at the 0.01 level (2-tailed).
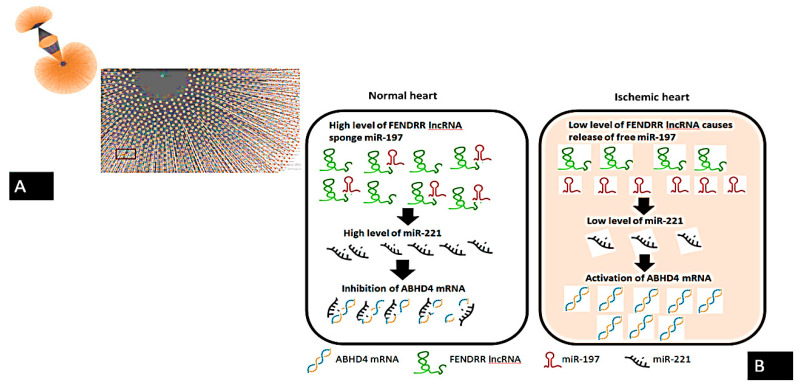
The downregulation of FENDRR lncRNA during ACS results in an increase in the expression of miRNA-197-5p and decrease in the level of miRNA-221-3p, which sequentially activates the ABHD4 mRNA. Results also go in hand with the ontology bioinformatics evidence that (FENDRR lncRNA, miRNA-197-5p, and miRNA-221-3p) networks synergistically regulate the ABHD4 mRNA expression in ACS, and thus shed light on a novel molecular mechanism in myocardial ischemia (Figure 4A,B and Figure 5).
Figure 5.
Summary of the molecular signaling of ABHD4-regulating RNA panel in ACS based on putative interactions: (A) ABHD4 interacting with both hsa-miRNA-221 and hsa-miRNA-197 as retrieved from miRWalk database, (B) Mechanistic signaling of ABHD4-regulating RNA panel in ACS. Based on the interaction between ABHD4 and retrieved RNAs network, we hypothesized that down-regulation of FENDRR lncRNA in ischemic heart results in the release of free miR-197 with subsequent downregulation of miR-221 accompanied with the activation of ABHD4.
4. Discussion
ACS is a main cause of disability and high death rate in developed countries [22], and ACS causes about 1/3 of all deaths in people older than 35 years in western countries [23]. The ECG is an important diagnostic tool in acute coronary syndrome; however, it lacks sensitivity and about 30–50% of patients may initially present symptoms with normal ECG [24]. Creatine kinase MB assessment is not only specific for MI and there are conditions with elevated CK-MB concentrations other than acute coronary syndrome. Several cardiac diseases as cardiac failure and arrhythmia may result in increased CK-MB concentration [25]. On the other hand, using cTn in ACS diagnosis requires careful inspection, as the diagnosis remains inconclusive for about 44% of patients who require additional modalities for diagnosis [26]. Thus, the ongoing search for novel early diagnostic biomarkers for ACS is unstoppable.
Recent studies found that ncRNAs including both miRNAs and lncRNAs are of value in the cardiovascular diseases diagnosis and treatment [27]. Target genes of certain miRNAs are often not validated. Moreover, several in silico predicted target genes may be physiologically irrelevant at lower physiological concentrations, or because of differences in localization between miRNAs and their targets, so we selected a RNA network including target gene, lncRNA, and miRNA to enrich our findings. We aim to evaluate the diagnostic accuracy of ABHD4-regulating RNAs (miRNA-197-5p as a marker of apoptosis; miRNA-221-3p as a marker of inflammatory response, cell adhesion and phospholipid metabolism dysregulation; and FENDRR lncRNA as a marker of myocardial development) for the early detection in patients with unstable angina with troponin level lower than the detection limit and patients who had more than fifty percent coronary artery occlusion. Results indicate that ABHD4-regulating RNAs were significantly dysregulated in UA and STEMI patients compared with healthy controls and that could detect symptomatic unstable angina patients with high sensitivity and specificity, and also estimate the severity of ACS with distinct differential expression in STEMI compared with unstable angina. ABHD4-regulating RNAs retrieval was based on a putative interaction and might be a novel biomarker in ACS.
ABHD4 is a paralog of ABHD5 [36], which is known to regulate lipolysis [37]; it is also known to interact with lipolysis regulatory proteins, to regulate autophagy and to have a role in energy and lipid metabolism [38]. The ABHD subfamily belongs to a large protein family that is characterized by the presence of α/β hydrolase fold [39]. ABHD4 gene is a critical regulator of phospholipid metabolism in mammals [40]. ABHD4 plays a significant role in anoikis resistance [41]. In our study, we reported up regulation of serum ABHD4 expression in ACS group compared with chest pain due to non-cardiac causes and healthy participants groups. To the best of our knowledge, it was first time to report association between ABHD4 mRNA dysregulation and ACS.
Xue et al. found high levels of miRNA-221-3p in blood vessels with atherosclerotic patches [31]. In addition, Coskunpinar et al. reported that miRNA-221-3p expression was deregulated in AMI patients [32]. Jia et al. reported that lower concentration of circulating miRNA-221 was significantly associated with coronary heart disease. In our study, we also reported downregulation of miRNA-221 expression in ACS patients.
miRNA-197 is located on human chromosome 1, with high expression in platelets [18]. miRNA-197 contributes to dyslipidemia associated with metabolic syndrome, resulting in coronary heart diseases [30]. Schulte et al. in a cohort study found that elevated levels of miRNA-197 is predictive of cardiovascular death [41]. Additionally, miRNA-197 was found to be correlated with myocardial fibrosis [32,41,42]. In this study, we reported the upregulation of miRNA-197 expression in ACS group compared with chest pain due to non-cardiac causes and healthy volunteers groups.
FENDRR lncRNA (Foxf1 adjacent noncoding developmental regulatory RNA) is a crucial player in heart development [43]. Çekin et al. declared that FENDRR expression was lower by 7 folds in coronary artery plaques [44]. In our study, we reported downregulation of FENDRR lncRNA expression in ACS group compared with chest pain due to non-cardiac causes and healthy participants groups.
Study limitations include small sample size collected only from one medical facility in Egypt. At the in silico data analysis, it was found that both miRNAs could interact with the selected mRNA and lncRNA with a score > 0.95 at CDS binding site (Supplementary Figures S10 and S11) that showed putative interaction with ABHD4 but there are several mismatches. Mismatches are also visible in the sequence alignment between ABHD4 and lncRNA FENDRR (Supplementary Figures S16–S18). Thus, further in vitro and in vivo studies are still required to confirm our findings.
5. Conclusions
In spite of the availability of cardiac troponin, there is still an urgent demand for novel biomarkers with higher diagnostic accuracy for early detection of ACS patients with troponin levels lower than the detection limit. In summary, ABHD4 regulating RNA panel based on putative interactions (marker of glycerophospholipd metabolism, cell damage, apoptosis, inflammation) and gene expression was assessed in sera samples from patients presented with acute chest pain, and it could (1) detect unstable angina patients and was confirmed by invasive coronary angiography and low troponin level and (2) detect STEMI patients with persistent ST-segment changes and high troponin level. Moreover, ABHD4 regulating RNA panel showed consistent differential gene expression in majority of UA patients and STEMI patients. Thus, it shed light on the underlying molecular mechanism associated with the ABHD4 mRNA panel and its regulatory RNA panel in unstable angina and STEMI patients.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/cells10061512/s1, Figure S1: Gene ontology of ABHD4 mRNA by KEGG map that was retrieved from GeneCards®, Figure S2: Gene expression of ABHD4 mRNA in heart that was retrieved from GeneCards®, Figure S3: Gene expression of ABHD4 mRNA in heart that was retrieved from The Human Protein Atlas database, Figure S4: Gene ontology and expression of ABHD4 mRNA in heart that was retrieved from Enricher tool, Figure S5: Pathway enrichment analysis of miR-197 by KEGG map that was retrieved from GeneCards®, Figure S6: Pathway enrichment analysis of miR-221-3p by KEGG map, Figure S7: Gene expression of miRNA-221-3p in heart that was retrieved from GeneCards®, Figure S8: ABHD4 mRNA is a direct target of miRNA-197-5p that was retrieved from miRWalk database, Figure S9: Alignment between ABHD4 mRNA and miRNA-197-5p that was performed using European bioinformatics institute database, Figure S10: ABHD4 mRNA is a direct target of miRNA-221-3p that was retrieved from miRWalk database, Figure S11: Alignment between ABHD4 mRNA and miRNA-221-3p that was performed using European bioinformatics institute database, Figure S12: Gene expression of FENDRR lncRNA in heart that was retrieved from GeneCards®, Figure S13: Gene expression of FENDRR lncRNA in heart that was retrieved from Enricher tool database, Figure S14: FENDRR lncRNA detailed isoform that was retrieved from LNCipedia database, Figure S15: FENDRR lncRNA structure that was retrieved from Lnc2atlas database, Figure S16: Alignment between ABHD4 mRNA and FENDRR lncRNA that was performed using European bioinformatics institute database, Figure S17: Alignment between hsa-miRNA-221-3p and FENDRR lncRNA that was performed using European bioinformatics institute database, Figure S18: Alignment between hsa-miRNA-221-3p and FENDRR lncRNA that was performed using LncTar, Figure S19: Alignment between hsa-miRNA-197-5p and FENDRR lncRNA that was performed using European bioinformatics institute database, Figure S20: Alignment between hsa-miRNA-197-5p and FENDRR lncRNA that was performed using LncTar, Table S1: Study population demographic and clinical characteristics.
Author Contributions
Study design, methodology, data analysis, drafting, and supervision was done by S.H.A.A. and M.M. M.S. shared in conceptualization, study design, data analysis, bioinformatic analysis, drafting and supervision. M.S.E.M. and H.E. shared in fund acquisition. S.S.E., M.S., A.M.A.E. and R.S. shared in methodology, statistical analysis, drafting and data collection. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by Academy of Science and Technology (ASRT), Jesor call 2018, Project ID: jesor_20173054.
Institutional Review Board Statement
The study was approved by the Ain Shams Research Ethics Committee, Faculty of Medicine, Egypt, dated 13/5/2019, FWA 000017585 in accordance to the guidelines of the Declaration of Helsinki.
Informed Consent Statement
Informed consent was taken from all participants involved in the study.
Data Availability Statement
The data reported in this study are available on request from the corresponding authors.
Conflicts of Interest
All the authors have no conflict of interest to disclose.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Moran A.E., Tzong K.Y., Forouzanfar M.H., Roth G.A., Mensah G.A., Ezzati M., Murray C.J., Naghavi M. Variations in ischemic heart disease burden by age, country, and income: The Global Burden of Diseases, Injuries, and Risk Factors 2010 study. Glob. Heart. 2014;9:91–99. doi: 10.1016/j.gheart.2013.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Windecker S. ESC Committee for Practice Guidelines: Providing knowledge to everyday clinical practice. Cardiovasc. Res. 2020;116:e146–e148. doi: 10.1093/cvr/cvaa154. [DOI] [PubMed] [Google Scholar]
- 3.Barnett K., Mercer S.W., Norbury M., Watt G., Wyke S., Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet. 2012;380:37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 4.White H.D., Chew D.P. Acute myocardial infarction. Lancet. 2008;372:570–584. doi: 10.1016/S0140-6736(08)61237-4. [DOI] [PubMed] [Google Scholar]
- 5.Thygesen K., Alpert J.S., White H.D., Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. Eur. Heart J. 2007:2525–2538. doi: 10.1093/eurheartj/ehm355. [DOI] [PubMed] [Google Scholar]
- 6.Suzuki K., Komukai K., Nakata K., Kang R., Oi Y., Muto E., Kashiwagi Y., Tominaga M., Miyanaga S., Ishikawa T., et al. The Usefulness and Limitations of Point-of-care Cardiac Troponin Measurement in the Emergency Department. Intern. Med. 2018;57:1673–1680. doi: 10.2169/internalmedicine.0098-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jaffe A.S., Ravkilde J., Roberts R., Naslund U., Apple F.S., Galvani M., Katus H. It’s time for a change to a troponin standard. Circulation. 2000;102:1216–1220. doi: 10.1161/01.CIR.102.11.1216. [DOI] [PubMed] [Google Scholar]
- 8.Piccioni A., Valletta F., Zanza C., Esperide A., Franceschi F. Novel biomarkers to assess the risk for acute coronary syndrome: Beyond troponins. Intern. Emerg. Med. 2020;15:1193–1199. doi: 10.1007/s11739-020-02422-z. [DOI] [PubMed] [Google Scholar]
- 9.Piccioni A., de Cunzo T., Valletta F., Covino M., Rinninella E., Raoul P., Zanza C., Mele M.C., Franceschi F. Gut Microbiota and Environment in Coronary Artery Disease. Int. J. Environ. Res. Public Health. 2021;18:4242. doi: 10.3390/ijerph18084242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu J., Wang L., Harvey-White J., Huang B.X., Kim H.Y., Luquet S., Palmiter R.D., Krystal G., Rai R., Mahadevan A., et al. Multiple pathways involved in the biosynthesis of anandamide. Neuropharmacology. 2008;54:1–7. doi: 10.1016/j.neuropharm.2007.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nardini M., Dijkstra B.W. Alpha/beta hydrolase fold enzymes: The family keeps growing. Curr. Opin. Struct. Biol. 1999;9:732–737. doi: 10.1016/S0959-440X(99)00037-8. [DOI] [PubMed] [Google Scholar]
- 12.Lord C.C., Thomas G., Brown J.M. Mammalian alpha beta hydrolase domain (ABHD) proteins: Lipid metabolizing enzymes at the interface of cell signaling and energy metabolism. Biochim. Biophys. Acta. 2013;1831:792–802. doi: 10.1016/j.bbalip.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Emirkan A., van Duijn C.M., Ugocsai P., Isaacs A., Pramstaller P.P., Liebisch G., Wilson J.F., Johansson A., Rudan I., Aulchenko Y.S., et al. Genome-wide association study identifies novel loci associated with circulating phospho- and sphingolipid concentrations. PLoS Genet. 2012;8:e1002490. doi: 10.1371/journal.pgen.1002490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jensen M.K., Rimm E.B., Rader D., Schmidt E.B., Sørensen T.I., Vogel U., Overvad K., Mukamal K.J. S447X variant of the lipoprotein lipase gene, lipids, and risk of coronary heart disease in 3 prospective cohort studies. Am. Heart J. 2009;157:384–390. doi: 10.1016/j.ahj.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kurano M., Kano K., Dohi T., Matsumoto H., Igarashi K., Nishikawa M., Ohkawa R., Ikeda H., Miyauchi K., Daida H., et al. Different origins of lysophospholipid mediators between coronary and peripheral arteries in acute coronary syndrome. J. Lipid Res. 2017;58:433–442. doi: 10.1194/jlr.P071803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ohkawa R., Kurano M., Sakai N., Kishimoto T., Nojiri T., Igarashi K., Hosogaya S., Ozaki Y., Dohi T., Miyauchi K., et al. Measurement of plasma choline in acute coronary syndrome: Importance of suitable sampling conditions for this assay. Sci. Rep. 2018;8:4725. doi: 10.1038/s41598-018-23009-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gaudet P., Livstone M.S., Lewis S.E., Thomas P.D. Phylogenetic-based propagation of functional annotations within the Gene Ontology consortium. Brief Bioinform. 2011;12:449–462. doi: 10.1093/bib/bbr042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee H.C., Simon G.M., Cravatt B.F. ABHD4 regulates multiple classes of N-acyl phospholipids in the mammalian central nervous system. Biochemistry. 2015;54:2539–2549. doi: 10.1021/acs.biochem.5b00207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vickers K.C., Rye K.A., Tabet F. MicroRNAs in the onset and development of cardiovascular disease. Clin. Sci. 2014;126:183–194. doi: 10.1042/CS20130203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wen Z., Zheng S., Zhou C., Yuan W., Wang J., Wang T. Bone marrow mesenchymal stem cells for post-myocardial infarction cardiac repair: Micrornas as novel regulators. J. Cell. Mol. Med. 2012;16:657–671. doi: 10.1111/j.1582-4934.2011.01471.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meder B., Keller A., Vogel B., Haas J., Sedaghat-Hamedani F., Kayvanpour E., Just S., Borries A., Rudloff J., Leidinger P., et al. MicroRNA signatures in total peripheral blood as novel biomarkers for acute myocardial infarction. Basic Res. Cardiol. 2011;106:13–23. doi: 10.1007/s00395-010-0123-2. [DOI] [PubMed] [Google Scholar]
- 22.Zhong J., He Y., Chen W., Shui X., Chen C., Lei W. Circulating microRNA-19a as a potential novel biomarker for diagnosis of acute myocardial infarction. Int. J. Mol. Sci. 2014;15:20355–20364. doi: 10.3390/ijms151120355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hong Q., Li O., Zheng W., Xiao W.Z., Zhang L., Wu D., Cai G.Y., He J.C., Chen X.M. LncRNA HOTAIR regulates HIF-1 α/AXL signaling through inhibition of miR-217 in renal cell carcinoma. Cell Death Dis. 2017;8:e2772. doi: 10.1038/cddis.2017.181. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 24.Li X., Zhou J., Huang K. Inhibition of the lncRNA Mirt1 attenuates acute myocardial infarction by suppressing NF-κB activation. Cell. Physiol. Biochem. 2017;42:1153–1164. doi: 10.1159/000478870. [DOI] [PubMed] [Google Scholar]
- 25.Li X., Dai Y., Yan S., Shi Y., Han B., Li J., Cha L., Mu J. Down-regulation of lncRNA KCNQ1OT1 protects against myocardial ischemia/reperfusion injury following acute myocardial infarction. Biochem. Biophys. Res. Commun. 2017;491:1026–1033. doi: 10.1016/j.bbrc.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 26.Vausort M., Wagner D.R., Devaux Y. Long noncoding RNAs in patients with acute myocardial infarction. Circ. Res. 2014;115:668–677. doi: 10.1161/CIRCRESAHA.115.303836. [DOI] [PubMed] [Google Scholar]
- 27.Roger V.L. Epidemiology of myocardial infarction. Med. Clin. N. Am. 2007;91:537–552. doi: 10.1016/j.mcna.2007.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jenkins C.M., Mancuso D.J., Yan W., Sims H.F., Gibson B., Gross R.W. Identification, cloning, expression, and purification of three novel human calcium-independent phospholipase A2 family members possessing triacylglycerol lipase and acylglycerol transacylase activities. J. Biol. Chem. 2004;279:48968–48975. doi: 10.1074/jbc.M407841200. [DOI] [PubMed] [Google Scholar]
- 29.Yu L., Li Y., Grisé A., Wang H. Lipid Transfer in Lipoprotein Metabolism and Cardiovascular Disease. Springer; Singapore: 2020. CGI-58: Versatile Regulator of Intracellular Lipid Droplet Homeostasis; pp. 197–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Simpson C.D., Hurren R., Kasimer D., MacLean N., Eberhard Y., Ketela T., Moffat J., Schimmer A.D. A genome wide shRNA screen identifies α/β hydrolase domain containing 4 (ABHD4) as a novel regulator of anoikis resistance. Apoptosis. 2012;17:666–678. doi: 10.1007/s10495-012-0723-4. [DOI] [PubMed] [Google Scholar]
- 31.Xue Y., Wei Z., Ding H., Wang Q., Zhou Z., Zheng S., Zhang Y., Hou D., Liu Y., Zen K., et al. MicroRNA-19b/221/222 induces endothelial cell dysfunction via suppression of PGC-1α in the progression of atherosclerosis. Atherosclerosis. 2015;241:671–681. doi: 10.1016/j.atherosclerosis.2015.06.031. [DOI] [PubMed] [Google Scholar]
- 32.Coskunpinar E., Cakmak H.A., Kalkan A.K., Tiryakioglu N.O., Erturk M., Ongen Z. Circulating miR-221-3p as a novel marker for early prediction of acute myocardial infarction. Gene. 2016;591:90–96. doi: 10.1016/j.gene.2016.06.059. [DOI] [PubMed] [Google Scholar]
- 33.Willeit P., Zampetaki A., Dudek K., Kaudewitz D., King A., Kirkby N.S., Crosby-Nwaobi R., Prokopi M., Drozdov I., Langley S.R., et al. Circulating microRNAs as novel biomarkers for platelet activation. Circ. Res. 2013;112:595–600. doi: 10.1161/CIRCRESAHA.111.300539. [DOI] [PubMed] [Google Scholar]
- 34.Karolina D.S., Tavintharan S., Armugam A., Sepramaniam S., Pek S.L., Wong M.T., Lim S.C., Sum C.F., Jeyaseelan K. Circulating miRNA profiles in patients with metabolic syndrome. J. Clin. Endocrinol. Metab. 2012;97:E2271–E2276. doi: 10.1210/jc.2012-1996. [DOI] [PubMed] [Google Scholar]
- 35.Nichols M., Townsend N., Scarborough P., Rayner M. Cardiovascular disease in Europe 2014: Epidemiological update. Eur. Heart J. 2014;35:2950–2959. doi: 10.1093/eurheartj/ehu299. [DOI] [PubMed] [Google Scholar]
- 36.Gibler W.B., Lewis L.M., Erb R.E., Makens P.K., Kaplan B.C., Vaughn R.H., Biagini A.V., Blanton J.D., Campbell W.B. Early detection of acute myocardial infarction in patients presenting with chest pain and nondiagnostic ECGs: Serial CK-MB sampling in the emergency department. Ann. Emerg. Med. 1990;19:1359–1366. doi: 10.1016/S0196-0644(05)82598-3. [DOI] [PubMed] [Google Scholar]
- 37.Pierce G.F., Jaffe A.S. Increased creatine kinase MB in the absence of acute myocardial infarction. Clin. Chem. 1986;32:2044–2051. [PubMed] [Google Scholar]
- 38.Katus H., Ziegler A., Ekinci O., Giannitsis E., Stough W.G., Achenbach S., Blankenberg S., Brueckmann M., Collinson P., Comaniciu D., et al. Early diagnosis of acute coronary syndrome. Eur. Heart J. 2017;38:3049–3055. doi: 10.1093/eurheartj/ehx492. [DOI] [PubMed] [Google Scholar]
- 39.Poller W., Dimmeler S., Heymans S., Zeller T., Haas J., Karakas M., Leistner D.M., Jakob P., Nakagawa S., Blankenberg S., et al. Non-coding RNAs in cardiovascular diseases: Diagnostic and therapeutic perspectives. Eur. Heart J. 2018;39:2704–2716. doi: 10.1093/eurheartj/ehx165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vieyres G., Reichert I., Carpentier A., Vondran F.W., Pietschmann T. The ATGL lipase cooperates with ABHD5 to mobilize lipids for hepatitis C virus assembly. PLoS Pathog. 2020;16:e1008554. doi: 10.1371/journal.ppat.1008554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schulte C., Molz S., Appelbaum S., Karakas M., Ojeda F., Lau D.M., Hartmann T., Lackner K.J., Westermann D., Schnabel R.B., et al. miRNA-197 and miRNA-223 predict cardiovascular death in a cohort of patients with symptomatic coronary artery disease. PLoS ONE. 2015;10:e0145930. doi: 10.1371/journal.pone.0145930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu W., Zheng J., Dong J., Bai R., Song D., Ma X., Zhao L., Yao Y., Zhang H., Liu T. Association of miR-197-5p, a circulating biomarker for heart failure, with myocardial fibrosis and adverse cardiovascular events among patients with stage C or D heart failure. Cardiology. 2018;141:212–225. doi: 10.1159/000493419. [DOI] [PubMed] [Google Scholar]
- 43.Grote P., Herrmann B.G. The long non-coding RNA Fendrr links epigenetic control mechanisms to gene regulatory networks in mammalian embryogenesis. RNA Biol. 2013;10:1579–1585. doi: 10.4161/rna.26165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Çekin N., Özcan A., Göksel S., Arslan S., Pınarbaşı E., Berkan Ö. Decreased FENDRR and LincRNA-p21 expression in atherosclerotic plaque. Anatol. J. Cardiol. 2018;19:131. doi: 10.14744/AnatolJCardiol.2017.8081. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data reported in this study are available on request from the corresponding authors.